Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer

You are here
- Volume 13, Issue 1
- Comparison of the Journey II bicruciate stabilised (JII-BCS) and GENESIS II total knee arthroplasty for functional ability and motor impairment: the CAPAbility, blinded, randomised controlled trial
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-2051-8451 Iain McNamara 1 , 2 ,
- Valerie Pomeroy 2 ,
- Allan B Clark 3 ,
- Graham Creelman 4 ,
- Celia Whitehouse 1 ,
- J Wells 2 ,
- B Harry 5 ,
- Toby O Smith 6 ,
- Juliet High 7 ,
- Ann Marie Swart 2 , 8 ,
- Celia Clarke 2
- 1 Norfolk and Norwich University Hospital , Norwich , UK
- 2 University of East Anglia , Norwich , UK
- 3 Norwich Medical School , University of East Anglia , Norwich , UK
- 4 Mental Health Act Review Panels , Norfolk and Suffolk , UK
- 5 Department of clinical neurosciences , University of Cambridge , Cambridge , UK
- 6 Faculty of Medicine and Health Sciences , University of East Anglia , Norwich , UK
- 7 Norwich Clinical Trials Unit , Norwich , UK
- 8 Health Sciences , University of East Anglia , Norwich , UK
- Correspondence to Professor Iain McNamara; iain.mcnamara{at}nnuh.nhs.uk
Objectives To determine if a newer design of total knee replacement (TKR) (Journey II BCS) produces superior patient-reported outcomes scores and biomechanical outcomes than the older, more established design (Genesis II).
Setting Patients were recruited from an NHS University Hospital between July 2018 and October 2019 with surgery at two sites. Biomechanical and functional capacity measurements were at a University Movement and Exercise Laboratory.
Participants 80 participants undergoing single-stage TKR.
Interventions Patients were randomised to receive either the Journey II BCS (JII-BCS) or Genesis II TKR.
Primary and secondary outcome measures Primary outcome was the Oxford Knee Score (OKS), at 6 months. Secondary outcomes were: OKS Activity and Participation Questionnaire, EQ-5D-5L and UCLA Activity scores, Timed Up and Go Test, 6 min walk test, lower limb kinematics and lower limb muscle activity during walking and balance.
Results This study found no difference in the OKS between groups. The OKS scores for the JII-BCS and Genesis II groups were mean (SD) 42.97 (5.21) and 43.13 (5.20) respectively, adjusted effect size 0.35 (-2.01,2.71) p=0.771
In secondary outcome measures, the Genesis II group demonstrated a significantly greater walking range-of-movement (50.62 (7.33) vs 46.07 (7.71) degrees, adjusted effect size, 3.14 (0.61,5.68) p=0.02) and higher peak knee flexion angular velocity during walking (mean (SD) 307.69 (38.96) vs 330.38 (41.40) degrees/second, adjusted effect size was 21.75 (4.54,38.96), p=0.01) and better postural control (smaller resultant centre of path length) during quiet standing than the JII-BCS group (mean (SD) 158.14 (65.40) vs 235.48 (176.94) mm, adjusted effect size, 59.91 (–105.98, –13.85) p=0.01.).
Conclusions In this study population, the findings do not support the hypothesis that the Journey II BCS produces a better outcome than the Genesis II for the primary outcome of the OKS at 6 months after surgery.
Trial registration number ISRCTN32315753 .
- HEALTH ECONOMICS
- Clinical trials
- ORTHOPAEDIC & TRAUMA SURGERY
- REHABILITATION MEDICINE
Data availability statement
Data are available on reasonable request. Reasonable requests for data will be considered by the trial team.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2022-061648
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
STRENGTHS AND LIMITATIONS OF THIS STUDY
This is a two arm, superiority, observer-blind, participant-blind and clinical staff-blind, randomised control trial.
It uses a wide variety of patient reported outcomes measures and biomechanical measurements to determine if one implant is superior to the other
The required sample size was achieved with only one person lost to follow-up.
A potential limitation is the relatively large number of secondary outcomes.
The surgeons all had a much greater familiarity with the implantations of Genesis II implants.
Original protocol for the study is mentioned here: https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-020-4143-4 .
Introduction
Despite total knee replacement (TKR) being a recommended surgical treatment for end-stage knee osteoarthritis, 1 up to 34% of all patients following TKR have poor functional outcomes. 2–6 With estimates of osteoarthritis of the knee affecting one in eight people in the USA 7 and 250 million individuals worldwide 8 the number of patients with intrusive symptoms after surgery is significant.
Multiple changes in implant design have been introduced to try to improve patient outcomes and while some implant design alterations have led to improvements in patient-reported outcome measures (PROMS) 9–11 and kinematics 12 13 not all have led to differences. 14–20
The Genesis II (Smith & Nephew, Memphis, Tennessee, USA) TKR has been reported to have good survivorship and patient satisfaction 13 21 and is commonly used in the UK 22 An evolutionary design, the Journey II BCS (JII-BCS; Smith & Nephew), also manufactured by Smith and Nephew, has been developed to improve kinematic outcome compared with the Genesis II by using a bicruciate design. 23 This design change has been supported by encouraging fluoroscopic studies. However, to date, no randomised controlled trials (RCTs) have been conducted to assess if there is a difference in the outcome compared with its predicate design. 24
This trial aimed to assess whether the JII-BCS would produce better patient reported and movement outcomes than the Genesis II.
The published protocol included the aims for investigating: the rotational profile around the native knee and following TKR; and patients’ experiences and surgeons’ experiences. 25 These findings will be reported in subsequent manuscripts.
Trial design, randomisation, blinding to intervention allocation, ethics and registration
A two-arm, superiority RCT comparing the JII-BCS knee implant (experimental intervention) to the Genesis II knee implant (control intervention) was performed. The trial was observer-blind, participant-blind and clinical staff-blind. Only the operating surgeon and theatre team knew which implant was used for an individual participant.
Trial participants were assigned to either the JII-BCS or Genesis II group using a computer-generated, 1:1 randomisation schedule stratified by site and age (<60 years = younger; ≥60 years = older). 26 27 Group allocation was revealed using REDCap, 28 29 the interactive web-randomisation system, to a member of the research team who was not involved in either the clinical care or assessments of any participant. Allocation was concealed from the surgical team until after the preoperation baseline measures were completed.
Sample size
The sample size was calculated from the Oxford Knee Score (OKS, primary outcome measure). 30 The RCT was powered at 80% with a 5% significance level to detect a minimally important clinical difference of five points 31 32 with an SD of 7.4 points. 33 Accounting for an estimated attrition rate of 10% at 6 months postsurgery the estimated sample size was 80 participants (40 per group).
Participants, setting and recruitment
Full eligibility criteria are provided in the published protocol. 25 In brief, participants were aged at least 18 years and met the clinical and radiological criteria for a single-stage TKR. People were excluded if they: had a fixed-flexion deformity of at least 15° or non-correctable varus/valgus deformity of at least 15°; had inflammatory arthritis or previous septic arthritis; had previous surgery to the collateral ligaments of the affected knee; had a contralateral TKR implanted less than 1 year earlier; had severe comorbidity that could present an unacceptable safety risk or were pregnant; were a private patient; were likely to be living outside the clinical centre catchment area at 6 months postsurgery or were enrolled on another clinical trial.
Patients were recruited at a university teaching hospital with surgery conducted at two sites. Outpatient physiotherapy was conducted in a single hospital. The Movement and Exercise Laboratory at the associated University (MoveExLab) was the setting for measures of functional capacity and biomechanics.
Interventions
All participants received routine NHS care for people with TKR irrespective of the implant received. This included following a standard postoperative rehabilitation of outpatient physiotherapy centred on knee strength and range of motion (ROM) exercises within the first 6 weeks after surgery. Patients received the same physiotherapy protocols and classes.
Experimental intervention
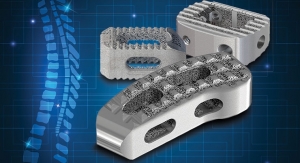
Participants in the experimental group received the JII-BCS. The JII-BCS is a dual-cam post designed to substitute for both the anterior cruciate ligament and posterior cruciate ligament. In addition the femoral and tibial components are asymmetric and the polyethylene insert is a medially concave and laterally convex shape. The device is designed to provide guided motion, and thus improve knee kinematics, and increase anteroposterior stability throughout knee flexion.
.Control intervention
Participants in the control group received the Genesis II (Smith and Nephew), posterior stabilised (PS) TKR. The design features specific to the implant and a lateralised trochlear groove to improve patellar contact and tracking, an externally rotated femoral implant design and an anatomically shaped tibial baseplates.
Surgical techniques
All four surgeons had extensive experience, at least 5 years, of the Genesis II implant. All undertook cadaveric training on the JII-BCS and declared that they were competent in the surgical technique having completed their operative learning curve before starting the trial. Both implants are uncoated, cemented implants. The surgical procedure followed the standard manual surgical approach and technique through a medial parapatellar approach in all cases with intramedullary femoral and tibial rods to provide the alignment of the components. Patella resurfacing was used in both groups.
Data collection schedule
Data collection time points for the primary outcome measure were: at least 1 day before surgery (baseline), 7±2 days after surgery (1 week postoperatively), 6–8±2 weeks after surgery (2 months), 6 months±4 weeks after surgery (outcome, primary time point). Secondary outcomes were collected at baseline, 2 months and 6 months. Any differences from these time points are provided in the outcome measures section.
Outcome measures
Primary outcome measure.
The OKS was the primary outcome measure. This is a 12-question patient self-assessment of knee function and pain 30 with values ranging from 0 (worst outcome) to 48 (best outcome).
Secondary outcome measures
Patient-reported outcome questionnaires.
The Oxford Knee Score Activity and Participation Questionnaire (OKS-APQ), which complements the OKS by assessing everyday activity and social participation. 34 The overall score is from 12 to 60 with 12 being the best outcome.
The EQ-5D-5L is a self-report questionnaire consisting of five questions and a Visual Analogue Scale. Higher values indicate better quality of life. 35
The UCLA Activity score (UCLA) to assess physical activity self-rating scale ranged from 0 (complete inactivity) to 10 (participation in impact sport).
Walking and balance functional ability
Timed Up and Go Test (TUG)—seconds to rise from chair, walk 3 m and return to sitting; mean of three trials. 36 The reported minimal detectable change after TKR is 2.27 s. 37 A lower value indicates better function.
Six min walk test—metres walked in 6 min around a 20 m circuit. 38 39 The reported minimal detectable change from baseline after TKR is 26 metres. 40 A higher value indicates greater function.
Modified Star-Excursion Test 41 (cm/leg length) where larger values indicate better balance.
Movement performance during walking and balance
For these simultaneous measures, participants wore shorts and were bare-footed. Reflective sensors were placed in accordance with the Plug-In Gait model (Vicon) for the lower limb and three-dimensional motion data were collected, at 100 HZ, with eight wall-mounted infrared cameras (Vicon Motion System, Oxford, UK). Three embedded force plates (BERTEC, Ohio, USA) were used to collect kinetic data at 2000 Hz for walking tasks and 100 Hz for balance tasks. Surface electromyographic sensors (EMG: Delsys) were placed bilaterally on the Vastus Medialis, Vastus Lateralis, Tibialis Anterior, Bicep Femoris and lateral head of the Gastrocnemius following SENIAM guidance. EMG data were collected at 2000 Hz.
For walking tasks, participants were asked to walk in a straight line along a 10 m walkway at their self-selected speed. For double stance balance activities, participants were instructed to stand with their feet shoulder-width apart. For single stance balance activities, participants were instructed to stand on one leg with hands-on-hips. Three trials of 10 s were recorded for each activity.
For the stair ambulation task, participants were asked to complete six ascents and six descents all unaided, leading with the operated limb for three trials and the non-operated limb for the remainder. The stairs had four steps. The first step was 16.5 cm, and the others were 15 cm high. Handrails were available if participants needed support.
Movement data were processed in accordance with the Vicon Plug-in Gait Model (Oxford Metrics, Oxford, UK). Raw EMG was filtered with pass bands at 10 and 500 Hz, rectified and low pass filtered using a fourth order Butterworth with a 10 Hz cut-off. Walking data were normalised to 101 data points for the gait cycle. Three trials of tasks were used to create a mean for each measure per participant. Values were extracted using a purpose-built MATLAB script. Data were processed by motion analysis experts in the research team.
Primary movement performance measures
The JII-BCS is expected to provide more normal kinematics during knee movement than Genesis II due to the design changes discussed earlier. Other authors have indicated that the femo-tibial relationship may be more normal during deep knee bend 42 and more stable during walking 43 Accordingly, people with the Journey prosthesis may 44 45 or may 43 have greater knee ROM, may walk faster, 46 47 and may have a longer stride length 46 47 than people receiving a comparison knee replacement. In addition, greater stability of the femur on the tibia could produce greater knee flexion angular velocity as dynamic knee loading could be more normal. However, there is only one non randomised study of 18 patients comparing the JII-BCS directly with the Genesis II. 45 Based on the available literature, the hypothesis driving the kinematic investigation was that people receiving the JII-BCS compared with those receiving the Genesis II would have greater walking velocity, step-length symmetry (resulting from longer stride length), knee ROM and peak knee flexion angular velocity.
Walking speed (metres/second). A higher value indicates better performance
Step length symmetry during walking. Step length ratio was calculated as ((2xOp)/Op+NOp))−1); where Op is the step length of the operated leg and NOp is the step length of the non-operated leg. Zero indicates perfect symmetry and best performance.
Knee ROM during walking (degrees). Higher values indicate better performance.
Peak knee flexion angular velocity during walking (degrees per second). This was inadvertently omitted from the statistical analysis plan (SAP). Higher value indicates better performance.
Secondary movement performance measures.
Double stance support (% of gait cycle). It was planned to measure cadence, (steps/min), step length (m) and stride length (m). However, there is redundancy with the temporal-spatial gait parameters of walking speed and step length symmetry which are included in the primary movement performance measures.
Peak extension and flexion moments of operated knee during the gait cycle (Nm/kg).
Hip and ankle ROM during walking.
Peak knee flexion angular velocity during stepping up onto a stair.
Percentage of gait cycle for peak activation of Vastus Medialis, Vastus Lateralis, Tibialis Anterior, Biceps Femoris and Lateral head of Gastrocnemius (% of gait cycle).
Balance measures were derived from kinetic data (from force plates) during standing still: single stance on the operated lower limb for 10 s with eyes open (yes/no) and duration maintained; resultant centre of pressure path length (COP cm) in double stance with eyes closed; and resultant COP velocity (cm/s) in double stance with eyes closed.
