- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games

Traveling while pregnant: Your complete guide
Unless you're nearing your due date or have certain complications, your healthcare provider will generally give you the green light for pregnancy travel. Here's how to safely explore – plus what to consider before making plans.

Is traveling while pregnant safe?
When to avoid pregnancy travel, when is the best time to travel while you're pregnant , can pregnant women travel during covid, when should you stop traveling while pregnant, your pregnancy travel checklist, when to call your doctor while traveling.
Yes, it's generally safe to travel during pregnancy as long as you're not too close to your due date and you're not experiencing any serious pregnancy complications. There are special precautions to take, of course, and you may find yourself stopping to use the bathroom more than you're used to, but that babymoon can be within reach.
Before you pack your suitcase, talk with your healthcare provider to make sure it’s safe for you to travel and that your destination is a good choice. You'll want to avoid places where infectious diseases are prevalent (or there are high outbreaks of Zika or malaria, for example). The COVID-19 pandemic has made people reconsider where they feel safe traveling as well; if you're fully vaccinated, the CDC says you can travel Opens a new window , but it's always best to check with your doctor first.
And bear in mind that the activities you take part in might be different than normal – you'll want to skip the Scuba diving lessons, for example (though snorkeling is okay!).
It's safe to fly when you're pregnant as well, and most airlines will allow you to fly domestically until about 36 weeks of pregnancy. International routes may have different rules, so be sure to check with your airline before booking anything. Your doctor will tell you to avoid flying, however, if you have a health concern that might require emergency care or any other health conditions that aren’t well controlled.
It's best to avoid traveling while pregnant if you have any health conditions that can be life-threatening to both you or your baby. If you have any of the following conditions, your doctor will almost certainly advise you against travel:
- Placental abruption
- Preeclampsia
- You're in preterm or active labor
- Cervical insufficiency (incompetent cervix)
- Premature rupture of membranes (PROM)
- A suspected ectopic pregnancy
- Vaginal bleeding
You might also need to be extra-cautious or skip travel if you're experiencing intrauterine growth restriction , you have placenta previa , or you have other conditions that may place your pregnancy at a higher risk. It’s always a good idea to discuss your concerns with your healthcare provider before travel regarding any medical conditions you have, and they'll be able to advise you on what's best, depending on the trip.
The sweet spot for pregnancy travel is during your second trimester , between 14 weeks and 27 weeks. By the second trimester, any struggles you’ve had with morning sickness and fatigue during the earlier weeks of pregnancy should have hopefully subsided – and after 12 weeks, your risk of miscarriage decreases significantly as well. And you're not too far along to worry about third trimester exhaustion or going into preterm labor yet, either.
Your energy levels are likely to be good during your second trimester too (bring on the sightseeing!), and it will still be relatively easy and comfortable for you to travel and move around at this time. Keep in mind that once you hit that third trimester, pregnancy travel might be more difficult as you find it harder to move around and stay still for long periods of time.
It's complicated (and often a personal decision based on your own risk factors), but the CDC says that if you're fully vaccinated against COVID-19, you can travel. Of course, it's important you still do everything you can to keep yourself and others around you safe, including following all mask-wearing and social distancing guidelines in the destination you visit.
Women are at an increased risk for severe illness if they contract COVID-19 while pregnant , and they're more likely to experience preterm birth and other poor pregnancy outcomes. (This is why the CDC, the American College of Obstetricians and Gynecologists, and the Society for Maternal-Fetal Medicine all recommend that women who are pregnant, breastfeeding, or are planning on becoming pregnant get the COVID vaccine .)
If you're vaccinated and decide to travel, the CDC advises avoiding international destinations that are designated Level 4, due to high rates of local COVID-19 transmission.
Take all this information into account and talk to your doctor before you decide on where and when to travel while you're pregnant. And if you experience any symptoms of COVID-19, whether while traveling or at home, call your healthcare provider as soon as possible.
The guidelines for when to stop traveling while you're pregnant vary based on your mode of travel, but more or less, you should wrap up travel before you're 36 weeks pregnant.
Most airlines will let pregnant women fly domestically until they're 36 weeks pregnant – and many cut that off earlier for international travel. This rule is often enforced on an honor system policy, but some airlines may ask for a doctor’s note – so make sure you have that from your healthcare provider if you're traveling in the third trimester, just in case.
Most cruise ships don't allow travel after 24 weeks of pregnancy. Some cruise lines' cutoff dates vary, so verify policies before booking a cruise.
As for road trips, there's no official deadline for when you need to stop traveling, but your personal comfort level (physically and emotionally) – and your doctor's advice – might help you decide. You can drive while pregnant all the way up until your due date, but things may get considerably less comfortable on longer trips as you approach full term.
Travel of any kind requires advance preparation, but when you're pregnant and traveling, that pre-trip checklist gets a little longer. Give yourself a little more time than usual to plan for a trip – and use the tips below to stay safe and comfortable on your next adventure.
Before you travel
- Talk to your healthcare provider to determine if your trip is safe for you and if there are any medical concerns to consider. It's a good idea to discuss any activities you plan to do while you're away too. If you're planning an international trip, make sure to ask about any vaccines you may need for the areas you're visiting.
- Make sure you know your prenatal test schedule. Plan travels around any prenatal tests you need to schedule, including ultrasounds and other important screening tests.
- Book an aisle seat. You'll likely be more comfortable being able to get up to stretch or go to the bathroom on longer flights.
- Buy travel insurance. You don't need special travel insurance when you're pregnant, but it's never a bad idea to secure a policy. You may want to consider one with a “cancel for any reason” clause that reimburses you for money lost on cancelled trips for reasons (read: any reason) beyond what’s listed on the base policy. Check with your personal health insurance, too, to make sure it covers potential pregnancy complications while traveling internationally (some don’t). Consider adding evacuation insurance as part of a travel insurance plan, too.
- Gather your medical records and health information . If you’re in your second or third trimester, ask your ob-gyn or midwife for a digital copy of your prenatal chart, and have that easily accessible during your trip. Typically, this chart includes your age, your blood type, the name and contact information for your healthcare provider, the date of your last menstrual period, your due date, information about any prior pregnancies, your risk factors for disease, results of pregnancy-related lab tests (including ultrasounds or other imaging tests), your medical and surgical history, and a record of vital signs taken at each visit.
- Keep a list of key names and numbers you may need in the event of an emergency saved on your phone and written on a piece of paper (in case your battery dies).
- Have a contingency plan for doctors and hospitals that will take your insurance where you're going in case you go into labor early or experience pregnancy complications that require urgent care while you're away from home.
- Pack medicines and prenatal vitamins. That might include an extended supply of prescriptions and over-the-counter remedies , too. Bring enough to cover your entire trip and a written prescription that you can fill if you lose anything. It's a good idea to keep prescription medicine in its original container, so if your bags are searched it will be clear that you're not using medication without a prescription.
- Prepare for the unexpected. On a road trip, that might mean an unexpected breakdown, so join an auto club that provides roadside assistance. Download any apps you use for renting cars and accessing boarding passes before you leave so you can easily reschedule things in the event of a last-minute cancellation.
- If you're flying during your third trimester, be sure to call the airline to check about the cutoff week for pregnancy travel. A note from your doctor that says you’re cleared to travel is always good to have when traveling during your third trimester.
During your trip
- Drink plenty of water and continue to eat healthy foods . Keep in mind that many restaurants abroad commonly serve unpasteurized foods (like soft cheeses and milk), which can be dangerous for pregnant women due to the presence of listeria.
- Avoid eating raw or undercooked meat or fish , drinks with ice (which may be contaminated), non-bottled water, and other foods that can cause traveler's diarrhea, which can be more of a problem for pregnant women than other people.
- On long flights and drives, take time to stretch by pulling over for a walk or strolling up and down the airplane aisle. And when seated, always wear your seat belt .
- Maternity compression socks are handy to have along – both in transit and worn under your clothes while you’re out and about exploring – because they can ease the symptoms of swollen feet and legs. These are a few of our favorite pregnancy compression socks .
- Take advantage of help. Many countries have dedicated lines in shops and airports for pregnant travelers, so don't feel any shame taking a shorter wait if you see one.
- Go easy on yourself. Remember, you're growing a baby. You might not have quite the stamina for sightseeing and late nights like you used to pre-pregnancy. Make the most of your vacation but don't fret you miss out on things because you need more downtime from exploring than you usually would.
- Don’t forget to get photos of your bump. When your baby is older, you'll have fun showing them all the places you traveled with them before they were born.
- Go for the comfy shoes. Travel during pregnancy is the best reason ever to forgo those strappy stilettos for your favorite sneakers .
- Pack snacks so you always have something to curb your appetite if there’s a long wait for a restaurant or you get stuck in transit or someplace remote with no food offerings.
- Try to be in the moment with your travel partners as much as possible. Once your baby is born, your attention will be pulled in a whole new direction.
If you have any medical concerns traveling while pregnant, don’t hesitate to pick up the phone and call your doctor for advice. The below are a few symptoms that definitely warrant calling your ob-gyn or health care provider or seeking emergency care while traveling or at home:
- Signs of pre-term labor (including a constant, low dull backache, bleeding, etc.)
- Ruptured membranes (your water breaks)
- Severe cramping
- Spiking blood pressure
- Severe nausea or vomiting
- COVID-19 symptoms
Was this article helpful?
Is it safe to fly while I'm pregnant?

Best compression socks for pregnancy

Is it safe to travel to high altitudes while pregnant?

When can I travel again after giving birth?

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
AAFP. 2020. Ultrasound during pregnancy. American Academy of Family Physicians. https://familydoctor.org/ultrasound-during-pregnancy/ Opens a new window [Accessed April 2023]
ACOG. 2020. FAQ055: Travel during pregnancy. American College of Obstetricians and Gynecologists. https://www.acog.org/womens-health/faqs/travel-during-pregnancy Opens a new window [Accessed April 2023]
CDC. 2019. Pregnant Travelers. https://wwwnc.cdc.gov/travel/yellowbook/2020/family-travel/pregnant-travelers Opens a new window [Accessed April 2023]
CDC. 2022. Domestic Travel During Covid-19. https://www.cdc.gov/coronavirus/2019-ncov/travelers/travel-during-covid19.html Opens a new window [Accessed April 2023]
CDC 2023. International Travel During Covid-19. https://www.cdc.gov/coronavirus/2019-ncov/travelers/international-travel-during-covid19.html Opens a new window [Accessed April 2023]
CDC. 2022. Covid-19: Pregnant and Recently Pregnant People. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/pregnant-people.html Opens a new window [Accessed April 2023]

Terry Ward is a freelance travel, health, and parenting writer who has covered everything from flying with toddlers to why you should travel with your kids even when they're too young to remember it. She lives in Tampa, Florida, with her husband and their young son and daughter, and enjoys camping, sailing, scuba diving, skiing, and almost anything else done in the great outdoors.
Where to go next

