

Meet the New CPT Codes to Report e-Visits in 2020
by Natalie Tornese | Published on Feb 10, 2020 | Medical Coding

Digital E/M services allow US health systems to care for patients remotely. Several factors are fuelling the growth of remote patient monitoring and telemedicine, such as the aging population, patient demand, looming provider shortage, increase in chronic conditions, and policies to promote reimbursement for e-visits. Recognizing the expanding role of telemedicine in the U.S., the American Medical Association introduced six new e-visit CPT codes, which came into effect from Jan. 1, 2020. Providers can use physician billing services to accurately report these new codes for online digital evaluation services and get optimal reimbursement.
Six new CPT Codes for e-Visits
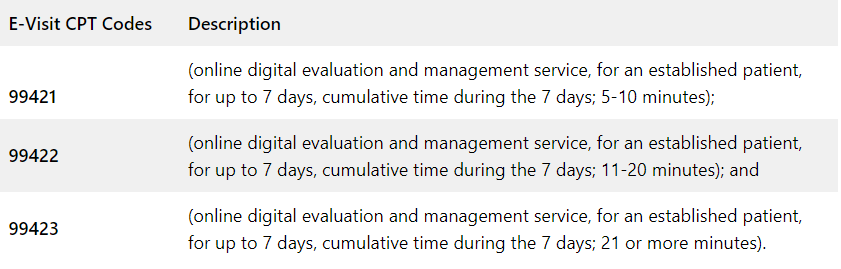
The 2020 Medicare Physician Fee Schedule (MPFS) describes e-Visits as non-face-to-face “patient-initiated digital communications that require a clinical decision that otherwise typically would have been provided in the office.” The six new codes for e-Visits are:
- 99421 , 99422 , and 99423 to report patient-initiated digital communication provided by a physician or other qualified healthcare professional
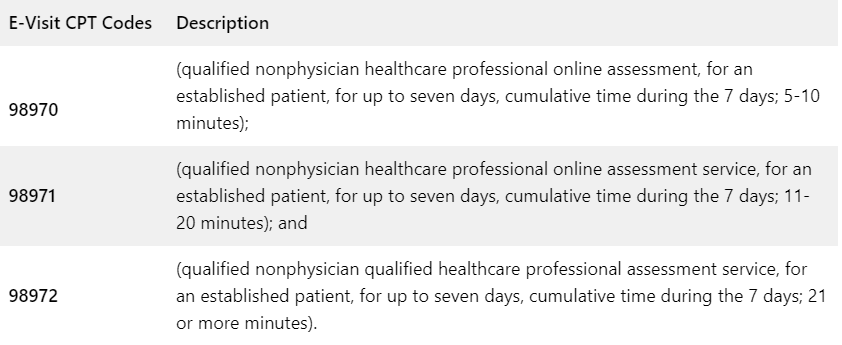
- 98970 , 98971 , and 98972 for digital communications with a non-physician healthcare professionals
“The new CPT codes will promote the integration of these home-based services that can be a significant part of a digital solution for expanding access to health care, preventing and managing chronic disease, and overcoming geographic and socioeconomic barriers to care,” said AMA President Patrice A. Harris, MD, MA.
Two New Codes for Self-measured Blood Pressure Monitoring (SMBP)
In addition to the above six codes, there are two new codes for SMBP in 2020.
High blood pressure or hypertension is a common problem that increases risk of heart attack and stroke risk. The goal of treatment is to bring the blood pressure level down to a healthy range (130/80 millimeters of mercury [mm Hg] or lower). SMBP can support this goal.
SMBP involves a patient’s regular use of personal blood pressure monitoring devices to assess and record blood pressure across different points in time outside of a clinical, community, or public setting, typically at home (www.cdc.gov). Monitoring blood pressure at home can help people newly diagnosed with high blood pressure or those struggling to reach their target. Harvard Health reported on research which showed that a period of home blood pressure monitoring – one week per month – was sufficient to guide people to better blood pressure control.
According to AMA Vice President of Health Outcomes Michael Rakotz, MD, SMBP provides clinically useful information to help physicians:
- more accurately diagnose and determine the need for treatment in people suspected of having uncontrolled high blood pressure based on routine office BP measurements
- compared to BPs obtained during a single office visit, SMBP provides more BPs over a longer period of time, which represents a more accurate picture of a patient’s BP
- Out-of-office measurements can better predict future cardiovascular risk than measurements taken in the office
In 2020, physician practices that educate patients to perform home blood-pressure monitoring can submit claims using two CPT codes associated with clinical services:
- 99473 Self-measured blood pressure using a device validated for clinical accuracy; patient education/training and device calibration
- 99474 Separate self-measurements of two readings one minute apart, twice daily over a 30-day period (minimum of 12 readings), collection of data reported by the patient and/or caregiver to the physician or other qualified health care professional, with report of average systolic and diastolic pressures and subsequent communication of a treatment plan to the patient
These codes will enable physicians to better diagnose and manage hypertension as well as help patients to play an active role in their care while at home.
Reporting 99421, 99422 and 99423 – Points to Note
- Codes 99421-99423 are for physicians and other qualified healthcare professionals (QHP)
- These codes can be used to report non-face-to-face patient initiated digital communications that require a clinical decision
- CPT code selection should be based on the time involved
- Communication between the patient and provider should be performed through HIPAA-compliant platforms (electronic health record portal or secure email)
- These codes should not be used for non evaluative electronic communication of test results
There are also guidelines on when not to bill online services when the patient is provided another service around the same time as online communication:
- Digital E/M followed by other E/M : If the patient initiates an online E/M service and then presents for a separately reported E/M within seven days, the online E/M work should be included in the separately reported E/M.
- E/M followed by online service : If the patient presents for an E/M and then initiates an online inquiry for the same problem or a related one within seven days, the online service should not be reported.
- Online E/M during post-op period : During the postoperative period, online inquiries related to a surgery should not be reported separately.
Hospitals and health systems are looking to expand care to the home or other non-traditional settings and work with patients and other care providers to improve outcomes and reduce costs. Providers who implement digital health care services can rely on medical billing outsourcing services to report the new codes correctly and get paid.

