- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2023 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support

What to Expect at Your First Psychiatrist Appointment
Amy Morin, LCSW, is a psychotherapist and international bestselling author. Her books, including "13 Things Mentally Strong People Don't Do," have been translated into more than 40 languages. Her TEDx talk, "The Secret of Becoming Mentally Strong," is one of the most viewed talks of all time.
:max_bytes(150000):strip_icc():format(webp)/VW-MIND-Amy-2b338105f1ee493f94d7e333e410fa76.jpg)
Prepare for the First Appointment
Make a list of concerns, during the appointment, after your first appointment, frequently asked questions.
It's normal to be a little nervous when you go to your first appointment with a psychiatrist, psychologist , or another mental health professional . You're probably not sure what to expect, which can lead to making you feel out of control.
While it can be nerve-wracking, there is nothing to fear. Your psychiatrist is there to help you learn more about the process and help you decide which steps to take next. It might take some time to find the right psychiatrist for you , but your mental health is worth the investment of time and energy.
This article discusses what you can expect during your first psychiatrist appointment. It covers how to prepare for your appointment, what to bring, and what you should do during and after your visit.
It's normal to feel a bit apprehensive before your first psychiatrist appointment. After all, discussing sensitive personal information with a stranger can be daunting for anyone. Your psychiatrist is a highly trained professional who is there to help, and there are steps you can take to make your first appointment a success.
Paperwork and Payment
Before your first psychiatrist appointment, you'll need to provide some basic information about yourself, such as your contact information, medical history, and insurance information. It may be possible to do this online before your appointment, but you can also often do this at the office when you arrive.
You should also sort out your payment details before your first appointment. Check with your insurer beforehand to see if your visit will be covered. Your insurance provider can also tell you if you need to get a referral from your primary care provider before your appointment.
Schedule your first appointment at a time when you can have a relaxed conversation with your psychiatrist. Avoid scheduling appointments when you're likely to be tired or stressed.
Medical History
Write down important information about your medical history. This should include:
- Any mental health diagnoses
- Medications you're taking
- Any psychiatric hospitalizations
- Any past therapy or treatment for a mental health condition
If you have any medical conditions that might affect your mental health, such as thyroid disease, diabetes, or heart disease, be sure to mention them to your psychiatrist.
Family medical history can also be relevant, so be sure to note if there is a history of psychiatric issues in your family.
Doctor's Questions
Your psychiatrist will want to know why you are seeing them, so they will ask questions such as:
- "Can you tell me what brings you here today?"
- "How are you feeling?"
- "What do you need help with?
- "What can I do to help you?"
The purpose of asking these questions is to get a better idea of your symptoms and their effects on your life. To prepare for your appointment, you might find it helpful to write down some of your symptoms to feel better able to answer these types of questions.
Pre-Appointment Anxiety
Your anxiety over this first appointment may be causing you to assume the worst or think treatment will be tougher than it actually is. For instance, you may think you have too many problems to tackle.
However, the reality is that your therapist will likely focus on just one or two issues, to begin with and move on from there. Being prepared for your first appointment can help you manage your anxiety and nervousness.
You can prepare for your first appointment by filling out paperwork, taking care of payment details, writing down your medical history, and thinking about questions your psychiatrist might ask. Remember that some nervousness is perfectly normal, and your therapist is there to help.
Prior to your appointment, make a list of everything you are feeling and any questions you have for your doctor or healthcare professional. You will also want to write down any details about triggers, as well as how your life is affected by each item.
For example, if you're feeling paranoid , you need to list not just the feeling but what you feel paranoid about and how it affects your life. List exactly what you are feeling and experiencing and how your life is affected.
When you break down your feelings and how they are affecting your daily life, you paint a very clear picture for the doctor. It's very difficult to do that on the spot in a short visit when your brain is spinning and you aren't prepared, so make the list ahead of time.
Try to avoid putting labels on your feelings or triggers as you talk to your therapist. Let the doctor do that. Therapists could inadvertently be influenced by your labels, affecting their diagnosis or treatment recommendations.
There are a number of things you can do during your appointment to make the process easier and ensure that you are getting the most out of the experience.
Be Open and Honest
It's important to be candid with your psychiatrist. In order to provide the best possible care, you need to be as honest and open as you can.
This often means talking about sensitive information of a highly personal nature. You might discuss topics such as your sexual history, family relationships, and drug use. While this may be difficult to share, it is important to remember that your psychiatrist can provide appropriate treatment unless they fully understand your situation.
Ask Questions
If you need more information or don't understand something your psychiatrist has said, ask for clarification. You might ask questions in the moment, or you might write them down so you can discuss them later.
Bring a Supportive Person
If you're feeling anxious about your first appointment, you may want to bring a supportive friend or family member with you. This person can provide emotional support and can help you remember what the psychiatrist says after the appointment.
It's normal to feel overwhelmed by all the information you might be taking in during that first appointment. You may find it helpful to take notes throughout your session. This can help you remember what you discussed, but it can also be a great way to reflect back on each session to think about what to talk about during your next appointment.
During your appointment, be honest with your psychiatrist, and don't be afraid to ask questions. You might opt to bring a trusted friend or take notes during your session so you can remember important details about your appointment.
When you arrive home after your first appointment, you may wish to add notes to your list. While the visit is fresh in your mind, make notes for things you wish to talk about in more depth in the future or feelings which you did not have time to address during the visit.
Take a moment as well to ask yourself if you want to keep seeing this person or if, instead, you would rather see a different mental health care provider. An important part of coping with any mental health condition is to develop a solid relationship with a psychiatrist or therapist you can trust.
Research suggests that the therapeutic alliance, or the rapport and relationship between you and your therapist, plays an essential role in treatment outcomes.
Mental health professionals, like all people, have a wide range of personalities, strengths, and weaknesses, and it's important to find the one who is right for you as an individual.
A Word From Verywell
Creating a detailed list can make your first appointment with a mental health professional go much more smoothly. Your doctor will appreciate your preparation, too. Remember to keep your list simple and limit it to feelings and experiences, taking care not to fill in diagnoses that could mislead both you and your therapist.
The length of your first appointment may vary depending on the individual therapist and your specific situation. In some cases, it might be the length of a regular session, which often lasts somewhere between 45 and 60 minutes. In other cases, your intake session will be the longest appointment, lasting between one and two hours.
Be sure to bring your insurance information to your first appointment. Also, take a list of all the medications you are currently taking. Note any psychiatric medications you may have taken in the past.
Copies of medical records can be helpful, but you can also bring handwritten information about your medical history. If you've been tracking information about your symptoms, moods, triggers, and self-care practices, be sure to bring those notes as well.
If you don't like your psychiatrist, then it is probably best to look for a different mental health provider. It is perfectly normal to not feel comfortable with every therapist you meet, so don't be afraid to keep looking. You might simply say that you don't feel like it's a good match and ask if they or your primary care physician can refer you to a different professional.
National Institute of Mental Health. Chronic illness and mental health: Recognizing and treating depression .
Sweeney A, Gillard S, Wykes T, Rose D. The role of fear in mental health service users' experiences: a qualitative exploration . Soc Psychiatry Psychiatr Epidemiol . 2015;50(7):1079–1087. doi:10.1007/s00127-015-1028-z
Crits-Christoph P, Rieger A, Gaines A, Gibbons MBC. Trust and respect in the patient-clinician relationship: preliminary development of a new scale . BMC Psychol . 2019;7(1):91. doi:10.1186/s40359-019-0347-3
Carey TA. Beyond patient-centered care: Enhancing the patient experience in mental health services through patient-perspective care . Patient Experience J. 2016; 3(2):46-49.
National Alliance on Mental Illness. How to prepare for your first psychiatric appointment .
By Marcia Purse Marcia Purse is a mental health writer and bipolar disorder advocate who brings strong research skills and personal experiences to her writing.
Condition Headquarters:
What to expect from your first psychiatrist visit, learn the questions you should ask, the tests you might have, whether you'll be put on medication—and more..

When your life is disrupted by difficult emotions, or if your mood swings are worrying your family or friends, it may be time to seek professional help . Psychiatrists are mental health providers with medical degrees (MDs or DOs) who evaluate the emotional and physical issues that contribute to your psychological problems. They can order or perform a full range of laboratory tests, prescribe medications when appropriate and work with you via talk therapy to help solve your problems.
Once you’ve booked an appointment with a psychiatrist, you may have questions about your first session. How do you prepare? What should you ask—and what should you be prepared to answer? Will you leave with an action plan? What if you’re uncomfortable with the doctor?
Kali Cyrus, MD, MPH , an Assistant Professor in the Yale Department of Psychiatry and Director of the Standardized Patient Program at Yale School of Medicine, answers the big questions about starting (or considering) psychiatric therapy.

What should you expect to cover?
“Come to that first appointment ready to talk about the major issues that you’re struggling with emotionally,” suggests Dr. Cyrus. Also, be prepared to share anything that did or didn’t work during previous encounters you may have had with mental health professionals.
You may discuss goals, and your psychiatrist might ask questions such as, “What do you hope to get out of our work together?” or “What does feeling well emotionally look like to you?”
You should also get a sense of how it feels to work with the psychiatrist, suggests Dr. Cyrus. “Does she or he feel like someone you could be comfortable working with in future sessions and sharing your innermost secrets with?”

What questions should you be ready for?
“Most initial psychiatric interviews have a typical structure—unless you’re coming in during an emotional crisis,” says Cyrus. Typically, you can expect the psychiatrist to ask you questions like:
- Why are you seeking therapy?
- What recent concerns or events have led you to seek therapy?
- Are you sad most days? Anxious ? Do you have thoughts of past or current abuse? Do you engage in drug or alcohol overuse?
- Do you have identity issues?
- Do you misinterpret others’ actions, the reality around you or things you hear?
- Do you have thoughts of wanting to harm yourself or others?
- Have you physically hurt yourself or others?
- Have you been in counseling before? If so, prepare to summarize the experience.
- Have you been on psychiatric medications in the past?
- Do you have any medical problems?
- Do you take any medications or have any allergies?
- What’s your past and current family structure like?
- Does anyone in the family ever struggle with mental health issues (diagnosed with a condition, hospitalized psychiatrically, suicide attempts, drug/alcohol abuse)?
- What’s your current social situation: home life, work life, hobbies, finances, exercise?
- What are your goals for treatment—what outcome would you want from this therapy?
- How do you envision the treatment?

What questions should you ask?
Just as your psychiatrist will ask you questions about your mental health issues, you may want to ask her questions—for example, about her experience with your condition or your options for treatment. You may ask:
- What kinds of people and problems do you work with most frequently?
- What do you think are my best treatment options?
- Can you outline the pros and cons of treatments?
- How long do people with problems like mine typically receive therapy?
- If I have an emergency, what should I do and how can I reach you? What types of communication do you prefer: phone, voicemail, text, email?

Will you be put on medication?
In most cases, a psychiatrist will not start you on medication at your first meeting unless you’ve been referred by another provider to specifically discuss medication. However, if you have an urgent concern, she may recommend one or more prescriptions to alleviate your distress in the short term, until she can develop a long-term plan for you. Finally, if you’ve been taking a medication, she may ask whether it's working for you—and if so, she might re-prescribe it.

What actions will you take to improve?
Your psychiatrist will probably create an action plan for you. For your immediate, distressing concerns, the plan may focus on helping you identify stressors and strategies you can use to remove or at least blunt those stressors, says Cyrus.
Another step the doctor might take is to refer you for treatment to another medical or mental health professional. She might do this if your issues are outside the scope of her area of expertise, or if you have an untreated medical problem that could contribute to your emotional issues. For example, if your concern is related to or worsened by a medical condition—such as diabetes, which has a link to depression—she may refer you to a specialist or a primary care physician for treatment.
If your condition requires a higher level of care—for example, if you need to be monitored frequently for your safety—your psychiatrist may refer you to a day program, such as a four- to eight-week class setting. If you’re experiencing a crisis, however, the psychiatrist may refer you to an inpatient hospital.