Coronavirus (COVID-19): Latest Updates | Visitation Policies Visitation Policies Visitation Policies Visitation Policies Visitation Policies | COVID-19 Testing | Vaccine Information Vaccine Information Vaccine Information
Health Encyclopedia
International travel while pregnant or breastfeeding, special considerations for traveling while pregnant.
Traveling during pregnancy is normal, and a lot of women do it. But it's important to think about potential problems that could come up during international travel. Also think about how you would get quality healthcare in the countries you are visiting. Get all of the vaccines you need before becoming pregnant instead of waiting to get them during pregnancy.
The American College of Obstetricians and Gynecologists says the safest time for a woman to travel is in the second trimester of her pregnancy, from 14 to 28 weeks. This is the time when you will feel your best. You are also at the lowest risk for spontaneous abortion (miscarriage) or premature labor. During the third trimester (28 to 40 weeks), many healthcare providers and midwives advise staying within a 300-mile radius of home because of potential problems, such as high blood pressure, phlebitis, and false or preterm labor. Generally, women are not allowed to travel by air after 36 weeks for domestic travel, and after 28 to 35 weeks for international travel. The decision on whether to travel and how far to travel at any time during pregnancy should be a joint decision between you and your healthcare provider.
For most pregnant women, flying does not pose a risk to the fetus from cosmic radiation. But aircrew and women who often fly may exceed radiation limits.
According to the CDC, pregnant women with the following conditions may be advised against traveling to countries that need pretravel vaccines. This list may be incomplete. So discuss your health history with your provider or midwife before planning travel:
History of miscarriage
Incompetent cervix
History of ectopic pregnancy
History of premature labor or premature rupture of membranes
History of or current placental abnormalities
Threatened miscarriage or vaginal bleeding during current pregnancy
Multiple fetuses in current pregnancy
History of pre-eclampsia, high blood pressure, or diabetes with any pregnancy
History of infertility or trouble getting pregnant
Pregnancy for the first time over the age of 35 years
Heart valve disease or congestive heart failure
History of blood clots
Severe anemia
Chronic organ system problems that need to be treated
You may also be advised against traveling to places that may have hazards. The list below may be incomplete. Talk about your travel plans with your healthcare provider or midwife before planning a trip.
Places with high altitudes
Places that have outbreaks of life-threatening food- or insect-borne infections
Places where malaria is common
Places where live-virus vaccines are needed or recommended
Healthy tips for traveling while pregnant
Here are tips for traveling while pregnant:
Try to plan ahead for any problems or emergencies that could come up before you travel. Check that your health insurance is valid while you are abroad. Also check to see whether the plan will cover a newborn, should you deliver while away. You may want to think about getting a supplemental travel and medical evacuation insurance.
Research medical facilities in your destination. Women in the last trimester of pregnancy should look for places that can manage complications of pregnancy, pre-eclampsia, and cesarean sections.
If you will need prenatal care while you are abroad, arrange for this before you leave. Talk with your healthcare provider or midwife to figure out the best way to handle this.
Know your blood type and check that blood is screened for HIV and hepatitis B in the areas you will be visiting.
Check that safe food and beverages, such as bottled water and pasteurized milk, are available at your destinations.
If flying, ask for an aisle seat at the bulkhead. This gives you the most space and comfort. If morning sickness is a problem, try to arrange travel during a time of day when you generally feel well. Seats over the wing in the midplane region will give you the smoothest ride.
Try to walk every half-hour during a smooth flight. Flex and extend your ankles often to prevent blood clots in the veins (thrombophlebitis).
Fasten your seat belt at the pelvis level, below your hips.
Drink plenty of fluids to stay hydrated. Aircraft cabins have low humidity.
Try to rest as much as possible while away. Exercise and activity during pregnancy are important but try not to overdo it.
Special considerations for traveling while breastfeeding
Breastfeeding gives babies the most nutritional start in life. It also gives them vital protection against certain infections. But traveling internationally while nursing can be challenging.
If you are breastfeeding only, you don't have to worry about sterilizing bottles or having clean water. You may get vaccines to protect against disease, depending on where you are traveling. But diseases such as yellow fever, measles, and meningococcal meningitis may be a threat to infants who can't be vaccinated at birth. Discuss this with both your healthcare provider and your infant's caregiver before you travel.
If you are feeding your baby formula, it's best to use powdered formula made with boiled water. You may also want to carry a supply of prepared infant formula in cans or ready-to-feed bottles for emergencies.
Breastfeeding helps lower the chance of your baby getting traveler's diarrhea. If you get traveler's diarrhea, drink more fluids and continue to nurse your baby.
Watch your eating and sleeping patterns, as well as your stress levels. This will affect your milk output. Drink more fluids. Stay away from alcohol and caffeine, as well as exposure to smoke.
If you are traveling without your infant, you will need to pump to maintain your milk supply. Check with TSA about transporting your milk on flights.
Medical Reviewers:
- Donna Freeborn PhD CNM FNP
- Heather M Trevino BSN RNC
- Michele Burtner CNM
- Ask a Medical Librarian Make an Appointment Patient Education Medline Plus: Pregnancy
Appointments at Mayo Clinic
- Pregnancy week by week
Is it safe to fly during pregnancy?
Generally, air travel before 36 weeks of pregnancy is considered safe for people who aren't dealing with any pregnancy problems. Still, if you're pregnant, it's a good idea to talk with your health care provider before you fly.
Your provider might suggest that you not fly if you have certain pregnancy complications that could get worse because of air travel or that could require emergency care. Examples include a history of miscarriage or vaginal bleeding, severe anemia, and high blood pressure or diabetes that's not well controlled. If you had preeclampsia during a previous pregnancy — a condition that causes high blood pressure and extra protein in urine — flying may not be advised. The same is true if you're pregnant with twins or other multiples.
Tell your provider how far you are flying, as the length of the flight might make a difference. Also, be aware that some airlines may not allow pregnant people on international flights. Check with your airline before you make travel arrangements.
After 36 weeks of pregnancy, your health care provider may advise against flying. And some airlines don't allow pregnant people to fly after 36 weeks. The airline also may require a letter from your health care provider that states how far along in your pregnancy you are and whether flying is advised.
If your health care provider says it's okay for you to fly, and your plans are flexible, the best time to travel by air might be during the second trimester. The risks of common pregnancy emergencies are lowest during that time.
When you fly:
- Buckle up. During the trip, keep your seatbelt fastened when you are seated, and secure it under your belly.
- Drink plenty of fluids. Low humidity in the airplane could cause you to become dehydrated.
- Avoid gassy foods and drinks before you fly. Gases expand during flight, and that could make you uncomfortable. Examples of foods and drinks to avoid include broccoli and carbonated soda.
- Think about medical care. Plan for how you'll get obstetric care during your trip if you need it. Bring copies of your medical information in case you need care while you're away.
Blood clots
Air travel can raise the risk for blood clots in the legs, a condition called venous thrombosis. The risk is higher for pregnant people. Moving your legs may help prevent this problem. Take a walk up and down the aisle every hour during the flight. If you must remain seated, flex and extend your ankles from time to time. In general, it's best to avoid tightfitting clothing, as that can hinder blood flow. Wearing compression stockings can help with blood circulation during a long flight.
Radiation exposure linked to air travel at high altitudes isn't thought to be a problem for most people who fly during pregnancy. But pilots, flight attendants and others who fly often might be exposed to a level of radiation that raises concerns during pregnancy. If you must fly frequently during your pregnancy, talk about it with your health care provider.
Mary Marnach, M.D.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Allergy medications during pregnancy
- AskMayoExpert. Health considerations for air travelers: Pregnancy considerations. Mayo Clinic; 2022.
- Air Travel During Pregnancy: ACOG Practice Bulletin No. 746. American College of Obstetricians and Gynecologists. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/08/air-travel-during-pregnancy. Accessed Dec. 1, 2022.
- Ram S, et al. Air travel during pregnancy and the risk of venous thrombosis. American Journal of Obstetrics and Gynecology. 2022; doi:10.1016/j.ajogmf.2022.100751.
Products and Services
- A Book: Taking Care of You
- A Book: Obstetricks
- Available Solutions for Prenatal Nutrition from Mayo Clinic Store
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- Ankle swelling during pregnancy
- Antibiotics and pregnancy
- Aspirin during pregnancy
- Pregnancy back pain
- Falling during pregnancy: Reason to worry?
- Fetal ultrasound
- Flu shot in pregnancy
- Headaches during pregnancy: What's the best treatment?
- Iron deficiency anemia during pregnancy: Prevention tips
- Leg cramps during pregnancy
- Pregnancy acne
- Pregnancy and fish
- Pregnancy constipation
- Pregnancy diet: Essential nutrients
- Pregnancy due date calculator
- Pregnancy exercises
- Pregnancy nutrition don'ts
- Pregnancy stretches
- Pregnancy weight gain
- Pregnant. Now What Happens?
- Prenatal testing
- Prenatal vitamins and pregnancy
- Sex during pregnancy
- Twin pregnancy
- Vaccines during pregnancy
- Vaping during pregnancy
- Working during pregnancy
- X-ray during pregnancy
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Expert Answers
- Air travel during pregnancy Is it safe
Let’s celebrate our doctors!
Join us in celebrating and honoring Mayo Clinic physicians on March 30th for National Doctor’s Day.
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
- Section 6 - Medical Tourism
- Section 7 - Travel & Breastfeeding
Pregnant Travelers
Cdc yellow book 2024.
Author(s): Romeo Galang, I. Dale Carroll, Titilope Oduyebo
- The Pretravel Consultation
Infectious Disease Concerns
Environmental health concerns, transportation considerations.
Pregnancy can cause physiologic changes that require special consideration during travel. With careful preparation, however, most pregnant people can travel safely.
Pretravel Consultation
The pretravel consultation and evaluation of pregnant travelers ( Box 7-01 ) should begin with a careful medical and obstetric history, specifically assessing gestational age and the presence of factors and conditions that increase risk for adverse pregnancy outcomes. A visit with an obstetric health care provider also should be a part of the pretravel assessment to ensure routine prenatal care and identify any potential problems. Instruct pregnant travelers to carry with them a copy of their prenatal records and physician’s contact information.
Review the pregnant person’s travel itinerary, including accommodations, activities, and destinations, to guide pretravel health advice. Discourage pregnant travelers from undertaking unaccustomed vigorous activity. Swimming and snorkeling during pregnancy generally are safe, but falls during waterskiing have been reported to inject water into the birth canal. Most experts advise against scuba diving for pregnant people because of risk for fetal gas embolism during decompression (see Sec. 4, Ch. 4, Scuba Diving: Decompression Illness & Other Dive-Related Injuries ). Riding animals, bicycles, or motorcycles presents risks for abdominal trauma.
Educate pregnant people on how to avoid travel-associated risks, manage minor pregnancy discomforts, and recognize more serious complications. Advise pregnant people to seek urgent medical attention if they experience contractions or premature labor; symptoms of deep vein thrombosis (e.g., unusual leg swelling and pain in the calf or thigh) or pulmonary embolism (e.g., unusual shortness of breath); dehydration, diarrhea, or vomiting; severe pelvic or abdominal pain; symptoms of preeclampsia (e.g., severe headaches, nausea and vomiting, unusual swelling, vision changes); prelabor rupture of the membranes; or vaginal bleeding.
Box 7-01 Pretravel consultation for pregnant travelers: a checklist for health care providers
☐ Review vaccination history (e.g., COVID-19, hepatitis A, hepatitis B, measles, pertussis, rubella, varicella, tetanus) and update vaccinations as needed (see text for contraindications during pregnancy)
☐ Policies and paperwork
- Discuss supplemental travel insurance, travel health insurance, and medical evacuation insurance; research specific coverage information and limitations for pregnancy-related health issues
- Advise travelers to check airline and cruise line policies for pregnant travelers
- Provide letter confirming due date and fitness to travel
- Provide copy of medical records
☐ Prepare for obstetric care at destination
- Advise traveler to arrange for obstetric care at destination, as needed
☐ Review signs and symptoms requiring immediate care, including
- Contractions or preterm labor
- Deep vein thrombosis or pulmonary embolism symptoms, which include unusual swelling of leg with pain in calf or thigh, unusual shortness of breath
- Pelvic or abdominal pain
- Preeclampsia symptoms (e.g., unusual swelling, severe headaches, nausea and vomiting, vision changes)
- Rupture of membranes
- Vomiting, diarrhea, dehydration
Contraindications to Travel During Pregnancy
Absolute contraindications are conditions for which the potential harm of travel during pregnancy always outweighs the benefits of travel to the pregnant person or fetus. Relative contraindications are conditions for which travel should be avoided if the potential harm from travel outweighs its benefits ( Box 7-02 ).
Although travel is rarely contraindicated during a normal pregnancy, pregnancies that require frequent antenatal monitoring or close medical supervision might warrant a recommendation that travel be delayed. Educate pregnant travelers that the risk of obstetric complications is greatest in the first and third trimesters of pregnancy.
Box 7-02 Contraindications to travel during pregnancy
Absolute contraindications.
- Abruptio placentae
- Active labor
- Incompetent cervix
- Premature labor
- Premature rupture of membranes
- Suspected ectopic pregnancy
- Threatened abortion / vaginal bleeding
- Toxemia, past or present
RELATIVE CONTRAINDICATIONS
- Abnormal presentation
- Fetal growth restriction
- History of infertility
- History of miscarriage or ectopic pregnancy
- Maternal age <15 or >35 years
- Multiple gestation
- Placenta previa or other placental abnormality
Planning for Emergency Care
Obstetric emergencies are often sudden and life-threatening. Advise all pregnant travelers (but especially those in their third trimester or otherwise at high risk) to identify, in advance, international medical facilities at their destination(s) capable of managing complications of pregnancy, delivery (including by caesarean section), and neonatal problems. Counsel against travel to areas where obstetric care might be less than the standard at home.
Many health insurance policies do not cover the cost of medical treatment for pregnancy or neonatal complications that occur overseas. Pregnant people should strongly consider purchasing supplemental travel health insurance to cover pregnancy-related problems and care of the neonate, as needed. In addition, pregnant travelers should consider medical evacuation insurance coverage in case of pregnancy-related complications (see Sec. 6, Ch. 1, Travel Insurance, Travel Health Insurance & Medical Evacuation Insurance ).
Medications
Over-the-counter drugs and nondrug remedies can help a pregnant person travel more comfortably. For instance, pregnant people can safely use a mild bulk laxative for constipation. In addition, several simple available remedies are effective in relieving the symptoms of morning sickness. Nonprescription remedies include ginger, available as a powder that can be mixed with food or drinks (e.g., tea), and as candy (e.g., lollipops). Similarly, pyridoxine (vitamin B6) is effective in reducing symptoms of morning sickness and is available in tablet form, as well as lozenges and lollipops. Antihistamines (e.g., dimenhydrinate, meclizine) often are used in pregnancy for morning sickness and motion sickness and appear to have a good safety record.
Carefully consider appropriate pain management and use of analgesics during pregnancy. Acetaminophen remains the nonopioid analgesic of choice during pregnancy. Although low-dose aspirin has been demonstrated to be relatively safe during pregnancy for certain clinical indications, it should be used cautiously. Aspirin can increase the incidence of abruption, and other anti-inflammatory agents can cause premature closure of the ductus arteriosus.
Various systems are used to classify drugs with respect to their safety in pregnancy . Refer to specific data about the effects of a given drug during pregnancy rather than depending on a classification. Counsel patients to help them make a balanced decision on the use of medications during pregnancy.
Vaccinations
In the best possible scenario, people should be up to date on routine vaccinations before becoming pregnant. The most effective way of protecting the infant against many diseases is to vaccinate the pregnant person. See a summary of current Advisory Committee on Immunization Practices (ACIP) guidelines for vaccinating pregnant people .
Coronavirus Disease 2019
Pregnant people are more likely to become more severely ill from coronavirus disease 2019 (COVID-19) than people who are not pregnant. Having COVID-19 during pregnancy increases a person’s risk of complications that can affect their pregnancy. For these reasons, the Centers for Disease Control and Prevention (CDC) recommends that people who are pregnant, trying to get pregnant, or who might become pregnant in the future get vaccinated against COVID-19 . As of August 2022, the COVID-19 vaccines authorized or approved for use in the United States are nonreplicating vaccines that do not cause infection in the pregnant person or the fetus. Pregnant people may choose to receive any of the COVID-19 vaccines authorized or approved for use in the United States; the ACIP does not state a preference.
COVID-19 vaccination can be safely provided before pregnancy or during any trimester of pregnancy. Available vaccines are highly effective in preventing severe COVID-19, hospitalizations, and deaths; data have shown that the benefits of vaccination during pregnancy, to both the pregnant person and their fetus, outweigh any potential risks. Pregnant people might want to speak with their health care provider before making a decision about receiving COVID-19 vaccine , but a consultation is not required before vaccination. Side effects from COVID-19 vaccination in pregnant people are like those expected among nonpregnant people. Pregnant people can take acetaminophen if they experience fever or other post-vaccination symptoms.
The ACIP recommends that all people who are or who will become pregnant during the influenza season have an annual influenza vaccine using inactivated virus. Influenza vaccines can be administered during any trimester.
The safety of hepatitis A vaccination during pregnancy has not been determined; because hepatitis A vaccine is produced from inactivated virus, though, the risk to the developing fetus is expected to be low. Weigh the risk associated with vaccination against the risk for infection in pregnant people who could be at increased risk for exposure to hepatitis A virus. According to the ACIP, pregnant people traveling internationally are at risk of hepatitis A virus infection; ACIP recommends vaccination during pregnancy for nonimmune international travelers.
Limited data suggest that developing fetuses are not at risk for adverse events resulting from vaccination of pregnant people with hepatitis B vaccine (for details, see Sec. 5, Part 2, Ch. 8, Hepatitis B ). ACIP recommends vaccinating pregnant people identified as being at risk for hepatitis B virus infection during pregnancy; risk factors include >1 sex partner during the previous 6 months, being evaluated or treated for a sexually transmitted infection, recent or current injection drug use, or having a HBsAg-positive sex partner. In November 2021, ACIP recommended vaccination of all adults 19–59 years old.
Japanese Encephalitis
Data are insufficient to make specific recommendations for use of Japanese encephalitis vaccine in pregnant people (see Sec. 5, Part 2, Ch. 13, Japanese Encephalitis ).
Live-Virus Vaccines
Most live-virus vaccines, including live attenuated influenza, measles-mumps-rubella, live typhoid (Ty21a), and varicella, are contraindicated during pregnancy. Postexposure prophylaxis of a nonimmune pregnant person exposed to measles can be provided by administering measles immune globulin (IG) within 6 days of exposure; for varicella exposures, varicella-zoster IG can be given within 10 days. Advise people planning to become pregnant to wait ≥4 weeks after receiving a live-virus vaccine before conceiving.
Yellow Fever
Yellow fever vaccine is the exception to the rule about live-virus vaccines being contraindicated during pregnancy. ACIP considers pregnancy a precaution (i.e., a relative contraindication) for yellow fever vaccine. If travel is unavoidable, and the risk for yellow fever virus exposure outweighs the vaccination risk, it is appropriate to recommend vaccination. If the risks for vaccination outweigh the risks for yellow fever virus exposure, consider providing a medical waiver to the pregnant traveler to fulfill health regulations. Because pregnancy might affect immune responses to vaccination, consider performing serologic testing to document an immune response to yellow fever vaccine. Furthermore, if a person was pregnant (regardless of trimester) when they received their initial dose of yellow fever vaccine, they should receive 1 additional dose before they are next at risk for yellow fever virus exposure (see Sec. 5, Part 2, Ch. 26, Yellow Fever ).
Meningococcal
According to the ACIP , pregnant (and lactating) people should receive quadrivalent meningococcal vaccine, if indicated. Meningococcal vaccine might be indicated for international travelers, depending on risk for infection at the destination (see Sec. 5, Part 1, Ch. 13, Meningococcal Disease ).
No adverse events linked to inactivated polio vaccine (IPV) have been documented among pregnant people or their fetuses. Vaccination of pregnant people should be avoided, however, because of theoretical concerns. IPV can be administered in accordance with the recommended immunization schedule for adults if a pregnant person is at increased risk for infection and requires immediate protection against polio (see Sec. 5, Part 2, Ch. 17, Poliomyelitis ).
Administer rabies postexposure prophylaxis with rabies immune globulin and vaccine after any moderate- or high-risk exposure to rabies; consider preexposure vaccine for travelers who have a substantial risk for exposure (see Sec. 5, Part 2, Ch. 18, Rabies ).
Tetanus-Diphtheria-Pertussis
Tetanus, diphtheria, and acellular pertussis vaccine (Tdap) should be given during each pregnancy irrespective of a person’s history of receiving the vaccine previously. To maximize maternal antibody response and passive antibody transfer to the infant, optimal timing for Tdap administration is between 27 and 36 weeks’ gestation (earlier during this time frame is preferred), but it may be given at any time during pregnancy.
Malaria Prophylaxis
Malaria, caused by Plasmodium spp. parasites transmitted by mosquitoes, can be much more serious in pregnant than in nonpregnant people and is associated with high risks of illness and death for both mother and fetus. Malaria in pregnancy can be characterized by heavy parasitemia, severe anemia, and profound hypoglycemia, and can be complicated by cerebral malaria and acute respiratory distress syndrome. Placental sequestration of parasites might result in fetal loss due to abruption, premature labor, or miscarriage. An infant born to an infected mother is apt to be of low birth weight, and, although rare, congenital malaria is possible.
Because no prophylactic regimen provides complete protection, pregnant people should avoid or delay travel to malaria-endemic areas. If travel is unavoidable, the pregnant person should take precautions to avoid mosquito bites and use an effective prophylactic regimen.
Chloroquine is the drug of choice for pregnant travelers going to destinations with chloroquine-sensitive Plasmodium spp., and mefloquine is the drug of choice for pregnant travelers going to destinations with chloroquine-resistant Plasmodium spp. Doxycycline is contraindicated because of teratogenic effects on the fetus after the fourth month of pregnancy. Primaquine is contraindicated in pregnancy because the infant cannot be tested for glucose-6-phosphate dehydrogenase deficiency, putting the infant at risk for hemolytic anemia. Atovaquone-proguanil is not recommended because of lack of available safety data. A list of the available antimalarial drugs and their uses and contraindications during pregnancy can be found in Sec. 5, Part 3, Ch. 16, Malaria .
Travel Health Kits
In addition to the recommended travel health kit items for all travelers (see Sec. 2, Ch. 10, Travel Health Kits ), pregnant travelers should pack antacids, antiemetic drugs, graduated compression stockings, hemorrhoid cream, medication for vaginitis or yeast infection, prenatal vitamins, and prescription medications. Encourage pregnant travelers to consider packing a blood pressure monitor if travel will limit access to a health center where blood pressure monitoring is available.
Respiratory and urinary infections and vaginitis are more likely to occur and to be more severe during pregnancy. Pregnant people who develop travelers’ diarrhea or other gastrointestinal infections might be more vulnerable to dehydration than nonpregnant travelers. Stress the need for strict hand hygiene and food and water precautions (see Sec. 2, Ch. 8, Food & Water Precautions ). Drinking bottled or boiled water is preferable to chemically treated or filtered water. Pregnant people should not consume water purified by iodine-containing compounds because of potential effects on the fetal thyroid (see Sec. 2, Ch. 9, Water Disinfection ).
As mentioned previously, pregnant people are at increased risk for severe COVID-19–associated illness (e.g., requiring invasive ventilation or extracorporeal membrane oxygenation) and death compared with people who are not pregnant. Underlying medical conditions (e.g., chronic kidney disease, diabetes, obesity) and other factors (e.g., age, occupation) can further increase a pregnant person’s risk for developing severe illness. Additionally, pregnant people with COVID-19 are at greater risk for preterm birth and other adverse outcomes.
Pregnant people, recently pregnant people, and those who live with or visit them should take steps to protect themselves from getting COVID-19. CDC recommends that people (including those who are pregnant) not travel internationally until they are up to date with their COVID-19 vaccines . Additional information for international travelers is available at CDC's International Travel website.
Hepatitis A and hepatitis E are both spread by the fecal–oral route (see Sec. 5, Part 2, Ch. 7, Hepatitis A , and Sec. 5, Part 2, Ch. 10, Hepatitis E ). Hepatitis A has been reported to increase the risk for placental abruption and premature delivery. Hepatitis E is more likely to cause severe disease during pregnancy and could result in a case-fatality rate of 15%–30%; when acquired during the third trimester, hepatitis E is also associated with fetal complications and fetal death.
Listeriosis & Toxoplasmosis
Listeriosis and toxoplasmosis (see Sec. 5, Part 3, Ch. 23, Toxoplasmosis ) are foodborne illnesses of particular concern during pregnancy because the infection can cross the placenta and cause spontaneous abortion, stillbirth, or congenital or neonatal infection. Warn pregnant travelers to avoid unpasteurized cheeses and uncooked or undercooked meat products. Risk for fetal infection increases with gestational age, but severity of infection is decreased.
Other Parasitic Infections & Diseases
Parasitic infections and diseases can be a concern, particularly for pregnant people visiting friends and relatives in low- and middle-income countries. In general, intestinal helminths rarely cause enough illness to warrant treatment during pregnancy. Most, in fact, can be addressed safely with symptomatic treatment until the pregnancy is over. On the other hand, protozoan intestinal infections (e.g., Cryptosporidium , Entamoeba histolytica , Giardia ) often do require treatment. These parasites can cause acute gastroenteritis, severe dehydration, and chronic malabsorption resulting in fetal growth restriction. E. histolytica can cause invasive disease, including amebic liver abscess and colitis. Pregnant people also should avoid bathing, swimming, or wading in freshwater lakes, rivers, and streams that can harbor the parasitic worms (schistosomes) that cause schistosomiasis (see Sec. 5, Part 3, Ch. 20, Schistosomiasis ).
Travelers’ Diarrhea
The treatment of choice for travelers’ diarrhea is prompt and vigorous oral hydration; azithromycin or a third-generation cephalosporin may, however, be given to pregnant people if clinically indicated. Avoid use of bismuth subsalicylate because of the potential impact of salicylates on the fetus. In addition, fluoroquinolones are contraindicated in pregnancy due to toxicity to developing cartilage, as noted in experimental animal studies.
Vectorborne Infections
Pregnant people should avoid mosquito bites when traveling in areas where vectorborne diseases are endemic. Preventive measures include use of Environmental Protection Agency–registered insect repellants , protective clothing, and mosquito nets (see Sec. 4, Ch. 6, Mosquitoes, Ticks & Other Arthropods ). For details on yellow fever vaccine and malaria prophylaxis during pregnancy, see above.
Zika virus is spread primarily through the bite of an infected Aedes mosquito ( Ae. aegypti and Ae. albopictus ) but can also be sexually transmitted. The illness associated with Zika can be asymptomatic or mild; some patients report acute onset of conjunctivitis, fever, joint pain, and rash that last for several days to a week after infection.
Birth defects caused by Zika virus infection during pregnancy include brain, eye, and neurodevelopmental abnormalities. Because of the risk for birth defects, CDC recommends pregnant people avoid travel to areas with a Zika outbreak, and, for the duration of the pregnancy, to avoid sex or use condoms with anyone who has traveled to a risk area.
Advise pregnant people considering travel to areas with Zika to carefully assess the risks of Zika infection during pregnancy; provide information about prevention strategies, signs and symptoms, and the limitations of Zika testing. Pregnant people should strictly follow steps to prevent mosquito bites and sexual transmission. See additional information, including the most current list of countries and territories where Zika is active . Guidance for pregnant people can be found on the CDC Zika website .
Pregnant people should be aware of specific current environmental issues in their international destinations (e.g., natural disasters, special events or gatherings, travel warnings). More information can be found at the CDC Travelers’ Health website and on the destination pages of the US Department of State website.
Air Quality
Air pollution causes more health problems during pregnancy because ciliary clearance of the bronchial tree is slowed, and mucus is more abundant. For more details on traveling to destinations where air quality is poor, see Sec. 4, Ch. 3, Air Quality & Ionizing Radiation .
Extremes of Temperature
Body temperature regulation is not as efficient during pregnancy, and temperature extremes can create more physiological stress on the pregnant person (see Sec. 4, Ch. 2, Extremes of Temperature ). In addition, increases in core temperature (e.g., heat exhaustion, heat stroke), might harm the fetus. The vasodilatory effect of a hot environment and dehydration might cause fainting. For these reasons, then, encourage pregnant travelers to seek air-conditioned accommodations and restrict their level of activity in hot environments. If heat exposure is unavoidable, the duration should be as short as possible to prevent an increase in core body temperature. Pregnant travelers should take measures to avoid dehydration and hyperthermia.
High Elevation Travel
Pregnant people should avoid activities at high elevation unless they have trained for and are accustomed to such activities; those not acclimated to high elevation might experience breathlessness and palpitations. The common symptoms of acute mountain sickness (insomnia, headache, and nausea) frequently are associated with pregnancy, and it might be difficult to distinguish the cause of the symptoms. Most experts recommend a slower ascent with adequate time for acclimatization. No studies or case reports show harm to a fetus if the mother travels briefly to high elevations during pregnancy; recommend that pregnant people not sleep at elevations >12,000 ft (≈3,600 m) above sea level, if possible. Probably the greatest concern is that high-elevation destinations often are inaccessible and far from medical care (see Sec. 4, Ch. 5, High Elevation Travel & Altitude Illness ).
Advise pregnant people to follow safety instructions for all forms of transport and to wear seat belts, when available, on all forms of transportation, including airplanes, buses, and cars (see Sec. 8, Ch. 5, Road & Traffic Safety ). A diagonal shoulder strap with a lap belt provides the best protection. The shoulder belt should be worn between the breasts with the lap belt low across the upper thighs. When only a lap belt is available, pregnant people should wear it low, between the abdomen and across the upper thighs, not above or across the abdomen.
Most commercial airlines allow pregnant travelers to fly until 36 weeks’ gestation. Some limit international travel earlier in pregnancy, and some require documentation of gestational age. Pregnant travelers should check with the airline for specific requirements or guidance, and should consider the gestational age of the fetus on the dates both of departure and of return.
Most commercial jetliner cabins are pressurized to an equivalent outside air pressure of 6,000–8,000 ft (≈1,800–2,500 m) above sea level; travelers might also experience air pressures in this range during travel by hot air balloon or on noncommercial aircraft. The lower oxygen tension under these conditions likely will not cause fetal problems in a normal pregnancy. People with pregnancies complicated by conditions exacerbated by hypoxia (e.g., preexisting cardiovascular problems, sickle cell disease, severe anemia [hemoglobin <8.0 g/dL], intrauterine fetal growth restriction) could, however, experience adverse effects associated with low arterial oxygen saturation.
Risks of air travel include potential exposure to communicable diseases, immobility, and the common discomforts of flying. Abdominal distention and pedal edema frequently occur. The pregnant traveler might benefit from an upgrade in airline seating and should seek convenient and practical accommodations (e.g., proximity to the lavatory). Pregnant travelers should select aisle seating when possible, and wear loose fitting clothing and comfortable shoes that enable them to move about more easily and frequently during flights.
Some experts report that the risk for deep vein thrombosis (DVT) is 5–10 times greater among pregnant than nonpregnant people, although the absolute risk is low. To help prevent DVT, pregnant travelers should stay hydrated, stretch frequently, walk and perform isometric leg exercises, and wear graduated compression stockings (see Sec. 8, Ch. 3, Deep Vein Thrombosis & Pulmonary Embolism ).
Cosmic radiation during air travel poses little threat to the fetus but might be a consideration for pregnant travelers who fly frequently (see Sec. 9, Ch. 3, . . . perspectives: People Who Fly for a Living—Health Myths & Realities ). Older airport security machines are magnetometers and are not harmful to the fetus. Newer security machines use backscatter x-ray scanners, which emit low levels of radiation. Most experts agree that the risk for complications from radiation exposure from these scanners is extremely low.
Cruise Ship Travel
Most cruise lines restrict travel beyond 24 weeks’ gestation (see Sec. 8, Ch. 6, Cruise Ship Travel ). Cruise lines might require pregnant travelers to carry a physician’s note stating that they are fit to travel, including the estimated date of delivery. Pregnant people should check with the cruise line for specific requirements or guidance. For pregnant travelers planning a cruise, provide advice about gastrointestinal and respiratory infections, motion sickness (see Sec. 8, Ch. 7, Motion Sickness ), and the risk for falls on a moving vessel, as well as the possibility of delayed care while at sea.
The following authors contributed to the previous version of this chapter: Diane F. Morof, I. Dale Carroll
Bibliography
Allotey J, Stallings E, Bonet M, Yap M, Chatterjee S, Kew T, et al.; PregCOV-19 Living Systematic Review Consortium. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ. 2020;370:m3320.
Bisson DL, Newell SD, Laxton C; on behalf of the Royal College of Obstetricians and Gynaecologists. Antenatal and postnatal analgesia. BJOG. 2018;126(4):114–24.
Centers for Disease Control and Prevention. Guidelines for vaccinating pregnant women. Atlanta: The Centers; 2014. Available from: www.cdc.gov/vaccines/pregnancy/hcp-toolkit/guidelines.html .
Dotters-Katz S, Kuller J, Heine RP. Parasitic infections in pregnancy. Obstet Gynecol Surv. 2011;66(8):515–25.
Hezelgrave NL, Whitty CJ, Shennan AH, Chappell LC. Advising on travel during pregnancy. BMJ. 2011;342:d2506.
Irvine MH, Einarson A, Bozzo P. Prophylactic use of antimalarials during pregnancy. Can Fam Physician. 2011;57(11):1279–81.
Magann EF, Chauhan SP, Dahlke JD, McKelvey SS, Watson EM, Morrison JC. Air travel and pregnancy outcomes: a review of pregnancy regulations and outcomes for passengers, flight attendants, and aviators. Obstet Gynecol Surv. 2010;65(6):396–402.
Rasmussen SA, Jamieson DJ, Honein MA, Petersen LR. Zika virus and birth defects—reviewing the evidence for causality. N Engl J Med. 2016;374(20):1981–7.
Rasmussen SA, Watson AK, Kennedy ED, Broder KR, Jamieson DJ. Vaccines and pregnancy: past, present, and future. Semin Fetal Neonatal Med. 2014;19(3):161–9.
Roggelin L, Cramer JP. Malaria prevention in the pregnant traveller: a review. Travel Med Infect Dis. 2014;12(3):229–36.
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Quick Links
- Make An Appointment
- Our Services
- Price Estimate
- Price Transparency
- Pay Your Bill
- Patient Experience
- Careers at UH
Schedule an appointment today