Holding a CPC certification from the American Academy of Professional Coders (AAPC), Natalie is a seasoned professional actively managing medical billing, medical coding, verification, and authorization services at OSI.
More from This Author
Facebook Twitter LinkedIn
Related Posts
- Navigating Colonoscopy Billing and Coding Guidelines
- Why Outsourcing Preauths and Insurance Verification Is a Game Changer
- Overview of the Dental Billing Process
- Appointment Scheduling
- Dental Insurance Verification
- Healthcare News
- Insurance Credentialing
- Insurance Verification and Authorizations
- Medical Billing
- Medical Coding
- Medical Outsourcing
- Specialty Billing
- Specialty Coding
- Medical Billing Services
- Podiatry Billing Services
- Pain Management Billing Services
- ASC - Surgery Center Billing Services
- Physical Therapy Billing Services

- 5 Star Billing
- Billing Software
- 1st Providers Choice
- eClinicalWorks
- Greenway Prime Suite
- IMS - Intelligent Medical Software
- NextGen -Meditouch
- Office Ally
- Practice Fusion
- SIS - Surgical Information Systems
Best Guide to E-Visit Documentation, Coding, and Billing

Categories: Coding , CPT Codes , Medical Billing
Tags: billing code , coding , cpt code tips , e visits in healthcare , medical billing
The American Academy of Family Physicians (AAFP) encourages safe, secure online interactions between physicians and patients, such as electronic visits or “virtual e-visits.” In non-emergency situations, e-visits can substitute for office visits with primary care providers. It is a fast and easy online procedure for patients to receive a diagnosis and treatment plan.
This article will give you the best guide to e-visit documentation, coding, and billing.
What Should Providers Know About E-visits?
An encounter must meet the following criteria to be considered an e-visit:
- The practice must have a well-established relationship with its patients.
- E-visits require patient consent and a communication request.
- The patient must initiate non-face-to-face electronic communication. For example, patient portal systems.
- Patients must not have seen an office visit to a physician or therapist for the same clinical concern in the past seven days.
- It is only possible to report e-visits every seven days.
- An e-visit is not the same as typical therapy sessions.
For e-visits, the following documentation requirements are needed:
- The main complaint with all evaluation and management services (E/M).
- The specifics of treatments, assessment of diagnoses or symptoms, evaluation, and conversation.
- An official patient consent record is backed up by a signature and captured in the clinical note. Moreover, e-visit software platforms accept scanned copies of signed consents. Some systems allow electronic signatures.
- The total time recorded over the seven days supporting the billable service.
List of Current Procedural Terminology (CPT) Codes That Require Providers to Follow Policies Set by Payers
The codes for online digital evaluation services (e-visits) used by doctors are complex. Below are the codes used:
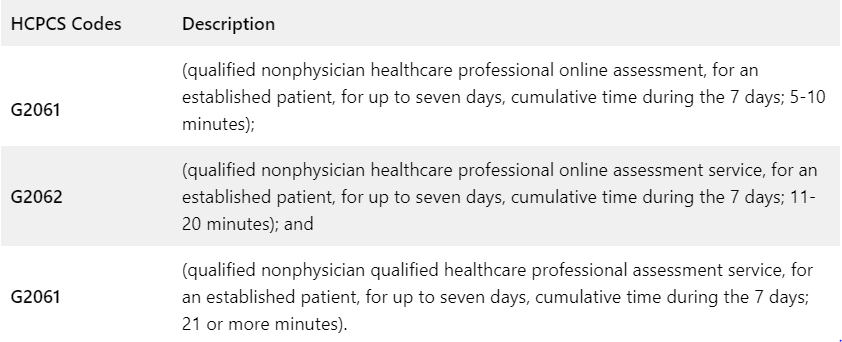
Medicare uses the following HCPCS codes and descriptors for qualified non-physician professionals for its online digital evaluation service (e-visit):
Private payers and workers’ compensation are using the following online digital evaluation service (e-visit) CPT codes and descriptors:
Do’s and Don’ts in Billing E-Visits
When the following conditions are met, you can bill an e-visit:
- The provider establishes a relationship with the patient.
- Response time by the provider is longer than five minutes.
- A provider responds through the patient portal to a message initiated by the patient.
- A visit meets the 2021 E/M guidelines.
- It has been seven days since the clinician last saw the patient.
- There is no global period for the same or similar condition for the patient.
- In this case, the provider is making a clinical decision that would normally be performed in the office (e.g., medication dose adjustment, ordering a test, or prescribing a new medication).
- A patient has consented to the e-visit and understands that he may be billed.
- For online digital E/M services, the service period includes all related work done within seven days by the reporting individual and other registered healthcare providers (RHPs) in the same group practice.
- The 7-day period begins when the reporting provider reviews the patient’s inquiry personally for the first time.
- A new/unrelated problem from the patient arises within seven days of the previous E/M visit for a different issue.
Do not bill an E-visit in the following situations:
- During the 7-day period, the provider may bill for other separately reported services (such as care management, INR monitoring, remote monitoring, etc.)
- The same or similar condition was billed to the patient for an e-visit within the past 7 days.
- The patient inquires about a surgical procedure that happens during the surgery’s postoperative period (global).
- Providers are simply disseminating results, processing medication requests, or scheduling appointments (for billing, E/M services must be performed).
- A separate face-to-face E/M service (either in person or via telehealth) happens (included in the E/M) during the 7-day period of the e-visit.
- Besides clinical staff time, only provider time can be included.
The AAFP published an algorithm in response to the growing number of virtual visits. It was developed by James Dom Dera, MD, FAAFP, to determine which code should be used for virtual services.
Tap Into Our Expertise
At 5 Star Billing Billing Services Inc , we offer the highest level of performance for high-quality medical billing and coding. Save your money by outsourcing to a professional billing service.
Schedule a call with our experts today!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
- Phone: 1-480-999-0180
- Terms of Use
- Privacy Policy
- Copyright Notice
- © 2024 5 Star Billing Services, Inc.
- AGA Journals
- AGA University
- AGA Research Foundation
- AGA Community
- AGA Job Board
- Create Account

Clinical Guidance
Our clinical guidelines and updates help you make the best evidence-based decisions for your patients.
- Library AGA’s guidelines, practice updates and care pathways in one place.
- Guideline Toolkits Comprehensive resources for managing diseases – Crohn’s disease now available.

Journals & Publications
Latest research and ideas from the GI field.
- Gastroenterology The premier journal in GI.
- Clinical Gastroenterology and Hepatology (CGH) The go-to resource in clinical GI.
- Cellular and Molecular Gastroenterology and Hepatology (CMGH) Impactful digestive biology research.
- Techniques and Innovations in Gastrointestinal Endoscopy (TIGE) Cutting-edge advances in GI endoscopy.
- Gastro Hep Advances Open access GI and hepatology journal.
- GI & Hepatology News AGA’s official newspaper.
- The New Gastroenterologist Insights for fellows and early career GIs.

