
Ectopic Supraventricular Arrhythmias
Various rhythms result from supraventricular foci (usually in the atria). Diagnosis is by electrocardiography. Many are asymptomatic and require no treatment.
(See also Overview of Arrhythmias .)
Ectopic supraventricular rhythms include
Atrial premature beats
Atrial tachycardia, multifocal atrial tachycardia, nonparoxysmal junctional tachycardia, wandering atrial pacemaker.
Atrial premature beats (APB), or premature atrial contractions (PAC), are common episodic impulses. They may occur in normal hearts with or without precipitating factors (eg, coffee, tea, alcohol, pseudoephedrine ) or may be a sign of a cardiopulmonary disorder. They are common in patients with chronic obstructive pulmonary disease (COPD). They occasionally cause palpitations.
Diagnosis is by electrocardiography (ECG—see figure Atrial premature beat ).
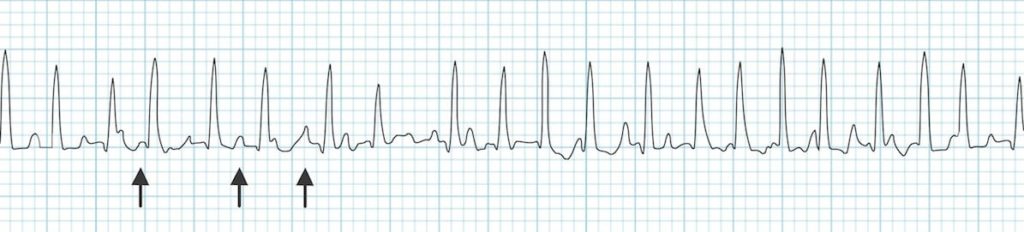
Atrial premature beat (APB)
Image courtesy of L. Brent Mitchell, MD.
APBs may be normally, aberrantly, or not conducted and are usually followed by a noncompensatory pause. Aberrantly conducted APBs (usually with right bundle branch block morphology) must be distinguished from premature beats of ventricular origin.
Atrial escape beats are ectopic atrial beats that emerge after long sinus pauses or sinus arrest. They may be single or multiple; escape beats from a single focus may produce a continuous rhythm (called ectopic atrial rhythm). Heart rate is typically slower, P wave morphology is typically different, and PR interval is slightly shorter than in sinus rhythm.
Atrial tachycardia is a regular rhythm caused by the consistent, rapid atrial activation from a single atrial focus. Heart rate is usually 150 to 200 beats/minute; however, with a very rapid atrial rate, nodal dysfunction, and/or digitalis toxicity, atrioventricular (AV) block may be present, and ventricular rate may be slower. Mechanisms include enhanced atrial automaticity and intra-atrial reentry.
Atrial tachycardia is the least common form (5%) of paroxysmal supraventricular tachycardia and usually occurs in patients with a structural heart disorder. Other causes include atrial irritation (eg, pericarditis
Symptoms are those of other tachycardias (eg, light-headedness, dizziness, palpitations, and rarely syncope).
Diagnosis is by electrocardiography (ECG); P waves, which differ in morphology from normal sinus P waves, precede QRS complexes but may be hidden within the preceding T wave (see figure True atrial tachycardia ).
True atrial tachycardia
Vagal maneuvers may be used to slow the heart rate, allowing visualization of P waves when they are hidden, but these maneuvers do not usually terminate the arrhythmia (demonstrating that the AV node is not an obligate part of the arrhythmia circuit).
Treatment involves managing causes and slowing ventricular response rate using a beta-blocker or calcium channel blocker. An episode may be terminated by direct current cardioversion . Pharmacologic approaches to termination and prevention of atrial tachycardia include antiarrhythmic drugs in class Ia, Ic, or III. If these noninvasive measures are ineffective, alternatives include overdrive pacing and ablation .
Multifocal atrial tachycardia (chaotic atrial tachycardia) is an irregularly irregular rhythm caused by the random discharge of multiple ectopic atrial foci. By definition, heart rate is > 100 beats/minute. On ECG, P-wave morphology differs from beat to beat, and there are ≥ 3 distinct P-wave morphologies. The presence of P waves distinguishes multifocal atrial tachycardia from atrial fibrillation . Except for the rate, features are the same as those of wandering atrial pacemaker. Symptoms, when they occur, are those of rapid tachycardia. Multifocal atrial tachycardia can be due to an underlying pulmonary disorder such as chronic obstructive pulmonary disease coronary artery disease , and electrolyte abnormalities such as hypokalemia . Treatment is directed at the underlying disorder.
