Mpox is on the rise: Who's eligible for a vaccine, and do you need a booster?
Mpox, formally known as Monkeypox, cases are on the rise, CDC says.
Mpox, formerly known as monkeypox, cases are on the rise here in the U.S., with nearly double the number of infections compared to the same time last year, according to Centers for Disease Control and Prevention data.
While the magnitude of the outbreak experienced in 2022 – where national cases topped 32,000 – is largely over, some high-risk groups need to continue taking precautions, experts say.
"Most of the cases that we're seeing reported are either unvaccinated or under-vaccinated, meaning they either never received a vaccine, or they only got one dose," Dr. Jenni McQuiston, deputy director of the CDC's high consequence pathogens and pathology division told ABC News.
The Jynneos vaccine comes in two doses and is recommended for those who have been exposed to someone with mpox as well as those who had a sex partner in the past 2 weeks who was infected. There are currently no recommendations for a booster. Locations offering the free vaccine can be found on the CDC websit e.
Others eligible for the shot are those who identify as gay, bisexual, or a man who has sex with other men who have had more than one sexual partner or been diagnosed with more than one sexually transmitted disease in the past six months. Those with immune-compromising conditions, such as HIV, are also eligible.

"Current guidance aims to curb this increase by targeting vaccination efforts toward high-risk groups and individuals with potential exposure to mpox, underscoring the importance of these preventive measures in our public health response," said Dr. John Brownstein, chief innovation officer at Boston Children's Hospital and an ABC News contributor.

MORE: Mpox cases nearly double what they were at the same time last year
While the mpox virus first started spreading among gay and bisexual men as well as certain other groups in the initial outbreak, the virus does not discriminate, experts say. It will spread between any two people.
Like many vaccines, the shot primarily works to protect against severe illness, though it may not guarantee avoiding infection. It typically takes about two weeks after the second dose to reach full protection.
"Vaccines don't always 100% prevent disease, they ultimately reduce the severity of disease. So, seeing people contract mpox after vaccination is not unexpected. But we have seen less severe disease in the majority of patients with mpox in this current outbreak," Dr. Richard Silvera, associate program director of the infectious diseases fellowship and assistant professor of medicine at the Icahn School of Medicine at Mount Sinai told ABC News.
The vaccine is typically given in two doses, 28 days apart. Those who only received one shot should receive their second dose regardless of when they received their first to maximize protection, experts say.
"They're not considered fully vaccinated until they have at least two doses. They don't need to start over or repeat it. They just need to get that second dose," McQuiston said.
"We are recommending that you go ahead and get that second dose no matter how much time has elapsed [since your first dose], McQuiston added.
Related Stories

Aid workers killed in Gaza: World Central Kitchen
- Apr 2, 11:39 PM

Thousands rally in India capital to challenge Modi
- Mar 31, 5:00 AM

Caitlin Clark set for final bow of NCAA career
- Apr 6, 1:01 AM
Those who previously received both shots are considered fully vaccinated. Public health authorities continue to investigate if a booster dose may be necessary in the future to bolster protection.
"We have some long-term efficacy studies that are ongoing and those are planned over the next several months. But right now, only one in four individuals for whom the vaccine is recommended, in terms of them being potentially at risk for mpox, have gotten fully vaccinated," McQuiston said.
Early research indicates that antibodies from vaccination decline one year after getting the shot, according to preliminary data being presented at the European Congress of Clinical Microbiology and Infectious Diseases conference in late April. Scientists studied about 100 people finding that over 40% had a detectable loss in antibodies one year after vaccination.
There are currently no concerns with vaccine supply, according to McQuiston. Dr. Silvera notes he has been helping people catch up on their vaccinations by providing a first or second dose.
New York City is currently dealing with triple the number of cases the city saw at the same time last year. The city is not experiencing any vaccine supply issues, according to a spokesperson for the NYC Department of Health.
The CDC sent out an alert to medical providers in December to look out for travelers into the U.S. as a more lethal type of the mpox virus circulates in the Democratic Republic of Congo. No cases of that virus type have appeared in the U.S. so far.
"We're watching what's happening in the Democratic Republic of Congo carefully…and we are preparing here in the United States as best we can," McQuiston said.
Aside from getting vaccinated, there are other ways to protect yourself from getting infected, experts say.
"Those regular precautions are really kind of the bread and butter of how to deal with a public health outbreak. So, really just communicating with your partners, asking them how their health has been, asking if they've had any exposure they're concerned about." Silvera added.
"Try to avoid physical contact with someone who may have had a recent exposure or has a lesion at the time. And if you do have a lesion, it is worth seeking out care. We do have medications that can shorten the duration of illness," Silvera added.
An antiviral drug, known as TPOXX, is available and can help treat more severe mpox cases and is available to those who are more likely to get severely ill, like those with immune-compromising conditions.
"The increase in cases is a stark reminder of the virus's presence and the ongoing need for vigilance and preventive measures," Brownstein said.

Israel waging 'war against humanity': Jose Andres
- Apr 6, 9:24 PM

Iran vows to avenge Syria strike blamed on Israel
- Apr 6, 2:09 PM
ABC News Live
24/7 coverage of breaking news and live events
We’re sorry, this site is currently experiencing technical difficulties. Please try again in a few moments. Exception: request blocked
Situation in Haiti April 5, 2024
U.s. citizens in haiti, update january 10, 2024, information for u.s. citizens in the middle east.
- Travel Advisories |
- Contact Us |
- MyTravelGov |
Find U.S. Embassies & Consulates
Travel.state.gov, congressional liaison, special issuance agency, u.s. passports, international travel, intercountry adoption, international parental child abduction, records and authentications, popular links, travel advisories, mytravelgov, stay connected, legal resources, legal information, info for u.s. law enforcement, replace or certify documents.
Share this page:
Democratic Republic of the Congo Travel Advisory
Travel advisory july 31, 2023, democratic republic of the congo - level 3: reconsider travel.
Reissued with obsolete COVID-19 page links removed.
Reconsider travel to the Democratic Republic of Congo due to crime and civil unrest . Some areas have increased risk. Read the entire Travel Advisory.
Do Not Travel To :
- North Kivu province due to crime , civil unrest , terrorism , armed conflict , and kidnapping .
- Ituri province due to crime , civil unrest , terrorism , armed conflict , and kidnapping .
- The eastern DRC region and the three Kasai provinces (Kasai, Kasai-Oriental, Kasai-Central) due to crime , civil unrest , armed conflict and kidnapping .
Country Summary: Violent crime, such as armed robbery, armed home invasion, and assault, is common and local police lack resources to respond effectively to serious crime. Assailants may pose as police or security agents.
Demonstrations are common in many cities and some have turned violent. Police have at times responded with heavy-handed tactics that resulted in civilian casualties and arrests.
The U.S. government has extremely limited ability to provide emergency consular services to U.S. citizens outside of Kinshasa due to poor infrastructure and security conditions.
Read the country information page for additional information on travel to the Democratic Republic of the Congo.
If you decide to travel to the Democratic Republic of the Congo:
- Avoid demonstrations.
- Use caution when walking or driving.
- Always have a copy of your U.S. passport and DRC visa. Keep originals in a secure location. Carry your U.S. passport and DRC visa when crossing provincial borders or flying domestically.
- Enroll in the Smart Traveler Enrollment Program (STEP) to receive Alerts and make it easier to locate you in an emergency.
- Follow the Department of State on Facebook and Twitter .
- Review the Country Security Report for the DRC.
- Prepare a contingency plan for emergency situations. Review the Traveler’s Checklist.
- Visit the CDC page for the latest Travel Health Information related to your travel.
North Kivu Province – Level 4: Do Not Travel
Violent crime, such as murder, rape, kidnapping, and pillaging, continue throughout North Kivu province. Road travelers are frequently targeted for ambush, armed robbery, and kidnapping.
Demonstrations and large gatherings can occur throughout these regions, especially in urban areas, and escalate to violence. Extrajudicial mobs can form rapidly and turn violent, posing a threat to humanitarian aid workers and other personnel operating in the area.
Terrorist and armed groups operating in North Kivu province have attacked military and civilian targets and represent an ongoing threat to humanitarian aid workers and other NGO personnel operating in the area.
Armed groups, individuals, and military forces routinely clash with each other. Civilians are frequently targeted in attacks.
The U.S. government is unable to provide emergency consular services to U.S. citizens in North Kivu province as U.S. government travel to these areas is restricted.
Visit our website for Travel to High- Risk Areas.
Ituri Province – Level 4: Do Not Travel
Violent crime, such as murder, rape, kidnapping, and pillaging, continue throughout Ituri province. Road travelers are frequently targeted for ambush, armed robbery, and kidnapping.
Terrorist and armed groups operating in Ituri province have attacked military and civilian targets and represent an ongoing threat to humanitarian aid workers and other NGO personnel operating in the area.
The U.S. government is unable to provide emergency consular services to U.S. citizens in Ituri province as U.S. government travel to these areas is restricted.
Visit our website for Travel to High-Risk Areas .
Eastern DRC Region and the Three Kasai Provinces – Level 4: Do Not Travel
Violent crime, such as murder, rape, kidnapping, and pillaging, continue throughout South Kivu, Tanganyika, Haut Lomami, Bas-Uele, and Haut-Uele and three Kasai provinces of Kasai Oriental, Kasai Central, and Kasai. Road travelers are frequently targeted for ambush, armed robbery, and kidnapping.
The U.S. government is unable to provide emergency consular services to U.S. citizens in eastern DRC and these provinces, as U.S. government travel to these regions is restricted.
Travel Advisory Levels
Assistance for u.s. citizens, democratic republic of the congo (d.r.c.) map, search for travel advisories, external link.
You are about to leave travel.state.gov for an external website that is not maintained by the U.S. Department of State.
Links to external websites are provided as a convenience and should not be construed as an endorsement by the U.S. Department of State of the views or products contained therein. If you wish to remain on travel.state.gov, click the "cancel" message.
You are about to visit:

- High contrast
- Press Centre
Search UNICEF
More than 1.7 million covid-19 vaccines arrive in the democratic republic of congo.