International Travel While Pregnant or Breastfeeding
Special considerations for traveling while pregnant.
Traveling during pregnancy is normal, and a lot of women do it. But it's important to think about potential problems that could come up during international travel. Also think about how you would get quality healthcare in the countries you are visiting. Get all of the vaccines you need before becoming pregnant instead of waiting to get them during pregnancy.
The American College of Obstetricians and Gynecologists says the safest time for a woman to travel is in the second trimester of her pregnancy, from 14 to 28 weeks. This is the time when you will feel your best. You are also at the lowest risk for spontaneous abortion (miscarriage) or premature labor. During the third trimester (28 to 40 weeks), many healthcare providers and midwives advise staying within a 300-mile radius of home because of potential problems, such as high blood pressure, phlebitis, and false or preterm labor. Generally, women are not allowed to travel by air after 36 weeks for domestic travel, and after 28 to 35 weeks for international travel. The decision on whether to travel and how far to travel at any time during pregnancy should be a joint decision between you and your healthcare provider.
For most pregnant women, flying does not pose a risk to the fetus from cosmic radiation. But aircrew and women who often fly may exceed radiation limits.
According to the CDC, pregnant women with the following conditions may be advised against traveling to countries that need pretravel vaccines. This list may be incomplete. So discuss your health history with your provider or midwife before planning travel:
History of miscarriage
Incompetent cervix
History of ectopic pregnancy
History of premature labor or premature rupture of membranes
History of or current placental abnormalities
Threatened miscarriage or vaginal bleeding during current pregnancy
Multiple fetuses in current pregnancy
History of pre-eclampsia, high blood pressure, or diabetes with any pregnancy
History of infertility or trouble getting pregnant
Pregnancy for the first time over the age of 35 years
Heart valve disease or congestive heart failure
History of blood clots
Severe anemia
Chronic organ system problems that need to be treated
You may also be advised against traveling to places that may have hazards. The list below may be incomplete. Talk about your travel plans with your healthcare provider or midwife before planning a trip.
Places with high altitudes
Places that have outbreaks of life-threatening food- or insect-borne infections
Places where malaria is common
Places where live-virus vaccines are needed or recommended
Healthy tips for traveling while pregnant
Here are tips for traveling while pregnant:
Try to plan ahead for any problems or emergencies that could come up before you travel. Check that your health insurance is valid while you are abroad. Also check to see whether the plan will cover a newborn, should you deliver while away. You may want to think about getting a supplemental travel and medical evacuation insurance.
Research medical facilities in your destination. Women in the last trimester of pregnancy should look for places that can manage complications of pregnancy, pre-eclampsia, and cesarean sections.
If you will need prenatal care while you are abroad, arrange for this before you leave. Talk with your healthcare provider or midwife to figure out the best way to handle this.
Know your blood type and check that blood is screened for HIV and hepatitis B in the areas you will be visiting.
Check that safe food and beverages, such as bottled water and pasteurized milk, are available at your destinations.
If flying, ask for an aisle seat at the bulkhead. This gives you the most space and comfort. If morning sickness is a problem, try to arrange travel during a time of day when you generally feel well. Seats over the wing in the midplane region will give you the smoothest ride.
Try to walk every half-hour during a smooth flight. Flex and extend your ankles often to prevent blood clots in the veins (thrombophlebitis).
Fasten your seat belt at the pelvis level, below your hips.
Drink plenty of fluids to stay hydrated. Aircraft cabins have low humidity.
Try to rest as much as possible while away. Exercise and activity during pregnancy are important but try not to overdo it.
Special considerations for traveling while breastfeeding
Breastfeeding gives babies the most nutritional start in life. It also gives them vital protection against certain infections. But traveling internationally while nursing can be challenging.
If you are breastfeeding only, you don't have to worry about sterilizing bottles or having clean water. You may get vaccines to protect against disease, depending on where you are traveling. But diseases such as yellow fever, measles, and meningococcal meningitis may be a threat to infants who can't be vaccinated at birth. Discuss this with both your healthcare provider and your infant's caregiver before you travel.
If you are feeding your baby formula, it's best to use powdered formula made with boiled water. You may also want to carry a supply of prepared infant formula in cans or ready-to-feed bottles for emergencies.
Breastfeeding helps lower the chance of your baby getting traveler's diarrhea. If you get traveler's diarrhea, drink more fluids and continue to nurse your baby.
Watch your eating and sleeping patterns, as well as your stress levels. This will affect your milk output. Drink more fluids. Stay away from alcohol and caffeine, as well as exposure to smoke.
If you are traveling without your infant, you will need to pump to maintain your milk supply. Check with TSA about transporting your milk on flights.

