Accessibilité
Afin d'être accessible au plus grand nombre, nous vous informons que vous avez la possibilité de modifier la taille d’affichage du contenu de notre site. Pour cela, voici les commandes à reproduire à l'aide de votre clavier :

Numéros d'urgence

- Standard et urgences

Présentation de l’équipe de Neuro-Radiologie Interventionnelle
L'équipe médicale NRI

Unité de Neuroradiologie Interventionnelle

Dr Richard BIBI
Responsable d’unité

Pr Denis HERBRETEAU
Professeur des Universités Praticien Hospitalier

Dr Grégoire BOULOUIS
Praticien Hospitalier

Dr Héloïse IFERGAN
Praticien Hospitalier
Dr Kevin JANOT

Dr Fouzi BALA
Service de Radiologie, Neuroradiologie Diagnostique Interventionnelle
Docteur Baptiste MOREL
Chef de Service
Pr Laurent BRUNEREAU
Chef de Pôle Imagerie
L’équipe est composée par ailleurs de :
- 14 manipulateurs d’électroradiologie médicale,
- 5 secrétaires dédiées,
- 2 attachés de recherche clinique.
Contact et prise de rendez-vous
Kevin Janot
Areas of expertise.
Many experts have expertise treating multiple conditions. MediFind uses a variety of data sources to determine what conditions a expert treats and their level of experience.
- Thrombectomy
- Brain Aneurysm
- Stent Placement
- Carotid Artery Disease
- Chronic Subdural Hematoma
- Craniectomy
- Endovascular Embolization
- Ganglioglioma
- Mesenteric Venous Thrombosis
- Subarachnoid Hemorrhage
- Subdural Hematoma
- Thrombophlebitis
About Kevin Janot
Kevin Janot practices in Tours, France. Janot is highly rated in 4 conditions, according to our data. His top areas of expertise are Stroke, Brain Aneurysm, COVID-19, Thrombectomy, and Stent Placement.
His clinical research consists of co-authoring 66 peer reviewed articles in the past 15 years.
Background & Education
Clinical research.
Clinical research consists of overseeing clinical studies of patients undergoing new treatments and therapies, and publishing articles in peer reviewed medical journals. Experts who actively participate in clinical research are generally at the forefront of the fields and aware of the most up-to-date advances in treatments for their patients.
66 Total Publications
Aller au contenu | Navigation | Accès directs | Connexion
- Bibliothèques
- Orientation & Insertion
- Nos unités de recherche
- Nos marchés publics
- Faculté Arts & Sciences Humaines (ASH) Voir le site
- Faculté Centre d'Études Supérieures de la Renaissance Voir le site
- Faculté Droit Economie & Sciences Sociales Voir le site
- Faculté IAE Voir le site
- IUT IUT de Blois Voir le site
- IUT IUT de Tours Voir le site
- Faculté Lettres & Langues Voir le site
- Faculté Médecine Voir le site
- Faculté Odontologie Voir le site
- Faculté Pharmacie Voir le site
- Ecole Polytech Tours Voir le site
- Faculté Sciences & Techniques Voir le site
- GIS Collegium Santé Voir le site
Personnel hospitalier du CHU
M. Kevin Janot
Coordonnées.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.22(2); 2020 May
Perfusion Imaging to Select Patients with Large Ischemic Core for Mechanical Thrombectomy
Basile kerleroux.
a Diagnostic and Therapeutic Neuroradiology, CHRU de Tours, Tours, France
Kevin Janot
Cyril dargazanli.
b Department of Interventional Neuroradiology, University Hospital Center of Montpellier, Gui de Chauliac Hospital, Montpellier, France
Dimitri Daly-Eraya
Wagih ben-hassen.
c Centre Hospitalier Sainte Anne, Neuroradiology Department, Paris University, INSERM U1266, Psychiatry and Neurosciences Institute of Paris, Paris, France
François Zhu
d University Hospital of Nancy, Department of Diagnostic and Therapeutic Neuroradiology, INSERM U1254, Nancy, France
Benjamin Gory
Jean françois hak.
e Department of Diagnostic and Interventional Neuroradiology, Timone Hospital, Aix Marseille University, Marseille, France
Charline Perot
f Neurology Department, Timone Hospital, Aix Marseille University, Marseille, France
Lili Detraz
g Department of Diagnostic and Interventional Neuroradiology, Guillaume et René Laennec University Hospital, Nantes, France
Romain Bourcier
Aymeric rouchaud.
h Department of Interventional Neuroradiology, Dupuytren University Hospital, Limoges, France
Géraud Forestier
Joseph benzakoun, gaultier marnat.
i Department of Diagnostic and Interventional Neuroradiology, Pellegrin Hospital-University Hospital of Bordeaux, Bordeaux, France
Florent Gariel
Pasquale mordasini.
j Institute of Diagnostic, Interventional and Pediatric Radiology and Institute of Diagnostic and Interventional Neuroradiology, University Hospital Bern, Inselspital, University of Bern, Bern, Switzerland
Johannes Kaesmacher
Grégoire boulouis, associated data, background and purpose.
Patients with acute ischemic stroke, proximal vessel occlusion and a large ischemic core at presentation are commonly not considered for mechanical thrombectomy (MT). We tested the hypothesis that in patients with baseline large infarct cores, identification of remaining penumbral tissue using perfusion imaging would translate to better outcomes after MT.
This was a multicenter, retrospective, core lab adjudicated, cohort study of adult patients with proximal vessel occlusion, a large ischemic core volume (diffusion weighted imaging volume ≥70 mL), with pre-treatment magnetic resonance imaging perfusion, treated with MT (2015 to 2018) or medical care alone (controls; before 2015). Primary outcome measure was 3-month favorable outcome (defined as a modified Rankin Scale of 0–3). Core perfusion mismatch ratio (CPMR) was defined as the volume of critically hypo-perfused tissue (Tmax >6 seconds) divided by the core volume. Multivariable logistic regression models were used to determine factors that were independently associated with clinical outcomes. Outputs are displayed as adjusted odds ratio (aOR) and 95% confidence interval (CI).
A total of 172 patients were included (MT n=130; Control n=42; mean age 69.0±15.4 years; 36% females). Mean core-volume and CPMR were 102.3±36.7 and 1.8±0.7 mL, respectively. As hypothesized, receiving MT was associated with increased probability of favorable outcome and functional independence, as CPMR increased, a difference becoming statistically significant above a mismatch-ratio of 1.72. Similarly, receiving MT was also associated with favorable outcome in the subgroup of 74 patients with CPMR >1.7 (aOR, 8.12; 95% CI, 1.24 to 53.11; P =0.028). Overall (prior to stratification by CPMR) 73 (42.4%) patients had a favorable outcome at 3 months, with no difference amongst groups.
Conclusions
In patients currently deemed ineligible for MT due to large infarct ischemic cores at baseline, CPMR identifies a subgroup strongly benefiting from MT. Prospective studies are warranted.
Introduction
In recent years, mechanical thrombectomy (MT) has demonstrated its compelling efficacy in reducing mortality and functional dependence for patients with acute ischemic stroke (AIS) due to anterior proximal vessel occlusion (PVO) [ 1 , 2 ]. Patients with an unfavorable imaging profile at baseline, assessed using magnetic resonance imaging (MRI) diffusion weighted imaging (DWI) volume core (≥70 mL) [ 1 ], or the computed tomography (CT)-based-Alberta Stroke Program Early CT score (ASPECTS) <6, were excluded in four of the seven randomized clinical trials that validated MT in AIS-PVO [ 3 ], precluding to draw strong conclusions in this subgroup. Hence they are typically not offered MT in clinical practice [ 1 ], despite converging evidence suggesting a benefit of MT despite large ischemic core (LIC), with almost 25% of patients experiencing favorable functional outcome after MT [ 3 - 9 ].
Perfusion imaging is used in the diagnostic work up of AIS to identify hypo-perfused yet not infarcted (e.g., ‘at-risk’ or ‘salvageable’) brain tissue [ 10 ], and to estimate the core perfusion mismatch ratio (CPMR) [ 2 ]. Nonetheless, perfusion data remain very scarce in patients with LIC before MT, while they are critically needed to pragmatically design future randomized trials, and better select patients for MT until then.
We hypothesized that perfusion imaging may enhance the effective selection of AIS-PVO patients with LIC by determining those likeliest to benefit from revascularization and tested this hypothesis in a cohort study using data from a multicenter cohort, by comparing the rates of favorable functional outcome, symptomatic intracerebral hemorrhage (sICH), and case-fatality in patients with DWI assessed baseline LIC (>70 mL) and perfusion who received MT versus patients who were treated with intravenous thrombolysis only. The hypothesis driving this analysis was that in patients with baseline large infarct cores, identification of significant remaining penumbral tissue, as assessed using CPMR, would translate to better outcomes after MT.
Study design
The study was a multicenter, core-lab adjudicated, observational retrospective cohort study. The “Jeunes en Neuroradiologie Interventionnelle Research Collaborative” (JENI-RC), is a recently launched trainee-led research network [ 11 ]. Local JENI-RC members were asked to provide de-identified data for patients with DWI ASPECTs 0–6 otherwise meeting study inclusion criteria (see below). Case report form items included demographics, relevant past medical history, sICH, and 3-month functional outcome. Imaging data were centralized by the internal core lab, for central assessment. Nine academic centers contributed data (eight in France, and one in Switzerland). This report was prepared according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement [ 12 ].
As for all non-interventional retrospective studies of de-identified data in France, written informed consent was waived and a commitment to compliance (reference methodology CPMR-3) was filed to the French National Information Science and Liberties Commission prior to data centralization, in respect to the General Data Protection Regulation.
Inclusion criteria
In the MT group, we included consecutive adult patients with AIS after 2015 if they had an occlusion of the intracranial internal carotid artery or of the M1 segment of the middle cerebral artery; had a large pretreatment ischemic core volume defined as 70 mL or more on magnetic resonance-DWI as assessed centrally; had no preexisting handicap as defined by a modified Rankin Scale (mRS) of 2 or higher; underwent MT; and if pre-treatment MR-T2* perfusion sequence had been performed. The control group was constituted by retrospectively querying the prospective intravenous tissue plasminogen activator (tPA) stroke data base at a single university hospital, to identify patients treated before MT related guidelines in 2015 who met the same criteria but did not receive MT due to guidelines compliance.
Imaging analysis and mismatch definition
The post-processing and images interpretation were performed centrally after complete de-identification, by an internal corelab (B.K. and G.B.), blinded to clinical data.
Ischemic core volumes (DWI volume) were calculated using Olea-Sphere version 3.0 software (Olea Medical, La Ciotat, France), by the semi-automated segmentation of brain tissue ipsilateral to the occlusion with apparent diffusion coefficient of 0.6×10 -3 mm 2 /sec or less. Perfusion maps were generated using the Olea-Sphere version 3.0 software then used to calculate critically hypo-perfused brain tissue, with an inferior threshold set, according to recent literature [ 13 ], at T max >6 seconds. As in previous large studies investigating core penumbral mismatch [ 14 , 15 ], we defined penumbral tissue as the volume of critically hypo-perfused tissue minus the DWI volume. Similarly, we defined the CPMR, as the volume of critically hypo-perfused tissue divided by the DWI volume, and defined a target mismatch as patients with a CPMR of 1.8 or above.
Assessment criteria
The primary endpoint was functional outcome assessed at 3 months, using the mRS, with a favorable outcome defined by a score of 3 or less, taking into account the inherent severity of AIS with baseline LIC, and in line with recent literature. Secondary end points included functional independence defined as mRS of 0–2. Ninety days mortality, and the rate of symptomatic intracerebral hemorrhage within 7 days (according to European Cooperative Acute Stroke Study [ECASS] II criteria) [ 16 ]. Substantial reperfusion was defined as a modified Thrombolysis in Cerebral Infarction score of 2B, 2C, or 3 [ 17 ].
Statistical analysis
Baseline characteristics of patients has been compared between MT group and control group. Continuous variables were summarized using mean±standard deviation or median (interquartile range) where appropriate, and discrete variables were summarized using counts (percentages). Chi-square test, Fisher-exact test, t-test, Mann-Whitney test were used as appropriate for the univariate analysis, with a P <0.05 as the threshold for statistical significance.
Clinical outcomes were compared between MT group and control group. First, multivariable logistic regression models were used to determine factors that were independently associated with clinical outcomes. Variables associated with the outcome in univariate analysis ( P ≤0.1) were entered into nominal logistic models, with a prespecified adjustment for age, infarct core, and CPMR. Backward elimination was then used to remove non-significant variables ( P >0.05). The adjusted odds ratios (aOR) and 95% confidence interval (CI) of having favorable outcome (model 1) and functional independence (model 2) were reported. Then, a sensitivity analysis was performed to assess for changes in the results in patients with a predefined CPMR cutoff of 1.8, as was reported in previous cornerstone studies analyzing the pertinence of CMPR in AIS-PVO patients [ 13 , 18 ]. Finally, a shift analysis of mRS score (of 0–6 points) based on the proportional odds model has been performed. All analyses were done using JMP Pro 14 (Institute Inc., Cary, NC, USA) software. Where needed, we derived 95% CI by bootstrapping (5,000 occurrences) statistical results [ 18 ].
Study population
Between January 2015 and July 2018, in the MT group a total of 971 patients with AIS-PVO and ASPECTs 0–6 were screened for inclusion. After applying inclusion criteria, 168 patients were evaluated by the core lab, of which 130 were finally included and analyzed in the MT group. Before 2015, a total of 154 patients with DWI-ASPECTs 0–6 were screened for inclusion in the control group, and 42 met study criteria ( Figure 1 ). A total of 172 were finally included in the present analysis (36% females, mean age 69.0±15.4 years) ( Table 1 for baseline clinical-imaging characteristics). Patients in the MT group were more frequently females (41% vs. 21%, P =0.03), less frequently received intravenous tPA (48.5% vs. 100%, P <0.01), were more frequently referred from an outside primary stroke center hospital (25.4% vs. 0%, P <0.01), were younger (66.2±14.9 years-old vs. 77.7±13.5, P <0.01). They did not differ otherwise in terms of baseline clinical parameters, notably for delay between onset and qualifying imaging ( P =0.58) and occlusion site ( P =0.82). Substantial recanalization was achieved in 111/140 patients in the MT group (79.3%).