KINSHASA, 03 MARCH 2021 – More than 1.7 million doses of COVID-19 vaccines have arrived in Kinshasa, the capital of the DRC. They were shipped to the country through COVAX, an alliance comprising the Coalition for Epidemic Preparedness Innovations (CEPI), Gavi, the Vaccine Alliance, and the World Health Organisation (WHO) working in partnership with UNICEF as key implementing partner.
The arrival of the vaccines is an historic step towards ensuring equitable distribution of COVID-19 vaccines worldwide. Their delivery is part of the largest vaccine procurement and supply operation in history. The vaccines in the DRC are part of a first wave of supplies that will continue over the next few weeks.
Medical authorities have decided to use the Astra Zeneca vaccine because it meets the DRC's existing storage conditions (between 2° and 8°C). A plan for the deployment of the COVID-19 vaccines across the country is being finalised.
The distribution is based on epidemiological data and WHO guidelines. The initial aim is to vaccinate 20 per cent of the population, including health workers (who represent 1 per cent of the population), people aged over 55 (6 per cent of the population) and people suffering from serious health conditions such as kidney disease, high blood pressure or diabetes (13 per cent of the population).
« The DRC is among the first countries in Africa to receive these vaccines, » said Health Minister Dr Eteni Longondo. The vaccinations will enable us to protect and save lives. We must encourage the target population to be vaccinated. »
The government submitted its request to the international community for COVID-19 vaccines in December. The Ministry of Health, through its Expanded Programme on Immunisation (EPI), will carry out the vaccinations at fixed sites throughout the country.
"This is an important moment for DRC, the African continent and COVAX - we are moving closer to our common goal of ensuring equitable access to COVID-19 vaccines, " said Emmanuel Bor, Gavi Country Manager. "Gavi is delighted to see the ambition of the COVAX Facility come to fruition with this first wave of deliveries that will protect the most vulnerable, including health workers on the front line in the fight against this pandemic in DRC. "
UNICEF is helping with the logistics of delivering the vaccines including the transport of injection materials and protection materials. The UN children’s agency will also ensure the quality and security of the cold chain and vaccine storage.
"The arrival of these vaccine doses in the DRC, which correspond to the first allocation of 6 million doses, is very encouraging news for beneficiaries who want to be vaccinated in complete safety, " said WHO Press Officer Dr Amédée Prosper Djiguimdé. "We need to work together to prioritise those most at risk of serious illness and death in the country in order to deliver on the promise of equitable access."
Gavi, with support from the WHO, UNICEF, and the EPI will train health personnel on the logistical aspects of providing vaccinations while raising awareness among the Congolese population before the actual vaccination process begins to operate.
The UK and American governments have meanwhile expressed their support for the vaccination scheme and their pride in supporting it financially.
"The UK is delighted that the DRC is among the first countries in the world to receive Covid-19 vaccines through the Covax initiative," said Juliette John, Director of British Cooperation. "With a commitment of $750 million, the UK is one of the founders and main donors of COVAX. Together with our international partners, we are working with the Government of the DRC to implement the national COVID-19 vaccination programme, in particular access to health vaccines for health workers and the most vulnerable."
U.S. Ambassador to the DRC Mike Hammer gave an equally warm response. "We welcome the arrival of vaccines against Covid-19 in the DRC," he said. "The U.S. is working with other partners around the world to stop the devastating effects of this on both public health and the economy. As part of this commitment, President Biden announced a US$4 billion contribution to support the international COVAX initiative and the United States is proud to work alongside the DRC government and other partners to bring this vaccine of vital importance to the Congolese people."
The European Union and its member countries are also supporting governments and partners in their efforts to prepare for this moment. They have been particularly active in working with some of the world's poorest countries to ensure global and equitable access to vaccines against COVID-19.
"Routine vaccination will continue to take place every day in health centres so that we can continue protecting children against vaccine-preventable diseases," said Edouard Beigbeder, UNICEF Representative in DRC.
The first phase of vaccine introduction for the year 2021 will target the four provinces of the DRC most affected by the pandemic: Kinshasa, North Kivu, Central Kongo and Haut-Katanga.
Note for editors
The list of pledges made by donors to Gavi COVAX AMC is available here .
The interactive ACT Accelerator Funding Tracker, which includes the details of COVAX funding, is available here .
About COVAX
COVAX, the vaccine pillar of the COVID-19 Tool Accelerator (ACT), is co-led by the Coalition for Epidemic Preparedness Innovations (CEPI), Gavi, the Vaccine Alliance (Gavi) and the World Health Organization (WHO) - working in partnership with vaccine manufacturers in developed and developing countries, as well as UNICEF, the World Bank, and others. It is the only global initiative that works with governments and manufacturers to ensure that COVID-19 vaccines are available worldwide for both high- and low-income countries.
The CEPI focuses on COVAX vaccine research and a development portfolio: it invests in the research and development of various promising vaccine candidates, with the aim of supporting the development of three safe and effective vaccines that can be made available to countries participating in the COVAX mechanism. As part of this work, CEPI has obtained the right of first refusal for about 1 billion doses for the COVAX facility. It has made strategic investments in vaccine manufacturing, including reserving the capacity to manufacture COVAX vaccine doses in a network of facilities and securing glass vials to hold 2 billion doses of vaccine. CEPI is also investing in the "next generation" of candidate vaccines, which will give the world additional options to control COVID-19 in the future.
Gavi focuses on the procurement and delivery of COVAX: it coordinates the design, implementation and administration of the COVAX installation and the Gavi AMC COVAX and works with its Alliance partners, UNICEF and WHO, as well as governments, on the preparation and delivery of doses in different countries. The COVAX facility is the COVID-19 global vaccine pooling mechanism through which COVAX will ensure fair and equitable access to vaccines for 190 participating economies, using an allocation framework formulated by WHO. To achieve this, the COVAX mechanism will pool the purchasing power of participating economies and provide volume guarantees for a range of promising candidate vaccines. The Gavi AMC COVAX is the financing mechanism that will support the participation of 92 low- and middle-income countries in the facility, providing access to safe and effective donor-funded doses of vaccines. Gavi raises funds for the COVAX AMC and finances the purchase of vaccines by UNICEF and the work of partners and governments in vaccine preparation and delivery, including support for cold chain equipment, technical assistance, syringes, vehicles and other aspects of the highly complex logistical operation of delivery. UNICEF and the Pan American Health Organization (PAHO) will act as procurement coordinators for the COVAX centre, assisting in the delivery of vaccines to COVAX AMC participants and others.
The WHO plays multiple roles within COVAX: it provides guidance on policy, regulation, safety, R&D, vaccine allocation, and vaccine preparation and supply to countries. Its Strategic Advisory Group of Experts (SAGE) on Immunization develops evidence-based immunization policy recommendations. Its Emergency Use Listing (EUL) and pre-qualification programmes ensure harmonised review and authorisation between member states. It provides global coordination and support to member states in monitoring vaccine safety. It has developed the target product profiles for COVID-19 vaccines and ensures technical coordination of R&D. WHO leads, together with UNICEF, the support to countries preparing to receive and administer vaccines. The Country Readiness and Delivery (CRD) work area includes Gavi and many other partners working at global, regional and country levels to provide tools, advice, monitoring and technical assistance in the field for planning and deployment of the vaccines. Together with COVAX's partners, WHO is also developing a no-fault compensation system within the framework of time-limited compensation and liability commitments.
UNICEF draws on its experience as the world's largest purchaser of vaccines and works with manufacturers and partners to purchase of COVID-19 vaccine doses, as well as freight, logistics and storage. UNICEF already procures more than 2 billion doses of vaccines per year for routine immunization and outbreak response on behalf of nearly 100 countries. In collaboration with the PAHO Revolving Fund, UNICEF is leading efforts to procure and supply doses of COVID-19 vaccine for COVAX. In addition, UNICEF, Gavi and WHO are working with governments around the clock to ensure that countries are ready to receive the vaccines, with appropriate cold chain equipment in place and health workers trained to administer them. UNICEF also plays a leading role in efforts to build confidence in vaccines, providing communication on vaccine confidence and tracking and addressing misinformation around the world.
Media contacts
Additional resources.

