From prenatal to postpartum, your benefits are designed to support you through each stage of your pregnancy.


A healthy pregnancy is just the beginning
We're dedicated to supporting healthy pregnancies, from early prenatal care in your first trimester all the way through childbirth and the months that follow.
Prenatal Care
Healthy pregnancy, maternity coverage, helpful resources.
Prenatal visits will allow you to follow the progress of your baby’s development and give you an opportunity to talk to your doctor about any pregnancy concerns. It's your chance to ask questions, discuss your medical history, weight, diet and lifestyle—and help you prepare for childbirth and life with a new baby. As soon as you think you might be pregnant, and in the first three months of pregnancy, you should visit your healthcare provider.
During your prenatal visits, you will:
- Discuss your health history and any pregnancy risks factors based on age, health and/or family history
- Receive an ultrasound and important lab work
- Learn your due date
- Discuss your delivery plans
Tips to help ensure the health of both you and your baby.
Consider prenatal vitamins
These provide important vitamins and minerals including folic acid, iron and calcium. Folic acid helps prevent neural tube birth defects, which affect the baby’s brain and spinal cord.
Proper nutrition during pregnancy helps your baby grow and develop. Experts recommend 6-11 servings of bread and grains, 2-4 servings of fruit, 4+ servings of vegetables, 4 servings of dairy and 3 servings of protein.
Cut caffeine
If you are pregnant or trying to become pregnant, you should have no more than 200 mg of caffeine a day, or the amount of one 12-ounce cup.
Stop smoking
Smoking during pregnancy can put yourself and your unborn baby at risk for serious health problems, including premature birth, certain birth defects and infant death.
Visit your dentist
During pregnancy, rising hormone levels can irritate gums, causing tenderness, swelling and bleeding. Brush and floss daily and see your dentist regularly.
Stay active
Whether you find relaxation in prenatal yoga or prefer to break a sweat with your workout, talk to your doctor about safe ways to stay active while you’re pregnant.
For members of the Service Benefit Plan, all prenatal and postpartum care is covered in full when you visit a Preferred professional provider. What you pay for facility care is based on the plan you're enrolled in.
What you pay when you visit Preferred providers:
Get a free blood pressure monitor.
It’s important to monitor your blood pressure when you’re pregnant. As part of our maternity benefits, pregnant members can get a blood pressure monitor at no cost by mailing this form to the address listed on the form . Eligible members can receive this benefit every two years.
Your mental health is just as important as your physical health
We also provide benefits to cover up to eight visits per year in full to treat depression associated with pregnancy (including depression during pregnancy, postpartum depression or both) when you use a Preferred provider .
These programs and resources can help you and your baby stay healthy every step of the way.
Office of Women's Health
This section of womenshealth.gov will help expectant mothers learn what to do before, during, and after pregnancy to give your baby a healthy start to life. Take their quiz to test your knowledge on pregnancy health.
USDA ChooseMyPlate Daily Food Plans
Create a personalized daily food plan that shows the foods and amounts that are right for you at your stage of pregnancy or when breastfeeding.
The American Congress of Obstetricians and Gynecologists
ACOG is the nation's leading group of physicians providing health care for women. Visit their site for fact sheets on pregnancy, labor, delivery and postpartum care.
March of Dimes
The mission of the March of Dimes is to improve the health of babies by preventing birth defects, premature birth and infant mortality. The non-profit organization helps moms have full-term pregnancies and healthy babies by researching and working to prevent the problems that threaten babies.
Focused on better maternal health
We’re committed to helping reduce maternal health disparities by making sure pregnant individuals, new parents and babies get the support they need during every stage of pregnancy.

Get support and earn rewards throughout your pregnancy
The Pregnancy Care Incentive Program offers expectant mothers support and rewards during each stage of pregnancy. You could be eligible* to earn a free Pregnancy Care Box packed with items you can use during and after pregnancy—and $75 in wellness rewards.
*You must be 18 or older on a FEP Blue Standard™ or FEP Blue Basic™ plan to earn this reward.

Your Pregnancy To-Do List
We know there’s a lot to think about when you’re expecting. Follow this helpful to-do list to promote good health and prepare for the arrival of your baby.
Learn more about pregnancy from BlueNews

Prenatal and Postpartum Care

How Financial Worries Can Affect You When You’re Expecting

Well-Child Visits Help Children Grow Big and Strong
Explore other health conditions, stay in the know.
Sign up to receive our monthly email newsletter, tips for healthy living and important updates.
You are leaving fepblue.org
We use cookies on this website to give you the best experience and measure website usage. By continuing to use this website, you consent to these cookies. For more information, view our privacy policy .
Well-Women Visits and Prenatal Care under the ACA’s Women’s Health Amendment
By: Susan Berke Fogel
Executive Summary
The Affordable Care Act (ACA) recognizes that preventive health services in general, and women’s preventive health services in particular, are critical to individual and community health, and that cost is often a barrier to accessing needed preventive care. In addition to the Essential Health Benefits requirement to cover maternity care and preventive services, the ACA adds § 2713(a)(4) to the Public Health Service Act (the Women’s Health Amendment) to require coverage of women’s health preventive services, including prenatal care, without cost sharing.
The Affordable Care Act (ACA) recognizes that preventive health services in general, and women?s preventive health services in particular, are critical to individual and community health, and that cost is often a barrier to accessing needed preventive care. In addition to the Essential Health Benefits requirement to cover maternity care and preventive services, the ACA adds § 2713(a)(4) to the Public Health Service Act (the Women’s Health Amendment) to require coverage of women’s health preventive services, including prenatal care, without cost sharing.
The ACA Requires Coverage of Preventive Services for Women
- Items or services that have a rating of A or B in the recommendations of the U.S. Preventive Services Task Force,
- The Centers for Disease Control and Prevention Advisory Committee on Immunization Practices (ACIP) recommended vaccinations,
- Preventive care and screenings for infants, children, and adolescents, as provided for in guidelines supported by the Health Resources and Services Administration (HRSA),
- Additional women’s health preventive care and screenings, to fill in the gaps and supplement the U.S. Preventive Services Task Force recommendations, and as provided for in guidelines supported by HRSA’s the Women’s Health Amendment.[2]
The recommended content of the [well-woman prenatal care] visit includes specific tests and procedures (e.g., blood pressure, weight, urine test, uterine size and fetal heart rate assessment, glucose tolerance testing, and screening for specific sexually transmitted infections and genetic or developmental conditions), as well as topics for counseling and guidance (e.g., tobacco avoidance and nutrition).[6]
——————————————–
Related Content
What makes medicaid, medicaid.
With the passage of the Affordable Care Act (ACA) in 2010, and the implementation of Medicaid expansions and Marketplaces…
Model Contraceptive Equity Act: Legislative Language and Issue Brief
UPDATED - December 2021. Contraceptive Equity is a policy framework under which contraceptive care is easily accessible and covered…
Contraceptive Equity in Action: A Toolkit for State Implementation
The National Health Law Program is dedicated to ensuring appropriate implementation and monitoring for states that have adopted Contraceptive…