Traveling in the Third Trimester of Pregnancy: My Best Tips

Traveling in the 3rd trimester?! Most people don’t realize that you can still travel just fine in the third trimester. Despite what you can read in many bias articles and forums, you can fly freely until 36 weeks. Naturally, assuming that you have an uncomplicated pregnancy.
While most people might prefer to stay at home and nest in the third trimester, I didn’t feel that need and wanted to travel more before the baby shows up.
One can say that I got lucky that I felt fine for most of my pregnancy . Truth to be told, apart from the awful rhinitis that I described in my other post, I was definitely functional most of the time. Like most people, I had back pain and neck pain every other day, but I guess I must have a higher tolerance for discomfort than most as nothing has stopped me doing what I wanted during late pregnancy.
Flying When Pregnant in the Third Trimester of Pregnancy
While some airlines officially say that while you’re allowed to travel until week 36th, you need to provide a letter from your doctor I was never asked to show such letter at any airport. Only on one occasion, when entering the plane Qatar Airlines staff hesitantly asked me if I was pregnant, but only to tell me to let them know if I needed anything during the flight.
Due to complications with birth I described in this post I had to fly at 39 weeks and still – no one wanted to see my doctor’s note.
[su_row class=””] [su_column size=”1/2″ center=”no” class=””]
I read many opinions that the best seat to get on the plane for pregnant women is aisle as you can freely go to the bathroom, I’m not entirely sure I’d agree.
Somehow I never peed that much on planes (I guess the baby knew to behave as he’s an avid traveler now ), but in the aisle seat I felt constantly disturbed by people passing by and taking their luggage, flight attendants serving food, that I started booking window seats, so I could take a nap in peace.
Just don’t book an emergency exit seat because they don’t recline. A seat that doesn’t recline is a nightmare for a pregnant woman!
[/su_column][su_column size=”1/2″ center=”no” class=””]

[/su_column] [/su_row]
Babymoon in the Third Trimester
Since Christmas fell at the end of my second trimester and we didn’t want to travel in the high season, we opted for a babymoon at the beginning of my third trimester.
What’s babymoon? It’s a vacation you take with your spouse before you have your baby – usually in the second trimester. It’s the last hurrah before a baby enters your world. Most people opt for a quiet resort stay or beach vacation.
In my case due my babymoon wasn’t the last trip, and it was definitely an active one. I was originally wanting to go to Bora Bora, but January is one of the worst months to go there (and to many other places we considered), so we opted for revisiting one of my old homes – South Africa .
We spent a week in and around Cape Town and it was awesome! While I couldn’t do certain activities due to pregnancy (like abseiling) they were many other things we could do, plus the food is delicious.
I played with the penguins, did some hiking (you can definitely hike when pregnant, you’ll just be slightly slower!), stuffed my face with fresh seafood, flew a helicopter, went up Table Mountain and relaxed at the beach.

Traveling in the Third Trimester of Pregnancy
New York City
After our babymoon in South Africa we flew back home to Italy for a few days before taking off to NYC. While a flight to NYC wasn’t an issue, I was very uncomfortable on the way back. I ended up standing up and walking for the first few hours before using my husband as a pillow for the remaining time of the flight. Ironically, the moment I got off the plane I was comfortable again.
One problem I noticed during my trip to NYC was my sensitiveness to cold. I’ve never liked the cold weather, but when pregnant I felt about three times colder than usual until week 32, and then I started feeling about three times warmer than usual. Fortunately, I was still able to fit in my regular sized big coat, but if you don’t, you might want to consider investing in coat extenders .
While in NYC we also picked up a stroller for our baby , since I was really set on the best stroller for traveling and it wasn’t available in Italy. Ironically, the airline broke our stroller seat on its first trip which turned out to be a good thing after all, as I’ve learned about different stroller policies and what to do in case your pram gets broken or lost .

London & Warsaw
As living an expat life comes with a lot of paperwork in different countries, soon after our trip to NYC I had to make a pit stop in Warsaw and London . Flights were short and easy, so I didn’t feel uncomfortable at all.

I was very worried that once I enter the third trimester I’m going to start feeling like crap and wouldn’t be able to get up from the sofa. Talking to other pregnant friends or new moms didn’t help.
Literally, everyone else who recently had a kid or were still pregnant were telling me that my hips will loosen up, that I’ll be waddling and tired all the time, that I’ll feel nauseous and have heartburn and my hands will get swollen.
None of these things ever happened in my case up until week 37. Even right before my due date I was actually wearing high heels and running. Sure, I felt bad here and there, but a quick rest for a bit was enough to make me feel better. However, the further along I was in my pregnancy, the more comfortable I felt on my feet – standing, walking, or even running, than sitting or laying down.
The worst thing was actually my psoriasis getting worse and worse and I felt very uncomfortable and annoyed because of that.
I’m not saying that none of the bad pregnancy symptoms won’t happen to you, but there’s no rule. You might feel like crap, but you might not, so do yourself a favor and stop getting scared by what other moms tell you. You do you and adjust your lifestyle and travels to the way you feel.
Skiing When Pregnant
That said since I didn’t want to miss out on the Italian winter I decided I feel well enough to go snowshoeing in the Dolomites and skiing in the Alps. Most moms give up on sports apart from simple maternity yoga, but upon my research, I realized that I wasn’t the only one who skied while pregnant.
I know people who skied, surfed or kept running in the third trimester and the baby turned out just fine. One would ask, is it safe? I’m an advanced skier and haven’t fallen for years, plus I obviously wasn’t going in for the hardest slopes available.

Comfortable Clothes for Pregnant Travelers
While I was lucky enough to wear non-maternity clothes up until mid-third trimester, later on, I found many other alternatives. I discovered good maternity clothes that aren’t only comfortable for traveling, but also affordable and not ugly.
Do you have any questions about traveling in the third trimester of pregnancy?
Share this:
Notify me of new posts by email.
When First Pregnancy is Easy: On Invisible Postpartum Consequences – annainthehouse.com
Tuesday 10th of March 2020
[…] No vomiting, no unbearable pains, nada. Just a little anemia at the very end, but that’s expected in most pregnancies. I was even still hiking and skiing (carefully) in my third trimester. […]
Saturday 25th of May 2019
Great! I'm happy for you. In my third trimester, I had such bad back pain that I barely walk. And before that the only commute I could handle was from home to work. So, there was no way to travel
Angie Silver
You did so well! After travelling at 28 weeks, I was like right I'm done! lol
Traveling While Pregnant

Planning to travel while you're pregnant? You'll want to know what's safe, what isn't, and which precautions to take before, during, and after your trip.
There are several factors that can affect travel during your pregnancy: your pregnancy stage when the trip is planned; whether there have been any complications during the pregnancy; the type of travel; and the distance that the trip will take you from home.
Pregnancy Stage: Travel Implications
Travel during the first and second trimesters is usually considered to be safe, although it may be more tiring than usual.
Traveling during the first trimester of pregnancy may pose a few challenges, especially if you're experiencing morning sickness, nausea, or fatigue. And the risk of bleeding or miscarriage is the greatest during these months.
The second trimester is the time in your pregnancy when you probably feel the best and have the most energy. This is a great time for a trip. In fact, vacationing with your partner during this period might be an ideal chance to spend some fun time alone together before the baby arrives!
Travel in the third trimester may be uncomfortable and can be risky, because you could go into labor many miles away from your own healthcare providers and hospital. Some airlines do not let women fly during their last month of pregnancy without a doctor's letter of permission. Quite often, that letter must be written within 72 hours of flight time.

Types of Travel
Traveling by car is likely to be the most comfortable means of getting around during pregnancy. When driving or riding in a car, stop every hour or two and walk around to stretch your legs — this will promote good circulation. Remember to always fasten your seat belt. Place the lap belt portion under your abdomen and position the shoulder harness between your breasts.
Flying shouldn't cause any problems in your first two trimesters. Be sure to:
Plan your schedule so that you're not rushed and have plenty of time between connecting flights
Request an aisle seat so that you have a little more room and can easily get to the bathroom as needed.
Walk up and down the aisle every hour or so to promote circulation in your legs.
While sitting, flex your feet toward your face and make circles with your feet.
Wearing support hose or flight socks also stimulates circulation in your legs when you have to sit for long periods of time.
Drink enough fluids to stay well hydrated.
Travel by boat, particularly if it's a large cruise ship, also should pose no particular problems in the first two trimesters. And most cruise ships have medical personnel aboard should you need assistance. If you're sensitive to motion, you might want to take medication to prevent motion sickness; ask your healthcare provider what would be safe to take during pregnancy. You can also wear the anti-nausea acupressure wristbands that are available over-the-counter at your pharmacy.
Long Distance and International Travel
If you plan to travel far from home, you can be prepared by being sure there are good sources of medical care at your destination. Take your pregnancy records with you, including tests you've had done, medications you're taking, your blood type, and any other information that might be helpful when you're out of town.
If you have to travel out of the country, it is important to take copies of your prescriptions for medications, in case your medications become lost. Be sure your immunizations are up to date before planning a trip to countries where vaccinations are necessary; also, keep in mind that some vaccines may not be safe to update during pregnancy.
Be aware that changes in climate or altitude and types of food could cause you more discomfort when you're pregnant. Limit exertion for a couple days after your arrival at your destination, particularly if the climate is hot or the altitude is high; this will allow your body to adjust to these changes.
In addition to the above considerations, always consult your healthcare provider before planning a trip, particularly if you'll be experiencing changes in altitude. She may be able to give you a medical contact in the area of your destination, in case you'd need to see a physician while you're away from home.
With a little advance planning and some wise precautions, travel during your pregnancy can be safe and enjoyable. Bon voyage!
Review this article:
Read more about pregnancy.
- Pregnancy Announcement
- Pregnancy Calendar
- Pregnancy Symptoms
- Baby Shower & Registry
- Prenatal Health and Wellness
- Preparing For Your New Baby
- Giving Birth
- Due Date Calculator
Join a World of Support
through Pregnancy and Parenthood.

