- Search Menu
- Advance Articles
- Editor's Choice
- Supplements
- Patient Perspectives
- Methods Corner
- Science for Patients
- Invited Commentaries
- ESC Content Collections
- Author Guidelines
- Instructions for reviewers
- Submission Site
- Why publish with EJCN?
- Open Access Options
- Self-Archiving Policy
- Read & Publish
- About European Journal of Cardiovascular Nursing
- About ACNAP
- About European Society of Cardiology
- ESC Publications
- Editorial Board
- Advertising & Corporate Services
- War in Ukraine
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, why patient journey mapping, how is patient journey mapping conducted, use of technology in patient journey mapping, future implications for patient journey mapping, conclusions, patient journey mapping: emerging methods for understanding and improving patient experiences of health systems and services.
Lemma N Bulto and Ellen Davies Shared first authorship.
Conflict of interest: none declared.
- Article contents
- Figures & tables
- Supplementary Data
Lemma N Bulto, Ellen Davies, Janet Kelly, Jeroen M Hendriks, Patient journey mapping: emerging methods for understanding and improving patient experiences of health systems and services, European Journal of Cardiovascular Nursing , 2024;, zvae012, https://doi.org/10.1093/eurjcn/zvae012
- Permissions Icon Permissions
Patient journey mapping is an emerging field of research that uses various methods to map and report evidence relating to patient experiences and interactions with healthcare providers, services, and systems. This research often involves the development of visual, narrative, and descriptive maps or tables, which describe patient journeys and transitions into, through, and out of health services. This methods corner paper presents an overview of how patient journey mapping has been conducted within the health sector, providing cardiovascular examples. It introduces six key steps for conducting patient journey mapping and describes the opportunities and benefits of using patient journey mapping and future implications of using this approach.
Acquire an understanding of patient journey mapping and the methods and steps employed.
Examine practical and clinical examples in which patient journey mapping has been adopted in cardiac care to explore the perspectives and experiences of patients, family members, and healthcare professionals.
Quality and safety guidelines in healthcare services are increasingly encouraging and mandating engagement of patients, clients, and consumers in partnerships. 1 The aim of many of these partnerships is to consider how health services can be improved, in relation to accessibility, service delivery, discharge, and referral. 2 , 3 Patient journey mapping is a research approach increasingly being adopted to explore these experiences in healthcare. 3
a patient-oriented project that has been undertaken to better understand barriers, facilitators, experiences, interactions with services and/or outcomes for individuals and/or their carers, and family members as they enter, navigate, experience and exit one or more services in a health system by documenting elements of the journey to produce a visual or descriptive map. 3
It is an emerging field with a clear patient-centred focus, as opposed to studies that track patient flow, demand, and movement. As a general principle, patient journey mapping projects will provide evidence of patient perspectives and highlight experiences through the patient and consumer lens.
Patient journey mapping can provide significant insights that enable responsive and context-specific strategies for improving patient healthcare experiences and outcomes to be designed and implemented. 3–6 These improvements can occur at the individual patient, model of care, and/or health system level. As with other emerging methodologies, questions have been raised regarding exactly how patient journey mapping projects can best be designed, conducted, and reported. 3
In this methods paper, we provide an overview of patient journey mapping as an emergent field of research, including reasons that mapping patient journeys might be considered, methods that can be adopted, the principles that can guide patient journey mapping data collection and analysis, and considerations for reporting findings and recognizing the implications of findings. We summarize and draw on five cardiovascular patient journey mapping projects, as examples.
One of the most appealing elements of the patient journey mapping field of research is its focus on illuminating the lived experiences of patients and/or their family members, and the health professionals caring for them, methodically and purposefully. Patient journey mapping has an ability to provide detailed information about patient experiences, gaps in health services, and barriers and facilitators for access to health services. This information can be used independently, or alongside information from larger data sets, to adapt and improve models of care relevant to the population that is being investigated. 3
To date, the most frequent reason for adopting this approach is to inform health service redesign and improvement. 3 , 7 , 8 Other reasons have included: (i) to develop a deeper understanding of a person’s entire journey through health systems; 3 (ii) to identify delays in diagnosis or treatment (often described as bottlenecks); 9 (iii) to identify gaps in care and unmet needs; (iv) to evaluate continuity of care across health services and regions; 10 (v) to understand and evaluate the comprehensiveness of care; 11 (vi) to understand how people are navigating health systems and services; and (vii) to compare patient experiences with practice guidelines and standards of care.
Patient journey mapping approaches frequently use six broad steps that help facilitate the preparation and execution of research projects. These are outlined in the Central illustration . We acknowledge that not all patient journey mapping approaches will follow the order outlined in the Central illustration , but all steps need to be considered at some point throughout each project to ensure that research is undertaken rigorously, appropriately, and in alignment with best practice research principles.
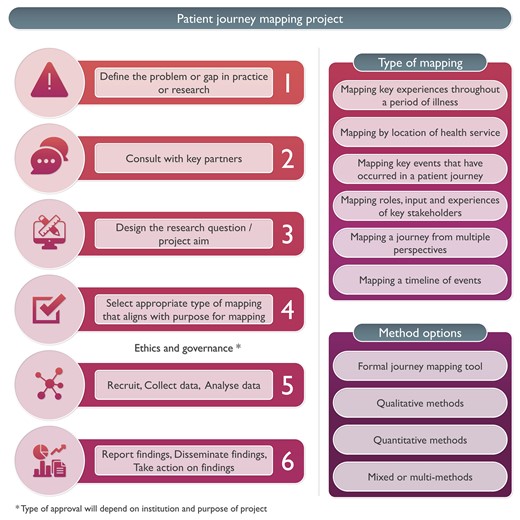
Steps for conducing patient journey mapping.
Five cardiovascular patient journey mapping research examples have been included in Figure 1 , 12–16 to provide specific context and illustrate these six steps. For each of these examples, the problem or gap in practice or research, consultation processes, research question or aim, type of mapping, methods, and reporting of findings have been extracted. Each of these steps is then discussed, using these cardiovascular examples.
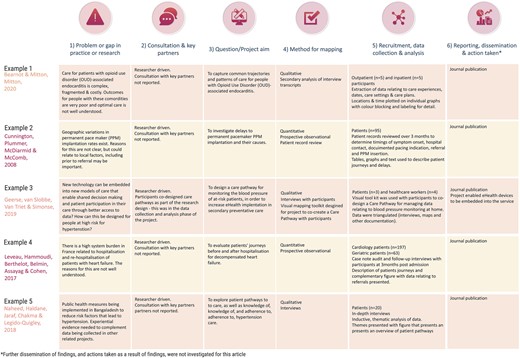
Examples of patient journey mapping projects.
Define the problem or gap in practice or research
Developing an understanding of a problem or gap in practice is essential for facilitating the design and development of quality research projects. In the examples outlined in Figure 1 , it is evident that clinical variation or system gaps have been explored using patient journey mapping. In the first two examples, populations known to have health vulnerabilities were explored—in Example 1, this related to comorbid substance use and physical illness, 13 and in Example 2, this related to geographical location. 13 Broader systems and societal gaps were explored in Examples 4 and 5, respectively, 15 , 16 and in Example 3, a new technologically driven solution for an existing model of care was tested for its ability to improve patient outcomes relating to hypertension. 14
Consultation, engagement, and partnership
Ideally, consultation with heathcare providers and/or patients would occur when the problem or gap in practice or research is being defined. This is a key principle of co-designed research. 17 Numerous existing frameworks for supporting patient involvement in research have been designed and were recently documented and explored in a systematic review by Greenhalgh et al . 18 While none of the five example studies included this step in the initial phase of the project, it is increasingly being undertaken in patient partnership projects internationally (e.g. in renal care). 17 If not in the project conceptualization phase, consultation may occur during the data collection or analysis phase, as demonstrated in Example 3, where a care pathway was co-created with participants. 14 We refer readers to Greenhalgh’s systematic review as a starting point for considering suitable frameworks for engaging participants in consultation, partnership, and co-design of patient journey mapping projects. 18
Design the research question/project aim
Conducting patient journey mapping research requires a thoughtful and systematic approach to adequately capture the complexity of the healthcare experience. First, the research objectives and questions should be clearly defined. Aspects of the patient journey that will be explored need to be identified. Then, a robust approach must be developed, taking into account whether qualitative, quantitative, or mixed methods are more appropriate for the objectives of the study.
For example, in the cardiac examples in Figure 1 , the broad aims included mapping existing pathways through health services where there were known problems 12 , 13 , 15 , 16 and documenting the co-creation of a new care pathway using quantitative, qualitative, or mixed methods. 14
In traditional studies, questions that might be addressed in the area of patient movement in health systems include data collected through the health systems databases, such as ‘What is the length of stay for x population’, or ‘What is the door to balloon time in this hospital?’ In contrast, patient mapping journey studies will approach asking questions about experiences that require data from patients and their family members, e.g. ‘What is the impact on you of your length of stay?’, ‘What was your experience in being assessed and undergoing treatment for your chest pain?’, ‘What was your experience supporting this patient during their cardiac admission and discharge?’
Select appropriate type of mapping
The methods chosen for mapping need to align with the identified purpose for mapping and the aim or question that was designed in Step 3. A range of research methods have been used in patient journey mapping projects involving various qualitative, quantitative, and mixed methods techniques and tools. 4 Some approaches use traditional forms of data collection, such as short-form and long-form patient interviews, focus groups, and direct patient observations. 18 , 19 Other approaches use patient journey mapping tools, designed and used with specific cultural groups, such as First Nations peoples using artwork, paintings, sand trays, and photovoice. 17 , 20 In the cardiovascular examples presented in Figure 1 , both qualitative and quantitative methods have been used, with interviews, patient record reviews, and observational techniques adopted to map patient journeys.
In a recent scoping review investigating patient journey mapping across all health care settings and specialities, six types of patient journey mapping were identified. 3 These included (i) mapping key experiences throughout a period of illness; (ii) mapping by location of health service; (iii) mapping by events that occurred throughout a period of illness; (iv) mapping roles, input, and experiences of key stakeholders throughout patient journeys; (v) mapping a journey from multiple perspectives; and (vi) mapping a timeline of events. 3 Combinations or variations of these may be used in cardiovascular settings in the future, depending on the research question, and the reasons mapping is being undertaken.
Recruit, collect data, and analyse data
The majority of health-focused patient journey mapping projects published to date have recruited <50 participants. 3 Projects with fewer participants tend to be qualitative in nature. In the cardiovascular examples provided in Figure 1 , participant numbers range from 7 14 to 260. 15 The 3 studies with <20 participants were qualitative, 12 , 14 , 16 and the 2 with 95 and 260 participants, respectively, were quantitative. 13 , 15 As seen in these and wider patient journey mapping examples, 3 participants may include patients, relatives, carers, healthcare professionals, or other stakeholders, as required, to meet the study objectives. These different participant perspectives may be analysed within each participant group and/or across the wider cohort to provide insights into experiences, and the contextual factors that shape these experiences.
The approach chosen for data collection and analysis will vary and depends on the research question. What differentiates data analysis in patient journey mapping studies from other qualitative or quantitative studies is the focus on describing, defining, or exploring the journey from a patient’s, rather than a health service, perspective. Dimensions that may, therefore, be highlighted in the analysis include timing of service access, duration of delays to service access, physical location of services relative to a patient’s home, comparison of care received vs. benchmarked care, placing focus on the patient perspective.
The mapping of individual patient journeys may take place during data collection with the use of mapping templates (tables, diagrams, and figures) and/or later in the analysis phase with the use of inductive or deductive analysis, mapping tables, or frameworks. These have been characterized and visually represented in a recent scoping review. 3 Representations of patient journeys can also be constructed through a secondary analysis of previously collected data. In these instances, qualitative data (i.e. interviews and focus group transcripts) have been re-analysed to understand whether a patient journey narrative can be extracted and reported. Undertaking these projects triggers a new research cycle involving the six steps outlined in the Central illustration . The difference in these instances is that the data are already collected for Step 5.
Report findings, disseminate findings, and take action on findings
A standardized, formal reporting guideline for patient journey mapping research does not currently exist. As argued in Davies et al ., 3 a dedicated reporting guide for patient journey mapping would be ill-advised, given the diversity of approaches and methods that have been adopted in this field. Our recommendation is for projects to be reported in accordance with formal guidelines that best align with the research methods that have been adopted. For example, COREQ may be used for patient journey mapping where qualitative methods have been used. 20 STROBE may be used for patient journey mapping where quantitative methods have been used. 21 Whichever methods have been adopted, reporting of projects should be transparent, rigorous, and contain enough detail to the extent that the principles of transparency, trustworthiness, and reproducibility are upheld. 3
Dissemination of research findings needs to include the research, healthcare, and broader communities. Dissemination methods may include academic publications, conference presentations, and communication with relevant stakeholders including healthcare professionals, policymakers, and patient advocacy groups. Based on the findings and identified insights, stakeholders can collaboratively design and implement interventions, programmes, or improvements in healthcare delivery that overcome the identified challenges directly and address and improve the overall patient experience. This cyclical process can hopefully produce research that not only informs but also leads to tangible improvements in healthcare practice and policy.
Patient journey mapping is typically a hands-on process, relying on surveys, interviews, and observational research. The technology that supports this research has, to date, included word processing software, and data analysis packages, such as NVivo, SPSS, and Stata. With the advent of more sophisticated technological tools, such as electronic health records, data analytics programmes, and patient tracking systems, healthcare providers and researchers can potentially use this technology to complement and enhance patient journey mapping research. 19 , 20 , 22 There are existing examples where technology has been harnessed in patient journey. Lee et al . used patient journey mapping to verify disease treatment data from the perspective of the patient, and then the authors developed a mobile prototype that organizes and visualizes personal health information according to the patient-centred journey map. They used a visualization approach for analysing medical information in personal health management and examined the medical information representation of seven mobile health apps that were used by patients and individuals. The apps provide easy access to patient health information; they primarily import data from the hospital database, without the need for patients to create their own medical records and information. 23
In another example, Wauben et al. 19 used radio frequency identification technology (a wireless system that is able to track a patient journey), as a component of their patient journey mapping project, to track surgical day care patients to increase patient flow, reduce wait times, and improve patient and staff satisfaction.
Patient journey mapping has emerged as a valuable research methodology in healthcare, providing a comprehensive and patient-centric approach to understanding the entire spectrum of a patient’s experience within the healthcare system. Future implications of this methodology are promising, particularly for transforming and redesigning healthcare delivery and improving patient outcomes. The impact may be most profound in the following key areas:
Personalized, patient-centred care : The methodology allows healthcare providers to gain deep insights into individual patient experiences. This information can be leveraged to deliver personalized, patient-centric care, based on the needs, values, and preferences of each patient, and aligned with guideline recommendations, healthcare professionals can tailor interventions and treatment plans to optimize patient and clinical outcomes.
Enhanced communication, collaboration, and co-design : Mapping patient interactions with health professionals and journeys within and across health services enables specific gaps in communication and collaboration to be highlighted and potentially informs responsive strategies for improvement. Ideally, these strategies would be co-designed with patients and health professionals, leading to improved care co-ordination and healthcare experience and outcomes.
Patient engagement and empowerment : When patients are invited to share their health journey experiences, and see visual or written representations of their journeys, they may come to understand their own health situation more deeply. Potentially, this may lead to increased health literacy, renewed adherence to treatment plans, and/or self-management of chronic conditions such as cardiovascular disease. Given these benefits, we recommend that patients be provided with the findings of research and quality improvement projects with which they are involved, to close the loop, and to ensure that the findings are appropriately disseminated.
Patient journey mapping is an emerging field of research. Methods used in patient journey mapping projects have varied quite significantly; however, there are common research processes that can be followed to produce high-quality, insightful, and valuable research outputs. Insights gained from patient journey mapping can facilitate the identification of areas for enhancement within healthcare systems and inform the design of patient-centric solutions that prioritize the quality of care and patient outcomes, and patient satisfaction. Using patient journey mapping research can enable healthcare providers to forge stronger patient–provider relationships and co-design improved health service quality, patient experiences, and outcomes.
None declared.
Farmer J , Bigby C , Davis H , Carlisle K , Kenny A , Huysmans R , et al. The state of health services partnering with consumers: evidence from an online survey of Australian health services . BMC Health Serv Res 2018 ; 18 : 628 .
Google Scholar
Kelly J , Dwyer J , Mackean T , O’Donnell K , Willis E . Coproducing Aboriginal patient journey mapping tools for improved quality and coordination of care . Aust J Prim Health 2017 ; 23 : 536 – 542 .
Davies EL , Bulto LN , Walsh A , Pollock D , Langton VM , Laing RE , et al. Reporting and conducting patient journey mapping research in healthcare: a scoping review . J Adv Nurs 2023 ; 79 : 83 – 100 .
Ly S , Runacres F , Poon P . Journey mapping as a novel approach to healthcare: a qualitative mixed methods study in palliative care . BMC Health Serv Res 2021 ; 21 : 915 .
Arias M , Rojas E , Aguirre S , Cornejo F , Munoz-Gama J , Sepúlveda M , et al. Mapping the patient’s journey in healthcare through process mining . Int J Environ Res Public Health 2020 ; 17 : 6586 .
Natale V , Pruette C , Gerohristodoulos K , Scheimann A , Allen L , Kim JM , et al. Journey mapping to improve patient-family experience and teamwork: applying a systems thinking tool to a pediatric ambulatory clinic . Qual Manag Health Care 2023 ; 32 : 61 – 64 .
Cherif E , Martin-Verdier E , Rochette C . Investigating the healthcare pathway through patients’ experience and profiles: implications for breast cancer healthcare providers . BMC Health Serv Res 2020 ; 20 : 735 .
Gilburt H , Drummond C , Sinclair J . Navigating the alcohol treatment pathway: a qualitative study from the service users’ perspective . Alcohol Alcohol 2015 ; 50 : 444 – 450 .
Gichuhi S , Kabiru J , M’Bongo Zindamoyen A , Rono H , Ollando E , Wachira J , et al. Delay along the care-seeking journey of patients with ocular surface squamous neoplasia in Kenya . BMC Health Serv Res 2017 ; 17 : 485 .
Borycki EM , Kushniruk AW , Wagner E , Kletke R . Patient journey mapping: integrating digital technologies into the journey . Knowl Manag E-Learn 2020 ; 12 : 521 – 535 .
Barton E , Freeman T , Baum F , Javanparast S , Lawless A . The feasibility and potential use of case-tracked client journeys in primary healthcare: a pilot study . BMJ Open 2019 ; 9 : e024419 .
Bearnot B , Mitton JA . “You’re always jumping through hoops”: journey mapping the care experiences of individuals with opioid use disorder-associated endocarditis . J Addict Med 2020 ; 14 : 494 – 501 .
Cunnington MS , Plummer CJ , McDiarmid AK , McComb JM . The patient journey from symptom onset to pacemaker implantation . QJM 2008 ; 101 : 955 – 960 .
Geerse C , van Slobbe C , van Triet E , Simonse L . Design of a care pathway for preventive blood pressure monitoring: qualitative study . JMIR Cardio 2019 ; 3 : e13048 .
Laveau F , Hammoudi N , Berthelot E , Belmin J , Assayag P , Cohen A , et al. Patient journey in decompensated heart failure: an analysis in departments of cardiology and geriatrics in the Greater Paris University Hospitals . Arch Cardiovasc Dis 2017 ; 110 : 42 – 50 .
Naheed A , Haldane V , Jafar TH , Chakma N , Legido-Quigley H . Patient pathways and perceptions of treatment, management, and control Bangladesh: a qualitative study . Patient Prefer Adherence 2018 ; 12 : 1437 – 1449 .
Bateman S , Arnold-Chamney M , Jesudason S , Lester R , McDonald S , O’Donnell K , et al. Real ways of working together: co-creating meaningful Aboriginal community consultations to advance kidney care . Aust N Z J Public Health 2022 ; 46 : 614 – 621 .
Greenhalgh T , Hinton L , Finlay T , Macfarlane A , Fahy N , Clyde B , et al. Frameworks for supporting patient and public involvement in research: systematic review and co-design pilot . Health Expect 2019 ; 22 : 785 – 801 .
Wauben LSGL , Guédon ACP , de Korne DF , van den Dobbelsteen JJ . Tracking surgical day care patients using RFID technology . BMJ Innov 2015 ; 1 : 59 – 66 .
Tong A , Sainsbury P , Craig J . Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups . Int J Qual Health Care 2007 ; 19 : 349 – 357 .
von Elm E , Altman DG , Egger M , Pocock SJ , Gøtzsche PC , Vandenbroucke JP , et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies . Lancet 2007 ; 370 (9596): 1453 – 1457 .
Wilson A , Mackean T , Withall L , Willis EM , Pearson O , Hayes C , et al. Protocols for an Aboriginal-led, multi-methods study of the role of Aboriginal and Torres Strait Islander health workers, practitioners and Liaison officers in quality acute health care . J Aust Indigenous HealthInfoNet 2022 ; 3 : 1 – 15 .
Lee B , Lee J , Cho Y , Shin Y , Oh C , Park H , et al. Visualisation of information using patient journey maps for a mobile health application . Appl Sci 2023 ; 13 : 6067 .
Author notes
- cardiovascular system
- health personnel
- health services
- health care systems
- narrative discourse
Email alerts
Related articles in pubmed, citing articles via.
- Recommend to Your Librarian
- Advertising and Corporate Services
- Journals Career Network
Affiliations
- Online ISSN 1873-1953
- Print ISSN 1474-5151
- Copyright © 2024 European Society of Cardiology
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Research article
- Open access
- Published: 15 April 2021
What does the patient have to say? Valuing the patient experience to improve the patient journey
- Raffaella Gualandi ORCID: orcid.org/0000-0001-8602-5249 1 ,
- Cristina Masella 2 ,
- Michela Piredda 3 ,
- Matteo Ercoli 1 &
- Daniela Tartaglini 1
BMC Health Services Research volume 21 , Article number: 347 ( 2021 ) Cite this article
6827 Accesses
19 Citations
2 Altmetric
Metrics details
Patient-reported data—satisfaction, preferences, outcomes and experience—are increasingly studied to provide excellent patient-centred care. In particular, healthcare professionals need to understand whether and how patient experience data can more pertinently inform the design of service delivery from a patient-centred perspective when compared with other indicators. This study aims to explore whether timely patient-reported data could capture relevant issues to improve the hospital patient journey.
Between January and February 2019, a longitudinal survey was conducted in the orthopaedics department of a 250-bed Italian university hospital with patients admitted for surgery; the aim was to analyse the patient journey from the first outpatient visit to discharge. The same patients completed a paper-and-pencil questionnaire, which was created to collect timely preference, experience and main outcomes data, and the hospital patient satisfaction questionnaire. The first was completed at the time of admission to the hospital and at the end of hospitalisation, and the second questionnaire was completed at the end of hospitalisation.
A total of 254 patients completed the three questionnaires. The results show the specific value of patient-reported data. Greater or less negative satisfaction may not reveal pathology-related needs, but patient experience data can detect important areas of improvement along the hospital journey. As clinical conditions and the context of care change rapidly within a single hospital stay for surgery, collecting data at two different moments of the patient journey enables researchers to capture areas of potential improvement in the patient journey that are linked to the context, clinical conditions and emotions experienced by the patient.
By contributing to the literature on how patient-reported data could be collected and used in hospital quality improvement, this study opens the debate about the use of real-time focused data. Further studies should explore how to use patient-reported data effectively (including what the patient reports are working well) and how to improve hospital processes by profiling patients’ needs and defining the appropriate methodologies to capture the experiences of vulnerable patients. These topics may offer new frontiers of research to achieve a patient-centred healthcare system.
Peer Review reports
Patient-reported data (satisfaction, preferences, outcomes and experience) have been increasingly studied with the aim of providing excellent patient-centred care [ 1 , 2 ]. In particular, the collection of patient experience data is emerging as an increasingly key component in assessing the quality of delivered health services [ 3 , 4 ]. Some authors have emphasised that understanding the patient experience represents an opportunity to design healthcare service delivery [ 5 , 6 ]. However, healthcare professionals need to understand whether and how patient experience data can inform the design of service delivery from a patient-centred perspective more pertinently than other indicators [ 7 , 8 , 9 , 10 ].
Studies in the service management literature have shown that it is possible to understand the experience starting from the customer journey. The term ‘customer journey’ refers to ‘the processual and experiential aspects of service processes as seen from the customer viewpoint’ [ 11 ]. Kankainen et al. [ 12 ] describe it as ‘the process of experiencing service through different touchpoints from the customer’s point of view’. Customer experience is shaped before, during and after interactions with the service provider. Moving from services to healthcare, the experience of care is not only a matter of interaction but a multifaceted and complex phenomenon in which the health status, the context of care and presence of different health staff play an important role in achieving clinical outcomes [ 9 , 13 ].
In the hospital context, the requirements of responding rapidly to the acute needs of patients through the integration of multiple actors and services increases this complexity. Timely movement of patients from one service to another is a necessary condition both for managing the volume of patients with different pathologies and for obtaining better clinical outcomes. Consequently, the patient experience of care and service delivery is the result of many successive touchpoints across services to receive care from different units, the totality of which constitutes the patient journey. Because on an individual level any experience is subjective, dynamic and context dependent [ 14 ], patient experience data collected at different points of the journey should make it possible to evaluate if there are discontinuities within the hospital units (e.g., inpatient ward) and between the different units (e.g., between hospital wards and operating rooms) crossed by the patient journey. Inter- and cross-organisational gaps such as obstructed data flow, unavailability of relevant information at points of intervention and a lack of services synchronisation may occur when a complete and consequential view of the whole process is missing. However, few studies have analysed how to improve the patient journey by starting from the patient experience of the service provided [ 15 ]. In particular, most of them focus only on a single step of the hospital journey without identifying which are the meaningful touchpoints for the patient [ 16 , 17 , 18 ]. Indeed, if on the one hand, the patient’s stay is itself composed of multiple steps within the hospital, the hospital journey is part of a larger patient journey, which extends further in time before and after hospitalisation. This is particularly the case for patients who have to undergo surgery, for which clinical examinations are required before admission and a follow-up is scheduled after discharge.
Furthermore, it is not yet clear what the best method is for collecting patient experience data throughout the patient journey [ 19 ]. A recent study analysed the hospital stay experience through the use of unstructured diaries completed in a patient’s own words. However, if, on the one hand, the authors confirm that it is possible to collect valuable data for the improvement of the service directly from the patient, then, on the other hand, the education level, age and clinical conditions could be a limit in understanding the experience of fragile patients [ 20 ].
The goal of the current study is twofold: 1) explore which data collected directly from the patient could be useful in improving the patient journey and 2) to analyse whether gathering timely patient experience data at different points of the patient journey within the hospital can capture areas for improvement in the patient journey.
Design and setting
A longitudinal survey was conducted in the orthopaedics department of a 250-bed Italian university hospital between January and February 2019. The unit of analysis was the journey of the orthopaedic patient from the first outpatient visit to hospital discharge. Accordingly, all patients who underwent major or minor orthopaedic surgery during the time period were considered for inclusion. The type of surgery and stage of the patient journey formed the analysis groups. The study was part of a larger hospital project to redesign the orthopaedic patient journey for hip or knee replacement surgery, here starting with the patient experience [ 19 , 21 ]. In particular, the data collected by the hospital management to assess the quality of the service and that are presented in this work were integrated with interviews and the shadowing of patients, whose results are reported in other papers. The entire project received ethical approval from the organisation’s Ethics Committee (Protocol n.: 25/16 OSS ComEt CBM).
The orthopaedics unit has 34 beds for ordinary hospitalisation or day surgery and is divided into two multispecialty wards: one for ordinary admissions and one mainly for day surgery recovery. Some of the healthcare staff working within the various services are specialised, and a large part is composed of staff in training (residents and degree course students of medicine, nursing and physiotherapy). A centralised team that includes administrative staff and bed manager nurses handles the admissions calls and reception procedures.
Reference terminology
To conduct the present research, the authors employed the following terms with corresponding meanings:
Patient-reported data: views and opinions of patients on the care and on the service they have experienced.
Patient satisfaction: ‘the extent to which the patient’s expectations were fulfilled’ [ 22 ].
Patient experience: ‘the sum of all interactions, shaped by an organisation’s culture, that influences patient perceptions, across the continuum of care’ [ 23 ].
Patient preference: ‘statements made by the patients regarding the relative desirability of a range of health experiences, treatment options and health states’ [ 24 ].
Patient outcomes: ‘any report of the status of a patient’s health condition that comes directly from the patient, without interpretation of the patient’s response by a clinician or anyone else’ [ 25 ].
Instruments
The current study was carried out with two different paper-and-pencil questionnaires delivered to the same patients at two different stages of the hospital patient journey. The first questionnaire was developed on purpose by the authors and completed by the patients at the time of admission to the hospital and at the end of hospitalisation. An English language version of the questionnaire is available as a supplementary file to this paper (see Additional file 1 ). The second questionnaire was the patient satisfaction questionnaire adopted by the hospital and completed by the patients at the end of hospitalisation. In this way, patient-reported outcomes (PRO), patient-reported experience (PRE), patient-reported satisfaction (PRS) and patient-reported preferences (PRP) were collected and analysed.
Figure 1 summarises the points of the patient journey where the data were collected and the focus of each questionnaire.
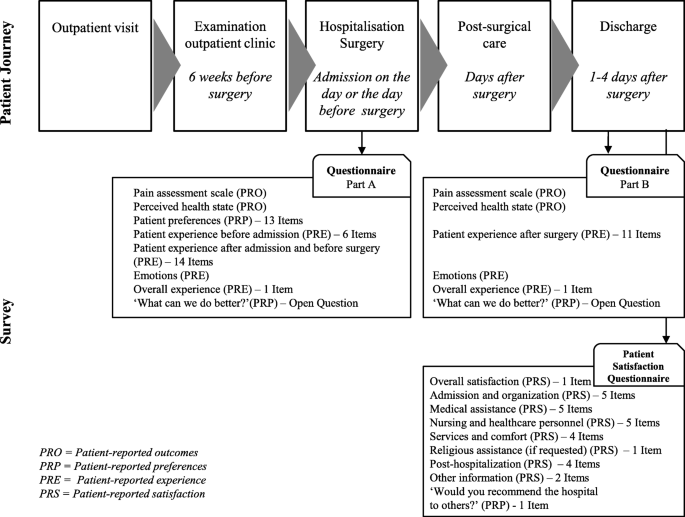
Patient journey and data collection
Consistent with the need to capture patient-reported data during a relatively rapid surgical pathway, the researchers chose to develop a questionnaire focused on the key themes that emerged from the results of the qualitative study previously conducted [ 19 ]. The questionnaire was developed by the first three authors to capture data on the following patient journey touchpoints: preadmission, admission to hospital, preparation for surgery, the postsurgery period and discharge. The purposes were the following: to create a questionnaire that is easy to read and fill in by the patient and to be administered at two key moments of the journey (at the time of admission before surgery and at discharge); to make the data more easily comparable between the different types of patient-reported data; to minimise the risk of patients not completing the questionnaire because of the high number of questions [ 26 ]; and to avoid less data being recorded in the case of elderly or low-educated patients [ 20 ].
The questionnaire items were identified to cover all the service quality dimensions indicated by Dagger [ 27 ] and Gustavsson [ 28 ]: interpersonal quality, technical quality, environmental quality, administrative quality, family quality and involvement quality. In addition, the international literature was consulted by the first and the second authors to develop a set of items evaluating the patient perspective on the level of importance of the different issues related to the hospital journey.
After a discussion between the authors, the questionnaire resulted in 37 closed items and one open question to be administered when the patient entered the hospital ward (Part A) and 15 closed items and one open question when the patient was discharged (Part B). The answers to the closed questions were possible within a 5- or 10-point Likert scale (depending on the items), on outcomes, preferences, experience and satisfaction.
Part A, which was administered upon arrival in the patient ward, included the following sections:
Pain assessment scale (0 = absent; 10 = the strongest pain) and perceived health state (0 = not satisfied at all; 5 = very satisfied);
Patient preferences: evaluation of the self-perceived impact of the different issues related to the hospital journey on the patient’s life (e.g., instructions on how to get to the hospital or in case of waiting; not feeling pain; trusting professionals, etc.) – 13 items (0 = not at all important; 5 = very important);
Positive or negative emotions experienced at the moment of completing the questionnaire by choosing the main ones from the Plutchik’s wheel: serenity, trust, anticipation, apprehension, fear and anger.
