CDC updates Covid isolation guidelines for people who test positive

People who test positive for Covid no longer need to isolate for five days , the Centers for Disease Control and Prevention said Friday.
The CDC’s new guidance now matches public health advice for flu and other respiratory illnesses: Stay home when you’re sick, but return to school or work once you’re feeling better and you’ve been without a fever for 24 hours.
The shift reflects sustained decreases in the most severe outcomes of Covid since the beginning of the pandemic, as well as a recognition that many people aren’t testing themselves for Covid anyway.
“Folks often don’t know what virus they have when they first get sick, so this will help them know what to do, regardless,” CDC director Dr. Mandy Cohen said during a media briefing Friday.
Over the past couple of years, weekly hospital admissions for Covid have fallen by more than 75%, and deaths have decreased by more than 90%, Cohen said.
“To put that differently, in 2021, Covid was the third leading cause of death in the United States. Last year, it was the 10th,” Dr. Brendan Jackson, head of respiratory virus response within the CDC’s National Center for Immunization and Respiratory Diseases, said during the briefing.
Many doctors have been urging the CDC to lift isolation guidance for months, saying it did little to stop the spread of Covid.
The experiences of California and Oregon , which previously lifted their Covid isolation guidelines, proved that to be true.
“Recent data indicate that California and Oregon, where isolation guidance looks more like CDC’s updated recommendations, are not experiencing higher Covid-19 emergency department visits or hospitalizations,” Jackson said.
Changing the Covid isolation to mirror what’s recommended for flu and other respiratory illnesses makes sense to Dr. David Margolius, the public health director for the city of Cleveland.
“We’ve gotten to the point where we are suffering from flu at a higher rate than Covid,” he said. “What this guidance will do is help to reinforce that— regardless of what contagious respiratory viral infection you have — stay home when you’re sick, come back when you’re better.”
Dr. Kristin Englund, an infectious diseases expert at the Cleveland Clinic, said the new guidance would be beneficial in curbing the spread of all respiratory viruses.
“I think this is going to help us in the coming years to make sure that our numbers of influenza and RSV cases can also be cut down, not just Covid,” she said.

Latest news on Covid
- Common Covid symptoms follow a pattern now, doctors say.
- Covid during pregnancy can cause health issues in babies.
- How big of a risk is coinfection with Covid and other viruses?
Still, the decision was likely to draw criticism from some clinicians who point to the fact that the U.S. logged 17,310 new Covid hospitalizations in the past week alone.
“It’s something that is likely to draw a wide array of opinions and perhaps even conflicting opinions,” said Dr. Faisal Khan, Seattle’s director of public health. “But [the CDC’s] rationale is sound in that the pandemic is now in a very different phase from where it was in 2021 or 2022 or 2023.”
Though the isolation guidelines have been wiped away, the CDC still encourages people to play it safe for five days after they are feeling better. That includes masking around vulnerable people and opening windows to improve the flow of fresh air indoors.
The majority of viral spread happens when people are the sickest. “As the days go on, less virus spreads,” Cohen said.
People at higher risk for severe Covid complications, such as the elderly, people with weak immune systems and pregnant women, may need to take additional precautions.
Dr. Katie Passaretti, chief epidemiologist at Atrium Health in Charlotte, said it was a “move in the positive direction.”
“We are continuing to edge into what the world looks like after Covid, with Covid being one of many respiratory viruses that are certain that circulate,” she said.
The new guidance is for the general public only, and does not include isolation guidelines in hospital settings, which is generally 10 days.
On Wednesday, the agency said that adults 65 and older should get a booster shot of the Covid vaccine this spring. It’s anticipated that the nation will experience an uptick in the illness later this summer.
Winter and summer waves of Covid have emerged over the past four years, with cases peaking in January and August, respectively, according to the CDC .
Another, reformulated, shot is expected to be available and recommended this fall.
CDC’s main tips for reducing Covid spread:
- Get the Covid vaccine whenever it is available. Cohen said that 95% of people who were hospitalized with Covid this past winter had not received the latest vaccine.
- Cover coughs and sneezes, and wash hands frequently.
- Increase ventilation by opening windows, using air purifiers and gathering outside when possible.
Erika Edwards is a health and medical news writer and reporter for NBC News and "TODAY."
- Departments
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
Understanding the CDC’s Updated COVID Isolation Guidance
The updated recommendations align guidance for COVID infection with that for other common respiratory viruses.
Aliza Rosen
For the first time since 2021, the Centers for Disease Control and Prevention has updated its COVID isolation guidance.
Specifically, it has shifted the recommendation that someone who tests positive for COVID isolate for five days to a timeline based on the progression of the person’s symptoms. The update is part of a larger strategy to provide one set of recommendations for most common respiratory illnesses , including COVID, influenza, and respiratory syncytial virus (RSV).
In this Q&A, virologist Andy Pekosz , PhD, a professor in Molecular Microbiology and Immunology , explains the CDC’s new isolation guidance, the reasons for the update, and why the prevention and treatment strategies we’ve all become accustomed to still play an important part in reducing respiratory virus transmission.
What are the updated recommendations for someone who comes down with a respiratory infection?
The updated guidance from the CDC is to “stay home and away from others (including people you live with who are not sick) if you have respiratory virus symptoms that aren't better explained by another cause.” You can resume normal activities once your symptoms are improving and you’ve been fever-free—without the aid of fever-reducing medications—for at least 24 hours.
For the five days after you resume your normal activities, you should take extra precautions, like wearing a well-fitting mask and maintaining distance from others, gathering outdoors or in well-ventilated areas, cleaning hands and high-touch surfaces often, and testing when possible before gathering with others. If symptoms or fever return, you should start back at square one: staying home and away from others until you’ve been improving and fever-free for at least 24 hours.
What should you do if you’re at higher risk of severe illness?
If you’re at higher risk of severe illness—generally, this is older adults and young children, pregnant people, people with disabilities, and people with compromised immune systems—seek testing and contact your physician. If you test positive for COVID or flu, there are antiviral medications that can be taken within a few days of symptom onset and are extremely effective in reducing the likelihood that your symptoms become severe or that you need to be hospitalized.
How does this differ from previous guidance?
Before this, the CDC recommended that people who test positive for COVID should isolate away from others for five days and wear a well-fitting mask around others for the following five days. This was different from the general guidance for other common respiratory viruses, like flu and RSV.
Now there is no one-size-fits-all duration for how long to isolate; rather, you can resume regular activities—ideally still using other prevention strategies, like masking and distancing—based on when your symptoms have improved and your fever has gone away.
This marks a significant change in guidance for people who test positive for COVID. Why has the guidance changed?
The CDC has simplified its recommendations for how long to stay home and isolate after testing positive or experiencing symptoms to be consistent across COVID-19, influenza, and RSV infections. This way, anyone who develops symptoms can follow the same isolation guidance, irrespective of what respiratory virus they’re infected with.
It’s important to note, though, that this guidance on how long to isolate is just one part of a larger strategy for combating respiratory viruses that includes:
- Being up to date on recommended vaccines.
- Practicing good hygiene regarding hand-washing, sneezing, and coughing.
- Being aware of antiviral treatment options for COVID-19 and influenza.
- Taking steps to improve indoor air quality.
If the guidance is the same for all respiratory viruses, is it still important to test to know what someone is sick with?
Yes, testing is still needed in order to get a prescription for antivirals to treat COVID-19 or influenza. Those antivirals have been shown to reduce disease severity in several different groups, so if you are in a high risk group, be sure to test early and contact your physician so you can get the antiviral prescriptions as soon as possible.
Testing can also play an important role in preventing transmission, particularly if you were recently around someone who has since become sick, or if you plan to spend time with someone who is at higher risk of severe infection.
For COVID in particular, rapid home antigen tests are a great way to determine whether you’re still infectious and able to infect others. Symptom severity can be fairly subjective and a presence or lack of symptoms does not always align with infectiousness , so testing out of isolation for COVID is still good practice if you have access to tests.
Does this new guidance mean that all of these respiratory viruses pose the same risk?
No, COVID-19 is still causing more cases and more severe disease than influenza or RSV. A person’s risk for severe infection will also vary based on a number of factors, including age and health conditions .
The updated guidance acknowledges that we can simplify the recommendations for what to do after becoming infected with a respiratory virus, as part of the larger strategy to address spread.
The CDC also recently recommended that people over age 65 receive an additional dose of this year’s COVID vaccine . What drove that decision?
There are a few reasons behind this new recommendation for older adults . First, most severe COVID infections are occurring in individuals 65 years and older who have not been vaccinated recently. The CDC’s recommendation notes that more than half of COVID hospitalizations between October 2023 and December 2023 occurred in adults over 65.
Second, we know immunity after vaccination wanes over a few months, so an additional dose will provide renewed protection through the spring. New COVID variants like JN.1 that are circulating now have some mutations that improve their ability to evade vaccine-induced immunity, but the antibodies made through vaccination still recognize them. It’s not a perfect match, but a second dose of this year’s vaccine will provide protection against current variants to an age group at increased risk of severe illness, hospitalization, and death.
When should people over 65 get this additional dose of the current COVID vaccine?
The recommendation from the CDC is for people 65 and older who have already received one dose of the 2023-24 COVID vaccine to get a second shot at least four months after their most recent dose .
For people in that age group who haven’t had the 2023-24 vaccine, there’s no need to wait. They can get their shot now to be protected through the spring.
Will there be an updated COVID-19 vaccine for these newer variants?
We can likely expect to see a new COVID-19 vaccine available this fall, just like we see new, updated influenza vaccines each fall. This spring—typically around May—a decision will be made on which variants the updated vaccine will be designed around, and like we saw in 2023, the new vaccine will be available in the fall as we head into the typical respiratory virus season.
Aliza Rosen is a digital content strategist in the Office of External Affairs at the Johns Hopkins Bloomberg School of Public Health.
- More Americans Could Benefit from Paxlovid for COVID Infection
- What to Know About the Updated COVID-19 Vaccine for Fall/Winter 2023
Related Content

What to Know About COVID FLiRT Variants
Rotavirus the Leading Cause of Diarrheal Deaths Among Children Under 5, New Analysis Finds

Outbreak Preparedness for All

Peter Agre’s Third Act

What’s Happening With Dairy Cows and Bird Flu
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.

Routine Vaccines
It’s important to be up to date on recommended routine vaccines prior to travel, including Flu, RSV and COVID-19.

Find a Clinic
Advice for Travelers
Personalized Health Information Tool for Global Travel
Disease Directory
Frequently Asked Questions
CDC Yellow Book
Pre-travel Rapid Evaluation Portal for Patients
Clinician Resources
Research and Surveillance
- Medical Tourism
- Cholera Information for Health Care Professionals
- COVID-19 Travel Information
- Travel Industry Resources

Learn about CDC’s Traveler Genomic Surveillance Program that detects new COVID-19 variants entering the country.

