

2021 CPT® Evaluation and Management (E/M) Coding Changes Friday, January 08, 2021
Click here for specialty-specific resources
Resources for Physician Practices
The AMA and the Centers for Medicare & Medicaid Services have completed a major overhaul of evaluation and management (E/M) office visit documentation and coding. These landmark changes to E/M office visit coding went into effect on January 1, 2021. This page includes links to AMA resources as well as specialty-specific resources to help you as you implement these changes in your practice.
The revisions to the E/M office visit CPT® codes (99201-99215) code descriptors and documentation standards directly address the continuing problem of administrative burden for physicians in nearly every specialty.
With these changes, documentation for E/M office visits will now be centered around how physicians think and take care of patients and not on mandatory standards that encouraged copy/paste and checking boxes. Key revisions include:
- Elimination of history and physical as elements for code selection.
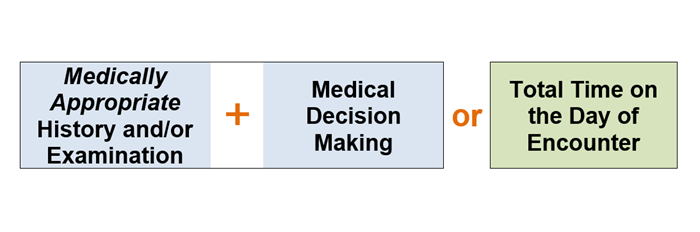
- Allow physicians to choose whether their documentation is based on Medical Decision Making (MDM) or Total Time.
- Modifications to the criteria for MDM.
- Deletion of CPT code 99201.
- Creation of a shorter prolonged services code.
AMA Resources
- CPT® (Current Procedural Terminology)
- CPT® Evaluation and Management : A historical overview and summary of the E/M coding revision for office visits.
Educational Modules
- Table illustrating the MDM revisions.
- 10-step checklist to prepare your practice for E/M office visit changes.
- Detailed PDF with the E/M code and guideline changes.
- Commercial health plans and E/M codes: Are commercial health plans required to adopt revisions to the E/M codes?
- Dec. 3, 2020: Will commercial payers, EHR vendors adopt revised E/M office-visit codes?
- Nov. 6, 2020: How 2021 E/M coding changes will reshape the physician note
- Aug. 5, 2020: E/M office-visit changes on track for 2021: What doctors must know
- Feb. 13, 2020: How 2021 E/M guidelines could ease physicians’ documentation burdens
- Nov. 19, 2019: E/M prep: Avoid these pitfalls in move to new office-visit codes
- Nov. 5, 2019: E/M prep: Your in-house practice checklist for 2021 transition
Specialty-Specific Resources:
- Addiction Medicine: Resources from ASAM
- Allergy, Asthma, & Immunology: Resources from AAAAI
- Regional Anesthesia and Pain Medicine: Article from ASRA (Dec. 7, 2020)
- Cardiology: Article from ACC (Dec. 23, 2020)
- Dermatology: Resources from AAD
- Emergency Medicine: Article from ACEP (Jan. 7, 2021)
- Endocrinology: Resources from Endocrine Society
- Family Medicine: Resources from AAFP
- Gastroenterology: Resources from AGA
- Internal Medicine: Resources from ACP
- Neurology: Resources from AAN
- Neurosurgery: Resources from CNS
- OB/GYN: Resources from ACOG
- ASCO Guide to 2021 Evaluation & Management Changes (October 2020)
- Ophthalmology: Resources from AAO
- Orthopaedic Surgery: Article from AAOS (Sep. 1, 2020)
- Otolaryngology: Article (Nov. 2020) and Resources from AAO-HNS