Clinical context and adverse events
Data on length of hospital stay and complications related to the surgery (eg, anaesthesia-related problems, bleeding, morbidities) were collected from a notes review. At each visit, participants were asked about their pain medication and if they had received additional treatment since their surgery/previous visit and what this entailed. Any need for revision surgery was recorded. All adverse events identified were tracked until resolution.
The SAP was finalised and agreed prior to database lock and analysis was completed blinded to group allocation ( online supplemental file ). For all outcomes the hypothesis tests and 95% CIs were two sided; and a p<0.05 was considered significant. An intention-to-treat analysis was conducted that is, all randomised participants regardless of their eligibility or adherence were analysed according to the treatment they were randomised to receive. The analysis was undertaken by the Trial Statistician using Stata V.16.
Supplemental material
For the primary outcome, the mean OKS at 6 months was compared between the control and experimental groups using a general linear model adjusting for site and age (<60 years/≥60 years). An adjusted analysis was conducted using the same model but adjusting for the OKS at baseline. The model assumptions were checked graphically, and sensitivity analysis done using a non-parametric bootstrap using 5000 repetitions.
All the other outcomes were analysed separately at 2 months and 6 months using the same general linear model specified above and a corresponding adjusted analysis. The exception was ability to balance for 10 s. This was analysed using a logistic regression model adjusting for site and age.
Patient and public involvement
A patient representative, who had previously undergone knee replacement surgery, was involved in the protocol development, assessment of the burden of the intervention and time taken to participate in the research and oversight of the trial as a member the trial management group. The representative also contributed to the planning and writing of research dissemination materials.
Participants were recruited between July 2018 and October 2019. Last follow-up visits were in October 2020 with some impact and delayed visits due to COVID-19.
In the published protocol, 25 the analysis plan included a per-protocol and safety analysis. This was not undertaken as the implants were used as intended so these populations would be the same as the intention-to-treat population.
Flow of participants through the trial
In total, 105 of 153 people screened were eligible to take part, 16 declined participation and eight were excluded for other reasons. Therefore, 81 of 153 people (53%) were recruited. All participants in the Genesis II group (n=40) received their allocated intervention. In the JII-BCS group (n=41), one participant withdrew prior to surgery (postrandomisation exclusion). Full details are in the Consolidated Standards of Reporting Trials (CONSORT) flow chart ( figure 1 ).
- Download figure
- Open in new tab
- Download powerpoint
Consolidated Standards of Reporting Trials (CONSORT) diagram.
Participant characteristics
There were no discernible baseline differences between the groups ( table 1 ).
- View inline
The baseline characteristics of participants
Primary outcome comparison: 6 months postoperatively
The OKS scores for the JII-BCS and Genesis II groups were mean (SD) 42.97 (5.21) and 43.13 (5.20), respectively. There was no significant difference between the groups: adjusted effect size 0.35 (−2.01,2.71) p=0.771 ( table 2 ).
Oxford Knee Scores (OKS, primary outcome), from baseline to 6 months after surgery (primary time point)
Secondary outcome comparisons: 6 months postoperatively
There were no differences between the two groups for any of the secondary patient reported outcomes ( online supplemental tables S1 ).
There was no difference between the JII-BCS and Genesis II groups in the time to complete the TUG Test or the distance covered in the 6 min walk test ( online supplemental table S2 ). The Star-Excursion Test was attempted by all participants but 59% of participants at baseline, 59% at follow-up and 63% at outcome were unable to complete it ( online supplemental table S3 ). Therefore, statistical analysis was not undertaken.
The primary movement performance measures are reported in table 3 . In summary at 6 months postsurgery, the Genesis II group had a significant advantage for knee ROM and peak knee flexion angular velocity during walking. There were no differences between the groups for walking speed or peak flexion angular knee velocity on stair climbing.
Movement performance primary measures during walking from baseline to 6 months postsurgery (primary time point): walk speed, step length symmetry, knee range of motion (ROM) and peak knee flexion angular velocity
Data for all secondary movement performance measures are provided in online supplemental tables S4–S8 . The only difference between groups that reached statistical significance was for COP path length in double stance with eyes closed ( online supplemental table S7 ). The mean (SD) values for the Genesis II and JII-BCS groups were 158.14 (65.40) mm and 235.48 (176.94) mm, respectively. Adjusted effect size was −59.91 (–105.98, –13.85) p=0.01 in favour of the Genesis II group.
Postoperative clinical context
There were no between-group significant differences for: length of stay, change in pain medication from randomisation or physiotherapy received ( online supplemental tables S9 and S10 ).
Adverse events
One patient with a JII-BCS developed acute swelling and pain in the knee and was systemically unwell at 4 months postoperatively. The joint aspiration demonstrated turbid fluid and an exchange of the polyethylene spacer and retention of the femoral and tibial components (Debridement And Implant Retention) was performed with postoperative antibiotic treatment. Subsequent microbiology was negative so infection was never conclusively demonstrated. The numbers and type of complications are reported in online supplemental table S11 .
The findings do not support the hypothesis that the JII-BCS produces a better outcome than the Genesis II for the primary outcome of the OKS at 6 months after surgery. No differences between groups were also found for: other patient-reported outcomes; measures of balance and walking function; hip and ankle ROM; knee moments during walking; double support time during walking and percentage of gait cycle for peak muscle activation. However, significant advantages for the control group (Genesis II) were found for: operated knee range-of-movement and peak knee flexion angular velocity during walking, and postural control (COP path length).
While some investigators have demonstrated differences between generations of knee designs 12 not all modern generation TKR designs have demonstrated an improvement in outcomes when compared with their predecessors. 15–20 48 One possible reason for this is that the predecessor is already producing good results and therefore is difficult to improve on. Regarding the JII-BCS, at the time of writing, only Bialy et al 45 have directly compared the Genesis II and the JII-BCS. Their study was non randomised and consisted of 18 patients between the two groups. They reported a greater supine range of movement of the JII-BCS compared with the Genesis II when measured with a long arm goniometer. They also reported an improvement in functional knee scores and stability when balancing. Their conclusions were that the JII-BCS restores more normal anatomy and kinematics which is correlates into the improvements that they found. None of the other papers reporting outcomes of the JII-BCS compared the JII-BCS to the Genesis II, none used a randomised design and none used methodology or outcomes that could be compared with the methodology used in this trial. 42–46 However, on the basis of the available literature, we measured outcomes that would be expected to be difference on the basis of the available literature, walking velocity, step-length symmetry (resulting from longer stride length), knee ROM and peak knee angular velocity.
Within our trial, we found differences in some biomechanical measures of motor impairment but not for others; patient-reported outcomes; and, walking and balance function. It is possible that knee range-of-movement during walking, walking symmetry, peak knee flexion angular velocity during walking and postural control (COP path length) are detecting motor impairment improvement for the Genesis II group and/or because statistical significance was a result of testing multiple outcomes. The latter explanation is clearly possible but knee range-of-movement is greater for people reporting good outcome after knee replacement than for those reporting poor outcome. 49 Moreover, knee range-of-movement has been found to be the main biomechanical effect of TKR 50 and to improve over time while other biomechanical measures do not. 50 51 Likewise, postural control improves over time 52 53 and approaches healthy control values. 52 Importantly, gait symmetry is an indicator of walking control 54 and, while of borderline statistical significance (p=0.05) can possibly detect differences following insertion of different prostheses. Peak knee angular velocity during walking is also an indicator of walking control 55 and has been found to change beneficially after insertion of the Genesis II prosthesis. 50 These findings indicate that secondary, in-depth, analysis of the biomechanical data should be undertaken.
A potential limitation is the relatively large number of secondary outcomes. However, this is also a strength as it ensured comprehensive examination of the potential impact of TKR on functional ability, motor impairment and health-related quality of life. Another potential limitation is that the surgeons all had a much greater familiarity with the Genesis II implants. However, all surgeons were very experienced with the Genesis II implant with at least 10 years of experience implanting the device. All surgeons received thorough training with the JII-BCS and the surgical technique and instrumentation are similar for both devices with only one additional femoral cut being necessary for the JII-BCS compared with the Genesis II. A key strength of this trial is that the required sample size was achieved with only one person lost to follow-up. Other strengths include minimisation of selection bias through a robust randomisation procedure and use of double blinding to minimise interpretation bias.
The lack of difference between implant designs is important for patients, surgeons, healthcare providers and implant companies. For the patient and surgeons, reassurance can be gained that older designs, with proven track record of function and survivorship, can provide the same patient reported and functional outcome as more modern designs. For the healthcare providers, older implants are often less expensive and, in the absence of clinical benefit with and demonstrable longevity, if the additional expenditure on more modern designs is avoided for the hundreds of thousands of patients undergoing surgery worldwide the cost savings are potentially significant. Finally, for the implant companies, it is more likely than not than implant design has reached a point when non-implant-related factors play a more important role in patient outcome. The future of design and innovation may come in the form of more modern surgical techniques such as robotic assisted implantation to assist in placing the knee in a more kinematically sympathetic position which in turn may allow the newer design philosophies to positively influence outcome. It is possible, only then in combination with modern surgical techniques, that improvements in patient outcomes can be realised but well-constructed surgical trials will need to answer such questions.
This study demonstrated no difference between the Genesis II and its successor the JII-BCS for PROMS, walking function, temporal-spatial gait parameters, balance ability and lower limb kinematic results at 6 months follow-up. However, significant advantages were seen in for the Genesis II in the operated knee range-of-movement, peak knee flexion angular velocity during walking and postural control.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
This study involves human participants and was approved by East of England – Cambridge Central Research Ethics Committee (reference 16/EE/0230). Participants gave informed consent to participate in the study before taking part.
Acknowledgments
The team would like to thank all the participants and families who gave their time to be part of this study; Antony Colles, Martin Pond and the NCTU data management team; Estelle Payerne; Amanda Thacker; NNUH sponsorship team and the safety monitoring committee members, Prof Marcus Flather and Prof Simon Donell. Also: Mr Charles Mann, Mr Nish Chirodian, Mr David Calder, Dr Nicola Hancock, Nursing and clinic staff at the Spire Hospital and NNUH, Prof Andoni Toms and the Radiology department at NNUH and Addenbrooke’s hospital, Cambridge, Dr Simon Horton and Dr Anne Killett
- Troelsen A , et al
- Cooper C , et al
- Beswick AD ,
- Gooberman-Hill R , et al
- Robinson RL ,
- Partridge CM , et al
- Kennedy LG ,
- Newman JH ,
- Ackroyd CE , et al
- Voaklander DC ,
- Suarez-Alma ME
- Cisternas MG ,
- Sacks JJ , et al
- Flaxman AD ,
- Naghavi M , et al
- Collados-Maestre I ,
- Lizaur-Utrilla A ,
- Gonzalez-Navarro B , et al
- Szubski CR , et al
- Jacobs WCH ,
- Christen B ,
- Wymenga AB , et al
- Hamilton DF ,
- Burnett R ,
- Patton JT , et al
- Pennington M ,
- Black N , et al
- Spelman T , et al
- Hörlesberger N ,
- Klim S , et al
- Liow MHL , et al
- Molloy IB ,
- Keeney BJ ,
- Sparks MB , et al
- Ranawat CS ,
- West S , et al
- Park CH , et al
- Behrend H ,
- Zdravkovic V ,
- Bösch M , et al
- Walker RW ,
- Evans JP , et al
- ↵ . Available from: National Joint Registry for England, Wales N ireland and the I of M . National joint registry , 2019 . Available: https://reports.njrcentre.org.uk/portals/0/pdfdownloads/njr 16th annual report 2019.pdf
- Grieco TF ,
- Dessinger GM , et al
- Pomeroy V ,
- Clark A , et al
- Merle-Vincent F ,
- Couris CM ,
- Schott A-M , et al
- O'Byrne M ,
- Harmsen S , et al
- Harris PA ,
- Thielke R , et al
- Minor BL , et al
- Fitzpatrick R ,
- Murray D , et al
- Tan Q , et al
- Dawson J , et al
- Williams DP ,
- O'Brien S ,
- Doran E , et al
- McKibbin H , et al
- Herdman M ,
- Lloyd A , et al
- Podsiadlo D ,
- Richardson S
- Kennedy DM ,
- Stratford PW ,
- Wessel J , et al
- Bennell K ,
- Naylor JM ,
- Buhagiar M , et al
- Kinzey SJ ,
- Armstrong CW
- Nachtrab J ,
- LaCour M , et al
- Aizawa T , et al
- Di Benedetto P ,
- Colombo A , et al
- Dec J , et al
- Kanamori A ,
- Kadone H , et al
- Amemiya K ,
- Omata M , et al
- Nunley RM ,
- Berend KR , et al
- Wretenberg P ,
- Lindgren V , et al
- Monda M , et al
- Yoshida Y ,
- Snyder-Mackler L
- Gauchard GC ,
- Meyer P , et al
- Moutzouri M ,
- Gleeson N ,
- Billis E , et al
- Patterson KK ,
- Nadkarni NK ,
- Black SE , et al
- Richards JD ,
- Pramanik A ,
- Sykes L , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
Twitter @tobyosmith
Contributors IM and VP drafted this paper. IM is the guarantor. All authors (IM, VP, ABC, GC, CW, JW, BH, TOS, JH and AMS) contributed to revisions of the manuscript, read and approved the final manuscript. All authors (IM, VP, ABC, GC, CW, JW, BH, TO, JH and AMS) contributed to the development of the trial protocol as well as conception or design of the work; the acquisition, analysis or interpretation of data for the work.
Funding This work was supported by an investigator initiated grant from Smith and Nephew, with both types of knee replacements supplied at the same cost.
Disclaimer The funders had no role in the design of the study, the data collection, the data analysis, interpretation of data, or writing of the manuscript.
Competing interests The trial was funded by Smith and Nephew via an unrestricted grant, administered by the Sponsor NNUH. Funding was used within NNUH for running the trial. Funds were provided via NNUH to UEA for the members of the trial team based in the movement and Exercise Laboratory (MoveExLab) at UEA and the clinical trials unit (CTU) based at UEA for statistics, and trial and data management.
Patient and public involvement Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:

- Smith & Nephew Manuals
- Medical Equipment
- JOURNEY II BCS
Smith & Nephew JOURNEY II BCS Manual
- page of 48 Go / 48
Table of Contents
- Intended Use, Indications, Contraindications
- Indications for Use
- Design Rational/Surgical Planning Rational
- NAVIO Surgical System Overview
- Navio Instrument Trays
- Positioning the System
- System and Patient Setup
- Bone Tracking Hardware
- Surgical Preferences
- Registration
- Ligament Balancing
- Implant Planning
- Implant Planning - Soft Tissue Balancing
- Bone Cutting
- Trial Reduction
- Cement and Close
- Recovery Procedure Guidelines
- Manufacturer Contact Information
Advertisement
Quick Links
- 1 Intended Use, Indications, Contraindications
- 2 Design Rational/Surgical Planning Rational
- 3 Navio Surgical System Overview
- 4 Manufacturer Contact Information
- Download this manual
Related Manuals for Smith & Nephew JOURNEY II BCS

Summary of Contents for Smith & Nephew JOURNEY II BCS
- Page 1 Surgical Technique for use with the JOURNEY™ II BCS and JOURNEY™ II CR...
- Page 2 NAVIO™ Surgical System Surgical Technique for use with the JOURNEY™ II BCS and JOURNEY™ II CR Smith & Nephew 500081, Rev B Issue Date: 2016-11-16 The following technique is for informational and educational purposes only. It is not intended to serve as medical advice. It is the responsibility of treating physicians to determine and utilize the appropriate products and techniques according to their own clinical judgment for each of their patients.
- Page 3 Introduction This procedure guide provides an overview of the recommended surgical technique for using the NAVIO™ surgical system technology with the JOUR- NEY™ II CR (Cruciate Retaining) and JOURNEY™ II BCS (Bi-Cruciate Stabilized) Knee System. Smith & Nephew recommends that users review this guide prior to performing total knee arthroplasty utilizing the NAVIO system.
Page 4: Table Of Contents
Page 5: intended use, indications, contraindications, page 6: design rational/surgical planning rational, page 7: navio surgical system overview, page 8: navio instrument trays, page 9: positioning the system, page 10: system and patient setup.
- Page 11 System and Patient Setup Upon making the incision, carefully debride and inspect the joint. If any prominent spurs or osteophytes are present, especially in the area of the superior posterior femoral condyle, remove them with an osteotome or rongeur, as they could inhibit the leg motion.
Page 12: Bone Tracking Hardware
- Page 13 Bone Tracking Hardware Slide the tracker clamp (with the clamp opening • oriented towards the camera) over the two bone screws until the bottom of the clamp is within 1 cm of the patient’s skin, taking care not to place the clamp where it is touching the patient's skin.
Page 14: Surgical Preferences
- Page 15 Surgical Preferences Rotational References The NAVIO™ Total Knee application allows the user to choose landmark collection preferences on the femur and the tibia in order to define rotational references, from which the implant component placement plan and ligament balancing information is calculated.
- Page 16 Surgical Preferences Joint Line Selection Preference The joint line selection is an optional selection, which allows the user to choose a landmark point on the femur and/or tibia and offset a line perpendicular to the mechanical axis from that point to a chosen distance (Figure 15, 16). This reference line is then displayed during the implant planning stage, to guide the component placement.
Page 17: Registration
- Page 18 Registration Ankle Center Using the point probe, input the locations of the medial and lateral malleoli points by identifying the most prominent portion (Figure 20). Ensure that the point probe is visible throughout the point collection. If the probe is not visible, check that the tracking spheres on the point probe array are not overlapping (in front, or behind) the tracking spheres on the tibia tracker array.
- Page 19 Registration Most Posterior Lateral Point • This point is used in conjunction with the anterior notch point and the most posterior medial point for initial sizing of the implant component. Figure 23. Anterior Notch Point • This point is used as a reference during prosthesis planning to prevent notching of the implant component.
- Page 20 Registration Femoral Condyle Rotational References Based on surgeon preference, there are three options on which the femur rotational reference frame can be defined . These rotational references are used during Implant Planning (Section 6) for component placement onto the patient anatomy. It is important to understand how these collections are taken on the patient’s bony anatomy so that they may be referenced properly during planning.
- Page 21 Registration Posterior Condylar Axis Collection • The femur posterior condyles selection for defining the femur rotational reference, uses the most medial and lateral posterior condyles collections, and allows the user to dial in the medial-lateral axis angle with respect to the two points collected. Figure 28.
- Page 22 Registration Medial Plateau Point • Take the singular low-point of cartilage wear on the medial side of the tibial plateau. Lateral Plateau Point • Attempt to access the lateral side of the tibial Figure 31. condyle by flexing the leg and internally rotating the tibia and manually distracting the joint.
- Page 23 Registration AP Axis Collection • While all of the other collections listed above are singular points referencing the tip of the point probe, this collection will reference the axis of the point probe. If the AP axis is selected for rotational reference collection, using the length of the pointer probe, collect the AP axis on the tibia, normal to the transepicondylar axis.
- Page 24 Registration Tibia Joint Line Reference [Optional- Based on Surgeon Preference] The tibia joint line reference allows the user to pick a landmark point on the bone surface and offset a line perpendicular to the mechanical axis from that point. Figure 37. Tibial Condyle Surface Mapping The Tibia Free Collection stage (Figure 38) offers a visualization of the tibial mechanical and rotational...
Page 25: Ligament Balancing
Page 26: implant planning.
- Page 27 Implant Planning 1. Using the cross section mode, in the transverse and coronal view, confirm that the component size provides adequate coverage on the digitized femur bone surface (Figure 41). Drag vertically on this view screen to visualize the superior-most part of the implant component on the bone (Figure 42).
- Page 28 Implant Planning 5. The implant components for JOURNEY II knee system are posterior referenced. Therefore, in order to have greater resection on the posterior bone, and to increase posterior gap, the component may be downsized, without any change to the anterior transition of the component on to the bone.
- Page 29 Implant Planning 1. Confirm the implant size using the transverse viewscreen (bottom left) and the tibia size up/ down button arrows in the right-hand control panel on the right side of the screen underneath the Tibia Size button. 2. Confirm the posterior slope, utilizing the sagittal view (upper right), NAVIO software will display the posterior slope within this viewscreen, which reflects the slope of the tibial implant component...
- Page 30 Implant Planning Button Mapping Femur While the NAVIO™ System for Total Knee Arthroplasty User’s Manual details each button on this screen, the following five buttons (Figure 46) are particularly critical to understand. - The Checkpoint Verification button is used to manually force a check of the checkpoints in the femur and tibia.
- Page 31 Implant Planning Button Mapping Tibia While the NAVIO™ System for Total Knee Arthroplasty User’s Manual details each button on this screen, the following five buttons (Figure 47) are particularly critical to understand. - The Checkpoint Verification button is used to manually force a check of the safety checkpoints in the femur and tibia.
Page 32: Implant Planning - Soft Tissue Balancing
- Page 33 Implant Planning - Soft Tissue Balancing Gap Balancing The goal of this stage is to have balanced extension and flexion gaps, with no overlap in either condyle, (i.e, medial or lateral). The extension gap will likely look unbalanced when comparing the medial and lateral space if no ligament release has been performed for a deformed knee.
- Page 34 Implant Planning - Soft Tissue Balancing Ligament Balancing Manipulations SCENARIO MANIPULATION Balance is tight Move tibial component inferior and/or in extension reduce thickness and flexion Balance Move tibial component superior and/or is loose in increase poly thickness extension and flexion Balance is tight Move femoral component superior.
- Page 35 Implant Planning - Soft Tissue Balancing Ligament Balancing Manipulations SCENARIO MANIPULATION Balance is loose in the Internally rotate the femur implant to medial compartment in balance gap in the medial and lateral flexion compartments Balance is tight in the Externally rotate the femur implant medial compartment in to balance gap in medial and lateral flexion...
Page 36: Bone Cutting
- Page 37 Bone Cutting Cut Guide Placement Prior to preparation of the locking features for cut guides on to the patient bone surface using the NAVIO™ handpiece in speed control, the user is presented with a cut guide placement screen, where the goal is to size the appropriate cut guide for the operation.
- Page 38 Bone Cutting The user has the ability to move the cut guide anterior and posterior, as well as rotate it in the cut plane. Confirm that the cut slot portion of the guide is not impinging on the bone surface by referencing the cross section view, as well as the 3D view (See Figure 58).
- Page 39 Bone Cutting Screen Overview Figure 60 shows a typical cutting screen with the following icons/buttons called out: - Checkpoint Verification button, used to activate a confirmation of the safety checkpoints on femur and tibia. - Change Bur button, used when the user switches bur size to tell the system about the change.
- Page 40 Bone Cutting Bone Preparation Warning: The NAVIO™ system does not prohibit cutting of soft tissue, which may be in the surgical area. Always use retractors to protect ligaments and other capsular structures. Use steady movement to minimize potential for ligament damage. Warning: NAVIO control modes do not establish “no-cut”...
- Page 41 Bone Cutting Cut Femur The handpiece is used to prepare four cylindrical features in the patient’s bone in order to lock the NAVIO™ femur cut guide onto the bone surface. 1. Align the handpiece tool, under speed control on the cut zone (areas color-coded purple, blue and green on the monitor), by utilizing the cross-hair visualization, and the tool’s eye view.
- Page 42 Bone Cutting 10. Ensure that the dial on the block is set to the zero mark, and tighten the dial using the Smith & Nephew JOURNEY 3.5 mm hex driver. Using the recommended saw, prepare the five planar femur cuts, as recommended by the implant manufacturer in the JOURNEY II Total knee surgical technique.
- Page 43 Bone Cutting Using the handpiece, prepare four features in the patient’s bone in order to lock the NAVIO™ tibia cut guide onto the bone surface. Make sure to uncover the tibia tracker array if it was covered for protection while burring the femur. 1.
Page 44: Trial Reduction
Page 45: cement and close, page 46: recovery procedure guidelines, page 47: notes, page 48: manufacturer contact information, this manual is also suitable for:, rename the bookmark, delete bookmark, delete from my manuals, upload manual.
(586) 436-3785
PATIENT PORTAL

- JOURNEY II – TOTAL KNEE REPLACEMENT
Over the years, we have received feedback from our patients about how Movement Orthopedics has helped them. We are proud to share some of these patient testimonials below.
The JOURNEY II BCS Knee
Recent advances in biomedical engineering software have opened a new chapter on high performance knee implants.
One remarkable breakthrough has been the creation of the JOURNEY II BCS knee, a second-generation knee replacement that combines the stability and natural motion of the human knee with new low-friction materials that may extend the life of the implant.
While the lifespan of a knee implant is heavily influenced by the materials used to make it, the natural feeling of the implant during physical activity is dependent upon the way the patient’s muscles, ligaments and tendons are addressed during surgery and by the implant’s shape within the body after surgery.
As discussed previously in this booklet, the knee is a hinge joint, but it does not swing like a simple door hinge. It has a complex rotational motion that you don’t notice is there – but many patients know when it’s not there after total knee replacement. Traditional implants attempt to recreate this subtle swing-and-rotate action with either a rotating platform (a simple pivot point) within the implant or by requiring an angled alignment of the implant during surgery.
With these traditional knee replacement designs, the muscles and ligaments around your new joint have to work harder because the implant’s slightly unnatural shapes and resulting motion make these soft tissues move in unfamiliar, stressful ways. This leads to joint pain, muscle fatigue and the unnatural feeling patients experience while walking or bending in the months after their procedure.
The JOURNEY II BCS knee, on the other hand, is designed to reproduce the original internal shapes and angled forces of the human knee through its full range of motion – accommodating the swing-and-rotate of the joint with the same engineering principles your real knee currently uses. Because of this, your soft tissues don’t have to readjust to new shapes and forces after surgery and your stride can return to its natural rhythm.
The JOURNEY II BCS knee also reproduces the stability provided by your anterior cruciate ligament (ACL) and your posterior cruciate ligament (PCL). Your ACL and PCL are key to the stability of your real joint and contribute to natural motion when your knee is fully extended and fully bent. No other knee implant reproduces both functions.
Implant Components
In the knee replacement procedure, each prosthesis is made up of four parts.
The tibial component has two elements – a metal base and a plastic insert – and replaces and the top of the tibia (shin bone). This prosthesis is made up of a metal tray attached directly to the bone and a high-density plastic spacer that provides the bearing surface.
The femoral component replaces the bottom of the thigh bone or femur. This component also replaces the groove where the patella or kneecap rides.
The patellar component replaces the surface of the knee cap, which rubs against the femur. The patella protects the joint, and the resurfaced patellar button will slide smoothly on the front of the joint. In some cases, surgeons do not resurface the patella.

Bearing Surfaces
One of the keys to a successful implant is its ability to withstand the rigors of daily activity, and central to that is the quality of the artificial surfaces that slide against each other, or articulate, in the new joint.
In knee implants, bearing surface options have been somewhat limited over the last few decades. The standard substance used for the femoral component is cobalt chrome, a metal alloy typified by its toughness and biocompatibility. However,even this high-quality industry standard has its shortcomings. Over time, this metal surface can become roughened by bone and bone cement particles trapped between the femoral component and the plastic tibial insert.
This roughened surface, when rubbing against the plastic component up to two million times per year, can more quickly wear out your implant. When that happens, you will have to undergo surgery to replace the plastic piece, the femoral component, and possibly even the tibial component. For this reason, implants have been shown to last between ten and fifteen years in the human body.
An exciting material to enter orthopaedics in recent years is OXINIUM ◊ Oxidized Zirconium. This remarkable material combines the strengths of ceramic and metal, such as wear-reduction and strength, but does not have the weaknesses, such as limited implant options and the possibility of fracture.
Zirconium is a biocompatible metal, similar to titanium. When the zirconium alloy undergoes a unique heating process, the surface of the metal transforms into a ceramic. Even though the new ceramic surface is 4,900 times more abrasion resistant than cobalt chrome, it retains the toughness and flexibility of the underlying metal.
Because it can achieve this remarkable reduction in implant wear without sacrificing strength as actual ceramic components do, oxidized zirconium implants have the potential to last significantly longer.
The Procedure
Knee replacement surgery typically takes between one and two hours to complete. This section will provide you with a brief, easy-to-understand description of the surgical procedure. (Please consult with your physician for details regarding your specific procedure.)
- An incision is made extending from the thigh, past the inside edge of the kneecap, and down to the shinbone.
- The end of the femur is shaped in preparation for sizing the femoral trial component.
- The top of the tibia is shaped for proper sizing of the tibial trial component.
- The trial units are put in place and the appropriate implant size is selected.
- The knee is assessed for alignment, stability, and range of motion.
- The underside of the kneecap is prepared and patella trial is selected.
- The trial units are removed and the final femoral, tibial, and patella components are implanted.
- The incision is closed, a drain is put in, and the post-operative bandaging is applied.

Bone Cuts

Implant Components

Implanted
All information provided on this website is for information purposes only. Every patient’s case is unique and each patient should follow his or her doctor’s specific instructions. Please discuss nutrition, medication and treatment options with your doctor to make sure you are getting the proper care for your particular situation. If you are seeking this information in an emergency situation, please call 911 and seek emergency help.
All materials copyright © 2020 Smith & Nephew, All Rights Reserved.

Sign up our newsletter to get update information, news or article about medical.