Sign up to get travel notices, clinical updates, & healthy travel tips.
See the full list of Travel Health Notices , including:
Level 2 - Practice Enhanced Precautions
- New Chikungunya in Maldives May 28, 2024
- Global Polio May 23, 2024
- Diphtheria in Guinea April 23, 2024
Level 1 - Practice Usual Precautions
- Updated Global Measles May 28, 2024
- New Meningococcal Disease in Saudi Arabia - Vaccine Requirements for Travel During the Hajj and Umrah Pilgrimages May 20, 2024
- Dengue in Asia and the Pacific Islands May 16, 2024
There are no Warning , Alert, Watch, COVID-19 Very High, COVID-19 High, COVID-19 Moderate, COVID-19 Low, COVID-19 Unknown, Level 4, or Level 3 notices currently in effect.
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
What to Do If You Test Positive for COVID-19 While Traveling
A fter two years of pandemic living, Americans are collectively ready for a vacation. About 85% of people in the U.S. expect to travel this summer, according to data from the industry trade group U.S. Travel Association. Many others aren’t even waiting that long. Almost 2.3 million people passed through U.S. Transportation Security Administration checkpoints on April 10, only slightly fewer than on that date in 2019.
No matter how much we might like to, though, it’s not always possible to take a vacation from COVID-19. The virus is still circulating widely , including in popular tourist destinations like the U.K., Germany, France, and Italy. That means getting sick while traveling is a real possibility—and one that can turn into an expensive and stressful logistical headache.
What happens if you get COVID-19 while traveling internationally?
To enter the U.S., international travelers currently need either a negative COVID-19 test result obtained within one day of their flight or proof that they have recovered from COVID-19 in the last 90 days. (This policy applies to both U.S. citizens and non-citizens, but children younger than 2 are exempt.) Without one of those documents, you cannot board a U.S.-bound flight. If you test positive, you should isolate and delay travel for 10 days , according to the U.S. Centers for Disease Control and Prevention (CDC).
But where do you stay if you need to quarantine abroad? And who pays for extended accommodations and rescheduled flights?
Specifics vary from country to country, but the short answer is that travelers are often on the hook. Exceptions to the test-to-return policy may be granted on an “extremely limited” basis, such as in the event of an emergency medical evacuation or humanitarian crisis, the CDC says—but the average vacationer won’t have many options beyond paying to extend their stay.
“Have a plan in case you have to remain overseas longer than anticipated,” the U.S. Department of State writes on its website . “This includes being ready to cover additional lodging costs, flight ticket change fees, and any other additional expenses they may incur due to the unexpected extension.”
Some travel insurance covers extra expenses incurred because of a COVID-19 case, but policies may not cover all costs related to an extension, according to a spokesperson for the U.S. Travel Insurance Association. “Travelers concerned about this potential disruption in their travels should first look for a policy that includes sickness or quarantine as a covered reason, and then determine which benefits quarantine falls under and the limits of those benefits,” they wrote in a statement.
A spokesperson for the State Department said travelers who must isolate should contact their hotels and airlines to arrange accommodations and re-book travel, and, if necessary, seek assistance from their nearest U.S. embassy or consulate. The spokesperson added that U.S. citizens traveling abroad are subject to local quarantine rules, which may differ from those of the U.S. CDC.
Certain countries maintain “quarantine hotels” where travelers can quarantine upon arrival (if required by that country) or ride out their isolation periods. USA Today reports that some resorts even offer discounted rates to guests who have to extend their stays to isolate. It’s smart to check ahead of time, however, as these hotels aren’t available in all areas and their costs vary widely.
Aliya Waldman, who is 29 and lives in Missouri, stayed in a quarantine hotel after catching COVID-19 during a March trip with the Birthright program, which organizes visits to Israel for Jewish young adults. Waldman was required to stay in the hotel for a full week, even though she tested negative after five days in isolation. She believes the costs of her stay and new return flight were covered by Birthright, but says the experience has made her think twice about traveling abroad independently during the pandemic. “I won’t be able to afford getting stuck in another country,” she says.
It’s not clear how long international travelers will have to abide by the CDC’s testing requirement. Four trade groups—the U.S. Travel Association, Airlines for America, American Hotel and Lodging Association, and U.S. Chamber of Commerce—recently urged the White House’s coronavirus czar to suspend that policy, since many Americans have some immunity to the virus from vaccination and prior exposure , and are thus at lower risk than they were earlier in the pandemic. “While providing little health benefit, this requirement discourages travel by imposing an additional cost and the fear of being stranded overseas,” they wrote in a joint letter .
What happens if you get COVID-19 while traveling within the U.S.?
There is no negative test requirement for most domestic transportation, only a mask mandate that the CDC said will be in place through at least May 3 . But that doesn’t mean you should get on a plane, train, or bus if you’re sick. The CDC says not to travel if you have symptoms of COVID-19 or have tested positive and not yet completed an isolation period. Without a testing requirement in place, though, that guideline depends heavily on the honor system.
Nonetheless, travelers who test positive for COVID-19 within the U.S. should self-isolate where they are, if there’s no way to get home via private transportation. Finding a place to do so can be tricky, though. Some U.S. cities with hotel quarantine programs, including New York City and Philadelphia , are winding them down, and Airbnb says guests should not check into a listing if they have COVID-19. Competing rental platform Vrbo, however, told Condé Nast Traveler that its private properties can be “an ideal lodging option for guests who need to quarantine or self-isolate.”
More Must-Reads from TIME
- How Selena Gomez Is Revolutionizing the Celebrity Beauty Business
- TIME100 Most Influential Companies 2024
- Javier Milei’s Radical Plan to Transform Argentina
- How Private Donors Shape Birth-Control Choices
- The Deadly Digital Frontiers at the Border
- What's the Best Measure of Fitness?
- The 31 Most Anticipated Movies of Summer 2024
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Write to Jamie Ducharme at [email protected]
- COVID-19 travel advice
Considering travel during the pandemic? Take precautions to protect yourself from COVID-19.
A coronavirus disease 2019 (COVID-19) vaccine can prevent you from getting COVID-19 or from becoming seriously ill due to COVID-19 . But even if you're vaccinated, it's still a good idea to take precautions to protect yourself and others while traveling during the COVID-19 pandemic.
If you've had all recommended COVID-19 vaccine doses, including boosters, you're less likely to become seriously ill or spread COVID-19 . You can then travel more safely within the U.S. and internationally. But international travel can still increase your risk of getting new COVID-19 variants.
The Centers for Disease Control and Prevention (CDC) recommends that you should avoid travel until you've had all recommended COVID-19 vaccine and booster doses.
Before you travel
As you think about making travel plans, consider these questions:
- Have you been vaccinated against COVID-19 ? If you haven't, get vaccinated. If the vaccine requires two doses, wait two weeks after getting your second vaccine dose to travel. If the vaccine requires one dose, wait two weeks after getting the vaccine to travel. It takes time for your body to build protection after any vaccination.
- Have you had any booster doses? Having all recommended COVID-19 vaccine doses, including boosters, increases your protection from serious illness.
- Are you at increased risk for severe illness? Anyone can get COVID-19 . But older adults and people of any age with certain medical conditions are at increased risk for severe illness from COVID-19 .
- Do you live with someone who's at increased risk for severe illness? If you get infected while traveling, you can spread the COVID-19 virus to the people you live with when you return, even if you don't have symptoms.
- Does your home or destination have requirements or restrictions for travelers? Even if you've had all recommended vaccine doses, you must follow local, state and federal testing and travel rules.
Check local requirements, restrictions and situations
Some state, local and territorial governments have requirements, such as requiring people to wear masks, get tested, be vaccinated or stay isolated for a period of time after arrival. Before you go, check for requirements at your destination and anywhere you might stop along the way.
Keep in mind these can change often and quickly depending on local conditions. It's also important to understand that the COVID-19 situation, such as the level of spread and presence of variants, varies in each country. Check back for updates as your trip gets closer.
Travel and testing
For vaccinated people.
If you have been fully vaccinated, the CDC states that you don't need to get tested before or after your trip within the U.S. or stay home (quarantine) after you return.
If you're planning to travel internationally outside the U.S., the CDC states you don't need to get tested before your trip unless it's required at your destination. Before arriving to the U.S., you need a negative test within the last day before your arrival or a record of recovery from COVID-19 in the last three months.
After you arrive in the U.S., the CDC recommends getting tested with a viral test 3 to 5 days after your trip. If you're traveling to the U.S. and you aren't a citizen, you need to be fully vaccinated and have proof of vaccination.
You don't need to quarantine when you arrive in the U.S. But check for any symptoms. Stay at home if you develop symptoms.
For unvaccinated people
Testing before and after travel can lower the risk of spreading the virus that causes COVID-19 . If you haven't been vaccinated, the CDC recommends getting a viral test within three days before your trip. Delay travel if you're waiting for test results. Keep a copy of your results with you when you travel.
Repeat the test 3 to 5 days after your trip. Stay home for five days after travel.
If at any point you test positive for the virus that causes COVID-19 , stay home. Stay at home and away from others if you develop symptoms. Follow public health recommendations.
Stay safe when you travel
In the U.S., you must wear a face mask on planes, buses, trains and other forms of public transportation. The mask must fit snugly and cover both your mouth and nose.
Follow these steps to protect yourself and others when you travel:
- Get vaccinated.
- Keep distance between yourself and others (within about 6 feet, or 2 meters) when you're in indoor public spaces if you're not fully vaccinated. This is especially important if you have a higher risk of serious illness.
- Avoid contact with anyone who is sick or has symptoms.
- Avoid crowds and indoor places that have poor air flow (ventilation).
- Don't touch frequently touched surfaces, such as handrails, elevator buttons and kiosks. If you must touch these surfaces, use hand sanitizer or wash your hands afterward.
- Wear a face mask in indoor public spaces. The CDC recommends wearing the most protective mask possible that you'll wear regularly and that fits. If you are in an area with a high number of new COVID-19 cases, wear a mask in indoor public places and outdoors in crowded areas or when you're in close contact with people who aren't vaccinated.
- Avoid touching your eyes, nose and mouth.
- Cover coughs and sneezes.
- Wash your hands often with soap and water for at least 20 seconds.
- If soap and water aren't available, use a hand sanitizer that contains at least 60% alcohol. Cover all surfaces of your hands and rub your hands together until they feel dry.
- Don't eat or drink on public transportation. That way you can keep your mask on the whole time.
Because of the high air flow and air filter efficiency on airplanes, most viruses such as the COVID-19 virus don't spread easily on flights. Wearing masks on planes has likely helped lower the risk of getting the COVID-19 virus on flights too.
However, air travel involves spending time in security lines and airport terminals, which can bring you in close contact with other people. Getting vaccinated and wearing a mask when traveling can help protect you from COVID-19 while traveling.
The Transportation Security Administration (TSA) has increased cleaning and disinfecting of surfaces and equipment, including bins, at screening checkpoints. TSA has also made changes to the screening process:
- Travelers must wear masks during screening. However, TSA employees may ask travelers to adjust masks for identification purposes.
- Travelers should keep a distance of 6 feet apart from other travelers when possible.
- Instead of handing boarding passes to TSA officers, travelers should place passes (paper or electronic) directly on the scanner and then hold them up for inspection.
- Each traveler may have one container of hand sanitizer up to 12 ounces (about 350 milliliters) in a carry-on bag. These containers will need to be taken out for screening.
- Personal items such as keys, wallets and phones should be placed in carry-on bags instead of bins. This reduces the handling of these items during screening.
- Food items should be carried in a plastic bag and placed in a bin for screening. Separating food from carry-on bags lessens the likelihood that screeners will need to open bags for inspection.
Be sure to wash your hands with soap and water for at least 20 seconds directly before and after going through screening.
Public transportation
If you travel by bus or train and you aren't vaccinated, be aware that sitting or standing within 6 feet (2 meters) of others for a long period can put you at higher risk of getting or spreading COVID-19 . Follow the precautions described above for protecting yourself during travel.
Even if you fly, you may need transportation once you arrive at your destination. You can search car rental options and their cleaning policies on the internet. If you plan to stay at a hotel, check into shuttle service availability.
If you'll be using public transportation and you aren't vaccinated, continue physical distancing and wearing a mask after reaching your destination.
Hotels and other lodging
The hotel industry knows that travelers are concerned about COVID-19 and safety. Check any major hotel's website for information about how it's protecting guests and staff. Some best practices include:
- Enhanced cleaning procedures
- Physical distancing recommendations indoors for people who aren't vaccinated
- Mask-wearing and regular hand-washing by staff
- Mask-wearing indoors for guests in public places in areas that have high cases of COVID-19
- Vaccine recommendations for staff
- Isolation and testing guidelines for staff who've been exposed to COVID-19
- Contactless payment
- Set of rules in case a guest becomes ill, such as closing the room for cleaning and disinfecting
- Indoor air quality measures, such as regular system and air filter maintenance, and suggestions to add air cleaners that can filter viruses and bacteria from the air
Vacation rentals, too, are enhancing their cleaning procedures. They're committed to following public health guidelines, such as using masks and gloves when cleaning, and building in a waiting period between guests.
Make a packing list
When it's time to pack for your trip, grab any medications you may need on your trip and these essential safe-travel supplies:
- Alcohol-based hand sanitizer (at least 60% alcohol)
- Disinfectant wipes (at least 70% alcohol)
- Thermometer
Considerations for people at increased risk
Anyone can get very ill from the virus that causes COVID-19 . But older adults and people of any age with certain medical conditions are at increased risk for severe illness. This may include people with cancer, serious heart problems and a weakened immune system. Getting the recommended COVID-19 vaccine and booster doses can help lower your risk of being severely ill from COVID-19 .
Travel increases your chance of getting and spreading COVID-19 . If you're unvaccinated, staying home is the best way to protect yourself and others from COVID-19 . If you must travel and aren't vaccinated, talk with your health care provider and ask about any additional precautions you may need to take.
Remember safety first
Even the most detailed and organized plans may need to be set aside when someone gets ill. Stay home if you or any of your travel companions:
- Have signs or symptoms, are sick or think you have COVID-19
- Are waiting for results of a COVID-19 test
- Have been diagnosed with COVID-19
- Have had close contact with someone with COVID-19 in the past five days and you're not up to date with your COVID-19 vaccines
If you've had close contact with someone with COVID-19 , get tested after at least five days. Wait to travel until you have a negative test. Wear a mask if you travel up to 10 days after you've had close contact with someone with COVID-19 .
- How to protect yourself and others. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html. Accessed Feb. 4, 2022.
- Domestic travel during COVID-19. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/travel-during-covid19.html. Accessed Feb. 4, 2022.
- Requirement for face masks on public transportation conveyances and at transportation hubs. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/face-masks-public-transportation.html. Accessed Feb. 4, 2022.
- International travel. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/international-travel/index.html. Accessed Feb. 4, 2022.
- U.S citizens, U.S. nationals, U.S. lawful permanent residents, and immigrants: Travel to and from the United States. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/international-travel-during-covid19.html. Accessed Feb. 4, 2022.
- Non-US. citizen, non-U.S. immigrants: Air travel to the United States. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/noncitizens-US-air-travel.html. Accessed Feb. 4, 2022.
- People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed Feb. 4, 2022.
- Stay up to date with your vaccines. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/stay-up-to-date.html. Accessed Feb. 4, 2022.
- Pack smart. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/page/pack-smart. Accessed Feb. 4, 2022.
- Travel: Frequently asked questions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/faqs.html. Accessed Feb. 7, 2022.
- Coronavirus (COVID-19) information. Transportation Security Administration. https://www.tsa.gov/coronavirus. Accessed Feb. 7, 2022.
- WHO advice for international traffic in relation to the SARS-CoV-2 Omicron variant (B.1.1.529). World Health Organization. https://www.who.int/news-room/articles-detail/who-advice-for-international-traffic-in-relation-to-the-sars-cov-2-omicron-variant. Accessed Feb. 7, 2022.
- VRHP/VRMA Cleaning guidelines for COVID-19. Vacation Rental Management Association. https://www.vrma.org/page/vrhp/vrma-cleaning-guidelines-for-covid-19. Accessed Feb. 7, 2022.
- Safe stay. American Hotel & Lodging Association. https://www.ahla.com/safestay. Accessed Feb. 7, 2022.
- Khatib AN, et al. COVID-19 transmission and the safety of air travel during the pandemic: A scoping review. Current Opinion in Infectious Diseases. 2021; doi:10.1097/QCO.0000000000000771.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- A Book: Future Care
- Antibiotics: Are you misusing them?
- COVID-19 and vitamin D
- Convalescent plasma therapy
- Coronavirus disease 2019 (COVID-19)
- COVID-19: How can I protect myself?
- Herd immunity and coronavirus
- COVID-19 and pets
- COVID-19 and your mental health
- COVID-19 antibody testing
- COVID-19, cold, allergies and the flu
- Long-term effects of COVID-19
- COVID-19 tests
- COVID-19 drugs: Are there any that work?
- COVID-19 in babies and children
- Coronavirus infection by race
- COVID-19 vaccine: Should I reschedule my mammogram?
- COVID-19 vaccines for kids: What you need to know
- COVID-19 vaccines
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- COVID-19: Who's at higher risk of serious symptoms?
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Extracorporeal membrane oxygenation (ECMO)
- Fever: First aid
- Fever treatment: Quick guide to treating a fever
- Fight coronavirus (COVID-19) transmission at home
- Honey: An effective cough remedy?
- How do COVID-19 antibody tests differ from diagnostic tests?
- How to measure your respiratory rate
- How to take your pulse
- How to take your temperature
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Loss of smell
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Multisystem inflammatory syndrome in children (MIS-C)
- Nausea and vomiting
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Shortness of breath
- Thermometers: Understand the options
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
- Vaccine guidance from Mayo Clinic
- Watery eyes
U.S. travel resources
- Check CDC recommendations for travel within the U.S.
- Review testing requirements for travel to the U.S.
- Look up restrictions at your destination .
- Review airport security measures .
Related resources
Your gift holds great power – donate today.
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
Shots - Health News
A guide to covid tests: when to test, what kind to use and what your results mean.
Melody Schreiber