- Pediatrics: Resources from AAP
- Physical Medicine and Rehabilitation: Resources from AAPM&R
- Psychiatry: Resources from APA
- Rheumatology: Article from ACR (Dec. 8, 2020)
- Surgery: Resources from ACS
- Urology: Resources from AUA
Categories :
- ACS Foundation
- Diversity, Equity, and Inclusion
- ACS Archives
- Careers at ACS
- Federal Legislation
- State Legislation
- Regulatory Issues
- Get Involved
- SurgeonsPAC
- About ACS Quality Programs
- Accreditation & Verification Programs
- Data & Registries
- Standards & Staging
- Membership & Community
- Practice Management
- Professional Growth
- News & Publications
- Information for Patients and Family
- Preparing for Your Surgery
- Recovering from Your Surgery
- Jobs for Surgeons
- Become a Member
- Media Center
Our top priority is providing value to members. Your Member Services team is here to ensure you maximize your ACS member benefits, participate in College activities, and engage with your ACS colleagues. It's all here.
- Membership Benefits
- Find a Surgeon
- Find a Hospital or Facility
- Quality Programs
- Education Programs
- Member Benefits
- Coding, Billing, and Payment
- E/M Coding and Billing Res...
- Office/Outpatient E/M Visi...
Office/Outpatient E/M Visit Coding Changes
New guidelines, new codes.
Physicians and other practitioners who are paid under the Medicare Physician Fee Schedule (MPFS) bill for common office or other outpatient visits for evaluation and management (E/M) services using a set of Current Procedural Terminology (CPT)* codes that distinguish visits based on the level of complexity, site of service, and whether the patient is new (CPT codes 99201-99205) or established (CPT codes 99211-99215).
For the first time since it was introduced in 1992, the office/outpatient E/M CPT code set has been extensively revised, including the addition of a new code to report incremental time associated with prolonged office or other outpatient services.
Effective January 1, 2021, new reporting guidelines were implemented and code selection for office/outpatient E/M services is based on:
Office/Outpatient E/M Codes
See the table that highlights the changes to the office/outpatient E/M code descriptors.
Reporting Guidelines
Look at the major differences in reporting guidelines for office/outpatient E/M visits.
History and Physical Examination
See how to document H&P for office/outpatient E/M services.
Take a look at the changes in time reporting requirements for office/outpatient E/M codes.
Medical Decision Making
See both the levels and elements of medical decision making.
Regulatory History and Advocacy
Take a look at the timeline and Medicare Physician Fee Schedule rulemaking process.
Frequently Asked Questions
You may have many questions about MDM, time and how to determine the level of an office/outpatient E/M visit. Find your answers here.
Our webinars show how surgeons should use office/outpatient E/M coding guidelines to properly report such services and avoid claims denials.
Contact ACS Advocacy
If you have questions about ACS Advocacy,
please contact The ACS Advocacy team.

