Root out friction in every digital experience, super-charge conversion rates, and optimize digital self-service
Uncover insights from any interaction, deliver AI-powered agent coaching, and reduce cost to serve
Increase revenue and loyalty with real-time insights and recommendations delivered to teams on the ground
Know how your people feel and empower managers to improve employee engagement, productivity, and retention
Take action in the moments that matter most along the employee journey and drive bottom line growth
Whatever they’re are saying, wherever they’re saying it, know exactly what’s going on with your people
Get faster, richer insights with qual and quant tools that make powerful market research available to everyone
Run concept tests, pricing studies, prototyping + more with fast, powerful studies designed by UX research experts
Track your brand performance 24/7 and act quickly to respond to opportunities and challenges in your market
Explore the platform powering Experience Management
- Free Account
- For Digital
- For Customer Care
- For Human Resources
- For Researchers
- Financial Services
- All Industries
Popular Use Cases
- Customer Experience
- Employee Experience
- Employee Exit Interviews
- Net Promoter Score
- Voice of Customer
- Customer Success Hub
- Product Documentation
- Training & Certification
- XM Institute
- Popular Resources
- Customer Stories
- Market Research
- Artificial Intelligence
- Partnerships
- Marketplace
The annual gathering of the experience leaders at the world’s iconic brands building breakthrough business results, live in Salt Lake City.
- English/AU & NZ
- Español/Europa
- Español/América Latina
- Português Brasileiro
- REQUEST DEMO
- Experience Management
- Sector Specific
- Patient Experience
- Patient Journey

Try Qualtrics for free
The patient journey: what it is and how it’s vital for success.
10 min read In the digital age, the patient experience has become more complex but also more critical as it relates to patient retention, reimbursement, and patient satisfaction. In order to thrive in today’s healthcare landscape, it’s important to look at the patient journey when aiming to improve the patient experience.
Does your healthcare organization ask patients for feedback following clinical encounters? This is a common approach used to improve the patient experience . You may gather key insights about a specific encounter, but you’ll miss out on an untapped system of important patient interactions throughout the care journey .
Stay up-to-date on patient experience management trends with our guide
Improving patient experiences requires looking at the entire healthcare ecosystem. Patients communicate with their healthcare providers through a variety of channels, while interacting with a wide range of departments and individuals along the way.
To stand out in the market and provide an optimal experience for your patients , hospitals and health systems should look beyond clinical service delivery and begin patient journey mapping.
The patient journey is the entire sequence of events that begins when the patient first develops a need for clinical care and engages with your organization. It follows the patient’s steps as they navigate your healthcare system, from initial scheduling to treatment to continuous care.
The patient journey vs. the patient experience
Why is the patient journey important? Each touchpoint of the patient engagement journey, from a simple visit to your website to checking in for an appointment, has downstream effects that can help or hinder meeting patient needs.
As the patient experience evolves , it’s important to expand how you are listening to your patients in order to close gaps and make continuous improvements.
In recent years, emphasis on the patient experience has become the focus of regulatory programs and payment incentives. Many quality measures today center around collecting patient feedback on the healthcare experience.
To satisfy these measures and drive quality improvement efforts, many organizations turn to post-transactional patient satisfaction surveys . The feedback from these surveys often measures only a limited set of touchpoints while overlooking other critical data from the full patient journey.
A holistic view
Patient experience programs often hone in on clinical service delivery, and many regulatory programs focus solely on numerical scores to measure improvement. These approaches may fail to identify pain points occurring in dozens of patient interactions within a healthcare system.
A holistic view of the patient journey is the key to modernizing and strengthening your efforts to meet your patients’ needs . By breaking down silos into separate patient events, you can begin to identify blind spots where hidden challenges exist in your patient experiences.
By the time your patients engage with their care providers, they’ve likely interacted with your organization a number of times. These interactions can occur digitally, over the phone, or in person. Navigating your website, verifying insurance coverage, and scheduling an appointment are all examples of pain points that may be creating barriers to care.
It’s easy to assume any given touchpoint is more or less important than another. The fact is that each one provides unique value to the patient’s experience. Each of them plays a role in helping the patient achieve their goals.
Patient engagement with your organization doesn’t begin when the patient is examined by the healthcare provider, or even when they enter your medical facility. From initial awareness to ongoing care, the patient journey encompasses every separate interaction throughout the process of seeking, receiving, and continuing care within a health system.
There are several stages of the patient journey you should consider.
What triggers the patient’s need for care, and how does the patient learn about your organization?
- Quality ratings and online reputation
- Campaign management
- Community involvement
Consideration
What drives a patient to choose your organization over another?
- Coverage and benefits
- Healthcare provider search
What impacts your patient’s ability to receive care or support from your organization?
- Patient portal
- Call center
- Price transparency
Service delivery
What is your patient’s experience with their clinical care?
- Interaction with healthcare professionals
- Check-in and check-out
- Discharge process
Ongoing care
What type of patient engagement occurs after a visit?
- Wellness and care management
- Social determinants of health
- Population health
All of these examples influence the way in which your patients make decisions. It’s essential to understand which touchpoints along the patient’s journey are the most impactful or leave the largest gaps in care. There are patient expectations surrounding each type of interaction.
Patient journey mapping
How do you move beyond patient feedback on service delivery and focus instead on the end-to-end patient journey? Patient journey mapping can provide context around what your patients experience as they move through the various channels of your organization.
A patient journey map is a visual representation of the steps the patient takes as they engage with your organization in order to receive care. Patient journey maps should capture pre-visit and post-visit touchpoints in addition to those that occur when the patient is onsite at your medical facility.
Your patient journey may be broad and applicable to your entire patient base, or it may be specific to certain specialties, patient personas , demographics , or health events.
Start with an inventory of all the touchpoints for which you currently collect patient feedback. Next, determine what’s missing. Envision moving through your organization from your patient’s point of view. Your patient journey map should include Interactions that take place pre-visit and post-visit, which are not always captured by traditional or regulatory surveys.
Benefits of patient journey mapping
There are many benefits to capturing key moments along the whole patient journey.
- A patient journey map allows you to walk in your patient’s shoes and think the way they think as they engage with your organization. Patient journey mapping looks at patient experiences from the outside in.
- Mapping your patient journeys helps you to hone in on the areas where you may not be listening to your patients, but should be.
- You can uncover inconsistencies, gaps in care, and common pain points with patient journey mapping. These are difficult to identify when you collect feedback only on service delivery. Collecting data around these areas can aid in process optimization and improve patient satisfaction.
- A patient journey map can give you a cross-functional view of your patient experience so you can engage all teams and stakeholders in gathering and understanding patient insights .
- Patient journey mapping provides context around behavior and attitudes as patients move throughout the channels of your organization. Are patients having to repeat paperwork? Do patients understand their follow-up care instructions? Are your patients able to easily navigate your patient portal? Patient journey mapping can help to answer these types of questions.
- Mapping the patient journey can transform your patient care approach from a reactive one to a proactive one.
Using patient journey data
Once you can visualize the end-to-end patient journey within your organization, it’s time to listen to your patients and start gathering data.
Gather the right data
Collect data on all the touchpoints of the patient journey. Understand how your patients are interacting with every aspect of your organization, including non-clinical interactions such as your website, scheduling, and billing. Involve multiple stakeholders during this process, including managers, doctors, nurses, other healthcare professionals, and administrative staff.
It’s important to capture all steps involved in each of these stages. For example, when looking for potential pain points surrounding the patient portal, consider how the patient sets up an account, logs in, navigates the interface, gets technical assistance, and so forth.
Also, consider patient expectations and usage–what are they using the portal to accomplish? Look for potential gaps in these experiences , such as paying a bill, contacting the provider with a question, reviewing test results, or scheduling an appointment.
Understanding the patient’s goals and actions along all the different paths of your patient journeys is essential to gathering the data you need to take action.
Understand the data
Gain insights using analytics , benchmarking, and visualizations to identify gaps and discover opportunities at each step of the patient’s journey. Trends along the various touchpoints can help you to discover pain points and identify opportunities.
It’s also important to engage all the right stakeholders when reviewing the data you collect. Involving the right teams and people is essential to understanding gaps and improving experiences.
Take action
Use the insights from all touchpoints along your patient journey to develop solutions to improve your patient experience.
A closed-loop system is ideal for taking action to close gaps along the patient journey. For example, if a patient gives a low score on a survey for your online scheduling tool, you could follow up with the patient to ensure they were able to schedule an appointment.
Using the data you collect to drive specific actions and feed into processes is vital to creating a seamless patient journey.
Why Qualtrics?
At Qualtrics, we want to enable you to listen to and understand your patients across all aspects of their journey, all within a single platform. Omnichannel distribution lets you gather feedback from patients from where they are at during each touchpoint, with powerful built-in analytics for uncovering meaningful insights.
The Qualtrics XM Platform™ provides a single source for all of your patient journey data. Real-time feedback displayed in role- and location-based dashboards helps deliver pertinent information to the right people, allowing you to take prompt action where needed.
Ready to collect data and drive action along your patient journey?
Related resources
Patient experience 12 min read, symptoms survey 10 min read, nurse satisfaction survey 11 min read, cahps surveys 6 min read, patient journey mapping 15 min read, patient feedback 15 min read, healthcare branding 13 min read, request demo.
Ready to learn more about Qualtrics?
Patient Satisfaction Questionnaires
Explore our comprehensive guide to understanding and utilizing a Patient Satisfaction Questionnaire. Discover samples, benefits, and download a free PDF today.

By Audrey Liz Perez on Apr 08, 2024.
Fact Checked by Nate Lacson.

What is a Patient Satisfaction Questionnaire?
A Patient Satisfaction Questionnaire is a critical tool used in healthcare settings to gather information about patients' experiences and satisfaction levels with the services they have received.
This tool offers a multi-faceted insight into the healthcare experience, touching on the quality of care, communication with medical staff, facilities, waiting times, and overall satisfaction. Whether it's the friendliness of the nursing staff, the medical facility's cleanliness, or the doctors' clarity of instructions, every detail of patient interaction can be assessed through this questionnaire.
Beyond mere feedback collection, a bridges healthcare providers and patients, fostering a collaborative relationship emphasizing patient voices. The data collected through this tool is quantitative and rich in qualitative insights, reflecting the patient's emotions, preferences, and expectations.
When used effectively, a patient satisfaction questionnaire pdf or paper form can catalyze change, encouraging healthcare facilities to align their services with the patient's needs, ultimately elevating the standard of care provided.
Printable Patient Satisfaction Questionnaire
Download this Patient Satisfaction Questionnaire to gather accurate feedback.
How does it work?
Understanding how a Patient Satisfaction Questionnaire functions is essential for healthcare providers and patients. It's a structured process that ensures patient voices are heard and their feedback contributes to continuous quality improvement.
Step 1: Distribute the Questionnaire
The patient satisfaction questionnaire sample is distributed to patients after a medical visit, either in person, via email, or through a web portal.
Step 2: Completion by the Patient
Patients complete the questionnaire, evaluating their healthcare experience on a 5-point scale.
Step 3: Collect and Analyze Responses
Responses are collected, and the data are analyzed to identify trends, strengths, and areas for improvement.
Step 4: Implement Changes
Based on the insights gathered, changes and enhancements can be made to address patient needs and enhance satisfaction.
Patient Satisfaction Questionnaires Example (sample)
We have provided a sample completed questionnaire within this guide. This patient satisfaction questionnaire sample clearly shows users how to complete it and what to expect from the questions. By viewing this example, healthcare providers can gain insight into the information they can expect to collect. At the same time, patients can familiarize themselves with the type of questions that may be asked.
Furthermore, this sample practically illustrates the patient satisfaction survey questionnaire free from biases and leading questions.
It demonstrates how carefully crafted questions can lead to authentic and meaningful feedback, ultimately contributing to actionable insights. Whether you are a healthcare provider looking to implement such questionnaires or a patient preparing to fill one out, the sample provided here is a valuable resource to understand the structure, content, and intent behind a well-designed Patient Satisfaction Questionnaire.
Download this Patient Satisfaction Questionnaire Example:

When would you use this Form?
The Patient Satisfaction Questionnaire is more than just a feedback form; it's an essential bridge that connects patient experience with healthcare excellence. This tool reflects the patient's journey within a healthcare facility by assessing various facets of medical service. Whether it's understanding their comfort level, communication experience, or satisfaction with treatment, these questionnaires enable healthcare providers to listen actively to their patients.
Employed in diverse healthcare scenarios, here's when it’s most appropriate to use this essential resource:
Post-Surgery Feedback
To gather patient experiences after surgical procedures, understand their comfort level, and evaluate their satisfaction with the post-surgical care and recovery process.
Outpatient Clinic Visits
During routine check-ups and consultations, these questionnaires help assess patient satisfaction with waiting times, interactions with staff, and overall visit experience.
Specialist Appointments
By employing the questionnaire during visits to medical specialists, healthcare providers can gauge the patient’s satisfaction with the specialized care and instructions received and their understanding of ongoing treatment plans.
Emergency Department Visits
Utilized to understand the patient’s perception of urgent care services, including their assessment of emergency care's timeliness, efficiency, and compassion.
Telemedicine Services
In an increasingly digital world, assessing satisfaction with remote healthcare services ensures that the quality and patient-centric approach is maintained, even when care is delivered virtually.
The benefits of a Patient Satisfaction Questionnaire extend far beyond the immediate feedback collection. It represents a comprehensive approach to healthcare that puts the patient at the center of all operations. By translating patient experiences and perceptions into actionable insights, these questionnaires forge a path toward continuous improvement, greater empathy, and a more responsive healthcare system.
Here's a closer look at the significant benefits:
1. Enhanced Patient-Centric Approach
It focuses on individual patient needs and preferences, enabling healthcare providers to tailor services that resonate with patient requirements and expectations.
2. Improvement in Care Quality
By identifying areas that need attention and improvement, healthcare providers can take targeted actions to enhance the quality of care, ensuring that it meets or exceeds patient expectations.
3. Strengthened Patient-Provider Relationship
Builds trust and promotes open communication by giving patients a voice in their healthcare experience, reinforcing mutual respect and collaboration.
4. Strategic Decision Making
Through insights gathered, healthcare administrators can make informed decisions regarding management strategies, resource allocation, and service enhancements, aligning them with patient needs and preferences.
5. Benchmarking Performance
The ability to compare performance with other facilities or industry standards helps set goals and identify areas where a facility can excel or needs improvement.
6. Increased Patient Retention
By understanding and addressing patient needs and preferences, healthcare providers can foster loyalty, ensuring that patients feel valued, heard, and cared for, encouraging continued patronage.
Commonly asked questions
Healthcare providers, including hospitals, clinics, and individual practitioners, commonly use Patient Satisfaction Questionnaires to understand and improve patient experiences.
These questionnaires are typically used after medical visits, surgeries, or treatments to collect patient care and satisfaction feedback.
Patient Satisfaction Questionnaires are distributed to patients for completion, and the responses are analyzed to understand patient perceptions, identify areas of strength and weakness, and make informed decisions for enhancing care quality.
Related Templates
New Patient Questionnaire
Download a comprehensive New Patient Form for accurate health assessment and personalized care.
Popular Templates
Medicare Eligibility Age Chart
Unlock key insights into Medicare eligibility with our detailed age chart and comprehensive guides, perfect for healthcare professionals and the public.
Coleman Block Test
Streamline the process of documentation during a Coleman Block Test with a patient by downloading our Coleman Block Test template today!
Appointment Schedule Template
Streamline scheduling process, optimize time management, and enhance productivity. Organize your appointment schedules with our Appointment Schedule Template.
Osteoporosis Care Plan
Developing an osteoporosis care plan is essential for managing this condition effectively. Download Carepatron's free PDF example to learn more.
Medicare Fact Sheet
Download a free Medicare Fact Sheet for your patients. Learn how Medicare works with our free template.
Antipsychotic Sedation Chart
Discover the essential functions of modern antipsychotic drugs, sedation charts, the benefits of medications, and how Carepatron enhances mental health treatment.
Conversation Skills Worksheet
Level up conversational abilities with our engaging Conversation Skills Worksheet. Practical exercises and goal-setting included. Download for free today!
Contingency Map
Understand and use Contingency Maps for behavior management in therapy, education, and parenting for improved decision-making.
Healthy and Unhealthy Food Worksheet
Download our free Healthy and Unhealthy Food Worksheet to help you identify nutritious choices and balance your diet. It includes a fun plate activity!
Diabetes Treatment Guidelines
Explore comprehensive Diabetes Treatment Guidelines for effective management and improved health outcomes.
Steinman Test
Learn about the Steinman Test, a diagnostic procedure for assessing shoulder stability and potential issues, in healthcare.
Medical Spa Business Plan
Discover how to launch and grow your medical spa with our comprehensive business plan guide. Tips, templates, and strategic insights for success.
PTSD Dissociation Test
Assess PTSD dissociation symptoms with Carepatron's free PDF download containing a test and examples for evaluation. Get insights and guidance on recognizing symptoms.
Medical Billing and Coding Practice Worksheets
Enhance medical billing & coding skills with our practice worksheets! Perfect for training & mastering critical concepts. Start learning today!
CVC Checklist
Discover an essential CVC checklist for efficient business operations. Streamline your processes and enhance productivity with our comprehensive guide.
Massage Therapy Invoice Template
Get access to a free Massage Therapy Invoice Template with Carepatron. Streamline your documentation and invoicing process with our PDF.
Ankle Injury Diagnosis Chart
Learn more about ankle injuries and have a step-by-step guide on diagnosing them with our free ankle injury diagnosis chart template.
Health Triangle Worksheets
Explore and improve your well-being across physical, mental, and social health with our comprehensive Health Triangle Worksheets.
Cholecystitis Treatment Guidelines
Explore our Cholecystitis Treatment Guidelines for managing acute conditions. Download the PDF now.
Schizophrenia Treatment Guidelines
Discover the latest Schizophrenia Treatment Guidelines, including antipsychotic medication, psychosocial interventions, and cognitive behavioral therapy.
Breast Cancer Treatment Guidelines
Explore comprehensive Breast Cancer Treatment Guidelines for informed decisions. Learn about the latest protocols and options for adequate care.
Rheumatoid Arthritis Diagnosis Criteria
Learn about the essential Rheumatoid Arthritis Diagnosis Criteria for accurate identification and timely treatment in healthcare.
Face Sheet (Medical)
Explore the benefits of using a medical face sheet for efficient patient care, including quick patient data access and insurance verification.
Medicare 8-minute Rule Chart
Master the Medicare 8-Minute Rule with our comprehensive chart and guide. Simplify billing for time-based therapy services and maximize reimbursement.
Cataract Evaluation
Streamline your Cataract Evaluation process by using our template for documentation. Download for free today!
Wheelchair Evaluation
Download our Wheelchair Evaluation template to streamlines the documentation process through a evaluation of clients' mobility and seating needs.
Pediatric BMI Chart
Download our Pediatric BMI Chart for a resource that can assist you in assessing and documenting a child's weight status.
Medical Fishbone Diagram
Explore the Medical Fishbone Diagram to identify the causes of healthcare issues with our free PDF template. Streamline problem-solving in clinical settings.
Navicular Stress Fracture Test
Explore diagnosis and treatment for navicular stress fractures with our free guide on tests, symptoms, and recovery strategies.
Triphasic BBT Chart
Discover how a Triphasic BBT Chart can help track fertility and early pregnancy signs. Download our free PDF for insights and examples.
Scaphoid Fracture Test
Explore the essential aspects of scaphoid fractures, including symptoms, risk factors, and treatments. Access our free Scaphoid Fracture Test PDF for better patient care.
Health Anxiety CBT Worksheets
Overcome health anxiety with our CBT worksheets designed to help you understand and manage your fears. Download our free example today.
Female Acupuncture Points Chart
Explore our Female Acupuncture Points Chart for a comprehensive guide on key acupuncture points and meridians to enhance women's health treatments.
Musculoskeletal Examination Checklist
Explore a comprehensive guide on musculoskeletal system examination, conditions, treatments, and FAQs with a free checklist PDF download.
Pain Management Coding Cheat Sheet
Streamline your medical billing and coding for pain management with our comprehensive cheat sheet. Download our free PDF today.
Massage Therapy Business Plan
Creating a massage therapy business plan? Download Carepatron's free PDF to guide you through the process and help you create a successful massage therapy business plan.
Food and Symptom Diary PDF
Track your food intake and symptoms on a symptom-free day with our convenient Food and Symptom Diary PDF report. Monitor your health quickly and effectively.
Newborn Exam Template
Streamline newborn examinations with our comprehensive template, ensuring thorough newborn assessment and care. Download now!
Learning Needs Assessment Nursing
Unleash your full potential! Master nursing skills & knowledge with Carepatron's LNA guide. Boost patient care & career growth.
Hypochondria Test
Explore our guide on illness anxiety disorder: signs, impact, and treatments. Download a free Hypochondria Test to start your journey to better health.
Binocular Vision Test
Carepatron's free PDF download provides a binocular vision test example that you can use to assess your vision. Learn more about binocular vision and how to conduct the test effectively.
Radical Forgiveness Worksheet
Unlock the power of Radical Forgiveness with our comprehensive worksheet. Guide your patients to healing and transformation with our template and guide.
PASS Assessment
Explore the use of a specialized test to assess postural control among stroke patients to craft a more targeted rehabilitation plan.
Eden's Test
Discover the significance of Eden's Test in diagnosing thoracic outlet syndrome. Learn how this maneuver aids in identifying neurovascular compression.
Esthetician Business Plan
Crafting an Esthetician Business Plan is crucial for success. Download Carepatron's free PDF to guide you in creating your own professional business plan.
Test for Muscle Weakness
Learn how to determine muscle weakness with Carepatron's free PDF download and example. This resource provides valuable information on assessing muscle strength and functionality.
Healthcare Marketing Plan
Download Carepatron's comprehensive Healthcare Marketing Plan PDF, which helps create a successful strategy that drives patient engagement, trust, and growth for your organization.
Hearing Aid Evaluation
Learn how to conduct a thorough hearing aid evaluation with our free PDF download. This comprehensive guide includes examples and tips for success.
Action Planning Worksheet
Maximize project success with our Action Planning Worksheet. Track and measure progress effectively. Download free templates for complete project management.
Pharmacy Technician Worksheets
Unlock pharmacy tech skills with our free worksheets for exam prep, skill refreshment, and practical knowledge. Download now.
Type 2 Diabetes Treatment Guidelines
Get comprehensive guidelines and examples for treating Type 2 Diabetes in Carepatron's free PDF download.
Pain Management Treatment
Discover effective pain management treatments and examples through Carepatron's free PDF download. Learn about various strategies to alleviate pain and improve your quality of life.
Therapy Invoice Template
Our Therapy Invoice Template streamlines billing processes, enhances professionalism, and effortlessly keeps you organized. Download now!
Muscle Test
Discover everything you need to know about muscle testing, examples, and Carepatron's free PDF download to help you better understand this technique.
Pisiform Fracture Test
Learn how to conduct the Pisiform Fracture Test. Get a free PDF template to record results and streamline your documentation.
90-90 Hamstring Test
Learn how to perform the 90-90 Hamstring Test. Access a free PDF template and example here.
Overhead Squat Assessment
Get access to a free Overhead Squat Assessment template. Learn how to perform this test and interpret the results.
Osteoarthritis Diagnosis Criteria
Understand the signs, causes, and effective criteria for diagnosis. Download our free PDF example for a detailed understanding.
Cervical Flexion Rotation Test
Discover the Cervical Flexion Rotation Test for assessing upper cervical spine dysfunction, ideal for diagnosing cervicogenic headaches and neck issues.
Norton Scale
Learn about the Norton Scale, a tool used in healthcare to assess the risk of pressure ulcers. Understand its significance and application.
Medical Diagnosis Form
This form helps healthcare professionals gather patient information for accurate diagnosis. Download a free medical diagnosis form template.
IFS Treatment Plan
Download Carepatron's free PDF example of an Internal Family Systems (IFS) treatment plan. Learn how to create a comprehensive treatment plan using IFS therapy techniques.
Beers Criteria Template
Explore the Beers Criteria Template, guiding principles for safer medication use in older adults—essential knowledge for healthcare professionals.
Non-Medical Home Care Assessment Form PDF
Download, print, and fill out our Non-Medical Home Care Assessment Form PDF for thorough evaluation and personalized care plans. Streamline your caregiving process today!
Miracle Question Worksheet
Use a helpful tool when practicing solution-focused therapy to engage and build motivation among clients. Download your free PDF here.
Premenstrual Dysphoric Disorder DSM-5
Explore the criteria of Premenstrual Dysphoric Disorder (PMDD) as outlined in DSM-5, shedding light on panic disorder and its impact on mental health.
AC Joint Test
Explore AC Joint Test procedures, results interpretation, and next steps for managing injuries like AC joint separation and arthritis.
Discover the ins and outs of the PVD Test with our comprehensive guide and template. Learn about its purpose, procedure, risks, and more.
Stinking Thinking Worksheet
Download our Stinking Thinking Worksheet to help clients challenge negative thoughts and cognitive distortions.
Snapping Hip Test
Gain access to an essential resource, the Snapping Hip Test, to assist you in diagnosing a snapping hip during physical assessments. Download today!
R Worksheets for Speech Therapy
Enhance your speech therapy sessions with R Worksheets, designed to improve articulation skills. Download the free PDF sample today!
Hip Quadrant Test
Learn how detailed records promote quality of care for patients with hip pathologies. Download our Hip Quadrant Test to document the process.
Multiple Sclerosis Test
Discover the symptoms, causes, diagnosis, and treatment options for Multiple Sclerosis and understand comprehensive care approaches.
MCL Injury Test
Discover key insights on MCL injuries, from symptoms and diagnosis to recovery. Get expert advice for effective treatment and healing.
Dermatomyositis Diagnosis Criteria
Learn about the diagnostic criteria for dermatomyositis and see an example with Carepatron's free PDF download. Get the information you need to understand this condition.
Hip Mobility Test
Learn how to assess your hip mobility with a simple test. Download Carepatron's free PDF guide with examples to improve hip flexibility and function.
Massage Chart
Explore our comprehensive Massage Chart for holistic healthcare solutions and techniques. Perfect for practitioners and enthusiasts alike!
Occupational Therapy Acute Care Cheat Sheet
Streamline patient recovery with key strategies for enhancing independence in acute settings. Download our free Occupational Therapy Acute Care Cheat Sheet.
Neck Pain Chart
Explore our comprehensive Neck Pain Chart for insights into causes, symptoms, and treatments. Find relief and understanding today.
School Readiness Assessment
Discover the benefits of our School Readiness Assessment template with a free PDF download to ensure children are prepared for kindergarten through grade three.
Sedation Scale Nursing (Ramsay Sedation Scale)
Discover key sedation scales used in nursing, including RASS and Ramsay Scale, for accurate patient sedation assessment in critical care settings.
Blood Tests for Lupus
Download a free Blood Tests for Lupus template. Learn the various types of tests used to diagnose this disease.
Neurological Exam Template
Discover the importance of neurological assessments for diagnosing and monitoring conditions with our comprehensive guide and template. templates
Homeopathic Dosage Chart
Discover the principles of homeopathy, dosage guidelines, and effectiveness, with references and a downloadable chart for practical use.
Gout Diagnosis Criteria
Uncover the essential Gout Diagnosis Criteria here, including symptoms, diagnostic tests, and the American College of Rheumatology guidelines.
Peroneal Tendon Tear Test
Learn about the Peroneal Tendon Tear Test and use our template to record results!
Ear Seeds Placement Chart
Learn what ear seeds are and download our Ear Seeds Placement Chart template!
Global Rating of Change Scale
Explore the Global Rating of Change Scale, a key tool to assess the clinical significance of patient-reported outcomes. Get your free PDF template now.
Physical Therapy Initial Evaluation
Unlock the benefits of Physical Therapy Initial Evaluation: a key step in personalized treatment planning for improved mobility and pain relief.
8-Week Group Counseling Plan
Discover a flexible template for creating effective 8-Week Group Counseling Plans, tailored to meet diverse needs and foster growth.
Osteoarthritis Treatment Guidelines
Learn about the management of osteoarthritis, treatments, causes, and care strategies. Access tips for managing symptoms and improving quality of life in our guide.
Prone Knee Bend Test
Learn about the Prone Knee Bend Test and how it assesses radicular pain.
PTSD Treatment Guidelines
Download our PTSD Treatment Guidelines template to access evidence-based treatment plans, diagnostic tools, and personalized care strategies.
Assess alcohol use with AUDIT-C: quick, accurate alcohol screening tests for hazardous drinking. Learn your risk level in minutes. Download our free template now!
Cincinnati Stroke Scale Scoring
Learn to quickly identify stroke symptoms with the Cincinnati Stroke Scale Scoring guide, which is essential for emergency responders and healthcare professionals.
Lupus Diagnosis Criteria
Download a helpful checklist tool to help diagnose lupus among patients for early identification and intervention. Access your free resource here!
Quadriceps Strain Test
Get access to a free Quadriceps Strain Test template. Learn how to interpret results and streamline your documentation with a free PDF.
Dysarthria Treatment Exercises
Discover effective dysarthria exercises to improve speech clarity. Download our free guide for tailored speech therapy techniques.
Antisocial Personality Disorder Test
Use a helpful evidence-based Antisocial Personality Disorder Test to identify ASPD symptoms among clients and improve health outcomes.
Persistent Depressive Disorder Test
Explore an evidence-based screening tool to help diagnose persistent depressive disorder among clients.
Normal Blood Sugar Levels Chart
Understand how a Normal Blood Sugar Levels Chart works. Get access to a free PDF template and example in this guide.
Height Weight Charts
Learn about height-weight charts and their use in healthcare practice. Find out your ideal weight and stay healthy!
Glasgow Coma Scale
The Glasgow Coma Scale (GCS) dates back to the 1970s and has become one of the most widely accepted measurements of impairment following brain injury. What better way to start using the GCS in your practice than with Carepatron’s free PDF GCS template download.
A1C Goals By Age Chart
Use our free A1C Goals by Age Chart to learn the recommended A1C goal for people of different ages. Download our free PDF and example here.
Medical Review Of Systems
Looking for a medical review of systems template and example? Download Carepatron’s free guide for a comprehensive medical review template and samples!
Ophthalmologic Exam
Check your patient's eye health and record their results using our ophthalmologic exam templates. Click here for a copy and a guide on how to use it.
Autoimmune Paleo Diet Food
Streamline your Autoimmune Paleo Diet with our comprehensive food list. Ideal for managing autoimmune conditions. Download the PDF now!
Neurological Examination Checklist
Optimize neurological assessments with our streamlined Neurological Examination Checklist Template.
Nurse Note Template
Get a head start every time you take notes for your patients and improve your time management with our free PDF nurse note template.
Discover the importance of Hematocrit tests in healthcare. Learn about uses, results, and more. Stay informed with our Hematocrit Test guide.
VA Disability Rating Chart
Download a free PDF template of a VA disability rating chart and an example to help you understand and track your VA disability ratings.
HGB A1C Conversion Chart
Efficiently convert HGB A1C values with our user-friendly HGB A1C Conversion Chart. Simplify diabetes management. Download PDF now.
Join 10,000+ teams using Carepatron to be more productive
Calculates the ROI of investing in our queuing and self-service solutions Learn More
Unlock the full potential of our solutions!
- What is Patient Experience & Why It Is Importance ?
A Comprehensive Guide to Patient Journey Mapping
- Author: Wavetec
- Published: January 26, 2024
Is regulating patient experience at your healthcare service a challenging task? If your patients leave the hospital unsatisfied with the service, we have a solution for you!
Patient journey mapping is vital in understanding your patient’s experience at every step of interaction with the hospital, whether virtual or physical. This allows you to empathize with your patients, facilitate their experience, and contribute in uncertain and stressful times.
Parallel to the patient’s journey, healthcare systems face increasing challenges in patient management, regulating space constraints, limiting healthcare providers, and budgeting. By mapping the patient journey , you can pinpoint the shortfalls in your management services, improve facilities, and increase patient turnout.
The patient journey map must be curated in detail, accounting for various touchpoints and patient perceptions. The most accurate method of measuring healthcare quality is pairing patient journey maps with patient satisfaction scores, such as the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAPHPS) and a Net Promoter Score (NPS) .
Higher scores speak volumes about your healthcare services, increase patient retention, and promise returns.
What is Patient Journey Mapping?
Patient Journey Mapping is a strategic tool in healthcare that visually illustrates the entire patient experience, from initial contact to post-treatment follow-up. It involves mapping out key touchpoints and stages, such as appointment scheduling, diagnosis, treatment, and aftercare.
This process allows healthcare providers to understand the patient’s pathway through the healthcare system comprehensively.
Amidst the changing landscape of the healthcare industry, patients look for service providers that offer a personalized experience. Besides renowned healthcare providers, patients look for a human-centric environment that provides timely and efficient services.
Moreover, modern consumer requirements demand a digital transformation of healthcare services.
Healthcare managers can use patient journey maps to visualize the blind spots and pain points in a patient’s experience. A distinguished healthcare service sees journey mapping as a powerful tool that tells about a patient’s well-being and connects care providers with their emotional journeys.
You can make your practices to be more empathetic and make a difficult journey seamless.
The Benefits of Patient Journey Mapping
Investing in patient experience mapping carries benefits for both parties, care providers and patients. We have highlighted some benefits of journey mapping below:
Improved patient communication
Identifying unaddressed patient issues helps build a connection with the patient. Keeping them at the model’s center and informing them of changes before their visit reduces frustration and confusion.
Continuous patient care
With a streamlined workflow, staff members and care providers can remove uncertainties from a patient’s care journey. An integrated healthcare system removes loopholes, such as overbooked appointments, which otherwise lead to negative patient feelings.
Personalized care
Given the nature of the treatment plans and services offered by the healthcare industry, a one-shoe-fits-all theory does not apply to the consumers. By integrating patient data with business models, you can provide a customized experience to the patients.
Turn-out increases when patients receive automated appointment reminders and physician availability updates.
Improved Efficiency
Patient journey maps identify the demand for time management and sensitivity in healthcare. Feasibility arrangements such as pre-booking appointments, receiving digital laboratory reports, and online consultations boost patient satisfaction.
Patient retention and profitability
Patient feedback is crucial to introducing or revising policies, growth opportunities, and consistent revenues.

Seamless Patient Journey
With our intuitive interface, patients can easily register, check-in, and monitor their queue status. This reduces their anxiety, improves their overall experience, and fosters a positive perception of your healthcare facility.
7 Key Stages in the Patient Journey
Patient journey mapping differs for each hospital or clinic, depending on the care level. Most tertiary care hospitals identify three key stages when patients experience mapping .
Touchpoints of each step may differ slightly in pregnancies, emergency services, and outpatient departments.
Let’s read about the details of each stage below:
1. Awareness:
- This stage often begins with recognizing symptoms, changes in health, or routine checkups revealing potential issues.
- Patients may notice something is amiss, prompting them to seek further information or professional advice.
2. Consideration:
- Information gathering kicks into high gear. Patients may research their symptoms, explore potential causes, and consider various treatment options.
- Seeking advice from healthcare professionals, friends, or family members becomes a key part of this stage.
3. Decision:
- Armed with information, patients make decisions about their course of action. This could involve choosing a specific healthcare provider, deciding on a treatment plan, or committing to lifestyle changes.
- The decision-making process may also involve discussions with healthcare professionals to ensure alignment with the patient’s values and preferences.
4. Engagement:
- This is the active phase, where patients interact with healthcare providers, undergo diagnostic tests, and initiate the chosen treatment plan.
- Open communication between the patient and the healthcare team is crucial during this stage to address concerns, clarify expectations, and ensure a collaborative approach.
5. Treatment and Recovery:
- The chosen treatment plan is implemented, whether it’s medication, surgery, therapy, or a combination of interventions.
- Recovery involves monitoring progress, managing potential side effects, and adapting the treatment plan as needed.
6. Follow-Up and Maintenance:
- Post-treatment, patients often enter a phase of follow-up care. This can include regular check-ups, monitoring for recurrence, and adjusting treatment plans as necessary.
- Lifestyle changes and ongoing self-care may be emphasized to maintain health and prevent future issues.
7. End-of-Life Care (if applicable):
- In cases of terminal illness, this stage involves compassionate and supportive care. Palliative care aims to enhance quality of life, manage symptoms, and provide emotional and spiritual support.
- This stage emphasizes open communication about end-of-life preferences and ensures a dignified and comfortable experience for the patient and their loved ones.
Analyzing the Patient Journey Map
Once you have designed a patient journey map for your service, the correct way of utilizing the maps is to identify the pain points. Next, we enlist and discuss some common hurdles patients face that delay prompt care, including internal and external factors or barriers to healthcare.
1- Pre-visit
- The patient feels anxious about the medical condition.
- The website needs more information about the healthcare facility to make patients satisfied. Your website must be SEO-friendly and listed on Google to regulate patient management.
- During this stage, missed phone calls and confusing appointment scheduling tasks lead to care provision delays.
- Limited communication with consultants before visiting
2- At the healthcare facility
- Filling out the pre-appointment questionnaire is time-consuming and makes patients uneasy.
- Lengthy waiting times and mismanaged queues for appointments reduces patient satisfaction. Patients waiting at the facility can be guided using digital signage that communicates announcements, turns, and navigates around the healthcare facility.
- Explaining old symptoms and information to the same care provider at every visit frustrates patients.
3- Post-treatment plan
- Billing and initiating the hospital discharge process is often tedious.
- Receiving feedback from patients to measure patient satisfaction.
- Unable to monitor the patient at home and set up follow-up appointments creates mistrust between the patient and the doctor.
Gain valuable insights
Leverage our healthcare queue management system’s data to make informed decisions to improve the patient experience. We have seen up to a 35% increase in patient satisfaction.
Patient Journey Mapping Template
We have designed templates of patient journey maps to help you make the best one for your hospital system. As shown in the samples, patients visiting different departments have specific touchpoints. For example, a patient scheduling his appointment for the outpatient department will research the clinic and the primary caregiver.

However, the primary concern for patients requiring urgent care will be prompt ambulance services and treatment. Despite the differences, all patient journey maps are based on three key stages: pre-hospital care, in-hospital care, and post-treatment plans.

Patient Journey Improvement Solutions
If you want to enhance patient flow management and boost patient satisfaction at your hospital, we recommend using pre-engineered solutions. There are many ways to improve the quality of service you provide to your patients.
One such solution is the Wavetec patient flow system. Adopting a digital healthcare system can optimize patient-doctor interaction and improve investment returns.
We have put together the most impactful solutions your facility can sign-up for each stage of the patient journey map. Here’s what they are:
- Online appointment and booking
- Queue management – People counting, WhatsApp Queuing, Queue management applications, Digital Signage
- Patient application
- Self-check-in kiosks
- Integrated manager dashboards and analytics
- Customer feedback reports
- Curbside pickups
Let’s learn about each solution and how it will benefit your healthcare center.
1. Simplify Online Appointment Booking

Before visiting the facility, patients can schedule online appointments and ticketing on the website or patient application with their preferred physician. This service allows your patients to book seamlessly, check-in and receive wait time or canceled appointment notifications. Satisfying your customer before they arrive mitigates their already-high worry levels.
2. Patient Management

Waiting in queues for examination rooms and healthcare providers is a major source of concern for patients. You can reduce perceived wait times by giving patients a virtual waiting room. This can be done by signing up for WhatsApp Queuing and the Queue Management Mobile App. These services give patients virtual tickets and wait time notifications, allowing them to manage time effectively.

Walk-in patients and patients with pre-booked appointments can also use automated, self-service kiosks at the facility to check in or reschedule appointments. Patients can scan the displayed QR code or use biometrics technology to receive tickets via SMS, Email or WhatsApp.
You can manage the patient count in the waiting area using a real-time counter and digital signage . This helps emergency case patients to navigate the hospital without confusion.
3. Promoting Patient Satisfaction
Many patients must visit the healthcare facility multiple times to collect laboratory reports, prescriptions, and medications. You can facilitate this tedious process by providing delivery and curbside pickup options. This regulates unnecessary traffic at your hospital and saves time for patients.