Flow chart. DWI, diffusion weighted imaging; ASPECTS, Alberta Stroke Program Early Computed Tomography Score; PWI, perfusion weighted imaging; MT, mechanical thrombectomy.
Baseline characteristics of included patients
Values are presented as mean±standard deviation or number (%).
MT, mechanical thrombectomy; NIHSS, National Institute of Health Stroke Scale; iv tPA, intravenous tissue plasminogen activator; ICA, internal carotid artery.
Core and penumbra
Mean core DWI volume was 102.3±36.7 mL and did not differ between groups. The volume of critically hypo-perfused tissue was larger in the MT group (mean 180.8±72.4 mL vs. 145.5±52.5 mL, P <0.01), which consequently demonstrated larger penumbral volumes (mean 76.8±63.7 mL vs. 48.8ml±40.9 mL, P <0.01) as well as higher CPMRS (mean 1.8±0.7 vs. 1.5±0.5, P <0.01). A total of 90 (52%), 65 (38%), and 53 (31%) patients had CPMRS above 1.6, 1.8, and 2.0 respectively ( Supplementary Figure 1 , in the supplemental material for detailed CPMR distribution in the cohort).
Functional outcomes
At 3 months, 73 (42.4%) patients had a favorable functional outcome (mRS 0–3), with no difference amongst groups prior to stratification by CPMR (43.1% in the MT vs. 40.5, P =0.86). Forty-one patients (23.8%) were functionally independent and 54 (31.4%) were deceased ( P =1.000) ( Table 2 ). Unfavorable outcome was associated with higher age, higher baseline NIHSS, history of hypertension, and diabetes mellitus ( Supplementary Table 1 ).
Outcome of included patients
Values are presented as number (%).
MT, mechanical thrombectomy; mRS, modified Rankin Scale; sICH, symptomatic intra-cranial hemorrhage.
Independent of, as well as within, treatment groups both larger core and larger penumbral volumes were associated with poor functional outcome in univariable analysis (185±67.9 mL in patients with mRS 4–6 vs. 154±68.4 mL in those with mRS 0–3, P <0.01; and 76±59 vs. 67±60, P =0.04) ( Figure 2 ).

Modified Rankin Scale at 3 months and initial diffusion weighted imaging (DWI) core volume and mismatch ratio per group.
In the entire population, there was no difference in favorable outcome between treatment groups ( P =0.68) ( Table 1 ). After adjusting for age, hypertension, diabetes, core volume, CPMR, delay to imaging, intravenous tPA before MT, and occlusion site, there was a significant interaction between MT effect and CPMR in both models (Model 1: aOR, 0.29; P =0.008; and Model 2: aOR, 0.4; P =0.047), indicating an increasing benefit of MT as CPMR increases ( Table 3 ). In the same model, with mismatch ratio dichotomized as a nominal variable (below or above 1.8) the odds ratio of the interaction term between treatment arm and mismatch ratio (>1.8), was 0.42 (95% CI, 0 to 0,82; P =0.02).
Multivariable models for outcome
aOR, adjusted odds ratio; CI, confidence interval; iv tPA, intravenous tissue plasminogen activator; ICA, internal carotid artery; MT, mechanical thrombectomy.
Analyzing the probability for favorable outcome in the fully adjusted model plotted against CPMR, we showed that receiving MT (vs. not receiving MT) was associated with increased probability of favorable outcome and functional independence, as CPMR increased, a difference becoming statistically significant above a CPMR of 1.72 for favorable outcome, and above 1.93 for functional independence ( Figure 3 ).

Probability of favourable functional outcome (A) or functional independence (B) by mismatch ratio, in patient receiving mechanical thrombectomy (yellow), and in the control group (blue).
As a sensitivity analysis, when stratifying by CPMR; in the sample of 65 patients with a CPMR of 1.8 or above, after adjusting for group specific outcome predictors (age, core volume, intravenous tPA, and CPMR), receiving MT was associated with a significant increase in the rate of favorable outcome (aOR, 999; 95% CI, 999 to infinite). Similarly, in the subgroup of 74 patients for which CPMR exceeded 1.7 (42% of favorable outcome in the MT group vs. 20% in the control group, P =0.031; receiving MT was associated with a significantly increased rate of favorable outcome) (aOR, 8.12; 95% CI, 1.24 to 53.11, P =0.028). Using ordinal regression, receiving MT was associated with overall favorable shift in mRS distribution (common risk ratio, 1.83; 95% CI, 1.01 to 3.44; P =0.049) ( Figure 4 ).

Modified Rankin Scale (mRS) distribution in patients receiving mechanical thrombectomy (MT) and those not receiving MT, stratified by core perfusion mismatch ratio (CPMR). IV, intravenous.
Finally, when restricting the sample to patients in the MT group, we found substantial recanalization to be associated with significantly higher odds of favorable outcome and of 3 months functional independence, in fully adjusted models (aOR, 53.7; 95% CI, 5.0 to 573; P <0.001; and aOR infinite, P <0.001, respectively). Lower age ( P <0.001), lower mismatch ratio ( P =0.03), and lower core volume ( P <0.001) were also associated with higher odds of favorable outcome, but the interaction between CPMR and substantial recanalization only tended towards significance ( P =0.058).
Secondary outcomes
At 3 months, 54 patients were deceased (31.5% in the MT vs. 30.9% in the control group, P =1). Fully adjusted model identified older age, larger core volume, higher CPMR, and diabetes mellitus as being associated with significantly higher mortality (all P <0.01) ( Table 2 ). Treatment group did not influence 3 months mortality rate ( Supplementary Tables 2 and 3 ).
A total of 31 of 161 patients with available data suffered from a sICH (20.6% in the MT group vs. 14.3%, P =0.48) ( Table 2 ). In our sample, receiving MT was not associated with higher odds of sICH (aOR, 1.94; 95% CI, 0.6 to 6.26; P =0.26). While larger infarct core was associated with more frequent sICH (aOR, 1.01 for each mL increase in core volume; 95% CI, 1 to 1.03; P =0.02), higher CPMR was not ( Supplementary Tables 4 and 5 ). In the MT group, substantial recanalization was not associated with decreased odds of sICH ( P =0.49).
In this multicenter collaborative study we showed that (1) MT is strongly beneficial on clinical outcome of patients with large infarct core at baseline, and persisting core/penumbral mismatch (CPMR >1.72 in our sample and by extension >1.8), with no heterogeneity in treatment effect across strata of CPMR and (2) that MT does not increase the odds of sICH and mortality.
The question of the best treatment approach for AIS-PVO patients with large infarct at baseline remains unanswered, despite being amongst the most timely and relevant in acute stroke care. There is indeed a critical need to assess treatment opportunities expansion to those patients that were excluded from princeps MT trials (especially patients with LIC, that are at critical risk of poor functional outcomes and for which guidelines remain ambiguous), and may in turn not be offered MT, despite a potential benefit. Until the results of dedicated trials such as Exploration of the limits of mechanical thrombectomy indications in a single action–Large Stroke Therapy Evaluation (IN EXTREMIS–LASTE) or Efficacy and Safety of Thrombectomy in Stroke With Extended Lesion and Extended Time Window (TENSION) become available, the community faces a challenge in the treatment strategy for this subgroup.
Expectedly, our results are in line with previous studies [ 3 , 4 , 7 , 19 - 21 ] demonstrating the direct correlation between larger infarct core sizes decreased odds of favorable functional outcome. In our sample as a whole, for every 10 mL increase in core volume, there was a 22% increase in the risk of unfavorable outcome, and a 26% increase in the risk of 90 days functional dependence. Our results, in that sense, confirm that presenting with a large infarct at baseline is of poorer prognosis and do support careful expectations’ management with families and caregivers.
Less intuitively, but substantiating our working hypothesis, increasing CPMR was also associated with lower chance of favorable outcome, with an odd decrease of 81% for every mismatch unit increase. This finding was not unexpected, since patients with higher CPMRS are at inherent higher risk for infarct progression within the hypo-perfused area, until recanalization or if recanalization doesn’t occur, or not fast enough. In our sample, the benefit of MT over the control group became significant above a CPMR of 1.72 corresponding to a minimal penumbral volume of 50.4 mL (e.g., if the patient has a core volume of exactly 70 mL) and was stable in the stratified subgroup of patients with CPMRS above 1.7. Although the conceptual framework supporting the benefit of MT in patients with PVO and target mismatch has been substantiated by a large number of publications, including the cornerstone studies from the diffusion and perfusion imaging evaluation for understanding stroke evolution (DEFUSE) group [ 13 , 22 ], there is still limited dedicated studies in the specific subgroup of patients with larger infarcts at baseline. Rebello et al. [ 5 ] demonstrated in a sample of 24 patients with large infarct cores assessed using CT perfusion (cerebral blood flow <30%; 70 mL) and an penumbra volumes (Tmax >6 seconds) above 40 to 50 mL that MT was associated with significant reduction in final infarct volumes (110±65 mL vs. 319±147 mL, P <0.001) but only a nonsignificant improvement in the overall distribution of mRS scores favoring the treatment group ( P =0.18). These neutral results with regards to clinical outcome, are likely due to insufficient power, in this subgroup limited by a binary design that excluded patients with limited mismatch, precluding to further test interaction between MT effects and CPMR. More recently, Campbell et al. [ 15 ] showed in post hoc analyses of individual patient level data from The Highly Effective Reperfusion evaluated in Multiple Endovascular Stroke Trials (HERMES) collaboration, that amongst the 583 patients with computed tomography perfusion (CTP), the interaction between CPMR and endovascular treatment effect was not significant ( P =0.15), but statistical power was strongly limited by the small number of patients not meeting criteria (less than 5% with a CPMR <1.8 amongst the 583 patients with CTP). In this study, CTP mismatch volume was negatively associated, in univariate analysis, with functional improvement (common odds ratio per 10 mL 0.96; 95% CI, 0.93 to 0.99; P =0.009) reinforcing the conceptual balance paradox by which larger mismatch volumes are associated with decreased favorable outcomes due to increased possibilities of infarct progression, and in turn explaining the increasing benefit of MT as CPMR increases, a notion that had not been confirmed before our study in patients with larger infarct cores.
In secondary analyses, we did not show a significant association between MT and the risk of sICH, and there was conversely a positive interaction between infarct core volume and treatment group, in favor of MT. There’s been several reports on the risk of sICH after MT in LIC, none of which showed an increase in the risk of sICH after MT except in the HERMES collaboration [ 3 ] where, for patients with ASPECTS 0–4, sICH was more frequent in the MT group, although not significantly (adjusted cOR, 3.94; 95% CI, 0.94 to 16.49; P interaction=0.025), and not reproduced when restricting the sample to patients with DWI volume ≥70 mL were no significant difference of sICH between EVT (1/23, 4.3%) and best medical treatment (2/37, 5.4%) was found [ 3 , 15 ]. Of critical note, the most important predictor of sICH and parenchymal hemorrhage is core volume, independent of treatment modality [ 3 , 7 , 19 , 20 , 23 ], likely explaining that successful reperfusion was associated with lower sICH in many “real life” recent studies [ 7 , 19 , 20 ]. Whether the benefits of not revascularizing a patient to prevent sICH, outweigh those of revascularization to prevent infarction extension is unknown, but very unlikely, especially in patients with important mismatch, at highest risk for infarct progression and progression to malignant infarction. Our study was neither powered nor designed to answer this question.
There’s a long ongoing debate on optimal imaging modality (CT or MRI) for AIS-PVO patients’ selection for revascularization strategies [ 24 - 26 ]. The main risk of patients’ selection in the context of AIS is over-selection, that is, to decline a patient a treatment that may have been beneficial. For patients with LIC, the question of over-selection is amongst the timeliest in modern stroke care. The first level of over-selection may happen at the core assessment level (e.g., dismissing a patient because of large infarct). Interestingly, in the HERMES collaboration [ 3 ], the treatment benefit in patients with ASPECTs 0–4 derived from the aggregation of CT and MRI ASPECTs data, and was likely contingent on the disproportionately larger effect size seen in the MRI subgroup (aOR, 3.57; 95% CI, 1.22 to 10.39 vs. aOR, 1.68; 95% CI, 0.58 to 4.87 in the CT group). Similarly, Campbell et al. [ 15 ] demonstrated that CTP was associated with significantly halved proportion of patients functional independence (OR, 0.47; 95% CI, 0.30 to 0.72; P =0.0007), and also with less functional improvement (cOR, 0.51; 95% CI, 0.36 to 0.72; P =0.0001) when compared to MRI, both studies reinforcing the notion that MRI may better select patients for MT, but at the inherent risk of overselecting. In that sense, our study provides critical answers with regards to outcome in patients with LIC by the use of MRI with known higher conspicuity and reproducibility to detect and measure infarct core when compared to CT (especially when ASPECTs is used) [ 27 ]. The second level of over-selection, accounting that patients are considered for MT even with a LIC, is perfusion imaging. Our study showed, using strict post processing method, that patients with a CPMR above 1.72 (and by extension, over 1.8) demonstrated more favorable outcomes when treated with MT but the benefit increase was expectedly linear and not sudden at a discrete threshold of 1.72. While this finding suggests that patients with lower CPMR are likely to also benefit from MT, more subjects would be needed to demonstrate it, the benefit would likely be lesser, and this would need to be confirmed in a larger scale study. Importantly, we did not demonstrate any harm derived from MT in patients with lower CPMR.
Altogether, by comforting patho-physiologically plausible and statistically stable answers the question of the benefit of MT in patients with LIC at baseline and persisting salvageable tissue, our study raises ethical and philosophical considerations. There is growing evidence that by withholding MT by fear of potential harm for some patients, we may actually dismiss a much larger of patients that may have benefited from revascularization. In that sense, by demonstrating the continuum of unfavorable outcome paralleling the increases in core as well as mismatch volumes, and by showing the increasing benefit of MT with increasing CPMR, we actually fuel the argument that perfusion imaging is not needed as it may delay revascularization in eligible patients (and be used to decline MT to patients with CPMRS in the lower ranges, despite potential benefit). With no evidence of harm from MT in any of the explored configurations in our sample and the above-mentioned continuums in treatment benefit increases, it may be reasonable not to withhold treatment based on strict-cut offs (e.g., the study specific 1.72, applicable only to our sample, or the more common 1.8), but to adjust treatment decisions to both outcome and patients/families’ centered expectations. Results from future trials may yield more definite answers to these questions, although the authors are not aware of any ongoing large randomized study using perfusion imaging as a selection criterion in patients with LIC.
Our study has limitations, most inherent to its design. It was a retrospective analysis, with a high risk of selection bias in included cases and important number of excluded cases due to the limited penetration of perfusion imaging for AIS amongst French centers and to the yet unusual use of MT in patients with LIC. For similar reasons, our sample size did not allow for a split into a derivation and a validation cohort, but we aimed at substantiating our estimates by various sensitivity analyses, which proved to be stable. We acknowledge that our control group was biased, by the fact that it included only patients who received intravenous tPA, and that this bias may have yielded underestimated estimates of the benefit of MT over best medical management. Lastly, using CPMR instead of CT allowed for more precise estimates of ischemic infarct cores, but make our results less generalizable beyond the pathophysiological rationale it provides.
In patients currently deemed ineligible for MT due to large infarct ischemic cores at baseline, CPMR identifies patients strongly benefiting from MT. These finding provide a data-driven framework supporting both the relevance of CPMR perfusion assessment at the acute phase of AIS due to PVO in patients with LIC, and the notion that there is no strict plausible cutoff in core or penumbral volumes above or below which MT may become harmful by comparison to best medical treatment alone. Our results may help at informing the design of future randomized trials and may, further, help inform clinical practice for more individualized decision making in this subgroup until higher level evidence becomes available.
The authors have no financial conflicts of interest.
Supplementary materials
Supplementary materials related to this article can be found online at https://doi.org/10.5853/jos.2019.02908 .
Supplementary Table 1.
Univariate analysis of outcome predictors (mRS 0–3)
Supplementary Table 2.
Univariable analysis of 90-day mortality
Supplementary Table 3.
Multivariable model of 90-day mortality predictors (pre specified adjustment for core volume, mismatch ratio, and treatment group)
Supplementary Table 4.
Univariable analysis of sICH (ECASS II) predictors
Supplementary Table 5.
Multivariable model of symptomatic intra-cranial hemorrhage predictors (pre specified adjustment for core volume, mismatch ratio and treatment group)
Supplementary Figure 1.
Distribution of core perfusion mismatch ratios (CPMRs) in the entire sample (A) and proportion of patients with CPMRs above 1.6, 1.8, and 2 (B).
Advertisement
Acute hydrocephalus and delayed cerebral infarction after aneurysmal subarachnoid hemorrhage
- Original Article - Vascular Neurosurgery - Aneurysm
- Published: 02 August 2022
- Volume 164 , pages 2401–2408, ( 2022 )
Cite this article
- Axel Masson ORCID: orcid.org/0000-0002-2650-5045 1 ,
- Grégoire Boulouis 1 ,
- Kevin Janot 1 ,
- Denis Herbreteau 1 ,
- Jean-Phlippe Cottier 1 ,
- Richard Bibi 1 ,
- Clara Cohen 2 ,
- Sandra Obry 1 ,
- Stéphane Velut 3 ,
- Aymeric Amelot 3 &
- Héloïse Ifergan 1
455 Accesses
5 Citations
1 Altmetric
Explore all metrics
Delayed cerebral infarction (DCIn) following aneurysmal subarachnoid hemorrhage (aSAH) is a major cause of morbi-mortality; yet, the causes for DCIn remain incompletely understood.
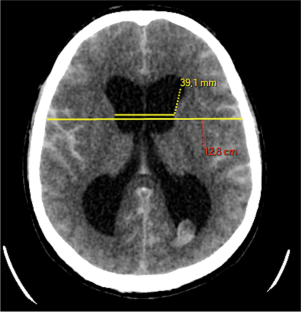
We tested the hypothesis that acute hydrocephalus could be related to the occurrence of DCIn, independently of the occurrence and severity of vasospasm.
Radiological and clinical data of patients treated at a single large volume academic center for aSAH between 2017 and 2019 were retrospectively analyzed. DCIn was defined as imaging stigma of cerebral infarction visible on 6-week imaging follow-up after aSAH. Hydrocephalus was defined on baseline imaging as a relative bicaudate index above 1. Cerebral vasospasm was defined by reduction of artery diameter in comparison with initial diameter. We used uni- and multivariable models to test the associations between these variables, hydrocephalus and DCIn.
Of 164 included patients, vasospasm occurred in 58 patients (35.4%), and DCIn in 47 (28.7%). Acute hydrocephalus was present in 85 patients (51.8%) on baseline CT. No relation was found between acute hydrocephalus and delayed cerebral infarction in our multivariate analysis (adjusted OR: 1.20 95% CI [0.43–3.37]; p = 0.732). Only vasospasm occurrence was independently associated with DCIn (adjusted OR: 10.97 95% CI [4.60–26.01]).
Our study did not show an association between acute hydrocephalus and DCIn after aSAH, after adjustment for the presence and severity of cerebral vasospasm.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Guidelines for the Neurocritical Care Management of Aneurysmal Subarachnoid Hemorrhage
Miriam M. Treggiari, Alejandro A. Rabinstein, … Stavropoula Tjoumakaris