A final open question: ‘What can we do better?’
Part B, administered upon discharge from the hospital ward, included the following sections:
The analysis of the internal consistency of the questionnaire through an analysis of the closed-ended items showed a high level of reliability (Cronbach’s alpha: patient perspective and preference 13 items > 0.7; patient experience before surgery 20 items > 0.8; patient experience after surgery 11 items > 0.8).
The patient satisfaction questionnaire included demographic data (age, gender, education and region of origin) and assessed patient satisfaction. The 28 items included a first question on overall satisfaction; the items were divided into seven macro-areas: admission and organisation; medical assistance; nursing and other healthcare personnel; services and comfort; religious assistance (if requested); posthospitalisation; and other information. A final question was ‘Would you recommend the hospital to others?’ with a 10-point Likert scale (from ‘Absolutely not” to ‘Absolutely yes’).
Data collection
An exploratory sample was used, including all orthopaedic patients admitted for surgery during the study period. The patients were recruited at the time of administrative admission for hospitalisation from among those who could understand and consent, speak Italian fluently and write. The data collected were part of the quality of service survey approved by the hospital management and included in the quality surveys in which the patient agreed to participate by signing the consent form at the time of hospital admission. In addition, a trained research assistant asked them for oral consent to participate by explaining the study’s purpose, discussing how participation was voluntary and about the anonymity of data collection.
The fourth author delivered the paper-and-pencil questionnaire to the patient to be filled out on the spot upon arrival in the hospital room (10-min duration) and upon discharge (15-min duration, including the patient satisfaction questionnaire). The same author collected the questionnaire after the patient had filled it in, monitored the completeness of the data and reported all the data on an Excel worksheet for subsequent analysis.
Data analysis
A score was created for each quantitative item of the questionnaire by coding the item response from ‘1’ if the experience was considered completely negative to ‘5’ if it was considered completely positive. A higher score indicates a positive experience and satisfaction with the hospital patient journey. Quantitative data were analysed with descriptive statistics, including the mean and standard deviation and by analysis of a significant difference between the following a priori established groups: type of surgery (major surgery or minor surgery) and time of the patient journey (at the entrance to the hospital and at discharge). Statistical analyses were performed using SPSS 21.0 (IBM Corp., Armonk, NY, USA). Qualitative data were analysed by the first author by reporting and classifying patient responses to the open question ‘What can we do better?’ Specifically, the content of the responses was classified according to the service quality dimensions of Dagger [ 27 ] and Gustavsson [ 28 ].
Sample characteristics
A total of 255 patients were included in the study; of them, only one patient refused to participate because of the limited time available to prepare for surgery upon entering the hospital. Table 1 shows the main characteristics of the participants. The participants had a mean age of 62 years (SD: 14; range: 18–96), and 80% were over the age of 50. The sample was equally distributed between men and women. The most frequent major surgical operations were knee replacement (53% of major surgery) and hip replacement (29%). The most frequent minor surgical procedures were knee arthroscopy (39% of minor surgery) and shoulder arthroscopy (36%). Of the patients admitted for major surgery, 49% had been admitted to the same hospital in the past, while 70% of the patients who had to undergo minor surgery were being admitted to the hospital for the first time.
The evaluation of the patient preferences on the different issues related to the hospital journey that were collected at the beginning of hospitalisation show that the five aspects considered most important for a good hospital journey experience are as follows: ‘Receive the best treatment for the related health conditions’ (Mean: 4.8, SD: 0.4); ‘Have clear instructions on how to prepare for surgery (therapy, fasting, surgery aids)’ (Mean: 4.8, SD: 0.4); ‘Have clear instructions on how to check in at the hospital’ (Mean: 4.7, SD: 0.5); ‘Have clear indications on the treatment pathway I will also have to take’ (Mean: 4.7, SD: 0.5); and ‘Receive explanations from staff in case of waiting’ (Mean: 4.7, SD: 0.5). The least important aspects among those listed are as follows: ‘Have explanations and understand everything that happens to me’ (Mean: 4.0, SD: 0.7); ‘Be involved in all decisions concerning my care’ (Mean: 3.9, SD: 0.8); ‘Feel comfortable in the environments where I have to be’ (Mean: 3.9, SD: 0.9); ‘Wait as little time as possible for a visit or for assistance’ (Mean: 3.9, SD: 0.9); and ‘Have a room where I am not disturbed and with hotel services (TV, landline, etc.)’ (Mean: 3.8, SD: 0.9). When asked if other aspects were important, one participant added ‘Empathic relationship with all the staff’, while another added ‘Admission in a clean facility like this’. No significant differences were found between the major and minor surgery patients.
Evaluating the patient journey at two different points
All patients completed the quantitative items of the experience questionnaire, which was administered on arrival and on discharge, and the satisfaction questionnaire, which was administered on discharge. On admission, 58% of patients answered the open question ‘What can we do better?’ and 68% answered the same question administered on discharge.
Table 2 reports the answers to the overall questions on patient-reported data, referring to the two moments in which the patients were interviewed.
PRO changed between the time of entry and time of discharge, with a different trend between major and minor surgery patients. Upon arrival at the hospital, orthopaedic patients who needed major surgery reported significant pain, here rated on a scale of 0 (absent) to 10 (the strongest pain); this decreased after surgery (Mean: 5.5, SD: 2.7 vs. Mean: 3.8, SD: 2.6). Pain remained constant and not particularly high in minor surgery patients (Mean: 2.8, SD: 2.4 vs. Mean: 2.6, SD: 2.7). The self-reported state of health assessed on a scale of values between 1 (not at all satisfied) to 5 (very satisfied) showed a more evident improvement in patients with major surgery between the time of arrival in the hospital and time of discharge (Mean: 3.7, SD: 0.8 vs., Mean: 4.0, SD: 0.6). Minor surgery patients reported a generally higher level of health than major surgery patients (Mean: 4.0 SD: 0.7 vs. Mean: 4.3, SD: 0.6). In these items, the age group does not seem to be significant.
Regarding the closed-answer items on the overall patient experience, an average of high scores, with a slight difference between the time of entry into the ward and time of discharge, was reported. On discharge, the hospital experience was rated with lower average scores than patient satisfaction. The patient satisfaction relating to hospitalisation showed significant high scores: on a score from 1 to 5, 97% of patients rated 4 (22.8%) or 5 (74.4%). Additionally, 95% of patients would recommend the hospital to other patients.
Table 3 reports how patients’ emotional status changed along the hospital journey. Trust and apprehension were the prevailing emotions at the time of arriving in the ward (respectively 37.8 and 20.5% of patients). Apprehension decreased noticeably among patients after surgery (6.3%), and serenity increased (from 21.7% before surgery to 46.1% at the time of discharge). The change is more evident in major surgery patients: 32.7% of them experienced apprehension or fear before surgery, decreasing to 13.1% at the time of discharge, with an increase in patient serenity from 5.8 to 14.8%.
Detecting areas of improvement by following the patient journey
When analysing the specific items in relation to the time of the journey, the data on experience and satisfaction showed differing information around some key topics. Table 4 shows the experience and satisfaction items that are the most related to the patient’s journey.
At the time of discharge, the patient satisfaction items reported high scores for the quality and cleanliness of the environment (Mean: 4.8, SD: 0.4). However, upon entering the ward, the patients rated the comfort of the room with one of the lowest experience scores (Mean: 4.3, SD: 1.0). The answers to the open questions show the reason for this: the patients wished to have a TV inside the wards and to have larger wards to move more easily with the orthopaedic aids they had to manage (wheelchair, crutches, etc.). One patient suggested the following solution: ‘Small hospital room for physiotherapy: creation of a dedicated space’ (Code: ORTO 63).
In the ‘Satisfaction’ items, patients recognised a high level of professionalism and competence in the healthcare staff (Mean: 4.8, SD: 0.6). However, in the ‘Experience’ questionnaire, the items concerning information received before surgery showed some of the lowest scores. The score on the information received to organise the hospitalisation and prepare for surgery was rated at 4.5 (SD: 0.8). Understandable explanations given before surgery by the doctor of everything the patient needed to know about surgery, length of stay and the postsurgery period was rated 4.3 (SD: 0.9). The same result was recorded for understandable explanations given by the anaesthesiologist on everything the patient needed to know about surgery and pain treatment. The answers to open questions showed that 29 patients would have liked more information concerning the different aspects of hospitalisation, including the necessary aids for surgery and postsurgery path. Two patients emphasised the need for more communication with family members when the patient was in the operating theatre. One patient expressed how this issue can always be improved: ‘In my opinion, improve the information given to patients on the path they have to take inside the hospital. I have been hospitalised five times and I always see an improvement, thanks for everything’ (Code: DS36).
The patient satisfaction questionnaire reported a high score on the availability of doctors and nursing and care staff (Mean: 4.7, SD: 0.7). For the experience items, the patients rated these aspects at 4.4 and 4.6, respectively, at the time of entering the ward. The average score decreased to 4.3 and 4.5, respectively, regarding the postsurgery stay. More specific data emerged from the open questions. The patients reported the need for more of a presence of and contact with doctors (38 quotes) and nurses (21 quotes), and this need was reported in particular regarding the postsurgery stay: ‘More time spent by staff in the postoperative period’ (Code: ORTO2). Twenty-one patients reported a lack of interaction with healthcare staff as a staff shortage problem: ‘Nurses are very professional and well trained, but there should be more of them’ (Code: DS37); ‘too few nurses during the shift to answer the call bells quickly’ (Code: ORTO151). Other patients added that the presence of so many students decreased their confidence in being properly cared for. For example, one patient said, ‘Stay longer with the patient without rushing, too many students unable to solve certain problems and too few nurses and doctors’ (Code: ORTO 116).
The question ‘Were you involved in decisions about your care?’ obtained the lowest score. Specifically, the average rating was 4.0 upon arrival in the ward and increased to 4.3 upon discharge. However, only one participant suggested greater patient involvement.
The satisfaction score on waiting times and admissions procedures was among the lowest (Mean: 4.5, SD: 0.8). The reasons for these scores were expanded by the answers to the open questions captured immediately after entering the ward: 53 patients reported that the waiting times between arrival at the hospital, admission procedures and room assignment were too long. One patient pointed out that hospital discharges and new entries needed to be better coordinated; another suggested that the patient should not come too early in the morning if admission was scheduled during the day; some patients asked for a reduction in the time between entering the hospital and actually entering the operating theatre.
Some hidden but not openly stated needs for adaptation by the patient to hospital rules are evident in this quote: ‘I found everything well, no complaints, I understood that having a relative’s personal assistance is impossible but I would have liked it’ (Code: ORTO26). In the presurgery period, the patients reported the desire for family members to be nearby when they wanted (Mean: 4.4, SD: 0.9). The score increased in the postoperative period (Mean: 4.7, SD: 0.6), and only nine patients stated they wanted more time with their families, with more flexible visiting hours and with their presence before surgery.
Although unsolicited, feedback on what works, in addition to what needs to be improved, was given. For example, one patient reported, ‘I did not expect to find such a comfortable environment with such professionalism from all the staff. Nothing is perfect, therefore everything is perfectible, but here, in this hospital, we are at a good point’ (Code: ORTO16). Another said, ‘Nothing to improve, on the contrary I would like to point out the particular care, attention and professionalism of the student F.A.’ (Code: ORTO33).
Table 5 reports the improvements suggested by the patients collected at the two different points of their journey.
Numerous studies have explored how different types of data collected directly from patients can improve the quality of care, while few studies have analysed whether the data reported by patients on a cross-hospital process can be useful to improve the process itself [ 29 , 30 ]. The current study was designed to explore whether patient-reported data, specifically experience data, can identify areas of improvement within the hospital and between the different units crossed by the patient journey.
By timely and simultaneously gathering preferences, satisfaction, outcomes and experience data, it is possible to have a complete picture of the hospital patient journey. In particular, the satisfaction and preference data measure the levels of importance given to different aspects by the patient— what is important for the patient experience—and outcomes data show the patient’s circumstances and present conditions— why it is important for the patient. Satisfaction data may not reveal pathology-related needs, while patient experience data can detect important areas of improvement along the hospital journey. In the current study, for instance, the score of preference for room comfort was one of the lowest items (Mean: 3.8). However, by answering to the open question on what can be improved, when the patient entered the room, he judged it not very comfortable (Mean: 4.3) because of the lack of space for movement with orthopaedic aids. The satisfaction item cannot capture this information (average score of 4.8 on the quality and cleanliness of the environments).
These same results also show how at the beginning of the journey, patients might consider an issue as not critical, but while living the hospital experience, it becomes important. As another example, although on admission, patients declared that waiting as little time as possible for a visit or for assistance was one of the least important aspects (Mean: 3.9), the satisfaction score on waiting times and admissions procedures was among the lowest (Mean: 4.5). Timely experience data show how as soon as the patient enters the room, he or she clearly remembers having waited too long from the moment of admission and suggests a better organisation of the hospitalisation.
Numerous factors can influence the patient experience. In the presurgery stage, trust and apprehension are the prevailing emotions (37.8 and 20.5% of patients, respectively), and the patient seems to lack knowledge of what to do. The experience data show that the scores related to information received to organise the hospitalisation and prepare for surgery and explanations given before surgery are very low. Improving information concerning the different aspects of hospitalisation, including the necessary aids for surgery and the postsurgery path, emerged as a fundamental need.
Even if related to a very specific case, the results of the current study show that patients do not have the technical competence to predict their needs before and after surgery; thus, nursing competence is needed to effectively anticipate patient needs and attend to the organisation of patient journeys to improve experiences of care. These data support the claim of a recent NHS report in which nurses are shown to play an essential role in the way in which data are collected, interpreted and used to improve care [ 10 ].
Because clinical conditions and the context of care change rapidly within a single hospital stay for surgery, capturing data at key moments in the journey, rather than at the end, can better represent the patient’s experience [ 31 ]. In particular, analysing the answers to the open question ‘What can we do better?’ allows for understanding what happened to the patient that may have influenced his or her experience (e.g., apprehension and pain before surgery, pathology and age-related needs, fast-track recovery, waiting without entertainment, etc.). Moreover, one patient may reveal the important needs made impossible by circumstances (e.g., need of having a family member being close to the patient before surgery made impossible by hospital organisation). For example, when redesigning fast-track recovery from major orthopaedic surgery, significant touchpoints for the patient should be treated with respect to his or her need for interaction with professionals, his or her emotional state and social conditions and by considering the changing circumstances he or she will face along the journey [ 19 , 32 , 33 ]. In particular, the emotional state should be better explored to understand how this variable affects patient experience along the journey and to improve ways of interacting with the patient: by giving more information, by offering support or simply by accompanying him or her in critical moments of the presurgery period.
In the present study, to encourage patient participation, the authors decided to ask a few questions at two critical moments of the journey: at the arrival before surgery and at discharge. Moreover, despite the older population involved, the simplicity of the questionnaire, which even used emoticons, made it possible to capture the experience of those patients who were able to read and write. In this way, a high rate of responses was achieved. Nevertheless, further studies should investigate how to collect real-time feedback from those who are unable to describe their own experience [ 34 ]. Moreover, because data were collected in paper format, the process of returning data to the management team and front-line professionals to stimulate quality improvement slowed down because of the necessary data analysis times. The challenges in handling real-time big data collection and storage in health information systems will bring new advancements in the continuous improvement process by immediately returning the patient-reported data at all organisational levels. These data should help redesign hospital care processes at the top and middle management levels in an integrated and patient-centred way. At the front-line level, healthcare professionals can immediately make corrections with micro-interventions, fixing the way of giving attention to the patient by focusing on his or her experiences.
In present study, patient-reported data on satisfaction and experience were significantly positive in almost all the items investigated, with an average score between 4 and 5 on a scale of 1 to 5. This result is in line with the literature showing that little variation occurs in the answers to questions about the quality of care with high patient satisfaction scores [ 35 , 36 ]. Further studies should investigate if the asymmetrical relationship between the health care professional and patient [ 37 ], the vulnerable situation of a patient [ 34 ] and the primary need to solve a clinical problem and fear of surgery that are deemed more important than anything else could result in high and undistributed response rates.
When asking the patient ‘What can we do better?’ the question assumes that the patient only identifies what does not work. However, patients are also able to report what worked well. Managers and health care teams should study which factors, from the patient’s point of view, determine a good experience and must be supported. Further studies should analyse whether positive patient-reported data may explain what factors produce a good patient journey experience and how they may reinforce the quality improvement solutions adopted and, hence, influence health professionals’ behaviour [ 38 ].
The results of the current study emphasise that personalised medicine should no longer only refer to the targeted therapy. This requires management teams to be able to customise the patient journey and identify different patient profiles, which should not be reduced to the clinical pathway.
The limitations of the current study are manifold; in large part, they are connected to the nature of the original project, which aimed to produce local actionable improvements in the setting. First, the results cannot be generalised: the study was conducted in a single hospital and only on how the orthopaedic surgical path; this influences the significance and transferability of the results. However, the study aimed to provide useful insights to hospital management to promote a review of the processes in a real patient-centred way. In particular, the results offer a stimulus for the debate on the use of patient experience data for the design of service delivery. Second, the orthopaedic surgical path is very different, for example, from the oncological one. Specifically, the orthopaedic surgical journey is generally shorter, has a beginning and an end and does not extend over time with a worsening of the initial clinical conditions. This aspect could influence the results and methodology should be tested on different clinical pathways, in particular by considering chronic pathologies. Finally, the authors preferred to use a questionnaire with relatively few questions instead of using the validated ones already present in the literature. The choice was made to favour real-time data collection and the patient’s response rate to the questions. These objectives have been achieved, and future studies will have to validate the single items for patients with different pathologies. However, by considering the very different and complex contexts in which each hospital operates, the literature will increasingly have to consider single longitudinal studies by starting from the analysis of the patient journey that takes place in each hospital.
Several issues would benefit from further exploration, including the impact of the patient-healthcare staff relationship in the hospital journey experience; the opportunity of bringing patients’ and professionals’ experiences together for joint knowledge of improvement solutions; and the study of new methodology to capture the real-time experiences of vulnerable patients.
Providing customers with quality experiences is a key competitive advantage in a range of service sectors, including the healthcare service. Measuring patient experiences is a practice increasingly used, and researchers and managers are seeking to understand how to use these measures to improve service delivery [ 39 , 40 , 41 ].
The current study provides insights for healthcare practitioners caring for patients in hospitals and those responsible for planning and designing the hospital patient journey. By contributing to the literature on how patient-reported data could be collected and used in hospital quality improvement, it also opens the debate about the use of real-time focused data when capturing experiences from vulnerable patients. Furthermore, the present study asks for a more positive perspective on patients’ data that can be used not only to detect what does not work, but also what is working well.
In different clinical settings, further studies should explore how to effectively use patient-reported data to improve hospital processes, profile patients’ needs and identify appropriate methodologies to capture the experiences of vulnerable patients. These topics may offer new frontiers of research to achieve a patient-centred healthcare system.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
Patient-reported outcomes
Patient-reported experience
Patient-reported satisfaction
Patient-reported preferences
Number count
Standard deviation
National Health Service (UK)
Murante AM, Seghieri C, Brown A, Nuti S. How do hospitalization experience and institutional characteristics influence inpatient satisfaction? A multilevel approach. Int J Health Plann Mgmt. 2014;29(3):e247–60. https://doi.org/10.1002/hpm.2201 .
Article Google Scholar
Klose K, Kreimeier S, Tangermann U, Aumann I, Damm K, RHO Group. Patient- and person-reports on healthcare: preferences, outcomes, experiences, and satisfaction - an essay. Heal Econ Rev. 2016;6(1):18. https://doi.org/10.1186/s13561-016-0094-6 .
Article CAS Google Scholar
Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3(1):e001570. https://doi.org/10.1136/bmjopen-2012-001570 .
Article PubMed PubMed Central Google Scholar
Nuti S, De Rosis S, Bonciani M, Murante AM. Rethinking Healthcare Performance Evaluation Systems towards the People-Centredness Approach: Their Pathways, their Experience, their Evaluation. Healthc Pap. 2017;17(2):56–64. doi: https://doi.org/10.12927/hcpap.2017.25408 . Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. 2013. https://www.gov.uk/government/publications/report-of-the-mid-staffordshire-nhs-foundation-trust-public-inquiry . Accessed 15 Jan 2020.
Francis R. Report of the mid Staffordshire NHS Foundation trust public inquiry. 2013. https://www.gov.uk/government/publications/report-of-the-mid-staffordshire-nhs-foundation-trust-public-inquiry . Accessed 15 Jan 2020.
Baig A, Dua A, Riefberg, V. How US state governments can improve customer service. 2014. McKinsey & Company. https://www.mckinsey.com/industries/public-sector/our-insights/how-us-state-governments-can-improve-customer-service . Accessed 15 Jan 2020.
Asprey A, Campbell JL, Newbould J, Cohn S, Carter M, Davey A, et al. Challenges to the credibility of patient feedback in primary healthcare settings: a qualitative study. Br J Gen Pract. 2013;63(608):e200–8. https://doi.org/10.3399/bjgp13X664252 .
Boiko O, Campbell JL, Elmore N, Davey AF, Roland M, Burt J. The role of patient experience surveys in quality assurance and improvement: a focus group study in English general practice. Health Expect. 2015;18(6):1982–94. https://doi.org/10.1111/hex.12298 .
Article PubMed Google Scholar
Ponsignon F, Smart A, Philps L. A customer journey perspective on service delivery system design: insights from healthcare. IJQRM. 35(3). https://doi.org/10.1108/IJQRM-03-2018-0073 .
Donetto S, Desai A, Zoccatelli G, Robert G, Allen D, Brearley S, et al. Organisational strategies and practices to improve care using patient experience data in acute NHS hospital trusts: an ethnographic study. Health Serv Deliv Res. 2019;7(34):112. https://doi.org/10.3310/hsdr07340 .
Følstad A, Kvale K. Customer journeys: a systematic literature review. JSTP. 2018;28(2):196–227. https://doi.org/10.1108/JSTP-11-2014-0261 .
Kankainen A, Vaajakallio K, Kantola V, Mattelmäki T. Storytelling group – a co-design method for service design. BIT. 2012;31(3):221–30. https://doi.org/10.1080/0144929X.2011.563794 .
Tax SS, McCutcheon D, Wilkinson IF. The service delivery network (SDN): a customer-centric perspective of the customer journey. J Serv Res. 2013;16(4):454–70. https://doi.org/10.1177/1094670513481108 .
Law EL-C, Roto V, Hassenzahal M, POS VA, Kort J. Understanding, scoping and defining user experience: a survey approach. Proceedings from the CHI conference. CHI; User experience April 7th 2009. Boston; 2009.
Gualandi R, Masella C, Tartaglini D. Improving hospital patient flow: a systematic review. BPMJ. 2019. https://doi.org/10.1108/BPMJ-10-2017-0265 .
Richardson S, Casey M, Hider P. Following the patient journey: older persons' experiences of emergency departments and discharge. Accid Emerg Nurs. 2007;15(3):134–40. https://doi.org/10.1016/j.aaen.2007.05.004 .
Kydd A. The patient experience of being a delayed discharge. J Nurs Manag. 2008;16(2):121–6. https://doi.org/10.1111/j.1365-2834.2008.00848.x .
Browall M, Koinberg I, Falk H, Wijk H. Patients' experience of important factors in the healthcare environment in oncology care. Int J Qual Stud Health Well-Being. 2013;6(8):20870. https://doi.org/10.3402/qhw.v8i0.20870 .
Gualandi R, Masella C, Viglione D, Tartaglini D. Exploring the hospital patient journey: what does the patient experience? PLoS One. 2019;14(12):e0224899. https://doi.org/10.1371/journal.pone.0224899 .
Article CAS PubMed PubMed Central Google Scholar
Webster CS, Jowsey T, Lu LM, Henning MA, Verstappen A, Wearn A, et al. Capturing the experience of the hospital-stay journey from admission to discharge using diaries completed by patients in their own words: a qualitative study. BMJ Open. 2019;9(3):e027258. https://doi.org/10.1136/bmjopen-2018-027258 PMID: 30862638; PMCID: PMC6429883.
Gualandi R, Masella C, Viglione D, Tartaglini D. Challenges and potential improvements in hospital patient flow: the contribution of frontline, top and middle management professionals. JHOM. 2020;34(8):829–48. https://doi.org/10.1108/JHOM-11-2019-0316 .
Crow R, Gage H, Hampson S, Hart J, Kimber A, Storey L, et al. The measurement of satisfaction with healthcare: implications for practice from a systematic review of the literature. Health Technol Assess. 2002;6(32):1–2.
The Beryl Institute, 2018, Available at: https://www.theberylinstitute.org/page/DefiningPatientExp . Accesed November 27, 2018.
Brennan PF, Strombom I. Improving health care by understanding patient preferences: the role of computer technology. J Am Med Inform Assoc. 1998;5(3):257–62. https://doi.org/10.1136/jamia.1998.0050257 .
Guidance for Industry: patient-reported outcome measures: use in medical product development to support labelling claims. Food and Drug Administration; 2009, p. 6; Accessed 10 Jan 2015; Available from: https://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM193282.pdf .
Kost RG, de Rosa JC. Impact of survey length and compensation on validity, reliability, and sample characteristics for Ultrashort-, short-, and long-research participant perception surveys. J Clin Transl Sci. 2018;2(1):31–7. https://doi.org/10.1017/cts.2018.18 .
Dagger TS, Sweeney JC, Johnson LW. A Hierarchical Model of Health Service Quality: Scale Development and Investigation of an Integrated Model. J Serv Res. 2007;10(2):123–42. https://doi.org/10.1177/1094670507309594 .
Gustavsson S, Gremyr I, Kenne SE. Designing quality of care--contributions from parents: Parents' experiences of care processes in paediatric care and their contribution to improvements of the care process in collaboration with healthcare professionals. J Clin Nurs. 2016;25(5–6):742–51. https://doi.org/10.1111/jocn.13050 .
Garratt AM, Solheim E, Danielsen K. National and cross-national surveys of patient experiences: a structured review. Report from Kunnskapssenteret (Norwegian knowledge Centre for the Health Services) no 7–2008. Oslo: Norwegian Knowledge Centre for the Health Services.
Beattie M, Murphy DJ, Atherton I, Lauder W. Instruments to measure patient experience of healthcare quality in hospitals: a systematic review. Syst Rev. 2015;23(4):97. https://doi.org/10.1186/s13643-015-0089-0 .
Kjellsson G, Clarke P, Gerdtham UG. Forgetting to remember or remembering to forget: a study of the recall period length in health care survey questions. J Health Econ. 2014;35:34–46. https://doi.org/10.1016/j.jhealeco.2014.01.007 .
Altringer B. The emotional experience of patient care: a case for innovation in health care design. J Health Serv Res Policy. 2010;15(3):174–7. https://doi.org/10.1258/jhsrp.2009.009064 .
McColl-Kennedy JR, Danaher TS, Gallan AS, Orsingher C, Lervik-Olsen L, Verma R. How do you feel today? Managing patient emotions during health care experiences to enhance well-being. J Bus Res. 2017;79:247–59. https://doi.org/10.1016/j.jbusres.2017.03.022 .
Goldberg SE, Harwood RH. Experience of general hospital care in older patients with cognitive impairment: are we measuring the most vulnerable patients' experience? BMJ Qual Saf. 2013;22(12):977–80. https://doi.org/10.1136/bmjqs-2013-001961 Epub 2013 Jul 18. PMID: 23868868; PMCID: PMC3888593.
Schoenfelder T, Klewer J, Kugler J. Determinants of patient satisfaction: a study among 39 hospitals in an in-patient setting in Germany. Int J Qual Health Care. 2011;23(5):503–9. https://doi.org/10.1093/intqhc/mzr038 .
Harrison R, Walton M, Kelly P, Manias E, Jorm C, Smith-Merry J, et al. Hospitalization from the patient perspective: a data linkage study of adults in Australia. Int J Qual Health Care. 2018;30(5):358–65. https://doi.org/10.1093/intqhc/mzy024 .
Pilnick A, Dingwall R. On the remarkable persistence of asymmetry in doctor/patient interaction: a critical review. Soc Sci Med. 2011;72(8):1374–82. https://doi.org/10.1016/j.socscimed.2011.02.033 Epub 2011 Mar 29. PMID: 21454003 .
Murante AM, Vainieri M, Rojas D, Nuti S. Health policy. Does feedback influence patient - professional communication? Empirical evidence from Italy. 2014;116(2–3):273–80. https://doi.org/10.1016/j.healthpol.2014.02.001 .
Manary MP, Boulding W, Staelin R, Glickman SW. The patient experience and health outcomes. N Engl J Med. 2013;368(3):201–3. https://doi.org/10.1056/NEJMp1211775 .
Article CAS PubMed Google Scholar
Coulter A, Locock L, Ziebland S, Calabrese J. Collecting data on patient experience is not enough: they must be used to improve care. BMJ. 2014;26:348–g2225. https://doi.org/10.1136/bmj.g2225 .
Chambers M, LeMaster J. Collecting and using patient experience data: caution, commitment and consistency are needed. Health Expect. 2019;22(1):1–2. https://doi.org/10.1111/hex.12863 .
Download references
Acknowledgements
Not applicable.
No funding was received for this research.
Author information
Authors and affiliations.
Campus Bio-Medico di Roma University, Rome, Italy
Raffaella Gualandi, Matteo Ercoli & Daniela Tartaglini
Politecnico di Milano, Milan, Italy
Cristina Masella
Research Unit Nursing Science, Campus Bio-Medico di Roma University, Rome, Italy
Michela Piredda
You can also search for this author in PubMed Google Scholar
Contributions
RG, CM and DT contributed to the study’s conception and design. Material preparation was performed by RG. Data collection was performed by ME. Data analysis was performed by RG and MP. The first draft of the manuscript was written by RG and CM contributed to the analysis and drafting of the article. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Raffaella Gualandi .
Ethics declarations
Ethics approval and consent to participate.
The study is part of a large project approved by the organisation’s Ethics Committee of University Campus Bio-Medico of Rome (Protocol n.: 25/16 OSS ComEt CBM), which included acquiring written consent for patient interviews and shadowing. The data reported in the current study and included in the project were part of a hospital assessment of patient satisfaction. The study was approved by the Management Team of the hospital.
Consent for publication
Competing interests.
The authors declare that they have no conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Questionnaire. Questionnaire used for the study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Gualandi, R., Masella, C., Piredda, M. et al. What does the patient have to say? Valuing the patient experience to improve the patient journey. BMC Health Serv Res 21 , 347 (2021). https://doi.org/10.1186/s12913-021-06341-3
Download citation
Received : 13 April 2020
Accepted : 03 April 2021
Published : 15 April 2021
DOI : https://doi.org/10.1186/s12913-021-06341-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Patient-reported data
- Patient experience
- Patient journey
- Process improvement
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Process mapping the...
Process mapping the patient journey: an introduction
- Related content
- Peer review
- Timothy M Trebble , consultant gastroenterologist 1 ,
- Navjyot Hansi , CMT 2 1 ,
- Theresa Hydes , CMT 1 1 ,
- Melissa A Smith , specialist registrar 2 ,
- Marc Baker , senior faculty member 3
- 1 Department of Gastroenterology, Portsmouth Hospitals Trust, Portsmouth PO6 3LY
- 2 Department of Gastroenterology, Guy’s and St Thomas’ NHS Foundation Trust, London
- 3 Lean Enterprise Academy, Ross-on-Wye, Hertfordshire
- Correspondence to: T M Trebble tim.trebble{at}porthosp.nhs.uk
- Accepted 15 July 2010
Process mapping enables the reconfiguring of the patient journey from the patient’s perspective in order to improve quality of care and release resources. This paper provides a practical framework for using this versatile and simple technique in hospital.
Healthcare process mapping is a new and important form of clinical audit that examines how we manage the patient journey, using the patient’s perspective to identify problems and suggest improvements. 1 2 We outline the steps involved in mapping the patient’s journey, as we believe that a basic understanding of this versatile and simple technique, and when and how to use it, is valuable to clinicians who are developing clinical services.
What information does process mapping provide and what is it used for?
Process mapping allows us to “see” and understand the patient’s experience 3 by separating the management of a specific condition or treatment into a series of consecutive events or steps (activities, interventions, or staff interactions, for example). The sequence of these steps between two points (from admission to the accident and emergency department to discharge from the ward) can be viewed as a patient pathway or process of care. 4