Investing in Patient Applications is a great marketing tool and a one-stop solution to patient worries. Individuals can learn more about your facility’s services, access laboratory reports, initiate billing, and receive updates and reminder notifications. This is particularly useful in conducting telehealth rotations with expecting mothers and palliative care patients who cannot visit the facility often.
4. Patient Feedback

Receiving your consumer’s feedback and solving their queries ensures a successful approach to patient journey mapping. Wavetec has designed a customer feedback solution to measure customer satisfaction and follow up on your staff’s performance.
Additionally, you can get a management portal for the hospital staff and care providers. This can be integrated with patient data to give healthcare providers complete information.
Softwares such as Spectra include dashboard analytics and reports on the performance of each department to help you identify the shortfalls. This will help you build a congregated team that runs operations smoothly in the patient’s best interest.
Studies have shown that facilities using solution experience up to a 50% decrease in missed appointments, optimizing resource utilization and increasing revenue.
The modern healthcare system requires providers to be more involved in providing a seamless patient experience. In this blog, we highlight the role of patient journey mapping to help you identify touchpoints in a patient’s journey. Before, during, and after treatment, it is crucial to comprehend the patient’s viewpoint to ensure proper care.
Patient journey solutions are, therefore, integral in distinguishing your healthcare facility. Investing in patient applications, queue management software, receiving customer feedback, and analyzing it is vital in improving your standing.
Adopt our solutions, transform the healthcare industry, and make your approach more empathetic!
- No translations available for this page
Patient journey 101: Definition, benefits, and strategies
Last updated
22 August 2023
Reviewed by
Melissa Udekwu, BSN., RN., LNC
Today’s patients are highly informed and empowered. They know they have choices in their healthcare, which can put healthcare providers under a lot of pressure to provide solutions and meet their patients’ expectations.
Just like any customer, patients embark on a journey that begins before they ever contact the provider. This makes understanding the journey and where improvements can be made extremely important. Mapping the patient journey can help practitioners provide better care, retain a solid customer base, and ultimately identify ways to improve patient health.
- What is the patient journey?
The patient journey is best described as the sequence of experiences a patient has from admission to discharge. This includes all the touchpoints between the patient and provider from beginning to end.
The patient journey continues through consultation, where they meet the potential caregiver. That portion of the journey includes interactions with a doctor and support staff, how long they wait to be seen, and the steps taken for diagnosis and treatment.
The patient’s post-care journey includes follow-ups from the healthcare provider, post-treatment care, and billing. For example, if the patient has questions about post-surgery care or how to read their invoice, how quickly their questions are answered and their problems resolved will impact their satisfaction.
Mapping the patient journey helps healthcare providers improve patient satisfaction at every step of the way. By collecting data at each stage and conducting an in-depth analysis, providers can identify patient concerns and make the necessary improvements to meet their patient satisfaction goals.
What is another name for the patient journey?
The term “patient funnel” describes the journey patients take from first learning about a healthcare provider or healthcare product to actually making an appointment or purchase. This “funnel” can be applied to any type of business, describing the stages a customer goes through to obtain a service.
- Understanding the stages of the patient journey
Each stage of the patient journey is essential to a positive patient experience . Gathering and analyzing data can alert healthcare providers to potential issues throughout the journey.
Data collection at each of the following stages will give healthcare providers the information they need to make the necessary improvements:
1. Awareness
Awareness is where the patient journey begins. This is when they first research symptoms and identify the need to see a medical professional.
They may consider at-home remedies and get advice from friends, social media, or websites. Once they identify the need for a healthcare provider, they continue their research via review sites, advertising campaigns, and seeking referrals from friends and family.
Determining the way patients become aware they need healthcare and the sources they use for research is important. The data collected at this stage could suggest your organization has an insufficient social media presence, inadequate advertising, or a website in need of an update.
To remedy these shortcomings, you might consider adding informational blogs to your website, performing a social media analysis, or closely monitoring customer reviews.
This stage in the patient journey is where the patient schedules services with the healthcare provider.
This engagement is essential for acquiring new patients and retaining current patients. Patients will contact you in several ways to schedule an appointment or get information. Most will call on the first attempt to schedule an appointment.
This is a crucial touchpoint in the journey. A new patient may become frustrated and move on if they find it difficult to access your services or are placed on hold for a long period or transferred numerous times.
Patient engagement occurs in other ways, such as your online patient portal, text messages, and emails. Your patients may interact differently, so it’s important to gather data that represents their preferred means of communication. Work to make the improvements required to correct access issues and ensure efficient communication.
The care stage can include everything from your patient’s interaction with the front desk to how long they have to wait in the examination room to see a doctor.
Check-in, check-out, admissions, discharge, billing, and of course, the actual visit with the healthcare provider are other touchpoints in the care stage.
There are a couple of ways to gather and analyze this data. Most organizations choose to analyze it holistically, even if it’s collected separately. For example, you might gather data about the patient’s interaction with the front desk, the clinical visit, and the discharge process, but you may want to analyze the care segment as a whole.
4. Treatment
Treatment may be administered in the office. For example, a patient diagnosed with hypertension may have medication prescribed. That medication is the treatment. Gathering information at this stage is critical to see how your patient views the healthcare provider’s follow-up or responses to inquiries.
In most cases, treatment extends beyond the initial clinical visit. For example, a patient might require additional tests to get a diagnosis. Providing the next steps to a patient in a timely manner and letting them know the test results is crucial to patient satisfaction .
5. Long term
A satisfied patient results in a long-term relationship and referrals to friends and family. Most of the data collected at this stage will be positive since the patient is continuing to use your services.
Gathering data after the treatment stage allows you to expand on the qualities that keep patients returning for your services in the long term.
- Benefits of patient journey mapping
The patient benefits from their healthcare provider understanding their journey and taking steps to improve it. Healthcare providers also reap several benefits, including the following:
1. Efficient patient care
When they understand the patient journey, healthcare providers can provide care more efficiently and spend less time and money on unnecessary, unwanted communications.
2. Proactive patient care
Proactive patient care is aimed at preventing rather than treating disease. For example, women who are over a certain age should have an annual mammogram, smokers may be tested for lung disease, and elderly women may need a bone density study. These preventative measures can help keep disease at bay, improve health outcomes, and build trust with patients.
3. Value-based patient care
Patients don’t want to feel they are being charged unfairly for their healthcare. Focusing on the individual patient promotes satisfaction and yields positive outcomes.
The Center for Medicare and Medicaid Services (CMS) has issued recent guidelines for participants that help offset the costs of high-quality care through a reward system.
4. Retention and referrals
Patients who are happy with their journey will keep returning for healthcare, and happy patients equal voluntary referrals. Many providers offer rewards to incentify referrals.
- How to get started with patient journey mapping
Follow the steps below to start the patient journey mapping process:
Establish your patient personas
Journey mapping is a great way to identify your patient’s characteristics so that their experience can be further enhanced.
Some of the following determinations can help you pinpoint your patient’s persona and establish protocols to provide a better service:
How do your patients prefer to communicate? Are they more comfortable with phone calls, texts, or other methods?
How are most patients finding your services? Are they being referred by friends or family members, or are they seeing advertisements?
Would the patient prefer in-person communication or telecommunication?
What are the patient’s expectations of care?
This data can be complex and widespread, but it can give you the information you need to more effectively and efficiently communicate with your patients.
Understand the entire patient lifecycle
Each patient is unique. Understanding the patient lifecycle can avoid confusion and miscommunication.
To positively engage the patient, you’ll need to gather data not only about communication methods but where they are in the patient journey, their health issue, and their familiarity with the healthcare provider’s procedures and treatment options.
Understand the moments of truth
With a few exceptions, most people seek healthcare services when they are ill or have a healthcare issue. These situations can cause patients to feel stressed and anxious. It’s these moments of interaction where compassion, knowledge, and understanding can provide relief and reassurance.
When patients see their healthcare provider, they are looking for solutions to problems. It’s the provider’s opportunity to identify these moments of truth and capitalize on them.
Get the data you need
Healthcare providers can collect vast amounts of data from patients, but the data collected rarely goes far enough in analyzing and determining solutions.
Your patients have high expectations regarding personalized treatment based on data. They want personalized, easy access to medical information and records, responsive treatments and follow-up, and communication in their preferred format.
You need more than clinical data to give patients what they want. You also need personal data that sets each patient apart and ensures a tailored experience.
For example, it might be challenging for parents of small children to contact the clinic and schedule appointments at certain times of the day. As a healthcare provider, you’ll need to be aware of the best times to contact this individual and offer simple methods for scheduling appointments.
Another example is patients with physical disabilities. You can take steps to improve their access to and experience at the healthcare facility.
Encourage referrals and loyalty
Although engagement on social media and online forums is becoming more and more common, the best way for new patients to find you is through referrals. Referrals stem from satisfactory experiences and trust.
Get started today
Go from raw data to valuable insights with a flexible research platform
Editor’s picks
Last updated: 27 June 2023
Last updated: 22 July 2023
Last updated: 11 September 2023
Last updated: 10 October 2023
Last updated: 16 November 2023
Last updated: 28 September 2023
Last updated: 12 October 2023
Last updated: 25 November 2023
Last updated: 3 July 2023
Last updated: 27 January 2024
Latest articles
Related topics, log in or sign up.
Get started for free
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Process mapping the...
Process mapping the patient journey: an introduction
- Related content
- Peer review
- Timothy M Trebble , consultant gastroenterologist 1 ,
- Navjyot Hansi , CMT 2 1 ,
- Theresa Hydes , CMT 1 1 ,
- Melissa A Smith , specialist registrar 2 ,
- Marc Baker , senior faculty member 3
- 1 Department of Gastroenterology, Portsmouth Hospitals Trust, Portsmouth PO6 3LY
- 2 Department of Gastroenterology, Guy’s and St Thomas’ NHS Foundation Trust, London
- 3 Lean Enterprise Academy, Ross-on-Wye, Hertfordshire
- Correspondence to: T M Trebble tim.trebble{at}porthosp.nhs.uk
- Accepted 15 July 2010
Process mapping enables the reconfiguring of the patient journey from the patient’s perspective in order to improve quality of care and release resources. This paper provides a practical framework for using this versatile and simple technique in hospital.
Healthcare process mapping is a new and important form of clinical audit that examines how we manage the patient journey, using the patient’s perspective to identify problems and suggest improvements. 1 2 We outline the steps involved in mapping the patient’s journey, as we believe that a basic understanding of this versatile and simple technique, and when and how to use it, is valuable to clinicians who are developing clinical services.
What information does process mapping provide and what is it used for?
Process mapping allows us to “see” and understand the patient’s experience 3 by separating the management of a specific condition or treatment into a series of consecutive events or steps (activities, interventions, or staff interactions, for example). The sequence of these steps between two points (from admission to the accident and emergency department to discharge from the ward) can be viewed as a patient pathway or process of care. 4
Improving the patient pathway involves the coordination of multidisciplinary practice, aiming to maximise clinical efficacy and efficiency by eliminating ineffective and unnecessary care. 5 The data provided by process mapping can be used to redesign the patient pathway 4 6 to improve the quality or efficiency of clinical management and to alter the focus of care towards activities most valued by the patient.
Process mapping has shown clinical benefit across a variety of specialties, multidisciplinary teams, and healthcare systems. 7 8 9 The NHS Institute for Innovation and Improvement proposes a range of practical benefits using this approach (box 1). 6
Box 1 Benefits of process mapping 6
A starting point for an improvement project specific for your own place of work
Creating a culture of ownership, responsibility and accountability for your team
Illustrates a patient pathway or process, understanding it from a patient’s perspective
An aid to plan changes more effectively
Collecting ideas, often from staff who understand the system but who rarely contribute to change
An interactive event that engages staff
An end product (a process map) that is easy to understand and highly visual
Several management systems are available to support process mapping and pathway redesign. 10 11 A common technique, derived originally from the Japanese car maker Toyota, is known as lean thinking transformation. 3 12 This considers each step in a patient pathway in terms of the relative contribution towards the patient’s outcome, taken from the patient’s perspective: it improves the patient’s health, wellbeing, and experience (value adding) or it does not (non-value or “waste”) (box 2). 14 15 16
Box 2 The eight types of waste in health care 13
Defects —Drug prescription errors; incomplete surgical equipment
Overproduction —Inappropriate scheduling
Transportation —Distance between related departments
Waiting —By patients or staff
Inventory —Excess stores, that expire
Motion —Poor ergonomics
Overprocessing —A sledgehammer to crack a nut
Human potential —Not making the most of staff skills
Process mapping can be used to identify and characterise value and non-value steps in the patient pathway (also known as value stream mapping). Using lean thinking transformation to redesign the pathway aims to enhance the contribution of value steps and remove non-value steps. 17 In most processes, non-value steps account for nine times more effort than steps that add value. 18
Reviewing the patient journey is always beneficial, and therefore a process mapping exercise can be undertaken at any time. However, common indications include a need to improve patients’ satisfaction or quality or financial aspects of a particular clinical service.
How to organise a process mapping exercise
Process mapping requires a planned approach, as even apparently straightforward patient journeys can be complex, with many interdependent steps. 4 A process mapping exercise should be an enjoyable and creative experience for staff. In common with other audit techniques, it must avoid being confrontational or judgmental or used to “name, shame, and blame.” 8 19
Preparation and planning
A good first step is to form a team of four or five key staff, ideally including a member with previous experience of lean thinking transformation. The group should decide on a plan for the project and its scope; this can be visualised by using a flow diagram (fig 1 ⇓ ). Producing a rough initial draft of the patient journey can be useful for providing an overview of the exercise.
Fig 1 Steps involved in a process mapping exercise
- Download figure
- Open in new tab
- Download powerpoint
The medical literature or questionnaire studies of patients’ expectations and outcomes should be reviewed to identify value adding steps involved in the management of the clinical condition or intervention from the patient’s perspective. 1 3
Data collection
Data collection should include information on each step under routine clinical circumstances in the usual clinical environment. Information is needed on waiting episodes and bottlenecks (any step within the patient pathway that slows the overall rate of a patient’s progress, normally through reduced capacity or availability 20 ). Using estimates of minimum and maximum time for each step reduces the influence of day to day variations that may skew the data. Limiting the number of steps (to below 60) aids subsequent analysis.
The techniques used for data collection (table 1 ⇓ ) each have advantages and disadvantages; a combination of approaches can be applied, contributing different qualitative or quantitative information. The commonly used technique of walking the patient journey includes interviews with patients and staff and direct observation of the patient journey and clinical environment. It allows the investigator to “see” the patient journey at first hand. Involving junior (or student) doctors or nurses as interviewers may increase the openness of opinions from staff, and time needed for data collection can be reduced by allotting members of the team to investigate different stages in the patient’s journey.
Data collection in process mapping
- View inline
Mapping the information
The process map should comprehensively represent the patient journey. It is common practice to draw the map by hand onto paper (often several metres long), either directly or on repositionable notes (fig 2 ⇓ ).
Fig 2 Section of a current state map of the endoscopy patient journey
Information relating to the steps or representing movement of information (request forms, results, etc) can be added. It is useful to obtain any missing information at this stage, either from staff within the meeting or by revisiting the clinical environment.
Analysing the data and problem solving
The map can be analysed by using a series of simple questions (box 3). The additional information can be added to the process map for visual representation. This can be helped by producing a workflow diagram—a map of the clinical environment, including information on patient, staff, and information movement (fig 3 ⇓ ). 18
Box 3 How to analyse a process map 6
How many steps are involved?
How many staff-staff interactions (handoffs)?
What is the time for each step and between each step?
What is the total time between start and finish (lead time)?
When does a patient join a queue, and is it a regular occurrence?
How many non-value steps are there?
What do patients complain about?
What are the problems for staff?
Fig 3 Workflow diagram of current state endoscopy pathway
Redesigning the patient journey
Lean thinking transformation involves redesigning the patient journey. 21 22 This will eliminate, combine and simplify non-value steps, 23 limit the impact of rate limiting steps (such as bottlenecks), and emphasise the value adding steps, making the process more patient-centred. 6 It is often useful to trial the new pathway and review its effect on patient management and satisfaction before attempting more sustained implementation.
Worked example: How to undertake a process mapping exercise
South Coast NHS Trust, a large district general hospital, plans to improve patient access to local services by offering unsedated endoscopy in two peripheral units. A consultant gastroenterologist has been asked to lead a process mapping exercise of the current patient journey to develop a fast track, high quality patient pathway.
In the absence of local data, he reviews the published literature and identifies key factors to the patient experience that include levels of discomfort during the procedure, time to discuss the findings with the endoscopist, and time spent waiting. 24 25 26 27 He recruits a team: an experienced performance manager, a sister from the endoscopy department, and two junior doctors.
The team drafts a map of the current endoscopy journey, using repositionable notes on the wall. This allows team members to identify the start (admission to the unit) and completion (discharge) points and the locations thought to be involved in the patient journey.
They decide to use a “walk the journey” format, interviewing staff in their clinical environments and allowing direct observation of the patient’s management.
The junior doctors visit the endoscopy unit over two days, building up rapport with the staff to ensure that they feel comfortable with being observed and interviewed (on a semistructured but informal basis). On each day they start at the point of admission at the reception office and follow the patient journey to completion.
They observe the process from staff and patient’s perspectives, sitting in on the booking process and the endoscopy procedure. They identify the sequence of steps and assess each for its duration (minimum and maximum times) and the factors that influence this. For some of the steps, they use a digital watch and notepad to check and record times. They also note staff-patient and staff-staff interactions and their function, and the recording and movement of relevant information.
Details for each step are entered into a simple table (table 2 ⇓ ), with relevant notes and symbols for bottlenecks and patients’ waits.
Patient journey for non-sedated upper gastrointestinal endoscopy
When data collection is complete, the doctor organises a meeting with the team. The individual steps of the patient journey are mapped on a single long section of paper with coloured temporary markers (fig 2 ⇑ ); additional information is added in different colours. A workflow diagram is drawn to show the physical route of the patient journey (fig 3 ⇑ ).
The performance manager calculates that the total patient journey takes a minimum of 50 minutes to a maximum of 345 minutes. This variation mainly reflects waiting times before a number of bottleneck steps.
Only five steps (14 to 17 and 22, table 2 ⇑ ) are considered both to add value and needed on the day of the procedure (providing patient information and consent can be obtained before the patient attends the department). These represent from 13 to 47 minutes. At its least efficient, therefore, only 4% of the patient journey (13 of 345 minutes) is spent in activities that contribute directly towards the patient’s outcome.
The team redesigns the patient journey (fig 4 ⇓ ) to increase time spent on value adding aspects but reduce waiting times, bottlenecks, and travelling distances. For example, time for discussing the results of the procedure is increased but the location is moved from the end of the journey (a bottleneck) to shortly after the procedure in the anteroom, reducing the patient’s waiting time and staff’s travelling distances.
Fig 4 Workflow diagram of future state endoscopy pathway
Implementing changes and sustaining improvements
The endoscopy staff are consulted on the new patient pathway, which is then piloted. After successful review two months later, including a patient satisfaction questionnaire, the new patient pathway is formally adopted in the peripheral units.
Further reading
Practical applications.
NHS Institute for Innovation and Improvement ( https://www.institute.nhs.uk )—comprehensive online resource providing practical guidance on process mapping and service improvement
Lean Enterprise Academy ( http://www.leanuk.org )—independent body dedicated to lean thinking in industry and healthcare, through training and academic discussion; its publication, Making Hospitals Work 23 is a practical guide to lean transformation in the hospital environment
Manufacturing Institute ( http://www.manufacturinginstitute.co.uk )—undertakes courses on process mapping and lean thinking transformation within health care and industrial practice
Theoretical basis
Bircheno J. The new lean toolbox . 4th ed. Buckingham: PICSIE Books, 2008
Mould G, Bowers J, Ghattas M. The evolution of the pathway and its role in improving patient care. Qual Saf Health Care 2010 [online publication 29 April]
Layton A, Moss F, Morgan G. Mapping out the patient’s journey: experiences of developing pathways of care. Qual Health Care 1998; 7 (suppl):S30-6
Graban M. Lean hospitals, improving quality, patient safety and employee satisfaction . New York: Taylor & Francis, 2009
Womack JP, Jones DT. Lean thinking . 2nd ed. London: Simon & Schuster, 2003
Cite this as: BMJ 2010;341:c4078
Contributors: TMT designed the protocol and drafted the manuscript; TMT, MB, JH, and TH collected and analysed the data; all authors critically reviewed and contributed towards revision and production of the manuscript. TMT is guarantor.
Competing interests: MB is a senior faculty member carrying out research for the Lean Enterprise Academy and undertakes paid consultancies both individually and from Lean Enterprise Academy, and training fees for providing lean thinking in healthcare.
Provenance and peer review: Not commissioned; externally peer reviewed.
- ↵ Kollberg B, Dahlgaard JJ, Brehmer P. Measuring lean initiatives in health care services: issues and findings. Int J Productivity Perform Manage 2007 ; 56 : 7 -24. OpenUrl CrossRef
- ↵ Bevan H, Lendon R. Improving performance by improving processes and systems. In: Walburg J, Bevan H, Wilderspin J, Lemmens K, eds. Performance management in health care. Abingdon: Routeledge, 2006:75-85.
- ↵ Kim CS, Spahlinger DA, Kin JM, Billi JE. Lean health care: what can hospitals learn from a world-class automaker? J Hosp Med 2006 ; 1 : 191 -9. OpenUrl CrossRef PubMed
- ↵ Layton A, Moss F, Morgan G. Mapping out the patient’s journey: experiences of developing pathways of care. Qual Health Care 1998 ; 7 (suppl): S30 -6. OpenUrl
- ↵ Peterson KM, Kane DP. Beyond disease management: population-based health management. Disease management. Chicago: American Hospital Publishing, 1996.
- ↵ NHS Modernisation Agency. Process mapping, analysis and redesign. London: Department of Health, 2005;1-40.
- ↵ Taylor AJ, Randall C. Process mapping: enhancing the implementation of the Liverpool care pathway. Int J Palliat Nurs 2007 ; 13 : 163 -7. OpenUrl PubMed
- ↵ Ben-Tovim DI, Dougherty ML, O’Connell TJ, McGrath KM. Patient journeys: the process of clinical redesign. Med J Aust 2008 ; 188 (suppl 6): S14 -7. OpenUrl PubMed Web of Science
- ↵ King DL, Ben-Tovim DI, Bassham J. Redesigning emergency department patient flows: application of lean thinking to health care. Emerg Med Australas 2006 ; 18 : 391 -7. OpenUrl CrossRef PubMed
- ↵ Mould G, Bowers J, Ghattas M. The evolution of the pathway and its role in improving patient care. Qual Saf Health Care 2010 ; published online 29 April.
- ↵ Rath F. Tools for developing a quality management program: proactive tools (process mapping, value stream mapping, fault tree analysis, and failure mode and effects analysis). Int J Radiat Oncol Biol Phys 2008 ; 71 (suppl): S187 -90. OpenUrl PubMed Web of Science
- ↵ Womack JP, Jones DT. Lean thinking. 2nd ed. London: Simon & Schuster, 2003.
- ↵ Graban M. Value and waste. In: Lean hospitals. New York: Taylor & Francis, 2009;35-56.
- ↵ Westwood N, James-Moore M, Cooke M. Going lean in the NHS. London: NHS Institute for Innovation and Improvement, 2007.
- ↵ Liker JK. The heart of the Toyota production system: eliminating waste. The Toyota way. New York: McGraw-Hill, 2004;27-34.
- ↵ Womack JP, Jones DT. Introduction: Lean thinking versus Muda. In: Lean thinking. 2nd ed. London: Simon & Schuster, 2003:15-28.
- ↵ George ML, Rowlands D, Price M, Maxey J. Value stream mapping and process flow tools. Lean six sigma pocket toolbook. New York: McGraw Hill, 2005:33-54.
- ↵ Fillingham D. Can lean save lives. Leadership Health Serv 2007 ; 20 : 231 -41. OpenUrl CrossRef
- ↵ Benjamin A. Audit: how to do it in practice. BMJ 2008 ; 336 : 1241 -5. OpenUrl FREE Full Text
- ↵ Vissers J. Unit Logistics. In: Vissers J, Beech R, eds. Health operations management patient flow logistics in health care. Oxford: Routledge, 2005:51-69.
- ↵ Graban M. Overview of lean for hospital. Lean hospitals. New York: Taylor & Francis, 2009;19-33.
- ↵ Eaton M. The key lean concepts. Lean for practitioners. Penryn, Cornwall: Academy Press, 2008:13-28.
- ↵ Baker M, Taylor I, Mitchell A. Analysing the situation: learning to think differently. In: Making hospitals work. Ross-on-Wye: Lean Enterprise Academy, 2009:51-70.
- ↵ Ko HH, Zhang H, Telford JJ, Enns R. Factors influencing patient satisfaction when undergoing endoscopic procedures. Gastrointest Endosc 2009 ; 69 : 883 -91. OpenUrl CrossRef PubMed Web of Science
- ↵ Del Rio AS, Baudet JS, Fernandez OA, Morales I, Socas MR. Evaluation of patient satisfaction in gastrointestinal endoscopy. Eur J Gastroenterol Hepatol 2007 ; 19 : 896 -900. OpenUrl CrossRef PubMed Web of Science
- ↵ Seip B, Huppertz-Hauss G, Sauar J, Bretthauer M, Hoff G. Patients’ satisfaction: an important factor in quality control of gastroscopies. Scand J Gastroenterol 2008 ; 43 : 1004 -11. OpenUrl CrossRef PubMed Web of Science
- ↵ Yanai H, Schushan-Eisen I, Neuman S, Novis B. Patient satisfaction with endoscopy measurement and assessment. Dig Dis 2008 ; 26 : 75 -9. OpenUrl CrossRef PubMed Web of Science
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 12, Issue 1
- Routine measurement of patient experience
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-2101-1353 Tim Benson 1 , 2 ,
- Alex Benson 3
- 1 R-Outcomes Ltd , Newbury , UK
- 2 Institute of Health Informatics , UCL , London , UK
- 3 R-Outcomes Ltd , London , UK
- Correspondence to Tim Benson; tim.benson{at}r-outcomes.com
Patient experience is a key pillar of healthcare quality. We describe a framework of three short generic measures covering Patient Experience, Result Satisfaction and Service Integration. The Result Satisfaction measure is described for the first time.
These measures capture twelve aspects of patient experience covering the relationship between patients and clinicians (Patient Experience), the immediate results of the consultation or treatment as perceived by patients (Result Satisfaction) and collaboration between different healthcare services and silos (Service Integration). Each measure has four items.
These measures are compared with three national measures: the Friends and Family Test and the General Practice Patient Survey used in England, and HCAHPS used in US hospitals. The expected benefits of national measures are not being achieved and we need to think again about how best to tailor health services to meet patients’ expectations.
The three measures described (Patient Experience, Result Satisfaction and Service Integration) are generic, short and have low reading ages. They share common forms and scoring schemes, which mean that they can be used individually or in combination at all levels of a healthcare provider.
- Patient-centred care
- Patient satisfaction
- Quality measurement
- Quality improvement methodologies
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjoq-2022-002073
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
All patients want and deserve a good experience of care. Patient experience is a key quality outcome, which can be used to improve quality, governance, accountability and choice. 1 However, it is also a complex, multiattribute concept that reflects patients’ perceptions and experiences of receiving care.
A short definition of patient experience is the sum of all interactions, shaped by an organisation’s culture, which influence patient perceptions across the continuum of care. 2 Patient experience is patient-reported perception of a healthcare organisation and their journey across the continuum of care. Patient-reported experience measures (known as PREMs) focus on the healthcare provider, which provides the service.
Patient experience has three dimensions: relational, functional and integration.
Relational experience relates to the interaction between clinician and patient. 3 This is the focus of most efforts to improve patient engagement and patient-centred care.
Functional experience, or Result Satisfaction, is about immediate benefits perceived by patients at the time. 4 This does not cover medium-term and long-term benefits or patient outcomes.
Integration experience, or Service Integration, relates to the patients’ experience of care, which cross traditional silos. 5 This is the focus of whole system approaches.
Measures are needed for all three. PREMs focus on the care provider, while patient-reported outcome measures are about the subject of care. 6 Patient experience is more objective than patient satisfaction. Some people are satisfied with standards of care that others find inadequate. However, patient experience surveys have been criticised for survey length, infrequent sampling frequency and slow feedback. 7
We should distinguish between things that impact health outcomes and those that are cosmetic. For example, good communication between staff and patients may lead to faster recovery, but the quality of wall-paper in the reception area probably does not.
All patients seek high levels of experience, effectiveness and safety. 8 Many PREMs are specific to particular types of care, such as inpatient stays, general practice appointments, outpatient visits, maternity care, care homes or domiciliary care. Our focus is on generic measures, which apply to all patients, irrespective of their problems or the type of treatment they receive.
This paper has three main aims.
First, it aims to show how the concept of patient experience can cover relational, functional and integration experience. These are different and complementary concepts.
Second, it describes some criteria used to develop new measures of functional and integration experience, as well as a modified measure of relational experience.
Third, it compares these measures in length and readability with three existing measures.
We used a similar development approach throughout. This involved literature review, informal focus groups with clinicians and users, and our own experience in developing questionnaires. Each measure evolved through multiple iterations over months or years until everyone was happy. The development and validation of any new measure is not something to be undertaken lightly. It always takes much longer than expected, even knowing that this is not a quick job.
We use four core criteria, which can be measured easily: relevance, responsiveness, brevity and readability. 9
Every question asked must be relevant and suitable for frequent, repeated use. Response rates are a measure of relevance. If people do not answer an item, this may be because it is not relevant, is worded ambiguously and they do not know how to answer, asks sensative or personal questions, or is inappropriate in some other way. In each case the question needs to be reviewed.
Responsiveness
Responses should be sensitive to the types of change that can be made by local staff and managers. Things that cannot easily be changed, such as clinic location, transport, parking, payments and regulations should not be asked routinely. Wording that generates noise or is not responsive to change should be avoided. Responsiveness can be measured by testing results statistically between different services, or before and after changes.
Measures should be as short as possible to minimise time to complete by patients (or proxies if patients are not able to complete it themselves). Respondent burden is a function of survey length. Word-count is a simple measure of brevity.
Readability
Wording needs to be clear to all respondents. This means that only simple words are used, which are widely understood in the same way by the target population. This also simplifies translations into other languages. Readability is a measure of clarity. Many readability measures have been developed including: the Flesch reading ease score, 10 the Gunning fog index, 11 the standard measure of gobbledygook 12 and the Flesch-Kincaid grade (FKG). 13
We use FKG, which equates roughly to the US school grade. Reading age is approximately FKG plus five. Statistics are based on the full published text, including instructions, framing statements, items and options. The word count and FKG were measured using Microsoft Word 365 (V.16.63).

