
- Introduction
- Palp/Percus
- Auscultation

Palpation/Percussion
Thoracic expansion:.
- Is used to evaluate the symmetry and extent of thoracic movement during inspiration.
- Is usually symmetrical and is at least 2.5 centimeters between full expiration and full inspiration.
- Can be symmetrically diminished in ankylosing spondylitis .
- Can be unilaterally diminished in chronic fibrotic lung disease , extensive lobar pneumonia, large pleural effusions, bronchial obstruction and other disease states.
Percussion:
Percussion is the act of tapping on a surface, thereby setting the underlying structures in motion, creating a sound and palpable vibration. Percussion is used to determine whether underlying structures are fluid-filled, gas-filled, or solid. Percussion:
- Penetrates 5 - 6 centimeters into the chest cavity.
- May be impeded by a very thick chest wall.
- Produces a low-pitched, resonant note of high amplitude over normal gas-filled lungs.
- Produces a dull, short note whenever fluid or solid tissue replaces air filled lung (for example lobar pneumonia or mass) or when there is fluid in the pleural space (for example serous fluid, blood or pus).
- Produces a hyperresonant note over hyperinflated lungs (e.g. COPD ).
- Produces a tympanitic note over no lung tissue (e.g. pneumothorax ).
Diaphragmatic excursion:
- Can be evaluated via percussion.
- Is 4-6 centimeters between full inspiration and full expiration.
- May be abnormal with hyperinflation , atelectasis , the presence of a pleural effusion , diaphragmatic paralysis, or at times with intra-abdominal pathology.
- Research article
- Open access
- Published: 27 January 2023
Clinical values of diaphragmatic movement in patients with chronic obstructive pulmonary disease
- Taehwa Kim 1 , 2 na1 ,
- Sungchul Huh 3 na1 ,
- Jae Heun Chung 1 , 2 ,
- Yun Seong Kim 1 , 2 ,
- Ra Yu Yun 3 , 4 ,
- Onyu Park 5 &
- Seung Eun Lee ORCID: orcid.org/0000-0002-4266-7722 1 , 2
BMC Pulmonary Medicine volume 23 , Article number: 33 ( 2023 ) Cite this article
2132 Accesses
1 Citations
1 Altmetric
Metrics details
The limitation of activity due to dyspnea in chronic obstructive pulmonary disease (COPD) patients is affected by diaphragmatic dysfunction and reduced lung function. This study aimed to analyze the association between diaphragm function variables and forced expiratory volume in the first second (FEV1) and to estimate the clinical significance of diaphragm function in the correlation between COPD severity and lung function.
This prospective, single-center, cross-sectional observational study enrolled 60 COPD patients in a respiratory outpatient clinic. Data for baseline characteristics and the dyspnea scale were collected. Participants underwent a pulmonary function test (PFT), a 6-minute walk test (6MWT), and diaphragm function by ultrasonography.
The right excursion at forced breathing showed the most significant correlation with FEV1 ( r = 0.370, p = 0.004). The cutoff value was 6.7 cm of the right diaphragmatic excursion at forced breathing to identify the FEV1 above 50% group. In the group with a right diaphragmatic excursion at forced breathing < 6.7 cm, modified Medical Research Council (mMRC), St. George's Respiratory Questionnaire and the total distance of 6MWT showed no difference between groups with FEV1 under and above 50% ( p > 0.05). In the group with ≥ 6.7 cm, mMRC and the total distance of 6MWT showed a significant difference between FEV1 under and above 50% ( p = 0.014, 456.7 ± 69.7 m vs. 513.9 ± 60.3 m, p = 0.018, respectively).
The right diaphragmatic forced excursion was closely related to FEV1, and analysis according to the right diaphragmatic forced excursion-based cut-off value showed a significant difference between both groups. When the diaphragm function was maintained, there was a lot of difference in the 6MWT’s factors according to the FEV1 value. Our data suggest that diaphragmatic function should be performed when interpreting PFT.
Peer Review reports
Introduction
The most common complaint in respiratory diseases regardless of the disease type is dyspnea [ 1 ]. COPD is characterized by worsening dyspnea during movement [ 2 ]. COPD restricts various activities of daily living due to shortness of breath, leading to poor quality of life and increased mortality and morbidity [ 3 ]. There are many causes of dyspnea; however, for patients with stable COPD, a major contributor is the weakening of the respiratory muscles, excluding conditions such as acute infectious diseases [ 4 ].
The diaphragm is the main respiratory muscle, particularly the inspiratory muscles. The weakness of the diaphragm in COPD has been extensively studied. Some studies have reported a significant reduction in diaphragmatic excursion in patients with COPD [ 5 , 6 , – 7 ]. Lung hyperinflation-associated shortening of the diaphragm has traditionally been considered a major cause of diaphragmatic weakness [ 8 ]. Also, there were previous studies about diaphragmatic thickness. Diaphragmatic thickness was a factor related to weaning and prognosis in patients under mechanical ventilation [ 9 , 10 ]. Recently, several studies have reported the clinical value of diaphragm ultrasonography according to COPD severity, and even compared to traditional methods, the diagnostic value of ultrasonography has proven to be reliable and useful [ 11 ]. Ultrasonography is also commonly used in medical facilities because it can be carried out anywhere, has no associated radiation risk, and can be used to adequately visualize the structure of the diaphragm [ 12 ].
Furthermore, 6MWT is an important tool for assessing exercise capacity and functional status in patients with COPD. Diaphragmatic weakness can impair physical performance, especially the 6MWT [ 13 , 14 ]. A previous study reported that pulmonary function was significantly correlated with the 6MWT in patients with severe and very severe COPD [ 15 ]. The relationship between 6MWT and PFT is a matter of connecting and understanding the respiratory muscles. PFT is used to measure the volume and flow rate of the lungs, and 6MWT is an important test for evaluating the exercise capacity and functional status of patients.
When we summarize the above, PFT correlates with 6MWT in COPD patients [ 15 ]. 6MWT can evaluate physical performance of COPD patients. Physical performance can also reflect diaphragmatic weakness [ 13 , 14 ]. Therefore, PFT correlates with 6MWT, 6MWT reflects physical performance, and physical performance was associated with diaphragmatic weakness. This relationship of PFT and diaphragmatic weakness can be expressed as follows for the patient. If the pulmonary function expressed by PFT is good, or if case which the power and strength of the respiratory muscles are good when PFT remains the same, breathing is more stable. Therefore, understanding the physiological principles of the respiratory muscle performance that establish the relationship these and compensate for this is important for managing the patient’s condition. Through this study, a review of the correlation between the PFT reflecting the 6MWT and diaphragm ultrasound features of respiratory muscle may be helpful to understand the physiological principles of patients with COPD.
Thus, this study aimed to analyze diaphragm movement characteristics using ultrasonography in patients with COPD and clarify its association with pulmonary function.
Study design and methods
Study design and participants.
This single-center, prospective, cross-sectional observational study recruited participants from a tertiary hospital outpatient respiratory clinic between April 2020 and April 2021. The inclusion criteria were: 1) patients 18 years old or older diagnosed with COPD by a pulmonologist; COPD diagnostic criterion was a post-bronchodilator FEV1/forced vital capacity (FVC) ratio < 0.70 based on the Global Initiative for Chronic Obstructive Lung Disease (GOLD), 2) patients who could maintain the required posture for diaphragm function measurement by ultrasonography and stable breathing during the examination such as 6MWT. Patients unable to cooperate with the examination and unstable patients requiring immediate medical intervention were excluded. Patients with interstitial lung disease featured on chest computed tomography (CT) that could affect diaphragm movement were also excluded.
Sixty-nine patients were enrolled, six of whom with combined interstitial lung disease on CT were excluded. Two patients were lost to follow-up, and one died before all examinations were completed. Finally, 60 patients completed all examinations for the study protocol and were included in the analysis.
All patients provided informed consent before participating in the study. Each patient’s clinical information was collected from four domains: pulmonary function, exercise capacity, body composition, and diaphragm function. Pulmonary function was evaluated through spirometry, MIP, and maximal expiratory pressure (MEP). Exercise capacity and body composition were assessed using the 6MWT and bioelectrical impedance analysis (BIA). Diaphragm dysfunction is defined as loss of muscle contractility [ 16 ]. To evaluated diaphragm dysfunction, we was assessed using ultrasonography in both the M-mode and B-mode for excursion and thickness, respectively.
Assessments
For patients who had performed a PFT within 1 month of participating in the study, the previous results were used and no retesting was performed. Patients who had no available PFT results within 1 month of participating in this study were reevaluated after enrollment. The Carefusion Vmax 20 (VIASYS Healthcare Inc. Sensormedics; Yorba Linda, CA, USA) was used for PFTs and FEV1, FVC, diffusing capacity of the lungs for CO, and total lung capacity were measured using the body plethysmography test. Regarding spirometry, the patients sat in a small booth and breathed into a mouthpiece. One technical expert from the Department of Respiratory Medicine conducted all the tests to maintain the consistency of the results.
MIP (PONY FX, COSMED Inc.; Rome, Italy) and MEP (PONY FX, COSMED Inc.; Rome, Italy) were measured in the sitting position using a portable mouth pressure meter. Three consecutive MIP and MEP measurements were taken, and the best result was recorded. The PFT was measured in a sitting position. A flanged mouthpiece was applied to the short and rigid tube of the measuring instrument and air leakage was checked around the mouthpiece before testing. The test was performed by an experienced examiner who has conducted the test for more than 8 years. MIP was measured by exhaling as deep as possible and inhaling as hard as possible for at least 1.5 s. MEP was measured by inhaling as deep as possible and exhaling as hard as possible for at least 1.5 s. Both measurements were made three times, and patients recovered to normal breathing patterns with at least a minute of break between measurements. The highest of the three measurements was recorded [ 17 ].
The 6MWT was performed according to the American Thoracic Society standards under the direction of a well-trained respiratory therapist at a 30 m indoor walking course [ 18 ]. Patients were encouraged by the instructor every minute and were allowed to rest or quit the test at any point. We measured the total distance and peripheral saturation with the portable oxygen meter. The patients’ body compositions were estimated indirectly using the BIA from a supine position (InBody S10, InBody, Co. Ltd., Seoul, Korea).
Diaphragm function was assessed using ultrasonography (LOGIQ E9, GE Healthcare; Chicago, IL, USA) obtained from both supine and sitting positions. It is generally accepted that there are positional differences in diaphragm contractility. The effects of gravitational loading on the diaphragm length-tension and body position-mediated changes in intra-abdominal pressure may explain the differences found. Not only that there is also a difference in the excursion between right and left. The excursion of the right diaphragm shows a lower value than that of the left diaphragm because the liver in the abdominal cavity restricts the movement of the right diaphragm. We also measured the diaphragm function in two positions based on this information. The supine position involved lying on the back or with the face upward while the sitting position was semi-seated (45–60 degrees). Both M-mode and B-mode imaging were used to evaluate diaphragmatic excursion and thickness, respectively. The mid-clavicular line and the liver were used as anatomical landmarks on the right side and the spleen on the left side to visualize the diaphragm in the M-mode. B-mode ultrasonography was used to measure the diaphragmatic thickness at the bilateral zone of apposition [ 19 ]. The diaphragm thickness was measured during quiet spontaneous breathing without peak inspiratory or expiratory maneuvers. The diaphragmatic thickness fraction was calculated as the difference between thickness at the end of inspiration and thickness at the end of expiration divided by thickness at the end of expiration x 100. The diaphragmatic excursion was measured as follows. The highest position of the diaphragm movement taken by the M-mode was considered to be the end-expiratory phase, whereas the lowest position was considered as the end-inspiratory phase.
The dyspnea scale used St. George's Respiratory Questionnaire (SGRQ) and the modified Medical Research Council scale (mMRC scale). The SGRQ is a self-administered questionnaire with 76 items [ 20 ]. This can identify the patient’s symptoms and the activities of daily life. mMRC scale is most commonly used in the assessment of dyspnea in chronic respiratory diseases and is a very useful and unrecognized dyspnea scale [ 21 ].
Statistical analysis
The data were analyzed using IBM SPSS (version 27.0; Chicago, IL, USA). The level of significance was set at p < 0.05. Descriptive statistics, including numbers, percentages, means, and standard deviations, were used to summarize each variable (demographics, PFTs, 6MWT, and diaphragmatic ultrasound results). The results were analyzed by independent t-test, cross-analysis, and frequency analysis. The correlation between the variables was analyzed by Pearson’s Correlation Coefficient, which confirmed the linear relationship between two variables using a scatterplot. The cut-off value was calculated using the receiver operating characteristic (ROC) curve analysis. The reference plane was 0.5 or more in the ROC curve, and the p -value < 0.05; hence, this result was adopted. Consequently, the cut-off value was confirmed when sensitivity and specificity were plotted in a line chart, which is the point where the two graphs meet.
Ethics statement
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed throughout this study. The study procedures were reviewed and approved by our Pusan National University Yangsan Hospital Institutional Review Board [IRB No. 05–2020-217].
FEV1 and diaphragm function
We assessed whether diaphragm function was associated with FEV1 (Fig. 1 ). In the total group analysis, both diaphragmatic excursion and thickness were associated with FEV1. However, the diaphragmatic excursion was more associated with FEV1 than thickness. Diaphragmatic excursion during forced breathing and in the supine position had a greater association with FEV1 than breathing at rest and in the sitting position. Additionally, when comparing the right and left under the same conditions, the right was more significant during forced breathing and in the supine position ( r = 0.370, p = 0.004,). Moreover, diaphragmatic thickness at right end-expiration was associated with FEV1. In summary, right ( r = 0.370, p = 0.004) and left ( r = 0.257, p = 0.048) diaphragmatic excursion during forced breathing in the supine position and diaphragmatic thickness at right end-expiration ( r = 0.310, p = 0.016) were significantly associated with FEV1.
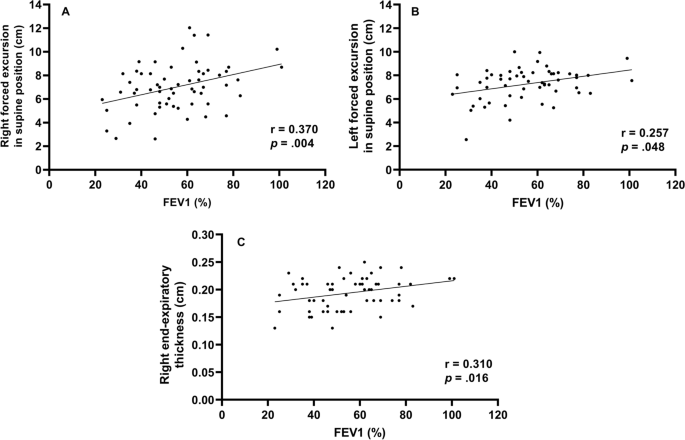
Correlation between forced expiratory volume in 1 s and diaphragm function Right forced excursion, and left forced excursion in the supine position and right end-expiratory thickness were correlated to forced expiratory volume in 1 s
Diaphragmatic function and BMI (body mass index)
To evaluate the function of the diaphragm muscle [ 22 ], the diaphragmatic excursion was measured at rest and during forced expiration (Supplement Table 1 ). In 60 patients, diaphragmatic excursion at rest in the supine position was 3.5 cm ± 1.2 on the right side and 3.5 cm ± 1.2 on the left side. During forced breathing, diaphragmatic excursion in the supine position was 6.9 cm ± 2.0 on the right side and 7.6 cm ± 1.6 on the left side. The total percent body fat was 24.2% ± 6.9. Segmental lean mass analysis was performed by direct segmental multi-frequency BIA. The lean mass was 90.5% ± 9.7 on the right arm, 88.1% ± 9.2 on the left arm, 94.5% ± 5.8 on the trunk, 95.7% ± 131.3 on the right leg, and 9.51% ± 8.8 on the left leg.
Cutoff value-associated characteristics
The ROC curve analysis of the diaphragm function variables was performed to identify the cutoff value for differentiating between FEV1 ≥ 50% and < groups. The cutoff value was ≤ 6.7 cm on the right diaphragmatic excursion at forced breathing with an area under the curve of 0.5 or more and p -value was 0.043. Right diaphragmatic excursion during forced breathing was less than the cut-off value of 6.7 cm for 26 patients and ≥ 6.7 cm for 43 patients (Table 1 ). There were no differences in age, sex, or smoking history between the two groups. The dyspnea scales such as mMRC, SGRQ, and GOLD were not significantly different between both groups. There were no differences in body mass index, percent body fat, or lean mass of the right or left legs between the groups. However, among the pulmonary function indicators, there were significant differences between the two groups. Specifically, FEV1, FVC, and MIP were significantly different (< 6.7 cm group vs. ≥ 6.7 cm group, FEV1: 49.2% ± 16.2 vs. 59.5% ± 17.2, p = 0.021; FVC: 76.2% ± 19.1 vs. 86.0% ± 15.5, p = 0.032; MIP: 67.4 cm H 2 O ± 25.1 vs. 86.5 cm H 2 O ± 28.7, p = 0.010). Concerning the 6MWT, there was a significant difference in SpO2 before 6MWT and the number of interruptions (SpO2 before 6MWT: 94.1% ± 2.7 vs. 95.3% ± 1.6, p = 0.038; number of interruptions: 4 [15.4%] vs. 0 [0%], p = 0.018). The left diaphragmatic excursion during forced breathing was also different between the two groups (6.8 cm ± 1.5 vs. 7.6 cm ± 1.3, p = 0.022) as well as the diaphragmatic thickness during right end-inspiration (0.3 cm ± 0.1 vs. 0.4 cm ± 0.1, p = 0.006). In addition, the ROC ≥ 6.7 cm group left diaphragmatic excursion was also measured with a value greater than that of the ROC < 6.7 cm group.