At Movement Orthopedics, we offer state-of-the-art treatment and urgent care for all your orthopedic needs.
- MEET THE PROVIDERS
- SPECIALTIES
- ONSITE SERVICES
- ORTHOPEDIC URGENT CARE
Bitcoin Payment
- PHYSICAL THERAPY
- CONTACT & LOCATION
- REQUEST AN APPOINTMENT
- PATIENT FORMS
Contact Info
- 43475 Dalcoma Drive Suite 250 | Clinton Township, MI 48038
- +(586) 436-3785
- +(586) 273-0109
- 36555 26 Mile Road Suite #2400 Lenox MI 48048
- Privacy Policy
- Powered by Smash Creative
Subscribe Free Magazine eNewsletter Checkout

JOURNEY II BCS Knee System Demonstrates Improved Patient Outcomes, Lower Healthcare Costs
Reduced cost is equivalent to approximately 10 percent in savings to the overall procedure price.

- Fifty-one percent less likely to be readmitted to the hospital within 30 days;
- Thirty-five percent more likely to be discharged to their home; and
- Forty-one percent less likely to be discharged to a skilled nursing facility for further care.
Related Features
Built to last: a roundtable on orthopedic implant manufacturing, will additive manufacturing revolutionize orthopedic product manufacture, study: attune knee linked to improved quality of life & reduced hospital stay, zimmer biomet announces fda clearance of the persona trabecular metal tibia, former alere executive named ceo of smith & nephew.
- CONMED Promotes Patrick Beyer to Newly Created COO Role
- Blue Arbor Gets FDA Breakthrough OK for Neuromuscular Interface
- FDA Clears SAIL Fusion's BowTie Sacroiliac Fusion System
- Accelus Adds Two New Members to its Board
- First-in-Human Hyalex Knee Cartilage Treatments Completed
March/April 2024
- Extreme Fixes for Orthopedic Extremity Surgery
- Print Shop: Insights on Orthopedic Additive Manufacturing
- Molding Is Taking Its Place in Orthopedic Device Manufacturing
- A View of Mixed-Reality Tech's Future in Orthopedics
- Improving Patient-Specific Outcomes with In-Silico Trials
Cookies help us to provide you with an excellent service. By using our website, you declare yourself in agreement with our use of cookies. You can obtain detailed information about the use of cookies on our website by clicking on "More information”. Got It
- Privacy Policy
- Terms And Conditions

Latest Breaking News From Nutraceuticals World

Latest Breaking News From Coatings World

Latest Breaking News From Medical Product Outsourcing

Latest Breaking News From Contract Pharma

Latest Breaking News From Beauty Packaging

Latest Breaking News From Happi

Latest Breaking News From Ink World

Latest Breaking News From Label & Narrow Web

Latest Breaking News From Nonwovens Industry

Latest Breaking News From Orthopedic Design & Technology

Latest Breaking News From Printed Electronics Now
Copyright © 2024 Rodman Media. All rights reserved. Use of this constitutes acceptance of our privacy policy The material on this site may not be reproduced, distributed, transmitted, or otherwise used, except with the prior written permission of Rodman Media.
AD BLOCKER DETECTED Our website is made possible by displaying online advertisements to our visitors. Please consider supporting us by disabling your ad blocker.

Dr. Henry Backe is an integral part of the Orthopaedic Specialty Group, P. C. team for over 25 years. Dr. Backe’s exceptional surgical skills are complemented by a personable style and dedication to the highest quality patient outcomes and satisfaction. He is a board certified orthopaedic surgeon and is fellowship trained in the area of hand and wrist and joint replacement.
Knee Specialist In The Greater Fairfield & Shelton Areas
Dr. Henry Backe treats knee conditions at his offices in Fairfield and Shelton, Connecticut. Dr. Backe of Orthopaedic Specialty Group P. C. , is a specialty trained orthopaedic surgeon specializing in knee conditions and injuries. As a leader in Orthopaedics, Dr. Backe offers innovative and less-invasive treatment options and state-of-the-art technologies that benefit his patients in many ways.

FAQs on Journey II
The journey ii bcs knee.
Recent advances in biomedical engineering software have opened a new chapter on high performance knee implants.
One remarkable breakthrough has been the creation of the JOURNEY II BCS knee, a second-generation knee replacement that combines the stability and natural motion of the human knee with new low-friction materials that may extend the life of the implant.
While the lifespan of a knee implant is heavily influenced by the materials used to make it, the natural feeling of the implant during physical activity is dependent upon the way the patient’s muscles, ligaments and tendons are addressed during surgery and by the implant’s shape within the body after surgery.
As discussed previously in this booklet, the knee is a hinge joint, but it does not swing like a simple door hinge. It has a complex rotational motion that you don’t notice is there – but many patients know when it’s not there after total knee replacement. Traditional implants attempt to recreate this subtle swing-and-rotate action with either a rotating platform (a simple pivot point) within the implant or by requiring an angled alignment of the implant during surgery.
With these traditional knee replacement designs, the muscles and ligaments around your new joint have to work harder because the implant’s slightly unnatural shapes and resulting motion make these soft tissues move in unfamiliar, stressful ways. This leads to joint pain, muscle fatigue and the unnatural feeling patients experience while walking or bending in the months after their procedure.
The JOURNEY II BCS knee, on the other hand, is designed to reproduce the original internal shapes and angled forces of the human knee through its full range of motion – accommodating the swing-and-rotate of the joint with the same engineering principles your real knee currently uses. Because of this, your soft tissues don’t have to readjust to new shapes and forces after surgery and your stride can return to its natural rhythm.
The JOURNEY II BCS knee also reproduces the stability provided by your anterior cruciate ligament (ACL) and your posterior cruciate ligament (PCL). Your ACL and PCL are key to the stability of your real joint and contribute to natural motion when your knee is fully extended and fully bent. No other knee implant reproduces both functions.
Implant Components
In the knee replacement procedure, each prosthesis is made up of four parts.
The tibial component has two elements – a metal base and a plastic insert – and replaces and the top of the tibia (shin bone). This prosthesis is made up of a metal tray attached directly to the bone and a high-density plastic spacer that provides the bearing surface.
The femoral component replaces the bottom of the thigh bone or femur. This component also replaces the groove where the patella or kneecap rides.
The patellar component replaces the surface of the knee cap, which rubs against the femur. The patella protects the joint, and the resurfaced patellar button will slide smoothly on the front of the joint. In some cases, surgeons do not resurface the patella.
Bearing Surfaces
One of the keys to a successful implant is its ability to withstand the rigors of daily activity, and central to that is the quality of the artificial surfaces that slide against each other, or articulate, in the new joint.
In knee implants, bearing surface options have been somewhat limited over the last few decades. The standard substance used for the femoral component is cobalt chrome, a metal alloy typified by its toughness and biocompatibility. However,even this high-quality industry standard has its shortcomings. Over time, this metal surface can become roughened by bone and bone cement particles trapped between the femoral component and the plastic tibial insert.
This roughened surface, when rubbing against the plastic component up to two million times per year, can more quickly wear out your implant. When that happens, you will have to undergo surgery to replace the plastic piece, the femoral component, and possibly even the tibial component. For this reason, implants have been shown to last between ten and fifteen years in the human body.
An exciting material to enter orthopaedics in recent years is OXINIUM ◊ Oxidized Zirconium. This remarkable material combines the strengths of ceramic and metal, such as wear-reduction and strength, but does not have the weaknesses, such as limited implant options and the possibility of fracture.
Zirconium is a biocompatible metal, similar to titanium. When the zirconium alloy undergoes a unique heating process, the surface of the metal transforms into a ceramic. Even though the new ceramic surface is 4,900 times more abrasion resistant than cobalt chrome, it retains the toughness and flexibility of the underlying metal.
Because it can achieve this remarkable reduction in implant wear without sacrificing strength as actual ceramic components do, oxidized zirconium implants have the potential to last significantly longer.
The Procedure
Knee replacement surgery typically takes between one and two hours to complete. This section will provide you with a brief, easy-to-understand description of the surgical procedure. (Please consult with your physician for details regarding your specific procedure.)
- An incision is made extending from the thigh, past the inside edge of the kneecap, and down to the shinbone.
- The end of the femur is shaped in preparation for sizing the femoral trial component.
- The top of the tibia is shaped for proper sizing of the tibial trial component.
- The trial units are put in place and the appropriate implant size is selected.
- The knee is assessed for alignment, stability, and range of motion.
- The underside of the kneecap is prepared and patella trial is selected.
- The trial units are removed and the final femoral, tibial, and patella components are implanted.
- The incision is closed, a drain is put in, and the post-operative bandaging is applied.
Ready to Live Pain Free?
Schedule an appointment with Dr. Henry Backe today!
PROFESSIONAL AFFILIATIONS

OUR LOCATION
305 Black Rock Turnpike Fairfield, CT 06825 Phone: (203) 337-2600
760 River Road Shelton, CT 06484 Phone: (203) 337-2600
OUR LOCATIONS
AREAS OF EXPERTISE
Hand Conditions & Treatments Knee Conditions & Treatments Hip Conditions & Treatments Sports Medicine Conditions & Treatments
- Robotic Assisted UKA
- Robotic Assisted TKA
- Robotic Assisted Revision Knee
- Computer Guided THA
- Data Visualization
- Partial Knee
- Primary Knee
- Revision Knee
- Oxinium™ in Knee
- VISIONAIRE™ Technology
- Primary Hip
- Revision Hip
- Oxinium™ in Hip
- PICO™
The JOURNEY II Bi-Cruciate Stabilized (BCS) Total Knee System
Watch a live surgical webcast featuring the Smith+Nephew JOURNEY II Bi-Cruciate (BCS) Total Knee System. On December 11, 2013, at 6:30pm EST, Steven Haas, MD, from the Hospital for Special Surgery, will perform the procedure. Fred Cushner, MD, Director of ISK, and designer of the JOURNEY II BCS will moderate the surgery, and Dave Mayman, MD, from the Hospital for Special Surgery will also participate from CCJR in Orlando, FL. The goal of the JOURNEY II BCS is to enable a higher level of function for total knee replacement patients – to not only relieve pain, but help them regain active lifestyles. Function, motion and durability are achieved through the unique features of the JOURNEY II BCS system-anatomic alignment, kinematics and advanced bearings.
December 11, 2013

Related Presenters

Fred Cushner, MD
Orthopaedic Surgeon
Fred D. Cushner, M.D. completed a fellowship in adult reconstruction and sports medicine at the Insall Scott Kelly Institute. Dr. Cushner remained on staff and is currently Director of this prestigious Institute.Dr. Cushner's practice ...
Steven B. Haas, MD
Dr. Steven B. Haas received his education and training at Harvard, Cornell and the University of Rochester. He is Chief of the Knee Service at Hospital for Special Surgery. Dr. Haas speaks extensively both nationally and internationally ...

David Mayman, MD
Dr. David Mayman is one of a handful of national experts in computer navigation in hip and knee replacement surgery. He performs over 700 computer-navigated joint replacement surgeries a year. "I believe that in the future all joint replacement ...
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.13(1); 2023