Aneurysmal Subarachnoid Hemorrhage: the Last Decade
Sean N. Neifert, Emily K. Chapman, … R. Loch Macdonald

Aneurysmal Subarachnoid Hemorrhage: Review of the Pathophysiology and Management Strategies
Marcey L. Osgood
Abbreviations
Subarachnoid hemorrhage
- Aneurysmal subarachnoid hemorrhage
Delayed cerebral ischemia
- Delayed cerebral infarction
Computed tomography
Magnetic resonance imaging
World federation of neurosurgical surgery
Bicaudate index
Relative bicaudate index
External ventricular drainage
Bakker AM, Dorhout SM, Algra A, Rinkel GJ (2007) Extent of acute hydrocephalus after aneurysmal subarachnoid hemorrhage as a risk factor for delayed cerebral infarction. Stroke 38:2496–2499. https://doi.org/10.1161/STROKEAHA.107.484220
Article PubMed Google Scholar
Balbi M, Koide M, Schwarzmaier SM, Wellman GC, Plesnila N (2017) Acute changes in neurovascular reactivity after subarachnoid hemorrhage in vivo. J Cereb Blood Flow Metab 37(1):178–187. https://doi.org/10.1177/0271678X15621253
Article CAS PubMed Google Scholar
Black PM (1986) Hydrocephalus and vasospasm after subarachnoid hemorrhage from ruptured intra-cranial aneurysms. Neurosurgery 18:12–16. https://doi.org/10.1227/00006123-198601000-00003
Bosche B, Graf R, Ernestus R-I, Dohmen C, Reithmeier T, Brinker G, Strong AJ, Dreier JP, Woitzik J (2010) Recurrent spreading depolarizations after subarachnoid hemorrhage decreases oxygen availability in human cerebral cortex. Ann Neurol 67(5):607–617. https://doi.org/10.1002/ana.21943
Article PubMed PubMed Central Google Scholar
Bosche B, Mergenthaler P, Doeppner TR, Hescheler J, Molcanyi M (2019) Complex clearance mechanisms after intraventricular hemorrhage and rt-PA treatment – a review on clinical trials. Transl Stroke Res. https://doi.org/10.1007/s12975-019-00735-6
Boulouis G, Labeyrie MA, Raymond J, Rodriguez-Régent C, Lukaszewicz AC, Bresson D, Ben Hassen W, Tristram D, Meder JF, Oppenheim C, Naggara O (2017) Treatment of cerebral vasospasm following aneurysmal subarachnoid haemorrhage: a systematic review and meta-analysis. Eur Radiol 27(8):3333–3342. https://doi.org/10.1007/s00330-016-4702-y
Brami J, Chousterman B, Boulouis G, Le Dorze M, Majlath M, Saint-Maurice JP, Civelli V, Froelich S, Houdart E, Labeyrie MA (2020) Delayed cerebral infarction is systematically associated with a cerebral vasospasm of large intracranial arteries. Neurosurgery 86(2):E175–E183. https://doi.org/10.1093/neuros/nyz340
Bretz JS, Von Dincklage F, Woitzik J, Winkler MK, Major S, Dreier JP, Bohner G, School M (2017) The Hijdra scale has significant prognostic value for the functional outcome of Fisher grade 3 patients with subarachnoid hemorrhage. Clin Neuroradiol 27(3):361–369. https://doi.org/10.1007/s00062-016-0509-0
Brouwers PJ, Dippel DW, Vermeulen M, Lindsay KW, Hasan D, van Gijn J (1993) Amount of blood on computed tomography as an independent predictor after aneurysm rupture. Stroke 24:809–814. https://doi.org/10.1161/01.str.24.6.809
Budohoski KP, Guilfoyle M, Helmy A, Huuskonen T, Czosnyka M, Kirollos R, Menon DK, Pickard JD, Kirkpatrick P (2014) The pathophysiology and treatment of delayed cerebral ischaemia following subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry 85(12):1343–1353. https://doi.org/10.1136/jnnp-2014-307711
Chen S, Lou J, Reis C, Manaenko A, Zhang J (2017) Hydrocephalus after subarachnoid hemorrhage: pathophysiology, diagnosis, and treatment. Biomed Rest Int 2017:8584753. https://doi.org/10.1155/2017/8584753
Article CAS Google Scholar
Dakson A, Kameda-Smith M, Staudt MD, Lavergne P, Makarenko S,Eagles ME, Ghayur H, Guo RC, Althagafi A, Chainey J, Touchette CJ, Elliott C, Iorio-Morin C, Tso MK, Green R Bargone L, Christie SD (2021) A nationwide prospective multicenter study of external ventricular drainage: accuracy, safety, and related complications. J Neurosurg: 1–9. https://doi.org/10.3171/2021.7.JNS21421 .
Ditz C, Leppert J, Neumann A, Krajewski KL, Gliemroth J, Tronnier VM, Küchler J (2020) Cerebral vasospasm following spontaneous subarachnoid hemorrhage: angiographic pattern and its impact on the clinical course. World Neurosurg 138:e913–e921. https://doi.org/10.1016/j.wneu.2020.03.146
Dong L, Zhou Y, Wang M, Yang C, Yuan Q, Fang X (2019) Whole-brain CT perfusion on admission predicts delayed cerebral ischemia following aneurysmal subarachnoid hemorrhage. Eur J Radiol 116:165–173. https://doi.org/10.1016/j.ejrad.2019.05.008
Dorsch NW, King MT (1994) A review of cerebral vasospasm in aneurysmal subarachnoid haemorrhage part I: incidence and effects. J Clin Neurosci 1(1):19–26. https://doi.org/10.1016/0967-5868(94)90005-1
Dupont SA, Wijdicks FM, Manno EM, Lanzino G, Rabinstein A (2009) Prediction of angiographic vasospasm after aneurysmal subarachnoid hemorrhage: value of the Hijdra sum scoring system. Neurocrit Care 11(2):172–176. https://doi.org/10.1007/s12028-009-9247-3
Etminan N, Beseoglu K, Heiroth HJ, Turowski B, Steiger HJ, Hanggi D (2013) Early perfusion computerized tomography imaging as a radiographic surrogate for delayed cerebral ischemia and functional outcome after subarachnoid hemorrhage. Stroke 44:1260–1266. https://doi.org/10.1161/STROKEAHA.111.675975
Fugate JE, Rabinstein AA, Wijdicks EF, Lanzoni G (2012) Aggressive CSF diversion reverses delayed cerebral ischemia in aneurysmal subarachnoid hemorrhage: a case report. Neurocrit Care 17:112–116. https://doi.org/10.1007/s12028-012-9723-z
Hammer A, Erbguth F, Hohenhaus M, Hammer CM, Lücking H, Gesslein M, Killer-Oberpfalzer M, Steiner HH, Janssen H (2021) Neurocritical care complications and interventions influence the outcome in aneurysmal subarachnoid hemorrhage. BMC Neurol 21(1):27. https://doi.org/10.1186/s12883-021-02054-6
Hammer A, Erbguth F, Hohenhaus M, Hammer CM, Lücking H, Gesslein M, Killer-Oberpfalzer M, Steiner HH, Janssen H (2021) Neurocritical care complications and interventions influence the outcome in aneurysmal subarachnoid hemorrhage. BMC Neurol 21:27. https://doi.org/10.1186/s12883-021-02054-6
Hasan D, Tanghe HL (1992) Distribution of cisternal blood in patients with acute hydrocephalus after subarachnoid hemorrhage. 31(4):374-8. https://doi.org/10.1002/ana.410310405
Hijdra A, van Gijn J, Nagelkerke NJ, Vermeulen M, van Crevel H (1988) Prediction of delayed cerebral ischemia, rebleeding, and outcome after aneurysmal subarachnoid hemorrhage. Stroke 19:1250–1256. https://doi.org/10.1161/01.str.19.10.1250
Hirashima Y, Hamada Y, Hamada H, Hayashi N, Kuwayama N, Origasa H, Endo S (2003) Independent predictors of late hydrocephalus in patients with aneurysmal subarachnoid hemorrhage – analysis by multivariate logistic regression model. Crebrovasc Dis 16(3):205–210. https://doi.org/10.1186/s13037-018-0160-6
Article Google Scholar
Hop JW, Rinkel GJ, Algra A, van Gijn J (1999) Initial loss of consciousness and risk of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Stroke 30:2268–2271. https://doi.org/10.1161/01.str.30.11.2268
Jingjing L, Nan J, Zhonghua Y, Xingquan Z (2012) Prognosis and treatment of acute hydrocephalus following aneurysmal subarachnoid haemorrhage. J Clin Neurosci 19(5):669–72. https://doi.org/10.1016/j.jocn.2011.06.032
Lindvall P, Runnerstam M, Birgander R, Koskinen LO (2009) The Fisher grading correlated to outcome in patients with subarachnoid haemorrhage. Br J Neurosurg 23(2):188–192. https://doi.org/10.1080/02688690802710668.Sano
MacDonald RL (2014) Delayed neurological deterioration after subarachnoid haemorrhage. Nat Rev Neurol 10(1):44–58. https://doi.org/10.1038/nrneurol.2013.246
Nakagawa I, Hironaka Y, Nishimura F (2013) Early inhibition of natriuresis suppresses symptomatic cerebral vasospasm in patients with aneurysmal subarachnoid hemorrhage. Cerebrovasc Dis 35:131–137. https://doi.org/10.1159/000346586
Neifert SN, Chapman EK, Martini ML, Shuman WH, Schupper AJ, Oermann EK, Mocco J, Macdonald RL (2021) Aneurismal subarachnoid hemorrhage: the last decade. Trans Stroke Res 12(3):428–446. https://doi.org/10.10007/s12975-020-00867-0
Roos YB, de Haan RJ, Beenen LF, Groen RJ, Albrecht KW, Vermeulen M (2000) Complications and outcome in patients with aneurysmal subarachnoid haemorrhage: a prospective hospital-based cohort study in The Netherlands. J Neurol Neurosurg Psychiatry 68(3):337–341. https://doi.org/10.1136/jnnp.68.3.337
Article CAS PubMed PubMed Central Google Scholar
Rowland MJ, Hadjipavlou G, Kelly M, Westbrook J, Pattinson KTS (2012) Delayed cerebral ischaemia after subarachnoid haemorrhage: looking beyond vasospasm. Br J Anaesth 109(3):315–329. https://doi.org/10.1093/bja/aes264
Sehba FA, Ryszard JH, Pluta M, Zhang JH (2012) The importance of early brain injury after subarachnoid hemorrhage. Prog Neurobiol 97(1):14–37. https://doi.org/10.1016/j.pneurobio.2012.02.003
Starnoni D, Maduri R, Hajdu SD, Pierzchala K, Giammattei L, Rocca A, Grosfilley SB, Saliou G, Messerer M, Roy (2019) Early perfusion computed tomography scan for prediction of vasospasm and delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. World Neurosurg 130:e743–e752. https://doi.org/10.1016/j.wneu.2019.06.213
van Asch CJ, van der Schaaf IC, Rinkel GJ (2010) Acute hydrocephalus and cerebral perfusion after aneurysmal subarachnoid hemorrhage. Am J Neuroradiol 31(1):67–70. https://doi.org/10.3174/ajnr.A1748
van Gijn J, Hijdra A, Wijdicks FM, Vermeulen M, Van Crevel H (1985) Acute hydrocephalus after aneurysmal subarachnoid hemorrhage. J Neurosurg 63(3):355–362. https://doi.org/10.3171/jns.1985.63.3.0355
Van der Steen WE, Leemans EL, van den Berg R, Roos YB, Marquering HA, Verbaan D, Majoie C (2019) Radiological scales predicting delayed cerebral ischemia in subarachnoid hemorrhage: systematic review and meta-analysis. Neuroradiology 61(3):247–256. https://doi.org/10.1007/s00234-019-02161-9
Vergouwen MDI, Vermeulen M, van Gijn J, Rinkel GJE, Wijdicks EF, Muizelaar JP, Mendelow AD, Juvela S, Yonas H, Terbrugge KG, Macdonald RL, Diringer MN, Broderick JP, Dreier JP, Roos YBWEM (2010) Definition of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage as an outcome event in clinical trials and observational studies: proposal of a multidisciplinary research group. Stroke 41:2391–2395. https://doi.org/10.1161/STROKEAHA.110.589275
Weidauer S, Lanfermann H, Raabe A, Zanella F, Seifert V, Beck J (2007) Impairment of cerebral perfusion and infarct patterns attributable to vasospasm after aneurysmal subarachnoid hemorrhage: a prospective MRI and DSA study. Stroke 38(6):1831–1836. https://doi.org/10.1161/STROKEAHA.106.477976
Yoshino M, Yoshimi Y, Taniguchi M, Nakamura S, Ikeda T (1999) Syndrome of inappropriate secretion of antidiuretic hormone associated with idiopathic normal pressure hydrocephalus. Intern Med 38(3):290–292. https://doi.org/10.2169/internalmedicine.38.290
Zhong Y, Xin H, Chao Y (2017) Endovascular therapy for vasospasm secondary to subarachnoid hemorrhage: a meta-analysis and systematic review. Clin Neurol Neurosurg 163:9–14. https://doi.org/10.1016/j.clineuro.2017.09.016
Download references
Author information
Authors and affiliations.
Department of Diagnostic and Interventional Neuroradiology, Bretonneau Hospital, University of Tours, Tours, France
Axel Masson, Grégoire Boulouis, Kevin Janot, Denis Herbreteau, Jean-Phlippe Cottier, Richard Bibi, Sandra Obry & Héloïse Ifergan