- For Ophthalmologists
- For Practice Management
- For Clinical Teams
- For Public & Patients
Museum of the Eye
- Latest Issue
- Back Issues (Nov. 2012 to present)
- Archive Highlights (pre Oct. 2012)
- Dr. Richard Mills' Opinions, 2002 to 2016
- Write For Us
- Corporate Webinars
- EyeNet Magazine
- / August 2020
- / New E/M Rules for Office Visits, Part 1: The Medically Relevant Patient History
New E/M Rules for Office Visits, Part 1: The Medically Relevant Patient History
- Mark Complete
Download PDF
If you have been using the office-based evaluation and management (E/M) codes, you’ll know that the history component involves an onerous series of steps—but not for much longer!
Almost gone are the days of obtaining and documenting a review of 10 or more body systems plus a past medical history, family history, and social history plus a chief complaint plus a minimum of four elements to the history of the present illness.
Big changes coming. Beginning Jan. 1, 2021, Medicare is streamlining the requirements for patient history when using office-based E/M codes 99202-99215. The history will need to be medically appropriate, which means that you need to document only information that will be medically relevant for the physician. What’s relevant? This will vary depending on the nature of the patient encounter.
This month and next month, Savvy Coder provides some typical examples seen daily in ophthalmic practices.
Get ready with technician training. While this change to the documentation requirements is great news, technicians will need some help. In addition to giving them the AAOE’s new resources (see “ Train Your Staff ”), ophthalmologists should walk their technicians through the types of information that are needed for a medically relevant history.
Who can obtain and document the history? Any part of the chief complaint or history that is recorded in the medical record by ancillary staff or the beneficiary (patient) does not need to be documented again by the billing practitioner. Instead, that person may review the information, update or supplement it as needed, and indicate in the record that he or she has done so.
Cataract Example
When patients are referred for cataract surgery, John T. McCallister, MD, asks that his technicians capture these details of their blurred vision.
- Laterality: Is the blurriness in the right eye, left eye, or both?
- Onset: Gradual or sudden?
- Duration: When did the blurred vision start?
- Effect on daily life: What activities are affected? Specifically ask about driving, working, reading, using a computer or device, watching television, and doing crafts or other activities.
- Glare or halos: Is the patient bothered by glare or halos? If so, during daytime and/or nighttime? In the rain? In certain indoor lighting conditions?
- Surgical history: Any history of refractive surgery? If so, what type of refractive surgery, when, how many times, and can we get past records?
- Injury: Any history of trauma or other injury?
- Eye disorders: Any concurrent eye disorders (e.g., blepharitis, diabetic retinopathy, dry eye syndrome, epiretinal membrane, epithelial basement membrane dystrophy, glaucoma, lattice degeneration, macular dystrophy, pseudoexfoliation syndrome, retinal tear or detachment, uveitis, etc.)?
- Medications: Taking, or have previously taken, any prostate or bladder medications? Any blood thinners?
- Family history: Any family members with eye issues?
- Allergies: Any medication allergies? Latex allergies?
- Anesthesia: Any adverse reactions to anesthesia?
- Noncovered services: What has the patient heard regarding premium IOLs and femtosecond lasers?
Dr. McCallister is a comprehensive ophthalmologist at Northern Virginia Ophthalmology Associates, which has offices near Alexandria and D.C.
Cornea Example
There are many potential indications for a corneal transplant, such as scarring, endothelial failure, dystrophy, infection, and trauma. That said, David B. Glasser, MD, considers the following as medically relevant:
- Chief complaint: What is the primary problem for which you seek consultation and possible surgery? What are the vision problems? Describe any pain or discomfort.
- Laterality: Right eye, left eye, or both? If both, which is worse?
- Duration: When did it start/how long has it been going on?
- Cause: Do you think anything in particular caused it?