Meetings & Learning
Earn CME, MOC and improve your skills.
- AGA University Your hub for the best in GI education – AGA Postgraduate Course, Tech Summit and more.
- Digestive Disease Week® The most prestigious GI meeting.
- Crohn's & Colitis Congress® The premier meeting on IBD.
- Maintenance of Certification Resources for maintaining certification.
- DDSEP® The leading self-assessment tool for GI.
- Inside Scope Podcast An AGA podcast with bite-sized education.

More than 16,000 professionals worldwide call AGA their professional home.
- Join AGA Join our diverse mix of professionals.
- Renew Membership Continue to receive exclusive benefits and discounts.
- Benefits Unrivaled by any other GI organization.
- Membership Directory Contact other AGA members.
- Recognition Awards We honor our esteemed members.
- Initiatives & Programs Advancing the science and practice of GI.
- Get Involved with AGA Help us achieve a world free from digestive diseases.
- Advocacy & AGA PAC Advancing public policies that support gastroenterology.

Practice Resources
Tools to maximize efficiency and help you deliver high-quality care.
- Practice Tools Cutting-edge resources to improve your patient care.
- New Technology & Techniques The latest innovations in GI.
- Quality & Performance Measures Support to meet reporting requirements.
- Reimbursement Tools to understand policies and advocate for reimbursement.
- GI Patient Center By specialists, for patients.

Research & Awards
Funding opportunities and other initiatives advancing discovery.
- Research Awards More than $2 million in annual research funding.
- Registries & Studies Data to support new techs and treatments.
- Gut Microbiome One of GI’s most promising areas of research.
- AGA Research Foundation Funding the future of gastroenterology.