Subgroup characteristics according to FEV1
To identify the clinical significance of diaphragm function with the relationship between lung function, and COPD severity, the two groups classified as a right diaphragmatic excursion at 6.7 cm of forced breathing were further divided into groups based on FEV1 (< 50% or ≥ 50%) (Table 2 ). There were significant differences in age (65.0 ± 7.8 years vs. 72.7 ± 6.2 years, p = 0.011), the GOLD score ( p < 0.001), FEV1/FVC (40.1% ± 14.7 vs. 55.%4 ± 11.4, p = 0.007), peak expiratory flow rate (183.3 L/min ± 80.4 vs. 275.8 L/min ± 113.8, p = 0.027), SpO2 after the 6MWT (85.9% ± 6.5 vs. 91.5% ± 2.2, p = 0.011), and left diaphragmatic excursion during forced breathing (6.2 cm ± 1.6 vs. 7.4 cm ± 1.0, p = 0.038).
When the group with the right diaphragmatic excursion ≥ 6.7 cm was further divided into subgroups according to FEV1 (< 50% or ≥ 50%) and analyzed, mMRC, GOLD score, FEV1/FVC, MIP, peak expiratory flow rate, 6MWT, SpO2 before and after the 6MWT, and right diaphragmatic thickness at end-expiration subgroups were significantly different between the two groups.
This study contains the following: 1) evidence that FEV1 is significantly correlated with diaphragm movement, 2) cutoff values for diaphragm movement in patients with COPD, and 3) evidence to support the claim that the function of the diaphragm should be considered when interpreting the patient’s condition based on their FEV1.
First, FEV1 was significantly correlated with diaphragm movement. Studies on the relationship between the diaphragm and pulmonary function in patients with COPD are ongoing and have consistently reported that the severity of COPD and diaphragm function are closely related. Some previous studies have evaluated the direct relationship between FEV1 and diaphragm function [ 23 , 24 ].
The results of this study is also consistent with those of previous studies showing that diaphragm movement and FEV1 are related. However, beyond the findings of previous results [ 23 ], in our study, diaphragmatic excursion and thickness were found to be more correlated to FEV1 on the right side than on the left side.
Like the previous study that the thickness of the diaphragm is related to the ventilator weaning mechanical ventilation [ 9 , 10 ], this result has confirmed that the right diaphragm thickness was significantly related not only to the weaning of the ventilator and the prognosis of the patient but also to FEV1.
Second, we provided a cutoff value for a right diaphragmatic forced excursion in patients with COPD. Although there are studies that have presented a reference [ 23 ] value for healthy persons, the significant contribution of this study is the proposed reference value for patients with COPD.
We analyzed the correlation using Pearson’s correlation coefficient and confirmed the factors of diaphragmatic function-related components side (right, left), thickness, and excursion that were most-related to FEV1. Among them, Rt. forced excursion (supine), Lt. forced excursion (supine) and Rt. end-expiratory thickness showed meaningful p -value in association with FEV1. In addition, these three factors were analyzed in the linear relationship with the scattered plot and showed a proportional relationship between FEV1. Finally, when all factors related to the diaphragmatic function were analyzed, the right forced excursion was statistically determined as the most meaningful factor in relation to FEV1. We also obtained the cut-off value of 6.7 cm through the ROC curve.
The range in diaphragmatic excursion values varies considerably depending on the patient’s condition. A previous study has suggested normal values based on sex and the side of the diaphragm using healthy individuals. When breathing deeply, the right diaphragmatic excursion was 7 cm ± 1.1 in men and 5.7 cm ± 1 in women ( p < 0.001) and the left diaphragmatic excursion were 7.5 cm ± 0.9 and 6.4 cm ± 1 in men and women, respectively ( p < 0.01) [ 23 ]. In our study, we also assessed excursion during deep breathing to provide a cut-off value for patients with COPD.
When analyzed by dividing them into two groups based on a cut-off value, the following evaluation factors showed significant differences ( p < 0.05): FEV1, FVC, MIP, left forced excursion, right diaphragmatic thickness during end-inspiration, 6MWT, the SpO2 before and after 6MWT, and interruption of the 6MWT.
These factors can be broadly divided into PFT-related and performance-related factors. As mentioned above, PFT-related factors such as MIP, left diaphragmatic forced excursion and right diaphragmatic thickness during end-inspiration were lower in the < 6.7 cm group. Moreover, the SpO2 level before the 6MWT was lower in the < 6.7 cm group, the overall 6MWT was shorter, and there were many interruptions in the 6MWT. These factors might reflect activity as a performance evaluation factor. Although generalizability is limited given the few patients and the fact that all the participants were outpatients who could walk; these results may reflect an actual patient’s status. However, these findings are intended for patients who can walk, suggesting that the cut-off value of 6.7 cm may be reliable in this population.
Finally, results concerning the degree of pulmonary function and correlations with the diaphragmatic movement were noteworthy. The two groups were analyzed based on the right diaphragmatic forced excursion (6.7 cm) and divided into subgroups based on FEV1 (< 50% vs. ≥ 50%). As a result, in the group that had maintained diaphragm function (≥ 6.7 cm), the MIP, portable peak flow meter, 6MWT, SpO2 before and after the 6MWT, and right diaphragmatic thickness at end-expiration were different between the two FEV1 groups. In summary, the difference between the two FEV1 groups was large when diaphragm function was maintained; when it was not maintained, there were no differences between the two FEV1 groups. Therefore, even in patients who maintained their FEV1 > 50%, when diaphragm function deteriorated, the patient’s 6MWT, SpO2 before and after the 6MWT were less predictable (they either deteriorated or were maintained). The patients whose FEV1 decreased < 50%, if the diaphragm function was maintained, the 6MWT could be better than that in patients with an FEV1 ≥ 50% and a reduced diaphragm function.
In conclusion, when interpreting a patient’s condition based on FEV1, it is important to assess diaphragm function, since the effect of the FEV1 value on the patient depends on how well the diaphragm function has been maintained.
In this study, when the diaphragm function was maintained, there were significant differences in MIP, peak expiratory flow rate, 6MWT, SpO2 before and after the 6MWT, and right diaphragmatic thickness at end-expiration according to FEV1 in patients with COPD. Even if the diaphragm function was not maintained, because there are still differences in the FEV1, it may be beneficial to consider diaphragmatic function measured by right diaphragm excursion as an additional indicator of function beyond the FEV1. Therefore, it can be clinically helpful to check whether the diaphragm is functioning properly when determining a patient’s condition based on FEV1.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Chronic obstructive pulmonary disease
Pulmonary function test
- 6-minute walk test
Forced expiratory volume in the first second
Maximal inspiratory pressure
International Classification of Diseases 11TH
Forced vital capacity
Global Initiative for Chronic Obstructive Lung Disease
Computed tomography
Maximal expiratory pressure
Bioelectrical impedance analysis
Modified Medical Research Council
Receiver operating characteristic
Body mass index
St. George's Respiratory Questionnaire
Niedermeyer J. Dyspnea in airway and pulmonary diseases. Internist. 2015;56(8):882–9.
Article CAS Google Scholar
Antoniu SA. Descriptors of dyspnea in obstructive lung diseases. Multidisciplinary respiratory medicine. 2010;5(3):216–9.
Article Google Scholar
Lopez AD, Shibuya K, Rao C, Mathers CD, Hansell AL, Held LS, et al. Chronic obstructive pulmonary disease: current burden and future projections. Eur Respir J. 2006;27(2):397–412.
Decramer M. Respiratory muscles in COPD: regulation of trophical status Verhandelingen. Koninklijke Academie voor Geneeskunde van Belgie. 2001;63(6):577–602 discussion −4.
CAS Google Scholar
Corbellini C, Boussuges A, Villafañe JH, Zocchi L. Diaphragmatic mobility loss in subjects with moderate to very severe COPD may improve after in-patient pulmonary rehabilitation. Respir Care. 2018;63(10):1271–80.
Crimi C, Heffler E, Augelletti T, Campisi R, Noto A, Vancheri C, et al. Utility of ultrasound assessment of diaphragmatic function before and after pulmonary rehabilitation in COPD patients. Int J Chronic Obstruct Pulmon Dis. 2018;13:3131–9.
He L, Zhang W, Zhang J, Cao L, Gong L, Ma J, et al. Diaphragmatic motion studied by M-mode ultrasonography in combined pulmonary fibrosis and emphysema. Lung. 2014;192(4):553–61.
Laghi F, Tobin MJ. Disorders of the respiratory muscles. Am J Respir Crit Care Med. 2003;168(1):10–48.
Goligher EC, Fan E, Herridge MS, Murray A, Vorona S, Brace D, et al. Evolution of diaphragm thickness during mechanical ventilation. Impact Inspiratory Effort Am J Respirat Cri Care Med. 2015;192(9):1080–8.
Goligher EC, Dres M, Fan E, Rubenfeld GD, Scales DC, Herridge MS, et al. Mechanical ventilation-induced diaphragm atrophy strongly impacts clinical outcomes. Am J Respir Crit Care Med. 2018;197(2):204–13.
Boussuges A, Rives S, Finance J, Brégeon F. Assessment of diaphragmatic function by ultrasonography: current approach and perspectives. World J Clin Cases. 2020;8(12):2408–24.
Sarwal A, Walker FO, Cartwright MS. Neuromuscular ultrasound for evaluation of the diaphragm. Muscle Nerve. 2013;47(3):319–29.
Criner G. 6-minute walk testing in COPD: is it reproducible? Eur Respir J. 2011;38(2):244–5.
Hernandes NA, Wouters EF, Meijer K, Annegarn J, Pitta F, Spruit MA. Reproducibility of 6-minute walking test in patients with COPD. Eur Respir J. 2011;38(2):261–7.
Chen H, Liang BM, Tang YJ, Xu ZB, Wang K, Yi Q, et al. Relationship between 6-minute walk test and pulmonary function test in stable chronic obstructive pulmonary disease with different severities. Chin Med J. 2012;125(17):3053–8.
Google Scholar
Minami T, Manzoor K, McCool FD. Assessing diaphragm function in Chest Wall and neuromuscular diseases. Clin Chest Med. 2018;39(2):335–44.
ATS/ERS Statement on Respiratory Muscle Testing. Am J Respir Crit Care Med. 2002;166(4):518–624.
ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111–7.
Matamis D, Soilemezi E, Tsagourias M, Akoumianaki E, Dimassi S, Boroli F, et al. Sonographic evaluation of the diaphragm in critically ill patients. Technique and clinical applications. Intensive Care Med. 2013;39(5):801–10.
Jones PW, Quirk FH, Baveystock CM. The St George's respiratory questionnaire. Respir Med. 1991;85 Suppl B(25-31):discussion 3-7.
Launois C, Barbe C, Bertin E, Nardi J, Perotin JM, Dury S, et al. The modified Medical Research Council scale for the assessment of dyspnea in daily living in obesity: a pilot study. BMC pulmonary medicine. 2012;12:61.
Dhungana A, Khilnani G, Hadda V, Guleria R. Reproducibility of diaphragm thickness measurements by ultrasonography in patients on mechanical ventilation. World J Critical Care Med. 2017;6(4):185–9.
Boussuges A, Gole Y, Blanc P. Diaphragmatic motion studied by m-mode ultrasonography: methods, reproducibility, and normal values. Chest. 2009;135(2):391–400.
Rocha FR, Brüggemann AK, Francisco DS, Medeiros CS, Rosal D, Paulin E. Diaphragmatic mobility: relationship with lung function, respiratory muscle strength, dyspnea, and physical activity in daily life in patients with COPD. Jornal brasileiro de pneumologia : publicacao oficial da Sociedade Brasileira de Pneumologia e Tisilogia. 2017;43(1):32–7.
Download references
Acknowledgements
Abstract has been published/presented in the Korean tuberculosis and respiratory society, the Korean tuberculosis and respiratory society fall academic presentation | 129 volume 0342 ~ 343, total 2 PAGES, 2021
https://journal.kstudy.com/ISS_Detail.asp?key=3921544&tname=kiss2002&code=YqldZWtoSqVtJTNEOTEnMSUmN/B%20Z%20xLJTNEVHJpZSUmNbNj2bRU4XB/JTNEMA ==
This study was supported by the Research Institute for Convergence of Biomedical Science and Technology (30–2020-003), Pusan National University Yangsan Hospital. The funding body played no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Taehwa Kim and Sungchul Huh contributed equally to this work.
Authors and Affiliations
Division of Respiratory, Allergy and Critical Care Medicine, Department of Internal Medicine, Pusan National University Yangsan Hospital and Pusan National University School of Medicine, Geumo-ro 20, Beomeo-ri, Yangsan-si, Gyeongsangnam-do, 50612, Republic of Korea
Taehwa Kim, Jae Heun Chung, Yun Seong Kim & Seung Eun Lee
BioMedical Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, South Korea
Department of Rehabilitation Medicine, Rehabilitation Hospital, Pusan National University Yangsan, Yangsan, South Korea
Sungchul Huh & Ra Yu Yun
Pusan National University School of Medicine, Yangsan, South Korea
College of Nursing, Pusan National University, Pusan National University Yangsan Hospital, Yangsan, South Korea
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: TK, SEL. Data acquisition and analysis: TK, OP, RYY, SH, JHC, SEL. Data interpretation: TK, RYY, SH, JHC, SEL. Validation: TK, JHC. Writing – original draft: SH, TK. Writing – review: SEL, JHC, YSK. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Seung Eun Lee .
Ethics declarations
Ethics approval and consent to participate.
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) [ 17 ]. The study was approved by Pusan National University Yangsan Hospital (PNUYH) Institutional Review Board (IRB No. 05–2020-217) and individual consent for this retrospective analysis was waived.
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest or funding sources to declare.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kim, T., Huh, S., Chung, J.H. et al. Clinical values of diaphragmatic movement in patients with chronic obstructive pulmonary disease. BMC Pulm Med 23 , 33 (2023). https://doi.org/10.1186/s12890-022-02220-7
Download citation
Received : 25 April 2022
Accepted : 02 November 2022
Published : 27 January 2023
DOI : https://doi.org/10.1186/s12890-022-02220-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cut-off value
BMC Pulmonary Medicine
ISSN: 1471-2466
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Effect of Chest Resistance and Expansion Exercises on Respiratory Muscle Strength, Lung Function, and Thoracic Excursion in Children with a Post-Operative Congenital Diaphragmatic Hernia
Affiliations.
- 1 Department of Health and Rehabilitation Sciences, College of Applied Medical Sciences, Prince Sattam Bin Abdulaziz University, Al-Kharj 11942, Saudi Arabia.
- 2 Department of Physical Therapy for Pediatrics, Faculty of Physical Therapy, Cairo University, Giza 12613, Egypt.
- 3 Department of Physical Therapy, Kasr Al-Aini Hospital, Cairo University, Giza 12613, Egypt.
- 4 Department of Pediatrics, College of Medicine, Prince Sattam Bin Abdulaziz University, Al-Kharj 11942, Saudi Arabia.
- 5 Department of Pediatrics, Faculty of Medicine, Al-Azhar University, Assuit 71524, Egypt.
- 6 Department of Physical Therapy for Surgery, Faculty of Physical Therapy, Cairo University, Giza 12613, Egypt.
- 7 Department of Physical Therapy, College of Medical Rehabilitation, Qassim University, Buraidah 51452, Saudi Arabia.
- 8 Department of Physical Therapy, El-Sahel Teaching Hospital, General Organization for Teaching Hospitals and Institutes, Cairo 11697, Egypt.
- PMID: 35627640
- PMCID: PMC9142097
- DOI: 10.3390/ijerph19106101
Background: Congenital diaphragmatic hernia (CDH) is a life-threatening condition with long-term complications including respiratory tract infections, respiratory muscle weakness, and abnormal lung functions. This study was designed to ascertain the effects of chest resistance and chest expansion exercises on respiratory muscle strength, lung function, and chest mobility in children with post-operative CDH.
Methods: This randomized controlled clinical study was conducted in the outpatient physiotherapy clinic at Prince Sattam bin Abdulaziz University. Thirty-two children with CDH aged 10-14 years between May 2020 and February 2021 were randomly allocated to the study group ( n = 16) and the control group ( n = 16). The control group underwent a usual chest physiotherapy program; however, the study group underwent a 12-week chest resistance exercise combined with chest expansion exercise in addition to usual chest physiotherapy, with three sessions per week. Respiratory muscle strength, lung function, and thoracic excursion were assessed pre- and post-treatment.
Results: Using the 2 × 2 repeated ANOVA, significant time × group interactions were detected in favor of the study group, FVC (F = 4.82, 95% CI = -15.6 to -0.97, p = 0.005, and η 2 = 0.16), FEV1 (F = 4.54, 95% CI = -11.99 to -2.8, p ˂ 0.001, and η 2 = 0.14), PImax (F = 5.12, 95% CI = -15.71 to -5.3, p ˂ 0.001, and η 2 = 0.15), and thoracic excursion (F = 4.41, 95% CI = -2.04 to -0.16, p = 0.036, and η 2 = 0.17).
Conclusions: Concurrent chest resistance and expansion exercises may improve respiratory muscle strength, lung function, and thoracic excursion in children with post-operative CDH. The study findings suggest that concurrent chest and chest expansion exercises be part of an appropriate pulmonary rehabilitation program in children with a history of CDH.
Keywords: chest expansion exercise; chest resistance exercise; diaphragmatic hernia; lung functions; respiratory muscle strength; thoracic excursion.