Additional resources for media.
About UNICEF
UNICEF works in some of the world’s toughest places, to reach the world’s most disadvantaged children. Across more than 190 countries and territories, we work for every child, everywhere, to build a better world for everyone.
Follow UNICEF on Twitter , Facebook , Instagram and YouTube
Related topics
More to explore, global deployment of rapid diagnostic tests to boost fight against cholera, six grave violations against children in times of war.
How children have become frontline targets in armed conflicts
Millions at risk from cholera due to lack of clean water, soap and toilets, and shortage of cholera vaccine
Water and the climate crisis: 10 things you should know.
The world needs to get water smart. Everyone has a role to play, and we cannot afford to wait
We’re sorry, this site is currently experiencing technical difficulties. Please try again in a few moments. Exception: request blocked
Cookies on GOV.UK
We use some essential cookies to make this website work.
We’d like to set additional cookies to understand how you use GOV.UK, remember your settings and improve government services.
We also use cookies set by other sites to help us deliver content from their services.
You have accepted additional cookies. You can change your cookie settings at any time.
You have rejected additional cookies. You can change your cookie settings at any time.
- Passports, travel and living abroad
- Travel abroad
- Foreign travel advice
Before you travel check that:
- your destination can provide the healthcare you may need
- you have appropriate travel insurance for local treatment or unexpected medical evacuation
This is particularly important if you have a health condition or are pregnant.
Emergency medical number
There’s no central number for emergency services. Check for local medical facilities and carry contact details with you.
Contact your insurance company quickly if you’re referred to a medical facility for treatment.
Health risks and recommended vaccines
Check TravelHealthPro’s current advice on the Republic of Congo to find out how to reduce the health risks you’ll face there.
TravelHealthPro also lists the recommended vaccines that could apply to you. At least 8 weeks before you travel, check how to get vaccines and whether you have to pay on the NHS travel vaccinations page .
The legal status and regulation of some medicines prescribed or bought in the UK can be different in other countries.
If you take medication, bring enough for your time in the Republic of Congo and make sure it is clearly labelled. Bring a copy of any prescription.
Read best practice when travelling with medicines on TravelHealthPro .
The NHS has information on whether you can take your medicine abroad .
Healthcare facilities in the Republic of Congo
Medical facilities in the country are limited, particularly in rural areas. Medical evacuation is likely to be necessary for all but the most basic treatments. If you become ill while in the Republic of Congo or straight after leaving the country, get immediate medical advice.
Make sure you have adequate travel and medical insurance to cover the cost of any medical treatment abroad and repatriation; this should specifically include the very high costs of evacuation by air ambulance.
FCDO has a list of medical providers in the Republic of Congo where some staff will speak English.
Travel and mental health
Read FCDO guidance on travel and mental health . There is also mental health guidance on TravelHealthPro .
Related content
Is this page useful.
- Yes this page is useful
- No this page is not useful
Help us improve GOV.UK
Don’t include personal or financial information like your National Insurance number or credit card details.
To help us improve GOV.UK, we’d like to know more about your visit today. We’ll send you a link to a feedback form. It will take only 2 minutes to fill in. Don’t worry we won’t send you spam or share your email address with anyone.
Overseas Refugee Health Guidance
Vaccination program for u.s.-bound refugees and visa 93 (v93) applicants.
- Intestinal Parasite Guidelines
Malaria Guidance
To promote healthy resettlement, CDC provides supplemental guidance to panel physicians caring for US-bound refugees. The Overseas Refugee Health Guidance provides panel physicians with supplemental guidance on vaccination, pre-departure treatments for malaria and intestinal parasites and fitness to travel. These activities are coordinated with the International Organization for Migration (IOM).
Learn more about the role of panel physicians in the US refugee resettlement program.
The table below describes the overseas immunization schedule recommended for U.S.-bound refugees and Visa 93 (V93) applicants. As part of the Vaccination Program for US-bound Refugees and V93 applicants:
- Overseas Panel sites that are not managed by the International Organization for Migration (IOM) follow an abbreviated vaccination schedule and provide only the vaccines highlighted in bold text routinely, unless specifically advised otherwise by CDC or the applicant is indicated to receive additional vaccines due to a medical condition.
- For logistical reasons, non-IOM Panel sites also are expected to provide only one dose of these vaccines, with the exception of measles, mumps, and rubella vaccine (MMR—or other measles-containing vaccines when MMR is unavailable), for which CDC recommends two doses prior to travel.
- First vaccine doses are given during the overseas medical examination, approximately 3–6 months before departure for most refugees.
- Second vaccine doses are typically given 1–2 months after the first dose.
- Refugees who undergo repeated medical examinations overseas may receive additional vaccine doses.
- HBsAg-positive persons do not receive hepatitis B vaccination overseas. They are counseled about the infection and about transmission prevention. Positive results are documented on the DS forms.
- HBsAg-negative persons receive up to two hepatitis B vaccine doses overseas, if due and if there are no known contraindications.
- HBsAg-negative household contacts of HBsAg-positive persons may be given an additional (third) dose of hepatitis B vaccine overseas to complete the series for full protection, if there is time to do so before departure. Because the third dose may be given near the time of departure, states should be aware that HBsAg results may be falsely positive within the first month after hepatitis B vaccination. CDC advises waiting at least 30 days following receipt of hepatitis B vaccine before testing for HBsAg.
Unlike immigrants, U.S.-bound refugees and V93 applicants are not legally required to receive routine vaccinations before travel to the United States. However, vaccination is strongly recommended and is offered overseas to protect health, prevent morbidity and travel delays due to disease outbreaks, and to facilitate earlier school enrollment for children after arrival.
- Note that during vaccine-preventable disease outbreaks and other situations of elevated vaccine-preventable disease risk, US-bound refugees may be required to receive certain vaccines. In these situations, guidance is provided directly to Panel site/s through CDC and IOM.
The vaccination schedule for US-bound refugees and V93 applicants is updated periodically based on changing Advisory Committee on Immunization Practices (ACIP) recommendations and advice from CDC subject matter experts.
Vaccination Program for U.S.-bound Refugees and V93s: Full Immunization Schedule (updated August 2023)
Prepared by the Immigrant and Refugee Health Branch, Division of Global Migration Health, CDC
Hepatitis B (HepB); Haemophilus influenzae type B (Hib); pneumococcal conjugate vaccine (PCV); diphtheria, tetanus, pertussis (DTP); oral polio vaccine (OPV); inactivated polio vaccine (IPV); tetanus, diphtheria (Td); meningococcal conjugate vaccine with protection against serogroups A, C, W, and Y (MenACWY); measles, mumps, and rubella (MMR)
1 Refugees and V93 applicants are tested for hepatitis B virus infection (using HBsAg) before vaccination and are offered vaccination if negative (and if a dose is due and there are no known contraindications).
2 These vaccines are sometimes given as part of a combination pentavalent or hexavalent vaccine, depending on the site and vaccine availability.
3 One dose of Hib vaccine is recommended for unimmunized refugees with asplenia, and for unimmunized HIV-positive persons up to age 18 years. Panels should refer to the US Refugee Admissions Program (USRAP) vaccination schedule for refugees with medical indications for details.
4 Highest available valency (e.g., 10, 13, 15, or 20 depending on availability on site). When available, PCV is offered to children 6 weeks to <5 years of age. A second dose is offered to children up to age 2 years. One dose of PCV will also be recommended for persons with certain medical conditions, regardless of age. For details, Panels should refer to the USRAP vaccination schedule for refugees with medical indications.
5 Children residing in refugee camps often receive several doses of whole-cell pertussis vaccine (DTwP) as part of the Expanded Program on Immunization (EPI). Therefore, children participating in the Vaccination Program for U.S.-bound Refugees are routinely offered only 1 dose of DTwP or acellular pertussis vaccine (DTaP) by overseas Panel sites, if due, in order to reduce the risk of severe local reactions associated with over-vaccination with tetanus-containing vaccines. CDC provides separate vaccination recommendations to overseas Panels during diphtheria outbreak situations.
6 All eligible US-bound refugees and V93 applicants are recommended to receive two doses of MMR (or, if MMR is nationally unavailable, another measles-containing vaccine) before departure for their protection, especially since the risk of measles outbreaks has increased globally . In specific outbreak or other measles risk situations, IOM and/or CDC will reach out directly to Panel sites with specific outbreak guidance, including guidance to provide one dose of measles vaccine to infants aged 6-11 months.
7 Only those COVID-19 vaccines authorized for emergency use (EUA) or approved under a Biologics License Application (BLA) by the US Food and Drug Administration (FDA) or listed for emergency use (EUL) by the World Health Organization (WHO). are counted towards the USRAP vaccination schedule. Eligible ages and total number of doses differ based on vaccine formulation and national regulations in countries of exam.
8 In some sites (including most Asia sites and some others), refugees ≥6 months old (including adults) may receive the inactivated influenza vaccine (1–2 doses depending on age, season, and vaccination history).
Additional Guidance for States Receiving US-bound Refugees and V93 Applicants:
- Valid historical vaccination records (such as camp vaccine cards) are counted toward the immunization schedule when available. These will be documented in the “vaccine history” columns on the DS-3025 Vaccination Documentation Worksheet.
- Note that during outbreaks of vaccine-preventable diseases which may affect US-bound refugees and V93 applicants, CDC provides separate, specific vaccination recommendations to overseas Panel sites.
- See Guidance for Evaluating and Updating Immunizations during the Domestic Medical Examination for Newly Arrived Refugees for further advice.
Intestinal Parasite Guidance
Guidance for overseas presumptive treatment of strongyloidiasis, schistosomiasis, and soil-transmitted helminth infections for refugees resettling to the united states.
Updates – the following are content updates from the previous version of the overseas guidance, which was posted in 2019
- Latin American and Caribbean refugees are now included, in addition to Asian, Middle Eastern, and African refugees.
- Recommendations for management of Strongyloides in refugees from Loa loa-endemic areas emphasize a screen-and-treat approach, rather than presumptive high-dose albendazole.
- Single-dose treatment of Strongyloides with ivermectin 200 mcg/Kg orally.
- Presumptive treatment with albendazole during any trimester of pregnancy is no longer recommended.
Summary of Recommendations
Recommendations for overseas presumptive treatment of intestinal parasites, precautions and contraindications to presumptive treatment, documentation.
Intestinal Parasite Guidance – PDF version for printing [PDF – 12 pages]
This document provides recommendations for the International Organization for Migration (IOM) physicians and other panel physicians who administer overseas predeparture presumptive treatment for intestinal parasites. While most recommendations have been implemented, not all refugee populations listed in this document are receiving all recommended pre-departure medications, due to funding restrictions and logistical challenges. For current implementation status in specific populations, see the Treatment Schedules for Presumptive Parasitic Infections for U.S.-Bound Refugees, administered by IOM. The recommendations in these guidelines may also be referenced by U.S. medical providers caring for refugees who will be receiving presumptive treatment after they arrive in the United States.
- Albendazole, single dose of 400 mg (200 mg for children 12-23 months) AND
- Ivermectin, 200 mcg/Kg orally as a single dose before departure to the United States.
- Ivermectin, 200 mcg/Kg orally as a single dose AND
- Praziquantel, 40 mg/kg, which may be divided in two doses before departure for the United States.
- Praziquantel, 40 mg/kg, which may be divided in two doses before departure to the United States.
- Refugees from Loa loa- endemic countries ( Box 1 ) in Africa should not receive presumptive ivermectin for strongyloidiasis prior to departure. Management of Strongyloides should be deferred until arrival in the United States, unless Loa loa is excluded by reviewing a daytime (10 AM to 2 PM) Giemsa-stained blood smear. Deferral of treatment for Strongyloides until after the refugee arrives in the United States is acceptable. Guidance is available for management of Strongyloides following arrival in the United States in the Domestic Intestinal Parasite Screening Guidance.
- Pre-departure presumptive and directed malaria treatment regimens must be administered as directly observed therapy.
- Test results and pre-departure treatment should be documented on the pre-departure medical screening form. If treatment was not administered, this should be clearly indicated along with the reason that treatment was not administered.
CDC Recommendations for Overseas Presumptive Parasite Treatment
* If available in country
In 1997, a Centers for Disease Control and Prevention (CDC) pilot project evaluated single-dose albendazole presumptive treatment in U.S.-bound Barawan Somali refugees. 1 This project demonstrated decreases in soil-transmitted parasites in refugees who received presumptive treatment. In May 1999, CDC extended this recommendation to all refugees resettling from sub-Saharan Africa (SSA) and Asia. In 2008, the recommendation was extended to refugees from the Middle East. Currently, most refugees from the countries listed in the Treatment Schedules for Presumptive Parasitic Infections for U.S.-Bound Refugees and without a contraindication are receiving a single dose of albendazole prior to departure.
Data indicates that pre-departure albendazole treatment has dramatically decreased the overall prevalence of soil-transmitted helminth infections in refugees. A large evaluation including more than 26,000 African and Asian refugees demonstrated single dose albendazole resulted in an absolute reduction of the prevalence of any soil-transmitted helminth from 20.8% to 4.7%, as measured by stool ova and parasite examination. 2 These findings support previous data in African refugees resettling to the United States, showing a similar decrease in soil-transmitted helminths following implementation of pre-departure albendazole treatment. Evaluations of the cost has shown clear cost-savings and estimated reduction in morbidity and mortality through conducting presumptive-treatment compared to post-arrival screen and treat, or no treatment program. 8 Despite this documented decrease in the overall prevalence of soil-transmitted helminth infections, a single dose of albendazole has very limited effect on infection with Strongyloides and no effect against Schistosoma spp. 2 , 3 , 4 , 5 A recent prospective evaluation of more than 2000 refugees resettling to the U.S. from camps on the Thailand-Burma border showed a dramatic decrease in soil-transmitted helminths and a decrease in potentially associated conditions in children (e.g. anemia, malnutrition) following treatment. 9 This evaluation also clearly demonstrated a reduction in the Strongyloides burden with the single dose albendazole in combination with ivermectin treatment prior to departure for the United States. In addition, a multicenter randomized-controlled superiority trial comparing single-dose vs. four-dose ivermectin treatment of Strongyloides (“Strong Treat 1 to 4”) showed similar efficacy between the two groups. 10
Refugees originating from the Middle East, Asia, North Africa, Latin America, and the Caribbean
Prior to departure for the United States, all refugees originating from the Middle East, Asia, North Africa, Latin American, & Caribbean should receive presumptive therapy with ivermectin for Strongyloides infection and with albendazole for infections caused by soil-transmitted helminths ( Table 1 ). Dosing for ivermectin may be based on weight and available tablet size ( Table 2 ).
Refugees originating from sub-Saharan Africa
Soil-transmitted helminths.
All refugees originating from sub-Saharan Africa should receive presumptive therapy with albendazole for infections caused by soil-transmitted helminths ( Table 1 ).
Strongyloides
Refugees from sub-Saharan Africa should also receive presumptive therapy for Strongyloides infection with ivermectin ( Table 1 ), but this will depend on whether they have originated from or resided in countries where Loa loa is endemic ( Box 1 ). The drug of choice for Strongyloides infection is ivermectin. However, cases of encephalopathy have occurred in patients treated with ivermectin during large-scale public health campaigns in areas of Africa where Loa loa is endemic. Although rare, this reaction is related to Loa loa microfilarial load. Therefore, ivermectin should be given only to persons originating from Africa who have resided in or come from countries or areas not considered endemic for Loa loa ( Box 1 ). Sub-Saharan African refugees who have resided in or are coming from areas endemic for Loa loa should not receive presumptive ivermectin, and management of Strongyloides should be deferred until they arrive in the United States (unless Loa loa is excluded by reviewing a daytime [10 AM to 2 PM] Giemsa-stained blood smear). High-dose albendazole (400 mg twice a day for 7 days) is an acceptable alternative and is considered safe in Loa loa infected people, if Loa loa infection cannot be excluded.
Schistosomiasis
Refugees from sub-Saharan Africa should also receive presumptive pre-departure therapy with praziquantel for schistosomiasis ( Table 1 ). Pre-departure dosing may be based on weight and available tablet size ( Table 2 ). If the refugee has never received presumptive therapy as part of a mass anti-helminth treatment campaign, and if it is logistically feasible, administering praziquantel first, followed by albendazole and ivermectin, may reduce the risk of adverse events caused by the release of antigens by dying parasites in persons with high parasite loads. However, if the refugee has received previous therapy, their parasite load can be assumed to be lower, and there would be no contraindication to administering praziquantel together with albendazole and ivermectin.
Special instructions for administration of presumptive pre-departure therapy
- Pre-departure regimens for presumptive treatment of intestinal parasites should be administered as directly observed therapy. While prescription and first-dose observation should be done by medical personnel, subsequent doses can be observed by nonmedical staff.
- Pregnancy testing should be performed before ivermectin or albendazole is administered.
- Ivermectin and albendazole may be administered concurrently according to World Health Organization (WHO) recommendations. In areas where refugees have received previous rounds of mass anti-helminth treatment, ivermectin, albendazole, and praziquantel co-administration is well tolerated. 6
- Praziquantel may be better tolerated if divided into two doses.
- There is no known contraindication to co-administration of these intestinal treatment regimens with malaria treatment medications. When time allows, spacing may improve tolerability. A sample 3-day combined treatment regimen for both parasites and malaria is presented in Table 3 .
- Albendazole Children <1 year of age should not receive presumptive treatment with albendazole. Further information on use of albendazole in pediatric patients can be found at the CDC, Division of Parasitic Diseases and Malaria website ( CDC – Hookworm – Resources for Health Professionals ).
- Ivermectin Children weighing <15 kg or measuring <90 cm should not receive presumptive treatment with ivermectin. Further information on use of ivermectin in pediatric patients can be found at the CDC, Division of Parasitic Diseases and Malaria website ( CDC – Strongyloides – Resources for Health Professionals ).
- Praziquantel The safety of praziquantel has not been established in children <4 years of age or <94 cm in height, so these children should not receive presumptive treatment. Further information on use of praziquantel in pediatric patients can be found at the CDC, Division of Parasitic Diseases and Malaria website ( Schistosomiasis – Resources for Health Professionals ).