Options and scoring
In each measure, the strength of each item is rated using four options. Each option is indicated in mutually supporting ways to reduce cognitive effort, avoid the need for training and improve face validity. These are:
Written labels.
Position decreasing in excellence from left to right.
Colour (green, yellow orange and red).
Smiley face emojis.
Written labels are the most important. You cannot use colour, position or emojis when the measure is completed during a telephone call.
The options may vary according to context. Our original paper on patient experience used excellent, good, fair and poor. 14 Here, we use the option set strongly agree, agree, neutral and disagree, with minor changes in item wording to mean the same things. There is benefit in using the same option set throughout. Each measure also includes a short preamble, which may be adapted to local context.
For analysis and reporting, each item is given a score on a 0–3 scale as follows: disagree 0, neutral 1, agree 2 and strongly agree 3. A summary score is calculated by adding the individual scores for each item, giving a scale with 13 possible values from 0 (4×disagree) to 12 (4×strongly agree). A high score is always good, and a low score is always bad. The summary score is blank if any item is missing.
For a population (more than one respondent), the mean scores are transformed to a 0–100 scale, where 0 (the floor) indicates that all respondents rated disagree and 100 (the ceiling) indicates that all respondents rated strongly agree. This is done by multiplying individual scores by 100 and dividing by 3 for items or by 12 for summary scores. This allows both mean item scores and mean summary scores to be scored 0–100, allowing comparison.
Patient experience
The Patient Experience measure (also known as howRwe) was developed during the period 2012–14 for regular routine use. For more information, see the original paper, which uses different options and pronouns. 14 The four dimensions are:
Compassion. This includes how individuals are treated directly, including empathy, emotional support, politeness, dignity, respect and privacy. The wording is ‘We treat you kindly’, where ‘we’ applies to the provider organisation and staff.
Communication. This broad area includes all aspects of communication between patients and their clinicians (both ways). It includes patient engagement, information provision, education, choice, consent, shared decision making and empowerment. (‘We listen and explain’).
Timeliness. This covers all types of delay, waiting, access, cancellation and responsiveness; it includes delays between referral and appointment, waiting to be seen and the time taken to answer a call from a bed or by telephone. (’We see you promptly’).
Reliability. This covers how well patients perceive the unit is managed, including safety, dependability, efficiency and whether information (eg, lab results) is available when and where needed and is acted on appropriately. (’We are well organised’).
The standard preamble is ‘How are we doing? (our recent care)’. However, this wording can be adapted to local context and the patient’s care pathway.
The PREM, showing the preamble, items and options is shown in figure 1 .
- Download figure
- Open in new tab
- Download powerpoint
Patient experience measure.
Result satisfaction
Result Satisfaction, or functional experience, covers the patient’s happiness, contentment and satisfaction with a specific session, stay or consultation. This measure was developed during 2022, and this is its first publication. It is designed for frequent routine use. The Result Satisfaction measure focuses on the patient’s perception of immediate results (outputs). The wording has been chosen to be apply to things which have happened, have been arranged or promised, as well as those those that have neither happened nor been promised.
The terms happy, pleased and content are often used synonymously but may have subtly different meanings. Happiness refers usually to immediate reactions, while pleased implies satisfaction and content refers to longer term expectation.
The order of questions goes from the past and specific, to the future and less specific.
We selected four dimensions for Result Satisfaction:
Consultation covers one-to-one face-to-face, video or telephone sessions with clinicians or provider staff. (‘I am happy with those I spoke to’).
Treatment covers all types of care, therapy and medication given, prescribed or changed. (‘I am pleased with my treatment (incl. medication)’).
Practical help covers arrangements made or promised, if any. (‘I am content with practical help’).
Plan covers future plans, tests and referrals, including doing nothing. (‘I am happy about the next steps’).
These questions should be used, for example, even when patients do not receive any treatment or medication, and when no special practical help has been arranged.
The format of the Result Satisfaction measure, showing the preamble, items and options is shown in figure 2 .
Result satisfaction measure.
Service integration
When people living with multiple conditions are asked about their healthcare, they often say that they want better integration between different siloed services. They dislike having to repeat their stories time and again; they do not think different services share information well between them and they are surprised that some staff do not even know what other services do. Above all, they want healthcare services to work as if they were a single joined-up service, not as a set of independent fiefdoms.
Service integration is a core premise of patient-centred care, but conflicts with the traditional medical model, which favours specialty-specific silos. From early in their careers, doctors and nurses specialise in specific conditions and modes of treatment, leading to integration barriers.
Most PREMs focus on one hospital or service, not integration over the patient pathway and across services. This problem matters less when a patient only has one condition, treated by a single specialist. However, most money is spent on people living with multiple conditions and treatment has become more complex.
The Service Integration measure was developed around 2017 for routine use. 9
The four dimensions ( figure 3 ) are:
Communication. How well services communicate. (‘Services talk to each other’).
Service knowledge. Patients’ perceptions of staff awareness of what other services do. (‘Staff know what other services do’).
Repetition. Whether patients need to repeat their stories endlessly. (‘You don’t have to repeat your story’).
Collaboration. How well different services work together as a team. (‘Different services work well together’).
Service integration measure.
The preamble is ’How well do services collaborate?’. The options are strongly agree, agree, neutral and disagree.
The scores obtained are often unexpectedly low, which provides further evidence that service integration is of real concern to patients.
Word count and readability
Table 1 shows the word count, FKG and reading age statistics for the Patient Experience, Result Satisfaction and Service Integration measures, together with those for three nationally used PREMs.
- View inline
The longer national measures, such as GPPS (General Practice Patient Survey) and HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems), include data used for classification, such as setting, age group, gender, ethnicity, etc.
The FFT (National Health Service Friends and Family Test) was introduced in the NHS in England in 2013. More than 90 million responses have been collected. The FFT was originally based on the Net Promoter Score. 15 Following criticism, 16 it was revised substantially in 2019 and now has just one quantitative question and one or more free text questions. 17 The text questions provide most of the value but need careful analysis.
The GPPS has been running since 2007. In 2022, the survey was sent to almost 2.5 million adults aged 16 years or over and registered with a GP practice in England. The survey had a national response rate of 29.1%, (down from 35.1% the previous year). It shows, for example, that patients find it harder to book GP appointments since COVID. 18
HCAHPS is the nationally mandated survey of inpatient experience in the USA, which has been used since 2006. HCAHPS data are reported to the Centres of Medicare and Medicaid Services and directly impacts payments to hospitals. In March 2021, 4439 hospitals submitted results with 25% response rate. 19
The Patient Experience (howRwe), Result Satisfaction and Service Integration measures capture different aspects of the perception that people have of encounters with their care providers. They illustrate three different dimensions of patient experience, which can only be measured by asking patients themselves. Each measure has been designed for frequent routine use. They may be used together or independently.
Other publications distinguish between relational and functional experience, 8 measured here by Patient Experience and Result Satisfaction, respectively, but, as far as we are aware, the relational, functional and integrated care aspects of patient experience have not been combined previously in a single set of short generic measures.
The Patient Experience (howRwe) measure has been widely used and shows that patients are generally well pleased with how they are treated by individual clinicians. The Result Satisfaction measure is new. The Service Integration measure has been less widely used than the Patient Experience measure, but notable differences have been identified between different services and localities.
Other measures address only one or two aspects of patient experience. Focus has been directed at patients’ perceptions of the different roles played by staff, such as doctors, nurses and admin staff. In our work, we do not usually draw these distinctions.
In mental health, self-reported patient satisfaction has been found to be reliable and valuable, but there is no consensus on a gold standard scale, its purpose, length or focus. 20
These measures are quick and easy to use in different ways. The questions can be asked on-line, prompted by email or SMS text message with a URL, face-to-face, by telephone or on paper. Whatever method is used, it is essential to agree the workflow with all staff concerned. Most patients are happy to answer short surveys if they are asked nicely, but not otherwise. An agreed plan is required to set out who does what, when and where, including how the results will be used to improve quality.
National surveys
National surveys such as GPPS and HCAHPS can teach some important lessons. These surveys have been running since the 2000s, but response rates have declined over the years. The response rate of GPPS has fallen from 44% in 2007 to 29% in 2022, in spite of sending non-responders three full copies by post and three nudges by SMS text message. Response rates differed by patient age from under 20% for those aged less than 55 to about 60% for those aged over 65. 21 On-line data collection accounted for under 41% of GPPS responses in 2022 (up from 37% in 2021). 18 The digital divide is still a real issue for many patients.
HCAHPS response rates have fallen over the years from over 33% in 2007 to 25% in 2021. They vary from 17% (Washington DC) to 36% (Nebraska). 22 There is evidence that high response rates are correlated with high satisfaction scores. 23
Most national surveys are mandated centrally and are anonymous to protect privacy and confidentiality. It is not possible to identify individual patients or individual clinicians. They are used primarily for national, regional and local comparisons between providers. They do not directly affect the care provided at the individual level.
Coulter and colleagues have pointed out that while national patient experience data has been collected for many years, few providers systematically use this information to improve services. They conclude that it is unethical to ask patients to comment on their experiences if these comments will be ignored. 24
Others have argued that existing approaches to measuring patient experiences are fragmented, duplicate effort, involve numerous requests for information and increase patient burden. They see patient experience as the starting point towards patient-centered care. They call for multistakeholder collaboration to deliver healthcare systems and interventions that are centred around and tailored to patient experience and help address patients’ priorities. 25
Strengths and limitations
The strengths of Patient Experience, Result Satisfaction and Service Integration measures are that they are short, have a low reading age and a common format and scoring scheme. They can be used individually, together or in combination with other measures. Having four items in each measure, and twelve items overall, provides a level of granularity which helps managers improve services. More details can be provided in a free-text comment box.
These measures give managers the opportunity to track how they are doing, identify any areas of concern and take remedial action as early as possible. Their generic form allows different services to be compared using the same metrics. They can be used at all levels within a healthcare organisation.
Weaknesses are that the Results Satisfaction measure is new and the Service Integration measure is quite new, so they are not yet widely used. More work is required to test these measures in a range of operational situations.
Conclusions
This paper describes three generic patient-reported measures of Patient Experience, Result Satisfaction and Service Integration, which together cover relational, functional and integration aspects of patient experience. All three measures are generic and share a common format and scoring scheme. They are shorter and have a lower reading age than measures used in national surveys.
Ethics statements
Patient consent for publication.
Not applicable.
- Neiderhauser V ,
- Marshburn D , et al
- Greene SM ,
- Bohren MA , et al
- Dollard J ,
- Marshall A , et al
- Muhlbacher A ,
- McLaughlin G
- Kincaid J ,
- Fishburne R ,
- Rogers R , et al
- Reichheld FF
- Cornwell J ,
- NHS England
- HCAHPS: Patients’ Perspectives of Care Survey
- Miglietta E ,
- Belessiotis-Richards C ,
- Ruggeri M , et al
- ↵ Centers for medicare & medicaid services . Baltimore, MD .: Available : https://www.hcahpsonline.org [Accessed 27 Jul 2022 ].
- Gnida J , et al
- Coulter A ,
- Ziebland S , et al
- Schroeder K ,
- Bertelsen N ,
- Scott J , et al
Twitter @timbenson
Contributors TB conceived and wrote the first draft of the paper. AB assisted in drafting and contributed to the design of the Result Satisfaction measure.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests TB and AB are employees of R-Outcomes, which owns the copyright of the Patient Experience, Result Satisfaction and Service Integration measures.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
- Skip to main content
- Skip to primary sidebar
- Skip to footer
- QuestionPro

- Solutions Industries Gaming Automotive Sports and events Education Government Travel & Hospitality Financial Services Healthcare Cannabis Technology Use Case NPS+ Communities Audience Contactless surveys Mobile LivePolls Member Experience GDPR Positive People Science 360 Feedback Surveys
- Resources Blog eBooks Survey Templates Case Studies Training Help center
Patient Journey Mapping: What it is, Benefits and 5 Steps to Do it