Fellows & Early Career
Resources designed for early career gastroenterologists.
- Resources Resources for every stage of your career.
- Fellowship Match Information for programs and candidates.
- AGA GTE® The first training exam for GI programs and fellows.
- Mentoring Connect with prospective mentors.
- Job Board Find your next opportunity.
Home > Practice Resources > Reimbursement > Coding > Coding and coverage for telehealth and eVisits during the COVID-19 crisis
Coding and coverage for telehealth during COVID-19
Resources and guidance to help GI practices navigate new coding rules to ensure maximum reimbursement for telehealth/eVisit services.
View additional COVID-19 resources here.
Featured COVID-19 coding resources
- Telehealth and virtual services coding guide (joint society) June 10, 2020
- Telehealth virtual physical exam tips (joint society) June 10, 2020
- AGA guide: Commercial telehealth coding policies April 6, 2020
Top five things gastroenterologists should know about telehealth
The following guide was developed jointly by AGA, AASLD, ACG and ASGE.
During the COVID-19 health emergency, CMS expanded access to telemedicine services, increasing payment for telephone evaluation and management (E/M) codes 99441-99443 to the level of office/outpatient E/M codes 99212-99214 ($46-$110). Previous rules expanded telehealth for all Medicare beneficiaries — not just those that have novel coronavirus — for the duration of the COVID-19 PHE, expanded payments for telehealth services to a variety of settings in addition to existing coverage for originating sites including physician offices, skilled nursing facilities and hospitals, allowed reporting for new patients was well as existing patients, and allowed two-way, real-time audio/visual telehealth services to be paid under the Medicare Physician Fee Schedule at the same amount as in-person services.
- Effective retroactively from March 1, 2020, national level payment for telephone (audio-only) E/M codes 99441-99443 will increase from $15, $31 and $39 respectively to $46, $56 and $110 to match office/outpatient E/M code payments for 99212-99214 (New in Medicare’s April 30 COVID-19 interim final rule with comment period (IRC)). You must report 99441-99443 with modifier 95 and place of service (POS) where the visit would have taken place in person prior to the public health emergency (e.g., 11-Office, 22-Hospital Outpatient, 23-ASC) in order to get the higher rates. Claims without modifier 95 will be paid at the lower rates.
- E/M level selection for telehealth (real-time audio/visual) can be based on medical decision making or time and CMS has temporarily removed any requirements regarding documentation of medical history and/or physical exam in the medical record during the COVID-19 crisis.
- Most telehealth services can be provided to both new and established patients, including 99201-99215 and 99441-99443.
- Clinicians can provide remote patient monitoring services to patients with acute and chronic conditions and can be provided for patients with only one disease.
- Physicians can supervise their clinical staff using virtual technologies when appropriate, instead of requiring in-person presence.
Hospitals and a range of clinicians, including doctors, nurse practitioners, clinical psychologists, nutrition professionals, and licensed social workers may now provide telehealth. As part of COVID-19 emergency declarations, many governors have relaxed licensure and other state telehealth requirements so please contact your state board of medicine or department of health for up-to-the minute information.
Medicare will allow audio-only telephone E/M visits to be reported as telehealth, but they must be reported with the telephone E/M codes 99441-99443. Only two-way, real-time audio/visual E/M visits can be reported using codes 99201-99215.
In addition to traditional telehealth platforms, during the PHE CMS will allow apps like FaceTime and Skype as acceptable platforms. Telehealth, both audio-only and interactive audio and video, can be provided for any reason, regardless of whether the telehealth service is related to the diagnosis and treatment of health conditions related to COVID-19. Penalties will not be imposed on physicians using telehealth in the event of noncompliance with the regulatory requirements under the Health Insurance Portability and Accountability Act (HIPAA) during the PHE.
Standard Medicare copays and deductibles still apply to telemedicine visits, but there’s flexibility. During the coronavirus emergency, health providers will be allowed to waive or reduce cost-sharing* for telehealth visits. However, beneficiaries are still liable for cost-sharing for these services in instances where the practitioner does not waive cost-sharing. Practitioners should educate beneficiaries on any applicable cost-sharing.