What tests might you get?
Before the psychiatrist prescribes medication for you, she may order blood or other tests to confirm that your emotional issues are not the result of—or worsened by—a medical issue. These tests may include:
- Blood tests to gauge kidney and liver function, blood count (CBC), thyroid function , cholesterol levels, blood sugar levels and blood levels of certain vitamins that can affect mood (such as B12). Tests may also include those for sexually transmitted infections that can manifest psychologically, such as syphilis. Your psychiatrist might order a urine test to screen for drugs and/or alcohol, as well.
- A physical exam , during which a doctor will note your vital signs, including weight, height, blood pressure and pulse.
- Screening tests for various mental health conditions, such as depression. In most cases, these are standardized questions which the psychiatrist will have you answer.

What if you’re uncomfortable talking?
This is a difficult question, says Cyrus. If you don’t feel comfortable talking to your therapist, one of the best (and hardest) things to do is to say it. The psychiatrist is trained to sense moments of discomfort and help you explore why you feel that way. What’s more, she is likely to engage you in a discussion designed to help make you feel more comfortable.
Part of the process of therapy is learning to recognize when that discomfort arises, and to keep talking about it. This helps you to better understand what from your past or present may contribute to your discomfort, and how to get past these moments when they reoccur.
Sometimes, a client and a psychiatrist may simply not be well suited to each other. If after a few visits, you feel that she isn’t responding to you or isn’t listening to you, discuss your discomfort with her. You may respond better to a different therapist.

What logistics will you discuss?
During your very first session, you’re likely to discuss “housekeeping” details. You’ll talk about the logistics of the therapy, says Cyrus, including the cost and how you’ll pay the psychiatrist, and whether all or part of therapy is covered by your insurance. You’ll also discuss whether the doctor offers any flexibility in the fee. Perhaps she offers an income-based sliding scale, if you have concerns about how to pay for treatment.
You and the psychiatrist will also work out your schedules to allow for regular visits, and will likely nail down an emergency contact.

What should you do after the first appointment?
First, make sure to leave the office with a schedule of appointments for the future. Your psychiatrist may also assign “homework” for you to complete. For example, she may ask you to keep a journal and jot down your feelings. Or, she may recommend adopting healthy behaviors designed to ease your emotional issues, such as getting enough sleep , eating healthfully and being physically active. Make sure to follow through with any “assignments” she gives you, and report back at your next session.
Then, pat yourself on the back. It’s often difficult to locate a psychiatrist and follow through on setting and attending an appointment, says Cyrus. You’re taking a step towards improving your mental health, which is as important as your physical health. Putting in the work to understand your thoughts and feelings can help guide your actions and lead to a happier future.


How to Prepare for Your Psychiatric Appointment
By Katherine Ponte, JD, MBA, CPRP; Mark Costa, M.D., MPH; and Anthony J. Pavlo, Ph.D.

Seeing a psychiatrist, particularly for the first time, can be intimidating. Seeking help can mean confronting the unknowns, like a possible diagnosis. Moreover, trusting a practitioner with your mental and emotional well-being puts you in a vulnerable position. While your loved ones can support you, they can’t treat you — thus, your psychiatrist holds a powerful position in your treatment.
A little preparation before your appointment, however, can go a long way. This begins with finding the confidence to self-advocate, as you are the expert in yourself. Only you can best express your goals, values and preferences, and you have the right to take an active role in your care. In fact, new research suggests that active involvement of patients in their health care may significantly enhance outcomes.
With that in mind, here’s how you can best prepare yourself for seeing a psychiatrist.
Do Your Research
One of the best ways to find a qualified psychiatrist is often through referrals from a talk therapist, primary care doctor or member of your support system. If you’d prefer to do your own search, you can use online directories available through mental health publications and websites like Psychology Today . Make sure to research the background and specialties of all psychiatrists you are considering to ensure that they fit your needs. Before scheduling an appointment, ask about insurance coverage.
Know Your Medical History
Before meeting with a psychiatrist, you may want to assemble your complete medical history. Be familiar with and ready to share any prior diagnosis, symptoms and a summary of current and past medication regimens (including doses, time periods taken and side effects). If you are unsure about your medical history, you can obtain this information from the clinician who prescribed past medications or your pharmacist.
Educate Yourself on the Basics
A little at-home education on mental health conditions can be extremely helpful. Read up on your condition, symptoms and possible treatment options. You won’t become an expert, but you can learn enough to ask more targeted questions.
Advocate for a Shared Decision-Making Treatment Approach
Shared decision-making (SDM) is a collaborative approach to making decisions about your care. SDM requires that psychiatrists, chosen family members and patients come to mutual agreement about plans for treatment. Ultimately, this approach assumes “ two experts ” in the room: The psychiatrist with specialized medical knowledge and the person with the expertise of their lived experience, values, preferences and goals.
You can ask your provider if they are familiar with shared decision-making and determine if they will include your thoughts and expertise when deciding about your treatment plan. Knowing up front how you will be involved in your treatment plan will help you decide whether this is the best provider for you.
Assess the Relationship Fit
Most likely, you do not feel comfortable with every person you meet. The same applies to working with mental health professionals. It often takes a few meetings to figure out whether you feel comfortable enough to work with someone. Connecting with your mental health professional is key — researchers have found that the quality of the therapeutic relationship (including their warmth, interest and responsiveness to your needs) has been shown to improve outcomes in psychotherapy.
After the first few appointments, it is important to consider whether you connect with your psychiatrist. Ask yourself:
- Did you feel you comfortable talking to them?
- Did you feel like they cared about what was important to you?
- Did you feel like you could express what was important to you?
Difficulties in these areas could suggest that this may not be the right psychiatrist for you. Talk about your concerns with your psychiatrist and decide whether switching to someone else would better support your needs .
Ask Questions
An effective psychiatrist should be willing to answer any questions you have — respectfully. Dismissing your questions may be a sign that they may limit your involvement in your care. Some possible questions to pose are:
- What is your treatment approach?
- How can I be involved in my care?
- I would like to be treated to achieve my life goals rather than to address symptoms. What do you think of this approach?
- What are my medication options? Can you thoroughly explain each one, including what symptoms they will treat?
- Can you carefully explain any side effects, including physical impacts, such as sedation or weight gain or activity restrictions such as alcohol consumption?
- How can side effects be addressed? Are there any adverse impacts with the other medications I am on (if applicable)?
- Are you available outside appointments to address medication and other concerns, such as refills and emergencies? What’s the best way to reach you?
- Are you able to recommend additional resources that might be helpful for me?
Keep Records
In between appointments, it can be helpful to keep a log of your moods, triggers, symptoms, medication observations and any self-care practices. These trends can be useful data to evaluate with your doctor, including progress between appointments. You can also use this information to make a list of discussion points for your next appointment.
A meaningful relationship with your psychiatrist is critical to receiving the best care possible. Your psychiatrist’s role is to share their expertise to guide you on your journey, but for the best results, this relationship requires your effort and preparation as well.
Katherine Ponte is happily living in recovery from severe bipolar I disorder. She’s the Founder of ForLikeMinds ’ mental illness peer support community, BipolarThriving : Recovery Coaching and Psych Ward Greeting Cards . Katherine is also a faculty member of the Yale University Program for Recovery and Community Health and has authored ForLikeMinds: Mental Illness Recovery Insights .
Mark Costa, M.D., MPH, is a psychiatrist and an Associate Research Scientist at the Yale University Program for Recovery and Community Health . He is the project coordinator of the Yale Post-Doctoral Research Training Program to Advance Competitive Integrated Employment for People with Psychiatric Disabilities.
Anthony J. Pavlo, Ph.D., is a clinical psychologist and an Associate Research Scientist at the Yale University Program for Recovery and Community Health . His research focuses on recovery-oriented and person-centered practices in mental health care, therapeutic relationships and shared decision-making for persons who are diagnosed with serious mental illnesses.
Submit to the NAMI Blog
We’re always accepting submissions to the NAMI Blog! We feature the latest research, stories of recovery, ways to end stigma and strategies for living well with mental illness. Most importantly: We feature your voices.
Check out our Submission Guidelines for more information.
Recent Posts
- From Gang Member to Mental Health Advocate
- How EMDR Healed My Trauma
- How Research Is Advancing Our Understanding of OCD
- Finding Treatment and Breaking the Cycle of Intergenerational Depression
- Individual Rights & Responsibilities
- Mental Health professionals
- Mental Health Systems
- Person With Mental Illness
- Treatment Settings
- December 2023
- October 2023
- September 2023
- August 2023
Find Your Local NAMI
Expert mental health information for everyone
Your first appointment
My name is Samantha and I'm a psychiatrist.
I work at a hospital and I would see you if you were referred by your GP, your general practitioner or any other specialist or even your counselor.
And you know, you might have a whole range of symptoms such as depression or anxiety or even memory problems.
We would have a chat about what's going on and how I can help you.
So it can be quite scary for someone to, come and see a psychiatrist for the first time - they may not have seen one before.
There's often a lot of stereotypes and I guess notions about what psychiatrists are and what we do. Seeing a psychiatrist for the first time can be a bit intimidating because the appointments are generally quite long. So we would have someone seen for about minutes and I think that's not unusual. And the reason for that is because we often want to gather quite a lot of information.
When someone comes to their first appointment I think hopefully they have a bit of an awareness of why they've come. So, if for example they've come because they're feeling depressed you know it would be useful to have some information about their previous treatments for example.
If they can, collate letters, or if they've written notes about how they've been feeling over the, last couple of days or couple weeks it can be really useful. Sometimes when you're put on the spot it can be really hard to think about you know what happened last week or the week before, so that can be really useful.
I also think it's really good to have a list of questions. Because at the end of the appointment when I do ask, "do you have any questions?" that can be really hard when you're put on the spot to have questions like, "when do I see you next?" “what's going to happen?" "is this information going to my GP?" So you can prepare that way, and a lot of patients actually do bring a lot of notes and lots and lots of papers.
Some people have often looked on the internet about particular treatments already, or ask about a particular diagnosis they think they've got. So people often do prepare. I think it's really good that they come in prepared with information.
As a psychiatrist I'm really interested in finding out a lot about the person themselves and about their background and their story, because this really helps guide what kind of treatments and what kind of things they would be interested in doing and how we can help manage these symptoms. And so we would ask things about obviously what they think the issues are, we'd ask about their family, their family history.
We often ask about their personal history and perhaps things like growing up and going to school and university and work life. Perhaps even relationships. If the person does have a history of depression or anxiety I would obviously ask a lot about that because we do want to know about what's happened to them in the past, what things have helped them, what hasn't. Because these things are going to help us try and help them in what's going to happen for their ongoing treatment.
I think it's actually really important that a patient does bring someone with them, if they want to. So, the reason for that would not just be for support but often as a psychiatrist I'm actually really interested in hearing what the family member or the spouse wants to say as well.
Try to think about seeing a psychiatrist like seeing any other specialty. Yes we do ask lots of questions and it might seem like an interrogation, but we're not analysing you, we're not making you sit on the couch and and turn your back to us, we're not doing anything like that.
You know, we're just really interested in finding out who you are, and why you're here.
What will happen?
Your first appointment with a psychiatrist will usually be 1–1.5 hours long.
Your psychiatrist will:
- listen to you talk about your concerns and symptoms
- ask questions about your general health
- ask about your family history
- take your blood pressure and do a basic physical check-up if it's required
- ask you to fill out a questionnaire.
There will usually be a lot of questions. The long appointment gives the psychiatrist time to listen to you and hear your whole story.
They might also want to speak with other health professionals or members of your family.
Your psychiatrist may order some more tests to help them understand what is going on.
Getting a diagnosis and treatment plan
It might take a few appointments for your psychiatrist to make a full diagnosis.
The next step is to work out a treatment plan.
A treatment plan is a combination of therapies that suit your health needs, personal preferences, family situation and age.
You and your psychiatrist will work together to develop a treatment plan that's right for you.
The psychiatrist might provide the treatment themselves, or they might recommend you see another health professional – for example a psychologist.
More about the treatments used by psychiatrists
What should I do before my first appointment?
When you telephone the practice, clinic or hospital to make an appointment, ask about:
- the psychiatrist's qualifications
- whether they have expertise in particular conditions, treatments or groups of patients
- what their fees are
- payment methods (e.g. credit card, EFTPOS) in Australia, some idea of how much you might get back from Medicare, and if they can process the refund for you
- their cancellation policy and possible fees for this
- their policy about contact with the practice or psychiatrist
- if they have admission rights at any private hospitals
- if you're changing psychiatrists, whether they need a 'transfer of care' letter from your previous psychiatrist
- whether you need to bring the referral letter to the appointment or send it ahead of time.
Read through any information that the clinic or practice manager has sent to you.
Try to write a list of questions you'd like your psychiatrist to answer.
Also think about or write down:
- the symptoms you have
- any stresses in your life
- other medical conditions you have
- any medication, herbal supplements or vitamins you're taking (how many, how often you take them and the tablet strength)
- ideas about what's helped or not helped in the past
- the supports you have (family, friends, colleagues, sporting groups etc.).
Bring in any documents you already have, such as your referral letter, blood test results or scans.
If you've done some research already, feel free to bring in the information or web links.
Can I bring someone with me?
You can bring a family member or friend to an appointment if you want. They can wait for you outside or come in for all or part of the appointment.
You don't have to bring someone if you don't want to.
What about confidentiality?
Anything you talk about with your psychiatrist is confidential.
Your psychiatrist may need to share some of your private information with other healthcare professionals.
Your psychiatrist might suggest involving family members in your assessment. They will discuss this with you first.
A psychiatrist may be required by law to share information or a person's medical record with others. Generally, your psychiatrist will tell you first if they need to do this.
What happens next?
After your first visit, the appointments might be shorter. Your psychiatrist will focus on checking your progress and adjusting treatments.
If your psychiatrist is providing you with psychological treatments (talking therapies), you will probably see them regularly.
Your psychiatrist might recommend you go back to your GP for regular check-ups. They may also arrange for you to see a psychologist, social worker or other therapist.
If your referral was for a second opinion or management plan only, you usually won't need to go back for another appointment.
- It can be useful to do some preparation before your appointment.
- Call the clinic, hospital or health service if you have questions before your appointment.
- You get a say in any treatment that is recommended for you.
- You can bring someone with you to an appointment.
You might also be interested in:
This is a general guide only, and does not replace individual medical advice. Please speak to your doctor for advice about your situation. The RANZCP is not liable for any consequences arising from relying on this information. Subject matter experts, people with lived experience of mental illness and carers all contributed to this fact sheet.
This website needs JavaScript enabled in order to work correctly; currently it looks like it is disabled. Please enable JavaScript to use this website as intended.
Hi, your browser is terribly old, so this website won't work too well for you. Please visit http://browsehappy.com to upgrade your browser.