Improving the patient pathway involves the coordination of multidisciplinary practice, aiming to maximise clinical efficacy and efficiency by eliminating ineffective and unnecessary care. 5 The data provided by process mapping can be used to redesign the patient pathway 4 6 to improve the quality or efficiency of clinical management and to alter the focus of care towards activities most valued by the patient.
Process mapping has shown clinical benefit across a variety of specialties, multidisciplinary teams, and healthcare systems. 7 8 9 The NHS Institute for Innovation and Improvement proposes a range of practical benefits using this approach (box 1). 6
Box 1 Benefits of process mapping 6
A starting point for an improvement project specific for your own place of work
Creating a culture of ownership, responsibility and accountability for your team
Illustrates a patient pathway or process, understanding it from a patient’s perspective
An aid to plan changes more effectively
Collecting ideas, often from staff who understand the system but who rarely contribute to change
An interactive event that engages staff
An end product (a process map) that is easy to understand and highly visual
Several management systems are available to support process mapping and pathway redesign. 10 11 A common technique, derived originally from the Japanese car maker Toyota, is known as lean thinking transformation. 3 12 This considers each step in a patient pathway in terms of the relative contribution towards the patient’s outcome, taken from the patient’s perspective: it improves the patient’s health, wellbeing, and experience (value adding) or it does not (non-value or “waste”) (box 2). 14 15 16
Box 2 The eight types of waste in health care 13
Defects —Drug prescription errors; incomplete surgical equipment
Overproduction —Inappropriate scheduling
Transportation —Distance between related departments
Waiting —By patients or staff
Inventory —Excess stores, that expire
Motion —Poor ergonomics
Overprocessing —A sledgehammer to crack a nut
Human potential —Not making the most of staff skills
Process mapping can be used to identify and characterise value and non-value steps in the patient pathway (also known as value stream mapping). Using lean thinking transformation to redesign the pathway aims to enhance the contribution of value steps and remove non-value steps. 17 In most processes, non-value steps account for nine times more effort than steps that add value. 18
Reviewing the patient journey is always beneficial, and therefore a process mapping exercise can be undertaken at any time. However, common indications include a need to improve patients’ satisfaction or quality or financial aspects of a particular clinical service.
How to organise a process mapping exercise
Process mapping requires a planned approach, as even apparently straightforward patient journeys can be complex, with many interdependent steps. 4 A process mapping exercise should be an enjoyable and creative experience for staff. In common with other audit techniques, it must avoid being confrontational or judgmental or used to “name, shame, and blame.” 8 19
Preparation and planning
A good first step is to form a team of four or five key staff, ideally including a member with previous experience of lean thinking transformation. The group should decide on a plan for the project and its scope; this can be visualised by using a flow diagram (fig 1 ⇓ ). Producing a rough initial draft of the patient journey can be useful for providing an overview of the exercise.
Fig 1 Steps involved in a process mapping exercise
- Download figure
- Open in new tab
- Download powerpoint
The medical literature or questionnaire studies of patients’ expectations and outcomes should be reviewed to identify value adding steps involved in the management of the clinical condition or intervention from the patient’s perspective. 1 3
Data collection
Data collection should include information on each step under routine clinical circumstances in the usual clinical environment. Information is needed on waiting episodes and bottlenecks (any step within the patient pathway that slows the overall rate of a patient’s progress, normally through reduced capacity or availability 20 ). Using estimates of minimum and maximum time for each step reduces the influence of day to day variations that may skew the data. Limiting the number of steps (to below 60) aids subsequent analysis.
The techniques used for data collection (table 1 ⇓ ) each have advantages and disadvantages; a combination of approaches can be applied, contributing different qualitative or quantitative information. The commonly used technique of walking the patient journey includes interviews with patients and staff and direct observation of the patient journey and clinical environment. It allows the investigator to “see” the patient journey at first hand. Involving junior (or student) doctors or nurses as interviewers may increase the openness of opinions from staff, and time needed for data collection can be reduced by allotting members of the team to investigate different stages in the patient’s journey.
Data collection in process mapping
- View inline
Mapping the information
The process map should comprehensively represent the patient journey. It is common practice to draw the map by hand onto paper (often several metres long), either directly or on repositionable notes (fig 2 ⇓ ).
Fig 2 Section of a current state map of the endoscopy patient journey
Information relating to the steps or representing movement of information (request forms, results, etc) can be added. It is useful to obtain any missing information at this stage, either from staff within the meeting or by revisiting the clinical environment.
Analysing the data and problem solving
The map can be analysed by using a series of simple questions (box 3). The additional information can be added to the process map for visual representation. This can be helped by producing a workflow diagram—a map of the clinical environment, including information on patient, staff, and information movement (fig 3 ⇓ ). 18
Box 3 How to analyse a process map 6
How many steps are involved?
How many staff-staff interactions (handoffs)?
What is the time for each step and between each step?
What is the total time between start and finish (lead time)?
When does a patient join a queue, and is it a regular occurrence?
How many non-value steps are there?
What do patients complain about?
What are the problems for staff?
Fig 3 Workflow diagram of current state endoscopy pathway
Redesigning the patient journey
Lean thinking transformation involves redesigning the patient journey. 21 22 This will eliminate, combine and simplify non-value steps, 23 limit the impact of rate limiting steps (such as bottlenecks), and emphasise the value adding steps, making the process more patient-centred. 6 It is often useful to trial the new pathway and review its effect on patient management and satisfaction before attempting more sustained implementation.
Worked example: How to undertake a process mapping exercise
South Coast NHS Trust, a large district general hospital, plans to improve patient access to local services by offering unsedated endoscopy in two peripheral units. A consultant gastroenterologist has been asked to lead a process mapping exercise of the current patient journey to develop a fast track, high quality patient pathway.
In the absence of local data, he reviews the published literature and identifies key factors to the patient experience that include levels of discomfort during the procedure, time to discuss the findings with the endoscopist, and time spent waiting. 24 25 26 27 He recruits a team: an experienced performance manager, a sister from the endoscopy department, and two junior doctors.
The team drafts a map of the current endoscopy journey, using repositionable notes on the wall. This allows team members to identify the start (admission to the unit) and completion (discharge) points and the locations thought to be involved in the patient journey.
They decide to use a “walk the journey” format, interviewing staff in their clinical environments and allowing direct observation of the patient’s management.
The junior doctors visit the endoscopy unit over two days, building up rapport with the staff to ensure that they feel comfortable with being observed and interviewed (on a semistructured but informal basis). On each day they start at the point of admission at the reception office and follow the patient journey to completion.
They observe the process from staff and patient’s perspectives, sitting in on the booking process and the endoscopy procedure. They identify the sequence of steps and assess each for its duration (minimum and maximum times) and the factors that influence this. For some of the steps, they use a digital watch and notepad to check and record times. They also note staff-patient and staff-staff interactions and their function, and the recording and movement of relevant information.
Details for each step are entered into a simple table (table 2 ⇓ ), with relevant notes and symbols for bottlenecks and patients’ waits.
Patient journey for non-sedated upper gastrointestinal endoscopy
When data collection is complete, the doctor organises a meeting with the team. The individual steps of the patient journey are mapped on a single long section of paper with coloured temporary markers (fig 2 ⇑ ); additional information is added in different colours. A workflow diagram is drawn to show the physical route of the patient journey (fig 3 ⇑ ).
The performance manager calculates that the total patient journey takes a minimum of 50 minutes to a maximum of 345 minutes. This variation mainly reflects waiting times before a number of bottleneck steps.
Only five steps (14 to 17 and 22, table 2 ⇑ ) are considered both to add value and needed on the day of the procedure (providing patient information and consent can be obtained before the patient attends the department). These represent from 13 to 47 minutes. At its least efficient, therefore, only 4% of the patient journey (13 of 345 minutes) is spent in activities that contribute directly towards the patient’s outcome.
The team redesigns the patient journey (fig 4 ⇓ ) to increase time spent on value adding aspects but reduce waiting times, bottlenecks, and travelling distances. For example, time for discussing the results of the procedure is increased but the location is moved from the end of the journey (a bottleneck) to shortly after the procedure in the anteroom, reducing the patient’s waiting time and staff’s travelling distances.
Fig 4 Workflow diagram of future state endoscopy pathway
Implementing changes and sustaining improvements
The endoscopy staff are consulted on the new patient pathway, which is then piloted. After successful review two months later, including a patient satisfaction questionnaire, the new patient pathway is formally adopted in the peripheral units.
Further reading
Practical applications.
NHS Institute for Innovation and Improvement ( https://www.institute.nhs.uk )—comprehensive online resource providing practical guidance on process mapping and service improvement
Lean Enterprise Academy ( http://www.leanuk.org )—independent body dedicated to lean thinking in industry and healthcare, through training and academic discussion; its publication, Making Hospitals Work 23 is a practical guide to lean transformation in the hospital environment
Manufacturing Institute ( http://www.manufacturinginstitute.co.uk )—undertakes courses on process mapping and lean thinking transformation within health care and industrial practice
Theoretical basis
Bircheno J. The new lean toolbox . 4th ed. Buckingham: PICSIE Books, 2008
Mould G, Bowers J, Ghattas M. The evolution of the pathway and its role in improving patient care. Qual Saf Health Care 2010 [online publication 29 April]
Layton A, Moss F, Morgan G. Mapping out the patient’s journey: experiences of developing pathways of care. Qual Health Care 1998; 7 (suppl):S30-6
Graban M. Lean hospitals, improving quality, patient safety and employee satisfaction . New York: Taylor & Francis, 2009
Womack JP, Jones DT. Lean thinking . 2nd ed. London: Simon & Schuster, 2003
Cite this as: BMJ 2010;341:c4078
Contributors: TMT designed the protocol and drafted the manuscript; TMT, MB, JH, and TH collected and analysed the data; all authors critically reviewed and contributed towards revision and production of the manuscript. TMT is guarantor.
Competing interests: MB is a senior faculty member carrying out research for the Lean Enterprise Academy and undertakes paid consultancies both individually and from Lean Enterprise Academy, and training fees for providing lean thinking in healthcare.
Provenance and peer review: Not commissioned; externally peer reviewed.
- ↵ Kollberg B, Dahlgaard JJ, Brehmer P. Measuring lean initiatives in health care services: issues and findings. Int J Productivity Perform Manage 2007 ; 56 : 7 -24. OpenUrl CrossRef
- ↵ Bevan H, Lendon R. Improving performance by improving processes and systems. In: Walburg J, Bevan H, Wilderspin J, Lemmens K, eds. Performance management in health care. Abingdon: Routeledge, 2006:75-85.
- ↵ Kim CS, Spahlinger DA, Kin JM, Billi JE. Lean health care: what can hospitals learn from a world-class automaker? J Hosp Med 2006 ; 1 : 191 -9. OpenUrl CrossRef PubMed
- ↵ Layton A, Moss F, Morgan G. Mapping out the patient’s journey: experiences of developing pathways of care. Qual Health Care 1998 ; 7 (suppl): S30 -6. OpenUrl
- ↵ Peterson KM, Kane DP. Beyond disease management: population-based health management. Disease management. Chicago: American Hospital Publishing, 1996.
- ↵ NHS Modernisation Agency. Process mapping, analysis and redesign. London: Department of Health, 2005;1-40.
- ↵ Taylor AJ, Randall C. Process mapping: enhancing the implementation of the Liverpool care pathway. Int J Palliat Nurs 2007 ; 13 : 163 -7. OpenUrl PubMed
- ↵ Ben-Tovim DI, Dougherty ML, O’Connell TJ, McGrath KM. Patient journeys: the process of clinical redesign. Med J Aust 2008 ; 188 (suppl 6): S14 -7. OpenUrl PubMed Web of Science
- ↵ King DL, Ben-Tovim DI, Bassham J. Redesigning emergency department patient flows: application of lean thinking to health care. Emerg Med Australas 2006 ; 18 : 391 -7. OpenUrl CrossRef PubMed
- ↵ Mould G, Bowers J, Ghattas M. The evolution of the pathway and its role in improving patient care. Qual Saf Health Care 2010 ; published online 29 April.
- ↵ Rath F. Tools for developing a quality management program: proactive tools (process mapping, value stream mapping, fault tree analysis, and failure mode and effects analysis). Int J Radiat Oncol Biol Phys 2008 ; 71 (suppl): S187 -90. OpenUrl PubMed Web of Science
- ↵ Womack JP, Jones DT. Lean thinking. 2nd ed. London: Simon & Schuster, 2003.
- ↵ Graban M. Value and waste. In: Lean hospitals. New York: Taylor & Francis, 2009;35-56.
- ↵ Westwood N, James-Moore M, Cooke M. Going lean in the NHS. London: NHS Institute for Innovation and Improvement, 2007.
- ↵ Liker JK. The heart of the Toyota production system: eliminating waste. The Toyota way. New York: McGraw-Hill, 2004;27-34.
- ↵ Womack JP, Jones DT. Introduction: Lean thinking versus Muda. In: Lean thinking. 2nd ed. London: Simon & Schuster, 2003:15-28.
- ↵ George ML, Rowlands D, Price M, Maxey J. Value stream mapping and process flow tools. Lean six sigma pocket toolbook. New York: McGraw Hill, 2005:33-54.
- ↵ Fillingham D. Can lean save lives. Leadership Health Serv 2007 ; 20 : 231 -41. OpenUrl CrossRef
- ↵ Benjamin A. Audit: how to do it in practice. BMJ 2008 ; 336 : 1241 -5. OpenUrl FREE Full Text
- ↵ Vissers J. Unit Logistics. In: Vissers J, Beech R, eds. Health operations management patient flow logistics in health care. Oxford: Routledge, 2005:51-69.
- ↵ Graban M. Overview of lean for hospital. Lean hospitals. New York: Taylor & Francis, 2009;19-33.
- ↵ Eaton M. The key lean concepts. Lean for practitioners. Penryn, Cornwall: Academy Press, 2008:13-28.
- ↵ Baker M, Taylor I, Mitchell A. Analysing the situation: learning to think differently. In: Making hospitals work. Ross-on-Wye: Lean Enterprise Academy, 2009:51-70.
- ↵ Ko HH, Zhang H, Telford JJ, Enns R. Factors influencing patient satisfaction when undergoing endoscopic procedures. Gastrointest Endosc 2009 ; 69 : 883 -91. OpenUrl CrossRef PubMed Web of Science
- ↵ Del Rio AS, Baudet JS, Fernandez OA, Morales I, Socas MR. Evaluation of patient satisfaction in gastrointestinal endoscopy. Eur J Gastroenterol Hepatol 2007 ; 19 : 896 -900. OpenUrl CrossRef PubMed Web of Science
- ↵ Seip B, Huppertz-Hauss G, Sauar J, Bretthauer M, Hoff G. Patients’ satisfaction: an important factor in quality control of gastroscopies. Scand J Gastroenterol 2008 ; 43 : 1004 -11. OpenUrl CrossRef PubMed Web of Science
- ↵ Yanai H, Schushan-Eisen I, Neuman S, Novis B. Patient satisfaction with endoscopy measurement and assessment. Dig Dis 2008 ; 26 : 75 -9. OpenUrl CrossRef PubMed Web of Science
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 04 December 2019
“Patient Journeys”: improving care by patient involvement
- Matt Bolz-Johnson 1 ,
- Jelena Meek 2 &
- Nicoline Hoogerbrugge 2
European Journal of Human Genetics volume 28 , pages 141–143 ( 2020 ) Cite this article
24k Accesses
18 Citations
25 Altmetric
Metrics details
- Cancer genetics
- Cancer screening
- Cancer therapy
- Health policy
“I will not be ashamed to say ‘ I don’t know’ , nor will I fail to call in my colleagues…”. For centuries this quotation from the Hippocratic oath, has been taken by medical doctors. But what if there are no other healthcare professionals to call in, and the person with the most experience of the disease is sitting right in front of you: ‘ your patient ’.
This scenario is uncomfortably common for patients living with a rare disease when seeking out health care. They are fraught by many hurdles along their health care pathway. From diagnosis to treatment and follow-up, their healthcare pathway is defined by a fog of uncertainties, lack of effective treatments and a multitude of dead-ends. This is the prevailing situation for many because for rare diseases expertise is limited and knowledge is scarce. Currently different initiatives to involve patients in developing clinical guidelines have been taken [ 1 ], however there is no common method that successfully integrates their experience and needs of living with a rare disease into development of healthcare services.
Even though listening to the expertise of a single patient is valuable and important, this will not resolve the uncertainties most rare disease patients are currently facing. To improve care for rare diseases we must draw on all the available knowledge, both from professional experts and patients, in order to improve care for every single patient in the world.
Patient experience and satisfaction have been demonstrated to be the single most important aspect in assessing the quality of healthcare [ 2 ], and has even been shown to be a predictor of survival rates [ 3 ]. Studies have evidenced that patient involvement in the design, evaluation and designation of healthcare services, improves the relevance and quality of the services, as well as improves their ability to meet patient needs [ 4 , 5 , 6 ]. Essentially, to be able to involve patients, the hurdles in communication and initial preconceptions between medical doctors and their patients need to be resolved [ 7 ].
To tackle the current hurdles in complex or rare diseases, European Reference Networks (ERN) have been implemented since March 2017. The goal of these networks is to connect experts across Europe, harnessing their collective experience and expertise, facilitating the knowledge to travel instead of the patient. ERN GENTURIS is the Network leading on genetic tumour risk syndromes (genturis), which are inherited disorders which strongly predispose to the development of tumours [ 8 ]. They share similar challenges: delay in diagnosis, lack of cancer prevention for patients and healthy relatives, and therapeutic. To overcome the hurdles every patient faces, ERN GENTURIS ( www.genturis.eu ) has developed an innovative visual approach for patient input into the Network, to share their expertise and experience: “Patient Journeys” (Fig. 1 ).
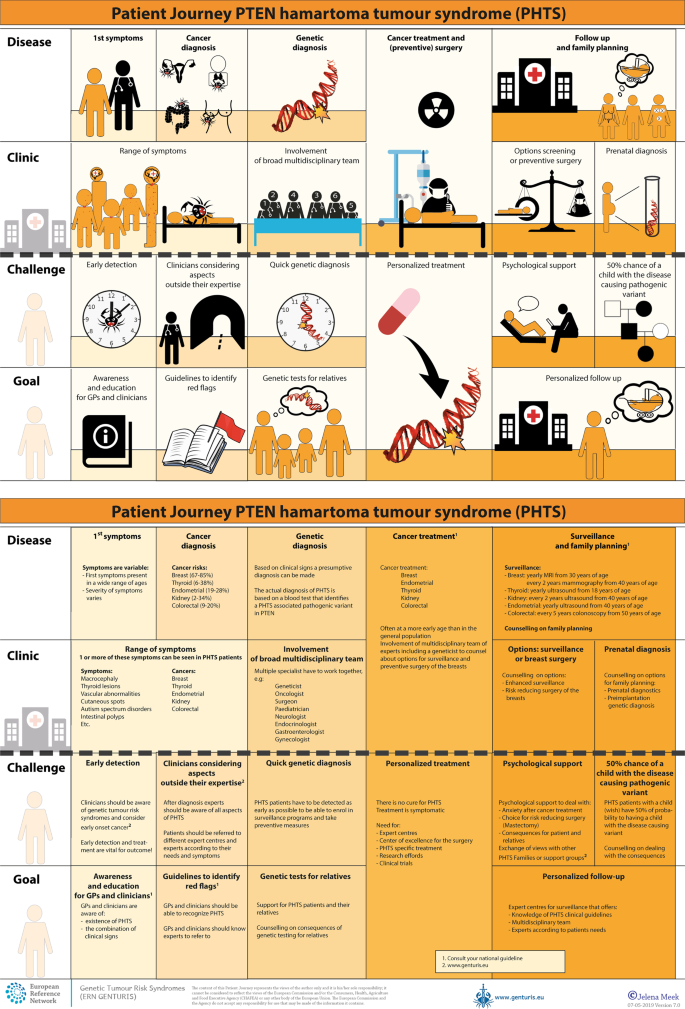
Example of a Patient Journey: PTEN Hamartoma Tumour Syndrome (also called Cowden Syndrome), including legend page ( www.genturis.eu )
The “Patient Journey” seeks to identify the needs that are common for all ‘ genturis syndromes ’, and those that are specific to individual syndromes. To achieve this, patient representatives completed a mapping exercise of the needs of each rare inherited syndrome they represent, across the different stages of the Patient Journey. The “Patient Journey” connects professional expert guidelines—with foreseen medical interventions, screening, treatment—with patient needs –both medical and psychological. Each “Patient Journey” is divided in several stages that are considered inherent to the specific disease. Each stage in the journey is referenced under three levels: clinical presentation, challenges and needs identified by patients, and their goal to improve care. The final Patient Journey is reviewed by both patients and professional experts. By visualizing this in a comprehensive manner, patients and their caregivers are able to discuss the individual needs of the patient, while keeping in mind the expertise of both professional and patient leads. Together they seek to achieve the same goal: improving care for every patient with a genetic tumour risk syndrome.
The Patient Journeys encourage experts to look into national guidelines. In addition, they identify a great need for evidence-based European guidelines, facilitating equal care to all rare patients. ERN GENTURIS has already developed Patient Journeys for the following rare diseases ( www.genturis.eu ):
PTEN hamartoma tumour syndrome (PHTS) (Fig. 1 )
Hereditary breast and ovarian cancer (HBOC)
Lynch syndrome
Neurofibromatosis Type 1
Neurofibromatosis Type 2
Schwannomatosis
A “Patient Journey” is a personal testimony that reflects the needs of patients in two key reference documents—an accessible visual overview, supported by a detailed information matrix. The journey shows in a comprehensive way the goals that are recognized by both patients and clinical experts. Therefore, it can be used by both these parties to explain the clinical pathway: professional experts can explain to newly identified patients how the clinical pathway generally looks like, whereas their patients can identify their specific needs within these pathways. Moreover, the Patient Journeys could serve as a guide for patients who may want to write, in collaboration with local clinicians, diaries of their journeys. Subsequently, these clinical diaries can be discussed with the clinician and patient representatives. Professionals coming across medical obstacles during the patient journey can contact professional experts in the ERN GENTURIS, while patients can contact the expert patient representatives from this ERN ( www.genturis.eu ). Finally, the “Patient Journeys” will be valuable in sharing knowledge with the clinical community as a whole.
Our aim is that medical doctors confronted with rare diseases, by using Patient Journeys, can also rely on the knowledge of the much broader community of expert professionals and expert patients.
Armstrong MJ, Mullins CD, Gronseth GS, Gagliardi AR. Recommendations for patient engagement in guideline development panels: a qualitative focus group study of guideline-naive patients. PloS ONE 2017;12:e0174329.
Article PubMed PubMed Central Google Scholar
Gupta D, Rodeghier M, Lis CG. Patient satisfaction with service quality as a predictor of survival outcomes in breast cancer. Supportive Care Cancer Off J Multinatl Assoc Supportive Care Cancer. 2014;22:129–34.
Google Scholar
Gupta D, Lis CG, Rodeghier M. Can patient experience with service quality predict survival in colorectal cancer? J Healthc Qual Off Publ Natl Assoc Healthc Qual. 2013;35:37–43.
Sharma AE, Knox M, Mleczko VL, Olayiwola JN. The impact of patient advisors on healthcare outcomes: a systematic review. BMC Health Serv Res. 2017;17:693.
Fonhus MS, Dalsbo TK, Johansen M, Fretheim A, Skirbekk H, Flottorp SA. Patient-mediated interventions to improve professional practice. Cochrane Database Syst Rev. 2018;9:Cd012472.
PubMed Google Scholar
Cornman DH, White CM. AHRQ methods for effective health care. Discerning the perception and impact of patients involved in evidence-based practice center key informant interviews. Rockville, MD: Agency for Healthcare Research and Quality (US); 2017.
Chalmers JD, Timothy A, Polverino E, Almagro M, Ruddy T, Powell P, et al. Patient participation in ERS guidelines and research projects: the EMBARC experience. Breathe (Sheff, Engl). 2017;13:194–207.
Article Google Scholar
Vos JR, Giepmans L, Rohl C, Geverink N, Hoogerbrugge N. Boosting care and knowledge about hereditary cancer: european reference network on genetic tumour risk syndromes. Fam Cancer 2019;18:281–4.
Article PubMed Google Scholar
Download references
Acknowledgements
This work is generated within the European Reference Network on Genetic Tumour Risk Syndromes – FPA No. 739547. The authors thank all ERN GENTURIS Members and patient representatives for their work on the Patient Journeys (see www.genturis.eu ).
Author information
Authors and affiliations.
SquareRootThinking and EURORDIS – Rare Diseases Europe, Paris, France
Matt Bolz-Johnson
Human Genetics, Radboud University Medical Center, Nijmegen, The Netherlands
Jelena Meek & Nicoline Hoogerbrugge
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Nicoline Hoogerbrugge .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Bolz-Johnson, M., Meek, J. & Hoogerbrugge, N. “Patient Journeys”: improving care by patient involvement. Eur J Hum Genet 28 , 141–143 (2020). https://doi.org/10.1038/s41431-019-0555-6
Download citation
Received : 07 August 2019
Revised : 04 October 2019
Accepted : 01 November 2019
Published : 04 December 2019
Issue Date : February 2020
DOI : https://doi.org/10.1038/s41431-019-0555-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Care trajectories of surgically treated patients with a prolactinoma: why did they opt for surgery.
- Victoria R. van Trigt
- Ingrid M. Zandbergen
- Nienke R. Biermasz
Pituitary (2023)
Designing rare disease care pathways in the Republic of Ireland: a co-operative model
- E. P. Treacy
Orphanet Journal of Rare Diseases (2022)
Rare disease education in Europe and beyond: time to act
- Birute Tumiene
- Harm Peters
- Gareth Baynam
Development of a patient journey map for people living with cervical dystonia
- Monika Benson
- Alberto Albanese
- Holm Graessner
Der klinische Versorgungspfad zur multiprofessionellen Versorgung seltener Erkrankungen in der Pädiatrie – Ergebnisse aus dem Projekt TRANSLATE-NAMSE
- Daniela Choukair
- Min Ae Lee-Kirsch
- Peter Burgard
Monatsschrift Kinderheilkunde (2022)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Patient journey 101: Definition, benefits, and strategies
Last updated
22 August 2023
Reviewed by
Melissa Udekwu, BSN., RN., LNC
Today’s patients are highly informed and empowered. They know they have choices in their healthcare, which can put healthcare providers under a lot of pressure to provide solutions and meet their patients’ expectations.
Just like any customer, patients embark on a journey that begins before they ever contact the provider. This makes understanding the journey and where improvements can be made extremely important. Mapping the patient journey can help practitioners provide better care, retain a solid customer base, and ultimately identify ways to improve patient health.
- What is the patient journey?
The patient journey is best described as the sequence of experiences a patient has from admission to discharge. This includes all the touchpoints between the patient and provider from beginning to end.
The patient journey continues through consultation, where they meet the potential caregiver. That portion of the journey includes interactions with a doctor and support staff, how long they wait to be seen, and the steps taken for diagnosis and treatment.
The patient’s post-care journey includes follow-ups from the healthcare provider, post-treatment care, and billing. For example, if the patient has questions about post-surgery care or how to read their invoice, how quickly their questions are answered and their problems resolved will impact their satisfaction.
Mapping the patient journey helps healthcare providers improve patient satisfaction at every step of the way. By collecting data at each stage and conducting an in-depth analysis, providers can identify patient concerns and make the necessary improvements to meet their patient satisfaction goals.
What is another name for the patient journey?
The term “patient funnel” describes the journey patients take from first learning about a healthcare provider or healthcare product to actually making an appointment or purchase. This “funnel” can be applied to any type of business, describing the stages a customer goes through to obtain a service.
- Understanding the stages of the patient journey
Each stage of the patient journey is essential to a positive patient experience . Gathering and analyzing data can alert healthcare providers to potential issues throughout the journey.
Data collection at each of the following stages will give healthcare providers the information they need to make the necessary improvements:
1. Awareness
Awareness is where the patient journey begins. This is when they first research symptoms and identify the need to see a medical professional.
They may consider at-home remedies and get advice from friends, social media, or websites. Once they identify the need for a healthcare provider, they continue their research via review sites, advertising campaigns, and seeking referrals from friends and family.
Determining the way patients become aware they need healthcare and the sources they use for research is important. The data collected at this stage could suggest your organization has an insufficient social media presence, inadequate advertising, or a website in need of an update.
To remedy these shortcomings, you might consider adding informational blogs to your website, performing a social media analysis, or closely monitoring customer reviews.
This stage in the patient journey is where the patient schedules services with the healthcare provider.
This engagement is essential for acquiring new patients and retaining current patients. Patients will contact you in several ways to schedule an appointment or get information. Most will call on the first attempt to schedule an appointment.
This is a crucial touchpoint in the journey. A new patient may become frustrated and move on if they find it difficult to access your services or are placed on hold for a long period or transferred numerous times.
Patient engagement occurs in other ways, such as your online patient portal, text messages, and emails. Your patients may interact differently, so it’s important to gather data that represents their preferred means of communication. Work to make the improvements required to correct access issues and ensure efficient communication.
The care stage can include everything from your patient’s interaction with the front desk to how long they have to wait in the examination room to see a doctor.
Check-in, check-out, admissions, discharge, billing, and of course, the actual visit with the healthcare provider are other touchpoints in the care stage.
There are a couple of ways to gather and analyze this data. Most organizations choose to analyze it holistically, even if it’s collected separately. For example, you might gather data about the patient’s interaction with the front desk, the clinical visit, and the discharge process, but you may want to analyze the care segment as a whole.
4. Treatment
Treatment may be administered in the office. For example, a patient diagnosed with hypertension may have medication prescribed. That medication is the treatment. Gathering information at this stage is critical to see how your patient views the healthcare provider’s follow-up or responses to inquiries.
In most cases, treatment extends beyond the initial clinical visit. For example, a patient might require additional tests to get a diagnosis. Providing the next steps to a patient in a timely manner and letting them know the test results is crucial to patient satisfaction .
5. Long term
A satisfied patient results in a long-term relationship and referrals to friends and family. Most of the data collected at this stage will be positive since the patient is continuing to use your services.
Gathering data after the treatment stage allows you to expand on the qualities that keep patients returning for your services in the long term.
- Benefits of patient journey mapping
The patient benefits from their healthcare provider understanding their journey and taking steps to improve it. Healthcare providers also reap several benefits, including the following:
1. Efficient patient care
When they understand the patient journey, healthcare providers can provide care more efficiently and spend less time and money on unnecessary, unwanted communications.
2. Proactive patient care
Proactive patient care is aimed at preventing rather than treating disease. For example, women who are over a certain age should have an annual mammogram, smokers may be tested for lung disease, and elderly women may need a bone density study. These preventative measures can help keep disease at bay, improve health outcomes, and build trust with patients.
3. Value-based patient care
Patients don’t want to feel they are being charged unfairly for their healthcare. Focusing on the individual patient promotes satisfaction and yields positive outcomes.
The Center for Medicare and Medicaid Services (CMS) has issued recent guidelines for participants that help offset the costs of high-quality care through a reward system.
4. Retention and referrals
Patients who are happy with their journey will keep returning for healthcare, and happy patients equal voluntary referrals. Many providers offer rewards to incentify referrals.
- How to get started with patient journey mapping
Follow the steps below to start the patient journey mapping process:
Establish your patient personas
Journey mapping is a great way to identify your patient’s characteristics so that their experience can be further enhanced.
Some of the following determinations can help you pinpoint your patient’s persona and establish protocols to provide a better service:
How do your patients prefer to communicate? Are they more comfortable with phone calls, texts, or other methods?
How are most patients finding your services? Are they being referred by friends or family members, or are they seeing advertisements?
Would the patient prefer in-person communication or telecommunication?
What are the patient’s expectations of care?
This data can be complex and widespread, but it can give you the information you need to more effectively and efficiently communicate with your patients.
Understand the entire patient lifecycle
Each patient is unique. Understanding the patient lifecycle can avoid confusion and miscommunication.
To positively engage the patient, you’ll need to gather data not only about communication methods but where they are in the patient journey, their health issue, and their familiarity with the healthcare provider’s procedures and treatment options.
Understand the moments of truth
With a few exceptions, most people seek healthcare services when they are ill or have a healthcare issue. These situations can cause patients to feel stressed and anxious. It’s these moments of interaction where compassion, knowledge, and understanding can provide relief and reassurance.
When patients see their healthcare provider, they are looking for solutions to problems. It’s the provider’s opportunity to identify these moments of truth and capitalize on them.
Get the data you need
Healthcare providers can collect vast amounts of data from patients, but the data collected rarely goes far enough in analyzing and determining solutions.
Your patients have high expectations regarding personalized treatment based on data. They want personalized, easy access to medical information and records, responsive treatments and follow-up, and communication in their preferred format.
You need more than clinical data to give patients what they want. You also need personal data that sets each patient apart and ensures a tailored experience.
For example, it might be challenging for parents of small children to contact the clinic and schedule appointments at certain times of the day. As a healthcare provider, you’ll need to be aware of the best times to contact this individual and offer simple methods for scheduling appointments.
Another example is patients with physical disabilities. You can take steps to improve their access to and experience at the healthcare facility.
Encourage referrals and loyalty
Although engagement on social media and online forums is becoming more and more common, the best way for new patients to find you is through referrals. Referrals stem from satisfactory experiences and trust.
Editor’s picks
Last updated: 27 June 2023
Last updated: 22 July 2023
Last updated: 11 September 2023
Last updated: 10 October 2023
Last updated: 16 November 2023
Last updated: 28 September 2023
Last updated: 12 October 2023
Last updated: 25 November 2023
Last updated: 3 July 2023
Last updated: 27 January 2024
Latest articles
Related topics, .css-je19u9{-webkit-align-items:flex-end;-webkit-box-align:flex-end;-ms-flex-align:flex-end;align-items:flex-end;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-flex-direction:row;-ms-flex-direction:row;flex-direction:row;-webkit-box-flex-wrap:wrap;-webkit-flex-wrap:wrap;-ms-flex-wrap:wrap;flex-wrap:wrap;-webkit-box-pack:center;-ms-flex-pack:center;-webkit-justify-content:center;justify-content:center;row-gap:0;text-align:center;max-width:671px;}@media (max-width: 1079px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}}@media (max-width: 799px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}} decide what to .css-1kiodld{max-height:56px;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;}@media (max-width: 1079px){.css-1kiodld{display:none;}} build next, decide what to build next.