Department of Diagnostic Neuroradiology, Orleans Hospital Center, Orleans, France
Clara Cohen
Department of Neurosurgery, Bretonneau Hospital, University of Tours, Tours, France
Stéphane Velut & Aymeric Amelot
You can also search for this author in PubMed Google Scholar
Corresponding authors
Correspondence to Axel Masson or Héloïse Ifergan .
Ethics declarations
Ethical approval.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
Axel Masson declares that he has no conflict of interest.
Grégoire Boulouis declares that he has no conflict of interest.
Kévin Janot declares that he has no conflict of interest.
Denis Herbreteau declares that he has no conflict of interest.
Jean-Philippe Cottier declares that he has no conflict of interest.
Richard Bibi declares that he has no conflict of interest.
Clara Cohen declares that she has no conflict of interest.
Sandra Obry declares that she has no conflict of interest.
Stéphane Velut declares that he has no conflict of interest.
Aymeric Amelot declares that he has no conflict of interest.
Héloïse Ifergan declares that she has no conflict of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Vascular Neurosurgery - Aneurysm
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Masson, A., Boulouis, G., Janot, K. et al. Acute hydrocephalus and delayed cerebral infarction after aneurysmal subarachnoid hemorrhage. Acta Neurochir 164 , 2401–2408 (2022). https://doi.org/10.1007/s00701-022-05321-8
Download citation
Received : 26 February 2022
Accepted : 17 July 2022
Published : 02 August 2022
Issue Date : September 2022
DOI : https://doi.org/10.1007/s00701-022-05321-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Acute hydrocephalus
- Find a journal
- Publish with us
- Track your research
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- For authors
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 16, Issue 3
- WEB shape modifications: angiography–histopathology correlations in rabbits
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-7305-3125 Kevin Janot 1 ,
- http://orcid.org/0000-0001-8422-9205 Grégoire Boulouis 1 ,
- http://orcid.org/0000-0003-4797-9693 Géraud Forestier 2 ,
- http://orcid.org/0000-0001-6748-2081 Fouzi Bala 1 ,
- Jonathan Cortese 3 , 4 ,
- http://orcid.org/0000-0002-2543-6535 Zoltán Szatmáry 4 ,
- http://orcid.org/0000-0002-0217-6910 Sylvia M. Bardet 4 ,
- Maxime Baudouin 5 ,
- Marie-Laure Perrin 4 ,
- Jérémy Mounier 4 ,
- Claude Couquet 4 ,
- Catherine Yardin 6 ,
- Guillaume Segonds 7 ,
- Nicolas Dubois 7 ,
- Alexandra Martinez 7 ,
- Pierre-Louis Lesage 7 ,
- Yong-Hong Ding 8 ,
- http://orcid.org/0000-0002-6786-9953 Ramanathan Kadirvel 8 ,
- http://orcid.org/0000-0003-4051-6450 Daying Dai 8 ,
- Charbel Mounayer 2 ,
- Faraj Terro 9 ,
- http://orcid.org/0000-0003-0902-3375 Aymeric Rouchaud 2 , 4
- 1 Interventional Neuroradiology , University Hospital of Tours , Tours , France
- 2 Interventional Neuroradiology , University Hospital of Limoges , Limoges , France
- 3 NEURI The Brain Vascular Center , Bicêtre University Hospital , Le Kremlin-Bicêtre , France
- 4 XLIM UMR CNRS 7252 , University of Limoges , Limoges , France
- 5 Radiology , University Hospital of Limoges , Limoges , France
- 6 Histology, Cytology, Cellular Biology and Cytogenetics , University Hospital of Limoges , Limoges , France
- 7 University of Limoges , Limoges , France
- 8 Radiology , Mayo Clinic , Rochester , Minnesota , USA
- 9 Cell Biology , University Hospital of Limoges , Limoges , France
- Correspondence to Dr Kevin Janot, Diagnostic and Interventional Neuroradiology, University Hospital of Tours, Tours, France; kevin.janot{at}hotmail.com
Background WEB Shape Modification (WSM) over time is frequent after aneurysm treatment. In this study, we explored the relationship between histopathological changes and angiographic evolution over time in experimental aneurysms in rabbits treated with the Woven EndoBridge (WEB) procedure.
Methods Quantitative WSM was assessed using flat-panel computed tomography (FPCT) during follow-up by calculating height and width ratio (HR, WR), defined as the ratio between either measurement at an index time point and the measurement immediately after WEB implantation. The index time point varied from 1 day to 6 months. HR and WR were evaluated with angiographic and histopathological assessments of aneurysm healing.
Results Final HR of devices varied from 0.30 to 1.02 and final WR varied from 0.62 to 1.59. Altogether, at least 5% of HR and WR variations were observed in 37/40 (92.5%) and 28/40 (70%) WEB devices, respectively, at the time of final assessment. There was no significant correlation between complete or incomplete occlusion groups and HR or WR (p=0.15 and p=0.43). Histopathological analysis revealed a significant association between WR and aneurysm healing and fibrosis 1 month following aneurysm treatment (both p<0.05).
Conclusion Using longitudinal FPCT assessment, we observed that WSM affects both the height and width of the WEB device. No significant association was found between WSM and aneurysm occlusion status. Although presumably a multifactorial phenomenon, the histopathological analysis highlighted a significant association between width variations, aneurysm healing and fibrosis in the first month following aneurysm treatment.
Data availability statement
Data are available upon reasonable request.
https://doi.org/10.1136/jnis-2023-020193
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
WHAT IS ALREADY KNOWN ON THIS TOPIC
WEB Shape Modification (WSM) over time is a frequent after aneurysm treatment, but physiopathology remains poorly understood and there are discrepant data in the literature regarding the association of WSM with aneurysm occlusion.
WHAT THIS STUDY ADDS
Our study shows that WSM is common after WEB implantation in rabbits. WSM is a continuous longitudinal phenomenon and is more intense during the first month after device implantation. This phenomenon affects the height but also the width of the device, the latter being associated in our sample with significantly more frequent aneurysmal histopathological healing and fibrosis. No significant association was found between WSM and aneurysm occlusion status.
HOW THIS STUDY MIGHT AFFECT PRACTICE
WSM might reflect aneurysm healing and is not associated with worse angiographic outcomes. Width ratio may serve as a reliable biomarker for future research investigating results of WEB devices.
Introduction
The Woven EndoBridge (WEB) device (Microvention, California, USA) is a commonly used intra-saccular flow-disrupter used to treat intracranial aneurysms with large series reporting evidence on its safety and efficacy, mainly in wide-neck bifurcation aneurysms. 1–3
WEB Shape Modification (WSM) is a commonly observed phenomenon during follow-up and was reported in up to 90.6% of patients 4–10 with contradictory data on its association with angiographic outcomes. Some studies found that aneurysmal recurrence was more common in case of WSM, 4 9 10 while other studies did not show a relation between WSM and incomplete aneurysm occlusion. 5 6 Pathophysiology of this phenomenon remains poorly understood although WSM is presumably multifactorial, part of it driven by “water-hammer effect” due to high inflow jet, the other part due to clot retraction secondary to intra-aneurysmal thrombosis and fibrosis induced by the healing process may contribute to this phenomenon. 11 12 Previous series may have suffered from a subjective visual qualitative assessment of WSM, preventing strong conclusions from being drawn regarding its association with aneurysm healing.
The elastase-induced aneurysm model in rabbits is adequate for testing neuro-interventional devices and was used to validate the Web Occlusion Scale (WOS). 13 A previous animal study from our group reported that a high fibrosis ratio could be associated with WEB shape changes in elastase induced aneurysm in rabbits. 14 However, in this previous work WSM evaluation was limited by the lack of 3D imaging, and of longitudinal assessment.
To explore the pathophysiology of WSM phenomenon in relation with aneurysm histopathological healing, we analyzed a series of rabbits treated with a WEB 17 device, followed-up longitudinally using flat-panel computed tomography (FPCT), and assessed with histopathological features at the time of last follow-up.
Materials and methods
Ethical statement.
The experimental procedures were authorized by the veterinary ethics committee and were conducted in accordance with European requirements 2010/63/EU on the housing and use of animals for scientific purposes.
Aneurysm creation
Elastase-induced aneurysms were created in 43 New Zealand white rabbits. After the rabbits were anesthetized, the right carotid artery was exposed and a 5F sheath ( Cordis Endovascular, Miami Lakes, FL ) was inserted and a bolus of 500 IU of heparin was administered. A 4F Fogarty balloon ( Baxter Healthcare Corporation, Irvine, CA ) was advanced through the sheath to the origin of the right common carotid artery and inflated with iodinated contrast to achieve flow arrest in the carotid. An aqueous porcine elastase suspension (approximately 100 U/ml; Worthington Biochemical Corporation, Lakewood, NJ ) mixed with iodinated contrast was incubated for 20 minutes in the dead space of the right common carotid artery above the inflated balloon.
Devices and treatment procedure
At least 3 weeks after their aneurysms were created the rabbits were treated using an angiographic system (Artis Icono, Siemens Healthineers, Germany). After anesthesia, the right common femoral artery was exposed, and a 5 French sheath ( Cordis Endovascular, Miami Lakes, FL ) was advanced into the artery. A bolus of 500 IU of heparin was administered and a 5F guiding catheter ( Envoy, Cordis Neurovascular Systems, Miami Lakes, FL ) was advanced into the brachiocephalic artery. Using a coaxial technique, a microcatheter (Via-17; Microvention) was advanced into the aneurysm. The size of the aneurysm was assessed using 3D acquisition and aneurysms were embolized using the appropriate WEB device among SLS4, SLS5, SLS6 and SLS7. Following the embolization, a final control digital subtraction angiography (DSA) and flat-panel computed tomography (FPCT) acquisitions were performed. No antiplatelet therapy was given during the post-operative period ( online supplemental figure A )
Supplemental material
Imaging follow-up.
The rabbits were all assessed with serial FPCT performed with the same monoplane angiographic system following WEB implantation (Artis Icono, Siemens Healthineers) at day 1, 7, and every month thereafter. An acquisition time of 14 s was used for all FPCT. The acquisitions parameters were the following: tube voltage of 70kV, pulse width of 4 ms, rotation scan of 200° (speed rotation 0,4°/f) and a field of view of 25 cm. Five hundred projections were thus acquired and images were analyzed at 16-bit scale with matrix reconstructions of 512×512. Slices thickness was 0.1 mm and a voxel size of 154 µm.
Sedation with ketamine was used before FPCT acquisition to decrease movement artifacts. The rabbit cohort was divided into three subgroups for sacrifice at 1 month, 3 months and 6 months.

