- Skip to main content
- Keyboard shortcuts for audio player

Health Care
Why an er visit can cost so much — even for those with health insurance.

Terry Gross
Vox reporter Sarah Kliff spent over a year reading thousands of ER bills and investigating the reasons behind the costs, including hidden fees, overpriced supplies and out-of-network doctors.
TERRY GROSS, HOST:
This is FRESH AIR. I'm Terry Gross. You wouldn't believe what some emergency rooms charge, or maybe you would because you've gotten bills. For example, one hospital charged $76 for Bacitracin antibacterial ointment. One woman who fell and cut her ear and was given an ice pack but no other treatment was billed $5,751. My guest, Sarah Kliff, is a health policy journalist at vox.com who spent over a year investigating why ER bills are so high even with health insurance and why the charges vary so widely from one hospital to the next.
Through crowdsourcing, she collected over a thousand ER bills from around the country. She interviewed many of the patients and the people behind the billing. She's reported her findings in a series of articles on Vox. She's also spent years reporting on the battle over health insurance policy. We'll get some updates on the state of Obamacare a little later in the interview.
Sarah Kliff, welcome back to FRESH AIR. Why did you want to do an investigation into emergency room billing?
SARAH KLIFF: You know, I wanted to do this because the emergency room is such a common place where Americans interact with the health care system. There are about 140 million ER visits each year. It's a place where you can't really shop for health care. You can't make a lot of decisions about where you want to go. So I think that is big-picture what got me interested.
Small picture was actually a bill that someone sent me almost three years ago now, where they took their daughter to the emergency room. A Band-Aid was put on the daughter's finger, and they left. And they got a $629 bill. And they said - you know, they - the parents sent this to me, saying, how could a Band-Aid cost $629? And I said, I don't know, but I'm going to find out. And that kind of opened up the door to this, you know, multi-year project I've been working on right now. It started with trying to figure out why a Band-Aid would cost $629.
GROSS: OK. So let's get to that $629 for treatment that was basically a Band-Aid placed on a finger. You investigated that bill.
KLIFF: Yes.
GROSS: Why'd it cost so much?
KLIFF: So what cost so much was really the facility fee. So this is a charge I hadn't heard about before as a health care reporter. This is a charge that hospitals make for just keeping their doors open, keeping the lights on, the cost of running an emergency room 24/7. So if you look at that particular patient's bill, the Band-Aid - you know, I hesitate to say only - but the Band-Aid only cost $7, which, as anyone who's bought Band-Aids knows, is quite expensive for a single Band-Aid.
But the other $622 of that bill were the hospital's facility fees for just walking in the door and seeking service. And these fees are not made public. They vary wildly from one hospital to another. And usually patients only find out what the facility fee of their hospital is when they receive the bill afterwards, like that patient, you know, that sent me this particular bill.
GROSS: And does the facility fee vary from facility to facility?
KLIFF: It does significantly. You know, I've seen some that are in the low hundreds. I've seen some that are in the high thousands. And it's impossible to know what facility fee you're going to be charged until you actually get the billing documents from your hospital. And if you try and call up a hospital and ask what the facility fee is, usually you won't get very far.
So it's this fee that, from all the ER bills I've read, is usually the biggest line item on the bill. But it's also one that is very, very difficult to get good information about until you've already been charged.
GROSS: So you're paying the facility fee to basically share in the cost of running the emergency room.
KLIFF: Yes, that's how hospital executives would describe the fee.
GROSS: But you don't know that when you're going to the emergency room.
KLIFF: You don't, no. And you don't know how much it'll be. You don't know how it's being split up between different patients. You don't know any of that.
GROSS: So is this also why one bill had $60 for the treatment of ibuprofen and another $238 for the treatment of eyedrops?
KLIFF: Yeah. And, you know, this is something I see all the time reading emergency bills - I've read about 1,500 of them at this point - is that things you could buy in a drugstore often cost significantly more in the emergency room. And the people I talked to who run hospitals will say this is because they have to be open all the time. They have to have so many supplies ready.
But I think one of the things that I find pretty frustrating is, you know, patients aren't usually told, we can give you an ibuprofen here, or you can pick some up at the drugstore if you leave, and the cost will be a fraction of what we would charge you here. That information often isn't conveyed to patients who are well enough, you know, to go to a drugstore on their own. But it's just huge variation for these simple items.
One place I see this a lot is pregnancy tests. If you're a woman who's of childbearing age, you go to the emergency room, they will often want to check if you're pregnant. I've seen pregnancy tests that cost a few dollars in emergency room. The most expensive one I saw was over $400. I believe that was at a hospital in Texas. It's just widespread variation for, you know, some pretty simple pieces of medical equipment.
GROSS: I want to get back to the $60 ibuprofen. Is that - does that include the facility fee? Or is that just for the ibuprofen, and the facility fee is separate?
KLIFF: That's just for the ibuprofen. The facility fee is totally separate.
GROSS: So how do they justify that?
KLIFF: They say they have to stock, like, a wide array of medicine, so they have to have everything on hand from ibuprofen, from, you know, expensive rabies treatments - I've talked to a lot of people who've been to the emergency room for exposure to bats and raccoons - and that they need to have all these things in stock. And, you know, one of the things you pay for at the emergency room is the ability to get any medication at any hour of the day right when you need it. I don't necessarily buy that explanation, to be clear. That's what I've heard from hospital executives.
I think it's pretty telling that ibuprofen has a very, very different price depending on which emergency room you go to. The fact that there's so much widespread price variation suggests to me that it's not just the cost of doing business driving it, that there's also business decisions being made behind ibuprofen that are driving the prices different hospitals are setting.
GROSS: Now, of course, trips to the emergency room aren't always as simple as getting a Band-Aid or ibuprofen or some eyedrops. I want you to describe the case of a young man who was hit by a pole on a city bus in San Francisco.
KLIFF: Yeah. So this patient, his name is Justin. He was a community college student in northern California, was walking down a sidewalk in downtown San Francisco one day. And there was a pole hanging off the back of the bus that wasn't where it's supposed to be. It essentially flew off the back of the bus, hit him in the face and knocked him unconscious.
And the next thing he knows, he's waking up at Zuckerberg San Francisco General, which is the only Level I trauma center in the city. He ends up needing a CT scan to check out some brain injuries. He needs some stitches. And then he's discharged. He ends up with a bill for $27,000.
But, you know, as I began figuring out through my reporting, San Francisco General does not contract with private insurance, and they end up pursuing him for the vast majority of that bill. He has $27,000 outstanding. And somewhat ironically, San Francisco General, it is the city hospital. It is run by the city of San Francisco. So this student is hit by a city bus, taken by an ambulance to the city hospital and ends up with a $27,000 bill as a result.
GROSS: So did he have insurance?
KLIFF: He did. He had insurance through his dad.
GROSS: So why doesn't Zuckerberg San Francisco General Hospital contract with private insurers?
KLIFF: So what they have told me when I've talked to some spokespeople there is that they are a safety net hospital, and that is, you know, definitely true. They generally serve a lower-income, often indigent population in San Francisco that would have trouble getting admitted and seeking care at other hospitals in the city. So they have told me that their focus is on serving those patients and that therefore, you know, they're not going to contract with private insurance companies.
The thing I found a little bit confusing about that, though, is there are lots of public hospitals, say, that, you know, also serve low-income populations. And some of them for their inpatient units, you know, for their scheduled surgeries, they're not going to contract with private insurance because they want to make sure beds are available for the publicly insured folks and people on Medicaid and Medicare.
But when it comes to the emergency room, you know, every other public hospital I was in touch with would contract with private insurers there because people don't decide if they're going to end up in the emergency room. So, you know, that's the justification they offered, that it is a hospital meant to serve those with public insurance. But it is not something you see public hospitals typically doing.
GROSS: Isn't - I think legislation was proposed in California to change that. Did that pass?
KLIFF: It's still pending in the California State Assembly. And the hospital has also promised to reform its billing practices, although we haven't seen what exactly their new plan is yet.
GROSS: So the position that Justin was in is that, like, he's unconscious. He's not asking to be taken anyplace. (Laughter) But he's unconscious. He's taken to the emergency room and ends up getting this $27,000 bill. I mean, that just seems so unfair, especially since he has insurance.
KLIFF: Yeah.
GROSS: Like, it's supposed to cover him for things like that (laughter).
KLIFF: Yeah. You know, there's one other patient who kind of makes this point really well who was also seen at San Francisco General. Her name is Nelly. And she fell off a climbing wall and, somewhat amazingly, you know, turns out she had a concussion. But one of the first things she does is she calls her insurance's nursing hotline to ask, should I go to the ER?
And they say yes. And she says, can I go to Zuckerberg San Francisco General? It's the closest. They say, no, don't go there. It's not in network. Go to another hospital. She gets to the other hospital, but the other hospital won't see her because she's a trauma patient. She fell from a really high height. And San Francisco General is the only trauma center in San Francisco. So she tries to go to an in-network hospital. She's then ambulance-transferred to Zuckerberg San Francisco General, and she ends up with another bill over $20,000 that the hospital was pursuing from her until I started asking questions from it, and the hospital ultimately dropped the bill.
But I think it's just such a frustrating situation for someone like Justin, for someone like Nellie (ph). They're either shopping for this good unconscious, they're really trying to do the right thing, and the health care system is just so stacked against the patient. It's so stacked for the hospital to be able to bill the prices that they want to bill.
GROSS: So apparently, the moral of the story is if you want to challenge your emergency room bill, you should get Sarah Kliff to write about you. (Laughter).
KLIFF: It's - (laughter). That's what some people have said. But there's only one of me, and there's about 2,000 bills in our database. And, you know, we have had over $100,000 in bills reversed as a result of our series. But I don't think it's a great way to run a health care system where we just, you know, the people who get their bills reversed are those who are lucky enough to have a reporter write a story about them.
GROSS: Yes. Agreed. Let me reintroduce you. If you're just joining us, my guest is Sarah Kliff. She's a senior policy correspondent at Vox, where she focuses on health policy. She also hosts the Vox podcast, "The Impact," about how policy actually affects people.
So we're going to take a short break, and then we'll talk more about emergency billing. And then later, we'll talk about what's left of Obamacare, and what the president and Congress and candidates are saying about health care, after this break. This is FRESH AIR.
(SOUNDBITE OF ALEXANDRE DESPLAT'S "SPY MEETING")
GROSS: This is FRESH AIR. And if you're just joining us, my guest is Sarah Kliff. We're talking about emergency room billing and why it's so unpredictable and often so incredibly high. She's a senior policy correspondent at Vox, where she focuses on health policy. She also hosts the Vox podcast, "The Impact," about how policy affects people.
So we were talking about the hidden facility fee, which most people don't know exists, and is responsible for a large chunk of a lot of emergency room bills. There's also, like, a trauma unit fee. It's a similar hidden fee in hospitals that have trauma centers in their emergency rooms. So explain the trauma fee and how that kicks in.
KLIFF: Yeah. This is something I also had never heard of till I started reading a lot of emergency room bills, and this is the fee that trauma centers charge for essentially assembling a trauma team to meet you when you're coming in and those folks out in the field, maybe the EMTs, for example, have determined that you meet certain trauma criteria.
So I've talked to people who have been charged trauma fees who were in serious car accidents. One case was a baby who fell from more than 3 feet, and that's considered to trigger a trauma activation. So this is essentially the price for having a robust trauma team - a surgeon, an anesthesiologist, nurses - all at the ready to receive you when you get to the hospital.
And again, these fees can be pretty hefty. San Francisco General, which, I've done the most reporting on their billing, you know, they can charge up to $18,000 for their trauma activation services. I wrote about one family who was visiting San Francisco from Korea when their young son rolled out of the hotel bed. They were nervous. They didn't know the American health care system well. So they called 911, which sent an ambulance, brought him over to the hospital. Turns out, he was fine. They gave him a bottle of formula. He took a nap and went home.
And then a few months later, they get an $18,000 charge for the trauma team that assembled for when that baby came to the hospital. And these are another, you know, pretty significant fee that, again, you don't really know about. You have no idea that the trauma team is assembling to meet you when you're coming into the hospital. You just find out after the fact. And you also have no say in the decision to assemble trauma. That's really left up to the hospital, not the patient.
GROSS: So I'm going to have you compare two possibilities. You go to an emergency room, and the bill is very high. There's two people who have the same problem who go to the emergency room. One of them has a copay. One of them has a high deductible that they haven't paid off yet. How are they treated differently, in terms of what they're billed for the emergency room visit?
KLIFF: Well, the person with the deductible will likely be billed significantly more. You know, if they're just, let's say, at the start of the year, they are going to essentially have to bear the costs of that emergency room visit up until the point they hit their deductible and the insurance kicks in, whereas the person who has a co-payment, they're just going to have to pay that flat fee and, you know, probably not worry about paying more, but there's often surprise bills lurking in the corner that could affect both of those patients as well.
GROSS: Like what?
KLIFF: So one of the most common things we see is out-of-network doctors working at in-network emergency rooms. So you know, you have an emergency, you look up a hospital, you see their ER is in network, so you go there. It turns out that emergency room is staffed by doctors who aren't in your insurance. There's pretty compelling academic research that suggests 1 in 5 emergency room visits involves a surprise bill like that one.
GROSS: That seems so unfair. How are you to know - if you're choosing a hospital that's in network, how are you to know whether the doctor treating you is in network or not?
KLIFF: You know, you really - there isn't a great way to tell, to be honest. This is - you know, when I had to go to the emergency room over the summer, you know, this is something I worried about. You know, I was seeing a doctor who worked for the hospital, but they were sending off my ultrasound to be read by a radiologist who I was never going to meet. I couldn't ask them if they were in-network. I just kind of had to cross my fingers and hope for the best, and luckily, I didn't get a surprise bill.
But I've talked to multiple patients who, you know, tried to do their research, who thought they were in network, only to get a bill, often for thousands of dollars, after leaving the emergency room, from someone who, you know, never mentioned to them, hey, I'm not in your network like this hospital is.
GROSS: So the bill that you'd get would be for the difference between what you pay when somebody is - when a doctor's in network and what you pay when they're not in network?
KLIFF: Yeah, often it's just what that out-of-network doctor wants to charge. So a good example of this is a patient I wrote about in Texas named Scott (ph), who was attacked in downtown Austin, left on the street unconscious, some bystander called him an ambulance, and he woke up at a hospital. And one of the first things he does, because this is the United States, is he gets on his phone and tries to figure out which hospital he is at, and, you know, is that in his insurance network? And he finds out - good news - it is. And a surgeon comes by, tells him he's going to need emergency jaw surgery because of the attack that happened.
So he says, OK. You know, he's not really in a place to go anywhere. Gets the surgery. Goes home. A few weeks later, he gets an $8,000 bill from that oral surgeon, who the insurance companies paid a smaller amount. The oral surgeon didn't have a contract with the insurance and said, you know, I think my services are worth a lot more, so pursued the balance of the bill from Scott.
GROSS: I have to say, I mean, that does seem unfair to the patient because they haven't been informed. They can't make a choice about it if they don't know. And, like, $8,000 is a lot of money.
KLIFF: Yeah. And I think, you know, even more, let's say he did say he was out of network. It kind of puts the patient in an unfair situation, too. You know, one of the things we talk about a lot in health policy is, what if we had more transparency? What if we let patients know the prices? What if we let patients know who is in and out of network? And that - it would be a good step.
But, you know, I think with someone like Scott, sitting in a hospital with a broken jaw, there's not much you can do with that information. He doesn't have, you know, the ability to go home, like, research, like, make an appointment with a new surgeon. So, you know, it'd be great if he knew that the doctor was out of network. It'd be even better if he had some kind of protections against those type of bills.
GROSS: What kind of protection could there be?
KLIFF: So we're actually seeing a lot of action on this in Congress. There's some pretty strong bipartisan support for tackling this specific issue and essentially holding the patient harmless. When there is a situation like Scott's, for example, where there's this $8,000 bill, that's really a dispute between a health insurance company and a doctor, where the doctor says, I want more money, the insurer says, I want to pay you less money. And what Congress wants to do - what a few states have already done with their laws - is said, you can't go to the patient for that money. You, the hospital, and you, the health insurance company, you have to get down to a table and work things out together.
And some state laws will set certain amounts that are allowed to be charged, other ones will force the insurance company and the hospital into an arbitration process. But the general concept is to take the patient out of this billing situation because, like you said, Terry, they really aren't in a position to negotiate. They aren't in a position to shop. They shouldn't be the ones who are left holding the bag at the end of the day.
GROSS: My guest is Sarah Kliff. She covers health policy for Vox. After a break, we'll talk more about why ER bills can have some unpleasant surprises, and she'll give us an update on Obamacare. And Maureen Corrigan will review two books about forgotten stories from Hollywood. I'm Terry Gross, and this is FRESH AIR.
(SOUNDBITE OF JESSICA WILLIAMS TRIO'S "KRISTEN")
GROSS: This is FRESH AIR. I'm Terry Gross. Let's get back to my interview with journalist Sarah Kliff, who covers health policy and how it affects people for Vox. For the past year and a half, she's been writing about why emergency room visits can be so expensive and the pricing so secretive and mysterious, as well as inconsistent from one hospital to the next. She collected over 1,000 bills and tracked down stories behind the billing. She interviewed many of the patients and the people behind the billing to decipher why ER bills can have some surprise costs.
Here's another surprise that often awaits people who go to emergency rooms - some insurance plans only cover true emergencies, and whether it is a true emergency is sometimes determined after the diagnosis is made. So how are you supposed to know before the diagnosis whether you're going to be categorized as a true emergency or not? Like, if you go to the hospital, you don't know if you have a broken bone or not.
KLIFF: Right.
GROSS: Somebody needs to X-ray it and tell you.
KLIFF: Right. The whole point you go to the emergency room is to help them figure out what the emergency is and what treatment you need. This is a policy that the insurance company Anthem has been pioneering for a few years. It's been in Kentucky. It's been in Georgia - a few other states. And, you know, I wrote about one patient out in Kentucky named Brittany, who - she was having really severe abdominal pain. She called her mom who is a nurse, and the nurse said, that might be appendicitis. You've got to get to the emergency room. Turns out it wasn't appendicitis. It was an ovarian cyst. She got it treated elsewhere later down the line.
And Anthem, you know, sent her a letter saying, we're not going to cover that visit because it was not a true emergency. She appealed it. Her appeal was denied. This is another one where, once I started asking them about it, the bill suddenly disappeared. But - and it seems like as Anthem has gotten more attention for this policy - they haven't announced it publicly, but some pretty compelling data The New York Times got their hands on suggest they've backed off this policy.
But it's just, you know - there are so many traps you can fall into going into an emergency room. It just feels like you're walking into this minefield, and this is kind of one of those mines that's lurking in there.
GROSS: Hospital pricing and emergency room pricing seems to vary so much from hospital to hospital. Are there, like, national guidelines that help determine what a hospital or a hospital emergency room charges for services? I mean, who decides, and why is there such a variation?
KLIFF: So hospital executives get to decide, and I think that is why there is such variation. There aren't really guidelines that they're following. You know, one thing you could do as a hospital executive - you could look at what Medicare charges - those prices are public - and, you know, maybe use that as a benchmark. There are some databases. There's one called FAIR Health, for example, where you could look and see, you know, some information on what local prices typically are. But in terms of, you know, what you want to charge, that's kind of up to you as someone running a hospital.
One of the things that's really, really unique about the United States, compared to our peer countries, is that we don't regulate health care prices. Nearly every other country in the developed world - they see health care something as, you know, akin to a utility that everyone needs, like electricity or water. It's so important that the government is going to step in and regulate the prices. That doesn't happen in the United States. You know, if you're a hospital, you just choose your prices. And, you know, that is, I think, why you see so much variation and why you see some really high prices in American health care.
GROSS: So what advice do you have for people who actually need an emergency room and don't want to get hit with a shocking bill afterwards?
KLIFF: Yeah, this is, you know, one of those questions - it just makes me a little frustrated that - 'cause this is the most common question I get - right? - is, how do I - how do we - how do I prevent a surprise bill? And I find it kind of upsetting that, you know, it has to be on the patient because honestly, there really isn't a great way to do this. I've talked to so many patients who tried so hard to avoid a big medical bill and weren't able to.
You know, there's certain things, yes, you can do. You can look up the network status of your hospital. You can try and badger each doctor you see about whether they are in network. You can try to be a really proactive patient, but I think that's just such a huge burden on people who are in, like, really emergent situations. And some people don't have that opportunity, you know, like Justin Zanders, the guy we were talking about earlier who was taken to a hospital while he was unconscious. I cannot think of anything he could've done to avoid that bill. It just was not possible.
GROSS: So your advice is, good luck.
KLIFF: Short of that, I mean, good luck. You know, I'm actually in the middle of reporting a story right now about people who have successfully negotiated down their bills. And, you know, you can certainly - if you do end up with a surprise bill, you can call up the hospital, see if there's a discount. Sometimes there will be. Sometimes there won't. You can call again. Customer service representatives - different ones - often offer you different discounts, I've learned from interviewing patients. You can ask for a prompt pay discount if you pay right away.
You can - you know, one health attorney who negotiates these a lot on behalf of patients - he says one of his favorite tactics is to choose the amount you want to pay; send a check with that amount; and in the note, write, paid in full; and hope they don't come after you after that. I have no idea if that works or not, but he says it works for his patients. But it's a mixed bag. And at the end of the day, the hospital has all the power. You can ask for discounts. You can ask nicely. You can ask angrily. It's up to the hospital if they want to grant you that or not.
GROSS: So what is the status of Obamacare now? You know, Republicans promised to repeal and replace. That didn't work out. So have Republicans given up on repeal and replace?
KLIFF: For the time, it seems pretty clear that repeal and replace is dead on arrival, especially with Democrats taking control of the House this year. Those proposals aren't being talked about as much. They're not really going anywhere. The one big thing we did see Republicans succeed at is repealing Obamacare's individual mandate, the requirement that all of us carry health insurance. That happened as part of the big tax package that passed at the end of 2017.
So we've seen, you know, President Trump, for example, essentially declare victory, declare that repealing the individual mandate is repealing Obamacare, so we're good on that goal. But, you know, generally, Obamacare is still standing. There are millions of people getting their coverage through the Affordable Care Act still today.
GROSS: So now that there's no individual mandate, conservative attorney generals are challenging Obamacare - the Affordable Care Act - and saying it's no longer constitutional after Congress's repeal of the individual mandate. Could you explain that?
KLIFF: Yeah, so this is a challenge that's come up through the courts in the past few months. Obamacare is constantly being challenged in court. It's been through multiple Supreme Court suits. This one - you know, it's a multiple-part argument, so I'll try my best to walk through it.
KLIFF: So essentially, it starts with the fact that the individual mandate - they weren't quite able to repeal it for boring technical reasons. But what they were able to do is change the fee for not having health insurance from $700 to $0. So it - in all practical terms, it feels like repealing it because there is no fee for not carrying health insurance. The individual mandate was upheld as a tax when the Supreme Court said, yes, this is constitutional. The government has a right to tax people. Now that there is no fee associated with not carrying health insurance, the conservative attorneys general who are bringing this case argue that it's not a tax anymore, and therefore, it is not constitutional. That whole defense that John Roberts wrote in 2012 is moot. So that's the first part of it.
They go even further and say the individual mandate is so core to the Affordable Care Act, it is not severable. And if you, the courts, rule the individual mandate unconstitutional, then you need to rule all of Obamacare unconstitutional. And the first judge who heard this case - he is a, you know, judge in a district court in Texas. He agreed with them. He agreed that - first step - that the individual mandate is no longer constitutional. And second step, that means that the entirety of Obamacare has to fall. This is now being appealed up to the 5th Circuit Court of Appeals.
And I will say there are a lot of critics of this case. There are a lot of people who were parties to previous Supreme Court challenges to Obamacare who think this is a bad legal argument and that it will not succeed. But it is already, you know, gone through the district court level. It's moving up to the appellate court level. It is something that is in the mix that could become a threat to the Affordable Care Act.
GROSS: Well, if it goes to the Supreme Court, it would be very interesting to see what Justice Roberts says since he voted for the ACA, saying that the individual mandate was a tax.
KLIFF: Yeah. You know, and I think where some legal scholars would see it shaking out is that the - someone like John Roberts, he might agree, OK, yeah, the individual mandate is unconstitutional, but would not make the leap to the second half of this, that the rest of the law has to fall.
I think one of the most compelling arguments against this case is that Congress knew what they were doing when they repealed the individual mandate. You know, they had the opportunity to repeal Obamacare. They didn't. They'd specifically took aim at this one specific part. So it feels like it might be a bit of a reach to argue that what Congress really meant to do was repeal all these other parts of the Affordable Care Act. But, you know, the Supreme Court is changing. We have a new justice. You know, we have a lot in the mix. So it's always an open question of how a decision like this could go.
GROSS: So correct me if I'm wrong here - the Department of Justice has sided with the conservative attorneys general who are challenging Obamacare, saying it's no longer constitutional, and I think that the Justice Department is also asking the judge to strike down the ACA's mandatory coverage of pre-existing conditions.
KLIFF: Yeah, that's right. So it's a kind of unusual situation. Usually, it's the Justice Department that is going to defend a federal law in court. But, you know, given the Trump administration's opposition to the Affordable Care Act, they have decided to side with the conservative attorneys general. They have a slightly different argument. They don't think all of Obamacare should fall if the mandate falls, but they do think some big parts, like you mentioned, the protections for pre-existing conditions, should be ruled unconstitutional if the mandate falls.
So this has led to a bit of an unusual situation where you've had this coalition of Democratic attorneys general step in and take over the case, basically saying that the federal government is going - is not going to defend the Affordable Care Act. We are going to defend the Affordable Care Act. So you have this coalition of Democratic attorneys general, led by the attorney general of California, stepping in and, you know, offering a defense as this case works its way up through the court system.
GROSS: Let's take a short break here, and then we'll talk some more. If you're just joining us, my guest is Sarah Kliff. She's senior policy correspondent at Vox, where she focuses on health policy. And she hosts the Vox podcast "The Impact," about how policy actually affects people. We'll be right back. This is FRESH AIR.
(SOUNDBITE OF THE WEE TRIO'S "LOLA")
GROSS: This is FRESH AIR. And if you're just joining us, my guest is Sarah Kliff, senior policy correspondent at Vox, where she focuses on health policy.
Do you think health insurance is shaping up to be a big issue in the 2020 campaign?
KLIFF: I do, and I think it's going to be a big issue both in the primary, where you're already seeing candidates get pressed on, should we still have private health insurance, and giving pretty different answers to that question.
And then I think one of the things you're also going to see is whoever is the Democratic nominee is probably going to run on Obamacare. They are going to point at the fact that President Trump tried to repeal the Affordable Care Act. That's pretty different than, you know, the 2012 election, where Democrats were pretty scared to run on Obamacare. It still wasn't popular. The benefits hadn't rolled out. In this past midterm and now again in the 2020 election, it seems pretty clear that Democrats are pretty excited to point out that Republicans wanted to repeal Obamacare. So I think it really will come up.
GROSS: What are some of the biggest falsehoods you've heard from politicians about health insurance costs or health insurance policy?
KLIFF: You know, one of the ones that's come up a lot is actually around the role of private health insurance. So I've - I don't know if it counts as a falsehood, but I think it's a bit of a misunderstanding of how health insurance often works is, you know, when I talk to single-payer supporters, most of them want to eliminate private insurance completely. They just don't think there is a role for it in the health care system.
And one of the things I think that's actually pretty interesting, when you look at any other country - you look at Canada, you look at the U.K., you look at France, which all have national health care systems - all of them have a private health insurance market, too. There are always some kind of gap in the system that the public insurance can't cover, where the government step - where the private industry steps in and offers coverage. In Canada, for example, their public health plan doesn't cover prescription drugs, so two-thirds of Canadians take out a private plan, often through their employer, like us, to cover prescription drugs, to cover their eyeglasses, to cover their dental. So I think that's a confusion I see a lot in the "Medicare for All" debate coming up right now.
I think the other thing I see a lot of confusion around - and we've talked about this a little bit with emergency room billing - is the role of transparency in health care. I see a lot of, you know, if we just made the prices public, like, that is what we need to do to fix the system, and I think that really misses the fact that, even if the prices were public, health care is so different from everything else we shop for. It might be - I think it is the only thing we purchase when we are unconscious.
GROSS: (Laughter).
KLIFF: And when you're unconscious, you're not really going to be great at price shopping. So I see that as, you know, a halfway solution that I often hear talked about here in Washington that would be great but is not going to suddenly result in, you know, prices dropping because they've been exposed in a spotlight.
GROSS: Is there a country that you think has a good health care model that we could borrow?
KLIFF: Oh, yeah. I've been thinking about this a lot lately actually. So I've gotten very interested in the Australia health care system, which is a little far away. But I think they're a really interesting model because they have a public system, everyone's enrolled in it, but they also really aggressively try and get people to buy a private plan, too, and that private plan will get you sometimes faster access to doctors, maybe a private room at a hospital.
It's really hard for me to see the U.S. creating a health care system, similar to Canada's actually, where you can't buy private insurance, where if you're rich or you're poor, everyone waits in the exact same queue, you can't jump to the front of the line. Because I think wealthier Americans have gotten so used to having really good access to health care that they would be very upset with a system like that.
I think Australia is a kind of interesting hybrid between, you know, where we're at in the U.S. right now and what Canada is like, where it says, yes, we're going to create a public system for everybody, but we're also going to have these private plans that compete against the public system. So I've become increasingly, you know, interested in how Australia's system works. And they have - about 47 percent of Australians are buying a private plan to cover the same benefits that the public plan does.
GROSS: So it's not supplemental. It's instead of.
KLIFF: Right. So it's very different from Canada. So in Canada, you can buy complementary insurance, you know, to cover the benefits the public plan doesn't but the government expressly outlaws supplemental insurance. You know, like, what people buy here to cover the gaps in Medicare, that is not allowed. You cannot buy your way to the front of the line in Canada.
One of my favorite sayings about the Canadian health care system is from a doctor in a book I read about Canadian health care is they said, you know, we're fine waiting in lines for health care in Canada as long as the rich people and the poor people have to wait in the exact same line. Their system is all about equality. And I just don't know that we're at a place as a country where we value the same sort of equality in our health care system.
GROSS: Is there any developed country around the world that has a system similar to ours with all these competing insurance companies and, you know, some government plans and, like, a thousand different bureaucracies that doctors have to deal with and that patients have to deal with?
KLIFF: Absolutely not. There's nothing like it. I mean, our system is so unique. I'd say the closest but it's not even close are a few countries that have national health care systems, but they do it through tightly regulated private health insurance plans. So if you look at, like, Netherlands or Israel, there isn't a government-run plan. Instead, in both countries, you actually have four tightly regulated health insurance plans that compete against each other for the citizens' business. I guess that's the closest, but that is so different from what we have here right now. There's really nothing like it in any developed country.
GROSS: Sarah Kliff, thank you so much for talking with us.
KLIFF: Well, thank you for having me.
GROSS: Sarah Kliff covers health policy for Vox, where you'll find her series about emergency room bills. After we take a short break, Maureen Corrigan will review two books about forgotten stories from Hollywood. This is FRESH AIR.
(SOUNDBITE OF GEORGE FENTON AND PHILHARMONIC ORCHESTRA'S "MISS SHEPHERD'S WALTZ")
Copyright © 2019 NPR. All rights reserved. Visit our website terms of use and permissions pages at www.npr.org for further information.
NPR transcripts are created on a rush deadline by an NPR contractor. This text may not be in its final form and may be updated or revised in the future. Accuracy and availability may vary. The authoritative record of NPR’s programming is the audio record.