- What to Expect at a Psychiatry Appointment
May is Mental Health Awareness Month. Psychiatry is a vital part of mental health treatment. In the United States, one in six people takes psychiatric medications. These medicines help people to live balanced, healthier lives.
Even with the prevalence of treatment options and prominence of medications, a stigma exists. These factors can make seeking treatment a daunting task.
Psychiatry today
There are approximately 28,000 psychiatrists in the United States. These doctors play an important role in health care, especially in the wake of the opioid crisis . Recruitment for psychiatrists is second only to family physicians.
In a previous post, we discussed the differences between psychiatry and psychology . Now, we’ll take a closer look at what it’s like to visit a psychiatrist.
Psychiatrists are medical doctors. These physicians can also practice psychotherapy. But the primary job of a psychiatrist is medication management. Larger practices may consist of a team of people.
These teams include various medical professionals capable of making diagnoses and prescribing medications. These include psychiatric nurse practitioners (NP) and physicians assistants (PA).
There may also be psychologists, licensed professional counselors and social workers. These team members may also be doctors, but they hold Ph.D.s and cannot prescribe medication.
Psychiatry appointment
Seeing a psychiatrist for the first time can be intimidating, but there is no need to worry. The following list tells you what to expect at a psychiatric appointment.
The first visit is the longest.
Phone a friend., write it down., a simple physical., get to know your psychiatrist., treatment plan., shorter sessions., psychiatry is worth it.
Dealing with a mental health diagnosis is as important as physical health. It may be new territory, but it is worth it to get you on a healthy path. It is often suggested to see a psychologist along with your psychiatrist. In the best case scenario, these doctors will work together on your treatment.
To facilitate this, both doctors will offer you a release form. These forms give them your permission to communicate freely to create the best treatment plan for your health. A psychologist spends more time with you and knows more details about your current state. They can share this information with your psychiatrist. Both doctors will help you achieve your mental health goals. If you’re looking to start your psychiatry journey, the Holiner Group team is here to help. We have locations in Dallas and McKinney . We have a talented staff and want to assist you. Contact us, today.
Have a Question? Let’s discuss it.
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- April 01, 2024 | VOL. 75, NO. 4 CURRENT ISSUE pp.307-398
- March 01, 2024 | VOL. 75, NO. 3 pp.203-304
- February 01, 2024 | VOL. 75, NO. 2 pp.107-201
- January 01, 2024 | VOL. 75, NO. 1 pp.1-71
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Relationship of Depression Screening and Physician Office Visit Duration in a National Sample
- Michael R. Schmitt Pharm.D., M.S.
- Michael J. Miller Dr.P.H.
- Donald L. Harrison Ph.D.
- Bryan K. Touchet M.D.
Search for more papers by this author
Major depressive disorder is a common, debilitating chronic illness with a lifetime prevalence of 16.2% and a 12-month prevalence of 6.6% in the U.S adult population ( 1 ). General depressive symptoms have been reported to have a lifetime prevalence affecting nearly one-fourth (23.1%) of U.S. adults ( 2 ). In 2000, the World Health Organization ranked depression as the fourth leading contributor to global burden of disease ( 3 ). In a study of 13 chronic conditions, only depression was associated with workplace attendance (presence and absence) and with critical incidents (such as job-related accidents, injuries, and other negative events) ( 4 ). As a common comorbidity, depression adds to the burden of many chronic disease states ( 5 , 6 , 7 , 8 , 9 , 10 ). Studies examining the costs of depression among U.S. workers have shown that employees with depression cost businesses $31 billion annually in lost productive time compared with peers without depression ( 11 ) and $51.5 billion in total workplace costs ( 12 ).
Given the high prevalence of depression and its adverse impact on medical expenditures and patient quality of life, one would expect that adequate detection and treatment would be key concerns among primary care providers ( 13 ). However, despite the consequences, depression often is unrecognized by physicians in a large proportion of patients ( 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 ). After reviewing available evidence and beginning in their 2002 recommendations ( 22 ), the U.S. Preventive Services Task Force (USPSTF) endorsed depression screening for adults (recommendation grade B) in primary care settings that have adequate systems to ensure accuracy of diagnosis, management, and treatment of the illness ( 23 ).
Although the USPSTF guidelines are well intended, the provision of preventive services may substantially add to the duration of physician visits. For example, a study examining primary care preventive services recommended by the 1996 USPSTF guidelines reported that absolute physician adherence to all recommendations and guidelines would increase a physician's workday by 7.4 hours ( 24 ). Other research examining USPSTF guidelines has found that, in general, preventive services add an average of 2.1 minutes per visit ( 25 ), with some services adding over five minutes to visit duration ( 26 ). A cost-utility analysis of depression screening before the implementation of the 2002 USPSTF recommendations estimated that depression screening added approximately six minutes to physician office visits when a nurse administered and a physician scored a depression screening instrument ( 27 ). However, the time necessary to conduct depression screening varies depending on the instrument and technique used, with no standard method endorsed by USPSTF.
The objective of this study was to evaluate the relationship between depression screening and duration of patients' visits with their primary care physician in a nationally representative sample of office visits. Quantifying differences in duration of physician visits with respect to use of depression screening while controlling the analyses for other factors that may influence physician time burden should provide evidence for policy makers as they consider actions to ensure that patients are routinely screened for depression and that facilitate optimal adherence to USPSTF guidelines.
Study design and overview
Patient and visit characteristics from a nationally representative sample of community-based family, general, and internal medicine primary care physicians' office visits were used to evaluate the relationship between depression screening and office visit duration.
Data source. Cross-sectional data from the 2005–2007 National Ambulatory Medical Care Survey (NAMCS) were used ( 28 ). The NAMCS is a national survey conducted by the National Center for Health Statistics of patient visits to non-federally employed, office-based physicians primarily engaged in direct patient care. The survey uses a three-stage probability design of primary sampling units, physicians' practices within those units, and patient visits within physicians' practices. Each visit is weighted by sampling probability, adjustment for nonresponse, physician specialty, and geographic location to obtain nationally representative estimates. These estimates were considered reliable if they had a standard error of 30% or less and if they were achieved with a sample of no fewer than 30 patient visits ( 28 ). This study was exempt from review by the University of Oklahoma Institutional Review Board because it used publicly available, deidentified data.
Inclusion and exclusion criteria. The 2005–2007 NAMCS data contained 87,835 unique visits. The USPSTF depression screening guidelines target adult patients of primary care physicians. Therefore, data were limited to visits including adult patients (≥18 years) of general and family practices and internal medicine physicians indicated to be the patient's primary care physician. We excluded from analysis visits with primary-reason-for-visit codes related to injuries, adverse effects, or test results; visits coded as administrative (examinations for unemployment, licensing, Social Security disability, and so on); and visits that were uncodable (that is, there was insufficient information). Because this study focused on physician time burden, visits indicating presence of nonphysician clinicians (such as nurse practitioners or physician assistants) were excluded from the analytical sample. Visit time outliers were eliminated by restricting visit time to a range from one to 60 minutes. Because only visits with complete data were analyzed in multivariable analyses, all visits containing variables of interest coded as missing were excluded, leaving a final analytical sample of 14,736 family, general, and internal medicine primary care adult office visits in the United States between 2005 and 2007.
Study variables. The dependent measure of interest was duration of physician time spent with a patient for a particular visit. Time spent with physicians is defined in the NAMCS data documentation as the amount of time (in minutes) that a physician spent with the patient, not including time spent waiting for an appointment or with another type of practitioner ( 28 ). Although defined as a continuous variable, the distribution of time spent with a physician in the NAMCS data was largely recorded in increments of five minutes of visit duration (five minutes, ten minutes, 15 minutes, and so on). To preserve the nature of the data while balancing the need for adequate sample sizes to achieve reliable estimates in data analysis, we defined the duration of time spent with a physician at an office visit as an ordinal measure of four 15-minute time increments (that is, one to 15 minutes, 16–30 minutes, 31–45 minutes, and 46–60 minutes). Prior analyses that have examined physician time using NAMCS data ( 26 , 29 ) dichotomized the time variable at the median visit duration. However, an ordered measure provides a more precise estimate of the associations between depression screening and physician time while respecting the analytical assumption of the nonnormal distribution of the data.
Several patient characteristics were used as control variables in the multivariable analysis. Age was dichotomized as patients aged 65 or older or those younger than 65. Race-ethnicity was defined as white non-Hispanic or "other" (including black non-Hispanic, Hispanic, Asian, Native Hawaiian or other Pacific Islander, American Indian or Alaska Native, or people of multiple races or ethnicities). The NAMCS documents 14 common chronic conditions, regardless of the diagnosis associated with that specific visit. Given its suspected relationship with depression screening, a diagnosis of depression (yes or no) was included as a separate control variable in the analyses. Of the 13 remaining possible, chronic conditions, the sum of the total number of chronic conditions was dichotomized as patients with more than the median number of chronic conditions or those with the median number or fewer.