- Copy/Paste Link Link Copied
What happens during prenatal visits?
What happens during prenatal visits varies depending on how far along you are in your pregnancy.
Schedule your first prenatal visit as soon as you think you are pregnant, even if you have confirmed your pregnancy with a home pregnancy test. Early and regular prenatal visits help your health care provider monitor your health and the growth of the fetus.
The First Visit
Your first prenatal visit will probably be scheduled sometime after your eighth week of pregnancy. Most health care providers won't schedule a visit any earlier unless you have a medical condition, have had problems with a pregnancy in the past, or have symptoms such as spotting or bleeding, stomach pain, or severe nausea and vomiting. 1
You've probably heard pregnancy discussed in terms of months and trimesters (units of about 3 months). Your health care provider and health information might use weeks instead. Here's a chart that can help you understand pregnancy stages in terms of trimesters, months, and weeks.
Because your first visit will be one of your longest, allow plenty of time.
During the visit, you can expect your health care provider to do the following: 1
- Answer your questions. This is a great time to ask questions and share any concerns you may have. Keep a running list for your visit.
- Check your urine sample for infection and to confirm your pregnancy.
- Check your blood pressure, weight, and height.
- Calculate your due date based on your last menstrual cycle and ultrasound exam.
- Ask about your health, including previous conditions, surgeries, or pregnancies.
- Ask about your family health and genetic history.
- Ask about your lifestyle, including whether you smoke, drink, or take drugs, and whether you exercise regularly.
- Ask about your stress level.
- Perform prenatal blood tests to do the following:
- Determine your blood type and Rh (Rhesus) factor. Rh factor refers to a protein found on red blood cells. If the mother is Rh negative (lacks the protein) and the father is Rh positive (has the protein), the pregnancy requires a special level of care. 2
- Do a blood count (e.g., hemoglobin, hematocrit).
- Test for hepatitis B, HIV, rubella, and syphilis.
- Do a complete physical exam, including a pelvic exam, and cultures for gonorrhea and chlamydia.
- Do a Pap test or test for human papillomavirus (HPV) or both to screen for cervical cancer and infection with HPV, which can increase risk for cervical cancer. The timing of these tests depends on the schedule recommended by your health care provider.
- Do an ultrasound test, depending on the week of pregnancy.
- Offer genetic testing: screening for Down syndrome and other chromosomal problems, cystic fibrosis, other specialized testing depending on history.
Prenatal Visit Schedule
If your pregnancy is healthy, your health care provider will set up a regular schedule for visits that will probably look about like this: 1
Later Prenatal Visits
As your pregnancy progresses, your prenatal visits will vary greatly. During most visits, you can expect your health care provider to do the following:
- Check your blood pressure.
- Measure your weight gain.
- Measure your abdomen to check your developing infant's growth—"fundal height" (once you begin to "show").
- Check the fetal heart rate.
- Check your hands and feet for swelling.
- Feel your abdomen to find the fetus's position (later in pregnancy).
- Do tests, such as blood tests or an ultrasound exam.
Talk to you about your questions or concerns. It's a good idea to write down your questions and bring them with you.
Several of these visits will include special tests to check for gestational diabetes (usually between 24 and 28 weeks) 3 and other conditions, depending on your age and family history.
In addition, the Centers for Disease Control and Prevention and the American Academy of Pediatrics released new vaccine guidelines for 2013 , including a recommendation for pregnant women to receive a booster of whooping cough (pertussis) vaccine. The guidelines recommend the shot be given between 27 and 36 weeks of pregnancy. 4
- Centers for Disease Control and Prevention. (2013). Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine (TDAP) in pregnant women―Advisory Committee on Immunization Practices (ACIP), 2012. Retrieved September 20, 2013, from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6207a4.htm

Model Profiles
Maternal infant health program.
Maternal Infant Health Program (MIHP) promotes healthy pregnancies, positive birth outcomes, and healthy infant growth and development with the long-term goal of reducing infant mortality and morbidity. Nurses and social workers provide professional case management and health education services, promote health equity, and provide individualized care to pregnant people, infants, and their caregivers. Families enrolled in the program may also be referred to or receive home visits from a registered dietitian, lactation consultant, and/or infant mental health specialist.
What is the model’s approach to providing home visiting services?
Home visits take place monthly or more often if needed. Services are provided prenatally and may last until the child is 18 months old, based on the needs of the infant and caregiver.
MIHP’s service population includes the following:
- Infants in the first 18 months of life eligible for Medicaid
- Pregnant persons eligible for Medicaid
Who is implementing the model?
Home Visitors
MIHP was implemented by 315 full-time equivalent (FTE) home visitors in 2022. The model requires home visitors to be registered nurses or licensed social workers. Registered nurses must have at least 1 year of experience providing community health, pediatric, or maternal/infant nursing services. Licensed social workers must have at least 1 year of experience providing social work services to families. Others providing services in the home may include licensed professionals with an infant mental health specialist endorsement; licensed nurses and social workers with valid, current certification as International Board Certified Lactation Consultants; and registered dietitians.
Supervisors
MIHP was implemented by 79 FTE supervisors in 2022, with at least 1 supervisor covering each of the 79 local agencies.
Where is the model implemented?
MIHP was implemented by 79 agencies in 114 locations in 1 state in 2022.

Families Served Through Evidence-Based Home Visiting in 2022
2% American Indian Alaska Native
<1% Native Hawaiian Pacific Islander
6% Another race
Primary language
95% English
2% Another language
Caregiver age
20% ≤21 years
47% 22-29 years
33% 30-44 years
<1% ≥45 years
Caregiver education
21% No HS diploma
66% HS diploma or GED
8% Some college or training
5% Bachelor's degree or higher
10% Hispanic or Latino
90% Not Hispanic or Latino
32% 1-2 years
Household income
100% Low-income status
Child insurance status
100% Public
Stay up to date on the latest home visiting information.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006 Feb-.

Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet].
Statistical brief #92 mental health and substance abuse-related emergency department visits among adults, 2007.
Pamela L Owens , PhD, Ryan Mutter , PhD, and Carol Stocks , RN, MHSA.
Published: July 2010 .
- Introduction
An estimated one in three individuals has suffered from a mental health or substance abuse condition within the last 12 months, 1 yet the community treatment system to support services for these individuals is regarded as ineffective. 2 This is particularly evident in emergency department (ED) utilization. The number of patients with mental health and substance abuse (MHSA) conditions treated in EDs has been on the rise for more than a decade. 3 Not only is this of concern to members of the mental health community, but also to the members of the emergency medicine community who are concerned that ED overcrowding results in decreased quality of care and increased likelihood of medical error. 4 As a specific example, a 2008 American College of Emergency Physicians' ED directors’ survey reported that patients with MHSA conditions not only have had increased ED boarding times, but also that the resource-intensive care required for these patients has an impact on the quality of care for all other patients in the ED. 5
This Statistical Brief presents data from the Healthcare Cost and Utilization Project (HCUP) Nationwide Emergency Department Sample (NEDS) on MHSA-related ED visits among adults in 2007. Specifically, patient and utilization characteristics of ED visits for MHSA are discussed and compared with all other types of ED visits. The distribution of MHSA-related ED visits are presented by age and primary expected payer. The MHSA conditions described here include those conditions found in the Diagnostic and Statistics Manual of Mental Disorders, Fourth Edition , excluding dementia and intellectual disabilities. The Brief also provides information about the types of MHSA conditions by age and primary expected payer. In addition to prevalence estimates, data on the likelihood of hospital admission are presented. Estimates are based on all-listed diagnoses. All differences between estimates noted in the text are statistically significant at the 0.05 level or better.
- In 2007, 12.0 million emergency department (ED) visits involved a diagnosis related to a mental health and/or substance abuse condition (MHSA), accounting for 12.5 percent of all ED visits in the U.S., or one out of every eight ED visits.
- MHSA-related ED visits were two and a half times more likely to result in hospital admission than ED visits related to non-MHSA conditions—nearly 41 percent of MHSA-related ED visits resulted in hospitalization.
- Medicare was billed most frequently for MHSA-related ED visits (30.1 percent), followed by private insurance (25.7 percent), uninsured (20.6 percent), and Medicaid (19.8 percent).
- Visits related to mental health conditions accounted for 63.7 percent of all MHSA-related ED visits. Substance abuse conditions accounted for 24.4 percent of all MHSA-related ED visits, and co-occurring MHSA conditions accounted for 11.9 percent.
- ED visits billed as uninsured were two to four times less likely to result in hospital admission, depending on the type of MHSA condition.
- Mood disorder was the most common MHSA reason for an ED visit (42.7 percent), followed by anxiety disorders (26.1 percent), and alcohol-related conditions (22.9 percent). The remaining common conditions included drug-related conditions, schizophrenia and other psychoses, and intentional self-harm.
General findings
In 2007, of the 95 million visits made to the emergency department (ED) by adults in the U.S., 12.0 million (12.5 percent) were related to MHSA ( table 1 )—4.1 million of which had mental health or substance abuse conditions listed as a primary diagnosis. Nearly 41 percent (4.8 million visits) of these MHSA-related ED visits resulted in hospital admission—an admission rate that is over two and a half times that for ED visits related to other conditions ( figure 1 ).
Characteristics of ED Visits Related to Mental Health and Substance Abuse Conditions among Adults, 2007.
MHSA-related ED visits were three to four times more likely to result in hospitalization than other types of ED visits, 2007. Source: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, Nationwide Emergency Department (more...)
Table 1 shows that the majority of MHSA-related ED visits were for women (53.9 percent). The largest percentage of MHSA-related ED visits (46.6 percent) were for younger adults ages 18 to 44 years, followed by 45 to 64 year olds (34.5 percent). Adults 65 years and older accounted for nearly one in five (18.9 percent) MHSA-related ED visits. Compared with ED visits for other conditions, those related to MHSA were more likely to be for 45 to 64 year olds (34.5 percent versus 25.8 percent) and less likely to be for adults 18 to 44 years (46.6 percent versus 52.4 percent) and 65 years and older (18.9 percent versus 21.8 percent).
Medicare, healthcare insurance for those 65 years and older or those on Social Security Disability Insurance, was billed more frequently for MHSA-related ED visits (30.1 percent), followed by private insurance (25.7 percent), uninsured (20.6 percent), and Medicaid (19.8 percent). In contrast, private insurance was billed more frequently for most other types of ED visits (34.5 percent), followed by Medicare (24.7 percent), uninsured (20.6 percent), and Medicaid (14.9 percent).
Types of MHSA-related ED visits
Table 1 shows the distribution of MHSA-related ED visits, including those related to only mental health conditions (i.e., not substance abuse condition), those related to only substance abuse conditions (i.e., not mental health conditions), and those related to co-occurring MHSA conditions. Over 7.6 million ED visits related to mental health conditions only, accounting for 63.7 percent of all MHSA-related ED visits. Nearly 3.0 million ED visits related to substance abuse conditions only, accounting for 24.4 percent of all MHSA-related ED visits. Over 1.4 million visits related to co-occurring MHSA conditions, accounting for 11.9 percent of MHSA-related ED visits.
Patient and payer characteristics of types of MHSA-related ED visits
Table 1 shows that ED visits related to mental health conditions were more likely to be for women (65.4 percent), while ED visits related to substance abuse conditions (29.3 percent) and co-occurring MHSA conditions (43.0 percent) were less likely to be for women and more likely to be for men. Regardless of the type of condition, MHSA-related ED visits were more likely to be for younger adults 18 to 44 years.
ED visits related to co-occurring MHSA conditions were disproportionately more likely to be for 18–44 year olds—58.8 percent of ED visits for co-occurring MHSA conditions were for 18–44 year olds (versus 42.7 percent for mental conditions only and 50.7 percent for substance abuse conditions only). ED visits related to mental health conditions were disproportionately more likely to be for the oldest adults 65 years and older (25.3 versus 9.1 and 5.2 percent related to substance abuse conditions and co-occurring MHSA conditions, respectively).
Medicare was billed more frequently for mental health-related ED visits (37.2 percent), followed by private insurance (27.5 percent) and Medicaid (18.3 percent). Fewer mental health-related ED visits were billed as uninsured (13.8 percent). In contrast, the largest percentage of substance abuse-related ED visits was billed as uninsured (35.6 percent). Private insurance accounted for 22.2 percent of substance abuse-related ED visits, followed by Medicaid (20.7 percent) and Medicare (16.3 percent). Nearly one-fourth of ED visits for co-occurring MHSA conditions were billed as uninsured (26.3 percent) or to Medicaid (25.7 percent) or private insurance (23.4 percent). Medicare accounted for 20.3 percent of ED visits related to co-occurring MHSA conditions.
Admission status for MHSA-related ED visits, by age and expected payer
Figure 1 highlights that ED visits related to co-occurring MHSA conditions were the most likely to result in hospital admission (57.1 percent), followed by visits related to mental health conditions (39.3 percent), and substance abuse conditions (36.6 percent). Figures 2 and 3 show that visits related to co-occurring MHSA conditions were more likely to result in hospital admission than either visits related to mental health only or substance abuse only within age and payer groups.
Admission rates for MHSA-related ED visits increased with age, 2007. Source: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, Nationwide Emergency Department Sample, 2007
Uninsured MHSA-related ED visits were two to four times less likely to result in hospitalization than visits billed to other payers, 2007. Source: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, Nationwide Emergency (more...)
Admission rates increased with age, regardless of the type of MHSA-related ED visits ( figure 2 ). ED visits for adults 18 to 44 years with mental health conditions were the least likely to result in hospital admission (20.3 percent), while ED visits for adults 65 years and older with co-occurring MHSA conditions were the most likely to result in admission (82.0 percent).
Hospital admission rates varied by expected payer ( figure 3 ). ED visits billed to Medicare were more likely to result in admission, regardless of the type of MHSA condition (58.9, 58.0, and 70.8 percent, related to mental health only, substance abuse only, and co-occurring MHSA, respectively). ED visits billed as uninsured were the least likely to result in hospital admission, regardless of the type of MHSA condition (15.1, 23.8, and 41.3 percent related to mental health only, substance abuse only and co-occurring MHSA, respectively).
Number and distribution of ED visits for the most frequent all-listed MHSA conditions, by age and expected payer
As shown in table 2 , the most common all-listed reason for a MHSA-related ED visit was mood disorder (42.7 percent of MHSA-related ED visits), followed by anxiety disorders (26.1 percent), alcohol disorders (22.9 percent), drug disorders (17.6 percent), schizophrenia and other psychoses (9.9 percent), and intentional self-harm (6.6 percent). The top five conditions accounted for 96.0 percent of all MHSA-related cases in the ED, taking into account that there may be multiple diagnoses on an ED record. Some variation was noted by age and expected payer. For example, among adults 65 years and older, mood disorders accounted for over half of the ED visits (52.0 percent) followed by anxiety disorders (28.8 percent), and schizophrenia and other psychoses (11.4 percent). Although mood disorders were the most frequent condition for all age groups and most payers, alcohol-related conditions were the most frequent condition among the uninsured.
Most Common All-Listed MHSA Conditions Seen During an ED Visit, 2007.
Figure 4 shows the age distribution for specific MHSA-related ED visits by condition. ED visits for intentional self-harm (69.0 percent) and drug abuse conditions (63.1 percent) were disproportionately more likely to be for young adults 18–44 years old—accounting for almost 500,000 ED visits and over 1.3 million ED visits in 2007, respectively.
The youngest adults disproportionately accounted for ED visits related to intentional self-harm and drug abuse conditions, 2007. Source: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, Nationwide Emergency Department (more...)
Figure 5 shows that the payer distribution for each of the MHSA condition specific ED visits varied considerably. For example, ED visits related to mood disorders and those related to schizophrenia and other psychoses were disproportionately more likely to be billed to Medicare (36.6 and 47.4 percent, respectively). ED visits related to drug abuse, alcohol abuse, and intentional self-harm were more frequently billed as uninsured than any other payer (33.3, 31.9, and 29.3 percent, respectively).
