Patient journey 101: Definition, benefits, and strategies
Last updated
22 August 2023
Reviewed by
Melissa Udekwu, BSN., RN., LNC
Today’s patients are highly informed and empowered. They know they have choices in their healthcare, which can put healthcare providers under a lot of pressure to provide solutions and meet their patients’ expectations.
Just like any customer, patients embark on a journey that begins before they ever contact the provider. This makes understanding the journey and where improvements can be made extremely important. Mapping the patient journey can help practitioners provide better care, retain a solid customer base, and ultimately identify ways to improve patient health.
- What is the patient journey?
The patient journey is best described as the sequence of experiences a patient has from admission to discharge. This includes all the touchpoints between the patient and provider from beginning to end.
The patient journey continues through consultation, where they meet the potential caregiver. That portion of the journey includes interactions with a doctor and support staff, how long they wait to be seen, and the steps taken for diagnosis and treatment.
The patient’s post-care journey includes follow-ups from the healthcare provider, post-treatment care, and billing. For example, if the patient has questions about post-surgery care or how to read their invoice, how quickly their questions are answered and their problems resolved will impact their satisfaction.
Mapping the patient journey helps healthcare providers improve patient satisfaction at every step of the way. By collecting data at each stage and conducting an in-depth analysis, providers can identify patient concerns and make the necessary improvements to meet their patient satisfaction goals.

What is another name for the patient journey?
The term “patient funnel” describes the journey patients take from first learning about a healthcare provider or healthcare product to actually making an appointment or purchase. This “funnel” can be applied to any type of business, describing the stages a customer goes through to obtain a service.
- Understanding the stages of the patient journey
Each stage of the patient journey is essential to a positive patient experience . Gathering and analyzing data can alert healthcare providers to potential issues throughout the journey.
Data collection at each of the following stages will give healthcare providers the information they need to make the necessary improvements:
1. Awareness
Awareness is where the patient journey begins. This is when they first research symptoms and identify the need to see a medical professional.
They may consider at-home remedies and get advice from friends, social media, or websites. Once they identify the need for a healthcare provider, they continue their research via review sites, advertising campaigns, and seeking referrals from friends and family.
Determining the way patients become aware they need healthcare and the sources they use for research is important. The data collected at this stage could suggest your organization has an insufficient social media presence, inadequate advertising, or a website in need of an update.
To remedy these shortcomings, you might consider adding informational blogs to your website, performing a social media analysis, or closely monitoring customer reviews.
This stage in the patient journey is where the patient schedules services with the healthcare provider.
This engagement is essential for acquiring new patients and retaining current patients. Patients will contact you in several ways to schedule an appointment or get information. Most will call on the first attempt to schedule an appointment.
This is a crucial touchpoint in the journey. A new patient may become frustrated and move on if they find it difficult to access your services or are placed on hold for a long period or transferred numerous times.
Patient engagement occurs in other ways, such as your online patient portal, text messages, and emails. Your patients may interact differently, so it’s important to gather data that represents their preferred means of communication. Work to make the improvements required to correct access issues and ensure efficient communication.
The care stage can include everything from your patient’s interaction with the front desk to how long they have to wait in the examination room to see a doctor.
Check-in, check-out, admissions, discharge, billing, and of course, the actual visit with the healthcare provider are other touchpoints in the care stage.
There are a couple of ways to gather and analyze this data. Most organizations choose to analyze it holistically, even if it’s collected separately. For example, you might gather data about the patient’s interaction with the front desk, the clinical visit, and the discharge process, but you may want to analyze the care segment as a whole.
4. Treatment
Treatment may be administered in the office. For example, a patient diagnosed with hypertension may have medication prescribed. That medication is the treatment. Gathering information at this stage is critical to see how your patient views the healthcare provider’s follow-up or responses to inquiries.
In most cases, treatment extends beyond the initial clinical visit. For example, a patient might require additional tests to get a diagnosis. Providing the next steps to a patient in a timely manner and letting them know the test results is crucial to patient satisfaction .
5. Long term
A satisfied patient results in a long-term relationship and referrals to friends and family. Most of the data collected at this stage will be positive since the patient is continuing to use your services.
Gathering data after the treatment stage allows you to expand on the qualities that keep patients returning for your services in the long term.
- Benefits of patient journey mapping
The patient benefits from their healthcare provider understanding their journey and taking steps to improve it. Healthcare providers also reap several benefits, including the following:
1. Efficient patient care
When they understand the patient journey, healthcare providers can provide care more efficiently and spend less time and money on unnecessary, unwanted communications.
2. Proactive patient care
Proactive patient care is aimed at preventing rather than treating disease. For example, women who are over a certain age should have an annual mammogram, smokers may be tested for lung disease, and elderly women may need a bone density study. These preventative measures can help keep disease at bay, improve health outcomes, and build trust with patients.
3. Value-based patient care
Patients don’t want to feel they are being charged unfairly for their healthcare. Focusing on the individual patient promotes satisfaction and yields positive outcomes.
The Center for Medicare and Medicaid Services (CMS) has issued recent guidelines for participants that help offset the costs of high-quality care through a reward system.
4. Retention and referrals
Patients who are happy with their journey will keep returning for healthcare, and happy patients equal voluntary referrals. Many providers offer rewards to incentify referrals.
- How to get started with patient journey mapping
Follow the steps below to start the patient journey mapping process:
Establish your patient personas
Journey mapping is a great way to identify your patient’s characteristics so that their experience can be further enhanced.
Some of the following determinations can help you pinpoint your patient’s persona and establish protocols to provide a better service:
How do your patients prefer to communicate? Are they more comfortable with phone calls, texts, or other methods?
How are most patients finding your services? Are they being referred by friends or family members, or are they seeing advertisements?
Would the patient prefer in-person communication or telecommunication?
What are the patient’s expectations of care?
This data can be complex and widespread, but it can give you the information you need to more effectively and efficiently communicate with your patients.
Understand the entire patient lifecycle
Each patient is unique. Understanding the patient lifecycle can avoid confusion and miscommunication.
To positively engage the patient, you’ll need to gather data not only about communication methods but where they are in the patient journey, their health issue, and their familiarity with the healthcare provider’s procedures and treatment options.
Understand the moments of truth
With a few exceptions, most people seek healthcare services when they are ill or have a healthcare issue. These situations can cause patients to feel stressed and anxious. It’s these moments of interaction where compassion, knowledge, and understanding can provide relief and reassurance.
When patients see their healthcare provider, they are looking for solutions to problems. It’s the provider’s opportunity to identify these moments of truth and capitalize on them.
Get the data you need
Healthcare providers can collect vast amounts of data from patients, but the data collected rarely goes far enough in analyzing and determining solutions.
Your patients have high expectations regarding personalized treatment based on data. They want personalized, easy access to medical information and records, responsive treatments and follow-up, and communication in their preferred format.
You need more than clinical data to give patients what they want. You also need personal data that sets each patient apart and ensures a tailored experience.
For example, it might be challenging for parents of small children to contact the clinic and schedule appointments at certain times of the day. As a healthcare provider, you’ll need to be aware of the best times to contact this individual and offer simple methods for scheduling appointments.
Another example is patients with physical disabilities. You can take steps to improve their access to and experience at the healthcare facility.
Encourage referrals and loyalty
Although engagement on social media and online forums is becoming more and more common, the best way for new patients to find you is through referrals. Referrals stem from satisfactory experiences and trust.
Get started today
Go from raw data to valuable insights with a flexible research platform
Editor’s picks
Last updated: 27 June 2023
Last updated: 22 July 2023
Last updated: 11 September 2023
Last updated: 10 October 2023
Last updated: 16 November 2023
Last updated: 28 September 2023
Last updated: 12 October 2023
Last updated: 25 November 2023
Last updated: 3 July 2023
Last updated: 27 January 2024
Latest articles
Related topics, log in or sign up.
Get started for free
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 04 December 2019
“Patient Journeys”: improving care by patient involvement
- Matt Bolz-Johnson 1 ,
- Jelena Meek 2 &
- Nicoline Hoogerbrugge 2
European Journal of Human Genetics volume 28 , pages 141–143 ( 2020 ) Cite this article
24k Accesses
18 Citations
25 Altmetric
Metrics details
- Cancer genetics
- Cancer screening
- Cancer therapy
- Health policy
“I will not be ashamed to say ‘ I don’t know’ , nor will I fail to call in my colleagues…”. For centuries this quotation from the Hippocratic oath, has been taken by medical doctors. But what if there are no other healthcare professionals to call in, and the person with the most experience of the disease is sitting right in front of you: ‘ your patient ’.
This scenario is uncomfortably common for patients living with a rare disease when seeking out health care. They are fraught by many hurdles along their health care pathway. From diagnosis to treatment and follow-up, their healthcare pathway is defined by a fog of uncertainties, lack of effective treatments and a multitude of dead-ends. This is the prevailing situation for many because for rare diseases expertise is limited and knowledge is scarce. Currently different initiatives to involve patients in developing clinical guidelines have been taken [ 1 ], however there is no common method that successfully integrates their experience and needs of living with a rare disease into development of healthcare services.
Even though listening to the expertise of a single patient is valuable and important, this will not resolve the uncertainties most rare disease patients are currently facing. To improve care for rare diseases we must draw on all the available knowledge, both from professional experts and patients, in order to improve care for every single patient in the world.
Patient experience and satisfaction have been demonstrated to be the single most important aspect in assessing the quality of healthcare [ 2 ], and has even been shown to be a predictor of survival rates [ 3 ]. Studies have evidenced that patient involvement in the design, evaluation and designation of healthcare services, improves the relevance and quality of the services, as well as improves their ability to meet patient needs [ 4 , 5 , 6 ]. Essentially, to be able to involve patients, the hurdles in communication and initial preconceptions between medical doctors and their patients need to be resolved [ 7 ].
To tackle the current hurdles in complex or rare diseases, European Reference Networks (ERN) have been implemented since March 2017. The goal of these networks is to connect experts across Europe, harnessing their collective experience and expertise, facilitating the knowledge to travel instead of the patient. ERN GENTURIS is the Network leading on genetic tumour risk syndromes (genturis), which are inherited disorders which strongly predispose to the development of tumours [ 8 ]. They share similar challenges: delay in diagnosis, lack of cancer prevention for patients and healthy relatives, and therapeutic. To overcome the hurdles every patient faces, ERN GENTURIS ( www.genturis.eu ) has developed an innovative visual approach for patient input into the Network, to share their expertise and experience: “Patient Journeys” (Fig. 1 ).
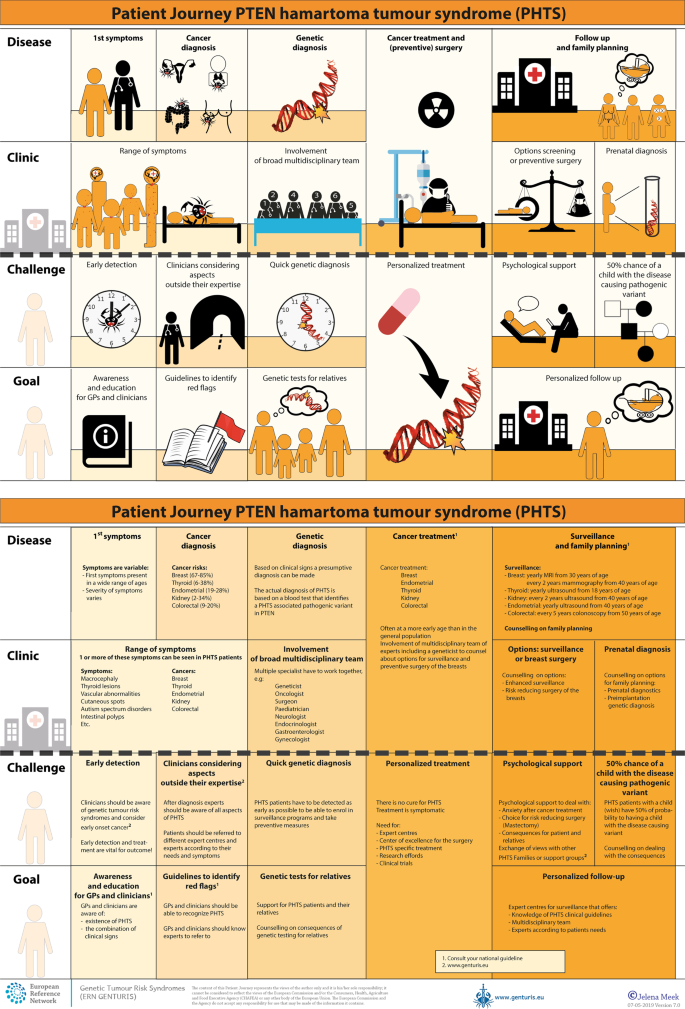
Example of a Patient Journey: PTEN Hamartoma Tumour Syndrome (also called Cowden Syndrome), including legend page ( www.genturis.eu )
The “Patient Journey” seeks to identify the needs that are common for all ‘ genturis syndromes ’, and those that are specific to individual syndromes. To achieve this, patient representatives completed a mapping exercise of the needs of each rare inherited syndrome they represent, across the different stages of the Patient Journey. The “Patient Journey” connects professional expert guidelines—with foreseen medical interventions, screening, treatment—with patient needs –both medical and psychological. Each “Patient Journey” is divided in several stages that are considered inherent to the specific disease. Each stage in the journey is referenced under three levels: clinical presentation, challenges and needs identified by patients, and their goal to improve care. The final Patient Journey is reviewed by both patients and professional experts. By visualizing this in a comprehensive manner, patients and their caregivers are able to discuss the individual needs of the patient, while keeping in mind the expertise of both professional and patient leads. Together they seek to achieve the same goal: improving care for every patient with a genetic tumour risk syndrome.
The Patient Journeys encourage experts to look into national guidelines. In addition, they identify a great need for evidence-based European guidelines, facilitating equal care to all rare patients. ERN GENTURIS has already developed Patient Journeys for the following rare diseases ( www.genturis.eu ):
PTEN hamartoma tumour syndrome (PHTS) (Fig. 1 )
Hereditary breast and ovarian cancer (HBOC)
Lynch syndrome
Neurofibromatosis Type 1
Neurofibromatosis Type 2
Schwannomatosis
A “Patient Journey” is a personal testimony that reflects the needs of patients in two key reference documents—an accessible visual overview, supported by a detailed information matrix. The journey shows in a comprehensive way the goals that are recognized by both patients and clinical experts. Therefore, it can be used by both these parties to explain the clinical pathway: professional experts can explain to newly identified patients how the clinical pathway generally looks like, whereas their patients can identify their specific needs within these pathways. Moreover, the Patient Journeys could serve as a guide for patients who may want to write, in collaboration with local clinicians, diaries of their journeys. Subsequently, these clinical diaries can be discussed with the clinician and patient representatives. Professionals coming across medical obstacles during the patient journey can contact professional experts in the ERN GENTURIS, while patients can contact the expert patient representatives from this ERN ( www.genturis.eu ). Finally, the “Patient Journeys” will be valuable in sharing knowledge with the clinical community as a whole.
Our aim is that medical doctors confronted with rare diseases, by using Patient Journeys, can also rely on the knowledge of the much broader community of expert professionals and expert patients.
Armstrong MJ, Mullins CD, Gronseth GS, Gagliardi AR. Recommendations for patient engagement in guideline development panels: a qualitative focus group study of guideline-naive patients. PloS ONE 2017;12:e0174329.
Article PubMed PubMed Central Google Scholar
Gupta D, Rodeghier M, Lis CG. Patient satisfaction with service quality as a predictor of survival outcomes in breast cancer. Supportive Care Cancer Off J Multinatl Assoc Supportive Care Cancer. 2014;22:129–34.
Google Scholar
Gupta D, Lis CG, Rodeghier M. Can patient experience with service quality predict survival in colorectal cancer? J Healthc Qual Off Publ Natl Assoc Healthc Qual. 2013;35:37–43.
Sharma AE, Knox M, Mleczko VL, Olayiwola JN. The impact of patient advisors on healthcare outcomes: a systematic review. BMC Health Serv Res. 2017;17:693.
Fonhus MS, Dalsbo TK, Johansen M, Fretheim A, Skirbekk H, Flottorp SA. Patient-mediated interventions to improve professional practice. Cochrane Database Syst Rev. 2018;9:Cd012472.
PubMed Google Scholar
Cornman DH, White CM. AHRQ methods for effective health care. Discerning the perception and impact of patients involved in evidence-based practice center key informant interviews. Rockville, MD: Agency for Healthcare Research and Quality (US); 2017.
Chalmers JD, Timothy A, Polverino E, Almagro M, Ruddy T, Powell P, et al. Patient participation in ERS guidelines and research projects: the EMBARC experience. Breathe (Sheff, Engl). 2017;13:194–207.
Article Google Scholar
Vos JR, Giepmans L, Rohl C, Geverink N, Hoogerbrugge N. Boosting care and knowledge about hereditary cancer: european reference network on genetic tumour risk syndromes. Fam Cancer 2019;18:281–4.
Article PubMed Google Scholar
Download references
Acknowledgements
This work is generated within the European Reference Network on Genetic Tumour Risk Syndromes – FPA No. 739547. The authors thank all ERN GENTURIS Members and patient representatives for their work on the Patient Journeys (see www.genturis.eu ).
Author information
Authors and affiliations.
SquareRootThinking and EURORDIS – Rare Diseases Europe, Paris, France
Matt Bolz-Johnson
Human Genetics, Radboud University Medical Center, Nijmegen, The Netherlands
Jelena Meek & Nicoline Hoogerbrugge
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Nicoline Hoogerbrugge .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Bolz-Johnson, M., Meek, J. & Hoogerbrugge, N. “Patient Journeys”: improving care by patient involvement. Eur J Hum Genet 28 , 141–143 (2020). https://doi.org/10.1038/s41431-019-0555-6
Download citation
Received : 07 August 2019
Revised : 04 October 2019
Accepted : 01 November 2019
Published : 04 December 2019
Issue Date : February 2020
DOI : https://doi.org/10.1038/s41431-019-0555-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Care trajectories of surgically treated patients with a prolactinoma: why did they opt for surgery.
- Victoria R. van Trigt
- Ingrid M. Zandbergen
- Nienke R. Biermasz
Pituitary (2023)
Designing rare disease care pathways in the Republic of Ireland: a co-operative model
- E. P. Treacy
Orphanet Journal of Rare Diseases (2022)
Rare disease education in Europe and beyond: time to act
- Birute Tumiene
- Harm Peters
- Gareth Baynam
Development of a patient journey map for people living with cervical dystonia
- Monika Benson
- Alberto Albanese
- Holm Graessner
Der klinische Versorgungspfad zur multiprofessionellen Versorgung seltener Erkrankungen in der Pädiatrie – Ergebnisse aus dem Projekt TRANSLATE-NAMSE
- Daniela Choukair
- Min Ae Lee-Kirsch
- Peter Burgard
Monatsschrift Kinderheilkunde (2022)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Search Menu
- Advance Articles
- Editor's Choice
- Supplements
- Patient Perspectives
- Methods Corner
- ESC Content Collections
- Author Guidelines
- Instructions for reviewers
- Submission Site
- Why publish with EJCN?
- Open Access Options
- Self-Archiving Policy
- Read & Publish
- About European Journal of Cardiovascular Nursing
- About ACNAP
- About European Society of Cardiology
- ESC Publications
- Editorial Board
- Advertising & Corporate Services
- War in Ukraine
- Journals on Oxford Academic
- Books on Oxford Academic
Article Contents
Introduction, why patient journey mapping, how is patient journey mapping conducted, use of technology in patient journey mapping, future implications for patient journey mapping, conclusions, patient journey mapping: emerging methods for understanding and improving patient experiences of health systems and services.
Lemma N Bulto and Ellen Davies Shared first authorship.
Conflict of interest: none declared.
- Article contents
- Figures & tables
- Supplementary Data
Lemma N Bulto, Ellen Davies, Janet Kelly, Jeroen M Hendriks, Patient journey mapping: emerging methods for understanding and improving patient experiences of health systems and services, European Journal of Cardiovascular Nursing , 2024;, zvae012, https://doi.org/10.1093/eurjcn/zvae012
- Permissions Icon Permissions
Patient journey mapping is an emerging field of research that uses various methods to map and report evidence relating to patient experiences and interactions with healthcare providers, services, and systems. This research often involves the development of visual, narrative, and descriptive maps or tables, which describe patient journeys and transitions into, through, and out of health services. This methods corner paper presents an overview of how patient journey mapping has been conducted within the health sector, providing cardiovascular examples. It introduces six key steps for conducting patient journey mapping and describes the opportunities and benefits of using patient journey mapping and future implications of using this approach.
Acquire an understanding of patient journey mapping and the methods and steps employed.
Examine practical and clinical examples in which patient journey mapping has been adopted in cardiac care to explore the perspectives and experiences of patients, family members, and healthcare professionals.
Quality and safety guidelines in healthcare services are increasingly encouraging and mandating engagement of patients, clients, and consumers in partnerships. 1 The aim of many of these partnerships is to consider how health services can be improved, in relation to accessibility, service delivery, discharge, and referral. 2 , 3 Patient journey mapping is a research approach increasingly being adopted to explore these experiences in healthcare. 3
a patient-oriented project that has been undertaken to better understand barriers, facilitators, experiences, interactions with services and/or outcomes for individuals and/or their carers, and family members as they enter, navigate, experience and exit one or more services in a health system by documenting elements of the journey to produce a visual or descriptive map. 3
It is an emerging field with a clear patient-centred focus, as opposed to studies that track patient flow, demand, and movement. As a general principle, patient journey mapping projects will provide evidence of patient perspectives and highlight experiences through the patient and consumer lens.
Patient journey mapping can provide significant insights that enable responsive and context-specific strategies for improving patient healthcare experiences and outcomes to be designed and implemented. 3–6 These improvements can occur at the individual patient, model of care, and/or health system level. As with other emerging methodologies, questions have been raised regarding exactly how patient journey mapping projects can best be designed, conducted, and reported. 3
In this methods paper, we provide an overview of patient journey mapping as an emergent field of research, including reasons that mapping patient journeys might be considered, methods that can be adopted, the principles that can guide patient journey mapping data collection and analysis, and considerations for reporting findings and recognizing the implications of findings. We summarize and draw on five cardiovascular patient journey mapping projects, as examples.
One of the most appealing elements of the patient journey mapping field of research is its focus on illuminating the lived experiences of patients and/or their family members, and the health professionals caring for them, methodically and purposefully. Patient journey mapping has an ability to provide detailed information about patient experiences, gaps in health services, and barriers and facilitators for access to health services. This information can be used independently, or alongside information from larger data sets, to adapt and improve models of care relevant to the population that is being investigated. 3
To date, the most frequent reason for adopting this approach is to inform health service redesign and improvement. 3 , 7 , 8 Other reasons have included: (i) to develop a deeper understanding of a person’s entire journey through health systems; 3 (ii) to identify delays in diagnosis or treatment (often described as bottlenecks); 9 (iii) to identify gaps in care and unmet needs; (iv) to evaluate continuity of care across health services and regions; 10 (v) to understand and evaluate the comprehensiveness of care; 11 (vi) to understand how people are navigating health systems and services; and (vii) to compare patient experiences with practice guidelines and standards of care.
Patient journey mapping approaches frequently use six broad steps that help facilitate the preparation and execution of research projects. These are outlined in the Central illustration . We acknowledge that not all patient journey mapping approaches will follow the order outlined in the Central illustration , but all steps need to be considered at some point throughout each project to ensure that research is undertaken rigorously, appropriately, and in alignment with best practice research principles.
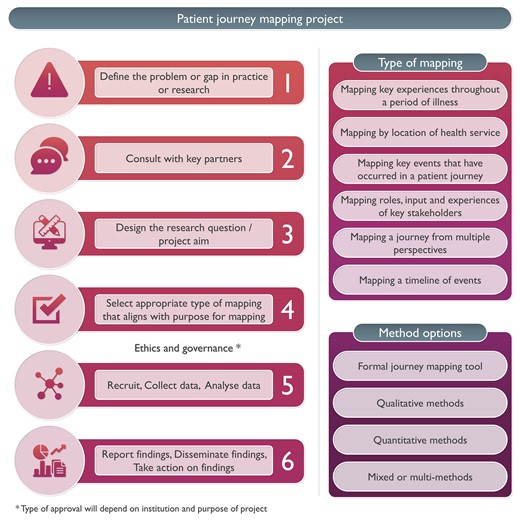
Steps for conducing patient journey mapping.
Five cardiovascular patient journey mapping research examples have been included in Figure 1 , 12–16 to provide specific context and illustrate these six steps. For each of these examples, the problem or gap in practice or research, consultation processes, research question or aim, type of mapping, methods, and reporting of findings have been extracted. Each of these steps is then discussed, using these cardiovascular examples.
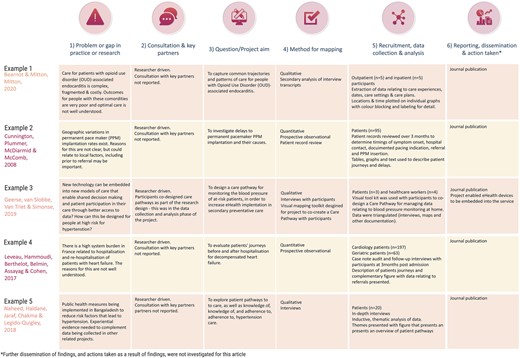
Examples of patient journey mapping projects.
Define the problem or gap in practice or research
Developing an understanding of a problem or gap in practice is essential for facilitating the design and development of quality research projects. In the examples outlined in Figure 1 , it is evident that clinical variation or system gaps have been explored using patient journey mapping. In the first two examples, populations known to have health vulnerabilities were explored—in Example 1, this related to comorbid substance use and physical illness, 13 and in Example 2, this related to geographical location. 13 Broader systems and societal gaps were explored in Examples 4 and 5, respectively, 15 , 16 and in Example 3, a new technologically driven solution for an existing model of care was tested for its ability to improve patient outcomes relating to hypertension. 14
Consultation, engagement, and partnership
Ideally, consultation with heathcare providers and/or patients would occur when the problem or gap in practice or research is being defined. This is a key principle of co-designed research. 17 Numerous existing frameworks for supporting patient involvement in research have been designed and were recently documented and explored in a systematic review by Greenhalgh et al . 18 While none of the five example studies included this step in the initial phase of the project, it is increasingly being undertaken in patient partnership projects internationally (e.g. in renal care). 17 If not in the project conceptualization phase, consultation may occur during the data collection or analysis phase, as demonstrated in Example 3, where a care pathway was co-created with participants. 14 We refer readers to Greenhalgh’s systematic review as a starting point for considering suitable frameworks for engaging participants in consultation, partnership, and co-design of patient journey mapping projects. 18
Design the research question/project aim
Conducting patient journey mapping research requires a thoughtful and systematic approach to adequately capture the complexity of the healthcare experience. First, the research objectives and questions should be clearly defined. Aspects of the patient journey that will be explored need to be identified. Then, a robust approach must be developed, taking into account whether qualitative, quantitative, or mixed methods are more appropriate for the objectives of the study.
For example, in the cardiac examples in Figure 1 , the broad aims included mapping existing pathways through health services where there were known problems 12 , 13 , 15 , 16 and documenting the co-creation of a new care pathway using quantitative, qualitative, or mixed methods. 14
In traditional studies, questions that might be addressed in the area of patient movement in health systems include data collected through the health systems databases, such as ‘What is the length of stay for x population’, or ‘What is the door to balloon time in this hospital?’ In contrast, patient mapping journey studies will approach asking questions about experiences that require data from patients and their family members, e.g. ‘What is the impact on you of your length of stay?’, ‘What was your experience in being assessed and undergoing treatment for your chest pain?’, ‘What was your experience supporting this patient during their cardiac admission and discharge?’
Select appropriate type of mapping
The methods chosen for mapping need to align with the identified purpose for mapping and the aim or question that was designed in Step 3. A range of research methods have been used in patient journey mapping projects involving various qualitative, quantitative, and mixed methods techniques and tools. 4 Some approaches use traditional forms of data collection, such as short-form and long-form patient interviews, focus groups, and direct patient observations. 18 , 19 Other approaches use patient journey mapping tools, designed and used with specific cultural groups, such as First Nations peoples using artwork, paintings, sand trays, and photovoice. 17 , 20 In the cardiovascular examples presented in Figure 1 , both qualitative and quantitative methods have been used, with interviews, patient record reviews, and observational techniques adopted to map patient journeys.
In a recent scoping review investigating patient journey mapping across all health care settings and specialities, six types of patient journey mapping were identified. 3 These included (i) mapping key experiences throughout a period of illness; (ii) mapping by location of health service; (iii) mapping by events that occurred throughout a period of illness; (iv) mapping roles, input, and experiences of key stakeholders throughout patient journeys; (v) mapping a journey from multiple perspectives; and (vi) mapping a timeline of events. 3 Combinations or variations of these may be used in cardiovascular settings in the future, depending on the research question, and the reasons mapping is being undertaken.
Recruit, collect data, and analyse data
The majority of health-focused patient journey mapping projects published to date have recruited <50 participants. 3 Projects with fewer participants tend to be qualitative in nature. In the cardiovascular examples provided in Figure 1 , participant numbers range from 7 14 to 260. 15 The 3 studies with <20 participants were qualitative, 12 , 14 , 16 and the 2 with 95 and 260 participants, respectively, were quantitative. 13 , 15 As seen in these and wider patient journey mapping examples, 3 participants may include patients, relatives, carers, healthcare professionals, or other stakeholders, as required, to meet the study objectives. These different participant perspectives may be analysed within each participant group and/or across the wider cohort to provide insights into experiences, and the contextual factors that shape these experiences.
The approach chosen for data collection and analysis will vary and depends on the research question. What differentiates data analysis in patient journey mapping studies from other qualitative or quantitative studies is the focus on describing, defining, or exploring the journey from a patient’s, rather than a health service, perspective. Dimensions that may, therefore, be highlighted in the analysis include timing of service access, duration of delays to service access, physical location of services relative to a patient’s home, comparison of care received vs. benchmarked care, placing focus on the patient perspective.
The mapping of individual patient journeys may take place during data collection with the use of mapping templates (tables, diagrams, and figures) and/or later in the analysis phase with the use of inductive or deductive analysis, mapping tables, or frameworks. These have been characterized and visually represented in a recent scoping review. 3 Representations of patient journeys can also be constructed through a secondary analysis of previously collected data. In these instances, qualitative data (i.e. interviews and focus group transcripts) have been re-analysed to understand whether a patient journey narrative can be extracted and reported. Undertaking these projects triggers a new research cycle involving the six steps outlined in the Central illustration . The difference in these instances is that the data are already collected for Step 5.
Report findings, disseminate findings, and take action on findings
A standardized, formal reporting guideline for patient journey mapping research does not currently exist. As argued in Davies et al ., 3 a dedicated reporting guide for patient journey mapping would be ill-advised, given the diversity of approaches and methods that have been adopted in this field. Our recommendation is for projects to be reported in accordance with formal guidelines that best align with the research methods that have been adopted. For example, COREQ may be used for patient journey mapping where qualitative methods have been used. 20 STROBE may be used for patient journey mapping where quantitative methods have been used. 21 Whichever methods have been adopted, reporting of projects should be transparent, rigorous, and contain enough detail to the extent that the principles of transparency, trustworthiness, and reproducibility are upheld. 3
Dissemination of research findings needs to include the research, healthcare, and broader communities. Dissemination methods may include academic publications, conference presentations, and communication with relevant stakeholders including healthcare professionals, policymakers, and patient advocacy groups. Based on the findings and identified insights, stakeholders can collaboratively design and implement interventions, programmes, or improvements in healthcare delivery that overcome the identified challenges directly and address and improve the overall patient experience. This cyclical process can hopefully produce research that not only informs but also leads to tangible improvements in healthcare practice and policy.
Patient journey mapping is typically a hands-on process, relying on surveys, interviews, and observational research. The technology that supports this research has, to date, included word processing software, and data analysis packages, such as NVivo, SPSS, and Stata. With the advent of more sophisticated technological tools, such as electronic health records, data analytics programmes, and patient tracking systems, healthcare providers and researchers can potentially use this technology to complement and enhance patient journey mapping research. 19 , 20 , 22 There are existing examples where technology has been harnessed in patient journey. Lee et al . used patient journey mapping to verify disease treatment data from the perspective of the patient, and then the authors developed a mobile prototype that organizes and visualizes personal health information according to the patient-centred journey map. They used a visualization approach for analysing medical information in personal health management and examined the medical information representation of seven mobile health apps that were used by patients and individuals. The apps provide easy access to patient health information; they primarily import data from the hospital database, without the need for patients to create their own medical records and information. 23
In another example, Wauben et al. 19 used radio frequency identification technology (a wireless system that is able to track a patient journey), as a component of their patient journey mapping project, to track surgical day care patients to increase patient flow, reduce wait times, and improve patient and staff satisfaction.
Patient journey mapping has emerged as a valuable research methodology in healthcare, providing a comprehensive and patient-centric approach to understanding the entire spectrum of a patient’s experience within the healthcare system. Future implications of this methodology are promising, particularly for transforming and redesigning healthcare delivery and improving patient outcomes. The impact may be most profound in the following key areas:
Personalized, patient-centred care : The methodology allows healthcare providers to gain deep insights into individual patient experiences. This information can be leveraged to deliver personalized, patient-centric care, based on the needs, values, and preferences of each patient, and aligned with guideline recommendations, healthcare professionals can tailor interventions and treatment plans to optimize patient and clinical outcomes.
Enhanced communication, collaboration, and co-design : Mapping patient interactions with health professionals and journeys within and across health services enables specific gaps in communication and collaboration to be highlighted and potentially informs responsive strategies for improvement. Ideally, these strategies would be co-designed with patients and health professionals, leading to improved care co-ordination and healthcare experience and outcomes.
Patient engagement and empowerment : When patients are invited to share their health journey experiences, and see visual or written representations of their journeys, they may come to understand their own health situation more deeply. Potentially, this may lead to increased health literacy, renewed adherence to treatment plans, and/or self-management of chronic conditions such as cardiovascular disease. Given these benefits, we recommend that patients be provided with the findings of research and quality improvement projects with which they are involved, to close the loop, and to ensure that the findings are appropriately disseminated.
Patient journey mapping is an emerging field of research. Methods used in patient journey mapping projects have varied quite significantly; however, there are common research processes that can be followed to produce high-quality, insightful, and valuable research outputs. Insights gained from patient journey mapping can facilitate the identification of areas for enhancement within healthcare systems and inform the design of patient-centric solutions that prioritize the quality of care and patient outcomes, and patient satisfaction. Using patient journey mapping research can enable healthcare providers to forge stronger patient–provider relationships and co-design improved health service quality, patient experiences, and outcomes.
None declared.
Farmer J , Bigby C , Davis H , Carlisle K , Kenny A , Huysmans R , et al. The state of health services partnering with consumers: evidence from an online survey of Australian health services . BMC Health Serv Res 2018 ; 18 : 628 .
Google Scholar
Kelly J , Dwyer J , Mackean T , O’Donnell K , Willis E . Coproducing Aboriginal patient journey mapping tools for improved quality and coordination of care . Aust J Prim Health 2017 ; 23 : 536 – 542 .
Davies EL , Bulto LN , Walsh A , Pollock D , Langton VM , Laing RE , et al. Reporting and conducting patient journey mapping research in healthcare: a scoping review . J Adv Nurs 2023 ; 79 : 83 – 100 .
Ly S , Runacres F , Poon P . Journey mapping as a novel approach to healthcare: a qualitative mixed methods study in palliative care . BMC Health Serv Res 2021 ; 21 : 915 .
Arias M , Rojas E , Aguirre S , Cornejo F , Munoz-Gama J , Sepúlveda M , et al. Mapping the patient’s journey in healthcare through process mining . Int J Environ Res Public Health 2020 ; 17 : 6586 .
Natale V , Pruette C , Gerohristodoulos K , Scheimann A , Allen L , Kim JM , et al. Journey mapping to improve patient-family experience and teamwork: applying a systems thinking tool to a pediatric ambulatory clinic . Qual Manag Health Care 2023 ; 32 : 61 – 64 .
Cherif E , Martin-Verdier E , Rochette C . Investigating the healthcare pathway through patients’ experience and profiles: implications for breast cancer healthcare providers . BMC Health Serv Res 2020 ; 20 : 735 .
Gilburt H , Drummond C , Sinclair J . Navigating the alcohol treatment pathway: a qualitative study from the service users’ perspective . Alcohol Alcohol 2015 ; 50 : 444 – 450 .
Gichuhi S , Kabiru J , M’Bongo Zindamoyen A , Rono H , Ollando E , Wachira J , et al. Delay along the care-seeking journey of patients with ocular surface squamous neoplasia in Kenya . BMC Health Serv Res 2017 ; 17 : 485 .
Borycki EM , Kushniruk AW , Wagner E , Kletke R . Patient journey mapping: integrating digital technologies into the journey . Knowl Manag E-Learn 2020 ; 12 : 521 – 535 .
Barton E , Freeman T , Baum F , Javanparast S , Lawless A . The feasibility and potential use of case-tracked client journeys in primary healthcare: a pilot study . BMJ Open 2019 ; 9 : e024419 .
Bearnot B , Mitton JA . “You’re always jumping through hoops”: journey mapping the care experiences of individuals with opioid use disorder-associated endocarditis . J Addict Med 2020 ; 14 : 494 – 501 .
Cunnington MS , Plummer CJ , McDiarmid AK , McComb JM . The patient journey from symptom onset to pacemaker implantation . QJM 2008 ; 101 : 955 – 960 .
Geerse C , van Slobbe C , van Triet E , Simonse L . Design of a care pathway for preventive blood pressure monitoring: qualitative study . JMIR Cardio 2019 ; 3 : e13048 .
Laveau F , Hammoudi N , Berthelot E , Belmin J , Assayag P , Cohen A , et al. Patient journey in decompensated heart failure: an analysis in departments of cardiology and geriatrics in the Greater Paris University Hospitals . Arch Cardiovasc Dis 2017 ; 110 : 42 – 50 .
Naheed A , Haldane V , Jafar TH , Chakma N , Legido-Quigley H . Patient pathways and perceptions of treatment, management, and control Bangladesh: a qualitative study . Patient Prefer Adherence 2018 ; 12 : 1437 – 1449 .
Bateman S , Arnold-Chamney M , Jesudason S , Lester R , McDonald S , O’Donnell K , et al. Real ways of working together: co-creating meaningful Aboriginal community consultations to advance kidney care . Aust N Z J Public Health 2022 ; 46 : 614 – 621 .
Greenhalgh T , Hinton L , Finlay T , Macfarlane A , Fahy N , Clyde B , et al. Frameworks for supporting patient and public involvement in research: systematic review and co-design pilot . Health Expect 2019 ; 22 : 785 – 801 .
Wauben LSGL , Guédon ACP , de Korne DF , van den Dobbelsteen JJ . Tracking surgical day care patients using RFID technology . BMJ Innov 2015 ; 1 : 59 – 66 .
Tong A , Sainsbury P , Craig J . Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups . Int J Qual Health Care 2007 ; 19 : 349 – 357 .
von Elm E , Altman DG , Egger M , Pocock SJ , Gøtzsche PC , Vandenbroucke JP , et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies . Lancet 2007 ; 370 (9596): 1453 – 1457 .
Wilson A , Mackean T , Withall L , Willis EM , Pearson O , Hayes C , et al. Protocols for an Aboriginal-led, multi-methods study of the role of Aboriginal and Torres Strait Islander health workers, practitioners and Liaison officers in quality acute health care . J Aust Indigenous HealthInfoNet 2022 ; 3 : 1 – 15 .
Lee B , Lee J , Cho Y , Shin Y , Oh C , Park H , et al. Visualisation of information using patient journey maps for a mobile health application . Appl Sci 2023 ; 13 : 6067 .
Author notes
Email alerts, citing articles via.
- Recommend to Your Librarian
- Advertising and Corporate Services
- Journals Career Network
Affiliations
- Online ISSN 1873-1953
- Print ISSN 1474-5151
- Copyright © 2024 European Society of Cardiology
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Process mapping the...
Process mapping the patient journey: an introduction
- Related content
- Peer review
- Timothy M Trebble , consultant gastroenterologist 1 ,
- Navjyot Hansi , CMT 2 1 ,
- Theresa Hydes , CMT 1 1 ,
- Melissa A Smith , specialist registrar 2 ,
- Marc Baker , senior faculty member 3
- 1 Department of Gastroenterology, Portsmouth Hospitals Trust, Portsmouth PO6 3LY
- 2 Department of Gastroenterology, Guy’s and St Thomas’ NHS Foundation Trust, London
- 3 Lean Enterprise Academy, Ross-on-Wye, Hertfordshire
- Correspondence to: T M Trebble tim.trebble{at}porthosp.nhs.uk
- Accepted 15 July 2010
Process mapping enables the reconfiguring of the patient journey from the patient’s perspective in order to improve quality of care and release resources. This paper provides a practical framework for using this versatile and simple technique in hospital.
Healthcare process mapping is a new and important form of clinical audit that examines how we manage the patient journey, using the patient’s perspective to identify problems and suggest improvements. 1 2 We outline the steps involved in mapping the patient’s journey, as we believe that a basic understanding of this versatile and simple technique, and when and how to use it, is valuable to clinicians who are developing clinical services.
What information does process mapping provide and what is it used for?
Process mapping allows us to “see” and understand the patient’s experience 3 by separating the management of a specific condition or treatment into a series of consecutive events or steps (activities, interventions, or staff interactions, for example). The sequence of these steps between two points (from admission to the accident and emergency department to discharge from the ward) can be viewed as a patient pathway or process of care. 4
Improving the patient pathway involves the coordination of multidisciplinary practice, aiming to maximise clinical efficacy and efficiency by eliminating ineffective and unnecessary care. 5 The data provided by process mapping can be used to redesign the patient pathway 4 6 to improve the quality or efficiency of clinical management and to alter the focus of care towards activities most valued by the patient.
Process mapping has shown clinical benefit across a variety of specialties, multidisciplinary teams, and healthcare systems. 7 8 9 The NHS Institute for Innovation and Improvement proposes a range of practical benefits using this approach (box 1). 6
Box 1 Benefits of process mapping 6
A starting point for an improvement project specific for your own place of work
Creating a culture of ownership, responsibility and accountability for your team
Illustrates a patient pathway or process, understanding it from a patient’s perspective
An aid to plan changes more effectively
Collecting ideas, often from staff who understand the system but who rarely contribute to change
An interactive event that engages staff
An end product (a process map) that is easy to understand and highly visual
Several management systems are available to support process mapping and pathway redesign. 10 11 A common technique, derived originally from the Japanese car maker Toyota, is known as lean thinking transformation. 3 12 This considers each step in a patient pathway in terms of the relative contribution towards the patient’s outcome, taken from the patient’s perspective: it improves the patient’s health, wellbeing, and experience (value adding) or it does not (non-value or “waste”) (box 2). 14 15 16
Box 2 The eight types of waste in health care 13
Defects —Drug prescription errors; incomplete surgical equipment
Overproduction —Inappropriate scheduling
Transportation —Distance between related departments
Waiting —By patients or staff
Inventory —Excess stores, that expire
Motion —Poor ergonomics
Overprocessing —A sledgehammer to crack a nut
Human potential —Not making the most of staff skills
Process mapping can be used to identify and characterise value and non-value steps in the patient pathway (also known as value stream mapping). Using lean thinking transformation to redesign the pathway aims to enhance the contribution of value steps and remove non-value steps. 17 In most processes, non-value steps account for nine times more effort than steps that add value. 18
Reviewing the patient journey is always beneficial, and therefore a process mapping exercise can be undertaken at any time. However, common indications include a need to improve patients’ satisfaction or quality or financial aspects of a particular clinical service.
How to organise a process mapping exercise
Process mapping requires a planned approach, as even apparently straightforward patient journeys can be complex, with many interdependent steps. 4 A process mapping exercise should be an enjoyable and creative experience for staff. In common with other audit techniques, it must avoid being confrontational or judgmental or used to “name, shame, and blame.” 8 19
Preparation and planning
A good first step is to form a team of four or five key staff, ideally including a member with previous experience of lean thinking transformation. The group should decide on a plan for the project and its scope; this can be visualised by using a flow diagram (fig 1 ⇓ ). Producing a rough initial draft of the patient journey can be useful for providing an overview of the exercise.
Fig 1 Steps involved in a process mapping exercise
- Download figure
- Open in new tab
- Download powerpoint
The medical literature or questionnaire studies of patients’ expectations and outcomes should be reviewed to identify value adding steps involved in the management of the clinical condition or intervention from the patient’s perspective. 1 3
Data collection
Data collection should include information on each step under routine clinical circumstances in the usual clinical environment. Information is needed on waiting episodes and bottlenecks (any step within the patient pathway that slows the overall rate of a patient’s progress, normally through reduced capacity or availability 20 ). Using estimates of minimum and maximum time for each step reduces the influence of day to day variations that may skew the data. Limiting the number of steps (to below 60) aids subsequent analysis.
The techniques used for data collection (table 1 ⇓ ) each have advantages and disadvantages; a combination of approaches can be applied, contributing different qualitative or quantitative information. The commonly used technique of walking the patient journey includes interviews with patients and staff and direct observation of the patient journey and clinical environment. It allows the investigator to “see” the patient journey at first hand. Involving junior (or student) doctors or nurses as interviewers may increase the openness of opinions from staff, and time needed for data collection can be reduced by allotting members of the team to investigate different stages in the patient’s journey.
Data collection in process mapping
- View inline
Mapping the information
The process map should comprehensively represent the patient journey. It is common practice to draw the map by hand onto paper (often several metres long), either directly or on repositionable notes (fig 2 ⇓ ).
Fig 2 Section of a current state map of the endoscopy patient journey
Information relating to the steps or representing movement of information (request forms, results, etc) can be added. It is useful to obtain any missing information at this stage, either from staff within the meeting or by revisiting the clinical environment.
Analysing the data and problem solving
The map can be analysed by using a series of simple questions (box 3). The additional information can be added to the process map for visual representation. This can be helped by producing a workflow diagram—a map of the clinical environment, including information on patient, staff, and information movement (fig 3 ⇓ ). 18
Box 3 How to analyse a process map 6
How many steps are involved?
How many staff-staff interactions (handoffs)?
What is the time for each step and between each step?
What is the total time between start and finish (lead time)?
When does a patient join a queue, and is it a regular occurrence?
How many non-value steps are there?
What do patients complain about?
What are the problems for staff?
Fig 3 Workflow diagram of current state endoscopy pathway
Redesigning the patient journey
Lean thinking transformation involves redesigning the patient journey. 21 22 This will eliminate, combine and simplify non-value steps, 23 limit the impact of rate limiting steps (such as bottlenecks), and emphasise the value adding steps, making the process more patient-centred. 6 It is often useful to trial the new pathway and review its effect on patient management and satisfaction before attempting more sustained implementation.
Worked example: How to undertake a process mapping exercise
South Coast NHS Trust, a large district general hospital, plans to improve patient access to local services by offering unsedated endoscopy in two peripheral units. A consultant gastroenterologist has been asked to lead a process mapping exercise of the current patient journey to develop a fast track, high quality patient pathway.
In the absence of local data, he reviews the published literature and identifies key factors to the patient experience that include levels of discomfort during the procedure, time to discuss the findings with the endoscopist, and time spent waiting. 24 25 26 27 He recruits a team: an experienced performance manager, a sister from the endoscopy department, and two junior doctors.
The team drafts a map of the current endoscopy journey, using repositionable notes on the wall. This allows team members to identify the start (admission to the unit) and completion (discharge) points and the locations thought to be involved in the patient journey.
They decide to use a “walk the journey” format, interviewing staff in their clinical environments and allowing direct observation of the patient’s management.
The junior doctors visit the endoscopy unit over two days, building up rapport with the staff to ensure that they feel comfortable with being observed and interviewed (on a semistructured but informal basis). On each day they start at the point of admission at the reception office and follow the patient journey to completion.
They observe the process from staff and patient’s perspectives, sitting in on the booking process and the endoscopy procedure. They identify the sequence of steps and assess each for its duration (minimum and maximum times) and the factors that influence this. For some of the steps, they use a digital watch and notepad to check and record times. They also note staff-patient and staff-staff interactions and their function, and the recording and movement of relevant information.
Details for each step are entered into a simple table (table 2 ⇓ ), with relevant notes and symbols for bottlenecks and patients’ waits.
Patient journey for non-sedated upper gastrointestinal endoscopy
When data collection is complete, the doctor organises a meeting with the team. The individual steps of the patient journey are mapped on a single long section of paper with coloured temporary markers (fig 2 ⇑ ); additional information is added in different colours. A workflow diagram is drawn to show the physical route of the patient journey (fig 3 ⇑ ).
The performance manager calculates that the total patient journey takes a minimum of 50 minutes to a maximum of 345 minutes. This variation mainly reflects waiting times before a number of bottleneck steps.
Only five steps (14 to 17 and 22, table 2 ⇑ ) are considered both to add value and needed on the day of the procedure (providing patient information and consent can be obtained before the patient attends the department). These represent from 13 to 47 minutes. At its least efficient, therefore, only 4% of the patient journey (13 of 345 minutes) is spent in activities that contribute directly towards the patient’s outcome.
The team redesigns the patient journey (fig 4 ⇓ ) to increase time spent on value adding aspects but reduce waiting times, bottlenecks, and travelling distances. For example, time for discussing the results of the procedure is increased but the location is moved from the end of the journey (a bottleneck) to shortly after the procedure in the anteroom, reducing the patient’s waiting time and staff’s travelling distances.
Fig 4 Workflow diagram of future state endoscopy pathway
Implementing changes and sustaining improvements
The endoscopy staff are consulted on the new patient pathway, which is then piloted. After successful review two months later, including a patient satisfaction questionnaire, the new patient pathway is formally adopted in the peripheral units.
Further reading
Practical applications.
NHS Institute for Innovation and Improvement ( https://www.institute.nhs.uk )—comprehensive online resource providing practical guidance on process mapping and service improvement
Lean Enterprise Academy ( http://www.leanuk.org )—independent body dedicated to lean thinking in industry and healthcare, through training and academic discussion; its publication, Making Hospitals Work 23 is a practical guide to lean transformation in the hospital environment
Manufacturing Institute ( http://www.manufacturinginstitute.co.uk )—undertakes courses on process mapping and lean thinking transformation within health care and industrial practice
Theoretical basis
Bircheno J. The new lean toolbox . 4th ed. Buckingham: PICSIE Books, 2008
Mould G, Bowers J, Ghattas M. The evolution of the pathway and its role in improving patient care. Qual Saf Health Care 2010 [online publication 29 April]
Layton A, Moss F, Morgan G. Mapping out the patient’s journey: experiences of developing pathways of care. Qual Health Care 1998; 7 (suppl):S30-6
Graban M. Lean hospitals, improving quality, patient safety and employee satisfaction . New York: Taylor & Francis, 2009
Womack JP, Jones DT. Lean thinking . 2nd ed. London: Simon & Schuster, 2003
Cite this as: BMJ 2010;341:c4078
Contributors: TMT designed the protocol and drafted the manuscript; TMT, MB, JH, and TH collected and analysed the data; all authors critically reviewed and contributed towards revision and production of the manuscript. TMT is guarantor.
Competing interests: MB is a senior faculty member carrying out research for the Lean Enterprise Academy and undertakes paid consultancies both individually and from Lean Enterprise Academy, and training fees for providing lean thinking in healthcare.
Provenance and peer review: Not commissioned; externally peer reviewed.
- ↵ Kollberg B, Dahlgaard JJ, Brehmer P. Measuring lean initiatives in health care services: issues and findings. Int J Productivity Perform Manage 2007 ; 56 : 7 -24. OpenUrl CrossRef
- ↵ Bevan H, Lendon R. Improving performance by improving processes and systems. In: Walburg J, Bevan H, Wilderspin J, Lemmens K, eds. Performance management in health care. Abingdon: Routeledge, 2006:75-85.
- ↵ Kim CS, Spahlinger DA, Kin JM, Billi JE. Lean health care: what can hospitals learn from a world-class automaker? J Hosp Med 2006 ; 1 : 191 -9. OpenUrl CrossRef PubMed
- ↵ Layton A, Moss F, Morgan G. Mapping out the patient’s journey: experiences of developing pathways of care. Qual Health Care 1998 ; 7 (suppl): S30 -6. OpenUrl
- ↵ Peterson KM, Kane DP. Beyond disease management: population-based health management. Disease management. Chicago: American Hospital Publishing, 1996.
- ↵ NHS Modernisation Agency. Process mapping, analysis and redesign. London: Department of Health, 2005;1-40.
- ↵ Taylor AJ, Randall C. Process mapping: enhancing the implementation of the Liverpool care pathway. Int J Palliat Nurs 2007 ; 13 : 163 -7. OpenUrl PubMed
- ↵ Ben-Tovim DI, Dougherty ML, O’Connell TJ, McGrath KM. Patient journeys: the process of clinical redesign. Med J Aust 2008 ; 188 (suppl 6): S14 -7. OpenUrl PubMed Web of Science
- ↵ King DL, Ben-Tovim DI, Bassham J. Redesigning emergency department patient flows: application of lean thinking to health care. Emerg Med Australas 2006 ; 18 : 391 -7. OpenUrl CrossRef PubMed
- ↵ Mould G, Bowers J, Ghattas M. The evolution of the pathway and its role in improving patient care. Qual Saf Health Care 2010 ; published online 29 April.
- ↵ Rath F. Tools for developing a quality management program: proactive tools (process mapping, value stream mapping, fault tree analysis, and failure mode and effects analysis). Int J Radiat Oncol Biol Phys 2008 ; 71 (suppl): S187 -90. OpenUrl PubMed Web of Science
- ↵ Womack JP, Jones DT. Lean thinking. 2nd ed. London: Simon & Schuster, 2003.
- ↵ Graban M. Value and waste. In: Lean hospitals. New York: Taylor & Francis, 2009;35-56.
- ↵ Westwood N, James-Moore M, Cooke M. Going lean in the NHS. London: NHS Institute for Innovation and Improvement, 2007.
- ↵ Liker JK. The heart of the Toyota production system: eliminating waste. The Toyota way. New York: McGraw-Hill, 2004;27-34.
- ↵ Womack JP, Jones DT. Introduction: Lean thinking versus Muda. In: Lean thinking. 2nd ed. London: Simon & Schuster, 2003:15-28.
- ↵ George ML, Rowlands D, Price M, Maxey J. Value stream mapping and process flow tools. Lean six sigma pocket toolbook. New York: McGraw Hill, 2005:33-54.
- ↵ Fillingham D. Can lean save lives. Leadership Health Serv 2007 ; 20 : 231 -41. OpenUrl CrossRef
- ↵ Benjamin A. Audit: how to do it in practice. BMJ 2008 ; 336 : 1241 -5. OpenUrl FREE Full Text
- ↵ Vissers J. Unit Logistics. In: Vissers J, Beech R, eds. Health operations management patient flow logistics in health care. Oxford: Routledge, 2005:51-69.
- ↵ Graban M. Overview of lean for hospital. Lean hospitals. New York: Taylor & Francis, 2009;19-33.
- ↵ Eaton M. The key lean concepts. Lean for practitioners. Penryn, Cornwall: Academy Press, 2008:13-28.
- ↵ Baker M, Taylor I, Mitchell A. Analysing the situation: learning to think differently. In: Making hospitals work. Ross-on-Wye: Lean Enterprise Academy, 2009:51-70.
- ↵ Ko HH, Zhang H, Telford JJ, Enns R. Factors influencing patient satisfaction when undergoing endoscopic procedures. Gastrointest Endosc 2009 ; 69 : 883 -91. OpenUrl CrossRef PubMed Web of Science
- ↵ Del Rio AS, Baudet JS, Fernandez OA, Morales I, Socas MR. Evaluation of patient satisfaction in gastrointestinal endoscopy. Eur J Gastroenterol Hepatol 2007 ; 19 : 896 -900. OpenUrl CrossRef PubMed Web of Science
- ↵ Seip B, Huppertz-Hauss G, Sauar J, Bretthauer M, Hoff G. Patients’ satisfaction: an important factor in quality control of gastroscopies. Scand J Gastroenterol 2008 ; 43 : 1004 -11. OpenUrl CrossRef PubMed Web of Science
- ↵ Yanai H, Schushan-Eisen I, Neuman S, Novis B. Patient satisfaction with endoscopy measurement and assessment. Dig Dis 2008 ; 26 : 75 -9. OpenUrl CrossRef PubMed Web of Science
Patient Journey Mapping: What it is and Why it Matters