Publication types
- Randomized Controlled Trial
- Exercise Therapy
- Hernias, Diaphragmatic, Congenital* / surgery
- Muscle Strength / physiology
- Respiratory Muscles / physiology
Grants and funding
- Open access
- Published: 18 April 2024
Positive effect of deep diaphragmatic breathing training on gastroesophageal reflux-induced chronic cough: a clinical randomized controlled study
- Shanshan Niu 1 , 2 na1 ,
- Tongyangzi Zhang 1 na1 ,
- Wanzhen Li 1 ,
- Siwan Wen 1 ,
- Lei Dong 1 ,
- Shengyuan Wang 1 ,
- Wenbo Shi 1 ,
- Cuiqin Shi 1 ,
- Yuqin Shen 4 ,
- Qianchun Huang 4 ,
- Yaling Tan 5 ,
- Xianghuai Xu 1 &
- Li Yu 1 , 3
Respiratory Research volume 25 , Article number: 169 ( 2024 ) Cite this article
261 Accesses
Metrics details
Background and Objective
To explore the efficacy of deep diaphragmatic breathing training (DEP) in patients with gastroesophageal reflux-induced chronic cough (GERC).
A randomized controlled study was conducted involving 60 GERC patients who were divided into the intervention group and the control group (each with 30 patients). Both groups received routine medication treatment for GERC, while the intervention group received DEP training additionally. Both groups were evaluated by cough symptom scores, Hull airway reflux questionnaire (HARQ), gastroesophageal reflux diagnostic questionnaire (GerdQ), generalized anxiety disorder scale-7 (GAD-7), patient health questionnaire-9 (PHQ-9), Pittsburgh sleep quality index (PSQI), the Leicester cough questionnaire (LCQ), as well as capsaicin cough sensitivity testing, B-ultrasound and surface electromyography (sEMG) of the diaphragmatic muscles before and after treatment. The cough resolution rate and changes of the above indictors was compared between the two groups after eight weeks of treatment.
After eight weeks of treatment, cough symptoms improved in both groups, but the cough resolution rate in the intervention group of 94% was significantly higher than that in the control group of 77% (χ 2 = 6.402, P = 0.041). The intervention group showed significant improvements to the control group in GerdQ (6.13(0.35) VS 6.57(0.77)), GAD-7 (0(0;1) VS 1(0;3)), PSQI (2(1;3) VS 4(3;6)), LCQ (17.19(1.56) VS 15.88(1.92)) and PHQ-9 (0(0;0) VS 0(0;3)) after treatment. Compared to control group, sEMG activity of the diaphragmatic muscle was significantly increased in the intervention group after treatment, measured during DEP (79.00(2.49) VS 74.65 (1.93)) and quiet breathing (72.73 (1.96) VS 67.15 (2.48)).
DEP training can improve cough symptoms as an adjunctive treatment in GERC patients.
Trial registration
The protocol was registered in February 2, 2022 via the Chinese Clinical Trials Register ( http://www.chictr.org.cn/ ) [ChiCTR2200056246].
Introduction
Gastroesophageal reflux-induced chronic cough (GERC) is a common subtype of gastroesophageal reflux disease (GERD) characterized by chronic cough as the main symptom [ 1 , 2 , 3 ]. The incidence of GERC varies by region and accounts for 5 to 40% of the causes of chronic cough [ 3 , 4 ]. With the deepening understanding, advances in examination methods and changes in lifestyles and dietary structure of GERC patients, the rate of GERC in China is increasing [ 5 , 6 ]. Current guidelines in China recommend a standard anti-reflux treatment course of at least eight weeks, but 36% of patients still require the use of neuro regulators to improve treatment, which often results in side effects such as drowsiness and dizziness [ 7 ]. The treatment of GERC, therefore, remains challenging with significant impacts on patient’s quality of life and economic prospects [ 8 , 9 ].
The main pathogenesis of GERD is the weakening of the anti-reflux barrier [ 10 ]. The high-pressure zone at the gastroesophageal junction, formed by the lower esophageal sphincter (LES), diaphragm and related structures, is a critical part of the anti-reflux barrier [ 11 ]. Once the function of the diaphragm and LES is impaired, the anti-reflux barrier weakens, leading to the occurrence of GERD.
Deep diaphragmatic breathing (DEP) training transforms chest breathing or mixed chest and abdominal breathing into DEP, using the contraction and relaxation of the diaphragm muscle to achieve deep and slow rhythmic breathing. Several recent studies have shown that DEP can improve symptoms in patients with chronic obstructive pulmonary disease by enhancing the function of the diaphragm [ 12 , 13 ]. Eherer et al. found that DEP can improve the quality of life of GERD patients, reduce esophageal acid exposure time and hypothesized that DEP could enhance diaphragmatic muscle tension to strengthen the anti-reflux barrier and improve symptoms of gastroesophageal reflux [ 14 ]. The use of DEP can also enhance the pinchcock effect of the diaphragm on the LES, strengthening the anti-reflux barrier [ 11 ]. Since GERC is a subtype of GERD and the cough symptoms in GERC patients are also partially due to impaired anti-reflux barrier function, it is hypothesized that DEP may have value as a new safe and non-invasive auxiliary treatment option in GERC treatment.
This prospective randomized controlled study aimed to explore the effects of combining DEP with anti-reflux drug therapy compared to drug therapy alone on cough symptoms, reflux symptoms, quality of life as well as sleep and psychological conditions in GERC patients.
This was a single-center, randomized, controlled prospective study that recruited suspected GERC patients who visited our department from August 2021 to December 2022. Complete medical history, physical examination, capsaicin cough sensitivity test, chest CT or X-ray examination, pulmonary function test, histamine bronchial provocation test, induced sputum cytology examination and multichannel intraluminal esophageal impedance and pH monitoring (MII-pH) data were collected. The research plan was approved by the Ethics Committee (2021-064) and registered in the Chinese Clinical Trial Registry. (ChiCTR2200056246). All study subjects were informed and signed informed consent forms.
The inclusion criteria included: ① suspected GERC, aged between 18 and 80 years, and had a cough course exceeding eight weeks; ② these patients had no obvious abnormalities on chest X-ray or chest CT images, pulmonary function with forced expiratory volume in one second/forced vital capacity (FEV1/FVC) exceeding 70%, percentage of predicted FEV1 value exceeding 80% of the expected value and ③ were able to complete DEP training. ④ MII-pH where acid exposure time (AET) exceeded 6% and/or symptom association probability (SAP) exceeding 95% and/or symptom index (SI) exceeding 50%. The exclusion criteria included: ① pregnant or lactating women, smoking or smoking cessation of fewer than two years; ② abnormal moist rales on lung auscultation; ③ symptoms such as fever, hemoptysis and dyspnea; ④ who were unable to read and understand the questionnaire, refusal to sign the informed consent form. And, the patient who had incomplete data or were violated of the treatment plan and loss of follow-up would be excluded from analysis.
The GERC diagnosis criteria [ 2 , 3 , 9 , 15 , 16 ] included a cough duration exceeding eight weeks, with or without typical reflux symptoms such as acid regurgitation and heartburn, MII-pH where acid exposure time (AET) exceeded 6% and/or symptom association probability (SAP) exceeding 95% and/or symptom index (SI) exceeding 50% and cough responsive to a stepwise anti-reflux therapy (cough symptom score decreased by > 50%).
Before the enrollment and follow-up period, both groups received health education in the out-patient department: (a) avoid oversaturated bedtime eating, acid, spicy and greasy food, coffee, acid drinks and smoking; (b) head of the bed elevation and avoiding meals within 3 hours of bedtime. After enrollment, subjects were randomly divided into the intervention and the control group by computer-generated numbers. Patients were scheduled at separate times to receive individual attention and to avoid interparticipant contact. Moreover, to reduce the chance of bias emerging, team members separately acted as participant interviewers, data collators and evaluators to ensure all data were handled objectively. The cough symptom score, capsaicin cough sensitivity, Hull airway reflux questionnaire (HARQ), gastroesophageal reflux diagnostic questionnaire (GerdQ), generalized anxiety disorder scale-7 (GAD-7), patient health questionnaire-9 (PHQ-9), Pittsburgh sleep quality index (PSQI), the Leicester cough questionnaire (LCQ) was evaluated every two weeks for eight weeks. The changes in the above observation indexes at each time point in the two groups of patients were analyzed and the cough treatment effectiveness rate and the time difference of relief of each observation index were evaluated. Before and after treatment evaluated diaphragm muscle function by, diaphragm mobility, diaphragmatic thickening fraction measured by ultrasound and surface diaphragmatic EMG activity detected by surface electromyography (sEMG) were measured to compare the differences between the two groups and further evaluate the effect of DEP on the diaphragm. The consort flow diagram of study is shown in Fig. 1 .
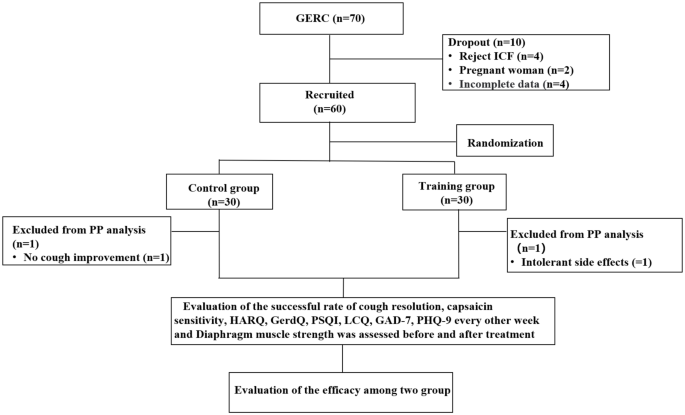
CONSORT (Consolidated Standards of Reporting Trials) flow diagram of the study. ICF: inform consent form; PP: pre-protocol; GERC: Gastroesophageal reflux-induced chronic cough; HARQ: Hull airway reflux questionnaire; GerdQ: Gastroesophageal reflux disease questionnaire; PSQI: Pittsburgh sleep quality index; LCQ: Leicester cough questionnaire; GAD-7: Generalized Anxiety Disorder Scale-7; PHQ-9: Patient Health Questionnaire-9
Therapeutic regimen
Both groups were given standard anti-reflux treatment of omeprazole (AstraZeneca, China) 20 mg twice daily and mosapride (HaoSen, China) 5 mg three times daily, for eight weeks. If no remission of cough was achieved where the cough symptom score decreased by less than 50%, intensified anti-reflux treatment including increasing the dose of proton pump inhibitor (PPI) or adding a neuromodulator such as baclofen (Novartis, China) was given. In addition to this, the intervention group received professional training from a DEP rehabilitation trainer.
Briefly, when training before the study, the patient comfortably laid on the back and placed his hands on the abdomen to feel how the abdominal wall moves in and out. Repeat this exercise 5 to 10 times. Make sure that his breathing rhythm is calm and steady, and that the inflow and outflow of air feels natural. During each DEP session, the therapist tried to achieve good communication with the patient to facilitate good understanding and collaboration.
After the training, they performed independent training twice a day for 20 min each time, with a breathing frequency of six to eight breaths per minute for the eight-week trial period and specific training methods are provided in supplement 1. The patients were video-guided and were given a checklist on which they recorded whether they had undertaken training. Besides, their relations upload training videos for us. When the patient returned for a follow-up visit every two weeks, the rehabilitation trainer evaluated the patient’s progress and provided guidance for training.
Outcome measures
The primary endpoint was the rate of cough resolution, as the sum of cough control and improvement. The cough was considered to be completely controlled when it disappeared, symptom score reduction of at least 50% was considered as cough improvement, and a cough symptom score reduction of less than 50%, no improvement, or aggravation was considered ineffective.
The second end-points included the changes in capsaicin cough sensitivity, HARQ, GerdQ, GAD-7, PHQ-9, PSQI, LCQ and diaphragm muscle performance.
Auxiliary examination
For the capsaicin cough sensitivity test, based on the measurement method reported by Fujimura et al. [ 17 ], the modified method established in reference to the ERS guideline [ 18 ] was used. The minimum concentration of capsaicin required to induce > 2 (C2) or > 5 (C5) coughs as the subject’s cough threshold to evaluate the cough sensitivity to capsaicin.
The Chinese version of the cough symptom score [ 19 ], which evolved from the English version established by Hsu et al. [ 20 ] and verified clinically in the undergraduate department, was used to evaluate cough symptoms. Cough frequency and severity were divided into six levels, from zero for no cough to five for severe coughing most of the day. The Chinese version of the HARQ [ 21 ], which corresponds to the English version of the HARQ designed by Morice et al. [ 22 ], was used to assess cough hypersensitivity in patients. The GerdQ to assess reflux-related symptoms [ 23 ], was used to score reflux-related symptoms. The LCQ was used to evaluate the patient’s quality of life measure of chronic cough [ 24 ] and the PSQI was used to evaluate the patient’s sleep quality [ 25 ]. The GAD-7 [ 26 ] and PHQ-9 [ 27 ] were used to evaluate changes in patient anxiety and depressive moods.
To measure the diaphragm muscle function by ultrasound, a professional ultrasound technician used a Medison RS80A ultrasound machine (Samsung, South Korea) to measure the diaphragm mobility and thickening ratio. The measurement methods included diaphragm excursion (DE), where the subject was placed in a semi-recumbent position with the head of the bed elevated at 20 to 40° and a linear probe was placed at the intersection of the midline of the anterior chest wall and the costal arch to measure the right diaphragm through the liver as an acoustic window, scanning towards the head side. After identifying the diaphragm, the machine was switched to M-mode and the line perpendicular to the posterior one-third of the diaphragm was sampled. The distances from the baseline to the highest point during three respiratory cycles on the vertical axis were measured and averaged to obtain DE [ 28 ].
For the diaphragm thickening fraction (DTF), the patient was in the same position and the thickness of the diaphragm was measured at the intersection of the eighth to ninth intercostal space and the anterior axillary line and mid-axillary line at the end of inspiration and expiration [ 29 ]. The calculation for DTF was the difference in thickness between the end inspiration and the end of expiration divided by the thickness at the end-expiration × 100%.
Surface electrodes were used to assess EMG of the diaphragm muscle. All electromyography signals detected by the electrodes were transmitted to a biological signal acquisition and analysis system (ECH Probes, Shanghai) and amplified and band-pass filtered in the range of 5 Hz to 1 kHz, with a gain of 104 times. Under the condition of 2–6 kHz modulo sampling, the raw electromyography signals were converted into root mean square (RMS) time-domain and frequency-domain data using ECH probes electromyography acquisition and analysis software. The subjects performed a diaphragmatic maximal voluntary contraction (MVC) by performing the combined Mueller-expulsive maneuver with visual feedback and the data were normalized. The skin was lightly cleansed with alcohol to minimize electrical impedance, placing the recoding electrodes at the junction of the right sixth to eighth ribs and the anterior axillary line and the reference electrode at the bottom away from the recording electrode [ 30 ]. The electrode placement was recorded in about to 167 anatomical landmarks to ensure consistency in electrode placement between visits and as far as possible to avoid interference of intercostal muscles. The subject was placed in a semi-recumbent position with the head of the bed elevated at 20 to 40°, and observing the activity of diaphragmatic myoelectric signals to determine whether it was respiratory contraction. After the electromyography signal was free of artifacts, the sEMG of the diaphragm was continuously recorded during quiet breathing and abdominal deep breathing. From each recording 10 breaths free of artifacts were selected at the end of each period. The mean values were calculated after RMS smoothing processing and MVC normalized, respectively.
Statistical analysis
According to previous studies [ 14 ], the effect size (d) for the two-tailed test was 0.80, the alpha value (a) was 0.05 and the statistical power (1-β) was 0.80. The sample size for the two groups was one-to-one, considering a dropout rate of 10%. Using G*Power 3.197, it was calculated that each group required 29 subjects and the total sample size was 58. To study the impact of outliers on the outcome, we used the Mahalanobis distance method to analyzed the two sets of results. By applying Mahalanobis distance method the outliers were refilled using the maximum value.
The primary efficacy analysis was evaluated using the modified intention-to-treat (ITT) method, which included all patients who received at least one dose of the study medication or a training session. All efficacy analyses were also assessed using the per-protocol (PP) method. Per-protocol population criteria included the following: subject received assigned study medication and DEP, was compliant with treatment.
For normally distributed data, the mean and standard deviation (SD) was used and for skewed distributed data, the median (Q1; Q3) were used. The cough threshold values C2 and C5 are logarithmically transformed and expressed as geometric mean for categorized data. The t-test, χ 2 test, or Mann-Whitney U test were used to compare between-group and within-group differences. Statistical analysis was performed using the SPSS 24.0 software package (SPSS, USA). A P value less than 0.05 was considered statistically significant.
General information
During the study period, a total of 70 GERC patients met the inclusion criteria. Ten patients were excluded due to exclusion criteria, including four patients who refused to sign the informed consent form, two pregnant women, four other patients with incomplete data. Sixty GERC patients were enrolled in the study, with 30 patients in the intervention group (56.7% of patients required additional treatment with neuromodulators) and 30 patients in the control group (53.3% of patients required additional treatment with neuromodulators). Adherence to DEP exercise training was achieved in 29 of 34 (85.3%), and taking medication in the control group was 29 of 32(90.6%). There was no statistical difference in adherence in each group (85.3% VS 90.6%; χ 2 = 6.402, P = 0.507). There were no differences in the general clinical information and baseline observation indicators between the two groups, shown in Tables 1 , 2 and 3 . During the treatment period, one patient in the intervention group experienced persistent intolerable diarrhea after one week of treatment and refused to continue treatment. One patient in the control group did not show improvement in cough after three weeks and refused further treatment, so both were considered treatment failures.