Pregnant people
- Albendazole Albendazole is currently a category C drug in the United States, and it should not be administered as presumptive treatment for U.S.-bound refugees during any trimester of pregnancy. When a reliable history of the person’s last menstrual period cannot be obtained, a pregnancy test should be performed. Pregnant people should have presumptive treatment deferred until after they arrive in the United States. Further information on use of albendazole during pregnancy can be found at the CDC, Division of Parasitic Diseases and Malaria website ( CDC – Hookworm – Resources for Health Professionals ).
- Ivermectin Ivermectin is a pregnancy category C drug. This medication should not be administered as a presumptive medication to a pregnant person. When a reliable history of the person’s last menstrual period cannot be obtained, a pregnancy test should be performed before presumptive treatment is administered. Further information on use of ivermectin during pregnancy can be found at the CDC, Division of Parasitic Diseases and Malaria website ( CDC – Strongyloides – Resources for Health Professionals ).
- Praziquantel Praziquantel is considered a pregnancy category B drug, and WHO recommends the presumptive treatment of pregnant people during any trimester of pregnancy in people from schistosomiasis-endemic areas. Further information on use of praziquantel during pregnancy can be found at the CDC, Division of Parasitic Diseases and Malaria website ( CDC – Schistosomiasis – Resources for Health Professionals ).
People who are breastfeeding
- Albendazole Albendazole presumptive therapy may be administered to people who are breastfeeding. Further information on use of albendazole during lactation can be found at the CDC, Division of Parasitic Diseases and Malaria website. ( CDC – Hookwork – Resources for Health Professionals ).
- Ivermectin Presumptive treatment with ivermectin should not be administered to people who are breastfeeding during the first week after birth. Further information on use of ivermectin during lactation can be found at the CDC, Division of Parasitic Diseases and Malaria website ( CDC – Strongyloides – Resources for Health Professionals ).
- Praziquantel Praziquantel is excreted in low concentrations in human milk. According to WHO guidelines for mass prevention campaigns, the use of praziquantel during lactation is safe. 7 For individual patients in clinical settings, praziquantel should be used in breast- feeding people only when the risk to the infant is outweighed by the risk of disease progression in the breastfeeding person in the absence of treatment. Further information on use of praziquantel during lactation can be found at the CDC, Division of Parasitic Diseases and Malaria website ( CDC – Schistosomiasis – Resources for Health Professionals ).
Refugees with cysticercosis infection
Persons who have neurocysticercosis infection may have seizures following treatment with albendazole or praziquantel, since these medications kill Taenia solium cysticerci, causing inflammation and provoking seizure activity in the brain. The true prevalence of neurocysticercosis in refugee populations is not well documented. Confirmed case reports of adverse events after treatment with albendazole or praziquantel remain rare in refugees. Refugees with known neurocysticercosis, an unexplained seizure disorder, or subcutaneous nodules consistent with cysticercosis should not receive presumptive treatment with either albendazole or praziquantel.
Physicians should consult the package inserts for additional information about ivermectin, albendazole, and praziquantel.
Test results and pre-departure treatment should be documented on the Predeparture Medical Screening (PDMS) form. IOM providers should also enter the information in the Migrant Management & Operational Systems Application (MiMOSA) prior to the refugees’ arrival, so it can be transmitted to CDC’s Electronic Disease Notification (EDN) system. The paper form, after entry into the electronic format, should be placed in the medical folder inside the IOM travel bag. These documents are physically carried by the refugees to the United States. If treatment was not administered, this should be clearly documented, along with the reason that treatment was not administered. For children and pregnant and breastfeeding people who do not receive presumptive therapy, the need for subsequent treatment should be clearly documented.
- Miller JM, Boyd HA, Ostrowski SR, et al. Malaria, intestinal parasites, and schistosomiasis among Barawan Somali refugees resettling to the United States: a strategy to reduce morbidity and decrease the risk of imported infections. Am J Trop Med Hyg. 2000;62:115-21.
- Swanson SJ, Phares CR, Mamo B, et al. Albendazole treatment and enteric parasites in United States-bound refugees. N Engl J Med 2012;366:1498-507.
- Geltman PL, Cochran J, Hedgecock C. Intestinal parasites among African refugees resettled in Massachusetts and the impact of an overseas pre-departure treatment program. Am J Trop Med Hyg. 2003;69(6):657-62.
- Muennig P, Pallin D, Sell RL, Chan MS. The cost effectiveness of strategies for the treatment of intestinal parasites in immigrants. N Engl J Med. 1999;340(10):773-9.
- Marti H, Haji HJ, Savioli L, et al. A comparative trial of a single-dose ivermectin versus three days of albendazole for treatment of Strongyloides stercoralis and other soil-transmitted helminth infections in children. Am J Trop Med Hyg. 1996;55(5):477-81.
- Mohammed KA, Haji HJ, Gabrielli AF, et al. Triple co-administration of ivermectin, albendazole and praziquantel in Zanzibar: a safety study. PLoS Negl Trop Dis. 2008;2(1):e171.
- World Health Organization. Preventive chemotherapy in human helminthiasis: a manual for health professionals and programme managers. 2006. Available at: http://whqlibdoc.who.int/publications/2006/9241547103_eng.pdf [PDF – 74 pages] .
- Maskery B, Coleman MS, Weinberg M, et al. Economic analysis of the impact of overseas and domestic treatment and screening options for intestinal helminth infection among US-bound refugees from Asia. PLoS NTD 2016. doi: https://doi.org/10.1371/journal.pntd.0004910
- Mitchell T, Lee D, Weinberg M, et al. Impact of enhanced health interventions for US-bound refugees: Evaluating best practices in migration health. Amer J Trop Med Hyg 2018;98(3):920-928.
- Buonfrate D, Salas-Coronas J, Muñoz J, et al. Multiple-dose versus single-dose ivermectin for Strongyloides stercoralis infection (Strong Treat 1 to 4): a multicentre, open-label, phase 3, randomised controlled superiority trial. Lancet Infect Dis. 2019 Nov;19(11):1181-1190. doi: 10.1016/S1473-3099(19)30289-0. PMID: 31558376.
Recommended medication regimen and standard dosing for presumptive treatment of parasitic infections.
- Although WHO states ivermectin and albendazole may be given concurrently, it is recommended that ivermectin be taken on an empty stomach and albendazole with fatty foods.
- All sub-Saharan African countries except Lesotho are considered endemic for schistosomiasis.
- Praziquantel, if not co-administered, should be administered at least one day prior to either ivermectin or albendazole. Praziquantel should be taken with liquids during a meal.
Praziquantel and ivermectin dosing based on weight and tablet size for predeparture presumptive treatment of US-bound refugees
- Better tolerated if divided into two doses
- Using 600-mg praziquantel tablets
- Using 3-mg ivermectin tablets
Sample 3-Day Combined Regimen for overseas presumptive treatment of parasites and malaria
*On the first day, praziquantel and artemether-lumefantrine should be administered 8 hours following initial dose; on days 2 and 3 should be administered twice a day, morning and evening.
Endemicity of Loa loa in African countries
Zouré HGM, Wanji S, Noma M, Amazigo UV, et al. (2011) The Geographic Distribution of Loa loa in Africa: Results of Large-Scale Implementation of the Rapid Assessment Procedure for Loiasis (RAPLOA). PLoS Negl Trop Dis 5(6): e1210. doi:10.1371/journal.pntd.0001210.
Recommendations
- Specific Populations and Precautions/Contraindications to Presumptive Anti-malarial Treatment
Malaria Guidance PDF version for printing [PDF – 8 pages]
In addition to the standard, legally required medical examination of refugees migrating to the United States, CDC recommends the following presumptive treatment for Plasmodium falciparum malaria. These recommendations apply to all refugees who are living in countries that are endemic for P. falciparum in sub-Saharan Africa. Currently, CDC does not recommend presumptive therapy for asymptomatic/subclinical malaria for U.S.-bound refugees relocating from lower endemic areas outside sub-Saharan Africa (e.g. Southeast Asia) unless specifically identified in subsequent, separate, documents (see Domestic Malaria Guidance ).
These guidance is intended for presumptive pre-departure treatment of asymptomatic/subclinical malaria and for directed treatment for special populations with malaria. Any patient with clinical symptoms of malaria should be referred to a healthcare facility for evaluation and treatment.
Studies have demonstrated high rates of malaria in refugees arriving in the United States and Canada from sub-Saharan Africa 1 , 2 . Despite progress in malaria control in the past decade, sub-Saharan Africa still has highly endemic areas. In some parts of Africa, prevalence rates of P. falciparum malaria exceed 75%. Beginning in 1999, U.S. bound refugee populations originating in sub-Saharan Africa began to receive predeparture treatment with sulfadoxine-pyrimethamine (SP, Fansidar™) to prevent P. falciparum malaria disease following arrival in the U.S. Worldwide, the malaria parasite, P. falciparum, has developed resistance to many drugs used for treatment. In many areas of Africa, P. falciparum resistance to SP (and chloroquine) has increased to levels where these drugs are no longer effective. Based on efficacy studies showing SP treatment failures 3 and on guidance from the World Health Organization, beginning in 2007, pre-departure SP was discontinued and replaced by artemisinin combination treatment (ACT), generally the fixed combination artemether-lumefantrine (AL).
Refugee populations relocating to the United States from countries outside sub-Saharan Africa would rarely originate in hyper- or holoendemic malaria, making asymptomatic/subclinical P. falciparum unlikely. Refugees from areas with lower endemic rates who are infected with P falciparum malaria will have clinical symptoms of infection. Therefore, refugee populations relocating to the United States from endemic areas other than sub-Saharan Africa should be tested for malaria if symptomatic. No presumptive treatment is recommended for these populations unless directed in separate guidance.
Special instructions:
- The malaria treatment should be completed no sooner than 5 days before departure.
This document provides guidance for presumptive treatment for asymptomatic P. falciparum malaria in refugees relocating to the United States ( Annex I ). Artemisinin derivatives are obtained from the sweet wormwood plant (Chinese: 青蒿 or qīnghāo). The optimal regimen is the artemisinin-based combination therapy, artemether-lumefantrine Tables 1 and 2 , Annex 1. However, when it is not accessible, other artemisinin-based combinations may be used until artemether-lumefantrine can be obtained. Currently artesunate-amodiaquine (ASAQ) is currently the preferred second line therapy, Annex 1. Dosing formulations for ASAQ are less standardized. When AL is unavailable and ASAQ will be used as a second option, Centers for Disease Control and Prevention (CDC) should be contacted for specific dosing instructions based on the formulation available in country. Specific populations including infants, pregnant women in the first trimester and those with other contraindications, delineated below, require directed treatment after diagnostic testing and should not receive presumptive treatment for asymptomatic malaria.
Specific Populations and Precautions / Contraindications to Presumptive Anti-malarial Treatment
Infants who weigh less than 5 kilograms (kg), pregnant women, lactating women breastfeeding infants who weigh under 5 kg were previously considered to have a contraindication for use of AL. In 2015, the World Health Organization (WHO) revised the guidance for the treatment of clinical malaria to include AL treatment for pregnant women during the second and third trimester, children weighing < 5 kg and for lactating women. 5 At this time, presumptive treatment with AL for asymptomatic malaria may be administered to pregnant women during their second and third trimester and to lactating women regardless of the weight of the infant. Children < 5 kg and women in their first trimester of pregnancy should not receive presumptive treatment but should receive testing and treatment if they are found to have malaria. In addition, all persons with a known allergy to AL or any component of the medication should not receive presumptive treatment with AL.
Refugees who do not receive presumptive treatment, including women during their first trimester of pregnancy and children < 5 kg, should have diagnostic testing, and if the tests show they have malaria, receive directed treatment. Diagnostic testing should be performed with blood smears or rapid diagnostic tests (RDT) with a kit agreed upon in consultation with CDC’s Division of Global Migration Health (DGMH). Both blood smear and RDT have limited sensitivity and do not rule out malaria. 4 Therefore, any refugee who develops clinical symptoms of malaria should receive further evaluation regardless of the screening test results. Treatment for clinical or laboratory confirmed malaria should be given according to national guidance. If no national guidance exist, consult with CDC regarding a treatment plan.
For information regarding domestic management of malaria (screening and presumptive treatment) for refugees after arrival in the United States, please see Domestic Refugee Guidance .
Summary malaria treatment and testing recommendations for asymptomatic refugees in sub-Saharan Africa relocating to the United States
1 Test with blood smear or rapid diagnostic test using a test kit agreed upon in consultation with DGMH 2 Malaria thick and thin smear or RDT
Dosing of artemether-lumefantrine for asymptomatic P. falciparum malaria
Specific information about acceptable pre-departure presumptive anti-malarial therapy regimens for sub-Saharan refugees relocating to the United States
- Formulation of artemether-lumefantrine: tablets containing 20 mg of artemether plus 120 mg of lumefantrine.
- Dose: artemether-lumefantrine (AL). Treat with the 6-dose schedule as described below in Table 2 .
- Other instructions: Administer with food.
- Metabolism of drug: Maximum blood levels occur 6–12 hours after The half-life is 88 hours in healthy persons and twice as long in persons with malaria. The drug is excreted via the liver and feces.
- Adverse effects: dizziness, fatigue, anorexia, nausea, vomiting, abdominal pain, palpitations, myalgia, sleep disorders, arthralgia, headache, rash.
- Children weighing less than 5 kg
- Pregnant women in the first trimester
- Persons with known hypersensitivity to either component
- Children weighing less than 5 kg: Test with blood smear or rapid diagnostic test using a test kit agreed upon in consultation with DGMH. Children who test positive for malaria should be treated according to national guidelines or consult CDC, if no national guidelines exist.
- Pregnant women: Test with blood smear or rapid diagnostic test using a test kit agreed upon in consultation with DGMH. Pregnant or lactating women who test positive for malaria should be treated according to national guidelines or consult CDC, if no national guidelines exist.
- Persons with known hypersensitivity to either artemether or lumefantrine may receive alternative treatment. If allergic to both artemether component, discuss with CDC.
- Persons with symptomatic malaria should be treated according to national guidelines or consult CDC if no national guidelines exist.
- Dosage and Formulation of Artesunate-amodiaquine (ASAQ) combination therapy. Various formulations are available and CDC should be contacted prior to using for guidance based on available formulations in the country of departure.
- Artesunate as in Option #1
- AQ is metabolized primarily in the liver, with plasma half-life of ~5 hours.
- Adverse effects. Nausea, vomiting, abdominal pain, diarrhea, itching, bradycardia (less common). Prolonged QT (avoid with other medications that prolong QT). Can induce toxic hepatitis and fatal agranulocytosis (with prolonged use). Overdosage can cause syncope, spasticity, convulsions and involuntary movements.
- Children weighing less than 5 kg (AS)
- First term of pregnancy (AS)
- Known hypersensitivity to either AS or AQ
- Known abnormal white blood count, kidney disease or severe hepatic disorder/disease (AQ)
- Caution should be exercised in patients on treatment drugs for HIV/AIDS (AQ), cases should be discussed with CDC prior to presumptive treatment.
- Known prolonged QTc or another medication known to lengthen QTc
- Maroushek SR, Aguilar EF, Stauffer W, Abd-Alla Malaria among refugee children at arrival in the United States. Ped Infect Dis J 2005;24(5):450-2, 2005.
- Ndao M, Bandyayera E, Kokosin E, et Comparison of blood smear, antigen detection, and nested-PCR methods for screening from regions where malaria is endemic after a malaria outbreak in Quebec, Canada. J Clin Microbiol 2004;42(6):2694-700.
- Phares CR, Kapella BK, Doney AC, et al. Presumptive treatment to reduce imported malaria among refugees from East Africa resettling in the United States. Amer J Trop Med Hyg 2011;85(4):612-615.
- Stauffer WM, Newberry A, Cartwright C, Rosenblatt J, et Evaluation of malaria screening in newly arriving refugees to the United States by microscopy and rapid antigen capture assay. Ped Infect Dis J . 2006 Oct;25(10):948-50.
- The World Health Organization. Guidelines for the treatment of malaria. Third Edition. Available online (accessed March 22, 2019)
- Technical Instructions for Panel Physicians
- Technical Instructions for Civil Surgeons
- Southern Border Health and Migration
- Global Health
- Global Health Protection and Security
- Division of Global Migration Health
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
This webpage presents data on COVID-19 cases with information on pregnancy status reported to CDC. COVID-19 is a nationally notifiable disease and reporting cases to CDC is supported by routine case notification through the National Notifiable Diseases Surveillance System (NNDSS), as well as resources provided through the CDC COVID-19 response. As of March 2022, CDC no longer recommends universal case investigation and contact tracing and recommends that health department jurisdictions prioritize specific settings and groups at increased risk. In addition, a decreasing number of case reports include information on pregnancy status. For these reasons CDC will stop reporting data on this page on July 19th, 2022. Information about findings from this data and about CDC’s ongoing data collection efforts to better understand the impact of COVID-19 during pregnancy can be found here .
In March 2022, CDC changed its data collection schedule to every 8 weeks for the nationwide COVID-19 infection-induced antibody seroprevalence (commercial laboratory) survey. It now includes information on antibodies for pediatric age groups (ages 6 months to 17 years). Adult antibody updates will be based on the national blood donor seroprevalence study .
This dashboard, which includes information for all age groups, has been updated through February 2022. Updated pediatric seroprevalence information from March 2022 is available here . CDC currently plans to end the nationwide SARS-CoV-2 antibody studies in December 2022.
Sign up to receive the COVID Data Tracker Weekly Review.
- Company History
- Mission Statement
- Philippines
- South Africa
- Afghanistan
- American Samoa
- Antigua and Barbuda
- British Virgin Islands
- Burkina Faso
- Canary Islands
- Cayman Islands
- Central African Republic
- Christmas Island
- Cocos (Keeling) Islands
- Cook Islands
- Cote d'Ivoire
- Democratic Republic of the Congo
- Dominican Republic
- Easter Island
- El Salvador
- Equatorial Guinea
- Falkland Islands
- Faroe Islands
- French Guiana
- French Polynesia
- Guinea-Bissau
- Liechtenstein
- Madeira Islands
- Marshall Islands
- Netherlands
- New Caledonia
- New Zealand
- Norfolk Island
- North Korea
- North Macedonia
- Northern Mariana Islands
- Palestinian Territories
- Papua New Guinea
- Pitcairn Islands
- Puerto Rico
- Republic of the Congo
- Saint Barthelemy
- Saint Helena
- Saint Kitts and Nevis
- Saint Lucia
- Saint Martin
- Saint Pierre-et-Miquelon
- Saint Vincent and the Grenadines
- Sao Tome and Principe
- Saudi Arabia
- Sierra Leone
- Sint Eustatius
- Solomon Islands
- South Georgia and the South Sandwich Islands
- South Korea
- South Sudan
- Switzerland
- Trinidad and Tobago
- Turkmenistan
- Turks and Caicos Islands
- U.S. Virgin Islands
- United Arab Emirates
- United Kingdom
- United States
- Wake Island
- Western Sahara
- Travel Vaccines
- Travel Health Consultations
- Travellers’ Diarrhea Kits
- Dengue Fever Prevention
- Malaria Prevention
- Chikungunya Prevention
- Zika Prevention
- Ebola Virus
- Yellow Fever
- Hepatitis A
- Japanese Encephalitis
- Hepatitis B
- Tickborne Encephalitis (TBE)
- Tetanus-Diphtheria-Pertussis
- Measles-Mumps-Rubella
- Influenza (Flu)
- Blood Tests
- Vitamin Injections
- Physician Referral Program
- London – Euston Travel Clinic