How can healthcare organizations make every stage of the patient journey better?
How was your last experience in a healthcare facility? Think about every step of that patient care journey - the phone calls, in person meetings, wait times, communication and all of the healthcare professional/ patient interactions. It’s a lot.
Healthcare organizations are working diligently to improve patient satisfaction and quality of care by asking, “How can we make the patient experience better?” But that’s no mean feat, trying to capture the multitude of challenges patients face when navigating a healthcare journey. That makes improving it even more difficult.
A first, fundamental step to improving patient experience is understanding what that experience looks like today. This is where patient journey mapping comes into play. You can use patient journey maps to understand the highs and lows, pain points and gaps to begin pinpointing which interventions will be most impactful. Then you can assess which changes you have the power to make.
As a result, you’ll be better able to manage your patient’s journey, improve care pathways and meet—and exceed—patient expectations, needs, and wants.
What is Patient Journey Mapping?
Patient journey mapping works to identify and understand the details of all patient touchpoints within a specific healthcare experience. It helps you visualize the process patients go through to receive care, complete a treatment plan, and/or reach a desired outcome. When done correctly, patient journey maps make it easier for you to identify pain points, discover opportunities and re-align treatment and care approaches across the entire healthcare system.
What makes up a patient’s journey?
A patient’s journey represents the entire sequence of events or touchpoints that a patient experiences within a given health system, with a specific provider, or within a specific facility. These touchpoints are either virtual or in-person. They range from the mundane to the nerve-wracking or life-changing. They comprise events from scheduling an appointment online to reviewing post-surgery instructions with a doctor.
It’s key for healthcare professionals and clinicians to recognize the patient journey extends well beyond the most obvious in-person interactions at a treatment facility. The patient journey happens before, during and after a healthcare service: pre-visit, during-visit, and post-visit. These include but are not limited to:
- Finding the right service or practitioner
- Scheduling an appointment
- Submitting a list of current medications
- Arriving at the medical facility
- Identifying where to check-in.
These experiences can instil a sense of reassurance or unease before a patient even receives care. In essence, they set the tone and expectations for the physical visit. A frustrating or confusing experience during the pre-visit stage will impact the emotional state of the patient and family for the rest of their interactions.
During-visit
- Checking in at the front desk
- Waiting in the lobby to be called
- Discussion with nurses before speaking to a doctor
- Family waiting for updates in the lobby during a procedure
- Care from doctor and staff.
There are an infinite number of touchpoints during the delivery of healthcare. Each one will have a different level of impact on the patient’s experience.
- Post-care instructions at hospital
- Hospital discharge process
- Completing a patient feedback survey
- Paying for the medical treatment
- Post-surgery calls or online messages from the nurse or doctor.
The patient experience after a hospital visit plays a vital role in either reinforcing a positive experience or mitigating a negative one. Actions such as post-appointment follow-ups extend the care relationship and may help the likelihood of the patient sticking to the treatment plan
All these individual touchpoints are crucial to understand. Altogether, these positive and negative experiences — no matter how big or small — comprise the patient journey.
Who are the stakeholders?
The healthcare ecosystem is complex, involving multiple stakeholders and a wide range of internal and external factors, including:
- People (patients, their families and caregivers, doctors, nurses, administration, parking attendants, volunteers)
- Technology and systems (online registration, parking tickets, surgery updates, mobile app, website, social media)
- Facilities (hospital campus navigation, parking availability, building accessibility).
Investigation of all players and systems involved is essential to seeing the multidimensional layers impacting the experience. To do this, patient journey maps should include the perspectives of patients, providers, and staff - and those perspectives must be of the same journey. Often, an interaction that occurs from one point of view will show only one reality. However, further investigation will show the many contributing factors across the care delivery process. This is only apparent by examining multiple perspectives.
Once you understand the entire journey, with pain points, you’ll be able to identify patterns across patient personas and different demographics, and any gaps within the healthcare process. You can then begin asking important questions like:
- Which moments are most painful?
- Why do they happen?
- What must we change in order to improve the experience?
- Who must we impact?
- Which do we have the power to change?
Benefits of patient journey mapping
Patient journey mapping provides the opportunity to turn the healthcare experience from a primarily reactive experience to a proactive one. By building out care journeys for your patients, you can close any gaps in provision and establish robust preventative routines that ultimately help your patients stay healthier for as long as possible. Engaging consumers and patients based on where they are and what they want, builds trust and confidence. That retains patients in your system and encourages them to make friends and family referrals.
But how does the process work?
- Streamline patient processes and workflows: upgrading the usability and functionality of online patient portals, websites and mobile apps can put more control in the patients’ hands, increasing patient flow and cutting operational expenses.
- Increase staff efficiency : enhancing internal online tools and creating automation within systems can assist hospital staff in implementing protocols and schedules and help them anticipate and solve problems more easily. It can help to align the expected service delivery with the actual one.
- Clear routes and direction across medical facilities: hospitals can be incredibly complicated to navigate - whether it’s using the right entrance, finding parking or making your way to the cafeteria for a snack. Improving signage, making visible pathways, and using landmarks to help orient users can help patients and families readily access the resources they need.
- Improve communication between patients and providers: exchanging patient information and coordinating care can be a challenge for providers and a frustration for patients. This misalignment can be due to silos within organizations, incompatible technology systems or many other factors. Working to bridge the appropriate organizational or technological gap can help alleviate stress and anxiety.
- Develop seamless and timely patient and family updates: waiting while a family member is in surgery or communicating with a doctor to secure care for a child is typically an extremely stressful process. Families wait anxiously for updates which can be infrequent and lacking detail. Implementing a seamless system for families to communicate directly and receive regular updates, through an app or text, can help ease these pain points.
- Better ‘in-between visit’ care and check-ins with patients and families: communication between patients, including families and caregivers and providers can feel ‘hit or miss.’ Patients may be scrambling to answer phone calls or missing phone calls only to find themselves unable to get hold of the provider when they call back. Alternatively, providers are challenged to communicate critical information to a wide range of patients. Establishing better communication systems can improve patient engagement, build the patient’s confidence in the care they receive, and ease the care provider’s job.
In short, we’re talking happier patients who experience better communication and levels of empathy at every stage of the patient journey.
What tools and methods are used for creating a patient journey map in healthcare?
There are many ways to undertake patient journey mapping, but doing it well isn’t always as simple as it may seem. It’s not a single exercise, moving from A to B. It’s more complex, involving a series of tools.
Our team at Highland has helped a lot of our clients create their first journey map . Grab a bunch of sticky notes and pens to start your map. Our process tends to go like this:
- Chart the course -work out what you want to achieve (your goal); determine whose journey you’re mapping, the start and end points; create the persona(s); think about what the stages of the journey may be.
- Prepare to interview - list your potential questions being mindful that you want the interviewee to recount events rather than share opinions. Schedule interviews with a tool like Calendly. Look into other available data (such as patient feedback).
- Interviews and coding - we interview in pairs so that one can speak whilst the other takes notes. With permission, record the interviews. Afterwards, code the responses according to thoughts, actions, experience etc. We use a simple Google Sheet to do this.
- Building blocks - go through the interviews and notes. Start mapping. Use a specific color of sticky note for each Building Block and add points to the wall in their themes.
- Identify opportunities - “mine” the wall for opportunities, presenting ideas to the team. Together, prioritise the top three or four to tackle.
Repeat this whole process with another persona or goal to examine.
Explore this journey mapping process in more detail
The outcome of this process should be that healthcare professionals can look after patients better. Using patient data collection to underpin your decision-making can transform your organization’s culture to one of continuous improvement. By referring constantly to patient data, you can identify the key areas to amend and improve to better the patient experience. Satisfied customers, those who’ve experienced a near seamless patient journey, will rate your facility highly and they’ll be more likely to generate new referrals.
Improve your customer experience with Highland Solutions’ help
You may know your healthcare facility like the back of your hand, but you only know it from your informed perspective. Getting a 360º view of the patient experience is the first step to improving it. A huge challenge for healthcare leaders like you is to recognize, understand and address the fact that the overall experience is created by the cumulative interactions across the various touchpoints in the healthcare journey: pre-visit, during-visit, and post-visit.
Despite years of expertise, it’s easy for healthcare providers and leaders to develop blind spots for persistent issues in the care process. Partnering with a knowledgeable research team to conduct patient journey mapping will bring expertise and a fresh perspective to your quality of care. It’s not only about uncovering in-depth insights via patient journey maps, but also translating them into actionable strategies to help you bridge any gaps between current and emerging patient needs and the present state of your healthcare organization.
Once on the right track, you’ll be enabled to manage and grow relationships at every stage of the patient journey. The more patient-centric you become, the better experience you build, reaching a higher quality of patient care, patient retention and loyalty, and improved health outcomes and overall well-being.
Get in touch to find out more about how we can help you with patient journey mapping
“Working with Highland is a really powerful experience for a company to be able to gain insights. To have real conversations with patients unlocks new pathways, ones that may be uncomfortable and uncover change, but they empower you to move forward in a way that feels really constructive.”
Chris Whitworth, Vice President, Treatment
Download “The Essential Guide to Launching a Digital Product for Experts & Expert Firms”