TRACK WITH TOOLS

LEARN WITH EXPERTS

GET REWARDED

Where You Already Belong
Healthy Pregnancy
Tips For Having a Healthy Pregnancy
Traveling While Pregnant: Tips and Cautions for Traveling During the Third Trimester

In today’s modern world, it’s often necessary to travel while you’re pregnant. While it’s best to restrict your activity during the third trimester, it’s still possible to travel safely provided you adhere to some basic principles. The comfort levels and safety of traveling while pregnant vary dramatically from one month to the other. Traveling during the first two trimesters is generally regarded as safe with no restrictions. The first trimester is often completely safe, but you may experience a bit more fatigue during this time. Only pregnant women that have been advised by their doctor to avoid travel during the first two trimesters should be concerned. Generally, airlines will prohibit you from traveling in your ninth month of pregnancy and some may limit your travel before then.
The Case for Avoiding Travel

Complications of Pregnancy
While most women can travel throughout the majority of their pregnancy and into the beginning of their third trimester, there are some women who should minimize all travel. Women who experience preterm contractions, pregnancy-induced hypertension, bleeding or gestational diabetes should limit their travel at all stages. If you feel a need to travel with any of these conditions, aim for short trips that are close to home. Often, you can find enjoyable activities within a 30-minute drive of any location. Your pregnancy is a good time to become more familiar with your home and area if you are in the high-risk pregnancy group.
Best Modes of Travel

Traveling by train is another good option for your first two trimesters. It should generally be avoided in the third trimester, but at other times it can be an enjoyable way of going a long distance. Traveling by train offers the convenience of a bathroom when you need it, comfortable seats and the ability to walk around whenever needed.
Boat traveling is also okay during the first two trimesters. Since most boats have medical personnel available, you should be able to get the help you need should a problem arise. Check with the cruise ship to ensure they will be able to accommodate you. Some insurance plans may not cover issues that occur aboard boats during a pregnancy since it’s not seen as an essential mode of transportation.
Flying is a good option during your first two trimesters, but many airlines may prohibit you from traveling during the third trimester without a recent note from your doctor. In some cases, they may not allow travel at all. It’s important to check with the airline you plan to travel with ahead of your travel dates to ensure you won’t experience any issues with the airline’s policies. If you have connecting flights, leave enough time to get between flights so that you don’t have to hurry. Drink lots of water or juice and wear support hose while flying to keep your circulation going.
When to Avoid Travel

- share
- tweet
Related Posts

If you're used to exercising on a regular basis, the thought of being pregnant and…

Traveling can be difficult at any time. But traveling while pregnant takes a few extra…

If you're a first-time mom, pregnancy is a whole new world. Although the idea of…
Stay in touch via Newsletter
- Name First Last
Prenatal Health
Pregnancy Basics
Everyday You
Preparing for Baby
Postpartum Basics
- About / Contact Us
- Privacy Policy
- Terms And Conditions
Other interesting websites from Medichron Publications
General information, professional audience.

- Pregnancy Classes

Travel During Pregnancy
As long as there are no identified complications or concerns with your pregnancy, it is generally safe to travel during your pregnancy. The ideal time to travel during pregnancy is the second trimester . In most cases, you are past the morning sickness of the first trimester and several weeks from the third stage of pregnancy when you are more easily fatigued .
Is it safe to travel during pregnancy?
Traveling by air is considered safe for women while they are pregnant; however, the following ideas might make your trip safer and more comfortable.
- Most airlines allow pregnant women to travel through their eighth month. Traveling during the ninth month is usually allowed if there is permission from your health care provider.
- Most airlines have narrow aisles and smaller bathrooms, which makes it more challenging to walk and more uncomfortable when using the restroom. Because of potential turbulence that could shake the plane, make sure you are holding on to the seatbacks while navigating the aisle.
- You may want to choose an aisle seat which will allow you to get up more easily to reach the restroom or just to stretch your legs and back.
- Travel on major airlines with pressurized cabins and avoid smaller private planes. If you must ride in smaller planes, avoid altitudes above 7,000 feet.
- Although doubtful, the risk of DVT can be further reduced by wearing compression stockings.
The Royal College of Obstetricians and Gynaecologists and the International Air Travel Association recommend that expecting mothers in an uncomplicated pregnancy avoid travel from the 37th week of pregnancy through birth. Avoiding travel from 32 weeks through birth is recommended for women who have complicated pregnancies with risk factors for premature labor, such as mothers carrying multiples.
Risk factors that warrant travel considerations include the following:
- Severe anemia
- Cardiac disease
- Respiratory disease
- Recent hemorrhage
- Current or recent bone fractures
Traveling by Sea During Pregnancy
Traveling by sea is generally safe for women while they are pregnant; the motion of the boat may accentuate any morning sickness or make you feel nauseous all over again. There are a few considerations to make your trip safer and more comfortable:
- Check with the cruise line to ensure that there is a health care provider on board in case there are any pregnancy complications .
- Review the route and port-of-calls to identify if there is access to any medical facilities if needed.
- Make sure any medications for seasickness are approved for women who are pregnant and that there is no risk to the developing baby.
- Seasickness bands use acupressure points to help prevent upset stomach and maybe a good alternative to medication.
International Travel During Pregnancy
Traveling overseas has the same considerations that local or domestic travel has, but it also has additional concerns that you need to know about before making an international trip. The information below is provided to help you assess whether an international trip is good for you at this time:
- It is important to talk with your health care provider before you take a trip internationally to discuss safety factors for you and your baby.
- Discuss immunizations with your health care provider and carry a copy of your health records with you.
- With international travel, you may be exposed to a disease that is rare here in the United States but is common in the country you visit.
- Contact the Centers for Disease Control and Prevention at (800) 311-3435 or visit their website at www.cdc.gov to receive safety information along with immunization facts related to your travels.
- Diarrhea is a common concern when traveling overseas because you may not be used to the germs and organisms found in the food and water of other countries. This can lead to a problem of dehydration .
Here are some tips to avoid diarrhea and help keep you safe:
- Drink plenty of bottled water
- Used canned juices or soft drinks as alternatives
- Make sure the milk is pasteurized
- Avoid fresh fruits and vegetables unless they have been cooked or can be peeled (such as an orange or a banana)
- Make certain that all meat and fish has been cooked completely; if you are unsure, do not eat it
Travel Tips During Pregnancy
Whether you are going by car, bus, or train, it is generally safe to travel while you are pregnant; however, there are some things to consider that could make your trip safer and more comfortable.
- It is essential to buckle-up every time you ride in a car. Make sure that you use both the lap and shoulder belts for the best protection of you and your baby.
- Keep the airbags turned on. The safety benefits of the airbag outweigh any potential risk to you and your baby.
- Buses tend to have narrow aisles and small restrooms. This mode of transportation can be more challenging. The safest thing is to remain seated while the bus is moving. If you must use the restroom, make sure to hold on to the rail or seats to keep your balance.
- Trains usually have more room to navigate and walk. The restrooms are usually small. It is essential to hold on to rails or seat backs while the train is moving.
- Try to limit the amount of time you are cooped up in the car, bus, or train. Keep travel time around five to six hours.
- Use rest stops to take short walks and to do stretches to keep the blood circulating.
- Dress comfortably in loose cotton clothing and wear comfortable shoes.
- Take your favorite pillow.
- Plan for plenty of rest stops, restroom breaks and stretches.
- Carry snack foods with you.
- If you are traveling any distance, make sure to carry a copy of your prenatal records.
- Enjoy the trip.
Want to Know More?
- How to Treat Jet Lag Naturally During Pregnancy
Compiled using information from the following sources:
1. Planning Your Pregnancy and Birth Third Ed. The American College of Obstetricians and Gynecologists, Ch. 5. William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 8.
2. Royal College of Obstetricians and Gynaecologists, Air Travel and Pregnancy (Scientific Impact Paper No. 1), https://www.rcog.org/uk, May 22, 2013.
BLOG CATEGORIES
- Can I get pregnant if… ? 3
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Breastfeeding 29
- Changes In Your Body 5
- Cord Blood 4
- Genetic Disorders & Birth Defects 17
- Health & Nutrition 2
- Is it Safe While Pregnant 54
- Labor and Birth 65
- Multiple Births 10
- Planning and Preparing 24
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Pregnancy Health and Wellness 149
- Pregnancy Products & Tests 8
- Pregnancy Supplements & Medications 14
- The First Year 41
- Week by Week Newsletter 40
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Paternity Tests 2
- Pregnancy Symptoms 5
- Prenatal Testing 16
- The Bumpy Truth Blog 7
- Uncategorized 4
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Women's Health 34
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
Share this post:
Similar post.

Preconception Wellness - Prepare for the Unexpected

Leg Cramps During Pregnancy

Prenatal Vitamin Limits
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
By Stacie Dunkle
“We don’t recommend international travel during pregnancy for first-time mothers,” said my nurse midwife. Those words stopped me in my tracks. As an officer in the Epidemic Intelligence Service with three years of experience working overseas, I couldn’t believe what this nurse was telling me. Rarely a month went by that I wasn’t waiting in a security line at the airport. “Why?” I asked. I was up-to-date on all of my vaccines, even yellow fever, which I knew shouldn’t be given during pregnancy, and I was well-practiced in methods for staying healthy in developing countries (wearing seatbelts and avoiding untreated drinking water, food from street vendors, raw vegetables, etc.). I began to wonder how I was going to break the news to my supervisor that I wouldn’t be able to conduct the investigation we were planning in Nepal in two weeks. We had been preparing for over a month. Our colleagues on the ground were ready to go, and my plane tickets were already booked.
Reality Check
When my partner and I decided to have a baby, I knew that once our little one arrived, my life would change dramatically. There would be no more hopping on planes to far-off places during public health emergencies—I’d have to think about who would watch my baby and how I’d cope with potentially missing all those precious moments with him. Still, the decision was easy since I had always wanted to have children and I was finally at a point in life when the timing felt right. Pregnancy can be a difficult thing to plan, of course, so when it did happen, somehow it still felt unexpected. Even more unexpected was how much my life was suddenly changing before the baby had even arrived.

“You’ll be taking a big risk,” the nurse said. “You can’t take any of the drugs we usually prescribe to prevent malaria.” Although most pregnant women can take a drug called mefloquine to prevent malaria, I couldn’t take it because of my personal health history. I wasn’t just thinking about myself anymore; I also had to consider my baby. Because of the serious risk associated with getting malaria during pregnancy, I decided it was best to cancel my trip.
Of course, my supervisor was very understanding. He had been planning to travel to Nepal as well, and with his guidance, our partners were able to carry out the investigation on their own. Although I was disappointed to not participate fully, I changed my focus to health issues that were closer to home and still traveled quite a bit. During my second trimester, I flew to Mexico, Ohio, Michigan, Canada, Arizona, and Florida. It’s too bad I couldn’t get double the frequent flyer miles while traveling for two! During these flights, I avoided lifting heavy baggage, always requested an aisle seat, and was careful to drink plenty of fluids and walk around every 30 minutes or so. Of course, the latter was no problem since I had to use the restroom that often anyway! I enjoyed traveling while pregnant and laughed thinking that my baby would be born already familiar with the sound of jet engines and having memorized the safety features aboard aircrafts.
The Home Stretch
When my third trimester arrived, I was offered an opportunity to travel to Lima, Peru to attend a training summit. It would be a valuable trip for me professionally because it would provide background for a project I was working on. I would be able to network with colleagues and focus my work to make it more useful to them. When I looked at the dates for the trip, I realized I would be 33 weeks pregnant upon departure and staying for a little over a week. I hesitated because many physicians don’t recommend traveling after 32 weeks, and most airlines restrict travel after 36 weeks for single, uncomplicated pregnancies. I was fortunate to have been very healthy during pregnancy and decided the trip was worth the risk, but swore I would cancel if any concerns came up before departure.
I still took a number of precautions before I committed to traveling. These included getting approval from my certified nurse midwife and reviewing CDC’s website of “ Health Information for Travelers to Peru .” My biggest concern was premature delivery in an unfamiliar country where Spanish is the primary language. My experience with Spanish is limited to high school classes and a few weeks traveling in Spain and Mexico. If I had to ask anything more than, “Dónde están los baños?” I would be out of luck; that included trying to describe symptoms I might be experiencing to a doctor. Fortunately, I have a friend who had just recently moved back to the US after living in Lima for a year. She was able to provide local English-speaking contacts and recommended an obstetrician and hospital where I could receive care. I also checked to make sure my health insurance would cover any medical expenses I might have had while travelling.

To everyone’s surprise, I went into labor six days later. My mind raced with questions. Will my baby be healthy arriving at 35 weeks? What would have happened if I had gone into labor in Peru without the support of my loved ones? After reviewing my medical records, my midwife predicted that my due date was off by at least a week and I was closer to full term than we had originally thought. My son was born the following night, completely healthy, into the loving arms of his mother, father, and grandparents. The question I kept asking myself was: if I had it to do again, would I have travelled so far knowing I was so close to delivery?