Nonparoxysmal junctional tachycardia is caused by abnormal automaticity in the AV node or adjacent tissue, which typically follows open heart surgery, acute inferior myocardial infarction, myocarditis, or digitalis toxicity. Heart rate is 60 to 120 beats/minute; thus, symptoms are usually absent. ECG shows regular, normal-appearing QRS complexes without identifiable P waves or with retrograde P waves (inverted in the inferior leads) that occur shortly before ( < 0.1 second) or after the QRS complex. The rhythm is distinguished from paroxysmal supraventricular tachycardia by the lower heart rate and gradual onset and offset. Treatment is directed at causes.
Wandering atrial pacemaker (multifocal atrial rhythm) is an irregularly irregular rhythm caused by the random discharge of multiple ectopic atrial foci. By definition, heart rate is ≤ 100 beats/minute. Except for the rate, features are the same as those of multifocal atrial tachycardia. Treatment is directed at causes.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.

A. KESH HEBBAR, M.D., AND WILLIAM J. HUESTON, M.D.
A more recent article on common types of supraventricular tachycardia is available.
Am Fam Physician. 2002;65(12):2479-2487
This is part I of a two-part article on common arrhythmias. Part II, “Ventricular Arrhythmias and Arrhythmias in Special Populations,” appears on page 2491 of this issue.
Family physicians frequently encounter patients with symptoms that could be related to cardiac arrhythmias, most commonly atrial fibrillation or supraventricular tachycardias. The initial management of atrial fibrillation includes ventricular rate control to provide adequate cardiac output. In patients with severely depressed cardiac output and recent-onset atrial fibrillation, immediate electrical cardioversion is the treatment of choice. Hemodynamically stable patients with atrial fibrillation for more than two days or for an unknown period should be assessed for the presence of atrial thrombi. If thrombi are detected on transesophageal echocardiography, anticoagulation with warfarin for a minimum of 21 days is recommended before electrical cardioversion is attempted. Patients with other supraventricular arrhythmias may be treated with adenosine, a calcium channel blocker, or a short-acting beta blocker to disrupt reentrant pathways. When initial medications are ineffective, radiofrequency ablation of ectopic sites is an increasingly popular treatment option.
Heart palpitations and cardiac arrhythmias are common problems encountered by family physicians. Patients may present with acute cardiac rhythm abnormalities. Although these arrhythmias are usually benign, they can indicate significant underlying heart disease. More often, patients have chronic arrhythmias, such as atrial fibrillation, that may require treatment to reduce the risk of future complications. The challenges for the family physician are to determine which arrhythmias are benign and which indicate probable cardiac malfunction, and to manage recurrent or chronic rhythm abnormalities.
This two-part article reviews common atrial and ventricular arrhythmias, with a focus on initial management decisions. Part I discusses supraventricular arrhythmias. Part II discusses ventricular arrhythmias and the management of rhythm abnormalities in special populations, including pregnant women, athletes, and children.
Atrial Fibrillation
Atrial fibrillation is the most common cardiac arrhythmia family physicians are likely to encounter. This rhythm abnormality affects 3 to 5 percent of patients more than 60 years of age 1 and becomes increasingly common with advancing age. The median age of patients with atrial fibrillation is 75 years, and the prevalence of the arrhythmia doubles every 10 years after the age of 55. 2 , 3 In the United States, atrial fibrillation is estimated to affect almost 9 percent of patients more than 75 years of age. 2
Most risk factors for atrial fibrillation are associated with structural or ischemic heart disease. Risk factors include hypertension, left ventricular hypertrophy, dilated and restrictive cardiomyopathies, coronary artery disease, chronic obstructive pulmonary disease, and diabetes in women. 1
The annual risk of stroke in patients with atrial fibrillation and normal valve function has been reported to be 4.5 percent per year. 4 Anticoagulation with warfarin (Coumadin) reduces the risk by about two thirds. 4 The mortality rate for stroke in patients with atrial fibrillation is approximately twice as high as the rate in patients without this rhythm abnormality. 5 Although anticoagulation is contraindicated in some elderly patients, a study in Great Britain 6 found that about 60 percent of patients identified in community screenings as having atrial fibrillation were eligible for, and would benefit from, this treatment.