Comparison of cough resolution rate between the two group
A total of 58 out of 60 GERC patients (97%) completed the study. After eight weeks of treatment, by the ITT analysis, the cough treatment efficacy in the intervention group of 94% was significantly higher than that in the control group at 77% (χ 2 = 6.402, P = 0.041), as same as the PP analysis (χ 2 = 7.196, P = 0.027), as shown in Fig. 2 .
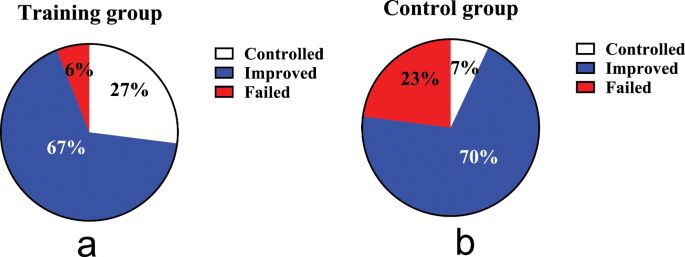
Comparison of therapeutic outcomes. ( a ): the cough treatment efficacy of the training group; ( b ): the cough treatment efficacy of the control group. The rate of cough resolution in the training group is significantly higher than in the control group (94% VS 77%, P = 0.041 by ITT, P = 0.027 by PP analysis)
Comparison of scales evaluation and capsaicin cough sensitivity before and after treatment
After eight weeks of treatment, according to ITT analysis, the intervention group showed more significant improvements than the control group in terms of nighttime cough symptoms score (Z = -2.027, P = 0.043), GerdQ (t = -2.800, P = 0.007), GAD-7 (Z = -2.096, P = 0.036), PSQI (Z = -3.705, P < 0.000), LCQ (t = 2.911, P = 0.005) and PHQ-9 (Z = -2.111, P = 0.035), while there was no statistically significant difference in capsaicin cough sensitivity (C2: t = 0.685, P = 0.496; C5: t = 1.070, P = 0.289) and HARQ (t = -1.754, P = 0.085) between the two groups. The intervention group showed faster relief of the nighttime cough symptoms score than the control group in the fourth week (Z = -2.667, P = 0.007), and.
LCQ, PHQ-9 and PSQI improved faster in the sixth week than the control group, as shown in Figs. 3 and 4 .
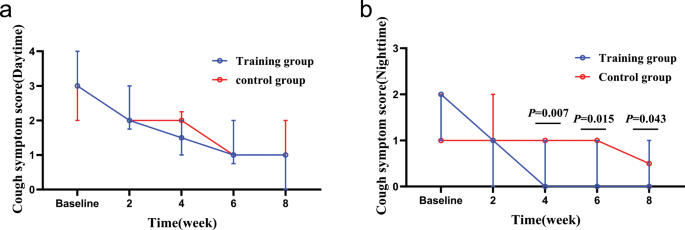
Changes in cough symptom score from baseline to the 8-week treatment between the two groups. ( a ): changes in daytime cough symptom score over time; ( b ): changes in nighttime cough symptom score over time. In the fourth week, the training group than the control group obviously relieve nighttime cough symptoms
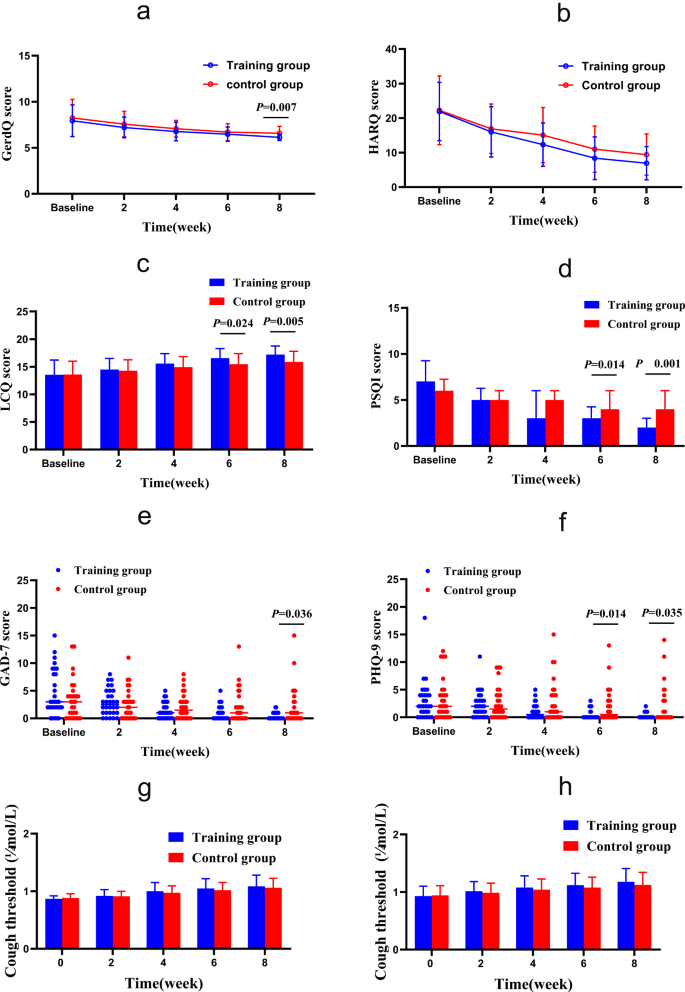
Changes of GerdQ, HARQ, LCQ, PSQI, GAD-7 and PHQ-9 from baseline to the 8-week treatment in the two groups. ( a ) GERC: Gastroesophageal reflux-induced chronic cough; ( b ) HARQ: Hull airway reflux questionnaire; ( c ) LCQ: Leicester cough questionnaire; ( d ) PSQI: Pittsburgh sleep quality index; ( e ) GAD-7: Generalized Anxiety Disorder Scale-7; ( f ) PHQ-9: Patient Health Questionnaire-9; ( g ) Capsaicin cough sensitivity: cough threshold C2; ( h ) Capsaicin cough sensitivity: cough threshold C5. *: P <0.05. After 8 weeks of treatment, GerdQ, LCQ, PSQI, GAD-7 and PHQ-9 in the intervention group were significantly relieved compared with those in the control group. In addition, LCQ, PSQI and PHQ-9 alleviated faster
There are also significant difference in the improvement of nighttime cough symptoms score, GerdQ, GAD-7, PSQI, LCQ and PHQ-9 in the intervention group was noted on PP analysis.
Comparison of DE, DTF and sEMGdi between the two groups
Before treatment, there was no significant difference in baseline data between the 22 patients in the intervention group and 20 in the control group, who completed the diaphragm examination ( P > 0.05) Supplementary Table 1 . The diaphragm mobility, diaphragm thickening rate and diaphragm sEMG activity of both groups during DEP were significantly higher than during quiet breathing, shown in Figs. 5 and 6 . Before treatment, the sEMGdi (training group: t = 7.808, P <0.001; control group: t = 8.172, P <0.001) during DEP has statistically significant contrast with quiet breathing which was consistent with DE (training group: t = 39.773, P <0.001; control group: t = 33.261, P <0.001) and DTF (training group: t = 17.970, P <0.001; control group: t = 14.620, P <0.001).
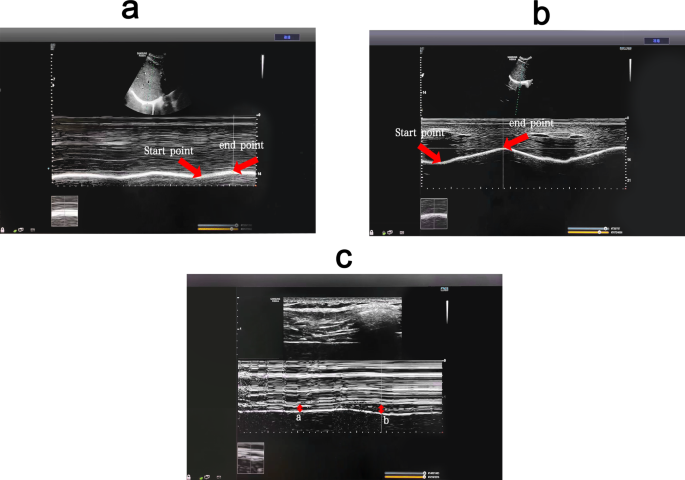
(Pre-treatment) Comparison of diaphragm excursion and diaphragm thickening fraction among breathing types. ( a ) Changes of diaphragm excursion at quiet breathing. ( b ) Changes of diaphragm excursion at abdominal deep breathing. ( c ) Changes of diaphragm thickness ( a : changes of diaphragm thickness at quiet breathing; b : changes of diaphragm thickness at abdominal deep breathing). DEP can significantly increase DE and DTF compared with quiet breathing. DEP, deep diaphragmatic breathing training; DE, diaphragmatic excursion; DTF, diaphragm thickening fraction
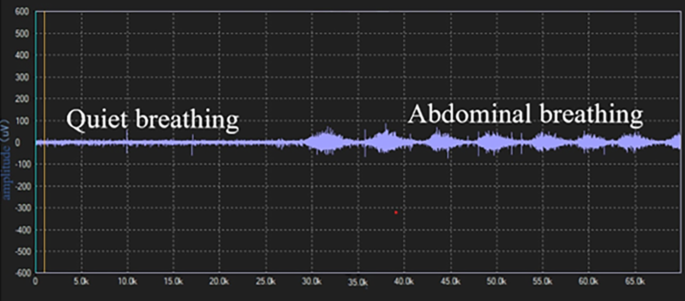
(Pre-treatment) Comparison of diaphragm EMG activity among breathing types Diaphragm sEMG activity was higher during abdominal than quiet breathing. sEMG: surface electromyogram activity
After eight weeks of treatment, the sEMGdi of the intervention group was significantly higher than that of the control group during DEP (t = 6.288, P <0.001) and quiet breathing (t = 8.136, P <0.001). The DTF of the intervention group at 169.50 (22.47) was significantly higher than that of the control group during DEP at 150.55 (25.54) (t = 2.558, P = 0.014). The measurement of DE showed that there was no statistically significant difference in diaphragm mobility between the two groups of both quiet breathing and DEP ( P > 0.05). (Table 4 .)
Comparison of DE, DTF and sEMGdi before and after treatment
In the intervention group, the post-treatment sEMG activity of the diaphragm muscle during both DEP and quiet breathing increased significantly compared to pre-treatment ( P < 0.05). The B-ultrasound measurement of diaphragm mobility during DEP of post-treatment increased significantly compared to pre-treatment( P < 0.05), while there was no statistically significant difference during quiet breathing ( P > 0.05). The DTF during both DEP and the quiet breathing of post-treatment increased compared to pre-treatment, but there was no statistically significant difference ( P > 0.05) Supplementary Table 2 . In the control group, there were no significant statistical differences observed in the post-treatment of the sEMG of the diaphragm in DEP ( P > 0.05) and quiet breathing ( P > 0.05) compared to pre-treatment. There were also no statistical differences in diaphragmatic excursion and DTF before and after treatment as well. Supplementary Table 3 .
The present study found that compared to single anti-reflux medication therapy, the combination of DEP can improve the effectiveness of GERC treatment. Compared to the control group, the intervention group showed more significant improvements in the overall evaluation of GerdQ, LCQ, PSQI, GAD-7 and PHQ-9.
The presence of GERC is an important extraesophageal manifestation of GERD. According to the pathogenesis of GERD, the weakening of the anti-reflux barrier function plays an important role in the occurrence and development of GERC. The LES and diaphragm are important components of the anti-reflux barrier. The LES is a circular muscle layer at the distal end of the esophagus. Its resting pressure is usually sufficient to prevent gastric contents from refluxing into the esophagus. However, when abdominal pressure increases, the diaphragm forms a second defense barrier to prevent reflux [ 31 ]. When LES is surgically removed, pressure can still be detected at the gastroesophageal junction [ 32 ], indicating that the diaphragm continues to maintain the anti-reflux barrier function, emphasizing the important role of the diaphragm in the anti-reflux barrier. Several studies have shown that respiratory training can increase diaphragm function [ 33 , 34 ]. The DEP technique mainly completes deep, slow and regular breathing through diaphragm contraction and relaxation. Eherer et al. found that DEP reduced acid reflux exposure in GERD patients, improved reflux symptoms and speculated that DEP training can train the crural diaphragm and reinforce the anti-reflux barrier [ 14 ].
Studies have also shown that most reflux events in GERD occur during periods of transient lower esophageal sphincter relaxation (TLESR) [ 35 ]. In addition to LES relaxation, the inhibition of the diaphragm muscle is an essential part of TLESR occurrence [ 31 ]. Banovcin et al. found that acid stimulation of the esophageal nerves can enhance gastric distension and cause a TLESR reflex, possibly by acid-activating sensory nerves in the esophagus and increasing the frequency of TLESR [ 36 ]. The use of PPIs can alleviate acid exposure-induced TLESR to some extent but cannot reduce reflux caused by LES and diaphragm dysfunction or decrease the frequency of reflux. Coughing caused by reflux is related to the total amount of proximal reflux and prolonged esophageal reflux exposure, rather than the pH value of the reflux, so most patients cannot benefit from acid suppression therapy [ 37 ].
Halland et al. found that DEP training can significantly reduce the frequency of reflux and decrease postprandial acid exposure, further improving cough symptoms in GERD [ 38 ].
Previous studies have indicated that both TLESR and the diaphragm muscle are regulated by the vagus nerve [ 39 ]. The nerve regulator baclofen is a γ-aminobutyric acid (GABA) receptor agonist that can regulate the vagus nerve pathway, reduce the occurrence of TLESR and decrease the frequency of reflux, thereby relieving cough symptoms in GERD, which is applied clinically [ 40 ]. However, some patients cannot tolerate baclofen due to the central nervous system side effects such as dizziness, drowsiness and fatigue [ 41 ]. The use of DEP training can directly or indirectly regulate the balance between sympathetic and parasympathetic nerves and is used in GERD, anxiety and other diseases [ 12 , 14 , 42 ]. Perhaps through the above mechanism, it can indirectly reduce the occurrence of TLESR, improve diaphragm function, reduce the use of baclofen and increase patient compliance with treatment.
Currently, the treatment for GERC includes medication, surgery, as well as non-pharmacological and non-surgical intervention. As people’s quality of life demands continue to rise, physical exercise and lifestyle modifications interventions for GERC are increasingly important. The guideline also points out that for suspected GERC patients without symptoms of acid reflux or heartburn, PPIs should not be the first choice and lifestyle and behavioral interventions should be prioritized [ 43 ]. Although non-pharmacological or lifestyle modifications interventions have been widely recommended for GERD patients in recent years, they are rarely mentioned for GERC patients. To the best of our knowledge, this study is the first clinical randomized controlled study on deep diaphragmatic breathing training interventions for GERC and it was concluded that this type of intervention could significantly improve the clinical symptoms of GERC patients in conjunction with medication therapy.
Based on the above mechanisms and research results, it is hypothesized that DEP training can improve the clinical symptoms of GERC patients by improving diaphragm muscle function, strengthening the anti-reflux barrier, regulating the vagal reflex, reducing the occurrence of TLESR.
To further confirm the mechanism of DEP training on the diaphragm, this study objectively evaluated diaphragm function through multiple methods. Transdiaphragmatic pressure is the main indicator for evaluating diaphragm contraction function [ 44 ], but it is invasive and difficult to widely implement in clinical practice. In recent years, studies have shown that diaphragm ultrasound can indirectly evaluate diaphragm contraction force assessing DE and DTF [ 45 ]. DE and DTF had be used to evaluate diaphragmatic function and predicted weaning from mechanical ventilation in many researches. To our knowledge, the usefulness of this technique in evaluating the changes in diaphragm function before and after DEP and speculating the effect of respiratory training on GERC has not been reported. The results showed that during DEP, diaphragm mobility was significantly increased compared to calm breathing, indicating that the diaphragm function increased accordingly, consistent with the results of Yamaguti et al. [ 13 ], and the DTF was significantly increased at post-treatment contrast to control group, indicating that DEP effectively trains the diaphragm. Compared with Wu W, et al. research on diaphragm mobility before and after rehabilitation [ 30 ], the change value did not change much and the ultrasonic sampling will be subject to echo error, for which the possibility of error cannot be excluded. The clinical significance of DEP needs to be further confirmed by large sample and multi-center independent studies. Moreover, the cause-and-effect relationship between the changes in the diaphragm and cough has not been established. Therefore, further research is necessary.
The sEMG can also quantify the work of respiratory muscles and serve as a non-invasive method to indirectly reflect respiratory muscle function [ 46 ]. In this study, sEMG was used to measure the diaphragm electromyographic activity of patients during DEP and calm breathing to evaluate changes in diaphragm contraction force. After 8 weeks of treatment, the diaphragm sEMG activity in the training group was increased in quiet breathing and deep abdominal breathing compared with those before training, in line with DE and DTF, indicating that the diaphragm function was improved under DEP. In the control group, the diaphragm electromyography activity showed an increasing trend at quiet breathing and a decreasing trend at abdominal deep breathing. The DE and DTF were not significantly or slightly increased. It may reflect that the diaphragm is prone to fatigue and its function has not improved and may be gradually deteriorating. Cough symptoms may reappear after drug withdrawal, which needs further study. The contamination of the signal picked up by surface electrodes aimed at recording diaphragm activity has also been reported. But, Similowski, et al., and Verin E, et al. [ 47 , 48 ] found that when two recording EMG electrodes are placed very close to one another, they are much more likely to record near-field potentials than far-field potentials. And the surface electrodes could be silent in response to cervical magnetic stimulation in patients with phrenic paralysis. Therefore, we believe that, surface electrodes may provide an uncontaminated diaphragm signal. And we will further to study the correlation of sEMG, di with EMGdi.