Original research
Comparison of the journey ii bicruciate stabilised (jii-bcs) and genesis ii total knee arthroplasty for functional ability and motor impairment: the capability, blinded, randomised controlled trial, iain mcnamara.
1 Norfolk and Norwich University Hospital, Norwich, UK
2 University of East Anglia, Norwich, UK
Valerie Pomeroy
Allan b clark.
3 Norwich Medical School, University of East Anglia, Norwich, UK
Graham Creelman
4 Mental Health Act Review Panels, Norfolk and Suffolk, UK
Celia Whitehouse
5 Department of clinical neurosciences, University of Cambridge, Cambridge, UK
Toby O Smith
6 Faculty of Medicine and Health Sciences, University of East Anglia, Norwich, UK
Juliet High
7 Norwich Clinical Trials Unit, Norwich, UK
Ann Marie Swart
8 Health Sciences, University of East Anglia, Norwich, UK
Celia Clarke
Associated data.
bmjopen-2022-061648supp001.pdf
Data are available on reasonable request. Reasonable requests for data will be considered by the trial team.
To determine if a newer design of total knee replacement (TKR) (Journey II BCS) produces superior patient-reported outcomes scores and biomechanical outcomes than the older, more established design (Genesis II).
Patients were recruited from an NHS University Hospital between July 2018 and October 2019 with surgery at two sites. Biomechanical and functional capacity measurements were at a University Movement and Exercise Laboratory.
Participants
80 participants undergoing single-stage TKR.
Interventions
Patients were randomised to receive either the Journey II BCS (JII-BCS) or Genesis II TKR.
Primary and secondary outcome measures
Primary outcome was the Oxford Knee Score (OKS), at 6 months. Secondary outcomes were: OKS Activity and Participation Questionnaire, EQ-5D-5L and UCLA Activity scores, Timed Up and Go Test, 6 min walk test, lower limb kinematics and lower limb muscle activity during walking and balance.
This study found no difference in the OKS between groups. The OKS scores for the JII-BCS and Genesis II groups were mean (SD) 42.97 (5.21) and 43.13 (5.20) respectively, adjusted effect size 0.35 (-2.01,2.71) p=0.771
In secondary outcome measures, the Genesis II group demonstrated a significantly greater walking range-of-movement (50.62 (7.33) vs 46.07 (7.71) degrees, adjusted effect size, 3.14 (0.61,5.68) p=0.02) and higher peak knee flexion angular velocity during walking (mean (SD) 307.69 (38.96) vs 330.38 (41.40) degrees/second, adjusted effect size was 21.75 (4.54,38.96), p=0.01) and better postural control (smaller resultant centre of path length) during quiet standing than the JII-BCS group (mean (SD) 158.14 (65.40) vs 235.48 (176.94) mm, adjusted effect size, 59.91 (–105.98, –13.85) p=0.01.).
Conclusions
In this study population, the findings do not support the hypothesis that the Journey II BCS produces a better outcome than the Genesis II for the primary outcome of the OKS at 6 months after surgery.
Trial registration number
ISRCTN32315753 .
STRENGTHS AND LIMITATIONS OF THIS STUDY
- This is a two arm, superiority, observer-blind, participant-blind and clinical staff-blind, randomised control trial.
- It uses a wide variety of patient reported outcomes measures and biomechanical measurements to determine if one implant is superior to the other
- The required sample size was achieved with only one person lost to follow-up.
- A potential limitation is the relatively large number of secondary outcomes.
- The surgeons all had a much greater familiarity with the implantations of Genesis II implants.
Original protocol for the study is mentioned here: https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-020-4143-4 .
Introduction
Despite total knee replacement (TKR) being a recommended surgical treatment for end-stage knee osteoarthritis, 1 up to 34% of all patients following TKR have poor functional outcomes. 2–6 With estimates of osteoarthritis of the knee affecting one in eight people in the USA 7 and 250 million individuals worldwide 8 the number of patients with intrusive symptoms after surgery is significant.
Multiple changes in implant design have been introduced to try to improve patient outcomes and while some implant design alterations have led to improvements in patient-reported outcome measures (PROMS) 9–11 and kinematics 12 13 not all have led to differences. 14–20
The Genesis II (Smith & Nephew, Memphis, Tennessee, USA) TKR has been reported to have good survivorship and patient satisfaction 13 21 and is commonly used in the UK 22 An evolutionary design, the Journey II BCS (JII-BCS; Smith & Nephew), also manufactured by Smith and Nephew, has been developed to improve kinematic outcome compared with the Genesis II by using a bicruciate design. 23 This design change has been supported by encouraging fluoroscopic studies. However, to date, no randomised controlled trials (RCTs) have been conducted to assess if there is a difference in the outcome compared with its predicate design. 24
This trial aimed to assess whether the JII-BCS would produce better patient reported and movement outcomes than the Genesis II.
The published protocol included the aims for investigating: the rotational profile around the native knee and following TKR; and patients’ experiences and surgeons’ experiences. 25 These findings will be reported in subsequent manuscripts.
Trial design, randomisation, blinding to intervention allocation, ethics and registration
A two-arm, superiority RCT comparing the JII-BCS knee implant (experimental intervention) to the Genesis II knee implant (control intervention) was performed. The trial was observer-blind, participant-blind and clinical staff-blind. Only the operating surgeon and theatre team knew which implant was used for an individual participant.
Trial participants were assigned to either the JII-BCS or Genesis II group using a computer-generated, 1:1 randomisation schedule stratified by site and age (<60 years = younger; ≥60 years = older). 26 27 Group allocation was revealed using REDCap, 28 29 the interactive web-randomisation system, to a member of the research team who was not involved in either the clinical care or assessments of any participant. Allocation was concealed from the surgical team until after the preoperation baseline measures were completed.
Sample size
The sample size was calculated from the Oxford Knee Score (OKS, primary outcome measure). 30 The RCT was powered at 80% with a 5% significance level to detect a minimally important clinical difference of five points 31 32 with an SD of 7.4 points. 33 Accounting for an estimated attrition rate of 10% at 6 months postsurgery the estimated sample size was 80 participants (40 per group).
Participants, setting and recruitment
Full eligibility criteria are provided in the published protocol. 25 In brief, participants were aged at least 18 years and met the clinical and radiological criteria for a single-stage TKR. People were excluded if they: had a fixed-flexion deformity of at least 15° or non-correctable varus/valgus deformity of at least 15°; had inflammatory arthritis or previous septic arthritis; had previous surgery to the collateral ligaments of the affected knee; had a contralateral TKR implanted less than 1 year earlier; had severe comorbidity that could present an unacceptable safety risk or were pregnant; were a private patient; were likely to be living outside the clinical centre catchment area at 6 months postsurgery or were enrolled on another clinical trial.
Patients were recruited at a university teaching hospital with surgery conducted at two sites. Outpatient physiotherapy was conducted in a single hospital. The Movement and Exercise Laboratory at the associated University (MoveExLab) was the setting for measures of functional capacity and biomechanics.
All participants received routine NHS care for people with TKR irrespective of the implant received. This included following a standard postoperative rehabilitation of outpatient physiotherapy centred on knee strength and range of motion (ROM) exercises within the first 6 weeks after surgery. Patients received the same physiotherapy protocols and classes.
Experimental intervention
Participants in the experimental group received the JII-BCS. The JII-BCS is a dual-cam post designed to substitute for both the anterior cruciate ligament and posterior cruciate ligament. In addition the femoral and tibial components are asymmetric and the polyethylene insert is a medially concave and laterally convex shape. The device is designed to provide guided motion, and thus improve knee kinematics, and increase anteroposterior stability throughout knee flexion.
Control intervention
- Participants in the control group received the Genesis II (Smith and Nephew), posterior stabilised (PS) TKR. The design features specific to the implant and a lateralised trochlear groove to improve patellar contact and tracking, an externally rotated femoral implant design and an anatomically shaped tibial baseplates.
Surgical techniques
All four surgeons had extensive experience, at least 5 years, of the Genesis II implant. All undertook cadaveric training on the JII-BCS and declared that they were competent in the surgical technique having completed their operative learning curve before starting the trial. Both implants are uncoated, cemented implants. The surgical procedure followed the standard manual surgical approach and technique through a medial parapatellar approach in all cases with intramedullary femoral and tibial rods to provide the alignment of the components. Patella resurfacing was used in both groups.
Data collection schedule
Data collection time points for the primary outcome measure were: at least 1 day before surgery (baseline), 7±2 days after surgery (1 week postoperatively), 6–8±2 weeks after surgery (2 months), 6 months±4 weeks after surgery (outcome, primary time point). Secondary outcomes were collected at baseline, 2 months and 6 months. Any differences from these time points are provided in the outcome measures section.
Outcome measures
Primary outcome measure.
The OKS was the primary outcome measure. This is a 12-question patient self-assessment of knee function and pain 30 with values ranging from 0 (worst outcome) to 48 (best outcome).
Secondary outcome measures
- The Oxford Knee Score Activity and Participation Questionnaire (OKS-APQ), which complements the OKS by assessing everyday activity and social participation. 34 The overall score is from 12 to 60 with 12 being the best outcome.
- The EQ-5D-5L is a self-report questionnaire consisting of five questions and a Visual Analogue Scale. Higher values indicate better quality of life. 35
- The UCLA Activity score (UCLA) to assess physical activity self-rating scale ranged from 0 (complete inactivity) to 10 (participation in impact sport).
- Timed Up and Go Test (TUG)—seconds to rise from chair, walk 3 m and return to sitting; mean of three trials. 36 The reported minimal detectable change after TKR is 2.27 s. 37 A lower value indicates better function.
- Six min walk test—metres walked in 6 min around a 20 m circuit. 38 39 The reported minimal detectable change from baseline after TKR is 26 metres. 40 A higher value indicates greater function.
- Modified Star-Excursion Test 41 (cm/leg length) where larger values indicate better balance.
For these simultaneous measures, participants wore shorts and were bare-footed. Reflective sensors were placed in accordance with the Plug-In Gait model (Vicon) for the lower limb and three-dimensional motion data were collected, at 100 HZ, with eight wall-mounted infrared cameras (Vicon Motion System, Oxford, UK). Three embedded force plates (BERTEC, Ohio, USA) were used to collect kinetic data at 2000 Hz for walking tasks and 100 Hz for balance tasks. Surface electromyographic sensors (EMG: Delsys) were placed bilaterally on the Vastus Medialis, Vastus Lateralis, Tibialis Anterior, Bicep Femoris and lateral head of the Gastrocnemius following SENIAM guidance. EMG data were collected at 2000 Hz.
For walking tasks, participants were asked to walk in a straight line along a 10 m walkway at their self-selected speed. For double stance balance activities, participants were instructed to stand with their feet shoulder-width apart. For single stance balance activities, participants were instructed to stand on one leg with hands-on-hips. Three trials of 10 s were recorded for each activity.
For the stair ambulation task, participants were asked to complete six ascents and six descents all unaided, leading with the operated limb for three trials and the non-operated limb for the remainder. The stairs had four steps. The first step was 16.5 cm, and the others were 15 cm high. Handrails were available if participants needed support.
Movement data were processed in accordance with the Vicon Plug-in Gait Model (Oxford Metrics, Oxford, UK). Raw EMG was filtered with pass bands at 10 and 500 Hz, rectified and low pass filtered using a fourth order Butterworth with a 10 Hz cut-off. Walking data were normalised to 101 data points for the gait cycle. Three trials of tasks were used to create a mean for each measure per participant. Values were extracted using a purpose-built MATLAB script. Data were processed by motion analysis experts in the research team.
The JII-BCS is expected to provide more normal kinematics during knee movement than Genesis II due to the design changes discussed earlier. Other authors have indicated that the femo-tibial relationship may be more normal during deep knee bend 42 and more stable during walking 43 Accordingly, people with the Journey prosthesis may 44 45 or may 43 have greater knee ROM, may walk faster, 46 47 and may have a longer stride length 46 47 than people receiving a comparison knee replacement. In addition, greater stability of the femur on the tibia could produce greater knee flexion angular velocity as dynamic knee loading could be more normal. However, there is only one non randomised study of 18 patients comparing the JII-BCS directly with the Genesis II. 45 Based on the available literature, the hypothesis driving the kinematic investigation was that people receiving the JII-BCS compared with those receiving the Genesis II would have greater walking velocity, step-length symmetry (resulting from longer stride length), knee ROM and peak knee flexion angular velocity.
- Walking speed (metres/second). A higher value indicates better performance
- Step length symmetry during walking. Step length ratio was calculated as ((2xOp)/Op+NOp))−1); where Op is the step length of the operated leg and NOp is the step length of the non-operated leg. Zero indicates perfect symmetry and best performance.
- Knee ROM during walking (degrees). Higher values indicate better performance.
- Peak knee flexion angular velocity during walking (degrees per second). This was inadvertently omitted from the statistical analysis plan (SAP). Higher value indicates better performance.
- Double stance support (% of gait cycle). It was planned to measure cadence, (steps/min), step length (m) and stride length (m). However, there is redundancy with the temporal-spatial gait parameters of walking speed and step length symmetry which are included in the primary movement performance measures.
- Peak extension and flexion moments of operated knee during the gait cycle (Nm/kg).
- Hip and ankle ROM during walking.
- Peak knee flexion angular velocity during stepping up onto a stair.
- Percentage of gait cycle for peak activation of Vastus Medialis, Vastus Lateralis, Tibialis Anterior, Biceps Femoris and Lateral head of Gastrocnemius (% of gait cycle).
- Balance measures were derived from kinetic data (from force plates) during standing still: single stance on the operated lower limb for 10 s with eyes open (yes/no) and duration maintained; resultant centre of pressure path length (COP cm) in double stance with eyes closed; and resultant COP velocity (cm/s) in double stance with eyes closed.
Clinical context and adverse events
Data on length of hospital stay and complications related to the surgery (eg, anaesthesia-related problems, bleeding, morbidities) were collected from a notes review. At each visit, participants were asked about their pain medication and if they had received additional treatment since their surgery/previous visit and what this entailed. Any need for revision surgery was recorded. All adverse events identified were tracked until resolution.
The SAP was finalised and agreed prior to database lock and analysis was completed blinded to group allocation ( online supplemental file ). For all outcomes the hypothesis tests and 95% CIs were two sided; and a p<0.05 was considered significant. An intention-to-treat analysis was conducted that is, all randomised participants regardless of their eligibility or adherence were analysed according to the treatment they were randomised to receive. The analysis was undertaken by the Trial Statistician using Stata V.16.
Supplementary data
For the primary outcome, the mean OKS at 6 months was compared between the control and experimental groups using a general linear model adjusting for site and age (<60 years/≥60 years). An adjusted analysis was conducted using the same model but adjusting for the OKS at baseline. The model assumptions were checked graphically, and sensitivity analysis done using a non-parametric bootstrap using 5000 repetitions.
All the other outcomes were analysed separately at 2 months and 6 months using the same general linear model specified above and a corresponding adjusted analysis. The exception was ability to balance for 10 s. This was analysed using a logistic regression model adjusting for site and age.
Patient and public involvement
A patient representative, who had previously undergone knee replacement surgery, was involved in the protocol development, assessment of the burden of the intervention and time taken to participate in the research and oversight of the trial as a member the trial management group. The representative also contributed to the planning and writing of research dissemination materials.
Participants were recruited between July 2018 and October 2019. Last follow-up visits were in October 2020 with some impact and delayed visits due to COVID-19.
In the published protocol, 25 the analysis plan included a per-protocol and safety analysis. This was not undertaken as the implants were used as intended so these populations would be the same as the intention-to-treat population.
Flow of participants through the trial
In total, 105 of 153 people screened were eligible to take part, 16 declined participation and eight were excluded for other reasons. Therefore, 81 of 153 people (53%) were recruited. All participants in the Genesis II group (n=40) received their allocated intervention. In the JII-BCS group (n=41), one participant withdrew prior to surgery (postrandomisation exclusion). Full details are in the Consolidated Standards of Reporting Trials (CONSORT) flow chart ( figure 1 ).