Several visit characteristics were also suspected to be related to visit duration. An indicator variable was created to document the number of prior visits a patient had made to the sampled physician in the previous 12 months. This variable was dichotomized as patients with up to two prior visits versus those with three or more prior visits. Primary payment type was defined as private insurance, Medicare, Medicaid, or other, which included worker's compensation, self-pay, no charge, other, or unknown. The NAMCS data also document the order for or provision of numerous diagnostic or screening tests. The independent variable of primary interest in this study was order for or provision of depression screening documented in the patient medical record. Depression screening was defined separately from the other diagnostic and screening tests by a dichotomous variable (yes or no). Because the data collected in the NAMCS regarding diagnostic and screening tests are limited to the description of "order for or provision of" a given test, the meaning of the term "depression screening" as used in this study was defined as physician intent to screen the patient for depression.
All other diagnostic and screening tests were collapsed into a single dichotomous variable indicating at least one test versus no tests. Measurements of vital signs, height, and weight were not included as diagnostic tests in the analysis because they are standard practice at family, general, and internal medicine primary care visits. The order for or provision of health education at a visit was dichotomized as yes or no. A final indicator variable for visit type was used to identify an acute care, chronic care (including routine and flare-up chronic care), or preventive care visit.
Univariate descriptive statistics were calculated to profile the study sample. Ordered logistic regression was used to evaluate the relationship between depression screening and primary care physician visit duration while controlling for important covariates in a multivariable model. Predicted probabilities were calculated from the multivariable ordered logistic regression to assess the distribution of visit duration time intervals stratified by visits with and without depression screening. To provide population estimates, all data management and analyses were performed in Stata, version 10.1 ( 30 ), with complex survey commands using Taylor-linearized variance estimation, sampling weights, and masked sampling design variables provided in the NAMCS data set ( 31 ). An a priori alpha level of .05 was the criterion for statistical significance.
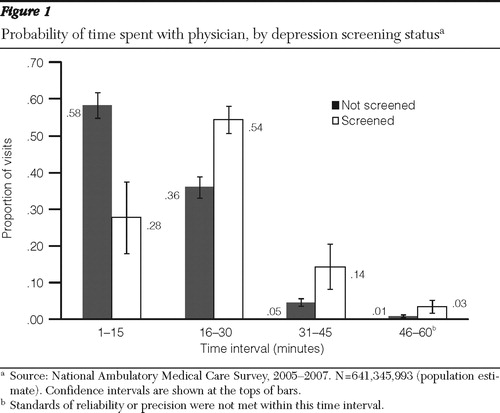
Several variables were associated with longer visit duration in the ordered logistic regression model ( Table 1 ). Most important, depression screening at a visit was associated with significantly higher odds of having a longer visit duration compared with visits not involving depression screening (adjusted odds ratio=3.66).
Subsequent to the primary analysis, the dependent variable, visit duration, was specified and tested in a number of ways in several multivariable post hoc analyses using an identical set of independent variables from the primary analysis and the same complex survey commands. Results of a multivariable linear regression analysis using physician visit duration (in minutes) as a continuous dependent variable demonstrated no variation in results compared with results presented in Table 1 . Multivariable models using log-linear, square root, and squared transformations of the continuous dependent variable also demonstrated no variation in results when compared with the ordered logistic model. It is important to note that none of these techniques normalized the distribution of the visit duration variable. Finally, to compare this study's results with prior NAMCS studies examining physician visit duration, the dependent variable was dichotomized at its median of 15 minutes in a logistic regression model. With the exception of number of prior visits in the previous 12 months (p=.184), the interpretation of results did not vary from the primary analysis using the ordered dependent variable.
15. Jones LR, Badger LW, Ficken RP, et al: Inside the hidden mental health network: examining mental health care delivery of primary care physicians. General Hospital Psychiatry 9:287–293, 1987 Google Scholar
16. Nielsen AC, Williams TA: Depression in ambulatory medical patients: prevalence by self-report questionnaire and recognition by nonpsychiatric physicians. Archives of General Psychiatry 37:999–1004, 1980 Google Scholar
17. Ormel J, Van Den Brink W, Koeter MW, et al: Recognition, management and outcome of psychological disorders in primary care: a naturalistic follow-up study. Psychological Medicine 20:909–923, 1990 Google Scholar
18. Schulberg HC, Saul M, McClelland M, et al: Assessing depression in primary medical and psychiatric practices. Archives of General Psychiatry 42:1164–1170, 1985 Google Scholar
19. Simon GE, Von Korff M: Recognition, management, and outcomes of depression in primary care. Archives of Family Medicine 4:99–105, 1995 Google Scholar
20. Von Korff M, Shapiro S, Burke JD, et al: Anxiety and depression in a primary care clinic: comparison of Diagnostic Interview Schedule, general health questionnaire, and practitioner assessments. Archives of General Psychiatry 44:152–156, 1987 Google Scholar
21. Wells KB, Hays RD, Burnam MA, et al: Detection of depressive disorder for patients receiving prepaid or fee-for-service care. Results from the Medical Outcomes Study. JAMA 262:3298–3302, 1989 Google Scholar
22. Pignone MP, Gaynes BN, Rushton JL, et al: Screening for depression in adults: a summary of the evidence for the US Preventive Services Task Force. Annals of Internal Medicine 136:765–776, 2002 Google Scholar
23. US Preventive Services Task Force: Screening for depression: recommendations and rationale. Annals of Internal Medicine 136:760–764, 2002 Google Scholar
24. Yarnall KSH, Pollak KI, Østbye T, et al: Primary care: is there enough time for prevention? American Journal of Public Health 93:635–641, 2003 Google Scholar
25. Stange KC, Flocke SA, Goodwin MA: Opportunistic preventive services delivery: are time limitations and patient satisfaction barriers? Journal of Family Practice 46:419–424, 1998 Google Scholar
26. Pollak KI, Krause KM, Yarnall KSH, et al: Estimated time spent on preventive services by primary care physicians. BMC Health Services Research 8:245, 2008 Google Scholar
27. Valenstein M, Vijan S, Zeber JE, et al: The cost-utility of screening for depression in primary care. Annals of Internal Medicine 134:345–360, 2001 Google Scholar
28. 2007 National Ambulatory Medical Care Survey (NAMCS) micro-data file documentation. Hyattsville, Md, National Center for Health Statistics, 2007 Google Scholar
29. Coco A, Mainous AG: Relation of time spent in an encounter with the use of antibiotics in pediatric office visits for viral respiratory infections. Archives of Pediatrics and Adolescent Medicine 159:1145–1149, 2005 Google Scholar
30. Stata Statistical Software, Version 10. College Station, Tex, Stata Corp, 2007 Google Scholar
31. Using Ultimate Cluster Models With NAMCS and NHAMCS Public Use Files. Hyattsville, Md, Centers for Disease Control and Prevention, National Center for Health Statistics, 2004. Available at www.cdc.gov/nchs/data/ahcd/ultimatecluster.pdf Google Scholar
32. Mauch D, Kautz C, Smith S: Reimbursement of Mental Health Services in Primary Care Settings. Rockville, Md, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, 2008 Google Scholar
33. Rost K, Smith GR, Matthews DB, et al: The deliberate misdiagnosis of major depression in primary care. Archives of Family Medicine 3:333–337, 1994 Google Scholar
34. Barney LJ, Griffiths KM, Jorm AF, et al: Stigma about depression and its impact on help-seeking intentions. Australian and New Zealand Journal of Psychiatry 40:51–54, 2006 Google Scholar
35. Fann JR, Berry DL, Wolpin S, et al: Depression screening using the Patient Health Questionnaire–9 administered on a touch screen computer. Psycho-oncology 18:14–22, 2009 Google Scholar
36. Katon WJ: Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biological Psychiatry 54:216–226, 2003 Google Scholar
37. Zeber JE, Vijan S, Valenstein M: The cost-utility of depression screening: usual care versus collaborative treatment; in Abstracts of the Academy for Health Services Research and Health Policy Annual Meeting 19:14, 2002 Google Scholar
38. Gilchrist VJ, Stange KC, Flocke SA, et al: A comparison of the National Ambulatory Medical Care Survey (NAMCS) measurement approach with direct observation of outpatient visits. Medical Care 42:276–280, 2004 Google Scholar
39. Stange KC, Zyzanski SJ, Smith TF, et al: How valid are medical records and patient questionnaires for physician profiling and health services research? A comparison with direct observation of patient visits. Medical Care 36:851–867, 1998 Google Scholar
- Association of primary care visit length with outpatient utilization, continuity, and care processes 20 December 2023 | Family Practice, Vol. 35
- Clinicians’ perceptions of barriers to cervical cancer screening for women living with behavioral health conditions: a focus group study 9 March 2022 | BMC Cancer, Vol. 22, No. 1
- BABEL (Better tArgeting, Better outcomes for frail ELderly patients) advance care planning: a comprehensive approach to advance care planning in nursing homes: a cluster randomised trial 23 March 2022 | Age and Ageing, Vol. 51, No. 3
- Docs with their eyes on the clock? The effect of time pressures on primary care productivity Journal of Health Economics, Vol. 77
- Preferred Functions of Personal Health Records in Rural Primary Health Clinics in Canada: Health Care Team Perspectives 20 January 2021 | Applied Clinical Informatics, Vol. 12, No. 01
- The Role of Screening in Depression Diagnosis and Treatment in a Representative Sample of US Primary Care Visits 6 August 2019 | Journal of General Internal Medicine, Vol. 35, No. 1
- International Journal of Human Rights in Healthcare, Vol. 12, No. 5
- Sandipan Bhattacharjee , M.S., Ph.D. ,
- Lisa Goldstone , M.S., Pharm.D. ,
- Nina Vadiei , Pharm.D. ,
- Jeannie K. Lee , Pharm.D., B.C.P.S. ,
- William J. Burke , M.D.
- Journal of General Internal Medicine, Vol. 33, No. 3
- Docs With Their Eyes on the Clock? The Effect of Time Pressures on Primary Care Productivity SSRN Electronic Journal
- Primary care doctors should not screen their patients for depression 12 May 2017 | Expert Review of Neurotherapeutics, Vol. 17, No. 7
- Research in Social and Administrative Pharmacy, Vol. 13, No. 3
- BMC Medicine, Vol. 15, No. 1
- Mental Health Treatment Associated with Community-Based Depression Screening: Considerations for Planning Multidisciplinary Collaborative Care 14 May 2013 | Annals of Pharmacotherapy, Vol. 47, No. 6
- BMC Family Practice, Vol. 14, No. 1
- Matthew B. Wintersteen , Ph.D.