Users report unexpectedly high data usage, especially during streaming sessions.

Users find it hard to navigate from the home page to relevant playlists in the app.

It would be great to have a sleep timer feature, especially for bedtime listening.

I need better filters to find the songs or artists I’m looking for.
Log in or sign up
Get started for free
Root out friction in every digital experience, super-charge conversion rates, and optimize digital self-service
Uncover insights from any interaction, deliver AI-powered agent coaching, and reduce cost to serve
Increase revenue and loyalty with real-time insights and recommendations delivered to teams on the ground
Know how your people feel and empower managers to improve employee engagement, productivity, and retention
Take action in the moments that matter most along the employee journey and drive bottom line growth
Whatever they’re are saying, wherever they’re saying it, know exactly what’s going on with your people
Get faster, richer insights with qual and quant tools that make powerful market research available to everyone
Run concept tests, pricing studies, prototyping + more with fast, powerful studies designed by UX research experts
Track your brand performance 24/7 and act quickly to respond to opportunities and challenges in your market
Explore the platform powering Experience Management
- Free Account
- For Digital
- For Customer Care
- For Human Resources
- For Researchers
- Financial Services
- All Industries
Popular Use Cases
- Customer Experience
- Employee Experience
- Net Promoter Score
- Voice of Customer
- Customer Success Hub
- Product Documentation
- Training & Certification
- XM Institute
- Popular Resources
- Customer Stories
- Artificial Intelligence
- Market Research
- Partnerships
- Marketplace
The annual gathering of the experience leaders at the world’s iconic brands building breakthrough business results, live in Salt Lake City.
- English/AU & NZ
- Español/Europa
- Español/América Latina
- Português Brasileiro
- REQUEST DEMO
- Experience Management
- Sector Specific
- Patient Experience
- Patient Journey Mapping
Try Qualtrics for free
Your complete guide to patient journey mapping.
15 min read Healthcare organizations can increase patient retention and improve patient satisfaction with patient journey mapping. Discover how to create a patient journey map and how you can use it to improve your organization’s bottom line.
What is the patient journey?
The patient journey is the sequence of events that begins when a patient first develops a need for care. Rather than focusing on service delivery, the patient journey encompasses all touchpoints of a patient’s healthcare experience–from locating healthcare providers and scheduling appointments, to paying the bill and continuing their care after treatment.
Examining the patient journey is essential to improving the patient experience. Not all interactions a patient has with your organization are weighted the same. Gathering patient feedback and understanding perceptions all along the patient journey can help you to identify moments of truth : the touchpoints that have the biggest impact on patient loyalty.
Download eBook: The 3 steps to driving human-centered healthcare experiences
The patient journey vs. the patient experience
Unlike traditional patient experience measurement, the patient journey looks not only at service delivery but also at the steps the patient takes before and after they engage directly with your organization. It recognizes that patient interactions with a healthcare system go well beyond the walls of the medical facility itself.
What are the stages of the patient journey?
There are several stages along the patient journey. When gathering patient feedback, you should make sure to capture insights at each of these stages.
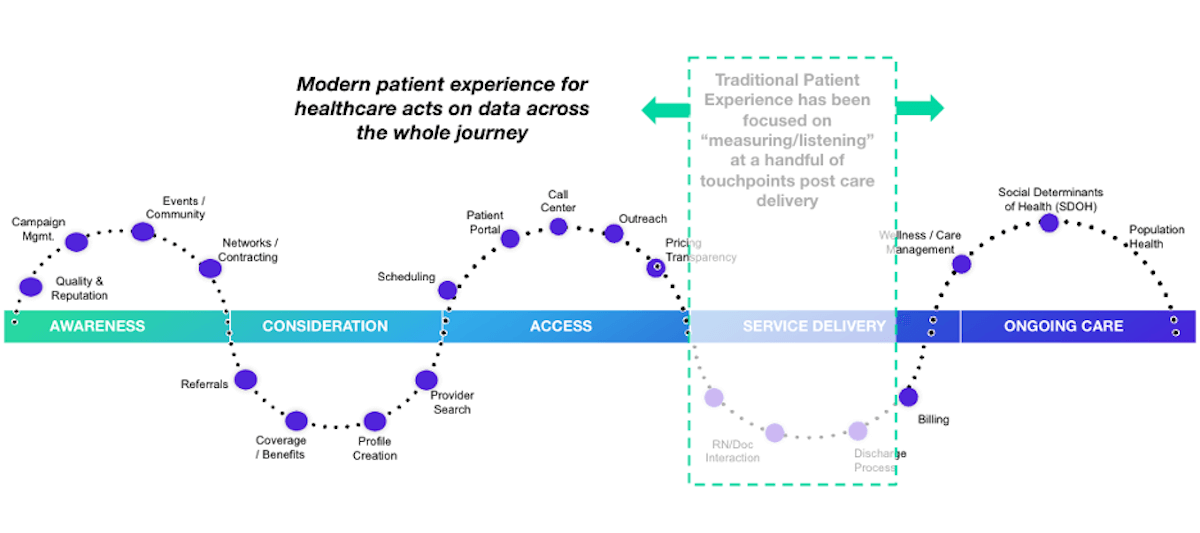
Stage 1: Awareness
The patient journey starts with awareness. In this stage, the patient identifies a need for care and begins searching for care providers. Examples of how patients learn about healthcare providers include online searches, review sites, marketing campaigns, networking, and community involvement.
Stage 2: Consideration
In the consideration stage, the patient weighs their options to determine if your health system can meet their needs. Factors patients consider include referrals, coverage and benefits, recommendations, access, and ratings and reviews. Often in this stage, patients interact with your website or social media pages or contact you via phone or email during this stage.
Stage 3: Access
The access stage is where the patient decides to schedule services with your healthcare organization. Direct patient engagement with your organization increases during this stage. You’ll engage with patients in a variety of ways including phone calls, the patient portal, text messages, and emails as part of the scheduling and new patient acquisition process.
Stage 4: Service delivery
The service delivery stage relates to the clinical care provided to your patients. Encompassed in this stage are the clinical visit itself, check-in and check-out, admission and discharge, and billing. Traditional patient satisfaction measurement centers around this stage of the patient journey.
Stage 5: Ongoing care
The ongoing care stage of the patient journey involves patient engagement that occurs after the interactions directly related to service delivery. In addition to wellness and care management, this stage may address social determinants of health and population health.
What is a patient journey map?
The best way to utilize the patient journey to enhance patient experiences is by journey mapping. A patient journey map is a visual tool that illustrates the relationship a patient has with a healthcare organization over time.
Patient journey mapping helps stakeholders to assess the patient experience from multiple perspectives. Journey maps provide a way to visualize the internal and external factors affecting patient flow and the different paths patients must take in order to reach their care goals.
What are the benefits of patient journey mapping?
Patient journey mapping can help you to visualize all of the steps patients take throughout the entire process of seeking, receiving, and continuing care. Creating a patient journey map is useful to identify pain points and gaps in care. Mapping the patient journey makes it easier to develop solutions that make a more seamless experience within your healthcare system.
Patient journey mapping benefits include:
- Creating shared ownership of the patient experience
- Refining your patient listening strategy
- Aligning your organization with a common view of the patient experience
- Measuring gaps between the intended experience for your patients versus the actual experience
- Identifying and resolving common pain points for your patients
Four types of patient journey maps
When creating a patient journey map, there are four types to consider. Each type of map has an intended purpose. You might start your patient journey mapping with only one type and incorporate the others as your efforts progress.
Current state
A current state journey map tells the story of what patients do, think, and feel as they interact with your organization today. This type of patient journey map is ideally created using patient data and observational data.
The current state journey map is best for driving incremental improvements to enhance the patient experience.
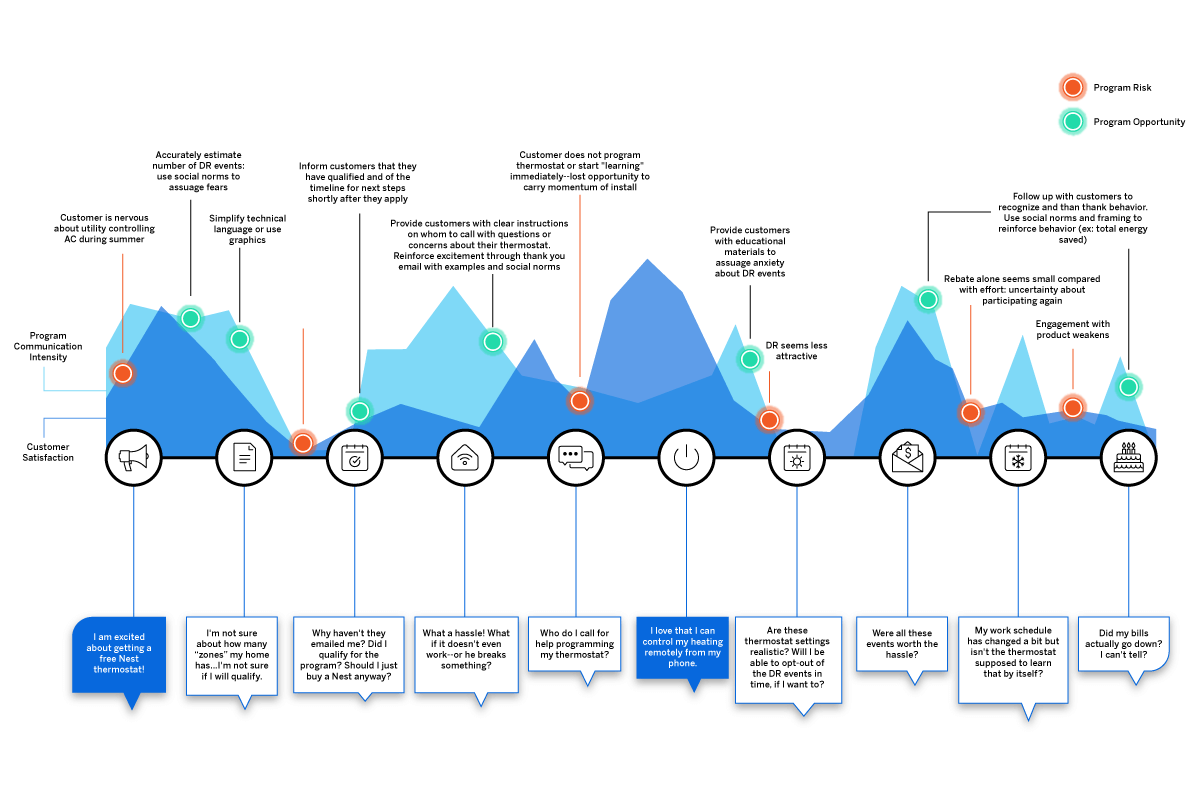

Future state
A future state patient journey map tells the story of what you want your patients to do, think, and feel as they interact with your organization in the future. This type of map should capture the ideal journey you’d like to see for your patients.
The future state journey map is an effective tool to drive strategy, align teams, and communicate your visions for new services, processes, and experiences.
Day in the life
A day in the life patient journey map illustrates what your patients do, think, and feel today, within a specific area of focus. Patient personas are particularly useful when creating day in the life maps; these are discussed in greater detail below.
This type of patient journey map is intended to capture what your patients experience both inside and outside of the healthcare system. Day in the life maps are valuable to address unmet needs and determine how and when you can better engage your patients.
Service blueprint
A service blueprint is a simplified diagram of a current state or future state patient journey map. In the service blueprint, you add layers to illustrate the systems of people, processes, policies, and technologies surrounding each patient touchpoint.
For current state patient journey maps, the service blueprint can help to identify root causes of pain points. For future state, the service blueprint is helpful to visualize the systems or processes that can be put in place to support the intended patient experience.
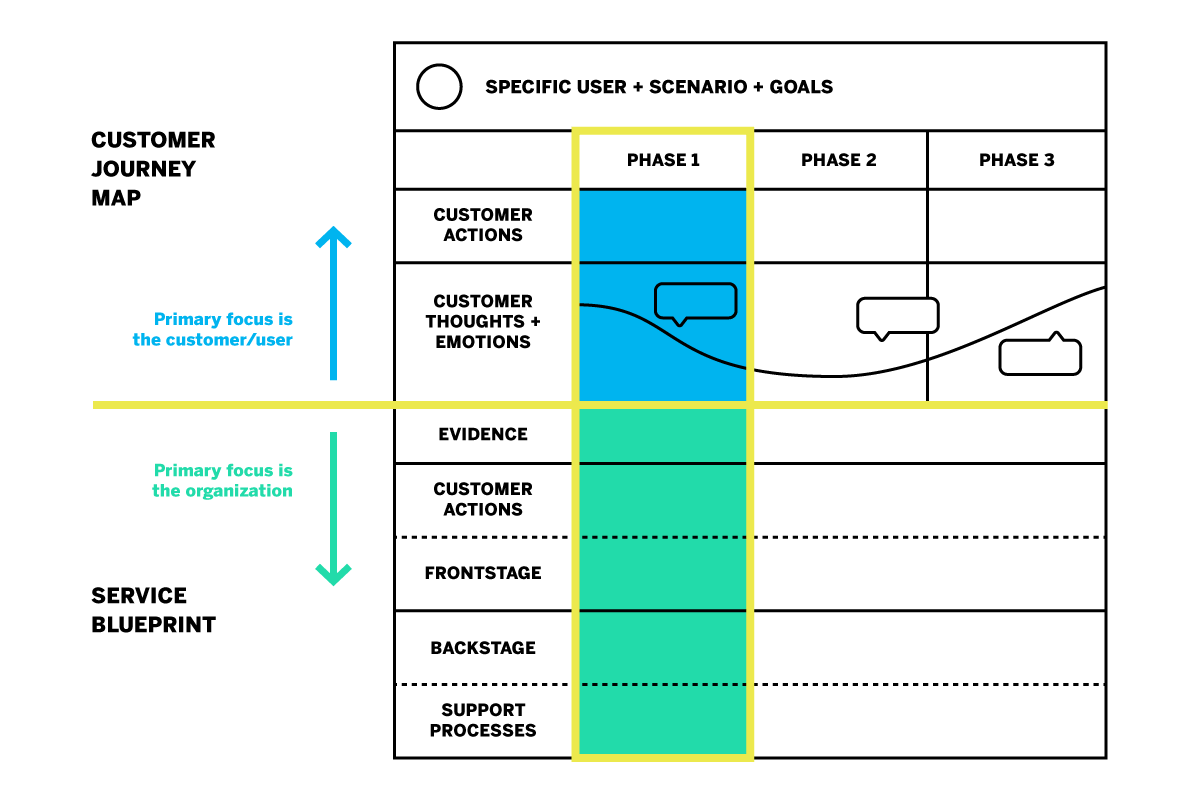
How do you create a patient journey map?
Now that you know about the different types of patient journey maps and their roles in driving patient experience improvement, how do you get started on creating your own?
The most useful maps are those which can expound upon each touchpoint of the healthcare journey with operational data, such as patient demographics, as well as real patient insights and perspectives. Using a platform that can capture this data will aid significantly in your patient journey mapping process.
Patient journey mapping: getting started
Before you get started, it’s a good idea to engage individuals across all departments and include input from multiple stakeholders. Once you’re ready, follow these steps to begin creating an effective patient journey map.
Identify your target audience
What type of patient journey will you be mapping? There may be varying patient journeys within your organization; for instance, an oncology patient’s journey will look very different from that of an expectant mother. The journey of a patient with health insurance will differ from that of a patient without insurance. To map the patient journey, you’ll want to create robust patient profiles you can use to segment and track like-populations throughout the healthcare experience.
Establishing patient personas and segments
Not every patient will have the same healthcare goals. Creating patient personas based on behaviors and preferences is a good way to differentiate the needs and more clearly understand the perspectives of the unique populations you serve.
The ideal patient persona will include the following information.
- Demographic information such as age group, gender, or location
- Healthcare-specific goals, conditions, and treatments
- Healthcare-specific challenges/pain points
- Engagement patterns and expressed feedback
- How your services fit into their life
- Barriers to care
Specify a goal for the patient’s journey
The patient personas you create will all have unique goals within the care journey. The patient has a specific goal in mind when they initiate contact with your organization, whether it is treatment of symptoms, a diagnosis for chronic issues, or surgery.
Every interaction along the patient journey influences how successful the patient feels about achieving this goal. When mapping the patient journey, you’ll want to consider how the various touchpoints affect the patient’s ability to meet this goal.
Identify the patient’s steps to accomplish their target goal
This step is about how the patient views their care journey within your health system–not about the actual processes and systems your organization has in place. Effective patient journey mapping requires you to see how the patient navigates the journey through their point of view.
Omni-channel listening is a valuable strategy in this step of journey mapping. Listening to your patients across all the channels can provide a clearer picture of their perceptions and behaviors as they engage with your organization.
Some steps the patient takes may not even include your organization, but might still affect how they are interacting with you directly. For example, if a patient logs into their health insurance portal to check coverage for healthcare services, they are not engaging with your organization but this is still a part of their care journey that may feed into their interactions with your organization later on.
Uncover perceptions along the journey
Gather patient feedback along the touchpoints of the care journey to identify key emotional moments that may disproportionately shape attitudes. These insights shed light on what’s working and what’s not; they can also be used to highlight the moments of truth that contribute to patient loyalty.
Patient perceptions are an important piece of patient journey mapping; it will be difficult to drive action without them.
Additional tips for creating the ideal patient journey map
Patient journey mapping is a continuous process. Creating the map is the first step, but the true value is dependent upon maintaining the map as you continue to gather insights and refine processes.
This leads to the second tip: be ready to take action! You can use a patient journey map to draw conclusions about your patients’ experiences within your organization, but awareness alone will yield no benefits. The journey map is a valuable tool to be used in your wider improvement efforts.
How do you drive action using a patient journey map?
Once your patient journey mapping is complete, it’s time to put it to good use. Here are five ways patient journey maps can be used to drive action.
Identify and fix problems
The visual layout of a journey map makes it ideal to identify gaps and potential pain points in your patient journeys. This will give you a better understanding of what’s working and what’s not. It will also help you to visualize where and how improvements can be made.
Build a patient mindset
Patient journey mapping enables you to incorporate more patient-centric thinking into your processes and systems. Use your map to challenge internal ideas of what patients want or need. Invite stakeholders to navigate the touchpoints along the healthcare journey to gain perspective.
Uncover unmet patient needs
By mapping the patient journey, you can build stronger patient relationships by listening across all channels to determine where experiences are falling short or where unmet needs emerge. This enables you to look for opportunities to expand alternatives, streamline initiatives, and create new, engaging ways for your patients to share feedback.
Create strategic alignment
Utilize your patient journey map to prioritize projects or improvement efforts. It can also help you to better engage interdepartmental staff to better understand policies and work together toward patient experience goals.
Refine measurement
Patient journey mapping is a great resource to use when defining patient satisfaction metrics and identifying gaps in how you currently gather insights.
How does patient journey mapping increase your bottom line?
Patient journey mapping can increase your bottom line by laying the foundation for improved patient satisfaction and higher retention.
Organizations across all industries are looking to understand customer journeys in order to attract and retain customers by gaining deeper insights into what drives the consumer experience.
As healthcare becomes more consumer-driven, health systems must similarly map the patient journey to improve the patient experience and boost retention. The cost of patient acquisition, combined with the fact that patients are willing to shop around for the best healthcare experience, means success depends on creating the most seamless patient journey possible.
The tools for success
For the most impactful patient journey mapping experience, you’ll want the ability to link your operational and experience data to your journey map’s touchpoints. Insights about what has happened at each touchpoint, as well as why it is happening, empower you to create experiences that meet patient expectations and drive up satisfaction.
Here are some best practice considerations as you develop your patient journey mapping strategy:
- Create a shared understanding throughout your health system of how your patients interact with your organization, and you’ll know the roles and responsibilities of your different teams
- Design a unique patient journey based on multichannel, real-time feedback from the patient
- Consider the frequency with which topics emerge in feedback, as well as the emotional intensity behind them to zero in on what improvements can drive the greatest impact
- Develop empathy and collaboration between teams, working together to achieve the same outcome
- Drive a patient-centric culture by developing a shared sense of ownership of the patient experience
- Connect your operational patient data with your patient experience feedback in one system
- Leverage a closed-loop feedback system that triggers actions for immediate responses to patient concerns
Qualtrics’ XM Platform™ is designed to support all of these actions throughout the journey mapping process.
The 3 steps to driving human-centered healthcare experiences
Related resources
Patient feedback 15 min read, healthcare branding 13 min read, patient journey 10 min read, patient experience 12 min read, symptoms survey 10 min read, nurse satisfaction survey 11 min read, cahps surveys 6 min read, request demo.
Ready to learn more about Qualtrics?
The Patient Journey
- Open Access
- First Online: 15 December 2020
Cite this chapter
You have full access to this open access chapter

- Elena Beleffi 5 ,
- Paola Mosconi 6 &
- Susan Sheridan 7
41k Accesses
2 Citations
The wide implementation of patient safety improvement efforts continues to face many barriers including insufficient involvement of all stakeholders in healthcare, lack of individual and organizational learning when medical errors occur and scarce investments in patient safety. The promotion of systems-based approaches offers methods and tools to improve the safety of care. A multidisciplinary perspective must include the involvement of patients and citizens as fundamental contributors to the design, implementation, and delivery of health services.
The patient journey is a challenging example of using a systems approach. The inclusion of the patient’s viewpoint and experience about their health journey throughout the time of care and across all the care settings represents a key factor in improving patient safety. Patient engagement ensures that the design of healthcare services are aligned with the values, the preferences, and needs of the patient community and integrates the real-life experience and the skills of the people to enhance patient safety in the patient journey.
The utmost priority to implement patient engagement is the training of patients. Therefore, training for both patients/families/advocates and health professionals is the foundation on which to build active engagement of patients and consequently an effective and efficient patient journey.
The chapter offers examples of successful training courses designed to foster strategic alliances among healthcare professionals and researchers with patients and their organizations. Training of patients constitutes the first step to develop shared knowledge, co-produced projects, and the achievement of active multilevel participation of patients for the implementation of patient safety in the patient journey.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others

Patient Experiences of Safety in Care Transitions
Top 10 interventions in paediatric patient safety.