GERC is a special type of GERD manifested by a prominent cough symptom. Eherer et al. [ 14 ] research demonstrated that diaphragmatic breathing significantly reduced acid exposure and improved symptoms of GERD. Compared to the research, the patients in our study had a much wider age range, were fatter, and the standard of living was higher, leading to more difficulty in curing. Our study showed that the intervention group showed significant improvement in their gastroesophageal reflux symptoms and quality of life compared to the control group, in line with Eherer et al. research. However, the cough symptoms relief was faster than gastroesophageal reflux symptoms. Some research showed that GREC pathogenesis mainly includes two theories: reflux theory and reflex theory. DEP may not only improve diaphragmatic function, but also is significantly associated with increased thalamic GABA levels and reduced sensitivity of the cough center. The pathogenesis of GERD is complex and the prime is reflux exposure, so it is slower to relieve than cough symptoms.
In recent years, the incidence of GERC has been increasing due to changes in people’s lifestyles, improvements in corresponding diagnostic techniques and increased awareness of the disease, which is making an increasingly significant impact on people’s quality of life [ 5 ]. The LCQ, GAD-7 and PHQ-9 can measure the quality of patients’ lives. Comparing GAD-7 and PHQ-9, LCQ can comprehensively evaluate the impact of cough on patients’ lives from the physiological, psychological and social aspects. This study used the LCQ score to comprehensively evaluate changes in patients’ quality of life and found that patients who underwent DEP training were able to improve their quality of life more quickly, strengthening their treatment compliance. For chronic cough patients, especially during the pandemic, long- term uncontrollable coughing can lead to anxiety and depression, and frequent nighttime coughing can affect sleep quality, exacerbating emotional disorders. Psychological disorders can worsen patients’ sensitivity to symptoms and reduce their treatment compliance and GERD patients are more prone to comorbid anxiety and depression, leading to treatment difficulties [ 10 , 49 ] and a detrimental cycle. The DEP training is a relaxation technique that may upregulate GABA [ 50 ], regulate the balance of the sympathetic and parasympathetic nervous systems, reduce cortisol secretion, lower respiratory rate and increase heart rate variability, relieving patients’ anxiety and other emotions [ 13 , 51 ] and reducing symptom sensitivity caused by these disorders. Gu et al. found that DEP training improved patients’ psychiatric disorders and improved sleep quality by reducing negative emotions [ 42 ]. The changes in cough symptoms, anxiety and depression and sleep quality in the intervention group in this study were consistent with the above research results, further supporting the benefits of DEP training for GERC.
Gabapentin, a widely used neural regulator in clinical practice, is a GABA derivative that inhibits synaptic neurotransmitter release, thereby inhibiting the sensitivity of the cough center to reduce coughing [ 7 ]. Previous studies in this department have found that gabapentin is effective for refractory GERC, possibly because these patients have cough center hypersensitization [ 52 ] and Streeter C, et al. found that breathing was significantly associated with increased thalamic GABA levels using magnetic resonance spectroscopy [ 50 ]. , which may be another mechanism for alleviating coughing in GERC patients.
HARQ and capsaicin cough sensitivity test were related to cough hypersensitivity. In this study, the HARQ and capsaicin cough sensitivity test showed an improvement trend after 8 weeks of training while these values showed no statistically significant difference(Supplementary Table 4 ), which further confirms the DEP may inhibit the sensitivity of the cough center and relieve cough symptoms in patients with GERC.
This study had some limitations. (1) In view of the pain of the examination, patients did not want to repeat the examination, especially after the symptoms improved, so we did not require the acquisition of esophageal manometry and MII-PH data in the design of the study protocol. While the improvement in diaphragmatic muscle function was observed through B-mode ultrasound and sEMG, the changes in pressure at the gastroesophageal junction and acid exposure could not be obtained. The direct relationship between diaphragmatic muscle strength enhancement and reflux cannot therefore be confirmed. (2) The ultrasonic sampling will be subject to echo error, for which the possibility of error cannot be excluded. (3) The sample size of this study is also relatively small, mainly because the proportion of these GERC patients was very low, and it is difficult for some patients to persist in training DEP, and larger studies may be needed to support the conclusions.
Conclusions
The DEP training may increase patients’ diaphragmatic muscle function, therefore, enhance anti-reflux barriers, improve cough treatment effectiveness in patients with GERC and alleviate symptoms of gastroesophageal reflux, improve quality of life, sleep quality and alleviate anxiety and depression.
Data availability
Some or all datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Abbreviations
acid exposure time
diaphragmatic excursion
deep diaphragmatic breathing training
diaphragm thickening fraction
forced expiratory volume in one second
forced vital capacity
γ-aminobutyric acid
Generalized Anxiety DisorderScale-7
gastroesophageal reflux-induced chronic cough
gastroesophageal reflux disease
Gastroesophageal reflux diagnostic questionnaire
Hull airway reflux questionnaire
inform consent form
intention-to-treat
Leicester cough questionnaire
lower esophageal sphincter
Multichannel intraluminal esophageal impedance and pH monitoring
maximal voluntary contraction
Patient Health Questionnaire-9
per-protocol
proton pump inhibitor
Pittsburgh sleep quality index
root mean square
symptom association probability
surface electromyogram activity
surface diaphragmatic EMG activity
symptom index
transient lower esophageal sphincter relaxation
Yu L, Wei W, Lv H-J, et al. Changes in the spectrum and frequency of causes for chronic cough: a retrospective analysis [J]. Chin J Tuberc Respir Dis. 2009;32:414–7.
Google Scholar
Chinese Medical Association of Respiratory Diseases Association Asthma Group. Guidelines for the diagnosis and treatment of coughing (2015). Chin J Tuberc Respir Dis. 2016;39:323–54.
Irwin RS. Chronic cough due to gastroesophageal reflux disease: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 Suppl):S80–94.
Article Google Scholar
Lai K, Chen R, Lin J et al. A prospective, multicenter survey on causes of chronic cough in China[J]. Chest, 2013, 143(3).
Ding H, Xu X, Wen S, et al. Changing etiological frequency of chronic cough in a tertiary hospital in Shanghai, China[J]. J Thorac Dis. 2019;11(8):3482–9.
Article PubMed PubMed Central Google Scholar
Chen Q, Qiu Z. Gastrointestinal Tract: Assessment and Treatment of Cough. Diagnosis and Treatment of Chronic Cough, 2021: 47–54.
Zhang M, Zhu Y, Dong R, et al. Gabapentin versus baclofen for treatment of refractory gastroesophageal reflux-induced chronic cough[J]. J Thorac Dis. 2020;12(9):5243–50.
Lv HJ, Qiu ZM. Refractory chronic cough due to gastroesophageal reflux: definition, mechanism and management[J]. World J Methodol. 2015;5(3):149–56.
Xu X, Lv H, Yu L, et al. A stepwise protocol for the treatment of refractory gastroesophageal reflux-induced chronic cough[J]. J Thorac Dis. 2016;8(1):178–85.
PubMed PubMed Central Google Scholar
Tack J, Pandolfino JE. Pathophysiology of gastroesophageal reflux Disease[J]. Gastroenterology. 2018;154(2):277–88.
Article CAS PubMed Google Scholar
Zachariah RA, Goo T, Lee RH. Mechanism and pathophysiology of gastroesophageal reflux Disease[J]. Gastrointest Endosc Clin N Am. 2020;30(2):209–26.
Article PubMed Google Scholar
Hamasaki H. Effects of diaphragmatic breathing on Health: a narrative Review[J]. Med (Basel), 2020, 7(10).
Yamaguti WP, Claudino RC, Neto AP et al. Diaphragmatic breathing training program improves abdominal motion during natural breathing in patients with chronic obstructive pulmonary disease: a randomized controlled trial. Arch Phys Med Rehabil 2012;93(4).
Eherer AJ, Netolitzky F, Hogenauer C, et al. Positive effect of abdominal breathing exercise on gastroesophageal reflux disease: a randomized, controlled study[J]. Am J Gastroenterol. 2012;107(3):372–8.
Gyawali CP, Kahrilas PJ, Savarino E, et al. Modern diagnosis of GERD: the Lyon Consensus[J]. Gut. 2018;67(7):1351–62.
Xu X, Chen Q, Liang S, et al. Comparison of gastroesophageal reflux disease questionnaire and multichannel intraluminal impedance pH monitoring in identifying patients with chronic cough responsive to anti-reflux therapy[J]. Chest. 2014;145(6):1264–70.
Fujimura M, Sakamoto S, Kamio Y, et al. Effects of methacholine induced bronchoconstriction and procaterol induced bronchodilation on cough receptor sensitivity to inhaled capsaicin and tartaric acid[J]. Thorax. 1992;47(6):441–5.
Article CAS PubMed PubMed Central Google Scholar
Morice AH, Fontana GA, Belvisi MG, et al. ERS guidelines on the assessment of cough. Eur Respir J. 2007;29:1256–76.
Zhao T, Qiu Z, Wang L, Li Y, Lv H, Qiu Z. Validation of the reliability and clinical value of the simplified cough score. Chin J Gen Pract. 2012;11:273–6.
Hsu JY, Stone RA, Logan-Sinclair RB, et al. Coughing frequency in patients with persistent cough: assessment using a 24 hour ambulatory recorder[J]. Eur Respir J. 1994;7(7):1246–53.
Huang Y, Yu L, Xu XH, et al. Validation of the Chinese version of Hull Airway Reflux Questionnaire and its application in the evaluation of chronic cough. Zhonghua Jie He He Hu Xi Za Zhi. 2016;39:355–61.
CAS PubMed Google Scholar
Morice AH, Faruqi S, Wright CE, et al. Cough hypersensitivity syndrome: a distinct clinical entity[J]. Lung. 2011;189(1):73–9.
Lacy B, Chehade R, Crowell M. A prospective study to compare a Symptom-based reflux disease questionnaire and Impedance-pH monitoring for the identification of gastroesophageal reflux disease: 46[J]. Am J Gastroenterol. 2010;105:S17.
Birring SS. Development of a symptom specific health status measure for patients with chronic cough: Leicester Cough Questionnaire (LCQ)[J]. Thorax. 2003;58(4):339.
Mollayeva T, Thurairajah P, Burton K, et al. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: a systematic review and meta-analysis[J]. Sleep Med Rev. 2016;25:52–73.
Dear BF, Titov N, Sunderland M, et al. Psychometric comparison of the generalized anxiety disorder scale-7 and the Penn State worry questionnaire for measuring response during treatment of generalised anxiety disorder[J]. Cogn Behav Ther. 2011;40(3):216–27.
Negeri ZF, Levis B, Sun Y, et al. Accuracy of the Patient Health Questionnaire-9 for screening to detect major depression: updated systematic review and individual participant data meta-analysis[J]. BMJ. 2021;375:n2183.
Boussuges A, Gole Y, Blanc P. Diaphragmatic motion studied by m-mode ultrasonography: methods, reproducibility, and normal values[J]. Chest. 2009;135(2):391–400.
Kim WY, Suh HJ, Hong SB, et al. Diaphragm dysfunction assessed by ultrasonography: influence on weaning from mechanical ventilation[J]. Crit Care Med. 2011;39(12):2627–30.
Wu W, Guan L, Li X, et al. Correlation and compatibility between surface respiratory electromyography and transesophageal diaphragmatic electromyography measurements during treadmill exercise in stable patients with COPD[J]. Int J Chron Obstruct Pulmon Dis. 2017;12:3273–80.
Boeckxstaens GE, Rohof WO. Pathophysiology of gastroesophageal reflux disease[J]. Gastroenterol Clin North Am. 2014;43(1):15–25.
Klein W. Sphincter like thoracoabdominal high pressure zone after gastrectomy[J]. Gastroenterology, 1993, 105.
Mittal RK, Rochester DF, Mccallum RW. Effect of the diaphragmatic contraction on lower-oesophageal sphincter pressure in man.[J]. Gut. 1988;28(12):1564–8.
Sun X, Shang W, Wang Z, et al. Short-term and long-term effect of diaphragm biofeedback training in gastroesophageal reflux disease: an open-label, pilot, randomized trial[J]. Dis Esophagus. 2016;29(7):829–36.
Roman S, Holloway R, Keller J et al. Validation of criteria for the definition of transient lower esophageal sphincter relaxations using high-resolution manometry[J]. Neurogastroenterol Motil, 2017, 29(2).
Banovcin P Jr., Halicka J, Halickova M, et al. Studies on the regulation of transient lower esophageal sphincter relaxations (TLESRs) by acid in the esophagus and stomach[J]. Dis Esophagus. 2016;29(5):484–9.
Herregods TVK, Pauwels A, Jafari J, et al. Determinants of reflux-induced chronic cough[J]. Gut. 2017;66(12):2057–62.
Halland M, Bharucha A, Crowell M, et al. Effects of diaphragmatic breathing on the pathophysiology and treatment of upright gastroesophageal reflux: a randomized controlled Trial[J]. Am J Gastroenterol. 2021;116(1):86–94.
Mittal RK, Fisher MJ. Electrical and mechanical inhibition of the crural diaphragm during transient relaxation of the lower esophageal sphincter[J]. Gastroenterology. 1990;99(5):1265–8.
Xu X, Chen Q, Liang S, et al. Successful resolution of refractory chronic cough induced by gastroesophageal reflux with treatment of baclofen. Cough. 2012;8(1):8.
Dong R, Xu X, Yu L, et al. Randomised clinical trial: gabapentin vs baclofen in the treatment of suspected refractory gastro-oesophageal reflux-induced chronic cough[J]. Aliment Pharmacol Ther. 2019;49(6):714–22.
Fangchen GU, Meifeng WANG, Zheng LIN, et al. Effect of abdominal deep breathing exercises on gastrointestinal and psychological symptom clusters in patients with gastroesophageal reflux disease[J]. Chin J Nurs. 2019;54(4):501–5.
Kahrilas PJ, Altman KW, Chang AB, et al. Chronic Cough due to Gastroesophageal Reflux in adults: CHEST Guideline and Expert Panel Report[J]. Chest. 2016;150(6):1341–60.
Kim MJ, Druz WS, Danon J, et al. Mechanics of the canine diaphragm[J]. J Appl Physiol. 1976;41(3):369–82.
Goligher EC, Laghi F, Detsky ME, et al. Measuring diaphragm thickness with ultrasound in mechanically ventilated patients: feasibility, reproducibility and validity[J]. Intensive Care Med. 2015;41(4):642–9.
Bellani G, Mauri T, Coppadoro A, et al. Estimation of patient’s inspiratory effort from the electrical activity of the diaphragm[J]. Crit Care Med. 2013;41(6):1483–91.
Similowski T, Mehiri S, Attali V, Duguet A, Straus C, Derenne JP. Comparison of magnetic and electrical phrenic nerve stimulation in assessment of phrenic nerve conduction time. J Appl Physiol. 1997;82:1190–9.
Verin E et al. Validation of improved recording site to measure phrenic conduction from surface electrodes in humans. J Appl Physiol 92.3(2002):967–74.
Yang XJ, Jiang HM, Hou XH, et al. Anxiety and depression in patients with gastroesophageal reflux disease and their effect on quality of life[J]. World J Gastroenterol. 2015;21(14):4302–9.
Streeter CC, Jensen JE, Perlmutter RM, et al. Yoga asana sessions increase brain GABA levels: a pilot study[J]. J Altern Complement Med. 2007;13(4):419–26.
Ma X, Yue ZQ, Gong ZQ, et al. The effect of diaphragmatic breathing on attention, negative affect and stress in healthy Adults[J]. Front Psychol. 2017;8:874.
Zhang Y, Qiu Z. Cough hypersensitivity syndrome [J]. Int J Respir. 2015;35(13):1015–8.
Download references
Acknowledgements
The authors are grateful to all the members of Dept. of Pulmonary and Critical Care Medicine and Tongji Hospital, Tongji University School of Medicine for the fruitful discussions and their contributions.
This study was supported by the National Natural Science Foundation of China (No. 82070102 and 82270114), the Project of Science and Technology Commission of Shanghai Municipality (No.22Y11901300, 21Y11901400 and 20ZR1451500), the Program of Shanghai Academic Research Leader (No. 22XD1422700), the Fund of Shanghai Youth Talent Support Program.
Author information
Shanshan Niua, Tongyangzi Zhanga and Wanzhen Li contributed equally to this work.

Authors and Affiliations
Department of Pulmonary and Critical Care Medicine, Tongji Hospital, School of Medicine, Tongji University, No. 389 Xincun Road, Shanghai, 200065, China
Shanshan Niu, Tongyangzi Zhang, Wanzhen Li, Siwan Wen, Lei Dong, Shengyuan Wang, Wenbo Shi, Cuiqin Shi, Xianghuai Xu & Li Yu
Department of Oncology, Shanghai Yangzhi Rehabilitation Hospital (Shanghai Sunshine Rehabilitation Center), School of Medicine, Tongji University, Shanghai, China
Shanshan Niu
Department of Allergy, Tongji Hospital, School of Medicine, Tongji University, No. 389 Xincun Road, Shanghai, 200065, China
Department of Cardiac Rehabilitation, Tongji Hospital, School of Medicine, Tongji University, No. 389 Xincun Road, Shanghai, 200065, China
Yuqin Shen & Qianchun Huang
Department of Neurology, Tongji Hospital, School of Medicine, Tongji University, No. 389 Xincun Road, Shanghai, 200065, China
You can also search for this author in PubMed Google Scholar
Contributions
Project design: LY, XHX and SSN. Data collection: SSN, TYZZ, and WZL. Data analysis: SSN, TYZZ, WZL, SWW,SYW and WBS. Manuscript preparation: SSN, TYZZ, WZL, CQS, QCH, and YLT. Revision: LD, CQS and YQS. Approval and submission: LY, XHX, SSN, TYZZ, WZL, SWW, LD, SYW, WBS, CQS, YQS, QCH and YLT.