You are using an outdated browser. Please upgrade your browser to improve your experience.
Skip to Site Navigation Skip to Page Content
- Physician Referrals
- Patient Resources
- Why UT Southwestern
Refine your search: Find a Doctor Search Conditions & Treatments Find a Location

Appointment New Patient Appointment or Call 214-645-8300
COVID; Mental Health
The psychiatrist will see you now (by virtual visit)
September 23, 2020
Eventually, the COVID-19 pandemic will end – all pandemics do. And when it does, one silver lining will remain: telemedicine, particularly for psychiatry care.
Seeing patients via virtual visits is not new to UT Southwestern, and that is especially true for those of us in psychiatry and psychology . Several years ago, I was part of a program to launch telepsychiatry to serve patients with transportation challenges in East, West, and Central Texas, and even here in the Metroplex.
This spring, we quickly ramped up our capabilities to offer more virtual care during the early stages of COVID-19. Today, we follow nearly 15,000 UT Southwestern patients through telepsychiatry – 90% of our visits are now virtual, which has increased our bandwidth, enabling us to see 20% more patients than we could before the pandemic.
For more than a decade, I’ve cared for patients across the world through telepsychiatry, providing mental health support through crises such as Ebola and times of war.
Throughout the challenges we've faced then and today, telepsychiatry has proven to be remarkably similar to in-person care. The most notable difference is that, as a patient, you are screen-to-screen with your doctor instead of face-to-face.
Studies show high patient satisfaction with telehealth formats, and our patient satisfaction scores have increased since the pandemic began. Most importantly, our patients enjoy the benefits of the format.
5 benefits of telepsychiatry
1. increased access to behavioral and mental health care.
Telemedicine has long been a critical resource for patients who don’t have easy access to brick-and-mortar facilities such as our Psychiatry Clinic . Even for people who live within the Metroplex, it’s not always convenient to physically visit a doctor.
For example, I care for moms with postpartum depression. Even when you're well, going anywhere with children can be an arduous expedition. And it’s not always easy or affordable to find childcare or transportation. Being able to visit with your doctor from home can remove some of those obstacles.
2. Crossing the 'digital divide'
According to the Texas 2036 Project , a data-driven nonprofit, nearly 1 million people in Texas do not have access to broadband internet service – roughly 31% of rural Texans and more than a third of Dallas households.
This "digital divide" can be seen as a hindrance to telepsychiatry. However, we've found that the majority of patients who use our platform do so from their mobile device, accessing the web through their smartphone data or Wi-Fi. The ability to access telepsychiatry from "mobile-first" platforms is vital.
Pew Research data show that 81% of Americans own smartphones, including 71% of people who live in rural communities and 71% of individuals earning less than $30,000 a year. Moreover, 20% of American adults use their smartphones as their sole internet source at home.
In our experience, mobile devices are not only sufficient for virtual visits but, in many cases, preferred because they can provide better image quality than the standard desktop or laptop PC. For example, I've visited with patients who looked content until they moved their head and device a certain way and I noticed they were crying. That's a big detail in a telepsychiatry exam that we might have missed via desktop camera.
3. Overcoming the stigma of mental health care
Negative attitudes and beliefs about seeking mental health care have decreased over the years, but some unfortunately remain. Telehealth bypasses the potential barriers of being seen walking into a psychiatry clinic or sitting in the waiting room because it allows patients to visit with a professional from the privacy of their own home.
4. Comfort and control
Telemedicine is surprisingly intimate. It’s a virtual house call – patients are, in a sense, inviting me into their homes. That’s a privilege and honor, and it shifts some control to the patients. When a visit is in a doctor’s office, we control the setting and workflow by default. But when it’s in your home, you’re in control, which really is as it should be.
5. Reducing the number of physical visits
I work with colleagues across the health care spectrum to enhance patients’ physical and mental health. Psychiatric care can be beneficial when dealing with cancer, complex pregnancy, and many other medical conditions. Telehealth psychiatry removes the burden of having to fit in yet another trip to the doctor's office.
Related reading: COVID-19 distress: Managing your mental health in a pandemic
How Virtual Care is Becoming the New House Call
Dr. John Warner discusses the evolution and future of virtual care with Alan Kramer, architect of UT Southwestern’s telemedicine strategy, and Dr. Suzanne Cole , an early adopter of video visits and Medical Director of Simmons Cancer Clinic at Richardson/Plano .
What to expect in your video visit
Your video visit will be similar to meeting your psychiatrist in the office. We'll review any testing you might have had, which is sent to your doctor in advance through MyChart .
Then we will talk about how you are feeling, discuss any new or changing symptoms, and go over your medications and treatment progress. From there, we will discuss next steps for your care, just as we would in the office.
Tips for a successful appointment
The few elements that will be different mainly cover positioning and lighting so that we can see and hear each other:
- Camera position and lighting are important so the doctor can clearly see your face and read your body language. We might ask you to adjust where you hold or set your device during our call.
- I also want my patients to be able to see me and be comfortable with my set-up. Patients sometimes ask me to turn off my ceiling fan or shift positions to avoid distracting movements and lights – we want patients to know they can tell us these things.
- Privacy is always a priority, whether we are meeting in person or virtually. When I talk with patients, I am the only one in my office and I close the door.
I ask patients to find a place to meet in which they feel safe and comfortable. They can decide how much privacy they want or need from their end. I’ve had visits in which a child or partner occasionally walks through the room or joins the visit. Based on the discussion, the patient may ask to pause in order to relocate for a little more privacy.
When you might need to come to the office
We'll ask you to visit the clinic only for the few aspects of care that can't be done virtually. These might include:
- Interventional treatments, such as electroconvulsive therapy (ECT) , repetitive transcranial magnetic stimulation (rTMS), or ketamine infusion therapy.
- Substance use disorder treatment. Some initial evaluations and drug testing sessions are still being done in person.
- Some geriatric psychiatry sessions. Many older patients are avid technology users, but some require in-person care.
If you do need to come to the clinic, UT Southwestern has extensive safety precautions and protocols in place to reduce the risk of COVID-19 exposure.
The future of telemedicine in psychiatry
Forthcoming technology will make telepsychiatry even more accessible for patients via mobile devices, particularly older patients. We're taking an approach with our platform that’s similar to Steve Jobs’ approach back in the 1980s – working toward making the interface easy to use, regardless of our patients’ level of tech-savviness.
Innovations in motion by my colleague Alan Kramer, M.P.H., Assistant Vice President for Health System Emerging Strategies at UT Southwestern, include single-touch or single-sign-on login instances for patients to securely access our telepsychiatry platform through their mobile devices. Biometric sign-ons such as thumbprint or recitation of a PIN number could be implemented for an additional layer of security.
For many mental health conditions, research shows that telehealth visits with a professional can be as effective as in-person visits . Equally as important, patients like the platform. I'm glad to say telehealth is here to stay, and it will only continue to improve.
To request a video visit for psychiatric care, call 214-645-8300 or request an appointment online .
More in: COVID , Mental Health

Next Article Flu, COVID, and RSV vaccines: Who should get them and when
More from COVID
COVID; Prevention
Flu, COVID, and RSV vaccines: Who should get them and when
- Julie Trivedi, M.D.
September 13, 2023

Brain; COVID; Heart
POTS or Long COVID? How to tell the difference
- Meredith Bryarly, M.D.
- Steven Vernino, M.D., Ph.D.
June 12, 2023

Omicron boosters: Do I need another COVID-19 shot, and when?
- James Cutrell, M.D.
September 12, 2022
What Texans need to know about monkeypox
- Helen King, M.D.
June 16, 2022

Sizing up the second booster: If, and when, to get another COVID-19 shot
April 22, 2022

Coping with crisis fatigue: 7 tips to ‘keep calm and carry on…’
- Kipp Pietrantonio, Ph.D.
March 3, 2022

COVID; Prevention; Your Pregnancy Matters
Maternal vaccination reduces newborn COVID-19 hospitalization risk by 61%
- Robyn Horsager-Boehrer, M.D.
February 22, 2022

Straight answers on Omicron, the fast-moving COVID-19 variant
- Sonja Bartolome, M.D.
January 20, 2022


Understanding Omicron, the new COVID-19 variant of concern
- Trish Perl, M.D.
December 22, 2021
More Articles
Appointment New Patient Appointment or 214-645-8300 or 817-882-2400
- Share via Facebook facebook
- Share via Twitter twitter
- Share via LinkedIn linkedin
- Share via Email email
- Print this page print
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Seven Actions to Ensure Safety in Psychiatric Office Settings
- Denise Neal , B.S.N., M.J., C.P.H.R.M.
Search for more papers by this author

Workplace violence can happen in any setting. The Centers for Disease Control and Prevention (CDC) defines workplace violence as “the act or threat of violence, ranging from verbal abuse to physical assaults directed toward persons at work or on duty.”
The possibility of being verbally or physically assaulted, stalked, or threatened by a patient is not only a concern but reality for psychiatrists, especially those with limited resources and lack of on-site security. The following actions are recommended to improve safety and security in psychiatric offices and should be tailored to each individual practice.
Conduct a workplace violence assessment and create a workplace violence prevention and response plan regardless of the size or location of your practice.
Assess for workplace hazards within and around the office and plan for the various types of violence that may occur, whether physical violence against staff or verbal violence/harassment/bullying.
Be sure to include, as appropriate, representatives from each discipline in your office.
If you sublet space, include the practitioners who use that space.
Consider involving law enforcement and risk management in your planning.
Review the plan with staff at least annually.
Control/restrict access to the office by patients, visitors, and contractors by providing individual access card readers and/or locks to staff only or limiting access to restricted areas.
Ensure patients, visitors, and contractors are escorted within the office and do not wander alone.
Install video surveillance cameras at entrances and exits and post signs indicating their presence as a deterrent to violence.
Employ an office “buddy” system—no one works alone, including afterhours, or goes to his or her car alone.
Don’t accept “friend” invitations from your patients on social media, and do not look up your patients on social media (consider boundary issues and privacy).
Be mindful of posting personal information about yourself, family, and friends that may reveal your habits.
Be aware of behaviors that are unwanted or distressing including threatening, harassing, and stalking behaviors.
For each occurrence of workplace violence/behavior incidents, document it and discussions about behavior expectations in the patient’s medical record.
Communicate concerning behavior to other multidisciplinary staff members.
Seek assistance from your risk manager, legal counsel, and security/law enforcement.
Avoid having your back to the exit, and turn your body sideways to allow a clear path to the exit if a quick escape is necessary.
Install panic buttons in each office, at the reception desk, and in bathrooms.
Wear an audible alarm.
Designate a safe room within the office should an escape not be possible.
There is a HIPAA exception for disclosure to prevent or lessen a serious and imminent threat to the health or safety of an individual or the public. When disclosing the threat, limit the disclosure to nonclinical information.
Terminate patients that display violent/aggressive/stalking behavior toward you or your staff and consider whether a restraining order/noncontact order is needed. (See “Risk Management Considerations When Terminating With Patients,” which is posted here .)
Provide clinical and nonclinical staff interactive, site-specific education and training.
Educate staff about the nonverbal cues of aggression, agitation, and behavior escalation that may lead to an assault.
Provide de-escalation and response training.
Consider self-defense/personal safety training. ■
This information is provided as a risk management resource for Allied World policyholders and should not be construed as legal or clinical advice. This material may not be reproduced or distributed without the express, written permission of Allied World Assurance Company Holdings Ltd., a Fairfax company (“Allied World”). Risk management services are provided by or arranged through AWAC Services Company, a member company of Allied World.
Denise Neal, B.S.N., M.J., C.P.H.R.M., is assistant vice president of the Risk Management Group, AWAC Services Company, a member company of Allied World.