Consolidated Standards of Reporting Trials (CONSORT) diagram.
Participant characteristics
There were no discernible baseline differences between the groups ( table 1 ).
The baseline characteristics of participants
EQ-5D-5L is a measure of health-related quality of life, in the range of −0.109 (worst possible state) and 1.0 (perfect health), anchored at 0 (death).
EQ-VAS is a health state assessment ranging between 0 and 100, in which 0 is worst imaginable health state and 100 is best imaginable health state.
OKS is a 12-item knee function assessment, ranging from 0 (worst score) to 48 (best score).
Timed Up and Go Test—seconds to rise from chair, walk 3 m and return to sitting; mean of three trials. A lower value indicates better function.
Six min walk test—metres walked in 6 min around a 20 m circuit A higher value indicates greater function.
The UCLA Activity score to assess physical activity self-rating scale ranged from 0 (complete inactivity) to 10.
*Thirt-nine participants.
†Thirt-eight participants.
Primary outcome comparison: 6 months postoperatively
The OKS scores for the JII-BCS and Genesis II groups were mean (SD) 42.97 (5.21) and 43.13 (5.20), respectively. There was no significant difference between the groups: adjusted effect size 0.35 (−2.01,2.71) p=0.771 ( table 2 ).
Oxford Knee Scores (OKS, primary outcome), from baseline to 6 months after surgery (primary time point)
Journey II BCS (JII-BCS)
*Adjusted for strata used in randomisation and for baseline scores.
APQ, Activity and Participation Questionnaire; VAS, Visual Analogue Scale.
Secondary outcome comparisons: 6 months postoperatively
Patient-reported outcome questionnaires.
There were no differences between the two groups for any of the secondary patient reported outcomes ( online supplemental tables S1 ).
Walking and balance functional ability
There was no difference between the JII-BCS and Genesis II groups in the time to complete the TUG Test or the distance covered in the 6 min walk test ( online supplemental table S2 ). The Star-Excursion Test was attempted by all participants but 59% of participants at baseline, 59% at follow-up and 63% at outcome were unable to complete it ( online supplemental table S3 ). Therefore, statistical analysis was not undertaken.
Movement performance during walking and balance
The primary movement performance measures are reported in table 3 . In summary at 6 months postsurgery, the Genesis II group had a significant advantage for knee ROM and peak knee flexion angular velocity during walking. There were no differences between the groups for walking speed or peak flexion angular knee velocity on stair climbing.
Movement performance primary measures during walking from baseline to 6 months postsurgery (primary time point): walk speed, step length symmetry, knee range of motion (ROM) and peak knee flexion angular velocity
Step length symmetry—step length ratio calculated as ((2xOp)/Op+NOP))−1); where Op is the step length of the operated leg and NOP is the step length of the non-operated leg. Zero indicates perfect symmetry and best performance.
Bold text is used to denote values achieving statisitcal significance
Data for all secondary movement performance measures are provided in online supplemental tables S4–S8 . The only difference between groups that reached statistical significance was for COP path length in double stance with eyes closed ( online supplemental table S7 ). The mean (SD) values for the Genesis II and JII-BCS groups were 158.14 (65.40) mm and 235.48 (176.94) mm, respectively. Adjusted effect size was −59.91 (–105.98, –13.85) p=0.01 in favour of the Genesis II group.
Postoperative clinical context
There were no between-group significant differences for: length of stay, change in pain medication from randomisation or physiotherapy received ( online supplemental tables S9 and S10 ).
Adverse events
One patient with a JII-BCS developed acute swelling and pain in the knee and was systemically unwell at 4 months postoperatively. The joint aspiration demonstrated turbid fluid and an exchange of the polyethylene spacer and retention of the femoral and tibial components (Debridement And Implant Retention) was performed with postoperative antibiotic treatment. Subsequent microbiology was negative so infection was never conclusively demonstrated. The numbers and type of complications are reported in online supplemental table S11 .
The findings do not support the hypothesis that the JII-BCS produces a better outcome than the Genesis II for the primary outcome of the OKS at 6 months after surgery. No differences between groups were also found for: other patient-reported outcomes; measures of balance and walking function; hip and ankle ROM; knee moments during walking; double support time during walking and percentage of gait cycle for peak muscle activation. However, significant advantages for the control group (Genesis II) were found for: operated knee range-of-movement and peak knee flexion angular velocity during walking, and postural control (COP path length).
While some investigators have demonstrated differences between generations of knee designs 12 not all modern generation TKR designs have demonstrated an improvement in outcomes when compared with their predecessors. 15–20 48 One possible reason for this is that the predecessor is already producing good results and therefore is difficult to improve on. Regarding the JII-BCS, at the time of writing, only Bialy et al 45 have directly compared the Genesis II and the JII-BCS. Their study was non randomised and consisted of 18 patients between the two groups. They reported a greater supine range of movement of the JII-BCS compared with the Genesis II when measured with a long arm goniometer. They also reported an improvement in functional knee scores and stability when balancing. Their conclusions were that the JII-BCS restores more normal anatomy and kinematics which is correlates into the improvements that they found. None of the other papers reporting outcomes of the JII-BCS compared the JII-BCS to the Genesis II, none used a randomised design and none used methodology or outcomes that could be compared with the methodology used in this trial. 42–46 However, on the basis of the available literature, we measured outcomes that would be expected to be difference on the basis of the available literature, walking velocity, step-length symmetry (resulting from longer stride length), knee ROM and peak knee angular velocity.
Within our trial, we found differences in some biomechanical measures of motor impairment but not for others; patient-reported outcomes; and, walking and balance function. It is possible that knee range-of-movement during walking, walking symmetry, peak knee flexion angular velocity during walking and postural control (COP path length) are detecting motor impairment improvement for the Genesis II group and/or because statistical significance was a result of testing multiple outcomes. The latter explanation is clearly possible but knee range-of-movement is greater for people reporting good outcome after knee replacement than for those reporting poor outcome. 49 Moreover, knee range-of-movement has been found to be the main biomechanical effect of TKR 50 and to improve over time while other biomechanical measures do not. 50 51 Likewise, postural control improves over time 52 53 and approaches healthy control values. 52 Importantly, gait symmetry is an indicator of walking control 54 and, while of borderline statistical significance (p=0.05) can possibly detect differences following insertion of different prostheses. Peak knee angular velocity during walking is also an indicator of walking control 55 and has been found to change beneficially after insertion of the Genesis II prosthesis. 50 These findings indicate that secondary, in-depth, analysis of the biomechanical data should be undertaken.
A potential limitation is the relatively large number of secondary outcomes. However, this is also a strength as it ensured comprehensive examination of the potential impact of TKR on functional ability, motor impairment and health-related quality of life. Another potential limitation is that the surgeons all had a much greater familiarity with the Genesis II implants. However, all surgeons were very experienced with the Genesis II implant with at least 10 years of experience implanting the device. All surgeons received thorough training with the JII-BCS and the surgical technique and instrumentation are similar for both devices with only one additional femoral cut being necessary for the JII-BCS compared with the Genesis II. A key strength of this trial is that the required sample size was achieved with only one person lost to follow-up. Other strengths include minimisation of selection bias through a robust randomisation procedure and use of double blinding to minimise interpretation bias.
The lack of difference between implant designs is important for patients, surgeons, healthcare providers and implant companies. For the patient and surgeons, reassurance can be gained that older designs, with proven track record of function and survivorship, can provide the same patient reported and functional outcome as more modern designs. For the healthcare providers, older implants are often less expensive and, in the absence of clinical benefit with and demonstrable longevity, if the additional expenditure on more modern designs is avoided for the hundreds of thousands of patients undergoing surgery worldwide the cost savings are potentially significant. Finally, for the implant companies, it is more likely than not than implant design has reached a point when non-implant-related factors play a more important role in patient outcome. The future of design and innovation may come in the form of more modern surgical techniques such as robotic assisted implantation to assist in placing the knee in a more kinematically sympathetic position which in turn may allow the newer design philosophies to positively influence outcome. It is possible, only then in combination with modern surgical techniques, that improvements in patient outcomes can be realised but well-constructed surgical trials will need to answer such questions.
This study demonstrated no difference between the Genesis II and its successor the JII-BCS for PROMS, walking function, temporal-spatial gait parameters, balance ability and lower limb kinematic results at 6 months follow-up. However, significant advantages were seen in for the Genesis II in the operated knee range-of-movement, peak knee flexion angular velocity during walking and postural control.
Supplementary Material
Acknowledgments.
The team would like to thank all the participants and families who gave their time to be part of this study; Antony Colles, Martin Pond and the NCTU data management team; Estelle Payerne; Amanda Thacker; NNUH sponsorship team and the safety monitoring committee members, Prof Marcus Flather and Prof Simon Donell. Also: Mr Charles Mann, Mr Nish Chirodian, Mr David Calder, Dr Nicola Hancock, Nursing and clinic staff at the Spire Hospital and NNUH, Prof Andoni Toms and the Radiology department at NNUH and Addenbrooke’s hospital, Cambridge, Dr Simon Horton and Dr Anne Killett
Twitter: @tobyosmith
Contributors: IM and VP drafted this paper. IM is the guarantor. All authors (IM, VP, ABC, GC, CW, JW, BH, TOS, JH and AMS) contributed to revisions of the manuscript, read and approved the final manuscript. All authors (IM, VP, ABC, GC, CW, JW, BH, TO, JH and AMS) contributed to the development of the trial protocol as well as conception or design of the work; the acquisition, analysis or interpretation of data for the work.
Funding: This work was supported by an investigator initiated grant from Smith and Nephew, with both types of knee replacements supplied at the same cost.
Disclaimer: The funders had no role in the design of the study, the data collection, the data analysis, interpretation of data, or writing of the manuscript.
Competing interests: The trial was funded by Smith and Nephew via an unrestricted grant, administered by the Sponsor NNUH. Funding was used within NNUH for running the trial. Funds were provided via NNUH to UEA for the members of the trial team based in the movement and Exercise Laboratory (MoveExLab) at UEA and the clinical trials unit (CTU) based at UEA for statistics, and trial and data management.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Ethics statements, patient consent for publication.
Not applicable.
Ethics approval
This study involves human participants and was approved by East of England – Cambridge Central Research Ethics Committee (reference 16/EE/0230). Participants gave informed consent to participate in the study before taking part.
JOURNEY II – Total Knee Replacement
The JOURNEY II BCS Knee
Recent advances in biomedical engineering software have opened a new chapter on high performance knee implants.

One remarkable breakthrough has been the creation of the JOURNEY II BCS knee, a second-generation knee replacement that combines the stability and natural motion of the human knee with new low-friction materials that may extend the life of the implant.
While the lifespan of a knee implant is heavily influenced by the materials used to make it, the natural feeling of the implant during physical activity is dependent upon the way the patient's muscles, ligaments and tendons are addressed during surgery and by the implant's shape within the body after surgery.
As discussed previously in this booklet, the knee is a hinge joint, but it does not swing like a simple door hinge. It has a complex rotational motion that you don't notice is there - but many patients know when it's not there after total knee replacement. Traditional implants attempt to recreate this subtle swing-and-rotate action with either a rotating platform (a simple pivot point) within the implant or by requiring an angled alignment of the implant during surgery.
With these traditional knee replacement designs, the muscles and ligaments around your new joint have to work harder because the implant's slightly unnatural shapes and resulting motion make these soft tissues move in unfamiliar, stressful ways. This leads to joint pain, muscle fatigue and the unnatural feeling patients experience while walking or bending in the months after their procedure.
The JOURNEY II BCS knee, on the other hand, is designed to reproduce the original internal shapes and angled forces of the human knee through its full range of motion - accommodating the swing-and-rotate of the joint with the same engineering principles your real knee currently uses. Because of this, your soft tissues don't have to readjust to new shapes and forces after surgery and your stride can return to its natural rhythm.
The JOURNEY II BCS knee also reproduces the stability provided by your anterior cruciate ligament (ACL) and your posterior cruciate ligament (PCL). Your ACL and PCL are key to the stability of your real joint and contribute to natural motion when your knee is fully extended and fully bent. No other knee implant reproduces both functions.
Implant Components

In the knee replacement procedure, each prosthesis is made up of four parts.
The tibial component has two elements - a metal base and a plastic insert - and replaces and the top of the tibia (shin bone). This prosthesis is made up of a metal tray attached directly to the bone and a high-density plastic spacer that provides the bearing surface.
The femoral component replaces the bottom of the thigh bone or femur. This component also replaces the groove where the patella or kneecap rides.
The patellar component replaces the surface of the knee cap, which rubs against the femur. The patella protects the joint, and the resurfaced patellar button will slide smoothly on the front of the joint. In some cases, surgeons do not resurface the patella.
Bearing Surfaces
One of the keys to a successful implant is its ability to withstand the rigors of daily activity, and central to that is the quality of the artificial surfaces that slide against each other, or articulate, in the new joint.
In knee implants, bearing surface options have been somewhat limited over the last few decades. The standard substance used for the femoral component is cobalt chrome, a metal alloy typified by its toughness and biocompatibility. However,even this high-quality industry standard has its shortcomings. Over time, this metal surface can become roughened by bone and bone cement particles trapped between the femoral component and the plastic tibial insert.
This roughened surface, when rubbing against the plastic component up to two million times per year, can more quickly wear out your implant. When that happens, you will have to undergo surgery to replace the plastic piece, the femoral component, and possibly even the tibial component. For this reason, implants have been shown to last between ten and fifteen years in the human body.
An exciting material to enter orthopaedics in recent years is OXINIUM ◊ Oxidized Zirconium. This remarkable material combines the strengths of ceramic and metal, such as wear-reduction and strength, but does not have the weaknesses, such as limited implant options and the possibility of fracture.
Zirconium is a biocompatible metal, similar to titanium. When the zirconium alloy undergoes a unique heating process, the surface of the metal transforms into a ceramic. Even though the new ceramic surface is 4,900 times more abrasion resistant than cobalt chrome, it retains the toughness and flexibility of the underlying metal.
Because it can achieve this remarkable reduction in implant wear without sacrificing strength as actual ceramic components do, oxidized zirconium implants have the potential to last significantly longer.
The Procedure
Knee replacement surgery typically takes between one and two hours to complete. This section will provide you with a brief, easy-to-understand description of the surgical procedure. (Please consult with your physician for details regarding your specific procedure.)
An incision is made extending from the thigh, past the inside edge of the kneecap, and down to the shinbone.
The end of the femur is shaped in preparation for sizing the femoral trial component.
The top of the tibia is shaped for proper sizing of the tibial trial component.
The trial units are put in place and the appropriate implant size is selected.
The knee is assessed for alignment, stability, and range of motion.
The underside of the kneecap is prepared and patella trial is selected.
The trial units are removed and the final femoral, tibial, and patella components are implanted.
The incision is closed, a drain is put in, and the post-operative bandaging is applied.
All information provided on this website is for information purposes only. Every patient's case is unique and each patient should follow his or her doctor's specific instructions. Please discuss nutrition, medication and treatment options with your doctor to make sure you are getting the proper care for your particular situation. If you are seeking this information in an emergency situation, please call 911 and seek emergency help.
All materials copyright © 2020 Smith & Nephew, All Rights Reserved.
You are using an outdated browser. Please upgrade your browser to improve your experience.

The Journey II Total Knee System: A Step Ahead – An Evolutionary New Design
Richard “alex” sweet ii, md, kate s. hamilton, pa-c, richard a. sweet, m.d. (retired 2022).
HOW THE NORMAL KNEE WORKS: It is a common misconception that the human knee functions as a simple hinge joint, with straight up and down flexion and extension. In reality the motion of the knee is much more complex, with six degrees of motion (not just the two of a hinge). As the knee bends and straightens, it also rotates internally and externally and slides front to back. Traditional total knee replacement designs have never been able to recreate the complex movement necessary for the knee to feel and function normally, especially in the high demand situations of a physical job or performing athletics.
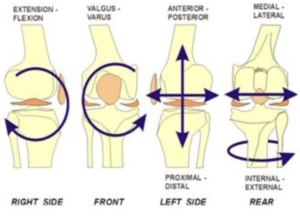
The Journey II Total Knee Medial Pivot Design The “ Normal Feeling ” Knee Replacement
The Journey II Knee is a revolutionary new knee replacement design. It incorporates several new design changes, the most significant of which is Medial Pivot design. These design changes include:
MEDIAL PIVOT DESIGN: A revolutionary new concept. It is the first true major design advancement in knee replacement surgery in decades. The Medial Pivot Design is the first TKR design to incorporate all 6 degrees of motion of the natural knee. It does so by creating a “cupped” almost ball-in-socket articulation between the plastic and the femur on the medial side of the joint (blue arrow) and a flat articulation between the plastic and the femur on the lateral side joint (red arrow). The resultant kinematics (mechanics) are such that the “ball in socket” articula-tion on the inside of the joint keeps the femur centered in one spot as the knee bends, while the “flat” articulation on the outside of the knee allows lateral femur to glide backwards and rotate like the normal knee. The result: normal kinematics are restored in the Medial Pivot Design TKR.
GREATER STABILITY: An added inherent benefit of the medial ball-in-socket “cupping” of the Medial Pivot design is that it improves front-to-back knee stability vs that of the conventional TKR. Given that the ACL is sacrificed in all TKR surgery, the added front-to-back stability of the Medial Pivot design is a crucial improvement.
NORMAL ANATOMY RESTORED: The Journey II re-establishes the subtleties of normal joint line anatomy (which are altered by the arthritis process and not corrected by conventional TKR surgery.