What do you think?
We want to hear from you. Have you traveled during pregnancy or had to pass on a trip because you were expecting? How has being a parent changed your career?
If you would like more information on traveling during pregnancy please visit http://wwwnc.cdc.gov/travel/yellowbook/2012/chapter-8-advising-travelers-with-specific-needs/pregnant-travelers.htm
15 comments on “Ticket for Two – International travel during pregnancy”
Comments listed below are posted by individuals not associated with CDC, unless otherwise stated. These comments do not represent the official views of CDC, and CDC does not guarantee that any information posted by individuals on this site is correct, and disclaims any liability for any loss or damage resulting from reliance on any such information. Read more about our comment policy » .
I was a little over 20 weeks pregnant with our first. We lived in Seoul, South Korea at the time. We were coming back to the states to visit for Christmas vacation. I was less then enthused about enduring a long 20 hour travel time haul to Boston. I have to say, we flew on Korean Air and it was a wonderfu! From my experience the flight crew on international airlines take great care of their passengers, especially the pregnant women!
Do you regret missing overseas opportunities and wish you had gotten pregnant after EIS?
(From Author Stacie Dunkle) Not at all. EIS is about developing skills to respond to disease outbreaks that occur both here in the US as well as internationally. It’s very important to me to have a balance of career and family. Thank you for your question!
We are currently a year into a journey the length of the Andes from Ushuaia to the the north of Colombia, and my wife became pregnant in Peru. We are frustrated by the lack of coherent advice available. Apart from the not at all helpful ‘Don’t go if you are pregnant’ which you encountered, we have read widely differing reports of risk levels in Colombia. Advice as to the safe altitudes varies from ‘anything above 800m to >1700m. The British seem to have Colombia as low risk for chloroquine resistant malaria anywhere outside the Amazon. The WHO have high risk areas in the Amazon AND along the pacific coast with particular pockets of danger near Panama and Venezuela. As we are travelling by vehicle the oft trotted out advice that you are safe in all cities is of no comfort to us as we have to drive between them through rural areas.
Another dilemma is what anti-malarials are safe in pregnancy. Mixed reports on Mefloquine although the CDC have just come out saying it’s safe (reflecting new FDA guidelines) despite reports of teratogenicity in rats. We tried the top three hospitals in Quito and none had anything but chloroquine despite Ecuador also having choloroquine resistant malaria. The official line from all of them is denial…that there is no malaria in Ecuador. We’re finding the same thing in Colombia…”As long as you don’t go to the jungle there’s no malaria here. Just use DEET (also contraindicated in pregnancy) and wear long sleeves and don’t go out after dusk”. My experience of the tropics is that determined mosquitoes are rarely put off by repellents for long.
If we can find mefloquine we’ll take it but we have major concerns. Data may show that there is little chance of teratogenicity or increased risk of still birth but it is well known for serious neurological side effects such as anxiety and depression and it does cross the placenta. So what affect does it have on a developing brain? No one knows. We have also read that chloroquine along with proguanil might be a safe alternative although proguanil suppresses folic acid so the advice is to take 5mg Folic acid a day which is basically an entire packet at the dosage strengths available here! It may be a blind alley anyway as we haven’t seen proguanil on sale here yet.
We are also facing up to the fact that we may also have to alter our plans due to lack of clear guidance and safeguards.
On the plus side Echo scans are very easy to get here and in these days of internet getting hold of literature on pregnancy has been no problem. Nutrition has been an problematic issue. Fruit is plentiful here which is great but salads are hard to find and even when they are they might have been washed in unsafe water. Concerns about picking up food poisoning are ramped up considerably since we knew about the pregnancy. Any further advice you can send our way would be greatly appreciated.
Sincerely Glyn Griffiths
I felt I had to be exra careful because I was an older mom. Absolutely no risk taking for me because this might have been my last chance to be a mother.
I was also lucky to be married to a man who felt I should be an at-home mom. We gave up a lot of economic advantages but we have felt it was well worth it over the years. I have worked at home on Fetal Alcohol Syndrome information retrieval for the past 15 years.
Please do not drink before, during or after your pregnancy if you are nursing. The behavioral problems caused by prenatal alcohol exposure are not worth the risk.
I think you made a good decision by cancelling your trip due to risks in the destination country.
After reading your experience I’m more in a dilema than I was before. I have a planned trip since last year to the US. It will be the end of this March and my pregnancy will come to week 11. Everything is set, ticket bought, accomodation paid and seminar fee also paid (I will attend a week seminar). My concerns are related to long travel (22hours from my country, Indonesia) and how expensive it would be in the US if anything happens. This is my first pregnancy aswell and I’m 36-year old mother to be. I don’t want to risk it…but I’m still torn in two..go or not.
@Peggy Oba: Thanks a lot for your comments and wise words.
This is a helpful story. I will be three months pregnant and am planning to travel to Galapagos and Peru with my partner and two year old. These are work trips and I really want to go, but still trying to weigh the risks. I had a normal pregnancy with my son but am considered high-risk because I am 38.
I was pregnant once and once was enough. In labor for 50 hours. I could not even imagine flying when pregnant, but “to each his own.” I asked doctor (I had already decided on a tubal after that pregnancy) if a “second would be as bad.” He said: “It could be worse.” Thus, the tubal and I have never, ever regretted it. Only wanted one child.
As an international business executive …extensive travel comes with the territory. I am an “older mom” in that my two year old son was born when I was 37. Presently, at the age of 39, my second son is due in the late Summer. I traveled fairly extensively with my now two year old and have trips to Amsterdam/London/Puerto Rico/Miami during my final trimester. The OB is completely fine with my travel and the airlines say that up to 36 weeks is fine.
With my first pregnancy, I lived in northern India. I took precautions to avoid malaria, typhus, TB, HIV, and food poisoning. I spent time in Amritsar and Delhi. My daughter is now 12 and healthy. I’m pregnant with my second and currently in Delhi, India, waiting to fly to the States for a holiday. Women here have babies, and healthy ones at that. If one takes precautions, traveling while pregnant is safe. We’ve lived in India for four years and not contracted maleria or Dengue fever. I don’t expect to now that I’m pregnant again. My point is that you can choose to be afraid or careful. Being afraid keeps you at home. Being careful allows you to make solid decisions and take calculated risks that lead can present opportunities.
I have planned to travel to India in my 13th week and return on 24th week of my pregnancy. This is my first pregnancy and I will be travelling alone. I am worried if it is safe to take a 22 hours flight and I want to know if something happens what are the services available on board. I spoke to airline but didn’t get satisfactory reply.
I am a student admitted already to do my masters in Cyprus from Africa, I just realized I will be a month pregnant when I travel. Please its really hard on me but please what advice have you for me. Am just 20 years old.
My sister has to travel out of the country in the coming week as she is pregnant I don’t want her to go at this time. She is 4 months pregnant, she anyway wants to go that is why I have booked tickets online using CouponZeta site but I still have that fear whether it is safe for her to travel at this time or not. After reading the above article I have that question am I doing any wrong thing allowing her to travel so long?
After reading your experience I’m more in a dilema than I was before. I have a planned trip since last year to the US. It will be the end of this March and my pregnancy will come to week 11. Everything is set, ticket bought, accomodation paid and seminar fee also paid (I will attend a week seminar). My concerns are related to long travel (22hours from my country, Indonesia) and how expensive it would be in the US if anything happens. This is my first pregnancy aswell and I’m 36-year old mother to be. I don’t want to risk it…but I’m still torn in two..go or not.
Post a Comment
Your email address will not be published. Required fields are marked *
To receive email updates about this page, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Flying while pregnant? Here’s what you need to know

Editors note: This guide has been updated with the latest information.
During pregnancy, seemingly harmless things like eating deli meat and cleaning your cat's litter box are suddenly off-limits, along with more obvious restrictions on sports like skiing and scuba diving.
But what about "grey area" activities like flying in an airplane?
There's no single set of guidelines governing air travel during pregnancy and every airline has different restrictions, timelines and requirements. Some airlines may also require a medical certificate from a primary attending doctor or midwife for air travel during the final months of pregnancy, though even that varies, with U.S. airlines typically offering more flexibility than international carriers.
For more TPG news delivered each morning to your inbox, sign up for our daily newsletter .
In the absence of clear guidelines, TPG turned to Dr. Nithya Gopal , a board-certified OB-GYN physician and the Director of OB-GYN services at Viva Eve in New York City, for her expert recommendations on safe air travel during pregnancy.
Here's what she had to say:
Is it safe to fly when you are pregnant?
There is no evidence of adverse pregnancy outcomes due to flying, according to Dr. Gopal.
"The general consensus is that it is safest to fly in the first and second trimesters," Dr. Gopal told The Points Guy. "While the first and third trimesters tend to be when the most obstetric emergencies are going to happen, I personally become more cautious with my patients after 32 weeks because of the increased risk for premature labor and the possibility of needing urgent medical attention when you are in the sky."

The most important thing you can do, no matter how far along you are in your pregnancy, is to consult with your healthcare provider before flying.
"Any time you are planning to fly during pregnancy , you should be having that conversation," Dr. Gopal said. Your provider will be familiar with any safety precautions you should take to ensure a safe and healthy flight.
Related: Guide to flying in each trimester of pregnancy
The airline you are flying may have its own cutoff, so you will want to confirm with it beforehand whether you will be allowed to fly if you are in (or nearing) your third trimester. We've included a chart below that outlines the rules for most major airline carriers.
What can you do to stay comfortable on a flight?

When you factor in morning sickness and general pregnancy discomfort with the increased risk for blood clots that all fliers need to be aware of, flying during pregnancy can be uncomfortable even when it is deemed safe.
Dr. Gopal shared her recommendations for addressing these common issues when you take to the (baby-) friendly skies during pregnancy. Her number one tip for staying comfortable while in flight is to wear compression socks to help maintain blood flow and reduce swelling in the legs.
In addition, "I also tell my patients to get up and move at least every hour when they are on the plane," Dr. Gopal said.
To prevent clotting, "some doctors may also prescribe a low-dose aspirin," she added. "It isn't something that is recommended by the American College of Obstetricians and Gynecologists (ACOG), but it isn't harmful, either."
If it's nausea or acid reflux that ail you, there are medications generally considered safe that you can take to alleviate your symptoms. These would be the same ones prescribed by your doctor for morning sickness, so speak with your provider before your flight to ensure you have what you need at the ready.
Dr. Gopal also advises wearing loose, unrestrictive clothing (along with your seatbelt, or course) and drinking extra fluids to counteract the pressurized air in the cabin and keep you hydrated.
"Over-the-counter Gas-X may also help with bloating that can happen as a result of the pressurized air," Dr. Gopal said.
Related: What happens when a baby is born in flight?
Must you speak with your healthcare provider before flying?

Even if your pregnancy is considered low-risk, it's always a smart idea to speak with your healthcare provider before flying. "There are a number of potential risks that go along with flying during pregnancy and those risks can change from week to week and month to month, so it's important to have that honest conversation with your doctor," Dr. Gopal said.
Related: Things You Should Do Before, During and After Flying to Stay Healthy
There are certain pregnancy conditions that may make flying more risky or unadvisable. If you are hypertensive, asthmatic or prone to clotting disorders, it's even more critical to speak with your doctor before flying.
Airline policies differ, but if you need documentation, it never hurts to include enough detail to satisfy the most stringent airline requirements.
"As with many things related to air travel, it's better to be safe than sorry," Dr. Gopal said. "It's definitely worth it, and sometimes necessary, to have medical documentation from your provider's office."
A thorough medical certificate or waiver should state:
- The number of weeks of pregnancy.
- The estimated delivery date.
- Whether the pregnancy is single or multiple.
- Whether there are any complications.
- That you are in good health and fit to travel through the date of your final flight.
Additionally, the certificate should be:
- Written on official clinic or hospital letterhead if possible.
- Signed by the doctor or attending midwife.
- Be dated no later than 72 hours before the departure date.
- Be written in clear, simple English.
Carry this certificate with you on your flight. Some airlines won't ask to see it, but others will. Some airlines also may have their own documentation requirements. See the chart below to find out which airlines require it.
Airline policies for pregnant women
Bottom line.

Even though it may be deemed safe, flying during pregnancy can be uncomfortable — and it is perfectly acceptable to implement your own cutoff for flying with your baby bump in tow. The majority of the time, though, flying is perfectly safe during pregnancy, providing that you follow the guidelines of the airline and your healthcare provider. Read on to learn more about traveling before, during and after pregnancy:
- What to expect in every trimester of pregnancy
- 4 tips for planning travel while planning a pregnancy
- Babymoon boom! These are the top 10 spots for a US getaway before the baby comes
- Flying with a baby checklist
Additional reporting by Katherine Fan and Tarah Chieffi.
Pregnancy travel insurance - here's what to know before you book

--> BY Jessica Humphries
Last updated . 20 December 2023
Relish the excitement of your travel plans with your blossoming baby bump by securing the right cover.
Enjoying a journey with a little one on the way? The thrill of travel is irresistible, but let’s face it – the logistics can pile up faster than you can say ‘jetlag’, and Mama – you’ve got enough on your plate. If your adventurous side still calls, despite having a baby on board, navigating the realm of travel insurance becomes a whole new adventure. Fear not, we’ve got everything you need to know about travel insurance when you’re pregnant right here.
Key things to consider before buying coverage
When you’re planning your trip with a baby on board, there are some things you’ll need to consider straight-up.
How far along are you?
We know you’ve heard the question a million times, but here’s where it really counts. When it comes to pregnancy and travel insurance, most insurers graciously cover single, uncomplicated pregnancies following natural conception. However, there’s a catch – the coverage window varies.

The best time to travel is within your second trimester.
Some providers extend their umbrella up to 30 weeks, while others gently fold it at 23 to 26 weeks pregnant. Most importantly, remember – the stork won’t deliver coverage for birth-related costs or newborn expenses. So, if you can, keep your window wide and travel within the sweet spot (more on that later).
Is pregnancy considered a ‘pre-existing medical condition’?
Thankfully, pregnancy isn’t generally considered a pre-existing medical condition when you’re obtaining travel insurance. If you’re under 26 weeks (at the time of travel) with just one bub on board, you may not need to declare it at all. However, honesty is key, especially if you’re dealing with a more complex pregnancy. Disclose the details to your insurer to make sure you’re covered.

Be prepared with pregnancy travel insurance for your safety.
What to look for in a pregnancy travel insurance policy
It’s time to dig into the details. Here’s what you’ll need to keep an eye out for in your travel insurance to make sure you and your bump have a smooth ride.

Travelling while pregnant can be a fulfilling experience. (Image: Josh Bean)
The benefits buffet
Navigating pregnancy with travel insurance is like entering an extensive buffet – enticing, filled with numerous options, and just a tad overwhelming. Yet, the crucial factor lies in the details. Delve into the fine print to ensure you grasp the details of the nitty gritty.

Tick off the benefits of your pregnancy coverage.
If you identify any gaps, ask your insurer about tailored policy add-ons for a personalised experience. Alternatively, explore other options that cater specifically to your unique pregnancy needs.
- Make sure your policy covers (on top of standard travel insurance staples):
- Unforeseen pregnancy challenges.
- Emergency medical coverage abroad: including expenses for unexpected illnesses, complications, or severe injuries related to your pregnancy.
- Trip cancellation protection.
- Around-the-clock travel assistance.

Make sure that your policy covers unexpected pregnancy challenges.
Cancellation considerations
If there’s ever a time when last-minute travel plans can swiftly change, it’s during pregnancy. Your pregnancy might even be a time when you consider locking in your coverage before finalising your booking. Locking in coverage ensures that in the event of unexpected pregnancy complications leading to a trip cancellation, you’re covered – no strings attached.

Consider last-minute travel changes especially when you’re travelling with a child.
Find out what’s excluded
Navigate the exclusion territory carefully. Be aware that certain conditions, like conception through IVF, expecting multiples, or planning travel after the approved gestational weeks, may lead to limited or no coverage.
Common exclusions:
- Conception through assisted reproduction (IVF).
- Seeking reimbursement for childbirth or newborn healthcare expenses if you give birth on your trip.
- Travelling against medical advice from your doctor.
- Expecting twins (or more!).
- Planning travel beyond the approved weeks according to your provider.
- Dealing with pregnancy complications (previous miscarriages or premature labour, gestational diabetes etc.) – disclose them to avoid issues.
- Routine pregnancy check-ups abroad.
Remember, some exclusions can be lifted with premium payments or a medical assessment.
Trimester travel tactics: A travel roadmap for every stage
When planning your travels, take your pregnancy stage into account for a seamlessly enjoyable journey tailored to each trimester.
First-trimester trail
The first 12 weeks are the opening act of your pregnancy journey. While generally safe for travel, be aware that morning sickness might steal the show. Consider scheduling your adventures post-week 12 to dodge any queasy interludes.

You may experience morning sickness during your first trimester.
Second-trimester bliss
The perfect time for a babymoon, your second trimester offers you a golden ticket to travel bliss, sans complications. Chat to your doctor, pack your bags, and make the most of this worry-free window.