- Patients as Partners
The Patient’s Journey Through the Health System
By Cristina Vaz de Almeida, PhD
Although the concept of “service experience” was defined as “a subjective state of consciousness with a variety of symbolic meanings, hedonic responses and aesthetic criteria,” the concept now represents the human experience (Holbrook & Hirschman, 1982). In a broader concept, the patient experience integrates the sum of all interactions of patients, families, and care partners with the healthcare workforce, driven by cultures that support a healthcare ecosystem across the care continuum within communities (Wolf et al., 2014). This experience extends to all health organizations, whether primary care, hospital, private, or public organizations.
If health literacy promotes good system navigability in the dimensions of access, understanding, and use of health services and information (Sørensen et al., 2012), it is then necessary to list the problems, difficulties, required changes, and consequent improvements to make in a patient’s navigation through the complex health system.
Some of the points listed in health units’ user satisfaction questionnaires (Ferreira et al., 2017) reveal that patients complain about usually waiting a long time for their consultation. If they are in a private health organization, it may happen that patients are jumping from room to room, as if they were in a board game. Whether by phone, virtually, or in person, patients must give explanations to several people until they reach a healthcare professional. And when they are with the professional, usually the focus is on the current problem and not on the entirety of the patient’s well-being. Then the patient takes the reverse route, to either pay or get results … and the path unfolds in multiple stops.
Specific configurations and design elements may differ throughout the service continuum, but the objectives of safety, efficiency, satisfaction, and high-quality service remain constant. Therefore, the first step must be to listen to the patient and integrate them, at minimum, in the preparatory processes of reflection on change.
This change, whether in the area of human interactions, in processes and flows, or in physical characteristics (spaces/environments) should revolve around the perceived satisfaction of the patient, because it is they who will essentially use the services. However, pleasant spaces, simplified and standardized flows, and kind, assertive, clear, and positive people benefit everyone, including health professionals (Vaz de Almeida, 2016, 2019; Vaz de Almeida & Belim, 2021a, 2021b). Regarding investment in spaces for people with dementia, for example, Hopkins and colleagues (2017) showed that there is some evidence to suggest that residents with dementia in nursing homes sleep better when exposed to high levels of blue light.
Figure 1. The Service Experience
The patient is rational and emotional, so all their surroundings need to be integrated according to the patient’s sensory organs. Thus, it is important to see the healthcare journey through the patient’s eyes: their observations, emotions, and feelings; the usual route they take for services (outpatient clinic, urgent care, hospitalization, specialty care, etc.); the sensory qualities of each space and the equipment available for use. It is this sensory walk that allows the work of cognition with emotion (Damásio, 2020) and that allows an organization to provide a unique, satisfying, and memorable experience for the patient (Figure 1).
If we take into account the Weick model (1979) and its adaptation of the theory of sociocultural evolution (description of the processes by which people adapt to changes in their social and cultural relations to survive), we can observe the three phases that delimit the communication process such as regulation, selection, and retention (Kreps, 2009). Retention processes are essential in taking into account the patient’s feelings and emotions, and are used to preserve what was learned in the processes of regulation and selection, creating a set of experiences about what resulted and did not result. This critical analysis guides future research and selection within healthcare (Kreps, 2009).
Ike et al. (2019) focus on the use of the arts as a new way to boost engagement and promote health communication and health literacy. Engaging with the arts allows health professionals to improve their clinical competence, promote well-being, and prevent burnout.
Also, according to Global Guide: City Friendly to the Elderly (World Health Organization, 2008), “the interpersonal dimension of communication is very important, and it should be emphasized that the best way to be informed is to remain active and involved in the community.”
If we understand that one of the “root” problems is that many patients lack a perfect understanding of how to follow up on the instructions given by health professionals, we can understand what is happening in the mind of a person with low health literacy.
If, as Damásio (2020) states, the representations of images and objects of the external world provoke a certain image in the mind that may or may not be perceived, we understand that when there is no such representation, no image is recorded or understood. When patients hear technical jargon that they do not understand, there is no representation of image and correct information in their mind. They either do not understand or mistranslate what has been transmitted to them.
We know (Espanha et al., 2016) that vulnerable patients with low health literacy need an increased effort from health systems and professionals to achieve a more positive and effective experience when navigating the health system. These patients are in need of enlightening information to understand their health, deal with risk factors, and recognize the importance of social determinants. Therefore, it is necessary to create specific strategies for each of these patient profiles throughout their life cycle (see Table 1).
Table 1. List of Profiles With Low Health Literacy and Difficulty in Understanding Technical Health Instructions
In this constant challenge for organizations, they need to understand the experience of their patients, not only at singular points of contact but throughout the patient’s journey.
Experiencing directly through the eyes of patients is one of the ways to identify areas for improvement and create new value. See Table 2 for some questions to ask the patient to improve your understanding of their experience:
Table 2. Questions to Assess the Patient’s Journey
Using these patient responses, it is possible to solve the problem through small steps that lead to an improvement in the patient’s journey. See Table 3 for some areas you can invest in to improve the patient experience.
Table 3. Investing in the System to Improve the Patient Journey
It is necessary to create teams and working groups to evaluate patients’ journey both in the health organization and in the related social organizations and community structures that interact with the healthcare system. By doing so, we can recover a value that all patients seek: quality and perceived satisfaction in the health system that leads to better outcomes and an increase in the health literacy of organizations and society as a whole.
Cristina Vaz de Almeida, PhD, is director of postgraduate health literacy at ISPA in Portugal.
Damásio, A. (2020). Feeling & Knowing – Making Minds Conscious. Temas e Debates.
Espanha, R., Ávila, P., & Mendes, R. M. (2016). Literacia em saúde em Portugal [Health literacy in Portugal]. Calouste Gulbenkian Foundation.
Ferreira, P. L., Raposo, V. M., & Pisco, L. (2017). A voz dos utilizadores dos cuidados de saúde primários da região de Lisboa e Vale do Tejo [The voice of primary health care users in the Lisbon and Tagus Valley region], Portugal. Ciência & Sa úde Coletiva , 22 (3), 747–758. https://doi.org/10.1590/1413-81232017223.33252016
Holbrook, M. B., & Hirschman, E. C. (1982). The experiential aspects of consumption: Consumer fantasies, feelings, and fun. Journal of Consumer Research, 9 (2), 132. https://doi.org/10.1086/208906
Hopkins, S., Morgan, P. L., Schlangen, L. J. M., Williams, P., Skene, D. J., & Middleton, B. (2017). Blue-enriched lighting for older people living in care homes: Effect on activity, actigraphic sleep, mood and alertness. Current Alzheimer Research, 14( 10), 1053–1062. https://doi.org/10.2174/1567205014666170608091119
Ike, J. D., Postlethwait, R., & Parker, R. (2019). Nurturing context: TRACE, the arts, medical practice, and health literacy. Information Services & Use, 39, 93–104. https://doi.org/10.3233/ISU-180040
Kreps, G. L. (2009). Applying Weick’s model of organizing to health care and health promotion: Highlighting the central role of health communication. Patient Education & Counseling , 74 (3), 347–355. https://doi.org/10.1016/j.pec.2008.12.002
Sørensen, K., Van den Broucke, S., Fullam, J., Doyle, G., Pelikan, J., Slonska, Z., & Brand, H. (2012). Health Literacy and public health: A systematic review and integration of definitions and models. BMC Public health , 12( 80,) 1-13.
Vaz de Almeida, C. (2016). Literacia em saúde: Os caminhos para uma maior capacitação dos profissionais de saúde [Health literacy: The paths to greater training of health professionals]. Congress of the Scientific Association of Nurses (ACE). Enformação Magazine , Supplement (July 2016), 8–15. https://www.acenfermeiros.pt//files/upload/revistas/suplemento-congace.pdf
Vaz de Almeida, C. (2019). Modelo de comunicação em saúde – ACP [Health communication model – ACP]. Enformação Magazine, 10 , 20–22. https://issuu.com/ace-enfermeiros/docs/10__revista_ace.pdf_1
Vaz de Almeida, C., & Belim, C. (2021a). Health professionals’ communication competences as a light on the patient pathway: The Assertiveness, Clarity, and Positivity (ACP) model. International Journal of Applied Research on Public Health Management, 6 (1), 14–29. https://doi.org/10.4018/IJARPHM.2021010102
Vaz de Almeida, C., & Belim, C. (2021b). Health professionals’ communication competences decide patients’ health: Proposal of a communication model. In A. Tkalac Verčič, R. Tench, & S. Einwiller (Eds.), Joy: Using strategic communication to improve well-being and organizational success, Vol. 5 (Chapter 12). Emerald Publishing. https://books.emeraldinsight.com/page/detail/Joy/?k=9781800432413
Weick, K. E. (1979). The social psychology of organizing. Addison-Wesley.
Wolf, J. A., Niederhauser, V., Marshburn, D., & LaVela, S. L. (2014). Defining patient experience. Patient Experience Journal , 1 (1).
https://pxjournal.org/journal/vol1/iss1/3
World Health Organization. (2008). Guia global: Cidade amiga do idoso [Global guide: City friendly to the elderly]. Organização Mundial da Saúde. https://www.who.int/ageing/GuiaAFCPortuguese.pdf
Be the Expert! Share this:
Root out friction in every digital experience, super-charge conversion rates, and optimize digital self-service
Uncover insights from any interaction, deliver AI-powered agent coaching, and reduce cost to serve
Increase revenue and loyalty with real-time insights and recommendations delivered to teams on the ground
Know how your people feel and empower managers to improve employee engagement, productivity, and retention
Take action in the moments that matter most along the employee journey and drive bottom line growth
Whatever they’re are saying, wherever they’re saying it, know exactly what’s going on with your people
Get faster, richer insights with qual and quant tools that make powerful market research available to everyone
Run concept tests, pricing studies, prototyping + more with fast, powerful studies designed by UX research experts
Track your brand performance 24/7 and act quickly to respond to opportunities and challenges in your market
Explore the platform powering Experience Management
- Free Account
- For Digital
- For Customer Care
- For Human Resources
- For Researchers
- Financial Services
- All Industries
Popular Use Cases
- Customer Experience
- Employee Experience
- Employee Exit Interviews
- Net Promoter Score
- Voice of Customer
- Customer Success Hub
- Product Documentation
- Training & Certification
- XM Institute
- Popular Resources
- Customer Stories
- Market Research
- Artificial Intelligence
- Partnerships
- Marketplace
The annual gathering of the experience leaders at the world’s iconic brands building breakthrough business results, live in Salt Lake City.
- English/AU & NZ
- Español/Europa
- Español/América Latina
- Português Brasileiro
- REQUEST DEMO
- Experience Management
- Sector Specific
- Patient Experience
- Patient Journey Mapping
Try Qualtrics for free
Your complete guide to patient journey mapping.
15 min read Healthcare organizations can increase patient retention and improve patient satisfaction with patient journey mapping. Discover how to create a patient journey map and how you can use it to improve your organization’s bottom line.
What is the patient journey?
The patient journey is the sequence of events that begins when a patient first develops a need for care. Rather than focusing on service delivery, the patient journey encompasses all touchpoints of a patient’s healthcare experience–from locating healthcare providers and scheduling appointments, to paying the bill and continuing their care after treatment.
Examining the patient journey is essential to improving the patient experience. Not all interactions a patient has with your organization are weighted the same. Gathering patient feedback and understanding perceptions all along the patient journey can help you to identify moments of truth : the touchpoints that have the biggest impact on patient loyalty.
Download eBook: The 3 steps to driving human-centered healthcare experiences
The patient journey vs. the patient experience
Unlike traditional patient experience measurement, the patient journey looks not only at service delivery but also at the steps the patient takes before and after they engage directly with your organization. It recognizes that patient interactions with a healthcare system go well beyond the walls of the medical facility itself.
What are the stages of the patient journey?
There are several stages along the patient journey. When gathering patient feedback, you should make sure to capture insights at each of these stages.
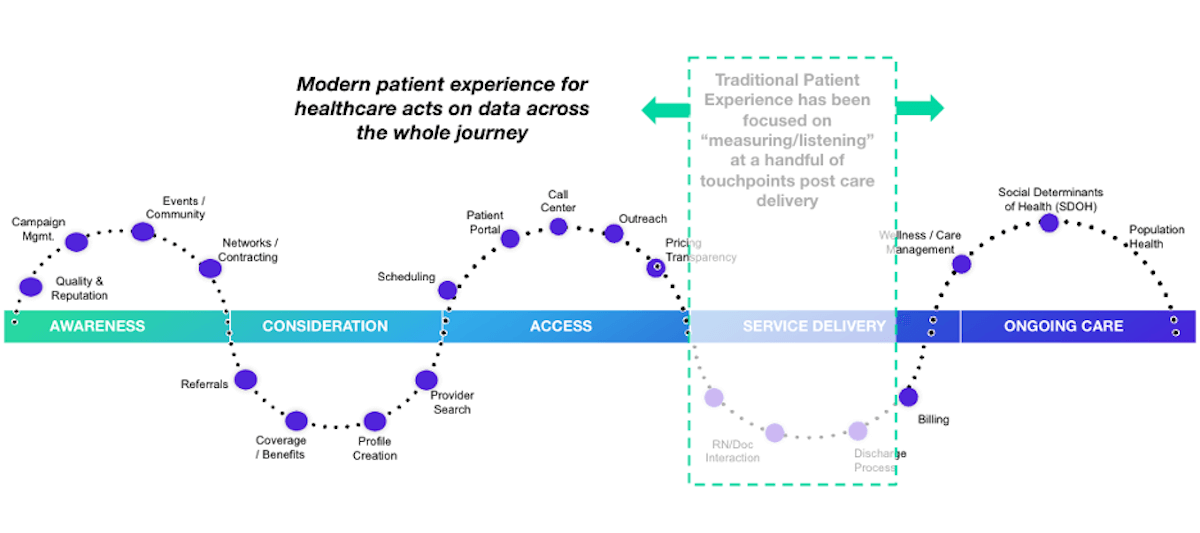
Stage 1: Awareness
The patient journey starts with awareness. In this stage, the patient identifies a need for care and begins searching for care providers. Examples of how patients learn about healthcare providers include online searches, review sites, marketing campaigns, networking, and community involvement.
Stage 2: Consideration
In the consideration stage, the patient weighs their options to determine if your health system can meet their needs. Factors patients consider include referrals, coverage and benefits, recommendations, access, and ratings and reviews. Often in this stage, patients interact with your website or social media pages or contact you via phone or email during this stage.
Stage 3: Access
The access stage is where the patient decides to schedule services with your healthcare organization. Direct patient engagement with your organization increases during this stage. You’ll engage with patients in a variety of ways including phone calls, the patient portal, text messages, and emails as part of the scheduling and new patient acquisition process.
Stage 4: Service delivery
The service delivery stage relates to the clinical care provided to your patients. Encompassed in this stage are the clinical visit itself, check-in and check-out, admission and discharge, and billing. Traditional patient satisfaction measurement centers around this stage of the patient journey.
Stage 5: Ongoing care
The ongoing care stage of the patient journey involves patient engagement that occurs after the interactions directly related to service delivery. In addition to wellness and care management, this stage may address social determinants of health and population health.
What is a patient journey map?
The best way to utilize the patient journey to enhance patient experiences is by journey mapping. A patient journey map is a visual tool that illustrates the relationship a patient has with a healthcare organization over time.
Patient journey mapping helps stakeholders to assess the patient experience from multiple perspectives. Journey maps provide a way to visualize the internal and external factors affecting patient flow and the different paths patients must take in order to reach their care goals.
What are the benefits of patient journey mapping?
Patient journey mapping can help you to visualize all of the steps patients take throughout the entire process of seeking, receiving, and continuing care. Creating a patient journey map is useful to identify pain points and gaps in care. Mapping the patient journey makes it easier to develop solutions that make a more seamless experience within your healthcare system.
Patient journey mapping benefits include:
- Creating shared ownership of the patient experience
- Refining your patient listening strategy
- Aligning your organization with a common view of the patient experience
- Measuring gaps between the intended experience for your patients versus the actual experience
- Identifying and resolving common pain points for your patients
Four types of patient journey maps
When creating a patient journey map, there are four types to consider. Each type of map has an intended purpose. You might start your patient journey mapping with only one type and incorporate the others as your efforts progress.
Current state
A current state journey map tells the story of what patients do, think, and feel as they interact with your organization today. This type of patient journey map is ideally created using patient data and observational data.
The current state journey map is best for driving incremental improvements to enhance the patient experience.
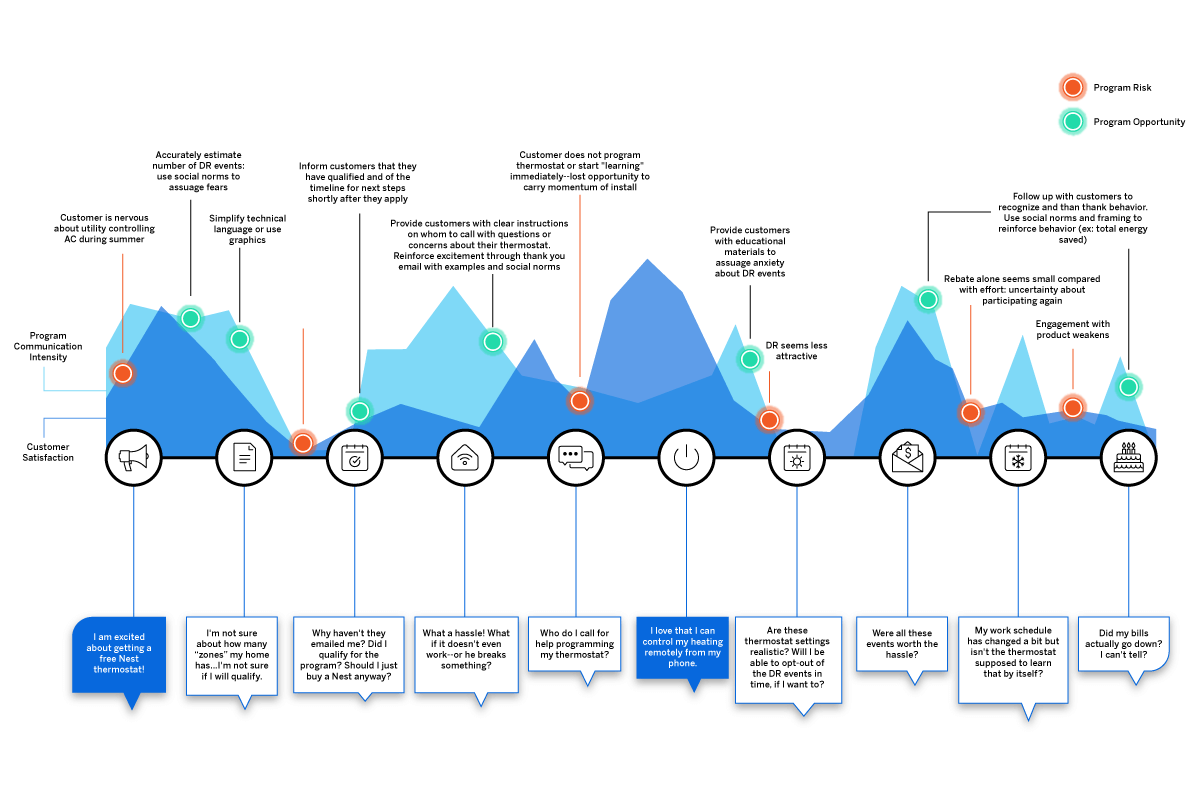
Future state
A future state patient journey map tells the story of what you want your patients to do, think, and feel as they interact with your organization in the future. This type of map should capture the ideal journey you’d like to see for your patients.
The future state journey map is an effective tool to drive strategy, align teams, and communicate your visions for new services, processes, and experiences.
Day in the life
A day in the life patient journey map illustrates what your patients do, think, and feel today, within a specific area of focus. Patient personas are particularly useful when creating day in the life maps; these are discussed in greater detail below.
This type of patient journey map is intended to capture what your patients experience both inside and outside of the healthcare system. Day in the life maps are valuable to address unmet needs and determine how and when you can better engage your patients.
Service blueprint
A service blueprint is a simplified diagram of a current state or future state patient journey map. In the service blueprint, you add layers to illustrate the systems of people, processes, policies, and technologies surrounding each patient touchpoint.
For current state patient journey maps, the service blueprint can help to identify root causes of pain points. For future state, the service blueprint is helpful to visualize the systems or processes that can be put in place to support the intended patient experience.
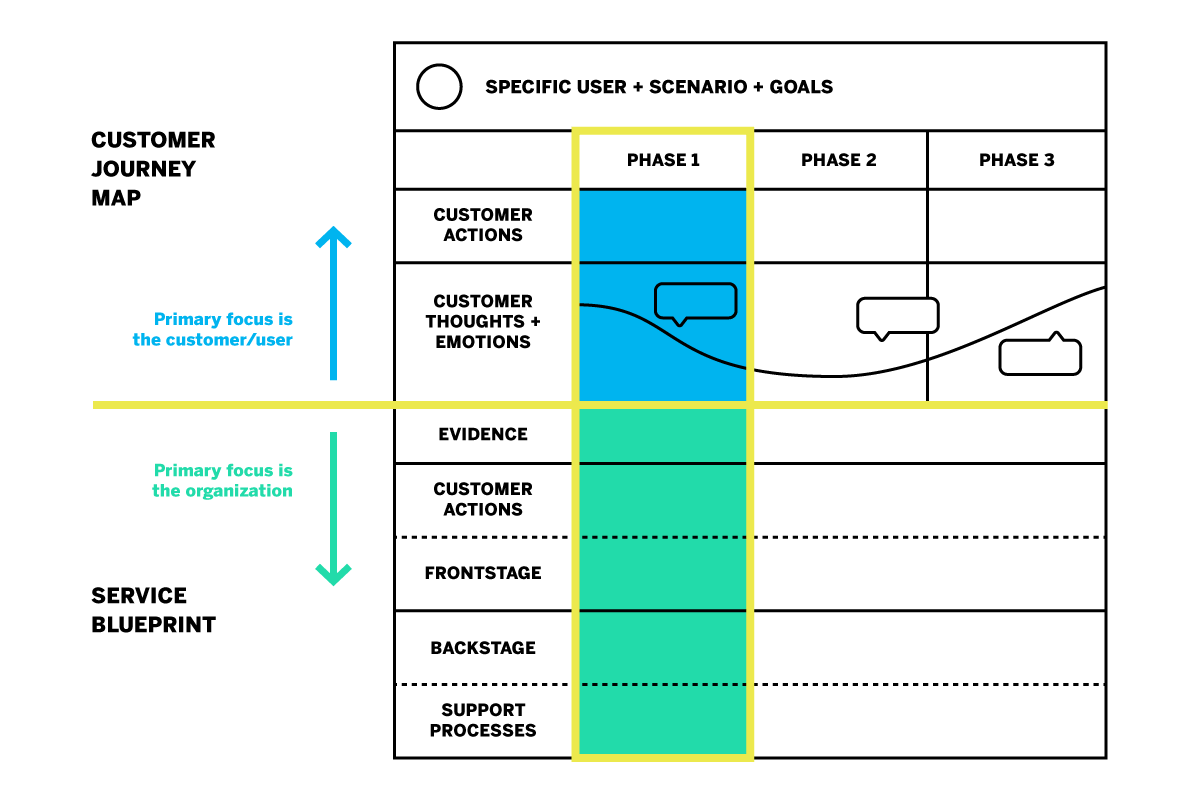
How do you create a patient journey map?
Now that you know about the different types of patient journey maps and their roles in driving patient experience improvement, how do you get started on creating your own?
The most useful maps are those which can expound upon each touchpoint of the healthcare journey with operational data, such as patient demographics, as well as real patient insights and perspectives. Using a platform that can capture this data will aid significantly in your patient journey mapping process.
Patient journey mapping: getting started
Before you get started, it’s a good idea to engage individuals across all departments and include input from multiple stakeholders. Once you’re ready, follow these steps to begin creating an effective patient journey map.
Identify your target audience
What type of patient journey will you be mapping? There may be varying patient journeys within your organization; for instance, an oncology patient’s journey will look very different from that of an expectant mother. The journey of a patient with health insurance will differ from that of a patient without insurance. To map the patient journey, you’ll want to create robust patient profiles you can use to segment and track like-populations throughout the healthcare experience.
Establishing patient personas and segments
Not every patient will have the same healthcare goals. Creating patient personas based on behaviors and preferences is a good way to differentiate the needs and more clearly understand the perspectives of the unique populations you serve.
The ideal patient persona will include the following information.
- Demographic information such as age group, gender, or location
- Healthcare-specific goals, conditions, and treatments
- Healthcare-specific challenges/pain points
- Engagement patterns and expressed feedback
- How your services fit into their life
- Barriers to care
Specify a goal for the patient’s journey
The patient personas you create will all have unique goals within the care journey. The patient has a specific goal in mind when they initiate contact with your organization, whether it is treatment of symptoms, a diagnosis for chronic issues, or surgery.
Every interaction along the patient journey influences how successful the patient feels about achieving this goal. When mapping the patient journey, you’ll want to consider how the various touchpoints affect the patient’s ability to meet this goal.
Identify the patient’s steps to accomplish their target goal
This step is about how the patient views their care journey within your health system–not about the actual processes and systems your organization has in place. Effective patient journey mapping requires you to see how the patient navigates the journey through their point of view.
Omni-channel listening is a valuable strategy in this step of journey mapping. Listening to your patients across all the channels can provide a clearer picture of their perceptions and behaviors as they engage with your organization.
Some steps the patient takes may not even include your organization, but might still affect how they are interacting with you directly. For example, if a patient logs into their health insurance portal to check coverage for healthcare services, they are not engaging with your organization but this is still a part of their care journey that may feed into their interactions with your organization later on.
Uncover perceptions along the journey
Gather patient feedback along the touchpoints of the care journey to identify key emotional moments that may disproportionately shape attitudes. These insights shed light on what’s working and what’s not; they can also be used to highlight the moments of truth that contribute to patient loyalty.
Patient perceptions are an important piece of patient journey mapping; it will be difficult to drive action without them.
Additional tips for creating the ideal patient journey map
Patient journey mapping is a continuous process. Creating the map is the first step, but the true value is dependent upon maintaining the map as you continue to gather insights and refine processes.
This leads to the second tip: be ready to take action! You can use a patient journey map to draw conclusions about your patients’ experiences within your organization, but awareness alone will yield no benefits. The journey map is a valuable tool to be used in your wider improvement efforts.
How do you drive action using a patient journey map?
Once your patient journey mapping is complete, it’s time to put it to good use. Here are five ways patient journey maps can be used to drive action.
Identify and fix problems
The visual layout of a journey map makes it ideal to identify gaps and potential pain points in your patient journeys. This will give you a better understanding of what’s working and what’s not. It will also help you to visualize where and how improvements can be made.
Build a patient mindset
Patient journey mapping enables you to incorporate more patient-centric thinking into your processes and systems. Use your map to challenge internal ideas of what patients want or need. Invite stakeholders to navigate the touchpoints along the healthcare journey to gain perspective.
Uncover unmet patient needs
By mapping the patient journey, you can build stronger patient relationships by listening across all channels to determine where experiences are falling short or where unmet needs emerge. This enables you to look for opportunities to expand alternatives, streamline initiatives, and create new, engaging ways for your patients to share feedback.
Create strategic alignment
Utilize your patient journey map to prioritize projects or improvement efforts. It can also help you to better engage interdepartmental staff to better understand policies and work together toward patient experience goals.
Refine measurement
Patient journey mapping is a great resource to use when defining patient satisfaction metrics and identifying gaps in how you currently gather insights.
How does patient journey mapping increase your bottom line?
Patient journey mapping can increase your bottom line by laying the foundation for improved patient satisfaction and higher retention.
Organizations across all industries are looking to understand customer journeys in order to attract and retain customers by gaining deeper insights into what drives the consumer experience.
As healthcare becomes more consumer-driven, health systems must similarly map the patient journey to improve the patient experience and boost retention. The cost of patient acquisition, combined with the fact that patients are willing to shop around for the best healthcare experience, means success depends on creating the most seamless patient journey possible.
The tools for success
For the most impactful patient journey mapping experience, you’ll want the ability to link your operational and experience data to your journey map’s touchpoints. Insights about what has happened at each touchpoint, as well as why it is happening, empower you to create experiences that meet patient expectations and drive up satisfaction.
Here are some best practice considerations as you develop your patient journey mapping strategy:
- Create a shared understanding throughout your health system of how your patients interact with your organization, and you’ll know the roles and responsibilities of your different teams
- Design a unique patient journey based on multichannel, real-time feedback from the patient
- Consider the frequency with which topics emerge in feedback, as well as the emotional intensity behind them to zero in on what improvements can drive the greatest impact
- Develop empathy and collaboration between teams, working together to achieve the same outcome
- Drive a patient-centric culture by developing a shared sense of ownership of the patient experience
- Connect your operational patient data with your patient experience feedback in one system
- Leverage a closed-loop feedback system that triggers actions for immediate responses to patient concerns
Qualtrics’ XM Platform™ is designed to support all of these actions throughout the journey mapping process.
The 3 steps to driving human-centered healthcare experiences
Related resources
Patient feedback 15 min read, healthcare branding 13 min read, patient journey 10 min read, patient experience 12 min read, symptoms survey 10 min read, nurse satisfaction survey 11 min read, cahps surveys 6 min read, request demo.
Ready to learn more about Qualtrics?

The Patient Journey: What it is and Why it Matters

- Share on Facebook
- Share on Twitter
- Share on LinkedIn
- Share on Email
Healthcare is under enormous pressure today.
Patient expectations about their service and experience have changed over the years. Patients have more choices about their care, and they’re more empowered with information about what they want their care experience to be. They expect you to interact with them on their terms, not yours. And with COVID-19 turning so much of our lives digital, this trend has only accelerated.
Having a robust marketing automation approach is critical to addressing these challenges in today’s environment. Meeting — and exceeding — patient expectations comes down to managing your patient’s engagement journey.
How can patient journeys improve care?
What patient journeys can do is turn the healthcare experience from a primarily reactive experience to a proactive one.
By building out journeys for your patient personas, you can close gaps in care, establishing robust preventative routines that ultimately help your patients stay as healthy as possible for as long as possible.
Engaging consumers and patients where they are builds trust and confidence that keeps patients in the system and encourages them to refer their friends and family to your practice. According to the Beryl Institute , 70% of patients will share a positive experience with others. But your bigger risk is that 76% will share a negative one. And with a negative experience, 43% of patients won’t go back to that provider, with 37% finding a different doctor altogether.
What is the patient journey?
A patient journey represents the entire sequence of events that a patient experiences within a given healthcare system or across providers, from scheduling an appointment for a regular checkup to receiving treatment for an illness or injury.
A patient journey is an ongoing process that incorporates all parts of the healthcare ecosystem, from hospitals to physicians, specialty care, and outpatient therapy.
While it is easy to think about a patient’s journey as those interactions you have with them before, during, and after an appointment, there are actually many other touchpoints that drive their overall journey. A comprehensive patient engagement strategy touches on all aspects of a patient’s relationship with a healthcare provider, including:
- Onboarding and Access
- Diagnosis and Treatment
- Adherence to Lifestyle or Behavioral Changes
- Ongoing and Proactive Health (Wellness)
- Referrals and Loyalty
How do I create the patient engagement journey?
Every single interaction with a patient is part of the patient engagement journey and a moment of truth for the health system or provider to add value.
In today’s value-based healthcare world, having that personalized experience is more important than ever. A patient engagement journey organizes those communication touchpoints and ensures you’re delivering the right information at the right time to the right person, and leveraging the appropriate communication channel. Millennials and Generation Z, for example, may be more likely to prefer a text, email, or chat to a phone call.
It’s about knowing your patients’ preferences — like that they prefer to be texted during the day while they’re at work or if they prefer an office vs. telehealth visit — and what’s going to make it easier for them, like sending automatic reminders the week and day before an appointment.
Whether it’s making sure you follow up with cardiac patients about weighing themselves daily after surgery to catch any water retention issues or asking colonoscopy patients whether or not they’ve been following post surgery protocols after discharge, it’s about continuity of care once a patient leaves the office or hospital so they have a quality outcome. From there, patients can more proactively drive their own wellness plan.
Here are important areas to focus on when creating your patient engagement journey:
Establish your patient personas
You need to know the different types of patients that are coming into your organization. You want to figure out:
- What are the most relevant needs of your patients?
- What are their communication and care preferences?
- How do they want to engage with you?
- What information do you already know about them?
To be able to craft the best possible patient experience, you first have to know more about your patients.
For example, there’s a well-known healthcare persona out there called the “Medical Mom” (which can, of course, be any individual taking care of themselves, their kids, their spouses, and may also be the caretaker for aging parents).
Let’s say this individual has three children, and they book annual physicals at their pediatrician, which happens to have offices in the same building as their own primary care physician. Wouldn’t it be nice if the office sent them one email reminder to schedule all five appointments, rather than five different emails? And when they do call, scheduling those appointments back-to-back so everyone is in and out in one afternoon?
A spreadsheet is not going to be able to do that for you. Collecting and managing the data required to drive complex, interconnected patient journeys requires more than a spreadsheet. In order to succeed, you’ll need to pay close attention to the entire patient lifecycle.
Understand the entire patient lifecycle
An appointment reminder is a great start to engaging a patient, but it’s just one event in an ongoing patient lifecycle that begins with preventative care and includes diagnostics, delivery of care, and post-operations.
For example, how many patients show up for routine blood work at their physician office and you find out they haven’t fasted for the appropriate amount of time? Sending a patient home is frustrating for them and it’s frustrating for you. If the appointment is at 2:00 PM, then that appointment reminder should have been sent at dinnertime the previous evening, reminding them that they can’t eat anything after a 6:00 AM breakfast the next morning.
You’ll want to tailor your communications based on whether the patient is new or existing, what their preferences are, and whether they have any specific or chronic health issues. From there, you need to…
Understand the moments of truth
The healthcare system is complicated, even for those who have been a part of it for decades. The key to building a great foundation for your patient engagement strategy is to put yourself in a typical patient’s shoes. Most patients don’t engage with the healthcare industry unless they’re feeling sick. That means they’re rarely at their best, and they’re not only anxious about getting better, but about the costs associated with that.
The best healthcare providers understand the moments of truth — opportunities for a positive touchpoint that can alleviate their stress and anxiety and help them get on the road to recovery. Every time you interact with a patient is an opportunity for a moment of truth, whether that be in person or via other channels of communication. It’s not only about establishing accurate moments of truth, but capitalizing on them.
It’s up to you to understand the places people need to be, how you want to communicate to them, and make every one of those touchpoints a positive experience. It doesn’t matter whether they’re physically in your office or not. Your patient engagement journey is what guides your patients to making the best possible decisions on their care so they get better.
The easier you make it for them to engage with you, the higher quality their care will be. Ultimately, you want your patients to be evangelists for your services based on their positive experiences. To do that, you’ll need to…
Get the data you need
Your patients expect personalization.
Personalization in healthcare used to mean created tailored treatment plans and clinical protocols. That’s still important, but patients expect more personalization around the entire experience, from access to communication to quality outcomes. It’s like turning on a light switch in your home: a patient just expects the light to turn on.
Personalization today means being able to see at-a-glance a patient’s healthcare record, communication preferences, and social determinants that may be impacting their overall health to give you a 360-degree picture .
To do this, you need more than clinical data.
You may have patients that constantly miss their appointments. By storing questions that go beyond health risks — say, that they’re a smoker — but to understand that they don’t have a car to get to the appointment in the first place is becoming a more important part of the process. Part of empathetic, compassionate care is understanding these environmental factors that can help patients get the care they need, whether that’s calling a Senior Shuttle, caregiver, or arranging a telehealth appointment instead.
Once you have the data, you can…
Encourage referrals and loyalty
The first place people look for a new doctor isn’t the Internet. It’s their friends and family. In an ideal world, every patient you have should be able to say, “Oh, I loved my experience with…”
Doing that starts with the technology you have. Before a patient ever comes in for treatment, you need to make sure they have a seamless experience that builds trust and encourages referrals and loyalty.
How do I get started with patient journey mapping?
It’s time to move away from the mindset to simply fill the top of the funnel with as many new potential patients and contacts with caregivers as possible. While this is still a requirement, it is just as crucial for organizations to get better at managing and growing relationships at every phase of the patient journey. Providers must engage with consumers in the marketplace to introduce them to their services of course, but it is of growing importance that they offer support throughout the entire diagnostic and treatment process.
As a Salesforce Platinum Partner with deep industry expertise, we have created a Foundation for Patient Engagement package — a complete strategy that starts with Health Cloud and facilitates a 360-degree view of the patient , as well as a comprehensive communication strategy, CTI integration, and the use cases driving patient acquisition, engagement, and loyalty.
Learn more about building your patient journey with Silverline.
From the Blog More articles about Provider