Jonathan Franklin

COVID-19 rapid tests are distributed in Brooklyn in late December. Self-tests are in short supply in many parts of the country. Bryan R. Smith/AFP via Getty Images hide caption
COVID-19 rapid tests are distributed in Brooklyn in late December. Self-tests are in short supply in many parts of the country.
Each week, we answer frequently asked questions about life during the coronavirus crisis. If you have a question you'd like us to consider for a future post, email us at [email protected] with the subject line: "Weekly Coronavirus Questions." See an archive of our FAQs here .
In an ideal world, the U.S. would be awash in COVID tests. Anyone exposed to COVID-19 could self-test and/or go to a lab or clinic for a test if necessary.
But right now, self-tests are in short supply in many parts of the country.
Americans can now order free at-home, rapid COVID-19 tests from the federal government, which the Postal Service says will be shipped "in late January."

The Postal Service is now taking orders for COVID-19 test kits

With omicron, you need a mask that means business
Test manufacturers are also ramping up production, so the hope is that at some point, although no one can say exactly when, you won't be seeing those "no tests available" signs at the local pharmacy or have to wait a week or more for tests ordered online.
What's more, the Centers for Disease Control and Prevention has changed its testing guidelines in the wake of the omicron surge in the U.S. — and public health researchers are critical of some of the recommendations.
The end result is a lot of confusion about testing and a lot of frequently asked questions. Here are some answers to queries you might have about COVID-19 tests.
What types of COVID tests are there?
There's the rapid, do-it-yourself home test, which involves swabbing your nose and takes about 15 minutes to display a result on a test strip provided in the kit. These typically cost about $20 to $24 for a package of two tests. Most commonly used at-home tests are antigen tests — antigens are basically the proteins from the virus that the rapid tests can identify.
Then there's the PCR test performed in a lab or clinic. PCR stands for polymerase chain reaction, which is a technique for amplifying trace amounts of virus DNA. Depending on how busy your local technicians are, you may have PCR results within a day or it may take several days. A PCR test usually costs about $150 without insurance.

COVID rapid tests can be hard to come by. This was the message in a pharmacy in Washington, D.C. Selena Simmons-Duffin/NPR hide caption
COVID rapid tests can be hard to come by. This was the message in a pharmacy in Washington, D.C.
Are there any other types of tests?
There's a third type of test: a blood test that looks for antibodies after you've been sick, and some samples can even be taken from a finger prick at home and sent to a lab. But they are not used to diagnose COVID-19.
Does health insurance cover testing?
Most insurance policies cover PCR and rapid tests administered by health providers. Since Jan. 15, private insurance companies are reimbursing members for over-the-counter COVID-19 diagnostic tests that have been authorized, cleared or approved by the Food and Drug Administration.
How many tests can I get under this new policy?
Up to eight per month.
Insurance companies and health plans will be required to cover eight free over-the-counter at-home tests per covered individual per month, according to the White House. For instance, a family of four all on the same plan would be able to get up to 32 of these tests covered by their health plan each month.
What if I have Medicare? Can I get reimbursed for testing?
At this time, those who are on Medicare will not be able to get their at-home COVID-19 tests reimbursed through the program, according to the Centers for Medicaid & Medicare Services .
Currently, among federal health care programs, only Medicaid and the Children's Health Insurance Program plans are required to fully cover the cost of at-home tests.
What's the difference between antigen and PCR tests?
The PCR test is much more sensitive in identifying an infection because it can amplify traces of the virus — in other words, even if you have a small amount of virus, it can detect it. So it can tell whether you're infected even a day or so after you develop what appear to be COVID-19 symptoms or a few days after exposure to someone with COVID-19.

The Coronavirus Crisis
A pediatrician's advice to parents of kids under 5 on omicron, travel and day care.
The antigen tests don't magnify the amount of virus in the sample you take, so you need a pretty high viral load to test positive. As Susan Butler-Wu , associate professor of clinical pathology at the Keck School of Medicine of University of Southern California, puts it: "It's a test for [determining whether you have] a lot of virus."
So you might test negative on a home test even if you are infected — at the beginning or the end of your illness, for example, when you don't have a lot of virus.
So which test should I go for?
The more urgent question, says Butler-Wu, is: "Which test can you get ?"
If you have symptoms and likely have been exposed to the virus by traveling or socializing, a positive antigen test is probably enough evidence that you have the virus, says Dr. Abraar Karan , an infectious disease physician at Stanford University.
As for PCR tests, availability depends on the demand in your community. Some testing facilities are slammed, with few appointments available and hours-long waits even if you can snag an appointment. And it can take several days to get results from a PCR test.

Goats and Soda
Omicron is spreading at lightning speed. scientists are trying to figure out why, what should i do while awaiting pcr test results.
While you're waiting for test results, if you have symptoms you should act as though the test is positive and quarantine.
If you've been exposed but don't have symptoms, the CDC says you can go out while wearing a well-fitting, protective mask if you're vaccinated and boosted.
Those who aren't vaccinated should quarantine after a known exposure until test results are in.
(See this story for guidelines about quarantining or self-isolating after an exposure.)
When should I test — and how many times?

It's time to recalculate your COVID 'risk budget.' Here's how
The answer depends on whether you can get tests — and what you're using them for. Tests can be used to tell you if you have COVID-19 – for instance, if you have symptoms or you've been around someone who tested positive. And they can also be used as an added precaution before socializing (which we'll discuss a couple of questions down).
If you've been exposed to someone with COVID-19, you should self-test. But not right away.
"If you've been exposed, wait a few days because testing right away could be negative," Karan says. After you wait, "then we'll be able to detect virus."
The CDC recommends testing either when symptoms develop or, if you aren't showing symptoms, five to seven days after exposure. That would give enough time for the body to develop a viral load that can be detected by a test.
With the omicron variant, there have been reports that rapid tests are negative during the first day or two of symptoms. So even if you're showing symptoms, you might want to wait a day or two to take the first test, especially if you have a limited supply of tests.

A home tester checks out the result on a test strip. Jennifer Swanson/NPR hide caption
A home tester checks out the result on a test strip.
How many home tests should I take?
At least two.
Why test twice? Home tests are most accurate when you use them serially — at least two over the course of a few days. And if you have a limited supply of home tests, you will want to aim for the time when you are most likely to get an accurate result — say, on Day 5 and Day 7 after exposure.

Tracking the coronavirus around the U.S.: See how your state is doing
"These tests absolutely have to be used serially, to be perfectly honest. They don't have the sensitivity to be used one-and-done if they're negative," Butler-Wu says. "By repeating it, you're allowing the virus to potentially grow more to the point, essentially, where now you can detect it."
"If that test is negative, all that's telling you is: At this point in time, you don't have a ton of virus in you," Karan says.
Should I get tested before seeing people?
"If you're going to visit Grandma or something, yeah, I would probably rapid-test before that," Karan says. "Or if I'm going somewhere where there's going be a lot of people. If I'm contagious that day [and don't know it], I could infect tons of people."
A positive test result will tell you to cancel your plans and stay home and isolate.
But negative results don't mean it's time to rip the mask off in social settings. Rapid tests could be negative before a party and positive during it, just a few hours later — even if you're vaccinated and boosted.
"To say that the negative test means being indoors unmasked — I think that needs to get rethought, pronto," Butler-Wu says.

Coronavirus world map: We've now passed the 200 million mark for infections
"Omicron has changed the game completely," she says. "We know from Christmas soirees that occurred in European places that those exact scenarios happened: vaccinated people, negative tests and there was still spread."
If I test negative — how accurate are negative tests?
There can be false negatives, especially soon after exposure when not much virus is present in your body, or if the virus is replicating somewhere other than where you were swabbed — for instance, in your throat instead of your nose.
That's why you should test at least twice.
According to a pre-omicron study , the Abbott BinaxNOW antigen test was 92.6% accurate at detecting the virus in symptomatic people and 78.6% accurate in asymptomatic people, compared to PCR results in cases where people had viable virus.
It is also possible to have a false negative from a PCR test.
"Any test is a snapshot of what's happening in the part of your body that was sampled at that moment. That's all it tells you," Butler-Wu says. "So, yes, PCR is more sensitive in that it can detect lower amounts of the virus. But if you're in the very early stages of incubating an infection and haven't reached what we call the 'limit of detection,' that too, can be negative."

Do you need to wear a mask indoors where you live? Check this map
What happens if i test positive.
When you test positive, you should isolate yourself for a minimum of five days and wear a mask for five days after that, according to the CDC. If you have rapid tests, you can use them after five days to see if you're still positive, which would mean you need to continue isolating.
If you were tested at a clinic, they report the results to the local public health department for you. If you test positive on a home test, you should notify the health department so it can keep track of how many cases your community has.

Are there ever false positives?
False positives are rare on PCR tests and usually happen because of contaminated samples, research has found .
A false positive on an antigen test is possible but fairly unlikely if the test is taken correctly, says Butler-Wu, especially if you develop symptoms and you know you've been exposed to someone with COVID-19. And a lot of people are being exposed at this current time of great spread to the omicron and delta variants.
If "there's a bunch of COVID and I'm symptomatic, it's probably a true positive," Butler-Wu says.
If you think you have a false positive from a home test, you can get a confirmatory PCR test if you can find one.
"If your PCR is negative, then it's possible that your rapid was a false positive," Karan says. "If you're able to do that, great."
When else are PCR tests recommended?
If you are at risk for severe illness, you should get a test in case you need medication for COVID-19. And some workplaces and schools require a negative PCR test to return after travel or a non-COVID illness.
Do the tests detect omicron?
Rapid tests may not be as accurate for omicron, the U.S. Food and Drug Administration said in late December — but they haven't released data yet on why they are less accurate and to what degree.
The FDA has also warned that three types of PCR tests may not detect omicron.
Because of these issues, if you're testing at home after symptoms or an exposure to someone with COVID-19, the use of two tests spaced a few days apart is critical.
Can I use a rapid test to get out of isolation or quarantine early?
No. You should complete at least five days of isolation after you test positive.
According to the CDC, you may end isolation five days after testing positive, as long as your symptoms are "resolving," including no fever for 24 hours, and you wear a mask "at all times when around others" for five more days.

Coronavirus FAQ: Remind me, what's the difference between isolation and quarantine?
The new guidance prompted criticism from public health experts. "I personally think a five-day lifting of isolation regardless of vaccination status, regardless of testing, regardless of anything — I am very concerned about it," Butler-Wu says. "I'm just looking at how often people who have COVID still shed infectious virus at five days, and it's quite a chunk."
On Tuesday, the CDC changed those recommendations to include taking a test on Day 5, if possible, but it stopped short of requiring a test.
But if you do test at that point and test positive, continue isolating until you test negative.
"If you have COVID, and your antigen [test] is still positive at five days, you're almost certainly still infectious," Butler-Wu says.
And viral load isn't the only factor for transmitting the virus. It also has to do with the situation you're in and human behavior, like how much you are talking or singing and whether you're masked, as well as environmental factors, like ventilation.
And what about taking a PCR test to end isolation?
PCR results can be positive for up to 12 weeks because they don't differentiate between viable and unviable viral particles, which means they may detect unviable virus after an infection has ended. So, a PCR test likely won't tell you when to end isolation.
Melody Schreiber (@m_scribe) is a journalist and the editor of What We Didn't Expect: Personal Stories About Premature Birth.
- antigen tests
- COVID tests
- COVID self tests

Explaining the New CDC Guidance on What To Do if You Have COVID-19
By Kate Yandell
Posted on March 15, 2024
Q: Is one day isolation sufficient to stop forward transmission of COVID-19?
A: People with COVID-19 could potentially transmit it to others well beyond a day after developing symptoms or testing positive. New guidance from the CDC advises people to isolate until they have been fever-free and with symptoms improving for at least 24 hours, and then take precautions for five days, which covers the period when “most people are still infectious.”
FULL ANSWER
The Centers for Disease Control and Prevention on March 1 updated its guidance on preventing the spread of respiratory viruses, consolidating advice on a range of common respiratory illnesses including COVID-19, flu and respiratory syncytial virus, or RSV.
Since December 2021 , the agency had recommended individuals isolate for at least five days after developing symptoms of COVID-19, or after a positive test if asymptomatic. After five days, the agency recommended various symptom-based criteria for leaving isolation combined with additional continued precautions, such as masking.