Always check with your doctor for any pregnancy reminders before travelling. (Image: Lucas Favre)
Third-trimester reality check
Some airlines may give side-eye glances if you’re deep into the third trimester, and many travel insurance providers will cap their coverage around the 26-week mark. If leisure is the plan, think twice before boarding that flight.

It’s best to travel with a companion.
As you embark on this exciting journey with a baby on board, remember that a well-informed approach to travel insurance during pregnancy is your ticket to peace of mind. From navigating coverage windows to crafting your personalised pregnancy passport and considering trimester-specific tactics, your wanderlust need not be put on hold. Embrace the adventure, plan wisely, and savour every moment of this unique chapter in your globetrotting story. Safe travels, mama!

Travelling during pregnancy can be your first milestone as a family.
For more tips and advice, read our travel insurance hub to help you navigate the ins and outs of what to do before you head overseas.
Leave your comment, cancel reply.
Save my name, email, and website in this browser for the next time I comment.
You might also like

Ski holiday insurance – the facts you need to know
Heading to the hills? Stay fancy-free in a winter wonderland by decoding the ins and outs of ski travel insurance first. As majestic snowflakes blank...

Everything you need to know about cruise insurance
Before setting sail, getting the lowdown on cruise insurance is a must. Standard travel insurance might not cut it, so making sure you have the right ...

10 ways to save money on your travel insurance
Dreaming of your next getaway? While travel insurance is a must, there’s no need to break the bank. Ready to make your travel dreams a reality but ...

How to get travel insurance when you have a medical condition
Don’t let pre-existing conditions be a roadblock to your wanderlust. Learn the ropes of securing the right travel insurance for a hassle-free advent...

Here’s what you’ll really want from your insurer when travel goes wrong
Turn hiccups into manageable adventures by finding the coverage you’ll wish for when plans hit a bump. Embarking on a travel adventure is a journey...

Here’s why travel will return bigger and better than before
Don’t cry because the ‘best years’ are behind you; smile because we now have the tools to travel bigger and better than ever before, writes Dilv...
Read our research on: Abortion | Podcasts | Election 2024
Regions & Countries
What the data says about abortion in the u.s..
Pew Research Center has conducted many surveys about abortion over the years, providing a lens into Americans’ views on whether the procedure should be legal, among a host of other questions.
In a Center survey conducted nearly a year after the Supreme Court’s June 2022 decision that ended the constitutional right to abortion , 62% of U.S. adults said the practice should be legal in all or most cases, while 36% said it should be illegal in all or most cases. Another survey conducted a few months before the decision showed that relatively few Americans take an absolutist view on the issue .
Find answers to common questions about abortion in America, based on data from the Centers for Disease Control and Prevention (CDC) and the Guttmacher Institute, which have tracked these patterns for several decades:
How many abortions are there in the U.S. each year?
How has the number of abortions in the u.s. changed over time, what is the abortion rate among women in the u.s. how has it changed over time, what are the most common types of abortion, how many abortion providers are there in the u.s., and how has that number changed, what percentage of abortions are for women who live in a different state from the abortion provider, what are the demographics of women who have had abortions, when during pregnancy do most abortions occur, how often are there medical complications from abortion.
This compilation of data on abortion in the United States draws mainly from two sources: the Centers for Disease Control and Prevention (CDC) and the Guttmacher Institute, both of which have regularly compiled national abortion data for approximately half a century, and which collect their data in different ways.
The CDC data that is highlighted in this post comes from the agency’s “abortion surveillance” reports, which have been published annually since 1974 (and which have included data from 1969). Its figures from 1973 through 1996 include data from all 50 states, the District of Columbia and New York City – 52 “reporting areas” in all. Since 1997, the CDC’s totals have lacked data from some states (most notably California) for the years that those states did not report data to the agency. The four reporting areas that did not submit data to the CDC in 2021 – California, Maryland, New Hampshire and New Jersey – accounted for approximately 25% of all legal induced abortions in the U.S. in 2020, according to Guttmacher’s data. Most states, though, do have data in the reports, and the figures for the vast majority of them came from each state’s central health agency, while for some states, the figures came from hospitals and other medical facilities.
Discussion of CDC abortion data involving women’s state of residence, marital status, race, ethnicity, age, abortion history and the number of previous live births excludes the low share of abortions where that information was not supplied. Read the methodology for the CDC’s latest abortion surveillance report , which includes data from 2021, for more details. Previous reports can be found at stacks.cdc.gov by entering “abortion surveillance” into the search box.
For the numbers of deaths caused by induced abortions in 1963 and 1965, this analysis looks at reports by the then-U.S. Department of Health, Education and Welfare, a precursor to the Department of Health and Human Services. In computing those figures, we excluded abortions listed in the report under the categories “spontaneous or unspecified” or as “other.” (“Spontaneous abortion” is another way of referring to miscarriages.)
Guttmacher data in this post comes from national surveys of abortion providers that Guttmacher has conducted 19 times since 1973. Guttmacher compiles its figures after contacting every known provider of abortions – clinics, hospitals and physicians’ offices – in the country. It uses questionnaires and health department data, and it provides estimates for abortion providers that don’t respond to its inquiries. (In 2020, the last year for which it has released data on the number of abortions in the U.S., it used estimates for 12% of abortions.) For most of the 2000s, Guttmacher has conducted these national surveys every three years, each time getting abortion data for the prior two years. For each interim year, Guttmacher has calculated estimates based on trends from its own figures and from other data.
The latest full summary of Guttmacher data came in the institute’s report titled “Abortion Incidence and Service Availability in the United States, 2020.” It includes figures for 2020 and 2019 and estimates for 2018. The report includes a methods section.
In addition, this post uses data from StatPearls, an online health care resource, on complications from abortion.
An exact answer is hard to come by. The CDC and the Guttmacher Institute have each tried to measure this for around half a century, but they use different methods and publish different figures.
The last year for which the CDC reported a yearly national total for abortions is 2021. It found there were 625,978 abortions in the District of Columbia and the 46 states with available data that year, up from 597,355 in those states and D.C. in 2020. The corresponding figure for 2019 was 607,720.
The last year for which Guttmacher reported a yearly national total was 2020. It said there were 930,160 abortions that year in all 50 states and the District of Columbia, compared with 916,460 in 2019.
- How the CDC gets its data: It compiles figures that are voluntarily reported by states’ central health agencies, including separate figures for New York City and the District of Columbia. Its latest totals do not include figures from California, Maryland, New Hampshire or New Jersey, which did not report data to the CDC. ( Read the methodology from the latest CDC report .)
- How Guttmacher gets its data: It compiles its figures after contacting every known abortion provider – clinics, hospitals and physicians’ offices – in the country. It uses questionnaires and health department data, then provides estimates for abortion providers that don’t respond. Guttmacher’s figures are higher than the CDC’s in part because they include data (and in some instances, estimates) from all 50 states. ( Read the institute’s latest full report and methodology .)
While the Guttmacher Institute supports abortion rights, its empirical data on abortions in the U.S. has been widely cited by groups and publications across the political spectrum, including by a number of those that disagree with its positions .
These estimates from Guttmacher and the CDC are results of multiyear efforts to collect data on abortion across the U.S. Last year, Guttmacher also began publishing less precise estimates every few months , based on a much smaller sample of providers.
The figures reported by these organizations include only legal induced abortions conducted by clinics, hospitals or physicians’ offices, or those that make use of abortion pills dispensed from certified facilities such as clinics or physicians’ offices. They do not account for the use of abortion pills that were obtained outside of clinical settings .
(Back to top)
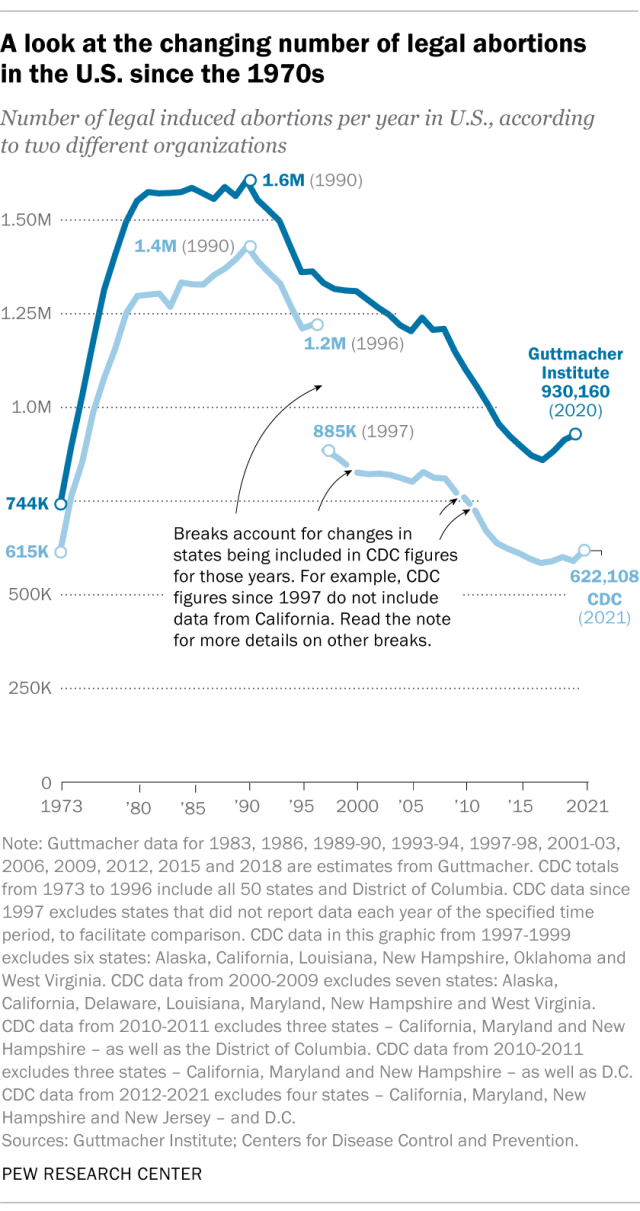
The annual number of U.S. abortions rose for years after Roe v. Wade legalized the procedure in 1973, reaching its highest levels around the late 1980s and early 1990s, according to both the CDC and Guttmacher. Since then, abortions have generally decreased at what a CDC analysis called “a slow yet steady pace.”
Guttmacher says the number of abortions occurring in the U.S. in 2020 was 40% lower than it was in 1991. According to the CDC, the number was 36% lower in 2021 than in 1991, looking just at the District of Columbia and the 46 states that reported both of those years.
(The corresponding line graph shows the long-term trend in the number of legal abortions reported by both organizations. To allow for consistent comparisons over time, the CDC figures in the chart have been adjusted to ensure that the same states are counted from one year to the next. Using that approach, the CDC figure for 2021 is 622,108 legal abortions.)
There have been occasional breaks in this long-term pattern of decline – during the middle of the first decade of the 2000s, and then again in the late 2010s. The CDC reported modest 1% and 2% increases in abortions in 2018 and 2019, and then, after a 2% decrease in 2020, a 5% increase in 2021. Guttmacher reported an 8% increase over the three-year period from 2017 to 2020.
As noted above, these figures do not include abortions that use pills obtained outside of clinical settings.
Guttmacher says that in 2020 there were 14.4 abortions in the U.S. per 1,000 women ages 15 to 44. Its data shows that the rate of abortions among women has generally been declining in the U.S. since 1981, when it reported there were 29.3 abortions per 1,000 women in that age range.
The CDC says that in 2021, there were 11.6 abortions in the U.S. per 1,000 women ages 15 to 44. (That figure excludes data from California, the District of Columbia, Maryland, New Hampshire and New Jersey.) Like Guttmacher’s data, the CDC’s figures also suggest a general decline in the abortion rate over time. In 1980, when the CDC reported on all 50 states and D.C., it said there were 25 abortions per 1,000 women ages 15 to 44.
That said, both Guttmacher and the CDC say there were slight increases in the rate of abortions during the late 2010s and early 2020s. Guttmacher says the abortion rate per 1,000 women ages 15 to 44 rose from 13.5 in 2017 to 14.4 in 2020. The CDC says it rose from 11.2 per 1,000 in 2017 to 11.4 in 2019, before falling back to 11.1 in 2020 and then rising again to 11.6 in 2021. (The CDC’s figures for those years exclude data from California, D.C., Maryland, New Hampshire and New Jersey.)
The CDC broadly divides abortions into two categories: surgical abortions and medication abortions, which involve pills. Since the Food and Drug Administration first approved abortion pills in 2000, their use has increased over time as a share of abortions nationally, according to both the CDC and Guttmacher.
The majority of abortions in the U.S. now involve pills, according to both the CDC and Guttmacher. The CDC says 56% of U.S. abortions in 2021 involved pills, up from 53% in 2020 and 44% in 2019. Its figures for 2021 include the District of Columbia and 44 states that provided this data; its figures for 2020 include D.C. and 44 states (though not all of the same states as in 2021), and its figures for 2019 include D.C. and 45 states.
Guttmacher, which measures this every three years, says 53% of U.S. abortions involved pills in 2020, up from 39% in 2017.
Two pills commonly used together for medication abortions are mifepristone, which, taken first, blocks hormones that support a pregnancy, and misoprostol, which then causes the uterus to empty. According to the FDA, medication abortions are safe until 10 weeks into pregnancy.
Surgical abortions conducted during the first trimester of pregnancy typically use a suction process, while the relatively few surgical abortions that occur during the second trimester of a pregnancy typically use a process called dilation and evacuation, according to the UCLA School of Medicine.
In 2020, there were 1,603 facilities in the U.S. that provided abortions, according to Guttmacher . This included 807 clinics, 530 hospitals and 266 physicians’ offices.
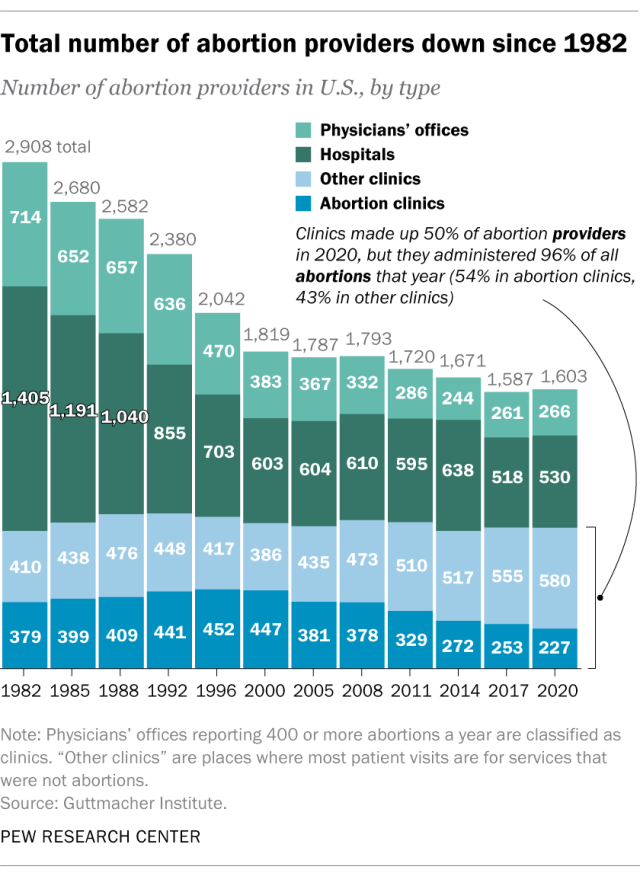
While clinics make up half of the facilities that provide abortions, they are the sites where the vast majority (96%) of abortions are administered, either through procedures or the distribution of pills, according to Guttmacher’s 2020 data. (This includes 54% of abortions that are administered at specialized abortion clinics and 43% at nonspecialized clinics.) Hospitals made up 33% of the facilities that provided abortions in 2020 but accounted for only 3% of abortions that year, while just 1% of abortions were conducted by physicians’ offices.
Looking just at clinics – that is, the total number of specialized abortion clinics and nonspecialized clinics in the U.S. – Guttmacher found the total virtually unchanged between 2017 (808 clinics) and 2020 (807 clinics). However, there were regional differences. In the Midwest, the number of clinics that provide abortions increased by 11% during those years, and in the West by 6%. The number of clinics decreased during those years by 9% in the Northeast and 3% in the South.
The total number of abortion providers has declined dramatically since the 1980s. In 1982, according to Guttmacher, there were 2,908 facilities providing abortions in the U.S., including 789 clinics, 1,405 hospitals and 714 physicians’ offices.
The CDC does not track the number of abortion providers.
In the District of Columbia and the 46 states that provided abortion and residency information to the CDC in 2021, 10.9% of all abortions were performed on women known to live outside the state where the abortion occurred – slightly higher than the percentage in 2020 (9.7%). That year, D.C. and 46 states (though not the same ones as in 2021) reported abortion and residency data. (The total number of abortions used in these calculations included figures for women with both known and unknown residential status.)
The share of reported abortions performed on women outside their state of residence was much higher before the 1973 Roe decision that stopped states from banning abortion. In 1972, 41% of all abortions in D.C. and the 20 states that provided this information to the CDC that year were performed on women outside their state of residence. In 1973, the corresponding figure was 21% in the District of Columbia and the 41 states that provided this information, and in 1974 it was 11% in D.C. and the 43 states that provided data.
In the District of Columbia and the 46 states that reported age data to the CDC in 2021, the majority of women who had abortions (57%) were in their 20s, while about three-in-ten (31%) were in their 30s. Teens ages 13 to 19 accounted for 8% of those who had abortions, while women ages 40 to 44 accounted for about 4%.
The vast majority of women who had abortions in 2021 were unmarried (87%), while married women accounted for 13%, according to the CDC , which had data on this from 37 states.
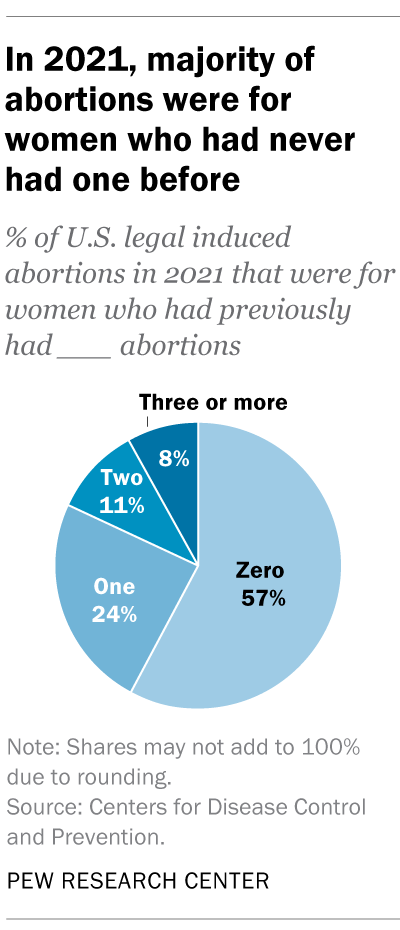
In the District of Columbia, New York City (but not the rest of New York) and the 31 states that reported racial and ethnic data on abortion to the CDC , 42% of all women who had abortions in 2021 were non-Hispanic Black, while 30% were non-Hispanic White, 22% were Hispanic and 6% were of other races.
Looking at abortion rates among those ages 15 to 44, there were 28.6 abortions per 1,000 non-Hispanic Black women in 2021; 12.3 abortions per 1,000 Hispanic women; 6.4 abortions per 1,000 non-Hispanic White women; and 9.2 abortions per 1,000 women of other races, the CDC reported from those same 31 states, D.C. and New York City.
For 57% of U.S. women who had induced abortions in 2021, it was the first time they had ever had one, according to the CDC. For nearly a quarter (24%), it was their second abortion. For 11% of women who had an abortion that year, it was their third, and for 8% it was their fourth or more. These CDC figures include data from 41 states and New York City, but not the rest of New York.
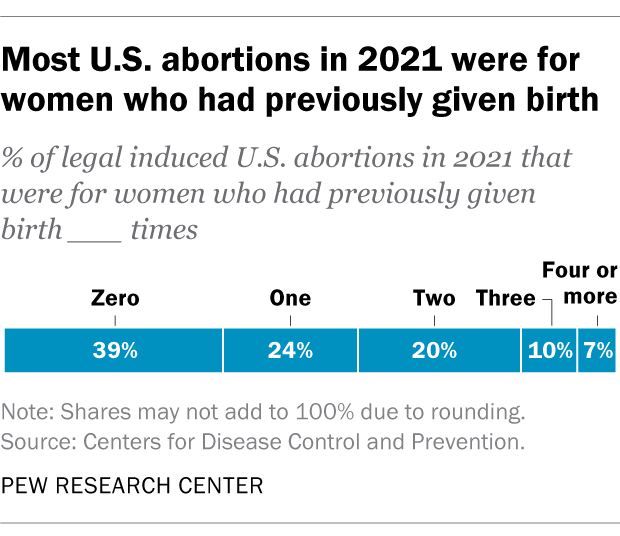
Nearly four-in-ten women who had abortions in 2021 (39%) had no previous live births at the time they had an abortion, according to the CDC . Almost a quarter (24%) of women who had abortions in 2021 had one previous live birth, 20% had two previous live births, 10% had three, and 7% had four or more previous live births. These CDC figures include data from 41 states and New York City, but not the rest of New York.
The vast majority of abortions occur during the first trimester of a pregnancy. In 2021, 93% of abortions occurred during the first trimester – that is, at or before 13 weeks of gestation, according to the CDC . An additional 6% occurred between 14 and 20 weeks of pregnancy, and about 1% were performed at 21 weeks or more of gestation. These CDC figures include data from 40 states and New York City, but not the rest of New York.
About 2% of all abortions in the U.S. involve some type of complication for the woman , according to an article in StatPearls, an online health care resource. “Most complications are considered minor such as pain, bleeding, infection and post-anesthesia complications,” according to the article.
The CDC calculates case-fatality rates for women from induced abortions – that is, how many women die from abortion-related complications, for every 100,000 legal abortions that occur in the U.S . The rate was lowest during the most recent period examined by the agency (2013 to 2020), when there were 0.45 deaths to women per 100,000 legal induced abortions. The case-fatality rate reported by the CDC was highest during the first period examined by the agency (1973 to 1977), when it was 2.09 deaths to women per 100,000 legal induced abortions. During the five-year periods in between, the figure ranged from 0.52 (from 1993 to 1997) to 0.78 (from 1978 to 1982).
The CDC calculates death rates by five-year and seven-year periods because of year-to-year fluctuation in the numbers and due to the relatively low number of women who die from legal induced abortions.
In 2020, the last year for which the CDC has information , six women in the U.S. died due to complications from induced abortions. Four women died in this way in 2019, two in 2018, and three in 2017. (These deaths all followed legal abortions.) Since 1990, the annual number of deaths among women due to legal induced abortion has ranged from two to 12.
The annual number of reported deaths from induced abortions (legal and illegal) tended to be higher in the 1980s, when it ranged from nine to 16, and from 1972 to 1979, when it ranged from 13 to 63. One driver of the decline was the drop in deaths from illegal abortions. There were 39 deaths from illegal abortions in 1972, the last full year before Roe v. Wade. The total fell to 19 in 1973 and to single digits or zero every year after that. (The number of deaths from legal abortions has also declined since then, though with some slight variation over time.)
The number of deaths from induced abortions was considerably higher in the 1960s than afterward. For instance, there were 119 deaths from induced abortions in 1963 and 99 in 1965 , according to reports by the then-U.S. Department of Health, Education and Welfare, a precursor to the Department of Health and Human Services. The CDC is a division of Health and Human Services.
Note: This is an update of a post originally published May 27, 2022, and first updated June 24, 2022.