In the rapidly evolving landscape of healthcare, patient-centered care has emerged as a crucial paradigm shift. As hospitals strive to deliver exceptional patient experiences and improve outcomes, understanding the patient journey has become paramount.
A customer journey map is a powerful tool that shares patients’ path from their first encounter with a healthcare facility to their final discharge. By visualizing this complex expedition, hospitals can gain invaluable insights into patient needs, pain points, and opportunities for enhancement, thereby revolutionizing the delivery of care.
The following article delves into the significance of patient journey maps for hospitals and their importance in optimizing patient experiences, streamlining processes, and ultimately elevating the standard of healthcare.
What is a Patient Journey Map?
A patient journey is a methodology that enables the analysis of a healthcare provider’s processes and value chain but from the patient’s viewpoint. This includes their possible solutions, pain points, emotions, touchpoints and user actions throughout the journey.
The patient journey map employs visual representation to gain deeper insights into how patients engage with a healthcare facility throughout their care journey. This unique approach is an evolution of the customer journey map , tailored specifically to the healthcare context. By employing this method, healthcare providers can unravel the intricacies of patient interactions, uncovering valuable information to enhance the quality of care provided.
The concept of the Patient Journey Map mirrors that of the Customer Journey Map, seeking to uncover areas of enhancement in patient care across various healthcare providers, including hospitals, fertility centers, and more.
Just as a skilled cartographer carefully crafts a map to navigate uncharted territories, patient journey maps chart the course of a patient’s experience, revealing hidden insights, unveiling opportunities for improvement, and ultimately guiding healthcare providers toward a destination of unparalleled patient satisfaction .
What are the benefits of implementing a Patient Journey Map?
Engaging in the patient journey proves immensely valuable as it enables us to provide patients with an optimal experience, meeting the very expectations that arise when seeking healthcare services.
The emotional aspect tied to the Patient Journey Map can be profoundly impactful, considering the inherent uncertainties often associated with visiting a healthcare facility.
Considering the unique personalities, fears, behaviors, and attitudes of different patient archetypes play a pivotal role in creating a tailored and pleasant experience for them. Thus, the patient journey map becomes a valuable tool benefiting both patients and healthcare service providers.
● Enhanced Communication with Patients:
By understanding the patient journey, healthcare providers can establish effective and continuous communication throughout the entire care process, addressing any doubts or uncertainties. Keeping patients well-informed and updated through appropriate channels reinforces the quality of care provided.
● Elimination of Blind Spots:
Clear comprehension of each stage of the patient journey helps bridge the gaps between patients and services. From the initial appointment request to discharge and follow-up, identifying and addressing potential blind spots ensures consistent and satisfactory solutions tailored to each patient’s unique situation.
● Streamlined Resolution of Pain Points:
Mapping the patient journey and defining archetypes enables a deeper understanding of patient concerns, particularly identifying which aspects of the service have the most negative impact. Pain points such as waiting times, unclear explanations, lack of empathy, or impersonalized treatments can be simplified and resolved more effectively.
Learn About: Complaint Resolution
● Process Optimization:
A well-defined patient journey optimizes workflow and allows for more efficient handling of all processes. Staff members become better equipped to anticipate and address patient issues promptly, offering alternatives that instill confidence and satisfaction.
● Continuous Improvement:
Implementing a Patient Experience model involves measuring patient experiences through a feedback system . Continuously updating the database with relevant information about patient journeys and their experiences leads to ongoing improvement in response times, customer service processes, and overall service quality .
What is a Patient Persona?
The patient persona represents an imaginary profile that encapsulates potential patients’ needs, goals, illnesses, conditions, emotions, behaviors, and knowledge.
By creating patient personas, healthcare providers can enhance the accuracy and anticipation of care and diagnosis processes, ultimately improving the experience of individuals seeking healthcare services.
5 Steps to Build Your Own Patient Journey Map
1. define the experience to map:.
Before diving into the Patient Journey Map, it is crucial to determine the specific experience you intend to outline. By establishing your objectives and identifying the type of information you seek to gather and how it will be utilized, you can ensure a more efficient mapping process right from the start.
2. Identify your Ideal Patient:
The majority of data used to construct the customer patient care journey will come directly from patient-clients. Thus, a key step is identifying the patient persona, which can be singular or multiple. You must decide whether the map will encompass various patient profiles or if separate maps will be created for each target patient.
To create the patient persona(s), gather feedback directly from patients and analyze their behaviors and data. Pose questions such as:
- What initially led the patient to seek your services?
- Which competitors did they research?
- How did they discover your website or company?
- What factors differentiated your brand from others? What influenced their decision (or lack thereof) to choose your services?
- What are their expectations when interacting with your company?
- Can they articulate what they appreciate about your company and what frustrates them?
- Have they ever contacted customer service? If so, how was their experience?
Once you have defined the patient persona(s), you can identify the distinct stages of the customer journey when engaging with your company.
3. Divide the Phases of the Customer Journey:
Throughout the customer-patient care journey, patient-clients progress through several discernible stages.
Phase #1: Pre-Visit
● DISCOVERY:
The patient journey initiates with a phase characterized by learning and concern. Patients embark on their healthcare journey upon recognizing a need or developing a concern related to a health issue.
For instance, if an individual experiences symptoms associated with being overweight, they may begin researching options for scheduling an appointment with a medical specialist. At this point, potential patients discover their specific needs and commence the process of investigating suitable solutions. They may turn to the internet, seek recommendations from friends and family, or explore other avenues. During this stage, it is recommended healthcare systems should provide educational support to aid individuals on their journey of understanding.
● CONSIDERATION:
Following their research, patients reach the consideration stage, having discovered your service. At this point, they possess some knowledge about your healthcare facility’s location and offerings, leading them to believe it could meet their needs. However, patients have also explored your competitors and are contemplating multiple options.
During the consideration stage, potential patients meticulously assess the information they come across, including service descriptions, pricing, contact pages, online inquiries, and reviews. They also evaluate the ease of accessing relevant information before scheduling an appointment and the availability of operating hours, among other factors.
Phase #3: Visit
● APPOINTMENT & ENGAGEMENT:
Having gathered sufficient information and progressed through the consideration phase, the patient ultimately chooses your service. This marks their first contact with the health center, which can occur in person, over the phone, via chat, email, or other means of communication.
During this stage, the patient schedules their appointment. The company must streamline the application process and maintain effective and proactive communication. It is crucial for this phase to be completed without complications.
● SERVICE DELIVERY:
Within the visit phase is the service delivery stage, where patients interact with various service providers at the health center. From the moment the patient enters the premises, the company must ensure an exceptional service experience.
Service delivery encompasses multiple micro-moments, necessitating comprehensive attention throughout the entire journey. Every interaction matters, from the reception care and waiting times to the core service itself—meeting the patient’s objective of being evaluated by a doctor or specialist.
Phase #3: After the Visit
● RETENTION:
The Patient journey doesn’t conclude after the initial visit. A crucial third phase occurs post-encounter, where efforts should be dedicated to fostering patient retention and encouraging their return for subsequent visits. Building strategies that monitor the patient experience is essential in designing loyalty programs to ensure patients return for future services.
● RECOMMENDATION:
Part of the post-visit phase involves patient recommendations, which heavily depend on the overall patient journey experience provided by the company. If patients have had a positive service encounter, they are likely to recommend it to others, benefiting your business.
However, it is important to remember that negative experiences are equally shared, and if patients are dissatisfied, they may spread negative feedback.
Promptly addressing any negative comments is crucial to resolving issues and preventing unfavorable recommendations.
Phase #4: Identify Touchpoints
An additional vital step in mapping the customer-patient care journey is identifying the various touchpoints between the patient and the healthcare facility. These interactions occur at different stages throughout the patient journey, and understanding these touchpoints aids in developing strategies that facilitate effective communication.
- Seeking information about healthcare centers: discovering the existence of the healthcare provider and the services it offers.
Investigation:
- Reviewing patient-client feedback: researching comments and feedback from other patients about their visit experiences at the health center.
- Exploring promotions: searching for economic benefits such as discounts, promotions, and bundled service packages.
Acquisition :
- Appointment Request: Contact or visit the health center to schedule an appointment.
- Provision of Personal Data: The health center will request personal information to finalize the appointment booking.
- Appointment Confirmation: After providing the required data, the appointment for the agreed date and time is confirmed.
- Patient Reception: The patient arrives at the health center at their scheduled appointment time.
- Waiting Room: The staff guides the patient to the designated waiting area.
- Consultation: The patient’s turn to be attended by the specialist.
- Payment: The process of settling the payment for the service, which may occur at any point during the service phase, depending on the health center’s policies.
- Patient Recommendations: Patients offer positive or negative feedback about the health center and its services.
- Loyalty Program: Incentives such as offers, promotions, discounts, or a points system to encourage future visits.
Recommendation:
- Complaint: If the patient has had a negative experience, they may file a complaint with the health center.
- Online Reviews: Patients share comments or criticisms about the service by posting reviews on the internet.
4. Identify Contact Channels
Patients engage with the health center through various channels throughout the patient journey. These channels, such as the health center itself, can be physical or online, including social media, email, applications, websites, and online forms.
Identifying the most utilized contact channels at each stage of the customer-patient care journey is crucial. This allows for the development of tailored strategies for each channel, meeting patient expectations at each phase.
Working on the patient journey is crucial for healthcare providers to deliver a high-quality experience to patients. By mapping their interactions, providers gain a deeper understanding of their patient personas, allowing them better to comprehend patient needs, desires, and circumstances to provide the desired care.
Patient Journey Map Example
To better understand what a Patient Journey Map is, we have created this fictitious example using one of the most reputable medical institutions in the healthcare sector, the Massachusetts General Hospital, as a reference.
In this example, we have included some generic touchpoints that are usually the most common in the interaction between a hospital and a patient.
Through this example, it would be possible to visualize the points of interaction between both parties and the perception that patients have of them, which can be positive or negative. This serves as a clear indicator for making adjustments and learning from what has been done well.
The Office of Patient Experience plays a vital role in facilitating initiatives to assess and enhance the quality of care experienced by patients and their families. They are responsible for evaluating each of these touchpoints and ensuring that appropriate actions are taken.
The Mass General Hospital is a benchmark not only in terms of service level but also in the implementation of methodologies and actions that guarantee the satisfaction of their patients. A clear example of this can be seen in the results of their annual HCAHPS survey, where they score above the national average in various aspects.
Willingness to Recommend Hospital Scores below show the percentage of patients who would “definitely recommend” Mass General to their friends and family.
To see the complete study, we invite you to visit their website and learn about it.
More Examples of Patient Journey Maps
Seeking inspiration to craft your own Patient Journey Map? Your search ends here!
Explore a collection of remarkable examples from top-notch brands, unveiling their initiatives that delight customers and foster loyalty.
Get set to revolutionize your own Patient Journey!
Mass General Hospital is renowned for providing exceptional care and taking special care in understanding the perspective of its patients. They achieve this through different tools, such as satisfaction surveys, internal and external feedback, and HCAHPS surveys .
Mayo Clinic is characterized by its focus on patient satisfaction and its extensive technical deployment to gather user and prospect feedback.
Cleveland Clinic is often ranked among the best hospitals in the United States. This recognition is not only due to its incredible facilities, global expansion, and well-prepared staff but also because of its remarkable focus on the experience they provide to its patients and clients.
Singapore General Hospital is one of the largest and oldest hospitals in Singapore. It has been a major healthcare institution providing a wide range of medical services and treatments since 1821.
Johns Hopkins Medicine has long recognized the significance of a positive patient and family experience during hospitalization, which is why they maintain a specific focus on patient satisfaction to achieve an optimal experience.
How can you enhance your Patient Journey Map based on your acquired knowledge?
The insights and recommendations shared above are likely to have sparked ideas about the potential impact of these initiatives across various industries, not just healthcare.
The first crucial step is to embrace a customer-centric approach, keeping their needs and expectations at the forefront. By doing so, the actions you take will have a meaningful impact on your customers and yield multiple benefits for your business.
At QuestionPro, we offer a range of tools and features specifically designed to help you achieve this objective.
QuestionPro SuiteCX is a Customer Journey Mapping Software that simplifies the process of creating your customer journey.
With a vast selection of templates and the ability to personalize user/buyer personas while incorporating your own data, you can conduct precise visual analyses at every touchpoint throughout your patient journey.
Start delighting your customers today!
MORE LIKE THIS

15 Best Customer Experience Software of 2024
May 2, 2024

Journey Orchestration Platforms: Top 11 Platforms in 2024
Top 12 Employee Pulse Survey Tools Unlocking Insights in 2024
May 1, 2024

Taking Action in CX – Tuesday CX Thoughts
Apr 30, 2024
Other categories
- Academic Research
- Artificial Intelligence
- Assessments
- Brand Awareness
- Case Studies
- Communities
- Consumer Insights
- Customer effort score
- Customer Engagement
- Customer Experience
- Customer Loyalty
- Customer Research
- Customer Satisfaction
- Employee Benefits
- Employee Engagement
- Employee Retention
- Friday Five
- General Data Protection Regulation
- Insights Hub
- Life@QuestionPro
- Market Research
- Mobile diaries
- Mobile Surveys
- New Features
- Online Communities
- Question Types
- Questionnaire
- QuestionPro Products
- Release Notes
- Research Tools and Apps
- Revenue at Risk
- Survey Templates
- Training Tips
- Uncategorized
- Video Learning Series
- What’s Coming Up
- Workforce Intelligence
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Patient Experience and Satisfaction with Inpatient Service: Development of Short Form Survey Instrument Measuring the Core Aspect of Inpatient Experience
* E-mail: [email protected]
Affiliation The Jockey Club School of Public Health and Primary Care, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong, China
Affiliation Nuffield Department of Population Health, University of Oxford, Oxford, United Kingdom
Current address: Alice Lee Centre for Nursing Studies, National University of Singapore, Singapore, Singapore
- Eliza L. Y. Wong,
- Angela Coulter,
- Paul Hewitson,
- Annie W. L. Cheung,
- Carrie H. K. Yam,
- Siu fai Lui,
- Wilson W. S. Tam,
- Eng-kiong Yeoh