How much does an ER visit cost?
$1,500 – $3,000 average cost without insurance (non-life-threatening condition), $0 – $500 average cost with insurance (after meeting deductible).

Average ER visit cost
An ER visit costs $1,500 to $3,000 on average without insurance, with most people spending about $2,100 for an urgent, non-life-threatening health issue. The cost of an emergency room visit depends on the severity of the condition and the tests, treatments, and medications needed to treat it.

Cost data is from research and project costs reported by BetterCare members.
Emergency room visit cost with insurance
The cost of an ER visit for an insured patient varies according to the insurance plan and the nature and severity of their condition. Some plans cover a percentage of the total cost once you meet your deductible, while others charge an average co-pay of $50 to $500 .
The No Surprises Act , effective January 1, 2022, protects insured individuals from unreasonably high medical bills for emergency services received from out-of-network providers at in-network facilities. The act also established a dispute resolution process for both insured and uninsured or self-pay individuals.
Cost of an ER visit without insurance
An ER visit costs $1,500 to $3,000 on average without insurance for non-life-threatening conditions. Costs can reach $20,000+ for critical conditions requiring extensive testing or emergency surgery. Essentially, the more severe your condition or issue, the more you are likely to pay for the ER visit.
Factors that impact ER visit costs
Many factors affect the cost of an ER visit, including:
Facility type – Freestanding emergency departments often cost 50% more than hospital-based emergency rooms.
Time of day – An ER visit at night typically costs more than the same type of visit during the day.
Level of care – The more severe your condition is, the more time and expertise it takes to diagnose and treat, and the higher the total ER visit cost.
Ambulance ride – An ambulance ride costs $500 to $1,300 on average, depending on whether you need basic or advanced life support during transport.
Medications – Oral medications, injections, or IVs needed during your stay all add the total cost of your ER visit.
Medical equipment & supplies – Any other supplies used to diagnose and treat you—such as a cast for a broken bone or bandages and sutures to close an open wound—increase the cost.
Testing – Each medical test is typically a separate charge. Tests may include urine tests, blood tests, X-rays, or other more advanced imaging tests.
Insurance coverage:
Out-of-pocket costs may be higher for those with high-deductible insurance plans.
While ER visit costs are generally higher for the uninsured, many hospitals offer discounts for self-pay patients.

ER facility fee by level
An ER facility fee ranges from $200 to $4,000 , depending on the severity level of your symptoms and condition. The facility fee is the cost to walk in the door and be evaluated by a physician. Other services you may need, such as lab tests, imaging, and surgical procedures, are charged separately.
To understand your ER bill: Emergency rooms rank severity levels 1 through 5, with Level 1 being the most severe or urgent. However, most of the billing codes for emergency room visits are reversed, with level 1 being the least severe.
Common conditions and procedures
The table below shows the average ER visit cost for common ailments. Prices vary greatly depending on how much testing and expertise is required to accurately diagnose and treat you.

Emergency room vs. urgent care
An ER visit costs $1,500 to $3,000 , while the average urgent care visit costs $150 to $250 without insurance. Urgent care facilities can treat most non-life-threatening conditions and typically have less wait time than the ER. For more detail, check out our guide comparing the cost of an emergency room vs. urgent care .
Other alternatives to the ER for less serious health issues include primary care, telemedicine, and free clinics. Check with the National Association of Free and Charitable Clinics to find a free clinic near you.
FAQs about ER visit costs
Why are er visits so expensive.
ER visits are expensive because emergency rooms run on a 24-hour schedule and require a large and wide range of staff, including front desk personnel, maintenance, nurses, doctors, and surgeons. ERs also run and maintain a lot of expensive equipment and need a constant supply of medications and medical supplies.
While ER visits can be expensive, ER bills are negotiable. If you receive an unexpectedly large ER bill, ask for a discount and question the coding.
Does insurance cover ER visits?
Insurance typically covers some or all of an ER visit, though you may need to meet a deductible first, depending on the plan. The Affordable Care Act requires insurance providers to cover ER visits for "emergency medical conditions" without prior authorization and regardless of whether they are in or out-of-network.
An "emergency medical condition" is considered something so severe that a reasonable person would seek help right away to avoid serious harm.
When should you go to the ER?
You should go to the ER for any serious, potentially life-threatening symptoms, including:
Trouble breathing
Serious head injury
Sudden severe pain
Severe burn
Severe allergic reaction
Major broken bones
Uncontrollable bleeding
Suddenly feeling weak or unable to move, speak, or walk
Sudden change in vision
Sudden confusion
Fever that does not resolve with over-the-counter medicine
Tips to reduce your ER bill
An ER visit can cost thousands of dollars, even if you have insurance. Here are some guidelines to ensure you are not overpaying:
Determine if you truly need an emergency room. If your health issue is not life threatening, consider going to an urgent care facility instead as the cost for the same care can be much less.
Go to a hospital-based ER. Freestanding ER centers typically cost much more than a hospital-based emergency room.
Call ahead to confirm payment options and the current wait time.
Ask about costs up front. If you are uninsured, consider asking the following questions to prevent you from surprises on your future bill:
Do you have discounted pricing for patients without insurance?
Will it cost less if I pay with cash?
What will the fee be for my specific issue?
Do you think I will need additional tests, and what will they cost?
How much do you charge for X-rays?
If I need medication, how much will it cost?
We use our proprietary database of project costs, personally contact industry experts to compile up-to-date pricing and insights, and conduct in-depth research to ensure accuracy in all our guides.

In this article
- Introduction
What is the average cost of an emergency room visit?
Will your health insurance cover the emergency room cost, when should you go to the emergency room, determining the average emergency room cost.