‘The big buzz’: a qualitative study of how safe care is perceived, understood and improved in general practice
- Patient journey
- Patient engagement
- Patient empowerment
- Patient safety
- Healthcare ergonomics
- Co-production
- Knowledge creation
1 Introduction
Almost 20 years after publication “To Err is Human: Building a Better Health System” (Kohn et al. 1999), patient safety is still not widely implemented. This report from the Institute of Medicine is the milestone that constituted a turning point for improving quality of care and patient safety identifying the need to rethink healthcare delivery to provide safe, effective, and efficient care.
The barriers of implementing patient safety as a driving force for change towards more effective healthcare include multiple factors: insufficient involvement of all stakeholders contributing to the care process, lack of willingness of organizations and individuals to learn from errors and scarce investments in patient safety improvement and research.
There is a growing need to promote systems approaches to finding solutions in healthcare to improve the safety of care, the quality of healthcare delivery, patients’ health and citizens’ well-being.
The discussion paper “Bringing a Systems Approach to Health” defines the systems approach as one “that applies scientific insights to understand the elements that influence health outcomes; models the relationships between those elements; and alters design, processes, or policies based on the resultant knowledge in order to produce better health at lower cost” [ 1 ].
A multidisciplinary approach must include the involvement of citizens and patients as fundamental contributors to the design, implementation, delivery, and evaluation of health services.
This means that citizen participation plays an essential role, bringing the unique point of view of patients and family members into the debate on patient safety and quality of care.
Patients and more generally citizens, when actively and systematically engaged, bring ideas and experiences which can support a collaborative and reciprocal learning process among the healthcare stakeholders. This produces knowledge that leads to improved practices, a real knowledge creation process where the dynamic participation of all actors in healthcare systems contribute to an active learning environment where the identification, the investigation, and the planning of solutions related to health incidents is a cyclic process enabling healthcare knowledge creation.
The added value of involving patients in healthcare is, respect to other more complex interventions, a low cost opportunity to take into consideration unconventional points of view creating and building knowledge and providing original insights and ideas that otherwise would not be considered.
Health professionals and patients’ skills and knowledge are acquired through individual experience or education and transferred to the health organizations in a perspective of co-production of healthcare. It is a merging of the efforts of those who produce and those who use the solutions to address health problems. It serves to establish a strengthened and long-term relationship in terms of trust and effectiveness and to distribute the responsibilities among all stakeholders [ 2 ].
In light of these arguments, the systems approach—inspired by the fundamentals of ergonomics and human factors (HFE)—creates new alliances between healthcare and engineering, of which patient journey is a challenging example [ 3 ].
Applying the systems approach to patient safety allows the analysis of the factors that characterize the encounters and the interactions between healthcare professionals and patients during the entire course of care. The observation of possible critical issues to the individual and specific encounter between clinician and patient is crucial in widening the scope of observation and research of the entire “journey” of the patient, taking into consideration the complexity of patient, their values and needs, their preferences, the economic and social context in which they live, and language and communication issues.
These observations and research should be carried out considering the interconnections and interactions together with the components of the processes; importance should be given to the context, and to manage the complexity, the value of a holistic approach.
2 The Patient Journey
A modern health system looks to the future in the context of the challenges imposed by the real world. It must manage the gap between guidelines and health protocols and what effectively happens and how reality is perceived by patients and family members.
It is more and more necessary to bring the patient’s point of view in the analysis of the care process, in the incident reporting and analysis, in the design and implementation of solutions and guidelines in healthcare.
Vincent and Amalberti in “Safer Healthcare” (2016) [ 4 ] stated that the incident analysis should broaden the class of events having consequences on patient safety. Incidents reported from the patient’s point of view should be included in addition to those suggested by health professionals. Additionally, when analyzing an incident, it should be done in the context of the patient journey rather than a single episode.
Instead of focusing on the individual encounter, it is necessary to extend the observation timeframe by applying the examination of contributing factors to each of the encounters that compose the patient journey (temporal series of encounters with healthcare facilities, a hospital unit, a specialist visit, a primary care clinic, a home health agency), considering both the negative and positive events and the points for improvement that were revealed (Fig. 10.1 ).
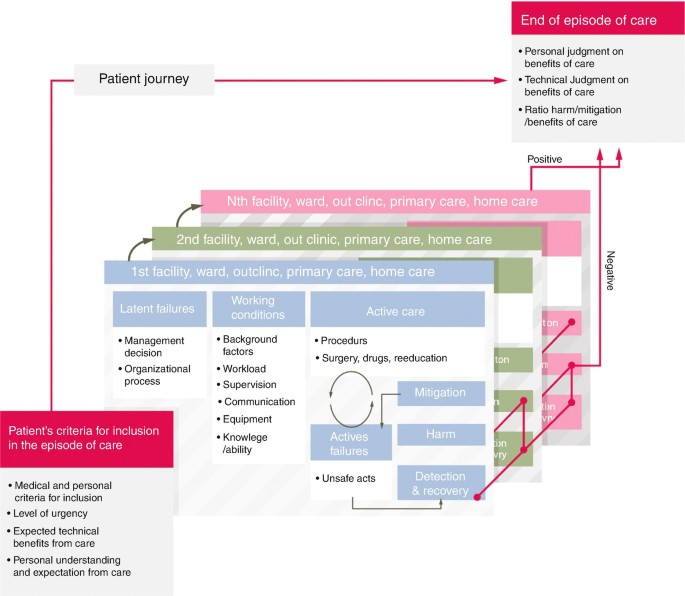
Analysis of safety along the patient journey
The adoption of this wider approach is unique in that it incorporates the patient’s perspective of safety and includes new features in the incident analysis such as asking patients to recount the episode of care, including patient and family in the investigation team when possible, asking patients the contributory factors from their point of observation and perception and involving patients and families in the reflections and comments on the disclosure process [ 4 ].
The episodes patients and families can highlight are often different from those that professionals are more accustomed to reporting. However, patients could be involved in further ways in incident reporting and assessment, and today patient-derived information constitutes a free and little used resource.
As per McCarthy’s definition, “patient journey mapping describes the patient experience, including tasks within encounters, the emotional journey, the physical journey, and the various touch points” [ 5 ]. Carayon and Woldridge define “patient journey as the spatio-temporal distribution of patients’ interactions with multiple care settings over time” [ 3 ], where at each point of touch with each healthcare service along the patient journey, the patient interacts with several system elements (task interaction, physical environment, interaction with tools and technologies, organization interaction, interaction with other organizations and other people, interaction with other people and teams within the organization) (Fig. 10.2 ).
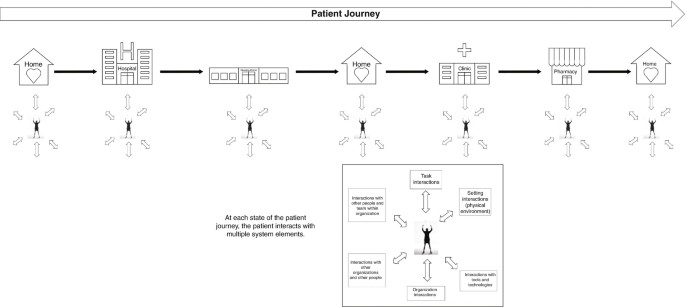
The patient journey as a set of interactions and transitions
The patient journey represents the time sequence of what happens to the patient, especially during transitions of care, in particular considering that the health professional who takes care of the patient only sees the portion of care for which he is responsible and in which he has an active role. Conversely, the patient is the only person who has a continuously active and first-hand role during their health journey. They alone are in possession of information that characterizes the entire care experience.
Moreover, when patients navigate their journey, they contact and interface with multiple work systems at several time points, where the sequence of interactions in the work systems determine the outcome experienced by patients and families, healthcare professionals, and health organizations. (Fig. 10.3 ). Each local work system is influenced by a wider socio-organizational context, which can be formal healthcare organization (such as hospital, primary care facility, nursing home) or informal (home).
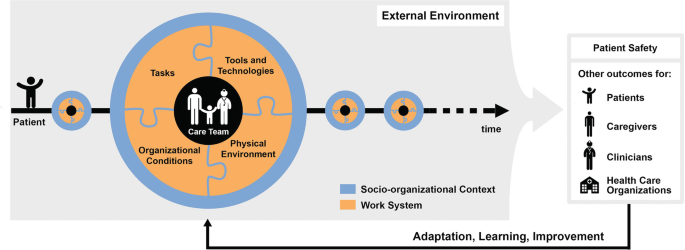
SEIPS 3.0 model: sociotechnical systems approach to patient journey and patient safety
Every point of the patient journey offers data on health outcomes and patient experience outcomes that should be used as feedback to redesign healthcare work systems in terms of adaptation, learning, improvement.
Patient’s experience represents an important resource in participatory collaborative design, especially in the patient journey where this experience is the result of multiple interactions across space and time.
3 Contextualizing Patient Safety in the Patient Journey
Many of the incidents or near-misses during healthcare are not due to serious errors, but to the combination of small failures, such as limited experience of a recently qualified doctor, use of obsolete equipment, an infection difficult to diagnose or inadequate communication within a team.
We know that the analysis of an incident requires looking back to the succession of events that have occurred and that led to the problematic episode, considering both active and latent errors, and all the aspects connected directly or indirectly. It is fundamental to examine the safety of the entire patient journey, all the encounters that make up the entire care process, to study the whole medical history of the patient in an attempt to reconstruct all the elements that characterize the “health journey”, not only from the viewpoint of the health professionals, but also from that of the patient and family.
In light of these arguments, new concepts, tools, models, and methods need to be embraced to support patient safety in the patient journey.
A significant contribution in terms of concepts, frameworks, and models is offered by Industrial and Systems Engineering, and often human factors and systems engineering (HF/SE) have an approach to include the preferences and the needs of stakeholders when designing solutions to address the critical aspects of a health process.
Human factors and ergonomics are described as “the scientific discipline concerned with the understanding of interactions among humans and other elements of a system, and the profession that applies theory, principles, data and methods to design in order to optimize human well-being and overall system performance. Practitioners of ergonomics and ergonomists contribute to the design and evaluation of tasks, jobs, products, environments and systems in order to make them compatible with the needs, abilities and limitations of people. Ergonomics helps harmonize things that interact with people in terms of people’s needs, abilities and limitations” [ 6 ].
Process models have found widespread use in drug management, visit planning, care transition, to name a few, and can offer tools and methods to investigate interprofessional and physician–patient communication, interruptions and health information handover.
Drawing from the finding of Carayon’s studies [ 3 ], the Systems Engineering Initiative for Patient Safety (SEIPS) model gives a description of five work system elements which when applied to a definite patient journey model should outline who (person) is doing what (tasks) with tool and technologies, taking into consideration the physical and organizational environment where all these activities take place. All these factors have to be examined for both patients and workers and the process analysis and modelling have to consider what patients and families/caregivers, healthcare professionals and workers actually do ( work-as-done versus work-as-imaginated ).
Patients, families, and caregivers are deeply involved in the healthcare process due to the tasks they carry out in the intermediate sectors of care between encounters. Away from direct interactions with professionals, they have to perform multiple actions requiring understanding of what behaviour to adopt, which instructions to follow, how to administer a medication and how to communicate with hospital doctors, general practitioner, and home healthcare professionals [ 3 ].
Taking into account what has been highlighted so far, one of the leading and most challenging keys to success in improving patient safety is to adopt a systems approach to patient safety which includes the patient’s perspective about their health journey throughout the time of care and across all the care settings.
This assumption highlights that patients and their families are valuable resources and can play an important role in patient safety improvement efforts. Viewing health systems as “co-producing systems”, patients can engage as partners in co-producing patient safety improvement activities individually, in groups and collectively. Individual patient and family member participation/co-production of safer care is fundamental. Equally as important is the co-management and co-governance of healthcare services, in addition to the engagement of communities in policy definition and designing activities.
In fact, patient engagement directs the design of healthcare systems towards the preferences, the values, the real-life experiences, and—not less important—the skills of the people to enhance patient safety in the patient journey.
Such a change of perspective involves multiple dimensions of interactions and relationship between patients and professionals, encompassing cooperation, dialogue and listening, trust, reciprocity and peer-to-peer work [ 2 ].
It follows that on the one hand the healthcare organizations have to demonstrate the willingness to support health professionals to effectively engage patients in the patient journey to achieve the common goal of reducing the risk of patient harm or incidents as well as the willingness to integrate patients and family members as partners into quality and safety improvement efforts. On the other hand, it is necessary to motivate and encourage patients and families/caregivers to actively participate during the individual care process for safer care as well as partner in organizational patient safety improvement efforts to ensure safer care for others.
The working group Patient and Family Involvement for the delivery of Safe and Quality Care [ 7 ] stated that the utmost priority to realize the patient involvement is the training of patients, followed by the promotion of interdisciplinary training programmes for healthcare professionals to promote patient and family engagement, the implementation of multilevel structures that allow for participatory processes by patients and smarter allocation of resources in healthcare that supports involving citizens in patient safety improvement efforts for better healthcare.
This working group was part of the activities of the “1st International Meeting about Patient safety for new generations—Florence, 31st August and 1st September 2018” organized by the Centre for Clinical Risk Management and Patient Safety, Tuscany Region—WHO Collaborating Centre for in Human Factors and Communication for the Delivery of Safe and Quality care [ 7 ].
Therefore, training for both patients/families/advocates and health professionals is a pillar on which to build active engagement of patients and consequently an effective and efficient patient journey. From this perspective, the participation of patients (i.e. representatives of patients’ associations and organizations, patient and citizen advocates) in training courses—specifically designed for this target audience of trainees and aimed to encourage co-production of care—is an essential and effective activity to co-produce a better healthcare system in terms of quality and safety of care.
Sharing a common language, promoting citizens’ and patients’ awareness of importance of co-production of care, teaching the key role that patients can play in making treatments safer (investments in health literacy), learning to work together and within a network (locally, regionally, and nationally/internationally) on priority safety and quality of care issues: these are some of the main strengths of training courses aimed to be at the basis of active engagement of patients and citizens.
Examples of successful training courses include “PartecipaSalute” and “Accademia del Cittadino” organized in Italy by Laboratory for Medical Research and Consumers Involvement of the Istituto di Ricerche Farmacologiche Mario Negri IRCCS and the Centre for Clinical Risk Management and Patient Safety, Tuscany Region. The following paragraph describes this educational experience which is specifically designed for citizens and patients to improve their knowledge and skills in patient safety and quality of care, with the aim of co-producing better healthcare services.
4 From PartecipaSalute to the Accademia del Cittadino: The Importance of Training Courses to Empower Patients
Over the last few years in the field of health and research and with regard to participation and involvement of citizens and patients, we have witnessed the transition from a paternalist to a partnership model. Individual citizens and those citizens involved in patients’ associations or groups have acquired a new role: no longer passive but actively involved in decision-making regarding health, healthcare, and research in the health field [ 8 , 9 ].
This is a progressive step-by-step process based on the recognition and implementation of the key concepts such as health literacy and empowerment. Health literacy, more properly used at individual level is defined as the capacity to obtain, read, understand, and use healthcare information in order to make appropriate health decisions and follow instructions for treatment [ 10 ]. Empowerment, more used at the community level, is a process that, starting from the acquisition of accurate knowledge and skills, enables groups to express their needs and more actively participate to request better assistance, care, and research. At this level, the availability of organized independent and evidence-based training courses is essential to allow people to be able to critically appraise and use information about the effects of healthcare interventions. Consequently, they will have the skills to participate in the multidisciplinary working groups (composed of researchers, health professionals, patient and citizen advocates, institutional representatives).
In the late 1990s, the Istituto di Ricerche Farmacologiche Mario Negri IRCCS held the first training courses of this kind focused at breast cancer associations. Some years later, within the project PartecipaSalute—a not-for-profit research project designed to foster a strategic alliance among healthcare professionals, patients, and their organizations—an ad hoc training programme for representatives of citizens’ and patients’ organizations was defined with a multimodule format [ 11 , 12 ]. This was an innovative approach, at least in the Italian setting in that period.
PartecipaSalute training programme has combined different experiences: the Mario Negri Institute IRCCS experience in collaborative research activities with patients’ associations, the Italian Cochrane Centre with the activities aimed at promoting the principles of evidence-based medicine, and Zadig long-term experience in health communication. The above promoters jointly developed the PartecipaSalute training programme on the belief that data are more important than opinions, and that every decision should be supported by well-conducted research data.
The spread of this belief to patients and citizens with the purpose of stronger involvement was a key point of PartecipaSalute training courses.
Therefore, patient, family, and community knowledge of the principles of how evidence is developed through clinical research is essential to make or support decisions in the health debate, to promote better clinical research, or to convey correct information. The strength of the PartecipaSalute programme was based on the exchange of experiences in an interactive way aimed at creating opportunities for discussion, overcoming the teacher–learner model. Each session started with an interactive discussion of a real situation—such as a screening, vaccination, therapy—and after sharing data, opinions or articles from media, evidence was presented and discussed, underlining significant methodological aspects. The programme offered the opportunity to debate the value and significance of the methodology offering critical appraisal tools. Each participant was invited to take an active part, starting from direct personal or associative experience. Table 10.1 presents the topics considered in the first three editions of the training programme. The participation was free, and different types of materials were provided including an ad hoc manual published by PartecipaSalute, copies of the PowerPoint presentation and articles.
Considering the characteristics of the programme and its modular structure, the PartecipaSalute training programme could be adapted to specific contexts. In fact, the experience of PartecipaSalute was adopted at the regional level by Regione Toscana (Centre for Clinical Risk Management and Patient Safety and the Quality of healthcare and Clinical pathways of Health Department, Tuscany Region) developing a more specific training programme called PartecipaSalute-Accademia del Cittadino (Academy of Citizen), focused on patient safety and risk management. In particular, after some modules on methods related to evidence-based medicine, uncertainties in medicine and information and communication in health, the training was mainly dedicated to regional and local activities on clinical risk management, the role of patients’ associations to improve patient safety and to support the implementation of best practices, the analysis and data of adverse events and risk assessment in terms of quality and safety in the care processes (Table 10.2 ).
The PartecipaSalute-Accademia del Cittadino joint training programme has been implemented in three editions over the last decade and has trained about 100 members of patient and citizen advocates representing 38 patients’ associations. The courses ranged from 5 to 3 modules of 2 days each in residential mode to allow participants to get to know each other and create a network of associations committed to be engaged in clinical research, quality, and healthcare safety issues.
The entire educational experience was characterized by the use of participatory training methods, based on working groups, practical exercises, lectures from experts with opportunities for discussions. As a result of this training course model, the participants were recognized as “expert patients” and were regularly involved in basic activities for promoting patient safety as auditors on significant events and helping to define policies on patient safety at the Tuscany regional level. In addition, they have participated in patient safety walkarounds in hospitals and in developing eight cartoons intended to promote the education of citizens for the prevention of the most diffused risks (such as prevention of infections, prevention of falls and handovers).
Feedback on the satisfaction on tutors, topics discussed and knowledge gained was regularly requested from participants through questionnaires distributed before and after the programme. In general, positive feedback was received; participants appreciated the interactive methods of work, the clarity of the language, and the effort to make difficult problems easy to understand. An ad hoc questionnaire was provided to the participants regarding the methodology of clinical research, always showing an improvement in the self-evaluated knowledge before and after the course. Feedback of the results of the evaluation was also shared with each participant. Most of participants reported their experience to other members of the organization. In particular, in the case of the Regione Toscana training, the possibility of immediately transferring what was learned in the course in all the activities in collaboration with the health institutions, policy makers, and health professionals—such as working groups on patient safety best practices, participation to audits, development of tools to improve health literacy—was appreciated.
Some limitations emerged from these experiences. The selection of participants is the first issue, not only because the training course is accessible to a small number of participants (in general no more than 30 participants), but also because the groups comprised of middle-aged and retired participants, with few younger ones. Additionally, there were few individual patient or family member representatives from patient associations. The majority of those representing patient associations were in managerial or leadership positions. Furthermore, it is difficult to choose between small, local, or bigger regional associations. Residential training courses also restricted the participation for geographical reasons.
The PartecipaSalute and ParteciaSalute-Accademia del Cittadino training experiences show that patients and citizens are willing to get actively involved in healthcare and the research debate. There is a real desire to improve their knowledge and skills on health and research issues and allow some general considerations regarding the active engagement of citizens representing associations and advocacy groups.
In conclusion, it is very important to invest in a process of empowerment aimed to have well-trained activists involved vigorously and constructively in the debate, design, and assessment of health and research. Switching from tokenism to active participation is necessary to effectively partner with patients and the general population to design, plan, and co-produce safer more effective healthcare, while also supporting better more patient-centred research [ 13 , 14 ].
Also, the training courses are feasible and useful, as has recently been discovered also by pharma or other groups that organize courses mainly focused on drugs and drug development, thus directing the participation of the groups more to market needs than to public health.
Furthermore, this training initiative facilitates the networking among associations in part overcoming the difficulties that derive from personalization and division among the associations representing citizens and patients.
Finally, this illustrates the importance of the design and promotion of training courses with institutions, such as the Regione Toscana, in order to be able to implement projects of real collaboration between institutions, healthcare professionals, and consumers’ and patients’ representatives.
5 Recommendations
A systemic approach to health can provide valuable models for wider implementation of patient safety. A multidisciplinary approach includes the involvement of citizens and patients as unique stakeholders in the design, implementation, delivery, and assessment of health services.
Involving patients in healthcare is an opportunity to bring uncommon points of view into policy making and to create shared knowledge between healthcare professionals and patients.
The implementation of patients’ and families’/caregivers’ perspectives in the patient journey is the golden opportunity to leverage crucial input, such as experiential knowledge, safer care, patient motivation, and trust and social cohesion into the co-production of safety solutions in healthcare. This represents a way to get closer to person-centred care, to create opportunities for patients to meet and share information and knowledge, to develop structures and policies for patient involvement at different levels (with healthcare systems, universities, and policy makers).
However, little has been done to overcome some healthcare systems barriers: the power imbalance between the doctor and patient, language differences, the lack of diffusion of non-technical skills and, last but not least, the lack of evidence about the value of patient involvement.
To be widely implemented, patient engagement in the patient journey requires courageous leadership, organizational efforts, a wider culture of safety of care, the implementation of multilevel structures for the engagement of patients and resources from smarter spending in healthcare.
Education is the landmark to integrate meaningful patient and citizen engagement in healthcare. Training of patients is the fundamental starting point to develop shared knowledge, co-produce projects, and implement an active multilevel participation of patients and families for the improvement of quality and safety of care.
Kaplan G, Bo-Linn G, Carayon P, Pronovost P, Rouse W, Reid P, Saunders R. Bringing a systems approach to health, Discussion Paper. Institute of Medicine and National Academy Engineering. 2013.
Google Scholar
Palumbo R. Contextualizing co-production of health care: a systematic literature review. Int J Public Sect Manag. 2016;29(1):72–90. https://doi.org/10.1108/IJPSM-07-2015-0125 .
Article Google Scholar
Carayon P, Wooldridge AR. Improving patient safety in the patient journey: contributions from human factors engineering. In: Smith AE, editor. Women in industrial and systems engineering. Key advances and perspective in emerging topics, Women in engineering and science, vol. 12. Cham: Springer; 2019. p. 275–99.
Vincent C, Amalberti R. Safer healthcare-strategies for the real world, vol. 5. Cham: Springer Open; 2016. p. 47–57.
Book Google Scholar
McCarthy S, O’Raghallaigh P, Woodworth S, Lim YL, Kenny LC, Adam F. An integrated patient journey mapping tool for embedding quality in healthcare service reform. J Decis Syst. 2016;25(Suppl 1):354–68. https://doi.org/10.1080/12460125.2016.1187394 .
International Ergonomics Association (IEA). Definition and domains of ergonomics. https://www.iea.cc/whats/ . Accessed 23 Dec 2019.
International Meeting about Patient safety for new medical generations—Florence, 31 Aug and 1 Sept 2018. http://iea2018.org/?page_id=4373 . Accessed 23 Dec 2019.
Castro EM, Van Regenmortel T, Vanhaecht K, Sermeus W, Van Hecke A. Patient empowerment, patient participation and patient-centeredness in hospital care: a concept analysis based on a literature review. Patient Educ Couns. 2016;99(12):1923–39. https://doi.org/10.1016/j.pec.2016.07.026 . Epub 2016 Jul 18.
Article PubMed Google Scholar
Coulter A, Ellins J. Effectiveness of strategies for informing, educating, and involving patients. Br Med J. 2007;335:24–7.
IOM. Health literacy: a prescription to end confusion. Washington DC: National Academies Press, 2004; Am J Prev Med. 2009;36(5):446–51.
Mosconi P, Colombo C, Satolli R, Liberati A. PartecipaSalute, an Italian project to involve lay people, patients’ associations and scientific-medical representatives on the health debate. Health Expect. 2007;10:194–204.
Mosconi P, Satolli R, Colombo C, Villani W. Does a consumer training work? A follow-up survey of the PartecipaSalute training programs. Health Res Policy Syst. 2012;10:27. https://doi.org/10.1186/1478-4505-10-27 .
Article PubMed PubMed Central Google Scholar
Ocloo J, Matthews R. From tokenism to empowerment: progressing patient and public involvement in healthcare improvement. BMJ Qual Saf. 2016;25:626–32. https://doi.org/10.1136/bmjqs-2015-004839 .
Chalmers I, Bracken MB, Djulbegovic B, Garattini S, Grant J, Gülmezoglu AM, Howells DW, Ioannidis JP, Oliver S. How to increase value and reduce waste when research priorities are set. Lancet. 2014;383:156–65. https://doi.org/10.1016/S0140-6736(13)62229-1 .
Download references
Author information
Authors and affiliations.
Centre for Clinical Risk Management and Patient Safety, Tuscany Region—WHO Collaborating Centre in Human Factors and Communication for the Delivery of Safe and Quality Care, Florence, Italy
Elena Beleffi
Laboratory for Medical Research and Consumers Involvement, Public Health Department, Istituto di Ricerche Farmacologiche Mario Negri IRCCS, Milan, Italy
Paola Mosconi
The Society to Improve Diagnosis in Medicine, Evanston, IL, USA
Susan Sheridan
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Elena Beleffi .
Editor information
Editors and affiliations.
London School of Hygiene and Tropical Medicine, London, UK
Liam Donaldson
Department of Hygiene and Public Health, Catholic University of the Sacred Heart, Rome, Italy
Walter Ricciardi
Italian Network for Safety in Healthcare, Florence, Italy
Riccardo Tartaglia
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Reprints and permissions
Copyright information
© 2021 The Author(s)
About this chapter
Beleffi, E., Mosconi, P., Sheridan, S. (2021). The Patient Journey. In: Donaldson, L., Ricciardi, W., Sheridan, S., Tartaglia, R. (eds) Textbook of Patient Safety and Clinical Risk Management . Springer, Cham. https://doi.org/10.1007/978-3-030-59403-9_10
Download citation
DOI : https://doi.org/10.1007/978-3-030-59403-9_10
Published : 15 December 2020
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-59402-2
Online ISBN : 978-3-030-59403-9
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Measuring the patient experience: Lessons from other industries
For hospitals and health systems, patient satisfaction is likely to become an increasingly important source of competitive advantage. Yet many providers cannot measure the patient experience comprehensively, an important first step in improving it.
Most health systems currently use a survey developed by the Centers for Medicare and Medicaid Services (CMS)—the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS)—to gauge how inpatients perceive their hospital stay as their basis for understanding patient satisfaction. While HCAHPS does provide important insights into the patient experience, it does not assess all of the important aspects of that experience. Furthermore, it was not designed to provide the level of detail needed for hospitals to link patient satisfaction with business performance.
Health systems that want to use patient satisfaction as a way to improve business performance need additional feedback and data to identify the factors that matter most to the patients they serve. Armed with the combined information, the health systems can then determine which investments in improving the patient experience can best help them meet their business objectives.
In this article, we describe a comprehensive approach health systems can use to better understand the patient experience and thereby improve patient satisfaction. This approach is based on the experience of companies in other industries that were able to markedly improve customer satisfaction levels.
Lessons from other industries
In other industries, high customer satisfaction levels have been linked with stronger loyalty, sales, and profits. McKinsey research in multiple industries has shown that companies that routinely achieve high customer satisfaction scores rely on best-practice measurement systems that:
- Link improvements in the customer experience with desired business outcomes (e.g., repeat sales)
- Enable the companies to identify the most important drivers of customer satisfaction and measure ongoing performance in those areas
- Uncover operational insights that enable the frontline staff to make continuous improvements in the customer experience
Applying these lessons in health systems
To date, few health systems have achieved significant business results through patient-experience initiatives. Yet, growing consumerism in the healthcare industry—a result of higher deductibles and copayments, network narrowing, and greater transparency into provider performance and costs—is likely to make patient-experience initiatives more of an imperative for the industry. The proliferation of provider-led health plans is also making it increasingly important for health systems to market themselves, and patient satisfaction could be a key differentiator in their marketing efforts.
The steps outlined below can enable providers to adapt best practices from other industries to the healthcare environment.
Link patient satisfaction to business outcomes
The first step for health systems is to determine the business outcomes they most want to focus on (e.g., total patient volume, patient retention, percentage of commercial patients). They should then conduct research to investigate the types of questions that will best enable them to gauge patient satisfaction in a way that ties into those objectives. For example, a major US health insurer discovered that customer agreement with the phrase “[company name] is the insurer for me” predicted loyalty in one of its most important member segments better than agreement with any other phrase did. Because member retention in that segment was one of its business objectives, the insurer then focused its efforts on how to increase the percentage of people in that segment who agreed with the phrase.
Next, health systems should conduct additional research to identify the factors that most strongly influence how patients respond to the chosen questions and the specific metrics that would enable them to assess performance in those areas. Over time, the combined data should permit the health systems to develop robust measurement systems that can uncover operational insights and enable continuous frontline improvements. To ensure that the measurement systems remain robust, health systems should repeat this fundamental research every few years so that their understanding of the patient experience is always current.
Identify the strongest influences on patient satisfaction
To determine which factors most strongly influence patient satisfaction, health systems must accurately understand the end-to-end inpatient journey, from pre-admission scheduling and testing through to follow-up care, as well as the role that price, service offerings, physician referrals, and brand play in determining where patients seek care (Exhibit 1).
The inpatient journey should then be broken down into discrete elements to identify the factors that can influence patient satisfaction at each step of the journey. Both clinical and nonclinical factors should be included. In-depth qualitative research (e.g., focus groups) and quantitative research (e.g., patient surveys) should then be conducted to pinpoint which factors most strongly influence satisfaction levels in ways that correlate with desired business objectives.
When conducting this research, two points are worth remembering. First, the factors with the strongest influence often vary by market and patient segment (e.g., expectant mothers, cardiovascular patients, emergency room patients). Thus, the journeys along different care pathways should be mapped separately to determine which factors influence each one. For example, a hospital in a competitive community that views its maternity services as a way to attract and retain patients would need to understand which elements of care during pregnancy, childbirth, and follow-up have the strongest impact on new mothers’ satisfaction levels.
Second, what patients say is important to them may not correlate with how satisfied they actually were with their inpatient stay. In our 2014 Consumer Health Insights Survey, for example, we asked the participants who reported having been hospitalized within the past three years to tell us which factors were most important in influencing their satisfaction with their hospital experience. We then compared those responses with the participants’ reported satisfaction levels to determine the relative (or derived) importance of each factor (Exhibit 2). The match-up was inexact. For example, most participants said that the outcome achieved was the strongest determinant of their satisfaction with care. However, empathy from nurses turned out to have a greater impact on actual satisfaction levels. Health systems need to understand the derived importance of various factors if they want to ensure that their improvement efforts yield significant results.
This type of careful qualitative and quantitative research can help health systems avoid costly errors. In our experience, many health systems make large investments to improve the patient experience but fail to achieve their desired objectives because they did not understand what really matters most to their patients. Leading customer-focused companies rarely make this mistake. For example, a major rental car company conducted interviews and surveys to improve the experience of business travelers, its most profitable customer segment. The research established that the most important source of satisfaction for these travelers was not the variety of vehicles (as the company had hypothesized), but the experience from landing at an airport to leaving the rental facility. The research also showed that the key elements influencing that experience were the speed of getting the rental car and communication about the status of the reservations before arrival. As a result, the company invested to streamline the arrival process and used technology to give customers frequent updates. The result: higher retention of business travelers.
HCAHPS: Overview
Since 2006, CMS has supported US hospitals in administering the 27-question HCAHPS survey, which asks patients to rate their experience on several dimensions (e.g., communication with doctors, cleanliness of the hospital environment). CMS then publishes the results online. Beginning in fiscal year 2013, CMS has also used each hospital’s aggregate HCAHPS score to reward top performers and penalize underperformers, putting almost $1 billion of reimbursement at stake. 1
At most providers, HCAHPS has increased the management teams’ focus on the patient experience and helped them begin to understand patients’ perspectives. HCAHPS has also allowed both the management teams and patients to compare how well different hospitals perform on patient experience. The McKinsey Consumer Health Insights Survey has shown that most consumers now say that rating sites are at least “somewhat important” when choosing a provider, but how often the scores actually influence a patient’s choice of provider remains unclear.
However, HCAHPS was not designed to link the patient experience with a hospital’s financial performance, and our analyses show that HCAHPS scores do not correlate strongly with financial metrics. For example, there is little correlation between HCAHPS scores and net revenue, inpatient gross revenue, or the percentage of patients with commercial insurance. Furthermore, researchers have found that the evidence linking HCAHPS scores with clinical outcomes is inconclusive. 2,3
The low correlation between HCAHPS scores and financial and clinical outcomes most likely reflects the fact that the survey does not investigate a number of factors that, our research suggests, may be strong determinants of patient satisfaction. Some of these affect the inpatient experience (e.g., keeping patients informed about the results of treatment); others occur before or after the inpatient stay (e.g., pre-admission testing and outpatient follow-up).
Thus, improving HCAHPS scores may help health systems increase their CMS reimbursement (and avoid penalties), but it may not enable them to achieve all of their other goals for patient satisfaction initiatives, such as increased volume. Therefore, they should undertake additional measures that complement their HCAHPS efforts so they can improve their performance in areas that could lead to increased loyalty, referrals, and profitable patient volume.
Uncover operational insights
As the car rental company example illustrated, it is not sufficient to identify the factors that matter most. Those factors must be broken down into their constituent parts—ideally, ones that can be monitored regularly. For example, if nurse empathy has a strong impact on patient satisfaction, health systems should track such things as total nursing time spent with each patient and timely response to call buttons. Similarly, if the most important factor influencing satisfaction with ER care is how quickly patients see a provider, health systems should routinely measure the average “door to doc” time.
Metrics such as these become key performance indicators (KPIs) that can be used to change behaviors in ways that improve the patient experience. The KPIs should, ideally, be assessed daily and results reported to the individual hospital units. The findings help the frontline staff determine where changes are needed and then test the changes to understand the impact they are achieving. The KPIs are thus an important complement to the monthly patient feedback survey scores. Although those surveys are the most important gauge of patient satisfaction, it may take weeks before the responses are processed and reported to the frontline. In contrast, the KPIs allow the staff to make meaningful, real-time adjustments to their activities and weave continuous improvement into daily operations. As a consequence, patient satisfaction is no longer just a marketing initiative but a component of the organization’s culture.
Leading customer-service companies have long used this approach. For example, a large consumer bank discovered that one of the primary factors influencing its customers’ satisfaction was how quickly it could respond to service disruptions; the speed with which its call center agents completed calls about disrupted service was an important subcomponent. The bank therefore began to track the average time call center agents spent handling these calls daily as a first step in improving its ability to address service disruptions.
Improving the patient experience can help health systems achieve their business objectives as well as increase their Medicare revenue. In some cases, it could also have spill-over effects, such as better clinical care delivery. The steps outlined above can help health systems deepen their understanding of the patient experience and identify the most effective ways to increase patient satisfaction.
Download the full article (PDF)
- Centers for Medicare and Medicaid Services. National provider call: Hospital value-based purchasing – FY 2013 actual percentage payment summary report. October 4, 2012.
- Isaac T et al. The relationship between patients’ perception of care and measures of hospital quality and safety. Health Services Research . 2010; 45(4): 1024–40.
- Rodak S. Improving HCAHPS scores alone is not the answer: Hospitals need a patient-centric foundation. Becker’s Infection Control & Clinical Quality . January 7, 2013.