Travel Vaccines and Advice for the Democratic Republic of the Congo

The Democratic Republic of the Congo (DRC), located in Central Africa, was previously known as Zaire. In area it is the second largest country in Africa.
Travellers visiting the DRC will have a lot to explore including rainforests and wildlife. They can also enjoy city life as well as the historical sites. Brazzaville is a great place for tourists to visit Brazzaville Basilica, the marketplace, the Congo River Rapids and the Lefini Faunal Reserve.
If you enjoy cruises, the DRC has a tour that takes you down the Congo River. It starts from the capital of Kisangani to the city of Kinshasa. This 1750-kilometre cruise is ideal if you have a lot of free time on your hands.
The Democratic Republic of the Congo is a great destination for tourists. There’s so much to explore. Whether you travel by train or by air, the DRC awaits you.
Do I Need Vaccines for the Democratic Republic of Congo?
Yes, some vaccines are recommended or required for Democratic Republic of Congo. The National Travel Health Network and Centre and WHO recommend the following vaccinations for Democratic Republic of Congo: COVID-19 , hepatitis A , hepatitis B , typhoid , cholera , yellow fever , rabies , meningitis , polio and tetanus .
See the bullets below to learn more about some of these key immunisations:
- COVID-19 – Airborne – Recommended for all travellers
- Hepatitis A – Food & Water – Recommended for most travellers to the region, especially if unvaccinated.
- Hepatitis B – Blood & Body Fluids – Recommended for travellers to most regions.
- Tetanus – Wounds or Breaks in Skin – Recommended for travelers to most regions, especially if not previously vaccinated.
- Typhoid – Food & Water – Jab lasts 3 years. Oral vaccine lasts 5 years, must be able to swallow pills. Oral doses must be kept in refrigerator.
- Cholera – Food & Water – Recommended for travel to most regions.
- Yellow Fever – Mosquito – Required for all travellers over 9 months of age.
- Rabies – Saliva of Infected Animals – High risk country. Vaccine recommended for long-stay travellers and those who may come in contact with animals.
- Meningitis – Airborne & Direct Contact – Located in the meningitis belt, vaccination is recommended during the dry season (Dec. – June)
- Polio – Food & Water – The DRC has had documented polio cases in the last year. Vaccination or a single adult booster is recommended.
See the tables below for more information:
Yellow fever is still a problem in the DRC. Proof of yellow fever vaccination is required to enter the country.
Zika is present in the DRC. Women who are pregnant or may become pregnant should avoid travel to the region. Steps should be taken to prevent mosquito bites and sexual exposure to the virus.
Malaria is a serious mosquito-borne disease which is present in the DRC. Antimalarials are the best form of prevention alongside repellents and mosquito netting.
Dengue and chikungunya are also present. Both are only preventable through repellents, netting and other anti-mosquito measures.
See our vaccinations page to learn more about these infections and vaccines. Ready to protect yourself? Book your travel health appointment today by calling or schedule online now .
Do I Need a Visa or Passport for the Democratic Republic of the Congo?
Visas are required for the DRC and must be obtained before arrival. Passports are required to be valid for an additional six months at the time of entry. Proof of yellow fever vaccination is required to enter the country. If you do not have proof of vaccination, you may be vaccinated on site, quarantined or returned to your previous location.
A departure tax of about $50 USD plus 5,000 Congolese Francs must be paid upon checking into a flight out of the country.
Sources: Embassy of the Democratic Republic of the Congo and GOV.UK
What is the Climate Like in the Democratic Republic of the Congo?
The DRC has an equatorial and tropical climates making it hot and humid. The average temperature around 26 degrees in the low central basin and 18 degrees at altitudes of 1,500 metres. The best time to travel to the DRC is during dry season.
Here is what to expect from the climate in DRC:
- Equatorial Climate – The temperature is stable throughout the year. There is a lot of rain during the months of April-May, and October-November. The least months with rainfall are January-February and June-July.
- Tropical Climate – This occurs to the north and south of the equatorial zone. The climate becomes tropical and the rainfall averages between 100 to 170 centimetres per year. The temperature is lower in the winter dry season but higher during the summer rainy season. The spring is the end of the dry season.
- The Mountains – In the east the DRC experiences the East African Rift that has created many lakes. The mountains affect precipitation, causing the west to have more rain whilst the east remains dry.
The coast experiences fog and low clouds because of the cool sea current. Travellers exploring the southern DRC will feel the dry season is more evident.
How Safe is the Democratic Republic of the Congo?
There are some parts of the DRC travellers should not visit. The eastern part of the DRC is not stable because of rebel and military groups. Violence has occurred including hurting civilians, killing, rape, and kidnapping. Pillaging is still happening in places like North Kivu, South Kivu, Tanganyika, Haut, Lomami, Ituri, Bas-Uele and Haut-Uele. Civil unrest is ongoing.
Travellers should stay away from demonstrations and large crowds. Protests can turn from peaceful to violent at any moment. People also need to be cautious of roadblocks and security forces. When you’re motoring, you should keep doors and windows locked. Don’t let soldiers get into the car with you. It’s important not to get into a vehicle with anyone.
If you need to communicate with a legitimate officer, you should ensure your doors are locked. Only leave your window open a little bit to communicate with the officer.
You need to have your identity papers with you to show the constable if the situation calls for them. It will make things easier if you follow the officer’s commands and if threatened, don’t resist.
If a crime occurs or you’re a victim of a crime, you should report it to the British embassy in the region.
Senkwekwe Gorilla Orphanage
Travellers who want to connect with the wildlife of the DRC should visit the gorilla orphanage. This orphanage can be found on the grounds of Mikeno Lodge. The Senkwekwe Gorilla Orphanage was named after a silverback killed defending the Rugendo group against poachers in 2007. Four gorillas now live in the orphanage and two of them, Ndakasi and Ndeze, survived the massacre.
Travellers who stay at the hotel have access to the gorilla orphanage for free. It is open from 8am-4pm, and it’s an experience tourists should not miss out on when they travel to the Democratic Republic of the Congo.
What Should I Take To the Democratic Republic of the Congo?
When you’re planning your trip to the DRC, there are some things you should consider taking with you.
- Packing – Sun cream, insect repellent, cotton clothing that is comfortable, good walking shoes, sunnies, and a camera with plenty of film are some of the essentials you’ll need for your trip.
- Currency/Money – International currency, especially the dollar and Euro, is widely accepted. There are also money changers available in many cities in the DRC. ATMS, that are internationally linked, are available in the larger cities, but they are not that reliable. When travellers tip, a 5% to 7% tip is expected. Most taxi drivers don’t expect tips but some ask for them. A good tip to have on you is CDF500, and it’s good to carry cash just in case of emergencies.
- Medicines and Supplies – Prescription medicines, medical supplies, over the counter medicines, a first aid kit, and supplies to prevent injury and illness are important things to consider on your trip to the DRC.
It doesn’t hurt to be prepared on your trip so ensure you take everything you need to travel and stay healthy.
Embassy of the United Kingdom in the Democratic Republic of the Congo
If you are in the Democratic Republic of the Congo and have an emergency (for example, been attacked, arrested or someone has died) contact the nearest consular services. Contact the embassy before arrival if you have additional questions on entry requirements, safety concerns or are in need of assistance.
British Embassy Kinshasa 83, Avenue Roi Baudouin Gombe Kinshasa Democratic Republic of the Congo Telephone: +243 81 556 6200. If the Embassy number is not available please ring +44 1908 516 666 Emergency Phone: 243 81 556 6200 or +44 1908 516666 Fax: +243 81 346 4291 Email: [email protected]
Ready to start your next journey? Ring us up at or book online now !
On This Page: Do I Need Vaccines for the Democratic Republic of the Congo? Do I Need a Visa or Passport for the Democratic Republic of the Congo? What is the Climate Like in the Democratic Republic of the Congo? How Safe is the Democratic Republic of the Congo? Senkwekwe Gorilla Orphanage What Should I Take To the Democratic Republic of the Congo? Embassy of the United Kingdom in the Democratic Republic of the Congo

- Privacy Policy
- Automatic Data Collection Statement
Mpox cases are far outpacing last year's numbers, CDC reports
Health officials are encouraging people at risk of mpox to seek vaccination, as cases are on the rise.