- Onset: Did it come on suddenly or gradually?
- Stability: Is it getting better or worse or has it been stable? If stable, for how long has it been stable?
- Associations: Does anything in particular make the symptoms better or worse?
- Effect on daily life: What activities does it affect? Driving, reading, any specifics?
- Surgical history: Any past eye surgery? What was the surgery and when did it take place?
- Medications: Any systemic or topical medications?
Dr. Glasser is the Academy Secretary for Federal Affairs.
Glaucoma Example
Under the new rules, Emily P. Jones, MD, will be asking her technicians to document the following elements for a typical glaucoma patient:
- Surgical history: Any history of prior eye surgeries?
- Family history: Is there a strong family history of glaucoma with glaucoma surgeries or vision loss at an early age?
- Medical history: Examples of pertinent histories include:
- A stroke resulting in homonymous visual field defects.
- A history of poorly controlled diabetes with renal disease, limb amputations, hospitalizations.
- A distant history of trauma to one eye.
- Medications: Examples of pertinent details include:
- Any glaucoma medications that a patient took in the past but did not tolerate or did not respond to?
- A history of asthma with use of inhalers that would make the patient a poor candidate for beta-blocker drops?
- Long-term use of oral or inhaled steroids?
- A history of exudative macular degeneration with intravitreal Avastin injections (which can lead to very elevated eye pressure).
Dr. Jones is a glaucoma specialist at the Devers Eye Center in Portland, Oregon.
Pediatric Example
Suppose a patient is referred by his pediatrician to your practice for strabismus?
Robert S. Gold, MD, FAAP, would want to make sure that the following information is documented in the patient’s record:
- Direction of misalignment: In, out, up, or down?
- Duration: Days, months, or years?
- Constant or intermittent strabismus?
- Double vision?
- Is it better or worse at certain times of day?
- Family history of strabismus/amblyopia?
- Eye history: Used glasses, patching, and/or undergone surgery?
- Pertinent information from past history, medical history, neurologic history, and genetic history (syndromes).
And what if you’re examining an adult strabismus patient? In that case, Dr. Gold would want the technician to also document any history of diabetes, hypertension, vascular problems, trauma, neurologic issues, and medications.
Dr. Gold is a pediatric ophthalmologist at Eye Physicians of Central Florida, with offices in the Orlando metropolitan area.
The Eye Visit Codes
What about the history component for Eye visit codes 92002–92014? Whether the patient is new or established, and whether the exam is limited or comprehensive, the history documentation requirements for Eye visit codes will be the same in 2021 as they were in 2020.
Increased E/M Payments
Payments for office-based E/M codes—but not for Eye visit codes—are slated for a “significant” increase on Jan. 1, 2021. The Centers for Medicare & Medicaid Services (CMS) will announce the size of those increases in November, when it publishes the 2021 Medicare Physician Fee Schedule. Unfortunately, unless Congress intervenes to amend CMS’ budget-neutrality mandate, these increases in E/M payments could result in cuts to other codes (see this month’s Academy Notebook ).
Further Reading
New E/M Rules for Office Visits, Part 2: How to Document the Retina Exam (September 2020, EyeNet )
Taking retina histories. Plus the nonoffice exam.
New E/M Rules for Office Visits, Part 3: The Medically Relevant Exam (October 2020, EyeNet )
Anterior segment and pediatric examples.
New E/M Rules for Office Visits, Part 4: Cornea and Oculofacial Exams (November 2020, EyeNet )
Cornea and oculofacial examples.
All content on the Academy’s website is protected by copyright law and the Terms of Service . This content may not be reproduced, copied, or put into any artificial intelligence program, including large language and generative AI models, without permission from the Academy.
- About the Academy
- Jobs at the Academy
- Financial Relationships with Industry
- Medical Disclaimer
- Privacy Policy
- Terms of Service
- Statement on Artificial Intelligence
- For Advertisers
- Ophthalmology Job Center
FOLLOW THE ACADEMY
Medical Professionals
Public & Patients