The new guidance drops the standard minimum of five days of isolation in favor of a symptom-based approach. The agency advises people to stay home and away from others when they are sick with a respiratory virus. People can cease isolation if, over a period of 24 hours, their overall symptoms have been improving and they have been fever-free without using fever-reducing medications.
Many people have had questions about what the new guidance means for people who have COVID-19. Some, like our reader, have referred to the idea that the guidance means only one day of isolation is needed. “do you agree with Biden that one day isolation for covid is fine and dandy??” asked one person on X, formerly known as Twitter.
But that’s not what Biden or the CDC is recommending.
“It’s not saying isolate for 24 hours,” epidemiologist Ronit Dalmat , a research scientist at the University of Washington, told us, referring to the CDC guidance. “It’s saying if you have a fever, absolutely stay home” until it has been gone for 24 hours, and also stay home until other symptoms are improving.
Nor does the CDC say people are guaranteed not to spread COVID-19 or other respiratory illnesses after their symptoms have improved. “Keep in mind that you may still be able to spread the virus that made you sick, even if you are feeling better,” the guidance says. “You are likely to be less contagious at this time, depending on factors like how long you were sick or how sick you were.”
The guidance recommends continuing to take precautions for five days after resuming normal activities. These include physical distancing, testing, improving air quality, using good hygiene and wearing a well-fitting mask, such as an N95 or KN95.
“The total number of days of precautions when sick, that is, a period of staying home and away from others plus 5 days of additional actions, covers the period during which most people are still infectious,” the CDC wrote in an FAQ.
“That whole period could be quite a while,” Dalmat said. “That could be 10 days for some people.”
The CDC said in background materials accompanying the new guidance that it looked at data from countries and states that had adopted similar policies for COVID-19 isolation and had not seen “clear increases in community transmission or hospitalization rates.”
“The updated guidance on steps to prevent spread when you are sick particularly reflects the key reality that many people with respiratory virus symptoms do not know the specific virus they are infected with,” the CDC said. The agency noted that its survey data indicated less than half of people with cold or cough symptoms would take an at-home COVID-19 test.
Some on social media have misinterpreted the guidance as an admission that it was always reasonable to liken COVID-19 to the flu, as was done early in the pandemic despite the marked difference in the diseases’ severity.
But the new CDC guidance acknowledges the continued seriousness of COVID-19 while also detailing the ways in which treatments, vaccines and population immunity have improved outcomes for people with the disease.
“COVID-19 remains a greater cause of severe illness and death than other respiratory viruses, but the differences between these rates are much smaller than they were earlier in the pandemic,” the CDC said . The agency explained that the risks are reduced due to the availability of COVID-19 treatments and population immunity to the virus, both from vaccination and prior infection. The agency also said that long COVID remains a risk, although the prevalence appears to be falling.
The Science on COVID-19 Transmission
Whether someone transmits COVID-19 depends on multiple factors . These include a person’s infectious viral load, but also the susceptibility of the people the infected person encounters and the precautions taken.
There’s no one-size-fits-all answer to how long a particular individual will shed infectious virus and how much they will shed. “Everybody has a slightly different ability to control the amount of virus in their system, which is a part of what makes the virus shed,” Dalmat said. Variation in how people’s bodies fight a virus affects “how much virus you are putting in the world that is infectious.”
There’s evidence that a relatively small number of people who shed particularly high levels of the virus over the course of their infections have been responsible for a disproportionate number of COVID-19 cases, and many people with COVID-19 do not infect others.
However, according to the CDC, the data on the typical overall length of shedding has not significantly changed, even as new variants of SARS-CoV-2 — the virus that causes COVID-19 — have arisen. “Even as the SARS-CoV-2 virus has continued to evolve, the duration of shedding infectious virus has remained relatively consistent, with most individuals no longer infectious after 8-10 days,” the agency said .
The CDC accompanied this statement with a figure showing data collected by the Respiratory Virus Transmission Network from five U.S. sites between November 2022 and May 2023 (see below). One line on the graph (light blue) shows how often researchers were able to isolate and grow — or culture — virus from people with COVID-19.
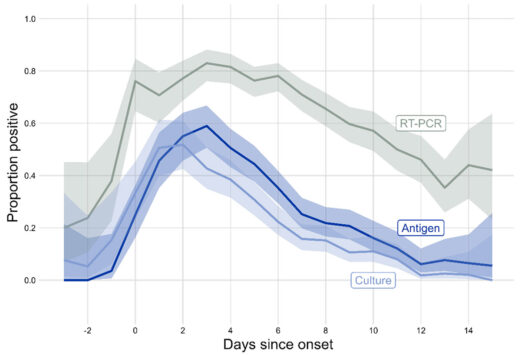
Trying to culture the virus that causes COVID-19 from a respiratory sample — a laborious process used in research — indicates whether someone is carrying infectious virus. The figure shows that the proportion of people with culturable virus began to increase two days before symptoms begin, or before a positive test for those who were asymptomatic, peaking around one to two days after symptom onset. After that, the rate began falling, with around one-third of people having culturable virus at day five. By day 10, the percentage had dropped to around 10%.
A different study , published in 2023 in the International Journal of Infectious Diseases, combined data from multiple studies done in people diagnosed with COVID-19 in 2021 and 2022. The average duration of shedding of culturable virus was just over five days from symptom onset or first positive PCR test, whichever came first.
Another metric for assessing infectiousness in people with COVID-19 is viral load, often measured as the amount of viral materials, such as RNA or proteins, found in a respiratory sample. A 2023 study published in Clinical Infectious Diseases found that median viral load for people diagnosed with COVID-19 peaked around three or four days after symptoms started. The study assessed people seeking testing for respiratory infections between April 2022 and April 2023.
Someone who is shedding infectious virus may or may not transmit it to others. One factor is that the average person is less susceptible to infection today than they were early in the pandemic, Dalmat said.
“Even if the person is producing the exact same amount of virus today as they could have three years ago, the people on the other end on average are less likely to get infected,” Dalmat said, explaining that today more than 98% of the population has had some exposure to COVID-19 itself, COVID-19 vaccines or both.
When people do get infected, the cases tend to be less severe. “Among the people who get infected with COVID these days, on average it is much rarer that it turns into a very serious illness,” Dalmat said, while also acknowledging that a lot of individuals “are still very vulnerable.” People at elevated risk for severe disease include those who are elderly or immune compromised.
While the CDC guidance harmonizes suggested precautions for COVID-19 and other common respiratory viruses, there are differences in the details of how COVID-19 and other respiratory viruses are spread.
The new guidance is meant to be a general rule of thumb but does not apply to health care settings or cases where there is an outbreak of a disease that requires special instructions, the CDC said. The CDC also said the agency is working on specific guidance for schools, which should be available prior to the 2024/2025 school year.
Masks, Tests and Other Precautions
Isolating from other people when sick is a key way to reduce one’s risk of spreading COVID-19. But the CDC guidance lists additional ways to reduce the chances of spreading a respiratory illness.
Masks can help prevent the wearer from spreading a respiratory virus. They can also protect others from inhaling a virus, particularly well-fitting masks such as N95 or KN95 respirators, the guidance says. Individuals can take measures to improve their hygiene and the air quality in their surroundings and maintain physical distance from others, such as by avoiding crowded spaces.
The CDC still recommends testing to help high-risk people who are sick determine whether to seek treatment for a specific virus. For instance, someone with COVID-19 may benefit from receiving Paxlovid within five days of when their symptoms start. The guidance also lists tests as a tool that can help people decide when they need to take precautions to avoid spreading disease.

At-home rapid antigen tests can be helpful for people who are recovering from COVID-19 and want to see if they still have infectious virus, Dalmat said. In their research, she and her colleagues found that among people who tested positive for COVID-19 on a rapid antigen test, subsequent negative antigen test results were “very, very highly correlated to whether you had infectious virus or not,” she said. That means people with COVID-19 who start to test negative on rapid antigen tests as they get better likely are no longer at risk of infecting others.
However, the CDC cautions that rapid antigen tests early in the course of a person’s infection often miss COVID-19. People who are sick should be taking precautions regardless of test results, Dalmat said. “They shouldn’t test and have a negative test be the end of it,” she said.
The authors of the Clinical Infectious Diseases study , which measured viral loads over the course of infection, wrote that “our data in combination with others’ suggest that symptomatic individuals testing positive for SARS-CoV-2 by PCR currently may not reliably test positive on a rapid antigen test until the third, fourth, or even fifth day of symptoms.”
The CDC guidance says people can end isolation when they have been fever-free and their symptoms have been improving for at least 24 hours. Dalmat cautioned that the definition of improving symptoms is somewhat ambiguous.
“Symptoms improving can mean different things to different people,” Dalmat said, adding that people should make sure their symptoms are truly getting better. “If your symptoms are not really improving – not kind of plateauing but really improving — you should continue to stay home and continue to take whatever measures you are taking in your household.”
Editor’s note: SciCheck’s articles providing accurate health information and correcting health misinformation are made possible by a grant from the Robert Wood Johnson Foundation. The foundation has no control over FactCheck.org’s editorial decisions, and the views expressed in our articles do not necessarily reflect the views of the foundation.
Branswell, Helen. “ CDC Eases Isolation Guidance for Covid and Other Respiratory Illnesses .” STAT. 1 Mar 2024.
“ Preventing Spread of Respiratory Viruses When You’re Sick .” CDC website. Updated 1 Mar 2024.
“ CDC’s Updated Respiratory Virus Guidance: What to Do When You Are Sick .” CDC website. 1 Mar 2024.
“ CDC Updates and Shortens Recommended Isolation and Quarantine Period for General Population .” CDC website. 27 Dec 2021.
“ Isolation and Precautions for People with COVID-19 .” CDC website. Updated 11 Mar 2023.
Cali Dreaming NaphiSoc (@NaphiSoc). “ Prof Hotez: do you agree with Biden that one day isolation for covid is fine and dandy?? ” X. 2 Mar 2024.
Dalmat, Ronit. Interview with FactCheck.org.
“ Respiratory Virus Guidance Update FAQs .” CDC website. Updated 1 Mar 2024.
“ Background for CDC’s Updated Respiratory Virus Guidance .” CDC website. Updated 1 Mar 2024.
Matt Kim 🇰🇷🇺🇸 (@mattattack009). “ Zero Accountability .” Instagram. 4 Mar 2024.
DiedSuddenly (@DiedSuddenly_). “ Turns out everything they told you about Covid was a lie. Of course they knew this 3 years ago, and they’ll show zero remorse for what they have done .” X. 2 Mar 2024.
Citizen Free Press (@CitizenFreePres). “ … and then one day, four years later on a Friday afternoon when no one was looking, the CDC admitted that the great conspiracy theory about Covid was true .” X. 1 Mar 2024.
Rieder, Rem. “ Trump’s Deceptive Comparison of the Coronavirus to the Flu .” FactCheck.org. 9 Sep 2020.
“ How is COVID-19 transmitted? ” FactCheck.org. Updated 11 Feb 2022.
Puhach, Olha et al. “ SARS-CoV-2 Viral Load and Shedding Kinetics .” Nature Reviews Microbiology. 2 Dec 2022.
Wu, Yu et al. “ Duration of Viable Virus Shedding and Polymerase Chain Reaction Positivity of the SARS-CoV-2 Omicron Variant in the Upper Respiratory Tract: A Systematic Review and Meta-Analysis .” International Journal of Infectious Diseases. 18 Feb 2023.
Frediani, Jennifer K. et al. “ The New Normal: Delayed Peak SARS-CoV-2 Viral Loads Relative to Symptom Onset and Implications for COVID-19 Testing Programs .” Clinical Infectious Diseases. 28 Sep 2023.
Cevik, Muge and Kalil, Andre C. “ Omicron Variant: Assessing the Duration of Viral Shedding and Its Implications .” Clinical Microbiology and Infection. 25 Nov 2022.
“ Risk Factors for Severe Illness from Respiratory Viruses .” CDC website. Updated 1 Mar 2024.
Wu, Katherine J. “ Why Are We Still Flu-Ifying COVID? ” The Atlantic. 28 Feb 2024.
“ Masks and Respiratory Viruses Prevention .” CDC website. Updated 1 Mar 2024.
“ Hygiene and Respiratory Viruses Prevention .” CDC website. Updated 1 Mar 2024.
“ Taking Steps for Cleaner Air for Respiratory Virus Prevention .” CDC website. Updated 1 Mar 2024.
“ About Physical Distancing and Respiratory Viruses .” CDC website. Updated 1 Mar 2024.
“ Preventing Respiratory Viruses .” CDC website. Updated 1 Mar 2024.
“ COVID-19 Treatments and Medications .” CDC website. Updated 15 Mar 2024.
“ Testing and Respiratory Viruses .” CDC website. Updated 1 Mar 2024.
Drain, Paul K. et al. “ Duration of Viral Infectiousness and Correlation with Symptoms and Diagnostic Testing in Non-Hospitalized Adults during Acute SARS-CoV-2 Infection: A Longitudinal Cohort Study .” Journal of Clinical Virology. 3 Mar 2023.
Take control of your money! Save, budget and navigate your finances easier with AARP Money Map.
AARP daily Crossword Puzzle
Hotels with AARP discounts
Life Insurance
AARP Dental Insurance Plans
AARP MEMBERSHIP — Limited Time Offer-Memorial Day Sale
Join AARP for just $9 per year with a 5-year membership. Join now and get a FREE Gift! Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
- right_container
Work & Jobs
Social Security
AARP en Español
- Membership & Benefits
AARP Rewards
- AARP Rewards %{points}%
Conditions & Treatments
Drugs & Supplements
Health Care & Coverage
Health Benefits

Staying Fit
Your Personalized Guide to Fitness

Get Happier
Creating Social Connections

Brain Health Resources
Tools and Explainers on Brain Health

Your Health
8 Major Health Risks for People 50+
Scams & Fraud
Personal Finance
Money Benefits