Emergency room (ER) visits are not something anyone plans for, but they are an inevitable fact of life. Whether you're suffering from a serious illness or have been in an accident, there are situations where you need emergency care. While these visits are vital for your health and well-being, they can also come with a hefty price tag if you're uninsured or the reason for your visit isn't covered. That's why it's essential to understand the average price of emergency room visits. You might be surprised how much they can vary depending on your insurance plan and what condition you're there to treat, but there are ways to protect yourself from high medical bills. Check out our guide below to learn what you can expect with regard to the emergency room cost when you are in a life-threatening situation.
According to most sources, the average cost of an emergency room visit in the United States is around $2,200, but this number can vary depending on a variety of factors, including the severity of the condition, where you live, and what type of insurance plan you have. For example, if you have health insurance through the Affordable Care Act (ACA), your out-of-pocket expenses will be capped. But, even with insurance, you may still end up paying several hundred dollars or more for an ER visit.
The ACA sets a number of limits on the out-of-pocket costs that individuals can be charged for healthcare services, including emergency room visits. However, this does not mean that you will have no cost for these services; it is likely that you may still need to pay copays, coinsurance, or deductibles in addition to what your insurance covers. Additionally, insurers are only required to provide coverage up until a patient's condition becomes stable—any other treatment costs could be on the consumer themselves if they choose an out-of-network provider or hospital.
To reduce the emergency room cost of a visit, you need to understand what kinds of conditions require this level of care. If you can avoid going to the ER for minor issues such as a cold or fever, you may be able to prevent a costly medical bill altogether. Furthermore, if you don’t have health insurance, many hospitals offer payment options like charity care and financial assistance programs to help people manage their medical bills.
It's a common worry for many people—what happens if you suddenly need to go to the emergency room? Will your health insurance cover the cost? Since 2010, the ACA requires insurance companies to cover the care you receive in the ER if you have an emergency medical condition. One of the key provisions of the ACA is that it requires insurance companies to cover emergency medical care for those that have an emergency medical condition regardless. This provision ensures individuals who experience sudden and unexpected medical emergencies will receive the care they need without worrying about the high cost of emergency room visits.
The ACA defines an emergency medical condition as a medical condition that manifests itself in such a way that a reasonable person would believe that the absence or the delay of emergency medical care could result in some type of serious harm or even death. It's crucial to note that the ACA does not require insurance companies to cover non-emergency care in the ER. If you go to the ER for a non-emergency condition such as a headache, flu, or minor injuries, your insurance company may not cover the cost of your visit. Take advantage of resources like our learning center at HealthInsurance.com to educate yourself on your plan.
Knowing when to go to the emergency room can be challenging for many individuals, particularly if your goal is to avoid paying a high emergency room cost for a visit that your insurance company deems unnecessary. While some medical emergencies are obvious, others may not be so clear-cut. In general, the emergency room is for medical emergencies that require immediate attention. Conditions that pose an imminent threat to the patient's life or health should be treated as emergencies. Some situations that warrant a visit to the nearest emergency room include:
- Difficulty Breathing
- Severe Abdominal Pain
- Head Injury
- Loss of Consciousness
- Allergic Reaction
- Heart Attack or Stroke Symptoms
Not all conditions require a trip to the ER and you do have some other options to consider when you're experiencing a medical issue. For non-life-threatening conditions, a visit to a primary care physician or urgent care center may be more appropriate. Patients with minor injuries, minor illnesses, or conditions that can wait until the next day or two should consider seeking non-emergency care. As a general rule, if you're in doubt or cannot handle the situation at home, seek emergency care or call 911. It is always better to be safe than sorry when it comes to your health.
The cost of an emergency room visit can vary greatly, depending on the hospital you go to, the level of treatment you require, and your insurance coverage. Knowledge of ER costs can help you make informed decisions when choosing an insurance plan . Some plans may have higher premiums but lower out-of-pocket expenses , while others may have lower premiums and higher costs when you need to use them. By researching the emergency room cost of visits, you'll be able to find a health insurance plan that fits your needs and budget. When you're ready to start learning about your options so you can get the insurance coverage you need, you can visit HealthInsurance.com to compare plans.
What to read next More on Short Term Medical →
Browse by category
Medicare Insurance
Information About Medicare By State
Browse Medicare Advantage Plans by State
Browse Medicare Drug Plans by State
Member Resources
Short Term Medical Insurance
Choice Advantage
Browse Short Term Medical Insurance Plans by State
ACA Insurance
Limited Fixed Indemnity Plans
Legion Limited Medical
Browse Limited Benefit Medical Insurance Plans by State
Accident Insurance
Browse Accident Insurance Plans by State
Dental Insurance
Delta Dental
United Concordia
Browse Dental Insurance Plans by State
Telemedicine Insurance
Florida Quotes
Georgia Quotes
North Carolina Quotes
Texas Quotes
Learning Center
Frequently Asked Questions
Prescription Drug Directory
Policy Holders Information
California Privacy Notice
Do Not Sell My Info
Interpreter Services
Notice of Nondiscrimination
Licensing for AgileCore
Licensing for Medicare
Quotes by State
© 2021-2024 HealthInsurance.com, LLC
Privacy Policy | Terms and Conditions
GENERAL DISCLAIMERS Healthinsurance.com is a commercial site designed for the solicitation of insurance from selected health insurance carriers and HealthInsurance.com , LLC is a licensed insurance agency. It is not a government agency. It is also not an insurer, or a medical provider. HealthInsurance.com , LLC is a licensed representative of Medicare Advantage (HMO, PPO, PFFS, and PDP) organizations that have a Medicare contract. Enrollment depends on the plan’s contract renewal. We do not offer every plan available in your area. Currently we represent nine carrier plan organizations nationally. Please contact Medicare.gov , 1-800-MEDICARE, or your local State Health Insurance Program (SHIP) to get information on all of your options. Alternatively, you may be referred, via a link, to a selected partner website, which is independently owned and operated and may have different privacy and terms of use policies from us. If you provide your contact information to us, an insurance agent/producer or insurance company may contact you. If you do not speak English, language assistance service, free of charge, is available to you; contact the toll-free number listed above. This site is not maintained by or affiliated with the federal government's Health Insurance Marketplace website or any state government health insurance marketplace. The plans we represent do not discriminate on the basis of race, color, national origin, age, disability, or sex. To learn more about a plan's nondiscrimination policy, please Learn more about a plan’s nondiscrimination policy here . Not all plans offer all of these benefits. Benefits may vary by carrier and location. Limitations and exclusions may apply. Multi-Plan_HIC_Web_M
We've detected unusual activity from your computer network
To continue, please click the box below to let us know you're not a robot.
Why did this happen?
Please make sure your browser supports JavaScript and cookies and that you are not blocking them from loading. For more information you can review our Terms of Service and Cookie Policy .
For inquiries related to this message please contact our support team and provide the reference ID below.
Thanks for visiting! GoodRx is not available outside of the United States. If you are trying to access this site from the United States and believe you have received this message in error, please reach out to [email protected] and let us know.
How Much Does an ER Visit Cost? Free Local Cost Calculator
It’s true that you can’t plan for a medical emergency, but that doesn’t mean you have to be surprised when it’s time to pay your hospital bill. In 2021, the U.S. government enacted price transparency rules for hospitals in order to demystify health care costs. That means it should be easier to get answers to questions like how much an ER visit costs.
While the question seems pretty straightforward, the answer is more complicated. Your cost will vary based on factors such as if you’re insured, whether you’ve met your deductible, the type of plan you have, and what your plan covers.
There is a lot to consider. This guide will take you through specific scenarios and answer questions about insurance plans, deductibles, co-payments, and discuss scenarios such as how much it costs if you go to the ER when it isn’t an emergency.
You’ll learn a few industry secrets too. Did you know that if you don’t have insurance you might see a higher bill? According to the Wall Street Journal , it’s common for hospitals to charge uninsured and self-pay patients higher rates than insured patients for the same services. So, where can you go if you can’t afford to go to the ER?
Keep reading for all this plus real-life examples and cost-saving tips.
How Much Does an ER Visit Cost Without Insurance?
Everything is more expensive in the ER. According to UnitedHealth, a trip to the emergency department can cost 12 times more than a typical doctor’s office visit. The average ER visit is $2,200, and doesn’t include procedures or medications.
If you want to get a better idea of what an ER visit will cost in your area, check out our medical price comparison tool that analyzes data from thousands of hospitals.
Compare Procedure Costs Near You
Other out-of-pocket expenses you may incur include bills from third parties. A growing number of emergency departments in the United States have become business entities separate from the hospital. So, third-party providers may bill you too, like:
- EMS services, like an ambulance or helicopter
- ER physicians
- Attending physician
- Consulting physicians
- Advanced practice nurses (CRNA, NP)
- Physician assistants (PA)
- Physical therapists (PT)
And if your insurance company fails to pay, you may have to pay these expenses out-of-pocket.
How Much Does an ER Visit Cost With Insurance?
The easiest way to estimate out-of-pocket expenses for an ER visit (or any other health care service) is to read your insurance policy. You’ll want to look for information around these terms:
- Deductible: The amount you have to pay out-of-pocket before your insurance kicks in .
- Copay: A set fee you pay upfront before a covered medical service or procedure.
- Coinsurance: The percentage you pay for a service or a procedure once you’ve met the deductible.
- Out-of-pocket maximum: The most you will pay for covered services in a rolling year. Once met, your insurance company will pay 100% of covered expenses for the rest of the year.
Closely related to out-of-pocket expenses like deductibles and co-insurance are premiums. A premium is the monthly fee you (or your sponsor) pay to the insurance company for coverage. If you pay a higher premium, you’ll have a lower deductible and fewer out-of-pocket costs whenever you use your insurance to pay for services such as a visit to the ER. The opposite is also true — high deductible health plans (HDHP) offer lower monthly payments but much higher deductibles.
Sample ER Visit Cost
Using a few examples from plans available on the Marketplace on Healthcare.gov (current as of November 2021), here’s how this might play out in real life:
Rob is a young, healthy, single guy. He knows he needs health insurance but he feels reasonably sure that the only time he’d ever use it is in case of an emergency. Here’s the plan he chooses:
Plan: Blue Cross/Blue Shield Bronze Monthly premium: $394 Deductible: $7,000 Out-of-pocket maximum: $7,000 ER coverage: 100% after meeting the deductible
Rob does the math and considers the worst case scenario. If he does go to the ER, he’ll pay full price if he hasn’t yet met his deductible. But since both his deductible and his maximum out-of-pocket are the same, $7,000 is the most he’ll have to pay before his insurance kicks in at 100%.
Now imagine that Rob gets married and is about to start a family. He might need a different insurance plan to account for more hospital bills, doctors appointments, and inevitable emergency room visits.
Since Rob knows he’ll be using his insurance more often, he picks a plan with a lower deductible that covers more things.
Plan: Bright HealthCare Gold Monthly premium: $643 Deductible: $0 Out-of-pocket maximum: $6,500 ER coverage: $500 Vision: $0 Generic prescription: $0 Primary care: $0 Specialist: $40
This time Rob goes with a zero deductible plan with a higher monthly premium. It’s more out-of-pocket each month, but since his plan covers doctor’s visits, prescription drugs, and vision, he feels more prepared as his lifestyle shifts into family mode.
If he has to go to the ER for any reason, all he’ll pay is $500 and his insurance pays the rest. And worse case scenario, the most he’ll pay out-of-pocket in a year is $6,500.
How Much Does an ER Visit Cost if You Have Medicare?
Medicare Part A only covers an emergency room visit if you’re admitted to the hospital. Medicare Part B covers 100% of most ER costs for most injuries, or if you become suddenly ill. Unlike private insurance and insurance purchased on the Affordable Care Act (ACA) Marketplace, Medicare rarely covers ER visits that happen while you’re outside of the United States.
To learn more, read: How to Use the Healthcare Marketplace to Buy Insurance
How Much Does an ER Visit Cost for Non-Emergencies?

When you have a sick child but lack insurance, haven’t met your deductible, or if you’re between paychecks, just knowing you can go to the ER without being hassled for money feels like such a relief. ER staff won’t demand payment upfront, and they usually don’t ask about insurance or assess your ability to pay until after discharge.
There are other reasons, too. You might be tempted to go to the ER for situations that are less than emergent because emergency departments provide easy access to health services 24/7, including holidays and the odd hours when your primary care physician isn’t available. If you’re one of the 61 million Americans who are uninsured or underinsured , you might go to the ER because you don’t know where else to go.
What you may not understand is the cost of an ER visit without insurance can total thousands of dollars. Consumers with ER bills that get sent to collections face some of the most aggressive debt collection practices of any industry. Collection accounts and charge-offs could affect your credit score for the better part of a decade.
Did you know that charges begin racking up as soon as you give the clerk your name and Social Security number? There are tons of horror stories out there about people receiving medical bills after waiting, some for many hours, and leaving without treatment.
4 ER Alternatives Ranked by Level of Care
First and foremost, if you’re experiencing a medical emergency, call 911 or go to the closest emergency room. Do not rely on this or any other website for advice or communication.
If you’re not sure whether your condition warrants immediate, high-level emergency care, you can always call your local ER and ask to speak to their triage nurse. They can quickly assess how urgent the situation is.
If you are looking for a lower-cost alternative to the ER, this list provides a few options. Each option is ranked by their ability to provide you with a certain level of care from emergent care to the lowest level, which is similar to the routine care you would receive at a doctor’s office.
1. Charitable Hospitals
There are around 1,400 charity hospitals , clinics, and pharmacies dedicated to serving low-income families, including the uninsured. Most charitable, not-for-profit medical centers provide emergency room services, making it a good option if you’re uninsured and worried about accruing substantial medical debt.
ERs at charitable hospitals provide the same type of medical care for conditions like trauma, broken bones, and life-threatening issues like chest pain and difficulty breathing. The major difference is the price tag. Emergency room fees at a charity hospital are usually flexible and almost always based on your income.
2. Urgent Care Centers
Urgent care centers are free-standing facilities designed to treat patients with serious but not life-threatening conditions. Also called “doc in a box,” these ambulatory care centers are a good choice for treating stable but chronic health issues, fever, urinary tract infections, back pain, abdominal pain, and moderately high blood pressure, to name a few.
Urgent care clinics usually have a medical doctor on-site. Some clinics offer point-of-care diagnostic tests like ultrasound and X-rays, as well as basic lab work. The average cost for an urgent care visit is around $180, according to UnitedHealth.
3. Retail Health Clinics
You may have noticed small retail health clinics (RHC) popping up in national drugstore chains like CVS, Walgreens, and in big-box stores like Target and Walmart. The Little Clinic is an example of an RHC that offers walk-in health care services at 190 supermarkets across the United States.
RHCs help low-acuity patients with minor medical problems like sore throat, cough, flu-like symptoms, and other conditions normally treated in a doctor’s office. If you think you’ll need lab tests or other procedures, an RHC may not be the best choice. Data from UnitedHealth puts the average cost for an RHC visit at $100.
4. Telehealth Visits
Telehealth, in some form, has been around for decades. Until recently, it was mostly used to provide access to care for patients living in the most remote or rural areas. Since 2020, telehealth visits over the phone, via chat, or through videoconferencing have become a legitimate and extremely cost-effective alternative to in-person office visits.
Telehealth is perfect for some types of mental health therapies, follow-up appointments, and triage. For self-pay, a telehealth visit only costs around $50, according to UnitedHealth.
Tips for Taking Control of Your Health Care

- Don’t procrastinate. Delaying the care you need for too long will end up costing you more in the end.
- Switch your focus from reactive care to proactive care. Figuring out how to pay for an ER visit is a lot harder (and costlier) than preventing an ER visit in the first place. Data show that preventive health care measures lead to fewer illnesses and better outcomes.
- Plan for the unknown. It’s inevitable that at some point in your life you’ll need health care. Start a savings account fund or better yet, enroll in a health savings account (HSA). If you’re employed (even part-time) you already qualify for an HSA. A contribution of just $9 a paycheck could add up to $468 tax-free dollars for you to spend on health care every year. Unlike the use-it-or-lose-it savings plans of the past, modern plans don’t expire. You can use HSA dollars to pay for out-of-pocket costs like copayments, deductibles, and for services that your health insurance may not cover, like dental and vision services.
- Advocate for yourself. There is nothing more empowering than taking charge of your health. Shop around for services and compare prices on procedures to make sure you’re getting the best prices possible.
- If you are uninsured or doing self-pay, negotiate your bill and ask for a cash discount.
Estimate the Cost of the ER Before You Need It
It’s stressful to think about money when you’re facing an emergency. Research the costs of your nearest ER before you actually need to go with Compare.com’s procedure cost comparison tool .
All you have to do is enter your ZIP code and you’ll immediately see out-of-pocket costs for ER visits at your local emergency rooms. It works for other medical services too, like MRIs, routine screenings, outpatient procedures, and more. Find the treatment you need at a price you can afford.
Disclaimer: Compare.com does not offer medical advice and is in no way a substitute for any medical advice received from health professionals. Compare.com is unable to offer any advice on any medical procedure you may need.

Nick Versaw leads Compare.com's editorial department, where he and his team specialize in crafting helpful, easy-to-understand content about car insurance and other related topics. With nearly a decade of experience writing and editing insurance and personal finance articles, his work has helped readers discover substantial savings on necessary expenses, including insurance, transportation, health care, and more.
As an award-winning writer, Nick has seen his work published in countless renowned publications, such as the Washington Post, Los Angeles Times, and U.S. News & World Report. He graduated with Latin honors from Virginia Commonwealth University, where he earned his Bachelor's Degree in Digital Journalism.
Compare Car Insurance Quotes
Get free car insurance quotes, recent articles.

Featured Clinical Reviews
- Screening for Atrial Fibrillation: US Preventive Services Task Force Recommendation Statement JAMA Recommendation Statement January 25, 2022
- Evaluating the Patient With a Pulmonary Nodule: A Review JAMA Review January 18, 2022
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
The Costs of US Emergency Department Visits
The US population made 144.8 million emergency department (ED) visits in 2017, costing a total of $76.3 billion, estimated a recent statistical brief from the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project (HCUP).
That year, 13.3% of the US population incurred an expense for an ED visit, and more than half of hospital inpatient stays originated with an ED visit. More than half of 2017 ED costs for the entire US, $39.5 billion, were incurred in large metropolitan areas. Aggregate ED visit costs and share of ED visit volume were highest for hospitals in the South. (ED charges were converted to costs using HCUP Cost-to-Charge Ratios based on Centers for Medicare & Medicaid Services hospital accounting reports.)
Read More About
Rubin R. The Costs of US Emergency Department Visits. JAMA. 2021;325(4):333. doi:10.1001/jama.2020.26936
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Watch CBS News
The most expensive states for ER visits, ranked
By Jessica Learish
December 4, 2020 / 3:56 PM EST / CBS News

Have you ever been in a hospital emergency room? Maybe you broke your leg or had a burst appendix. When medical emergencies strike, an ER visit could spell the difference between life and death.
But, like many things in the American health care system , the cost of this kind of life-saving hospital care varies widely based on where you live or which hospital you visit.
Hospital Pricing Specialists collected billing data from nearly 4,500 hospitals across the country to gauge the average price of a moderate-severity ER visit — the most common kind of visit — in each state. (Think acute pain of unknown origin, or a fever greater than 100.5 degrees Fahrenheit.)
The overall price tag is made up of emergency room charges, lab and radiology tests, pharmacy and supply costs, and other hospital fees. Each line item also includes charges that go toward paying the health care providers themselves.
In this gallery, the numbers are presented before any medical insurance is applied. Here are the 50 states (and Washington, D.C.) ranked by the pre-insurance cost of a moderate-severity ER visit.
51. Maryland

A moderate-severity ER visit in Maryland costs an average of $623 before insurance.