Are You Happy With Your Practice Collections ?
Hit enter to search or esc to close.

CY 2023 Revised Guidelines for Office Visits
Streamline legacy accounts receivable resolution.
Contact us today!
Helping Physician Groups to Stay Profitable
Don’t let your accounts receivables, stress you.
Contact our Account Receivables Specialist today!

Newly Released CY 2023 CPT Code Set
The American Medical Association (AMA) has recently released the Current Procedural Terminology (CPT) code set for 2023, which contains updates that aim to reduce the medical coding burden for evaluation and management (E/M) visits. In this article, out of all Evaluation and Management (E/M) guidelines, we will be focussing on revised guidelines for office visits. It includes defining, new and established patients; initial and subsequent services; and services reported separately. Let’s understand the basic classification of Evaluation and Management (E/M) services before discussing revised guidelines for office visits.
Classification of Evaluation and Management (E/M) Services
The E/M section is divided into broad categories, such as office visits, hospital inpatient or observation care visits, and consultations. Most of the categories are further divided into two or more subcategories of E/M services. For example, there are two subcategories of office visits (new patient and established patient) and there are two subcategories of hospital inpatient and observation care visits (initial and subsequent). The subcategories of E/M services are further classified into levels of E/M services that are identified by specific codes.
The basic format of codes with levels of E/M services based on medical decision-making (MDM) or time is the same. First, a unique code number is listed. Second, the place and/or type of service is specified (e.g., office or other outpatient visits). Third, the content of the service is defined. Fourth, time is specified. The place of service and service type is defined by the location where the face-to-face encounter with the patient and/or family/caregiver occurs. For example, service provided to a nursing facility resident brought to the office is reported with an office or other outpatient code.
New and Established Patients
Solely for the purposes of distinguishing between new and established patients, professional services are those face-to-face services rendered by physicians and other qualified healthcare professionals who may report evaluation and management services.
New Patient: A new patient is one who has not received any professional services from the physician or other qualified health care professional or another physician or other qualified health care professional of the exact same specialty and subspecialty who belongs to the same group practice, within the past three years.
Established Patient: An established patient is one who has received professional services from the physician or other qualified health care professional or another physician or other qualified health care professional of the exact same specialty and subspecialty who belongs to the same group practice, within the past three years.
In the instance where a physician or other qualified health care professional is on call for or covering for another physician or other qualified health care professional, the patient’s encounter will be classified as it would have been by the physician or other qualified health care professional who is not available. When advanced practice nurses and physician assistants are working with physicians, they are considered as working in the exact same specialty and subspecialty as the physician. Note that, no distinction is made between new and established patients in the emergency department. E/M services in the emergency department category may be reported for any new or established patient who presents for treatment in the emergency department.
Initial and Subsequent Services
Some categories apply to both new and established patients (e.g., hospital inpatient or observation care). These categories differentiate services by whether the service is the initial service or a subsequent service. For the purpose of distinguishing between initial or subsequent visits, professional services are those face-to-face services rendered by physicians and other qualified healthcare professionals who may report evaluation and management services.
Initial Service: An initial service is when the patient has not received any professional services from the physician or other qualified health care professional or another physician or other qualified health care professional of the exact same specialty and subspecialty who belongs to the same group practice, during the inpatient, observation, or nursing facility admission and stays.
Subsequent Service: A subsequent service is when the patient has received professional service(s) from the physician or other qualified health care professional or another physician or other qualified health care professional of the exact same specialty and subspecialty who belongs to the same group practice, during the admission and stays.
In the instance when a physician or other qualified health care professional is on call for or covering for another physician or other qualified health care professional, the patient’s encounter will be classified as it would have been by the physician or other qualified health care professional who is not available. When advanced practice nurses and physician assistants are working with physicians, they are considered as working in the exact same specialty and subspecialty as the physician. For reporting hospital inpatient or observation care services, a stay that includes a transition from observation to inpatient is a single stay. For reporting nursing facility services, a stay that includes transition(s) between skilled nursing facility and nursing facility level of care is the same stay.
Services Reported Separately
The ordering and actual performance and/or interpretation of diagnostic tests/studies during a patient encounter are not included in determining the levels of E/M services when the professional interpretation of those tests/studies is reported separately by the physician or other qualified health care professional reporting the E/M service. Tests that do not require separate interpretation (e.g., tests that are results only) and are analyzed as part of MDM do not count as an independent interpretation, but may be counted as ordered or reviewed for selecting an MDM level.
The performance of diagnostic tests/studies for which specific CPT codes are available may be reported separately, in addition to the appropriate E/M code. The interpretation of the results of diagnostic tests/studies (i.e., professional component) with the preparation of a separate distinctly identifiable signed written report may also be reported separately, using the appropriate CPT code and, if required, with modifier 26 appended.
The physician or other qualified health care professional may need to indicate that on the day a procedure or service identified by a CPT code was performed, the patient’s condition required a significant separately identifiable E/M service. The E/M service may be caused or prompted by the symptoms or condition for which the procedure and/or service was provided. This circumstance may be reported by adding modifier 25 to the appropriate level of E/M service. As such, different diagnoses are not required for reporting of the procedure and the E/M services on the same date.
To discuss revised guidelines for office visits, we referred to ‘ 2023 CPT E/M descriptors and guidelines published by American Medical Association (AMA). Note that these guidelines are to be used by the reporting physician or other qualified healthcare professional to select the appropriate level of service. These guidelines do not establish documentation requirements or standards of care. The main purpose of documentation is to support the care of the patient by current and future healthcare team(s). These guidelines are for services that require a face-to-face encounter with the patient and/or family/caregiver.
We hope this article has given you a good understanding of revised guidelines for office visits, you can visit the AMA reference link for a detailed understanding. If you are busy in patient care and can’t keep track of E/M coding updates, we can assist you. Medical Billers and Coders (MBC) is a leading medical billing company providing complete revenue cycle services .
We take complete ownership of billing services and ensure accurate payment collection for delivered services. To know more about our medical billing and coding services, email us at: [email protected] or call us at: 888-357-3226 .
CPT Copyright 2022: American Medical Association
Looking for a Medical Billing Quote?
Are you looking for more than one billing quotes?
Are you looking for more than one billing quotes ?
Would You like to Increase Your Collections?