Aneurysm grading
On the day of final DSA follow-up, anesthesia was performed, and surgical access of the left femoral artery was performed in a similar way to that used for the embolization procedure. A 5F catheter was placed in the aortic arch and DSA was performed. Angiographic occlusion of the aneurysm was assessed using the Web Occlusion Scale (WOS). 15 Scores were dichotomized into complete occlusion (WOS A+WOS B) and adequate occlusion (WOS A+WOS B + WOS C).
FPCT analysis
FPCT acquisitions were reviewed for all devices over the period of follow-up until sacrifice. WEB height and average width were measured by an experienced operator (KJ) on each FPCT using multiplanar reconstructions (MPR) with Horos Software (Horos Medicale Image Software, version 3.3.6, https//horosproject.org). Height distance was assessed on coronal views by the distance between proximal and distal markers. Width distance was calculated by the average of two orthogonal measurements on an axial view measured on an orthogonal plan at the line between the two markers in the middle height of the device. To assess the interobserver variability of WEB measurements, a second reader (FB) performed the same measurements in a random sample of 10% of the study sample size.
Quantitative WSM assessment using FPCT
We calculated a height ratio (HR) and a width ratio (WR) for each implanted WEB using FPCT analysis. The height ratio was defined as the ratio between the height measured at a time point (day 1, day 7, month 1, month 2, month 3, month 4, month 5 or month 6) and the initial height measured immediately after WEB deployment (day 0). The width ratio was defined as the ratio between the average width estimated at a time point (day 1, day 7, month 1, month 2, month 3, month 4, month 5 or month 6) and the initial average (day 0). Using FPCT, WSM was defined by HR or WR variations along the time. ( online supplemental figure B )
Histomorphological analysis
For histological study, the aneurysms were harvested and fixed in 10% formalin solution for at least 24 hours. The specimens were then dehydrated in graded ethanol and embedded in methyl methacrylate resin. Slices in the plane perpendicular to the aneurysm neck were cut with a laser microtome (TissueSurgeon, LLS ROWIAK GmbH, Hanover, Germany) 16 and stained with either hematoxylin-eosin or Masson’s trichrome. Two histopathologists, blinded to the angiographic results, performed the histological analysis of aneurysm healing using an ordinal histological grading scale as previously described by Dai et al . 17 This score takes account of three criteria: Dome healing, Neck healing and Neck compaction. Neck healing is assessed by both gross and microscopic inspection. Healing at the neck tends to progress from unorganized thrombus to thin layers of hypocellular tissue permitting us to attribute scores ranging from 0 to 4. Scores from both gross and microscopic evaluations are averaged to yield a single neck score. Dome healing is assessed using the microscopic image only; it tends to progress from unorganized thrombus to amorphous extracellular matrix which enables us to attribute a score from 0 to 5. Compaction at the neck is assessed by using both angiographic and histologic images from concave to convex aspect (range 0–3).
Masson’s trichrome stains in blue collagen and therefore allows us to evaluate collagen deposition, which reflects the extent of fibrosis, within the aneurysmal sac. Collagen levels within the aneurysm were quantified using a threshold method in Image/Fiji software. Fibrosis was expressed as the rate of collagen-positive area over the total area of the aneurysm cavity.
Statistical analysis
Continuous variables were described as mean (SD±SD), or median (interquartile range (IQR)) and compared in multivariable analyses using a t-test, or the Wilcoxon test as appropriate. Categoric variables were presented as a number (percentage of total) and compared using the Chi-squared or Fisher’s exact tests.
Associations between HR and histological healing or fibrosis ratio were evaluated using a simple linear fit (bivariate correlation), and the association between WR and histological healing or fibrosis ratio was evaluated by univariable polynomial logistic regression to account for the two ways of variation of the WR (less or greater than 1).
To assess inter-rater agreement of WEB quantitative measurements, we calculated the intraclass correlation coefficient (ICC) for the two readers.
We also conducted a sensitivity analysis to evaluate a potential association between the sizing of implanted WEB devices and HR or WR variations. Methodology and results are presented in supplemental data and supplemental figure E .
A p-value of 0.05 was considered statistically significant. Analyses were performed using JMP, Version 17 (SAS Institute Inc., Cary, NC, 1989–2021).
Rabbits and aneurysms
Forty-three aneurysms in 43 consecutive rabbits were treated with fifth generation WEB devices (SLS 4, SLS 5, SLS 6 or SLS 7). The mean (SD) aneurysm neck, width and height were 3.6±1 mm, 3.3±0.7 mm and 7±1.9 mm, respectively. Two rabbits died during the follow-up (at 1 week and 2 months) and DSA images were unavailable for one rabbit, yielding a sample of 40 rabbits for the final analysis. Nineteen rabbits were sacrificed at 1 month, 12 rabbits were sacrificed at 3 months and 9 rabbits were sacrificed at 6 months.
Angiographic findings
In the pooled analysis, 14/40 (35%) aneurysms demonstrated complete occlusion (WOS A+B) and 34/40 (85%) aneurysms demonstrated adequate occlusion (WOS A+B + C). No significant difference in complete or adequate occlusion was observed between 1 month, 3 month and 6 month follow-up groups (p=0.36). Detailed angiographic results regarding subgroups for sacrifice at 1 month, 3 months and 6 months are presented in online supplemental figure C .
Interobserver agreement was excellent for all three MPR measurements with ICC values of 0.89 (95% confidence interval (CI) 0.31 to 0.97) for the height, 0.94 (95% CI 0.76 to 0.98) and 0.96 (95% CI 0.93 to 0.98) for the two orthogonal distances of width 18 ( figure 1 and online supplemental figure D )
- Download figure
- Open in new tab
- Download powerpoint
Aneurysm treatment with WEB device followed during 3 months. Non-subtracted DSA depicted WSM between day 0 and 3 month follow-up confirmed by FPCT (HR=0.94 and WR=0.75). Final angiogram showed a complete occlusion (WOS A). A=non-subtracted DSA at day 0; B=non-subtracted DSA at day 90; C=final angiogram at day 90; D=FPCT in coronal view at day 0; E=FPCT in coronal view at day 90; F=final angiogram in 3D volume rendering angiography.
Height analysis using HR
In the pooled analysis, the final HR of WEB devices varied from 0.30 to 1.02 compared with the height measured on the FPCT performed immediately after WEB implantation. The HR decreased over time and more intensely during the first month. Indeed, 37/40 WEB devices (92.5%) had at least 5% of HR variations compared with the initial FPCT (day 0) ( figure 2 ).
Analysis of height ratio (HR) and width ratio (WR) over time. A=Final HR calculated for each rabbit followed. The grey zone indicates 5% cut-off around HR=1. B=Longitudinal evolution of HR along the time. The HR calculated for each FPCT are drawn for the three groups of follow-ups. The curves analysis shows a continuous decrease of the HR over time with a more intense decrease during the first follow-ups. C=Final WR calculated for each rabbit followed. The gray zone indicates 5% cut-off around WR=1. D=Longitudinal evolution of WR along the time the width ratio calculated for each FPCT is drawn and shows a continuous evolution of the WR along the time. Moreover, WR could vary in two different directions which finally makes a larger or a narrower web device.
No significant difference of mean HR was observed between the occlusion groups: 0.77±0.11 (complete occlusion) vs 0.84±0.17 (incomplete occlusion), (p=0.15).
Width analysis using WR
WSM was also observed with the width analysis. In the pooled analysis, final WR of WEB devices varied from 0.62 to 1.59, meaning the WEB device can become larger (WR>1) or narrower (WR<1) over time :17/40 (42.5%) WEBs had a narrower width at the end of the follow-up compared with post-implantation measurement and 21/40 (52.5%) had larger width. Width variations varied over time with larger variation during the first month. Indeed, 28/40 WEB devices (70%) had at least 5% of WR variations compared with initial FPCT (day 0) ( figure 2 ).
No significant difference of mean WR was observed between the occlusion groups: 0.98±0.20 (complete occlusion) vs 1.03±0.20 (incomplete occlusion), (p=0.43).
Histopathological findings: aneurysmal healing scores and fibrosis
In our sample, histologic healing scores could be estimated for 37 aneurysms (17 in the 1 month follow-up group, 11 in the 3 months follow-up group and 9 in the 6 months follow-up group) and varied from 2 to 11 (7.7±2.6). Fibrosis rates could be estimated for 35 aneurysms (16 in the 1 month follow-up group, 10 in the 3 months follow-up group and 9 in the 6 months follow-up group) and varied from 3% to 97.4% (35.5±30.0).
Association with follow-up
The mean (SD) histologic healing score was 7.6±3.0 for the 1 month group (n=17), 7.7±1.8 for the 3 months group (n=11) and 7.8±2.9 for the 6 months group (n=9) with no significant difference between follow-up groups (p=0.77). However, the fibrosis rate was significantly higher in the 6 month group (59.8%±18.8% (n=9) vs 27.4%±14.7% in the 1 month group (n=16) and 29.6%±25.4% in the 3 month group (n=10) ; p=0.02).
Association with angiographic occlusion
The mean histologic healing score was significantly higher in the complete occlusion group (WOS A & B) compared with the incomplete occlusion group (WOS C & D):9.3±1.2 vs 6.7±2.8, respectively (p<0.001). The fibrosis rate was also higher in the complete occlusion group (51.9%±25.1% compared with 27.2%±23.9% in the incomplete occlusion group; p=0.008).
Association with WSM
HR was not significantly associated with a fibrosis ratio (n=35) or aneurysm healing score (n=37) in the linear regression analysis (β estimate : −0.212; p=0.106)( figures 3 and 4 ).
Significant correlation between fibrosis ratio and width ratio (A) and Aneurysm Healing score and width ratio (B) at 1 month follow-up. As the width ratio could change in two different ways, we used a polynomial fitting for correlation analysis; for both variations, significant higher fibrosis rates or healing scores were seen.
Correlation between histopathological analysis and quantitative analysis of WSM with FBCT. Aneurysm healing score was evaluated at 10 and fibrosis ratio measured at 78%. On FPCT, Height ratio (HR) and Width ratio (WR) were respectively measured at 0.72 and 0.89. A=histopathological slice with HES staining; B=histopathological slice with Trichrome Masson stain; C=coronal view on FPCT at day 0; D=coronal view on FPCT at day 90.
The final WR was associated with dome organization (n=37; β estimate : 8.02; p<0.01) but not with micro-neck analysis (n=37; β estimate : 2.26; p=0.44)
In the group of rabbits sacrificed at month-1, final WR was also associated with the fibrosis ratio (n=16 ; β estimate : 250.38; p=0.03) and aneurysm healing score (n=17 ; β estimate: 30.14; p=0.04) ( figures 3 and 4 ).
However, in the group of rabbits sacrificed at month-3 and month-6, final WR was not associated with the fibrosis ratio (respectively n=10 with β estimate: −0.239; p=0.56 and n=9 with β estimate: 57.20; p=0.79) or aneurysm healing scores (respectively n=11 with β estimate: 7.4; p=0.80 and n=9 with β estimate: 15.9; p=0.40).
In this study we showed that quantitative WSM affects both the width and the height of the device, and is associated with histopathological markers of aneurysm healing, independently of angiographic measures of occlusion.
Interestingly between the first and last assessment, the WR of the WEB device varied in our sample from 0.62 to 1.59 which indicated that the WEB device could be narrowed or enlarged. This finding, to our knowledge, has been evaluated in only one previous study in humans 10 in which the authors showed a univariate association with worse angiographic outcome, but for which no histopathological assessment was obviously available. In a distinct setting, our analysis did not show any correlation between WR variations and angiographic outcomes. Yet, a statistically significant correlation was found in the subsample of rabbits sacrificed at 1 month, the time-point with the most pronounced WSM, aneurysmal healing scores and fibrosis ratio were significantly associated with final WR. This novel result suggests that aneurysm healing could be associated to WSM and may even be a direct contributor to changes in transverse diameters.
No significant association was found between final WR and aneurysm healing or fibrosis in 3 month and 6 month groups. This loss of significance at later time points may first be explained by a lack of power to confirm trends. There were indeed fewer rabbits in 3 month (n=12) and 6 month groups (n=9) compared with the 1 month group (n=19). Moreover, WSM phenomenon is more pronounced during the first weeks following implantation, and tends to be smaller magnitude thereafter. This may also be due to the process of aneurysm histological healing, that have been shown to be more pronounced during the first month following aneurysm possibly resulting in less histological differences in the 3 month or 6 month group. 19
In a previous study in rabbits, we also assessed the potential intrications of fibrosis with WSM and angiographic outcomes. 14 As assessed in previous studies with other embolization devices such as coils or flow-diverter stents, clot retraction during thrombus organization is a common phenomenon. 20 21 In turn, WSM could be the result of intra-aneurysmal fibrosis induced by the thrombus trapped in the aneurysm sac and invaded by mesenchymal cells and fibroblasts responsible for collagen deposition. 14 19 Intra-aneurysmal fibrosis is among the most plausible mechanisms underlying aneurysm healing, being mandatory for neck endothelialization and aneurysm exclusion. In turn, aneurysm healing and fibrosis related reactions could lead to intra-aneurysmal/intrasaccular clot retraction and traction of a WEB device. In distinct settings, similar findings have been previously reported in experimental studies in which higher fibrosis increased coils retraction with more angiographic neck remnants but with perfect histological healing and arterial reconstruction at the level of the neck. 22 The incidence of clot retraction appears to be higher in wide neck or large aneurysms which are the target of the WEB device, 17 and may present a variation of neck scarring. Similar to Brinjikji et al ., who reported that healing mechanisms in coiled aneurysms could be ongoing up to 1 year after treatment, we also showed variations of HR and WR in this study up to the latest follow-up, that is 6 months following deployment. 19
Our quantitative assessment using FPCT showed that 37/40 WEB devices (92.5%) had at least 5% of HR variations and 28/40 WEB devices (70%) had at least 5% of WR variations compared with the first measurements on FPCT (day 0). This rate is quite higher compared with a previous rabbit study from our group, probably due to the quantitative approach in the present work. 14 This previous study only evaluated WSM using non-subtracted DSA in working projection, 14 using a dichotomized subjective assessment of WSM, with potential imperfect interrater agreement. Yet, our results are in line with the work by Rosskopf et al who reported that in 29/32 (90.6%) patients, the height reduction of the WEB device was at least 5%, also using quantitative measurements with CT-scan analyses. 8 In both studies, WSM was not associated with worse angiographic results. 8 This last point remains a widely debated topic in the literature with major disagreements between studies. 4–6 8–10 These disagreements may emerge from differences in WSM assessment (using non-subtracted DSA, 4–6 10 vaso-CT 9 or computerized tomography (CT) scans 7 8 ).
FPCT has proven to be an interesting tool to precisely evaluate intravascular devices including WEB. 9 23 A quantitative approach of the WSM with repeated FPCT acquisitions over a long time period following aneurysm treatment showed that WSM is present in all implanted WEB devices in variable proportions (final HR and final WR of WEB devices respectively varied from 0.30 to 1.02 and 0.62 to 1.59 compared with the height and the width measured on FPCT immediately after implantation). The time curve analysis demonstrated an early and continuous phenomenon in accordance with previous observations ( figure 2 ). 6 8 9
The present work also provides insight to the most recent advances of the WEB device, by giving preclinical data on the fifth generation of the WEB device (the “17-system”), with fewer wires that permits delivery of smaller WEB devices through a 0.017-inch microcatheter. 24 25 This study is, indeed, the first to evaluate the fifth generation of WEB device in elastase-induced aneurysm in rabbits, reporting similar aneurysm occlusion rates than previous series in rabbits with previous generations of WEB devices with 14/40 (35%) of complete occlusion and 34/40 (85%) of adequate occlusion 13 14 26 at the last follow-up. WEB-17 also appears to be subject to WEB shape changes after aneurysm treatment as with previous generations of these devices.
No antiplatelet therapy was given to rabbits in our study. As antiplatelet therapy could independently affect the aneurysm healing process, we chose not to use it in our study which included histological analysis. The effect of antiplatelet therapy on aneurysm healing has been shown in an animal study which analyzed aneurysm healing after hydrocoils embolization and reported that antiplatelet treatments decrease the area of organized tissue in the aneurysm sac. 27 Further, the association between antiplatelet and aneurysm healing after WEB device implantation was discussed in two clinical studies; the “BOSS1 phenomenon” which corresponds to a persistent blood flow inside a WEB device, likely due to a partial aneurysm healing could be associated with antiplatelet therapy in a post-operative period. 28 29
Interestingly, in these two studies, WSM were less frequently observed in the case of persistent blood flow inside a WEB device (BOSS1) compared with other angiographic results. 28 29 This point supports our theory that WSM could be related to the aneurysm healing process including intra-aneurysmal tissue organization and fibrosis process, in relation to platelet aggregation.
Our study has several limitations. First, we only used WEB-17 SLS devices while we have previously showed that WEB device type could influence aneurysm healing and device shape changes after implantation. 29 The use of a newer WEB generation is in line with the device’s technical evolution and the anticipated widening use of WEB17-SLS. Second, we did not consider other factors that could influence WSM incidence after WEB treatment, such as intra-aneurysmal blood flow parameters, 11 aneurysm morphology, device type and sizing, 14 anti-platelet therapy in the post-operative period, and WEB orientation after deployment. 30 Computational fluid dynamics (CFD) simulations have also shown that WEB changes could be positively correlated with flow into the aneurysm. 11 Third, the sample size was relatively small. However, to our knowledge this is the largest study assessing the correlation between quantitative WEB measurements and histologic data with a detailed angiographic analysis using FPCT.
In experimental aneurysms in a rabbit model, we showed WSM to be a common phenomenon affecting both the height and width of the device without significant association with worse angiographic outcome. Also, WSM appears to be a continuous phenomenon even if more intense early during follow-up. Although presumably a multifactorial phenomenon, we found a significant association between width variations and aneurysm healing and fibrosis at the first month following aneurysm treatment.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
The experimental procedures were authorized by the French Ministry of Higher Education, Research and Innovation (APAFIS #28943-2021011310199793 v1). They were carried out on the EMIS research platform (Limoges, FRANCE), in accordance with European requirements 2010/63/EU on the housing and use of animals for scientific purposes.
- Heiferman DM ,
- Inoa V , et al
- Cognard C , et al
- Szikora I ,
- Barreau X , et al
- Cognard C ,
- Herbreteau D ,
- Narata AP , et al
- Amelot A , et al
- Le Bras A , et al
- Rosskopf J ,
- Dreyhaupt J , et al
- Cortese J ,
- Girot JB , et al
- Fiehler J ,
- Bester M , et al
- Mihalea C ,
- Da Ros V , et al
- Rouchaud A ,
- Brinjikji W ,
- Ding Y-H , et al
- Rouchaud A , et al
- Fiorella D ,
- Byrne J , et al
- Verhaegen C ,
- Kautbally S ,
- Zapareto DC , et al
- Lewis DA , et al
- Cicchetti DV ,
- Shoinralter D ,
- Kallmes DF ,
- Raymond J ,
- Darsaut T ,
- Salazkin I , et al
- Sadasivan C ,
- Seong J , et al
- Dai D , et al
- Neki H , et al
- van Rooij SBT ,
- Peluso JP ,
- Sluzewski M , et al
- Pagiola I , et al
- Kadirvel R , et al
- Xi G , et al
- Nguyen HA ,
- Manceau P-F , et al
- Popescu SD ,
- Mihalea C , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
Twitter @gboulouis, @FouziBala
Contributors KJ conceived and composed the initial draft manuscript framework, acquired the data, wrote the original draft and is responsible for the overall content as the guarantor ; GB, AR, FB were responsible for writing, reviewing and editing the manuscript; GF, JC, ZS, SMB, MB, MLP, JM, CC,CY, ND, GS, AM, PLL,YHD, RK, DD, CM, FT all reviewed and edited the draft. All authors approved of the final version of the manuscript before submission for publication.
Funding WEB devices used for this work are provided by Microvention. This work was partially supported by Microvention and the French Radiology Society.
Competing interests AR reports consulting for Balt and Microvention.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
- Preplanned tours
- Daytrips out of Moscow
- Themed tours
- Customized tours
- St. Petersburg
Moscow Metro
The Moscow Metro Tour is included in most guided tours’ itineraries. Opened in 1935, under Stalin’s regime, the metro was not only meant to solve transport problems, but also was hailed as “a people’s palace”. Every station you will see during your Moscow metro tour looks like a palace room. There are bright paintings, mosaics, stained glass, bronze statues… Our Moscow metro tour includes the most impressive stations best architects and designers worked at - Ploshchad Revolutsii, Mayakovskaya, Komsomolskaya, Kievskaya, Novoslobodskaya and some others.
What is the kremlin in russia?
The guide will not only help you navigate the metro, but will also provide you with fascinating background tales for the images you see and a history of each station.
And there some stories to be told during the Moscow metro tour! The deepest station - Park Pobedy - is 84 metres under the ground with the world longest escalator of 140 meters. Parts of the so-called Metro-2, a secret strategic system of underground tunnels, was used for its construction.
During the Second World War the metro itself became a strategic asset: it was turned into the city's biggest bomb-shelter and one of the stations even became a library. 217 children were born here in 1941-1942! The metro is the most effective means of transport in the capital.
There are almost 200 stations 196 at the moment and trains run every 90 seconds! The guide of your Moscow metro tour can explain to you how to buy tickets and find your way if you plan to get around by yourself.