Visit your office

Every year around now, as spring begins to revive the landscape, I like to take a tour of my office from the perspective of a patient visiting our facility for the first time, because more often than not, the internal environment could use a bit of a revival as well.
We tend not to notice gradual deterioration in the workplace we inhabit every day: Carpets fade and dull with constant traffic and cleaning; wallpaper and paint accumulate dirt, stains, and damage; furniture gets dirty and dented, fabric rips, hardware goes missing.
When did you last take a good look at your waiting room? Have your patients been snacking and spilling drinks in there, despite the signs begging them not to? Is the wallpaper smudged on the walls behind chairs, where they rest their heads? How are the carpeting and upholstery holding up?
Even if you don’t find anything obvious, it’s wise to check periodically for subtle evidence of age: Find some patches of protected carpeting and flooring – under desks, for example – and compare them with exposed floors.
And look at the decor itself; is it dated or just plain old looking? Any interior designer will tell you he or she can determine quite accurately when a space was last decorated, simply by the color and style of the materials used. If your office is stuck in the ’90s, it’s probably time for a change.
If you’re planning a vacation this summer (and I hope you are), that would be the perfect time for a redo. Your patients will be spared the dust and turmoil, tradespeople won’t have to work around your office hours, and you won’t have to cancel any hours that weren’t already canceled. Best of all, you’ll come back to a clean, fresh environment.
Start by reviewing your color scheme. If it’s hopelessly out of date and style, or if you are just tired of it, change it. Wallpaper and carpeting should be long-wearing industrial quality, paint should be high-quality eggshell finish to facilitate cleaning, and everything should be professionally applied. (This is neither the time nor place for do-it-yourself experiments.) And get your building’s maintenance crew to fix any nagging plumbing, electrical, or heating/air conditioning problems while pipes, ducts, and wires are more readily accessible.
If your wall decorations are dated and unattractive, now would be a good time to replace at least some of them. This need not be an expensive proposition. I recently redecorated my exam room walls with framed photos from my travel adventures, to very positive responses from patients and staff alike. If you’re not an artist or photographer, invite family members, local artists, or talented patients to display some of their creations on your walls.
Plants are great accents and excellent stress reducers for apprehensive patients, yet many offices have little or no plant life. If you are hesitant to take on the extra work of plant upkeep, consider using one of the many corporate plant services that rent you the plants, keep them healthy, and replace them as necessary.
Furniture is another important element in keeping your office environment fresh and inviting. You may be able to resurface and reupholster what you have now, but if not, shop carefully. Beware of nonmedical products promoted specifically to physicians, as they tend to be overpriced. If you shop online, remember to factor in shipping costs, which can be considerable for furniture. Don’t be afraid to ask for discounts; you won’t get them if you don’t ask.
This is also a good time to clear out old textbooks, magazines, and files that you will never open again – not in this digital age.
Finally, spruce-up time is an excellent opportunity to inventory your medical equipment. We’ve all seen vintage offices full of gadgets that were state-of-the-art decades ago. Nostalgia is nice, but would you want to be treated by a physician whose office could be a Smithsonian exhibit titled, “Doctor’s Office Circa 1975?” Neither would your patients, for the most part. In fact, many of them – particularly younger ones – assume that doctors who don’t keep up with technologic innovations don’t keep up with anything else, either.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News.
Recommended Reading
- MDedge Home
- Clinician Reviews
- Dermatology
- Emergency Medicine
- Endocrinology/Diabetes
- Family Medicine
- Federal Practitioner
- Gastroenterology
- Hematology/Oncology
- Infectious Disease
- Internal Medicine
- Obstetrics And Gynecology
- Pulmonology
- Rheumatology

TheraThink.com
A mental health billing service, the definitive guide to psychiatry cpt codes [+cheat sheet pdf].
Psychiatry CPT Codes are numerous and nuanced. This guide will teach you the most common psychiatry CPT codes, psychiatry addon codes, psychiatry evaluation and management codes, and how to bill psychiatry CPT codes.
There are quite a few medical billing CPT codes for Psychiatry services and psychiatrists to use, some reimbursed more often or at higher rates than others.
We at TheraThink provide a billing service that can help de-code which psychiatry CPT codes to use. This guide will also help you find out which codes to pick.
We will offer you a quick guide on most common psychiatry CPT Codes, explain evaluation and management (E/m) codes, and then provide an exhaustive list of all Psychiatry CPT codes.
Common Psychiatric CPT Codes

Diagnostic, Evaluation, Intake CPT Code:
- 90791 – Psychiatric Diagnostic Evaluation without medical services ( usually just one/client is covered )
- 90792 – Psychiatric Diagnostic Evaluation with medical services
Outpatient Mental Health CPT Codes :
- 90832 – Psychotherapy, 30 minutes ( 16-37 minutes ).
- 90834 – Psychotherapy, 45 minutes ( 38-52 minutes ).
- 90837 – Psychotherapy, 60 minutes ( 53 minutes and over) .
- 90846 – Family or couples psychotherapy, without patient present.
- 90847 – Family or couples psychotherapy, with patient present.
- 90839 – Psychotherapy for crisis, 60 minutes ( 30-74 minutes ).
- +90840 – Add-on code for an additional 30 minutes ( 75 minutes and over ). Used in conjunction with 90839.
Psychotherapy CPT Codes with Evaluation & Management Services:
- 90833 – Evaluation and Management with 30 Minutes Psychotherapy
- 90836 – Evaluation and Management with 45 Minutes Psychotherapy
- 90838 – Evaluation and Management with 60 Minutes Psychotherapy
Psychiatry CPT Code Cheat Cheat PDF
Here is a downloadable Psychiatry CPT Code Cheat Sheet PDF:
Psychiatry CPT Code Cheat Sheet PDF
Or in image format:
Download Part 1
Download Part 2

If you need help choose the right CPT code to use for your insurance claims, we help translate billing into English with our mental health billing service .
Evaluation and Management Psychiatric CPT Codes

Here is a list of the most common evaluation and management psychiatry CPT codes:
- 99201 – 10 Minutes
- 99202 – 20 Minutes
- 99203 – 30 Minutes
- 99204 – 45 Minutes
- 99205 – 60 Minutes

- 99211 – 5 Minutes
- 99212 – 10 Minutes
- 99213 – 15 Minutes
- 99214 – 25 Minutes
- 99215 – 40 Minutes
- 99241 – 15 Minutes
- 99242 – 30 Minutes
- 99243 – 40 Minutes
- 99244 – 60 Minutes
- 99245 – 90 Minutes
- 99251 – 20 Minutes
- 99252 – 40 Minutes
- 99253 – 55 Minutes
- 99254 – 80 Minutes
- 99255 – 110 Minutes
Reimbursement Rates for Psychiatrists
Please check out our extensive guide to 2021 reimbursement rates for psychiatrists .
Psychiatry CPT Codes List
It’s extremely important to note that many of these codes will not be covered by a client’s insurance policy, may require authorization, or may have specific modifiers required depending on how services are rendered.
If you don’t want to manage any of this work, we’re happy to help do the insurance billing for your psychiatry practice .
Extended Session Add-On CPT Codes for Psychiatric Services
Psychiatry cpt code modifiers.
Here is a short list of the most common CPT Code modifiers that would be used while rending psychiatric services.
CPT Code Modifier 22
- Unusual Procedure Services
This modifier is used when the work associated with the service provided is greater than that usually required for the listed code.
CPT Code Modifier 25
- Significant, Separately Identifiable Evaluation and Management Service by the Same Physician on the Same Day of the Procedure or Other Service
This modifier is used to indicate that on the day a procedure or service identified by a CPT code was performed, the patient’s condition required a significant, separately identifiable E/M service above and beyond the other service provided or beyond the usual pre- and postoperative care associated with the procedure performed.
CPT Code Modifier 26
- Professional Component
This modifier is used for procedures that are a combination of a physician component and a technical component.
When the physician component is reported separately, this modifier is added to the usual procedure.
CPT Code Modifier 52
- Reduced Services
This modifier is used to report a service that is reduced in time.
Setting & Documentation Guidelines for Psychiatric Services
These services are typically set in an office location.
Please review the Medicare guidelines for E/M guidelines and documentation for exhaustive detail:
https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/eval-mgmt-serv-guide-ICN006764.pdf
Unusual Psychiatry CPT Code Descriptions
These descriptions are directly copied from the American Psychiatric Association’s coding pamphlet.
Please refer to their documentation here: https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/Practice-Management/Coding-Reimbursement-Medicare-Medicaid/Coding-Reimbursement/cpt-primer-for-psychiatrists.pdf
These services are often not reimbursed by insurance companies. Call their insurance plan to obtain authorization or have a mental health billing service like ours help.
CPT Code 90865
Narcosynthesis for Psychiatric Diagnostic and Therapeutic Purposes (e.g. sodium amobarbital (Amytal) interview)
This procedure involves the administration, usually through slow intravenous infusion, of a barbiturate or a benzodiazepine in order to suppress inhibitions, allowing the patient to reveal and discuss material that cannot be verbalized without the disinhibiting effect of the medication. This code is reimbursed by most insurers.
CPT Code 90867
Therapeutic Repetitive Transcranial Magnetic Stimulation (TMS) initial treatment, including cortical mapping, motor threshold determination, delivery and management
CPT Code 90868
Subsequent TMS Delivery and Management, per session
CPT Code 90869
Subsequent TMS Motor Threshold Re-Determination with Delivery and Management
CPT Code 90870
Electroconvulsive Therapy (Includes Necessary Monitoring); Single seizure
This code is for electroconvulsive therapy (ECT), which involves the application of electric current to the patient’s brain for the purposes of producing a seizure or series of seizures to alleviate mental symptoms. ECT is used primarily for the treatment of depression that does not respond to medication.
The code includes the time the physician takes to monitor the patient during the convulsive phase and during the recovery phase. When the psychiatrist also administers the anesthesia for ECT, the anesthesia service should be reported separately, using an anesthesia code. ECT is covered by most insurance plans.
CPT Code 90875
Individual Psychophysiological Therapy Incorporating Biofeedback
Training by any Modality (face-to-face with the patient), With Psychotherapy (e.g., insight-oriented, behavior modifying, or supportive psychotherapy); approximately 20-30 minutes and,
CPT Code 90876
approximately 45-50 minutes
These two procedures incorporate biofeedback and psychotherapy (insight oriented, behavior modifying, or supportive) as combined modalities conducted face-to-face with the patient.
They are distinct from biofeedback codes 90901 and 90911, which do not incorporate psychotherapy and do not require face-to-face time. Medicare will not reimburse for either of these codes
CPT Code 90880
Hypnotherapy
Hypnosis is the procedure of inducing a passive state in which the patient demonstrates increased amenability and responsiveness to suggestions and commands, provided they do not conflict seriously with the patient’s conscious or unconscious wishes.
Hypnotherapy may be used for either diagnostic or treatment purposes. This procedure is covered by most insurance plans .
CPT Code 90882
Environmental Intervention for Medical Management Purposes on a Psychiatric Patient’s Behalf With Agencies, Employers, or Institutions
The activities covered by this code include physician visits to a work site to improve work conditions for a particular patient, visits to community-based organizations on behalf of a chronically mentally ill patient to discuss a change in living conditions, or accompaniment of a patient with a phobia in order to help desensitize the patient to a stimulus.
Other activities include coordination of services with agencies, employers, or institutions. This service is covered by some insurance plans, but because some of the activities are not face-to-face, the clinician should check with carriers about their willingness to reimburse for this code.
CPT Code 90885
Psychiatric Evaluation of Hospital Records, Other Psychiatric Reports, Psychometric and/or Projective Tests, and Other Accumulated Data for Medical Diagnostic Purposes
Although this would seem to be a very useful code, because reviewing data is not a face-to-face service with the patient, Medicare will not reimburse for this code and some commercial carriers have followed suit.
Medicare considers the review of data to be part of the pre-/postwork associated with any face-to-face service.
CPT Code 90887
Interpretation or Explanation of Results of Psychiatric, Other Medical Examinations and Procedures, or Other Accumulated Data to Family or Other Responsible Persons, or Advising Them How to Assist Patient
Medicare will not reimburse for this service because it is not done face-to-face with the patient, and clinicians should verify coverage by other insurers to ensure reimbursement. It is appropriate to use an E/M code in the hospital where floor time is expressed in coordination of care with the time documented.
CPT Code 90889
Preparation of Report of Patient’s Psychiatric Status, History, Treatment, or Progress (Other Than for Legal or Consultative Purposes) for Other Physicians, Agencies, or Insurance Carriers
Psychiatrists are often called upon to prepare reports about the patient for many participants in the healthcare system. This code would be best used to denote this service. However, because this is not a service provided face-to-face with a patient, Medicare will not reimburse for this code either, and clinicians should verify coverage by other insurers.
CPT Code 90899
Unlisted Psychiatric Service or Procedure
This code is used for services not specifically defined under another code. It might also be used for procedures that require some degree of explanation or justification.
If the code is used under these circumstances, a brief, jargon-free note explaining the use of the code to the insurance carrier might be helpful in obtaining reimbursement. If it is used for a service that is not provided face-to-face with a patient, the psychiatrist should check with the patient’s insurer regarding reimbursement.
CPT Codes 95970, 95974, 95975
Neurostimulators, Analysis–Programming
These codes have been approved for vagus nerve stimulation (VNS) therapy for treatment-resistant depression. Clinicians performing VNS therapy should use the appropriate code from the 95970, 95974, and 95975 series of codes found in the neurology subsection of the CPT manual. Medicare will not reimburse for these codes.
Brief Office Visit for the Sole Purpose of Monitoring or Changing Drug
Prescriptions Used in the Treatment of Mental Psychoneurotic and Personality Disorders – M0064 is not, in fact, a CPT code. It is a HCPCS Level II code (CPT codes are HCPCS Level I), part of the HCPCS system used by Medicare and Medicaid. M0064 should only be used for the briefest medication check with stable patients
Source: https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/Practice-Management/Coding-Reimbursement-Medicare-Medicaid/Coding-Reimbursement/cpt-primer-for-psychiatrists.pdf
Other Source: https://www.aacap.org/App_Themes/AACAP/docs/clinical_practice_center/business_of_practice/cpt/2018_CPT_module_revised_March_2018.pdf
e/m codes evaluation and management codes mental health billing psych codes psych cpt codes psychiatry billing psychiatry codes psychiatry cpt codes psychiatry reimbursement rates
Our Mental Health Insurance Billing Services
- Daily Claims Filing & Submission
- Daily Claims Processing
- Eligibility & Benefits Verification (in 2 business days)
- EOB & Payment Accounting
- Appeals, Rejections, Denials
- Appointment Reminders (Email or SMS)
- Appointments Calendar
- EAP / Medicare / Medicaid / TriCare Billing
- Credentialing Services
- Network status verification.
- Month-by-Month Contract: No risk trial period
- Free Account Setup - we input your data at signup.
- Claim Tracking & Updates
- EFT & ERA Forms Processing
- Free 30 Day Trial
- Learn more..
You can call, text, or email us about any claim, anytime, and hear back that day. We are your billing staff here to help.
Affordable & Transparent Service
- We charge a percentage of the allowed amount per paid claim (only paid claims)
- No per claim submission fee
- No annual or monthly subscription fee
- No hidden fees
- ICD10 Ready, HIPAA Compliant
Reliable & Dedicated to Customer Service
Our mental health insurance billing staff is on call Monday – Friday, 8am-6pm to ensure your claims are submitted and checked up on with immediacy.
We understand that it's important to actually be able to speak to someone about your billing. Every provider we work with is assigned an admin as a point of contact. You'll always be able to get in touch.
Your access portal for updated claims and reports is secured via our HTTPS/SSL/TLS secured server. Our data is encrypted and backed up to HIPAA compliant standards.
Inquire about our mental health insurance billing service
Get your billing handled.
It's our goal to ensure you simply don't have to spend unncessary time on your billing.
You want to get paid quickly, in full, and not have to do more than spend 10 or 15 minutes to input your weekly calendar.
You want to know you can call your billing admin, a real person you've already spoken with, and get immediate answers about your claims.
You want to not have to deal with it!
Learn how to offload your mental health insurance billing to professionals, so you can do what you do best.
“As private practitioners, our clinical work alone is full-time. Add in the unnecessarily difficult insurance billing system and we run the risk of working way over full-time. TheraThink provides an affordable and incredibly easy solution. My daily insurance billing time now is less than five minutes for a full day of appointments. My cost is a percentage of what is insurance-approved and it’s my favorite bill to pay each month! Denny and his team are responsive, incredibly easy to work with, and know their stuff. I cannot capture in words the value to me of TheraThink. Thank you. You free me to focus on the work I love!”
Book a Demo
Book a demo
December 8, 2022
Finding and Furnishing Your Psychiatry Office: From Leasing to Decor