Provider Personalization in Healthcare: 6 Keys To Successful Patient Experiences

Provider Prioritize Patient Experiences with EHR CRM Integration

Provider The Future of AI for Healthcare Providers
We don't support internet explorer.
Please use Chrome, Safari, Firefox, or Edge to view this site.
- Definitive Healthcare (View)
- Monocl (ExpertInsight)
- Populi (Claims analytics)
- Carevoyance (Sales accelerator)
Patient Journey
What is a patient journey.
Patient journey is a term referring to a patient’s experience throughout an episode of care, beginning at admission and concluding with hospital discharge.
The renewed focus on patient experience in recent years stems from growing trends in healthcare consumerization and value-based care initiatives . To remain competitive, providers are beginning to consider patients more as customers and, consequently, are working to improve the overall healthcare experience and keep patients within their networks.
Why is the patient journey important in healthcare?
Patient journey mapping allows healthcare providers and other industry stakeholders to gain a better understanding of the patient experience and to find new ways to improve all points of the patient journey.
By understanding the patient journey, providers can build a hyper-targeted experience that addresses the unique needs of each patient and delivers more successful patient outcomes. Improved patient experiences can also save providers money — for example, by reducing the average time to diagnosis.
Share this Glossary Entry
Related links.
How Patient Journeys Influence Medical Device Strategy Consumerization 2.0: The Patient Joins the Care Team Top 8 Healthcare Trends in 2020
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Donaldson L, Ricciardi W, Sheridan S, et al., editors. Textbook of Patient Safety and Clinical Risk Management [Internet]. Cham (CH): Springer; 2021. doi: 10.1007/978-3-030-59403-9_10

Textbook of Patient Safety and Clinical Risk Management [Internet].
Chapter 10 the patient journey.
Elena Beleffi , Paola Mosconi , and Susan Sheridan .
Affiliations
Published online: December 15, 2020.
The wide implementation of patient safety improvement efforts continues to face many barriers including insufficient involvement of all stakeholders in healthcare, lack of individual and organizational learning when medical errors occur and scarce investments in patient safety. The promotion of systems-based approaches offers methods and tools to improve the safety of care. A multidisciplinary perspective must include the involvement of patients and citizens as fundamental contributors to the design, implementation, and delivery of health services.
The patient journey is a challenging example of using a systems approach. The inclusion of the patient’s viewpoint and experience about their health journey throughout the time of care and across all the care settings represents a key factor in improving patient safety. Patient engagement ensures that the design of healthcare services are aligned with the values, the preferences, and needs of the patient community and integrates the real-life experience and the skills of the people to enhance patient safety in the patient journey.
The utmost priority to implement patient engagement is the training of patients. Therefore, training for both patients/families/advocates and health professionals is the foundation on which to build active engagement of patients and consequently an effective and efficient patient journey.
The chapter offers examples of successful training courses designed to foster strategic alliances among healthcare professionals and researchers with patients and their organizations. Training of patients constitutes the first step to develop shared knowledge, co-produced projects, and the achievement of active multilevel participation of patients for the implementation of patient safety in the patient journey.
10.1. Introduction
Almost 20 years after publication “To Err is Human: Building a Better Health System” (Kohn et al. 1999), patient safety is still not widely implemented. This report from the Institute of Medicine is the milestone that constituted a turning point for improving quality of care and patient safety identifying the need to rethink healthcare delivery to provide safe, effective, and efficient care.
The barriers of implementing patient safety as a driving force for change towards more effective healthcare include multiple factors: insufficient involvement of all stakeholders contributing to the care process, lack of willingness of organizations and individuals to learn from errors and scarce investments in patient safety improvement and research.
There is a growing need to promote systems approaches to finding solutions in healthcare to improve the safety of care, the quality of healthcare delivery, patients’ health and citizens’ well-being.
The discussion paper “Bringing a Systems Approach to Health” defines the systems approach as one “that applies scientific insights to understand the elements that influence health outcomes; models the relationships between those elements; and alters design, processes, or policies based on the resultant knowledge in order to produce better health at lower cost” [ 1 ].
A multidisciplinary approach must include the involvement of citizens and patients as fundamental contributors to the design, implementation, delivery, and evaluation of health services.
This means that citizen participation plays an essential role, bringing the unique point of view of patients and family members into the debate on patient safety and quality of care.
Patients and more generally citizens, when actively and systematically engaged, bring ideas and experiences which can support a collaborative and reciprocal learning process among the healthcare stakeholders. This produces knowledge that leads to improved practices, a real knowledge creation process where the dynamic participation of all actors in healthcare systems contribute to an active learning environment where the identification, the investigation, and the planning of solutions related to health incidents is a cyclic process enabling healthcare knowledge creation.
The added value of involving patients in healthcare is, respect to other more complex interventions, a low cost opportunity to take into consideration unconventional points of view creating and building knowledge and providing original insights and ideas that otherwise would not be considered.
Health professionals and patients’ skills and knowledge are acquired through individual experience or education and transferred to the health organizations in a perspective of co-production of healthcare. It is a merging of the efforts of those who produce and those who use the solutions to address health problems. It serves to establish a strengthened and long-term relationship in terms of trust and effectiveness and to distribute the responsibilities among all stakeholders [ 2 ].
In light of these arguments, the systems approach—inspired by the fundamentals of ergonomics and human factors (HFE)—creates new alliances between healthcare and engineering, of which patient journey is a challenging example [ 3 ].
Applying the systems approach to patient safety allows the analysis of the factors that characterize the encounters and the interactions between healthcare professionals and patients during the entire course of care. The observation of possible critical issues to the individual and specific encounter between clinician and patient is crucial in widening the scope of observation and research of the entire “journey” of the patient, taking into consideration the complexity of patient, their values and needs, their preferences, the economic and social context in which they live, and language and communication issues.
These observations and research should be carried out considering the interconnections and interactions together with the components of the processes; importance should be given to the context, and to manage the complexity, the value of a holistic approach.
10.2. The Patient Journey
A modern health system looks to the future in the context of the challenges imposed by the real world. It must manage the gap between guidelines and health protocols and what effectively happens and how reality is perceived by patients and family members.
It is more and more necessary to bring the patient’s point of view in the analysis of the care process, in the incident reporting and analysis, in the design and implementation of solutions and guidelines in healthcare.
Vincent and Amalberti in “Safer Healthcare” (2016) [ 4 ] stated that the incident analysis should broaden the class of events having consequences on patient safety. Incidents reported from the patient’s point of view should be included in addition to those suggested by health professionals. Additionally, when analyzing an incident, it should be done in the context of the patient journey rather than a single episode.
Instead of focusing on the individual encounter, it is necessary to extend the observation timeframe by applying the examination of contributing factors to each of the encounters that compose the patient journey (temporal series of encounters with healthcare facilities, a hospital unit, a specialist visit, a primary care clinic, a home health agency), considering both the negative and positive events and the points for improvement that were revealed (Fig. 10.1 ).
Analysis of safety along the patient journey
The adoption of this wider approach is unique in that it incorporates the patient’s perspective of safety and includes new features in the incident analysis such as asking patients to recount the episode of care, including patient and family in the investigation team when possible, asking patients the contributory factors from their point of observation and perception and involving patients and families in the reflections and comments on the disclosure process [ 4 ].
The episodes patients and families can highlight are often different from those that professionals are more accustomed to reporting. However, patients could be involved in further ways in incident reporting and assessment, and today patient-derived information constitutes a free and little used resource.
As per McCarthy’s definition, “patient journey mapping describes the patient experience, including tasks within encounters, the emotional journey, the physical journey, and the various touch points” [ 5 ]. Carayon and Woldridge define “patient journey as the spatio-temporal distribution of patients’ interactions with multiple care settings over time” [ 3 ], where at each point of touch with each healthcare service along the patient journey, the patient interacts with several system elements (task interaction, physical environment, interaction with tools and technologies, organization interaction, interaction with other organizations and other people, interaction with other people and teams within the organization) (Fig. 10.2 ).
The patient journey as a set of interactions and transitions
The patient journey represents the time sequence of what happens to the patient, especially during transitions of care, in particular considering that the health professional who takes care of the patient only sees the portion of care for which he is responsible and in which he has an active role. Conversely, the patient is the only person who has a continuously active and first-hand role during their health journey. They alone are in possession of information that characterizes the entire care experience.
Moreover, when patients navigate their journey, they contact and interface with multiple work systems at several time points, where the sequence of interactions in the work systems determine the outcome experienced by patients and families, healthcare professionals, and health organizations. (Fig. 10.3 ). Each local work system is influenced by a wider socio-organizational context, which can be formal healthcare organization (such as hospital, primary care facility, nursing home) or informal (home).
SEIPS 3.0 model: sociotechnical systems approach to patient journey and patient safety
Every point of the patient journey offers data on health outcomes and patient experience outcomes that should be used as feedback to redesign healthcare work systems in terms of adaptation, learning, improvement.
Patient’s experience represents an important resource in participatory collaborative design, especially in the patient journey where this experience is the result of multiple interactions across space and time.
10.3. Contextualizing Patient Safety in the Patient Journey
Many of the incidents or near-misses during healthcare are not due to serious errors, but to the combination of small failures, such as limited experience of a recently qualified doctor, use of obsolete equipment, an infection difficult to diagnose or inadequate communication within a team.
We know that the analysis of an incident requires looking back to the succession of events that have occurred and that led to the problematic episode, considering both active and latent errors, and all the aspects connected directly or indirectly. It is fundamental to examine the safety of the entire patient journey, all the encounters that make up the entire care process, to study the whole medical history of the patient in an attempt to reconstruct all the elements that characterize the “health journey”, not only from the viewpoint of the health professionals, but also from that of the patient and family.
In light of these arguments, new concepts, tools, models, and methods need to be embraced to support patient safety in the patient journey.
A significant contribution in terms of concepts, frameworks, and models is offered by Industrial and Systems Engineering, and often human factors and systems engineering (HF/SE) have an approach to include the preferences and the needs of stakeholders when designing solutions to address the critical aspects of a health process.
Human factors and ergonomics are described as “the scientific discipline concerned with the understanding of interactions among humans and other elements of a system, and the profession that applies theory, principles, data and methods to design in order to optimize human well-being and overall system performance. Practitioners of ergonomics and ergonomists contribute to the design and evaluation of tasks, jobs, products, environments and systems in order to make them compatible with the needs, abilities and limitations of people. Ergonomics helps harmonize things that interact with people in terms of people’s needs, abilities and limitations” [ 6 ].
Process models have found widespread use in drug management, visit planning, care transition, to name a few, and can offer tools and methods to investigate interprofessional and physician–patient communication, interruptions and health information handover.
Drawing from the finding of Carayon’s studies [ 3 ], the Systems Engineering Initiative for Patient Safety (SEIPS) model gives a description of five work system elements which when applied to a definite patient journey model should outline who (person) is doing what (tasks) with tool and technologies, taking into consideration the physical and organizational environment where all these activities take place. All these factors have to be examined for both patients and workers and the process analysis and modelling have to consider what patients and families/caregivers, healthcare professionals and workers actually do ( work-as-done versus work-as-imaginated ).
Patients, families, and caregivers are deeply involved in the healthcare process due to the tasks they carry out in the intermediate sectors of care between encounters. Away from direct interactions with professionals, they have to perform multiple actions requiring understanding of what behaviour to adopt, which instructions to follow, how to administer a medication and how to communicate with hospital doctors, general practitioner, and home healthcare professionals [ 3 ].
Taking into account what has been highlighted so far, one of the leading and most challenging keys to success in improving patient safety is to adopt a systems approach to patient safety which includes the patient’s perspective about their health journey throughout the time of care and across all the care settings.
This assumption highlights that patients and their families are valuable resources and can play an important role in patient safety improvement efforts. Viewing health systems as “co-producing systems”, patients can engage as partners in co-producing patient safety improvement activities individually, in groups and collectively. Individual patient and family member participation/co-production of safer care is fundamental. Equally as important is the co-management and co-governance of healthcare services, in addition to the engagement of communities in policy definition and designing activities.
In fact, patient engagement directs the design of healthcare systems towards the preferences, the values, the real-life experiences, and—not less important—the skills of the people to enhance patient safety in the patient journey.
Such a change of perspective involves multiple dimensions of interactions and relationship between patients and professionals, encompassing cooperation, dialogue and listening, trust, reciprocity and peer-to-peer work [ 2 ].
It follows that on the one hand the healthcare organizations have to demonstrate the willingness to support health professionals to effectively engage patients in the patient journey to achieve the common goal of reducing the risk of patient harm or incidents as well as the willingness to integrate patients and family members as partners into quality and safety improvement efforts. On the other hand, it is necessary to motivate and encourage patients and families/caregivers to actively participate during the individual care process for safer care as well as partner in organizational patient safety improvement efforts to ensure safer care for others.
The working group Patient and Family Involvement for the delivery of Safe and Quality Care [ 7 ] stated that the utmost priority to realize the patient involvement is the training of patients, followed by the promotion of interdisciplinary training programmes for healthcare professionals to promote patient and family engagement, the implementation of multilevel structures that allow for participatory processes by patients and smarter allocation of resources in healthcare that supports involving citizens in patient safety improvement efforts for better healthcare.
This working group was part of the activities of the “1st International Meeting about Patient safety for new generations—Florence, 31st August and 1st September 2018” organized by the Centre for Clinical Risk Management and Patient Safety, Tuscany Region—WHO Collaborating Centre for in Human Factors and Communication for the Delivery of Safe and Quality care [ 7 ].
Therefore, training for both patients/families/advocates and health professionals is a pillar on which to build active engagement of patients and consequently an effective and efficient patient journey. From this perspective, the participation of patients (i.e. representatives of patients’ associations and organizations, patient and citizen advocates) in training courses—specifically designed for this target audience of trainees and aimed to encourage co-production of care—is an essential and effective activity to co-produce a better healthcare system in terms of quality and safety of care.
Sharing a common language, promoting citizens’ and patients’ awareness of importance of co-production of care, teaching the key role that patients can play in making treatments safer (investments in health literacy), learning to work together and within a network (locally, regionally, and nationally/internationally) on priority safety and quality of care issues: these are some of the main strengths of training courses aimed to be at the basis of active engagement of patients and citizens.
Examples of successful training courses include “PartecipaSalute” and “Accademia del Cittadino” organized in Italy by Laboratory for Medical Research and Consumers Involvement of the Istituto di Ricerche Farmacologiche Mario Negri IRCCS and the Centre for Clinical Risk Management and Patient Safety, Tuscany Region. The following paragraph describes this educational experience which is specifically designed for citizens and patients to improve their knowledge and skills in patient safety and quality of care, with the aim of co-producing better healthcare services.
10.4. From PartecipaSalute to the Accademia del Cittadino: The Importance of Training Courses to Empower Patients
Over the last few years in the field of health and research and with regard to participation and involvement of citizens and patients, we have witnessed the transition from a paternalist to a partnership model. Individual citizens and those citizens involved in patients’ associations or groups have acquired a new role: no longer passive but actively involved in decision-making regarding health, healthcare, and research in the health field [ 8 , 9 ].
This is a progressive step-by-step process based on the recognition and implementation of the key concepts such as health literacy and empowerment. Health literacy, more properly used at individual level is defined as the capacity to obtain, read, understand, and use healthcare information in order to make appropriate health decisions and follow instructions for treatment [ 10 ]. Empowerment, more used at the community level, is a process that, starting from the acquisition of accurate knowledge and skills, enables groups to express their needs and more actively participate to request better assistance, care, and research. At this level, the availability of organized independent and evidence-based training courses is essential to allow people to be able to critically appraise and use information about the effects of healthcare interventions. Consequently, they will have the skills to participate in the multidisciplinary working groups (composed of researchers, health professionals, patient and citizen advocates, institutional representatives).
In the late 1990s, the Istituto di Ricerche Farmacologiche Mario Negri IRCCS held the first training courses of this kind focused at breast cancer associations. Some years later, within the project PartecipaSalute—a not-for-profit research project designed to foster a strategic alliance among healthcare professionals, patients, and their organizations—an ad hoc training programme for representatives of citizens’ and patients’ organizations was defined with a multimodule format [ 11 , 12 ]. This was an innovative approach, at least in the Italian setting in that period.
PartecipaSalute training programme has combined different experiences: the Mario Negri Institute IRCCS experience in collaborative research activities with patients’ associations, the Italian Cochrane Centre with the activities aimed at promoting the principles of evidence-based medicine, and Zadig long-term experience in health communication. The above promoters jointly developed the PartecipaSalute training programme on the belief that data are more important than opinions, and that every decision should be supported by well-conducted research data.
The spread of this belief to patients and citizens with the purpose of stronger involvement was a key point of PartecipaSalute training courses.
Therefore, patient, family, and community knowledge of the principles of how evidence is developed through clinical research is essential to make or support decisions in the health debate, to promote better clinical research, or to convey correct information. The strength of the PartecipaSalute programme was based on the exchange of experiences in an interactive way aimed at creating opportunities for discussion, overcoming the teacher–learner model. Each session started with an interactive discussion of a real situation—such as a screening, vaccination, therapy—and after sharing data, opinions or articles from media, evidence was presented and discussed, underlining significant methodological aspects. The programme offered the opportunity to debate the value and significance of the methodology offering critical appraisal tools. Each participant was invited to take an active part, starting from direct personal or associative experience. Table 10.1 presents the topics considered in the first three editions of the training programme. The participation was free, and different types of materials were provided including an ad hoc manual published by PartecipaSalute, copies of the PowerPoint presentation and articles.
Topics considered in PartecipaSalute [4] and PartecipaSalute-Accademia del Cittadino training courses
Considering the characteristics of the programme and its modular structure, the PartecipaSalute training programme could be adapted to specific contexts. In fact, the experience of PartecipaSalute was adopted at the regional level by Regione Toscana (Centre for Clinical Risk Management and Patient Safety and the Quality of healthcare and Clinical pathways of Health Department, Tuscany Region) developing a more specific training programme called PartecipaSalute-Accademia del Cittadino (Academy of Citizen), focused on patient safety and risk management. In particular, after some modules on methods related to evidence-based medicine, uncertainties in medicine and information and communication in health, the training was mainly dedicated to regional and local activities on clinical risk management, the role of patients’ associations to improve patient safety and to support the implementation of best practices, the analysis and data of adverse events and risk assessment in terms of quality and safety in the care processes (Table 10.2 ).
Topic integration in the PartecipaSalute-Accademia del Cittadino joint courses
The PartecipaSalute-Accademia del Cittadino joint training programme has been implemented in three editions over the last decade and has trained about 100 members of patient and citizen advocates representing 38 patients’ associations. The courses ranged from 5 to 3 modules of 2 days each in residential mode to allow participants to get to know each other and create a network of associations committed to be engaged in clinical research, quality, and healthcare safety issues.
The entire educational experience was characterized by the use of participatory training methods, based on working groups, practical exercises, lectures from experts with opportunities for discussions. As a result of this training course model, the participants were recognized as “expert patients” and were regularly involved in basic activities for promoting patient safety as auditors on significant events and helping to define policies on patient safety at the Tuscany regional level. In addition, they have participated in patient safety walkarounds in hospitals and in developing eight cartoons intended to promote the education of citizens for the prevention of the most diffused risks (such as prevention of infections, prevention of falls and handovers).
Feedback on the satisfaction on tutors, topics discussed and knowledge gained was regularly requested from participants through questionnaires distributed before and after the programme. In general, positive feedback was received; participants appreciated the interactive methods of work, the clarity of the language, and the effort to make difficult problems easy to understand. An ad hoc questionnaire was provided to the participants regarding the methodology of clinical research, always showing an improvement in the self-evaluated knowledge before and after the course. Feedback of the results of the evaluation was also shared with each participant. Most of participants reported their experience to other members of the organization. In particular, in the case of the Regione Toscana training, the possibility of immediately transferring what was learned in the course in all the activities in collaboration with the health institutions, policy makers, and health professionals—such as working groups on patient safety best practices, participation to audits, development of tools to improve health literacy—was appreciated.
Some limitations emerged from these experiences. The selection of participants is the first issue, not only because the training course is accessible to a small number of participants (in general no more than 30 participants), but also because the groups comprised of middle-aged and retired participants, with few younger ones. Additionally, there were few individual patient or family member representatives from patient associations. The majority of those representing patient associations were in managerial or leadership positions. Furthermore, it is difficult to choose between small, local, or bigger regional associations. Residential training courses also restricted the participation for geographical reasons.
The PartecipaSalute and ParteciaSalute-Accademia del Cittadino training experiences show that patients and citizens are willing to get actively involved in healthcare and the research debate. There is a real desire to improve their knowledge and skills on health and research issues and allow some general considerations regarding the active engagement of citizens representing associations and advocacy groups.
In conclusion, it is very important to invest in a process of empowerment aimed to have well-trained activists involved vigorously and constructively in the debate, design, and assessment of health and research. Switching from tokenism to active participation is necessary to effectively partner with patients and the general population to design, plan, and co-produce safer more effective healthcare, while also supporting better more patient-centred research [ 13 , 14 ].
Also, the training courses are feasible and useful, as has recently been discovered also by pharma or other groups that organize courses mainly focused on drugs and drug development, thus directing the participation of the groups more to market needs than to public health.
Furthermore, this training initiative facilitates the networking among associations in part overcoming the difficulties that derive from personalization and division among the associations representing citizens and patients.
Finally, this illustrates the importance of the design and promotion of training courses with institutions, such as the Regione Toscana, in order to be able to implement projects of real collaboration between institutions, healthcare professionals, and consumers’ and patients’ representatives.
10.5. Recommendations
A systemic approach to health can provide valuable models for wider implementation of patient safety. A multidisciplinary approach includes the involvement of citizens and patients as unique stakeholders in the design, implementation, delivery, and assessment of health services.
Involving patients in healthcare is an opportunity to bring uncommon points of view into policy making and to create shared knowledge between healthcare professionals and patients.
The implementation of patients’ and families’/caregivers’ perspectives in the patient journey is the golden opportunity to leverage crucial input, such as experiential knowledge, safer care, patient motivation, and trust and social cohesion into the co-production of safety solutions in healthcare. This represents a way to get closer to person-centred care, to create opportunities for patients to meet and share information and knowledge, to develop structures and policies for patient involvement at different levels (with healthcare systems, universities, and policy makers).
However, little has been done to overcome some healthcare systems barriers: the power imbalance between the doctor and patient, language differences, the lack of diffusion of non-technical skills and, last but not least, the lack of evidence about the value of patient involvement.
To be widely implemented, patient engagement in the patient journey requires courageous leadership, organizational efforts, a wider culture of safety of care, the implementation of multilevel structures for the engagement of patients and resources from smarter spending in healthcare.
Education is the landmark to integrate meaningful patient and citizen engagement in healthcare. Training of patients is the fundamental starting point to develop shared knowledge, co-produce projects, and implement an active multilevel participation of patients and families for the improvement of quality and safety of care.
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
- Cite this Page Beleffi E, Mosconi P, Sheridan S. The Patient Journey. 2020 Dec 15. In: Donaldson L, Ricciardi W, Sheridan S, et al., editors. Textbook of Patient Safety and Clinical Risk Management [Internet]. Cham (CH): Springer; 2021. Chapter 10. doi: 10.1007/978-3-030-59403-9_10
- PDF version of this page (884K)
In this Page
- Introduction
- The Patient Journey
- Contextualizing Patient Safety in the Patient Journey
- From PartecipaSalute to the Accademia del Cittadino: The Importance of Training Courses to Empower Patients
- Recommendations
Related information
- PubMed Links to PubMed
Similar articles in PubMed
- The patient experience of patient-centered communication with nurses in the hospital setting: a qualitative systematic review protocol. [JBI Database System Rev Implem...] The patient experience of patient-centered communication with nurses in the hospital setting: a qualitative systematic review protocol. Newell S, Jordan Z. JBI Database System Rev Implement Rep. 2015 Jan; 13(1):76-87.
- The future of Cochrane Neonatal. [Early Hum Dev. 2020] The future of Cochrane Neonatal. Soll RF, Ovelman C, McGuire W. Early Hum Dev. 2020 Nov; 150:105191. Epub 2020 Sep 12.
- A qualitative systematic review of internal and external influences on shared decision-making in all health care settings. [JBI Libr Syst Rev. 2012] A qualitative systematic review of internal and external influences on shared decision-making in all health care settings. Truglio-Londrigan M, Slyer JT, Singleton JK, Worral P. JBI Libr Syst Rev. 2012; 10(58):4633-4646.
- Review Health professionals' experience of teamwork education in acute hospital settings: a systematic review of qualitative literature. [JBI Database System Rev Implem...] Review Health professionals' experience of teamwork education in acute hospital settings: a systematic review of qualitative literature. Eddy K, Jordan Z, Stephenson M. JBI Database System Rev Implement Rep. 2016 Apr; 14(4):96-137.
- Review Evidence Brief: The Effectiveness Of Mandatory Computer-Based Trainings On Government Ethics, Workplace Harassment, Or Privacy And Information Security-Related Topics [ 2014] Review Evidence Brief: The Effectiveness Of Mandatory Computer-Based Trainings On Government Ethics, Workplace Harassment, Or Privacy And Information Security-Related Topics Peterson K, McCleery E. 2014 May
Recent Activity
- The Patient Journey - Textbook of Patient Safety and Clinical Risk Management The Patient Journey - Textbook of Patient Safety and Clinical Risk Management
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Exploring the hospital patient journey: What does the patient experience?
Contributed equally to this work with: Raffaella Gualandi, Cristina Masella
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Writing – original draft
* E-mail: [email protected]
Affiliation Department of Nursing, Università Campus Bio-Medico di Roma, Rome, Italy
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft
Affiliation Department of Management Economics and Industrial Engineering, Politecnico di Milano, Milan, Italy
Roles Data curation, Formal analysis, Investigation, Project administration
Roles Conceptualization, Supervision
- Raffaella Gualandi,
- Cristina Masella,
- Daniela Viglione,
- Daniela Tartaglini

- Published: December 5, 2019
- https://doi.org/10.1371/journal.pone.0224899
- Peer Review
- Reader Comments
To understand how different methodologies of qualitative research are able to capture patient experience of the hospital journey.
A qualitative study of orthopaedic patients admitted for hip and knee replacement surgery in a 250-bed university hospital was performed. Eight patients were shadowed from the time they entered the hospital to the time of transfer to rehabilitation. Four patients and sixteen professionals, including orthopaedists, head nurses, nurses and administrative staff, were interviewed.
Through analysis of the data collected four main themes emerged: the information gap; the covering patient-professionals relationship; the effectiveness of family closeness; and the micro-integration of hospital services. The three different standpoints (patient shadowing, health professionals’ interviews and patients’ interviews) allowed different issues to be captured in the various phases of the journey.
Conclusions
Hospitals can significantly improve the quality of the service provided by exploring and understanding the individual patient journey. When dealing with a key cross-functional business process, the time-space dynamics of the activities performed have to be considered. Further research in the academic field can explore practical, methodological and ethical challenges more deeply in capturing the whole patient journey experience by using multiple methods and integrated tools.
Citation: Gualandi R, Masella C, Viglione D, Tartaglini D (2019) Exploring the hospital patient journey: What does the patient experience? PLoS ONE 14(12): e0224899. https://doi.org/10.1371/journal.pone.0224899
Editor: Rosemary Frey, University of Auckland, NEW ZEALAND
Received: July 10, 2019; Accepted: October 23, 2019; Published: December 5, 2019
Copyright: © 2019 Gualandi et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting Information files.
Funding: The author(s) received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
In the healthcare knowledge-based system, literature has given increasing attention over time to improving clinical knowledge, including by making use of the patient's insider perspective [ 1 – 3 ]. In particular, patient experience of healthcare and the delivery of care is emerging as an important area of knowledge, but one that is sometimes overlooked [ 4 , 5 ].
The Beryl Institute defines patient experience as “the sum of all interactions, shaped by an organization’s culture, that influence patient perceptions, across the continuum of care”[ 6 ]. Wolf et al. specify that interactions are “The orchestrated touchpoints of people, processes, policies, communications, actions, and environment” and patient perceptions are “what is recognized, understood and remembered by patients and support people”[ 7 ].
In the last few years, emphasis on the emotional drivers of engagements has led many authors to enhance the customer experience starting from an analysis of the customer journey [ 8 ]. In the hospital context, the patient journey is a key cross-functional business process where patient and providers share action and information flows between people and systems across various touchpoints. Providers aim to manage hospital patient flow in order to provide safe and efficient patient care while ensuring the best use of hospital resources (i.e.: beds, operating theatres, clinics and specialized staff). Poor patient flow may result in decreasing levels of productivity, increasing risk of harming patients and decreasing levels of quality perceived by patients [ 9 – 11 ]. Patients aim to receive the best care together with a high quality of service. As a matter of fact, the patient is the only actor who experiences the whole path by connecting each step of the journey. Therefore, hospitals can significantly improve the quality of the service provided by exploring and understanding the individual patient journey [ 12 – 14 ].
Many tools may be used to measure and understand patient experience [ 15 , 16 ]. Surveys are the methods mainly used to capture the patient experience and to evaluate the quality and safety of various clinical processes [ 17 , 18 ]. However, questionnaires or traditional static observation may not be well-suited to reveal all the aspects of patient experience [ 19 ]. In the complex hospital environment, multiple factors can affect the patient experience, including the time-space dynamics of the activities performed and the patients’ perceptions and emotions lived at the time of the experience [ 20 ]. Moreover, some authors emphasize that what the patient remembers is different from what he/she experiences in real-time, depending on the length of the recall period [ 21 , 22 ]. Therefore, as what the patient remembers may change over time, gathering accurate and immediate data on the experience lived also depends on the time of the interview.
A recent study reports how the use of unstructured diaries completed in a patient’s own words can capture the hospital-stay experience from the patient’s own perspective. However, it is not clear how real-time experiences are reported in relation to high-emotional situations or clinical activities that can interfere with the patient’s ability and willingness to write (i.e. during the transfer to the operating theatre or in the post-operative period, immediately after surgery). Furthermore, the authors show how study participants with a tertiary education wrote more in their diaries than those without [ 23 ]. This could potentially eliminate important aspects of the experience lived by vulnerable people.
Some authors have emphasized the value of shadowing for phenomenological research, by giving a more complete picture of the phenomenon in the real-time context of an organization [ 24 , 25 ]. Patient shadowing may have an especially valuable role in gaining insights into complex cross-hospital processes, in particular when dealing with vulnerable people who could be excluded from interview studies [ 26 , 27 ]. Furthermore, some studies have reported how, through shadowing methodology, it is possible to assess the lived experience of patients in a patient-centred perspective [ 28 , 29 ]. However, methodological and ethical issues of shadowing still need to be explored in greater depth [ 25 , 30 ].
While on the one hand patient experience is increasingly considered as a driver for health services improvement, on the other it is still not clear how to capture the whole patient experience in traversing hospital services [ 31 – 33 ]. Therefore, this study seeks to explore which aspects of the hospital patient journey experience may be captured by the three different standpoints: patient shadowing, health professionals’ interviews and patients interviews. Accordingly, it aims to answer the following questions: what does the patient experience through the hospital journey? How can it be captured?
Materials and methods
Study design.
This study was a qualitative study with a phenomenological‐hermeneutic approach using participant interviews and patient shadowing [ 34 , 35 ]. The Consolidated Criteria for Reporting Qualitative Research—COREQ checklist was used as a guideline to report the study data [ 36 ]. The study was undertaken in a 250-bed Italian academic teaching hospital. Orthopaedic patients undergoing total hip (THA) or knee arthroplasty (TKA) were selected in order to analyse a standard clinical path ( Fig 1 ). Urgently admitted patients were excluded due to the different clinical path they have to follow. The unit of analysis was the hospital patient’s journey starting from the first outpatient visit and concluding with the first follow-up visit. The study was approved by the Hospital Ethics Committee.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0224899.g001
Data collection
Between August 2016 and April 2017, a total of twelve patients and sixteen key professionals were invited to participate and all agreed. There were no prior relationships between researchers and patients; two researchers knew some healthcare professionals because they worked in the same hospital, though in different units and without patient care roles. The possibility of coercion was minimized by guaranteeing data anonymity, by requesting voluntary participation in the study and by dealing with issues on which the researchers had no power to influence anything or anyone at hospital managerial level.
A convenience sample of patients was selected based on whether their inpatient admission and follow-up visit fell within the observation period. Inclusion criteria were: patients scheduled to undergo surgery for THA or TKA, for the shadowing phase; patients who had had a THA or TKA ad were in follow-up, for the interviews. Exclusion criteria were: <18 years, inability to understand, not wanting to participate, inability to read/speak Italian. Patients were asked to participate in the study at the time they arrived in the hospital. The first author invited patients to participate in the study when they met at the hospital for preoperative tests or on the day of admission. Patients accepting the invitation were provided with further information about the project by the first author, and were asked to sign their consent to participate in the study and to the anonymous use of their data.
Eight patients admitted between August and September 2016 were selected for the shadowing phase. A shadowing methodology was used in order to provide an embodied understanding of patients’ experiences in context [ 26 ]. Two female students from the nursing and industrial engineering degree courses, with no roles in the delivery of patient care, were trained for data collection by the first author. In this way, the risk of not reporting negative feedback during the study by the participants, and subjective interpretations by the authors in capturing data, was minimized. Patients were shadowed from the time of hospital admission to the time of discharge, with the shadower observing the patient during daytime hours and completing a data collection form prepared by the research group. This involved recording every step of the hospital journey process, by analysing each touchpoint and including time, patient, caregiver, activity, shadower’s observations, and impressions. In particular, touchpoint observations indicated where patients and families go (setting), with whom they come into contact, how long the experience at each touchpoint takes (time), what patients and caregivers do, and a description of any comments of the patient and family, including any observable emotional state of the patient. By considering patients’ emotion as consistent responses to internal or external events, the Plutchik’s model was used as framework to understand its intensity in a positive or negative characterization [ 37 ]. In particular, Plutchik suggests emotions are low, medium or high-intensity, and if left unchecked, they can intensify. Accordingly, the patient's emotional journey was also assessed in reference to external events that altered the patient's emotional level.
Patient care procedures were not noted because they were not relevant for the current research objectives. The shadower observed the patients during all hospital transfers and entered the patients’ rooms only to verify their general state and to gather any statements about their experience. The shadower was mainly passive during the observation, but was active in informal conversations. This level of proximity made it possible for the patients not to perceive shadowers as intrusive or disrespectful of their privacy.
Between September 2016 and April 2017, four patients and sixteen healthcare professionals participated in face-to-face open interviews lasting 30–45 minutes and performed by the first and the third author. A few main open questions were identified by the research group in order to analyse the main steps of the patients’ journeys, the patients’ experiences, and their reported emotions. Patients were interviewed at the first outpatient follow-up visit ( Fig 1 ), scheduled one month after discharge from the ward, in order to include their perceptions of discharge.
In order to capture viewpoints representing various different roles, a collaborative purposive sampling technique was used among professionals with different level of professional experience who take care of orthopaedic patients. In particular, according to Benner’s stages of clinical competence [ 38 ], two nurses with experience of at least five years, identified as expert nurses by their managers, and three nurses with experience of up to four years, identified as competent nurses, were selected. In addition, two orthopaedic surgeons and one medical doctor under training were involved. Finally, three members of the administrative staff, the director responsible for the quality of care processes, and the head nurses of the units involved in the patient journeys (i.e.: two Ward Units, one Surgery Room, one Rehabilitation Unit), were interviewed.
All interviews were audio-recorded and transcribed verbatim with participant permission. Data from the field notes and the interviews were transferred to an Excel spreadsheet database to systematize them and for the subsequent analysis.