More than 570 cases of mpox have been detected in the U.S. so far in 2024 — nearly double the number seen by this time last year.
This infection rate doesn't come close to that seen at the peak of the mpox outbreak in early August 2022 , when the U.S. saw an average of about 470 new cases in a week. However, the new data highlight that mpox is still circulating and that there's still a need for people who are at risk of infection to get vaccinated.
The most widely used mpox vaccine in the U.S., called JYNNEOS , is given in two doses spaced a month apart. A person is fully vaccinated two weeks after their second dose, and no booster shots are currently recommended. You can check whether you're eligible for the vaccine and where to get the shots on the Centers for Disease Control and Prevention (CDC) website . Various local health departments, such as those of New York City and San Francisco , also have their own vaccine-site finders.
The vaccine is not widely recommended to everyone. Rather, select groups — for example, gay and bisexual men with recent sexually transmitted infection (STI) diagnoses — have been identified as at risk of mpox and made eligible for the shots.
Related: Should everyone get a monkeypox vaccine?
"Most of the cases that we're seeing reported are either unvaccinated or under-vaccinated, meaning they either never received a vaccine, or they only got one dose," Dr. Jenni McQuiston , deputy director of the CDC's High-Consequence Pathogens and Pathology division, told ABC News .
Mpox, formerly known as monkeypox , is caused by a relative of the now-eradicated variola virus, which causes smallpox . Mpox viruses come in two broad types: clade I and clade II. Clade I is more likely than clade II to cause severe and fatal disease. Although clade I has not been detected in the U.S. to date, it's possible that travelers could carry the viruses to the country from other places, such as the Democratic Republic of the Congo, the CDC cautioned in December 2023 . The JYNNEOS vaccine guards against both clades.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
In general, mpox viruses can cause flu-like symptoms, such as fever, muscle aches, fatigue and swollen lymph nodes. However, during the outbreak's peak in 2022, not all cases involved such symptoms . The disease's characteristic pox rashes typically start out as discolored patches and then progress to raised bumps, blisters, and large, pus-filled pimples that scab over and slough off. Depending on the case, these rashes may first appear around the face and in the oral cavity and then spread to the extremities, or they may initially show up around the genitals and anus.
People with severely weakened immune systems, including those with HIV ; children younger than 1 year; people with a history of eczema; and people who are pregnant face a higher risk of severe disease from mpox. The disease most often spreads through close contact with an infected person, especially through contact with their rashes.
Since May 2022, when the mpox outbreak hit the U.S., the country has seen more than 30,000 cases, most of which occurred in 2022 . By the start of 2023, infection rates had slowed — the U.S. recorded 298 cases between Jan. 1 and March 23, 2023. Compare that to this year, when 576 cases were reported in the same time frame, according to the CDC . (The agency adds that these case counts are provisional and subject to change.)
More than 110 of the cases this year were in New York City, 64 were in California and 50 were in Florida.
Anyone can catch mpox, but from the start of the outbreak, the disease has disproportionately affected gender-diverse and transgender people and also men who have sex with men. People in these groups who have had recent STI diagnoses or who have had more than one recent sex partner are recommended to get vaccinated for mpox.
However, CDC data suggest that mpox vaccination among these and other at-risk groups is not as high as it should be, with large portions of the at-risk population missing one or both vaccine doses.
"We felt like it was really important to get the word out that there is a continued risk from this virus. It's still here," Dr. Brandy Darby , director of the Division of Surveillance and Investigation in the Office of Epidemiology at the Virginia Department of Health, told CNN . The department recently issued a notice about the dozen mpox cases it's seen so far in 2024, in part because it saw 12 in all of 2023.
— Why are sexually transmitted infections on the rise in the US?
— The deadliest viruses in history
— What does it mean for a disease to be 'endemic'?
"We also wanted to give people time to protect themselves ahead of Pride season" in June, Darby said. "We're hoping this might encourage people to go ahead and get vaccinated so they can go out and enjoy their celebrations and not have to worry so much about mpox."
This article is for informational purposes only and is not meant to offer medical advice.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun ? Send us your questions about how the human body works to [email protected] with the subject line "Health Desk Q," and you may see your question answered on the website!

Nicoletta Lanese is the health channel editor at Live Science and was previously a news editor and staff writer at the site. She holds a graduate certificate in science communication from UC Santa Cruz and degrees in neuroscience and dance from the University of Florida. Her work has appeared in The Scientist, Science News, the Mercury News, Mongabay and Stanford Medicine Magazine, among other outlets. Based in NYC, she also remains heavily involved in dance and performs in local choreographers' work.
Man in critical condition after catching deadly 'B virus' from wild monkeys in Hong Kong
Bite from toilet rat hospitalizes man in Canada
Low tides reveal Bronze Age fortress that likely defended against Irish mainland
Most Popular
By Sneha Khedkar April 05, 2024
By Ben Turner April 05, 2024
By Harry Baker April 05, 2024
By Laura Geggel April 05, 2024
By Elise Poore April 05, 2024
By Keumars Afifi-Sabet April 05, 2024
By Sascha Pare April 05, 2024
By Patrick Pester April 05, 2024
By Daisy Dobrijevic April 05, 2024
By Joanna Thompson April 05, 2024
- 2 James Webb telescope confirms there is something seriously wrong with our understanding of the universe
- 3 April 8 total solar eclipse: Everything you need to know
- 4 'Gambling with your life': Experts weigh in on dangers of the Wim Hof method
- 5 Cholesterol-gobbling gut bacteria could protect against heart disease
- 3 'Gambling with your life': Experts weigh in on dangers of the Wim Hof method
- 4 Cholesterol-gobbling gut bacteria could protect against heart disease
- 5 NASA engineers discover why Voyager 1 is sending a stream of gibberish from outside our solar system
- Clinical Trials
Chikungunya Outbreak Travel Alert Reissued for Timor-Leste

A multi-month chikungunya virus outbreak continues impacting the residents of Timor-Leste (East Timor). As of late March 2024, 195 chikungunya cases have been reported in Timor-Leste.
To alert international travelers, the U.S. CDC reissued a Level 2 - Practice Enhanced Precautions, Travel Health Advisory on April 5, 2024.
Data sources indicate tourist arrivals in East Timor increased to 3,718 in the first quarter of 2022.
Additionally, neighboring countries have also reported chikungunya cases in 2024: Thailand (139), Pakistan (26), and Malaysia (6).
This mosquito-transmitted disease is caused by the chikungunya virus. Most people infected develop some symptoms, but related fatalities are rare.
However, people at risk for more severe disease include newborns infected around the time of birth, older adults, and people with medical conditions such as high blood pressure, diabetes, or heart disease.
According to the CDC, if you are pregnant, reconsider traveling to Timor-Leste.
There is no specific treatment for chikungunya, but the CDC's Advisory Committee on Immunization Practices recommends the newly approved IXCHIQ® vaccine for some travelers.
Timor-Leste is also experiencing dengue outbreaks and a resurgence of the Zika virus in the Ermera municipality in 2024.
As of late February 2024, l ocal media reported 27 Zika cases and 460 dengue cases.
Our Trust Standards: Medical Advisory Committee
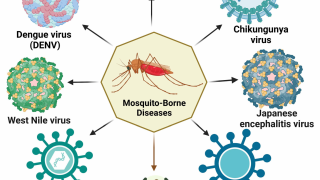
- Today's news
- Reviews and deals
- Climate change
- 2024 election
- Fall allergies
- Health news
- Mental health
- Sexual health
- Family health
- So mini ways
- Unapologetically
- Buying guides
Entertainment
- How to Watch
- My watchlist
- Stock market
- Biden economy
- Personal finance
- Stocks: most active
- Stocks: gainers
- Stocks: losers
- Trending tickers
- World indices
- US Treasury bonds
- Top mutual funds
- Highest open interest
- Highest implied volatility
- Currency converter
- Basic materials
- Communication services
- Consumer cyclical
- Consumer defensive
- Financial services
- Industrials
- Real estate
- Mutual funds
- Credit cards
- Credit card rates
- Balance transfer credit cards
- Business credit cards
- Cash back credit cards
- Rewards credit cards
- Travel credit cards
- Checking accounts
- Online checking accounts
- High-yield savings accounts
- Money market accounts
- Personal loans
- Student loans
- Car insurance
- Home buying
- Options pit
- Investment ideas
- Research reports
- Fantasy football
- Pro Pick 'Em
- College Pick 'Em
- Fantasy baseball
- Fantasy hockey
- Fantasy basketball
- Download the app
- Daily fantasy
- Scores and schedules
- GameChannel
- World Baseball Classic
- Premier League
- CONCACAF League
- Champions League
- Motorsports
- Horse racing
- Newsletters
New on Yahoo
- Privacy Dashboard
What is the killed measles vaccine and what does it mean if you got one
Last month, the Centers for Disease Control and Prevention issued a warning over the increase in measles outbreaks. And this week, the Chicago Department of Public Health warned about possible measles exposure at several city locations.
Related: Chicago Health warns of possible measles exposure on CTA buses, city schools
While measles is most dangerous for young children and pregnant women, the CDC warns everyone – especially those planning international travel of any kind – should get vaccinated to prevent the virus’ spread.
As far as who does not need the MMR Vaccine, the CDC lists the following criteria:
You have written documentation of adequate vaccination:
at least one dose of a measles, mumps, and rubella virus-containing vaccine administered on or after the first birthday for preschool-age children and adults not at high risk for exposure and transmission
two doses of measles and mumps virus-containing vaccine for school-age children and adults at high risk for exposure and transmission, including college students, healthcare personnel, international travelers, and groups at increased risk during outbreaks
You have laboratory confirmation of past infection or had blood tests that show you are immune to measles, mumps, and rubella.
You were born before 1957.
LIVE measles vaccine vs the killed measles vaccine
Additionally, the CDC says, “if you received a measles vaccine in the 1960s, you may not need to be revaccinated.”
Those who received the vaccine in the 1960s should check their vaccine records. If you received the “LIVE measles vaccine in the 1960s,” the CDC says you do not need to be revaccinated.
The killed measles vaccine is an earlier formulation of measles vaccine that is no longer used. The CDC says if your vaccine documentation indicates you received the killed measles vaccine, you should talk with you healthcare provider about getting revaccinated with the current MMR vaccine.
The CDC says this recommendation is intended to “protect those who may have received killed measles vaccine, which was available in 1963-1967 and was not effective.”
Measles outbreaks: Is the vaccine good for life or do you need a booster?
Additionally, according to the CDC, being before 1957 provides only presumptive evidence for measles, mumps, and rubella. “Before vaccines were available, nearly everyone was infected with measles, mumps, and rubella viruses during childhood. The majority of people born before 1957 are likely to have been infected naturally and therefore are presumed to be protected against measles, mumps, and rubella.” Healthcare personnel born before 1957 without laboratory evidence of immunity or disease should consider getting two doses of MMR vaccine.”
For the latest news, weather, sports, and streaming video, head to WGN-TV.
Recommended Stories
Tennessee hires marshall's kim caldwell as women's basketball coach.
Tennessee hired Kim Caldwell as their next women's basketball coach. Caldwell previously coached at Marshall and Division II Glenville State.

Junkyard Gem: 1972 Saab 96
A 1972 Saab 96 with Ford V4 engine, found in a British scrapyard.
Iowa vs. South Carolina live scores, updates: Caitlin Clark breaks NCAA tournament all-time scoring record
Follow along as we track all the action between Iowa and South Carolina in the NCAA title game.
Working from home isn't going away, even if some CEOs wish it would
When I started working from home in the late 1980s as a freelance technical writer, I was clearly an outlier. Over time, though, that slowly changed, and the pandemic — along with generationally shifting views on work-life balance — accelerated worker sentiment away from going into a formal office every day, even if some CEOs wish it weren’t so. Today, 14% of U.S. workers work at home full time (including me), and that number is expected to increase to 20% by next year, according to data published by USA Today.
Target set to launch new paid membership program this week
Under the new paid Target Circle 360 membership, shoppers will be able to benefit from same-day delivery and other perks starting April 7.
Fintech representation in YC's Demo Days is definitely shrinking
This week, we’re looking at just how many fintech companies made it into Y Combinator’s Winter 2024 cohort, how much funding slid in the first quarter, and more! Y Combinator held demo days for its Winter Cohort this week. Of the 260 companies in the latest cohort, nearly 30 of them, or 8%, were classified as fintech.
Jay Powell really wants Americans to know he is not thinking about politics
The Fed chairman went out of his way to make it clear this week that the Fed is free from personal or political bias as he continues to navigate a red-hot political year.
MLB and players union exchange barbs over pitch clock after brutal run of pitcher injuries
Shane Bieber and Spencer Strider both have damaged elbows. It's not a good time to be a pitcher right now.
Stephen Strasburg retires after years of injury struggles, and months-long standoff with Nationals
Stephen Strasburg made eight starts after signing a $245 million contract in 2019.
Attempted murder charge against LSU RB Trey Holly rejected by grand jury
Holly was arrested in connection with a February shooting that left two people injured.
Elizabeth Hurley has used this Estee Lauder serum for 25 years and it's 50% off
The actress/model/swimwear designer has the inside track to the fountain of youth.
Rock these jeans, mama! Lee's 'slim and sleek' pair for women 50+ is nearly 60% off
More than 16,000 shoppers say this flattering denim has a five-star fit and feel.
Why gas prices in California ‘have gone ballistic'
California's gas prices have surged more than the rest of the nation as the state grapples with less output from its refineries.
Israel and Hamas reach six months of war. Here's where the conflict stands.
April 7 marks six months since Hamas unleashed a deadly and unprecedented attack on Israel, which subsequently declared war against the militant group. Here's where the conflict stands.
This $10 'parking garage for glasses' is a must for your spring organization spree
Never lose your specs again with a soft magnetic holder that 13,000 shoppers love.
Game on! This complete pickleball set is just $14 — that's over 50% off
See what all the fuss is about with this ultra-affordable kit.
How Hallmark's 'When Calls the Heart' fandom, the Hearties, became a key part of the show's success
"I’ve been on shows with fandoms, but I’ve never been on a show with a fandom that is full of so much goodwill," showrunner Lindsay Sturman told Yahoo Entertainment.
Polestar’s carbon hunter plans to make everybody's EVs even cleaner
Fredrika Klaren is head of sustainability at Polestar. She has to walk the climate walk, no matter how irksome and inconvenient.
The stifling impact high inflation has on retirement savers
For many Americans, the daily costs of living have made saving for retirement a struggle. They’ve paused contributions to retirement accounts, pared them back, or dipped into these funds.
iOS music apps in the EU can now send users to external websites for purchase
Apple will make it easier for you to pay for music purchases and subscriptions outside of its payment system, if you're living in a European Union country.
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
Kenya Traveler View
Travel health notices, vaccines and medicines, non-vaccine-preventable diseases, stay healthy and safe.
- Packing List
After Your Trip