- Published: April 10, 2015
- https://doi.org/10.1371/journal.pone.0122299
- Reader Comments
Patient experience reflects quality of care from the patients’ perspective; therefore, patients’ experiences are important data in the evaluation of the quality of health services. The development of an abbreviated, reliable and valid instrument for measuring inpatients’ experience would reflect the key aspect of inpatient care from patients’ perspective as well as facilitate quality improvement by cultivating patient engagement and allow the trends in patient satisfaction and experience to be measured regularly. The study developed a short-form inpatient instrument and tested its ability to capture a core set of inpatients’ experiences. The Hong Kong Inpatient Experience Questionnaire (HKIEQ) was established in 2010; it is an adaptation of the General Inpatient Questionnaire of the Care Quality Commission created by the Picker Institute in United Kingdom. This study used a consensus conference and a cross-sectional validation survey to create and validate a short-form of the Hong Kong Inpatient Experience Questionnaire (SF-HKIEQ). The short-form, the SF-HKIEQ, consisted of 18 items derived from the HKIEQ. The 18 items mainly covered relational aspects of care under four dimensions of the patient’s journey: hospital staff, patient care and treatment, information on leaving the hospital, and overall impression. The SF-HKIEQ had a high degree of face validity, construct validity and internal reliability. The validated SF-HKIEQ reflects the relevant core aspects of inpatients’ experience in a hospital setting. It provides a quick reference tool for quality improvement purposes and a platform that allows both healthcare staff and patients to monitor the quality of hospital care over time.
Citation: Wong ELY, Coulter A, Hewitson P, Cheung AWL, Yam CHK, Lui Sf, et al. (2015) Patient Experience and Satisfaction with Inpatient Service: Development of Short Form Survey Instrument Measuring the Core Aspect of Inpatient Experience. PLoS ONE 10(4): e0122299. https://doi.org/10.1371/journal.pone.0122299
Academic Editor: Vineet Gupta, University of California San Diego, UNITED STATES
Received: September 4, 2014; Accepted: February 19, 2015; Published: April 10, 2015
Copyright: © 2015 Wong et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Data Availability: All relevant data are within the paper.
Funding: This work was supported by Grant numbers: 8110001414 (Hong Kong Hospital Authority); Funder's website: http://www.ha.org.hk/ . The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
Input from patients is a fundamental feature of patient-centred care [ 1 , 2 ]. Direct feedback from patients is considered the best way to measure the quality of their experiences [ 3 , 4 ]. It has proved useful to ask patients to report on detailed aspects of what happened during a specific care episode, rather than asking them to rate their satisfaction using general evaluation categories [ 4 – 6 ]. Standardized patient experience questionnaires are widely used for assessing the quality of healthcare from the patient’s perspective [ 7 ]. One of the most widely used patient experience surveys is the Adult Inpatient Survey, which was originally developed for use in England by the Picker Institute Europe [ 8 – 10 ]. A validated core set of items (PPE-15) that identified key aspects of patients’ experience was subsequently developed in 2002 [ 11 , 12 ].
Patients’ experience is influenced by the structure of the health system. Hong Kong is an ex-British colony and therefore has a tax-base funded health system and hospital settings similar to those in the United Kingdom. In 2010, a validated instrument measuring patients’ experience, the Hong Kong Inpatient Experience Questionnaire (HKIEQ), was developed by adapting the General Inpatient Questionnaire of the Care Quality Commission in England and integrating it with findings from a local validation study [ 13 , 14 ]. The HKIEQ has good structural validity and reflects the multidimensionality of patients’ experiences of different aspects of care during hospitalization. The questionnaire consists of 54 items, and the responses can be turned into scores relating to specific, actionable quality improvement measures. However, the length of the questionnaire limits its use. The development of a short-form version of HKIEQ is thus important for maintaining the momentum of the quality improvement culture and for soliciting patients’ views on a regular basis. This study designed a Short-form Hong Kong Inpatient Experience Questionnaire (SF-HKIEQ) consisting of a core set of items from the HKIEQ that reflect the most important components of patient experiences from the perspectives of both patients and healthcare professionals.
Study design
The HKIEQ consists of 54 evaluative items in 9 dimensions [ 13 , 14 ]. To develop a short-form version, a core set of items was identified using a two-stage approach: (1) a consensus conference; and (2) a cross-sectional validation survey.
Stage 1: Consensus Conference.
- an item included in the core set should be applicable to as many respondents as possible;
- core set measures should be highly correlated with the original measures at 0.9 or above [ 22 ];
- the internal consistency of the core set should reach 0.7 or above (KR-20’ is effectively Cronbach’s alpha statistic for dichotomous variables) [ 23 , 24 ]; and
- item-to-total correlations, corrected for overlap, should exceed 0.3 for items within a measure [ 25 ].
The literature suggests that a sample size of 15 should be sufficient to yield saturation on the face-validity of a questionnaire [ 16 ]. In Hong Kong, all of the public hospitals are managed by the Hospital Authority under seven geographical clusters. We therefore invited 2–3 health professionals currently working on healthcare quality, patient engagement or patient satisfaction surveys from each of the seven geographical clusters to attend the consensus conference.
Stage 2: Validation Survey.
We carried out a cross-sectional telephone survey of the preliminary scale and evaluated its acceptability, appropriateness and psychometric properties. The target population was Hong Kong citizens with a Hong Kong Identity Card, 18 years or older, Cantonese-speaking, who had had at least one overnight stay in one of the medical departments (surgery, orthopaedics and traumatology, emergency medicine, gynaecology, ear/nose/throat, clinical oncology and ophthalmology) at one of the 25 major acute and rehabilitation public hospitals in Hong Kong. Users of psychiatric or obstetric care, dentistry, hospice, infirmary, paediatrics, intensive care, anaesthesiology, and “other” departments were excluded from the survey. We estimated that about 500 participants would be sufficient for validation purposes, taking into consideration the number of items [ 26 – 29 ].
Data Collection
First, a summary of suggested criteria for developing a core set of items was presented to participants during the first round of the consensus conference. The experts were invited to express their views and then indicate their preferences for the proposed approaches. In the second round of the consensus conference, an amended version of the core set based on the chosen criteria was generated and the experts were asked to re-rate their preferences. Delphi methodology suggests that a minimum 75% level of consensus should be achieved; the number of rating rounds to achieve consensus depends on the level of consensus reached in each round [ 17 ].
Once the framework and face validity of the core set were established, a cross-sectional telephone survey was conducted. The participants were 500 patients who had been discharged from one of the 25 major acute and rehabilitation Hong Kong public hospital 48 hours to 1 month before the interviews, which were conducted between November 2012 and December 2012. The participants were asked to report their most recent inpatient experience using both the long-form HKIEQ and the short-form version [ 14 ].
Statistical Analysis
At the consensus conference, the choice of development approach was recorded using descriptive statistics to assess when the pre-specified level of 75% agreement was reached. Qualitative feedback about the criteria revisions was also recorded. For the validation survey, the data entry, management and analysis were performed using PASW version 18.0. Double-entry data input was used to ensure accuracy. The descriptive statistics of the sampled demographics were presented using frequencies and percentages or mean values, as appropriate. The effects of issues such as the percentage of missing values on individual items and the total completion interview time on the acceptability of the questionnaire were assessed [ 24 , 30 ]. Missing values were estimated based on the proportion of patients who refused to answer items or answered “Don’t know”/“Forgot”. The average interview completion time was calculated to test the appropriateness of the survey instrument length.
Each item on both the HKIEQ and the short-form was coded as a dichotomous “problem score” that indicates the presence or absence of a problem [ 11 ]. A problem was defined as a subjectively evaluated aspect of health care that could be improved. For example, the categorical answers for the item Did you have confidence and trust in the doctors treating you? was: (1) Yes, always; (2) Yes, sometimes; and (3) No. Options (2) and (3) for this items were coded as a “problem” for this aspect of care. To evaluate the construct validity of the short-form, a Spearman rank correlation of the summative problem scores was computed to compare the short-form and the HKIEQ. It was suggested that the selected core items should be highly correlated with the original measures, with a coefficient of 0.9 or above [ 22 ]. The Cronbach’s alpha coefficients (KR-20) and the item-to-total coefficient (corrected for overlap) were then estimated to test the internal consistency reliability of the instrument, which assessed whether the items in the questionnaire measured the same concept. A KR-20 coefficient of at least 0.7 generally indicates good reliability among scales, whereas a coefficient below 0.6 suggests the item should be rechecked [ 23 , 24 ]. The Spearman correlation coefficient (ρ) should exceed 0.3 for items within a measure [ 25 ].
Ethical Consideration
Ethical approval was obtained from the Clinical Research Ethics Committees of the Hospital Authority. All of the participants were informed of their rights, and were given information about the purpose of the study and details of the research procedures before the telephone interview. Verbal informed consent was obtained from each of the participants before the interview started. The participants were allowed to withdraw from the study at any point. Initial screening for eligible patients was conducted and their agreement to participate in the study was obtained by hospital staff and verified by our research team. All of the participants’ consents or refusals were documented by the interviewer. To ensure the quality of the interviews, the interviewers were monitored. All of the data were kept confidential and anonymous.
The study workflow is shown in Fig 1 .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0122299.g001
Stage 1: Consensus Conference
Fifteen nominated experts from public hospitals were invited to attend the consensus conference. Three refused due to unavailability and 12 experts attended. The experts had a mean of 5.8 years (SD: 3.2 years) of working experience in the field of patient engagement. The target minimum of 75% consensus on the development of the preliminary version of the core set of HKIEQ items was reached with two rounds of consensus conference.
First Round of Consensus Conference.
In the first round of the consensus conference, three approaches to the development of a core set of items were presented: (1) a psychometric approach using the four psychometric criteria listed above; (2) a problem-oriented approach focusing on the items that achieved low scores in the first population-based Patient Satisfaction Survey in 2010; and (3) a domain-oriented approach that included at least one item from each of the nine domains of the HKIEQ selected by ranking the item-to-total correlations. All of the experts (12/12, 100%) agreed to adopt the psychometric approach; 22 items were thereafter selected for inclusion as a core set ( Table 1 ). In addition, the participants suggested that items covering similar topics needed to be rephrased to make the instrument simple and brief.
https://doi.org/10.1371/journal.pone.0122299.t001
Second Round of Consensus Conference.
In the second round of the consensus conference, two ways of condensing items were discussed ( Table 2 ): condensing the five items related to information seeking into two items; and condensing the seven items related to specific job roles (physician, nurse and healthcare assistant) into three items. Four models based on the two ways of condensing the items were presented: (1) condensing for both information and role-related items; (2) condensing for information questions only, (3) condensing for role-related items only, and (4) no item condensing. One hundred per cent of the participants agreed that model 2, condensing for information only, was the best strategy. On this basis, a preliminary version of the short-form consisting of 19 items was developed.
https://doi.org/10.1371/journal.pone.0122299.t002
Stage 2: Validation Survey
Seven-hundred and thirty-five patients were approached and 516 patients completed the survey, giving a 70.2% response rate. The demographic characteristics of the respondents are given in Table 3 . Their mean age was 63 years (S.D: 17.5 years, range 18–99 years) and half of them (50%) were men. Compared with the corresponding discharge population of 22,019 cases with a mean age of 65 years during the study period, the respondents were significantly younger (p<0.05) and fewer lived in old age homes (p<0.05). In terms of education level, 50.4% had a primary education or below, 39.0% had a secondary education and 10.3% had a post-secondary/tertiary education or above. The length of stay in hospital was 1 week or less for 77.7% of the patients and more than 1 week for 22.3%.
https://doi.org/10.1371/journal.pone.0122299.t003
Acceptability and Appropriateness.
On average, the participants spent 18 minutes (S.D.: 4 minutes) and 9 minutes (S.D.: 2 minutes) completing the HKIEQ and short-form, respectively. The number of missing values ranged from 0.2% to 10% in the HKIEQ, whereas it was significantly reduced in the short-form, ranging from 0.2% to 1%.
Psychometric Properties: Construct Validity and Internal Reliability.
To test the short-form’s construct validity, a Spearman’s rank correlation coefficient for the relationship between the summative scores in the short-form and the HKIEQ was calculated. The result was ρ = 0.92, which was statistically significant (p<0.05) and generally satisfactory, as recommended (ρ≥0.9) [ 11 ]. To test the internal reliability, the KR-20 coefficient of the summative scores across items within the core set was calculated: it was 0.86, which was higher than the recommended α≥0.7 [ 23 , 24 ]. The relationship between each individual item and the summative score of the short-form (item-to-total correlation, corrected with overlap) ranged from a Spearman correlation coefficient of 0.11 to 0.59; 17 out of 19 items (89%) complied with the recommended Spearman correlation coefficient (ρ) ≥0.3 [ 11 , 25 ]. The two items that fell below this recommended level were Item 1 Did you get the help you needed from staff? (eating meals, going to the toilet, movement in/out of bed), which achieved a correlation of 0.11, and Item 2 Did hospital staff tell you who to contact if you were worried about your condition or treatment after you left hospital?, which achieved a correlation of 0.23. When these two items were removed from the core set, the re-calculated Spearman’s rank correlation coefficient for the summative scores was slightly reduced from ρ = 0.92 to ρ = 0.90, which was still statistically significant (p<0.05), and the internal reliability improved a bit to α = from 0.70 to α = 0.87.
The survey responses to the condensed item Were you told in a clear and understandable way how to take your medication and about the side effects to watch for when you went home? indicated that around 33% of patients reported a problem with this experience. In the original HKIEQ, 13% and 38% of patients reported problems with taking medicine correctly and lacking information about side effects, respectively. To have a more precise and differential measures of patients’ experience, it was suggested that the condensed item be changed to match the two original items in the HKIEQ.
The final core set contained 18 items derived from the original HKIEQ, which mainly covered relational aspects of care along four dimensions of a patient’s journey: hospital staff, patient care and treatment, information on leaving hospital and overall impression ( Table 4 ).
https://doi.org/10.1371/journal.pone.0122299.t004
This is the first study to validate a core set of measures for patient experience and satisfaction in Hong Kong. The core set of 18 items, named the Short-Form of the Hong Kong Inpatient Experience Questionnaire (SF-HKIEQ), was derived from the HKIEQ. Through rigorous research, we demonstrated that the SF-HKIEQ is a reliable and valid measure of key aspects of inpatients’ experience; although abbreviated from a much larger questionnaire, it maintains internal consistency and reliability.
That the short-form dramatically increased the survey’s acceptability was demonstrated by its maximum missing values of 1%, compared with the maximum missing values of 10% in the HKIEQ [ 14 ]. The SF-HKIEQ’s high reliability was evidenced by a Cronbach’s α (0.86) which gives it the same internal consistency as the original PPE-15 in England (0.86), and in various other countries (ranged from 0.80–0.87) [ 11 , 12 ]. The item-to-total correlations were also good; the recommended level of 0.3, corrected for overlap, was achieved for all of the items in the HKIEQ. The original version of the HKIEQ had a Spearman’s rank correlation coefficient of p = 0.75 [ 14 ]; the SF-HKIEQ had an even higher test-retest reliability in the 2-week interval of p = 0.92. The analysis demonstrated that the SF-HKIEQ is superior to HKIEQ for individual comparisons, implying its stability in repeated assessments.
Interestingly, the set of core items reflected HK patients’ concerns about the relational aspects of their care, such as privacy, respect, dignity and trust; receipt of clear and understandable information; availability of healthcare staff; emotional support and pain control; and information about medication side effects, danger signs to watch out for, and contact points for post-discharge support. These findings are similar to those of other short-form inpatient experience tools in Europe and the US [ 11 , 20 , 31 , 32 ]. In addition, the SF-HKIEQ further highlights patient concerns about post-discharge support, while the 15-item Picker Patient Experience Questionnaire (PPE-15) in the UK includes items on conflicting information given by healthcare staff and the extent of shared-decision making [ 11 ]. The 24-item Quality from the Patient’s Perspective (short-form of QPP) used in Sweden includes items on waiting time and room characteristics [ 31 ]. The 10-item Generic Short Patient Experiences Questionnaire (GS-PEQ) used in Norway includes items about waiting time, shared-decision making and safe care [ 32 ]; and the 18-item Short-Form Patient Satisfaction Questionnaire (PSQ-18) used in the US includes items on waiting time, safe care, right to access own medical records and having a business-like relationship with healthcare staff [ 20 ]. These differences in health systems, society, culture and values, and patients’ expectations about healthcare quality may influence the psychometric structure of the measuring tool. Our study, therefore, provides some new and important information.
Other aspects of patients’ experience of hospital care, such as access, food and cleanliness of the environment, which are not included in the SF-HKIEQ, reflected their lower priority for HK patients. Surprisingly, the issue of waiting time, which is highlighted in media headlines, was not regarded as a top priority by HK patients. In line with focus group findings, HK patients tend to be more accepting of the need to wait, indicating their appreciation of staff workloads and the pressures on the capacity of public healthcare provision [ 13 ].
The study has some limitations. First, the participants who were recruited for the validation survey were significantly younger and less likely to live in an old age home than the general discharge population. The results when this self-report measure is used to survey all of the users of a public hospital may be different. Second, although the SF-HKIEQ was proved to have good reliability and validity, it only captures the key aspects of inpatient experience, whereas the original version of the HKIEQ collects a comprehensive view of inpatient experience. However, the SF-HKIEQ’s has higher acceptability and may be more accurate than the HKIEQ when used for individual comparisons. Finally, our study used a cross-sectional design; longitudinal studies are needed to establish its sensitivity to change.
The SF-HKIEQ, a locally validated core item scale, has been found to provide a good representative picture of key inpatient experiences in a hospital setting. It also provides an easy and quick mechanism for capturing hospitalization experiences that can be used for continuous quality improvement. The items in the questionnaire have a high degree of face validity, construct validity and internal reliability consistency. We suggest that the short-form instrument can be used to involve both healthcare staff and patients in the monitoring of the quality of hospital care and to heighten their awareness of this important aspect of patients’ lives.
Acknowledgments
This study was commissioned by the Hospital Authority (HA) and we would like to express our heartfelt thanks to HA for giving us this valuable opportunity to develop the core set of questionnaire for measuring patient experience in Hong Kong public hospitals. In particular, we wish to thank all panel experts for their advice on the development of the SF-HKIEQ. We also wish to thank the colleagues of the Department of Patient Relations and Engagement for their assistance in conducting the study. Last but not least, we also wish to thank all staff in the 25 HA hospitals for supporting and coordinating the survey in their hospital and all patients who participated in the survey by providing their valuable opinions and feedback.
Author Contributions
Conceived and designed the experiments: ELYW. Performed the experiments: ELYW AWLC CHKY SFL. Analyzed the data: ELYW AWLC WWST CHKY SFL EKY. Contributed reagents/materials/analysis tools: ELYW AWLC CHKY SFL EKY. Wrote the paper: ELYW AC PH.
- View Article
- PubMed/NCBI
- Google Scholar
- 2. Hurst J, Jee-Hughes M (2001) Performance Measurement and Performance Management in OECD Health Systems.
- 4. Coulter A, Fitzpatrick R, Cornwell J (2009) The Point of Care Measures of patients' experience in hospital: purpose, methods and uses. London, UK: The King's Fund.
- 7. Garratt AM, Solheim E, Danielsen K (2008) National and cross-national surveys of patient experiences: a structured review. Report from Kunnskapssenteret (Norwegian Knowledge Centre for the Health Services) No 7–2008. Oslo: Norwegian Knowledge Centre for the Health Services.
- 8. Care Quality Commission (CQC) (2014) Inpatient survey 2013. Care Quality Commission.
- 9. Picker Institute Europe (2012) Patient & service user experience surveys. Oxford, UK: Picker Institute Europe.
- 10. Gerteis M, Edgman-Levitan S, Daley J, Delbanco TL (1993) Through the Patient's Eyes: Understanding and Promoting Patient-Centered Care. San Francisco: Jossey Bass.
- 15. Linstone HA, Turoff M (2002) The Delphi Method—Techniques and Applications: Addison-Wesley Pub. Co., Advanced Book Program.
- 20. Marshall GN, Hays RD (1994) The Patient Satisfaction Questionnaire Short-Form (PSQ-18). Santa Monica, CA.
- 22. Ware JE (1994) User Manual for the SF12. 2nd edition. Boston: The Health Institute.
- 23. Nunnally J, Bernstein H (1994) Psychometric Theory (3rd ed). New York: McGraw Hill.
- 25. Kline P (2000) A Psychometrics Primer. London: Free Association Books.

- Sales CRM Software
- Application Portals
- Call Center CRM
- Mobile CRM App
- Omnichannel Communication CONVERSE
- Reporting Dashboard SIERA
- Lead Management System
- Opportunity Management
- Sales Process Automation
- Sales Tracking
- Door-to-Door Sales
- Remote Team Management
- Field Sales CRM
- Merchant Onboarding App
- App UI/UX Customizer CASA
- Outside Sales CRM
- Field Force Automation
- Collections Management
- Field Force Tracking
- Event Campaign Management
- Bancassurance Management
- Marketing Automation
- Chatbot - Website
- Chatbot - WhatsApp
- Landing Pages
- Email Campaigns
- Lead Capture Automation
- Lead Engagement
- BTL Marketing Automation
- Advanced Marketing Analytics
- Hospitals and Clinics
- Hospice and Palliative Care
- Fertility Clinics
- Dental Care
- Diagnostics Labs
- ACQUISITION
- Patient Intake Automation
- Patient Appointment Scheduling
- Healthcare Call Center Solution
- Patient Experience Management
- Self-serve Patient Portals
- EHR Integration
- Physician Empanelment
- Security and Compliance
- Patient Engagement
- Higher Education
- Pre-schools and K12
- Training Institutions
- Overseas Education
- Student Recruitment Software
- Admission Portal
- Teacher Onboarding
- Publisher Portal
- Admission Software
- Credit Unions
- Securities and Trading
- Lending CRM
- Loan Origination System
- WhatsApp Lending Bot
- Debt Recovery Automation
- Bancassurance Solution
- PAPERLESS ONBOARDING
- e-KYC Solution
- Video KYC Solution
- Merchant Onboarding
- Merchant Lifecycle Management
- Travel and Hospitality
- Agriculture
- Home Improvement
- View by Industries
- 10 Best Patient Satisfaction Survey Questions

Patients today have high expectations. They want easy appointment scheduling, short wait times, and a seamless overall experience. It’s crucial to understand that even a slight unpleasant experience can cause them to seek care elsewhere.
Now the question arises: How can healthcare professionals ensure they live up to these expectations and provide the greatest experience possible?
Well, instead of speculating, why not ask your patients? They are the ones experiencing the service and are best to uncover what you lack.
And how do you ask the patients?
Patient satisfaction survey questions can be the ideal tool to help you find your areas of improvement.
But first, let’s understand what a patient satisfaction survey is and why you need one.
What is a patient satisfaction survey?
A patient satisfaction survey is a method/tool used to understand patient’s satisfaction levels and experience for the services provided. It typically involves a series of questions designed to gather feedback on various aspects such as; the quality of care, communication with healthcare providers, wait-time, facility cleanliness, and overall satisfaction.
The feedback collected helps healthcare organizations identify areas for improvement and implement changes to ensure patient-centered care .
Why do you need a patient satisfaction survey?
A patient satisfaction survey is essential for several reasons:
1. Collecting feedback for improvement
Patient satisfaction surveys allow patients to express their experiences and concerns. Organizations can address shortcomings and deliver better healthcare services by understanding patient perspectives.
2. Providing patient-centered care
Patient satisfaction surveys enable healthcare providers to adopt a patient-centered approach. By gathering patient feedback, you can better understand patient needs. This information will help tailor services to meet those needs and expectations and provide a more personalized healthcare experience.
3. Measuring team performance
Patient satisfaction surveys help you evaluate the performance of your healthcare organization. It provides data on how smooth the service delivery and interaction with the staff was. This information helps in measuring team productivity and efficiency.
4. Encouraging transparency
Patient satisfaction surveys encourage transparency in healthcare. It ensures that you listen to patients’ concerns and are committed to providing the best patient experience.
5. Improving patient retention and loyalty
Patient satisfaction surveys can also tell how likely patients are to recommend your services to others. This information indicates that patients who are satisfied with the service will recommend others and stay loyal to you. It helps build long-lasting relationships with patients and improve patient retention.
Before we move to survey questions, we first need to understand the metrics one needs to measure from a patient satisfaction survey. These metrics will help you draft the right questions.
Metrics to monitor patient satisfaction
Here are the metrics to measure using a patient satisfaction survey:
Overall satisfaction score
This metric provides an overall assessment of patient satisfaction based on their experience with the healthcare provider or facility.
Likelihood to recommend
Often measured using the Net Promoter Score (NPS), this metric assesses the likelihood of patients recommending the healthcare provider or facility to others.
Communication effectiveness
This metric evaluates how effectively patients can communicate with healthcare providers : For this metric, you can include questions like: – Did you receive all the appointment details well in advance? – Did the provider explain all the information clearly? – Were your questions appropriately addressed?
Wait times
Wait time at the hospital or clinics directly affects patient satisfaction. Measuring this metric helps understand the situation better and find the bottlenecks to address. You may include questions about the time spent in the waiting room, waiting for test results, or waiting for appointments.
Staff courtesy and respect
This metric measures the level of courtesy and respect shown by healthcare staff towards patients.
Facility cleanliness and comfort
Evaluating the cleanliness and comfort of the healthcare facility is also a metric. It includes aspects such as the cleanliness of waiting areas, restrooms, and patient rooms, as well as the comfort of seating, bedding, and other amenities.
Care coordination and information sharing
This metric assesses how well healthcare providers coordinate care and share information with patients. You can include questions on whether patients received clear instructions for follow-up care, were they informed about medication changes, or were they involved in decision-making regarding their treatment.
Accessibility and convenience
This metric measures patient satisfaction with the accessibility and convenience of healthcare services. You can include questions about the appointment scheduling process, ease of getting through to the provider’s office, and availability of convenient appointment times.
Having known the metrics to be included in a patient satisfaction survey question, let’s now have a look at some of the examples for better understanding.
Patient satisfaction survey questions
You need to ask the right questions to effectively track your drawbacks. So here are the top patient satisfaction survey questions to include in your feedback form .
We will present the patient survey questions and explain why these examples are important.
1. How did you find the experience of booking appointments?
a) Very easy
b) Easy
c) Somewhat easy
d) Difficult
e) Somewhat difficult
f) Very difficult
Ask your patients how easy they found to book an appointment at your clinic or hospital. The easier your booking process, the higher is the patient satisfaction.
People who say they found booking difficult are best to find your drawbacks. You can include a follow-up question and ask them what they specifically didn’t like.
Tip to make booking appointments faster:
You can provide online bookings to help patients book appointments easily. Insert lead capture forms on your website and connect it with your healthcare CRM .
Place toll-free contact numbers on your website. Connect it with a call distribution mechanism in your CRM . It can redirect the call to the available agent to avoid any missed calls.
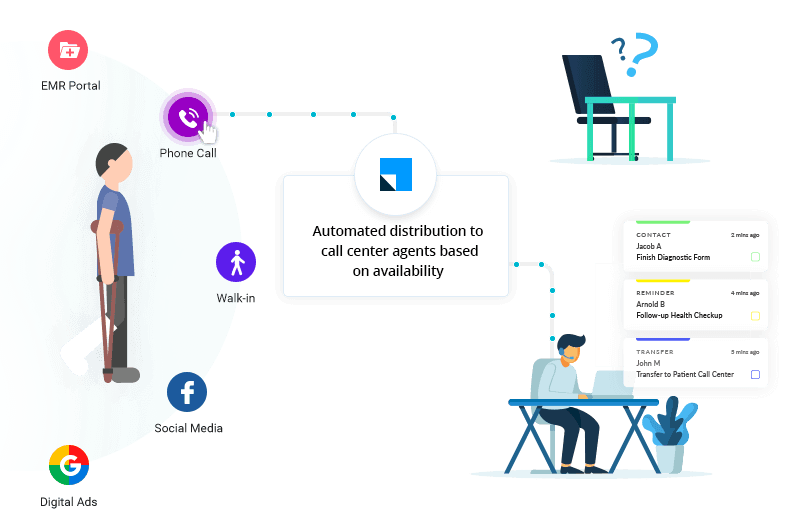
Set up automation to notify representatives and care managers about website form submission or missed calls.
2. Were our staff empathetic to your needs?
a) Vey empathetic
b) Empathetic
c) Somewhat empathetic
d) Not empathetic