Data analysis
Data analysis was performed on three levels as suggested by Ricoeur [ 30 ]: a naïve reading, a structural analysis and a critical analysis and discussion. The first author performed a thematic analysis of the text material. In the structural analysis, the units of meaning (what was said) were reflected in units of significance (what the texts were talking about) from which the key themes emerged ( Table 1 ). Patients’ emotions, reported or observed, were classified according to Plutchik’s Wheel of Emotions [ 37 ]. After that, a critical analysis was carried out by the researchers in order to analyse the coding process, the categories and the meanings that emerged.
https://doi.org/10.1371/journal.pone.0224899.t001
The main characteristics of the participants involved in the study are reported in Table 2 . Patients involved ranged in age from 56–78 years with an average age of 67.3 years, and they were hospitalized on average 4.4 days. All had a regular clinical trajectory with no noteworthy complications. Healthcare professionals ranged in age from 29–61 years with an average age of 38.8 years and a work experience average of 10.6 years.
https://doi.org/10.1371/journal.pone.0224899.t002
The hospital patient journey
In the patient hospital journeys studied, seven main phases and forty-four consequent steps were traced by shadowing patients and interviewing the main actors. Table 3 shows which steps were identified from the interviews and which from the shadowing. In particular, the patient shadowing enabled more accurate reconstruction of all the steps, compared to what patients narrated after a period of time. This information can be obtained from the health professionals' interviews only by summarizing their different points of view. Furthermore, through shadowing it was possible to detect that within the hospital the patient went through eighteen different places and was in contact with more than fifty different health professionals. The patients’ emotions as reported by the health professionals corresponded to what was observed by shadowing, but they did not match the general state of serenity reported by patients when interviewed.
https://doi.org/10.1371/journal.pone.0224899.t003
The three different standpoints, (i.e.: patient shadowing, healthcare professional interviews and patient interviews) allowed different issues to be captured at the various phases of the journey. In particular, the shadowing was able to capture the 'connections' between one stage and another of the journey, such as movement from admissions to the ward and transport from the ward to the operating theatre, while the journey narrated by each professional and patient allowed the most significant touchpoints to be identified ( Table 3 ).
When interviewed about a month after discharge, patients remembered a generally positive experience, linked specifically to the success of surgery and to a good relationship with the professionals. They showed appreciation and satisfaction and they declared that there were no major problems to deal with. One patient reported "I was fine , look , I have to say the night of the surgery I was fine , the next day they also made me get up . They made me sit in the chair , my head was spinning a little , so it's not that ehm … then nothing else , everything else went well” (Patient 1); Another reported “What can I say ? Better than that I don't think it is; that… we may be worse , but I have not found that I was worse , and I have only good things to say about the professor and all his assistants” (Patient 3).
However, when shadowed, some discrepancies emerged. When going independently to the ward patients experienced confusion and anxiety, due to not having clearly understood indications, and to the waiting times before entering the assigned ward (Patient 5, 6, 7, 8, 9,12). Another critical step was the transfer and waiting in the operating theatre. They felt 'lost' when they were transferred and emotions of fear and anxiety emerged (Patient 10; 11). These experiences also emerged from the interviews with professionals (Healthcare professional 4, 6, 8, 12, 14 16).
Some other interesting points, detected by the shadowing, reveal how the hospital environment and management of patient flow can affect the patient experience, in particular on the day of admission. After the administrative acceptance, one patient took the wrong elevator and did not immediately reach the indicated ward. When arriving at the entrance of the ward, he found it difficult to use the intercom. When entering the ward, he was dissatisfied with the lack of staff to welcome him. When waiting in the room for surgery he showed apprehension and he reported a desire to have more information and to have a family member nearby (Patient 9). Another patient reported having received incorrect information to reach the ward and that the hospital directional signs were too small and difficult to read (Patient 1).
During the journey it is possible to identify some key steps, though with different levels of importance from patients’ and professionals’ perspectives. From the patient perspective and by shadowing the journey, the day of hospitalization was the most critical, and they experienced mainly negative emotions (Patient 5, 6, 7, 8, 9,12). From the interviews with the professionals it emerges that when returning to the ward after surgery patients were calm (Healthcare professional 7, 8, 16) but in the following days, they began to experience a lack of autonomy and this could make them nervous (Healthcare professional 13). Professionals involved in the pre-hospitalization phase report that waiting in the days before hospital admission can negatively affect patient experience. Patients can feel abandoned, if no one gives them information on the outcome of the outpatient clinic examination, or if all the procedures related to hospitalization are not properly programmed (Healthcare professional 1, 9).
Through analysis of the data collected four main themes emerged underlying both the shadowing and the interviews: the information gap; the covering patient-professionals relationship; the effectiveness of family closeness; and the micro-integration of hospital services.
The most significant issues are reported below.
The information gap
When interviewed, patients did not mention any problems with the information received in the course of their hospital journey. However, when patients were shadowed on arrival at the hospital, they did not seem to be aware of any information regarding their hospitalization (e.g. visiting hours for family members, the hospital route to the ward), but asked the first professionals they met. The patients seemed lost, especially after going through the admission process and on looking for their assigned wards. Moreover, when they arrived in the ward they needed information about their hospitalization, but healthcare professionals did not immediately assist them (Patient 5, 6, 9). This seemed to contribute to their state of anxiety about the surgery. This issue is confirmed by what the professionals reported. When they arrive at the hospital, patients put the same questions to any professional they come into contact with (Healthcare professional 4, 6). A nurse reports how each patient has "so many anxieties , fears , uncertainties , questions , as soon as he steps into the ward and I follow him , until he leaves the ward" (Healthcare professional 1). A head nurse reports "Family members also ask many questions . Many times it seems that what was already explained by the doctor , actually , has not sunk in ( … ) And so here they repeat the same questions many times , in different ways . What worries them a lot ( … ) is what will happen after discharge , when ‘I find him at home or in a rehabilitation clinic’” (Healthcare professional 13). Apprehension before surgery was observed in one patient, even though the patient claimed to have received very good information on how the surgery would be performed (Patient 2).
The time of waiting while the patient is in the operating theatre seems endless for family members, and waiting without information is a cause of anxiety (Healthcare professional 6). Professionals recognize the importance of informing the patient and family members about procedures, clinical pathways and pain management, before surgery (Healthcare professional 1, 2, 4, 7).
The covering patient-professionals relationship
The relationship between patient and professionals is a key issue for the quality of the service perceived by the patient, even when the health care provider fails to respond immediately to the patient's needs. Indeed, as many as 35 touchpoints occur throughout the patient journey ( Table 3 ). What the patient thinks and feels on this topic, emerges especially from the interviews, while the shadowing is not able to immediately capture thoughts or observations re-elaborated by the patient. In particular, when interviewed the patients remember, even after some time, some aspects of the relationship with professionals that are not directly related to clinical care, but which are perceived as being of value for the patients, since in these they receive attention as an individual. Even after some time, a patient remembered: “Early in the morning the nurse came to say goodbye before she went off duty , because I was being discharged later that day , so she wouldn't see me again . Really good . ” (Patient 3). A patient also remembered a rough response to a request for help to get dressed after the X-ray during outpatient clinic examination (Patient 2). Moreover, a patient pointed out how reassuring the relationship with the surgeon could be just before the surgery (Patient 3). One of the key moments appears to be the contact with the anaesthesiologist and the surgeon while the patient is waiting in the operating theatre: “Then the anaesthesiologist told me ‘Don’t worry , my dear , we do the epidural , we will sedate you’” (Patient 1). From the professionals’ perspective, the relationship with the patient is a key point to "buffer" a series of disruptions in the hospital journey and to reassure the patient: “ Patients always thank us because even if there is a gap in the organization and the patient has to wait a little , we apologize in the best way , with a smile" (Healthcare professional 3). As the nurse is the first person patients encounter when entering the ward, she knows she has the important role of reassuring patients by explaining to them how to orientate themselves in the ward and which procedures will be carried out, even if patients should already have been informed about all these things (Healthcare professional 4). Professionals recognize the importance of calming patients through interaction with the surgeon especially when they are waiting just before surgery (Healthcare professional 3, 13). An orthopaedist reports, “When you check or welcome the patient in the operating surgery where the surgeon and the anaesthesiologist are , the patient sees them and this helps him or her a lot , and so one thing that I think is in our favour ( … ) is communication , the possibility of having a point of reference” (Healthcare professional 3).
The effectiveness of family closeness
Family closeness is felt to be important for both patients and professionals, if programmed at the right times of the clinical journey. From the patient interviews and from shadowing it emerges that patients like family members to stay with them when waiting for surgery (Patient 4, 9). Once the surgery has been performed, when fears are diminished and pain is controlled, patients do not consider the presence of family members necessary, in particular immediately after returning to the ward from the operating theatre (Patient 1, 4). From the shadowing it emerges that after the first few days, when patients have recovered from the post-operative stage and close assistance has diminished, they then like to be with their family without interruptions for clinical-assistance reasons (Patient 10).
For professionals, family presence is important especially shortly before and after surgery, to reassure family members that the patient is doing well (Healthcare professional 5, 7, 13). When possible, professionals try to facilitate this, even outside regular visiting hours (Healthcare professional 13). In the days after surgery, “It is mainly relatives who come from outside the city who logically stay here , maybe in a hotel or some bed & breakfast , and would like to stay in the room all day; because they say–quite rightly , as I realize– : ‘But I have nothing else to do; my husband , my wife , my son is there . I'm with him’” (Healthcare professional 12). At this stage of the clinical journey, professionals do not see the closeness of family members as a need of the patient. Immediately after surgery, patients prefer to rest rather than having many people in their room. Conversely, the presence and closeness of family can greatly affect the patient experience in the rehabilitation period, especially when it comes to discharging elderly patients (Healthcare professional 15).
The micro-integration of hospital services
Even for a relatively simple routine surgical pathway, patients go through multiple stages. The behind-the-scenes coordination remains invisible to them and they are able to capture only some of the effects related to it. By contrast, professionals emphasize many critical issues in the management of the patient journey that affect the patient's experience.
When interviewed, patients reported the difficulty of having to move from one clinic to another during the outpatient clinic examination (Patient 1). Before hospital admission, an admissions office administrator shows how necessary it is to “decrease calls to the patient ( …), also depending on their age which is on average quite advanced …. cut out some calls that often from their point of view are unconnected . For instance , on one day I call you for admission , then the doctor calls you for blood tests , then another doctor calls you to arrange the meeting ( …), then if you take cardioaspirin the doctor calls you to give you information on cardioaspirin … All these calls could be grouped into maybe one by the doctor and one by the administrative staff” (Healthcare professional 10). At the time of hospital admission some critical points are revealed by the shadowing. After arriving at the hospital, patients waited an average of 21 minutes before being taken in charge by the Administrative Office to carry out admission procedures. At the end of the administrative registration procedures, patients made their own way to the ward, taking an average of 11 minutes. In this time, patients could get lost; they experienced anxiety about not getting to the right place, and waited outside the closed door of the ward without knowing what to do (Patient 5, 6, 7, 9). During their hospitalization, patients reported a lack of communication: a drug intolerance reported in their previous admissions had not been recorded in the notes. Orthopaedists reported critical issues concerning the management of operating theatres, such as delays in transporting patients from the ward to the operating theatre or delays in preparing the operating theatre for the next operation (Healthcare professional 2, 3). The accumulation of such delays could lead to the cancellation of the last scheduled patient, with a negative impact on the patient who had been waiting in a state of anxiety for many hours (Healthcare professional 2). A head nurse reported that waiting for transport to and from the radiology department for the post-operative radiography could slow down all the care processes, make the patient wait unnecessarily, and increase the pain, due to the temporary suspension of the continuous-infusion pain-killer (Healthcare professional 12). Finally, a patient reported that she was offered no choice when she was transferred to the rehabilitation unit recommended by the doctors, and she expressed the desire for a follow-up visit by the same doctor who had operated on her (Patient 1).
Exploring the individual patient journey can lead healthcare organizations to improve patient experience by focusing on the patient perspective, rather than the provider perspective [ 39 ]. Understanding what organizations can do to improve patient experience is critical [ 40 ]. However, the literature is still exploring the best methods to capture the patient's experience [ 17 , 23 , 30 ]. This study deals with the lived experience of orthopaedic patients by capturing the different points of view of patients and professionals on individual hospital patient journeys. Patients’ reported experience is analysed by shadowing them during hospitalization and by interviewing them at the end of the whole journey.
Historically, researchers and health care managers have focused on the study of how to achieve effective care through the definition of clinical pathways and by increasing patient adherence to treatment. However, reducing the patient's path to the clinical perspective may fail to reveal aspects that are relevant to patients, that influence their experience and their perception of quality of service [ 42 , 42 ]. In this study on patients’ hospital journeys, some important issues emerged through the shadowing of the hospital journey of the patients, and interviews with the key players. With the integrated use of these methods it was possible to identify which touchpoints are most critical for the patient, when family closeness is most effective, and how professionals can provide for the needs shown by patients over the entire journey. If on one hand the study of clinical pathways is now heading towards the active involvement of patients in decisions related to their own health issues [ 43 ], on the other hand the analysis of the hospital journey from a patient perspective can lead organizations to improve cross-hospital processes by creating procedures and focusing healthcare professionals on overall patient experience.
In line with Liberati's analysis [ 30 ], the shadowing method can contribute to patient-centredness by considering all the aspects of service delivery, not just the clinical one. In this study, both interviews and shadowing are able to “see the world from someone else’s point of view” [ 24 ]. However, the patient’s observations, focused on the whole service experienced, can reveal areas of potential improvement of the patient experience not otherwise identifiable. Shadowing highlights what the patient experiences in the different contexts and when going through one service and on to another, which professionals do not see since this falls outside the scope of their direct responsibility. Moreover, unlike using diaries completed by patients [ 23 ], this methodology allows the patient to be observed in the moment and in the spaces in which the relationship with the professionals takes place. However, this necessarily determines a subjective interpretation of what the researcher observes with respect to what the patient affirms.
Unlike what was pointed out by Gill [ 44 ], when dealing with the patient journey perspective, shadowing has an important potential for revealing invisible steps and spaces of the journey, more than intimate spaces and micro-processes of the decision. It is true that even now, in the healthcare sector, the provider establishes the patient path, while the patient is 'carried forward' through processes designed and managed by others.
In this study, when interviewed after time, patients focused on the overall clinical experience, forgetting other issues related to their hospitalization. For example, when interviewed, patients reported that they had had all the information they needed, while when shadowed shortly before the surgery the same patients appeared lost and asked for information from all the professionals they met. These data are also confirmed by interviews with professionals, who reported how highly emotional touchpoints, such as telling the patient they needed an operation, or the time immediately before transfer to the operating theatre, may affect patients’ perceptions and the effectiveness of the information [ 41 , 45 ]. As suggested by Ziebland, there is a difference between what patients said they experienced and what they actually experienced in real-life settings [ 20 ]. In this sense, the use of shadowing helps to understand the experience in a real time context. Moreover, it is always useful to evaluate whether the tools and information methods used for giving information to patients are effective, and which is the best moment for each patient to receive all the information they need, by considering their ability to absorb the information in a stressful situation [ 46 – 48 ].
In this study, both patients and professionals recognized the value of a personalized relationship in improving patient experience. Moreover, professionals report how a good relationship with the patient can compensate for the organization's inefficiencies. Interaction with the patient is especially important in the perceived patient-critical touchpoints. However, relevant steps of the journey are different from patients’ and from professionals’ points of view. From the patient’s point of view, the most critical steps occur when entering the hospital and just before surgery, where their emotional involvement is greater. On the other hand, from the professionals’ point of view, planning hospitalization and preparing patients for surgery is one of the most critical steps that affect patient experience. Indeed, patients, when interviewed, seem not to perceive critical issues in what happens ‘behind the scenes’, while professionals are able to identify issues related to the organization that can positively or negatively affect patients’ experience. These results highlight how frontline professionals are the key players in transforming organizational procedures into personalized care pathways, but the misalignment of views should be considered when improving the hospital journey by including the patients’ perspective.
The study has important limitations with respect to the sample and the setting considered and therefore its potential for generalization may be limited. The issues that emerged would need to be studied in depth in different care settings and with other types of patients to allow comparison of data and methodologies.
Patients’ experiences have become increasingly central to assess the performance of healthcare organizations and to redesign the services around the real needs of patients [ 20 , 41 , 42 , 45 , 49 ]. In this study, the analysis of the hospital journey from the patient perspective and the integration of three different standpoints, patient shadowing, healthcare professional interviews and patient interviews, highlights important areas of improvement otherwise hidden by the analysis of the clinical pathway only.
The nature of the study and its originality by subject matter and methods adopted can stimulate both academics and healthcare managers to explore important new fields. On the one hand, it is important to further investigate methodologies for capturing the patient experience and use it deeply and effectively at various organizational levels. In this way, shadowing seems to give a more patient-centric perspective, but it raises questions about its effectiveness as a single methodology for gathering the whole patient experience within a complex hospital process. On the other hand, the results of this study are a starting-point for healthcare managers who want to improve a key cross-functional hospital process in which the patient is the main actor. By considering the overall patient experience, as well as services performance and clinical pathways, they will able to create a distinctive value both for the patient and for the organization.
Acknowledgments
We are grateful to Eugenia Di Sabatino and Michela Ceri for their contribution to data collection.
- View Article
- PubMed/NCBI
- Google Scholar
- 6. The Beryl Institute Website, Defining Patient Experience. Available from: http://www.theberylinstitute.org/?page=DefiningPatientExp . Accessed April 20, 2019
- 10. Litvak E. Managing Patient Flow in Hospitals: Strategies and Solutions, Joint Commission Resources; 2nd Ed. Eugene Litvak Editor; 2010.
- 11. The Health Foundation. Improving patient flow. Learning report. The Health Foundation, 90 Long Acre, London WC2E 9RA; 2013.
- 19. Czarniawska B. Shadowing and Other Techniques for Doing Fieldwork in Modern Societies. ISBN: 978-91-47-08780-8. Liber/Copenhagen Business School Press; 2007.
- 20. Ziebland S, Coulter A, Calabrese JD, Locock L. Understanding and using health experiences. Oxford University Press; 2013.
- 37. Plutchik R. The Nature of Emotions: Clinical Implications. In: Clynes M., Panksepp J. (eds) Emotions and Psychopathology. Springer, Boston, MA; 1988.
- 38. Benner P. From novice to expert: Excellence and power in clinical nursing practice. Menlo Park: Addison-Wesley:13–34; 1984.

What is palliative care? A patient’s journey through the system
Research Fellow, Palliative Medicine Physician, Monash University
Research Fellow, Department of Medicine, The University of Melbourne
Professor, VCCC Chair of Palliative Medicine, The University of Melbourne
Disclosure statement
Anna Collins receives research funding from Victorian Cancer Agency and the Bethlehem Griffiths Research Foundation.
Jennifer Philip receives funding from Victorian Cancer Agency, Bethlehem Griffiths Research Foundation
Matthew Grant does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
Monash University and University of Melbourne provide funding as founding partners of The Conversation AU.
View all partners
This article is part of our series on demystifying palliative care , where experts explain the process of end-of-life care in Australia.
A diagnosis of a serious illness has a multitude of consequences. There may be significant symptoms related to the disease such as pain, breathing difficulties, nausea, fatigue and weakness.
Such illnesses often limit a person’s ability to do the shopping and chores, attend the many medical appointments required, and can potentially lead to social isolation.
What is palliative care?
Rebecca lived with her husband, Rob, and six-year-old son, Jack. She was 34 when she met the palliative care doctor, after being diagnosed with a particularly aggressive lung cancer. She had undergone extensive surgery and was due to have radiotherapy and chemotherapy. She was struggling with some ongoing pain after her operation.
Her cancer doctor suggested she see the palliative care team to help manage her pain so she could cope better with the next steps of her cancer treatment.
According to the World Health Organisation , palliative care
improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual.

In Rebecca’s case, palliative care was recommended for the additional issues she had associated with her treatment. Palliative care involves a team of doctors, nurses, allied health and other volunteers who work together to provide an extra layer of support to the person and their family.
Palliative care teams are commonly involved with illnesses such as heart, lung or kidney disease, cancer or advanced dementia. Involving palliative care allows for better control of symptoms and an improved sense of quality of life. It also helps the family of the person who is ill. With better symptom control and support, this frequently translates to less time spent in hospital.
A number of studies have even shown early involvement of palliative care can lead to improved survival .
Read more: Palliative care should be embraced, not feared
Palliative care doctors
Rebecca attended an appointment to meet one of the palliative care doctors at the cancer centre. The doctor explained his expertise in pain control and Rebecca felt comfortable with his proposed management plan.
Rebecca’s palliative care doctor changed her medications slightly to address her pain. They also talked about her diagnosis, how it had thrown her life upside down and the treatment planned.
Rebecca spoke of being determined, scared and keen to hold a sense of routine for Jack, who was just starting school. Over the next few months, Rebecca saw her palliative care doctor once or twice just to check in. But mostly she was busy with her cancer treatments and her pain was now pretty stable.
A few months later Rebecca rang the hospital asking to see the palliative care doctor because her pain seemed to be getting worse. On assessment, this pain was different, with a number of concerning features. Together with Rebecca’s oncologist, more scans were ordered. These revealed her cancer had returned and spread to many parts of her body.
Rebecca’s palliative care doctor altered the pain medications, including prescribing a drug that targets nerve pain. The medications were slowly increased over time to reduce the chance of side effects such as drowsiness. After two weeks, Rebecca felt the pain was well controlled, and she was back doing the things she wanted to focus on at home.
Palliative care doctors are specialist physicians skilled in treating symptoms associated with serious illnesses such as pain, nausea, fatigue and appetite problems. A key component of their role is facilitating difficult discussions about prognosis, stopping various treatments and exploring the medical decisions a person would want at different stages of their illness.

Palliative care experts work closely with other health professionals , such as oncologists, cardiologists, psychologists and social workers, to address all the effects of a serious illness. This may include ordering investigations and scans, through to organising community services (such as personal carers) or walking aids, and providing support for family and carers.
Guidance through difficulties
However, one thing after another was happening for Rebecca with her cancer. She was admitted to hospital at least twice as a result of complications from her cancer or its treatment. She felt like she was not getting much time to draw breath between each event.
Rebecca knew her palliative care doctor pretty well by now. They had some conversations that helped focus how Rebecca wanted to spend her energies. When her palliative care doctor asked, given all that was happening, what was important for her, Rebecca had two hopes.
She still wanted to fight and stay hopeful of beating or, at least, holding her cancer at bay. And, after some thought, Rebecca quietly offered that even more important was being a great mum.

The next couple of months were pretty stormy. Rebecca was feeling much weaker and was increasingly spending time on the couch or in bed. She was clearly nearing the final part of her life.
At her wish, Rebecca decided to try yet another new form of chemotherapy, but also spent some time talking to her palliative care doctor and formulating a clear plan that she wanted to be home with Jack. If or when further problems came, she wanted to remain at home. She had already been linked in to community palliative care supports some time earlier, so knew these nurses well and trusted them.
Read more: Take control over the end of your life: what you need to know about advance care directives
One of the nurses from the community palliative care team offered their support in helping talk to Jack about what was going on for his mum. Rebecca felt relieved knowing there was someone to help with this.
Palliative care services at the end of life
As things worsened, the palliative care nurses were visiting her every day and, recognising the change, they contacted the palliative care doctor, who also went to see Rebecca at home.
It was a cold, rainy day. The house was warm and Rebecca was in a bed set up by the glass windows in the living area. Her husband Rob and two sisters were sitting nearby at the kitchen bench having a cup of tea. Her cat was lying close beside her. Jack was leaning up against his mum’s bed doing some colouring.

The palliative care doctor didn’t stay long. Rebecca was mostly sleeping and only waking for moments every now and again. They spoke just a little – she seemed comfortable. Rebecca died a few days later. According to the nurses, she became sleepier, until she didn’t wake at all in her last 12 hours.
Palliative care is provided in many settings. This may include hospital or private clinics, as a medical team in the hospital, in a palliative care unit or hospice, or in the community. GPs are often an integral component of this team.
Read more: Assisted dying is one thing, but governments must ensure palliative care is available to all who need it
Community teams involve specialist nurses, doctors and other health professionals, and visit patients’ homes for regular assessment and care. This might mean providing equipment such as a comfortable hospital bed, visiting doctors and nurses to oversee medications and ensure a person experiences minimal pain, or talking with children about death .
These services often provide 24-hour phone support or urgent assessment in the home as things pop up or possible concerns arise. Unfortunately, access to these services and the expertise available are hugely variable, especially in rural and regional areas.
Between 60-70% of Australians wish to die at home, yet only 14% do , with 54% of people dying in hospitals. Having discussions in advance about a person’s priorities if their health worsens, and the care people might want including where they would like to be, may enable planning for these eventualities.
While these discussions are painful and frequently difficult, with clear plans in place, like Rebecca was able to make, palliative care helps people stay at home and, for many, to die at home.
Read more in the series:
It’s not all about death: conversations with patients in palliative care
Palliative care for children often involves treating the whole family
Looking after a dying loved one at home? Here’s what you need to know
Five common myths about palliative care and what the science really says
- End-of-life care
- Palliative care
- Terminal illness
- Death and dying
- End of life
- Demystifying palliative care

Faculty of Law - Academic Appointment Opportunities

Executive Dean, Faculty of Health

Regional Engagement Officer - Shepparton

Lecturer/Senior Lecturer, Earth System Science (School of Science)

Sydney Horizon Educators (Identified)
- Prognostic Significance of CAD-RADS in Suspec
- Low vs High Blood Pressure Targets in Critica
European Immunization Week: Challenges and...
- Engaging Pharmacists in Atrial Fibrillation...
- Navigating Connectivity Challenges in Hospita

Moderna's AI Revolution: Transforming Healthc

Optimising Healthcare: The Power of Value...

Toward Greener Anaesthesia Practices: Mitigat
Seven steps to the ‘perfect patient information journey’.
- Wed, 7 Nov 2018
HealthManagement, Volume 18 - Issue 6, 2018

Leadership comes first.
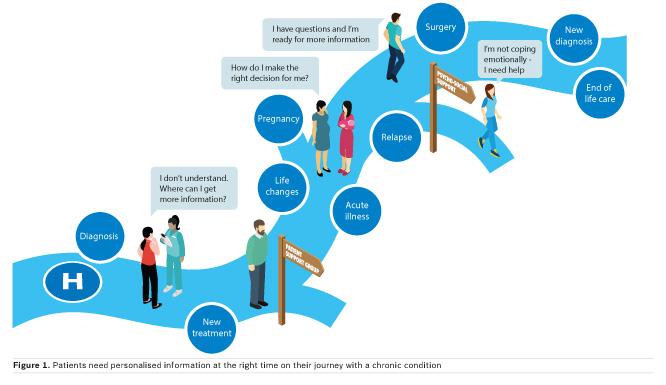
- Shared decision-making
- Long-term conditions care and support planning
- Patient choice
- Social prescribing
- Patient activation
- Personal health budgets
Why healthcare information?
Patients’ responsibilities and rights, what needs to change, the perfect patient information journey.

Leadership is critical
- Who will lead the seven-step process?
- Who can review available patient information sources from other sources and approve them?
- Who will be responsible for embedding patient information within care pathways?
- Who will make sure all staff know what is available?
Learning from pilots
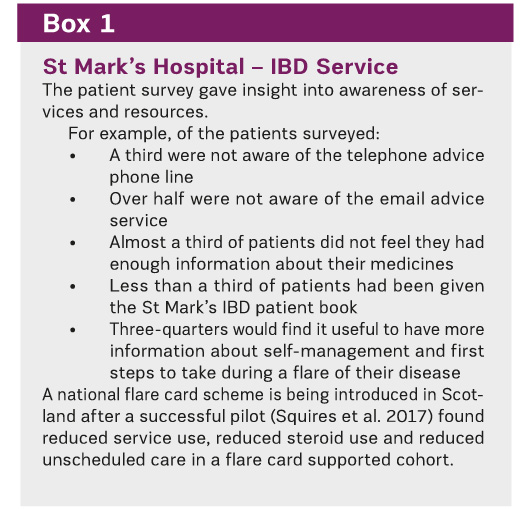
Ensure delivery of patient rights to information
- Patient information is a management issue, it can improve outcomes and reduce service use if people are empowered to self manage.
- Patient information underpins the six pillars of personalised care
- Patients report being uninformed about their care and only 56% of hospital in-patients felt involved in decisions about treatment
- Ensuring information is health literate makes services accessible and helps tackle inequality
- PIF has developed a 7-step process to deliver a perfect patient information journey
- If the NHS wants people to take more responsibility for their health it needs to provide or signpost information they can use and act upon
Conflict of interest
«« Why doctors need leadership training
What's taking so long? Smashing population health silos »»
References:
Care Quality Commission (2017) Adult inpatient survey 2017. Available from cqc.org.uk/publications/surveys/adult-inpatient-survey-2017
Coulter A, Collins A (2011) Making shared decision-making a reality: no decision about me, without me. London: The King’s Fund. Available from kingsfund.org.uk/sites/default/files/Making-shared-decision-making-a-reality-paper-Angela-Coulter-Alf-Collins-July-2011_0.pdf
Department of Health and Social Care (2012) NHS Constitution for England. Available from gov.uk/government/publications/the-nhs-constitution-for-england
Duman M et al. (2015) Is knowledge power? Using information and support to empower patients. London: Patient Information Forum. Available from pifonline.org.uk/wp-content/uploads/2015/03/ Is-knowledge-power.-Using-information-and-supportto-empower-patients.pdf
National Institute for Health and Care Excellence (2016) Shared Decision-Making Collaborative, A Consensus Statement. Available from nice.org.uk/Media/Default/About/what-we-do/SDM-consensus-statement.pdf
NHS England (2017) Personalised care framework. Available from england.nhs.uk/personalised-health-and-care-framework
Patient Information Forum (2013) Making the Case forInformation: the evidence for investing in high-quality health information for patients and the public. Available from pifonline.org.uk/wp-content/uploads/2014/11/PiF-Case-for-Information-Report-Final-Full-Report.pdf
Squires SI et al. (2017) Implementing a self-management strategy in inflammatory bowel disease (IBD): patient perceptions, clinical outcomes and the impact on service. Frontline Gastroenterology 8(4): 272-8.