Expected payer was associated with specific MHSA-related ED visits, 2007. Source : Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, Nationwide Emergency Department Sample, 2007; based on all-listed diagnoses. Missing (more...)
- Data Source
The estimates in this Statistical Brief are based upon data from the HCUP 2007 Nationwide Emergency Department Sample (NEDS). The statistics can also be generated from HCUPnet, a free, online query system that provides users with immediate access to the largest set of publicly available, all-payer national, regional, and State-level hospital care databases from HCUP.
- Definitions
Diagnoses, ICD-9-CM, and Clinical Classifications Software (CCS)
The principal diagnosis is that condition established after study to be chiefly responsible for the patient’s admission to the hospital. Secondary diagnoses are concomitant conditions that coexist at the time of admission or that develop during the stay. All-listed diagnoses include the principal diagnosis plus these additional secondary conditions.
ICD-9-CM is the International Classification of Diseases, Ninth Revision, Clinical Modification , which assigns numeric codes to diagnoses. There are about 13,600 ICD-9-CM diagnosis codes.
CCS categorizes ICD-9-CM diagnoses and procedures into clinically meaningful categories. 6 This “clinical grouper” makes it easier to quickly understand patterns of diagnoses and procedures. Mental health conditions include CCS 650–659, 662, and 670. Substance abuse conditions include CCS 661 and 662.
Case definition
All-listed CCS diagnosis and external cause of injury codes used to identify mental health and substance abuse cases included:
Adjustment disorders
Anxiety disorders
Attention-deficit, conduct, and disruptive behavior disorders
Disorders usually diagnosed in infancy, childhood, or adolescence including pervasive development disorders, tic disorders, and elimination disorders
Impulse control disorders, not elsewhere classified
Mood disorders
Personality disorders
Schizophrenia and other psychotic disorders
Alcohol-related disorders
Drug-related disorders
Intentional self-harm/suicide and intentional self-inflicted injury
Miscellaneous disorders, including eating disorders, mental disorders in pregnancy, dissociative disorders, factitious disorders, sleep disorders, and somatoform disorders
Although dementia (CCS=653) and intellectual disability/developmental disorders (CCS=654) are listed in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition , these diagnoses, which are frequently characterized by the development of multiple cognitive impairments related to medical conditions, frequently require more medical than psychiatric treatment and thus are excluded from the analysis.
Treat-and-release ED visits
Treat-and-release ED visits were those ED visits in which patients are treated and released from that ED (i.e., they are not admitted to that specific hospital). While the majority of treat-an-release patients (92.2%) were discharged home, some were transferred to another acute care facility (1.5%), left against medical advice (1.7%), went to another type of long-term or intermediate care facility (nursing home or psychiatric treatment facility) (1.6%), referred to home health care (0.5%) or died (0.2%), or discharged alive but the destination is unknown (2.2%).
ED visits resulting in hospital admission
ED visits resulting in a hospital stay included those patients initially seen in the ED and then admitted to the same hospital.
Types of hospitals included in HCUP
HCUP is based on data from community hospitals, defined as short-term, non-Federal, general and other hospitals, excluding hospital units of other institutions (e.g., prisons). HCUP data include OB-GYN, ENT, orthopedic, cancer, pediatric, public, and academic medical hospitals. They exclude long-term care, rehabilitation, psychiatric, and alcoholism and chemical dependency hospitals, but these types of ED visits are included if they are from community hospitals.
Unit of analysis
The unit of analysis is the ED visit, not a person or patient. This means that a person who visits the ED multiple times in one year will be counted each time as a separate ED visit.
Payer is the primary expected payer for the ED visit. To make coding uniform across all HCUP data sources, payer combines detailed categories into more general groups:
Medicare includes fee-for-service and managed care. Medicare is a Health Insurance Program for people age 65 or older, some disabled people under age 65 (social security disability insurance), and people of all ages with End-Stage Renal Disease (permanent kidney failure treated with dialysis or a transplant).
Medicaid includes fee-for-service and managed care Medicaid patients.
Private insurance includes Blue Cross, commercial carriers, and private HMOs and PPOs.
Other includes Workers’ Compensation, TRICARE/CHAMPUS, CHAMPVA, Title V, and other government programs.
Uninsured includes an insurance status of “self-pay” and “no charge.”
When more than one payer is listed for a hospital discharge, the first-listed payer is used.
- For More Information
For more information about HCUP, visit www.hcup-us.ahrq.gov .
For additional HCUP statistics, visit HCUPnet, our interactive query system, at www.hcup.ahrq.gov .
For information on hospitalizations in the U.S., download HCUP Facts and Figures: Statistics on Hospital-Based Care in the United States in 2007 , located at http://www.hcup-us.ahrq.gov/reports.jsp .
For a detailed description of HCUP, more information on the design of the NEDS, and methods to calculate estimates, please refer to the following publications:
Steiner, C., Elixhauser, A., Schnaier, J. The Healthcare Cost and Utilization Project: An Overview. Effective Clinical Practice 2002;5(3):143–51.
Introduction to the HCUP Nationwide Emergency Department Sample, 2007 . Online. January, 2010. U.S. Agency for Healthcare Research and Quality. http://www.hcup-us.ahrq.gov/db/nation/neds/NEDS_2007_Introduction_v5.pdf
Houchens, R., Elixhauser, A. Final Report on Calculating Nationwide Inpatient Sample (NIS) Variances, 2001 . HCUP Methods Series Report #2003-2. Online. June 2005 (revised June 6, 2005). U.S. Agency for Healthcare Research and Quality. http://www.hcup-us.ahrq.gov/reports/CalculatingNISVariances200106092005.pdf
National Comorbidity Survey and National Comorbidity Survey Replication (NCS-R). Available at: www .hcp.med.harvard.edu/ncs . NCS-R Twelve-month Prevalence Estimates. Table 2. Available at: http://www .hcp.med.harvard .edu/ncs/ftpdir /NCS-R_12-month_Prevalence_Estimates .pdf
Institute of Medicine. Committee on Crossing the Quality Chasm: Adaptation to Mental Health and Addictive Disorders. Improving the Quality of Health Care for Mental and Substance-Use Conditions. Washington, D.C.: National Academies Press. 2006.
Larkin, G.L., Claassen, C.A., Edmond, J.A., Pelletier, A. J., and Camargo, C.A. Trends in U.S. Emergency Department Visits for Mental Health Conditions, 1992 to 2001. Psychiatric Services. 2005;56:671–677.
Institute of Medicine. Hospital-Based Emergency Care at the Breaking Point. Washington, D.C.: Institute of Medicine. 2004.
American College of Emergency Physicians (ACEP) Psychiatric and Substance Abuse Survey 2008. Fact Sheet. Available at: http://www .acep.org/uploadedFiles /ACEP/Advocacy /federal_issues /PsychiatricBoardingSummary.pdf
HCUP CCS. Healthcare Cost and Utilization Project (HCUP). June 2009. U.S. Agency for Healthcare Research and Quality, Rockville, MD. www .hcup-us.ahrq.gov /toolssoftware/ccs/ccs.jsp
Suggested Citation
Owens P.L., Mutter R., Stocks C. Mental Health and Substance Abuse-Related Emergency Department Visits among Adults, 2007 . HCUP Statistical Brief #92. July 2010. Agency for Healthcare Research and Quality, Rockville, MD. http://www .hcup-us.ahrq .gov/reports/statbriefs/sb92.pdf
About the NEDS : The HCUP Nationwide Emergency Department Sample (NEDS) is a nationwide database of hospital-based ED visits. The NEDS is nationally representative of all community hospital-based emergency departments (i.e., short-term, non-Federal, non-rehabilitation hospital-based emergency departments). The NEDS is a 20% stratified sample of hospital-based EDs and includes records on all patients, regardless of payer. The NEDS contains information on 26 million records (unweighted) on ED visits at over 950 hospitals in 27 states. The vast size of the NEDS allows the study of topics at both the national and regional levels for specific subgroups of patients. The NEDS is produced annually, beginning with the 2006 data year.
About HCUPnet : HCUPnet is an online query system that offers instant access to the largest set of all-payer health care databases that are publicly available. HCUPnet has an easy step-by-step query system, allowing for tables and graphs to be generated on national and regional statistics, as well as trends for community hospitals in the U.S. HCUPnet generates statistics using data from HCUP's Nationwide Inpatient Sample (NIS), the Kids' Inpatient Database (KID), the Nationwide Emergency Department Sample (NEDS), the State Inpatient Databases (SID) and the State Emergency Department Databases (SEDD).
- Cite this Page Owens PL, Mutter R, Stocks C. Mental Health and Substance Abuse-Related Emergency Department Visits among Adults, 2007. 2010 Jul. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006 Feb-. Statistical Brief #92.
- PDF version of this page (271K)
In this Page
- Healthcare Cost and Utilization Project (HCUP)
- Nationwide Inpatient Sample (NIS)
- Kids' Inpatient Database (KID)
- Nationwide Emergency Department Sample (NEDS)
- State Inpatient Databases (SID)
- State Ambulatory Surgery Databases (SASD)
- State Emergency Department Databases (SEDD)
- HCUP Overview
- HCUP Fact Sheet
- HCUP Partners
- HCUP User Support
Similar articles in PubMed
- Review Costs of Emergency Department Visits for Mental and Substance Use Disorders in the United States, 2017. [Healthcare Cost and Utilizatio...] Review Costs of Emergency Department Visits for Mental and Substance Use Disorders in the United States, 2017. Karaca Z, Moore BJ. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. 2006 Feb
- Review Emergency Department Visits for Injurious Falls among the Elderly, 2006. [Healthcare Cost and Utilizatio...] Review Emergency Department Visits for Injurious Falls among the Elderly, 2006. Owens PL, Russo CA, Spector W, Mutter R. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. 2006 Feb
- Review Expected Payers and Patient Characteristics of Maternal Emergency Department Care, 2019. [Healthcare Cost and Utilizatio...] Review Expected Payers and Patient Characteristics of Maternal Emergency Department Care, 2019. McDermott KW, Reid LD, Owens PL. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. 2006 Feb
- Review Racial and Ethnic Differences in Emergency Department Visits Related to Substance Use Disorders, 2019. [Healthcare Cost and Utilizatio...] Review Racial and Ethnic Differences in Emergency Department Visits Related to Substance Use Disorders, 2019. Owens PL, Moore BJ. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. 2006 Feb
- Review Emergency Department Visits Involving Dental Conditions, 2018. [Healthcare Cost and Utilizatio...] Review Emergency Department Visits Involving Dental Conditions, 2018. Owens PL, Manski RJ, Weiss AJ. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. 2006 Feb
Recent Activity
- Mental Health and Substance Abuse-Related Emergency Department Visits among Adul... Mental Health and Substance Abuse-Related Emergency Department Visits among Adults, 2007 - Healthcare Cost and Utilization Project (HCUP) Statistical Briefs
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Nuvo & Ouma Partner to Deliver World’s First Telehealth & Remote Monitoring Solution for Pregnancy
Combination of clinical telehealth excellence & FDA-cleared remote monitoring platform provides a one-of-a-kind solution for next generation pregnancy care