- Proposed platform, app aim to improve life quality in Parkinson’s
ParkProReakt project working to create 'digital solution' for patients

by Mary Chapman | May 8, 2024
Share this article:

Scientists at the Fraunhofer Institute for Applied Information Technology (FIT) in Germany are collaborating on a project with the aim of creating a digital platform and application that, used with a wearable device, can track the course of Parkinson’s disease and potentially improve patients’ quality of life.
Called ParkProReakt and involving 10 partners, the project is slated to run through next year and is coordinated by a Philipps University of Marburg neurology team. About 400,000 people in Germany are living with Parkinson’s, according to a Fraunhofer FIT press release , and for many, “getting to the doctor’s office is a challenge,” meaning that “new symptoms often go unrecognized by patients and their loved ones.”
The partners aim to develop a web platform and smartphone app, dubbed Active PD, that pairs with an Apple Watch via Bluetooth, facilitating communication between Parkinson’s patients and their healthcare professionals. Data collected through the app would be transmitted to the platform and available to patients’ doctors.
The overarching aim is to improve patient care and mitigate the burden on caregivers, with both, or either, using the tool to help assess changes that occur throughout the course of the progressive neurodegenerative disease. The platform’s goal is to foster communication between patients and doctors, enable regular checkups, and permit patients to receive self-help support, all designed to improve quality of life in Parkinson’s. The app will allow certain patient values to be tracked and transmitted directly to the patient’s physician. Rather than awaiting new information, doctors can react to the smallest clinical deviations.
“We hope our digital solution will give providers a better window on patients’ day-to-day lives and have a positive impact on their quality of life,” said Daniel Wolferts, a scientist at Fraunhofer FIT.

Study explores factors that shape patients’ quality of life
Active pd platform, app would track parkinson’s, help improve quality of life.
Because each patient journey is different, regular monitoring in Parkinson’s disease can allow for quicker interventions. However, such monitoring, and routine patient examinations, can be difficult to facilitate, especially for those in rural areas. Consequently, according to the researchers, patients may only be seen by their treatment teams every six months or at even longer intervals.
The Active PD concept is undergoing validation testing in a clinical study with 170 patients over six months. In the trial, the intervention group will use the digital tool, while a control group will receive conventional treatment with no technological device. The patients are asked to complete standardized Parkinson’s-related tests twice weekly using the app and watch, which records their movements through sensors.
The tests focus on patient motor skills and overall condition, helping doctors and other healthcare team members to better assess their Parkinson’ symptoms and respond quickly. For example, patients are asked to perform finger exercises in front of the mobile phone’s camera, tapping their thumb and index finger together as quickly as they can several times consecutively. During the test, an image recognition feature detects the two digits and measures the distance between them. An additional exercise has the patient opening and closing a fist rapidly several times.
“Parkinson’s patients have a hard time making these movements quickly and fluidly due to the disease,” Wolferts said.
The study also calls for the employment of sensors to determine whether patients can hold one of their hands still for a certain period without trembling, which can be a challenge in Parkinson’s.
To allow emotional support to be provided as needed, participants must answer questions about their overall wellbeing. Escalating color codes of green, yellow, and red are used to alert the physician if a patient’s condition dramatically worsens. The app may also be used to report patient falls and other incidents.
Wolferts and his team are tasked with designing a user-friendly website and app, currently in the prototype stage.
How do we visualize the data in both applications in a user-friendly way for all the different groups concerned? … How can we make it so patients can undergo the necessary testing and examinations right on their phone without facing too big a motor challenge? Those are the kinds of questions we’re working on.
“How do we design an app for Parkinson’s patients, and what kind of information do these people want to get? How do we visualize the data in both applications in a user-friendly way for all the different groups concerned, and how do we meet the requirements most effectively? How can we make it so patients can undergo the necessary testing and examinations right on their phone without facing too big a motor challenge? Those are the kinds of questions we’re working on,” Wolferts said.
The project’s end goal is to create a cross-sector care model that’s “proactive, demand-driven, [and] follows a holistic approach,” connecting patients and caregivers with their healthcare team, including any specialists. All would be able to communicate together via the digital platform.
“If we’re successful, we might also ultimately be able to expand the concept to cover other neurological diseases,” Wolferts said.
About the Author

Recent Posts
- Deep brain stimulation surgery was life-changing for my husband
- STEM-PD Phase 1 trial advances with positive early safety findings
- Phase 1 trial in Sweden to test IRL757 for neurological apathy
- Phase 1/2a trial of NK cell therapy SNK01 wins FDA clearance
Recommended reading
DBS for Parkinson’s better than meds alone for quality of life: Study
Study: Clinicians must act to ease stigma of Parkinson’s disease
Lcig, dbs show quality of life gains, symptom easing: real-world study, subscribe to our newsletter.
Get regular updates to your inbox.

David Vakhtangishvili of Andromeda Health on How Tech-Driven Transformation Meets Modern Patient Expectations in Healthcare
T he evolution of consumer expectations mirrors the rapid advancement of technology. No longer content with passive, one-size-fits-all experiences, modern consumers demand personalized, seamless, and user-friendly services that cater to their unique needs and preferences. The COVID-19 pandemic further amplified this trend, with patients becoming increasingly discerning about the quality of care they receive and how it is delivered.
David Vakhtangishvili , with his rich background in healthcare technology, has keenly observed and responded to these changing dynamics. With a career spanning over two decades, Vakhtangishvili has actively participated in this transformation, using technology to bridge the gap between traditional healthcare delivery and modern patient expectations.
His latest venture, Andromeda Health, exemplifies the use of advanced technologies to bridge the gap between patient expectations and industry capabilities.
Patient Expectations in the Digital Age
With the rise of more sophisticated technologies, patients have grown accustomed to the convenience and personalization offered by consumer-centric services across various industries. This shift in mindset has permeated the healthcare sector, with patients seeking a more streamlined and tailored approach to managing their health and wellness.
"Patients are no longer passive recipients of care," explains Vakhtangishvili. "They want to be active participants in their healthcare journey, with access to real-time information, seamless communication, and a user-friendly experience."
This evolution in patient expectations has exposed inefficiencies within the traditional healthcare system. Fragmented processes, long wait times, complex insurance processes, jumping from one source to another, and lack of personalized care often hinder optimal care delivery. These challenges have prompted a transformation prioritizing patient convenience and accessibility.
How Technology Responded
In response to the previously mentioned expectations of modern patients, technology and health experts have collaborated to develop innovative solutions that enhance the healthcare experience.
Vakhtangishvili explains that this innovation drive primarily focuses on creating more patient-centric services. These were done to meet medical needs and provide convenience and seamless interaction across various healthcare processes.
In the U.S., advancements in telemedicine have dramatically expanded access to care, allowing patients to consult with physicians from the comfort of their homes. Furthermore, wearable technology enables continuous health condition monitoring, providing crucial real-time data for disease management and prevention.
Mobile health applications (mHealth apps) have also emerged, allowing patients to manage their health freely and control it by providing personalized tracking, reminders, and educational resources. From monitoring vital signs and medication adherence to facilitating communication with healthcare providers, mHealth apps have revolutionized how patients engage with their healthcare journey.
“Technology has emerged as a key player in addressing these modern expectations, ” Vakhtangishvili mentions. “ Whether it be telemedicine or AI-driven diagnostics, innovations are making healthcare more accessible and personalized.”
Andromeda Health: A Case Study in Innovation
As a veteran in the healthcare industry, from leading Georgian Healthcare Group to now pioneering Andromeda Health, Vakhtangishvili has actively contributed to the industry's transformation.
Recognizing the fragmentation and inefficiencies within the traditional healthcare system, he designed Andromeda Health to streamline and integrate various components of healthcare delivery in one platform.
Andromeda Health is a comprehensive digital healthcare platform connecting doctors, clinics, hospitals, insurance providers, pharmacies, and laboratories into a cohesive virtual ecosystem.
Vakhtangishvili believes that consolidating these disparate core elements of the patient journey unburdens patients and users from needing to jump from one platform to another to fulfil all their medical needs. With Andromeda Health, they can receive an uninterrupted and seamless patient journey, addressing the modern consumer's demand for efficiency and convenience.
Playing upon artificial intelligence (AI) and automation technologies, Andromeda Health introduces solutions like AERIES (Automated Enhanced Real-time Insurance Eligibility Solution) and AERIPAS (Automated Enhanced Real-time Insurance Prior Authorizations Solution). The latter streamlines the often-cumbersome process of insurance verification.
Vakhtangishvili explains that AERIES and AERIPAS enhance operational efficiency and ensure timely access to care for patients. This empowers patients and healthcare providers by automating administrative tasks, facilitating seamless data exchange, and enabling real-time communication and collaboration.
As a fully integrated, cross-border, and cross-silos one-stop shop, Vakhtangishvili ensured its robustness by catering to multiple patient requests simultaneously without the fear of lagging or service interruption.
“Andromeda Health represents a significant leap forward in healthcare technology, ” Vakhtangishvili asserts. “ Our team believes we can profoundly change the healthcare ecosystem with the right technologies, proper business models, and operational excellence. Being a singularity solution, not only do we build a borderless marketplace in its front end that provides a true shop-around experience for ultimate end-users, the patients. We also help all involved businesses (payers, providers, rev-cycle companies, and retailers) increase their efficiency and throughput, reduce costs, and grow revenues, simultaneously. And, finally, all of this is done in a Tier 4 cyber security cloud infrastructure, safely and uninterruptedly."
The Journey for More
Despite the advancement of U.S. healthcare technology that Andromeda Health represents, Vakhtangishvili believes this is just the beginning. He recognizes that pursuing healthcare innovation not just for him but for the whole industry is an ongoing process. Technology and patient needs are changing, thus, there is always room for further improvement and growth.
With experts like Vakhtangishvili, U.S. healthcare technology will not stagnate but will continuously move forward, driven by a pursuit of solutions that strike a harmonious balance between cutting-edge technology and the human touch.
The ultimate goal is to create customer-centric solutions that leverage the power of technology as an ally, enhancing the healthcare experience while preserving the essential human elements of compassion, empathy, and personalized care.

A Physician’s Journey into the Minds of Coma Patients
In studying people with severe brain injuries, Columbia neurologist Jan Claassen hopes to better identify those likely to regain consciousness.
Nick LaRock was going to pull through . Physically, at least.
A thirty-three-year-old high-school history teacher, LaRock had been discovered by his girlfriend sprawled out on the floor of his Manhattan apartment late one Sunday evening, moaning incomprehensibly. Rushed by ambulance to Columbia University Irving Medical Center, Columbia’s shared medical campus with NewYork-Presbyterian Hospital, he arrived unconscious and unresponsive, fighting for his life. Doctors in the neurocritical-care unit recognized that LaRock had suffered a massive brain hemorrhage and took extraordinary measures to save him, even bringing in surgeons to drill a hole in his skull to relieve pressure that threatened to irreparably damage his brain. Their efforts paid off. A few days later, LaRock was stable but in a coma, his motionless body surrounded by a humming nest of life-support machines that regulated his breathing and other vital functions.
Now, looking back on that time in January 2021, LaRock’s parents recall the relief they felt at learning that Nick would survive, but also the troubling questions that soon weighed on them. “I remember asking one of the doctors, ‘Are we past the point where he’s going to die?’ and she said, ‘Yes, I think so.’ That was obviously a big moment for us,” says Joseph LaRock, Nick’s father. “Of course, you’re next wondering, When is he going to wake up? And what is he going to be like when he does?” says Beth LaRock, Nick’s mother. “I mean, is he still going to be our Nick? Is he still going to be my boy, or is he going to be a shell of himself?”
Nick’s parents couldn’t bring themselves to ask the doctors those questions. Afraid of the answers they might receive, they distracted themselves by searching for clues that their son might be mentally present. Every morning, having driven three hours from their home on Long Island, where Joe works as a restaurant manager and Beth runs a program for adults with developmental disabilities, they would slip quietly into their son’s room, kiss him on the forehead, and perch themselves on chairs beside his bed. They would stroke his chilly hands, whisper reassurances, and wait for any glint of recognition — a tilt of the head, the flutter of an eyelid, the squeeze of a finger. When these signs didn’t come, they would talk to him nonetheless. “I would give him updates about his younger sister, my job at the restaurant, the New York Jets, the weather — anything I could think of,” says Joe. “I’d tell him that we knew he was in there. And that we needed him back.”
By any standard neurological assessment, their son’s prospects for recovery did not look good. Nick had experienced immense bleeding in his brain and now, nearly a week later, had still not opened his eyes. He appeared to be slipping into a long-term coma — a state that few patients with brain injuries ever awaken from with their personalities and mental faculties intact. “Nick’s injury was severe, and time was not on his side,” says Jan Claassen , a Columbia neurologist who directs CUIMC’s neurocritical-care unit and helped coordinate Nick’s treatment.

The longer a patient remains unresponsive, Claassen explains, the less likely they will achieve a good cognitive recovery, if they do awaken. Instead, they might emerge in a semiconscious, cognitively diminished state, requiring round-the-clock care. Many such patients spend the rest of their days hooked up to ventilators and feeding tubes, battling respiratory and urinary-tract infections. “If a person doesn’t regain consciousness within a week or two, we get very concerned,” Claassen says, noting that brain-injured patients who don’t awaken within that time frame are often taken off life support to prevent their prolonged suffering.
Yet Claassen, who is a leading authority on brain injuries, also believes that not all coma patients are as mentally incapacitated as they appear to be. At the time of Nick’s injury, he was conducting an unusual clinical trial at CUIMC in which every brain-injured patient who seemed to be in a coma was, with their family’s permission, given a series of sophisticated tests designed to reassess their brain function.
Joe and Beth LaRock agreed to have Nick evaluated. They were told that the results of the test would not inform Nick’s care, since the technique was experimental, but that his participation could eventually help others. So once or twice a day, in the morning and afternoon, members of Claassen’s research team gently put earbuds into Nick’s ears and played a series of recorded messages that asked him to perform simple physical tasks, like squeezing and relaxing his right hand. A collection of electroencephalogram (EEG) sensors stuck to Nick’s scalp then recorded the electrical pops and crackles of his neurons, which were transmitted to a supercomputer located down the hall. There a team of Columbia data scientists and biostatisticians would analyze the millions of resulting data points using an artificial-intelligence program, looking for clues that Nick might have heard the commands, understood them, and attempted to respond. Gradually, a pattern emerged. The computer detected what no neurologist could have: Nick was in there .
The word “coma” is derived from the ancient Greek koma , meaning deep sleep, but the condition that it describes — a prolonged state of unconsciousness caused by injury or illness — has only become common in the modern era. Before the mid-twentieth century, most people who experienced severe brain injuries, whether from strokes, oxygen deprivation, or blows to the head, quickly died. That is because the brain, when traumatized, loses its ability to coordinate essential bodily functions. Most critically, it stops transmitting motor signals that control reflexive muscle movements, including those in the diaphragm that draw air into the lungs; without them, a person asphyxiates. Only when mechanical ventilators became widely available in hospitals, in the 1950s and 1960s — a development inspired by the polio epidemic — did it become possible to sustain large numbers of brain-injured patients in comas. “Around then, modern emergency medical services also proliferated,” says Claassen, “which meant that people could be stabilized at the scene of injury and transported to hospitals quickly enough to be saved by the new equipment.”
Soon the study of brain injuries was among the most rapidly evolving and intellectually vibrant areas in medicine. By carefully observing patients who emerged from comas, physicians discovered previously unknown “disorders of consciousness,” including the vegetative state, a condition in which patients may open their eyes but are otherwise unresponsive and unaware; and the minimally conscious state, in which they may show intermittent awareness and attempts at communication. These disorders were initially thought to be chronic, but researchers eventually realized that some patients improved over time, which contributed to a new understanding of the brain’s capacity for reorganization, repair, and regeneration. There were other surprises too. In the 1960s, the American neurologists Fred Plum and Jerome Posner noticed that a tiny percentage of patients who appeared to be in a vegetative state were actually fully conscious and intellectually intact. Paralyzed except for their eyes, they could not respond to their examiners and so had been written off as mentally vacant. Plum and Posner called the condition “locked-in syndrome.” These patients could be taught to communicate by blinking and glancing from side to side — a method that the French journalist Jean-Dominique Bauby famously used to dictate his 1997 memoir about living with the syndrome, The Diving Bell and the Butterfly . Neurologists say that the discovery of locked-in syndrome had a profound impact on their field, impressing upon clinicians the need to be exceptionally vigilant when conducting exams, lest they miss the desperate human peering back into their penlights.
“I was taught that someone who remained in a coma for more than just a couple of days after a brain injury was basically hopeless. But I saw for myself that wasn’t true.”
Claassen, who grew up outside Cologne, Germany, began his career at the University of Hamburg’s teaching hospital, caring for coma patients, in the late 1990s. At that time, he recalls, neurologists who treated people in the earliest stages of brain injury had to be masters of improvisation. Because only a few decades of clinical history had been amassed on the topic, doctors received little guidance from textbooks or senior colleagues on important matters such as how to improve a comatose patient’s chances for recovery or when to speak with family members about the possibility of withdrawing life support. Those clinical guideposts that did exist, Claassen says, often underestimated patients’ prospects. “As a young doctor, I was taught that someone who remained in a coma for more than just a couple of days after a brain injury was basically hopeless,” says Claassen, a tall and slender fifty-five-year-old with piercing blue eyes and a gentle demeanor. “But I saw for myself that wasn’t true.”
Despite the stressful, fast-paced, and sometimes chaotic nature of his work — the nonstop decisions about continuing or withdrawing life support, in particular, are said to contribute to high rates of burnout among doctors in neurocritical-care units — Claassen thrived, seeing endless opportunities to advance both clinical care and scientific knowledge. “I’ll never forget the first time I saw a patient who’d appeared to be lost forever wake up,” he says. “One day he was completely unresponsive, and the next time I saw him he was sitting at a table playing cards. There was something about that transformation that left me awestruck. I knew I had to devote my life to helping these people. And I had to learn everything possible about what their experiences revealed about human consciousness — what it is, why it breaks down, and how it can arise again.”
In Hamburg, Claassen dove into clinical research, exploring new ways of diagnosing and assessing the severity of brain injuries. He came to CUIMC in 1999, lured in part by the medical center’s embrace of new electrophysiological and neuroimaging technologies that he believed were poised to revolutionize his field. For example, physicians in Columbia’s neurocritical-care unit had just begun to use computational analysis of EEG signals to peer inside patients’ brains in real time and better diagnose and treat their injuries. They had also started to compile an unusually large database of patient outcomes, which they studied for insights into the effectiveness of their treatments. “I thought this was critically important, because although we’d gotten very, very good at saving the lives of people who’d suffered brain injuries, we still knew little about how to improve their chances of having a good recovery,” Claassen says. “To make progress, we had to observe the brain in new ways.”
Over the next few years, Claassen achieved a number of breakthroughs using EEG and other brain-monitoring techniques. In one series of influential studies, he and colleagues discovered that some comatose patients experience life-threatening brain seizures that are only detectable with EEG. They showed that administering anti-seizure drugs to these patients may save their lives. In a related line of research, Claassen’s team demonstrated that miniaturized EEG sensors implanted in the heads of coma patients can help identify when they need interventions to adjust their blood pressure, oxygen levels, and other vitals. Many of the protocols that the Columbia team developed are now followed by physicians around the world.
In 2014, Claassen was named the head of CUIMC’s neurocritical-care unit, an eighteen-bed facility that treats all types of brain injuries, from strokes to blunt traumas to side effects of heart attacks. He quickly set about expanding its research operations, hiring data scientists, investing in supercomputing technology, and encouraging its physicians to innovate whenever possible. “We also cultivated partnerships with faculty in other Columbia units, including the Department of Biomedical Informatics, the Department of Neurological Surgery, and the Data Science Institute,” he says. “I thought that if we brought the full weight of the University’s intellectual resources to bear on studying brain injuries, we could really move the needle on the quality of care that’s available.”
Claassen soon saw an opportunity to make a big impact. Around the time he was appointed chief of the neurocritical-care unit, the field of neurology was abuzz with speculation about several anomalous case studies that had cropped up in the medical literature. The cases all involved patients who appeared to be unconscious but whose brain activity suggested they were alert. One British woman diagnosed as being in a vegetative state was slid into a functional magnetic resonance imaging (fMRI) machine and asked to imagine that she was swinging a tennis racket. She exhibited patterns of neuronal activity that indicated that she was enthusiastically playing along. Similar results were found in others who had suffered different types of brain injuries and since shown no outward signs of awareness. The neurologists behind the accounts had given the phenomenon a name — “covert consciousness” — but knew little about it.
“Some compared it to locked-in syndrome, except that these patients couldn’t even move their eyes, so they seemed to be really locked in,” says Claassen. “Which is obviously terrifying.”
But how conscious were these people, exactly? Were they fully aware of themselves and their surroundings or only faintly so? And how common was the phenomenon?
Many neurologists were skeptical that it would be possible to gain a proper understanding of covert consciousness because of practical constraints. The fMRI scanner, which produces highly detailed brain images and was therefore the first choice of many scientists studying the condition, was only suitable for observing small numbers of patients with severe brain injuries. People hooked up to life-support machines and those with metal implants could not easily go into the scanner. Meanwhile, an EEG, although easier to administer, was seen as poorly suited to detecting signs of covert consciousness in bustling hospital settings, where its sensors tended to pick up stray electrical signals from other medical equipment.
“You can deal with that kind of electrical interference pretty easily when using EEG to observe broad patterns of neuronal activity, which is how the tool has traditionally been used, but if you’re attempting to observe a person’s individual thoughts, as when looking for signs of covert consciousness, it would be more difficult,” says Claassen. “Then you’d face a serious analytic challenge.”
Yet as someone who had been working with EEG his entire career and knew its strengths and limitations, Claassen thought that he could adapt the technology for this purpose. He saw advantages in using the relatively cheap tool, which was widely available in hospitals around the world. “If we developed a test that worked, we wanted patients everywhere to have access to it,” says Claassen, noting that he drew inspiration from earlier research by Cornell neurologist Nicholas Schiff, who had shown that EEG could be used to detect covert consciousness in quieter settings. So in the summer of 2014, Claassen and his colleagues launched the first major effort to identify people with the condition in a neurocritical-care unit.
On a recent Thursday morning, in a small, sparsely furnished office in CUIMC’s neurology department, Qi Shen, a Columbia data scientist, is looking at two large computer screens. Her eyes dart back and forth between the brightly colored digital images of human brains. “Most of the time, it’s like we’re looking into mist,” says Shen, who is a member of Claassen’s research team. “And then if we’re persistent, we may see a picture emerge — very faintly at first. We can then examine the data in many different ways to determine if we’re truly detecting a signal amidst the noise.”
The signal that Shen is hunting for? Consider it the shadow of a human thought. It will appear as a distinct and consistent difference in the levels of neuronal activity in various brain regions as a person hears commands played for them over headphones. For someone who is conscious but immobile, this could be an attempt at communication. A tiny salutation back from the void.
“We’re looking specifically at regions that are responsible for higher cognitive functions, including language comprehension, to make sure we’re detecting signals that represent active engagement with the stimuli,” says Claassen, who is seated beside Shen.
This work is challenging in part because of the brain’s sheer complexity. Even when it is injured and functioning at a reduced level, its hundred billion neurons are still firing constantly. The imprecision of EEG sensors adds to the challenge. “They’ll detect electrical activity in brain regions other than the ones we’re interested in and even in other parts of the body, including the heart,” says Claassen. “We need to do a lot of creative analytics to weed out artifacts from our data.”