View and Report Scams in Your Area

AARP Foundation Tax-Aide
Free Tax Preparation Assistance

AARP Money Map
Get Your Finances Back on Track

How to Protect What You Collect
Small Business
Age Discrimination

Flexible Work
Freelance Jobs You Can Do From Home

AARP Skills Builder
Online Courses to Boost Your Career

31 Great Ways to Boost Your Career

ON-DEMAND WEBINARS
Tips to Enhance Your Job Search

Get More out of Your Benefits

When to Start Taking Social Security

10 Top Social Security FAQs

Social Security Benefits Calculator

Medicare Made Easy
Original vs. Medicare Advantage

Enrollment Guide
Step-by-Step Tool for First-Timers

Prescription Drugs
9 Biggest Changes Under New Rx Law

Medicare FAQs
Quick Answers to Your Top Questions
Care at Home
Financial & Legal
Life Balance

LONG-TERM CARE
Understanding Basics of LTC Insurance

State Guides
Assistance and Services in Your Area

Prepare to Care Guides
How to Develop a Caregiving Plan

End of Life
How to Cope With Grief, Loss
Recently Played
Word & Trivia
Atari® & Retro
Members Only
Staying Sharp
Mobile Apps
More About Games

Right Again! Trivia

Right Again! Trivia – Sports

Atari® Video Games

Throwback Thursday Crossword
Travel Tips
Vacation Ideas
Destinations
Travel Benefits

Outdoor Vacation Ideas
Camping Vacations

Plan Ahead for Summer Travel

AARP National Park Guide
Discover Canyonlands National Park

History & Culture
8 Amazing American Pilgrimages
Entertainment & Style
Family & Relationships
Personal Tech
Home & Living
Celebrities
Beauty & Style

Movies for Grownups
Summer Movie Preview

Jon Bon Jovi’s Long Journey Back

Looking Back
50 World Changers Turning 50

Sex & Dating
Spice Up Your Love Life

Friends & Family
How to Host a Fabulous Dessert Party

Home Technology
Caregiver’s Guide to Smart Home Tech

Virtual Community Center
Join Free Tech Help Events

Create a Hygge Haven

Soups to Comfort Your Soul
AARP Solves 25 of Your Problems
Driver Safety
Maintenance & Safety
Trends & Technology

AARP Smart Guide
How to Clean Your Car

We Need To Talk
Assess Your Loved One's Driving Skills

AARP Smart Driver Course

Building Resilience in Difficult Times

Tips for Finding Your Calm

Weight Loss After 50 Challenge

Cautionary Tales of Today's Biggest Scams

7 Top Podcasts for Armchair Travelers

Jean Chatzky: ‘Closing the Savings Gap’

Quick Digest of Today's Top News

AARP Top Tips for Navigating Life

Get Moving With Our Workout Series
You are now leaving AARP.org and going to a website that is not operated by AARP. A different privacy policy and terms of service will apply.
Go to Series Main Page
Have COVID-19? Here’s How Long You Need to Isolate
Vaccines, treatments remain highly important for older adults.
Rachel Nania,
It’s been more than four years since the coronavirus started circulating in the U.S., and in that time, the official guidance on what you should do to avoid catching and spreading it has changed — and it's changing again.
The Centers for Disease Control and Prevention (CDC) announced on March 1 that people with COVID-19 can return to work, school and other activities if their symptoms are mild and improving, and they’ve been fever-free for at least 24 hours without the help of fever-reducing medicine.

AARP Membership — $12 for your first year when you sign up for Automatic Renewal
Get instant access to members-only products and hundreds of discounts, a free second membership, and a subscription to AARP the Magazine.
Once normal activities resume, additional prevention steps are recommended for at least five days to help curb disease spread.
These steps — wearing a mask, improving air quality in your home, keeping up with handwashing, and keeping a distance from others — are especially important for older adults and people who spend time around older adults, the CDC says. Seeking treatment for COVID-19 and staying up to date on vaccines is also key for older adults and others who are at higher risk for a severe case of COVID-19.
Previous COVID guidelines called for people to isolate for at least five days from the start of symptoms or a positive test, and to wear a mask though day 10 in order to avoid spreading the illness to others.
The CDC says the new guidance “brings a unified approach to addressing risks from a range of common respiratory viral illnesses, such as COVID-19, flu, and RSV , which can cause significant health impacts and strain on hospitals and health care workers.” A unified approach makes recommendations easier to follow, the public health agency says, and it makes it more likely that people will adopt them.
The change also “reflects how the circumstances around COVID-19 in particular have changed," the CDC said in a statement. “While it remains a threat, today it is far less likely to cause severe illness because of widespread immunity and improved tools to prevent and treat the disease.” At this point, the majority of people in the population have built up some sort of immunity to COVID-19, either through vaccination, infection or both, health experts say.
The updated guidelines are just for community settings; the CDC says; there are no changes to respiratory virus guidance for healthcare settings.

AARP NEWSLETTERS

%{ newsLetterPromoText }%
%{ description }%
Privacy Policy
ARTICLE CONTINUES AFTER ADVERTISEMENT
Don’t ignore treatment, vaccines
Find covid-19 vaccines in your state.
AARP's 53 state and territory COVID-19 vaccine guides can help you find vaccines near you and provide the latest answers to common questions about costs, eligibility and availability.
Jodie Guest, a professor and senior vice chair in the department of epidemiology at Emory University’s Rollins School of Public Health, says it’s important to not dismiss the virus and to remember that “COVID is still a very significant burden of long-term illness and death.”
The latest federal data shows that more than 17,300 Americans are still being hospitalized each week from COVID-19; more than 1,500 people in the U.S. died from COVID-19 the week of Feb. 3.
“We still must use the commonsense solutions we know work to protect ourselves and others from serious illness from respiratory viruses — this includes vaccination, treatment and staying home when we get sick,” CDC Director Mandy Cohen, M.D., said in a statement.
AARP® Vision Plans from VSP™
Exclusive vision insurance plans designed for members and their families
Paul Offit, M.D., an infectious disease physician at Children’s Hospital of Philadelphia and author of the book Tell Me When It’s Over: An Insider’s Guide to Deciphering COVID Myths and Navigating Our Post-Pandemic World , told AARP that when it comes to COVID-19, “at least half of the hospitalizations and deaths in people who are at high risk are in people who never [got treated].”
A recent study published in January found that only 12.2 percent of 309,755 patients eligible for Paxlovid received a prescription. Another study, yet to be peer reviewed, found that only 9.7 percent of more than 1 million high-risk patients received the treatment.
Paxlovid and other antiviral medications, such as Lagevrio and Veklury, are recommended for older adults — who make up the majority of COVID-19 hospitalizations and deaths — and people with underlying health conditions, like heart disease or lung disease .

LEARN MORE ABOUT AARP MEMBERSHIP.
These medications “work extremely well at mitigating symptoms and shortening the amount of time that people are sick, and how sick they feel while they have it,” Guest says.
The key is starting these antiviral medications right away — within the first five days of symptom onset, says William Schaffner, M.D., a professor of preventive medicine and infectious diseases at Vanderbilt University School of Medicine.
“We tend to say ‘Oh, I’ll see if it gets better tomorrow. I don’t want to bother the doctor with this,’” Schaffner says. “Do this as quickly as possible, because if you have either flu or COVID, instituting the treatments early gives you the best benefit. The longer you wait, the less effective the treatments are.”
Another tool available to older adults is a spring vaccine. Health officials said on Feb. 28 that adults 65 and older should get another COVID-19 vaccine this spring “to provide added protection that may have decreased over time for those at highest risk.”
The vaccine that’s being recommended for the spring shot is the same vaccine that was made available in the fall of 2023. Three versions of this vaccine are available in doctors’ offices and pharmacies: an mRNA vaccine from Moderna, an mRNA vaccine from Pfizer-BioNTech and a protein-based vaccine from Novavax.
Another important point, Offit says, is to remember that it’s not just COVID-19 that can cause people to get seriously ill. Flu and RSV send hundreds of thousands of people to the hospital each year, too. Like COVID, there are also vaccines to help prevent severe illness from these infections.
Offit says the key message is to stay home if you’re sick. “Or if you can’t stay home because your work doesn’t allow you to stay home, then wear a mask,” he says.
“The bottom line is that when people follow these actionable recommendations to avoid getting sick, and to protect themselves and others if they do get sick, it will help limit the spread of respiratory viruses, and that will mean fewer people who experience severe illness,” National Center for Immunization and Respiratory Diseases Director Demetre Daskalakis, M.D., said in a statement. “That includes taking enhanced precautions that can help protect people who are at higher risk for getting seriously ill.”
Editor's note: This story, first published Feb. 16, 2024, has been updated to reflect a change in guidelines.
Rachel Nania is an award-winning health editor and writer at AARP.org, who covers a range of topics including diseases and treatments.
Discover AARP Members Only Access
Already a Member? Login

More on Health

5 Things to Know About the New COVID-19 Vaccines

Are Vaccines Still Free?

Do You Have a Cold? The Flu? COVID? Or RSV?
A few tricks for telling the illnesses apart
Recommended for You
AARP Value & Member Benefits

Learn, earn and redeem points for rewards with our free loyalty program

AARP® Dental Insurance Plan administered by Delta Dental Insurance Company
Dental insurance plans for members and their families

The National Hearing Test
Members can take a free hearing test by phone

AARP® Staying Sharp®
Activities, recipes, challenges and more with full access to AARP Staying Sharp®
SAVE MONEY WITH THESE LIMITED-TIME OFFERS
Advertisement
What’s Going on With the Testing Requirement for Travel?
The requirement to test for Covid before flying to the United States is hated by many travelers and the U.S. travel industry. But the government shows no sign of getting rid of it.
- Share full article

By Heather Murphy
- Published May 19, 2022 Updated June 10, 2022
[Update: The United States will lift the virus testing mandate for international air travelers on June 12. Read more here .]
As countries, including Canada and Britain , have lifted their Covid testing requirements for vaccinated visitors in recent months, some Americans are irate that they still have to show a negative test to board a flight back to the United States.
Jason Miller, a 37-year-old software engineer who lives in Texas, is so frustrated with the rule that he recently sent letters to the White House and several lawmakers and began encouraging others to do the same. “I support the C.D.C., still wear a N95 mask when in crowds and when I travel,” he said. But, he no longer feels that the rule provides value, in large part because “the testing has not stopped variants from entering the country.”
Other travelers have posted similar comments on social media, and a good portion of the travel industry in the United States has made clear it feels the same way.
But they have gotten little satisfaction from the Biden administration and public health officials.
On May 6, Jen Psaki, then the White House press secretary, said she was “not aware of a timeline” for ending the testing requirement and that the administration would base its decision on a Centers for Disease Control and Prevention recommendation. As to what, specifically, the C.D.C. is using to determine whether testing is still necessary, an agency spokeswoman offered the vague explanation that it “is looking at different indicators” and “evaluating all guidance and orders based on the latest science and state of the pandemic.”
The obligatory test has not just created logistical hassles, it has fundamentally shifted the experience of traveling internationally, travelers say.
“It was always in the forefront of my mind,” said Danielle Bradbury, 42, who recently spent 12 days in Israel for her job developing medical devices while her husband cared for their two children back in Boston. “Every time I left the hotel, I asked myself, how much risk of not being able to get home am I putting myself in?”
Why was testing started in the first place?
In January 2021 , when the C.D.C. first instituted the rule that all U.S.-bound travelers 2 years and older had to show a negative test or proof of recovery before boarding a flight, the United States joined a sea of countries experimenting with different ways to slow the virus’s spread across borders. A statement from the State Department announcing the requirement played up the difficulty in getting a test abroad, suggesting that the rule also aimed to discourage Americans from traveling internationally. At that point fewer than 10 percent of Americans were vaccinated and case counts were rising, hitting a record of more than 300,000 new cases on Jan. 8.
Testing was not the first travel limitation the United States had deployed. In the winter of 2020, President Trump banned visitors from China, much of Europe , Brazil and Iran. When President Biden took office he layered the testing requirement on top of the travel bans. (He also expanded the ban to India .)
In late 2021, the United States pivoted away from country-specific bans and doubled down on testing, shortening the window from within three days of travel to one day, even for vaccinated Americans. By then it had become clear that vaccinated people could also spread the coronavirus . (Most unvaccinated visitors from abroad were prohibited from entering the country, even with testing.)
How effective has the policy been?
It depends how you define success, said Jeremy Goldhaber-Fiebert, a professor of health policy at Stanford University. If success was reducing the number of infected people who flew to the United States, he said, the testing requirement achieved that.
“It certainly prevented people who tested positive from getting on planes and it almost certainly prevented some amount of transmission on aircraft and in airports,” he said.
The exact number of infected people who were prevented from boarding planes is unknown, however, because no one tracks whether a passenger cancels a flight because of Covid. Most of the evidence is anecdotal; lots of people have stories about testing positive before flying home.
If success means keeping new variants out of the country, then it failed, said Dr. William Morice , the chair of lab medicine and pathology at the Mayo Clinic.
“The reality is that none of these measures have prevented the rapid global spread of any variant of concern,” he said.
But if success was not preventing the arrival of new variants, but instead delaying their arrival so that hospitals and authorities could be more prepared, then it may have worked. Mark Jit , a professor of vaccine epidemiology at the London School of Hygiene and Tropical Medicine, who has studied the effectiveness of travel requirements, said that this is what testing does well.
“Testing can prevent the peak from being reached so quickly,” he said.
Still, once a variant is already widespread in a country, he found, a travel test has little effect.
Why are many countries getting rid of testing requirements now?
Explanations from authorities include readiness to enter a new phase of the pandemic, high vaccination rates and a determination that new variants are manageable.
“The current variant is making people less ill and the number of people being admitted to intensive care is limited,” the Netherlands government said in a typical statement in March, as it ended travel testing, among other Covid-related recommendations.
What’s the argument for getting rid of the U.S. requirement?
The primary argument is that it’s not doing enough good to rationalize the hassle.
Dr. Tom Frieden, who was the C.D.C. director during the Ebola outbreak of 2014, was among those who made this point. “Between super-effective vaccinations that we have and Paxlovid, which is a super-effective treatment, Omicron is less deadly than flu most years and we don’t require people to test for flu before they get on a plane,” he said. “If a more dangerous variant emerges,” he noted, “that’s a very different situation.”
Others argue that it doesn’t make sense to inconvenience so many people for a system that’s full of holes. Antigen tests — one option for travelers to the United States — are notoriously unreliable in the early stage of infection, said Anne Wyllie, a microbiologist at the Yale School of Public Health. For this reason she called the requirement “hygiene theater.”
The testing requirement is not just annoying for travelers, it’s economically damaging, according to the U.S. Travel Association, a trade group. In a recent letter to Dr. Ashish K. Jha, the White House Covid coordinator, signed by more than 260 businesses, including airlines, cruise operators, casinos, tourism boards, Disney Parks and a zoo, the group said “the economic costs associated with maintaining the measure are significant.”
“Given the slow economic recovery of the business and international travel sectors, and in light of medical advancements and the improved public health metrics in the U.S., we encourage you to immediately remove the inbound testing requirement for vaccinated air travelers,” the group wrote.
A survey commissioned by the group found that 46 percent of international travelers would be more likely to visit the United States without the requirement. A similar survey by the Points Guy, a site that specializes in traveling with credit card points and miles, found that more than half of its participating readers would be more likely to travel abroad without the requirement.
What’s the argument for keeping the policy?
Meegan Zickus, who runs a Facebook group for people with weakened immune systems, said that testing has become more important since the mask requirement went away. Without a testing requirement, most travelers are not going to bother to test or stay home, even if they suspect that they are infected, she said.
“Judging by the past two years, the only way to protect others is some type of enforced testing,” she said, because “the moral compass points directly to self.”
Dr. Seema Yasmin , a public health doctor and the director of the Stanford Health Communication Initiative, echoed this point. “I would say that it can give a high level of reassurance when 75 percent of people are not wearing a mask and might even be coughing and sneezing loudly,” Dr. Yasmin said.
(Though airplane ventilation systems appear to significantly mitigate spread of the coronavirus, research suggests that people sitting within a few rows still pose a risk to one another.)
“Some testing is better than none,” said Nathaniel Hafer , a molecular biologist at the UMass Chan Medical School.
Many countries also use testing to incentivize vaccination by waiving the requirement for vaccinated people, said Meghan Benton , a research director at the Migration Policy Institute, which tracks travel requirements. The United States encourages vaccination in its own way by prohibiting most unvaccinated visitors from abroad from entering.
Could a lawsuit end testing the way it did the mask mandate?
Given that there are currently at least four pending lawsuits that challenge the international testing requirement, some wonder whether it might be struck down by a judge’s decision, as the requirement to wear a mask on airplanes and other forms of transport was in April.
Lawrence O. Gostin, a professor of global health law at Georgetown Law, does not think so. The C.D.C. can require testing from visitors entering the country from abroad because of the Public Health Service Act, which was explicitly created to prevent the introduction of dangerous infectious diseases in the United States, he said.
The rule, he said, “would be exceedingly difficult to successfully challenge in the courts, even for the most conservative judges.”