Sign up for our weekly newsletter
Fresh data delivered Saturday mornings
Key facts about the abortion debate in America
Public opinion on abortion, three-in-ten or more democrats and republicans don’t agree with their party on abortion, partisanship a bigger factor than geography in views of abortion access locally, do state laws on abortion reflect public opinion, most popular.
About Pew Research Center Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .

IMAGES
VIDEO
COMMENTS
During a healthy pregnancy, occasional air travel is almost always safe. Most airlines allow you to fly domestically until about 36 weeks of pregnancy. Your ob-gyn can provide proof of your due date if you need it. If you are planning an international flight, the cut-off for traveling may be earlier.
Download any apps you use for renting cars and accessing boarding passes before you leave so you can easily reschedule things in the event of a last-minute cancellation. If you're flying during your third trimester, be sure to call the airline to check about the cutoff week for pregnancy travel. A note from your doctor that says you're ...
"The third trimester is generally more uncomfortable, it's a good idea to be near your healthcare provider as your due date approaches." ... In some cases, like international travel, you may ...
Generally, women are not allowed to travel by air after 36 weeks for domestic travel, and after 28 to 35 weeks for international travel. The decision on whether to travel and how far to travel at any time during pregnancy should be a joint decision between you and your healthcare provider or midwife. According to the CDC, pregnant women with ...
If you're taking an international flight, you may be prohibited from flying even earlier in your pregnancy. In general, the best time to travel while pregnant is mid-pregnancy (weeks 14 through 18). During the first trimester, you may feel too nauseated and tired to withstand long trips — or enjoy yourself once you get where you're going.
During the third trimester (28 to 40 weeks), many healthcare providers and midwives advise staying within a 300-mile radius of home because of potential problems, such as high blood pressure, phlebitis, and false or preterm labor. Generally, women are not allowed to travel by air after 36 weeks for domestic travel, and after 28 to 35 weeks for ...
If your health care provider says it's okay for you to fly, and your plans are flexible, the best time to travel by air might be during the second trimester. The risks of common pregnancy emergencies are lowest during that time. When you fly: Buckle up. During the trip, keep your seatbelt fastened when you are seated, and secure it under your ...
Pregnant travelers should avoid travel to areas with malaria, as it can be more severe in pregnant women. Malaria increases the risk for serious pregnancy problems, including premature birth, miscarriage, and stillbirth. If you must travel to an area with malaria, talk to your doctor about taking malaria prevention medicine.
Planning for Emergency Care. Obstetric emergencies are often sudden and life-threatening. Advise all pregnant travelers (but especially those in their third trimester or otherwise at high risk) to identify, in advance, international medical facilities at their destination(s) capable of managing complications of pregnancy, delivery (including by caesarean section), and neonatal problems.
The American College of Obstetricians and Gynecologists says the safest time for a woman to travel is in the second trimester of her pregnancy, from 14 to 28 weeks. This is the time when you will feel your best. You are also at the lowest risk for spontaneous abortion (miscarriage) or premature labor. During the third trimester (28 to 40 weeks ...
Most people don't realize that you can still travel just fine in the third trimester. Despite what you can read in many bias articles and forums, you can fly freely until 36 weeks. Naturally, assuming that you have an uncomplicated pregnancy. While most people might prefer to stay at home and nest in the third trimester, I didn't feel that ...
Travel during the first and second trimesters is usually considered to be safe, although it may be more tiring than usual. Traveling during the first trimester of pregnancy may pose a few challenges, especially if you're experiencing morning sickness, nausea, or fatigue. And the risk of bleeding or miscarriage is the greatest during these months.
However, travel plans during the third trimester can often be accommodated as well (unless you're cruising, but we'll get into that). Restrictions on Plane Travel During Pregnancy. ... While this is most important for international travel, it may need to be considered for travel within your country as well (like, with air conditions with ...
It should generally be avoided in the third trimester, but at other times it can be an enjoyable way of going a long distance. Traveling by train offers the convenience of a bathroom when you need it, comfortable seats and the ability to walk around whenever needed. Boat traveling is also okay during the first two trimesters.
The beginning and end of the third trimester are quite different. Changes come even more quickly in the third trimester. You enter the third trimester about 28 weeks pregnant and end it with a newborn. This means that types of travel that are possible at 27 and 28 weeks pregnant may be inadvisable, or even prohibited, at 37 and 38 weeks pregnant.
For the third trimester, one unlikely travel essential hero is flushable wet wipes, which make bathroom trips more soothing for those tender parts. ... Don't overpay: Save big on international ...
Travel During Pregnancy. As long as there are no identified complications or concerns with your pregnancy, it is generally safe to travel during your pregnancy. The ideal time to travel during pregnancy is the second trimester. In most cases, you are past the morning sickness of the first trimester and several weeks from the third stage of ...
The second trimester is widely considered the safest time to travel during pregnancy. Many of the risks of your first trimester will have passed by then, as well as some of the more challenging symptoms. However, the risk of the third trimester, such as the risk of preterm delivery, hasn't kicked in yet.
When my third trimester arrived, I was offered an opportunity to travel to Lima, Peru to attend a training summit. ... International travel is risky at any point during pregnancy, since both travel and pregnancy can be unpredictable. Although CDC and health care providers can provide knowledge, guidance, and recommendations, it is up to each ...
Virgin Australia. No restrictions. Travel permitted; requires a medical certificate dated within 10 days of departure date once you reach 28 weeks. For flights longer than four hours, travel is not permitted after 36 weeks of pregnancy (32 weeks if pregnant with multiples), or within 48 hours of normal vaginal delivery.
Occasional air travel during pregnancy is generally safe. Recent cohort studies suggest no increase in adverse pregnancy outcomes for occasional air travelers 1 2. Most commercial airlines allow pregnant women to fly up to 36 weeks of gestation. Some restrict pregnant women from international flights earlier in gestation and some require ...
When it comes to pregnancy and travel insurance, most insurers graciously cover single, uncomplicated pregnancies following natural conception. However, there's a catch - the coverage window varies. The best time to travel is within your second trimester. Some providers extend their umbrella up to 30 weeks, while others gently fold it at 23 ...
International Arabic ... Travel Destinations ... openly support restrictions even in the third trimester — or pivot to the border or the economy.
The vast majority of abortions occur during the first trimester of a pregnancy. In 2021, 93% of abortions occurred during the first trimester - that is, at or before 13 weeks of gestation, according to the CDC. An additional 6% occurred between 14 and 20 weeks of pregnancy, and about 1% were performed at 21 weeks or more of gestation.