Despite these challenges, Claassen’s team has managed to produce the most detailed descriptions to date of covert consciousness in acutely brain-injured patients. This research, based on observations of hundreds of CUIMC patients and published in numerous papers, suggests that the phenomenon is real, surprisingly common, and a useful indicator of a patient’s potential for recovery.
“We’re still a couple of years away from incorporating this into practice, because our technology needs fine-tuning,” Claassen says, “but we’ve certainly demonstrated that covert consciousness is a major clinical concern and that detecting it has great potential to guide patient care.”
The Columbia researchers’ first big discovery on the topic came in 2019, when they showed that about 15 percent of brain-injured patients in comas exhibit signs of covert consciousness, which is also known as cognitive-motor dissociation, or CMD. They also found that these patients are much more likely to awaken from a coma and achieve a robust recovery. Then last year they found evidence that covert consciousness is caused by a communication breakdown between the brain regions responsible for higher-order cognition and the brain regions that control muscle movement.
Still, major questions remain unanswered. Claassen’s team has yet to determine, for example, the level of consciousness of the patients who respond to their commands. The scientists can only say for certain that these patients are sufficiently aware to distinguish between prompts like “start opening and closing your right hand” and “stop opening and closing your right hand.” The Columbia scientists have attempted to communicate with these patients in more meaningful ways, inviting them to open or close their hands to convey meaning in the style of Morse code, but the results so far are difficult to interpret. “We’re not sure if they’re cognitively incapable of participating in a higher-level interaction or if something else might be getting in the way — like they’re confused, distracted, or simply frustrated,” says Ángela Velázquez, a Columbia physician involved in the project. “But we’re continuing to improve our methods and remain optimistic that we may reach them.”
Claassen says that he has spoken to patients who regained their mental faculties after testing positive for covert consciousness, and he’s found that so far none can recall their time in the neurocritical-care unit. From Claassen’s perspective, this is a mixed blessing. “Of course, it’s fortunate that they don’t seem to remember a possibly traumatic experience,” he says. “On the other hand, it means that this phenomenon remains a mystery, a black box that we cannot peer into.” He still operates on the assumption that some coma patients may be fully conscious and that memories could be formed. “The human mind is very adept at blocking out terrible experiences,” he says. “That certainly could be happening here.”
Joseph J. Fins, a Cornell physician and medical ethicist who has written extensively about covert consciousness, says that the prevailing opinion among scientists who study the phenomenon is that people who test positive for it likely possess a wide range of cognitive abilities. “I think it’s possible that some of these patients are fully aware, others barely awake, and still others somewhere in between,” he says. “Clearly it’s a moral imperative for us to try to reach them if possible.”
Today, the Columbia researchers are pressing forward in their attempts to make contact with patients who are unresponsive. Their most ambitious plan is to develop a brain–computer interface similar to those that have been used to decode the thoughts of paralyzed people and to help them control keyboards and other communication devices. Claassen imagines that such a technology, by detecting distinct patterns of brain activity, could enable patients to answer yes-or-no questions and even summon hospital staff when they need help. “Are they in pain, uncomfortable, feeling hot or cold, or extremely anxious?” he says. “Being able to express themselves would dramatically improve the care we provide and make them feel less isolated.”
The scientists are also fine-tuning their EEG test to make it more accurate. For now their methods are adequate for studying covert consciousness and estimating its prevalence but not for informing the care of individual patients. For example, people who are conscious but unable to comprehend language — a common result of brain injuries — will slip through the cracks, since their brains will be unable to process spoken requests and demands. (To identify such patients, Claassen’s team is now expanding the test to include a nonverbal component that looks for brain signals that indicate a person is aware of other types of stimuli.) False positives are also a concern. The key to improving the diagnostic, Claassen says, is to build a much larger database of patient results. To this end, the Columbia doctors continue to screen their own coma patients for covert consciousness, while also making their data-gathering methods and analytic algorithms freely available to the research community, to encourage others to join the effort. Claassen has also helped found an international nonprofit, the Curing Coma Campaign, in part to promote research on covert consciousness.
“This is a topic of such urgency that we need to break down institutional barriers and pool our knowledge and resources, so that we can get this technology out into the world as rapidly and safely as possible,” says Claassen. The team recently helped physicians at the University of Miami’s teaching hospital implement their testing methods, and it is in conversation with several other institutions that are interested in collaborating.
Perfecting the EEG test is critical, Claassen says, because its results are likely to inform the agonizing decisions that many families confront about whether to take their loved ones off life support. In the US and Europe today, the majority of people who remain comatose for more than a couple of weeks following a brain injury are removed from life support. “It’s around that point that you need to perform surgical procedures, including a tracheotomy and the insertion of a feeding tube, to sustain patients,” Claassen says. Decisions about withdrawing life support in such circumstances are ultimately made by families in close consultation with physicians, who often struggle to provide guidance, since an individual’s chances for recovery are difficult to assess. “Clearly some patients will have no chance of waking up,” he says, “and we can identify them early on.” These include people with catastrophic injuries to the midbrain and brainstem. “But in other patients, it’s extremely difficult to predict recovery,” he says. “It’s as much art as science.” For families, he says, the lack of clarity can be exasperating. “These are people who are facing one of the most difficult decisions they’ll ever have to make. What they would like to do is know the future.”
The picture is clouded by a lack of long-term epidemiological data. Since at some hospitals people are kept on life support for less than a week, it’s difficult to know how many of them might ultimately awaken and recover if they were sustained for longer. Claassen and his colleagues have conducted research aimed at addressing this question, too. In one study, published in the journal Neurocritical Care in 2022, he and several Columbia colleagues tracked the lives of people who had slipped into comas after suffering severe brain injuries in Japan, where, for a variety of cultural and legal reasons, comatose patients are rarely taken off life support. The Columbia team’s findings offered a measure of reassurance to Western neurologists, showing that Japanese physicians’ initial assessments of their patients’ long-term chances for recovery usually proved accurate. “In other words, patients who might have been removed from life support early on if they’d been in the US, based on the apparent severity of their conditions and other factors, did not, in fact, end up faring well on the whole,” says Claassen. Yet the Columbia researchers also discovered that a small minority of Japanese patients who were initially predicted to have no chance of meaningful recovery did eventually wake up, with some regaining a high level of cognitive function and even managing to live independently. It is the promise of identifying patients like these, whose inner life and potential is hidden from conventional diagnostics, that drives Claassen. Yet he insists that his test for covert consciousness must be made foolproof before it can be introduced in the clinic. Imagine, he offers, if a patient were to be disconnected from life support simply for having been erroneously labeled as not having covert consciousness. Or if someone were to be kept alive for months or years in an unresponsive state, possibly suffering, on the faulty belief that she did.
“We have to get this absolutely right, so that we don’t mislead people in either direction,” Claassen says.
In some ways, the Columbia team’s research has already influenced the clinical care that they provide. With a deepened appreciation for how unpredictable brain injuries can be, Claassen says, he and his colleagues have rededicated themselves to helping family members navigate the difficult process of serving as surrogates for their loved ones’ care decisions. “We encourage a lot of open conversations about how comatose patients would likely regard the uncertainties surrounding their prognosis and the available care options, and how they would wish to proceed,” he says. And at the bedside, doctors and nurses in Claassen’s unit are careful to avoid speaking about patients as if they are not there. “We always operate on the assumption they can hear us speaking,” Claassen says. “And we encourage their loved ones to do the same.”
After one week in a coma, Nick LaRock began to move his fingers. Then he tilted his head slightly, toward a window. And his breathing changed: rather than inhaling in sync with his ventilator, he suddenly seemed to be battling it, insisting on his own rhythm.
“He sounded like he was gasping at first, and I hollered for the nurse,” remembers his mother, Beth. “But she told me it was a good sign — it meant that he was starting to breathe on his own.”
The next few days brought more surprises, for Nick’s parents and doctors alike. He opened his eyes. Said his name. Held up two fingers. Picked up a cup of water and drank from it. Spoke a full sentence. “Whenever he talked, he sounded groggy, like he was still half asleep, and he was very confused,” says his father, Joe. “But it was Nick. We could tell. He was coming back to us.”
In the hallways of CUIMC’s neurocritical-care unit that week, Claassen says, doctors and nurses walked a little lighter, smiled a little wider. “When a very sick patient starts showing signs of recovery, it’s definitely something that we celebrate,” he says. “Everybody is excited. You might even hear whoops of joy.”

By the end of his second week at CUIMC, Nick was conversing with his caretakers, albeit in a laconic drawl that his family said was new, and he was cleared for transfer to another hospital closer to his home. Soon after, he entered a rehabilitation center on Long Island, where he began the hard work of starting his life over. Paralyzed on the right side of his body as a result of the brain hemorrhage, he spent the next several months relearning how to walk, navigate stairs, climb in and out of bed, shower, and dress himself. Suffering from mild cognitive impairment, he had to be taught to read, spell, and enunciate certain words.
“In movies, we’re used to seeing people come out of comas and pick up their lives right where they left off, but the reality is very different, especially for people who’ve suffered severe brain injuries,” says Claassen. “Recovery is a very long, slow, and painful process.”
Today Nick is living on his own, in an apartment in Upper Manhattan. A mild-mannered, composed, and agreeable young man, he speaks reflectively about the challenges he’s faced over the past three years. He is not currently working but dreams of returning to the classroom. He taught American history in New York City schools for ten years before his injury and says the job was the core of his identity. “I’ve actually tried to go back to teaching but found it too difficult,” he says. “I don’t know if that will change.” Reading is still arduous for him, and he says he is self-conscious now in a way that he wasn’t before the injury, when he could easily hold thirty-five boisterous teenagers in rapt attention. “I struggle to find the right words and formulate my thoughts,” he says. “Other people might not notice, but I do, and it bothers me.” Even if he cannot teach, he says, he will be fine. He notes that he’s given up many other things as a result of his paralysis: playing saxophone and ukulele, golfing, bicycling, gaming, slicing vegetables, and wearing shirts with buttons. “And I’ve survived,” he says. “I’m just a different person now. I’m more likely to be found sitting in the park, simply enjoying being here. I feel very lucky.”
From a medical standpoint, Claassen says, Nick’s recovery has been extraordinary. “Considering the severity of his original injury and the length of his coma, it’s tremendous,” he says. “Quite unexpected.”
The supercomputer in Claassen’s office predicted it, though. Back in 2021, every time Columbia researchers asked Nick to imagine opening his hand and then closing it again, they observed two distinct patterns of neuronal activity in his brain’s motor-control center. These patterns closely resembled those seen in fully conscious, healthy subjects who had undergone the same exercise. Nick, like other former patients identified by the Columbia researchers as having covert consciousness, doesn’t remember this. But he doesn’t remember anything from three months before his brain hemorrhage until nearly four months after it. “From October 2020 until May 2021 is just kind of wiped from my mind,” he says.
Even if the Columbia team’s experimental new diagnostic had been in clinical use at the time, it would have had little bearing on Nick’s care. He woke up several days before his Columbia doctors would have talked to his parents about long-term life-support options.
So the real question is this: are there many more people lying unresponsive in hospital beds right now who might similarly spring to life, if only given additional time to heal? And if so, is it possible to identify them? “It’s difficult to know for sure — there are uncertainties at every turn here,” says Claassen. “But we need to look, and we are making great progress.”
This article appears in the Spring/Summer 2024 print edition of Columbia Magazine with the title "Hidden Minds."
More From Health & Medicine

Legendary Child Psychiatrist Clarice Kestenbaum Looks Back — and Forward
At 95, the Columbia professor emerita of clinical psychiatry reflects on an ever-developing field

How Much Plastic Is in Bottled Water? You Probably Don’t Want to Know
Columbia researchers find sobering evidence that bottled water contains far more microplastic particles than previously estimated

Heading a Soccer Ball Does Cause Brain Damage, Experts Say
Researchers find long-term changes in brain structure and function in amateur players
Stay Connected.
Sign up for our newsletter.
General Data Protection Regulation
Columbia University Privacy Notice
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 13, Issue Suppl 2
- Journey of healthcare quality and patient safety in Pakistan
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-6419-4452 Zakiuddin Ahmed 1 , 2 ,
- Khalid Masood Gondal 3 ,
- Javad Akram 4
- 1 Riphah Institute of Healthcare Improvement and Safety (RIHIS) , Riphah International University (RIU) , Karachi , Pakistan
- 2 Health Research Advisory Board (HealthRAB) , Karachi , Pakistan
- 3 Fatima Jinnah Medical University (FJMU) , Lahore , Pakistan
- 4 Pakistan Society of Internal Medicine (PSIM) , Lahore , Pakistan
- Correspondence to Dr Zakiuddin Ahmed; zakiuddinahmed{at}gmail.com
https://doi.org/10.1136/bmjoq-2024-002850
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
- Safety culture
- Healthcare quality improvement
- Quality improvement
Journey of healthcare quality and patient safety in Pakistan is marked by continuous challenges on one hand, yet slow and steady progress on the other. While Pakistan has been struggling with limited healthcare resources and lack of commitment or policy from the government, recent years have witnessed a surge in patient safety and healthcare quality initiatives from all sectors enabling a safer healthcare environment,[1-2].
Before the year 2000, like most other countries, both the government as well as the private health sector in Pakistan did not recognise or prioritise quality and patient safety as a significant component of healthcare. The focus was mainly on treating illnesses rather than providing quality care. Additionally, a realisation about medical errors in hospitals was not present,[1-2]
In the early 2000s, the situation slowly began to change. The first annual symposia on ‘Quality in Healthcare’ at Health Asia Conferences and Exhibition 2004 in Karachi marked the initiation of a formal conversation on healthcare quality and patient safety at a national level. In 2006, the Aga Khan University Hospital (AKUH) became the first Institute in Pakistan to receive accreditation from the Joint Commission International (JCI) leading to setting higher patient safety and quality standards in the country,[3-5]. In 2009, the Health Chapter of Quality and Productivity Society of Pakistan (QPSP) was established which unfortunately discontinued after 2 years due to lack of resources, commitment and financial support. Later on, a larger and more organised national initiative with the name of ‘Healthcare Quality and Safety Association of Pakistan (HQSAP)’ was launched in 2018. In the year 2010 a seminal workshop called ‘Patient First’ was launched all over Pakistan that raised awareness about the importance of patient-centredness as a fundamental of healthcare.
The journey of patient safety and healthcare quality in Pakistan picked up momentum when Riphah International University (RIU), playing a visionary and leadership role, established the Riphah Institute of Healthcare Improvement and Safety (RIHIS) in 2015,[7]. This was the first of its kind dedicated institute of patient safety in the region, which was launched with the mission of creating a reliable health ecosystem that delivers safe and quality healthcare to patients and enables harm-free care with zero medical errors.
In May 2016, RIHIS organised the 1st International Conference on Patient Safety (ICPS) under the theme ‘Patient Safety: Right or Privilege’ which gathered both national and international quality and patient safety experts along with all the major stakeholders,[8-9]. From 2017 to 2023, RIHIS continued to successfully organise the 2nd, 3rd, 4th, 5th, and 6th ICPS, focusing on various themes including ‘Value Based Healthcare’, ‘From Knowledge to Improvement’, ‘Speak Up for Patient Safety’, ‘Implementation Research in Healthcare Quality and Safety’ and ‘Engaging Patients and Families to Co-design Safety’. These conferences, which were co-hosted by leading organisations like Aga Khan University Hospital, Combined Military Hospital, Rawalpindi Medical University, Liaquat National Hospital and Fatima Jinnah Medical University, played a pivotal role in advancing efforts to establish a patient-centric ecosystem in Pakistan. The 7th ICPS is planned to take place on 10–11 May 2024 in Islamabad with the theme of ‘Diagnostic Safety’.
WHO Pakistan office, College of Physicians and Surgeons Pakistan (CPSP), Pakistan Medical and Dental Council (PMDC), National Institutes of Health (NIH) Pakistan, Punjab Healthcare Commission (PHCC), Sindh Healthcare Commission (SHCC), Islamabad Healthcare Regulatory Authority (IHRA), Health Services Academy (HSA) and other leading organisations have been supporting the cause of healthcare quality and patient safety in Pakistan along with endorsing ICPS every year making it the official annual gathering of healthcare quality and patient safety experts.
At each ICPS a Patient Safety Declaration was proposed which was endorsed by all participating organisations and participants. Patient Safety Champion Awards have been given to doctors, nurses, pharmacists, allied health professionals every year who have been championing the cause of patient safety in Pakistan. Similarly, Health Research Advisory Board (HealthRAB) has been giving the ‘Prof. Dr. Tahir Shamsi Patient Safety Research Award’ for best research in healthcare quality and patient safety every year at the ICPS. These conferences have brought several global leaders, domain experts, regulators, academia and other stakeholders working in patient safety and healthcare quality to the country, facilitating the exchange of ideas, knowledge and best practices.
WHO formally contracted RIHIS in the year 2019 with an Agreement for Performance of Work for developing the National Quality & Safety Policy & Strategy and conducting the implementation of the Patient Safety Friendly Hospital Initiative (PSFHI) at leading hospitals across the country. In addition, it also included the development of a report on the situational analysis of patient safety in Pakistan,[10]. This formal initiative of WHO resulted in the Indus Hospital and Health Network and the Tabba Health Institute receiving the PSFHI level 1 status,[11-12]. At present, eight hospitals in Pakistan are implementing the PSFHI,[13]. WHO country office has contributed significantly to establishing healthcare quality and patient safety in Pakistan by launching the PSFHI, celebrating World Patient Safety Day with strategic partners like NIH, RIHIS and others, organising the Patient Safety Technical Working Group workshops with the Ministry of Health, supporting ICPS every year, and commissioning the National Framework on Patient Safety and Quality of Care.
An important landmark in the journey of quality was the creation of provincial health care commissions. Punjab became the first province to lead this initiative and formed the PHCC in 2010 after which Sindh, Khyber Pakhtunkhwa, Balochistan and Islamabad followed suit. These provincial and federal health care commissions developed their own minimum service delivery standards which require all healthcare facilities and providers to register themselves and comply with these standards. These health care commissions significantly contributed towards standardising and improving the quality of care in Pakistan.
Shifa International Hospital in Islamabad, which became the second hospital to get accredited by JCI in 2017, is also one of the leading institutions in Pakistan that has contributed significantly in healthcare quality and patient safety. Shaukat Khanum Cancer & Research Center earned JCI accreditation for its hospitals in Lahore and Peshawar in 2018 and 2019, respectively. AKUH established its Center of Patient Safety in 2020, keeping in line with its history of adding value to the journey of quality care and patient safety in Pakistan.
In the year 2019, RIHIS entered into a Memorandum of Understanding (MoU) with medical universities across Pakistan and in 2020 it established the first two centres of patient safety at Dow University of Health Sciences (DUHS) and Jinnah Sindh Medical University (JSMU). These efforts were followed by a significant milestone when NIH Pakistan developed and launched National Guidelines for Infection Prevention and Control and inaugurated a Center for Occupational and Patient Safety (COPS) which provides strategic guidance to healthcare professionals, enabling transformative changes in the often-neglected area of patient and occupational safety,[14]. Supported by RIHIS as part of the MoU between the two entities, this centre plays a pivotal role in advancing healthcare quality and patient safety standards.
AKUH and Islamic International Medical College (IIMC) of Riphah International University (RIU) became the first two medical colleges which included patient safety in their undergraduate curriculum by using the WHO and Institute for Healthcare Improvement modules. Peshawar Medical College also followed suit and introduced patient safety in its curriculum. Later on PMDC recommended patient safety to be taught in all medical colleges which facilitated the nationwide adoption of this discipline,[15-16]. Jinnah Sindh Medical University also developed a curriculum, with the help of AKUH and RIHIS, which is being taught at all its constituent medical and dental colleges in Karachi.
In 2022, RIHIS took the initiative and led the formation of a Regional Consortium of Patient Safety (RCPS) which includes experts and leaders in patient safety from 18 regional countries. In August 2022, the first meeting of RCPS was organised by RIHIS in collaboration with the Institute of Global Health Innovation, Imperial College London.
In Pakistan, there has been ongoing advancement in raising awareness and conducting research on patient safety and healthcare quality. Leading this effort, RIHIS launched the first dedicated journal focused on patient safety, titled the Journal of Healthcare Quality and Safety (JHQS),[17]. Following this milestone, RIHIS partnered with BMJ Open Quality to launch the BMJ Open Quality Riphah Pakistan Edition,[18].
The journey of patient safety in Pakistan stands as evidence of the steadfast commitment of numerous individuals, institutes, societies and organisations. However, the quest for patient safety remains ongoing and is never truly over. As we celebrate these achievements let us view them as the foundation for building a safer healthcare system. Let us all, patients, healthcare providers, policymakers and educators, commit ourselves to creating a healthcare system in Pakistan where every patient feels safe, valued and well-cared for.’
About this issue
This first-of-its-kind collaborative initiative between BMJ Open Quality and RIHIS provides a platform for encouraging and publishing relevant and local research from a low-middle income country focusing on various areas of healthcare quality, improvement and patient safety. This dedicated research journal will not only foster a culture of patient safety and healthcare quality in Pakistan but will also contribute valuable knowledge and local evidence to the global healthcare landscape. This first issue of this special edition includes articles covering various topics such as patient safety in dentistry, safe practices for adult intravenous push medication, regional perspectives on patient safety policies and initiatives and the impact of compassion and leadership on patient safety and quality in healthcare systems.
Supplemental material
Ethics statements, patient consent for publication.
Not applicable.
Ethics approval
Acknowledgments.
Publication of this article is made Open Access with funding from the Nationwide Quality of Care Network.
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
Contributors ZA played a significant role in conceptualising the editorial theme, outlining the structure and providing critical insights. Additionally, he contributed substantially to the drafting and revising process, ensuring clarity and coherence in the final piece. KMG made substantial contributions to the editorial by offering unique perspectives and insights derived from his expertise. He also played a pivotal role in crafting specific sections of the editorial. From the initial stages of conceptualisation to the final revisions, JA provided valuable input that shaped the editorial’s narrative.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Provenance and peer review Not commissioned; internally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Correction: mHealth intervention to improve quality of life in patients with chronic diseases during the COVID-19 crisis in Paraguay: A study protocol for a randomized controlled trial
- The PLOS One Staff

Published: May 9, 2024
- https://doi.org/10.1371/journal.pone.0303726
- Reader Comments
The affiliation for the 12 th author is incorrect. Marta Miragall is not affiliated with #4 but with #5: Department of Personality, Evaluation and Psychological Treatment, Faculty of Psychology, University of Valencia, Valencia, Spain.
The publisher apologizes for the error.
- View Article
- PubMed/NCBI
- Google Scholar
Citation: The PLOS One Staff (2024) Correction: mHealth intervention to improve quality of life in patients with chronic diseases during the COVID-19 crisis in Paraguay: A study protocol for a randomized controlled trial. PLoS ONE 19(5): e0303726. https://doi.org/10.1371/journal.pone.0303726
Copyright: © 2024 The PLOS One Staff. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Journey of healthcare quality and patient safety in Pakistan
Affiliations.
- 1 Riphah Institute of Healthcare Improvement and Safety (RIHIS), Riphah International University (RIU), Karachi, Pakistan [email protected].
- 2 Health Research Advisory Board (HealthRAB), Karachi, Pakistan.
- 3 Fatima Jinnah Medical University (FJMU), Lahore, Pakistan.
- 4 Pakistan Society of Internal Medicine (PSIM), Lahore, Pakistan.
- PMID: 38719524
- DOI: 10.1136/bmjoq-2024-002850
Keywords: Healthcare quality improvement; Quality improvement; Safety culture.
Publication types
- Patient Safety* / standards
- Patient Safety* / statistics & numerical data
- Quality of Health Care* / standards
- Quality of Health Care* / statistics & numerical data
University of Utah Hospital
General questions.
- Billing & Insurance

You are listening to Bundle of Hers :
S7E6: Beyond Borders — The Journey of an International Medical Graduate
1 in 5 U.S. physicians was born and educated abroad, according to the AAMC. Non-U.S. international medical graduates—different from Americans who attend medical school abroad—face various obstacles in getting to and practicing medicine in America.
In S7E6, Nina Mercado Garcia, an international medical graduate from Colombia, joins Hạ to talk about her unique journey into medicine. From her initial decision to pursue medicine in Colombia to navigating the complexities of practicing in the U.S., Nina shares insights into the challenges and barriers faced by international medical graduates, shedding light on the disparities in opportunities and recognition. Nina's story highlights the significance of global collaboration and exchange in the medical field, and her aspiration to leverage the skills and knowledge gained in America to contribute to health care initiatives worldwide.
This content was originally produced for audio. Certain elements such as tone, sound effects, and music, may not fully capture the intended experience in textual representation. Therefore, the following transcription has been modified for clarity. We recognize not everyone can access the audio podcast. However, for those who can, we encourage subscribing and listening to the original content for a more engaging and immersive experience.
All thoughts and opinions expressed by hosts and guests are their own and do not necessarily reflect the views held by the institutions with which they are affiliated.
Host: Hạ Lê
Guest: Nina Mercado Garcia
Producer: Chloé Nguyễn
Editor: Mitch Sears
Connect with 'Bundle of Hers'
BOH on IG: instagram.com/bundleofhers Email: [email protected] thescoperadio.com bundleofhers.com
More Episodes
- S7 Extra: Finding Your Community in Medical School — Live from Second Look Day
- S7E5: Strategies for Change. Implementing Equity in Medical Training
- S7E4: Balancing Medicine with Non-Medical Partners
- S7E3: Navigating the New Normal — Medical Residency Interviews in the Virtual Era
- S7E2: Breaking Through the Barriers of Medical School Admission
- S7E1: Authentic Exploration in Medicine
- S6 Extra: Embracing Change—The Art of Letting Go
- S6E24: Identity, Growth, and Legacy
- S6E23: Health at Every Size®
- S6E22: The Complexities of The American Dream
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Donaldson L, Ricciardi W, Sheridan S, et al., editors. Textbook of Patient Safety and Clinical Risk Management [Internet]. Cham (CH): Springer; 2021. doi: 10.1007/978-3-030-59403-9_10