*The share of costs covered by your insurance that you pay out of your own pocket. This term generally includes deductibles, coinsurance, and copayments, or similar charges, but it doesn’t include premiums, balance billing amounts for non-network providers or the cost of non-covered services.
Source: www.healthcare.gov/glossary/cost-sharing/
Below is a listing of common CPT codes and Medicare coverage for telemedicine services.
Telehealth visits
Medicare telehealth services include office visits and consultations, among other services, provided by an eligible provider using an interactive two-way telecommunications system with real-time audio and video or audio-only telephone. Clinicians can report telehealth visits for both new and established patients on any real-time, non-public communication platform, such as FaceTime and Skype, and sets payment the same as in-person E/M visits during the COVID-19 PHE (see FAQs above).
E/M level selection can be based on medical decision making (MDM) or typical time listed in the CPT code description and CMS has temporarily removed any requirements regarding documentation of medical history and/or physical exam in the medical record during the COVID-19 crisis.
Select the appropriate code (99201-99215) and use the place of service (POS) that would have been reported had the service been furnished in person (e.g., 11-Office, 22-Hospital Outpatient, 23-Ambulatory Surgery Center). This will allow Medicare to pay for the service at the same rate that would have been paid if the service was furnished in person based on the provider’s location (i.e., facility or non-facility). Providers must also append telehealth modifier 95 to claim lines to identify that the service was furnished via telehealth. Providers who continue to use the general telehealth POS 02 code will be paid at the “facility” rate.
E/M Values and National Payments
Below are a list of codes and their physician work Medicare relative value units (RVUs) and approximate National office-based payment. E/M code levels must be assigned based on current Medicare E/M coding guidelines and rules.
*A list of all available codes for telehealth services can be found on the CMS website .
Telephone evaluation and management service
CPT codes to describe telephone E/M are time-based. Effective March 1, 2020, payment for telephone E/M code 99441-99443 are equivalent to 99212-99214 and can be used for new or established patient during the PHE. Use modifier 95 and place of service (POS) where the visit would have taken place in person prior to the public health emergency (e.g., 11-Office, 22-Hospital Outpatient, 23-ASC). Check if your commercial payers pay for these services before reporting the codes for non-Medicare beneficiaries.
- CPT Code 99441 – Telephone evaluation and management service by a physician or other qualified health care professional who may report evaluation and management services provided to an established patient, parent, or guardian not originating from a related E/M service provided within the previous 7 days nor leading to an E/M service or procedure within the next 24 hours or soonest available appointment; 5-10 minutes of medical discussion [$46]
- CPT Code 99442 – 11-20 minutes of medical discussion [$76]
- CPT Code 99443 – 21-30 minutes of medical discussion [$110]
e-Consultations
e-Consultations are interprofessional telephone, internet or EHR provider-to-provider consultations. Code selection is time-based.
- CPT Code 99446 – Interprofessional telephone/Internet/electronic health record assessment and management service provided by a consultative physician, including a verbal and written report to the patient’s treating/requesting physician or other qualified health care professional; 5-10 minutes of medical consultative discussion and review [$18]
- CPT Code 99447 – 11-20 minutes of medical consultative discussion and review [$37]
- CPT Code 99448 – 21-30 minutes of medical consultative discussion and review [$56]
- CPT Code 99449 – 31 minutes or more of medical consultative discussion and review [$74]
- CPT Code 99451 – Interprofessional telephone/Internet/electronic health record assessment and management service provided by a consultative physician, including a written report to the patient’s treating/requesting physician or other qualified health care professional, 5 minutes or more of medical consultative time [$37]
- CPT Code 99452 – Interprofessional telephone/Internet/electronic health record referral service(s) provided by a treating/requesting physician or other qualified health care professional, 30 minutes [$37]
Note – For commercial payors, check with your individual payer’s policies directly for more information on coverage for telemedicine services.
CMS designed a CPT code selection grid located at the bottom of the Medicare Telemedicine Health Care Provider Fact Sheet .
Additional resources
For the latest information on federal policy and payment changes related to telehealth in the midst of COVID-19, visit the CMS Current Emergencies site .