Maine hospitals charge an average of $952 for moderate-severity emergency room visits.
49. West Virginia

A visit to a West Virginia ER will run you $1,127 on average.
48. Montana

The average price of emergency hospital care in Montana is $1,138.
47. Louisiana

A visit to a Louisiana ER costs an average of $1,184 before insurance.
To alleviate overcrowding at local hospitals, this New Orleans field hospital was built in 2020 to accommodate up to 1,000 COVID-19 patients.
46. Massachusetts

Hospitals charge an average of $1,200 for moderate-severity ER visits in Massachusetts.
45. North Dakota

Have a medical emergency in North Dakota? The average price tag for a moderate-severity visit will be around $1,245.
44. Michican

Visits to emergency rooms in Michigan cost an average of $1,273.

Kansas hospitals charge around $1,294 per moderate-severity ER visit.
42. Arkansas

It will run you around $1,304 to receive care in an Arkansas ER.

Iowa hospitals charge an average of $1,377 per ER visit.
Here, volunteers on the Strawberry Point Ambulance Service pose during a Christmas snowstorm.
40. Vermont

It costs an average of $1,386 for an ER visit in Vermont.
39. Wyoming

Hospitals in Wyoming charge an average of $1,411 per moderate-severity ER visit.

Visits to the ER in Ohio cost an average of $1,435 before insurance.

On average, ER visits in Oregon cost $1,437 before insurance.
36. Minnesota

Minnesota hospitals charge an average of $1,462 per moderate-severity ER visit.

In Utah, the average ER visit costs around $1,464.
34. Oklahoma

Before insurance, an ER visit in Oklahoma costs around $1,466.
33. Connecticut

Connecticut emergency rooms charge an average of $1,493 before insurance.
31 (TIE). Wisconsin

A moderate-severity ER visit in Wisconsin will cost you around $1,496.
31 (TIE). Alabama

In Alabama, you'll pay an average of $1,496 for a moderate-severity ER visit.
30. New Mexico
It costs $1,574 for a moderate-severity ER visit in New Mexico.
29. Mississippi

Mississippi hospitals have an average sticker price of $1,583 per ER visit.
28. North Carolina

It costs an average of $1,589 for ER treatment in North Carolina.
26 (TIE). Georgia

Georgia emergency rooms charge an average of $1,596 before insurance.
26 (TIE). Delaware

Before insurance, an ER visit in Delaware costs around $1,596.
25. Indiana

Hospitals in Indiana charge an average of $1,618 per ER visit.
24. South Dakota
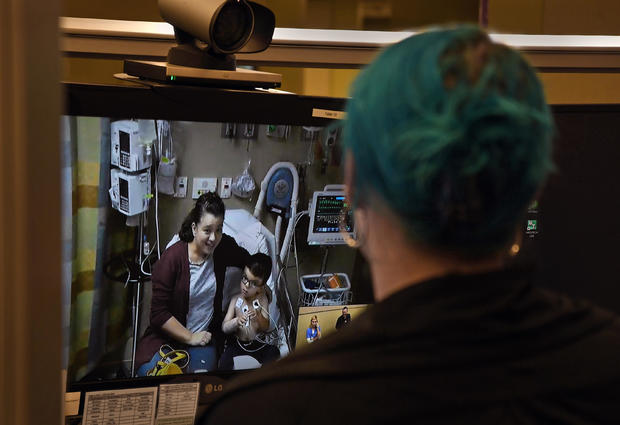
The average sticker price of a South Dakota ER visit is $1,641.
23. Pennsylvania

A moderate-severity ER visit in Pennsylvania costs $1,645 before insurance.
22. New York

The average visit to the ER in New York comes in at $1,668.
21. Missouri

Missouri hospitals charge $1,717 before insurance.
20. Kentucky

In Kentucky, hospitals bill an average of $1,740 per ER visit.
19. Rhode Island

Before insurance, the average Rhode Island ER visit costs $1,750.
18. South Carolina

It costs an average of $1,758 for an ER visit in South Carolina.
17. New Hampshire
In New Hampshire, a moderate-severity ER visit costs an average of $1,787.
16. Illinois

For an ER visit in Illinois, hospitals bill an average of $1,818 before insurance.
15. Washington

Washington hospitals charge $1,841, on average, for each ER visit.
Here, a COVID-19 survivor donates convalescent plasma in Seattle.
14. Nebraska

Nebraska emergency rooms charge an average of $1,844 before insurance.
13. Washington D.C.

In the nation's capital, hospitals charge $1,879 for the average moderate-severity ER visit.
12. Tennessee

In this Appalachian state, the average ER visit rings up at $1,883 before insurance.
11. Virginia

Hospitals in Virginia charge ER patients an average of $1,941 for moderate-severity cases.

On average, it costs $2,070 to receive ER treatment in Alaska.

An ER visit in Hawaii costs an average of $2,076 before insurance.

The average visit to the ER in Idaho comes in at $2,159.

It costs an average of $2,283 per visit to an Arizona emergency room.

Everything is bigger in Texas? The ER bills are certainly quite large. Hospitals charge an average of $2,318 per visit.

Before insurance, the average Nevada emergency room bill rings in at $2,583.
4. Colorado

Hospitals in Colorado charge an average of $2,886 per ER visit.
3. California

ER visits in the Golden State cost an average of $2,960 before insurance.

2. New Jersey
New Jersey hospitals bill a whopping $3,087 per ER visit before insurance.

Florida is the most expensive state for emergency room visits. Moderate-severity ER patients are billed an average of $3,102 before. insurance.

Here's Why Hospital Bills Are So High In The U.S. Health Care System

This is Part 4 of an 11-part series. Read the full series here .
Americans will spend over $4 trillion on health care this year, and the federal government projects that will rise to more than $6 trillion in the next seven years. Health care costs are growing faster than the economy, and a big portion of those bills is paid by employers and those with commercial insurance coverage.
High premiums also mean that employers like Tom Savidge have to keep worrying about how they’ll pay for their company plans.
Ever since Savidge opened his first mental health clinic in Greenville, North Carolina, 17 years ago, he’s struggled to keep up with the cost of his employees’ health care. And one major hospitalization can have a big impact on the bottom line.
“At one point in time, we had an employee who had a heart attack and ended up being in the hospital,” Savidge said. “That year alone resulted in about a 30% increase in just one year.”
Savidge has had to spend a lot more time worrying about health care costs than he first anticipated. He’s offered preventative health programs, and switched insurance providers more than once. He even opened up an on-site pharmacy with lower cost medicines. But he says the bill for employee care has almost tripled since he started out, so he’s had to cut back on other things.
“It definitely impacted raises and bonuses,” Savidge said. “Especially when you had markups of 10, 15, 20, 25% on an annual basis.”
Over the last three decades, the cost of American medical care has more than doubled even after accounting for inflation, according to the Kaiser Family Foundation . And a lot of the burden has fallen on private employers, like Savidge, and those with individual insurance policies, says Gerard Anderson, a health policy professor at Johns Hopkins University. “The private sector is paying four-and-a-half times what the rest of the industrialized countries are paying,” Anderson said, “whereas the Medicare program is paying about one-and-half times.”
The Medicare program sets the rates it will pay based on hospital costs. But private payers have to negotiate with every hospital and doctor. And Anderson says lack of competition is a big part of the problem. Much of the Charlotte region, for example, is dominated by three hospital systems: Atrium Health, Novant Health and the much smaller CaroMont Health. He says that mirrors metropolitan areas across the country.
“If you’re an insurer, you have to have that particular health care system in your network, and so they can charge whatever they want because you, as an insurer, can’t say no,” Anderson said.
Anderson says another problem is that insurance companies may not even be motivated to rein in costs for many large, self-insured company plans because they earn a percentage of the bill.
“They have no incentive — as long as they maintain the business — of getting the lowest price,” Anderson said.
Over the past three decades, hospital systems have been consolidating rapidly, merging with other hospitals and buying up physician practices.
And when hospitals consolidate, prices go up . On average, private insurance plans pay 247% of what Medicare pays, according to the RAND Corp. , a nonpartisan think tank.
And that’s just the national average. North Carolina hospitals charge private payers 273% of Medicare rates, says RAND analyst Christopher Whaley.

South Carolina, where health systems are more highly consolidated, ranks second highest in the country in terms of how much its hospitals charge people with private insurance. On average, hospitals there charge people with commercial insurance 344% of Medicare rates.
“That’s almost a hundred percentage points higher than the national average,” Whaley said.
Hospitals argue consolidation isn’t the problem. Cody Hand, a senior executive with the North Carolina Hospital Association, admits prices for private payers are high, but he said hospitals have to charge them more because Medicare pays too little.
“Medicare is a very low payer across the board,” Hand said. “(For most services) it’s less than 80% of the cost they reimburse. And so because of that, we have to figure out how to collect that difference somewhere else in order to stay open.”
But If that were true, Whaley said, then hospitals with more Medicare patients would have to charge their private patients more. But the data doesn’t show that.
“There’s actually no relationship between a hospital’s share of patients that are on Medicare and Medicaid and that hospital’s prices,” Whaley said.
Another reason prices are high, Hand said, is that hospitals have to spend a lot on salaries and equipment. American doctors and nurses earn more than their counterparts in other wealthy countries. Specialists here make an average of $316,000 a year — more than twice as much as the average compensation in nine comparable countries, according to one 2018 study. And, Hand said, hospitals are willing to pay more to get the top talent.
“The private sector is paying four-and-a-half times what the rest of the industrialized countries are paying, whereas the Medicare program is paying about one-and-half times.”
“ It just goes back to the competition argument,” Hand said. “You know, in order to attract the best you have to pay for the best.”
But studies show large hospital systems are also responsible for pushing up some physician charges. When they buy up doctor practices, hospitals often tack an additional fee onto the doctor’s bill. Hospitals say that additional fee helps cover the cost of operations, but consumer advocates say the charges can run into the hundreds of dollars .
Buying up doctors’ offices can also be very lucrative for large hospitals because those doctors then refer their patients back to the hospital for lab tests and procedures. And Whaley said reimbursement is greater for in-hospital tests.
“If you can move things like lab tests and MRIs from outside the hospital to inside the hospital then you can increase how much you get paid ,” he said.
Duke University law professor Barak Richman said large hospitals can use their market dominance to become even more dominant. As an example, he points to a contract the former Carolinas HealthCare System required insurers to sign. Carolinas HealthCare eventually grew into the 42-hospital system Atrium Health.
“Atrium said, ‘If you’re going to contract with us at all, you have to promise us that you will not steer your patients to lower-cost hospitals,’” Richman said. “So this basically is a contractual provision in which Atrium was exercising its market power. And the Department of Justice thought it was an abuse of its market power and it was anti-competitive.”
After the Department of Justice sued in 2016, Atrium agreed to eliminate the clause. It issued a news release at the time saying it hadn’t broken the law and that the contracts in question were created “as long ago as 2001.” But Richman said that by the time the clause was finally eliminated almost 20 years later, Atrium had become a big player.
Big players can push up costs. Even if they do good things with that income, like invest in medical research, Richman said that it amounts to a tax on everyone with private health insurance.
“It falls on every premium payer like a flat fee,” Richman said. “A family that is earning $40,000 is paying the same in premiums as a family that’s earning $ 4 million.”
Sign up for our daily headlines newsletter
- The Frequency - The latest WFAE stories each weekday morning.