Kevin McCarthy’s Rebranding Tour
April 14, 2024 at 3:00 pm EDT By Taegan Goddard Leave a Comment
Politico : “Six months after his ouster as speaker of the House, McCarthy is trying to write his own history. Although still comparatively young at 59 in an era of octogenarian politicians, it’s hard to imagine a world in which the first line of his obituary is not that he was the first speaker ever removed from office.”
“So now, McCarthy seems to have set himself to the task of shaping how future generations remember that moment and the eight months he spent wielding the gavel — even if it requires a selective retelling of what happened with a few big omissions.”

Recent Posts
Iran sought mass casualties in israel.
“Iran’s weekend aerial attack on Israel was designed to cause mass casualties and infrastructure damage, senior U.S. officials said, an assessment that complicates deliberations on how to respond to Tehran…
Johnson Signals He Won’t Put Senate Bill on Floor
“Speaker Mike Johnson (R-LA) on Sunday did not indicate that he would put the Senate-passed supplemental package on foreign aid on the floor this week, despite mounting pressure from Democrats…
Teamsters Make Another Move Toward the GOP
“The Teamsters union’s political action committee is jumping into the Missouri Senate race, contributing $5,000 to Sen. Josh Hawley’s (R-MO) re-election campaign,” Axios reports. “In the past, the PAC has…
‘A Six-Week-Long Media Extravaganza’
An attorney for Donald Trump brushed off the significance of his first criminal trial, which is scheduled to begin Monday, saying the case is merely a “six-week-long media extravaganza,” The…
The Intercept Is Running Out of Money
“The Intercept, the left-wing U.S. newsroom that’s been a thorn in Joe Biden’s side and a hub for pro-Palestinian coverage, is nearly out of money and facing its own bitter…
It’s Hard to Get Excited About Trump’s First Criminal Trial
Rick Hasen: “In watching some of the breathless coverage of Donald Trump’s ‘hush money’ trial, I’m reminded of the 2004 quote from former U.S. Defense Secretary Donald Rumsfeld that, ‘You…
Cash at Menendez Home Was Not From His Bank
“When Senator Robert Menendez was charged last year with corruption after investigators found $486,000 in cash stashed around his house in New Jersey, he offered a simple, ‘old-fashioned’ explanation: It…
Kristi Noem Is Now Barred from Much of Her State
“Four of South Dakota’s federally recognized Native American tribes have barred the state’s governor, Kristi Noem — a Republican whose name has been floated as a potential running mate for…
U.S. Economy Expected to Keep Powering Higher
Wall Street Journal: “In the latest quarterly survey by The Wall Street Journal, business and academic economists lowered the chances of a recession within the next year to 29% from…
Exchange of the Day
New Hampshire Gov. Chris Sununu (R) was interviewed on ABC News by George Stephanopoulos: STEPHANOPOULOS: Just to sum up. You support Trump for president even if he’s convicted in the…
The Americans Crossing Biden’s $400,000 Tax Line
Wall Street Journal: “In his successful 2020 presidential run, Biden pledged to protect households from tax increases if their income was below that threshold. He reupped the promise for his…
Small Investors in Trump Media Reckon with Collapse
The Washington Post notes that supporters of Donald Trump “investing in Truth Social is less a business calculation than a statement of faith in the former president and the business…
Trump Supporters Chant ‘Genocide Joe’
“‘Genocide Joe’ is a phrase used by pro-Palestine protesters against President Biden because of his unconditional support of Israel amid its onslaught in Gaza,” the Washington Post reports. “But supporters…
Homicides Are Plummeting in American Cities
“Homicides in American cities are falling at the fastest pace in decades, bringing them close to levels they were at before a pandemic-era jump,” the Wall Street Journal reports. “Nationwide,…
Trump Considers Fundraising Prowess of Running Mate
“As former President Donald Trump sifts through potential running mates, he has peppered some advisers and associates with a direct question: Which Republican could best help him raise money for…
The Fortune Behind Elise Stefanik’s Humble Origins Myth
“From the start of her electoral career a decade ago, House GOP Conference Chair—and potential 2024 vice presidential nominee—Elise Stefanik has stressed her supposedly rough-cut origins, telling a story in…
Trump Plays to a Jury of Millions
“The first criminal trial of Donald Trump will begin on Monday, and the 45th president thinks he can win — no matter what the jury decides. Mr. Trump will aim…
Key Witness Against Trump Is an Admitted Liar
Politico: “Michael Cohen, the former president’s fixer-turned-foe, is expected to tell jurors in the criminal trial starting Monday that Trump directed him to pay $130,000 in hush money to porn…
Justices to Decide If Rioters Can Face Obstruction Charges
Washington Post: “On Tuesday, the Supreme Court will hear oral arguments about whether prosecutors improperly stretched the law by charging people with that violation in the first place.” “The high…
RFK Jr. Says He Qualified for Iowa Ballot
Robert F. Kennedy Jr. said he met the requirements to appear on Iowa’s general election ballot in November following a “convention” he held in West Des Moines Saturday, the Des…
About Political Wire