Request a Call Back
An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
CMS Newsroom
Search cms.gov.
- Physician Fee Schedule
- Local Coverage Determination
- Medically Unlikely Edits
Evaluation & Management Visits
This page contains guidance regarding documentation and payment under the Medicare Physician Fee Schedule for evaluation and management (E/M) visits.
- Physician Fee Schedule (PFS) Payment for Office/Outpatient Evaluation and Management (E/M) Visits – Fact Sheet (PDF) - Updated 01/14/2021
- Evaluation and Management (E/M) Visit Frequently Asked Questions (FAQs) (PDF)
- Evaluation and Management Services MLN Publication
- FAQs: Split (or Shared) Visits and Critical Care Services (PDF) : Posted 4/7/2022

Stanford Cancer Institute
Search stanford cancer institute.
- Clinical Trials

The Stanford Cancer Institute (SCI) Clinical Trials Office (CTO) provides regulatory, administrative, research support, budget, and educational services to SCI investigators conducting cancer clinical trials.
- Clinical Trials Office
Our Services
The Stanford Cancer Institute Clinical Trials Office facilitates translational research through extensive support services.

Clinical Research Staff Oversight
SCI-CTO provides central coordination and oversight of clinical staff to ensure consistent processes, regulatory compliance, and improved efficiencies.
Research Services
SCI-CTO provides a centralized resource that assists clinical researchers with scientific review, regulatory management, pre-award financial management, quality assurance, training and education, data collection, and monitoring.

Training and Education
SCI-CTO provides staff orientation training and ongoing education, supports investigator training, and manages the development and maintenance of Standard Operating Procedures (SOPs), Practice Guidelines, and study management tools.
Monitoring Services
Quality control monitoring of SCI clinical trials are conducted by SCI-CTO quality monitors or third-party monitors. Our external quality monitoring visits are primarily conducted remotely.

Scientific Review Committee
The SCI oversees the conduct of research studies investigated by SCI investigators, ensuring the research is of scientific merit, high quality, reliable, and verifiable.
Faculty and Staff Services
Staff and faculty members can find SCI-CTO's internal secure documents accessible through our intranet.

- Patient Care
- Health Equity
- Shared Resources
Stanford Medicine
Health care.