Corresponding authors
Correspondence to Xianghuai Xu or Li Yu .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the Ethics Committee of Tongji Hospital (The ethics approval number is 2021-064). The protocol was registered in the Chinese Clinical Trials Register ( http://www.chictr.org.cn/ ) (ChiCTR2200056246). Written informed consent was obtained from all participants before enrollment.
Consent for publication
Written informed consent for publication was obtained from all participants.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Niu, S., Zhang, T., Li, W. et al. Positive effect of deep diaphragmatic breathing training on gastroesophageal reflux-induced chronic cough: a clinical randomized controlled study. Respir Res 25 , 169 (2024). https://doi.org/10.1186/s12931-024-02783-5
Download citation
Received : 17 October 2023
Accepted : 21 March 2024
Published : 18 April 2024
DOI : https://doi.org/10.1186/s12931-024-02783-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Deep diaphragmatic breathing training
- Chronic cough
- Gastroesophageal reflux
- Non-pharmacological treatment
Respiratory Research
ISSN: 1465-993X
- General enquiries: [email protected]
- Open access
- Published: 21 December 2022
Assessment of diaphragmatic role in dyspneic patients with pleural effusion
- Heba Mohamed Shalaby ORCID: orcid.org/0000-0002-4640-8613 1 &
- Hieba Gamal Ezzelregal ORCID: orcid.org/0000-0002-0872-7103 1
The Egyptian Journal of Bronchology volume 16 , Article number: 69 ( 2022 ) Cite this article
1434 Accesses
Metrics details
Dyspnea that is caused by pleural effusion and affects patients’ quality of life may not be resolved after lung expansion following pleural tapping. This study aims to investigate the role that changes in the diaphragmatic shape and movement play in the development of dyspnea in those patients.
Thirty patients with pleural effusions and dyspnea were evaluated before and at 24 h after therapeutic thoracentesis. The primary outcomes are to investigate changes in diaphragmatic shape and movement before and after thoracentesis by chest ultrasound to evaluate factors causing effusion-related dyspnoea, while the secondary outcomes are firstly to investigate the effect of pleural effusion on the cardiorespiratory, functional, and diaphragmatic variables in causing dyspnea and secondly to detect the percentages and demographics of patients who experience post-drainage dyspnea improvement.
Thirty patients with age >18 years old who had moderate to massive pleural effusion (either of benign or malignant etiology), with breathlessness were recruited from the Chest Department, Ultrasonography Unit, Ain-Shams University Hospitals. Almost all (96.7%) of the studied patients experienced shortness of breath with a mean modified Borg Score of 5.13 ± 1.78, tapping of varying amounts of pleural fluid ranging from 1000 to 2000 ml.
There is a highly significant improvement in the diaphragmatic excursion, with non-significant improvement in diaphragmatic shape, although nonsignificant correlation between diaphragmatic excursion and functional parameters (M. Borg score, spirometry, and 6MWD: 6-min walk distance), but a significant negative correlation between diaphragmatic excursion and amount of drained effusion ( P value 0.045 and 95% CI for OR 1.041–36.779). 63.3% of patients experienced dyspnea improvement after thoracocentesis, and they showed highly significant improvements in M. Borg dyspnea score, spirometry, pulse rate, respiratory rate, 6MWD, and blood oxygen saturation.
In this study, we conclude that the improvement of the diaphragmatic excursion was negatively correlated with the amount of drained effusion, but no significant correlation was detected with the functional parameters and effusion-related indices that may be caused by the small sample size of the study.
Dyspnea is a subjective suffering of breathing difficulty. It affects up to 80% of patients with malignant pleural effusion [ 1 , 2 , 3 ] and a greater percentage of those with heart failure-associated effusions [ 4 ]. It was found that pleural effusions can have a large effect, on breathing, quality of life [ 5 ], sleep [ 6 ], and exercise capacity [ 7 ].
It was previously thought that the presence of dyspnea usually depends on the effusion amount, but other factors like the patient’s cardiopulmonary condition and anemia are playing pivotal roles [ 8 ]. Although post-drainage lung expansion results in breathlessness improvement, changes in the diaphragmatic shape and movement recently are found to have the main role in dyspnea development in those patients [ 8 , 9 ].
This work studies the changes in diaphragmatic shape and movement following thoracentesis and evaluation of other factors contributing to effusion-related dyspnea for better management and decision-making for those patients.
This was a prospective cohort study conducted at the Ultrasonography Unit and Pulmonary Function Unit, Chest Department, Ain Shams University Hospitals, in Cairo, Egypt. Using Epi Info 7 program for the sample size calculation, with a margin of error = 10% and at 95% confidence level, the sample size of at least 30 participants was needed.
The primary outcomes are to investigate changes in diaphragmatic shape and movement before and after thoracentesis by chest ultrasound to evaluate factors causing effusion-related dyspnea, while the secondary outcomes are firstly to investigate the effect of pleural effusion on the cardiorespiratory, functional, and diaphragmatic variables in causing pre-drainage dyspnea and secondly to detect percentage and demographics of patients who experience post-drainage dyspnea improvement.
Inclusion criteria
Thirty patients with inclusion criteria are as follows: age >18 years old with pleural effusion (either of benign or malignant etiology) ≥ 25% of hemithorax and had breathlessness. Convenient non-random sampling was used to recruit the study sample. All patients fulfilling the inclusion criteria were included in the study till the completion of the sample size.
Exclusion criteria
The exclusion criteria are as follows: any loculated, complicated pleural effusion that necessitates surgical interventions, pleural effusion in children, mechanically ventilated patients with pleural effusion, bedridden or immobile patients with pleural effusion, patients with mental illness, pleural effusion associated with trapped lung (e.g., presence of endobronchial lesion), pleural effusion in patients with chronic liver failure, hypoalbuminemia, and any associated cause of rapid transudation.
After informed written consent from all enrolled patients or their legal guardians, all were subjected to a thorough history taking and clinical examination, standard full-size posteroanterior CXR at the time of pleural effusion diagnosis, baseline pre-drainage evaluations which included vital signs, oxygen saturation by pulse oximetry, breathlessness score (resting Borg score), serum albumin, pleural pH, transthoracic ultrasound to evaluate shape and movement of the diaphragm, spirometry, 6-min walk test (distance walked in 6 min on a straight walking track), measured according to the American Thoracic Society guidelines [ 10 ]. All of these pre-parameters were repeated again after 24–36 h from thoracentesis of at least 1000 cc pleural fluid.
It was performed according to the standard practice discussed in detail previously [ 10 ] using a Viasys Health Care spirometer, D-97204 Hochberg, Germany. The spirometry indices recorded were forced expiratory volume in the first second (FEV1), forced vital capacity (FVC), and FEV 1 /FVC ratio.
Six minute walk test (6MWT)
A 6-min walk test (6MWT) was done following the American Thoracic Society’s guidelines for the 6MWT. The patients were asked to walk for 6-min over a 30-m hallway at their own pace. The same examiner administered each examination without any encouragement. The test was stopped if patients suffered chest pain, extreme dyspnea, muscle cramps, disorientation, malaise, or hypotension. At end of the test, the total distance walked was recorded in meters. A pulse oximeter was used to measure peripheral oxygen saturation (Spo 2 ) and heart rate before and after the 6MWT (model LOX100C; Lepu Medical, Inc; Heartcare, China) [ 10 ].
Ultrasonographic evaluation
Diaphragm ultrasound was done using MindrayDP-1100Plus (2015) Shanghai, China, ultrasonographic machine for the assessment of diaphragmatic mobility and diaphragmatic excursion at the side of effusion.
Patient position
The patient would be in a supine position, and the researcher sat down on a chair on the right side of the bed at the level of the patient’s abdomen; the ultrasound device was beside him at the level of the head of the patient and then the examination was done to the affected side of effusion. The advantages of the supine position are as follows: less overall variability, less side-to-side variability, greater reproducibility, and excursion were known to be greater in the supine position for the same volume inspired than in sitting or standing positions [ 11 ].
Diaphragmatic excursion
The examination was done using a 3.5C (bandwidth 2–5 MHz) convex-phased array probe (low-frequency probe with greater depth and allowing to assess excursion), with B mode set as the default mode on the device screen. The probe of the ultrasound was put at an anterior axillary line, right/left subcostal after application of the ultrasound gel and is directed medially, cephalic, and dorsally using the liver/spleen as an acoustic window for better illustration of the diaphragm. First, switch to M mode observing the diaphragmatic movement during inspiration and expiration, then the freeze button on the ultrasound device is pressed, followed by measurement of the difference between the diaphragmatic position during inspiration and expiration, and lastly, the diaphragmatic excursion during breathing was recorded.
Thoracentesis procedure
Thoracentesis guided with chest ultrasound privileged HCP according to hospital policies and procedures was performed by the authors who are a trained pulmonologist using the standard technique in pleural tapping. The procedure was terminated if the spontaneous cessation of pleural fluid drainage or if the patient experienced discomfort with increasing symptoms such as coughing, dyspnea, chest pain, and/or vasovagal manifestations [ 12 ].
All the study steps were consistent with the ethical principles of the Declaration of Helsinki for medical research involving human subjects and were approved by the Faculty of Medicine, Ain Shams University, FMASU R 08/2020/2021.
Statistical data analysis
It was done in line with the objectives by using the SPSS program (Statistical Package for Social Sciences) software version 18. Qualitative variables were presented as percentages and Quantitative variables were presented as mean ± SD. Student’s “ t ” test and Pearson’s correlation coefficient were used as a test of significance, p <0.05 was considered as significant.
This was a prospective cohort study that included 30 patients who had pleural effusion, and 53.3% of them were males. Their mean ages were 53.70 ± 15.57 ranging from 18 to 72 years, and their mean BMI was 27.89 ± 6.96 ranging from 13.84 to 40 kg/cm 2 . The majority of them had secondary education (43.3%), and 86.7% were married. One fifth of them had no comorbidities. Eighty percent of them had different comorbidities and associated causative conditions such as diabetes mellitus, hypertension, chronic kidney disease, tuberculosis, breast cancer, pneumonia, adenocarcinoma lung, and anemia representing (13.3%, 16.7%, 6.7%, 6.7%, 16.7%, 10%, 6.7%), respectively (Table 1 ).
Almost all (96.7%) of the studied patients experienced shortness of breath Their mean modified Borg Score was 5.13 ± 1.78 ranging from 2 to 9. Less commonly chest pain (70%), followed by dry cough and fever (13.3%, 6.7%), respectively (Table 2 ).
Chemistry of almost all (96.7%) of the involved pleural effusions was exudative, and 56.7% of them were left-sided which was mainly moderate to massive (from three to five as CXR classification done). More than 70% of the effusion causes were due to malignancy with adenocarcinoma, metastatic adenocarcinoma, mesothelioma, and NHL (40%, 23.3%, 6.7%, and 3.3%), respectively. 23.3% of the effusions were related to infections. The only cause of transudate pleural (3.3%) effusion was heart failure. Tapping of different varying amounts of pleural fluid ranging from 1000 to 2000 ml and stoppage of tapping was done due to chest pain and coughing mainly which occurred in 36.7% and 30%, respectively (Table 3 ).
All 30 participants completed all the pre- and post-thoracentesis tests, they showed highly significant improvements in M. Borg dyspnea score, FVC (L), FVC (%), FEV 1 (L), FEV 1 (%), pulse rate (beat/m), respiratory rate, diaphragmatic excursion, and 6-min walk distance (6MWD) with ( P value 0.001) for all except blood oxygen saturation ( P value 0.003) (Fig. 1 ). Also, it was detected that diaphragmatic excursion was affected significantly by effusion duration (Fig. 2 ). These highly significant improvements were in the form of a highly significant increase in all previously mentioned pre thoracentesis functional assessments except pulse rate and respiratory rate (they were highly significantly decreased). They also showed a significant change in the diaphragmatic movement by M mode chest ultrasound ( P value 0.03) (Fig. 3 ). No significant change was shown in the diaphragmatic shape by B mode chest ultrasound ( P value 0.781) after thoracentesis (Table 4 ).
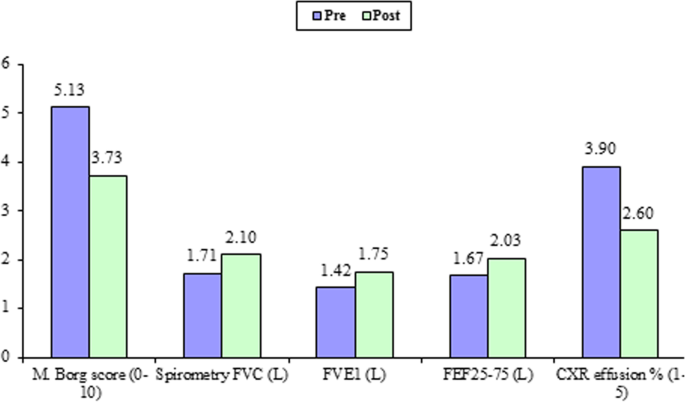
Improvement in functional and radiologic parameters after therapeutic thoracocentesis
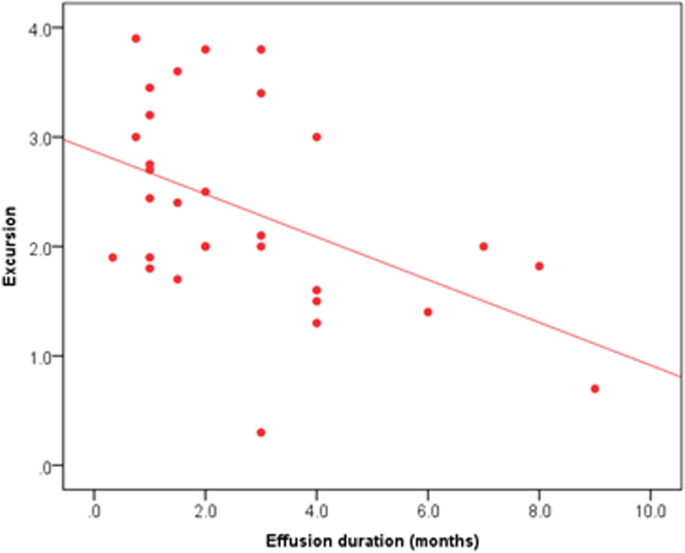
Significant relation between duration of effusion and diaphragmatic excursion
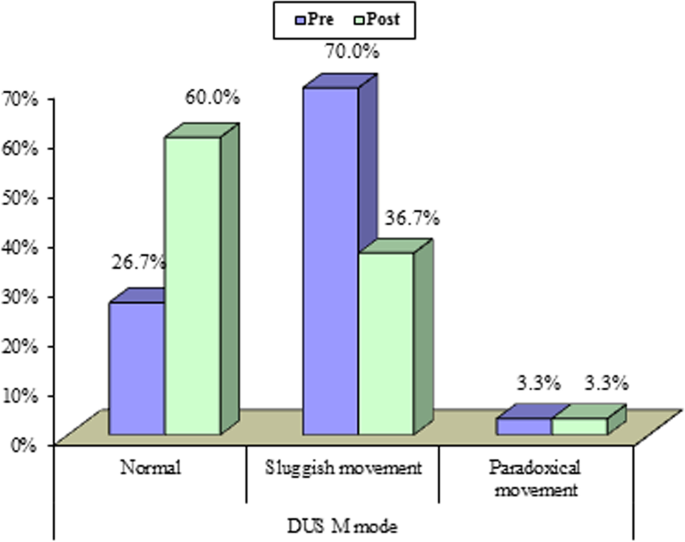
Diaphragmatic ultrasound in patients with pleural effusion showed improvement in shape and movement after therapeutic thoracocentesis
No significant correlation was found between the improvement of diaphragmatic excursion and neither the studied functional assessments (spirometry, 6 MWD) nor effusion-related indices, but the amount of effusion drained was found to be negatively correlated with the improvement of diaphragmatic excursion ( P value 0.043) (Table 5 ).
Breathing difficulty is an annoying symptom that affects the quality of life in patients with pleural effusions, and it is composed of a number of perceptions, including the sensation of effort, chest tightness, and air hunger [ 3 ]. It was found that pleural effusions can have a large effect on breathing, quality of life [ 5 ], sleep [ 6 ], and on exercise capacity [ 7 ].
It was previously thought that the presence of dyspnea usually depends on the effusion amount, the patient’s cardiopulmonary condition, and the presence of associated anemia. Many confounding and complicated factors contribute to effusion-related dyspnoea which remained not so clear. Better management and decision-making for those patients need more studies hoping to understand the underlying challenging process well. This work studied the change in diaphragmatic function following thoracentesis and evaluated it as one of the factors contributing to effusion-related dyspnoea.
Almost all the study participants (96.6%) were complaining of shortness of breath with their M. Borg dyspnea score was 5.13 ± 1.78 ranging from 2 to 7. After aspiration of 1263.33 ± 341.88 ml ranging from 1000 to 2000 ml of pleural fluid, a highly significant decrease in M. Borg dyspnea score was documented 3.73 ± 1.20 ranging from 1 to 7 with a P value of 0.001. Pleural effusions are associated with abnormalities in gas exchange, respiratory mechanics, respiratory muscle function, and hemodynamics, but the association between these abnormalities and breathlessness remains unclear. Also, the response following thoracentesis remains uncertain [ 13 ].