Be aware of current health issues in Kenya. Learn how to protect yourself.
Level 2 Practice Enhanced Precautions
- Global Polio January 05, 2024 Some international destinations have circulating poliovirus. Before any international travel, make sure you are up to date on your polio vaccines. Destination List: Afghanistan, Algeria, Benin, Botswana, Burkina Faso, Burundi, Cameroon, Central African Republic, Chad, Côte d'Ivoire (Ivory Coast), Democratic Republic of the Congo, Egypt, Guinea, Indonesia, Israel, including the West Bank and Gaza, Kenya, Madagascar, Malawi, Mali, Mauritania, Mozambique, Niger, Nigeria, Pakistan, Republic of the Congo, Somalia, Sudan, Tanzania, including Zanzibar, Yemen, Zambia, Zimbabwe
⇧ Top
Check the vaccines and medicines list and visit your doctor at least a month before your trip to get vaccines or medicines you may need. If you or your doctor need help finding a location that provides certain vaccines or medicines, visit the Find a Clinic page.
Routine vaccines
Recommendations.
Make sure you are up-to-date on all routine vaccines before every trip. Some of these vaccines include
- Chickenpox (Varicella)
- Diphtheria-Tetanus-Pertussis
- Flu (influenza)
- Measles-Mumps-Rubella (MMR)
Immunization schedules
All eligible travelers should be up to date with their COVID-19 vaccines. Please see Your COVID-19 Vaccination for more information.
COVID-19 vaccine
Active cholera transmission is widespread in Kenya. Cholera is rare in travelers. Certain factors may increase the risk of getting cholera or having severe disease ( more information ). Avoiding unsafe food and water and washing your hands can also help prevent cholera.
Vaccination may be considered for children and adults who are traveling to areas of active cholera transmission.
Cholera - CDC Yellow Book
Hepatitis A
Recommended for unvaccinated travelers one year old or older going to Kenya.
Infants 6 to 11 months old should also be vaccinated against Hepatitis A. The dose does not count toward the routine 2-dose series.
Travelers allergic to a vaccine component or who are younger than 6 months should receive a single dose of immune globulin, which provides effective protection for up to 2 months depending on dosage given.
Unvaccinated travelers who are over 40 years old, immunocompromised, or have chronic medical conditions planning to depart to a risk area in less than 2 weeks should get the initial dose of vaccine and at the same appointment receive immune globulin.
Hepatitis A - CDC Yellow Book
Dosing info - Hep A
Hepatitis B
Recommended for unvaccinated travelers younger than 60 years old traveling to Kenya. Unvaccinated travelers 60 years and older may get vaccinated before traveling to Kenya.
Hepatitis B - CDC Yellow Book
Dosing info - Hep B
CDC recommends that travelers going to certain areas of Kenya take prescription medicine to prevent malaria. Depending on the medicine you take, you will need to start taking this medicine multiple days before your trip, as well as during and after your trip. Talk to your doctor about which malaria medication you should take.
Find country-specific information about malaria.
Malaria - CDC Yellow Book
Considerations when choosing a drug for malaria prophylaxis (CDC Yellow Book)
Malaria information for Kenya.
Cases of measles are on the rise worldwide. Travelers are at risk of measles if they have not been fully vaccinated at least two weeks prior to departure, or have not had measles in the past, and travel internationally to areas where measles is spreading.
All international travelers should be fully vaccinated against measles with the measles-mumps-rubella (MMR) vaccine, including an early dose for infants 6–11 months, according to CDC’s measles vaccination recommendations for international travel .
Measles (Rubeola) - CDC Yellow Book
Meningitis (Meningococcal disease)
Recommended for travelers 2 months old or older traveling to areas of Kenya that are part of the meningitis belt during the dry season.
Meningococcal disease - CDC Yellow Book
Meningitis Belt Map
In Kenya poliovirus has been identified in the past year.
Travelers to Kenya are at increased risk of exposure to poliovirus.
Vaccine recommendations : Adults traveling to Kenya who received a complete polio vaccination series as children may receive a single lifetime booster dose of inactivated polio vaccine; travelers who are unvaccinated or not fully vaccinated should receive a complete polio vaccination series before travel. Children who are not fully vaccinated will be considered for an accelerated vaccination schedule .
Polio - CDC Yellow Book
Polio: For Travelers
Rabid dogs are commonly found in Kenya. If you are bitten or scratched by a dog or other mammal while in Kenya, there may be limited or no rabies treatment available.
Consider rabies vaccination before your trip if your activities mean you will be around dogs or wildlife.
Travelers more likely to encounter rabid animals include
- Campers, adventure travelers, or cave explorers (spelunkers)
- Veterinarians, animal handlers, field biologists, or laboratory workers handling animal specimens
- Visitors to rural areas
Since children are more likely to be bitten or scratched by a dog or other animals, consider rabies vaccination for children traveling to Kenya.
Rabies - CDC Yellow Book
Recommended for most travelers, especially those staying with friends or relatives or visiting smaller cities or rural areas.
Typhoid - CDC Yellow Book
Dosing info - Typhoid
Yellow Fever
Required for travelers ≥1 year old arriving from countries with risk for YF virus transmission. 1
Recommended for all travelers ≥9 months old except as follows. Generally not recommended for travel limited to: the city of Nairobi (the capital); the counties of the former North Eastern Province (Mandera, Wajir, and Garissa); or the counties (except Taita-Taveta) of the former Coast Province (Kilifi, including the city of Malindi; Kwale; Lamu; Mombasa, including the city of Mombasa; Tana River) .
Yellow Fever - CDC Yellow Book
- Avoid contaminated water
Leptospirosis
How most people get sick (most common modes of transmission)
- Touching urine or other body fluids from an animal infected with leptospirosis
- Swimming or wading in urine-contaminated fresh water, or contact with urine-contaminated mud
- Drinking water or eating food contaminated with animal urine
- Avoid contaminated water and soil
Clinical Guidance
Schistosomiasis
- Wading, swimming, bathing, or washing in contaminated freshwater streams, rivers, ponds, lakes, or untreated pools.
Avoid bug bites
African tick-bite fever.
- Avoid Bug Bites
African Tick-bite fever
Chikungunya
- Mosquito bite
Crimean-Congo Hemorrhagic fever
- Tick bite
- Touching the body fluids of a person or animal infected with CCHF
- Mosquito bite
Leishmaniasis
- Sand fly bite
- Avoid animals
Marburg Hemorrhagic Fever
- Touching infected animals (including bats and primates) or their body fluids
- Touching body fluids (blood or sweat) from an infected person
- Touching objects contaminated with the body fluids of a person infected with Ebola or Marburg virus
- Avoid sick people
- Avoid animals and areas where they live
Marburg virus
Rift Valley Fever
- Touching blood, body fluids, or tissue of infected livestock
Rift Valley fever
Airborne & droplet
- Breathing in air or accidentally eating food contaminated with the urine, droppings, or saliva of infected rodents
- Bite from an infected rodent
- Less commonly, being around someone sick with hantavirus (only occurs with Andes virus)
- Avoid rodents and areas where they live
Tuberculosis (TB)
- Breathe in TB bacteria that is in the air from an infected and contagious person coughing, speaking, or singing.
Learn actions you can take to stay healthy and safe on your trip. Vaccines cannot protect you from many diseases in Kenya, so your behaviors are important.
Eat and drink safely
Food and water standards around the world vary based on the destination. Standards may also differ within a country and risk may change depending on activity type (e.g., hiking versus business trip). You can learn more about safe food and drink choices when traveling by accessing the resources below.
- Choose Safe Food and Drinks When Traveling
- Water Treatment Options When Hiking, Camping or Traveling
- Global Water, Sanitation and Hygiene | Healthy Water
- Avoid Contaminated Water During Travel
You can also visit the Department of State Country Information Pages for additional information about food and water safety.
Prevent bug bites
Bugs (like mosquitoes, ticks, and fleas) can spread a number of diseases in Kenya. Many of these diseases cannot be prevented with a vaccine or medicine. You can reduce your risk by taking steps to prevent bug bites.
What can I do to prevent bug bites?
- Cover exposed skin by wearing long-sleeved shirts, long pants, and hats.
- Use an appropriate insect repellent (see below).
- Use permethrin-treated clothing and gear (such as boots, pants, socks, and tents). Do not use permethrin directly on skin.
- Stay and sleep in air-conditioned or screened rooms.
- Use a bed net if the area where you are sleeping is exposed to the outdoors.
What type of insect repellent should I use?
- FOR PROTECTION AGAINST TICKS AND MOSQUITOES: Use a repellent that contains 20% or more DEET for protection that lasts up to several hours.
- Picaridin (also known as KBR 3023, Bayrepel, and icaridin)
- Oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD)
- 2-undecanone
- Always use insect repellent as directed.
What should I do if I am bitten by bugs?
- Avoid scratching bug bites, and apply hydrocortisone cream or calamine lotion to reduce the itching.
- Check your entire body for ticks after outdoor activity. Be sure to remove ticks properly.
What can I do to avoid bed bugs?
Although bed bugs do not carry disease, they are an annoyance. See our information page about avoiding bug bites for some easy tips to avoid them. For more information on bed bugs, see Bed Bugs .
For more detailed information on avoiding bug bites, see Avoid Bug Bites .
Stay safe outdoors
If your travel plans in Kenya include outdoor activities, take these steps to stay safe and healthy during your trip.
- Stay alert to changing weather conditions and adjust your plans if conditions become unsafe.
- Prepare for activities by wearing the right clothes and packing protective items, such as bug spray, sunscreen, and a basic first aid kit.
- Consider learning basic first aid and CPR before travel. Bring a travel health kit with items appropriate for your activities.
- If you are outside for many hours in heat, eat salty snacks and drink water to stay hydrated and replace salt lost through sweating.
- Protect yourself from UV radiation : use sunscreen with an SPF of at least 15, wear protective clothing, and seek shade during the hottest time of day (10 a.m.–4 p.m.).
- Be especially careful during summer months and at high elevation. Because sunlight reflects off snow, sand, and water, sun exposure may be increased during activities like skiing, swimming, and sailing.
- Very cold temperatures can be dangerous. Dress in layers and cover heads, hands, and feet properly if you are visiting a cold location.
Stay safe around water
- Swim only in designated swimming areas. Obey lifeguards and warning flags on beaches.
- Practice safe boating—follow all boating safety laws, do not drink alcohol if driving a boat, and always wear a life jacket.
- Do not dive into shallow water.
- Do not swim in freshwater in developing areas or where sanitation is poor.
- Avoid swallowing water when swimming. Untreated water can carry germs that make you sick.
- To prevent infections, wear shoes on beaches where there may be animal waste.
Schistosomiasis, a parasitic infection that can be spread in fresh water, is found in Kenya. Avoid swimming in fresh, unchlorinated water, such as lakes, ponds, or rivers.
Keep away from animals
Most animals avoid people, but they may attack if they feel threatened, are protecting their young or territory, or if they are injured or ill. Animal bites and scratches can lead to serious diseases such as rabies.
Follow these tips to protect yourself:
- Do not touch or feed any animals you do not know.
- Do not allow animals to lick open wounds, and do not get animal saliva in your eyes or mouth.
- Avoid rodents and their urine and feces.
- Traveling pets should be supervised closely and not allowed to come in contact with local animals.
- If you wake in a room with a bat, seek medical care immediately. Bat bites may be hard to see.
All animals can pose a threat, but be extra careful around dogs, bats, monkeys, sea animals such as jellyfish, and snakes. If you are bitten or scratched by an animal, immediately:
- Wash the wound with soap and clean water.
- Go to a doctor right away.
- Tell your doctor about your injury when you get back to the United States.
Consider buying medical evacuation insurance. Rabies is a deadly disease that must be treated quickly, and treatment may not be available in some countries.
Reduce your exposure to germs
Follow these tips to avoid getting sick or spreading illness to others while traveling:
- Wash your hands often, especially before eating.
- If soap and water aren’t available, clean hands with hand sanitizer (containing at least 60% alcohol).
- Don’t touch your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.
- Cover your mouth and nose with a tissue or your sleeve (not your hands) when coughing or sneezing.
- Try to avoid contact with people who are sick.
- If you are sick, stay home or in your hotel room, unless you need medical care.
Avoid sharing body fluids
Diseases can be spread through body fluids, such as saliva, blood, vomit, and semen.
Protect yourself:
- Use latex condoms correctly.
- Do not inject drugs.
- Limit alcohol consumption. People take more risks when intoxicated.
- Do not share needles or any devices that can break the skin. That includes needles for tattoos, piercings, and acupuncture.
- If you receive medical or dental care, make sure the equipment is disinfected or sanitized.
Know how to get medical care while traveling
Plan for how you will get health care during your trip, should the need arise:
- Carry a list of local doctors and hospitals at your destination.
- Review your health insurance plan to determine what medical services it would cover during your trip. Consider purchasing travel health and medical evacuation insurance.
- Carry a card that identifies, in the local language, your blood type, chronic conditions or serious allergies, and the generic names of any medications you take.
- Some prescription drugs may be illegal in other countries. Call Kenya’s embassy to verify that all of your prescription(s) are legal to bring with you.
- Bring all the medicines (including over-the-counter medicines) you think you might need during your trip, including extra in case of travel delays. Ask your doctor to help you get prescriptions filled early if you need to.
Many foreign hospitals and clinics are accredited by the Joint Commission International. A list of accredited facilities is available at their website ( www.jointcommissioninternational.org ).
In some countries, medicine (prescription and over-the-counter) may be substandard or counterfeit. Bring the medicines you will need from the United States to avoid having to buy them at your destination.
Malaria is a risk in Kenya. Fill your malaria prescription before you leave and take enough with you for the entire length of your trip. Follow your doctor’s instructions for taking the pills; some need to be started before you leave.
Select safe transportation
Motor vehicle crashes are the #1 killer of healthy US citizens in foreign countries.
In many places cars, buses, large trucks, rickshaws, bikes, people on foot, and even animals share the same lanes of traffic, increasing the risk for crashes.
Be smart when you are traveling on foot.
- Use sidewalks and marked crosswalks.
- Pay attention to the traffic around you, especially in crowded areas.
- Remember, people on foot do not always have the right of way in other countries.
Riding/Driving
Choose a safe vehicle.
- Choose official taxis or public transportation, such as trains and buses.
- Ride only in cars that have seatbelts.
- Avoid overcrowded, overloaded, top-heavy buses and minivans.
- Avoid riding on motorcycles or motorbikes, especially motorbike taxis. (Many crashes are caused by inexperienced motorbike drivers.)
- Choose newer vehicles—they may have more safety features, such as airbags, and be more reliable.
- Choose larger vehicles, which may provide more protection in crashes.
Think about the driver.
- Do not drive after drinking alcohol or ride with someone who has been drinking.
- Consider hiring a licensed, trained driver familiar with the area.
- Arrange payment before departing.
Follow basic safety tips.
- Wear a seatbelt at all times.
- Sit in the back seat of cars and taxis.
- When on motorbikes or bicycles, always wear a helmet. (Bring a helmet from home, if needed.)
- Avoid driving at night; street lighting in certain parts of Kenya may be poor.
- Do not use a cell phone or text while driving (illegal in many countries).
- Travel during daylight hours only, especially in rural areas.
- If you choose to drive a vehicle in Kenya, learn the local traffic laws and have the proper paperwork.
- Get any driving permits and insurance you may need. Get an International Driving Permit (IDP). Carry the IDP and a US-issued driver's license at all times.
- Check with your auto insurance policy's international coverage, and get more coverage if needed. Make sure you have liability insurance.
- Avoid using local, unscheduled aircraft.
- If possible, fly on larger planes (more than 30 seats); larger airplanes are more likely to have regular safety inspections.
- Try to schedule flights during daylight hours and in good weather.
Medical Evacuation Insurance
If you are seriously injured, emergency care may not be available or may not meet US standards. Trauma care centers are uncommon outside urban areas. Having medical evacuation insurance can be helpful for these reasons.
Helpful Resources
Road Safety Overseas (Information from the US Department of State): Includes tips on driving in other countries, International Driving Permits, auto insurance, and other resources.
The Association for International Road Travel has country-specific Road Travel Reports available for most countries for a minimal fee.
For information traffic safety and road conditions in Kenya, see Travel and Transportation on US Department of State's country-specific information for Kenya .
Traffic flows on the left side of the road in Kenya.
- Always pay close attention to the flow of traffic, especially when crossing the street.
- LOOK RIGHT for approaching traffic.
Maintain personal security
Use the same common sense traveling overseas that you would at home, and always stay alert and aware of your surroundings.
Before you leave
- Research your destination(s), including local laws, customs, and culture.
- Monitor travel advisories and alerts and read travel tips from the US Department of State.
- Enroll in the Smart Traveler Enrollment Program (STEP) .
- Leave a copy of your itinerary, contact information, credit cards, and passport with someone at home.
- Pack as light as possible, and leave at home any item you could not replace.
While at your destination(s)
- Carry contact information for the nearest US embassy or consulate .
- Carry a photocopy of your passport and entry stamp; leave the actual passport securely in your hotel.
- Follow all local laws and social customs.
- Do not wear expensive clothing or jewelry.
- Always keep hotel doors locked, and store valuables in secure areas.
- If possible, choose hotel rooms between the 2nd and 6th floors.
Healthy Travel Packing List
Use the Healthy Travel Packing List for Kenya for a list of health-related items to consider packing for your trip. Talk to your doctor about which items are most important for you.
Why does CDC recommend packing these health-related items?
It’s best to be prepared to prevent and treat common illnesses and injuries. Some supplies and medicines may be difficult to find at your destination, may have different names, or may have different ingredients than what you normally use.
If you are not feeling well after your trip, you may need to see a doctor. If you need help finding a travel medicine specialist, see Find a Clinic . Be sure to tell your doctor about your travel, including where you went and what you did on your trip. Also tell your doctor if you were bitten or scratched by an animal while traveling.
If your doctor prescribed antimalarial medicine for your trip, keep taking the rest of your pills after you return home. If you stop taking your medicine too soon, you could still get sick.
Malaria is always a serious disease and may be a deadly illness. If you become ill with a fever either while traveling in a malaria-risk area or after you return home (for up to 1 year), you should seek immediate medical attention and should tell the doctor about your travel history.
For more information on what to do if you are sick after your trip, see Getting Sick after Travel .
Map Disclaimer - The boundaries and names shown and the designations used on maps do not imply the expression of any opinion whatsoever on the part of the Centers for Disease Control and Prevention concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Approximate border lines for which there may not yet be full agreement are generally marked.
Other Destinations
If you need help finding travel information:
Message & data rates may apply. CDC Privacy Policy
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.