66% of patients feel providers don’t take the time to understand patient needs or explain options.
(Source: https://www.prophet.com/patientexperience/the-current-state-of-the-patient-experience.html)
This leaves patients disgruntled as they don’t receive the best care. Also, they might leave you for your competitor. So, always remember to include this question in your healthcare survey.
Tip: Train your staff to be caring and dedicated to patients.
3. How long did you have to wait until the doctor attends to you?
a) As I expected
b) Had to wait more than I expected
Cutting waiting times is one of the main goals of any healthcare organization. You want to serve patients as quickly as possible to provide satisfaction and timely care.
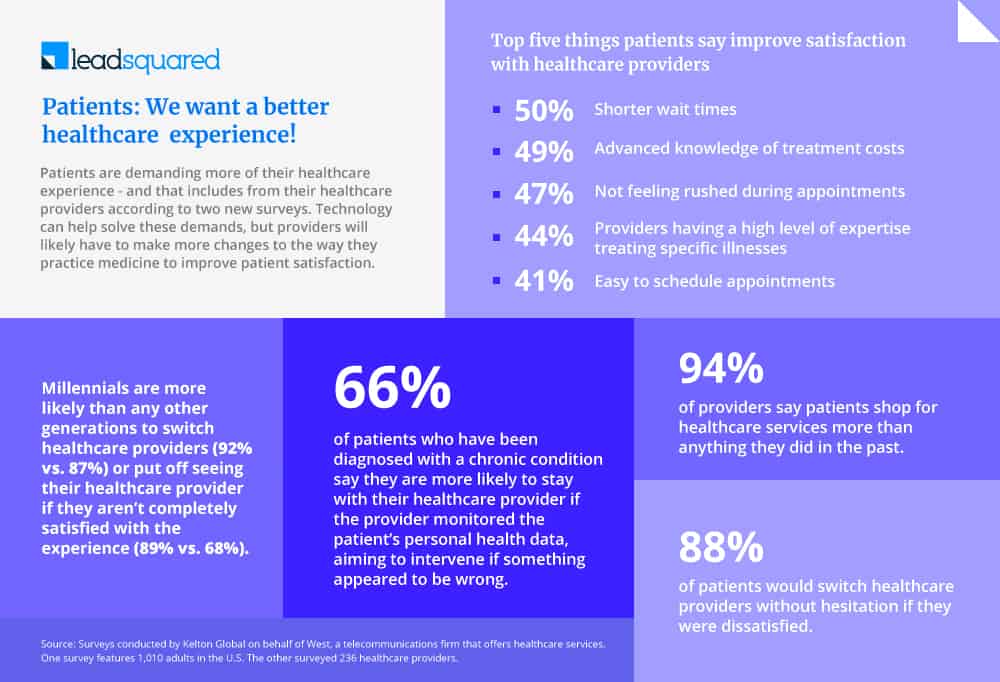
Your wait time should be on par with your industry average. Including this in your patient experience survey question will help you immensely.
Tip to reduce appointment waiting time:
Automate the healthcare process using workflow automation to reduce waiting times.
You can use HIPAA compliant appointment scheduling system to minimize no-shows and improve patient flow .
Manage recurring patients and set up timely reminders for patients to ensure availability.
4. Were you satisfied with the doctor you were allocated with?
a) Somewhat satisfied
b) Satisfied
c) Somewhat satisfied
d) Dissatisfied
e) Very dissatisfied
Healthcare organizations recommend the best doctor based on the data collected or patient requirements. However, the recommendations may not always be effective. It’s important to ask this question so that you can improve your doctor’s recommendation process.
Tip to automate and map doctor-patients:
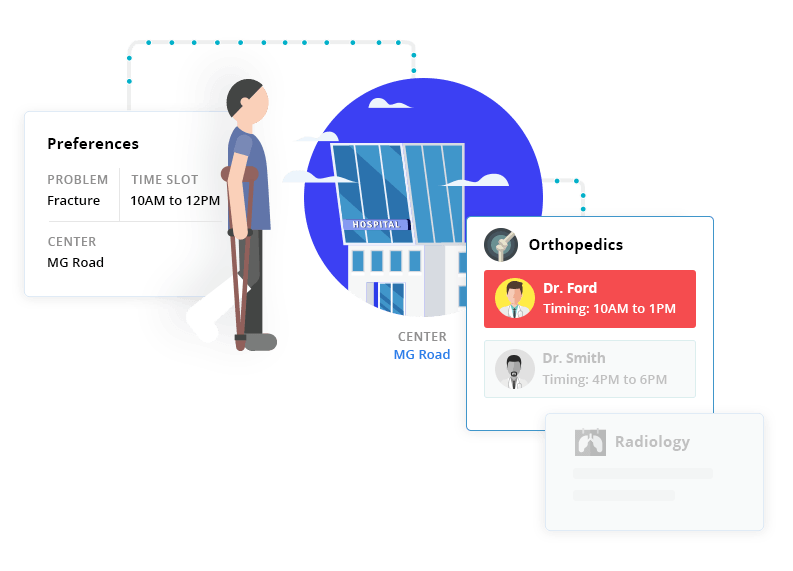
Map patients to doctors of your or their choice using distribution mechanisms in CRM. Using the patient inquiry form automate on the mapping on the basis of region, time, specialty, medical history.
5. How easy is it to navigate our facility?
A lot of time is wasted in finding the right doctor’s room or the X-ray room in a facility. The staff is also not always around to help out. Improving facility navigability improves patient satisfaction, reduces response times, and speeds up care delivery.
Tip: Use signs and maps to help patients find their way.
6. How happy are you with the doctor’s treatment?
a) Happy
b) Somewhat happy
c) Okay
Sometimes, patients are not treated well by doctors. Maybe they are too busy, or they just view patients as a business. If certain doctors are bringing a bad name to your establishment, it’s time for a change.
Tip: To overcome this challenge, ensure to onboard the right doctors. Also allocate enough time between appointments so that the doctor can spend time with patients and understand them without any hurry.
7. Were we able to answer all your questions?
a) Somewhat yes
b) Yes
c) Some questions left unanswered
d) No
It’s vital to resolve all your patient queries to provide good service. A patient will obviously not be at ease when he has questions about his health.
Your website is the best place to answer all common questions of patients. Additionally, make sure your staff picks up the phone and replies to emails.
Use the healthcare marketing system to build landing pages, automate emails to build lasting relationships.
8. How likely are you to recommend us to your friends and family?
It’s something you need to ask all your patients. For one, it gives you an insight into the overall impression they have of your practice.
a) Very likely
b) Likely
c) Somewhat likely
d) Not very likely
e) Never
This question directly helps you discover how your patients feel. If someone is ready to recommend your business, then obviously you are doing a good job.
9. How much do you rate us? (5 being the highest rating)
This one’s a simple rating, but it tells you where you are in the customer experience journey.
a) 1
b) 2
c) 3
d) 4
e) 5
Rating is another direct way to measuring patient satisfaction. If someone gives a bad rating, you can ask them to mention what they didn’t like.
10. What are the things you feel we should improve upon?
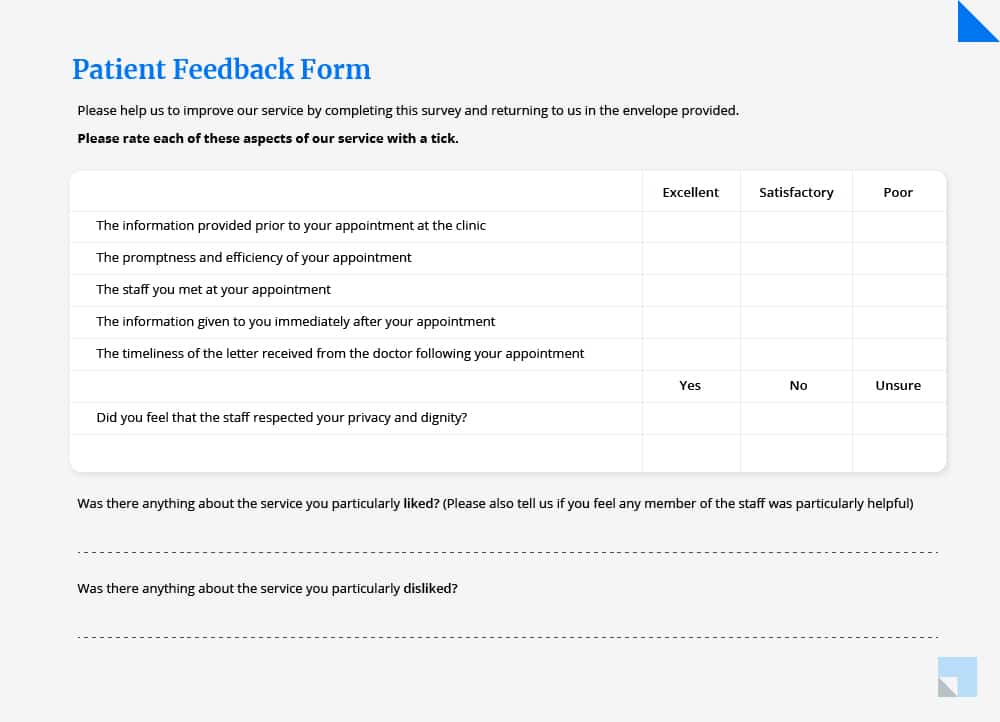
This is a perfect health care satisfaction survey question that gives you the opportunity to discover what the patients don’t like. Just provide a blank space after the question so that patients can type in their answers.
Tip: Take cues from patients and improve your shortcoming to enhance the patient experience and patient care.
ChatGPT prompt for patient satisfaction survey
AI is nearly changing everything, and it’s amazing how you can use it to improve the efficiency of your daily work. One such great example is ChatGPT.
If you want to create your own personalized patient satisfaction survey questions, you can try doing it through ChatGPT. You use it to build case specific questions like to measure satisfaction for IPD and OPD patient separately. Below are a few prompts to get you started:
Prompt 1: Write 10 patient satisfaction survey questions for outpatient feedback with 5 options to rate it on a scale of 1-5.
Prompt 2: Write 10 patient satisfaction survey questions to measure post-operative support provided by the hospital with 5 options to rate it on a scale of 1-5.
Prompt 3: Write 10 patient satisfaction survey questions for inpatient feedback with 5 options to rate it on a scale of 1-5.
Be creative and create different surveys for different departments to understand the exact problem statement and improve patient experience.
Automate Feedback Gathering with Healthcare CRM
HIPAA Compliant Healthcare CRMs like LeadSquared can automate the whole process of collecting patient feedback. You can send feedback forms and surveys via emails, text, or notifications.
The solution also helps track patient satisfaction survey questions. You can manage customer interactions and perform better healthcare marketing .
You can even automate your operations, patient management, and a plethora of tasks. Get in touch with us to know more about how LeadSquared can help your healthcare business grow.
Patient satisfaction score is the metric used to understand the satisfaction level of patients for the care provided. You can measure it using patient satisfaction surveys where patients rate their experience on a scale of 1-5.
Yes, patient satisfaction is an important KPI for healthcare organizations. It helps you to understand if the patients are satisfied with the quality of service, interaction with the staff or with overall care provided. Patient satisfaction is a direct indicator of the growth and success of a healthcare organization.
The Net Promoter Score (NPS) is a single-question metric that measures how patients feel about your healthcare organization and the services it offers. The usual question asked is: How likely are you to recommend [hospital name] to a friend, family or colleague? It also acts as an important indicator for the growth of your practice.
- EHR integration with healthcare CRM software

Awantika is a healthcare marketer with LeadSquared. She has been a part of the content and product marketing game for almost 3 years. You can connect with her on LinkedIn or write to her at [email protected].
Table of Contents
- Share on Facebook
- Share on Twitter
- Share on WhatsApp
- Share on LinkedIn
Want to see LeadSquared in action?
- Customer Portal
- Performance Management
- Dev Platform LAPPS
- Help Portal
- Pricing SALES
- Pricing MARKETING
- Education CRM
- Healthcare CRM
- Insurance CRM
- Banking CRM
- Real Estate
- Marketplace CRM
- Manufacturing CRM
- What is CRM
- What is lead management
- What is vendor management
- What is sales management
- Case Studies
- Guides & Blogs
- Compare CRM
- CRM Glossary
- Sales Glossary
- Media & News
GET IN TOUCH
(+1) 732-385-3546 (US)
080-46971075 (India Sales)
080-46801265 (India Support)
62-87750-350-446 (ID)
- Legal & Compliance

NHS Patient Surveys
This website provides information and documentation to help healthcare organisations and approved contractors implement the surveys across the NHS Patient Survey Programme. You can also find published results from all our surveys and read about why you received a questionnaire.
Find survey materials and reports
Information, documentation and results for the current surveys running within the NHS Patient Survey Programme
Access survey data
Download data and results from recently published surveys across the NHS Patient Survey Programme
Received a questionnnaire?
Read about why you were sent a questionnaire and how your personal information is used
Survey instructions
Generic information and guidance relevant to all surveys across the programme
NHS Trust FAQs
Answers to common questions on running a survey
Approved contractors
Organisations approved by CQC to conduct a survey on behalf of an NHS Trust
Search Picker
Home Research & insights The Cancer Patient Experience Survey shows overall experiences have improved, but more support is still needed
The Cancer Patient Experience Survey shows overall experiences have improved, but more support is still needed
The vast majority of people living with and beyond cancer rate their overall NHS care highly – despite tens of thousands not receiving enough care, support, or practical advice.
These are the results of a new survey of more than 67,000 people. The research – conducted prior to the Covid-19 pandemic – asked people living with and beyond cancer about all aspects of their care and treatment.
Overall, 95% of patients rated their care as seven or above out of ten – one of the key positive results the survey includes from throughout people’s cancer care journeys. Results showed a significant improvement in the proportion of people who felt they were told sensitively that they had cancer (86% in 2019 up from 85% in 2018). More than nine in ten (92%) were given the name of a Clinical Nurse Specialist who would support them through their treatment, and 85% found this person very or quite easy to contact. Almost all (94%) had hospital staff tell them whom to contact if they were worried about their condition or treatment after leaving hospital.
While these are very welcome results, some key areas still need to be improved. Only two thirds (67%) of patients were definitely offered practical advice and support in dealing with side effects from treatment, and only 52% were definitely given enough care and support from health or social services during their cancer treatment. 37% were not given information about how to get financial help or benefits from hospital staff. This means many people have been left struggling with side effects or financial difficulties at a time when they are most vulnerable.
There were also gaps around care planning and communication. Only 38% of respondents said that they were given a written care plan setting out their needs and goals to care for them. Whilst this was an improvement from 35% in 2018, it continues to fall short of the ambition set out in the NHS Long Term Plan for Cancer that “by 2021, where appropriate, every person diagnosed with cancer will have access to personalised care, including needs assessment, a care plan and health and wellbeing information and support.”
Commenting on the survey, Chris Graham, CEO of Picker, said:
The annual national cancer patient experience survey is a vital window into the experiences of people receiving cancer care through the NHS. This year’s results show that most people report good experiences overall, and broad satisfaction with clinical services is improving from a high base. This is great news – but it is a concern that there remain significant gaps in the wider care and support that people are given. A cancer diagnosis can be a life changing experience with wide implications not just for a person’s health but also their broader wellbeing – and so it is important that people are able to access comprehensive support that addresses their circumstances. These survey results provide important insight, and all NHS organisations should take careful note of their findings. But it’s also important to acknowledge that the survey was conducted before the coronavirus pandemic and lockdown, which will create new challenges for the provision of cancer services. In responding to these, it’s vital that providers focus on the things that matter most to patients – including the eight dimensions of the Picker Principles of Person Centred Care
Each year the number of new cancer diagnoses in England continues to increase, with over 320,000 new cases in 2018 and an average of 878 new cancer diagnoses on average each day of 2018*. According to the PHE Cancer Board Plan 2017-2021 patient experience is as important as safety and clinical effectiveness: “How patients experience the care pathway and to what extent they can make informed decisions are fundamental to their quality of life while living with and beyond cancer and at the end of life”. We call on all NHS providers to review the survey results to identify areas for improvement in people’s experiences.
*Source May 2020 Cancer registration statistics
Notes to editors
- The 2019 Cancer Patient Experience Survey was conducted by Picker on behalf of NHS England and NHS Improvement.
- The survey is a crucial source of information for healthcare professionals working to improve the care of people using England’s cancer services. The 2019 survey was the 9th iteration of the national survey, which monitors progress on cancer care and informs quality improvements and the work of cancer charities and stakeholder groups.
- A total of 143 NHS Trusts across England that provide cancer care took part in the survey.
- 67,858 patients responded to the survey (61% response rate).
- Full details of the survey methodology, questions, and results are available on the dedicated survey website.
Related research and insights
Cardiomyopathy uk will partner with picker to evaluate the care experience of those living with cardiomyopathy in 2024..
Community Mental Health Survey 2023 Infographic
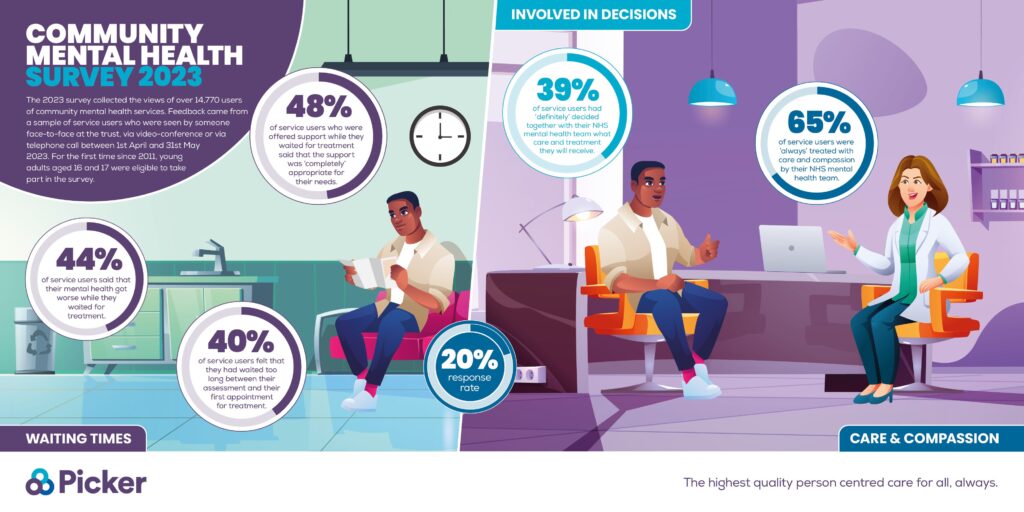
Talk to us about person centred care
Sign up to our newsletter, privacy overview.
The Handbook Reviews Team has thoroughly researched and tested the products and services we write about and may earn a commission based on purchases made.
Rex MD Review: Expert Reviewed in 2024
We mystery-shopped 26 telehealth providers of ED medication to help you determine the best option for you. Here’s our experience with Rex MD.