4930 Del Ray Avenue, Bethesda, MD 20814 301-654-2055
Connect with aga.
© American Gastroenterological Association

- Privacy Overview
- Strictly Necessary Cookies
- Cookie Policy
This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
If you disable this cookie, we will not be able to save your preferences. This means that every time you visit this website you will need to enable or disable cookies again.
More information about our Cookie Policy
Repertoire Magazine
Promoting Excellence in Healthcare Sales
E-visits addressed with new CPT® codes
Six new CPT® codes for 2020 reflect the growth of non-visual digital evaluation services, that is, electronic health records and patient portals.
What’s more, for the first time, the CPT code set for 2020 will include two codes to support self-measured blood pressure monitoring.
The CPT Editorial Panel “agreed that the expanded use of electronic health records and associated, HIPAA-complaint secure patient portals has renewed focus on the important role played by non-visual digital patient-physician communication (i.e. e-visits),” Mark Synovec, M.D., chair of the CPT Editorial Panel, told Repertoire in an email.
Three of the new codes – 99421, 99422, 99423 – describe patient-initiated digital communications provided by a physician or other qualified healthcare professional. Three additional codes – 98970, 98971, 98972 – describe services provided by a non-physician healthcare professional.
2020 is not the first year that CPT codes have addressed online evaluation and management services. Since 2008, CPT codes 99444 and 98969 have described such services.
But “these codes were not widely adopted by payers due to a lack of clear definitions surrounding the work involved in these online visits,” said Synovec. “Furthermore, the current online evaluation and management codes did not fully characterize the evolution that has occurred with these services.”
With the CPT codes will come coverage, said Synovec. In its Proposed Rule for 2020, the Centers for Medicare & Medicaid Services proposed assigning RVUs, or relative value units, to codes 99421, 99422 and 99423, he said. Many private payers will follow Medicare’s lead, he added.
The agency has proposed that the non-physician healthcare professional codes (98970, 98971, 98972) be covered through HCPCS G-codes, for services and procedures that are under review for coverage. “[T]he Panel will be working to revise these CPT codes to try and meet the requirements of Medicare in 2020.”
Self-measured BP monitoring Prior to 2020, the CPT code set never included self-measured blood pressure monitoring (SMBP), said Synovec. Four ambulatory blood pressure monitoring codes (93784, 93786, 93788, 93790) exist, but they only describe continuous monitoring over at least 24 hours.
“These new SMBP codes are more closely aligned with clinical guidelines that have shown the advantage of collecting blood pressure outside of the clinic setting for diagnosis of hypertension, which can result in measurement errors, a smaller number of measurements, and white coat hypertension,” he said. They are congruous with recent recommendations by the United States Preventive Services Task Force, which found that SMBP is a valid alternative method of confirmation when other methods are not available.
Current Procedural Terminology (CPT) codes offer doctors and healthcare professionals a uniform language for coding medical services and procedures to streamline reporting, increase accuracy and efficiency. They are also used for administrative management purposes, such as claims processing and developing guidelines for medical care review.
The CPT code set is maintained, updated and modified by the CPT Editorial Panel, with authorization of the AMA Board of Trustees. The panel is composed of 17 members. Of these, 11 are physicians nominated by the national medical specialty societies and approved by the AMA Board of Trustees. One of the 11 is reserved for expertise in performance measurement. One physician is nominated from each of the following: Blue Cross and Blue Shield Association, America’s Health Insurance Plans, American Hospital Association, and CMS. The remaining two seats on the panel are reserved for members of the CPT Health Care Professionals Advisory Committee.
New CPT codes
Code Description
Self-measured BP monitoring
Source: AMA
- About Repertoire
- Media Guide
- Excellence in Sales
- Hall of Fame