TEL AVIV, ISRAEL & AUSTIN, TEXAS, December 13, 2022 – Nuvo Group (Nuvo), the creators of INVU by Nuvo™, an FDA-approved remote pregnancy monitoring platform, and Ouma Health (Ouma), a total maternity telehealth services company, today announced a strategic partnership to deliver an innovative joint solution that provides clinical excellence in maternity telehealth and FDA-cleared remote fetal surveillance technology. The joint solution is designed to address some of the biggest challenges in pregnancy care today, by enabling equitable access to care, improving preventative care delivery, and reducing high individual and system-level costs.
The joint solution is a “one-stop shop” for remote pregnancy care that includes:
- Innovative platform for remote patient monitoring (RPM) including FDA-cleared non-stress tests (NST), along with devices for diabetes and hypertension management
- 24/7/365 maternity telehealth clinical services available in all fifty US states, including access to maternal-fetal medicine specialists, midwives, perinatal nurse navigators, lactation consultants, and behavioral health specialists with expertise in perinatal mood disorders
Nuvo and Ouma were both founded with shared principles: building solutions based on clinical evidence, improving clinical outcomes, and increasing patients’ access to care and peace of mind. Nuvo’s FDA-cleared, clinically validated remote monitoring solution and Ouma’s network of telehealth clinicians extend medical-grade monitoring and highly trained maternity care experts to fit into patients’ lives and schedules.
“The innovative joint offering from Nuvo and Ouma addresses critical gaps in the pregnancy care journey while maintaining the highest levels of medical care and allowing patients access when and where they need it,” said Kelly Londy, CEO of Nuvo Group. “We are happy to work with Ouma to give employers, health systems, and payers the ability to impact areas of pregnancy care that need it the most.”
“An effective strategy aimed at improving maternity outcomes needs to include an early recognition system coupled with immediate access to expert care,” said Sina Haeri, MD, MHSA, CEO and co-founder of Ouma. “By combining a market-ready RPM solution with world-class clinical services, we aim to deliver the clinical care in the comfort of the patient’s home, saving the family unnecessary time commuting to appointments, absenteeism from work for routine visits, and most importantly, immediate access to expert care in case of clinical need for timely intervention.”
Self-insured employers, health systems, and payers can all benefit from adopting this new solution for the flexibility, scalability, and convenience it provides their organizations, patients, and members. More than half (54%) of counties in the United States offer very limited or no access to maternity care. Within these counties, more than 2.2 million women of child-bearing age live in full maternity care deserts – areas with no hospital offering obstetric care, no birthing center, or no obstetric provider. Additionally, 1-in-3 patients change insurance providers from preconception to postpartum, though this solution provides an important competitive advantage to improve member satisfaction, retention, and improved outcomes.
Recent News & Announcements