Dr. Carlene MacMillan, M.D.
You’re opening your own private psychiatry practice and decided you want to see patients in person (at least part of the time). Maybe you'll be prescribing controlled substances that require an in-person visit.
Maybe you offer TMS or ketamine treatments. Or, doing things face-to-face just works better for you and your patients. In any case, your practice space sets the setting for you and your patients.
In this guide, we’ll cover what you need to keep in mind to find and furnish your psychiatry office space:
- Find your office
- Negotiate your lease
- Get insurance for the space
- Furnish and decorate your space to create a warm and welcoming environment
Find Physical Office Space
If you’ve decided to see patients in person, you’ll need a professional space to see them. Your first instinct may be that you need your own space, but many psychiatrists rent space part-time. Others go in on renting a space with other professional staff to divide up office time and costs. If decide to buy a space, you may be able to sub-lease to other professionals looking for part-time space.
How to find part-time shared office space
Real estate agents can be great if you’re looking to rent a space that’s completely yours. But, if you’re looking to share a space, I recommend using local listservs or Facebook groups for mental health and wellness professionals.
You can Google “therapy rental spaces” in major metro cities. There you’ll find professional listservs with one day a week or even hourly rentals. There’s no equivalent of a national WeWork for therapy office space as far as I know, but there are many smaller local businesses cropping up that do this. Lina.co is one example (in NY and FL only for now), and I know folks who’ve had positive experiences.
Also, check online marketplaces such as Craigslist. You can always reach out to local business owners who you suspect may not be using their space full-time. Or, pulse your professional network for interest in sharing a space.
Co-locating with complementary types of medical professionals is a good idea. Pediatrician’s office if you see kids, OB-GYN if doing women’s mental health, or even primary care if you want to work in a more collaborative model.
Location, zoning, and security matters
Before you sign any office lease, you’ll want to think about location. Ask yourself these questions:
Marketing/Discoverability considerations
- Is the location in an area frequented by your target demographic?
- What is the concentration of other psychiatry practices in the area? You might find a location with fewer psychiatry practices around so your practice stands out.
- On the flip side, you might share a building with other mental health professionals to boost referrals. For example, my new office space is in a suite with massage therapists, acupuncturists, therapists, a ketamine psych NP, etc., and we plan to cross-refer.
Privacy and safety considerations
- What is the access like on nights and weekends? If there is a doorman, do people need to sign in and if so, can they just do first name/last initial to preserve privacy?
- Does the location have a “storefront?” This may be less discrete. Is it on a higher floor? If yes, this can pose safety risks.
- Do you need to be close to public transportation or have easy parking?
- What is an acceptable commute time?
Landlord and zoning considerations
- This is super important: Is the landlord comfortable with a medical/mental health practice being in the building/are there any zoning considerations? If you’re doing any procedures and blood draws, this can get complicated and not all spaces are able to allow this.
- Stigma against patients with mental health concerns exists. Make sure the landlord is aware and open to what your business does.
Create the perfect space for your practice
When it comes time to evaluate spaces, here are some questions to keep in mind:
- How does the rental/mortgage cost factor into your budget ? What is the minimum number of hours you need to see patients monthly to make the space worth it?
- Is your space compliant with The Americans with Disabilities Act (ADA)?
- Is there a waiting room AND a place to see patients? If it’s a shared space, is there a receptionist? Is there space for one if you plan to have one?
- If you plan to treat children, is the waiting room friendly to children?
- How does noise transfer?
- Tips for soundproofing : Ask about any special sound insulation. You can consult with someone familiar with soundproofing therapy offices. You can for the builder to place sound-dampening filters in the ceiling during construction. These filters muffle voices.
- Note that soundproofing an already built-out space can be cost-prohibitive. But, you can use things like felt wallpaper and various sound-absorbing wall hangings. This is actually a HUGE issue for therapy spaces and most are not done well. Search for felt wallpaper for soundproofing and you should find something suitable.
- Where are the bathrooms? Is there a gender-neutral bathroom? Are they accessible to patients with disabilities? Do they offer changing stations for patients with young children?
- Will you and your patients feel safe in the space? If needed, are appropriate safety precautions put in place? (e.g., security guard, buzzers, locks)
- Make sure there are locks in place that can be defeated if needed by you or your staff in the event of an emergency. For example, a deadbolt in a single bathroom that the patient can lock themselves in can be dangerous. I speak from experience here, unfortunately. I also recommend investing in a panic button/keychain for each room.
- Is it important to you to form a community with others who work in the space? Consider making fliers/brochures or postcards about your practice and ask if you can keep them in a common waiting area.
- Is it furnished? How will that affect your ability to pay for other up-front costs?
- If unfurnished, consider getting a free business account with companies like Wayfair for more discounts. Wayfair and similar companies will also separate what furniture is “commercial grade.” If you plan to stay in a space for a long time, commercial grade is the way to go.
- Or, if you don’t mind replacing furniture every couple of years, cheaper is fine. Consider working with an interior designer who gets deep discounts on furnishings. That may offset the cost of the designer and save you a ton of time.
- Is it discreet for patients to enter/exit?
- Consider what signage you'll need for your practice. Will individual offices need signs/numbers? A sign in the lobby? Does the landlord allow you to hang signs outside? If so, what are the restrictions?
- Does it have windows, natural sunlight, and/or nice views? Lighting can play a big role in changing the mood of a space. Encourage bringing in plants, fidget toys (yes, even for adults),
- Does it have central heat / AC?

Negotiate Your Lease Terms or Purchase
Once you find a space that works for you, you’ll want to make sure your lease clearly states what you get with the space. If a space or amenity isn't written into the lease, assume you don't have access to it!
According to the American Psychiatric Association , a good lease should clearly state, but not be limited to the following terms:
- Square footage of the office
- Storage space
- Snow removal
- Utilities (Are they included? Are you charged based on your individual or total building usage?)
- Cleaning services
- Twenty-four-hour access to the office
- What insurance coverage is required
- Policies for remodeling and redecorating
- Sublet policies
- An escape clause for certain unforeseen incidents that require you to leave your practice
- Language giving you first rights to new space that becomes available, should you decide to expand.
What is the lease term?
- For subleases and very part-time, month-to-month or annual terms are common.
- For a one-year lease or less, you don’t need to worry about consulting a commercial real estate attorney.
- For a real commercial lease, the terms are usually much longer: 3-10 years. If you’re embarking on a lease like that, consult with a commercial real estate attorney. Do not sign a multi-year lease without your attorney! I can’t stress this enough.
- With a real multi-year commercial lease, you can negotiate to bundle the costs of the buildout or renovations into the cost of the lease. An attorney can help with this. Many leases also will ask for a “personal guarantor” or “good guy guarantee” and a lawyer will help protect your interests there.
Additionally, you may want to think about:
- Building maintenance responsibility
- Elevator service
- Security services
- Snow/ice removal
Get the Proper Insurance for Your Physical Space
With a physical office space comes new insurance needs. There are a couple of different types of insurance policies you may consider.
General Liability Insurance
General liability insurance covers accidental third-party damage that arises in an in-person space, such as damage to patient property or even patient injuries. Often thought of as “slip and fall” coverage, general liability insurance can cover patient property damage, medical bills, and legal fees, among others. Note that general liability insurance does not cover damage to your own property.
Business Personal Property Insurance
Business personal property insurance protects your business equipment, like laptops, cell phones, and other durable equipment. If you work from home, it may cover some furniture too.
Commercial Property Insurance
Commercial property insurance protects your physical office space, whether rented or owned, plus tools, equipment, inventory, furniture, and personal property. If you work from home, it typically provides more comprehensive coverage than homeowners insurance. It usually protects against fire, a burst water pipe, storms, and some natural disasters.
Business Owner’s Policy
I recommend you consider a business owner’s policy as it’s the most robust type of insurance. It bundles a few types of insurance together, like commercial property insurance and general liability insurance.
The policy can also include things like medical equipment and “business interruption insurance” should something happen that renders the space unusable for a period of time.
You’ll be covered for things like a power failure that causes medication stored in a fridge to spoil, a lot of cybersecurity stuff, if an employee steals from the company, etc. A business owner’s policy is worth it rather than a super basic general liability policy—unless you’re super part-time and small-scale with no employees or space of your own.
Other Types of Insurance
The insurance policies listed above only protect your space, property, and injury to patients and their property. You’ll also want to look into comprehensive malpractice policy, as well as workers comp insurance, and cyber insurance (if not included in the BOP—which it often is).
Functional Essentials for your Practice
Medical equipment.
Before we talk decorations, let’s talk functional equipment. This may include:
- A pulse oximeter
- A scale that can also measure height if seeing children,
- A blood pressure cuff
- TMS equipment if you offer TMS
- Software for monitoring vitals if you offer ketamine or esketamine. Check if your EHR integrates with anything that tracks vitals. Osmind integrates directly with Caretaker software!