Coding for E/M home visits changed this year. Here’s what you need to know
CPT has revised codes for at-home evaluation and management (E/M) services as of Jan. 1, 2023. Services to patients in a private residence (e.g., house or apartment) or temporary lodgings (e.g., hotel or shelter) are now combined with services in facilities where only minimal health care is provided (e.g., independent or assisted living) in these code families:
Home or residence E/M services, new patient
• 99341, straightforward medical decision making (MDM) or at least 15 minutes total time,
• 99342, low level MDM or at least 30 minutes total time,
• 99344 (code 99343 has been deleted), moderate level MDM or at least 60 minutes total time,
• 99345, high level MDM or at least 75 minutes total time.
Home or residence services, established patient
• 99347, straightforward MDM or at least 20 minutes total time,
• 99348, low level MDM or at least 30 minutes total time,
• 99349, moderate level MDM or at least 40 minutes total time,
• 99350, high level MDM or at least 60 minutes total time.
Select these codes based on either your level of medical decision making or total time on the date of the encounter , similar to selecting codes for office visits . The E/M codes specific to domiciliary, rest home (e.g., boarding home), or custodial care (99324-99238, 99334-99337, 99339, and 99340) have been deleted, and the above codes should also be used in those settings.
When total time on the date of the encounter exceeds the threshold for code 99345 or 99350 by at least 15 minutes, you can add code 99417 to report prolonged services. The exception to this is for patients with Medicare. For those patients, report prolonged home or residence services to Medicare with code G0318 in addition to 99345 (requires total time ≥140 minutes) or 99350 (requires total time ≥110 minutes). Code G0318 is not limited to time on the date of the encounter, but includes any work within three days prior to the service or within seven days after.
Services provided in facilities where significant medical or psychiatric care is available (e.g., nursing facility, intermediate care facility for persons with intellectual disabilities, or psychiatric residential treatment facility) are reported with codes 99304-99310 .
— Cindy Hughes, CPC, CFPC
Posted on Jan. 19, 2023
- Chronic care
- Medicare/Medicaid
- Physician compensation
- Practice management
- Reimbursement
- Value-based payment
Other Blogs
- Quick Tips from FPM journal
- AFP Community Blog
- Fresh Perspectives
- In the Trenches
- Leader Voices
- RSS ( About RSS )
Disclaimer: The opinions and views expressed here are those of the authors and do not necessarily represent or reflect the opinions and views of the American Academy of Family Physicians. This blog is not intended to provide medical, financial, or legal advice. Some payers may not agree with the advice given. This is not a substitute for current CPT and ICD-9 manuals and payer policies. All comments are moderated and will be removed if they violate our Terms of Use .
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