MedArrive partners with Ouma to bring in-home maternal care to Medicaid members

Ouma presents research at 2023 SMFM Annual Pregnancy Meeting

Ouma selected as ATA Telehealth Innovators Challenge Finalist
Ouma services.

An official website of the United States government
The .gov means it’s official. A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Telehealth for maternal health services
Billing for maternal telehealth.
As you are preparing to launch your maternal telehealth care program, take time to fully understand your billing options .
You may need to consider extra staffing or additional training so your office is ready to seamlessly handle telehealth billing.
The COVID-19 public health emergency led the Center for Medicare and Medicaid Services (CMS) to expand its coverage for telehealth care . Many state Medicaid programs and private insurers are also covering telehealth appointments the same as an in-person appointment, with patients paying their typical co-pays.
You can also choose to offer a discounted cash pay program or private payment options for the underinsured or the uninsured. One possible way to offer discounted payment is to find stakeholders willing to partner with you. You could also explore local, state, and federal grant funding options.
Get more information on billing for direct-to-consumer telehealth .
Medicare billing guidance
The following common Current Procedural Terminology (CPT®) and Healthcare Common Procedure Coding System (HCPCS) codes are used to bill for services for telemedicine in maternal health, and include updates provided to the 2022 Medicare Physician Fee Schedule - PFS (PDF).
Coding guidance is subject to change. Please refer to the complete list of telehealth services covered by Medicare during the COVID-19 public health emergency from the Centers for Medicare & Medicaid Services.
Although Medicare reimburses for audio and video telehealth, audio-only reimbursement is currently covered only during the COVID-19 public health emergency.
Audio-only or video telehealth
*Remains available until December 31, 2023
**Will expire at some point after the COVID-19 public health emergency is declared over
Medicare telemedicine health care provider fact sheet — Centers for Medicare & Medicaid Services (CMS)

Home Visiting and Support for Pregnant Women Issue Brief
← explore all resources.
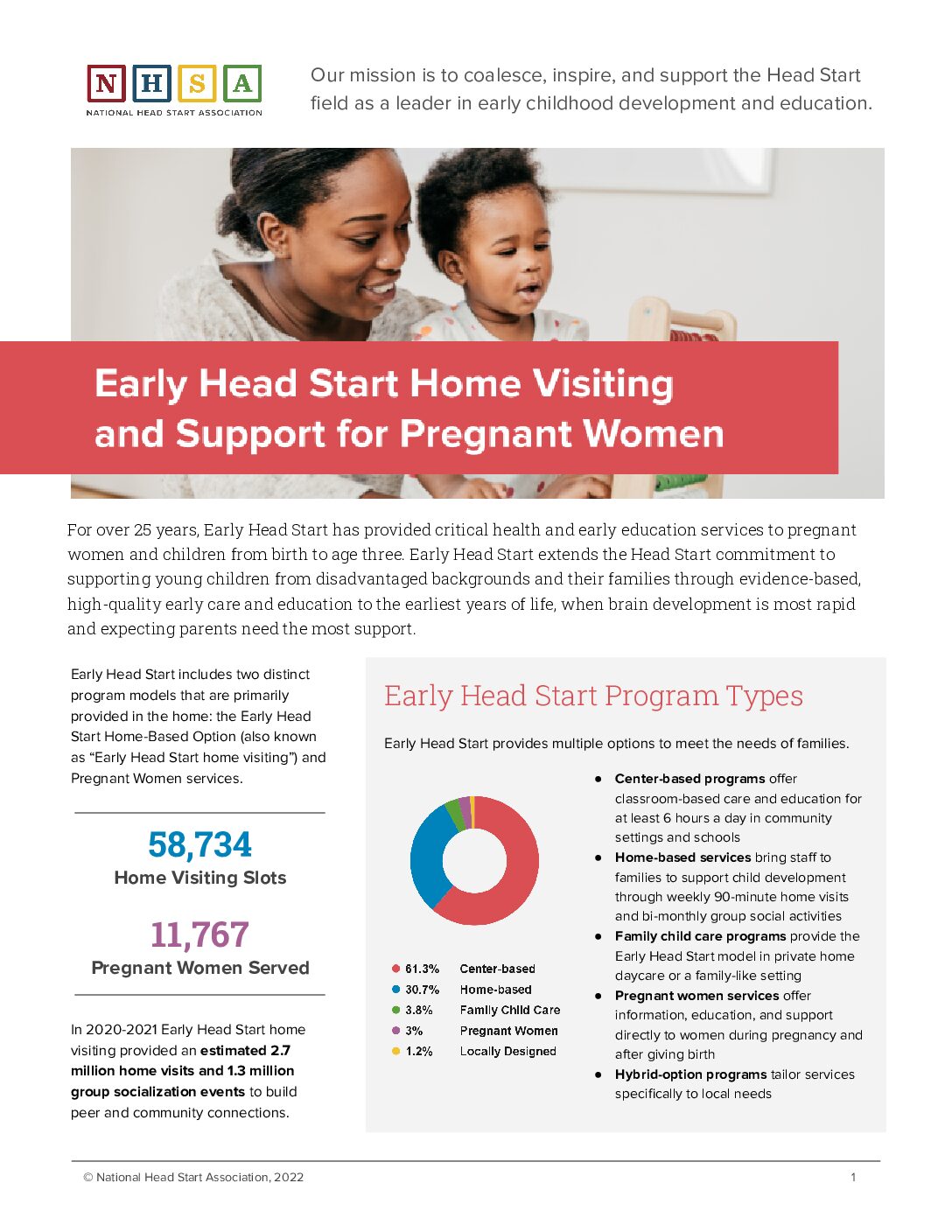
Early Head Start home visiting provides services in the home to vulnerable children and families, connecting pregnant women and their families to prenatal care, fostering strong parent-child relationships, and supporting the role of parents as their children’s first and primary teachers. One-third of all Early Head Start slots are designated home-visiting or prenatal services.
The recommended reauthorization of the MIECHV program highlights the importance of quality programs. Early Head Start is proud to be one of MIECHV’s approved evidence-based models. Download the full brief and learn more about their important work.
Fact Sheet Citations
Related Content
Early head start rising, home visitors in wv approach families with understanding.
Kansas Home Visiting