IMPROVED QUADRICEPS STRENGTH: The Journey II, as opposed to other TKR designs, moves the contact point between the femur and the tibia forward to its normal position (blue arrow right as compared to orange arrow of traditional TKA designs). Reestablishing this forward contact point results in increased quadriceps strength (like being on the long end of a teeter-totter) GREATER RANGE OF MOTION: The Journey II design changes the anatomy of the back of the femoral component to mimic that of the normal knee (blue arrow left). The result is to provide for an extra 15 degrees of flexion versus what is expected in a conventional TKR. The cumulative result of these design changes of the Journey II TKR is that patients experience a knee replacement with improved kinematics, speedier recovery, better ultimate range of motion, enhanced stability, and ultimate functional ability for high demand situations at full recovery.
Design Limitations of Past Conventional TKRs Conventional knee replacements work well at what they are designed to do: rid the patient of arthritis and provide a new artificial knee that will function adequately. As TKR surgery has expanded into younger more active age groups who place a higher demand on their new knee, the goal of only eliminating arthritic pain is no longer sufficient. Design limitations of the conventional knee replacement that can inhibit the return to normal functioning and can lead to patient dissatisfaction include: 1. ABNORMAL KINEMATICS: The knee is NOT a hinge. A conventional knee replacement forces the knee to flex and extend like a hinge on a door, with a straight simple up and down motion. The normal knee, however, does not function like a hinge. Instead, as it bends and straightens, there is flowing rotation and front to back sliding to its kinematics. Only the Journey II TKA recreates these kinematic movements. 2. ALTERED ANATOMY: With conventional knee replacement surgery, anatomy of the knee is altered in several ways. When looking at a normal knee from the front, the joint line is not perpendicular to the tibia as it is with conventional TKR surgery, but instead is at a slight angle with the inside of the joint being slightly lower than the outside. To compensate, the femur must be correspondingly rotated to keep the ligaments balanced. This can lead to abnormal forces on the knee, creating sensations of instability, dissatisfaction, and potential early failure of the knee replacement. 3. DIMINISHED QUADRICEPS STRENGTH: In conventional TKR surgery the contact point between the femur and tibia is shifted towards the back of the knee. This shift causes abnormal (called “paradoxical”) motion to occur when the knee starts to bend. The mechanical effect is that the strength of the quadriceps muscle is weakened. This is of clinical importance as a patient with a conventional TKR attempts to squat, climb steps, or perform other high demand activities.
Results of Conventional TKR Surgery Design Limitations: The result of the limitations noted above is that the ligaments and capsule of the knee see an altered knee anatomy, altered knee kinematics, and a weakened quadriceps muscle. This can cause a range of problems from:
- A patient perceiving a subtle sensation that the knee does not “feel normal”
- More significant problems such as less range of motion, reduced stability, a weak knee/quadriceps complex, intermittent soreness/swelling, problems with stair climbing, and difficulties engaging in recreational activities and vigorous work.
Conclusion The Journey II TKA is truly a revolutionary step forward in the design of total knee implants. With proper surgical technique and in the hands of a well-trained surgeon, the Journey II knee can produce results superior to the traditional total knee design. It is our goal as your surgical team to continue to improve our surgical techniques and to look for new advances in technology that allow us to give you the best result possible.
Louisville Orthopaedic Clinic
4130 Dutchman's Lane, Suite 300,Louisville 40207 (502) 897-1794
1425 State St., ,New Albany 47150 (812) 920-0408

- Elbow and Shoulder
- Foot and Ankle
- Hand and Wrist
- Neck and Back
- Center for Orthopedic Spine & Pain
- Hand Specialists
- Sports Medicine
- Total Joint Center
- Our Providers
- Physical Therapy
- Privacy Policy
- Areas Served
- Educational Videos
- Publications
- Patient Forms

- En Español

- Medical Devices
- Radiation-Emitting Products
- Vaccines, Blood & Biologics
- Animal & Veterinary
- Tobacco Products
Class 2 Device Recall JOURNEY II BCS
This website has been translated to Spanish from English, and is updated often. It is possible that some links will connect you to content only available in English or some of the words on the page will appear in English until translation has been completed (usually within 24 hours). We appreciate your patience with the translation process. In the case of any discrepancy in meaning, the English version is considered official. Thank you for visiting esp.fda.gov/tabaco.
JOURNEY II Total Knee Replacement
- Before Surgery
- Day of Surgery
- After Surgery
- Patient Forms (Read Only)
- Billing Information
- Good Faith Estimate
- Your Rights and Protections Against Surprise Medical Bills
- Patient’s Rights and Responsibilities
- Advance Directives
- Helpful Reminders
- In the News
The JOURNEY II BCS Knee
Recent advances in biomedical engineering software have opened a new chapter on high performance knee implants.

One remarkable breakthrough has been the creation of the JOURNEY II BCS knee, a second-generation knee replacement that combines the stability and natural motion of the human knee with new low-friction materials that may extend the life of the implant.
While the lifespan of a knee implant is heavily influenced by the materials used to make it, the natural feeling of the implant during physical activity is dependent upon the way the patient's muscles, ligaments and tendons are addressed during surgery and by the implant's shape within the body after surgery.
As discussed previously in this booklet, the knee is a hinge joint, but it does not swing like a simple door hinge. It has a complex rotational motion that you don't notice is there - but many patients know when it's not there after total knee replacement. Traditional implants attempt to recreate this subtle swing-and-rotate action with either a rotating platform (a simple pivot point) within the implant or by requiring an angled alignment of the implant during surgery.
With these traditional knee replacement designs, the muscles and ligaments around your new joint have to work harder because the implant's slightly unnatural shapes and resulting motion make these soft tissues move in unfamiliar, stressful ways. This leads to joint pain, muscle fatigue and the unnatural feeling patients experience while walking or bending in the months after their procedure.
The JOURNEY II BCS knee, on the other hand, is designed to reproduce the original internal shapes and angled forces of the human knee through its full range of motion - accommodating the swing-and-rotate of the joint with the same engineering principles your real knee currently uses. Because of this, your soft tissues don't have to readjust to new shapes and forces after surgery and your stride can return to its natural rhythm.
The JOURNEY II BCS knee also reproduces the stability provided by your anterior cruciate ligament (ACL) and your posterior cruciate ligament (PCL). Your ACL and PCL are key to the stability of your real joint and contribute to natural motion when your knee is fully extended and fully bent. No other knee implant reproduces both functions.
Implant Components

In the knee replacement procedure, each prosthesis is made up of four parts.
The tibial component has two elements - a metal base and a plastic insert - and replaces and the top of the tibia (shin bone). This prosthesis is made up of a metal tray attached directly to the bone and a high-density plastic spacer that provides the bearing surface.
The femoral component replaces the bottom of the thigh bone or femur. This component also replaces the groove where the patella or kneecap rides.
The patellar component replaces the surface of the knee cap, which rubs against the femur. The patella protects the joint, and the resurfaced patellar button will slide smoothly on the front of the joint. In some cases, surgeons do not resurface the patella.
Bearing Surfaces
One of the keys to a successful implant is its ability to withstand the rigors of daily activity, and central to that is the quality of the artificial surfaces that slide against each other, or articulate, in the new joint.
In knee implants, bearing surface options have been somewhat limited over the last few decades. The standard substance used for the femoral component is cobalt chrome, a metal alloy typified by its toughness and biocompatibility. However,even this high-quality industry standard has its shortcomings. Over time, this metal surface can become roughened by bone and bone cement particles trapped between the femoral component and the plastic tibial insert.
This roughened surface, when rubbing against the plastic component up to two million times per year, can more quickly wear out your implant. When that happens, you will have to undergo surgery to replace the plastic piece, the femoral component, and possibly even the tibial component. For this reason, implants have been shown to last between ten and fifteen years in the human body.
An exciting material to enter orthopaedics in recent years is OXINIUM ◊ Oxidized Zirconium. This remarkable material combines the strengths of ceramic and metal, such as wear-reduction and strength, but does not have the weaknesses, such as limited implant options and the possibility of fracture.
Zirconium is a biocompatible metal, similar to titanium. When the zirconium alloy undergoes a unique heating process, the surface of the metal transforms into a ceramic. Even though the new ceramic surface is 4,900 times more abrasion resistant than cobalt chrome, it retains the toughness and flexibility of the underlying metal.
Because it can achieve this remarkable reduction in implant wear without sacrificing strength as actual ceramic components do, oxidized zirconium implants have the potential to last significantly longer.
The Procedure
Knee replacement surgery typically takes between one and two hours to complete. This section will provide you with a brief, easy-to-understand description of the surgical procedure. (Please consult with your physician for details regarding your specific procedure.)
An incision is made extending from the thigh, past the inside edge of the kneecap, and down to the shinbone.
The end of the femur is shaped in preparation for sizing the femoral trial component.
The top of the tibia is shaped for proper sizing of the tibial trial component.
The trial units are put in place and the appropriate implant size is selected.
The knee is assessed for alignment, stability, and range of motion.
The underside of the kneecap is prepared and patella trial is selected.
The trial units are removed and the final femoral, tibial, and patella components are implanted.
The incision is closed, a drain is put in, and the post-operative bandaging is applied.
All information provided on this website is for information purposes only. Every patient's case is unique and each patient should follow his or her doctor's specific instructions. Please discuss nutrition, medication and treatment options with your doctor to make sure you are getting the proper care for your particular situation. If you are seeking this information in an emergency situation, please call 911 and seek emergency help.
All materials copyright © 2020 Smith & Nephew, All Rights Reserved.

10 February 2022
Smith+nephew announces first surgery for its journey◊ ii medial dished system for total knee arthroplasty.
Smith+Nephew (LSE:SN, NYSE:SNN), the global medical technology business, today announces the first completed surgery using its JOURNEY II Medial Dished (MD) System for total knee arthroplasty (TKA). The procedure was performed by Dr. Ran Schwarzkopf, Orthopedic Adult Hip and Knee Reconstruction at NYU Langone Health.
JOURNEY II Medial Dished further completes the JOURNEY II portfolio by offering a tibial insert that can provide more normal kinematics, or motion, in both cruciate-retaining and cruciate-sacrificing procedures. 1-5* Recent total knee implants are designed to try and better replicate this motion found in a healthy knee which has been shown to improve both patient satisfaction and performance. However, only Smith+Nephew’s JOURNEY II TKA System has been shown to restore anatomical shape, position and motion. 2-6 This anatomical design has led to a smoother recovery, improved function and higher patient satisfaction. 5-12,**
Dr. Schwarzkopf commented, “Adding a medial dished component to the JOURNEY II TKA portfolio is a significant development and expands the options I’m able to offer my patients. It allows me to optimize the kinematics for my patient’s while also providing good stability in either a cruciate-retaining or cruciate-sacrificing total knee replacement procedure.”
JOURNEY II MD is designed with a more constraining medial side, compared to a standard tibial insert, to promote more normal kinematics and provide additional stability if the PCL has been resected or is not in good condition. 1-5* Over the last few years, the concept of a tibial insert that helps drive better knee kinematics has been rapidly growing and JOURNEY II has led in this space. The Medial Dished insert is the next step of innovation allowing Smith+Nephew to offer a unique solution in this space.
“We are very excited about the launch JOURNEY II Medial Dished,” said Randy Kilburn, Executive Vice President & General Manager, Orthopaedic Reconstruction, Robotics and Digital for Smith+Nephew. “Our customers have expressed an interest in medial dished inserts and we are pleased to provide new treatment options that expand the clinical indications of the already successful JOURNEY II Knee System”.
Smith+Nephew's JOURNEY II Medial Dished is now available in the United States for total knee replacement.
About Smith+Nephew
Smith+Nephew is a portfolio medical technology business focused on the repair, regeneration and replacement of soft and hard tissue. We exist to restore people’s bodies and their self-belief by using technology to take the limits off living. We call this purpose ‘Life Unlimited’. Our 18,000 employees deliver this mission every day, making a difference to patients’ lives through the excellence of our product portfolio, and the invention and application of new technologies across our three global franchises of Orthopaedics, Advanced Wound Management and Sports Medicine & ENT.
Founded in Hull, UK, in 1856, we now operate in more than 100 countries, and generated annual sales of $4.6 billion in 2020. Smith+Nephew is a constituent of the FTSE100 (LSE:SN, NYSE:SNN). The terms ‘Group’ and ‘Smith+Nephew’ are used to refer to Smith & Nephew plc and its consolidated subsidiaries, unless the context requires otherwise.
For more information about Smith+Nephew, please visit www.smith-nephew.com and follow us on Twitter , LinkedIn , Instagram or Facebook .
Forward-looking Statements
This document may contain forward-looking statements that may or may not prove accurate. For example, statements regarding expected revenue growth and trading margins, market trends and our product pipeline are forward-looking statements. Phrases such as "aim", "plan", "intend", "anticipate", "well-placed", "believe", "estimate", "expect", "target", "consider" and similar expressions are generally intended to identify forward-looking statements. Forward-looking statements involve known and unknown risks, uncertainties and other important factors that could cause actual results to differ materially from what is expressed or implied by the statements. For Smith+Nephew, these factors include: risks related to the impact of COVID-19, such as the depth and longevity of its impact, government actions and other restrictive measures taken in response, material delays and cancellations of elective procedures, reduced procedure capacity at medical facilities, restricted access for sales representatives to medical facilities, or our ability to execute business continuity plans as a result of COVID-19; economic and financial conditions in the markets we serve, especially those affecting health care providers, payers and customers (including, without limitation, as a result of COVID-19); price levels for established and innovative medical devices; developments in medical technology; regulatory approvals, reimbursement decisions or other government actions; product defects or recalls or other problems with quality management systems or failure to comply with related regulations; litigation relating to patent or other claims; legal compliance risks and related investigative, remedial or enforcement actions; disruption to our supply chain or operations or those of our suppliers (including, without limitation, as a result of COVID-19); competition for qualified personnel; strategic actions, including acquisitions and dispositions, our success in performing due diligence, valuing and integrating acquired businesses; disruption that may result from transactions or other changes we make in our business plans or organisation to adapt to market developments; and numerous other matters that affect us or our markets, including those of a political, economic, business, competitive or reputational nature. Please refer to the documents that Smith+Nephew has filed with the U.S. Securities and Exchange Commission under the U.S. Securities Exchange Act of 1934, as amended, including Smith+Nephew's most recent annual report on Form 20-F, for a discussion of certain of these factors. Any forward-looking statement is based on information available to Smith+Nephew as of the date of the statement. All written or oral forward-looking statements attributable to Smith+Nephew are qualified by this caution. Smith+Nephew does not undertake any obligation to update or revise any forward-looking statement to reflect any change in circumstances or in Smith+Nephew's expectations.
◊ Trademark of Smith+Nephew. Certain marks registered US Patent and Trademark Office.
- Smith+Nephew 2021. TM-21-148.
- Iriuchishima T, Ryu K. A Comparision of Rollback Ratio between Bicruciate Substituting Total Knee Arthroplasty and Oxford Unicompartmental Knee Arthroplasty. J Knee Surg. 2018;31(6):568-572.
- Murakami K, Hamai S, Okazaki K, et al. Knee kinematics in bi-cruciate stabilized total knee arthroplasty during squatting and stair-climbing activities. J Orthop. 2018;15(2):650-654.
- Carpenter RD, Brilhault J, Majumdar S, Ries MD. Magnetic resonance imaging of in vivo patellofemoral kinematics after total knee arthroplasty. Knee. 2009;16(5):332-336.
- Smith LA, Nachtrab J, LaCour M, et al. In Vivo Knee Kinematics: How Important Are the Roles of Femoral Geometry and the Cruciate Ligaments? J Arthroplasty. 2021;36:1445-1454.
- Grieco TF, Sharma A, Dessinger GM, Cates HE, Komistek RD. In Vivo Kinematic Comparison of a Bicruciate Stabilized Total Knee Arthroplasty and the Normal Knee Using Fluoroscopy. J Arthroplasty. 2018;33(2):565-571.
- Murakami K, Hamai S, Okazaki K, et al. In vivo kinematics of gait in posterior-stabilized and bicruciate-stabilized total knee arthroplasties using image-matching techniques. Int Orthop. 2018;42(11):2573-2581.
- Noble PC, Gordon MJ, Weiss JM, et al. Does Total Knee Replacement Restore Normal Knee Function? Clin Orthop Relat Res. 2005;431:157–165.
- Nodzo SR, Carroll KM, Mayman DJ. The Bicruciate Substituting Knee Design and Initial Experience. Techniques in Orthopaedics. 2018;33(1):37-41.
- Takubo A, Ryu K, Iriuchishima T, Tokuhashi Y. Comparison of Muscle Recovery Following Bi-cruciate Substituting versus Posterior Stabilized Total Knee Arthroplasty in the Asian Population. J Knee Surg. 2017;30(7):725-729.
- Mayman DJ, Patel AR, Carroll KM. Hospital Related Clinical and Economic Outcomes of a Bicruciate Knee System in Total Knee Arthroplasty Patients. Poster presented at: ISPOR Symposium;19-23 May, 2018; Baltimore, Maryland, USA
- Kosse NM, Heesterbeek PJC, Defoort KC, Wymenga AB, Hellemondt GG. Minor adaptations in implant design bicruciate-substituted total knee system improve maximal flexion. Poster presented at: 2nd World Arthroplasty Congress;19-21 April, 2018; Rome, Italy.
*Based on JOURNEY II BCS and CR Evidence
**Compared to non-JOURNEY II knees
- Contrast Mode
- Increase Font Size
- Decrease Font Size
- Reset Font Default
- Accessibility Options
- Back to Main Site