In this work, improvement of patients’ dyspnea score after thoracentesis was accompanied by a highly significant improvement in all documented spirometric indices FVC (L), FVC (%), FEV 1 (L), and FEV 1 (%) (1.71 ± 0.49 versus 2.10 ± 0.50, 45.28 ± 10.93 versus 55.37 ± 10.90, 1.42 ± 0.45 versus 1.75 ± 0.46, and 45.89 ± 12.19 versus 56.97 ± 13.42, respectively) with a P value of 0.001.
Some studies have demonstrated significant improvement after the removal of as little as 800 mL of pleural fluid [ 14 ]. Uniform and slow withdrawal of the pleural fluid is essential. The incidence of re-expansion pulmonary edema is increased by the rapid removal of large volumes of fluid. Finally, the inversion of a hemidiaphragm documented by chest sonography may explain the discrepancy between previous studies [ 15 , 16 ].
Others demonstrated that the PM (paradoxical movement) group showed significant improvements in lung function, gas exchange, and dyspnea following thoracocentesis, whereas the NPM (non-paradoxical movement) group did not show any significant change in any parameter. The NPM group also had better lung function, gas exchange, and dyspnea before thoracocentesis [ 17 ].
On a deep look for these improvements, we found that there were no significant correlations between any of these functional indices and the difference in the diaphragmatic excursion (excursion improvement after thoracentesis) except in the amount of effusion which was found to be negatively correlated with the improvement in the diaphragmatic excursion. Also, no effusion-related factors (type, duration, cause, side) were found to be correlated to the improvement in a diaphragmatic excursion. Different attributions could explain these non-significant correlations; in the small sample size of this study population, the etiology of pleural effusion as 73.3% of patients had malignant pleural effusion that could impair diaphragmatic excursion by more than benign causes of pleural effusion. Also, other factors such as the rate of pleural fluid accumulation (almost all effusions were exudates) and the amount of thoracic involvement of effusions were mainly from 25 to 50%, only one case showed a paradoxically moving diaphragm. Sometimes when the amount of tapping exceeds 1L, rapid lung inflation and re-expansion pulmonary edema with a larger amount of tapped effusion are associated with an irritative cough that affects the voluntary diaphragmatic function and hence its excursion.
Different studies agree that the increase in lung volumes is small and does not correlate [ 18 ] or poorly correlate [ 14 ] with the amount of aspirated pleural fluid irrespective of whether the effusion is a transudate or exudate [ 19 ]. Animal and human studies suggest that expansion in the thoracic cage is the principal mechanism by which extra volume is generated to accommodate the effusion and helps preserve lung volumes. In anesthetized dogs, infusion of saline inside the pleural cavity increased thoracic cage volume by two thirds of the total volume instilled but only reduced the functional residual capacity (FRC) by one third of the total volume instilled [ 20 , 21 ].
The increase in thoracic cage volume was achieved mainly through the downward displacement of the diaphragm [ 21 , 22 ]. In rats, bilateral pleural effusions also increased both the anteroposterior and lateral rib cage diameters [ 23 ]. Acute pleural effusions increase respiratory system elastance by increasing lung elastance, likely via lung distortion and decreases in FRC. The effect of pleural effusions on lung resistance is unclear. Pleural effusions do not appear to alter chest wall elastance or resistance [ 21 , 23 ]. Our knowledge of the effect of effusion on lung volume in humans comes mainly from changes measured pre-thoracentesis and post-thoracentesis. Although thoracentesis can improve the forced expiratory volume in the first second (FEV1) vital capacity [ 17 , 23 ], the magnitudes of increase are highly variable and often do not correlate with the volume of fluid drained. The effect of thoracentesis on FEV1 and vital capacity appears to be greater in patients with the paradoxical movement of their hemidiaphragm [ 23 ]
This study had some limitations; in the small sample of the study population, patients with pleural effusions should be selected almost matched at least as regards BMI, etiology, and size of pleural effusions. Adding whole lung volumes not only a spirometer will add accurate assessment in relation to diaphragmatic assessment pre- and post-thoracentesis.
Thoracentesis improves lung functions including spirometry and 6MWD, but not all of these improvements after thoracentesis were correlated to the improvement in a diaphragmatic excursion.
Availability of data and materials
The data sets used during the current study are available from the corresponding author on reasonable request.
Abbreviations
Body mass index
Diabetes mellitus
Hypertension
Chronic kidney disease
Tuberculosis
Modified Borg
Respiratory rate
Diaphragmatic ultrasound
Minute walk distance
Forced vital capacity
Forced expiratory volume in the first second
Forced expiratory flow
Paradoxical movement
Valdés L, San-José E, Ferreiro L et al (2013) Combining clinical and analytical parameters improves prediction of malignant pleural effusion. Lung 191:633–643
Article Google Scholar
Tanrikulu AC, Abakay A, Kaplan MA et al (2010) A clinical, radiographic and laboratory evaluation of prognostic factors in 363 patients with malignant pleural mesothelioma. Respiration 80:480–487
Nieder C, Kämpe TA, Engljähringer K (2018) Does patient-reported dyspnea reflect thoracic disease characteristics in patients with incurable cancer? Anticancer Res 38:901–904
Google Scholar
Nazemiyeh M, Dorraji A, Nouri-Vaskeh M et al (2019) Congestive heart failure is the leading cause of pleural effusion in the north-west of Iran. J Cardiovasc Thorac Res 11:244–247
Sivakumar P, Saigal A, Ahmed L (2020) Quality of life after interventions for malignant pleural effusions: a systematic review. BMJ Support Palliat Care 10:45–54
Marcondes BF, Vargas F, Paschoal FH et al (2012) Sleep in patients with large pleural effusion: impact of thoracentesis. Sleep Breath 16:483–489
Cartaxo AM, Vargas FS, Salge JM et al (2011) Improvements in the 6-min walk test and spirometry following thoracentesis for symptomatic pleural effusions. Chest 139:1424–1429
Muruganandan S, Azzopardi M, Thomas R et al The PLeural effusion and symptom evaluation (PLEASE) study of breathlessness in patients with a symptomatic pleural effusion. Eur Respir J. https://doi.org/10.1183/13993003.00980-2019
Porcel JM PLEASE, take a deep breath. Eur Respir J 55:2000501. https://doi.org/10.1183/13993003.00501-2020
Holland AE, Spruit MA, Troosters T, Puhan MA, Pepin V, Saey D et al (2014) An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J 44:1428–1446
Eugenio O, Michael C, John P, Kiran J (2001) Ultrasound evaluation of diaphragmatic motion. J Ultrasound Med 20:597–604
Antunes G, Neville E, Duffy J, Ali N, Pleural Diseases Group, Standards of Care Committee, British Thoracic Society (2003) BTS guidelines for the management of malignant pleural effusions. Thorax 58(suppl 2):ii29–ii38
Thomas R, Jenkinsd S, Eastwood PR, Leea G, Singh B (2015) Physiology of breathlessness associated with pleural effusions. Curr Opin Pulm Med 21(4):338–345
Light RW, Stansbury DW, Brown SE (1986) The relationship between pleural pressures and changes in pulmonary function after therapeutic thoracentesis. Am Rev Respir Dis 133:658–661
CAS Google Scholar
Pien GW, Gant MJ, Washam CL, Sterman DH (2001) Use of implantable pleural catheter for trapped lung syndrome in patients with malignant pleural effusion. Chest 119:1641–1646
Article CAS Google Scholar
Villena V, Lopez-Encuentra A, Pozo F, De-Pablo A, Martin-Escribano P (2000) Measurement of pleural pressure during therapeutic thoracentesis. Am J Respir Crit Care Med 162:1534–1538
Wang LM, Cherng JM, Wang JS (2007) Improved lung function after thoracocentesis in patients with paradoxical movement of a hemidiaphragm secondary to a large pleural effusion. Respirology 12:719–723
Brown NE, Zamel N, Aberman A (1978) Changes in pulmonary mechanics and gas exchange following thoracocentesis. Chest 74:540–542
Light RW, Stansbury DW, Brown SE (1981) Changes in pulmonary function following therapeutic thoracocentesis (abstract). Chest 80:341
Dechman G, Mishima M, Bates JH (1994) Assessment of acute pleural effusion in dogs by computed tomography. J Appl Physiol 76:1993–1998
Krell WS, Rodarte JR (1985) Effects of acute pleural effusion on respiratory system mechanics in dogs. J Appl Physiol 59:1458–1463
Sousa AS, Moll RJ, Pontes CF et al (1995) Mechanical and morphometrical changes in progressive bilateral pneumothorax and pleural effusion in normal rats. Eur Respir J 8:99–104
Dechman G, Sato J, Bates JH (1993) Effect of pleural effusion on respiratory mechanics, and the influence of deep inflation, in dogs. Eur Respir J 6:219–224
Download references
Acknowledgements
All deep thanks, gratitude, and appreciation to all participants who accepted to share their data in this study.
Not available.
Author information
Authors and affiliations.
Chest Department, Ain Shams University, 3 Ali Elabbady street, Ain shams, Cairo, Egypt
Heba Mohamed Shalaby & Hieba Gamal Ezzelregal
You can also search for this author in PubMed Google Scholar
Contributions
HM has put the design of the work and data acquisition and analysis, interpreted the data, and revised the manuscript. HG shared data interpretation and extensively shared in writing the results and was a major contributor to writing the manuscript. The authors have read and approved the final manuscript.
Corresponding author
Correspondence to Hieba Gamal Ezzelregal .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the Ethical Committee Board of Ain Shams University and in accordance with the Declaration of Helsinki (FWA: 000017585) (FMASU R 08/2020/2021). Informed written consent was taken from all enrolled patients.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Shalaby, H.M., Ezzelregal, H.G. Assessment of diaphragmatic role in dyspneic patients with pleural effusion. Egypt J Bronchol 16 , 69 (2022). https://doi.org/10.1186/s43168-022-00170-6
Download citation
Received : 14 May 2022
Accepted : 05 December 2022
Published : 21 December 2022
DOI : https://doi.org/10.1186/s43168-022-00170-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Chest ultrasound
- Thoracentesis
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Multidiscip Respir Med
- v.17; 2022 Jan 12

Diaphragmatic excursion by ultrasound: reference values for the normal population; a cross-sectional study in Egypt
Ahmed e. kabil.
1 Chest Diseases Department, Faculty of Medicine, Al-Azhar University, Cairo, Egypt
2 Chest Diseases Department, Faculty of Medicine for Girls, Al-Azhar University, Cairo, Egypt
3 College of Medical Rehabilitation Sciences, Taibah University, Medina, Saudi Arabia
Mahmoud Elsaeed
Houssam eldin hassanin, ibrahim h. yousef, heba h. eltrawy, ahmed m. ewis, ahmed aboseif, abdallah m. albalsha, sawsan elsawy, abdul rahman h. ali.
4 Mahatma Gandhi University, Meghalaya, India
Publisher's note: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Measurement of diaphragmatic motion by ultrasound is being utilized in different aspects of clinical practice. Defining reference values of the diaphragmatic excursion is important to identify those with diaphragmatic motion abnormalities. This study aimed to define the normal range of diaphragmatic motion (reference values) by Mmode ultrasound for the normal population.
Healthy volunteers were included in this study. Those with comorbidities, skeletal deformity, acute or chronic respiratory illness were excluded. Diaphragmatic ultrasound in the supine position was performed using a lowfrequency probe. The B-mode was applied for diaphragmatic identification, and the M-mode was employed for the recording of the amplitude of diaphragm contraction during quiet breathing, deep breathing and sniffing.
The study included 757 healthy subjects [478 men (63.14%) and 279 women (36.86%)] with normal spirometry and negative history of previous or current respiratory illness. Their mean age and BMI were 45.17 ±14.84 years and 29.36±19.68 (kg/m 2 ). The mean right hemidiaphragmatic excursion was 2.32±0.54, 5.54±1.26 and 2.90±0.63 for quiet breathing, deep breathing and sniffing, respectively, while the left hemidiaphragmatic excursion was 2.35±0.54, 5.30±1.21 and 2.97±0.56 cm for quiet breathing, deep breathing and sniffing, respectively. There was a statistically significant difference between right and left diaphragmatic excursion among all studied subjects. The ratio of right to left diaphragmatic excursion during quiet breathing was (1.009±0.19); maximum 181% and minimum 28%. Only 19 cases showed a right to left ratio of less than 50% (5 men and 14 women). The diaphragmatic excursion was higher in males than females. There was a significant difference in diaphragmatic excursion among age groups. Age, sex and BMI significantly affected the diaphragmatic motion.
Conclusions
Diaphragmatic excursion values presented in this study can be used as reference values to detect diaphragmatic dysfunction in clinical practice. Diaphragmatic motion is affected by several factors including age, sex and body mass index.
Introduction
The diaphragm is the main muscle of respiration [ 1 ]. Diaphragmatic excursion is 1-2 cm during tidal breathing and 7-11 cm during deep inspiration [ 2 ]. The assessment of diaphragmatic function is important for diagnosis and follow up of various physiologic and pathologic conditions [ 1-4 ]. Several methods exist for the evaluation of diaphragmatic function. These methods include fluoroscopy [ 3 ], computed tomography [ 4 ], magnetic resonance imaging [ 2 ], and ultrasonography [ 5 ]. Thoracic ultrasound has been reported to be a useful tool for the examination of diaphragmatic function [ 6 ]. It is a bedside non-invasive tool that provides various techniques for evaluation of diaphragmatic function including measurement of diaphragmatic excursion and thickness as well as changes during different phases of inspiration [ 7 ]. Ultrasonography has been proved to be superior to fluoroscopy and can provide accurate measurement of diaphragmatic excursion [ 3 ]. Previous studies highlighted the lack of reference values for diaphragmatic excursion in the normal population which complicates diagnosing abnormal diaphragmatic motion in certain diseases. No data is available about diaphragmatic motion in the normal Egyptian population and no reference data are available to compare with. This study aimed to explore the normal diaphragmatic excursion in the Egyptian population by M-mode ultrasonography.
This is a cross-sectional study that initially included 780 participants. Twenty-three subjects were excluded due to poor images or failed visualization of one hemidiaphragm, rendering the finally included number 757 individuals (478 males and 279 females), all had normal lung functions with no history of chest disease. Smokers, those with acute respiratory illness, chronic respiratory disease, associated comorbidities, physical disability, abnormal pulmonary function tests or history of anesthesia within the past six months were excluded from the study.
Pulmonary functions were done using spirometry (Spirosift 5000; Fukuda Denshi, Beijing, China). The operator encouraged all subjects verbally to exhale as fast and as deep as possible. Each subject performed at least three technically accepted measurements, and the best of them was selected for statistical analysis. All measurements were performed according to ERS/ATS standards [ 7 ].
Diaphragmatic ultrasound
All sonographic examinations were done by the research team. Inter-operator and intra-operator variability were excellent (data not shown). Examinations were performed at quiet temperature (22-25C°). All subjects were asked to rest for 30 min before sonography. Ultrasonography was done using an ultrasound device (SSI6000; Sonoscape, Nanshan, China), while subjects located in the supine position. Examinations were performed using 3.5 MHz curvilinear probe. Each hemidiaphragm was first visualized by Bmode, then M-mode was used to evaluate diaphragmatic excursion in tidal breathing, deep breathing and sniff. The right hemidiaphragm was measured by positioning the probe between the midclavicular and midaxillary lines below the right costal margin (subcostal approach), using the liver as an acoustic window. The probe was directed medially, cephalic and dorsally. When the hemidiaphragm was well visualized, the M-mode was applied to measure the excursion [ 8 ]. The left hemidiaphragm was visualized using the spleen as an acoustic window. The probe was positioned between the left midclavicular and midaxillary lines below the left costal margin. The probe was directed in the same way as the right side [ 8 ]. Targeting to improve visualization of the left hemidiaphragm, and overcome the small acoustic window of spleen, the probe was sometimes displaced caudally in the abdomen to obtain a better angle for visualization. The diaphragm was seen as a single echogenic line ( Figure 1 ), moving towards the probe during inspiration and away from the probe during expiration [ 5 ]. Diaphragmatic excursion was defined as the difference between the highest point and steep point (amplitude). The diaphragmatic excursion was recorded in different respiratory phases; tidal breathing (normal quiet inspiration), deep inspiration (holding up breathing after maximal inspiration), and sniffing (quick nasal inspiration with a closed mouth) ( Figure 2 ). The direction of movement was also observed (normal or paradoxical), as absent or paradoxical motion may indicate diaphragm paralysis.
Statistical analysis
All data were analyzed by SPSS (Statistical Package for Social Sciences) software version 19 (IBM corp., Armonk, NY, USA) after data cleaning and check. Numerical data were presented as mean ±SD, while categorical data were presented as number (percentage). Independent sample t-test and ANOVA were used for comparisons, Pearson correlation coefficient for testing the relationship between diaphragmatic excursion and demographic parameters, and linear regression analysis for the detection of factors affecting diaphragmatic motion. The significance level was set at a p≤0.05.