Goddard spent more than a decade as managing director and chief operating officer of a prominent investment firm in New York City. Previously, he was a policy adviser to a U.S. Senator and Governor.
Goddard is also co-author of You Won - Now What? (Scribner, 1998), a political management book hailed by prominent journalists and politicians from both parties. In addition, Goddard's essays on politics and public policy have appeared in dozens of newspapers across the country.
Goddard earned degrees from Vassar College and Harvard University. He lives in New York with his wife and three sons.
Goddard is the owner of Goddard Media LLC .
Praise for Political Wire
“There are a lot of blogs and news sites claiming to understand politics, but only a few actually do. Political Wire is one of them.”
— Chuck Todd, host of “Meet the Press”
“Concise. Relevant. To the point. Political Wire is the first site I check when I’m looking for the latest political nugget. That pretty much says it all.”
— Stuart Rothenberg, editor of the Rothenberg Political Report
“Political Wire is one of only four or five sites that I check every day and sometimes several times a day, for the latest political news and developments.”
— Charlie Cook, editor of the Cook Political Report
“The big news, delicious tidbits, pearls of wisdom — nicely packaged, constantly updated… What political junkie could ask for more?”
— Larry Sabato, Center for Politics, University of Virginia
“Political Wire is a great, great site.”
— Joe Scarborough, host of MSNBC’s “Morning Joe”
“Taegan Goddard has a knack for digging out political gems that too often get passed over by the mainstream press, and for delivering the latest electoral developments in a sharp, no frills style that makes his Political Wire an addictive blog habit you don’t want to kick.”
— Arianna Huffington, founder of The Huffington Post
“Political Wire is one of the absolute must-read sites in the blogosphere.”
— Glenn Reynolds, founder of Instapundit
“I rely on Taegan Goddard’s Political Wire for straight, fair political news, he gets right to the point. It’s an eagerly anticipated part of my news reading.”
— Craig Newmark, founder of Craigslist.

Harper's Bazaar
Just a Few of the Biggest Concert Tours of 2024, from Olivia Rodrigo to Bad Bunny
Posted: April 14, 2024 | Last updated: April 14, 2024

Listening to your favorite musician at home is fun, but there's nothing quite like the experience of singing along with them, and tons of more fans, live. And as luck would have it, 2024 is shaping up to be a massive year for some of the world's top musical acts, so chances are your favorite performer might be stopping at a city near you soon.
Ahead, we rounded up some of the biggest concert tours of 2024, ranging from Taylor Swift's mega-popular Eras Tour to Drake and J. Cole's exciting It's All A Blur Tour - Big as the What?—set to kick off this winter. You can also expect tour dates from classic icons like Stevie Nicks, Billy Joel, Bruce Springsteen, and more.

1) Taylor Swift
Undoubtedly one of the biggest concert tours ever, Taylor Swift's Eras Tour will continue right through 2024. The international leg of the tour kicked off in Japan, where she played four shows in Tokyo. She'll also stop in Melbourne, Singapore, Paris, Madrid, London, Milan, and more before returning to the States to play in the fall.
There's nothing like seeing T. Swift IRL, but don't fret if you're unable to nab tickets—the Eras Tour movie is now available to stream from the comfort of your home.

2) Olivia Rodrigo
This is not a drill—"Drivers License" singer Olivia Rodrigo will be hitting the road on tour starting at the end of February. The Guts World Tour runs from February through mid-August and has dates in Nashville, Toronto, Chicago, and New York City, among others. Even cooler? Rodrigo will have a stacked list of special guests—like PinkPantheress, Remi Wolf, The Breeders, and Chappell Roan—with her.
3) Red Hot Chili Peppers
Did you hear the good news? The Red Hot Chili Peppers have extended their global tour through summer 2024. The buzzy stadium tour, which kicked off in June 2022, will now run until July 2024 and bring the California-based band to places like Los Angeles, Tampa, Toronto, and Salt Lake City.

4) Bad Bunny
It's fitting that "Monaco" rapper Bad Bunny titled his tour Most Wanted —it's slated to be one of the year's hottest tours. Planned to help promote his latest studio album, Nadie Sabe Lo Que Va a Pasar Mañana , Most Wanted will kick off in Salt Lake City on February 21 and run through May 26.

5) Billy Joel
If you haven't yet seen Billy Joel perform live, there's still time! The Piano Man has added more tour dates to his schedule, stopping in cities like Tampa, New York, Denver, and St. Louis this year. Even more exciting? He'll share the stage with fellow iconic performers Sting and Stevie Nicks for some of these dates.

Mitski recently announced that she's expanding her North American tour dates , and we couldn't be more excited. The months-long tour, which supports her 2023 studio album The Land Is Inhospitable and So Are We, has a long list of stops, including Miami Beach, Philadelphia, Brooklyn, and Paris.

There's nothing quite like a Madonna concert, that's for sure. The singer's Celebration Tour , which started last October, continues straight through the spring with dates in Seattle, San Francisco, Mexico City, and more. Besides her eye-catching sets, chart-topping songs, and impressive choreography, concertgoers also get a glimpse of the performer's fantastic costumes, which include looks from Versace and Jean Paul Gaultier.

8) Bleachers
The New Jersey-founded rock band, which is fronted by Jack Antonoff—known for producing albums for top acts like Taylor Swift, Lorde, and Lana Del Rey—not only has announced a new album but a new tour , too. The tour will start in the UK in March, ending fittingly in the band's home state of New Jersey in mid-June. Check out their newly released music video for "Tiny Moves" if you need a Bleachers fix in the meantime.

9) Nicki Minaj
Nicki fans rejoice: the rapper and singer might be coming to a city near you soon as part of her Pink Friday 2 World Tour. The massive tour will include performances in Brooklyn, Oakland, and Baltimore, with stops at Dreamville Festival and Rolling Loud California along the way.

10) Blink 182
Live out all of your nineties and early aughts pop-punk dreams with one of Blink 182's One More Time Tour dates. The tour, which supports the band's ninth studio album, One More Time..., will bring the trio to cities all over the globe, including Sydney, Santiago, Portland, and Boston. The tour's supporting act is Pierce the Veil, which is also worth checking out.

11) Stevie Nicks
The oh-so-magical Stevie Nicks continues her touring streak with a bunch of 2024 concert dates . Set to begin in Atlantic City, NJ on February 10, Nicks will visit a dozen cities throughout the U.S. this year, such as New Orleans, Omaha, and Chicago. "Let's keep this party going in 2024," the singer-songwriter posted on her Instagram in September to announce the newly added tour dates.

12) The 1975
The 1975 is showing no signs of slowing down. The British band, famous for hits like "Somebody Else" and "Robbers," has extended their 2023 tour through 2024. Titled Still...At Their Very Best , the 22-date tour will open in Glasgow on February 8 and conclude in Amsterdam on March 24.
13) Drake and J. Cole
Rap greats Drake and J. Cole come together for the It's All a Blur Tour – Big As the What? which is guaranteed to be a good time. Drake, fresh off his 2023 It's All a Blur tour with 21 Savage, is set to hit dozens of cities starting in February, many of which J. Cole will also be in tow for. Scoop up tickets ASAP, as Drake's shows are known to sell out.

14) Janet Jackson
Superstar Janet Jackson is also extending her 2023 tour, Together Again , into 2024 with dates in Anaheim, Austin, New Orleans, and Hartford. Even cooler? Jackson's supporting act is the 2000s southern rap legend Nelly.

15) Rolling Stones
If you've ever dreamed of seeing the Rolling Stones perform live in person, now's your chance. The iconic rockers, who released their studio album Hackney Diamonds this past fall, are returning on the road for a 16-date tour with shows throughout the United States and Canada. Concertgoers can expect a mix of new tunes and Stones classics.
16) Bruce Springsteen
Famous for countless listenable hits like "Born to Run" and "Glory Days," Bruce Springsteen is set to embark on a massive world tour this year with his band, The E Street Band. The much-anticipated tour will take the Boss and his crew to cities such as Phoenix, San Diego, Dublin, and Madrid, from March through November.

17) John Mayer
Be sure to catch John Mayer's solo tour this year, which will bring the guitarist and crooner to cities throughout Europe. This leg, an extension of his popular 2023 solo tour, will kick off in Stockholm on March 13 and finish in Dublin on March 29.

18) Shania Twain
Okay, this one is technically a residency , but we're excited nonetheless. Shania Twain, most known for her incredible outfits (her hooded leopard print look, anyone?) and hits like "Man! I Feel Like a Woman!" is setting up shop in Vegas starting May 10. Twain's residency will take place at the Bakkt Theater at Planet Hollywood on and off throughout December 2024.

All good things must come to an end. The Eagles, known for "Hotel California" and other amazing rock songs, began their final concert tour this winter. It launched in Phoenix on January 20, with March 16 as its last date in the United States. Eagles fans won't want to miss this one.

20) Alanis Morisette: The Triple Moon Tour
Alanis Morisette joins forces with Joan Jett and the Blackhearts for their 2024 Triple Moon Tour , which has dates in North America and Canada. This tour is a great one to catch this summer, as it's slated to run from June through August.
More for You
Use this 2-word phrase when your boss asks you to do more work than you have time to do, according to a therapist
The Cavs threw last game to manipulate NBA Playoff matchups, and it could haunt them
These Are 10 Smells That Cats Absolutely Hate
I Lost White Friends When I Finally Spoke Out
19 Common Behaviors of Highly Intelligent People
78 Riddles for Adults That Will Test Your Smarts
Sen. Fetterman breaks with President Biden on US response to Iran attacks: 'We should have Israel's back'
How to 'quiet quit,' from a former teacher who did it for 2 years so she could enjoy a better life while still getting a paycheck
Anheuser-Busch has ‘learned their lesson’: Former exec Anson Frericks
10 Ways To Deodorize Your Musty Basement That Work Like Magic
Harvard-trained psychologist: If you use any of these 9 phrases every day, ‘you're more emotionally secure than most'
'We got it wrong': WeightWatchers CEO on weight loss
Fallout from Trump's bid to overturn election loss heads to Supreme Court
Damning Warning Issued Over Florida Insurance Market
Founder of Toms shoes went on a men’s retreat with other entrepreneurs to combat his loneliness and depression: ‘I lost a lot of my clear meaning and purpose’
Retired colonel says this shows ‘Iranians clearly sending signal’ to the US
I'm a millennial without a college degree. I have 10 years of work experience, but I'm thinking about going back to school because it seems like the only way to get ahead.
Cover Up Unsightly Floor Scratches In A Pinch With This All-Natural Item
18 Ways to Tell if Someone Has a High IQ
Top 30 Most Difficult Songs to Sing
"Adaptative endovascular strategy to the CloT MRI in large intracranial vessel occlusion" (VECTOR): Study protocol of a randomized control trial
Affiliations.
- 1 Department of Neuroradiology, University Hospital of Tours, 2, boulevard Tonnellé, 37000 Tours, France. Electronic address: [email protected].
- 2 University Hospital of Nancy, France.
- 3 Department of Neuroradiology, University Hospital of Tours, 2, boulevard Tonnellé, 37000 Tours, France.
- 4 Saint-Anne Hospital, Paris, France.
- 5 La Pitie-Salpetrière Hospital, Paris, France.
- 6 University Hospital of Rennes, Rennes, France.
- 7 University Hospital of Montpellier, Montpellier, France.
- 8 Bicêtre Hospital, Le Kremlin-Bicêtre, France.
- 9 University Hospital of Angers, Angers, France.
- 10 University Hospital of Bordeaux, Bordeaux, France.
- 11 Regional Hospital of Vannes, Vannes, France.
- 12 University Hospital of Nantes, Nantes, France.
- 13 University Hospital of Brest, Brest, France.
- 14 University Hospital of Lille, Lille, France.
- 15 University Hospital of Amiens, Amiens, France.
- 16 University Hospital of Lyon, Lyon, France.
- 17 University Hospital of Limoges, Limoges, France.
- 18 University Hospital of Reims, Reims, France.
- 19 Regional Hospital of Bayonne, Bayonne, France.
- 20 Foch Hospital, Suresnes, France.
- 21 Department of Biostatistics, University Hospital of Lille, Lille, France.
- PMID: 31726072
- DOI: 10.1016/j.neurad.2019.11.001
A correlation between the susceptibility vessel sign (SVS) and red thrombi has been identified in MRI. We hypothesized that the Embotrap allow better retrieving of SVS+ thrombi. The AdaptatiVe Endovascular strategy to the CloT MRI in large intracranial vessel Occlusion (VECTOR) trial is a multicenter, prospective and randomized study designed to compare a first-line strategy combining Embotrap added to contact aspiration (CA) versus CA alone in patients with SVS+ occlusions.
Keywords: Clot; MRI; Mechanical thrombectomy; Stroke.
Copyright © 2019 Elsevier Masson SAS. All rights reserved.
Publication types
- Clinical Trial Protocol
- Endovascular Procedures / methods*
- Intracranial Thrombosis / diagnostic imaging*
- Intracranial Thrombosis / surgery*
- Magnetic Resonance Imaging / methods*
- Multicenter Studies as Topic
- Prospective Studies
- Randomized Controlled Trials as Topic
- Thrombectomy / methods*
- FanNation FanNation FanNation
- Swimsuit SI Swimsuit SI Swimsuit
- Sportsbook SI Sportsbook SI Sportsbook
- Tickets SI Tickets SI Tickets
- Shop SI Shop SI Shop
- Free Agency
- What's on TV
- Racing Racing Racing
- Home Home Home
- F1 Formula 1 Formula 1
- NASCAR NASCAR NASCAR