What is MCH Home Visiting?

- Spring Member Drive
- Join our nonprofit and nonpartisan newsroom today to build a better California for tomorrow.
- Newsletters
- Environment
- 2024 Voter Guide
- Digital Democracy
- Daily Newsletter
- Data & Trackers
- California Divide
- CalMatters for Learning
- College Journalism Network
- What’s Working
- Youth Journalism
- Manage donation
- News and Awards
- Sponsorship
- Inside the Newsroom
- CalMatters en Español
California hospitals keep closing their labor wards. Can lawmakers do anything about it?

Share this:
- Click to share on X (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on WhatsApp (Opens in new window)

Two California lawmakers introduced bills intended to slow maternity ward closures after a CalMatters investigation found nearly 50 hospitals had ended labor and delivery services between 2012 and 2023.
Lea esta historia en Español
In just the first few months of 2024, four California hospitals have closed or announced plans to close their maternity wards.
The closures are part of an accelerating trend unfolding across the state, creating maternity care deserts and decreasing access to prenatal care. In the past three years, 29 hospitals stopped delivering babies, according to a CalMatters investigation on maternity ward closures . Nearly 50 obstetrics departments have closed over the past decade.
Now, California lawmakers are trying to slow the trend.
Assemblymember Akilah Weber and Sen. Dave Cortese are pursuing legislation to increase transparency around planned maternity ward closures, potentially giving counties and the state time to intervene.
Weber, a Democrat from La Mesa, wants hospitals to notify the state a year in advance if labor and delivery services are at risk of ending. The measure would also require the state to conduct a community impact report when a hospital indicates that it may lose maternity care.
Cortese, a Democrat from Campbell, wants to increase the public notification requirement of an impending closure from 90 days to 120 days and require the hospital to conduct an analysis of how a closure could increase costs for the county health system, where the next closest maternity wards are located and who is most likely to be affected.
Cortese’s bill would also require increased notification for planned closures of inpatient psychiatric services.
“We cannot continue to just discuss these issues and not implement policies to prevent or mitigate the harms and the continued disparities,” Weber said during an Assembly Health Committee hearing Tuesday.
Groups representing doctors and reproductive health advocates support the measure. Cortese’s bill is supported by nurses and consumer health advocates.
Why are California maternity wards closing?
Ryan Spencer, a lobbyist for the regional chapter of American College of Obstetricians and Gynecologists who testified in support of Weber’s measure, said there are often situations during birth where “every minute can be the difference between life and death.”
“What if you are a patient like this and literally had nowhere to go who had to drive hours upon hours to get care? We have to find a way to end this crisis,” Spencer said during his testimony.
Learn more about legislators mentioned in this story.
Dave Cortese
Democrat, State Senate, District 15 (Campbell)
Akilah Weber
Democrat, State Assembly, District 79 (La Mesa)
Maternity wards are closing for a number of reasons, according to hospital administrators. They cite labor shortages, increasing costs, low reimbursements and declining birth rates.
The California Hospital Association opposes Cortese’s bill and has registered “concerns” about Weber’s. The group argues that neither bill will address the underlying reasons for maternity ward closures and may cause hospitals to terminate services sooner as employees leave and patients look elsewhere for care, said Kirsten Barlow, vice president of policy with the hospital association during a Senate hearing earlier this month.
Current law requires hospitals to notify the public 90 days before a proposed service cut, but doesn’t require additional notification to be given to the state. Weber said that 90 days is “clearly not sufficient for the state to be able to intervene.”
Maternity care deserts emerge
CalMatters found that 12 counties have no hospital delivering babies, including Madera County where the sudden closure of the county’s only hospital in 2022 spurred a flurry of emergency legislation supporting distressed hospitals .
Madera Community Hospital now is on track to reopen, but without a maternity ward. The company reopening the hospital, American Advanced Management, has indicated that low insurance reimbursement rates factored into its decision to open without labor and delivery.
“Reopening maternity would be like reopening two hospitals at the same time,” Matthew Beehler, chief strategy officer at American Advanced Management, previously told CalMatters.
Still, the bill authors and advocates are adamant that access to maternity care is a necessity. National studies indicate that rates of preterm birth increase and women receive less prenatal care when labor and delivery units shut down, particularly in rural areas. CalMatters found that maternity closures in California disproportionately impact low-income and Latino communities.
“This is really a very simple bill. It doesn’t do much. It creates a public hearing opportunity at the local level to deal with issues that are…absolutely vital to the survival of our constituents,” Cortese said during a Senate Health Committee hearing on his measure.
Supported by the California Health Care Foundation (CHCF), which works to ensure that people have access to the care they need, when they need it, at a price they can afford. Visit www.chcf.org to learn more.
More on maternal health

Vast stretches of California lose maternity care as dozens of hospitals shut labor wards