Office Technology
You’ll likely want to get standard office technology up and running as well. This includes:
- Strong internet
- An efficient scanner for when patients bring in records ( this one is a classic for clinicians and lawyers ).
- A phone (if not just using your cell phone). Some services like Spruce Health allow the use of one’s cell phone as well as VoIP phones within the office.
- Voice over the internet protocol (VoIP) and electronic fax. Hardly anyone uses landlines these days for either phone or fax. I want to emphasize: you do NOT need a fax machine, just an electronic fax solution. No one needs to buy a physical fax machine again!
- A quality EHR that streamlines intake, measurement-based care, and payments/superbills.
- Fax machine
- A secure storage cabinet and/or fridge.
- You’ll need a safe if storing medications and special medical fridges if storing any meds that require refrigeration—some of which also lock if it’s a controlled substance.
- A tablet/iPad for completing forms electronically and checking in. This is more portable and cost-effective than a kiosk and can be helpful if you don’t have a receptionist.
- A comfortable office desk chair —one with orthopedic support. This is a hot discussion on forums, but many people swear by the pricey Herman Miller Aeron chairs. Check for deals online through second-hand resellers to get them at a fraction of the full-price cost. There are also less expensive alternatives. Still, plan to spend several hundred dollars on a comfortable chair. Your back will thank you later!
- Consider if you’ll be sitting in a different chair when meeting with patients than when working at your desk. If you like to use a laptop while in that non-desk chair, consider an “air desk” or other laptop stand for a laptop.
Telehealth tools
- If you plan to have hybrid meetings or sessions with multiple people in your office and others on video, consider purchasing a Meeting Owl. 360 camera views and audio makes a huge difference in meetings. It can also help record audio and video when paired with something like Zoom—which is helpful for supervision sessions.
- A ring light setup to light your face when conducting telehealth or virtual meetings and presentations from the office.
Designing and Furnishing Your Therapeutic Space
We all know the power of setting in any therapeutic context. The way you lay out your space sets the tone from the moment the patient walks in.
When brainstorming office layouts, furniture, and artwork, a great place to start is by searching Pinterest boards. Search terms like “mental health office” and “therapist office” will likely also turn up more results than “psychiatry office.”
It can be daunting to furnish and decorate your space for the first time. Let’s cover the do’s and don’ts of psychiatry office decor.
The American Psychological Association recommends the following design practices:
- Calming colors : Keep the colors light and soothing. Soft, neutral colors such as light blue, beige, or pale green can help create a relaxing atmosphere in the office. Avoid using bright or bold colors, as these can be distracting.
- Create a cozy atmosphere : Use soft lighting, cozy blankets, and plush pillows to create a warm and inviting atmosphere in the office. This can help your clients feel more at ease and comfortable during their sessions.
- Try to bring in nature: whether that be plants, artwork, or window views. People often prefer natural-colored wood over glass and chrome. Choose low-maintenance plants that don't need a lot of sunlight, such as spider plants or succulents. I recently discovered plants you only need to water once a month. They have a reservoir of water you add to monthly (e.g. EasyPlant).
- I ncorporate positive distractions. For example, a fish tank or inviting artwork that can give patients a mini brain break. Provide fidget toys or Rubik’s cubes. Avoid anything that could be used to self-harm with or that could be a choking hazard for a child
- Placement: You’ll want to hang artwork at eye-level. Keep in mind that you and your patient will be sitting down, so you’ll want to put the art lower than you would your home for instance.
- Keep your space neat and organized . When it comes to creating a healing space for your patients, less is more. Avoid clutter! (A cluttered space can create a cluttered mind).
- Display your credentials to establish early credibility.

What NOT to do when decorating your psychiatry office:
- No cheesy inspirational artwork. This can come across as off-putting when people are in distress
- Avoid things like Buddha statutes and other “spiritual” items unless they’re central and essential to your work.
- Think carefully about any sort of family pictures that you include on your desk. It can be ok to include them but know that anything in your office is “grist for the therapeutic mill” and could be brought up by the patients.
- Think about what could get dirty easily—especially when there is bad weather—and choose fabrics and colors accordingly.
The layout of your furniture can make or break the feng-shui of your space. Dr. Liddicoat in the The Psychiatric Times offers tactical furniture and layout suggestions.
- Arrange seating between a patient and you to be at a 45-degree angle, as sitting directly opposite can be seen as confrontational.
- Consider having a couch for a patient to sit on that empowers a patient to choose their distance from you. (We also like this because it’s inclusive of patients of all body sizes).
- Place a side table with a light, tissue box, and other decorative items next to each person.
- Place a clock on a table or shelf that’s at least visible to the psychiatrist—and ideally visible to both parties—to keep track of time during the session.
- Avoid placing furniture between your seat and the patient.
- Ideally, a patient will have full visibility to the exit door from where they’re sitting and an easier path to the door than you.
- Consider placing a positive distraction directly across from where the patient will sit, such as a window or artwork.
- Design your space with moveable furniture, so you can rearrange as needed.
Dr. Liddicoat also has 10 waiting area design strategies that may be helpful for your practice.
Where to buy furniture and decorations for your psychiatry office:.
1) Online retailers: You can find a wide selection of decorations for your office on online retailers such as Amazon or Etsy. These websites offer a wide variety of options, from wall art to plants to throw pillows, so you can easily find what you're looking for.
2) Wayfair: You can get a free business account with companies like Wayfair for extra discounts. Wayfair and similar companies will also separate what furniture is “commercial grade.” If you plan to stay in a space for a long time, commercial grade is the way to go.
3) Home decor stores: Home decor stores such as Pottery Barn or West Elm may have a selection of decorations that are suitable for a psychiatry office. These stores have a range of options, from furniture to wall art to plants, so you can find everything you need in one place.
Conclusion:
There’s a lot that goes into finding, leasing, and furnishing your psychiatry office space. By following these suggestions, you’ll create a setting that’s warm and inviting for your patients.
If you’ve been following along in our “starting your practice series,” you’re so close to seeing patients! In future articles, we’ll talk about practice policies, marketing your practice, and cultivating a community for continuous learning.
Discover what’s next in mental health care. Join the Psychiatry Tomorrow newsletter.
Join 1000+ clinicians

We’re Hiring!
Discover what's next in mental health care >>
If you, or someone you know, is in crisis or needs immediate assistance, please call 911 immediately. To talk to someone now, please call the National Suicide Prevention Lifeline at 1-800-273-8255 .
Osmind Inc. © 2024 All Rights Reserved.
Privacy Policy
Terms of Service

IMAGES
VIDEO
COMMENTS
Before your first psychiatrist appointment, you'll need to provide some basic information about yourself, such as your contact information, medical history, and insurance information. It may be possible to do this online before your appointment, but you can also often do this at the office when you arrive. You should also sort out your payment ...
Your psychiatrist might order a urine test to screen for drugs and/or alcohol, as well. A physical exam, during which a doctor will note your vital signs, including weight, height, blood pressure and pulse. Screening tests for various mental health conditions, such as depression. In most cases, these are standardized questions which the ...
How to Prepare for Your Psychiatric Appointment. DEC. 10, 2021. By Katherine Ponte, JD, MBA, CPRP; Mark Costa, M.D., MPH; and Anthony J. Pavlo, Ph.D. Seeing a psychiatrist, particularly for the first time, can be intimidating. Seeking help can mean confronting the unknowns, like a possible diagnosis. Moreover, trusting a practitioner with your ...
Your first appointment with a psychiatrist will usually be 1-1.5 hours long. Your psychiatrist will: listen to you talk about your concerns and symptoms. ask questions about your general health. ask about your family history. take your blood pressure and do a basic physical check-up if it's required. ask you to fill out a questionnaire.
For this reason the initial visit will take at least 2 hours, so please plan your day accordingly, bring with you anything you may need to make your time more comfortable, and plan on arriving about 15 minutes before your appointment time. Future appointments are typically shorter and take approximately 45 minutes.
Psychiatry appointment. Seeing a psychiatrist for the first time can be intimidating, but there is no need to worry. The following list tells you what to expect at a psychiatric appointment. The first visit is the longest. Your intake appointment can take one to two hours. You'll fill out paperwork and assessments to help determine a diagnosis.
General Hospital Psychiatry 9:287-293, 1987 Google Scholar. 16. Nielsen AC, Williams TA: Depression in ambulatory medical patients: prevalence by self-report questionnaire and recognition by nonpsychiatric physicians. Archives of General Psychiatry 37:999-1004, 1980 Google Scholar. 17.
The first visit with a psychiatric provider is typically 60-90 minutes in length and is a comprehensive appointment that goes over your concerns and history. Every provider is a bit different in their approach but typically you will fill out new patient paperwork prior to your visit which will help inform your provider of your history and ...
What to expect in your video visit. Your video visit will be similar to meeting your psychiatrist in the office. We'll review any testing you might have had, which is sent to your doctor in advance through MyChart.. Then we will talk about how you are feeling, discuss any new or changing symptoms, and go over your medications and treatment progress.
Quick Guide to 2021 E/M Office/Outpatient Services (99202 - 99215) Coding Changes (.pdf) includes the summary below along with information on the new time ranges, prolonged services codes and a medical decision making table with psychiatric specific examples. The guide can be printed and serve as a handy resource as you adapt to the changes.
For new telepsychiatry encounters provided to patients under the waiver that would have been office visits, psychiatrists should consider their office as the place of service (POS) and use the place of service code 11, just as you did when you were seeing your patients in person. ... CMS issued a new ruling permitting audio only telephone care ...
Mental health-related office visits to physicians with other specialties were lowest compared with primary care and psychiatrist visits when private insurance; Medicare; or Medicaid or CHIP was the primary expected source of payment. However, among those with no insurance, the percentage of visits to other specialties (8%) was lower only when
Avoid having your back to the exit, and turn your body sideways to allow a clear path to the exit if a quick escape is necessary. Install panic buttons in each office, at the reception desk, and in bathrooms. Wear an audible alarm. Designate a safe room within the office should an escape not be possible. Call 911 if you fear for your safety or ...
If your office is stuck in the '90s, it's probably time for a change. If you're planning a vacation this summer (and I hope you are), that would be the perfect time for a redo. Your patients will be spared the dust and turmoil, tradespeople won't have to work around your office hours, and you won't have to cancel any hours that weren ...
Learn which Psychiatry CPT codes to use when doing your mental health insurance billing. Take advantage of our Osychiatry CPT codes cheat sheet PDF. Navigation. ... E/M - New Patient Office Visit - 10 Minutes: 99202: E/M - New Patient Office Visit - 20 Minutes: 99203: E/M - New Patient Office Visit - 30 Minutes: 99204:
This is true even if you work from home. If your schedule does not allow it, a telemedicine psychiatry appointment may be a better choice than a no-show for an in-office visit. You can see a doctor from your location of choice, be it at home or your office. Telepsychiatry appointments can be conducted outside business hours, as well.
Office visit for a 70-year-old male, established patient, with stable depression and recent mild forgetfulness. RY CC 13-year-old male seen for follow up visit for mood and behavior problems. Visit attended by patient and father; history obtained from both. 70-year-old male seen for follow up visit for depression. Visit attended by patient and
Returns psychiatry office visit costs per zip code for new and established patients. Last updated: Jul 11, 2022 ...
Place a side table with a light, tissue box, and other decorative items next to each person. Place a clock on a table or shelf that's at least visible to the psychiatrist—and ideally visible to both parties—to keep track of time during the session. Avoid placing furniture between your seat and the patient.
In 1938, it was granted town status. [citation needed]Administrative and municipal status. Within the framework of administrative divisions, it is incorporated as Elektrostal City Under Oblast Jurisdiction—an administrative unit with the status equal to that of the districts. As a municipal division, Elektrostal City Under Oblast Jurisdiction is incorporated as Elektrostal Urban Okrug.