A healthy sex life can be an important component of overall mental health. Erectile dysfunction (ED) is a common condition, affecting about 30 million U.S. men *. ED does more than just impact physical capabilities; it deeply influences mental health, contributing to feelings of anxiety, depression, and diminished self-esteem .
Rex MD offers a streamlined, discreet avenue for obtaining ED treatment online—though it’s always best to see your doctor first to rule out related medical issues and fully understand how these treatments could affect you. By providing access to licensed health care professionals and personalized prescription medication plans without the need for an in-office visit, Rex MD aims to alleviate the stress and stigma often associated with seeking help for ED. Whether you feel uncomfortable speaking to a provider in person or you simply live far away from a doctor’s office, telehealth ED care can reduce barriers to health care and foster a sense of empowerment among patients.
Although the causes of ED may be complicated, successful treatment is possible. Judy Scheel , a psychotherapist specializing in sexual and intimacy issues, explains, “Our bodies often convey through symptoms what we have difficulty articulating in our hearts and minds; be patient with yourself, be curious about the cause, have realistic expectations about medicine, understand that communication with a partner often helps the person with the ED to feel less pressure, shame and expectation and judgment.”
Our October 2023 survey of 360 men who sought ED treatment from online providers like Rex MD found that most patients report improvement in overall mental health and self-esteem after initiating treatment. Let’s take a look at exactly what is involved with utilizing Rex MD’s telehealth ED treatment services.
*For brevity, we refer to all people assigned male at birth as men throughout this guide.
Rex MD overview

- Cost : $1.80–$10 per pill, on a recurring subscription.
- Prescribes medication: Yes.
- Medications offered: Sildenafil (generic Viagra) and tadalafil (generic Cialis).
- Delivery : Two-day free shipping in discreet packaging.
- Accepts insurance: No.
Insights from our testers
Rex MD is an easy-to-use telehealth platform for ED treatment. It offers two medications: sildenafil (generic Viagra) or tadalafil (generic Cialis) . There is no difference in the contents of the generic and brand-name option medications. Sildenafil is offered in 50- or 100mg single-dose tablets, and tadalafil is offered in 10- or 20mg single-dose tablets or 2.5- or 5mg daily-dose tablets. The choice between the two medications will depend on your medical history and preferences.
Sildenafil is fast-acting, taking 30–60 minutes to take effect and lasting four to six hours. It should be taken on an empty stomach. Tadalafil is slower-acting, taking one to two hours, but it is effective for longer (around 36 hours) and can be taken with or without food. If you plan on engaging in more spontaneous sexual activity, you may take a daily low dose of tadalafil.
Here’s a breakdown of the ordering process with Rex MD:
- Sign up and questionnaire.
The journey begins with a simple signup process on the Rex MD website, where you fill out a detailed health questionnaire consisting of 32 questions. Towards the end of the questionnaire, you indicate which medication and dose you prefer.
Our tester flagged a few possible concerns with the intake questionnaire. Proof of identity or age isn’t required (unlike other online medication suppliers like Lemonaid Health ), so prescriptions can possibly go to unapproved patients. Also, you are asked if your blood pressure is low, normal, high, or very high rather than having to provide the numerical reading. This means that patients may not obtain real, recent blood pressure readings, which could be dangerous because these medications are high-risk for those with higher blood pressure.
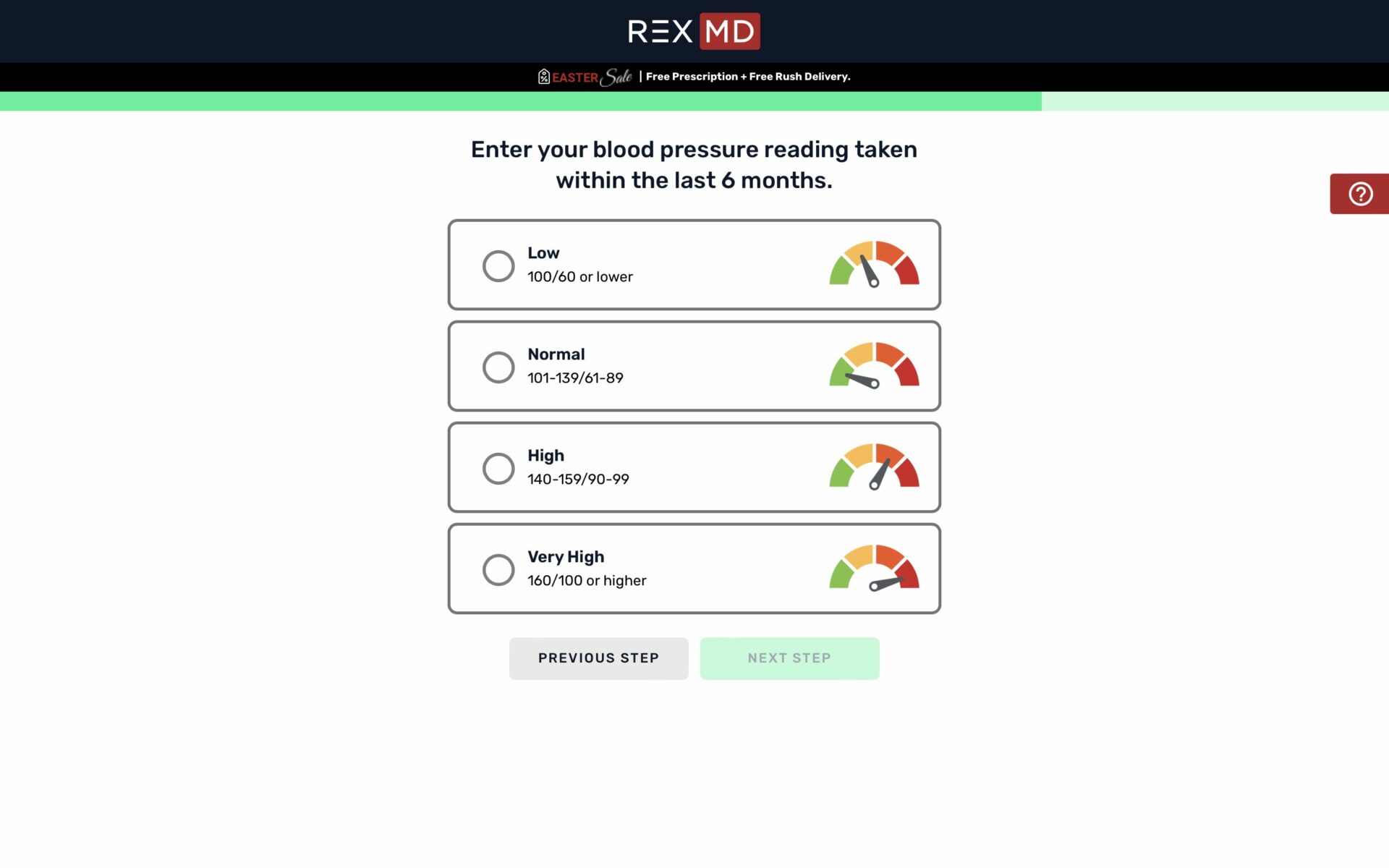
- Provider review and medication shipment .
Depending on your state’s laws, a provider will review your answers and immediately provide a prescription or request a phone or video consultation. In Colorado, we were given a prescription right away. Shipping is free and takes only two days. The packaging is discreet, consisting of brown cardboard with no labeling. The shipping is notable because our survey found that discreet packaging is one of the most important factors in determining which online medication supplier to use.
- Ongoing care and future prescriptions .
After the first order, you are automatically put on a recurring shipping schedule every one, three, six, or 12 months, depending on the time frame and amount you selected during the questionnaire. Some users may find this convenient, while others may prefer to place subsequent orders when needed and not be tied to a subscription. While we wish that there was an “as-needed” service to select, you may cancel or delay your subscription at any time by calling Rex MD or messaging the patient portal.
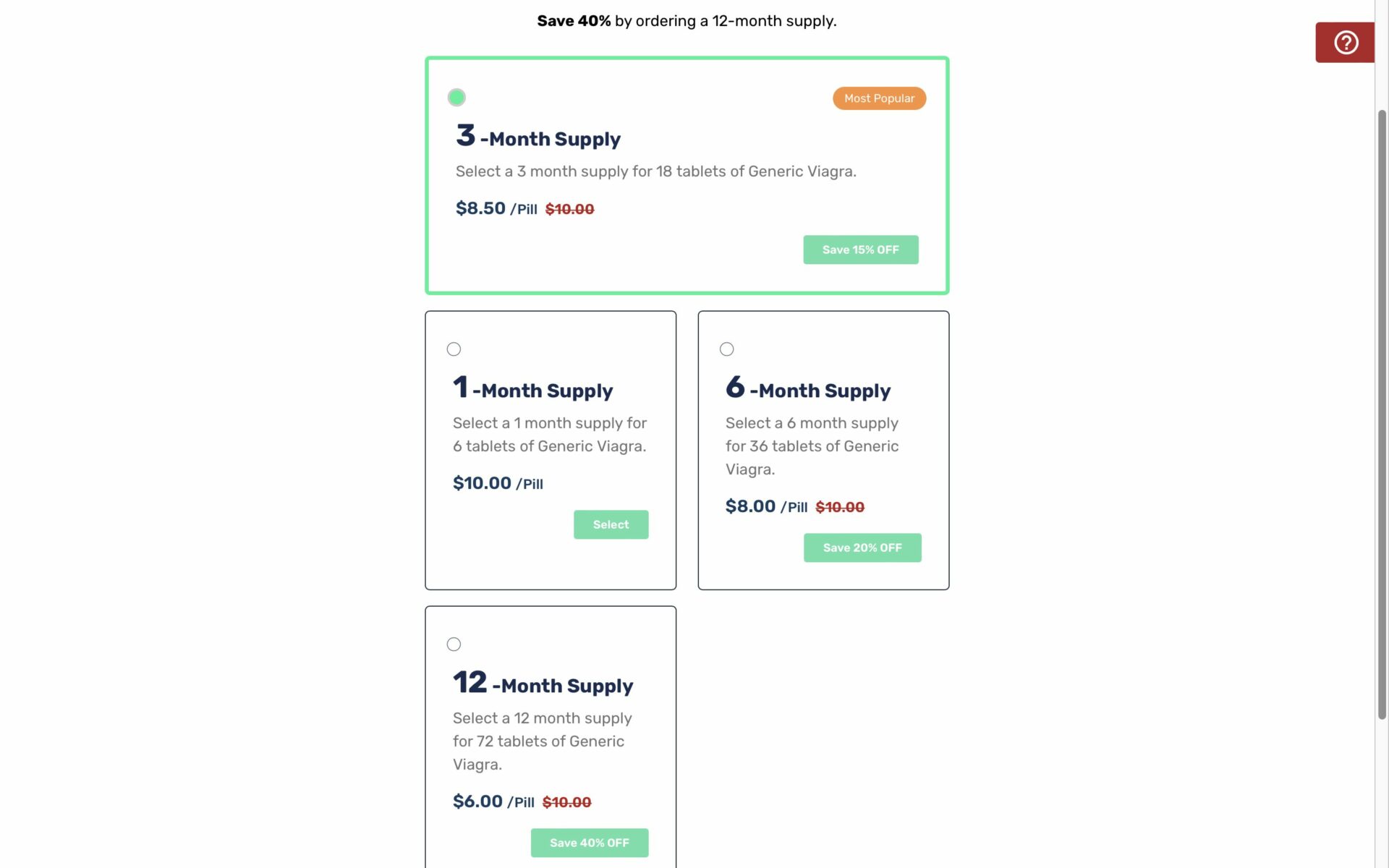
Free follow-up care is available through the patient portal. We found that Rex MD providers efficiently and thoroughly answer patient questions. Yearly consultations are required to reevaluate your medical history and medication needs to determine if your prescription is still right for you.
Overall, our tester found their experience with Rex MD overwhelmingly positive. The service destigmatizes seeking help for ED, providing a solution that is both accessible and reliable. The convenience of having consultations and receiving medication without leaving home, combined with the discreet and professional nature of the service, makes Rex MD a good option for anyone seeking support for erectile dysfunction.
We caution that streamlined online medical services like Rex MD may miss other serious health conditions because no physical exam is required. You are also not as likely to develop a close relationship with your provider, especially if no phone or video consultation is conducted.
“In a perfect world, people would have access to in-person care. Although telehealth has created tremendous opportunities for people, it can also increase detachment from actual relationships. A condition as sensitive as ED would likely benefit from the initial appointment bedding in person so that the prescribing practitioner can get to know the patient, make a proper assessment, and perhaps, most importantly, make a connection,” explains Scheel.
Whether you decide to seek ED meditation in person or through an online platform comes down to personal preference and comfort level. Those with more complicated medical histories may want to consider in-person care, at least for the initial consultation.
What other users are saying
Rex MD is the fifth most popular online ED treatment platform our October 2023 survey respondents tried, with Hims and GoodRx being the most popular. Most men we spoke with are pleased with their experience with telehealth ED medication providers like Rex MD—over 76 percent of respondents are “very satisfied” with their experience
Many men wish they had not waited so long to seek care. In October 2023, we conducted a focus group of men who had used online telehealth services for ED medication. One told us, “I thought something was wrong with me that shouldn’t be. I was embarrassed to even talk about it with my primary care physician, which, in hindsight, is crazy. There was a stigma associated with this thing that I definitely didn’t want anybody else to know.”
HelpGuide Handbook’s erectile dysfunction testing methodology
The Handbook Team has tested 26 telehealth platforms that offer prescription medication for erectile dysfunction. Our team acts as mystery shoppers to compare each platform’s screening process, navigation, cost, delivery time, and restrictions. Our testers complete the sign-up process, fill out questionnaires, click through all educational information, and note available medications and dosages.
To learn about what happens after someone submits their information to a provider, our team has surveyed 360 men who have gotten erectile dysfunction medication online. The team also holds multiple focus groups with real users to get more candid responses about the effects of erectile dysfunction treatment.
To learn more about how we review ED medication platforms and treatments, read our full erectile dysfunction methodology .
The Handbook
If you learn five things about Rex MD for erectile dysfunction treatment, here’s what you should know:
Compare Rex MD with other online ED platforms
Rex md cost and payment options.
Rex MD currently only offers the generic versions of Viagra (sildenafil) and Cialis (tadalafil). The cost is determined by the amount purchased. Orders automatically renew in the timeframe chosen at the time of purchase (one, three, six, or 12 months). You can cancel your subscription anytime by calling or messaging through the patient portal.
For single-dose sildenafil (50mg or 100mg) and tadalafil (10mg or 20mg), the cost is:
- $6 per pill for 72 tablets every 12 months.
- $8 per pill for 36 tablets every six months.
- $8.50 per pill for 18 tablets every three months.
- $10 per pill for six tablets every month.
For daily-dose tadalafil (2.5mg or 5mg), the cost is:
- $1.80 per pill for 360 tablets every 12 months.
- $2.40 per pill for 180 tablets every six months.
- $2.91 per pill for 90 tablets every three months.
- $3 per pill for 30 tablets every month.
Payment options
As with most telehealth ED medication providers, Rex MD does not accept insurance. Payment is accepted through PayPal, Visa, Master Card, American Express, Discover, or an HSA/FSA card. If you’re looking for an online ED treatment platform that accepts insurance, try PlushCare .
Our final verdict
Rex MD can offer a convenient solution for men seeking ED treatment, integrating the ease of online consultations with the reliability of direct, straight-to-your-door shipments. Our Handbook Team likes that a licensed medical professional reviews your medical history before providing a prescription but warns that the lack of a physical exam may lead to missed medical concerns or connection between patient and caregiver. The subscription model eliminates the need to reorder medication manually, but some individuals may prefer receiving their medication as needed instead of recurring shipments. Overall, we think Rex MD can be a good option for men seeking a discreet and convenient approach to managing ED.
Frequently asked questions
Does rex md operate on a subscription model.
Yes, Rex MD operates on a subscription model, allowing customers to receive their ED medications on a regular basis. You can cancel or delay your subscription at any time by calling or logging in to the patient portal.
Do I need a prescription to use Rex MD?
Yes, a prescription is necessary to use Rex MD. The service includes an initial consultation with a licensed health care professional who evaluates your medical history to determine the most suitable treatment plan. If medication is deemed appropriate for your situation, a prescription will be issued, which Rex MD can fulfill.
Is Rex MD legitimate?
Rex MD is a legitimate telehealth service specializing in the treatment of ED. It connects patients with licensed health care professionals in their state, offering a legal and safe pathway to obtain ED medications.
Does Rex MD have Viagra or Cialis?
Rex MD provides access to two popular FDA-approved ED medications: generic Viagra (sildenafil) and generic Cialis (tadalafil).
- U.S. Department of Health and Human Services. (n.d.) Definition & facts for erectile dysfunction. National Institute of Diabetes and Digestive and Kidney Diseases. Link
- Quang, N., Van Truong, L., Chung, E., Van Quang, B., Quang Long, L., Thanh Ngoc, N., Anh Minh, N., Mai Anh, D., Nguyen Dinh Thanh, N., & Truong Nam, N. Predicting Anxiety and Depression Among Erectile Dysfunction Patients: A Cross-Sectional Study. American Journal of Men’s Health. (2024; January). 18(1). Link
- HelpGuide Erectile Dysfunction Survey. 360 respondents. Conducted using Pollfish. Launched Oct. 26, 2023.

IMAGES
VIDEO
COMMENTS
Consistent with the need to capture patient-reported data during a relatively rapid surgical pathway, the researchers chose to develop a questionnaire focused on the key themes that emerged from the results of the qualitative study previously conducted [].The questionnaire was developed by the first three authors to capture data on the following patient journey touchpoints: preadmission ...
Patient journey mapping can increase your bottom line by laying the foundation for improved patient satisfaction and higher retention. Organizations across all industries are looking to understand customer journeys in order to attract and retain customers by gaining deeper insights into what drives the consumer experience.
The patient journey is the entire sequence of events that begins when the patient first develops a need for clinical care and engages with your organization. It follows the patient's steps as they navigate your healthcare system, from initial scheduling to treatment to continuous care.
Six underlying metrics which patient satisfaction should be measured on are: Quality of medical care. Interpersonal skills displayed by medical professionals. Transparency and communication between care provider and patient. Financial aspects of care. Access to doctors and other medical professional. Accessibility of care.
The current study was carried out with two different paper-and-pencil questionnaires delivered to the same patients at two different stages of the hospital patient journey. The first questionnaire was developed on purpose by the authors and completed by the patients at the time of admission to the hospital and at the end of hospitalisation.
The Patient Satisfaction Questionnaire is more than just a feedback form; it's an essential bridge that connects patient experience with healthcare excellence. This tool reflects the patient's journey within a healthcare facility by assessing various facets of medical service.
The Experience Journey of the Patient. A recurrent and prominent theme in discussions of the patient experience is centering the patient's perception or perspective on the health care they receive (7,13).Health-care providers who seek to understand the patient's perspective of their experience will obtain a greater understanding of the patient experience.
Patient Journey Mapping is a strategic tool in healthcare that visually illustrates the entire patient experience, from initial contact to post-treatment follow-up. It involves mapping out key touchpoints and stages, such as appointment scheduling, diagnosis, treatment, and aftercare. ... Filling out the pre-appointment questionnaire is time ...
The patient journey is best described as the sequence of experiences a patient has from admission to discharge. This includes all the touchpoints between the patient and provider from beginning to end. A patient's journey begins before they even walk through the doors of a doctor's office or hospital. It may start when they research ...
Process mapping enables the reconfiguring of the patient journey from the patient's perspective in order to improve quality of care and release resources. This paper provides a practical framework for using this versatile and simple technique in hospital. Healthcare process mapping is a new and important form of clinical audit that examines how we manage the patient journey, using the ...
Introduction. All patients want and deserve a good experience of care. Patient experience is a key quality outcome, which can be used to improve quality, governance, accountability and choice.1 However, it is also a complex, multiattribute concept that reflects patients' perceptions and experiences of receiving care. A short definition of patient experience is the sum of all interactions ...
4. Identify Contact Channels. Patients engage with the health center through various channels throughout the patient journey. These channels, such as the health center itself, can be physical or online, including social media, email, applications, websites, and online forms.
The 18 items mainly covered relational aspects of care under four dimensions of the patient's journey: hospital staff, patient care and treatment, information on leaving the hospital, and overall impression. ... (2002) The Picker Patient Experience Questionnaire: development and validation using data from in-patient surveys in five countries ...
3. Measuring team performance. Patient satisfaction surveys help you evaluate the performance of your healthcare organization. It provides data on how smooth the service delivery and interaction with the staff was. This information helps in measuring team productivity and efficiency. 4. Encouraging transparency.
The 18 items mainly covered relational aspects of care under four dimensions of the patient's journey: hospital staff, patient care and treatment, information on leaving the hospital, and overall impression. ... while the 15-item Picker Patient Experience Questionnaire (PPE-15) in the UK includes items on conflicting information given by ...
The Questionnaire. A good questionnaire for your patients is the next major step of the patient journey. A questionnaire lays the foundation of information to be used during the exam. It's important that the questionnaire isn't only about vision, but also about lifestyle, and digital eye strain symptoms.
Patient journey mapping projects have been undertaken using a variety of data collection and analytical approaches that have included physically tracking patients' movements through health services (Barton et al., 2019), interviewing or surveying patients, family members and healthcare workers about experiences of navigating a health system or ...
Patient journey and data collection. values represented by emoticons = bad experience; = great experience); v) Positive or negative emotions experienced at the moment of completing the questionnaire by choosing the main ones from the Plutchik's wheel: serenity, trust, anticipation, apprehension, fear and anger.
We used a Delphi consensus methodology to describe the trajectory of patients with AD through routine care in our area. Figure 1 shows an overview of the approach to defining the patient journey. The Delphi questionnaire, developed in a focus group meeting based on a state-of-the-art internal report, was structured into three blocks covering relevant stages of the trajectory of AD: (1) from ...
Background This study was aimed to preliminary validate a cross-disease psychometric measure to assess the psycho-social experience of family caregiver engagement in healthcare (Caregiving Health Engagement Scale, CHE-s), which refers to the caregiver's psychological attitude to be an active, skilled and motivated player in the care process of their loved ones. Method The study consisted of ...
We first constructed a patient journey map (PJM) for easy verification of disease treatment data from the perspective of the patient. ... Traditionally, common ways to measure the UX of an interactive product include the AttrakDiff questionnaire, the User Experience Questionnaire (UEQ), or the modular evaluation of key Components of User ...
NHS Patient Surveys. This website provides information and documentation to help healthcare organisations and approved contractors implement the surveys across the NHS Patient Survey Programme. You can also find published results from all our surveys and read about why you received a questionnaire.
Overall, 95% of patients rated their care as seven or above out of ten - one of the key positive results the survey includes from throughout people's cancer care journeys. Results showed a significant improvement in the proportion of people who felt they were told sensitively that they had cancer (86% in 2019 up from 85% in 2018).
Rex MD is the fifth most popular online ED treatment platform our October 2023 survey respondents tried, with Hims and GoodRx being the most popular. Most men we spoke with are pleased with their experience with telehealth ED medication providers like Rex MD—over 76 percent of respondents are "very satisfied" with their experience.
Approximately 500,000 babies are born with sickle cell disease each year, although most patients in low- and middle-income countries remain undiagnosed until they experience symptoms. The program needed a new leader, and on January 1, 2023, Jane Hankins , MD, left the Department of Hematology to join the Department of Global Pediatric Medicine ...
Speaking up by healthcare providers is an essential assertive communication strategy for ensuring patient safety and preventing incidents. However, more is needed to know about speaking up and instruments to assess it in the Korean context. Therefore, we assessed the psychometric properties of the Korean version of the Speaking Up about Patient Safety Questionnaire (KSUPS-Q) for measuring ...