Sue Farrington
Related articles, is blockchain impacting the healthcare arena, blockchain solves healthcare data obstacles, who stands to benefit from healthcare blockch, how blockchain will transform healthcare, latest articles, decision-making in the icu.
- Journal Article
Decision-making in the ICU is a multifaceted process that involves clinical assessment, collaboration among multidisciplinary teams, ethical considerations, evidence-based practice, communication, and continuous adaptation to evolving clinical scenarios. Balancing the complex factors requires
Dealing With Uncertainty in ICU Decision-Making: A Practical Guide
When the stakes are high, and the path ahead is uncertain, the decisions made, especially if a patient continues to worsen, can be sources of self-torment and can haunt us for a long time. Our goal is to suggest ways to steer decision-making for intensivists in the face of uncertainty by prop
The Least Bad Decision: Crisis Standards of Care After the Pandemic
COVID-19 was an emergency that lasted for years and left few regions of the world untouched. The pandemic shone a spotlight on both the strengths and weaknesses of our disaster planning. What worked, what did not, and how can we better plan for future emergencies? The COVID-19 pandemic fo
Latest News

- Movers & Shakers

Younes Ammari Joins Moment* as Medical Prompt

Ameenay Khan is Appointed as Manager of Healt

Tye Farrow Honored with Salutogenic Project...

Stanford Medicine Children’s Health Welcomes...

KnowledgeLab 2024

34th Conference Of EWMA 2024

Second EVSS Regional Leading Vascular Science

ESMO Preceptorship on Colorectal Cancer 2024

ESMO Preceptorship on Supportive and Palliati
- Advertising
- Submit Article
- Author Guide
- Privacy Policy
- Cookie Policy
- Terms and conditions
- Copyright and permissions
- Editorial Board
- White Papers & Case Studies
- IMAGING Highlights
- ICU Highlights
- EXEC Highlights
- IT Highlights
- CARDIO Highlights
- HealthManagement
- ICU Management
- (E)Hospital
- Imaging Management
- Imaging Management French
- Healthcare IT
- Cardiology Management
- IQ - Interventional Quarter
- List your event
- Past Events
- International Association
- National Association
- Universities - Institutions
- Guest Posts
- I-I-I DigiFlash
Communities
- Decision Support
- Women's Health
- Enterprise Imaging
- Artificial Intelligence
- Finance Management
- Cybersecurity
- Sustainability
- Digital Transformation

Rue Villain XIV 53-55
B-1050 brussels, belgium, tel: +357 86 870 007, e-mail: [email protected], emea & row office, 166, agias filaxeos, cy-3083, limassol, cyprus, headquarters, kosta ourani, 5, petoussis court, 5th floor, cy-3085 limassol, cyprus.
- Find Providers
- Medical Services
- Get Care Now
- Schedule an Appointment
- Find a Career
- Log in to My IU Health
- Thrive by IU Health
- We are IU Health
- Patient Stories
- Health & Wellness
Philanthropy-funded murals offer deep meaning for patients and caregivers at Schwarz Cancer Center
April 26, 2024, iu health north hospital.
“When a patient completes a journey through cancer treatment, they’ve gotten through something very hard. That’s not just their success,” says Ann Bredensteiner, manager of integrative health and supportive care at IU Health Joe and Shelly Schwarz Cancer Center . “It’s also the success of their family, their caregivers, and all the people who worked so hard to get them to that point. They’ve also left a lasting impression on our hearts.”
To capture those impressions, patients at Schwarz Cancer Center have a new way to celebrate the completion of their journeys through radiation treatment. Schwarz Cancer Center team members tapped local visual artist, Skye Smith to create a series of five similar paintings of trees. Smith’s trees start off with bare branches. Over time, patients will add thumbprint leaves marking the completion of their treatment at Schwarz Cancer Center. Donors to IU Health Foundation contributed the funds for the murals.
“I love that this project will continue to evolve,” Smith said. “It’s such a collaborative artwork. There’s something magical about being able to tangibly mark the end of a treatment and the beginning of a new chapter. When patients put their fingerprints on the trees, I hope they see and feel a sense of connection with patients who came before them.”
Erica Pitcock, supervisor of radiation oncology at Schwarz Cancer Center, first shared the idea for the trees after she saw something similar at another cancer center. Bredensteiner took the idea and ran with it.
“I knew we had some funding available through the Foundation,” Bredensteiner said. “I ran the idea past Senior Development Officer Leigh-Ann Erickson. She thought it would be a great use of the funds and encouraged me to pursue the project.”
Schwarz Cancer Center team members were the first to add their prints to the trees.
“We call them our trees of hope,” Pitcock said. “They help show patients they’re not alone. They represent community and teamwork. Our hope is five to 10 years from now the hallways will be filled with completed trees and we can keep the tradition going.”
“Donors don’t have to give a huge amount of money to make a big difference,” Bredensteiner said. “All resources that come through IU Health Foundation are used to take care of patients in ways we wouldn’t ordinarily be able to do. This art can uplift someone’s mental health and provide hope at the end of their journey to leave that mark on the wall. I’d say that’s just as important as a clinical outcome, in many ways.”
To join donors supporting patients at Schwarz Cancer Center, contact Leigh-Ann Erickson at [email protected] or make a gift on the IU Health Foundation website by selecting IU Health North Hospital in the location field and selecting Schwarz Cancer Fund in the dropdown asking where to direct your gift.
Exploring the hospital patient journey: What does the patient experience?
Affiliations.
- 1 Department of Nursing, Università Campus Bio-Medico di Roma, Rome, Italy.
- 2 Department of Management Economics and Industrial Engineering, Politecnico di Milano, Milan, Italy.
- PMID: 31805061
- PMCID: PMC6894823
- DOI: 10.1371/journal.pone.0224899
Purpose: To understand how different methodologies of qualitative research are able to capture patient experience of the hospital journey.
Methods: A qualitative study of orthopaedic patients admitted for hip and knee replacement surgery in a 250-bed university hospital was performed. Eight patients were shadowed from the time they entered the hospital to the time of transfer to rehabilitation. Four patients and sixteen professionals, including orthopaedists, head nurses, nurses and administrative staff, were interviewed.
Results: Through analysis of the data collected four main themes emerged: the information gap; the covering patient-professionals relationship; the effectiveness of family closeness; and the micro-integration of hospital services. The three different standpoints (patient shadowing, health professionals' interviews and patients' interviews) allowed different issues to be captured in the various phases of the journey.
Conclusions: Hospitals can significantly improve the quality of the service provided by exploring and understanding the individual patient journey. When dealing with a key cross-functional business process, the time-space dynamics of the activities performed have to be considered. Further research in the academic field can explore practical, methodological and ethical challenges more deeply in capturing the whole patient journey experience by using multiple methods and integrated tools.
- Attitude to Health
- Hospital-Patient Relations*
- Hospitalization*
- Middle Aged
- Patient Care
- Patients / psychology*
- Quality of Health Care
Grants and funding
- Open access
- Published: 17 April 2024
Navigating outpatient care of patients with type 2 diabetes after hospital discharge - a qualitative longitudinal study
- Léa Solh Dost 1 , 2 ,
- Giacomo Gastaldi 3 ,
- Marcelo Dos Santos Mamed 4 , 5 &
- Marie P. Schneider 1 , 2
BMC Health Services Research volume 24 , Article number: 476 ( 2024 ) Cite this article
252 Accesses
Metrics details
The transition from hospital to outpatient care is a particularly vulnerable period for patients as they move from regular health monitoring to self-management. This study aimed to map and investigate the journey of patients with polymorbidities, including type 2 diabetes (T2D), in the 2 months following hospital discharge and examine patients’ encounters with healthcare professionals (HCPs).
Patients discharged with T2D and at least two other comorbidities were recruited during hospitalization. This qualitative longitudinal study consisted of four semi-structured interviews per participant conducted from discharge up to 2 months after discharge. The interviews were based on a guide, transcribed verbatim, and thematically analyzed. Patient journeys through the healthcare system were represented using the patient journey mapping methodology.
Seventy-five interviews with 21 participants were conducted from October 2020 to July 2021. The participants had a median of 11 encounters (min–max: 6–28) with HCPs. The patient journey was categorized into six key steps: hospitalization, discharge, dispensing prescribed medications by the community pharmacist, follow-up calls, the first medical appointment, and outpatient care.
Conclusions
The outpatient journey in the 2 months following discharge is a complex and adaptive process. Despite the active role of numerous HCPs, navigation in outpatient care after discharge relies heavily on the involvement and responsibilities of patients. Preparation for discharge, post-hospitalization follow-up, and the first visit to the pharmacy and general practitioner are key moments for carefully considering patient care. Our findings underline the need for clarified roles and a standardized approach to discharge planning and post-discharge care in partnership with patients, family caregivers, and all stakeholders involved.
Peer Review reports
Care transition is defined as “the movement patients make between healthcare practitioners and settings as their condition and care needs change in the course of a chronic or acute illness” [ 1 ]. The transition from hospital to outpatient care is a particularly vulnerable period for patients as they move from a medical environment with regular health monitoring to self-management, where they must implement a large amount of information received during their hospital stay [ 2 , 3 , 4 , 5 , 6 ]. This transition period can be defined as “the post-hospital syndrome,” which corresponds to a transient period of vulnerability (e.g., 30 days) for various health problems, such as stress, immobility, confusion, and even cognitive decline in older adults, leading to complications [ 7 ]. Furthermore, discharged patients may experience a lack of care coordination, receive incomplete information, and inadequate follow-ups, leading to potential adverse events and hospital readmissions [ 8 , 9 , 10 ].
People with type 2 diabetes mellitus (T2D) represent a high proportion of hospitalized patients, and their condition and medications are associated with a higher rate of hospital readmission [ 11 , 12 , 13 ]. Moreover, T2D is generally associated with multiple comorbidities. This complex disease requires time-consuming self-management tasks such as polypharmacy, adaptations of medication dosages, diet, exercise, and medical follow-up, especially during care transition [ 14 , 15 , 16 ].
Various interventions and practices, such as enhanced patient education, discharge counseling, and timely follow-up, have been studied to improve care transition for patients with chronic diseases; however, they have shown mixed results in reducing costs and rehospitalization [ 17 , 18 , 19 , 20 ]. In addition, patient perspectives and patient-reported outcomes are rarely considered; however, their involvement and monitoring are essential for seamless and integrated care [ 21 , 22 ]. Care integration, an approach to strengthening healthcare systems in partnership with people, focuses on patient health needs, the quality of professional services, and interprofessional collaboration. This approach prevents care fragmentation for patients with complex needs [ 23 , 24 ]. Therefore, knowledge of healthcare system practices is essential to ensure integrated, coordinated, and high-quality care. Patient perspectives are critical, considering the lack of literature on how patients perceive their transition from hospital to autonomous care management [ 25 , 26 ].
Patients’ journeys during hospitalization have been described in the literature using various methods such as shadowing, personal diaries, and interviews; however, patients’ experiences after hospital discharge are rarely described [ 26 , 27 ]. Jackson et al. described the complexity of patient journeys in outpatient care after discharge using a multiple case study method to follow three patients with chronic obstructive pulmonary disease from hospitalization to 3 months post-discharge [ 26 ]. The literature does not provide an in-depth understanding of the experiences of patients with comorbidities during care transition upon hospital discharge. The assumption about the patient journey after discharge is that multiple and multi-professional encounters will ensure the transition of care from hospitalization to self-management, but often without care coordination.
This study aimed to investigate the healthcare trajectories of patients with comorbidities, including T2D, during the 2 months following hospital discharge and to examine patients’ encounters with healthcare professionals (HCPs).
While this article focuses on patients’ journeys to outpatient care, another article describes and analyzes patients’ medication management, knowledge, and adherence [ 28 ]. This study followed the Consolidated Criteria for Reporting Qualitative Research (COREQ).
Study design and population
A qualitative longitudinal research approach was adopted, with four individual semi-structured interviews over 2 months after discharge (approximately 3, 10, 30, and 60 days after discharge) that took place at home, by telephone, secured video call, or at the university at the participant’s convenience. Participants were recruited during hospitalization. The inclusion criteria were patients with T2D, with at least two other comorbidities, at least one medication change during hospitalization, hospitalization duration of at least 3 days, and those who returned home after discharge and self-managed their medications. A family caregiver could also participate in the interviews alongside to participants.
Researcher characteristics
All the researchers were trained in qualitative studies. The ward diabetologist and researcher (GG) who enrolled the patients in the study participated in most participants’ care during hospitalization. LS (Ph.D. student and community pharmacist) was unknown to participants and presented herself during hospitalization as a “researcher” rather than a pharmacist to avoid any risk of influencing participants’ answers. MS is a professor in pharmacy, whose research focuses on medication adherence in chronic diseases and aims at better understanding this behavior and its consequences for patients and the healthcare system. MDS is a researcher, linguist, and clinical psychologist, with a particular interest in patients living with chronic conditions such as diabetes and a strong experience in qualitative methodology and verbal data analysis.
Data collection
The interviews were based on four semi-structured interview guides based on existing frameworks and theories: the World Health Organization’s five dimensions for adherence, the Information-Motivation-Behavioral Skills model, and the Social Cognitive Theory [ 29 , 30 , 31 ]. For in-depth documentation of participants’ itinerary in the healthcare system, the interview guides included questions on the type, reason, and moment of the HCP’s encounters and patient relationships with HCPs. Interview guides are available in Supplementary File 1 . During the development phase of the study, the interview guides were reviewed for clarity and validity and adapted by two patient partners from the Geneva University Hospitals’ Patient Partner Platform for Research and Patient and Public Involvement. Thematic saturation was considered reached when no new code or theme emerged and new data repeated previously coded information [ 32 ]. Sociodemographic and clinical data were collected from hospital databases and patient questionnaires. The interviews were audio-recorded, anonymized, and transcribed verbatim.
Data analysis
The sociodemographic and clinical characteristics were descriptively analyzed. Transcriptions were double-coded until similar codes were obtained, and thematic analysis, as described by Braun and Clarke [ 33 , 34 ], was used in a systematic, iterative, and comparative manner. A patient journey mapping methodology was used to illustrate the trajectories of each participant and provide a comprehensive understanding of their experiences. Patient journey mapping is a visual method adapted from the marketing industry that is increasingly used in various health settings and contexts to illustrate and evaluate healthcare services and patient experiences [ 35 ]. In this analysis, we used the term “healthcare professionals” when more than one profession could be involved in participants’ healthcare. Otherwise, when a specific HCP was involved, we used the designated profession (e.g. physicians, pharmacists).
A. Participants description
Twenty-one participants were interviewed between October 2020 and September 2021, generating 75 interviews. All participants took part in Interview 1, 19 participants in Interview 2, 16 participants in Interview 3 and 19 participants in Interview 4, with a median duration of 41 minutes (IQR: 34-49) per interview. Interviews 1,2,3 and 4 took place respectively 5 days (IQR: 4-7), 14 days (13-20), 35 days (33-38), and 63 days (61-68) after discharge. Nine patients were newly diagnosed with T2D, and 12 had a previous diagnosis of T2D, two of whom were untreated. Further information on participants is described in Table 1 . The median number of comorbidities was six (range: 3–11), and participants newly diagnosed with diabetes tended to have fewer comorbidities (median: 4; range: 3–8). More detailed information regarding sociodemographic characteristics and medications has been published previously [ 28 ].
B. Journey mappings
Generic patient journey mapping, presented in Fig. 1 , summarizes the main and usual encounters participants had with their HCPs during the study period. Generic mapping results from all individual patient journey mappings from discharge to 2 months after discharge are available in Supplementary File 2 .
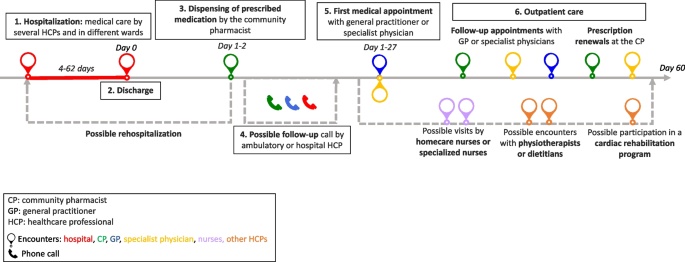
Generic patient journey mapping from hospitalization to two months after discharge
During the 2 months following discharge, the participants had a median number of 10 (range: 6–28) encounters with HCPs. The HCPs met by participants are represented in Fig. 2 . All participants visited their pharmacists at least once, and 16 of the 21 participants met their general practitioners (GPs) at least once. Five participants received home care assistance, four went to an outpatient cardiac rehabilitation program, and five were readmitted during the study period.
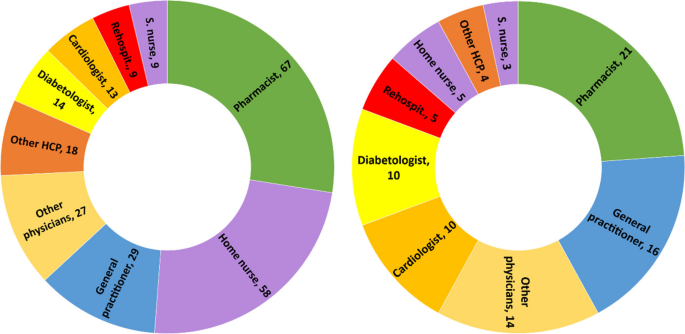
Healthcare professionals seen by participants during the study period. left: n=cumulative encounters; right: n=encountered at least once. Abbreviation: S.nurse: specialized nurse; Other physicians: ophthalmologists, neurologists, hematologists, immunologists, addictologists; other HCP: physiotherapists, dietitians, massage therapist
The first HCP encountered was at the community pharmacy on the same day or day after discharge, except for one participant who did not pick up her medication. The first medical appointment with a physician occurred between days 1 and 27 after discharge (median: 8; IQR: 6-14).
Participants newly diagnosed with diabetes had a closer follow-up after discharge than participants with a former diagnosis of T2D (median: 7; IQR: 6–10 vs median: 9; IQR: 5–19), fewer encounters with HCPs (median: 8; IQR: 7–10 vs. 11; IQR: 8–17), and fewer comorbidities (median: 4; IQR: 4–7 vs. 7; IQR: 5–9). Most participants newly diagnosed with T2D or receiving insulin treatment benefited from either a follow-up call, home visit by a nurse, or diabetes care appointment.
C. Qualitative analysis
Transcripts were analyzed longitudinally and categorized into six key steps based on the verbal data. These key steps, shown in Fig. 1 , represent the identified thematic categories and refer to the following elements: 1. Hospitalization, 2. Discharge, 3. Dispensing of prescribed medications at the pharmacy, 4. Possible follow-up call, 5. First medical appointment, and 6. Outpatient care.
Hospitalization: hospital constraints and care organization
Most participants thought they had benefited from adequate medical care by committed and attentive HCPs but highlighted different constraints and gaps. Some participants noted constraints related to the hospital environment, such as loss of autonomy during their stay, lack of privacy, and the large number of hospital staff encountered. This resulted in participants repeating the same information several times, causing frustration, misunderstanding and a lack of coordination for some participants:
“Twenty or thirty staff members come in during the day! So, it's hard to keep track of [what] is bein g said or done. The best thing for me [...] would be to have clear information from just one person.” Participant 8; interview 1 (P18.1)
Participants had different opinions on the hospital’s care organization. Some participants found that care coordination between the wards was well-organized. In contrast, others highlighted poor coordination and communication between the hospital wards, resulting in long waiting times, care fragmentation, and contradictory or unclear information. Some participants felt that they did not benefit from comprehensive and integrated care and that the hospital staff focused on the cause of their hospitalization, neglecting other comorbidities:
“They were not interested [in my diabetes and my sight]. I was there for the heart and that was where [my care] stopped.” P17.1
Patients’ involvement in decision-making regarding medical care varied. Some participants were involved in their care and took part in medical decisions. Written information, adequate communication, and health professionals’ interest in patients were highlighted by some participants:
“They took the information sheet and they explained everything to me. They didn't just come once; they came several times to explain everything to me.” P5.1
Other participants found the information difficult to understand, particularly because of their fatigue and because the information was provided orally.
Discharge: an unclear process
The discharge process was unclear for patients who could not identify a specific related outpatient medical visit or a key step that summarized their hospital stay and prepared them for discharge:
“Well, there's no real preparation [for discharge]. I was waiting for them to give me the go-ahead so I could go home, that’s all...” P7.4
For some participants, outpatient care follow-up was organized before discharge by the hospital team (generally by making an appointment with the patient’s GP before discharge), whereas others had no post-discharge follow-up scheduled during their hospitalization. Approximately half of the participants refused follow-ups during their hospitalization, such as home care services provided by a nurse, or a rehabilitation hospital stay. The main reason for this refusal was that patients did not perceive the need for follow-up:
“It's true that I was offered a lot of services, which I turned down because I didn't realize how I would manage back at home.” P22.2
Dispensing prescribed medications by the community pharmacist: the first HCP seen after discharge
On behalf of half the participants, a family caregiver went to the usual community or hospital outpatient pharmacy to pick up the medications. The main reasons for delegation were tiredness or difficulty moving. In some cases, this missed encounter would have allowed participants to discuss newly prescribed medications with the pharmacist:
“[My husband] went to get the medication. And I thought afterward, […] that I could have asked [the pharmacist]: “But listen, what is this medication for?” I would have asked questions” P2.3
Participants who met their pharmacist after hospital discharge reported a range of pharmaceutical practices, such as checking the prescribed medication against medication history, providing information and explanations, and offering services such as the preparation of pillboxes. For some, the pharmacists’ work at discharge did not differ from regular prescriptions, whereas others found that they received further support and explanations:
“She took the prescription […] checked thoroughly everything and then she wrote how, when, and how much to take on each medication box. She managed it very well and I had good explanations.” P20.3
Some participants experienced problems with generic substitution, the unavailability of medications, or dispensing errors, complicating their journey through the healthcare system.
Possible follow-up call by HCP: an unsystematic practice
Some participants received a call from their GP or hospital physician a few days after discharge to check their health or answer questions. These calls reassured participants and their caregivers, who knew they had a point of contact in case of difficulty. Occasionally, participants received calls from their community pharmacists to ensure proper understanding and validate medication changes issued during hospitalization. Some participants did not receive any calls and were disappointed by the lack of follow-up:
“There is no follow-up! Nobody called me from the hospital to see how I was doing […]” P8.2
First medical appointment: a key step in the transition of care
The first medical appointment was made in advance by the hospital staff or the patient after discharge. For some participants, this first appointment did not differ from usual care. For most, it was a crucial appointment that allowed them to discuss their hospitalization and new medications and organize their follow-up care. Being cared for by a trusted HCP enabled some patients to feel safe, relieved, and well-cared for, as illustrated by the exchange between a patient and her daughter:
Daughter: When [my mom] came back from the GP, she felt much better [...] It was as if a cork had popped. Was it psychological? Patient: Maybe… I just felt better. D: Do you think it was the fact that she paid attention to you as a doctor? P: She took care of me. She did it in a delicate way. [silence] - P23.2
Some participants complained that their physicians did not receive the hospital discharge letter, making it difficult to discuss hospitalization and sometimes resulting in delayed care.
Outpatient care: a multifaceted experience
During the 2 months after hospital discharge, participants visited several physicians (Fig. 2 ), such as their GP and specialist physicians, for follow-ups, routine check-ups, medical examinations, and new prescriptions. Most participants went to their regular pharmacies to renew their prescriptions, for additional medication information, or for health advice.
Some participants had home care nurses providing various services, such as toileting, care, checks on vital functions, or preparing weekly pill boxes. While some participants were satisfied with this service, others complained that home nurses were unreliable about appointment times or that this service was unnecessary. Some participants were reluctant to use these services:
“The [homecare nurse] makes you feel like you're sick... It's a bit humiliating.” P22.2
Specialized nurses, mostly in diabetology, were appreciated by patients who had dedicated time to talk about different issues concerning diabetes and medication and adapted explanations to the patient’s knowledge. Participants who participated in cardiac rehabilitation said that being in a group and talking to people with the same health problems motivated them to undertake lifestyle and dietary changes:
“In the rehabilitation program, I’m part of a team [of healthcare professionals and patients], I have companions who have gone through the same thing as me, so I’m not by myself. That's better for motivation.” P16.2
Navigating the outpatient healthcare system: the central role of patients
Managing medical appointments is time-consuming and complex for many participants. Some had difficulty knowing with whom to discuss and monitor their health problems. Others had difficulty scheduling medical appointments, especially with specialist physicians or during holidays. A few participants did not attend some of their appointments because of physical or mental vulnerabilities. Restrictions linked to the type of health insurance coverage made navigating the healthcare system difficult for some participants:
“Some medications weren't prescribed by my GP [...] but by the cardiologist. So, I must ask my GP for a delegation to see the cardiologist. And I have to do this for three or four specialists... Well, it’s a bit of a hassle […] it's not always easy or straightforward”. P11.2
Some participants had financial difficulties or constraints, such as expenses from their hospitalization, ambulance transportation, and medications not covered by their health insurance plans. This led to misunderstandings, stress, and anxiety, especially because some participants could not return to work or, to a lesser extent, because of their medical condition.
To ensure continuity of care, some participants were proactive in their case management, for example, by calling to confirm or obtain further information on an appointment or to ensure information transfer. Written convocations for upcoming medical appointments and tailored explanations helped the participants organize their care. Family caregivers were also key in taking participants to various consultations, reminding them, and managing their medical appointments.
Information transfer: incomplete and missing information
Information transfer between and within settings was occasionally lacking. Even weeks after hospitalization, some documents were not transmitted to outpatient physicians, sometimes delaying medical care. Some participants reported receiving incomplete, unclear, or contradictory information from different HCPs, sometimes leading to doubts, seeking a second medical opinion, or personal searches for information. A few proactive participants ensured good information transmission by making a copy of the prescription or sending copies of their documents to physicians:
“My GP hasn't received anything from the hospital yet. I’ve sent him the PDF with the medication I take before our appointment […] Yes, It’s the patient that does all the job.” P10.3
Interprofessional work: a practice highlighted by some participants
Several participants highlighted the interprofessional work they observed in the outpatient setting, especially because they had several comorbidities; therefore, several physicians followed their care:
“My case is very complex! For example, between the cardiologist and the diabetologist, they need to communicate closely because there could be consequences or interactions with the medications I take [for my heart and my diabetes].” P4.2
Health professionals referred their patients to the most appropriate provider for better follow-up (e.g., a nurse specializing in addictology referred a patient to a nurse specializing in diabetology for questions and follow-up on blood sugar levels). Interprofessional collaboration between physicians and pharmacists was noted by some participants, especially for prescription refills or ordering medications.
Patient-HCPs relationships: the importance of trust
Trust in the care relationship was discussed by the participants regarding different HCPs, especially GPs and community pharmacists. Most participants highlighted the communication skills and active listening of healthcare providers. Knowing an HCP for several years helped build trust and ensure an updated medical history:
“I've trusted this pharmacist for 20 years. I can phone her or go to the pharmacy to ask any question[...] I feel supported.” P3.2
Some participants experienced poor encounters owing to a lack of attentive listening or adapted communication, especially when delivering bad news (new diagnoses or deterioration of health status). Professional competencies were an important aspect of the patient-HCP relationship, and some participants lost confidence in their physician or pharmacist because of inadequate medical or pharmaceutical care management or errors, such as the physician prescribing the wrong medication dosage, the pharmacist delivering the wrong pillbox or the general practitioner refusing to see a patient:
“I think I'll find another doctor… In fact, the day I was hospitalized, I called before to make an appointment with her and she refused to see me […] because I had a fever, and I hadn’t done a [COVID] test.” P6.2
Most participants underlined the importance of their GP because they were available, attentive to their health issues, and had a comprehensive view of their medications and health, especially after hospitalization:
“Fortunately, there are general practitioners, who know everything. With some specialists, the body is fragmented, but my GP knows the whole body.” P14.1
After hospitalization, the GP’s role changed for some participants who saw their GP infrequently but now played a central role.
Community pharmacist: an indistinct role
Pharmacists and their teams were appreciated by most participants for their interpersonal competencies, such as kindness, availability, professional flexibility, and adaptability to patients’ needs to ensure medication continuity (e.g., extension of the prescription, home delivery, or extending time to pay for medications). The role of community pharmacists varied according to the participants. Some viewed pharmacists as simple salespeople:
“It's like a grocery store. [...] I go there, it's ordered, I take my medication, I pay and I leave.” P23.3
For others, the pharmacist provided medication and advice and was a timely source of information but did not play a central role in their care. For others, the pharmacist’s role is essential for medication monitoring and safety:
“I always go to the same pharmacy […] because I know I have protection: when [the pharmacist] enters the medications in his computer, if two medications are incompatible, he can verify. [...] There is this follow-up that I will not have if I go each time somewhere else.” P10.4
The patient journey mapping methodology, coupled with qualitative thematic analysis, enabled us to understand and shed light on the intricacies of the journey of polypharmacy patients with T2Din the healthcare system after discharge. This provided valuable insights into their experiences, challenges, and opportunities for improvement.
This study highlights the complex pathways of patients with comorbidities by considering the population of patients with T2D as an example. Our population included a wide variety of patients, both newly diagnosed and with known diabetes, hospitalized for T2D or other reasons. Navigating the healthcare system was influenced by the reason for hospitalization and diagnosis. For example, newly diagnosed participants with T2D had a closer follow-up after discharge, participants were more likely to undergo cardiac rehabilitation after infarction, and participants with a former T2D diagnosis were more complex, with more comorbidities and more HCP encounters. Our aim was not to compare these populations but to highlight particularities and differences in their health care and these qualitative data reveal the need for further studies to improve diabetes management during inpatient to outpatient care transition.
The variability in discharge practices and coordination with outpatient care highlights the lack of standardization during and after hospital discharge. Some participants had a planned appointment with their GP before discharge, others had a telephone call with a hospital or ambulatory physician, and some had no planned follow-up, causing confusion and stress. Although various local or national guidelines exist for managing patients discharged from the hospital [ 36 , 37 , 38 , 39 ], there are no standard practices regarding care coordination implemented in the setting of this study. The lack of local coordination has also been mentioned in other studies [ 5 , 40 , 41 ].
Our results also raise questions about the responsibility gap in the transition of care. Once discharged from the hospital, who is responsible for the patient until their first medical appointment? This responsibility is not clearly defined among hospital and outpatient care providers, with more than 25% of internal medicine residents indicating their responsibility for patients ending at discharge [ 42 , 43 ]. Importance should be given to clarifying when and who will take over the responsibility of guaranteeing patient safety and continuity of care and avoiding rehospitalization [ 44 ].
The first visit with the community pharmacist after discharge and the referring physician were the key encounters. While the role of the GP at hospital discharge is well-defined, the community pharmacist’s role lacks clarity, even though they are the first HCP encountered upon hospital discharge. A meta-analysis showed the added value of community pharmacists and how their active participation during care transition can reduce readmission [ 18 ]. A better definition of the pharmacist’s role and integration into care coordination could benefit patient safety during the transition and should be assessed in future studies.
Our findings showed that the time elapsed between discharge and the first medical appointment varied widely (from 1 to 27 days), correlating with findings in the literature showing that more than 80% of patients see their GP within 30 days [ 45 ]. Despite the first medical appointment being within the first month after discharge, some patients in our study reported a lack of support and follow-up during the first few days after discharge. Care coordination at discharge is critical, as close outpatient follow-up within the first 7–10 days can reduce hospital readmission rates [ 46 , 47 ]. Furthermore, trust and communication skills are fundamental components of the patient-HCP relationship, underlined in our results, particularly during the first medical appointment. Relational continuity, especially with a particular HCP who has comprehensive patient knowledge, is crucial when patients interact with multiple clinicians and navigate various settings [ 48 , 49 ].
Navigating the outpatient healthcare system after discharge was complex for most participants and relied heavily on patient involvement and responsibility. While some participants who received clear information felt more empowered and engaged in their care, others highlighted the difficulty in organizing their care during this vulnerable period. Such difficulties in case management have been described previously [ 50 , 51 ]. Moreover, services proposed by HCPs (e.g., home assistance) do not always correspond to patient needs and are sometimes refused. This highlights the tension between HCPs’ medical recommendations, priorities, and patient expectations. This tension between medical priorities and patient needs was felt during hospitalization and shaped the 2 months following discharge. HCPs need to assess patient needs and preferences during hospitalization and transition for follow-up services. They must also ensure that the offered services meet at least the most relevant of patients’ perceived needs to improve seamless care and patient safety [ 52 , 53 ].
Examples of a lack of communication and information transfer were described in our results at different levels among HCPs, between participants or family caregivers, and HCPs, and these findings correlate with the literature [ 3 , 54 , 55 , 56 ]. Although family caregivers play an important role in supporting patients in the healthcare system, they are also additional interlocutors, leading to missed opportunities for patient-pharmacist interactions when dispensing discharged medication. Therefore, it is paramount to integrate and involve family caregivers in shared decision-making and communicate with patients remotely when they are not present [ 57 ].
Opportunities to improve the discharge of patients returning home after discharge without home care are highlighted in this article. Our insights can serve as a valuable foundation for healthcare providers and policymakers seeking to optimize patient experience and quality of care in the post-discharge phase. Different professionals should be integrated into standard practice through guidelines to ensure improved collaboration from hospital discharge to outpatient care. During hospitalization:
an appointment should be scheduled with the referring physician shortly after discharge to guarantee continuity of care
a hospital discharge interview should be conducted in a systematic way to summarize and securely close the hospitalization
the community pharmacist should be informed before the patient’s discharge to prepare and reconcile medications before and after hospitalization
In outpatient care:
an in-person or phone encounter with the pharmacy team should be scheduled for the patient and/or caregivers at discharge
a contact point (phone number, email, or virtual chat assistant) or scheduled follow-up should be implemented to answer questions and redirect patients before they can meet with the referring physician
a long-term and active communication channel between HCPs should be established.
In other countries, several outpatient services are already available for patients discharged home to enhance continuity of care and patient safety after discharge. The telehealth-based Transitional Care Management Programme, a local initiative in a New York hospital, involves contacting discharged patients 24 to 48 hours after discharge to support understanding of discharge instructions, medication access, follow-up appointments, and social needs [ 58 ]. The Australian Government has introduced the Transition Care Program that provides short-term care for older people, including social work, nursing support, personal care, and allied health care [ 59 ]. In England, the NHS has introduced the Discharge Medicines Service (DMS) in community pharmacies, which aims to improve communication between hospitals and community pharmacies and to ensure that patients understand changes to their medications [ 60 ].
Limitations
This study has several limitations. First, the accuracy of the encounter dates with HCPs, as described by the participants, could not be verified using a second data source (e.g., medical or pharmacy records). Additionally, recall biases cannot be excluded, especially during interviews 3 and 4, which took place at longer intervals (20 days between interviews 2 and 3 and 30 days between interviews 3 and 4). Nevertheless, our findings express a patient's representation of their healthcare system navigation experience. Secondly, these results may not be generalizable to populations with other long-term diseases, even though we recruited patients with different reasons for hospitalization, including age, sex, and comorbidities. In addition, the study region is predominantly an urban area with a high density of HCPs, which may influence patient journeys in the healthcare system. Finally, we excluded patients whose medications were managed by HCPs because these patients might have had different experiences, difficulties, and needs. This exclusion criterion was chosen because our objective was to investigate patients’ medication self-management, as described in another article [ 28 ].
A patient’s journey in the 2 months following discharge is unique for each individual and constitutes a complex and adaptive process. Despite the active role of numerous HCPs, navigation in outpatient care after discharge relies heavily on the involvement and responsibilities of polypharmacy. The findings of this study highlight the need to standardize the approach for discharge planning and post-discharge care in partnership with patients and caregivers. Preparation for discharge, the first visit to the pharmacy, and the first appointment with the GP are key moments for all patients, along with the involvement of other medical and nurse specialists, as needed. Standardizing practices, clarifying responsibilities, integrating community pharmacists during the transition, empowering patients, and enhancing interprofessional communication and collaboration should be explored and implemented to achieve better patient outcomes and a more seamless healthcare journey for individuals transitioning from the hospital to the community.
Availability of data and materials
The qualitative codes in French and anonymized patient datasets are available from the corresponding author on reasonable request. Individual patient journeys are provided in the Supplementary Files.
Abbreviations
General practitioner
Healthcare professional
type 2 diabetes mellitus
Coleman EA, Boult C. Improving the quality of transitional care for persons with complex care needs. J Am Geriatr Soc. 2003;51(4):556–7.
Article PubMed Google Scholar
Allen J, Hutchinson AM, Brown R, Livingston PM. User experience and care for older people transitioning from hospital to home: Patients’ and carers’ perspectives. Health Expect. 2018;21(2):518–27.
Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. Jama. 2007;297(8):831–41.
Article CAS PubMed Google Scholar
Allen J, Hutchinson AM, Brown R, Livingston PM. Quality care outcomes following transitional care interventions for older people from hospital to home: a systematic review. BMC Health Serv Res. 2014;14:346.
Article PubMed PubMed Central Google Scholar
Hesselink G, Flink M, Olsson M, Barach P, Dudzik-Urbaniak E, Orrego C, et al. Are patients discharged with care? A qualitative study of perceptions and experiences of patients, family members and care providers. BMJ Qual Saf. 2012;21(Suppl 1):i39-49.
World Health Organization (WHO). Transitions of Care. 2016.
Google Scholar
Krumholz HM. Post-hospital syndrome–an acquired, transient condition of generalized risk. N Engl J Med. 2013;368(2):100–2.
Article CAS PubMed PubMed Central Google Scholar
Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–28.
Banholzer S, Dunkelmann L, Haschke M, Derungs A, Exadaktylos A, Krähenbühl S, et al. Retrospective analysis of adverse drug reactions leading to short-term emergency hospital readmission. Swiss Med Wkly. 2021;151:w20400.
World Health Organization (WHO). Medication Safety in Transitions of Care. 2019.
Müller-Wieland D, Merkel M, Hamann A, Siegel E, Ottillinger B, Woker R, et al. Survey to estimate the prevalence of type 2 diabetes mellitus in hospital patients in Germany by systematic HbA1c measurement upon admission. Int J Clin Pract. 2018;72(12):e13273.
Blanc AL, Fumeaux T, Stirnemann J, Dupuis Lozeron E, Ourhamoune A, Desmeules J, et al. Development of a predictive score for potentially avoidable hospital readmissions for general internal medicine patients. PLoS One. 2019;14(7):e0219348.
Hansen LO, Greenwald JL, Budnitz T, Howell E, Halasyamani L, Maynard G, et al. Project BOOST: effectiveness of a multihospital effort to reduce rehospitalization. J Hosp Med. 2013;8(8):421–7.
Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of Type 2 Diabetes - Global Burden of Disease and Forecasted Trends. J Epidemiol Glob Health. 2020;10(1):107–11.
Iglay K, Hannachi H, Joseph Howie P, Xu J, Li X, Engel SS, et al. Prevalence and co-prevalence of comorbidities among patients with type 2 diabetes mellitus. Curr Med Res Opin. 2016;32(7):1243–52.
Russell LB, Suh DC, Safford MA. Time requirements for diabetes self-management: too much for many? J Fam Pract. 2005;54(1):52–6.
PubMed Google Scholar
Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: a systematic review. Ann Intern Med. 2011;155(8):520–8.
Lussier ME, Evans HJ, Wright EA, Gionfriddo MR. The impact of community pharmacist involvement on transitions of care: a systematic review and meta-analysis. J Am Pharm Assoc. 2020;60(1):153.
Article Google Scholar
Donzé J, John G, Genné D, Mancinetti M, Gouveia A, Méan M, et al. Effects of a Multimodal Transitional Care Intervention in Patients at High Risk of Readmission: The TARGET-READ Randomized Clinical Trial. JAMA Intern Med. 2023.
Leppin AL, Gionfriddo MR, Kessler M, Brito JP, Mair FS, Gallacher K, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095–107.
Noonan VK, Lyddiatt A, Ware P, Jaglal SB, Riopelle RJ, Bingham CO 3rd, et al. Montreal Accord on Patient-Reported Outcomes (PROs) use series - Paper 3: patient-reported outcomes can facilitate shared decision-making and guide self-management. J Clin Epidemiol. 2017;89:125–35.
Hesselink G, Schoonhoven L, Barach P, Spijker A, Gademan P, Kalkman C, et al. Improving patient handovers from hospital to primary care: a systematic review. Ann Intern Med. 2012;157(6):417–28.
(WHO) WHO. Systems in the who European region: framework for action on integrated health services delivery. Copenhagen: WHO; 2016.
Damery S, Flanagan S, Combes G. The effectiveness of interventions to achieve co-ordinated multidisciplinary care and reduce hospital use for people with chronic diseases: study protocol for a systematic review of reviews. Syst Revi. 2015;4(1):64.
Noor F, Gulis G, Karlsson LE. Exploration of understanding of integrated care from a public health perspective: a scoping review. J Public Health Res. 2023;12(3):22799036231181210.
Jackson K, Oelke ND, Besner J, Harrison A. Patient journey: implications for improving and integrating care for older adults with chronic obstructive pulmonary disease. Can J Aging. 2012;31(2):223–33.
Gualandi R, Masella C, Viglione D, Tartaglini D. Exploring the hospital patient journey: what does the patient experience? PLoS One. 2019;14(12):e0224899.
Solh Dost L, Gastaldi G, Schneider M. Patient medication management, understanding and adherence during the transition from hospital to ambulatory care – a qualitative longitudinal study in polymorbid type 2 diabetes patients. BMC Health Services Research, in press
World Health Organization (WHO). Adherence to long-term therapies: Evidence for action. 2003.
Fisher JD, Fisher WA, Amico KR, Harman JJ. An information-motivation-behavioral skills model of adherence to antiretroviral therapy. Health Psychol. 2006;25(4):462–73.
Bandura A. Health promotion from the perspective of social cognitive theory. Psychol Health. 1998;13(4):623–49.
Hennink MM, Kaiser BN, Marconi VC. Code saturation versus meaning saturation: how many interviews are enough? Qual Health Res. 2016;27(4):591–608.
Braun V, Clarke V. Reflecting on reflexive thematic analysis. Qual Res Sport Exercise Health. 2019;11(4):589–97.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Davies EL, Bulto LN, Walsh A, Pollock D, Langton VM, Laing RE, et al. Reporting and conducting patient journey mapping research in healthcare: a scoping review. J Adv Nurs. 2023;79(1):83–100.
California pharmacists association. Transitions of Care Resource Guide https://cdn.ymaws.com/www.cshp.org/resource/resmgr/Files/Practice-Policy/For_Pharmacists/transitions_of_care_final_10.pdf . Accessed 20 Nov 2023.
National Health Service (NHS). Guidance: Hospital discharge and community support guidance. 2022. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1087354/Hospital-Discharge-and-Community-Support-Guidance-2022-v2.pdf . Accessed 01 Apr 2024.
Winnipeg Regional Health Authority. Safe Patient Discahrge Guideline. 2017. https://wrha.mb.ca/files/guideline-safe-discharge.pdf . Accessed 01 Apr 2024.
Haute Autorité de Santé, France. Check-List de Sortie d'hospitalisation supérieure à 24 heures https://www.has-sante.fr/jcms/c_2035081/fr/check-list-de-sortie-d-hospitalisation-superieure-a-24h . Accessed 04 Apr 2024.
Wong ELY, Yam CHK, Cheung AWL, Leung MCM, Chan FWK, Wong FYY, et al. Barriers to effective discharge planning: a qualitative study investigating the perspectives of frontline healthcare professionals. BMC Health Serv Res. 2011;11(1):242.
Urban R, Paloumpi E, Rana N, Morgan J. Communicating medication changes to community pharmacy post-discharge: the good, the bad, and the improvements. Int J Clin Pharm. 2013;35(5):813–20.
Young E, Stickrath C, McNulty MC, Calderon AJ, Chapman E, Gonzalo JD, et al. Internal medicine residents’ perceived responsibility for patients at hospital discharge: a national survey. J Gen Intern Med. 2016;31(12):1490–5.
Jones CD, Vu MB, O’Donnell CM, Anderson ME, Patel S, Wald HL, et al. A failure to communicate: a qualitative exploration of care coordination between hospitalists and primary care providers around patient hospitalizations. J Gen Intern Med. 2015;30(4):417–24.
Watts R, Pierson J, Gardner H. Co-ordination of the discharge planning process in critical care. J Clin Nurs. 2007;16(1):194–202.
Roughead EE, Kalisch LM, Ramsay EN, Ryan P, Gilbert AL. Continuity of care: when do patients visit community healthcare providers after leaving hospital? Intern Med J. 2011;41(9):662–7.
Riverin BD, Strumpf EC, Naimi AI, Li P. Optimal timing of physician visits after hospital discharge to reduce readmission. Health Serv Res. 2018;53(6):4682–703.
Coppa K, Kim EJ, Oppenheim MI, Bock KR, Conigliaro J, Hirsch JS. Examination of post-discharge follow-up appointment status and 30-day readmission. J Gen Intern Med. 2021;36(5):1214–21.
Haggerty JL, Roberge D, Freeman GK, Beaulieu C. Experienced continuity of care when patients see multiple clinicians: a qualitative metasummary. Ann Fam Med. 2013;11(3):262–71.
Baker R, Freeman G, Boulton M, Windridge K, Tarrant C, Low J, et al. Continuity of care: patients’ and carers’ views and choices in their use of primary care services. Report for the national co-ordinating center for NHS Service Delivery and Organisation R & D (NCCSDO). 2006.
Arora VM, Prochaska ML, Farnan JM, D’Arcy MJt, Schwanz KJ, Vinci LM, et al. Problems after discharge and understanding of communication with their primary care physicians among hospitalized seniors: a mixed methods study. J Hosp Med. 2010;5(7):385–91.
Allen J, Hutchinson AM, Brown R, Livingston PM. User experience and care integration in transitional care for older people from hospital to home: a meta-synthesis. Qual Health Res. 2016;27(1):24–36.
Krook M, Iwarzon M, Siouta E. The discharge process-from a patient’s perspective. SAGE Open Nurs. 2020;6:2377960819900707.
PubMed PubMed Central Google Scholar
Huber DL, McClelland E. Patient preferences and discharge planning transitions. J Prof Nurs. 2003;19(4):204–10.
Ravenscroft E. Navigating the health care system: insights from consumers with multimorbidity. J Nurs Healthcare Chronic Illness. 2010;2:215–24.
Ancker JS, Witteman HO, Hafeez B, Provencher T, Van de Graaf M, Wei E. The invisible work of personal health information management among people with multiple chronic conditions: qualitative interview study among patients and providers. J Med Internet Res. 2015;17(6):e137.
Manias E, Gerdtz M, Williams A, McGuiness J, Dooley M. Communicating about the management of medications as patients move across transition points of care: an observation and interview study. J Eval Clin Pract. 2016;22(5):635–43.
Mackie BR, Mitchell M, Marshall AP. Patient and family members’ perceptions of family participation in care on acute care wards. Scandinavian J Caring Sci. 2019;33(2):359–70.
Michelle E, Rachel CSF, Jonathan S, Priscilla H, Farrukh NJ. Telehealth-based transitional care management programme to improve access to care. BMJ Open Qual. 2023;12(4):e002495.
Department of Health and Aged Care, Australia. Transition Care Programme. https://www.health.gov.au/our-work/transition-care-programme . Accessed 03 Apr 2024
National Health Service (NHS) Discharge Medicines Service. 2021. https://www.england.nhs.uk/primary-care/pharmacy/pharmacy-services/nhs-discharge-medicines-service/ . Accessed 03 Apr 2024
Download references
Acknowledgments
The authors would like to thank all the patients who took part in this study. We would also like to thank the Geneva University Hospitals Patients Partners +3P platform as well as Mrs Tourane Corbière and Mr Joël Mermoud, patient partners, who reviewed interview guides for clarity and significance.
Open access funding provided by University of Geneva This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
School of Pharmaceutical Sciences, University of Geneva, Geneva, Switzerland
Léa Solh Dost & Marie P. Schneider
Institute of Pharmaceutical Sciences of Western Switzerland, University of Geneva, Geneva, Switzerland
Division of Endocrinology, Diabetes, Hypertension and Nutrition, Department of Medicine, Geneva University Hospitals, Geneva, Switzerland
Giacomo Gastaldi
Institute of Psychology and Education, University of Neuchatel, Neuchâtel, Switzerland
Marcelo Dos Santos Mamed
Institute of Psychology, University of Lausanne, Lausanne, Switzerland
You can also search for this author in PubMed Google Scholar
Contributions
LS, GG, and MS conceptualized and designed the study. LS and GG screened and recruited participants. LS conducted the interviews. LS, GG, and MS performed data analysis and interpretation. LS drafted the manuscript and LS and MS worked on the different versions. MDS contributed its expertise and external opinion as a clinical psychologist and linguist. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Léa Solh Dost or Marie P. Schneider .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval was sought and granted by the Cantonal Research Ethics Commission, Geneva (CCER) (2020-01779). Informed consent to participate was obtained for all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Interview guides.
Additional file 2.
Individual patient journey mappings from discharge to 2 months after discharge.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Solh Dost, L., Gastaldi, G., Dos Santos Mamed, M. et al. Navigating outpatient care of patients with type 2 diabetes after hospital discharge - a qualitative longitudinal study. BMC Health Serv Res 24 , 476 (2024). https://doi.org/10.1186/s12913-024-10959-4
Download citation
Received : 17 January 2024
Accepted : 07 April 2024
Published : 17 April 2024
DOI : https://doi.org/10.1186/s12913-024-10959-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Type 2 diabetes mellitus
- Outpatient care
- Hospital discharge
- Qualitative research
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Managing the Surgical Patient's Journey Through the Hospital
Daniel brockman , bvsc certvr, certsao, dacvs, decvs, royal veterinary college, alison young , davn (surgery), vts (surgery), rvn, royal veterinary college.