©2024 Stanford Medicine

IMAGES
VIDEO
COMMENTS
Peter Hollmann, MD Christopher Jagmin, MD Barbara Levy, MD. History of E/M Workgroup. E/M Revisions for 2021: Office and Other Outpatient Services. New Patient (99201-99205) Established Patient (99211-99215) Medical Decision Making (MDM) Time. Prolonged Services.
The American Medical Association (AMA) has established new coding and documentation guidelines for office visit/outpatient evaluation and management (E/M) services, effective Jan. 1, 2021.
The AMA made many revisions to the E/M guidelines as part of the 2021 update for office and outpatient visit codes. The 2023 guidelines required additional updates to incorporate the latest code changes. In some cases, the guidelines remained the same or changed to apply the 2021 guideline updates to additional E/M categories.
For example, 99202 Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and straightforward medical decision making … has a current time range of 15-29 minutes. Beginning Jan. 1, 2024, the provider must meet or exceed 15 minutes of total service time before you can bill this code by time.
The new rules for coding evaluation and management (E/M) office visits are a big improvement but still a lot to digest. 1, 2 To ease the transition, previous FPM articles have laid out the new ...
CMS adopted these new E/M coding guidelines. As a result of the changes to medical decision making and time-based coding, the RUC revised the 2021 relative value units (RVUs) for office visit E/M ...
Aug. 5, 2020: E/M office-visit changes on track for 2021: What doctors must know; Feb. 13, 2020: How 2021 E/M guidelines could ease physicians' documentation burdens ; Nov. 19, 2019: E/M prep: Avoid these pitfalls in move to new office-visit codes; Nov. 5, 2019: E/M prep: Your in-house practice checklist for 2021 transition
• The revisions to the E/M documentation guidelines are only applicable to the office/outpatient new patient and established patient visit E/M codes (99202-99215). For all other E/M services performed, such as consultations, inpatient E/M, observation E/M and critical care , services will continue to be governed by the existing E/M
You should continue to use the CMS 1995 and/or 1997 Documentation Guidelines for Evaluation and Management Services for all E/M categories except office/other outpatient services (99202-99215). Use the 2021 CPT® documentation guidelines for office visits (99202-99215), only. 3. Do you have to document both total time and medical decision ...
Split (or Shared) E/M Services. CPT Codes 99202-99205, 99212-99215, 99221-99223, 99231-99239, 99281-99285, & 99291-99292. A split (or shared) service is an E/M visit where both a physician and NPP in the same group each personally perform part of a visit that each 1 could otherwise bill if provided by only 1 of them.
Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and low level of medical decision making. When using time for code selection, 30-44 minutes of total time is spent on the date of the encounter. 99204. Office or other outpatient visit for the ...
New Guidelines, New Codes. Physicians and other practitioners who are paid under the Medicare Physician Fee Schedule (MPFS) bill for common office or other outpatient visits for evaluation and management (E/M) services using a set of Current Procedural Terminology (CPT)* codes that distinguish visits based on the level of complexity, site of service, and whether the patient is new (CPT codes ...
To discuss revised guidelines for office visits, we referred to '2023 CPT E/M descriptors and guidelines published by American Medical Association (AMA). Note that these guidelines are to be used by the reporting physician or other qualified healthcare professional to select the appropriate level of service.
Whether the patient is new or established, and whether the exam is limited or comprehensive, the history documentation requirements for Eye visit codes will be the same in 2021 as they were in 2020. Increased E/M Payments. Payments for office-based E/M codes—but not for Eye visit codes—are slated for a "significant" increase on Jan. 1 ...
The new 2021 guidelines for office visits (99202-99215) do not require a level of ROS to meet a coding requirement. It will be performed based on what the provider determines to be medically appropriate for the encounter. Regarding who can document elements of the E/M, this information was included in the 2019 Medicare Physician Fee Schedule ...
The national average for family physicians' usage of the level 4 code (99214) is slowly increasing and is approaching 50% of established patient office visits (it's now above 50% for our Medicare ...
The American Medical Association (AMA) has recently released the Current Procedural Terminology (CPT) code set for 2023, which contains updates that aim to reduce the medical coding burden for evaluation and management (E/M) visits. In this article, out of all Evaluation and Management (E/M) guidelines, we will be focussing on revised ...
Evaluation & Management Visits. This page contains guidance regarding documentation and payment under the Medicare Physician Fee Schedule for evaluation and management (E/M) visits. Physician Fee Schedule (PFS) Payment for Office/Outpatient Evaluation and Management (E/M) Visits - Fact Sheet (PDF) - Updated 01/14/2021.
Coding Level 4 Ofice Visits Using the New E/M Guidelines. Determining whether the visit you've just finished should be coded as a level 4 could be as simple as asking yourself three questions ...
The Stanford Cancer Institute (SCI) Clinical Trials Office (CTO) provides regulatory, administrative, research support, budget, and educational services to SCI investigators conducting cancer clinical trials. ... Our external quality monitoring visits are primarily conducted remotely. SCI-CTO PRISM Guidelines PRISM Monitoring Training Session ...
Care components. Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or examination and low level of medical decision making. When using time for code selection, 30-44 minutes of total time is spent on the date of the encounter.