52 Places for a Changed World
The 2022 list highlights places around the globe where travelers can be part of the solution.
Follow New York Times Travel on Instagram , Twitter and Facebook . And sign up for our weekly Travel Dispatch newsletter to receive expert tips on traveling smarter and inspiration for your next vacation. Dreaming up a future getaway or just armchair traveling? Check out our 52 Places for a Changed World for 2022.
An earlier version of this article misspelled the surname of the chair of lab medicine and pathology at the Mayo Clinic. It is Dr. William Morice, not Omrice.
How we handle corrections
Heather Murphy is a reporter on the Travel desk. She welcomes tips, questions and complaints about traveling during the pandemic. More about Heather Murphy
How Long Should I Wait After Testing Positive Before Traveling?
- Last updated May 26, 2024
- Difficulty Beginner
- Category Travel

As our world continues to grapple with the ongoing COVID-19 pandemic, many individuals find themselves navigating the uncertainties of traveling while balancing the need for precautionary measures. One burning question that arises time and again is, How long should I wait after testing positive before traveling? The answer to this question is not a simple one and has sparked debates among health experts, travelers, and policymakers alike. In this article, we will delve into various perspectives, considerations, and guidelines to help shed light on this crucial issue. Whether you're planning a much-awaited vacation or a necessary business trip, understanding the recommended waiting period after a positive COVID-19 test is essential in safeguarding your health and the well-being of those around you.
What You'll Learn
Test result validity for travel, quarantine period after a positive test, guidelines for traveling after a positive test, precautions to take when traveling after testing positive.

As the world begins to open up and travel restrictions are easing, many people are eager to plan their next trip. However, it is important to remember that COVID-19 is still a very real threat, and precautions must be taken to ensure the safety of yourself and others. One crucial aspect of traveling during the pandemic is understanding the validity of your COVID-19 test results.
When planning to travel, most countries and airlines require travelers to provide a negative COVID-19 test result taken within a specific timeframe before their departure. The validity of the test results varies depending on the country and airline policies, so it is essential to research and understand the requirements of your specific destination before making any travel plans.
The most common type of COVID-19 test used for travel purposes is the PCR (polymerase chain reaction) test. This test is considered the gold standard for COVID-19 testing due to its high accuracy in detecting the virus. The PCR test detects the genetic material of the virus and can determine if a person is currently infected.
The validity of a PCR test result for travel is typically measured based on the time between the test and the departure date. Most countries and airlines require the test to be taken within 72 hours, although some may have different timeframes, such as 48 or 96 hours. It is crucial to check the specific requirements of your destination to ensure you comply with their regulations.
It is important to note that the validity of the test result refers to the time the sample was collected, not the time you received the result. In most cases, you will receive your test result within 24 to 48 hours, but it is advisable to get tested well in advance to allow for any delays or unexpected circumstances.
When getting tested for travel, it is crucial to use a reputable testing facility that provides accurate and reliable results. Before booking an appointment, research local testing centers, labs, or hospitals that are approved for travel testing. Make sure they meet the requirements of your destination, such as providing an official test result document with the necessary information, including the date and time of the test, type of test conducted, and the lab's accreditation.
In addition to a negative COVID-19 test result, some destinations may also require travelers to fill out health declaration forms or undergo additional screening procedures upon arrival. Familiarize yourself with any additional requirements and ensure that you comply with them to avoid any setbacks or complications during your journey.
It is worth noting that even with a negative test result, it is important to continue practicing COVID-19 safety guidelines during your travel. Wear a mask, practice social distancing, wash your hands frequently, and avoid crowded places. Remember that test results are momentary and are not a guarantee of your current health status.
In conclusion, when planning to travel during the pandemic, it is crucial to understand the validity of your COVID-19 test results. Research the requirements of your specific destination and ensure that your test result is within the required timeframe. Use reputable testing facilities and follow all additional requirements set by your destination. Lastly, continue practicing COVID-19 safety precautions during your travel to protect yourself and others.
Exploring Sin City: Is it Safe to Travel to Vegas While Pregnant?
You may want to see also
After testing positive for COVID-19, it is important to follow the guidelines and recommendations given by healthcare professionals and authorities. One crucial aspect to consider is the quarantine period that must be completed before considering any travel plans.
The quarantine period serves as a way to prevent the spread of the virus to others and reduce the risk of further transmission. The duration of the quarantine period may vary depending on the guidelines provided by local health departments or the Centers for Disease Control and Prevention (CDC).
In general, the CDC advises that individuals who test positive for COVID-19 should isolate themselves for a minimum of 10 days from the onset of symptoms. This means that individuals should not travel or leave their isolation area until this period has been completed.
It is important to note that for individuals who test positive but do not experience any symptoms, the CDC recommends isolating for at least 10 days starting from the date of the positive test. Additionally, individuals should be symptom-free for at least 24 hours before ending their isolation period.
During the quarantine period, it is crucial to continue monitoring for any symptoms of COVID-19. If symptoms worsen or new symptoms develop, it is important to consult a healthcare professional for further guidance.
It is also important to follow any additional guidelines or requirements that may be imposed by airlines, transportation authorities, or the destination you are traveling to. Some countries or states may have specific entry requirements, including pre-travel testing or proof of vaccination.
In addition to completing the required quarantine period, it is important to continue practicing preventive measures to reduce the risk of spreading the virus. This includes wearing masks, maintaining physical distance, practicing good hand hygiene, and avoiding large gatherings.
Traveling while still within the quarantine period or experiencing symptoms is not recommended, as it can increase the risk of spreading the virus to others. It is essential to prioritize public health and follow the guidelines set forth by healthcare professionals and authorities.
Overall, after testing positive for COVID-19, it is important to follow the recommended quarantine period and guidelines provided by health authorities. This will help protect yourself and others, and reduce the risk of further transmission of the virus.
The Best Places to Sell Your Travel Money After Your Vacation
If you have recently tested positive for COVID-19, it is important to take appropriate precautions before considering any travel plans. It is crucial to prioritize your health and the well-being of others by not exposing more people to the virus. However, if you need to travel, there are guidelines to follow to ensure the safety of yourself and others.
The first and most important guideline is to isolate yourself. The Centers for Disease Control and Prevention (CDC) recommends that individuals with COVID-19 isolate themselves for at least 10 days, starting from the day symptoms first appeared, or from the day of your positive test if you are asymptomatic. This isolation period is crucial to prevent the spread of the virus to others.
After the 10-day isolation period, you can consider traveling if you meet the following criteria:
- Improvement in symptoms: Your symptoms should have improved, including a resolution of fever without the use of fever-reducing medications.
- No fever: You should not have had a fever for at least 24 hours, without the use of fever-reducing medications.
- Respiratory symptoms improving: Your cough or shortness of breath should have significantly improved.
It is important to note that some people with COVID-19 may continue to test positive for the virus even after their symptoms improve. However, this does not mean that you are still contagious. According to the CDC, most people are no longer contagious 10 days after their symptoms first appeared, as long as they have gone at least 24 hours without a fever and their symptoms have improved.
If you have had close contact with someone who has COVID-19 but you do not have symptoms, the CDC recommends quarantining for 14 days from the last day of close contact. It is best to wait until the end of the quarantine period before considering any travel.
Before traveling, it is essential to check the travel restrictions and requirements of your destination. Some places may have certain limitations or regulations in place to prevent the spread of the virus. It is also advisable to take a COVID-19 test before traveling, even if you have already tested positive. This can help provide peace of mind and ensure that you are no longer shedding the virus.
During your travel, it is crucial to continue practicing good hygiene measures. Wear a mask, wash your hands frequently, and maintain physical distancing whenever possible. Avoid crowded places and close contact with others, especially if you are traveling in an area with high infection rates.
Lastly, if you develop any COVID-19 symptoms during or after your travel, it is essential to get tested again and isolate yourself until you can confirm the results.
In conclusion, if you have tested positive for COVID-19, it is important to prioritize your health and the well-being of others. Follow the guidelines provided by the CDC, including isolating yourself for at least 10 days, and ensure that you meet the necessary criteria before considering any travel plans. Stay informed about travel restrictions and requirements, practice good hygiene measures during your travel, and be vigilant for any symptoms that may arise. Remember, your actions can have a significant impact on preventing the spread of the virus.
A Comprehensive Guide on How to Apply for a Travel Visa to Cuba
If you have recently tested positive for a contagious disease, it is crucial to take necessary precautions before traveling. These precautions not only help to protect yourself but also prevent the spread of the infection to others. Here are some essential measures you should consider when planning to travel after testing positive:
- Follow the advice of healthcare professionals: Consult your healthcare provider for guidance on whether it is safe for you to travel. They can provide specific recommendations based on your health condition and the nature of the infectious disease.
- Wait until you are no longer contagious: It is vital to wait until you are no longer contagious before traveling. The duration of contagiousness varies depending on the disease, so it is crucial to follow the advice of your healthcare provider. They can provide information on when it is safe for you to resume your regular activities, including travel.
- Get retested if necessary: In some cases, your healthcare provider may recommend getting retested to ensure that you are no longer contagious. This is particularly important for diseases where symptoms may persist even after the infectious period has passed.
- Obtain clearance from your healthcare provider: Before traveling, ask your healthcare provider for a clearance letter stating that you are no longer contagious and it is safe for you to travel. This document may be required by airlines, immigration authorities, or other organizations.
- Wear a mask: When traveling, especially in crowded areas, wearing a mask can help to prevent the spread of the infection to others. Choose a mask that provides a proper fit and offers adequate filtration.
- Practice good hand hygiene: Wash your hands frequently with soap and water for at least 20 seconds, especially before eating or touching your face. If soap and water are not available, use hand sanitizer with at least 60% alcohol.
- Maintain physical distance: Try to maintain at least 6 feet of distance from others whenever possible, especially in crowded places such as airports or public transportation.
- Avoid close contact with high-risk individuals: If you have been in close contact with individuals who are more vulnerable to the infection, such as elderly or immunocompromised individuals, consider postponing your travel plans until you are no longer contagious.
- Be aware of travel restrictions and guidelines: Stay updated on travel restrictions, quarantine requirements, and guidelines imposed by local authorities at your destination. These regulations may change frequently, so it is crucial to stay informed before and during your trip.
- Monitor your symptoms: Even if you have recovered from the infection, continue to monitor your symptoms and seek medical attention if they worsen or if new symptoms develop. This is especially important if you plan to travel to a location where medical facilities may be limited.
Remember, even if you have tested positive and taken the necessary precautions, it is important to continue following general guidelines for preventing the spread of infectious diseases, such as wearing a mask, practicing good hand hygiene, and maintaining physical distance. By taking these precautions, you can help protect yourself and others while traveling after testing positive for a contagious disease.
Determining the Size of My Schwinn Traveler: A Guide for Cyclists
Frequently asked questions.
If you have tested positive for COVID-19, you should not travel until you have completed the recommended isolation period and have received clearance from a healthcare professional. The Centers for Disease Control and Prevention (CDC) advises that you should quarantine for at least 10 days from the onset of symptoms or from the date of your positive test if you are asymptomatic.
If you have recovered from COVID-19 and have completed the recommended isolation period, you may be able to travel. However, it is important to check the guidelines and restrictions of your destination, as some countries or states may have additional requirements or quarantine measures in place. It is also essential to continue following all necessary precautions, such as wearing masks and practicing good hygiene, during your travel.
If you have previously tested positive for COVID-19 but now test negative, you may be allowed to travel depending on the specific guidelines of your destination. However, it is crucial to consult with a healthcare professional or local health authorities to ensure it is safe and permissible for you to travel. Keep in mind that testing negative does not guarantee that you can't spread the virus, so it is still important to follow all necessary precautions to avoid transmission.
Many countries and states have implemented travel restrictions or requirements for individuals who have tested positive for COVID-19. These restrictions may include mandatory quarantine upon arrival, presenting negative test results after recovery, or providing proof of recovery through documentation. It is crucial to research and understand the specific guidelines and regulations of your destination before making any travel plans. Additionally, it is always advisable to consult with healthcare professionals or health authorities for accurate and up-to-date information.