An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006 Feb-.
Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet].
Statistical brief #268 costs of emergency department visits in the united states, 2017.
Brian J. Moore , Ph.D. and Lan Liang , Ph.D.
Published: December 8, 2020 .
- Introduction
Emergency department (ED) visits have grown in the United States, with the rate of increase from 1996 to 2013 exceeding that for hospital inpatient care. 1 In 2017, 13.3 percent of the U.S. population incurred at least one expense for an ED visit. 2 Furthermore, more than 50 percent of hospital inpatient stays in 2017 included evidence of ED services prior to admission. 3 Trends in ED volume vary significantly by patient and hospital characteristics, but an examination of nationwide costs by these characteristics has not yet been explored in the literature. 4
This Healthcare Cost and Utilization Project (HCUP) Statistical Brief presents statistics on the cost of ED visits in the United States using the 2017 Nationwide Emergency Department Sample (NEDS). Total ED charges were converted to costs using HCUP Cost-to-Charge Ratios based on hospital accounting reports from the Centers for Medicare & Medicaid Services (CMS). ED visits include patients treated and released from the ED, as well as those admitted to the same hospital through the ED. Aggregate costs, average costs, and number of ED visits are presented by patient and hospital characteristics. Because of the large sample size of the NEDS data, small differences can be statistically significant. Thus, only percentage differences greater than or equal to 10 percent are discussed in the text.
- There were 144.8 million total emergency department (ED) visits in 2017 with aggregate ED costs totaling $76.3 billion (B).
- Aggregate ED costs were higher for females ($42.6B, 56 percent) than males ($33.7B, 44 percent); 55 percent of total ED visits were for females.
- Average cost per ED visit increased with age, from $290 for patients aged 17 years and younger to $690 for patients aged 65 years and older.
- As community-level income increased, shares of aggregate ED costs decreased and average cost per visit increased.
- In rural areas, one half of ED visit costs were for patients from the lowest income communities.
- The expected payer with the largest share of aggregate costs was private insurance in large metropolitan areas (31.4 percent of $39.5B) and Medicare in micropolitan (34.0 percent of $7.6B) and rural (37.3 percent of $5.5B) areas.
- Patients aged 18–44 years represented the largest share of aggregate ED costs in large metropolitan, small metropolitan, and micropolitan areas (36.4, 34.2, 32.5 percent, respectively). Patients aged 65 years and older represented the largest share of aggregate ED costs in rural areas (32.5 percent).
Aggregate costs for emergency department (ED) visits by patient sex and age group, 2017
Figure 1 presents aggregate ED visit costs by patient sex and age group in 2017 as well as number of ED visits. Estimates of aggregate cost use the product of the number of cases and the average estimated cost per visit to account for records with missing ED charge information. Aggregate cost decompositions among different descriptive statistics or using multiple levels of aggregation in a single computation could lead to slightly different total cost estimates due to the use of slightly different and more specific estimates of the missing information.
Aggregate ED visit costs by patient sex and age, 2017. Abbreviation: ED, emergency department Notes: Statistics for ED visits with missing or invalid patient characteristics are not presented. Patient age and sex were each missing for <0.1% of (more...)
- Aggregate ED visit costs in 2017 were higher overall for females than for males. Of the $76.3 billion in aggregate ED visit costs in 2017, females accounted for $42.6 billion (55.9 percent) and males accounted for $33.7 billion (44.1 percent). This cost differential was largely driven by a difference in ED visit volume, with females having a larger number of ED visits than males (80.2 vs. 64.6 million visits, or 55.4 vs. 44.6 percent of visits). Females had higher aggregate ED visit costs and more ED visits for all age groups except children. The discrepancy was highest for patients aged 18–44 years, with aggregate ED visit costs for females approximately 50 percent higher than costs for males ($15.9 vs. $10.7 billion), followed by patients aged 65 years and older, for which aggregate ED visit costs were approximately one-third higher for females than for males ($11.5 vs. $8.6 billion).
Costs of ED visits by patient characteristics, 2017
Table 1 presents the aggregate and average costs for ED visits, the number of ED visits, and the distributions of costs and visits, by select patient characteristics in 2017.
Aggregate costs, average costs, and number of ED visits by patient characteristics, 2017.
- In 2017, aggregate ED visit costs totaled $76.3 billion across 144.8 million ED visits, with an average cost per visit of $530. Aggregate ED visit costs totaled $76.3 billion in the United States in 2017, encompassing 144.8 million ED visits with an average cost per visit of $530. Routine discharge was the most frequent disposition from the ED, representing 80.8 percent of aggregate ED costs and a similar share of ED visits. Transfers represented 6.2 percent of aggregate ED costs but just 3.0 percent of ED visit volume because they had the highest average cost of any discharge disposition at $1,100 per ED visit. In contrast, ED visits resulting in an inpatient admission to the same hospital had the lowest average cost of any discharge disposition at $360 per ED visit and represented 9.4 percent of aggregate ED costs and 14.0 percent of ED visits.
- The share of aggregate ED visit costs attributed to patients aged 65 years and older was higher than the share of ED visits for this group, and the average cost per visit was highest among patients aged 65 years and older. Aggregate ED visit costs among patients aged 65 years and older totaled $20.2 billion (26.4 percent of the $76.3 billion total for the entire United States in 2017) despite just 29.2 million ED visits from patients in this age group (20.2 percent of the 144.8 million total). Conversely, the share of aggregate ED costs attributed to patients aged 17 years and younger was substantially lower than this group’s corresponding share of ED visits (10.3 percent of ED costs vs.18.5 percent of ED visits). This differential is due in part to the difference in average cost per visit, which increased with age. The average cost per visit among patients aged 65 years and older was more than twice as high as average costs among patients aged 17 years and younger ($690 vs. $290 per visit).
- Medicaid as the primary expected payer had the lowest average cost per ED visit, more than 50 percent lower than average costs for Medicare and one-third lower than for private insurance. Medicaid as the primary expected payer had an average cost per ED visit that was more than 50 percent lower than average costs per visit for Medicare ($420 vs. $660 per visit) and one-third lower than average costs for private insurance ($420 vs. $560 per visit). Due in part to these differences in average costs by expected payer, Medicare represented 30.1 percent of aggregate ED visit costs but 24.1 percent of total ED visits. In contrast, Medicaid represented 25.0 percent of ED costs but 31.5 percent of ED visits.
- As community-level income increased, the share of aggregate ED visit costs decreased and average cost per ED visit increased. The share of ED visit costs and ED visits decreased as community-level income increased. Patients residing in communities with the lowest income (quartile 1) represented roughly one-third of aggregate ED visit costs and ED visits (31.4 and 34.3 percent, respectively). Patients residing in quartiles 2 and 3 represented approximately one-fourth and one-fifth of aggregate ED visit costs and ED visits, respectively. Patients residing in communities with the highest income (quartile 4) represented less than one-fifth of aggregate ED costs and ED visits (18.1 and 16.0 percent, respectively). In contrast, average cost per ED visit increased as community-level income increased, ranging from $480 in communities with the lowest income (quartile 1) to $600 in communities with the highest income (quartile 4).
- The share of aggregate ED visit costs was highest among patients residing in large metropolitan areas. Aggregate ED visit costs for large metropolitan areas totaled $39.5 billion in 2017, more than half of the $76.3 billion in ED costs for the entire United States. The share of aggregate ED costs in large metropolitan areas was analogous to the overall distribution of ED visits in these areas: 51.8 percent of aggregate ED costs and 50.4 percent of ED visits.
Distribution of aggregate ED visit costs for location of patient residence by patient characteristics, 2017
Figures 2 – 4 present the distribution of aggregate costs for ED visits based on the location of the patient’s residence by age ( Figure 2 ), community-level income ( Figure 3 ), and primary expected payer ( Figure 4 ).
Aggregate ED visit costs by age and patient location, 2017. Abbreviations: B, billion; ED, emergency department; M, million Notes: Statistics for ED visits with missing or invalid patient characteristics are not presented. Patient age and patient location (more...)
Aggregate ED visit costs by primary expected payer and patient location, 2017. Abbreviations: B, billion; ED, emergency department; M, million Notes: Statistics for ED visits with missing or invalid patient characteristics are not presented. Expected (more...)
Aggregate ED visit costs by community-level income and location of patient’s residence, 2017. Abbreviations: B, billion; ED, emergency department; M, million Notes: Statistics for ED visits with missing or invalid patient characteristics are not (more...)
Figure 2 presents the distribution of aggregate costs for ED visits by patient age based on the location of the patient’s residence in 2017.
- Patients aged 18–44 years represented the largest share of aggregate ED visit costs in all locations except rural areas where patients aged 65 years and older represented the largest share. Compared with other age groups, patients aged 18–44 years represented the largest share of aggregate ED visit costs in large metropolitan areas in 2017 (36.4 percent). The share of ED costs attributed to patients aged 18–44 years also was larger than for other age groups in small metropolitan and micropolitan areas (34.2 and 32.5 percent, respectively). Overall, the share of ED costs attributed to patients aged 18–44 years decreased as urbanization decreased, from 36.4 percent in large metropolitan areas to 29.8 percent in rural areas. In rural areas, patients aged 65 years and older accounted for the largest share of aggregate ED visit costs (32.5 percent) compared with other age groups. The share of ED costs attributed to patients aged 65 years and older increased as urbanization decreased, from 24.7 percent in large metropolitan areas to 32.5 percent in rural areas. The share of aggregate ED visit costs attributed to patients aged 45–64 years and those aged 17 years and younger were similar across all patient locations (approximately 28 and 10 percent, respectively).
Figure 3 presents the distribution of aggregate costs for ED visits by quartile of community-level household income in the patient’s ZIP Code based on the location of the patient’s residence in 2017.
- In large metropolitan areas, patients residing in communities with the highest and lowest incomes represented the largest shares of aggregate ED visit costs. For other locations, patients in communities with lower incomes represented the largest share of ED costs. Patients residing in communities with the highest and lowest incomes (quartiles 4 and 1) accounted for 28.1 and 26.6 percent, respectively, of the $39.5 billion in aggregate ED visit costs in large metropolitan areas in 2017. In contrast, patients residing in communities with the two lowest income quartiles represented the largest share of ED costs for other patient locations (small metropolitan, micropolitan, and rural).
- As urbanization decreased, the share of aggregate ED visit costs for patients in the lowest income quartile increased and the share for those in the highest income quartile decreased. The share of aggregate ED visit costs attributed to patients residing in communities in the lowest income quartile (quartile 1) increased as urbanization decreased, from 26.6 percent in large metropolitan areas to 48.8 percent in rural areas. In contrast, the share of ED visit costs attributed to patients residing in communities in the highest income quartile (quartile 4) decreased as urbanization decreased, from 28.1 percent in large metropolitan areas to 1.2 percent in rural areas.
Figure 4 presents the distribution of aggregate costs for ED visits by primary expected payer based on the location of the patient’s residence in 2017.
- Private insurance as the primary expected payer accounted for the largest share of aggregate ED visit costs among patients living in large metropolitan areas. Medicare represented the largest share of ED costs in micropolitan and rural areas. Compared with other primary expected payers, private insurance represented the largest share of aggregate ED visit costs among those living in large metropolitan areas in 2017 (31.4 percent). The share of ED costs attributed to private insurance decreased as urbanization decreased, from 31.4 percent in large metropolitan areas to 27.9 percent in rural areas. More than one-third of ED visit costs were attributed to Medicare as the primary expected payer in micropolitan and rural areas. The share of ED costs attributed to Medicare increased as urbanization decreased, from 28.0 percent in large metropolitan areas to 37.3 percent in rural areas.
Costs of ED visits by hospital characteristics, 2017
Table 2 presents the aggregate and average costs for ED visits, the number of ED visits, and the distributions of costs and visits, by select hospital characteristics in 2017.
Aggregate costs, average costs, and number of ED visits by hospital characteristics, 2017.
- Aggregate ED visit costs were highest for hospitals located in the South in 2017. Aggregate ED visit costs in the South were $27.5 billion in 2017 (36.1 percent of the total $76.3 billion for the United States). The share of ED visit volume for the South was even larger (40.0 percent of the 144.8 million total visits). The distribution of aggregate ED visit costs across other hospital characteristics largely followed the pattern of the number of ED visits. Aggregate ED costs were highest in private, nonprofit hospitals; teaching hospitals; and hospitals not designated as a trauma center (72.0, 64.1, and 52.5 percent of ED costs, respectively). ED visits at private, for-profit hospitals had lower average costs per visit than did visits at either private, nonprofit or public hospitals ($420 vs. $540 and $550 per visit).
- About Statistical Briefs
Healthcare Cost and Utilization Project (HCUP) Statistical Briefs provide basic descriptive statistics on a variety of topics using HCUP administrative healthcare data. Topics include hospital inpatient, ambulatory surgery, and emergency department use and costs, quality of care, access to care, medical conditions, procedures, and patient populations, among other topics. The reports are intended to generate hypotheses that can be further explored in other research; the reports are not designed to answer in-depth research questions using multivariate methods.
- Data Source
The estimates in this Statistical Brief are based upon data from the HCUP 2017 Nationwide Emergency Department Sample (NEDS).
- Definitions
Types of hospitals included in the HCUP Nationwide Emergency Department Sample
The Nationwide Emergency Department Sample (NEDS) is based on emergency department (ED) data from community acute care hospitals, which are defined as short-term, non-Federal, general, and other specialty hospitals available to the public. Included among community hospitals are pediatric institutions and hospitals that are part of academic medical centers. Excluded are long-term care facilities such as rehabilitation, psychiatric, and alcoholism and chemical dependency hospitals. Hospitals included in the NEDS have EDs, and no more than 90 percent of their ED visits result in admission.
Unit of analysis
The unit of analysis is the ED visit, not a person or patient. This means that a person who is seen in the ED multiple times in 1 year will be counted each time as a separate visit in the ED.
Costs and charges
Total ED charges were converted to costs using HCUP Cost-to-Charge Ratios based on hospital accounting reports from the Centers for Medicare & Medicaid Services (CMS). a Costs reflect the actual expenses incurred in the production of hospital services, such as wages, supplies, and utility costs; charges represent the amount a hospital billed for the case. For each hospital, a cost-to-charge ratio constructed specifically for the hospital ED is used. Hospital charges reflect the amount the hospital billed for the entire ED visit and do not include professional (physician) fees.
Total charges were not available on all NEDS records. About 13 percent of all ED visits (weighted) in the 2017 NEDS were missing information about ED charges, and therefore, ED cost could not be estimated. For ED visits that resulted in admission, 24 percent of records were missing ED charges. For ED visits that did not result in admission, 11 percent of records were missing ED charges. The missing information was concentrated in the West (59 percent of records missing ED charges). For this Statistical Brief, the methodology used for aggregate cost estimation was analogous to what is recommended for the estimation of aggregate charges in the Introduction to the HCUP NEDS documentation. b Aggregate costs were estimated as the product of number of visits and average cost per visit in each reporting category. If a stay was missing total charges, average cost was imputed using the average cost for other stays with the same combination of payer characteristics. Therefore, a comparison of aggregate cost estimates across different tables, figures, or characteristics may result in slight discrepancies.
How HCUP estimates of costs differ from National Health Expenditure Accounts
There are a number of differences between the costs cited in this Statistical Brief and spending as measured in the National Health Expenditure Accounts (NHEA), which are produced annually by CMS. c The largest source of difference comes from the HCUP coverage of ED treatment only in contrast to the NHEA inclusion of inpatient and other outpatient costs associated with other hospital-based outpatient clinics and departments as well. The outpatient portion of hospitals’ activities has been growing steadily and may exceed half of all hospital revenue in recent years. On the basis of the American Hospital Association Annual Survey, 2017 outpatient gross revenues (or charges) were about 49 percent of total hospital gross revenues. d
Smaller sources of differences come from the inclusion in the NHEA of hospitals that are excluded from HCUP. These include Federal hospitals (Department of Defense, Veterans Administration, Indian Health Services, and Department of Justice [prison] hospitals) as well as psychiatric, substance abuse, and long-term care hospitals. A third source of difference lies in the HCUP reliance on billed charges from hospitals to payers, adjusted to provide estimates of costs using hospital-wide cost-to-charge ratios, in contrast to the NHEA measurement of spending or revenue. HCUP costs estimate the amount of money required to produce hospital services, including expenses for wages, salaries, and benefits paid to staff as well as utilities, maintenance, and other similar expenses required to run a hospital. NHEA spending or revenue measures the amount of income received by the hospital for treatment and other services provided, including payments by insurers, patients, or government programs. The difference between revenues and costs includes profit for for-profit hospitals or surpluses for nonprofit hospitals.
Location of patients’ residence
Place of residence is based on the urban-rural classification scheme for U.S. counties developed by the National Center for Health Statistics (NCHS) and based on the Office of Management and Budget (OMB) definition of a metropolitan service area as including a city and a population of at least 50,000 residents. For this Statistical Brief, we collapsed the NCHS categories into four groups according to the following:
Large Metropolitan
- Large Central Metropolitan: Counties in a metropolitan area with 1 million or more residents that satisfy at least one of the following criteria: (1) containing the entire population of the largest principal city of the metropolitan statistical area (MSA), (2) having their entire population contained within the largest principal city of the MSA, or (3) containing at least 250,000 residents of any principal city in the MSA
- Large Fringe Metropolitan: Counties in a metropolitan area with 1 million or more residents that do not qualify as large central metropolitan counties
Small Metropolitan
- Medium Metropolitan: Counties in a metropolitan area of 250,000–999,999 residents
- Small Metropolitan: Counties in a metropolitan area of 50,000–249,999 residents
Micropolitan:
- Micropolitan: Counties in a nonmetropolitan area of 10,000–49,999 residents
- Noncore: Counties in a nonmetropolitan and nonmicropolitan area
Community-level income
Community-level income is based on the median household income of the patient’s ZIP Code of residence. Quartiles are defined so that the total U.S. population is evenly distributed. Cut-offs for the quartiles are determined annually using ZIP Code demographic data obtained from Claritas, a vendor that produces population estimates and projections based on data from the U.S. Census Bureau. e The value ranges for the income quartiles vary by year. The income quartile is missing for patients who are homeless or foreign.
Expected payer
- Medicare: includes fee-for-service and managed care Medicare
- Medicaid: includes fee-for-service and managed care Medicaid
- Private insurance: includes commercial nongovernmental payers, regardless of the type of plan (e.g., private health maintenance organizations [HMOs], preferred provider organizations [PPOs])
- Self-pay/No charge: includes self-pay, no charge, charity, and no expected payment
- Other payers: includes other Federal and local government programs (e.g., TRICARE, CHAMPVA, Indian Health Service, Black Lung, Title V) and Workers’ Compensation
ED visits that were expected to be billed to the State Children’s Health Insurance Program (SCHIP) are included under Medicaid.
- Northeast: Maine, New Hampshire, Vermont, Massachusetts, Rhode Island, Connecticut, New York, New Jersey, and Pennsylvania
- Midwest: Ohio, Indiana, Illinois, Michigan, Wisconsin, Minnesota, Iowa, Missouri, North Dakota, South Dakota, Nebraska, and Kansas
- South: Delaware, Maryland, District of Columbia, Virginia, West Virginia, North Carolina, South Carolina, Georgia, Florida, Kentucky, Tennessee, Alabama, Mississippi, Arkansas, Louisiana, Oklahoma, and Texas
- West: Montana, Idaho, Wyoming, Colorado, New Mexico, Arizona, Utah, Nevada, Washington, Oregon, California, Alaska, and Hawaii
Discharge status
Discharge status reflects the disposition of the patient at discharge from the ED and includes the following categories reported in this Statistical Brief: routine (to home); admitted as an inpatient to the same hospital; transfers (transfer to another short-term hospital; other transfers including skilled nursing facility, intermediate care, and another type of facility such as a nursing home); and all other dispositions (home healthcare; against medical advice [AMA]; died in the ED; or destination unknown).
Hospital characteristics
Data on hospital ownership and status as a teaching hospital was obtained from the American Hospital Association (AHA) Annual Survey of Hospitals. Hospital ownership/control includes categories for government nonfederal (public), private not-for-profit (voluntary), and private investor-owned (proprietary). Teaching hospital is defined as having a residency program approved by the American Medical Association, being a member of the Council of Teaching Hospitals, or having a ratio of full-time equivalent interns and residents to beds of 0.25 or higher.
Hospital trauma level
- Level I centers have comprehensive resources, are able to care for the most severely injured, and provide leadership in education and research.
- Level II centers have comprehensive resources and are able to care for the most severely injured, but do not provide leadership in education and research.
- Level III centers provide prompt assessment and resuscitation, emergency surgery, and, if needed, transfer to a level I or II center.
- Level IV/V centers provide trauma support in remote areas in which no higher level of care is available. These centers resuscitate and stabilize patients and arrange transfer to an appropriate trauma facility.
For this Statistical Brief, trauma hospitals were defined as those classified by the ASC/COT as a level I, II, or III trauma center. This is consistent with the classification of trauma centers used in the NEDS. The ACS/COT has a program that verifies hospitals as trauma level I, II, or III. h It is important to note that although all level I, II, and III trauma centers offer a high level of trauma care, there may be differences in the specific services and resources offered by hospitals of different levels. Trauma levels IV and V are designated at the State level (and not by ACS/COT) with varying criteria applied across States.
The Healthcare Cost and Utilization Project (HCUP, pronounced "H-Cup") is a family of healthcare databases and related software tools and products developed through a Federal-State-Industry partnership and sponsored by the Agency for Healthcare Research and Quality (AHRQ). HCUP databases bring together the data collection efforts of State data organizations, hospital associations, and private data organizations (HCUP Partners) and the Federal government to create a national information resource of encounter-level healthcare data. HCUP includes the largest collection of longitudinal hospital care data in the United States, with all-payer, encounter-level information beginning in 1988. These databases enable research on a broad range of health policy issues, including cost and quality of health services, medical practice patterns, access to healthcare programs, and outcomes of treatments at the national, State, and local market levels.
- Alaska Department of Health and Social Services
- Alaska State Hospital and Nursing Home Services Association
- Arizona Department of Health Services
- Arkansas Department of Health
- California Office of Statewide Health Planning and Development
- Colorado Hospital Association
- Connecticut Hospital Association
- Delaware Division of Public Health
- District of Columbia Hospital Association
- Florida Agency for Health Care Administration
- Georgia Hospital Association
- Hawaii Laulima Data Alliance
- Hawaii University of Hawai’i at Hilo
- Illinois Department of Public Health
- Indiana Hospital Association
- Iowa Hospital Association
- Kansas Hospital Association
- Kentucky Cabinet for Health and Family Services
- Louisiana Department of Health
- Maine Health Data Organization
- Maryland Health Services Cost Review Commission
- Massachusetts Center for Health Information and Analysis
- Michigan Health & Hospital Association
- Minnesota Hospital Association
- Mississippi State Department of Health
- Missouri Hospital Industry Data Institute
- Montana Hospital Association
- Nebraska Hospital Association Services
- Nevada Department of Health and Human
- New Hampshire Department of Health & Human
- New Jersey Department of Health
- New Mexico Department of Health
- New York State Department of Health
- North Carolina Department of Health and Human Services
- North Dakota (data provided by the Minnesota Hospital Association)
- Ohio Hospital Association
- Oklahoma State Department of Health
- Oregon Association of Hospitals and Health Systems
- Oregon Office of Health Analytics
- Pennsylvania Health Care Cost Containment Council
- Rhode Island Department of Health
- South Carolina Revenue and Fiscal Affairs Office
- South Dakota Association of Healthcare Organizations
- Tennessee Hospital Association
- Texas Department of State Health Services
- Utah Department of Health
- Vermont Association of Hospitals and Health Systems
- Virginia Health Information
- Washington State Department of Health
- West Virginia Department of Health and Human Resources, West Virginia Health Care Authority
- Wisconsin Department of Health Services
- Wyoming Hospital Association
- About the NEDS
The HCUP Nationwide Emergency Department Sample (NEDS) is a unique and powerful database that yields national estimates of emergency department (ED) visits. The NEDS was constructed using records from both the HCUP State Emergency Department Databases (SEDD) and the State Inpatient Databases (SID). The SEDD capture information on ED visits that do not result in an admission (i.e., patients who were treated in the ED and then released from the ED, or patients who were transferred to another hospital); the SID contain information on patients initially seen in the ED and then admitted to the same hospital. The NEDS was created to enable analyses of ED utilization patterns and support public health professionals, administrators, policymakers, and clinicians in their decision making regarding this critical source of care. The NEDS is produced annually beginning in 2006. Over time, the sampling frame for the NEDS has changed; thus, the number of States contributing to the NEDS varies from year to year. The NEDS is intended for national estimates only; no State-level estimates can be produced. The unweighted sample size for the 2017 NEDS is 33,506,645 (weighted, this represents 144,814,803 ED visits).
- For More Information
For other information on emergency department visits, refer to the HCUP Statistical Briefs located at www.hcup-us.ahrq.gov/reports/statbriefs/sb_ed.jsp .
- HCUP Fast Stats at www.hcup-us.ahrq.gov/faststats/landing.jsp for easy access to the latest HCUP-based statistics for healthcare information topics
- HCUPnet, HCUP’s interactive query system, at www.hcupnet.ahrq.gov/
For more information about HCUP, visit www.hcup-us.ahrq.gov/ .
For a detailed description of HCUP and more information on the design of the Nationwide Emergency Department Sample (NEDS), please refer to the following database documentation:
Agency for Healthcare Research and Quality. Overview of the Nationwide Emergency Department Sample (NEDS). Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality. Updated December 2019. www.hcup-us.ahrq.gov/nedsoverview.jsp . Accessed February 3, 2020.
- Acknowledgments
The authors would like to acknowledge the contributions of Nils Nordstrand of IBM Watson Health.
The HCUP Cost-to-Charge Ratios (CCRs) for NEDS Files were not publicly available at the time of publication, so an internal version was used in this Statistical Brief.
Agency for Healthcare Research and Quality. HCUP Nationwide Emergency Department Sample (NEDS) Database Documentation. Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality. Updated April 27, 2020. www .hcup-us.ahrq.gov /db/nation/neds/nedsdbdocumentation.jsp . Accessed October 27, 2020.
For additional information about the NHEA, see Centers for Medicare & Medicaid Services (CMS). National Health Expenditure Data. CMS website. Updated December 17, 2019. www .cms.gov/Research-Statistics-Data-and-Systems /Statistics-Trends-and-Reports /NationalHealthExpendData/index .html?redirect= /NationalHealthExpendData/ . Accessed February 3, 2020.
American Hospital Association. TrendWatch Chartbook, 2019. Table 4.2. Distribution of Inpatient vs. Outpatient Revenues, 1995–2017. www .aha.org/system/files /media/file/2019 /11/TrendwatchChartbook-2019-Appendices .pdf . Accessed March 19, 2020.
Claritas. Claritas Demographic Profile by ZIP Code. https://claritas360.claritas.com/mybestsegments/. Accessed February 3, 2020.
American Trauma Society. Trauma Information Exchange Program (TIEP). www .amtrauma.org/page/TIEP . Accessed June 11, 2020.
MacKenzie EJ, Hoyt DB, Sacra JC, Jurkovich GJ, Carlini AR, Teitelbaum SD, et al. National inventory of hospital trauma centers. JAMA. 2003;289(12):1515–22. [ PubMed : 12672768 ]
American College of Surgeons Committee on Trauma, Verification, Review, and Consultation Program for Hospitals. Additional details are available at www .facs.org/quality-programs/trauma/vrc . Accessed July 17, 2020.
Moore BJ (IBM Watson Health), Liang L (AHRQ). Costs of Emergency Department Visits in the United States, 2017. HCUP Statistical Brief #268. December 2020. Agency for Healthcare Research and Quality, Rockville, MD. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb268-ED-Costs-2017.pdf .
- Cite this Page Moore BJ, Liang L. Costs of Emergency Department Visits in the United States, 2017. 2020 Dec 8. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006 Feb-. Statistical Brief #268.
- PDF version of this page (326K)
In this Page
- Healthcare Cost and Utilization Project (HCUP)
- Nationwide Inpatient Sample (NIS)
- Kids' Inpatient Database (KID)
- Nationwide Emergency Department Sample (NEDS)
- State Inpatient Databases (SID)
- State Ambulatory Surgery Databases (SASD)
- State Emergency Department Databases (SEDD)
- HCUP Overview
- HCUP Fact Sheet
- HCUP Partners
- HCUP User Support
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Costs of Emergency Department Visits for Mental and Substance Use Disorders in the United States, 2017. [Healthcare Cost and Utilizatio...] Review Costs of Emergency Department Visits for Mental and Substance Use Disorders in the United States, 2017. Karaca Z, Moore BJ. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. 2006 Feb
- Review Expected Payers and Patient Characteristics of Maternal Emergency Department Care, 2019. [Healthcare Cost and Utilizatio...] Review Expected Payers and Patient Characteristics of Maternal Emergency Department Care, 2019. McDermott KW, Reid LD, Owens PL. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. 2006 Feb
- Review Emergency Department Visits Involving Dental Conditions, 2018. [Healthcare Cost and Utilizatio...] Review Emergency Department Visits Involving Dental Conditions, 2018. Owens PL, Manski RJ, Weiss AJ. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. 2006 Feb
- Review Overview of Emergency Department Visits Related to Injuries, by Cause of Injury, 2017. [Healthcare Cost and Utilizatio...] Review Overview of Emergency Department Visits Related to Injuries, by Cause of Injury, 2017. Weiss AJ, Reid LD, Barrett ML. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. 2006 Feb
- Review Racial and Ethnic Differences in Emergency Department Visits Related to Substance Use Disorders, 2019. [Healthcare Cost and Utilizatio...] Review Racial and Ethnic Differences in Emergency Department Visits Related to Substance Use Disorders, 2019. Owens PL, Moore BJ. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. 2006 Feb
Recent Activity
- Costs of Emergency Department Visits in the United States, 2017 - Healthcare Cos... Costs of Emergency Department Visits in the United States, 2017 - Healthcare Cost and Utilization Project (HCUP) Statistical Briefs
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Health Spending
- Quality of Care
Access & Affordability
Health & Wellbeing
- Price Transparency
- Affordability
- Prescription Drugs
Outpatient visits billed at increasingly higher levels: implications for health costs
By Hope Schwartz Twitter , Gary Claxton , Matthew Rae Twitter , and Cynthia Cox Twitter
February 27, 2023
Stay Connected
Get the best of the Health System Tracker delivered to your inbox.
The cost of an outpatient visit to a physician’s office, urgent care center, or emergency department depends in part on the level of service provided. Providers and facilities generally charge higher prices for more complex visits, and insurers pay larger reimbursements. Patients with deductibles or co-insurance may have higher out-of-pocket costs for more complex visits, too. Although there are standardized guidelines for how to determine the complexity of a visit, there is a trend towards visits being billed at higher levels over time. This could reflect increases in actual acuity and the intensity of services required, or changes in billing practices, or both. There is concern that providers may be inappropriately billing for more complex—and thus more expensive—services, a practice known as “ upcoding .”
In this analysis, we review the literature on coding practices, and using claims data we examine trends in complexity coding across outpatient practice settings from 2004 to 2021. We look at private, large employer-based insurance claims from the Merative MarketScan Commercial Claims and Encounters database for non-elderly people. We examine the distribution of code levels in physician offices, urgent care centers, and emergency departments over time, for all evaluation and management claims and for specific diagnoses. This analysis only includes evaluation and management claims and does not include additional visit-associated bills such as laboratory tests or other services.
Over the 18-year period of our analysis, we find that claims across all three sites of care trended towards higher level codes, even among specific, common diagnoses like urinary tract infections and headaches. The average age of this population stayed consistent over time. However, we do not assess whether health status worsened with time, so we are not able to assess whether increases in billed complexity represent actual changes in clinical characteristics. These trends could therefore be explained by multiple factors beyond upcoding, such as increasing clinical acuity, changes in services provided, or care for some diseases shifting from the inpatient to the outpatient setting.
These changes are contributing to higher outpatient health spending. We find that in 2021, outpatient evaluation and management spending was 4% higher in both physician offices and emergency departments than it would have been if visits were coded at the same levels as in 2011.
How is visit complexity determined, and how might it affect costs?
Visit complexity is determined by the level of evaluation and management services billed by the provider or hospital. Evaluation and management services are billed using American Medical Association Current Procedural Terminology ( CPT ) codes, and AMA guidelines for assigning these codes are approved by the Center for Medicare and Medicaid Services . Level 1 visits are the lowest complexity cases, with less time required or straightforward medical decision making, while level 5 visits are the highest complexity cases, with more time required or very complex medical decision making. Payers generally reimburse a higher rate for more complex cases to reflect the increased resources and time required to treat these cases.
Related Content:
How does U.S. life expectancy compare to other countries?
How does health spending in the U.S. compare to other countries?
Several prior studies have shown that outpatient costs are increasing and that providers are billing for more complex services. A KFF analysis of U.S. healthcare price growth found that the average price of an outpatient office visit grew faster than inflation from 2003-2019, and that the share of level 4 visits increased from less than 1-in-5 (19%) to more than 1-in-3 (36%) during the same period. Similar trends have been documented in the emergency department and inpatient hospital setting. While the reasons behind increasing visit complexity are likely multifactorial, these trends have raised concerns whether some providers might be “ upcoding ,” or inflating medical complexity to receive higher payments.
Some of this trend toward more complex coding may be explained by an aging and more medically complex population requiring more outpatient services. In the emergency department, there is some correlation between number of services provided and complexity billed, but this relationship does not completely explain the increases in complexity levels billed. One study found that of all physicians who provided outpatient, inpatient, or other evaluation and management services for Medicare beneficiaries in 2010, physicians who consistently bill at the highest complexity levels treat patients who are similar in age and diagnoses to their counterparts.
Regardless of the reason behind it, the trend toward billing for higher complexity services appears to have led to increased spending on outpatient services. The Center for Public Integrity found that higher codes for routine office visits led to a $6.6 billion increase in Medicare payments from 2001-2010, and that higher codes in the emergency department increased costs by $1 billion from 2001-2008.
Outpatient claims are billed at higher levels over time
In this analysis, we find a trend toward higher level claims in physician offices, urgent care centers and emergency departments, though this trend is most pronounced in emergency departments. Taking claims from all three settings, we find that the share of moderate intensity (level 3) claims decreased from the majority (60%) of claims in 2004 to less than half (45%) in 2021. Meanwhile, higher intensity level 4 claims almost doubled in frequency, from 19% in 2004 to 37% in 2021. The shares of claims at each level remained relatively stable during the COVID-19 pandemic in 2020 and 2021. Levels 3 and 4 claims continued to be the most common during this time; however level 5 claims continued to increase in frequency to 6% in 2021. During the pandemic, level 1 and 2 claims also increased to 4% and 7% respectively by 2021.
In emergency departments, level 4 and 5 codes now make up the majority of claims
In the emergency department, the most common claim in 2004 was level 3. However, by 2021, level 4 was the most common and accounted for over one third (35%) of claims. Level 5 claims increased in frequency from 8% of emergency department claims in 2004 to a quarter of claims by 2021. The growing number of urgent care centers in the past two decades may contribute to increased acuity in emergency departments by siphoning less sick patients away from emergency departments. However, we also find that visit complexity is rising outside of the emergency department.
In outpatient physician offices, the share of level 4 claims has grown
In outpatient physician offices, the share of higher level claims also grew over time. Level 3 claims remained the most common from 2004 to 2021, but the share of level 3 claims reduced from 61% in 2004 to 48% in 2021. In 2004, level 4 claims accounted for 1-in-5 outpatient office claims, which increased to over one third of claims in 2021 (38%). Across the period of our study, outpatient physician offices had a relatively low proportion of the lowest level (level 1) and the highest level (level 5) claims.
In urgent care centers, higher level claims are also becoming more common
In urgent care centers, level 3 and 4 claims accounted for 76% of claims in 2004 and reached 93% of claims by 2019, before down trending during the pandemic years. Level 4 claims grew from less than a quarter (21%) of all urgent care claims in 2004 to almost half (49%) before the pandemic. The share of lower complexity claims decreased during this time. In 2004, almost a quarter of claims (23%) were level 1 or level 2. By 2019, level 2 claims made up 5% and level 1 claims made up 0% of all claims in urgent care centers. During 2020 and 2021, we observed a growth in level 1-3 claims at urgent care centers, and a decrease in level 4 claims. These changes may represent shifting health care utilization during the pandemic, changes in billing practices, or a combination of multiple factors.
Even for specific diagnoses, trends in claim levels are consistent over time
Over time more people in the U.S. have been diagnosed with comorbid conditions , which may make patients more complex or resource intensive to treat and may contribute to the increasing complexity of outpatient claims. However, we find that trends in coding levels are reflected even in diseases that are less likely to be worsening over time or in which comorbidities have a smaller impact. We restrict our analysis to younger people (<65), who are less likely to have chronic conditions , and we also find that the average age of our population remained consistent during our analysis, suggesting that the aging population is not a contributor to the increases in billing complexity we find.
For urinary tract infections visits are increasingly coded at higher levels
For urinary tract infections, moderate complexity (level 3) claims were over half (54%) of emergency department claims and two-thirds (67%) of all outpatient office claims in 2004. By 2021, level 3 claims accounted for only 31% of emergency department claims and 57% of outpatient office claims. In the emergency department, 1-in-5 claims for urinary tract infections was level 5 in 2021.
The majority of headache claims are now level 4 or 5
For headache, level 3 claims were the most common in 2004 in both physician offices (58%) and emergency departments (41%). By 2021, level 4 claims were the majority in both settings. In the emergency department, the share of level 5 claims more than tripled from 2004 to 2021.
Emergency evaluation and management claims are 4.5 times as expensive as office claims, on average
In 2021, the average cost of evaluation and management services was almost 5 times as expensive in the emergency department ($556) compared to outpatient physician offices ($125). Emergency department claims also have the most variation in cost by level. The average level 5 claim is over $400 more expensive than the average level 1 claim. Urgent care evaluation and management claims cost $147, on average.
The cost of higher level claims are growing faster than the cost of lower level claims
For each practice setting, costs of claims are growing at different rates. The emergency department saw the largest relative increase in evaluation and management costs at all levels. Level 1 claims increased in cost by 138%, and level 5 claims increased by 185% from 2004 to 2021. In offices, the cost of Level 1 visits remained relatively flat, increasing by 3%, while the cost of the highest complexity (Level 5) outpatient office claim increased by 79%. In urgent care centers, the gap between the lowest complexity and highest complexity claims also widened. The cost of level 1 claims remained flat, while the cost of level 5 claims increased by 59%.
Implications for outpatient spending
Next, we examine how much lower 2021 spending would have been if visits were billed at the same levels as 10 years earlier. To do this, we multiply the average cost of each level claim in 2021 (e.g., the average level 5 emergency visit in 2021 was $556) times the share of visits that were billed at that level in 2011 (e.g., 16% of emergency visits were billed at level 5 in 2011). We calculate hypothetical total spending on evaluation and management services for the 2021 population using 2021 costs and 2011 levels, and we compare this to the actual 2021 spending using 2021 levels.
We find that if outpatient visit levels were coded the same in 2021 as they were in 2011, there would have been significant cost-savings in 2021. Both physician office and emergency department evaluation and management spending would have been 4% lower in 2021 than 2021 actual spending. Using 2004 levels instead of 2011 levels, emergency department spending would be 11% lower and office spending would be 10% lower in 2021 than actual 2021 spending. The majority of the cost saving would come from outpatient office claims because they make up a larger share of the outpatient evaluation and management spending we studied (69%) compared to emergency departments (27%) and urgent cares (3%). These numbers do not identify the portion of cost savings related to changes in services provided versus changes in billing patterns, since we did not control for clinical characteristics of the population.
Discussion
Over time, outpatient visits are being coded at higher levels, thus resulting in higher costs. We find that if the distribution of claim levels had stayed consistent over the prior ten years, outpatient evaluation and management costs would have been 4% lower in 2021. Of the outpatient settings we studied, emergency department evaluation and management claims are coded at the highest levels and are the most expensive, on average; however, outpatient office visits are the largest contributor to aggregate outpatient health expenditures because of the larger number of office visits.
The trend toward higher levels is seen across all outpatient settings, including emergency departments, urgent care centers, and physician offices. Increasing levels of visit complexity could reflect changes in billing, services provided, patient acuity, or a combination of factors. We did not control for clinical acuity; however, we did observe a trend towards higher claim levels even for specific conditions that are less likely to be worsening over time or for which comorbidities have a smaller impact, like headaches and urinary tract infections.
Overall, our findings demonstrate that regardless of the driving factors, increasing billing at higher levels for outpatient care has led to substantial increases in outpatient visit spending at the health system level. For consumers who bear the marginal costs of more expensive services—those with co-insurance or deductibles —this trend impacts out-of-pocket costs in addition to overall health system costs.
This analysis is based on data from the Merative MarketScan Commercial Database, which contains claims information provided by a sample of large employer plans. This analysis used claims for almost 14 million people representing about 17% of the 85 million people in large group market plans (employers with a thousand or more workers) from 2004-2021. To make MarketScan data representative of large group plans, weights were applied to match counts in the Current Population Survey for enrollees at firms of a thousand or more workers by sex, age and state. Claims were included if they were below the 99.5 th percentile of costs.
Claims were included and classified by location if their place of service was in the emergency department, office, or urgent care. We included claims that were classified as both professional and facility charges, if they were associated with evaluation and management procedure codes. Evaluation and management claims in the emergency department included 99281-99285, which are evaluation and management CPT codes that are specific to the emergency department. Note that in 2023 , 99281 is no longer being used for physician encounters and these codes are now based only on complexity of medical decision-making; however these changes do not affect the time period included in our analysis. In the office, we included the outpatient established patient evaluation and management codes, which are 99211-99215, because the vast majority of visits in outpatient physician offices were for established patients. In urgent care, visits were relatively evenly divided between new and established patients, so we created an aggregate complexity level from 1-5 combining CPT codes 99211-99215 (established patients) and 99201-99205 (new patients). Primary headache, upper respiratory tract infection and urinary tract infection were defined by ICD-9 and ICD-10 codes included in each claim. Enrollees were considered to have a certain diagnosis if the relevant ICD code appeared in the “Diagnosis 1” on the claim.
This analysis has some limitations. First, we analyzed only spending that happened within the specific place in our analysis (emergency department, office, or urgent care). Some visits, especially emergency department visits, have testing such as imaging or lab studies that occur outside of the emergency department in a different part of the hospital, and these are not included in our analysis. Second, the MarketScan database includes only charges incurred under the enrollees’ plan and do not include balance billing to enrollees which may have occurred during the study period.
About this site
The Peterson Center on Healthcare and KFF are partnering to monitor how well the U.S. healthcare system is performing in terms of quality and cost.
More from Health System Tracker
How have costs associated with obesity changed over time.
How financially vulnerable are people with medical debt?
Looking for more data?
Find out more details about U.S. healthcare from our updated dashboard.
A Partnership Of
Share health system tracker.
Why Did My Emergency Room Visit Cost So Much?