IMAGES
VIDEO
COMMENTS
E-visits should not be billed on the same day the physician reports an office visit E/M service (CPT codes 99202-99205 and 99211-99215) for the same patient. Additionally, e-visits should not be ...
These services can only be reported when the billing practice has an established relationship with the patient. For these E-Visits, the patient must generate the initial inquiry and communications can occur over a 7-day period. The services may be billed using CPT codes 99421-99423 and HCPCS codes G2061-G2063, as applicable.
The six new codes for e-Visits are: 99421, 99422, and 99423 to report patient-initiated digital communication provided by a physician or other qualified healthcare professional. 98970, 98971, and 98972 for digital communications with a non-physician healthcare professionals. Code. Description.
E-visits should not be billed on the same day the physician reports an office visit E/M service (CPT codes 99201-99205 and 99211-99215) for the same patient. Additionally, e-visits should not be ...
Best Guide to E-Visit Documentation, Coding, and Billing. The American Academy of Family Physicians (AAFP) encourages safe, secure online interactions between physicians and patients, such as electronic visits or "virtual e-visits.". In non-emergency situations, e-visits can substitute for office visits with primary care providers.
20. Can PTs bill CPT codes 99421, 99422 and 99423 for an e-visit? No. These are evaluation and management, or E/M, codes, for e-visits and PTs are not permitted to independently bill for E/M visits. The non-physician e-visit codes are CPT codes 98970-98972 for commercial payers and HCPCS codes G2061-G2063 for Medicare. (March 18) 21.
Analyze E-Visit Criteria. What are E-visits? E-visits are non-face-to-face, patient-initiated communications through secure online portals such as electronic health record (EHR) portals, secure email, or other digital applications. ... separate payment for CPT® codes 98966-98968 and CPT® codes 99441-99443." ...
The new CPT codes report online digital evaluation services, or e-visits. The codes describe patient-initiated digital communications provided by physicians or other qualified health professionals—codes 99421, 99422 and 99423. Three others describe similar interactions when they involve a nonphysician health professional—98970, 98971 and 98972.
Medicare will allow audio-only telephone E/M visits to be reported as telehealth, but they must be reported with the telephone E/M codes 99441-99443. ... CPT codes to describe telephone E/M are time-based. Effective March 1, 2020, payment for telephone E/M code 99441-99443 are equivalent to 99212-99214 and can be used for new or established ...
Report an e-visit code only once per 7 consecutive days. Select the appropriate CPT code based on the cumulative time spent providing e-visit services to each patient, through a patient portal, over the course of the 7 days. Day 1 of the 7 days begins on the first date you provide an e-visit. Telephone calls do not count toward the time for e ...
E-visits (online E/M visits), Virtual check-ins (assessments by telephone or other telecommunication device to determine whether an in-office encounter is needed for the patient's concern),
1 E-Visits REIMBURSEMENT POLICY E-Visits Active _____ Policy Number: General Coding - 008 Policy Title: E-Visits Section: General Coding Effective Date: 03/24/15 _____ Description This policy addresses coverage and coding for E visits. Definitions An E-visit is a patient-initiated, limited online evaluation and management healthcare service
As of Jan. 1, 2021, CMS permanently allows PTs in private practice and facility-based settings to render e-visits (CPT codes 98970-98972) under Medicare. Here is brief guide to using e-visits under Medicare. If you need more explanation, return to APTA's article Furnishing and Billing E-Visits: Addressing Your Questions.
For qualified nonphysician healthcare professionals (QNHPs) who cannot perform and bill for E/M services, you'll report code range 98966-98968 for telephone-based services. Billing update: The interim final rule indicates that CMS will reimburse for 99441-99443 during the extent of the COVID-19 PHE. Additionally, both new and established ...
Video Visit Established Patient E/M Telephone E/M Online Digital E/M Virtual Check-ins CPT 2021 Time Range 2021 Pmt wRVU CPT Time 2021 PHE Pmt 2021 PHE wRVU CPT Time 2021 Pmt wRVU CPT Time 2021 Pmt wRVU 99211 NA $23.03 0.18 G2010 NA $12.21 0.18 99212 10-19 min $56.88 0.70 99441 5-10 min $56.88 0.70 99421 5-10 min $15.00 0.25 G2012 5-10 min $14. ...
Billing and coding guidance. Do not report e-visit services for less than five minutes. Report e-visit services once per seven-day period. Do not count G2061, G2062 or G2063 time otherwise reported with other services. ... Five days into the e-visit, the father and psychologist reconnect to assess the child's symptoms, assess a follow-up ...
The new rules for coding evaluation and management (E/M) office visits are a big improvement but still a lot to digest. 1, 2 To ease the transition, previous FPM articles have laid out the new ...
New CPT codes. E-visits. Code Description. 99421. Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 5-10 minutes. 99422. Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 11-20 minutes.
Split (or Shared) E/M Services. CPT Codes 99202-99205, 99212-99215, 99221-99223, 99231-99239, 99281-99285, & 99291-99292. A split (or shared) service is an E/M visit where both a physician and NPP in the same group each personally perform part of a visit that each 1 could otherwise bill if provided by only 1 of them.
The basic format of codes with levels of E/M services based on medical decision making (MDM) or time is the same. First, a unique code number is listed. Second, the place and/or type of service is specified (eg, office or other outpatient visit). Third, the content of the service is defined. Fourth, time is specified.
The 2021 E/M office visit coding changes allow physicians to code visits based solely on total time, which is defined as the entire time you spent caring for the patient on the date of the visit.
A visit spanning two calendar dates is "a single service and is reported on one calendar date," even if the services are continuous services beginning on one calendar date and extending through midnight into the next. ... E/M Coding: Follow These 5 Tips to Solidify Your Inpatient Care Coding Stay on top of the hospital E/M revisions. For ...
After the 2021 E/M office visit coding changes, most family physicians can find the right code for many of their visits just by answering these two questions. (Part One of a five-part series on E ...
Select these codes based on either your level of medical decision making or total time on the date of the encounter, similar to selecting codes for office visits. The E/M codes specific to ...