COMMENTS
Vaccination may be considered for children and adults who are traveling to areas of active cholera transmission. Cholera - CDC Yellow Book. Hepatitis A. Recommended for unvaccinated travelers one year old or older going to the Congo. Infants 6 to 11 months old should also be vaccinated against Hepatitis A.
COVID-19 Vaccine Information: Are vaccines available in the Democratic Republic of the Congo for U.S. citizens to receive? Yes. Vaccines are available at the following approved locations in Kinshasa. Contact local INRB offices for vaccine locations in Goma, Bukavu, and other locations. People interested in receiving the vaccine should contact a ...
A negative PCR test is still required to depart the DRC, regardless of vaccination status. Travelers are still subject to the COVID-19 requirements of all cities, airports, and airlines involved in their travel plans. ... Consult the CDC website for the most up-to-date information. ... Democratic Republic of the Congo, 310 Avenue des Aviateurs ...
The CDC sent out an alert to medical providers in December to look out for travelers into the U.S. as a more lethal type of the mpox virus circulates in the Democratic Republic of Congo.
COVID-19 Information. Last updated: 10/17/2022. The CDC's Order requiring proof of vaccination for non-U.S. citizen nonimmigrants to travel to the United States is still in effect. For more information see Requirement for Proof of COVID-19 Vaccination for Air Passengers . Check the CDC website for additional information and Frequently Asked ...
For additional travel information. Enroll in the Smart Traveler Enrollment Program (STEP) to receive security messages and make it easier to locate you in an emergency. Call us in Washington, D.C. at 1-888-407-4747 (toll-free in the United States and Canada) or 1-202-501-4444 (from all other countries) from 8:00 a.m. to 8:00 p.m., Eastern ...
On 21 March 2022, the US Centers for Disease Control and Prevention (CDC) issued a Travel Alert for polio in Africa; the Democratic Republic of the Congo is currently considered a high risk to travelers for polio; the CDC recommends that before any international travel, anyone unvaccinated, incompletely vaccinated, or with an unknown polio ...
Read the country information page for additional information on travel to the Democratic Republic of the Congo. If you decide to travel to the Democratic Republic of the Congo: Avoid demonstrations. Use caution when walking or driving. Always have a copy of your U.S. passport and DRC visa. Keep originals in a secure location.
Doses of COVID-19 vaccines landing in Kinshasa, DR Congo on 2 March 2021. KINSHASA, 03 MARCH 2021 - More than 1.7 million doses of COVID-19 vaccines have arrived in Kinshasa, the capital of the DRC. They were shipped to the country through COVAX, an alliance comprising the Coalition for Epidemic Preparedness Innovations (CEPI), Gavi, the ...
The information provided for each country includes any State health requirements as well as WHO recommendations for yellow fever vaccination, polio vaccination, and malaria prophylaxis. The country list is produced after consultation with the States Parties to the International Health Regulations (2005) (IHR), and includes input from WHO ...
Rep. Congo. Specific. Advice. Travellers'. Diarrhea Kits. Available. Not to be confused with its Democratic counterpart, the Republic of the Congo borders the country of Gabon to the east and shares coastline with the Democratic Republic of the Congo to the west. Brazzaville is a burgeoning metropolis in the southern region of the country.
The Centers for Disease Control and Prevention (CDC) has issued a Level 4 Travel Health Notice for Democratic Republic of the Congo due to COVID-19. Democratic Republic of the Congo has resumed most transportation options, (including airport operations and re-opening of borders) and business operations (including day cares and schools).
Health risks and recommended vaccines. Check TravelHealthPro's current advice on the Republic of Congo to find out how to reduce the health risks you'll face there. TravelHealthPro also lists ...
The Overseas Refugee Health Guidance provides panel physicians with supplemental guidance on vaccination, pre-departure treatments for malaria and intestinal parasites and fitness to travel. These activities are coordinated with the International Organization for Migration (IOM). Learn more about the role of panel physicians in the US refugee ...
CDC's home for COVID-19 data. Visualizations, graphs, and data in one easy-to-use website. ... Data Tracker Home Trends Maps Hospitalizations Deaths Emergency Department Visits Vaccination Distribution & Coverage Vaccine Effectiveness Variants & Genomic Surveillance Traveler-Based Genomic Surveillance Wastewater Surveillance Post-COVID ...
Specific. Advice. Travellers'. Diarrhea Kits. Available. The Democratic Republic of the Congo (DRC), located in Central Africa, was previously known as Zaire. In area it is the second largest country in Africa. Travellers visiting the DRC will have a lot to explore including rainforests and wildlife. They can also enjoy city life as well as ...
Since May 2022, when the mpox outbreak hit the U.S., the country has seen more than 30,000 cases, most of which occurred in 2022. By the start of 2023, infection rates had slowed — the U.S ...
COVID-19 vaccination in Democratic Republic of Congo was made possible using COVAX, an international scheme to make safe and effective COVID-19 vaccines worldwide. [2] More than 90% of the doses received are the Oxford-AstraZeneca vaccine manufactured in India. [2] Congo received 1.7 million doses via COVAX.
US CDC travel Advisory April 5, 2024. (Precision Vaccinations News) A multi-month chikungunya virus outbreak continues impacting the residents of Timor-Leste (East Timor). As of late March 2024, 195 chikungunya cases have been reported in Timor-Leste. To alert international travelers, the U.S. CDC reissued a Level 2 - Practice Enhanced ...
Those who received the vaccine in the 1960s should check their vaccine records. If you received the "LIVE measles vaccine in the 1960s," the CDC says you do not need to be revaccinated. The ...
All international travelers should be fully vaccinated against measles with the measles-mumps-rubella (MMR) vaccine, including an early dose for infants 6-11 months, according to CDC's measles vaccination recommendations for international travel. Measles (Rubeola) - CDC Yellow Book. Meningitis (Meningococcal disease)