Emergency room visits are notoriously expensive. Just a few hours in the ER can cost you thousands of dollars, with or without insurance.
But how is your ER visit cost calculated, and how can you tell whether your hospital bill is correct?
We scored some insider tips from Goodbill medical coding expert Christine Fries, who has analyzed thousands of ER hospital bills for accuracy. Here are answers to frequently asked questions we get from Goodbill customers about how to understand and vet ER visit costs.
Why did I get 2 bills for my ER visit?

Patients are usually surprised when their first ER hospital bill is quickly followed by a separate hospital bill with similar-sounding charges but different amounts. This is normal and a byproduct of how hospitals bill patients for the services rendered at the hospital, Fries says.
The institutional bill, also known as the facility bill, charges you for the procedures, tests, and administrative costs from the hospital.
The professional bill, also known as the physician bill, charges you for the work and time of the physician who treated you. This generally includes services from doctors, anesthesiologists, or specialists who are affiliated with the hospital but aren’t employed by the hospital.
Expect to get two bills from your ER visit — one for facility charges, and the other for professional or physician charges.
For more information on the different types of hospital bills, see our itemized bill guide . Goodbill currently helps patients negotiate institutional bills, not professional bills, so our guidance below pertains to institutional bills only.
My diagnosis turned out to be minor. Why was I charged so much?
It’s important to remember that your ER visit costs are based on the symptoms you first describe upon entering the hospital, not your eventual diagnosis, Fries says.
When a patient walks into the emergency room complaining of chest pains, for example, the hospital’s objective is to run tests and administer procedures that can help rule out life-threatening conditions. Even if the doctor ends up discharging the patient with a non life-threatening diagnosis like indigestion, the hospital has already spent the resources to rule out more severe possibilities like a heart attack.
Your ER visit costs are based on the symptoms you first describe upon entering the hospital, not your eventual diagnosis.
“Look at your symptoms first, not what you were diagnosed with,” Fries says. “The level of your ER visit is guided by the symptoms you described, and by the tests the hospital thought were needed based on those symptoms.”
Why was I charged for an ‘ER Visit Level’ 3, 4, or 5? Is this based on severity?
Hospitals will bill you for a line item called “ER Visit Level” that is based on the complexity of your treatment. ER visit levels range from 1-5: ER visit level 1 is the most mild, while ER visit level 5 is the most severe. The level also determines how much the hospital can charge you, from least expensive to most expensive. You may sometimes hear ER visit levels described by their corresponding Current Procedural Terminology (CPT) codes of 99281, 99282, 99283, 99284 and 99285.
To decide the proper ER visit level, hospitals typically follow certain guidelines from the American College of Emergency Physicians (ACEP) . ER level 1-2 visits are reserved for treatment of mild cases like bug bites and sunburns. The majority of ER visits fall between ER visit levels 3-5, with ER visit level 4 being the most common, Fries says.
“Most emergency room claims will qualify as a 99284, because you only need something as simple as IV fluids to get you there,” Fries says.
The majority of ER visits fall between ER visit levels 3-5, with ER visit level 4 being the most common.
Here’s a simple rule of thumb for determining whether your ER visit level was correctly assigned.
ER Visit Level 4
An ER visit level 4 typically requires a minimum of two diagnostic tests — like a lab plus an EKG, or a lab plus an X-ray. Or, any administration of fluids through IV will automatically qualify your visit as an ER visit level 4.
ER Visit Level 5
An ER visit level 5 typically requires a minimum of three diagnostic tests — for example, a lab plus EKG and X-ray. Or, any type of imaging scan like a CT scan or MRI where a patient must ingest or be injected with contrast material, will automatically qualify your visit as an ER visit level 5.