Why tortillas sold in California may be forced to add a new ingredient
We want to hear from you
Want to submit a guest commentary or reaction to an article we wrote? You can find our submission guidelines here . Please contact CalMatters with any commentary questions: [email protected]
Kristen Hwang Health Reporter
Kristen Hwang is a health reporter for CalMatters covering health care access, abortion and reproductive health, workforce issues, drug costs and emerging public health matters. Her series on soaring rates... More by Kristen Hwang
We've recently sent you an authentication link. Please, check your inbox!
Sign in with a password below, or sign in using your email .
Get a code sent to your email to sign in, or sign in using a password .
Enter the code you received via email to sign in, or sign in using a password .
Subscribe to our newsletters:
- WeeklyMatters Catch up on the top stories in California with a summary of our reporting and commentary from the past week.
- Weekly Walters Get a digest of new insights from veteran journalist Dan Walters, who holds powerful people in California accountable.
- WhatMatters Start your day with a comprehensive rundown of the most important stories in California politics and policy.
- Inequality Insights Your weekly must-read to stay on top of inequality, one of California’s most pressing issues.
Sign in with your email
Lost your password?
Try a different email
Send another code
Sign in with a password

IMAGES
VIDEO
COMMENTS
The Pregnancy Care Incentive Program offers expectant mothers support and rewards during each stage of pregnancy. You could be eligible* to earn a free Pregnancy Care Box packed with items you can use during and after pregnancy—and $75 in wellness rewards. *You must be 18 or older on a FEP Blue Standard™ or FEP Blue Basic™ plan to earn ...
08-20 Request for Application for Mental Health Services Act (MHSA) Workforce Education an d Training Funding for Regional Partnerships. 08-13 Funding Augmentation to the MHSA WET Component. 07-14 MHSA WET Component - Proposed Three-Year Program and Expenditure Plan Guidelines, FYs 2006-07, 2007-08, and 2008-09
The recommended content of the [well-woman prenatal care] visit includes specific tests and procedures (e.g., blood pressure, weight, urine test, uterine size and fetal heart rate assessment, glucose tolerance testing, and screening for specific sexually transmitted infections and genetic or developmental conditions), as well as topics for counseling and guidance (e.g., tobacco avoidance and ...
Goal 1: Improve access to quality health services. Goal 2: Foster a health care workforce able to address current and emerging needs. Goal 3: Achieve health equity and enhance population health. Goal 4: Optimize HRSA operations and strengthen program management.
This Maternal, Infant, and Early Childhood Home Visiting Orientation Guide provides an overview of the MIECHV Program, with information that will be useful to state, territory, and local implementing agency (LIA) employees who are new to MIECHV. It is a companion resource to Best Practices for Onboarding New MIECHV Employees: A Toolkit, which ...
Bipartisan support for the Maternal, Infant, and Early Childhood Home Visiting program is strong. Evidence-based home visiting programs are proven and cost-effective services that improve the ...
New requirement for evidenced-informed home visits in 2021. Objective of the home visiting program is to improve maternal and infant health outcomes and reduce maternal and infant morbidity and mortality, especially in individuals identified to be at risk. Home visits for all first-time parents, parents/caregivers of infants with additional ...
Apps are also available to provide educational information for mothers. One example, Text4baby, provides regular text messages on nutrition, doctor visits, pregnancy and baby milestones, and other important health topics. While rural hospitals are working to address these challenges and improve access to maternal health, they cannot do this alone.
Your first prenatal visit will probably be scheduled sometime after your eighth week of pregnancy. Most health care providers won't schedule a visit any earlier unless you have a medical condition, have had problems with a pregnancy in the past, or have symptoms such as spotting or bleeding, stomach pain, or severe nausea and vomiting. 1 You've probably heard pregnancy discussed in terms of ...
The Health Resources and Services Administration yesterday awarded states and territories an additional $81 million in emergency funding from the American Rescue Plan Act for the Maternal, Infant, and Early Childhood Home Visiting Program, which provides voluntary home visits to improve maternal and child health for families in high-risk communities.
Well-Child Visit: Early childhood is a time of rapid growth and development. Well-child visits are an important opportunity for health care providers to evaluate children's physical, social, and emotional development and to provide essential preventive care including regular immunizations. 19,20. Home visiting
Maternal Infant Health Program (MIHP) promotes healthy pregnancies, positive birth outcomes, and healthy infant growth and development with the long-term goal of reducing infant mortality and morbidity. Nurses and social workers provide professional case management and health education services, promote health equity, and provide individualized ...
Patient and payer characteristics of types of MHSA-related ED visits. Table 1 shows that ED visits related to mental health conditions were more likely to be for women (65.4 percent), while ED visits related to substance abuse conditions (29.3 percent) and co-occurring MHSA conditions (43.0 percent) were less likely to be for women and more likely to be for men.
MHSA Funded PEI Program Summary #3 . Project SUCCESS . Background - Project SUCCESS (Schools Using Coordinated Community Efforts to Strengthen Students), is a SAMHSA model program that prevents and reduces substance use and abuse and associated behavioral issues among high risk, multi ‐ problem adolescents.
24/7/365 maternity telehealth clinical services available in all fifty US states, including access to maternal-fetal medicine specialists, midwives, perinatal nurse navigators, lactation consultants, and behavioral health specialists with expertise in perinatal mood disorders. Nuvo and Ouma were both founded with shared principles: building ...
The following common Current Procedural Terminology (CPT®) and Healthcare Common Procedure Coding System (HCPCS) codes are used to bill for services for telemedicine in maternal health, and include updates provided to the 2022 Medicare Physician Fee Schedule - PFS (PDF). Coding guidance is subject to change. Please refer to the complete list ...
The Health Resources and Services Administration yesterday awarded states and territories $40 million in emergency funding from the American Rescue Plan Act for the Maternal, Infant, and Early Childhood Home Visiting Program, which provides voluntary home visits to improve maternal and child health for families in high-risk communities.. Families that cannot access home visiting services due ...
For a healthy pregnancy, your doctor will probably want to see you on the following recommended schedule of prenatal visits: Weeks 4 to 28: 1 prenatal visit a month. Weeks 28 to 36: 1 prenatal ...
Early Head Start home visiting provides services in the home to vulnerable children and families, connecting pregnant women and their families to prenatal care, fostering strong parent-child relationships, and supporting the role of parents as their children's first and primary teachers. One-third of all Early Head Start slots are designated ...
Home visitors and families develop strong relationships and trust. They meet regularly to address families' needs. The Program aims to: Improve the overall health of mothers and children. Get children ready to succeed in school. Improve families' economic well-being. Connect families to other resources in their community (for example WIC.
As part of the Kansas Maternal and Child Health (MCH) program, grantees may opt to implement Home Visiting services to provide information, education, initiate referrals, and assist with accessing community systems of care within the target population of pregnant women, mothers, and infants (birth to 12 months.) The primary goals are to support healthy pregnancies, improve birth outcomes, and ...
The AIM Capacity Program and the Integrated Maternal Health Services Program are part of HRSA's effort to address maternal mortality and severe maternal morbidity. Please review the eligibility and project narrative sections for each program carefully. Please note that the program requirements for each of these programs are different, and ...
Maternity wards are closing for a number of reasons, according to hospital administrators. They cite labor shortages, increasing costs, low reimbursements and declining birth rates. ... when they need it, at a price they can afford. Visit www.chcf.org to learn more. More on maternal health. Vast stretches of California lose maternity care as ...