- Cagri Burak Author Reviewer Traveller

- Pop Panupong Author Reviewer Traveller
It is awesome. Thank you for your feedback!
We are sorry. Plesae let us know what went wrong?
We will update our content. Thank you for your feedback!
Leave a comment
Travel photos, related posts.

Exploring the World: Traveling 1 Month Before Your Visa Expires
- Mar 16, 2024

Do Senators Cover Their Own Travel Expenses?
- May 14, 2024

Exploring the Winter Wonder of Harbin: A Comprehensive Guide to Traveling to Harbin, China
- May 09, 2024

Exploring Malaysia While Pregnant: Travel Tips and Considerations
- May 15, 2024

The Ultimate Guide to Getting from Nashville Airport to Downtown Hotels
- May 18, 2024

Exploring the Travel Leaders Group's Drug Testing Policy: What Travelers Should Know
- May 26, 2024
New COVID-19 FLiRT variants are now the dominant variant. Could there be a summer surge?
The Centers for Disease Control and Prevention has detected a new set of COVID-19 variants nicknamed FLiRT in wastewater surveillance, according to data from the agency.
From April 28 through May 11, the variant, labeled KP.2 , makes up about 28% of the cases in the United States, according to the CDC. That makes it the new dominant variant in the country, overtaking JN.1. The JN.1 variant , which spread globally over the winter, made up about 16% of COVID-19 cases in the U.S. in the same two-week span.
KP.1.1, another FLiRT variant that is circulating, made up about 7% of COVID-19 cases in that two-week span, according to CDC data.
"The CDC is tracking SARS-CoV-2 variants KP.2 and KP.1.1, sometimes referred to as 'FLiRT,' and working to better understand their potential impact on public health," the agency said in an emailed statement to USA TODAY last week.
"Currently, KP.2 is the dominant variant in the United States, but laboratory testing data indicate low levels of SARS-CoV-2 transmission overall at this time. That means that while KP.2 is proportionally the most predominant variant, it is not causing an increase in infections as transmission of SARS-CoV-2 is low," the CDC said in the statement.
According to the CDC, only 22.6% of adults reported having received an updated 2023-24 COVID-19 vaccine since September 2023. Data also shows that vaccination coverage increased by age and was highest among adults 75 and older.
FLiRT variant: There's a new COVID-19 variant called FLiRT: Here's what you need to know about it
What are the 'FLiRT' variants?
FLiRT is the term being used to describe a whole family of different variants, including KP.2, JN.1.7 and any other variants starting with KP or JN that appear to have picked up the same set of mutations, according to Andy Pekosz, PhD, a professor in molecular microbiology and immunology at the Bloomberg School of Public Health at Johns Hopkins University, in an article posted by the university.
"They are all descendants of the JN.1 variant that has been dominant in the U.S. for the past several months," Pekosz said in the article. "Viruses like SARS-CoV-2 mutate frequently, and when they mutate to evade recognition by antibodies, this often weakens their ability to bind to the cells they want to infect. We then see mutations appear that improve that binding ability."
Will there be a summer surge in COVID cases due to 'FLiRT' variants?
Pekosz said a summer surge is certainly possible, and that the FLiRT variants would be high on his list of viruses that could cause another wave of infections in the U.S.
"That said, our definition of a wave has changed; while we still see case rates rise and fall throughout the year, we see much lower numbers of cases of hospitalizations or deaths than we saw in the first couple years of the pandemic," Pekosz said in the article.
Pekosz also noted that while the waves are becoming smaller, they are still impacting our susceptible populations: the elderly, people who are immunocompromised, and those with other secondary medical conditions.
Symptoms of COVID 'FLiRT' variant
According to the CDC, there are "no current indicators" that KP.2 would cause more severe illness than other strains. The agency said it would continue to monitor community transmission of the virus and how vaccines perform against this strain.
The "FLiRT" variant reportedly has similar symptoms to those from JN.1 which include:
- Fever or chills
- Sore throat
- Congestion or runny nose
- Muscle aches
- Difficulty breathing
- New loss of taste or smell
- "Brain fog" (feeling less wakeful and aware)
- Gastrointestinal symptoms (upset stomach, mild diarrhea, vomiting)
The CDC notes that the list does not include all possible symptoms and that symptoms may change with new variants and can vary by person.
In general, the agency says, people with COVID-19 have a wide range of symptoms , ranging from mild to severe illness. Symptoms may appear two to 14 days after exposure.
Latest COVID guidance from the CDC
In March 2024, the CDC updated its COVID-19 guidance so people who test positive for the virus will no longer be directed to isolate at home for five days.
Health officials announced a new policy focusing on actions people can take to reduce spreading a variety of common respiratory viruses, such as influenza, respiratory syncytial virus (RSV) and COVID-19. Those actions include staying home when sick, staying up to date with vaccines, practicing good hygiene and improving indoor air quality.
The change marked the first time the agency has revised its coronavirus guidelines since 2021. It is intended for people and employers, not for hospitals or nursing homes that have separate guidance, the CDC said.
CDC officials called the change a streamlined approach that’s easier for people to understand and more in line with circulating respiratory viruses that spread the same way and have similar symptoms.
Contributing: Eduardo Cuevas, Adrianna Rodriguez, Ken Alltucker, Mary Walrath-Holdridge and Mike Snider
Gabe Hauari is a national trending news reporter at USA TODAY. You can follow him on X @GabeHauari or email him at [email protected].
"Your browser does not support JavaScript. If the webpage function is not working properly, please enable the browser JavaScript status."
- Acts and Regulations
- Publications
- Important Diseases
- Travelers’ Health
- Travel Health Notices
- Foreigners’ Health
- Infection Control and Biosafety
- Vaccine-Preventable Diseases Control
- Research & Development
- End TB Special Project
- Preparedness and Response
- Field Epidemiology Training Program
- Research Reports
- Internship(training) Programs Guidelines
- Taiwan National Infectious Disease Statistics System
- Statistics of HIV/AIDS
- Disease Surveillance Express
- Influenza Express
- National Notifiable Disease Surveillance Report
- Weekly Report of Enterovirus Infection
- School-based Surveillance Report
- Taiwan Healthcare-associated infection and Antimicrobial resistance Surveillance System
- Taiwan CDC Open Data Portal
- Taiwan IHR National Focal Point Contact Information
- International Cooperation
- International Conference
- APEC Related Events
- Foreign Visitors
- Relative Resources
- School Visits

- Advanced Search
- Press Releases
- Current Topics
"Tuberculosis: Stop, Screen, and Listen – Advancing Screening in Response to World Tuberculosis Day's Theme 'Yes! We Can End TB' – Silent Tuberculosis Leaves No Trace"
Taiwan Meets Criterion of Mpox Elimination set by WHO. People Eligible for Mpox Vaccination Are Reminded to Receive Two Doses of Vaccines to Protect Their Own Health and Prevention Results.
Everyone Joins Hands to Stay Healthy: Second Phase of Influenza Vaccine Rollout Begins on November 1
Get a Flu Shot for Health and Happiness: government-funded influenza vaccination campaign launched in stages on October 2
First phase of vaccination campaign for XBB.1.5-adapted COVID-19 vaccine starts today; people aged 65 and over advised to get vaccinated
Taiwan CDC hosts APEC Conference on Managing Infectious Diseases on Cross-Border Cruise Ships in the Post-COVID-19 Era: Application of Digital Technology, bringing experts, scholars, and cruise operators together in Taipei to strengthen resilience of epidemic prevention on cruise ships and promote safe cross-border travel
US and Taiwan co-organize International Training Workshop on Molecular Diagnosis for Zika participated by 12 countries in Southeast Asia to strengthen Asia-Pacific regional capacity to tackle Zika virus
U.S. and Taiwan co-organized International Conference on Dengue Prevention and Control and International Dengue Expert Consultation Meeting to tackle increasing dengue threat caused by global warming together
30 Years of Field Epidemiology Training Program in Taiwan
The 11th Taipei International Conference on HIV/AIDS - Turn the Tide, Stop on Me
International Expert Meeting—Challenges and Opportunities in Prevention and Control of Rabies
APEC Conference on the Innovation, Achievement and Sustainable Development in Public Health Emergency Response Systems 10 years after SARS Epidemic
Speech by Minister of Health at Contract-signing Ceremony between Department of Health and Ministry of Justice
Speech by Minister of Justice at Contract-signing Ceremony between Department of Health and Ministry of Justice
Director's Tribute to Dr. Lee Jong-wook
Premier's Opening Address to the 8th Taipei International Conference on HIV/AIDS
Diseases & Conditions
Programs & campaigns, data & statistics.
- MyServiceNSW
- Manage account
- Logout of MyServiceNSW
Testing and what to do if you have COVID-19
How to get a test if you think you might have COVID-19, and what to do if you test positive.

COVID-19 update – 30 May 2024
COVID-19 is at high levels in the community.
Read the latest data from NSW Health .
Continue to protect other people. Please stay home if you have any cold or flu symptoms. Wear a mask if you need to leave home.
Learn how to keep yourself and others COVID-safe .
Getting a test for COVID-19
Which covid test should i do.
Guidance on which test is best for you.
Information for people exposed to COVID-19
Understand your risk and what you can do to protect yourself and your loved ones.
Symptoms and how it spreads
Learn about the symptoms of COVID-19, when they appear and how it spreads.
Advice for higher risk groups
Some people are at higher risk of severe illness from COVID-19. Find information on how to protect yourself and others from becoming very unwell.
If you're at higher risk of severe illness, talk to your doctor about PCR tests.
Managing your COVID-19 illness
What to do if you test positive.
Advice on how you can safely manage mild symptoms at home.
Antiviral medicines
Find out if you're eligible for antiviral medicines and how to access them.
Information on long-term symptoms you may experience due to COVID-19, and where to seek support.
COVID-19 guidance for families
Advice for parents and carers on COVID safety in schools and early childhood education services.
Advice for workers
What to do if you test positive and information about returning to work.
Guidance for businesses
What you need to do as an employer to manage the risk to colleagues and customers.
Easy Read and in-language resources
Easy read information on covid-19, in-language and translated covid-19 support, contact us and find translation help.
- Service NSW – information and advice for NSW residents and businesses. Phone 13 77 88
- Healthdirect – government-funded 24-hour health advice. Phone 1800 022 222
- Disability Gateway – information for people with disability. Phone 1800 643 787
- Mental health support, services and programs
- Service NSW Savings Finder – find rebates and vouchers relevant to you
- Business Concierge – tailored advice from Business Connect advisors. Phone 13 77 88
- Translating and Interpreting Service (TIS National) – free service provided by the Australian Government. Phone 13 14 50
CDC Updated COVID Guidelines for 2024: What to Do if You Test Positive
This marks a major change in how to deal with a positive test.