- Request an Appointment
JOURNEY II – Total Knee Replacement
The JOURNEY II BCS Knee
Recent advances in biomedical engineering software have opened a new chapter on high performance knee implants.

One remarkable breakthrough has been the creation of the JOURNEY II BCS knee, a second-generation knee replacement that combines the stability and natural motion of the human knee with new low-friction materials that may extend the life of the implant.
While the lifespan of a knee implant is heavily influenced by the materials used to make it, the natural feeling of the implant during physical activity is dependent upon the way the patient's muscles, ligaments and tendons are addressed during surgery and by the implant's shape within the body after surgery.
As discussed previously in this booklet, the knee is a hinge joint, but it does not swing like a simple door hinge. It has a complex rotational motion that you don't notice is there - but many patients know when it's not there after total knee replacement. Traditional implants attempt to recreate this subtle swing-and-rotate action with either a rotating platform (a simple pivot point) within the implant or by requiring an angled alignment of the implant during surgery.
With these traditional knee replacement designs, the muscles and ligaments around your new joint have to work harder because the implant's slightly unnatural shapes and resulting motion make these soft tissues move in unfamiliar, stressful ways. This leads to joint pain, muscle fatigue and the unnatural feeling patients experience while walking or bending in the months after their procedure.
The JOURNEY II BCS knee, on the other hand, is designed to reproduce the original internal shapes and angled forces of the human knee through its full range of motion - accommodating the swing-and-rotate of the joint with the same engineering principles your real knee currently uses. Because of this, your soft tissues don't have to readjust to new shapes and forces after surgery and your stride can return to its natural rhythm.
The JOURNEY II BCS knee also reproduces the stability provided by your anterior cruciate ligament (ACL) and your posterior cruciate ligament (PCL). Your ACL and PCL are key to the stability of your real joint and contribute to natural motion when your knee is fully extended and fully bent. No other knee implant reproduces both functions.
Implant Components

In the knee replacement procedure, each prosthesis is made up of four parts.
The tibial component has two elements - a metal base and a plastic insert - and replaces and the top of the tibia (shin bone). This prosthesis is made up of a metal tray attached directly to the bone and a high-density plastic spacer that provides the bearing surface.
The femoral component replaces the bottom of the thigh bone or femur. This component also replaces the groove where the patella or kneecap rides.
The patellar component replaces the surface of the knee cap, which rubs against the femur. The patella protects the joint, and the resurfaced patellar button will slide smoothly on the front of the joint. In some cases, surgeons do not resurface the patella.
Bearing Surfaces
One of the keys to a successful implant is its ability to withstand the rigors of daily activity, and central to that is the quality of the artificial surfaces that slide against each other, or articulate, in the new joint.
In knee implants, bearing surface options have been somewhat limited over the last few decades. The standard substance used for the femoral component is cobalt chrome, a metal alloy typified by its toughness and biocompatibility. However,even this high-quality industry standard has its shortcomings. Over time, this metal surface can become roughened by bone and bone cement particles trapped between the femoral component and the plastic tibial insert.
This roughened surface, when rubbing against the plastic component up to two million times per year, can more quickly wear out your implant. When that happens, you will have to undergo surgery to replace the plastic piece, the femoral component, and possibly even the tibial component. For this reason, implants have been shown to last between ten and fifteen years in the human body.
An exciting material to enter orthopaedics in recent years is OXINIUM ◊ Oxidized Zirconium. This remarkable material combines the strengths of ceramic and metal, such as wear-reduction and strength, but does not have the weaknesses, such as limited implant options and the possibility of fracture.
Zirconium is a biocompatible metal, similar to titanium. When the zirconium alloy undergoes a unique heating process, the surface of the metal transforms into a ceramic. Even though the new ceramic surface is 4,900 times more abrasion resistant than cobalt chrome, it retains the toughness and flexibility of the underlying metal.
Because it can achieve this remarkable reduction in implant wear without sacrificing strength as actual ceramic components do, oxidized zirconium implants have the potential to last significantly longer.
The Procedure
Knee replacement surgery typically takes between one and two hours to complete. This section will provide you with a brief, easy-to-understand description of the surgical procedure. (Please consult with your physician for details regarding your specific procedure.)
The names of the below pictures are Bonecuts , Implant Components and Implanted respectively

An incision is made extending from the thigh, past the inside edge of the kneecap, and down to the shinbone.
The end of the femur is shaped in preparation for sizing the femoral trial component.
The top of the tibia is shaped for proper sizing of the tibial trial component.
The trial units are put in place and the appropriate implant size is selected.
The knee is assessed for alignment, stability, and range of motion.
The underside of the kneecap is prepared and patella trial is selected.
The trial units are removed and the final femoral, tibial, and patella components are implanted.
The incision is closed, a drain is put in, and the post-operative bandaging is applied.
All information provided on this website is for information purposes only. Every patient's case is unique and each patient should follow his or her doctor's specific instructions. Please discuss nutrition, medication and treatment options with your doctor to make sure you are getting the proper care for your particular situation. If you are seeking this information in an emergency situation, please call 911 and seek emergency help. All materials copyright © 2020 Smith & Nephew, All Rights Reserved.
3700 N 24th Street Suite 160 Phoenix, AZ 85016
- My Practice
- Specialties
- Patient Info
- Med. Professionals


IMAGES
VIDEO
COMMENTS
JOURNEY II Total Knee Arthroplasty. Total knee arthroplasty patients report unmet levels of satisfaction, particularly for more active or demanding activities. 1,2 The JOURNEY II System is designed to help patients rediscover their normal through a smoother recovery, *3,4 improved function *4-8 and higher patient satisfaction *2,4-6. Brochure.
JOURNEY II BCS with SYNC Performance Instruments JOURNEY™ II BCS Bi-Cruciate Stabilized Knee System SYNC Performance Instruments. Nota Bene The technique description herein is made available to the healthcare professional to illustrate the suggested treatment for the uncomplicated procedure. In the final analysis, the preferred treatment
Objectives To determine if a newer design of total knee replacement (TKR) (Journey II BCS) produces superior patient-reported outcomes scores and biomechanical outcomes than the older, more established design (Genesis II). Setting Patients were recruited from an NHS University Hospital between July 2018 and October 2019 with surgery at two sites. Biomechanical and functional capacity ...
JOURNEY™ II Bi-Cruciate Stabilized (BCS) Knee featuring the Distal Bur Technique using the NAVIO Surgical System. David Rovinsky, MD, performs a robotic-assisted JOURNEY™ II Bi-Cruciate Stabilized (BCS) knee surgery with NAVIO™ Surgical System featuring the distal bur technique.
ORTHOPAEDICS. JOURNEY II XR Bi-Cruciate Retaining Knee System. While JOURNEY II TKA has been shown to restore anatomical shape, position and motion, 1-4 the JOURNEY II XR system goes a step further by allowing the ACL to be retained. An anatomical design is intended to help a smoother recovery, improved function and higher patient satisfaction ...
Page 1 Surgical Technique for use with the JOURNEY™ II BCS and JOURNEY™ II CR...; Page 2 NAVIO™ Surgical System Surgical Technique for use with the JOURNEY™ II BCS and JOURNEY™ II CR Smith & Nephew 500081, Rev B Issue Date: 2016-11-16 The following technique is for informational and educational purposes only. It is not intended to serve as medical advice.
This is a pragmatic, triple-blinded, parallel, superiority, randomised controlled trial of the JOURNEY II BCS (intervention) versus GENESIS II (control) in patients with primary osteoarthritis undergoing TKR. Embedded in the clinical trial is a qualitative investigation of participants' confidence in the TKR received and their experiences of ...
The JOURNEY II BCS Knee. Recent advances in biomedical engineering software have opened a new chapter on high performance knee implants. One remarkable breakthrough has been the creation of the JOURNEY II BCS knee, a second-generation knee replacement that combines the stability and natural motion of the human knee with new low-friction materials that may extend the life of the implant.
The JOURNEY II BCS knee, on the other hand, is designed to reproduce the original internal shapes and angled forces of the human knee through its full range of motion - accommodating the swing-and-rotate of the joint with the same engineering principles your real knee currently uses. Because of this, your soft tissues don't have to readjust ...
The JOURNEY II BCS is a member of the JOURNEY II Total Knee Arthroplasty (TKA) system, which also includes JOURNEY II Cruciate Retaining (CR) and the recently launched bi-cruciate retaining JOURNEY II XR. Smith & Nephew is a global medical technology business dedicated to helping healthcare professionals improve people's lives. With ...
The JOURNEY II BCS Knee. Recent advances in biomedical engineering software have opened a new chapter on high performance knee implants. One remarkable breakthrough has been the creation of the JOURNEY II BCS knee, a second-generation knee replacement that combines the stability and natural motion of the human knee with new low-friction materials that may extend the life of the implant.
The JOURNEY™ II BCS provides more mobility in the lateral compartment than other total knee systems provide, to replicate normal knee kinematics. For patients who presented with significant varus or valgus deformities (> 15°), morbid obesity, or deficient collateral ligaments, the surgeon decided if additional implant constraint was ...
The goal of the JOURNEY II BCS is to enable a higher level of function for total knee replacement patients - to not only relieve pain, but help them regain active lifestyles. Function, motion and durability are achieved through the unique features of the JOURNEY II BCS system-anatomic alignment, kinematics and advanced bearings. ...
JOURNEY II bi-cruciate stabilized (BCS) knee system, a guided motion total knee arthroplasty (TKA), has been reported to reproduce physiological knee kinematic motion with good clinical outcomes. However, this guided system may be sensitive to the femorotibial rotational alignment.
The Genesis II (Smith & Nephew, Memphis, Tennessee, USA) TKR has been reported to have good survivorship and patient satisfaction 13 21 and is commonly used in the UK 22 An evolutionary design, the Journey II BCS (JII-BCS; Smith & Nephew), also manufactured by Smith and Nephew, has been developed to improve kinematic outcome compared with the ...
The JOURNEY II BCS Knee . Recent advances in biomedical engineering software have opened a new chapter on high performance knee implants. One remarkable breakthrough has been the creation of the JOURNEY II BCS knee, a second-generation knee replacement that combines the stability and natural motion of the human knee with new low-friction materials that may extend the life of the implant.
Partial knees treat only the affected part of the knee, while allowing the patient to keep their healthy ligaments. JOURNEY II UK System combines clinically successful features to present a third-generation, unicompartmental knee platform featuring: Intraoperative sizing flexibility. OXINIUM Technology bearing surface. Tissue-conscious design.
The Journey II TKA is truly a revolutionary step forward in the design of total knee implants. With proper surgical technique and in the hands of a well-trained surgeon, the Journey II knee can produce results superior to the traditional total knee design. It is our goal as your surgical team to continue to improve our surgical techniques and ...
JOURNEY II BCS CONSTRAINED ARTICULAR INSERT Size 5-6, 10 MM Left, REF 74029262; knee prosthesis: Code Information: UDI/DI 00885556176467, Batch Number 22BM17564 ... 978-749-1440 Manufacturer Reason for Recall: The JRNY II BCS XLPE ART ISRT SZ 5-6 LT 10MM was laser etched, labeled and packaged as a JRNY II BCS CNSTRD ART ISRT 5-6 LT 10MM. And ...
The JOURNEY II BCS Knee . Recent advances in biomedical engineering software have opened a new chapter on high performance knee implants. One remarkable breakthrough has been the creation of the JOURNEY II BCS knee, a second-generation knee replacement that combines the stability and natural motion of the human knee with new low-friction materials that may extend the life of the implant.
JOURNEY II MD is designed with a more constraining medial side, compared to a standard tibial insert, ... *Based on JOURNEY II BCS and CR Evidence **Compared to non-JOURNEY II knees. We design and manufacture technology that takes the limits off living. We support healthcare professionals to return their patients to health and mobility, helping ...
Discover the latest innovations and solutions from Smith & Nephew, a global medical technology business, in this informative and interactive brochure.
The JOURNEY II BCS knee, on the other hand, is designed to reproduce the original internal shapes and angled forces of the human knee through its full range of motion - accommodating the swing-and-rotate of the joint with the same engineering principles your real knee currently uses. Because of this, your soft tissues don't have to readjust to ...