Introduction
Surgery is frequently performed in small animal practice with operations ranging from routine elective sterilization procedures to complex urgent or emergency procedures. In order to manage the surgical patient in an optimal way, the clinical team will need to be in command of every aspect of the animal’s management. This process begins with an accurate diagnosis whenever this is possible and includes carefully considered conversation with the animal’s owner so as to gain informed consent for the intended procedure. In addition, sufficiently detailed communication with those involved with the in-hospital care needs of the animal must take place so that the nursing and surgical teams can deliver preoperative, intra-operative, and postoperative care that is both thorough and tailored to that animal’s needs. Finally, the home-care requirements and any follow-up appointments will need to be explained to the animal’s owner at the time of discharge, so that the ongoing recovery can be carefully managed and any complications identified quickly and addressed appropriately. From a medical perspective, an accurate diagnosis and selection of the appropriate surgical procedure are critical, as is the proficient performance of anesthesia and the surgical procedure as well as careful, postoperative care. The true foundation of a successful patient journey, however, is in the way communications surrounding the treatment happen, and the detail they contain.
Part 1: Prior to and Upon Admission
Owner communication, discussing the procedure.
Prior to admission of the animal, the veterinarian should make it clear to the owners, in lay terms, what procedure(s) are going to be performed on their pet, what the intended outcome should be, what potential unintended outcomes or complications may occur (ie, the hazards of such an intervention), and the time gap until the next communication about their pet’s progress.
Informed Consent
Ideally, all owners should then provide their informed consent to the procedure, in the form of a signed “consent” form that identifies the animal and owner, names the planned surgical procedure, contains an estimate of cost, and mentions the more common potential complications. Prior to admission, the animal should be fitted with a temporary identification collar.
Preoperative Patient Preparation
History taking.
The acquisition of a complete medical history from the pet owner is essential. For healthy animals undergoing elective surgery such as sterilization, this serves to ensure that the animal is suitably “ready”; so, vaccination history, worming history, and recent feeding history must be established at admission. For sick animals, this is the first step to learn what might be wrong and will inform subsequent investigations and diagnostic tests. Although this can be time consuming, careful attention to the historical features of disease can yield massive benefits in terms of definition and refinement of the “problem list” and organ system involvement.
Physical Examination
The surgeon should perform a complete physical examination of the patient prior to all nonemergent surgery. Aspects of the examination that should be emphasized include:
Overall state of mentation and mobility
Body condition score
Mucous membrane color and capillary refill time
Oral examination
Superficial palpation of the neck, thorax, abdomen, and limbs
Arterial pulse rate and quality
Peripheral lymph node palpation
Abdominal palpation
Auscultation of the thoracic cavity heart sounds, rhythm, and lung sounds
Examination of external genitalia
Rectal examination
Part 2: The Preoperative Period
Preparing the team, preoperative preparation.
The clinical team is ultimately responsible for preparing the patient for surgery. This preparation may be minimal for healthy animals undergoing elective surgery but may be more complicated for sick animals. It is essential that careful attention is given to the animal’s medical stability in order to optimize the chance of successful anesthetic and surgical outcome. Such considerations include:
Has food been withheld for an appropriate length of time?
Is intravenous fluid therapy required prior to anesthesia?
Are electrolyte and acid-base corrections necessary prior to anesthesia?
In order to ensure appropriate preparation of the patient, verbal and written communications must be provided for the patient care team so that everyone knows the patient signalment (breed, age, sex); what the animal has been admitted for; what it is having done and when; what preoperative blood tests or treatments, including fluid therapy, are required; and whether or not food or fluids can be made available for the animal to take orally. The written instructions on the “treatment sheet” should be signed by the responsible veterinarian and placed in a prominent location so that all those involved can easily refer to them.
Checklists have become the standard of care in human medicine and have greatly reduced the incidence of intraoperative errors. Although these seem “mechanical” in approach, having pre-agreed checklists to ensure full attention is paid to presurgical, anesthetic, and surgical preparations has been shown to reduce errors and lead to a more efficient surgical team and less wasted time. These checklists are easy to produce and should take little time to complete but should form part of the regular routine as well as forming part of the patient record so that they can be referred back to, should the need arise. 1 For instance, simple protocols such as painting the nails of the limb to be operated with an elective orthopedic procedure at the time of admission may in fact prevent the wrong limb from being operated on.
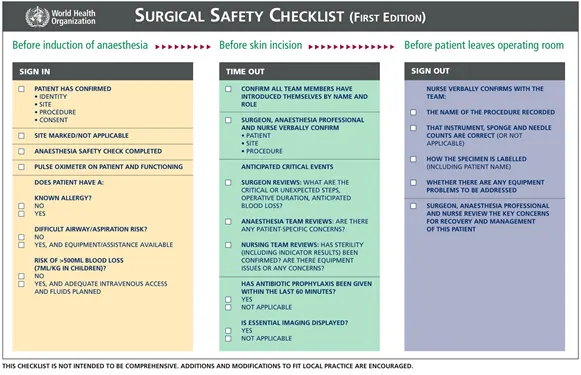
Example of preoperative checklist
Preparing the Patient
Principles of perioperative antibiotic use.
The use of antibiotics in surgery has the potential to reduce the incidence of postoperative wound infection; however, antibiotics are not a substitute for aseptic surgical technique, gentle tissue handling, adequate hemostasis, and the judicious use of suture material. The use of prophylactic antibiotics must also be weighed against the potential adverse effects such as organ toxicity, hypersensitivity reactions, development of resistant infections, and the potential for emergence of resistant strains of bacteria in the environment .
The goal of prophylactic antibiotics is to have adequate levels of the drug in the wound and surrounding tissues at the time of surgery. To be effective, the antibiotic concentration in the tissues should be greater than the minimum inhibitory concentration (MIC) for the bacterial isolates that are most likely to contaminate the wound. The concentration of antibiotics in the tissues is determined by the specific absorption, delivery, and elimination phases for the drug. To ensure rapid absorption, it is generally recommended to administer perioperative antibiotics intravenously (IV) to ensure maximum effectiveness. Antibiotic delivery to the tissues can be affected by protein-binding, lipid solubility, and other diffusion barriers such as the blood:prostate barrier. Antibiotic elimination is usually through renal excretion and/or hepatic biotransformation.
Most common antibiotics will reach peak serum concentrations within 30 to 60 minutes after IV administration and should, therefore, be given at least 30 minutes prior to surgery.
Antibiotic concentrations in the wound fluid parallel the serum concentrations due to the increased capillary permeability at the wound site and the high surface area to volume ratio in the wound compartment. Repeat doses of antibiotics may be necessary to maintain effective wound concentrations depending upon the potential bacterial contaminates, the duration of surgery, and the elimination profile of the drug. There is no proven benefit to administering prophylactic antibiotics any longer than 24 hours after surgery.
Recommended Antibiotic Protocol
The use of prophylactic antibiotics is indicated if the surgical procedure has a high risk of infection (>5%) or if the consequences of postoperative infection would be extremely devastating to the patient.
Cefazolin is an excellent choice for antimicrobial prophylaxis in small animal surgery. It has a low toxicity and excellent in-vitro activity against coagulase-positive Staphylococcus spp and Escherichia coli . The dosing protocol should be 20 mg/kg given slowly IV 30 minutes prior to surgery . It should be repeated, given slowly, IV every 3 hours intraoperatively until wound closure.
Cefuroxime is another excellent choice for perioperative use in surgery with better gram-negative spectrum. The dosing protocol should be 20 mg/kg given slowly IV 30 minutes prior to surgery . It should be repeated every 2 to 3 hours intraoperatively during surgery.
Surgical procedures that have a high risk of contamination with gram-negative or anaerobic bacteria may need a combination of antibiotics. Rational choices would include a metronidazole and fluoroquinolone combination or an aminoglycoside and metronidazole combination.
Wound Classification and the Use of Antibiotics
Wounds are classified into four categories based on an estimate of the degree of contamination. The classification of the wound will determine if antibiotics are indicated and whether they will be used in a prophylactic or therapeutic manner. As a general rule, prophylactic antibiotics are not indicated for routine clean surgical procedures unless surgical implants (eg, total hip replacement) are being used or the consequences of infection would be devastating for the patient. Certain clean-contaminated procedures warrant prophylactic antibiotics if the contamination is from an area that has a high bacterial population and is likely to cause infection (eg, colonic surgery). Contaminated and dirty procedures warrant antibiotic treatment that may be considered either prophylactic or therapeutic depending upon the timing of the administration of the antibiotics.
Wound Categories
Clean - relatively nontraumatic (ie, sharp trauma), not inflamed, no break in sterile technique, and where the respiratory, gastrointestinal, and/or urogenital tracts are not entered.
Clean-contaminated - gastrointestinal or respiratory tract entered without spillage, urogenital tract entered without infected urine, oropharynx entered, minor break in sterile technique.
Contaminated - gross spillage from gastrointestinal or respiratory tract, entering biliary or urogenital tract when infection is present, major break in sterile technique, fresh traumatic wound.
Dirty - bacterial infection is encountered. Examples include traumatic wounds with devitalized tissue, foreign material, or the presence of pus.
Antibiotics: Prophylactic vs Therapeutic
The administration of antibiotics is common practice in veterinary medicine that should be based on basic principles of bacteriology and pharmacology. Appropriate antibiotic therapy requires a thorough knowledge of the wound classification system, sources of bacterial contamination, common bacterial isolates and their susceptibility, common antibiotics and their spectrum, and basic dosing recommendations.
Antibiotics that are administered before the onset of infection or contamination are considered prophylactic antibiotics. Antibiotics that are administered after infections are already established are considered therapeutic antibiotics.
The goal of prophylactic antibiotics is to reduce the number of bacteria within a wound to such a level that the body's own defenses can control the contamination and prevent postoperative infection. The rational use of prophylactic antibiotics is based on the understanding of the risk for infection and the knowledge of the type of bacteria most likely to contaminate the wound.
The use of therapeutic antibiotics can be classified as either empiric or definitive . If the antibiotics are administered without the results of culture and susceptibility testing from the wound then they are considered empiric. If the antibiotics are administered based on culture and susceptibility testing from the wound then they are considered definitive.
Factors Influencing the Development of Wound Infection
Type and length of surgical procedure - prolonged surgical procedures increase local tissue damage and disrupt local immune responses. Each additional hour of anesthesia time over the first hour increases risk for infection by 30%. 2
Degree of wound contamination - Total bacterial burden will influence the development of surgical site infection.
The use of implants or foreign material - surgical implants or excess suture material left in the wound may trap bacteria or disrupt local immune responses.
Type of bacteria contaminating the wound - certain bacteria may have increased virulence or resistance, making treatment more difficult.
Host immune competence - immune suppression due to disease, chemotherapy, or malnutrition may increase the risk for wound infection.
Spectrum of activity and concentration of the antibiotics used - inappropriate choice of antimicrobial or dosing protocol may result in treatment failure.
Sources of Wound Contamination
Exogenous sources - operating room equipment, instruments, surgical implants, surgery personnel, and bedding.
Endogenous sources - patient's own microbial flora from skin, mucosal surfaces, gastrointestinal, respiratory, and urogenital tracts. The most common types of bacteria isolated from infected wounds of dogs are coagulase-positive Staphylococcus spp and E coli . These bacteria are part of the normal flora on the skin and in the gastrointestinal tract. Prophylactic antibiotics should be directed at these bacteria unless specific culture results are available. Other gram-positive, gram-negative, or anaerobic bacteria may be encountered when dealing with other wounds or procedures such as colonic surgery, otitis externa, or bite wounds.
Part 3: The Operative Period
Immediately prior to surgery, ensure the team is prepared.
Preoperative checklist (see Part 2: The Preoperative Period )
Preparation of patient and personnel
Prevention of surgical site infection (SSI)
Duties, roles, and communications
Controlling the controllable - organization and preparation, rather than speed, to minimize total anesthesia time. Preparation of anesthetic equipment and surgical instruments prior to the procedure, to promote efficiency.
Utilize "Time-Out"
Similar to checklists, it has been shown that taking time out to introduce the surgery team, the patient, the intended procedure, and the concerns about risks from a surgical and anesthetic perspective, prior to commencing surgery, reduces operating room mistakes. 3 This should also form part of the surgical ritual.
The Surgical Period
Aseptic technique.
Veterinarians perform many different routine and complex surgical procedures on a daily basis. Important factors for preventing postoperative infection include maintaining a clean hospital environment and practicing sterile techniques. A thorough understanding of the principles of aseptic surgery and proper techniques for equipment sterilization are necessary to reduce the incidence of postoperative infections.
Preparation of the Surgeon
Scrub suit - a comfortable, clean, lint-free, cotton/polyester blend that is easily cleaned. The scrub suit provides a partial barrier to micro-organisms and reduces the contamination of the surgical field. Laundering should take place within the practice at a temperature >70°C. Drying scrubs in an electric dryer is important, as it is this drying element that plays a significant role in reducing the bacterial burden. 4
Shoe covers - used for covering street shoes to prevent contamination of the operating room from outside bacteria.
Cap and mask - used to prevent droplets of saliva from entering the surgical site when talking. Masks filter particulate matter of various sizes depending upon the type of weave and material of the mask.
Gowns - worn to provide a barrier between the surgeon and the patient. Gowns can be either disposable or reusable and are usually made of high density cotton that is coated with a water repellent or made of synthetic materials. There are advantages and disadvantages for each type of gown including cost, barrier capability, cleaning requirements, and longevity that must be considered for each practice.
Hand Scrub vs Hand Rub - Traditional hand scrubs involve timed preparation of the surgeons’ hands, typically with povidone-iodine or chlorhexidine gluconate. Additionally, new hand rubs with alcohol-based agents have actually been shown to be more efficacious than surgical scrubs at reducing bacterial flora on the surgeon’s hands. 5
Gloves - worn to reduce the transmission of micro-organisms from surgeon to patient and vice-versa. Usually made of latex or vinyl that is coated on the inside with talc (magnesium silicate) or corn starch to make donning easier. Puncture holes develop relatively easily so gloves should not be considered completely impervious and do not replace an effective hand preparation.
Preparation of the Patient
Hair removal - perform a wide clip using clippers immediately prior to surgery. Use a sharp blade and avoid accidental cuts or burns. Clipping hours or days before surgery increases the chance of wound infection by allowing bacteria to colonize the cuts in the skin. Razors are not recommended for hair removal because they are more likely to cut the skin and increase the chance for wound complications. Excess hair should be vacuumed away before preparing the skin.
Skin disinfection - the most common skin disinfectants are povidone-iodine antiseptic solution diluted in sterile saline (used for areas involving mucous membranes) or chlorhexidine gluconate (for intact skin). The surgical site is initially prepared outside the operating room with chlorhexidine gluconate diluted in water at a 50:50 ratio. The final surgical site preparation is performed in the operating room. This is done in back and forth motion, horizontally and vertically, over the incision site with a single use chlorhexidine scrub followed by sterile alcohol wipe. Alternatively, the scrub can be performed in a circular fashion starting from the incision site and working outwards toward the edge of the clipped area. A spray of alcohol and/or a disinfectant solution can be applied as the final step in surgical site preparation.
Draping - sterile disposable coated-paper or reusable cotton drapes can be used for isolating the surgical site. The drapes are usually placed in a four-corner pattern overlapping with each one. The drape on the side closest to the surgeon should be placed first and then the other drapes systematically placed, being careful not to contaminate them as they are positioned. Hands should be protected by wrapping them in the corners of the drape as they are placed on the patient. In order to prevent contamination, the drape should not be moved closer to the surgical site once it has been placed on the patient.
The Analgesia Protocol
The value of a well thought out analgesic protocol is incontrovertible in terms of animal welfare and overall speed of recovery from a surgical procedure. The modern analgesia provision is for pre-emptive administration of analgesia (prior to surgery) that often involves more than one analgesic formulation (eg, opioid, nonsteroidal anti-inflammatory drug [ NSAID ] , and local anesthetic). Postoperative analgesia should be continued with parenteral administration of medication (typically opioids) in the hospital and should ideally be based on the results of an objective measure of animal discomfort or pain score (See Short Form of the Glasgow Composite Pain Scale ). Finally, there should be provision of oral medication (typically oral NSAIDs) at the time of patient discharge.
Hypothermia can increase perioperative blood loss, increase anesthetic recovery time, increase risk of cardiac arrhythmias, slow drug metabolism, and increase wound infection. It is important to use (safe) warming devices immediately after induction of anesthesia such as purpose-made warm air or warm water circulating blankets. Warning: thermal injury can result from prolonged exposure to heating devices set at temperatures that are only moderately too high.
Immediately After Surgery
Before closing.
Counting of the consumables should happen before any body cavity is closed:
Swabs/sponges (radio-opaque marked)
Instruments
Ideally, there should be one clinical waste bag per operating room, one per procedure.
Clean surgical incisional site with sterile swabs and sterile saline. Apply sterile dressing over wound and leave it on the site for 24 to 48 hours.
Establish who will notify owner about the results of the procedure.
Ensure a quiet recovery area is ready for the patient.
Part 4: The Postoperative Period & Patient Discharge
Following removal of the endotracheal tube, recovering animals should be placed in a quiet recovery area under direct observation and carefully monitored until fully conscious; this promotes a calm recovery while continuing to warm the patient.
Healthy animals undergoing elective surgery should not require postoperative fluid therapy but sick animals may need to continue fluid therapy after surgery. Body temperature should be monitored and warming blankets provided, if necessary. In addition, frequent monitoring of mucous membrane color, respiratory rate and effort, and pulse rate and quality should be done during this time. The intensity of postoperative care required varies for each patient and depends, again, on the age of the animal, nutritional and immune status, nature of the underlying disease, and the surgical procedure performed.
The presumption should be that the animal is experiencing pain and analgesia should be provided until the animal is conscious enough to undergo meaningful pain scoring (See Part 3: The Operative Period , under The Analgesia Protocol ); after that time, analgesia provision should be guided by the pain scoring.
Patient Discharge
The key to successful recovery of a surgical patient is the early identification and management of any complications. It will be the responsibility of the surgeon to explain potential complications to the owners at the time of discharge so they know how to identify concerns and bring them to the attention of the veterinary team. To facilitate this, it is essential that the communication at discharge equips the owners with the information they need regarding ongoing monitoring of their pet’s general demeanor and monitoring of the surgical site for signs of complications (eg, increased pain, redness, swelling, wound discharge). In addition, the discharge instructions should provide information about the ongoing administration of analgesia and any other management requirements of the wound, or its dressings or bandages. It is particularly critical for an animal that is being discharged with a limb bandage that the owner knows when it needs to be changed and what signs to look for that might indicate early bandage-related complications. The discharge conversation does not need to be lengthy and can be facilitated by providing the client with a discharge instruction sheet to read prior to the face-to-face discharge conversation.
An example of a discharge sheet is below. It should contain the patient details, the final diagnosis (if appropriate), and what procedure was performed. Critically, from the owner’s perspective, it should explain whether and how much the animal can be exercised, what ongoing medication is needed and how it is given, whether food and water can be given normally, and when they are due back with the pet for follow-up examination/suture removal.
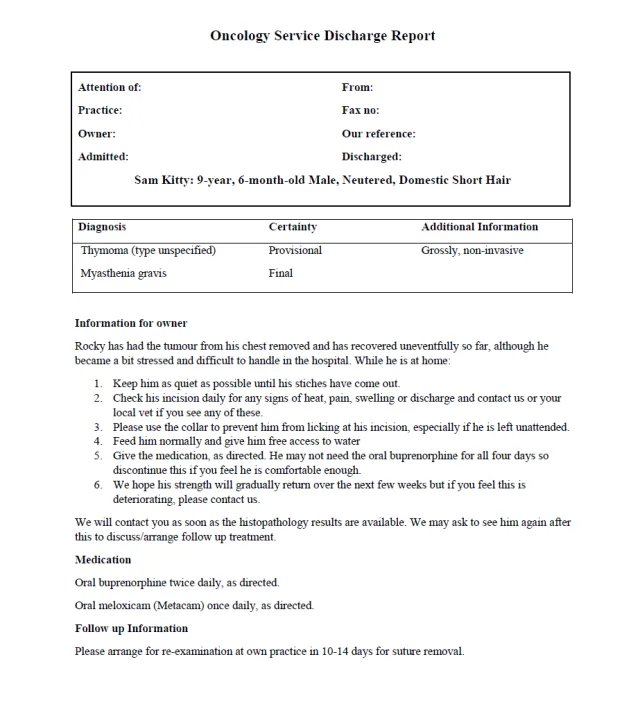
Example of a discharge sheet
Successful management of the surgical patient requires excellent communication, detailed preparation, and manual dexterity. Clients must be advised of what treatment is being planned and must give their informed consent. The most efficient way to remove doubt about patient treatment, and thereby reduce the risk for errors, is to introduce checklists and standard operating procedures that encourage all members of the care team to carefully examine what is being done and why. In addition, it is essential to develop a culture within the team, whereby if questions or concerns arise, anyone can voice these without fear of reprisal and that this should be done in the best interest of delivering optimal patient care. Preparation and efficiency, not rushing the surgical procedure, are the key to keeping total anesthesia time to a minimum. Finally, including the owners in the postoperative recuperation is facilitated by providing carefully thought out, concise discharge instructions that outline their responsibilities.
Connect with Us
- Agri-Commodities
- Asean Economic Community
- Banking & Finance
- Business Sense
- Entrepreneur
- Executive Views
- Export Unlimited
- Harvard Management Update
- Monday Morning
- Mutual Funds
- Stock Market Outlook
- The Integrity Initiative
- Editorial cartoon
- Design&Space
- Digital Life
- 360° Review
- Biodiversity
- Climate Change
- Environment
- Envoys & Expats
- Health & Fitness
- Mission: PHL
- Perspective
- Today in History
- Tony&Nick
- When I Was 25
- Wine & Dine
- Live & In Quarantine
- Bulletin Board
- Public Service
- The Broader Look
Today’s front page, Monday, April 29, 2024