What do experts think of the updated guidelines?
How to protect people around you if you test positive.
With over four years since the COVID-19 pandemic started, a lot has changed. For many, life has gone back to normal, treating the Coronavirus like the common cold. And while the virus continues to pop up (like the latest FLiRT COVID variants ), the Centers for Disease Control and Prevention (CDC) has changed its COVID-19 protocol recommendations for 2024, updating them to reflect the changing severity and transmission of the virus.
The updated guidance throws out the previous five-day isolation recommendation for a more relaxed approach. The CDC is also now lumping COVID-19 recommendations with those of the flu and RSV .
“CDC is making updates to the recommendations now because the U.S. is seeing far fewer hospitalizations and deaths associated with COVID-19 and because we have more tools than ever to combat flu, COVID, and RSV,” the organization said in a statement online.
The CDC also stressed the importance of “core prevention steps and strategies” to lower the risk of getting seriously ill from a respiratory virus, including staying up to date with vaccines, practicing good hand hygiene, and focusing on cleaner air by trying to bring in more fresh outside air, purifying indoor air (by using the best air purifiers ), and gathering outside instead of inside.
Meet the experts: William Schaffner, M.D., an infectious disease specialist and professor at the Vanderbilt University School of Medicine; and Amesh A. Adalja, M.D., senior scholar at the Johns Hopkins Center for Health Security
But many (understandably) want to know what they should now do when they get sick with COVID-19. Here’s what the CDC says, along with how infectious disease doctors feel about the changes.
What to do if you test positive for COVID-19
If you test positive for COVID-19 or have respiratory virus symptoms (like a fever, chills, fatigue, cough, runny nose, and/or headache) that aren’t explained by another cause, the CDC recommends that you stay home and away from others. During that isolation period, it's best to wear a high-quality, well-fitting mask, like an N95 mask, when you need to be around others.
The CDC says that you can go back to your normal activities when you’ve been fever-free without the use of fever-reducing medication, and feeling better for at least 24 hours.
When you go back to your normal activities, the CDC recommends that you “take added precaution” for the next five days, like using masks, practicing physical distancing, and testing yourself when you’ll be around other people indoors.
“Keep in mind that you may still be able to spread the virus that made you sick, even if you are feeling better,” the CDC says. “You are likely to be less contagious at this time, depending on factors like how long you were sick or how sick you were.”
If you develop a fever or start to feel worse after you’ve gone back to your normal activities, the CDC recommends that you stay home and away from others for at least 24 hours until your symptoms get better and you haven’t had a fever without the help of fever-reducing medication. Once you go back to your usual routine, the CDC recommends again taking extra precautions for the next five days.
If you’re at high risk for serious complications from COVID-19, are immunocompromised, or are over 65, it’s a good idea to contact your doctor to see if you may benefit from taking an antiviral medication like Paxlovid , says William Schaffner, M.D., an infectious disease specialist and professor at the Vanderbilt University School of Medicine.
Infectious disease experts are supportive of the CDC’s change. “It’s a good thing and will be welcomed by the general public, which has largely been doing this on their own for some time,” Dr. Schaffner says. Dr. Schaffner says he and several other people in the infectious disease community have been urging the CDC to revise the guidelines for a while. “The CDC waited a bit to make sure that the current trends in COVID really were sustained,” he says.
Infectious disease expert Amesh A. Adalja, M.D., senior scholar at the Johns Hopkins Center for Health Security, says he’s “supportive” of the new guidelines. “They reflect the fact that the context of COVID-19—the respiratory virus infection for which we have the most tools—has changed,” he says. “Similar updates to the guidelines were made in California, Oregon, and many other countries and, in that respect, the CDC was lagging.”
Dr. Schaffner points out that, while people continue to get seriously ill and die from COVID-19, that’s no longer the case for most of the American public. “Well over 90% of the U.S. population has had some experience with COVID, through infection or vaccination, or both,” he says. “The virus itself is not as virulent or severe as it once was, and it appears to produce somewhat milder disease now."
Shortening the isolation period should have “no measurable impact” on how much COVID-19 spreads in the general population, Dr. Schaffner says.
To protect others around you if you test positive for COVID-19, the CDC recommends isolating—including from members of your household—until you’ve been fever-free without the help of fever-reducing medications for 24 hours. “This is especially important if you’re around anyone who is at high risk of serious disease,” Dr. Schaffner says.
Masking up when you need to be around others and carefully washing your hands can also help limit the spread, the CDC notes. It’s also a good idea to take steps to create cleaner indoor air, like opening doors and windows and using exhaust fans, per the CDC . You can even try adding an air purifier to your space.
The updated COVID boosters help protect against serious infection, so getting vaccinated is one of your best lines of defense against serious illness. Dr. Schaffner stresses the importance of getting the COVID-19 vaccine when you’re healthy, as well. “So many people have not taken advantage of the updated vaccine,” he says. “But the vast majority of people being hospitalized today because of COVID are unvaccinated.”
This article is accurate as of press time. However, as the COVID-19 pandemic rapidly evolves and the scientific community’s understanding of the coronavirus develops, some of the information may have changed since it was last updated. While we aim to keep all of our stories up to date, please visit online resources provided by the CDC , WHO , and your local public health department to stay informed on the latest news. Always talk to your doctor for professional medical advice.
COVID-19 Symptoms to Know in 2024

Leaky Blood Vessels May Cause Long COVID Brain Fog

CDC: Older Adults to Receive Another COVID Booster

Here’s What Researchers Think Causes Long COVID

Exercise May Make Long COVID Worse for Some

What It’s Really Like to Live With Long COVID

The Dangerous COVID-Heart Health Connection
What Is the COVID-19 Variant, JN.1?
How Many COVID Variants Are There?

What Does a Dry Cough Feel Like?
What Is HV.1? Doctors Break It Down.
CDC cuts the recommended isolation and quarantine periods for coronavirus infections
People who test positive need to isolate themselves for 5 days if they don’t show symptoms. the change reflects “what we know about the spread of the virus” and vaccine protection, the cdc chief says..

People who test positive for the coronavirus need to isolate themselves for only five days if they don’t show symptoms, the Centers for Disease Control and Prevention said Monday. This cuts in half the earlier recommendation of 10 days of isolation.
Data shows that the majority of coronavirus transmission “occurs early in the course of illness,” the CDC explained — generally in the one or two days before symptoms begin and two or three days after.
“Therefore, people who test positive should isolate for 5 days and, if asymptomatic at that time, they may leave isolation if they can continue to mask for 5 days to minimize the risk of infecting others,” the CDC said in a statement .
The CDC has also updated its recommended quarantine period for people exposed to the virus. It says unvaccinated people should quarantine for five days, followed by five days of “strict mask use.” Exposed people who are more than six months past their second dose of the Pfizer-BioNTech or Moderna vaccines, or two months out from a Johnson & Johnson vaccine, should also quarantine for five days.
People who have gotten their booster shot don’t need to quarantine after exposure but should wear a mask for the next 10 days.
“The Omicron variant is spreading quickly and has the potential to impact all facets of our society,” said the CDC’s director, Dr. Rochelle Walensky, in a statement. “CDC’s updated recommendations for isolation and quarantine balance what we know about the spread of the virus and the protection provided by vaccination and booster doses. These updates ensure people can safely continue their daily lives.”
Dr. Megan Ranney, the associate dean at Brown University’s School of Public Health, tweeted Monday that a major reason the federal government altered isolation requirements is due to the economic strain of a full quarantine.
“Our economy is going to shut down if everyone has to isolate for 10 days. Luckily the science backs up the move, at least partially,” she tweeted. “On the one hand: I’m all for following the science for the vaccinated & asymptomatic. No reason to keep people home unnecessarily.”
Kudos, she said, to the CDC “for recognizing that our knowledge has changed -- and the virus has changed” especially for the vaccinated.
Ranney said what would make this decision even safer would be to require a rapid test before ending isolation.
The CDC doesn’t currently require this step and rapid, at-home COVID tests have been hard to come by during the omicron surge.
The Biden administration, which has come under pressure for not increasing widespread availability of at-home tests, last week rolled out a plan to set up federal testing across the country. The government will also buy a half-billion at-home COVID test kits and mail them out. But deliveries won’t start until January.
The new guidance comes days after the CDC loosened rules for how long health care workers should isolate after infection with the coronavirus, from 10 days to seven days. If there were staffing shortages, that isolation time could be further reduced.
The next day, New York officials followed suit , reducing to five the number of days for health care workers to isolate after a positive coronavirus test. On NPR’s Morning Edition on Monday, Dr. Anthony Fauci praised the move .
Five days of quarantine should be enough for health care workers, Fauci said, adding: “That’s going to be under consideration of whether or not we want to diminish it” for the general public.
In the U.S. as of Monday, 242 million people have received at least one dose of a COVID-19 vaccine, 205 million are fully vaccinated and 66 million have received a booster, according to the CDC’s COVID Data Tracker .
Copyright 2021 NPR. To see more, visit https://www.npr.org.


IMAGES
COMMENTS
Consider getting a COVID-19 test if you: Develop COVID-19 symptoms before, during, or after travel. Will be traveling to visit someone who is at higher risk of getting very sick from COVID-19. Were in a situation with a greater risk of exposure during travel (e.g., in an indoor, crowded space like an airport terminal while not wearing a mask).
PCR tests are the "gold standard" for COVID-19 tests. They are a type of nucleic acid amplification test (NAAT), which are more likely to detect the virus than antigen tests. Your sample will usually be taken by a healthcare provider and transported to a laboratory for testing. It may take up to 3 days to receive results.
Do not travel if you test positive or have symptoms of COVID-19; immediately isolate yourself, and follow public health recommendations. After traveling internationally - Get tested with a viral test 3-5 days after travel AND stay home for 7 days after travel. Even if your test is negative, stay home for the full 7 days. If your
Wear a mask around other people when you have COVID-19. Wear a mask for 10 days after you start feeling sick. Wear a mask for 10 days after you test positive. Wear a mask with extra protection. The mask must cover your nose and mouth. The mask must fit under your chin. The mask must be snug on your face.
March 1, 2024, 10:01 AM PST. By Erika Edwards. People who test positive for Covid no longer need to isolate for five days, the Centers for Disease Control and Prevention said Friday. The CDC's ...
Before travel, encourage patients to have a healthcare contingency plan in place, should they test positive for COVID-19 while abroad (see Travel Insurance, Travel Health Insurance, and Medical Evacuation Insurance chapter). For mild disease, medications that are typically available over the counter can be used to alleviate symptoms.
Before this, the CDC recommended that people who test positive for COVID should isolate away from others for five days and wear a well-fitting mask around others for the following five days. This was different from the general guidance for other common respiratory viruses, like flu and RSV.
COVID-19. Travel: Frequently Asked Questions and Answers. Updated Apr. 2, 2021 Print. The COVID-19 pandemic is a rapidly evolving situation and CDC guidance is updated frequently. General. Check CDC's Domestic Travel or International Travel pages for the latest recommendations for fully vaccinated and unvaccinated travelers.
More. Learn about CDC's Traveler Genomic Surveillance Program that detects new COVID-19 variants entering the country. Sign up to get travel notices, clinical updates, & healthy travel tips. CDC Travelers' Health Branch provides updated travel information, notices, and vaccine requirements to inform international travelers and provide ...
test, as long as you do not have symptoms of COVID-19. If you have had a positive viral test in the past 3 months, and you have met the criteria to end isolation, travel with a copy of your test results and a letter from your doctor or health department that states you have been cleared for travel. More Information Travel During COVID-19 ...
If you're traveling without being fully vaccinated, you can take some steps to protect yourself and the people around you: Get a COVID test 1 to 3 days before you leave. Wear a mask on public ...
What to Know About the C.D.C. Guidelines on Vaccinated Travel. In updated recommendations, the federal health agency said both domestic and international travel was low risk for fully vaccinated ...
The CDC says not to travel if you have symptoms of COVID-19 or have tested positive and not yet completed an isolation period. Without a testing requirement in place, though, that guideline ...
People with a positive test result should follow CDC's COVID-19 isolation guidance. Testing people who have recently tested positive, and recovered from COVID-19 If someone has had exposure to someone with COVID-19 and is asymptomatic, but has had COVID-19 within the past 30 days*, testing to identify a new infection is generally not recommended.
Today, CDC is streamlining its COVID-19 guidance to help people better understand their risk, how to protect themselves and others, what actions to take if exposed to COVID-19, and what actions to take if they are sick or test positive for the virus. COVID-19 continues to circulate globally, however, with so many tools available to us for ...
Testing before and after travel can lower the risk of spreading the virus that causes COVID-19. If you haven't been vaccinated, the CDC recommends getting a viral test within three days before your trip. Delay travel if you're waiting for test results. Keep a copy of your results with you when you travel.
Paxlovid treatment helps prevent hospitalization and death due to COVID-19. COVID-19 rebound has been reported to occur between 2 and 8 days after initial recovery and is characterized by a recurrence of COVID-19 symptoms or a new positive viral test after having tested negative. A brief return of symptoms may be part of the natural history of ...
A guide to COVID tests: When to test, what kind to use and what your results mean. COVID-19 rapid tests are distributed in Brooklyn in late December. Self-tests are in short supply in many parts ...
A: People with COVID-19 could potentially transmit it to others well beyond a day after developing symptoms or testing positive. New guidance from the CDC advises people to isolate until they have ...
Previous COVID guidelines called for people to isolate for at least five days from the start of symptoms or a positive test, and to wear a mask though day 10 in order to avoid spreading the illness to others. The CDC says the new guidance "brings a unified approach to addressing risks from a range of common respiratory viral illnesses ...
In January 2021, when the C.D.C. first instituted the rule that all U.S.-bound travelers 2 years and older had to show a negative test or proof of recovery before boarding a flight, the United ...
10 days. Time taken for symptoms to show after exposure. 2 to 14 days. Time taken for a negative test after exposure. Typically 5 to 7 days. Time taken for a positive test after exposure. Typically 2 to 14 days. Travel restrictions after testing positive. Varies by country and mode of transport.
Latest COVID guidance from the CDC In March 2024, the CDC updated its COVID-19 guidance so people who test positive for the virus will no longer be directed to isolate at home for five days.
2023 - 8. 24. Taiwan CDC hosts APEC Conference on Managing Infectious Diseases on Cross-Border Cruise Ships in the Post-COVID-19 Era: Application of Digital Technology, bringing experts, scholars, and cruise operators together in Taipei to strengthen resilience of epidemic prevention on cruise ships and promote safe cross-border travel.
Trip interruption travel insurance will reimburse you for missed portions of your trip if you're forced into quarantine due to a positive Covid test. It can cover 100% to 200% of your prepaid ...
COVID-19 update - 23 May 2024. COVID-19 remains at moderate levels. Read the latest data from NSW Health. Continue to protect other people. Please stay home if you have any cold or flu symptoms. Wear a mask if you need to leave home. Learn how to keep yourself and others COVID-safe.
If you test positive for COVID-19 or have respiratory virus symptoms (like a fever, chills, fatigue, cough, runny nose, and/or headache) that aren't explained by another cause, the CDC ...
Open doors to let in air from outside. Open windows to let in air from outside. Use fans to clear the air in your home. Use a portable air cleaner to help filter the air in your home. The best portable air cleaners are called "HEPA" cleaners. Easy to read information about what to do if you have been around someone with COVID-19.
People who test positive need to isolate themselves for 5 days if they don't show symptoms. The change reflects "what we know about the spread of the virus" and vaccine protection, the CDC chief says.
CDC and Food Safety. CDC determines prevention measures for foodborne illness and works with partners. May 2, 2024. More food safety content. Educational Materials and Videos. Collection of social media, videos, infographics and other resources. May 2, 2024. Foods That Can Cause Food Poisoning.