Textbook of Patient Safety and Clinical Risk Management [Internet].
Chapter 10 the patient journey.
Elena Beleffi , Paola Mosconi , and Susan Sheridan .
Affiliations
Published online: December 15, 2020.
The wide implementation of patient safety improvement efforts continues to face many barriers including insufficient involvement of all stakeholders in healthcare, lack of individual and organizational learning when medical errors occur and scarce investments in patient safety. The promotion of systems-based approaches offers methods and tools to improve the safety of care. A multidisciplinary perspective must include the involvement of patients and citizens as fundamental contributors to the design, implementation, and delivery of health services.
The patient journey is a challenging example of using a systems approach. The inclusion of the patient’s viewpoint and experience about their health journey throughout the time of care and across all the care settings represents a key factor in improving patient safety. Patient engagement ensures that the design of healthcare services are aligned with the values, the preferences, and needs of the patient community and integrates the real-life experience and the skills of the people to enhance patient safety in the patient journey.
The utmost priority to implement patient engagement is the training of patients. Therefore, training for both patients/families/advocates and health professionals is the foundation on which to build active engagement of patients and consequently an effective and efficient patient journey.
The chapter offers examples of successful training courses designed to foster strategic alliances among healthcare professionals and researchers with patients and their organizations. Training of patients constitutes the first step to develop shared knowledge, co-produced projects, and the achievement of active multilevel participation of patients for the implementation of patient safety in the patient journey.
10.1. Introduction
Almost 20 years after publication “To Err is Human: Building a Better Health System” (Kohn et al. 1999), patient safety is still not widely implemented. This report from the Institute of Medicine is the milestone that constituted a turning point for improving quality of care and patient safety identifying the need to rethink healthcare delivery to provide safe, effective, and efficient care.
The barriers of implementing patient safety as a driving force for change towards more effective healthcare include multiple factors: insufficient involvement of all stakeholders contributing to the care process, lack of willingness of organizations and individuals to learn from errors and scarce investments in patient safety improvement and research.
There is a growing need to promote systems approaches to finding solutions in healthcare to improve the safety of care, the quality of healthcare delivery, patients’ health and citizens’ well-being.
The discussion paper “Bringing a Systems Approach to Health” defines the systems approach as one “that applies scientific insights to understand the elements that influence health outcomes; models the relationships between those elements; and alters design, processes, or policies based on the resultant knowledge in order to produce better health at lower cost” [ 1 ].
A multidisciplinary approach must include the involvement of citizens and patients as fundamental contributors to the design, implementation, delivery, and evaluation of health services.
This means that citizen participation plays an essential role, bringing the unique point of view of patients and family members into the debate on patient safety and quality of care.
Patients and more generally citizens, when actively and systematically engaged, bring ideas and experiences which can support a collaborative and reciprocal learning process among the healthcare stakeholders. This produces knowledge that leads to improved practices, a real knowledge creation process where the dynamic participation of all actors in healthcare systems contribute to an active learning environment where the identification, the investigation, and the planning of solutions related to health incidents is a cyclic process enabling healthcare knowledge creation.
The added value of involving patients in healthcare is, respect to other more complex interventions, a low cost opportunity to take into consideration unconventional points of view creating and building knowledge and providing original insights and ideas that otherwise would not be considered.
Health professionals and patients’ skills and knowledge are acquired through individual experience or education and transferred to the health organizations in a perspective of co-production of healthcare. It is a merging of the efforts of those who produce and those who use the solutions to address health problems. It serves to establish a strengthened and long-term relationship in terms of trust and effectiveness and to distribute the responsibilities among all stakeholders [ 2 ].
In light of these arguments, the systems approach—inspired by the fundamentals of ergonomics and human factors (HFE)—creates new alliances between healthcare and engineering, of which patient journey is a challenging example [ 3 ].
Applying the systems approach to patient safety allows the analysis of the factors that characterize the encounters and the interactions between healthcare professionals and patients during the entire course of care. The observation of possible critical issues to the individual and specific encounter between clinician and patient is crucial in widening the scope of observation and research of the entire “journey” of the patient, taking into consideration the complexity of patient, their values and needs, their preferences, the economic and social context in which they live, and language and communication issues.
These observations and research should be carried out considering the interconnections and interactions together with the components of the processes; importance should be given to the context, and to manage the complexity, the value of a holistic approach.
10.2. The Patient Journey
A modern health system looks to the future in the context of the challenges imposed by the real world. It must manage the gap between guidelines and health protocols and what effectively happens and how reality is perceived by patients and family members.
It is more and more necessary to bring the patient’s point of view in the analysis of the care process, in the incident reporting and analysis, in the design and implementation of solutions and guidelines in healthcare.
Vincent and Amalberti in “Safer Healthcare” (2016) [ 4 ] stated that the incident analysis should broaden the class of events having consequences on patient safety. Incidents reported from the patient’s point of view should be included in addition to those suggested by health professionals. Additionally, when analyzing an incident, it should be done in the context of the patient journey rather than a single episode.
Instead of focusing on the individual encounter, it is necessary to extend the observation timeframe by applying the examination of contributing factors to each of the encounters that compose the patient journey (temporal series of encounters with healthcare facilities, a hospital unit, a specialist visit, a primary care clinic, a home health agency), considering both the negative and positive events and the points for improvement that were revealed (Fig. 10.1 ).
Analysis of safety along the patient journey
The adoption of this wider approach is unique in that it incorporates the patient’s perspective of safety and includes new features in the incident analysis such as asking patients to recount the episode of care, including patient and family in the investigation team when possible, asking patients the contributory factors from their point of observation and perception and involving patients and families in the reflections and comments on the disclosure process [ 4 ].
The episodes patients and families can highlight are often different from those that professionals are more accustomed to reporting. However, patients could be involved in further ways in incident reporting and assessment, and today patient-derived information constitutes a free and little used resource.
As per McCarthy’s definition, “patient journey mapping describes the patient experience, including tasks within encounters, the emotional journey, the physical journey, and the various touch points” [ 5 ]. Carayon and Woldridge define “patient journey as the spatio-temporal distribution of patients’ interactions with multiple care settings over time” [ 3 ], where at each point of touch with each healthcare service along the patient journey, the patient interacts with several system elements (task interaction, physical environment, interaction with tools and technologies, organization interaction, interaction with other organizations and other people, interaction with other people and teams within the organization) (Fig. 10.2 ).
The patient journey as a set of interactions and transitions
The patient journey represents the time sequence of what happens to the patient, especially during transitions of care, in particular considering that the health professional who takes care of the patient only sees the portion of care for which he is responsible and in which he has an active role. Conversely, the patient is the only person who has a continuously active and first-hand role during their health journey. They alone are in possession of information that characterizes the entire care experience.
Moreover, when patients navigate their journey, they contact and interface with multiple work systems at several time points, where the sequence of interactions in the work systems determine the outcome experienced by patients and families, healthcare professionals, and health organizations. (Fig. 10.3 ). Each local work system is influenced by a wider socio-organizational context, which can be formal healthcare organization (such as hospital, primary care facility, nursing home) or informal (home).
SEIPS 3.0 model: sociotechnical systems approach to patient journey and patient safety
Every point of the patient journey offers data on health outcomes and patient experience outcomes that should be used as feedback to redesign healthcare work systems in terms of adaptation, learning, improvement.
Patient’s experience represents an important resource in participatory collaborative design, especially in the patient journey where this experience is the result of multiple interactions across space and time.
10.3. Contextualizing Patient Safety in the Patient Journey
Many of the incidents or near-misses during healthcare are not due to serious errors, but to the combination of small failures, such as limited experience of a recently qualified doctor, use of obsolete equipment, an infection difficult to diagnose or inadequate communication within a team.
We know that the analysis of an incident requires looking back to the succession of events that have occurred and that led to the problematic episode, considering both active and latent errors, and all the aspects connected directly or indirectly. It is fundamental to examine the safety of the entire patient journey, all the encounters that make up the entire care process, to study the whole medical history of the patient in an attempt to reconstruct all the elements that characterize the “health journey”, not only from the viewpoint of the health professionals, but also from that of the patient and family.
In light of these arguments, new concepts, tools, models, and methods need to be embraced to support patient safety in the patient journey.
A significant contribution in terms of concepts, frameworks, and models is offered by Industrial and Systems Engineering, and often human factors and systems engineering (HF/SE) have an approach to include the preferences and the needs of stakeholders when designing solutions to address the critical aspects of a health process.
Human factors and ergonomics are described as “the scientific discipline concerned with the understanding of interactions among humans and other elements of a system, and the profession that applies theory, principles, data and methods to design in order to optimize human well-being and overall system performance. Practitioners of ergonomics and ergonomists contribute to the design and evaluation of tasks, jobs, products, environments and systems in order to make them compatible with the needs, abilities and limitations of people. Ergonomics helps harmonize things that interact with people in terms of people’s needs, abilities and limitations” [ 6 ].
Process models have found widespread use in drug management, visit planning, care transition, to name a few, and can offer tools and methods to investigate interprofessional and physician–patient communication, interruptions and health information handover.
Drawing from the finding of Carayon’s studies [ 3 ], the Systems Engineering Initiative for Patient Safety (SEIPS) model gives a description of five work system elements which when applied to a definite patient journey model should outline who (person) is doing what (tasks) with tool and technologies, taking into consideration the physical and organizational environment where all these activities take place. All these factors have to be examined for both patients and workers and the process analysis and modelling have to consider what patients and families/caregivers, healthcare professionals and workers actually do ( work-as-done versus work-as-imaginated ).
Patients, families, and caregivers are deeply involved in the healthcare process due to the tasks they carry out in the intermediate sectors of care between encounters. Away from direct interactions with professionals, they have to perform multiple actions requiring understanding of what behaviour to adopt, which instructions to follow, how to administer a medication and how to communicate with hospital doctors, general practitioner, and home healthcare professionals [ 3 ].
Taking into account what has been highlighted so far, one of the leading and most challenging keys to success in improving patient safety is to adopt a systems approach to patient safety which includes the patient’s perspective about their health journey throughout the time of care and across all the care settings.
This assumption highlights that patients and their families are valuable resources and can play an important role in patient safety improvement efforts. Viewing health systems as “co-producing systems”, patients can engage as partners in co-producing patient safety improvement activities individually, in groups and collectively. Individual patient and family member participation/co-production of safer care is fundamental. Equally as important is the co-management and co-governance of healthcare services, in addition to the engagement of communities in policy definition and designing activities.
In fact, patient engagement directs the design of healthcare systems towards the preferences, the values, the real-life experiences, and—not less important—the skills of the people to enhance patient safety in the patient journey.
Such a change of perspective involves multiple dimensions of interactions and relationship between patients and professionals, encompassing cooperation, dialogue and listening, trust, reciprocity and peer-to-peer work [ 2 ].
It follows that on the one hand the healthcare organizations have to demonstrate the willingness to support health professionals to effectively engage patients in the patient journey to achieve the common goal of reducing the risk of patient harm or incidents as well as the willingness to integrate patients and family members as partners into quality and safety improvement efforts. On the other hand, it is necessary to motivate and encourage patients and families/caregivers to actively participate during the individual care process for safer care as well as partner in organizational patient safety improvement efforts to ensure safer care for others.
The working group Patient and Family Involvement for the delivery of Safe and Quality Care [ 7 ] stated that the utmost priority to realize the patient involvement is the training of patients, followed by the promotion of interdisciplinary training programmes for healthcare professionals to promote patient and family engagement, the implementation of multilevel structures that allow for participatory processes by patients and smarter allocation of resources in healthcare that supports involving citizens in patient safety improvement efforts for better healthcare.
This working group was part of the activities of the “1st International Meeting about Patient safety for new generations—Florence, 31st August and 1st September 2018” organized by the Centre for Clinical Risk Management and Patient Safety, Tuscany Region—WHO Collaborating Centre for in Human Factors and Communication for the Delivery of Safe and Quality care [ 7 ].
Therefore, training for both patients/families/advocates and health professionals is a pillar on which to build active engagement of patients and consequently an effective and efficient patient journey. From this perspective, the participation of patients (i.e. representatives of patients’ associations and organizations, patient and citizen advocates) in training courses—specifically designed for this target audience of trainees and aimed to encourage co-production of care—is an essential and effective activity to co-produce a better healthcare system in terms of quality and safety of care.
Sharing a common language, promoting citizens’ and patients’ awareness of importance of co-production of care, teaching the key role that patients can play in making treatments safer (investments in health literacy), learning to work together and within a network (locally, regionally, and nationally/internationally) on priority safety and quality of care issues: these are some of the main strengths of training courses aimed to be at the basis of active engagement of patients and citizens.
Examples of successful training courses include “PartecipaSalute” and “Accademia del Cittadino” organized in Italy by Laboratory for Medical Research and Consumers Involvement of the Istituto di Ricerche Farmacologiche Mario Negri IRCCS and the Centre for Clinical Risk Management and Patient Safety, Tuscany Region. The following paragraph describes this educational experience which is specifically designed for citizens and patients to improve their knowledge and skills in patient safety and quality of care, with the aim of co-producing better healthcare services.
10.4. From PartecipaSalute to the Accademia del Cittadino: The Importance of Training Courses to Empower Patients
Over the last few years in the field of health and research and with regard to participation and involvement of citizens and patients, we have witnessed the transition from a paternalist to a partnership model. Individual citizens and those citizens involved in patients’ associations or groups have acquired a new role: no longer passive but actively involved in decision-making regarding health, healthcare, and research in the health field [ 8 , 9 ].
This is a progressive step-by-step process based on the recognition and implementation of the key concepts such as health literacy and empowerment. Health literacy, more properly used at individual level is defined as the capacity to obtain, read, understand, and use healthcare information in order to make appropriate health decisions and follow instructions for treatment [ 10 ]. Empowerment, more used at the community level, is a process that, starting from the acquisition of accurate knowledge and skills, enables groups to express their needs and more actively participate to request better assistance, care, and research. At this level, the availability of organized independent and evidence-based training courses is essential to allow people to be able to critically appraise and use information about the effects of healthcare interventions. Consequently, they will have the skills to participate in the multidisciplinary working groups (composed of researchers, health professionals, patient and citizen advocates, institutional representatives).
In the late 1990s, the Istituto di Ricerche Farmacologiche Mario Negri IRCCS held the first training courses of this kind focused at breast cancer associations. Some years later, within the project PartecipaSalute—a not-for-profit research project designed to foster a strategic alliance among healthcare professionals, patients, and their organizations—an ad hoc training programme for representatives of citizens’ and patients’ organizations was defined with a multimodule format [ 11 , 12 ]. This was an innovative approach, at least in the Italian setting in that period.
PartecipaSalute training programme has combined different experiences: the Mario Negri Institute IRCCS experience in collaborative research activities with patients’ associations, the Italian Cochrane Centre with the activities aimed at promoting the principles of evidence-based medicine, and Zadig long-term experience in health communication. The above promoters jointly developed the PartecipaSalute training programme on the belief that data are more important than opinions, and that every decision should be supported by well-conducted research data.
The spread of this belief to patients and citizens with the purpose of stronger involvement was a key point of PartecipaSalute training courses.
Therefore, patient, family, and community knowledge of the principles of how evidence is developed through clinical research is essential to make or support decisions in the health debate, to promote better clinical research, or to convey correct information. The strength of the PartecipaSalute programme was based on the exchange of experiences in an interactive way aimed at creating opportunities for discussion, overcoming the teacher–learner model. Each session started with an interactive discussion of a real situation—such as a screening, vaccination, therapy—and after sharing data, opinions or articles from media, evidence was presented and discussed, underlining significant methodological aspects. The programme offered the opportunity to debate the value and significance of the methodology offering critical appraisal tools. Each participant was invited to take an active part, starting from direct personal or associative experience. Table 10.1 presents the topics considered in the first three editions of the training programme. The participation was free, and different types of materials were provided including an ad hoc manual published by PartecipaSalute, copies of the PowerPoint presentation and articles.
Topics considered in PartecipaSalute [4] and PartecipaSalute-Accademia del Cittadino training courses
Considering the characteristics of the programme and its modular structure, the PartecipaSalute training programme could be adapted to specific contexts. In fact, the experience of PartecipaSalute was adopted at the regional level by Regione Toscana (Centre for Clinical Risk Management and Patient Safety and the Quality of healthcare and Clinical pathways of Health Department, Tuscany Region) developing a more specific training programme called PartecipaSalute-Accademia del Cittadino (Academy of Citizen), focused on patient safety and risk management. In particular, after some modules on methods related to evidence-based medicine, uncertainties in medicine and information and communication in health, the training was mainly dedicated to regional and local activities on clinical risk management, the role of patients’ associations to improve patient safety and to support the implementation of best practices, the analysis and data of adverse events and risk assessment in terms of quality and safety in the care processes (Table 10.2 ).
Topic integration in the PartecipaSalute-Accademia del Cittadino joint courses
The PartecipaSalute-Accademia del Cittadino joint training programme has been implemented in three editions over the last decade and has trained about 100 members of patient and citizen advocates representing 38 patients’ associations. The courses ranged from 5 to 3 modules of 2 days each in residential mode to allow participants to get to know each other and create a network of associations committed to be engaged in clinical research, quality, and healthcare safety issues.
The entire educational experience was characterized by the use of participatory training methods, based on working groups, practical exercises, lectures from experts with opportunities for discussions. As a result of this training course model, the participants were recognized as “expert patients” and were regularly involved in basic activities for promoting patient safety as auditors on significant events and helping to define policies on patient safety at the Tuscany regional level. In addition, they have participated in patient safety walkarounds in hospitals and in developing eight cartoons intended to promote the education of citizens for the prevention of the most diffused risks (such as prevention of infections, prevention of falls and handovers).
Feedback on the satisfaction on tutors, topics discussed and knowledge gained was regularly requested from participants through questionnaires distributed before and after the programme. In general, positive feedback was received; participants appreciated the interactive methods of work, the clarity of the language, and the effort to make difficult problems easy to understand. An ad hoc questionnaire was provided to the participants regarding the methodology of clinical research, always showing an improvement in the self-evaluated knowledge before and after the course. Feedback of the results of the evaluation was also shared with each participant. Most of participants reported their experience to other members of the organization. In particular, in the case of the Regione Toscana training, the possibility of immediately transferring what was learned in the course in all the activities in collaboration with the health institutions, policy makers, and health professionals—such as working groups on patient safety best practices, participation to audits, development of tools to improve health literacy—was appreciated.
Some limitations emerged from these experiences. The selection of participants is the first issue, not only because the training course is accessible to a small number of participants (in general no more than 30 participants), but also because the groups comprised of middle-aged and retired participants, with few younger ones. Additionally, there were few individual patient or family member representatives from patient associations. The majority of those representing patient associations were in managerial or leadership positions. Furthermore, it is difficult to choose between small, local, or bigger regional associations. Residential training courses also restricted the participation for geographical reasons.
The PartecipaSalute and ParteciaSalute-Accademia del Cittadino training experiences show that patients and citizens are willing to get actively involved in healthcare and the research debate. There is a real desire to improve their knowledge and skills on health and research issues and allow some general considerations regarding the active engagement of citizens representing associations and advocacy groups.
In conclusion, it is very important to invest in a process of empowerment aimed to have well-trained activists involved vigorously and constructively in the debate, design, and assessment of health and research. Switching from tokenism to active participation is necessary to effectively partner with patients and the general population to design, plan, and co-produce safer more effective healthcare, while also supporting better more patient-centred research [ 13 , 14 ].
Also, the training courses are feasible and useful, as has recently been discovered also by pharma or other groups that organize courses mainly focused on drugs and drug development, thus directing the participation of the groups more to market needs than to public health.
Furthermore, this training initiative facilitates the networking among associations in part overcoming the difficulties that derive from personalization and division among the associations representing citizens and patients.
Finally, this illustrates the importance of the design and promotion of training courses with institutions, such as the Regione Toscana, in order to be able to implement projects of real collaboration between institutions, healthcare professionals, and consumers’ and patients’ representatives.
10.5. Recommendations
A systemic approach to health can provide valuable models for wider implementation of patient safety. A multidisciplinary approach includes the involvement of citizens and patients as unique stakeholders in the design, implementation, delivery, and assessment of health services.
Involving patients in healthcare is an opportunity to bring uncommon points of view into policy making and to create shared knowledge between healthcare professionals and patients.
The implementation of patients’ and families’/caregivers’ perspectives in the patient journey is the golden opportunity to leverage crucial input, such as experiential knowledge, safer care, patient motivation, and trust and social cohesion into the co-production of safety solutions in healthcare. This represents a way to get closer to person-centred care, to create opportunities for patients to meet and share information and knowledge, to develop structures and policies for patient involvement at different levels (with healthcare systems, universities, and policy makers).
However, little has been done to overcome some healthcare systems barriers: the power imbalance between the doctor and patient, language differences, the lack of diffusion of non-technical skills and, last but not least, the lack of evidence about the value of patient involvement.
To be widely implemented, patient engagement in the patient journey requires courageous leadership, organizational efforts, a wider culture of safety of care, the implementation of multilevel structures for the engagement of patients and resources from smarter spending in healthcare.
Education is the landmark to integrate meaningful patient and citizen engagement in healthcare. Training of patients is the fundamental starting point to develop shared knowledge, co-produce projects, and implement an active multilevel participation of patients and families for the improvement of quality and safety of care.
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
- Cite this Page Beleffi E, Mosconi P, Sheridan S. The Patient Journey. 2020 Dec 15. In: Donaldson L, Ricciardi W, Sheridan S, et al., editors. Textbook of Patient Safety and Clinical Risk Management [Internet]. Cham (CH): Springer; 2021. Chapter 10. doi: 10.1007/978-3-030-59403-9_10
- PDF version of this page (884K)
In this Page
- Introduction
- The Patient Journey
- Contextualizing Patient Safety in the Patient Journey
- From PartecipaSalute to the Accademia del Cittadino: The Importance of Training Courses to Empower Patients
- Recommendations
Related information
- PubMed Links to PubMed
Similar articles in PubMed
- The patient experience of patient-centered communication with nurses in the hospital setting: a qualitative systematic review protocol. [JBI Database System Rev Implem...] The patient experience of patient-centered communication with nurses in the hospital setting: a qualitative systematic review protocol. Newell S, Jordan Z. JBI Database System Rev Implement Rep. 2015 Jan; 13(1):76-87.
- The future of Cochrane Neonatal. [Early Hum Dev. 2020] The future of Cochrane Neonatal. Soll RF, Ovelman C, McGuire W. Early Hum Dev. 2020 Nov; 150:105191. Epub 2020 Sep 12.
- A qualitative systematic review of internal and external influences on shared decision-making in all health care settings. [JBI Libr Syst Rev. 2012] A qualitative systematic review of internal and external influences on shared decision-making in all health care settings. Truglio-Londrigan M, Slyer JT, Singleton JK, Worral P. JBI Libr Syst Rev. 2012; 10(58):4633-4646.
- Review Health professionals' experience of teamwork education in acute hospital settings: a systematic review of qualitative literature. [JBI Database System Rev Implem...] Review Health professionals' experience of teamwork education in acute hospital settings: a systematic review of qualitative literature. Eddy K, Jordan Z, Stephenson M. JBI Database System Rev Implement Rep. 2016 Apr; 14(4):96-137.
- Review Evidence Brief: The Effectiveness Of Mandatory Computer-Based Trainings On Government Ethics, Workplace Harassment, Or Privacy And Information Security-Related Topics [ 2014] Review Evidence Brief: The Effectiveness Of Mandatory Computer-Based Trainings On Government Ethics, Workplace Harassment, Or Privacy And Information Security-Related Topics Peterson K, McCleery E. 2014 May
Recent Activity
- The Patient Journey - Textbook of Patient Safety and Clinical Risk Management The Patient Journey - Textbook of Patient Safety and Clinical Risk Management
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- ALL MOSCOW TOURS
- Getting Russian Visa
- Top 10 Reasons To Go
- Things To Do In Moscow
- Sheremetyevo Airport
- Domodedovo Airport
- Vnukovo Airport
- Airports Transfer
- Layover in Moscow
- Best Moscow Hotels
- Best Moscow Hostels
- Art in Moscow
- Moscow Theatres
- Moscow Parks
- Free Attractions
- Walking Routes
- Sports in Moscow
- Shopping in Moscow
- The Moscow Metro
- Moscow Public Transport
- Taxi in Moscow
- Driving in Moscow
- Moscow Maps & Traffic
- Facts about Moscow – City Factsheet
- Expat Communities
- Groceries in Moscow
- Healthcare in Moscow
- Blogs about Moscow
- Flat Rentals
Healthcare in Moscow – Personal and Family Medicine
Emergency : 112 or 103
Obstetric & gynecologic : +7 495 620-41-70
About medical services in Moscow

Moscow polyclinic
Emergency medical care is provided free to all foreign nationals in case of life-threatening conditions that require immediate medical treatment. You will be given first aid and emergency surgery when necessary in all public health care facilities. Any further treatment will be free only to people with a Compulsory Medical Insurance, or you will need to pay for medical services. Public health care is provided in federal and local care facilities. These include 1. Urban polyclinics with specialists in different areas that offer general medical care. 2. Ambulatory and hospitals that provide a full range of services, including emergency care. 3. Emergency stations opened 24 hours a day, can be visited in a case of a non-life-threatening injury. It is often hard to find English-speaking staff in state facilities, except the largest city hospitals, so you will need a Russian-speaking interpreter to accompany your visit to a free doctor or hospital. If medical assistance is required, the insurance company should be contacted before visiting a medical facility for treatment, except emergency cases. Make sure that you have enough money to pay any necessary fees that may be charged.
Insurance in Russia

Travelers need to arrange private travel insurance before the journey. You would need the insurance when applying for the Russian visa. If you arrange the insurance outside Russia, it is important to make sure the insurer is licensed in Russia. Only licensed companies may be accepted under Russian law. Holders of a temporary residence permit or permanent residence permit (valid for three and five years respectively) should apply for «Compulsory Medical Policy». It covers state healthcare only. An employer usually deals with this. The issued health card is shown whenever medical attention is required. Compulsory Medical Policyholders can get basic health care, such as emergencies, consultations with doctors, necessary scans and tests free. For more complex healthcare every person (both Russian and foreign nationals) must pay extra, or take out additional medical insurance. Clearly, you will have to be prepared to wait in a queue to see a specialist in a public health care facility (Compulsory Medical Policyholders can set an appointment using EMIAS site or ATM). In case you are a UK citizen, free, limited medical treatment in state hospitals will be provided as a part of a reciprocal agreement between Russia and UK.
Some of the major Russian insurance companies are:
Ingosstrakh , Allianz , Reso , Sogaz , AlfaStrakhovanie . We recommend to avoid Rosgosstrakh company due to high volume of denials.
Moscow pharmacies

A.v.e pharmacy in Moscow
Pharmacies can be found in many places around the city, many of them work 24 hours a day. Pharmaceutical kiosks operate in almost every big supermarket. However, only few have English-speaking staff, so it is advised that you know the generic (chemical) name of the medicines you think you are going to need. Many medications can be purchased here over the counter that would only be available by prescription in your home country.
Dental care in Moscow

Dentamix clinic in Moscow
Dental care is usually paid separately by both Russian and expatriate patients, and fees are often quite high. Dentists are well trained and educated. In most places, dental care is available 24 hours a day.
Moscow clinics

«OAO Medicina» clinic
It is standard practice for expats to visit private clinics and hospitals for check-ups, routine health care, and dental care, and only use public services in case of an emergency. Insurance companies can usually provide details of clinics and hospitals in the area speak English (or the language required) and would be the best to use. Investigate whether there are any emergency services or numbers, or any requirements to register with them. Providing copies of medical records is also advised.
Moscow hosts some Western medical clinics that can look after all of your family’s health needs. While most Russian state hospitals are not up to Western standards, Russian doctors are very good.
Some of the main Moscow private medical clinics are:
American Medical Center, European Medical Center , Intermed Center American Clinic , Medsi , Atlas Medical Center , OAO Medicina .
Several Russian hospitals in Moscow have special arrangements with GlavUPDK (foreign diplomatic corps administration in Moscow) and accept foreigners for checkups and treatments at more moderate prices that the Western medical clinics.
Medical emergency in Moscow

Moscow ambulance vehicle
In a case of a medical emergency, dial 112 and ask for the ambulance service (skoraya pomoshch). Staff on these lines most certainly will speak English, still it is always better to ask a Russian speaker to explain the problem and the exact location.
Ambulances come with a doctor and, depending on the case, immediate first aid treatment may be provided. If necessary, the patient is taken to the nearest emergency room or hospital, or to a private hospital if the holder’s insurance policy requires it.
Our Private Tours in Moscow
Moscow metro & stalin skyscrapers private tour, moscow art & design private tour, soviet moscow historical & heritage private tour, gastronomic moscow private tour, «day two» moscow private tour, layover in moscow tailor-made private tour, whole day in moscow private tour, all-in-one moscow essential private tour, tour guide jobs →.
Every year we host more and more private tours in English, Russian and other languages for travelers from all over the world. They need best service, amazing stories and deep history knowledge. If you want to become our guide, please write us.
Contact Info
+7 495 166-72-69
119019 Moscow, Russia, Filippovskiy per. 7, 1
Mon - Sun 10.00 - 18.00

IMAGES
VIDEO
COMMENTS
Introduction. Quality and safety guidelines in healthcare services are increasingly encouraging and mandating engagement of patients, clients, and consumers in partnerships. 1 The aim of many of these partnerships is to consider how health services can be improved, in relation to accessibility, service delivery, discharge, and referral. 2, 3 Patient journey mapping is a research approach ...
Introduction. Throughout the world, the patient experience is recognized as an independent dimension of health-care quality, along with clinical effectiveness and patient safety (1,2).Health-care organizations across the United States are focusing on how to "deliver a superior patient experience" ().Quality is a key driver of these industry-wide changes, as are the shifts in health-care ...
Therefore, hospitals can significantly improve the quality of the service provided by exploring and understanding the individual patient journey [ 12 - 14 ]. Many tools may be used to measure and understand patient experience [ 15, 16 ]. Surveys are the methods mainly used to capture the patient experience and to evaluate the quality and ...
The type of surgery and stage of the patient journey formed the analysis groups. The study was part of a larger hospital project to redesign the orthopaedic patient journey for hip or knee replacement surgery, here starting with the patient experience [19, 21]. In particular, the data collected by the hospital management to assess the quality ...
Process mapping enables the reconfiguring of the patient journey from the patient's perspective in order to improve quality of care and release resources. This paper provides a practical framework for using this versatile and simple technique in hospital. Healthcare process mapping is a new and important form of clinical audit that examines how we manage the patient journey, using the ...
A "Patient Journey" is a personal testimony that reflects the needs of patients in two key reference documents—an accessible visual overview, supported by a detailed information matrix. The ...
Therefore, hospitals can significantly improve the quality of the ser-vice provided by exploring and understanding the individual patient journey [12-14]. Many tools may be used to measure and understand patient experience [15, 16]. Surveys are the methods mainly used to capture the patient experience and to evaluate the quality and safety of ...
Patient journey maps can be generated using a variety of techniques (8,9), can be used to identify problems, and can suggest improvements to the care process . ... From the patient perspective, quality of care means meeting the health goal(s) as quickly as possible. Systems can support shared care planning, thus increasing patient health goal ...
2. BACKGROUND. Patient journey mapping is the health care-specific term for journey mapping that can assist with improving the patient experience. It can be applied to existing processes that have room for improvement, as well as evaluating the success of new interventions being implemented in the system.
Importance of patient journey in quality of care: the need for patient-centric approach in medical protocols, guidelines, and ethical standards. 26.2 Introduction. The healthcare system can be a complex and overwhelming experience for patients, especially when they are faced with illness or injury. To ensure that patients receive the best care ...
An integrated patient journey mapping tool for embedding quality in healthcare service reform. J. Decis. Syst. 25(sup1), 354-368 (2016) Article Google Scholar Meyer, M.A.: Mapping the patient journey across the continuum: lessons learned from one patient's experience. J. Patient Exp. 6(2), 103-107 (2019)
The patient journey is best described as the sequence of experiences a patient has from admission to discharge. This includes all the touchpoints between the patient and provider from beginning to end. ... (CMS) has issued recent guidelines for participants that help offset the costs of high-quality care through a reward system. 4. Retention ...
INTRODUCTION. Medical researchers have long pointed to the importance of understanding the realistic picture of the patient journey: the chronological sequence of how a patient seeks and receives care from the healthcare system. 1, 2 Capturing an accurate overview of the patient journey can help identify sources of variability, evaluate why patients respond differently to the same overarching ...
What is the patient journey? The patient journey is the sequence of events that begins when a patient first develops a need for care. Rather than focusing on service delivery, the patient journey encompasses all touchpoints of a patient's healthcare experience-from locating healthcare providers and scheduling appointments, to paying the bill and continuing their care after treatment.
The promotion of systems-based approaches offers methods and tools to improve the safety of care. A multidisciplinary perspective must include the involvement of patients and citizens as fundamental contributors to the design, implementation, and delivery of health services. The patient journey is a challenging example of using a systems approach.
To determine which factors most strongly influence patient satisfaction, health systems must accurately understand the end-to-end inpatient journey, from pre-admission scheduling and testing through to follow-up care, as well as the role that price, service offerings, physician referrals, and brand play in determining where patients seek care ...
2. Conceptual foundation for the integrated patient journey Map. Pickles et al. (Citation 2008) provide a framework for healthcare service reform and improvement that addresses performance, regulatory constraints, and patient experience goals using the following components of good design: Functionality, Engineering, and Aesthetics of Experience.. Functionality aims towards designing for ...
Active PD platform, app would track Parkinson's, help improve quality of life. Because each patient journey is different, regular monitoring in Parkinson's disease can allow for quicker interventions. However, such monitoring, and routine patient examinations, can be difficult to facilitate, especially for those in rural areas.
"Patients are no longer passive recipients of care," explains Vakhtangishvili."They want to be active participants in their healthcare journey, with access to real-time information, seamless ...
Plum and Posner called the condition "locked-in syndrome." These patients could be taught to communicate by blinking and glancing from side to side — a method that the French journalist Jean-Dominique Bauby famously used to dictate his 1997 memoir about living with the syndrome, The Diving Bell and the Butterfly. Neurologists say that the ...
Motor neuron disease is a devastating incurable condition with a severe effect on autonomy and quality of life of patients and their relatives. Treatment primarily consists of marginally disease-modifying neuroprotective therapies, which include measures to alleviate disease-related symptoms such as muscle cramps, sialorrhoea, dysphagia and respiratory insufficiency; and the provision of ...
Journey of healthcare quality and patient safety in Pakistan is marked by continuous challenges on one hand, yet slow and steady progress on the other. While Pakistan has been struggling with limited healthcare resources and lack of commitment or policy from the government, recent years have witnessed a surge in patient safety and healthcare quality initiatives from all sectors enabling a ...
This week, The Lancet published the findings from COMMEND, the largest clinical trial to date of a psychological intervention for people with motor neuron disease (MND). This devastating, incurable neurodegenerative disease results from the loss of motor neurons in the motor cortex and spinal cord, causing progressive paralysis and eventual death. More than half of people with MND die within 2 ...
The Patient-Reported Observations on Medical Procedure Timeliness (PROMPT) for Breast Patients study, a 2-year quality collaborative of the ACS National Accreditation Program for Breast Centers (NAPBC), was completed in January 2024. In the first year of PROMPT, 322 NAPBC-accredited sites contributed data from 2019 to 2021 on four timely metrics:
Escrivá-Martínez T, Vara MD, Czeraniuk N, Denis M, Núñez-Benjumea FJ, Fernández-Luque L, et al. (2022) mHealth intervention to improve quality of life in patients with chronic diseases during the COVID-19 crisis in Paraguay: A study protocol for a randomized controlled trial. PLoS ONE 17(11): e0273290. pmid:36346807
Journey of healthcare quality and patient safety in Pakistan BMJ Open Qual. 2024 May 7;13(Suppl 2):e002850. doi: 10.1136/bmjoq-2024-002850. Authors Zakiuddin Ahmed 1 2 , Khalid Masood Gondal 3 , Javad Akram 4 Affiliations 1 Riphah Institute of Healthcare ...
Because of this, many expats in Russia choose to take out private medical treatment which is widely available in many areas. Patients access doctors, dentists, and medical specialists through the state system or privately. In recent years, some state facilities have begun to offer private treatment to those with insurance.
In S7E6, Nina Mercado Garcia, an international medical graduate from Colombia, joins Hạ to talk about her unique journey into medicine. From her initial decision to pursue medicine in Colombia to navigating the complexities of practicing in the U.S., Nina shares insights into the challenges and barriers faced by international medical ...
The Patient Journey. A modern health system looks to the future in the context of the challenges imposed by the real world. It must manage the gap between guidelines and health protocols and what effectively happens and how reality is perceived by patients and family members.
These include 1. Urban polyclinics with specialists in different areas that offer general medical care. 2. Ambulatory and hospitals that provide a full range of services, including emergency care. 3. Emergency stations opened 24 hours a day, can be visited in a case of a non-life-threatening injury.