© Michael Madrid-USA TODAY Network
Rory McIlroy Had Savage Line on How 15-Handicap Golfers Would Fare at 2024 Masters
- Author: Patrick Andres
One of the central appeals of golf, as much as any other televised sport, is that it is hard for everyone .
If you think your local course is beating you up on a particular weekend, you need only to go home and turn on your television to find courses around the world beating up on the best players on the planet. There is a sense of universality in the sport's futility.
On Saturday, one brave reporter asked Rory McIlroy to apply this logic to this weekend's windy conditions at Augusta National. Would an average, 15-handicap duffer really fare appreciably worse than the world's best?
That bubble quickly burst.
"It's hard because a 15-handicap doesn't usually get the ball in the air far enough for the wind to affect it," McIlroy said. "But they would've struggled."
Dagger from Rors. 😢 #themasters pic.twitter.com/GOPkivlKOY — Golf Digest (@GolfDigest) April 13, 2024
The question was particularly audacious because, well, McIlroy has struggled at times this tournament, as he exited Saturday's third round tied for 21st place at three over par.
The moral of the story: If ever offered the opportunity to play Augusta, check your ego at the door.
Latest News

NASCAR United Rentals Work United 500 Predictions, Picks & Odds: Phoenix

FanDuel Sportsbook Promotion for The Daytona 500: Score $150 Bonus

Daytona 500 Postponed, Creating Unprecedented Monday Doubleheader

NASCAR Daytona 500 Predictions, Picks & Odds From Daytona Int’l Speedway

Kevin Harvick Buys Ricky Bobby’s Mansion From ‘Talladega Nights’
'Race your race': How Akshay Bhatia remains focused while eyeing second TOUR win
Change Text Size
SAN ANTONIO — The leader of the Valero Texas Open says he doesn’t have all the answers. He’s growing into them.
Akshay Bhatia is a one-time PGA TOUR winner and has been a professional since 2019, but the fact remains: He is only 22 years old. Someone that young might prefer to avoid embracing the stress of leading a tournament after 54 holes, especially with a four-stroke lead. But Bhatia seems to almost thrive on it.
He has certain ways of dealing with it all. For example, on Saturday morning, after he discussed with his sports psychologist the many possibilities, good and bad, that come with playing in the last group with a lead, Bhatia took a black marker and wrote the words “Race Your Race” on his left wrist. It was a reminder for the part of him that is still young and raw.
“I’m just going at my own pace, focusing on myself, keeping the blinders right in front of me,” he said. “I looked at it all the time.”
It seemed to work. Bhatia shot 4-under 68 on a rain-softened TPC San Antonio, growing his lead to four. He made two bogeys, six birdies and a lot of new fans. He said he never let his mind wander into dark places. He relied on the lessons his mental coach, Ryan Davis of the Center for Athletic Performance Enhancement, has been trying to embed. He kept his head up, his eyes straight ahead.
“I was never calm today,” Bhatia admitted, “and it was the hardest thing to deal with. It’s just so hard. You feel so tense, and all these things in your stomach, your mind can kind of go one way. I kept to my game plan.”
Akshay Bhatia drains birdie putt at Valero
The winner of the 2023 Barracuda Championship, Bhatia has a story that many now know. He grew up in California and North Carolina. He skipped college. He wanted the dream of professional golf sooner than most. A lot of it has been hard: the travel, the emotions, the business, the grind, the belief, the faith. He’s growing and leaning into those complexities in ways his peers admire.
“We all battle,” said Brendon Todd, who played with Bhatia in the third round. “Golf is an emotional, stressful sport. That’s why we love it.”
Bhatia, Todd said, projects a quiet sense of duty — as if his acceptance of the difficulty of tournament golf strengthens him.
His conversations with Davis, by phone or on Zoom, help him find his way. He does so at his own pace. They talk about more than golf shots or winning tournaments, Bhatia said. They talk about the things a 22-year-old might not understand yet about performing under difficult conditions and learning to love that life choice regardless of whether he succeeds.
“I’ve never had an easy life growing up,” Bhatia said. “So anytime anyone sees, ‘Oh, this kid’s making a ton of money, he’s playing on the PGA TOUR, he’s won on the PGA TOUR, that’s just not it. There’s so much more to it than just golf.”
But the golf? This week, there’s been no one better at it than Bhatia.
He shot a 9-under 63 on a rugged, wind-scraped Oaks Course in round one. He followed that with a 2-under 70 to move his lead to five. After 54 holes, he ranks first in Strokes Gained: Tee to Green, second in Approach the Green, second in Putts per Green in Regulation and fifth in Strokes Gained: Around the Green. He looks untouchable. He knows he is not.
“I was talking to my psychologist last night,” Bhatia said. “Just all the stories that could happen. What if I lose this lead? What if this lead goes to 10? So many things are in your mind.”
By the end of a cooler, misty and slightly less windy Saturday afternoon in south Texas, the questions haven’t gone away. Bhatia wasn’t running from them. He was moving toward them. After his round, Bhatia spoke openly — almost enthusiastically — about the challenges he faces with one round to go. He said there was no use in pretending.
“I’m just true to myself,” he said. “I mean, I’d rather speak it to someone than not at all. I love sharing my story. I love being honest and whether I get hate for it or not, it doesn’t matter. It’s kind of who I am and who I try to be.”

COMMENTS
CHRU de Tours - La recherche médicale en NRI CHRU de Tours - La recherche médicale en NRI. Contacts Contacts. Nous contacter ... Dr Kevin JANOT. Praticien Hospitalier. Dr Fouzi BALA. Praticien Hospitalier. Service de Radiologie, Neuroradiologie Diagnostique Interventionnelle. Docteur Baptiste MOREL.
Kevin Janot practices in Tours, France. Janot and is highly rated in 3 conditions, according to our data. His top areas of expertise are Stroke, Brain Aneurysm, COVID-19, Thrombectomy, and Stent Placement. His clinical research consists of co-authoring 63 peer reviewed articles in the past 15 years.
Prenez RDV en ligne avec Dr Kevin JANOT: Radiologue, Conventionné secteur 1. Adresse : 2 Boulevard Tonnellé, 37000 Tours. ... Chef de clinique des universités - Centre Hospitalier Régional Universitaire de Tours - Tours - Service de Neuroradiologie Interventionnelle. 2019 - 2019 ...
Kevin Janot Aymeric Rouchaud Endovascular treatment is the first-line therapy for most intracranial aneurysms; however, recanalisation remains a major limitation.
M. Kevin Janot. Radiologie et imagerie médicale UFR de Médecine. Coordonnées. Mail [email protected]. Pratique Inscription Offre de formation Santé Sport Culture Contacts Plans d'accès ...
Kevin Janot. Background and Purpose: Better understanding about thrombus composition seems necessary, as treatment of acute ischemic stroke (AIS) is focus on clot chemical dissolution and ...
Affiliations 1 Hôpital Bretonneau, université François-Rabelais de Tours, centre hospitalier régional universitaire de Tours, service de neuroradiologie interventionnelle, 37000 Tours, France. Electronic address: [email protected]. 2 Centre hospitalier universitaire de Besançon, service de neurologie, 25000 Besançon, France.; 3 Hôpital Bretonneau, université François-Rabelais de ...
Zoltan Szatmary, 1, 2 Jérémy Mounier, 2 Kevin Janot, 2, 3 Jonathan Cortese, 2, 4 Claude Couquet, 2 Frédéric Chaubet, 5, 6 Ramanathan Kadirvel, 7 Sylvia M Bardet, 2 Charbel Mounayer, 1, 2 and Aymeric Rouchaud 1, 2
Kevin Janot 1 , Denis Herbreteau 2 , Aymeric Amelot 3 , Guillaume Charbonnier 4 , Fakhreddine Boustia 2 , Ana Paula Narata 2 , Basile Kerleroux 2 , ... 1 University Hospital of Tours, Neuroradiology Department, 2, boulevard Tonnellé, 37000 Tours, France. Electronic address: [email protected].
[email protected]. Extended author information available on the last page of the article / Published online: 13 June 2022. Neuroradiology (2022) 64:2363-2371.
This was a multicenter, retrospective, core lab adjudicated, cohort study of adult patients with proximal vessel occlusion, a large ischemic core volume (diffusion weighted imaging volume ≥70 mL), with pre-treatment magnetic resonance imaging perfusion, treated with MT (2015 to 2018) or medical care alone (controls; before 2015).
Kevin Janot, Service de Neuroradiologie Diagnostique et Interventionnelle, CHRU de Tours, 2 Boulevard Tonnellé, 37000 Tours, France. ... On behalf of the JENI Research Collaborative. Authors' contribution. Kevin Janot: Conceptualization, acquisition of data, and writing—original draft preparation. Guillaume Charbonnier: Acquisition of data ...
Department of Diagnostic and Interventional Neuroradiology, Bretonneau Hospital, University of Tours, Tours, France. Axel Masson, Grégoire Boulouis, Kevin Janot, Denis Herbreteau, Jean-Phlippe Cottier, Richard Bibi, Sandra Obry & Héloïse Ifergan. Department of Diagnostic Neuroradiology, Orleans Hospital Center, Orleans, France. Clara Cohen
Basile Kerleroux 1 , Kevin Janot 1 , Cyril Dargazanli 2 , Dimitri Daly-Eraya 2 , Wagih Ben-Hassen 3 , François Zhu 4 , Benjamin Gory 4 , Jean François Hak 5 , Charline Perot 6 , Lili Detraz 7 , Romain Bourcier 7 , Aymeric Rouchaud 8 , Géraud Forestier 8 , Joseph Benzakoun 3 , Gaultier Marnat 9 , Florent Gariel 9 , Pasquale Mordasini 10 ...
Kevin Janot. Diagnostic and Interventional Neuroradiology Department, University Hospital of Tours, Tours, France ... MD, MSc, Diagnostic and Interventional Neuroradiology Department, University Hospital of Tours, France, 2 Bd Tonnellé, Tours, France. Email: [email protected] Metrics and citations Metrics. Journals metrics. This article was ...
Correspondence to Dr Kevin Janot, Diagnostic and Interventional Neuroradiology, University Hospital of Tours, Tours, France; kevin.janot{at}hotmail.com Abstract In this study, we explored the relationship between histopathological changes and angiographic evolution over time in experimental aneurysms in rabbits treated with the Woven EndoBridge ...
The goal of endovascular treatment (EVT) for stroke due to Large Vessel Occlusion is to achieve recanalization of the occluded vessel as quickly and completely as possible. 1 The first studies that proved the efficacy of EVT in 2015 considered a partial recanalization (TICI 2b) at the end of the procedure, whatever the number of passes, 2-6 as a technical success.
Private Sightseeing Tours in Moscow: Check out 6 reviews and photos of Viator's Private Moscow Metro Tour
While Moscow is beautiful above-ground, it's fascinating underground. On this tour you will visit two of Moscow's most interesting underground attractions: the beautifully decorated Metro system, and the Bunker 42 anti-nuclear facility. Your private guide will tell you all about the history of these places, and answer any questions you might have. You'll see a different side of Moscow on ...
Private and Luxury in Moscow: Check out 17 reviews and photos of Viator's Private Guided Moscow Underground Palaces Metro Tour
Moscow Metro. The Moscow Metro Tour is included in most guided tours' itineraries. Opened in 1935, under Stalin's regime, the metro was not only meant to solve transport problems, but also was hailed as "a people's palace". Every station you will see during your Moscow metro tour looks like a palace room. There are bright paintings ...
Kevin Janot 1 , Grégoire Boulouis 2 , Géraud Forestier 3 , Fouzi Bala 2 , Jonathan Cortese 4 5 , Zoltán Szatmáry 5 , Sylvia M Bardet 5 , Maxime Baudouin 6 , Marie-Laure Perrin 5 , Jérémy Mounier 5 , Claude Couquet 5 , Catherine Yardin 7 , Guillaume Segonds 8 , Nicolas Dubois 8 , Alexandra Martinez 8 , Pierre-Louis Lesage 8 , Yong-Hong ...
Kevin McCarthy's Rebranding Tour. The former speaker wants to shape how history remembers him — with some clever truth-bending and big omissions. Ben Jacobs is a writer based in Washington, D ...
In a five-question session on Sunday after Woods finished his final-round 77, Woods was asked his impressions of Al-Rumayyan and if he felt the PGA Tour was any closer to a deal with him. "I don ...
Kevin McCarthy's Rebranding Tour. April 14, 2024 at 3:00 pm EDT By Taegan Goddard Leave a Comment. Politico: "Six months after his ouster as speaker of the House, McCarthy is trying to write his own history. Although still comparatively young at 59 in an era of octogenarian politicians, it's hard to imagine a world in which the first line ...
The tour will start in the UK in March, ending fittingly in the band's home state of New Jersey in mid-June. Check out their newly released music video for "Tiny Moves" if you need a Bleachers fix ...
Kevin Janot 1 , François Zhu 2 , Basile Kerleroux 3 , Grégoire Boulouis 4 , Eimad Shotar 5 , Kevin Premat 5 ... 1 Department of Neuroradiology, University Hospital of Tours, 2, boulevard Tonnellé, 37000 Tours, France. Electronic address: [email protected].
That bubble quickly burst. "It's hard because a 15-handicap doesn't usually get the ball in the air far enough for the wind to affect it," McIlroy said. "But they would've struggled." Dagger from ...
SAN ANTONIO — On his third night of owning the lead in the Valero Texas Open, Akshay Bhatia had trouble sleeping. His mind raced. He needed to settle down. He needed to set a goal. He arrived at ...
He's growing into them. Akshay Bhatia is a one-time PGA TOUR winner and has been a professional since 2019, but the fact remains: He is only 22 years old. Someone that young might prefer to ...