Totally, 757 healthy subjects with normal spirometry were included in this study [478 men (63.14%) and 279 women (36.86%)]. The mean age of the study population was 45.17±14.84 years. Men were significantly older, had significantly higher FVC% and VT%, while women had significantly higher body mass index (BMI) and better FEF25-75% ( Table 1 ). There was a statistically significant difference between right and left diaphragmatic excursion among all studied subjects ( Table 2 ). The ratio of right to left diaphragmatic excursion during quiet breathing was (1.009±0.19); maximum 181% and minimum 28%. Only 19 cases showed a right to left ratio less than 50% (5 men and 14 women). Right diaphrag- matic motion was significantly higher in men than in women ( Table 3 ). There were significant differences in diaphragmatic excursion among age groups ( Table 4 ). However, there were no statistically significant differences among BMI categories ( Table 5 ). A statistically significant positive correlation was found between age and right diaphragmatic excursion during both deep breathing and sniffing, and between age and left hemidiaphragmatic excursion during deep breathing (r=0.045, p˂0.001, r=0.117, p=0.001, r=0.190, p˂0.001, respectively). A statistically significant negative correlation was observed between age and left hemidiaphragmatic excursion during quiet breathing (r=-0.098, p=0.007). On the other hand, a statistically significant negative correlation was detected between BMI and right hemidiaphragmatic excursion during deep breathing and sniffing, and between BMI and left hemidiaphragmatic excursion during deep breathing (r = 0.182, p˂0.001; r = -0.094, p=0.009; r = -0.142, p˂0.001, respectively). A positive correlation between BMI and left hemidiaphragmatic excursion was found during quiet breathing (r = 0.148, p˂0.001) ( Table 6 ). Regression analysis revealed that sex, age, BMI and pulmonary functions affect diaphragmatic motion (good predictors). Age, sex and BMI index significantly affect diaphragmatic motion by variable extents during different types of breathing.

Right diaphragm visualization by B-mode ultrasound. The diaphragm is seen as a thick white line moving with respiration. The liver is used as an echogenic window.

Visualization and measurement of right diaphragmatic excursion by M-mode ultrasound. The diaphragm is seen as a white line moving with respiration. The diaphragmatic excursion is measured as the amplitude of wave seen in M-mode during breathing.
Demographic data and pulmonary functions of the studied population.
# Comparison between men and women
* p<0.05.
Diaphragmatic excursion in the normal population.
Diaphragmatic excursion according to sex.
# Comparison between men and women; *p<0.05.
Diaphragm accounts for three fourths of lung ventilation [ 9 ]. Diaphragmatic imaging is important for the diagnosis of diaphragmatic dysfunction or paralysis [ 3 , 9 ]. Normal values of diaphragmatic excursion are important to evaluate abnormalities in different diseases [ 8 ]. Diaphragmatic dysfunction (weakness or paralysis) is usually underdiagnosed in clinical practice [ 10 ]. Normal values can be used to detect either hypokinesia or hyperkinesia [ 11 ]. In this study we found that the mean diaphragmatic excursion for right hemidiaphragm during quiet breathing was 2.32±0.54 cm, while that for the left one was 2.35±0.54 cm. The mean diaphragmatic excursion during deep breathing was 5.54±1.26 cm for the right side and 5.30±1.21 cm for the left, whereas the excursion during sniffing was 2.90±0.63 cm for the right side and 2.97±0.56 cm for the contralateral hemidiaphragm. These results are in line with the results of previous reports [ 5-7 ]. Normal diaphragmatic excursion in tidal breathing in previous studies was reported to be from 1-2.5 cm [ 8 ]. These values can be affected by age, sex, body composition [ 12 , 13 ], scanning position, and phase of inspiration [ 14 ]. Right diaphragmatic excursion was shown to be significantly better in men than in women ( Table 3 ). The same results were reported by Kantarci et al . who in their study reported a significant difference in diaphragmatic motion between male and female subjects [ 13 ]. In their study, sex was the most significant factor affecting diaphragmatic function. In our study, there was a significant difference in diaphragmatic excursion among age groups ( Table 4 ). Similar results were reported in previous studies [ 6 , 8 ]. Boussuges et al. [ 8 ] reported a higher diaphragmatic excursion in men than women in all types of breathing. This can be attributed to differences in height, weight, age [ 6 , 8 ], diaphragmatic mass, diaphragmatic fiber type property, metabolic activity, contractile properties and environmental factors [ 9 ].
In the current study, a statistically significant positive correlation was observed between age and diaphragmatic excursion during both deep breathing and sniffing in the right side, and during deep breathing only in the left one. Besides, a statistically significant negative correlation was revealed between age and left hemidiaphragmatic excursion during quiet breathing ( Table 4 ). Kantarci et al . [ 13 ] found that diaphragmatic function is significantly lower in the individuals below 30 years when compared to those aged more than 30 years.
We did not find any significant statistical differences among BMI categories ( Table 5 ). However, there was a significant positive correlation between BMI and left hemidiaphragmatic excursion during quiet breathing ( Table 6 ). Moreover, regression analysis showed that age, sex and BMI are the main factors that significantly affect diaphragmatic excursion. Kantarci et al . [ 13 ] reported a significant difference in diaphragmatic motion according to BMI categories and explained this by the difference in fat and muscle composition. In the same context, Scarlata et al . [ 12 ] reported a significant correlation between diaphragmatic motion and gender, age, weight and height. This difference is clinically important for the identification of those with a risk of low diaphragmatic function to include them in rehabilitation programs. This discrepancy between studies may be due to different demographic characters and distribution of population in different body mass index categories. Increased diaphragmatic motion with increased BMI may be attributed to differences in height or the increased diaphragm weight with increased body weight [ 10 ]. This can be confirmed through the assessment of diaphragmatic thickness by ultrasonography.
Diaphragmatic excursion according to age groups.
Diaphragmatic excursion according to BMI.
Correlation with body mass index and age and diaphragmatic excursion.
BMI, body mass index; **correlation is significant at the 0.01 level (2-tailed).
The strengths of this study include the large number of studied populations, different age groups and body composition. This study reflects the normal distribution of diaphragmatic excursion in the normal population in Egypt. Knowing normal references for diaphragmatic ultrasound measurements can be of clinical value in identifying and diagnosing diaphragmatic paralysis, as well as exploring the cause and predicting the prognosis of diaphragm paralysis [ 15 ]. Diaphragmatic ultrasound normal values can be also used to predict the response to treatment as in rehabilitation programs, in addition to setting cut-off values to predict successful weaning parameters from mechanical ventilation. Likewise, it can be used to evaluate diaphragmatic function before and after surgeries. Furthermore, these values can also predict diaphragmatic dysfunction and deconditioning [ 15 ]. They can be applied as a predictor of mechanical ventilation-induced diaphragm dysfunction, too [ 16 ]. The unequal distribution of age groups, the disparity of BMI among different age groups, together with the inability to perform a simultaneous assessment of pulmonary functions and diaphragmatic motion by ultrasound due to technical difficulties are the main limitations of this study. The study included only Egyptian volunteers, which may be considered another limitation, so large worldwide studies are recommended to reach worldwide normal values that can be applied to all countries. Also, further studies are needed for assessments of diaphragmatic functions in patients with chronic respiratory diseases.
Diaphragmatic excursion values presented in this study can be used as reference values to detect diaphragmatic dysfunction in clinical practice. There is a significant statistical difference between right and left hemidiaphragmatic movement during all types of breathing (quiet, deep and sniffing). Age, sex and BMI significantly affect diaphragmatic motion with variable extents during different types of breathing. The assessment of diaphragmatic motion by ultrasound could be a useful indicator for the diagnosis and follow up of respiratory diseases, and could be added to outcomes in clinical trials. Further studies to assess other factors that may affect the diaphragmatic motion including metabolic factors and other anthropometric parameters are required.

Top 14 things to do and attractions in Mytishchi
Navigate forward to interact with the calendar and select a date. Press the question mark key to get the keyboard shortcuts for changing dates.
Navigate backward to interact with the calendar and select a date. Press the question mark key to get the keyboard shortcuts for changing dates.
1 St. Basil's Cathedral
2 All-Russian Exhibition Center

3 Kva-Kva Park
4 fest mytishchi drama and comedy theatre, 5 mytishchi arena.
Track your travel spending and split costs with friends
Plan your trip. Keep your budget organized. Split the cost between tripmates. Wanderlog does it all.
6 Mytishchi Park Of Culture And Leisure
7 monument to the hero of the soviet union raspopova nina maksimovna, 8 teatr kukol ognivo, 9 mytishchi history and art museum, 10 mytishchinskaya kartinnaya galereya, 11 perlovskiy park, 12 xl outlet, 13 interactive einstein museum, 14 zamaniya, family adventure park, what's the weather like in mytishchi.
It depends on when you visit! We've compiled data from NASA on what the weather is like in Mytishchi for each month of the year: see the links below for more information.
- Weather in Mytishchi in January
- Weather in Mytishchi in February
- Weather in Mytishchi in March
- Weather in Mytishchi in April
- Weather in Mytishchi in May
- Weather in Mytishchi in June
- Weather in Mytishchi in July
- Weather in Mytishchi in August
- Weather in Mytishchi in September
- Weather in Mytishchi in October
- Weather in Mytishchi in November
- Weather in Mytishchi in December
Explore nearby places
- Lesnyye Polyany
- Dolgoprudny
- Zagoryanskiy
- Ptitsefabriki
- Pekhra-Pokrovskoye
- Ivanovskoye
- Bratovshhina
- Likino-Dulevo
All related maps of Mytishchi
- Map of Mytishchi
- Map of Korolev
- Map of Zdravnitsa
- Map of Nagornoye
- Map of Yubileyny
- Map of Cherkizovo
- Map of Boltino
- Map of Pirogovo
- Map of Pogorelki
- Map of Tarasovka
- Map of Sorokino
- Map of Lesnyye Polyany
- Map of Povedniki
- Map of Ostashkovo
- Map of Oboldino
- Map of Zhostovo
- Map of Suponevo
- Map of Dolgoprudny
- Map of Zagoryanskiy
- Map of Izmaylovo
- Map of Moskovsky
- Map of Ptitsefabriki
- Map of Pekhra-Pokrovskoye
- Map of Ivanovskoye
- Map of Komyagino
- Map of Yuryevo
- Map of Bratovshhina
- Map of Fedoskino
- Map of Danki
- Map of Shatura
- Map of Likino-Dulevo
Mytishchi throughout the year
- Mytishchi in January
- Mytishchi in February
- Mytishchi in March
- Mytishchi in April
- Mytishchi in May
- Mytishchi in June
- Mytishchi in July
- Mytishchi in August
- Mytishchi in September
- Mytishchi in October
- Mytishchi in November
- Mytishchi in December
Looking for day-by-day itineraries in Mytishchi?
Get inspired for your trip to Mytishchi with our curated itineraries that are jam-packed with popular attractions everyday! Check them out here:
- 1-Day Mytishchi Itinerary
- 2-Day Mytishchi Itinerary
- 3-Day Mytishchi Itinerary
- Itinerary + map in one view
- Live collaboration
- Auto-import hotels and reservations
- Optimize your route
- Offline access on mobile
- See time and distance between all your places

IMAGES
VIDEO
COMMENTS
Palpation of the chest includes evaluation of thoracic expansion, percussion, and evaluation of diaphragmatic excursion. These techniques may be used to evaluate suspected abnormalities. Thoracic expansion: Is used to evaluate the symmetry and extent of thoracic movement during inspiration.
To test for symmetric chest expansion, place your thumbs at the level of the 10th ribs with your fingers loosely grasping and parallel to the lateral rib cage. Then slide them medially just enough to create a small skin fold between your thumbs, as shown. ... To measure diaphragmatic excursion, ask your patient to inhale and hold it. Percuss ...
The pulmonary examination consists of inspection, palpation, percussion, and auscultation. The inspection process initiates and continues throughout the patient encounter. Palpation, confirmed by percussion, assesses for tenderness and degree of chest expansion. Auscultation, a more sensitive process, confirms earlier findings and may help to ...
Diaphragmatic excursion. Diaphragmatic excursion is the movement of the thoracic diaphragm during breathing. Normal diaphragmatic excursion should be 3-5 cm, but can be increased in well-conditioned persons to 7-8 cm. This measures the contraction of the diaphragm. It is performed by asking the patient to exhale and hold it.
Comparison of post values of both techniques in Diaphragmatic Excursion and Chest Expansion is summarised in Table 5. In Diaphragmatic Excursion, difference in postintervention values at the Midclavicular line on the right side was found to be 0.07 ± 0.21 (p= 0.393) and on the left side was found to be -0.04 ± 0.23 (p= 1.00); Difference in ...
Concurrent chest resistance and expansion exercises may improve respiratory muscle strength, lung function, and thoracic excursion in children with post-operative CDH. The study findings suggest that concurrent chest and chest expansion exercises be part of an appropriate pulmonary rehabilitation program in children with a history of CDH.
16. This improvement in lung volume during thoracentesis may lead to better coupling of the lung and chest wall, reestablishing the physiological pleural pressure pattern in subjects with expandable lung. This improvement in diaphragm function may contribute to dyspnea relief in patients with expandable lung.
Stroke survivors have been reported to have reduced diaphragmatic excursion with a higher position of the affected diaphragm, ... Jung JH, and Kim NS, .Effects of inspiratory muscle training on diaphragm thickness, pulmonary function, and chest expansion in chronic stroke patients. J Korean Soc Phys Med2013; 8: 59-69. Crossref. Google Scholar ...
Background In patients with chronic obstructive pulmonary disease (COPD), the maximum level of diaphragm excursion (DEmax) is correlated with dynamic lung hyperinflation and exercise tolerance. This study aimed to elucidate the utility of DEmax to predict the improvement in exercise tolerance after pulmonary rehabilitation (PR) in patients with COPD. Methods This was a prospective cohort study ...
To evaluate diaphragmatic excursion as a quantitative metric for change in lung volume between inspiratory and expiratory chest computed tomography (CT) images. Methods A 12-month retrospective review identified 226 chest CT exams with inspiratory and expiratory phase imaging, 63 in individuals referred with diagnosis of asthma by ICD9/10 code.
Background Although the pathophysiological mechanisms involved in the development of dyspnoea and poor exercise tolerance in patients with COPD are complex, dynamic lung hyperinflation (DLH) plays a central role. Diaphragmatic excursions can be measured by ultrasonography (US) with high intra- and interobserver reliability. The objective of this study was to evaluate the effect of ...
Diaphragmatic function and BMI (body mass index) To evaluate the function of the diaphragm muscle [], the diaphragmatic excursion was measured at rest and during forced expiration (Supplement Table 1).In 60 patients, diaphragmatic excursion at rest in the supine position was 3.5 cm ± 1.2 on the right side and 3.5 cm ± 1.2 on the left side.
Background: Congenital diaphragmatic hernia (CDH) is a life-threatening condition with long-term complications including respiratory tract infections, respiratory muscle weakness, and abnormal lung functions. This study was designed to ascertain the effects of chest resistance and chest expansion exercises on respiratory muscle strength, lung function, and chest mobility in children with post ...
Diaphragmatic excursion for patients was measured on GE make, Voluson S8 series ultrasound machine. The assessment was done in supine position using M-mode and B-mode techniques in quiet and deep breathing scenarios. ... COPD can cause hyperkyphosis in later stage which reduces the expansion of the chest wall. A study proved that diaphragmatic ...
The mean percentage changes between A/C and SBT in diaphragm excursion, T i, and E-T index between the two patient groups are compared in Table 4. A decrease in diaphragmatic E-T index less than 3.8% during transition from A/C to SBT had a sensitivity of 79.2% and a specificity of 75% in predicting successful extubation (AUC, 0.77) ( Fig 2 C).
The measurement methods included diaphragm excursion (DE), where the subject was placed in a semi-recumbent position with the head of the bed elevated at 20 to 40° and a linear probe was placed at the intersection of the midline of the anterior chest wall and the costal arch to measure the right diaphragm through the liver as an acoustic ...
Scapulocostal syndrome (SCS) is a subset of myofascial pain syndrome affecting the posterior shoulder and upper back area. Some of the affected muscles are attached to the rib cage, which may affect diaphragmatic mobility and chest expansion. The purpose of this study was to investigate the characteristics of diaphragmatic mobility and chest expansion in patients with SCS. Twenty-nine patients ...
Dyspnea that is caused by pleural effusion and affects patients' quality of life may not be resolved after lung expansion following pleural tapping. This study aims to investigate the role that changes in the diaphragmatic shape and movement play in the development of dyspnea in those patients. Thirty patients with pleural effusions and dyspnea were evaluated before and at 24 h after ...
Furthermore, diaphragmatic excursion is an index for respiratory muscle fatigue during the SBT. Some authors had reported a lower accuracy for diaphragmatic excursion compared to most of the available data and suggested that this lower accuracy is due to the heterogeneity of the patients included in the meta-analyses , . Therefore, separate ...
Mytishchi is a city and the administrative center of Mytishchinsky District in Moscow Oblast, Russia, which lies 19 km northeast of Russia's capital Moscow on the Yauza River and the Moscow-Yaroslavl railway. The city was an important waypoint for traders on the Yauza River, the Yaroslavl Highway passes through the city. Mytishchi is famous for its aqueduct, built in 1804, the first water ...
There are 6 ways to get from Moscow to Mytishchi by train, subway, bus, rideshare, taxi, or car. Select an option below to see step-by-step directions and to compare ticket prices and travel times in Rome2rio's travel planner.
The ratio of right to left diaphragmatic excursion during quiet breathing was (1.009±0.19); maximum 181% and minimum 28%. Only 19 cases showed a right to left ratio of less than 50% (5 men and 14 women). The diaphragmatic excursion was higher in males than females. There was a significant difference in diaphragmatic excursion among age groups.
Nidhi Bisht — Google review. St. Basil's Cathedral is a landmark and iconic symbol of Moscow, Russia. Located on Red Square, it is one of the most recognizable and visited cathedrals in the world. The cathedral was built in the 16th century during the reign of Ivan the Terrible, and it is known for its colorful onion domes and unique ...