PHAP, PAPO partner for ethical interactions in the healthcare sector
- April 29, 2024
- 3 minute read

Several organizations representing patient organizations, medical device and biopharmaceutical industry associations, healthcare professional and hospital groups have partnered to advance patient welfare through ethical interactions.
The Philippine Consensus Framework for Ethical Collaboration is an initiative being pushed forward by country counterparts of reputable global healthcare organizations namely the International Alliance of Patient Organizations (IAPO), World Medical Association (WMA), International Council of Nurses (ICN), International Federation of Pharmaceutical Manufacturers & Associations (IFPMA), and International Pharmaceutical Federation (IPF).
These international organizations developed the “Consensus Framework for Ethical Collaboration Between Patients’ Organizations, Healthcare Professionals, and the Pharmaceutical Industry” in support of high-quality patient care.
In 2020, the Philippines became one of the Asia Pacific Economic Cooperation (APEC) nations that has adopted its own Consensus Framework. The goal is to put patients at the center of all healthcare efforts through the advancement of ethical principles.
“We welcome the Consensus Framework as a commitment to putting the patients’ interests as top priority when making medical decisions. All these crucial interactions must be in support of patients for us to be better informed and empowered to decide on the most appropriate treatment from the options available to us. The ethical and professional conduct of everyone in the healthcare community is critical to ensuring that patients’ rights are protected and that the patients have the ability to make decisions based on their needs and preferences,” said Philippine Alliance of Patient Organizations (PAPO) President Ms. Karen Alparce- Villanueva.
PAPO is the umbrella organization of 50 disease-specific patient groups representing at least a million Filipino patients nationwide. Their aim is to strengthen the voice of the patients in the country so that the healthcare system is designed and delivered in a way that will answer the needs of patients. PAPO is also a member of the International Alliance of Patient Organizations
(IAPO) which is a unique global alliance of national, regional and international groups representing patients as well as holds a Non-State Actor status with the World Health Organization (WHO).
“We are honored to be one of the signatories of the Philippine Consensus for Ethical Collaboration as this initiative is aligned with our mandate to promote ethics and professional conduct in the pharmaceutical industry and the healthcare ecosystem. The Pharmaceutical and Healthcare Association of the Philippines and our Members are united in our resolve to act ethically and professionally so that all medical decisions will be made in the best interest of patients,” said PHAP President Dr. Diana Edralin.
A member of the IFPMA, PHAP represents the biopharmaceutical medicines and vaccines industry in the country. Its Members are in the forefront of research and development efforts for COVID-19 and other diseases that affect Filipinos.
The Consensus Framework is a principles-based commitment to support ethical conduct across the organizations from government, to private sector, not-for-profit groups, healthcare professionals and providers, and patient associations.
It builds on the APEC Mexico City Principles for Voluntary Codes of Business Ethics in the Biopharmaceutical Sector which was adopted in 2011 during the U.S. APEC host year and recognized by APEC Leaders and Ministers.
The Philippine Consensus Framework espouses the following principles: Put Patients First; Support Basic and Ethical Research and Innovation; Ensure Independence and Ethical Conduct; Promote Transparency and Accountability; Establish Trust and Solidarity; Prioritize Quality Care and Innovation; and Foster Respect for All.
Meanwhile, the Consensus Framework does not replace the individual ethical codes of its 20 organizational signatories representing patients, healthcare providers, nurses, pharmacists, medical technologists, hospitals, non-profit international organizations, medical device and biopharmaceutical industry.
The PHAP Code of Practice, for example, remains in full force among its members.
“As a sector that strongly believes in the conduct of professional business practices, PHAP has undertaken pioneering initiatives in helping ensure that we remain committed to promoting people’s health with integrity. We established the PHAP Code of Practice in 1993 to govern our actions, and we are proud of our members because they have deeply embedded integrity in their culture, decisions and interactions,” said PHAP Executive Director Mr. Teodoro Padilla.
Adherence to the PHAP Code of Practice is a requirement for its membership. It is aligned with the Mexico City Principles, the Code of Practice of the International Federation of Pharmaceutical Manufacturers and Associations (IFPMA), and the Department of Health (DOH) Administrative Order on DOH AO 2015-0053 Implementing Guidelines on the Promotion and Marketing of Prescription Products and Medical Devices. It is also aligned with international and local laws and regulations.

Revolutionizing patient engagement: A new model for clinical trials recruitment unveiled
- BusinessMirror
- April 26, 2024

No respite: Extreme heat hounding Pinoys this Friday and Saturday, 7K schools halt face-to-face classes
- Claudeth Mocon-Ciriaco
- April 25, 2024

Get better sleep with these 5 tips from experts
- Kenya Hunter / The Associated Press

2 Filipino pharma companies win healthcare awards in Singapore
- Manuel Cayon

TMC South Luzon, Landers Superstore Nuvali’s partnership officially begins

Vaccination is still the most effective method vs pertussis

DOH told to expedite flu immunization campaign for seniors to prevent outbreaks

DEATH TALKS: End-of-life planning is healthy, practical–insurer
- Roderick Abad

Healthway Cancer Care Hospital offers world-class cancer care at affordable prices
- Anne Ruth Dela Cruz

Leading the Way: Precision Imaging Sets New Standards in Cancer Diagnosis

New clinical trials recruitment model powered by AI, blockchain launched in PHL

Drop in Chronic Kidney Disease in Type 2 Diabetes seen with new drug
- John Eiron R. Francisco

Borough Lasik Center expands to Bacolod City, opens 2nd satellite clinic

For Makati Medical Center, the future is now with acquisition of da Vinci XI Robotic System

Asian Hospital extends medical services through HEAL Program

PHL is a complex, inspiring case study in sexual, reproductive health, rights–UNFPA
- Rizal Raoul Reyes

Go bats for improved public health services

Fullerton Health revolutionizers preventive healthcare in PHL with mWell
Seeing magenta new heat warning system signals extreme danger.
- Seth Borenstein / AP Science Writer
- April 23, 2024

Health and wellness corporate giveaways promote well-being among employees
- April 20, 2024
Input your search keywords and press Enter.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- For authors
- New editors
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Online First
- How my ACL injury recovery journey led me to the medical field?
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Haiqiang Huang 1 , 2
- 1 Department of Orthopedics , The Second Affiliated Hospital, Jiangxi Medical College, Nanchang University , Nanchang , Jiangxi , China
- 2 The Second Clinical Medical College , Jiangxi Medical College, Nanchang University , Nanchang , Jiangxi , China
- Correspondence to Haiqiang Huang, Department of Orthopedics, The Second Affiliated Hospital, Nanchang University Jiangxi Medical College, Nanchang, Jiangxi, China; 4203121456{at}email.ncu.edu.cn
https://doi.org/10.1136/bjsports-2023-108012
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
- Anterior Cruciate Ligament
- Athletic Injuries
During a basketball game, I was hit on the inside of my left knee by an offensive player, resulting in an anterior cruciate ligament (ACL) injury and a dislocation of my patella. To recover as quickly as possible, I went to the Second Affiliated Hospital of Nanchang University for an arthroscopic ACL reconstruction surgery. After going through months of rehabilitation, my knee was finally back to a level that allowed me to resume all my activities. As an ordinary person from a small town, this experience deeply made me appreciate the nobility and sanctity of medicine. Since then, I have been determined to become a doctor. Through hard work and dedication, I have successfully enrolled in the Jiangxi Medical College at Nanchang University.
Initial healthcare pathway
After the injury, I was swiftly transported to the local county hospital. Given my young age, the physician recommended a non-surgical treatment approach, encompassing functional knee bracing and activity modification. 1 However, after 2 weeks of this treatment, my symptoms worsened. For effective treatment, my mother took me to a major city hospital. There, a thorough examination, including an MRI, 2 identified both an ACL injury and patellar dislocation. Immediate ACL reconstruction was recommended, but the invasive nature of the surgery gave us pause. Considering my age and concerns about the surgical scar impacting my appearance and prognosis, 3 the doctor advised seeking minimally invasive surgery (surgery to minimise patient injury through very small incisions and specialised instruments) at a provincial tertiary hospital.
ACL surgery
After careful consideration, we decided to undergo this less invasive arthroscopic procedure. As I was transported to the operating room on a transfer bed, it was my first surgical experience, and I was engulfed by a mixture of fear and anxiety. Dr Hao reassured me with a comforting gesture and words, ‘It’s okay, don't be nervous’. The anaesthesiologist then administered the anaesthesia, and the operation began.
On awakening, I found Dr Hao already standing before me. He explained, ‘ACL reconstruction is just the beginning of treatment, not the end’. Responding, I expressed my fervent desire to return to the basketball court, to run and play sports again. Dr Hao advised gently, ‘Ensure to stay active and employ scientific rehabilitation methods. With active and scientific approaches, your recovery will be swift, allowing you to resume your normal life’.
Postsurgical rehabilitation
On the third day postoperation, I was successfully discharged from the hospital, yet the journey of postoperative rehabilitation lay ahead. By researching and following the doctor’s advice, I devised a scientific rehabilitation plan for myself. Throughout this journey, I gained a profound appreciation for the medical profession, which further deepened my interest in medicine.
Early rehab phase (1–2 weeks after surgery):
I worked on quadriceps exercises to prevent muscle atrophy. Usually, I would lie in bed and try to contract my quadriceps. It was not an easy process for me; I often feel pain.
I also practised patellar mobilisation on my doctor’s advice to prevent knee joint adhesions. I would lie down with my knee straight. Then, I gently massaged around the kneecap with my fingers to relax the muscles and tissues. Next, I'd gently hold the patella and move it up, down, left and right. My family had received a detailed demonstration from my doctor beforehand, so I rarely experienced discomfort during this exercise.
Intermediate rehab phase (2–6 weeks after surgery):
I engaged in joint range of motion exercises. It started with passive exercises, where I gently flexed and extended my knee using my hands, which was quite easy. However, what followed was painful and lengthy active exercises. During these, I had to wear a professional knee brace that helped record changes in my joint’s range of motion. Sometimes, it felt like my brain could not control my knee, and my joint range of motion would fluctuate unpredictably, even decreasing at times, which was extremely frustrating and disheartening. But with the consistent encouragement from my doctor and loved ones, I kept at it and eventually achieved good recovery results.
Late rehab phase (after 6 weeks post-surgery):
Six weeks postsurgery, my doctor removed my knee brace and noticed that the diameter of my left thigh was 3 cm smaller compared with my healthy right side. My doctor advised me to continue strengthening my quadriceps until both thighs were of equal diameter. Of course, I also had to face the subsequent long-term rehabilitation training, which required persistent determination and an optimistic mindset. After 10 months, I was completely out of rehabilitation.
During this process, I continued to appreciate the distinct allure of medicine and expressed my gratitude to my attending physician, Dr Hao. I also came to understand that for a patient, while surgery is critical, the role of scientific postsurgical rehabilitation is equally indispensable. Therefore, in my clinical work and study, I sincerely assist every patient undergoing ACL reconstruction, hoping they can recover better.
Through this injury, surgery and rehabilitation experience, medicine took root in my heart, guiding me to a career in medicine and renewing my relationship with Dr Hao, my attending physician at the time, as his student ( figure 1 ). As both a patient and a medical student, I believe there are three main reasons why I was able to return to my normal life so quickly after my ACL reconstruction:
The selection of the correct surgical approach.
Maintaining a healthy and persistent mental state during rehabilitation.
Developing a scientific rehabilitation programm. 6
- Download figure
- Open in new tab
- Download powerpoint
Photo of the patient with Dr. Hao.
Ethics statements
Patient consent for publication.
Consent obtained directly from patient(s).
Ethics approval
Not applicable.
Acknowledgments
I would like to express my gratitude to my attending physician and mentor Professor Liang Hao (Department of Orthopedics, The Second Affiliated Hospital, Jiangxi Medical College, Nanchang University, Nanchang, China) for providing me with surgical treatment and rehabilitation training, guidance during the writing process of this manuscript, and assistance in my medical career. Thanks to my classmates Bofan Chen, Haimin Zeng (The Second Clinical Medical College, Jiangxi Medical College, Nanchang University, Nanchang, China) and Jie Peng (Department of Sports Medicine, Huashan Hospital, Fudan University, Shanghai, China; The Second Clinical Medical College, Jiangxi Medical College, Nanchang University, Nanchang, China), for their encouragement and support, as well as their assistance in the writing and revision process of this manuscript. The Sports Medicine Team (Department of Orthopedics, The Second Affiliated Hospital, Jiangxi Medical College, Nanchang University, Nanchang, China) for their help in my surgical treatment and rehabilitation training.
- Diermeier TA ,
- Rothrauff BB ,
- Engebretsen L , et al
- van Geuns RJ ,
- Wielopolski PA ,
- de Bruin HG , et al
- Hutchison J
- Benjaminse A ,
- Gokeler A ,
- van der Schans CP
- van Melick N ,
- van Cingel REH ,
- Brooijmans F , et al
- Kotsifaki R ,
- Korakakis V ,
- King E , et al
Contributors HH is the sole author of this piece.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient and public involvement statement The author of this article, HH, is a participating patient in the content of this article. Professor Liang Hao participated in the patient's surgery, and the Sports Medicine Team from the Second Affiliated Hospital of Jiangxi Medical College, Nanchang University participated in the patient's rehabilitation treatment.
Provenance and peer review Not commissioned; externally peer-reviewed.
Read the full text or download the PDF:

- Research Overview
- Research Activities
- Research Resources
- Training & Education
- Collaborate With NCATS
- Funding Overview
- Open Funding Opportunities
- Small Business Programs
- Funding Policy & Operating Guidelines
- Grant Information
- Challenges and Prize Competitions
- Scientific Review
- Conference Grant Information
- Resources for You
- Resources for Researchers
- Resources for Trainees
- Resources for Rare Disease Patients and Advocates
- News & Events Overview
- Newsletters
- Scientific Publications
- Infographics & Fact Sheets
- NCATS Overview
- About Translational Science
- Advisory Committees
- Careers at NCATS
- Director's Corner
- Divisions & Offices
Rare Disease Day at NIH 2024: Showcasing Voices and New Opportunities
April 23, 2024

Attendees at Rare Disease Day at NIH. ( NCATS )
On Feb. 29, 2024 — the rarest day of the year — patients, clinicians, researchers, drug developers and advocates traveled to the NIH main campus or tuned in to NIH VideoCast for Rare Disease Day (RDD) at NIH. More than 2,000 people attended RDD at NIH. Co-sponsored by NCATS and the NIH Clinical Center, the annual event raises awareness about rare diseases and the people they affect. It also highlights NIH partnerships that advance research and new treatments. This year’s event included scientific sessions, patient stories, scientific posters and exhibits, and art and film exhibits.
NIH is working hard to address the significant and often unmet needs of those affected by rare diseases. In her remarks, NIH Director Monica M. Bertagnolli, M.D., emphasized that rare diseases span across NIH’s research portfolio.
“We at NIH believe that caring for people with rare diseases is at the heart of everything that we do,” she said.
RDD at NIH speakers addressed a wide range of topics, including the rare disease diagnostic odyssey, drug repurposing and development, gene therapy, artificial intelligence (AI), and public-private partnerships. Many of their stories highlighted NIH’s integral role in addressing rare diseases from all angles — research, therapeutic development and information sharing.

NCATS Director Joni L. Rutter, Ph.D., talking with Rare Disease Day at NIH attendees. ( NCATS )
“Rare Disease Day is a day to celebrate our successes, to honor those we hold dear and honor those we’ve lost,” said NCATS Director Joni L. Rutter, Ph.D. “And today, we pause, granting ourselves the space for creativity and contemplation, so that tomorrow, we can speed up with a renewed sense of purpose.” Rutter recently published a guest NIH blog post that highlights the need to communicate about rare diseases research.
The Diagnostic Odyssey: Through the Lens of Patients and Caregivers
Dominique C. Pichard, M.D., director of the NCATS Division of Rare Diseases Research Innovation, shared the obstacles she faced in obtaining a diagnosis and treatment for her daughter, who has Rett syndrome . Pichard — a clinician and leader in rare diseases research — advocated for her daughter’s diagnosis. She had recognized that her daughter showed signs of Rett syndrome — a neurodevelopmental condition that is often marked by loss of developmental abilities between 6 to 18 months of age.
Pichard’s concerns were largely dismissed by her daughter’s physicians. “I was not seen; I was not heard,” she recounted. “But in my gut, I knew.”
Almost one year after raising concerns, Pichard finally received a diagnosis for her daughter. Her experience — known as the “diagnostic odyssey” — reflects the struggles faced by families in the rare diseases community. Patients may wait as long as 15 years to receive a correct diagnosis .
Jessica Swanson shared the challenges that her family faced in finding a diagnosis for her daughter, Isla, who began experiencing tonic-clonic seizures at age 7 months. After years without answers, Swanson turned to the Undiagnosed Diseases Network (UDN) . Just before her 10th birthday, Isla was diagnosed with CDKL5-deficiency disorder .

Jessica Swanson shares about her family’s journey to diagnosis at Rare Disease Day at NIH. ( NCATS )
Swanson explained that the diagnosis provided the family with a label, a community and hope for the future. She emphasized the value of building connections with other patients and families. “The absence of a diagnosis left us in a state of perpetual uncertainty, exasperating an emotional toll on our family,” Swanson recounted. “The rare disease community, however, taught us ‘rare’ does not equal ‘alone.’ And there is strength in shared experiences.”
The UDN is a research program that combines basic and clinical research to help individuals who have sought a clinical diagnosis without success — and their families — understand their health conditions. The program is supported by 17 institutes and centers at NIH, including NCATS. It is led by the National Institute of Neurological Disorders and Stroke.
Shortening the diagnostic odyssey is only part of the challenge. Helping all people with rare diseases access treatments in an equitable way is another major effort. Seema R. Lalani, M.D., spoke on Project GIVE (Genetic Inclusion by Virtual Evaluation) , which is funded by NCATS . Project GIVE focuses on a community-based partnership to reduce health disparities and improve access to care for children in Texas’ Rio Grande Valley, a historically underserved region.
Project GIVE uses Consultagene, a patient referral platform that provides educational resources and genetics health care services that have helped families obtain diagnoses and begin treatments. To date, 109 patients have been enrolled in Project GIVE, and 61 families have received whole-genome sequencing results. Thus far, 17 families have received a resolved diagnosis, and 2 have received a partially resolved diagnosis.
Project GIVE is just one example of NCATS’ efforts to foster community engagement, educate providers, and help to reduce health disparities for families affected by rare diseases. During her remarks, Lalani quoted parents of children with rare diseases in the Rio Grande Valley, including this reflection: “Project GIVE gave [us] not only hope but peace of mind. We were able to finally receive a diagnosis after years of trying to find an answer … I can’t put into words how thankful we all are.”
Artificial Intelligence for Rare Diseases: Exploring New Possibilities
Manisha Balwani, M.D., M.S., FACMG; Kimberly A. Moran, Ph.D., M.B.A., CDP; Ewy A. Mathé, Ph.D.; Christine Cutillo, M.M.C.i. ( NCATS )
Speakers also explored AI and its role in rare diseases research. NIH has recognized that AI can assist with data-driven discovery in various areas of biomedical research, including rare diseases. The speakers discussed ways to make AI tools more inclusive and equitable. They shared stories that demonstrated using AI to shorten the diagnostic odyssey, identify patients for clinical trials, and build tools for drug repurposing. They also discussed how to protect patient privacy and enhance data sharing.
Kimberly A. Moran, Ph.D., M.B.A., explained how she uses AI to identify patterns within groups of people with myasthenia gravis , a rare autoimmune neuromuscular disease. Insights from these data may help identify patients who have not yet received a diagnosis for this disorder. Moran explained that AI can help clinicians predict patients’ symptoms and develop personalized treatments. She also emphasized the importance of discussing AI technologies with patients.
Moran noted doctors should explain the implications and potential of patients’ sharing their data. “It’s going to take this entire community — to be educated, to be literate in terms of data and understanding the power,” she said. “We see the rare disease community willing to give their data … but this will come to be a personal choice in the future.”
AI may improve diagnoses, predict the effects of treatments, and match patients to the right treatment, explained Ewy A. Mathé, Ph.D., director of informatics in the NCATS Division of Preclinical Innovation. AI can also help researchers ask new questions to test, find new treatments, and study many diseases at once. Mathé explained how CURE ID , an AI-driven data collection tool built by NCATS and the U.S. Food and Drug Administration (FDA), can help researchers find rare disease treatments among existing drugs.
Public-Private Partnerships: Leveraging Unique Funding Models

Eric P. Hoffman, Ph.D., and Sharon Hesterlee, Ph.D., with Dominique C. Pichard, M.D. ( NCATS )
Public-private partnerships are another key approach that NCATS uses to speed the development of treatments for rare diseases. Eric P. Hoffman, Ph.D., and Sharon Hesterlee, Ph.D., shared how a partnership between NCATS and ReveraGen BioPharma, Inc., led to FDA approval of vamorolone , a drug used to treat Duchenne muscular dystrophy (DMD) .
ReveraGen’s business model for developing vamorolone used venture philanthropy partners rather than venture capital investors. ReveraGen also had a different kind of partnership with NCATS, through its Therapeutics for Rare and Neglected Diseases (TRND) program . TRND supports preclinical development of drugs to treat rare or neglected disorders. With help from the TRND program, ReveraGen demonstrated that the steroid compound VBP15 could be used to treat DMD symptoms with minimal side effects.
Hesterlee explained that the philanthropic model helped ReveraGen obtain funding for a drug that had great potential but had not captured the interest of more traditional investors.
“The community recognized that this was a need, and it was worth doing,” she said. “And so, from that sense, it really worked well to have the nonprofit investment.” Hesterlee and Hoffman emphasized that this partnership model can be used for efforts focused on other rare diseases.
Rare Diseases Research and Resources
The personal and powerful stories from RDD at NIH underscored the breadth and impact of NIH and NCATS rare diseases research and other activities. They also showcased many great research and educational resources, including those below, that the community can access any time.
- Genetic and Rare Diseases (GARD) Information Center
- Platform Vector Gene Therapy (PaVe-GT) Pilot Project
- Bespoke Gene Therapy Consortium
- Rare Diseases Registry Program (RaDaR)
- Somatic Cell Genome Editing Program
- NCATS Toolkit for Patient-Focused Therapy Development
- RARe-SOURCE
Last updated on April 23, 2024

IMAGES
VIDEO
COMMENTS
Therefore, hospitals can significantly improve the quality of the service provided by exploring and understanding the individual patient journey [ 12 - 14 ]. Many tools may be used to measure and understand patient experience [ 15, 16 ]. Surveys are the methods mainly used to capture the patient experience and to evaluate the quality and ...
The Experience Journey of the Patient. A recurrent and prominent theme in discussions of the patient experience is centering the patient's perception or perspective on the health care they receive (7,13).Health-care providers who seek to understand the patient's perspective of their experience will obtain a greater understanding of the patient experience.
Therefore, hospitals can significantly improve the quality of the ser-vice provided by exploring and understanding the individual patient journey [12-14]. Many tools may be used to measure and understand patient experience [15, 16]. Surveys are the methods mainly used to capture the patient experience and to evaluate the quality and safety of ...
A patient's journey begins before they even walk through the doors of a doctor's office or hospital. It may start when they research symptoms, treatment options, and healthcare providers. It can include referrals from friends, information found on social media, or advertisements.
A recent study analysed the hospital stay experience through the use of unstructured diaries completed in a patient's own words. ... evaluation of the self-perceived impact of the different issues related to the hospital journey on the patient's life (e.g., instructions on how to get to the hospital or in case of waiting; not feeling pain ...
patient experience of the hospital journey. Methods. A qualitative study of orthopaedic patients admitted for hip and knee replacement surgery in. a 250-bed university hospital was performed ...
Schwannomatosis. A "Patient Journey" is a personal testimony that reflects the needs of patients in two key reference documents—an accessible visual overview, supported by a detailed ...
Introduction. Quality and safety guidelines in healthcare services are increasingly encouraging and mandating engagement of patients, clients, and consumers in partnerships. 1 The aim of many of these partnerships is to consider how health services can be improved, in relation to accessibility, service delivery, discharge, and referral. 2, 3 Patient journey mapping is a research approach ...
Process mapping enables the reconfiguring of the patient journey from the patient's perspective in order to improve quality of care and release resources. This paper provides a practical framework for using this versatile and simple technique in hospital. Healthcare process mapping is a new and important form of clinical audit that examines how we manage the patient journey, using the ...
It helps you visualize the process patients go through to receive care, complete a treatment plan, and/or reach a desired outcome. When done correctly, patient journey maps make it easier for you to identify pain points, discover opportunities and re-align treatment and care approaches across the entire healthcare system.
The patient is rational and emotional, so all their surroundings need to be integrated according to the patient's sensory organs. Thus, it is important to see the healthcare journey through the patient's eyes: their observations, emotions, and feelings; the usual route they take for services (outpatient clinic, urgent care, hospitalization, specialty care, etc.); the sensory qualities of ...
The patient journey is the entire sequence of events that begins when the patient first develops a need for clinical care and engages with your organisation. It follows the patient's steps as they navigate your healthcare system, from initial scheduling to treatment to continuous care. Learn how you can collect data and drive action along ...
Effective patient journey mapping requires you to see how the patient navigates the journey through their point of view. Omni-channel listening is a valuable strategy in this step of journey mapping. Listening to your patients across all the channels can provide a clearer picture of their perceptions and behaviors as they engage with your ...
Engaging consumers and patients where they are builds trust and confidence that keeps patients in the system and encourages them to refer their friends and family to your practice. According to the Beryl Institute, 70% of patients will share a positive experience with others. But your bigger risk is that 76% will share a negative one.
Patient journey is a term referring to a patient's experience throughout an episode of care, beginning at admission and concluding with hospital discharge.. The renewed focus on patient experience in recent years stems from growing trends in healthcare consumerization and value-based care initiatives.To remain competitive, providers are beginning to consider patients more as customers and ...
The wide implementation of patient safety improvement efforts continues to face many barriers including insufficient involvement of all stakeholders in healthcare, lack of individual and organizational learning when medical errors occur and scarce investments in patient safety. The promotion of systems-based approaches offers methods and tools to improve the safety of care. A multidisciplinary ...
Purpose To understand how different methodologies of qualitative research are able to capture patient experience of the hospital journey. Methods A qualitative study of orthopaedic patients admitted for hip and knee replacement surgery in a 250-bed university hospital was performed. Eight patients were shadowed from the time they entered the hospital to the time of transfer to rehabilitation ...
A patient's journey through the system Published: October 29, 2017 3:11pm EDT Matthew Grant , Monash University , Anna Collins , The University of Melbourne , Jennifer Philip , The University of ...
And in 2016, only 56% of hospital in-patients felt involved in decisions about their treatment (Care Quality Commission 2017). ... Putting patients in control through access to information and support will enable people to take greater responsibility. ... services can create a 'Perfect Patient Information Journey' and transform the ...
"When a patient completes a journey through cancer treatment, they've gotten through something very hard. That's not just their success," says Ann Bredensteiner, manager of integrative health and supportive care at IU Health Joe and Shelly Schwarz Cancer Center.. "It's also the success of their family, their caregivers, and all the people who worked so hard to get them to that point.
Purpose: To understand how different methodologies of qualitative research are able to capture patient experience of the hospital journey. Methods: A qualitative study of orthopaedic patients admitted for hip and knee replacement surgery in a 250-bed university hospital was performed. Eight patients were shadowed from the time they entered the hospital to the time of transfer to rehabilitation.
The patient's journey. So you can put the operation into context for the patient, here is a typical "patient journey" for elective or planned surgery: 1. G.P. referral: the patient's General Practitioner decides that the patient has a condition that may require surgery and refers the patient to the hospital (usually a few days or weeks later). 2.
among hospital patients3,15-19 and many attempts have been made to redress this.20-26 In some cases, ... Patient Journey through Enteral Nutritional Care 189. and alternative feeding methods must be consid-ered. A range of access routes is available and, similarly, there are many different products which ...
The transition from hospital to outpatient care is a particularly vulnerable period for patients as they move from regular health monitoring to self-management. This study aimed to map and investigate the journey of patients with polymorbidities, including type 2 diabetes (T2D), in the 2 months following hospital discharge and examine patients' encounters with healthcare professionals (HCPs).
Introduction. Surgery is frequently performed in small animal practice with operations ranging from routine elective sterilization procedures to complex urgent or emergency procedures. In order to manage the surgical patient in an optimal way, the clinical team will need to be in command of every aspect of the animal's management.
Several organizations representing patient organizations, medical device and biopharmaceutical industry associations, healthcare professional and hospital groups have partnered to advance patient ...
Conclusion. Through this injury, surgery and rehabilitation experience, medicine took root in my heart, guiding me to a career in medicine and renewing my relationship with Dr Hao, my attending physician at the time, as his student ().As both a patient and a medical student, I believe there are three main reasons why I was able to return to my normal life so quickly after my ACL reconstruction:
Artificial intelligence (AI) has emerged as a powerful tool in healthcare significantly impacting practices from diagnostics to treatment delivery and patient management. This article examines the progress of AI in healthcare, starting from the field's inception in the 1960s to present-day innovative applications in areas such as precision medicine, robotic surgery, and drug development. In ...
Project GIVE uses Consultagene, a patient referral platform that provides educational resources and genetics health care services that have helped families obtain diagnoses and begin treatments. To date, 109 patients have been enrolled in Project GIVE, and 61 families have received whole-genome sequencing results.
Among those, a total of 31,857 COVID-19 cases have been detected; 4 patients are in hospital; and 126 patients have tests pending. There have been 262 in-hospital deaths. ... Throughout the pandemic, OHSU offered low-barrier drive-through testing that has tracked surges in case counts, at various points accommodating as many as 700 people a day ...