I’m not pregnant. Why did I get charged for a pregnancy test?
Many female patients get frustrated when they’re charged for a pregnancy test, even when they’re absolutely certain they’re not pregnant. But this is standard practice and a way for hospitals to protect against unknown pregnancies, Fries says.
If you’re an adult pre-menopausal female, you can count on being asked to do a urine or blood pregnancy test before the hospital will treat you. It’s too risky to both the patient and hospital to administer injections, scans or drugs in the off chance that a patient is unknowingly pregnant.
If you're a female, expect to get a pregnancy test during your ER visit — even if you're not pregnant.
On your itemized ER bill, your pregnancy test will usually show up with a description like “human chorionic gonadotropin (hCG),” which is the hormone being tested. This charge will generally fall under the CPT codes 84702 or 84703 if it’s a blood test, or 81025 if it’s a urine test.
What are some other common ER services I might see on my hospital bill?
Here are a few common procedure names that often show up in your ER visit costs, and what they mean in plain English:
Metabolic panel
This is a bundle of lab tests run from a single blood draw. Patients may get a “basic” metabolic panel under CPT code 80048, or a “comprehensive” metabolic panel under CPT code 80053. These panels cover a set of individual tests that might otherwise be individually charged. For example, a “comprehensive” metabolic panel must include testing for all of the following:
- Carbon dioxide
- Phosphatase, alkaline
- Transferase, alanine amino
- Transferase, aspartate amino
- Urea nitrogen
Venipuncture
Any time you get your blood drawn through a needle, this charge under CPT code 36415 is the line item that bills you for the needle.
This test under CPT code 83690 measures your levels of lipase, which is an enzyme that helps break down fat in your intestines. Your lipase levels may be elevated if you have pancreatitis, which is an inflammation of the pancreas gland.
What are some ER visit cost errors I should look out for?
When analyzing a patient’s ER visit costs for errors, Fries says she goes straight to one place first: Hydration services. If you recall being administered fluids through an IV bag, chances are you got hydration services during your ER visit.
“Hydration services should always be questioned,” Fries says.
Coding guidelines require that the two CPT codes for this service, 96360 and 96361, meet a minimum time requirement of 31 minutes in order for one unit to be billed. These 31 minutes must also be “stand alone” — meaning that the administration of the service cannot overlap with any other type of infusion service. Often, hospitals don’t meet these requirements, rendering the charge unbillable.
Hydration services are a common source of errors in ER hospital visit costs. You can tell if you're being overcharged by checking your medical record.
To verify whether you’re being charged properly, you’ll need your medical record, Fries says. Look for hydration service “start” and “stop” times, which are usually included in the Medication Administration Report (MAR) section of your record. If the hydration service duration is less than 31 minutes of standalone time, you have a strong case to dispute the charge with your hospital. To find out how to get your medical records online, visit our Medical Records guide .
I don’t see any CPT codes on my bill. How can I get them?
CPT codes are the common language used across all hospitals to describe a certain procedure. They’re what enables our medical coders at Goodbill to analyze hospital bills for errors, line item by line item. They also help us compare prices apples-to-apples across hospitals.
CPT codes are the standard language used to describe a certain procedure across all hospitals. They're key to helping you identify errors or inflated charges in your ER hospital bill.
Unfortunately, the hospital bill you get in the mail is most likely a consolidated summary of your ER visit costs and won’t include CPT codes. You’ll need an “itemized bill” from your hospital to get a line-by-line breakdown of each charge, complete with the CPT code and cost.
The good news is that you’re legally entitled under HIPAA to get access to this information. To learn more about your patient rights and how to obtain your itemized bill, check out our Patient Right of Access guide .
Are there other topics you’d like us to cover? Email us at [email protected] and let us know.
Guides, news, and articles to help you tackle hospital bills.

How to Negotiate Your Hospital Bill
Read our expert tips on how to negotiate your hospital bill to save up to thousands of dollars.

Itemized Bill: Your Key to Negotiating
Itemized bills provide key details that can help you negotiate your hospital bill.
.jpg)
Can Hospital Bills Affect My Credit?
You have time before your bill can go to collections or affect your credit.
Negotiating hospital bills has never been this easy.
Building trust and confidence into every health care transaction.

© 2022 Goodbill, Inc.

Mississippi Today
Pulitzer Prize-winning Nonprofit News
Mississippi hospital officials say marketplace insurance helps, but not as much as Medicaid

Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to email a link to a friend (Opens in new window)
- Click to print (Opens in new window)
Mississippi Senate leaders point to one component of the federal Affordable Care Act health care law as a reason not to expand Medicaid to provide health care coverage to the working poor.
The Senate has passed legislation to allow only those earning less than 100% of the federal poverty level (about $15,000 annually for an individual) and who are working to be covered by Medicaid.
A state House plan would provide Medicaid coverage to those earning up to 138% of the federal poverty level (about $20,000 annually) as is allowed under the Patient Protection and Affordable Care Act, also known as Obamacare.
House and Senate leaders are expected to begin negotiations in the coming days in an attempt to work out the differences between the two chambers.
One reason Senate leaders give for not expanding to provide Medicaid coverage to those earning between 100% and 138% of the federal poverty level is that people who fall into that income category can obtain private insurance through another component of the ACA – the Affordable Care Act Marketplace or “exchange.” People can receive private insurance through the exchange and receive federal help to pay for the policy.
“We want to keep more people on the exchange. The reimbursements (to health care providers) are better,” through the exchange than through Medicaid, said Senate Medicaid Chairman Kevin Blackwell, R-Southaven. “A lot of the argument for expansion has been to help the hospitals. Well, if you are going to take the people who currently have commercial insurance and put them on Medicaid, you just killed your hospitals.”
While the exchange policies assist people who otherwise would not have access to health care coverage, the problem, according to Mississippi hospital officials, is that they often lose money when treating low income people who have the marketplace coverage.
“The bottom line is that Medicaid reimburses at a higher rate,” said Lee McCall, chief executive officer of Neshoba General Hospital in Philadelphia. He said there are some private insurance policies that pay Mississippi hospitals a better reimbursement rate, but not the marketplace plans.
“Most of those marketplace plans, I kind of call catastrophic coverage … ,” McCall said. “For the most part the deductibles are so high many people cannot afford to pay them.”
Kim Hoover, interim chief executive officer of the Mississippi Hospital Association, said Medicaid actually pays state hospitals at the commercial rate – or at the same rate paid by private insurance companies.
Gov. Tate Reeves’ Division of Medicaid got approval from federal Medicaid officials to pay at that higher rate last year. The state’s hospitals agreed to pay the local matching funds needed to draw down the additional Medicaid dollars to pay at the commercial rate.
With the better rate the hospitals now receive from Medicaid, Hoover said, “The main difference between the two is the typically high deductibles for hospital services on the exchange plans. If the patient deductible isn’t paid, then the plan doesn’t pay the hospital the full payment. By comparison, Medicaid patients have no deductible.
“No deductible combined with the commercial rate means that Medicaid is typically better for providers and patients than the exchange plans,” Hoover continued.
Hoover cited an example of “a 54-year-old male in Hinds County making $17,000 a year could pay a monthly premium of $16.85 with a deductible of $6,350 for one of the exchange plans. In this case, the deductible is over 33% of the person’s pre-tax income. Recently, Mississippi led the nation in medical debt bankruptcies. Medicaid expansion would better protect these patients from medical debt.”
Granted, thanks to changes made to the exchange during the pandemic, low income people can get a policy better than what Hoover described. With federal help people between 100% and 138% of the federal poverty level can get a plan with little or no monthly premiums. But there are still out of pocket costs or deductibles for the policyholder on the marketplace plans, though currently less than the amount cited by Hoover.
For instance, on the federal HealthCare.gov website where Mississippians would go to obtain a marketplace plan, a 40-year-old earning $19,000 annually could obtain a plan with a monthly premium of less than $5. But there would be $1,650 out of pocket expenses for one plan.
In general, out of pocket expenses represent the most a person would pay in a year for in-network health care services.
The benefits offered by the marketplace plans have been enhanced through COVID-19 relief legislation passed during the President Joe Biden Administration. Because of that legislation, people pay lower monthly premiums and less in out of pocket expenses than they did previously.
Robin Rudowitz, director of Program on Medicaid and the Uninsured for KFF, said the “the enhanced coverage subsides” people currently are benefitting from are set to expire in 2025. After that, people will be paying more for premiums and more in deductibles and out of pocket expenses.
In addition, Rudowitz pointed out that according to a recent consumer survey, people with Medicaid, even though they generally have more serious health care issues and thus more opportunities for problems, rate their coverage through Medicaid higher than those on private marketplace plans rate their policies.
State Insurance Commissioner Mike Chaney was one of the first state officials to argue in favor of expanding Medicaid just to those earning less than 100% of the federal poverty level to ensure the people above that income level remained in the marketplace.
READ MORE: Negotiations begin: Where do House, Senate, governor stand on Medicaid expansion? Is there room for compromise?
Chaney said there are about 140,000 Mississippians between 100% and 138% of the federal poverty level who have insurance through the marketplace. Under the federal law, if those people are eligible for Medicaid expansion, through an expansion in their state, they no longer would receive the federal help with the private insurance option. With no federal financial assistance, low income people would not be able to afford the marketplace plans.
Moving those people to Medicaid “would destroy the exchange,” Blackwell said. But 40 other states have expanded Medicaid, and they still have exchange policies for those earning too much to qualify for Medicaid expansion.
Some states, such as Arkansas, have used Medicaid expansion funds to pay for private policies for those who would qualify for Medicaid expansion. The federal government allows those states to use their Medicaid expansion funds to pay for the costs of the private health insurance.
READ MORE : Speaker White on Medicaid expansion negotiations: ‘Come for the savings, stay for the compassion’
The federal government pays 90% of the health care costs for Medicaid expansion. But the federal government would not recognize the Senate plan as Medicaid expansion and thus would pay only 77% of the costs, thus costing the state more to cover fewer people, according to various studies. The federal government also will pay Mississippi an additional nearly $700 million over a two-year period as an incentive to expand Medicaid.
KFF, the national non profit that studies health care issues, “estimates that approximately 166,000 uninsured adults would be eligible for expansion – this includes 102,000 who currently fall into the coverage gap (earning less than 100% of the federal poverty level) and another 64,000 who have incomes between 100% and 138% and could be eligible for marketplace coverage but not enrolled.”
In addition there are 140,000 Mississippians who have private insurance through the exchange would have to drop their policy and sign up for Medicaid if expansion is approved by the Legislature.
Based on the experiences of hospital officials, replacing those private policies with Medicaid would not necessarily be a bad thing.
Republish This Story
Republish our articles for free, online or in print, under a Creative Commons license.
Republish this article

This work is licensed under a Creative Commons Attribution-NoDerivatives 4.0 International License .
- Look for the "Republish This Story" button underneath each story. To republish online, simply click the button, copy the html code and paste into your Content Management System (CMS).
- Editorial cartoons and photo essays are not included under the Creative Commons license and therefore do not have the "Republish This Story" button option. To learn more about our cartoon syndication services, click here .
- You can’t edit our stories, except to reflect relative changes in time, location and editorial style.
- You can’t sell or syndicate our stories.
- Any web site our stories appear on must include a contact for your organization.
- If you share our stories on social media, please tag us in your posts using @MSTODAYnews on Facebook and @MSTODAYnews on Twitter.
- You have to credit Mississippi Today. We prefer “Author Name, Mississippi Today” in the byline. If you’re not able to add the byline, please include a line at the top of the story that reads: “This story was originally published by Mississippi Today” and include our website, mississippitoday.org .
- You cannot republish our editorial cartoons, photographs, illustrations or graphics without specific permission (contact our managing editor Kayleigh Skinner for more information). To learn more about our cartoon syndication services, click here .
- Our stories may appear on pages with ads, but not ads specifically sold against our stories.
- You can only publish select stories individually — not as a collection.
by Bobby Harrison, Mississippi Today April 11, 2024
This <a target="_blank" href="https://mississippitoday.org/2024/04/11/mississippi-exchange-marketplace-medicaid-expansion-private-insurance-legislature/">article</a> first appeared on <a target="_blank" href="https://mississippitoday.org">Mississippi Today</a> and is republished here under a Creative Commons license.<img src="https://i0.wp.com/mississippitoday.org/wp-content/uploads/2024/01/MT_icon-logo-favicon-1.png?fit=134%2C150&ssl=1" style="width:1em;height:1em;margin-left:10px;"><img id="republication-tracker-tool-source" src="https://mississippitoday.org/?republication-pixel=true&post=1115014&ga4=G-VSX4B701MS" style="width:1px;height:1px;">
Bobby Harrison
Bobby Harrison, Mississippi Today’s senior capitol reporter, covers politics, government and the Mississippi State Legislature. He also writes a weekly news analysis which is co-published in newspapers statewide. A native of Laurel, Bobby joined our team June 2018 after working for the North Mississippi Daily Journal in Tupelo since 1984. He is president of the Mississippi Capitol Press Corps Association and works with the Mississippi State University Stennis Institute to organize press luncheons. Bobby has a bachelor's in American Studies from the University of Southern Mississippi and has received multiple awards from the Mississippi Press Association, including the Bill Minor Best Investigative/In-depth Reporting and Best Commentary Column.
- Search Please fill out this field.
- Manage Your Subscription
- Give a Gift Subscription
- Newsletters
- Sweepstakes
Kate Beckinsale Shares New Photos from Hospital Bed as a Friend Visits Her
Beckinsale first revealed she was in the hospital in early March when she shared two teary-eyed pictures
:max_bytes(150000):strip_icc():format(webp)/Biopicture-7aed89e79c07468e879a00bb6ff007dc.jpg)
Kate Beckinsale/Instagram
Kate Beckinsale is sharing more snaps from the hospital.
On Thursday, April 4, the actress, 50, shared an update from her hospital stay as she posted a series of snaps with the caption, “🥜🥜🌈🌈🖕🏻😢🌈🌈🥜🥜."
Beckinsale has been posting photos from the hospital since early March, but she hasn't confirmed the reason for her being there.
In the first shot from the carousel, Beckinsale posed in a hospital bed in a pair of cat-print silk pajamas with her pal Jonathan Voluck, who was paying a visit to the star. The duo appeared to be wearing peanut headbands as they flashed a smile at the camera in the snap, while a collagen supplement could also be seen on the star's nightstand.
Beckinsale then shared a photo of a rainbow in the sky before posting a jar full of wooden words that featured the label, “F---s to give.”
In the fourth slide, Beckinsale revealed the book Grief Is For People by Sloane Crosley, before sharing another snap of a rainbow.
She then concluded the carousel post with another shot of herself and Voluck.
“The Clive pajamas! Sending love & healing 💖,” one person commented, while another added, “I saw the rainbow today too!! I hope you feel better soon!!! 🫰🏽💐.”
Fashion designer Ramona Agruma , who is also the fiancée of actress Rebel Wilson , also wrote, “Sending you lots of love 💗💗💗.”
Never miss a story — sign up for PEOPLE's free daily newsletter to stay up-to-date on the best of what PEOPLE has to offer, from juicy celebrity news to compelling human interest stories.
On March 19, Beckinsale remembered her late dad , Richard Beckinsale, with an emotional Instagram post, days after first revealing she was in the hospital. Richard died in 1979 of a heart attack at the age of 31. Her stepfather Roy Battersby also died at age 87 on Jan. 10.
While Beckinsale hasn't confirmed the reason behind her hospitalization, she has denied being treated for a ruptured cyst or endometriosis. Responding to one of her followers who said that her "ruptured cyst must have taken such a toll" on her, Beckinsale replied n the comments section, "I didn’t have a ruptured cyst since 2019. But thank you so much for your kind wishes x."
Beckinsale shared that she'd suffered a ruptured ovarian cyst in January 2019.
She first sparked concerns with her more recent hospital stay when she shared two teary-eyed photos of herself from the hospital and referred to being "sick” in an Instagram post on March 11.
"Happy birthday and UK Mother’s Day this last week to my incredible mother,” she wrote at the time. “Thank you to those that love us and support us when it’s s— and try to make sure there are some bits that aren’t. And for looking after our dogs when we can’t, and lead us to remember happy things when we can’t. And turn up when we are sick and sit with us . . And send balloons and check in and pull us out of wells with love.”
Meanwhile, the Farming star also marked her Easter holiday at the hospital by showing off a pair of festive-themed socks .
“Happy Easter 🐰🐇🐣,” her caption read as she shared two snaps of her black pajama pants and bunny socks from a hospital bed.
Related Articles

Therapy dogs visit kids at Kaiser Permanente on National Pet Day

SAN DIEGO — The pitter-patter of paws is not always something you expect to hear inside a hospital.
However, at the pediatric unit at Kaiser Permanente San Diego Medical Center, a few puppy-paws are a warm welcome.
“You can train a dog to do almost anything, but you can’t train them to be calm, gentle, sweet and that’s him," said Carol Stevens, a pet therapy volunteer, describing her poodle "Georgie-Porgie."
Steven retired from a sales position at Kaiser in 2008 and has been volunteering her time bringing her therapy dog to the hospitals ever since.
"You would be amazed [by] the people who laugh, and giggle, and smile who perhaps haven't done that for a few days because of where they are, and if I can do that in the life of someone, why wouldn't you do that?" said Stevens.
Thursday morning was a busy one at the hospital's pediatric unit.
Several therapy dogs made their way from one room to another, greeting patients and staff to put a smile on their faces.
"It was great to have visitors, especially furry visitors," said one patient's mother. Her son has been in the hospital for close to a week.
According to John Hopkins Medicine:
"Research has shown that simply petting a dog lowers the stress hormone cortisol, while the social interaction between people and their dogs actually increases levels of the feel-good hormone oxytocin"
Sign up for the Breaking News Newsletter and receive up to date information.
Now signed up to receive the breaking news newsletter..

Nominate a Leader Today!

Gaza City Dispatch
Israeli Army Withdraws From Major Gaza Hospital, Leaving Behind a Wasteland
Al-Shifa Hospital as seen from an Israeli military position at a private clinic outside the hospital on Sunday in Gaza City. Credit...
Supported by
- Share full article
By Patrick Kingsley
Photographs by Avishag Shaar-Yashuv
The journalists were among a small group of international reporters brought by the Israeli army to Al-Shifa Hospital on Sunday. To join the tour, they agreed to stay with the Israeli forces at all times and not to photograph the faces of certain commandos.
- April 2, 2024
Al-Shifa Hospital in Gaza City, once the fulcrum of Gaza’s health system and now an emblem of its destruction, stood in ruins on Sunday, as if a tsunami had surged through it followed by a tornado.
The emergency department was a tidy, off-white building until Israeli troops returned there in March. Two weeks later, it was missing most of its facade, scorched with soot, and punctured with hundreds of bullets and shells.
The eastern floors of the surgery department were left open to the breeze, the walls blown off and the equipment buried under mounds of debris. The bridge connecting the two buildings was no longer there, and the plaza between them — formerly a circular driveway wrapping around a gazebo — had been churned by Israeli armored vehicles into a wasteland of uprooted trees, upturned cars and a half-crushed ambulance.
The hospital was the largest in Gaza, one of its biggest employers and a shelter for thousands of Gazans during war. I had visited its wards in calmer times, meeting Palestinians wounded in a previous conflict and doctors battling Covid-19. When I returned this week, the place was disfigured almost beyond recognition after a 12-day battle between Israeli soldiers and Gazan gunmen and an earlier raid by the Israeli military.
During a two-hour visit, I saw no Palestinians, but the Israeli soldiers who brought me there said there were still gunmen inside one building and a group of patients and doctors in another. Occasionally, we heard short bursts of gunfire. When the soldiers brought us to a vantage point overlooking the hospital, they told us not to linger long in the window in case a sniper saw us.

The symbolism of this hellscape differs according to the beholder, amid a deep divergence about how the conflict should be reported and explained.
To the Israelis who brought me to Al-Shifa on Sunday, the carnage is the result of Hamas’s decision to turn a civilian institution into a military stronghold, leaving Israel with no option but to enter it by force: Exhibit A in what they see as a war of necessity that they did not start.
“We had no alternative,” said Rear Adm. Daniel Hagari, Israel’s chief military spokesman, who led the visit. “We wanted to leave those places functional, but what happened was Hamas and Islamic Jihad were barricading and firing at our forces from the beginning.”
To the Palestinians who returned to Al-Shifa on Monday, searching for dead bodies after the Israelis withdrew, it was the embodiment of Israel’s perceived disregard for civilian life and infrastructure in its pursuit of Hamas: Exhibit A in what they see as a genocide of Gazans.
“As you see, this is Al-Shifa hospital after it was invaded and destroyed by the Israeli occupation forces,” said Motasem Dalloul, a Palestinian journalist, in a self-filmed video he sent from the wreckage on Monday.
“Or what was once Al-Shifa Hospital,” added Mr. Dalloul.
When we met before the war, Mr. Dalloul said that he is not a Hamas member but speaks regularly to its leaders and cadres; he has also acted as an interpreter for its officials.
Walking further through the compound, Mr. Dalloul encountered another man who blamed Israel for the destruction. “This occupation will die, Netanyahu will die, America will die — no matter how much they bomb us,” the unnamed man shouted. “No matter how much they bomb us and destroy Al-Shifa, the occupation will die,” he repeated.
Analysts have said that Israel’s return to Al-Shifa, more than four months after it was first captured, represents a strategic failure: It is the result of Israel’s unwillingness to set in motion any transition of power to forces independent of Hamas, creating a vacuum that has allowed Hamas to regroup.
The Israeli soldiers at Al-Shifa on Sunday portrayed the raid as a success. In one swoop, they said, they had killed about 200 fighters and captured 500 more — the majority, they said, of the remaining militants in northern Gaza. Gazan officials said hundreds of civilians were killed, a charge denied by Israel, and The New York Times could not independently verify either account.
In any case, the soldiers’ departure, hours later, means it will be possible for Hamas to return once again, unimpeded, raising the chances that Israel could return for a third raid in the future.
The Israeli military first captured the hospital site during a raid in November, exposing and destroying a subterranean tunnel network that Israel said was a Hamas command center.
After withdrawing from most of the city in January, the military returned to the hospital in March because it said remnants of Hamas’s military wing had regrouped in Israel’s absence, according to the officers who were escorting the international journalists, including two from The New York Times, to the site on Sunday.
To join the tour, we agreed not to photograph the faces of certain commandos and to stay with the Israeli forces at all times, but otherwise agreed to no other restrictions.
Israel’s naval commando unit, Shayetet 13, swept into the hospital compound early on March 18. By Israel’s account, the destruction began after Hamas gunmen refused to surrender and started shooting at the Israeli forces, prompting them to return fire.
A spokesman for Hamas, Basem Naim, declined to comment on the claim that Hamas was operating inside the hospital but denied that its fighters were there; Hamas’s armed wing has said that it fired on Israeli forces in the vicinity of Al-Shifa, but stopped short of saying that it fought inside the compound.
The Israeli military said that one of the first men killed on March 18 was a security chief, Faiq Mabhouh, whose death was later mourned in a statement from Hamas. A map supplied by the Israeli military said there were at least 13 gunfights that broke out across different parts of the campus over the following two weeks, as the soldiers searched for holdouts hiding throughout the site.
The military said the damage to the emergency and surgery departments was so great because the gunmen had entrenched themselves inside those buildings, one of them inside an elevator shaft, forcing the Israeli commandos to fire repeatedly at their positions. The military said that it found several weapons caches hidden inside the hospital.
The military said the fighting was compounded by Gazan armed groups located outside the compound who also fired at Israeli soldiers, leading to gun battles around its perimeter and the killing of two Israeli soldiers outside the hospital. Hamas said on its social media platforms that its snipers and mortar teams had fired at Israeli forces in the vicinity of the hospital.
To support its claim of Hamas’s presence at the hospital, the Israeli military displayed digital copies of documents, branded with the logo of Hamas’s military wing, that it said were found at the site and which purported to document a meeting of the group’s militants inside the hospital. The Times could not verify the authenticity of the documents.
The Hamas-run authorities in Gaza have accused Israel of killing patients and displaced people sheltering at the hospital, as well as detaining innocent people.
Yahia Al-Kayyali, a 58-year-old doctor, said he was detained by the Israeli Army during the raid while sheltering with his family at a building close to the hospital.
In a phone interview, Dr. Al-Kayyali said the soldiers forced him to strip, a common practice that Israel says is meant to ensure detainees do not conceal weapons, before beating him and his son, interrogating and blindfolding them, taking them to the roof and forcing them to sit on shattered glass for several hours.
They were later released after being made to walk south, he said.
“The soldiers treated us like animals,” he said.
The Israeli soldiers who escorted us on Sunday strongly denied any accusation of wrongdoing. They said they had evacuated more than half of the medics and patients to other health facilities, as well as allowing the vast majority of the 6,000 civilians who had sheltered at the hospital to move south. They said they had detained 900 people, 500 of whom they said were militants and about 400 others who were still being investigated. The numbers could not be independently verified.
“I’ve been here for 14 days,” said the Shayetet 13 commander, who asked to remain anonymous in line with military protocol. “It’s my soldiers. As far as I know, these accusations are a lie.”
According to both Israeli and Palestinian officials, more than 100 patients and medics were moved to a building on the western side of the compound, away from the worst of the fighting.
But there the narratives diverge. The Israeli military says that it did its best to provide food, water and medical care. The Gazan health ministry said in a statement that the remaining patients were left without enough medicine, clean water, food or sanitation, leaving some with septic wounds containing maggots.
“The situation as reported by many of the staff is horrific and inhumane,” the health ministry’s statement said.
Citing Palestinian medics, the World Health Organization said in a statement on Sunday that 21 patients had died since the raid began, and those remaining lacked diapers and bags for urine.
To Taysir al-Tanna, a surgeon who said he had worked for 25 years at Al-Shifa, the destruction of his hospital felt like a national tragedy.
He recounted by phone how the hospital — one of the largest employers in both Gaza and the Israeli-occupied West Bank — had formed “a central place in our country.”
“Now, it’s become a wasteland,” Dr. al-Tanna said. “Try to imagine what that feels like.”
Aaron Boxerman contributed reporting from Jerusalem, and Iyad Abuheweila from Istanbul.
Patrick Kingsley is the Jerusalem bureau chief, covering Israel and the occupied territories. He has reported from more than 40 countries, written two books and previously covered migration and the Middle East for The Guardian. More about Patrick Kingsley
Our Coverage of the Israel-Hamas War
News and Analysis
The Israeli military announced what it called a precise operation to kill members of Hamas in Gaza , a day after a strike there killed three sons of one of the most senior leaders of the group.
Hamas said that it did not have 40 living hostages in Gaza who met specific criteria for an exchange with Israel under a proposed cease-fire deal, raising fears that more hostages may be dead than previously believed.
There has been no apparent work done yet on increasing aid to Gaza by opening an additional border crossing from Israel and accepting shipments at a nearby Israeli port, but Israel said that both changes remain in the works.
Psychedelics and Trauma: Thousands of festival-goers were using mind-altering substances when Hamas-led fighters attacked on Oct 7. Now, scientists are studying the effects of such drugs at a moment of trauma .
Turmoil at J Street: The war in Gaza has raised serious concerns within the Jewish political advocacy group about its ability to hold a middle position without being pulled apart by forces on the right and the left.
Challenging Democratic Leaders: Protests over the Biden administration’s handling of the war in Gaza are disrupting the activities of Democratic officials, complicating their ability to campaign during a pivotal election year .
Germany’s Upended Arts Scene: Berlin, the home of boundary-pushing artists from around the world, has been turned upside down by debates about what can and can’t be said about Israel and the war in Gaza .
Advertisement
Judge denies release from psychiatric institute for woman involved in 'Slender Man' attack

A Wisconsin judge has refused to release from a mental institution a woman who is serving a sentence for brutally stabbing a peer as a child to earn the favor of the fictional horror character Slender Man in a case that shocked the nation a decade ago.
Morgan Geyser, now 21, in January had requested to be released from the Winnebago Mental Health Institute, and proceedings started Wednesday and continued Thursday.
Waukesha County Circuit Judge Michael Bohren on Thursday determined Geyser posed a risk of harming herself or others, or of damaging property, and denied her release.
Geyser was sentenced to 40 years in a mental hospital in 2018 after pleading guilty to attempted first-degree intentional homicide in the brutal stabbing of her then-sixth-grade classmate Payton Leutner.
In the May 31, 2014 , attack , Geyser, along with peer Anissa Weier, lured Leutner, when they were all 12 years old, to a park in Waukesha after a sleepover, and Geyser repeatedly stabbed Leutner as Weier egged her on , prosecutors previously said.
Leutner was stabbed 19 times and barely survived, officials said.
They told investigators they did it to earn the favor of the fictional horror character Slender Man , and to become his servants and protect their families from him, The Associated Press reported.
Geyser had requested to be released in January, marking the second time she put in such a request. In 2022, she had also tried for conditional release , but withdrew the petition two months after filing it.
In Wednesday’s proceedings, two psychologists testified. One said Geyser claimed she had been faking psychotic symptoms, which “doesn’t line up” with years of observation and treatment, The Associated Press reported.
Dr. Kenneth Robbins, another doctor who prepared a conditional release report for Geyser, said in court Thursday he believed it was “an appropriate time” for her to be conditionally released to a group home.
“Morgan has improved quite dramatically and needs things that the institution can no longer offer,” he said. “No suggestion that she’s dangerous at this time and the kinds of things that Morgan needs, in my view, help with socialization, help with education, help with becoming independent, are things that Winnebago can no longer provide in an effective way.”
Weier also pleaded guilty to attempted second-degree intentional homicide and was sentenced to 25 years in a mental institution. Weier was released under strict conditions in September 2021 after almost four years. At the time, Judge Bohren ruled that she no longer posed a threat.
Breaking News Reporter

IMAGES
COMMENTS
For the past year and a half, she's been writing about why emergency room visits can be so expensive and the pricing so secretive and mysterious, as well as inconsistent from one hospital to the next.
Hospital emergency rooms are more expensive than urgent care centers. Patients can save time and money by choosing the right facility. Updated: March 5, 2024 ... The cost of a hospital emergency room visit can be 5-10X the cost of an urgent care visit, and the majority of hospital visits are considered non-emergency.
An ER visit costs $1,500 to $3,000 on average without insurance, with most people spending about $2,100 for an urgent, non-life-threatening health issue. The cost of an emergency room visit depends on the severity of the condition and the tests, treatments, and medications needed to treat it. Average ER visit cost - Chart.
Average Cost for ER Visits. In 2019, the average cost for an ER visit by an insured patient was $1,082. Those who were uninsured spent an average of $1,220. Average costs can vary by state and illness but range from $623-$3,087.
That might include a system that encourages home visits, since hospital visits are so expensive, he added. "(Patients) like it better and it's cheaper," Emanuel said.
According to most sources, the average cost of an emergency room visit in the United States is around $2,200, but this number can vary depending on a variety of factors, including the severity of the condition, where you live, and what type of insurance plan you have. For example, if you have health insurance through the Affordable Care Act ...
Secrecy around the price of hospital care has made visits in some places prohibitively expensive—and has fostered huge disparities, forcing people to pay far more for care depending on where ...
As noted, the average cost for an emergency room visit can be anywhere between $2,400 to $2,600. If you visit the ER without insurance, you could end up paying that entire amount — or more — yourself. According to Health System Tracker, 25% of ER visits cost $3,043 or more. People who have employer health plans still pay, on average, $646 ...
Everything is more expensive in the ER. According to UnitedHealth, ... Medicare Part A only covers an emergency room visit if you're admitted to the hospital. Medicare Part B covers 100% of most ER costs for most injuries, or if you become suddenly ill. Unlike private insurance and insurance purchased on the Affordable Care Act (ACA ...
Medicare and Medicaid pay less than the cost of caring for program beneficiaries - a shortfall of $75.8 billion in 2019 borne by hospitals. 8. Hospitals provided $41.6 billion in uncompensated care, both free care and care for which no payment is made by patients, in 2019. 9. Private insurance and others often make up the difference.
Urgent care centers are usually cheaper. The authors of the 2021 study state that the average cost of treatment at an urgent care center is $156, while the same treatment may cost $570 or more at ...
Going to the hospital is a stressful, often confusing, and potentially expensive experience. Whether it's a visit to the emergency room in the middle of the night or a planned surgical procedure ...
The average cost of a hospital admission among large employer plans increased by roughly $10,000 (68%) from 2008 to 2018 ... inpatient hospital admissions were most expensive in the San Diego, CA, area in both 2008 and 2018. ... There is considerable variation in the cost of outpatient visits depending on the severity and complexity of the visit.
The US population made 144.8 million emergency department (ED) visits in 2017, costing a total of $76.3 billion, estimated a recent statistical brief from the Agency for Healthcare Research and Quality's Healthcare Cost and Utilization Project (HCUP).. That year, 13.3% of the US population incurred an expense for an ED visit, and more than half of hospital inpatient stays originated with an ...
The average cost of treating common primary care treatable conditions at a hospital ED is $2,032, according to UnitedHealth Group. That number is 12 times higher than visiting a physician office ($167) and 10 times higher than traveling to an urgent care center ($193) to treat those same conditions. In other words, visiting either a physician ...
Florida is the most expensive state for emergency room visits. Moderate-severity ER patients are billed an average of $3,102 before. insurance. First published on December 4, 2020 / 3:56 PM EST
In Part 4 of WFAE's series The Price We Pay, reporter Dana Miller Ervin explores why, starting with rising hospital costs. In 2021, Americans will spend more than $ 4 trillion on health care, and ...
We analyzed the top 20 metropolitan statistical areas (MSAs) by population, where data are available. Overall, the San Diego, CA area had the most expensive average ED visits ($3,761 on average). San Diego ED visits were more than twice as expensive as Baltimore, MD, the least expensive MSA in our analysis ($1,645 on average).
Introduction. Emergency department (ED) visits have grown in the United States, with the rate of increase from 1996 to 2013 exceeding that for hospital inpatient care. 1 In 2017, 13.3 percent of the U.S. population incurred at least one expense for an ED visit. 2 Furthermore, more than 50 percent of hospital inpatient stays in 2017 included evidence of ED services prior to admission. 3 Trends ...
That was an expensive decision: It has the highest price for rabies shots among 24 hospitals that included the service in their newly released data sets. ... A few weeks after the visit, the ...
A strep throat visit costs an average of $75, as an example of a common ailment. Here is the average cost for nearly two dozen types of care at urgent care facilities across the nation.
Several prior studies have shown that outpatient costs are increasing and that providers are billing for more complex services. A KFF analysis of U.S. healthcare price growth found that the average price of an outpatient office visit grew faster than inflation from 2003-2019, and that the share of level 4 visits increased from less than 1-in-5 (19%) to more than 1-in-3 (36%) during the same ...
Emergency room visits are notoriously expensive. Just a few hours in the ER can cost you thousands of dollars, with or without insurance. ... The level also determines how much the hospital can charge you, from least expensive to most expensive. You may sometimes hear ER visit levels described by their corresponding Current Procedural ...
Senate investigating whether ER care has been harmed by growing role of private-equity firms. Sen. Gary Peters said he was concerned that emergency medicine staffing companies "may be engaging in ...
Kim Hoover, interim chief executive officer of the Mississippi Hospital Association, said Medicaid actually pays state hospitals at the commercial rate - or at the same rate paid by private insurance companies. Gov. Tate Reeves' Division of Medicaid got approval from federal Medicaid officials to pay at that higher rate last year.
Kate Beckinsale shared a carousel post on April 4 featuring new photos of her hospital stay, including receiving a visit from a friend and her view of a rainbow.
SAN DIEGO — The pitter-patter of paws is not always something you expect to hear inside a hospital. However, at the pediatric unit at Kaiser Permanente San Diego Medical Center, a few puppy-paws ...
April 8, 2024, 5:41 PM PDT. By Evan Bush and Aria Bendix. Google searches about "hurt eyes" spiked Monday afternoon, just after many U.S. communities experienced the total solar eclipse. The ...
The Israeli soldiers at Al-Shifa on Sunday portrayed the raid as a success. In one swoop, they said, they had killed about 200 fighters and captured 500 more — the majority, they said, of the ...
Morgan Geyser had been sentenced to 40 years in a mental hospital in 2018 in connection with the brutal 2014 stabbing of her sixth-grade peer when they were both 12.