The first step in managing a patient with atrial fibrillation is to decide whether there is a high likelihood of safe conversion to sinus rhythm or whether the patient should be allowed to remain in atrial fibrillation. A patient with recent onset of atrial fibrillation (within the previous 12 months) and no evidence of enlargement of the left atrium has a greater chance of achieving and maintaining sinus rhythm. If the arrhythmia is long-standing and the patient is not a suitable candidate for rate cardioversion, initial treatment should focus on ventricular rate control, with consideration given to long-term stroke prophylaxis.
Restoration of Sinus Rhythm
Patients who present within 48 hours of the onset of new atrial fibrillation are candidates for cardioversion with a low risk of embolism. Conversion to sinus rhythm can be attempted by electrical shock or with antiarrhythmic drugs. Patients who have been in atrial fibrillation for more than 48 hours or for an undetermined period are more likely to have atrial thrombi and may develop emboli with immediate electrical or medical (pharmacologic) cardioversion.
Atrial thrombi are not evident on transthoracic echocardiograms, but they can been seen on transesophageal echocardiograms. 7 If the transesophageal echocardiogram reveals thrombi, anticoagulation is recommended before cardioversion is attempted. Anticoagulation can be accomplished using warfarin, with the dosage adjusted to achieve an International Normalized Ratio (INR) between 2.0 and 3.0 for a minimum of 21 days. 8
If the transesophageal echocardiogram does not show thrombi on multiplane views, cardioversion can be attempted. Short-term anticoagulation with heparin should be started before the procedure, and warfarin therapy should be initiated after cardioversion. 8
When rhythm conversion is indicated, it can be accomplished using direct-current cardioversion or pharmacologic therapy. Synchronized cardioversion is currently considered the treatment of choice for the restoration of sinus rhythm and, in appropriately selected patients, has a success rate of at least 80 percent. 4 Cardioversion is also indicated in patients with hypotension, angina, heart failure, or other evidence of severe compromise caused by atrial fibrillation. 5
Medical cardioversion of atrial fibrillation may be achieved with class IA drugs (quinidine, disopyramide [Norpace], procainamide [Procanbid]) or with amiodarone (Cordarone). In the past, quinidine was frequently used for both cardioversion and maintenance of sinus rhythm in patients who had undergone electrical cardioversion. However, because of the proarrhythmic action of class IA agents and their detrimental effects on left ventricular function, these drugs are now used less often than amiodarone for primary therapy of atrial fibrillation. 4
Amiodarone therapy is successful in 86 percent of patients who have had atrial fibrillation for less than two years. 4 , 9 Treatment is also effective in 40 to 60 percent of patients with long-standing atrial fibrillation that has been resistant to other agents and to electrical cardioversion. 4 Amiodarone can be given in a dosage of 200 mg a day, which is lower than the dosages that have been associated with thyroid abnormalities and pulmonary fibrosis. Although there is little risk of toxicity when amiodarone is given in a low dosage, it is prudent to monitor patients for the development of thyroid, pulmonary, hepatic, and cardiac side effects.
Findings on the usefulness of various agents for the conversion of atrial fibrillation, based on the evidence-based practice program of the Agency for Healthcare Research and Quality, are summarized in Table 1 . 10 Although drugs such as digitalis preparations and sotalol (Betapace) are sometimes used for rate control, they are not effective for converting atrial fibrillation to sinus rhythm. 10 , 11
If external electrical cardioversion is unsuccessful and antiarrhythmic drug therapy fails, other measures can be used. However, these approaches are usually reserved for use in patients who cannot tolerate atrial fibrillation and patients who have associated systolic dysfunction. Techniques include internal electrical cardioversion through the application of electrical current to pulmonary veins via a transcatheter cathode 4 and radiofrequency ablation of the atrioventricular node with insertion of a ventricular pacemaker. 12 In addition, an implantable atrial defibrillator can be used to provide rapid cardioversion in patients with atrial fibrillation that cannot be controlled with medications. 13
Rate Control in Chronic Atrial Fibrillation
In patients in whom rhythm conversion is not indicated or those who have new-onset atrial fibrillation with a rapid ventricular response, treatment may be needed to control the ventricular rhythm. Excessive ventricular rates may result in diminished cardiac output because of poor filling time, and in ischemia because of increased myocardial oxygen demand. Medications used for ventricular rate control in patients with atrial fibrillation are listed in Table 2 . 14
Acute management of ventricular rates can usually be achieved with intravenously administered diltiazem (Cardizem), given in an initial bolus of 15 to 20 mg (0.25 mg per kg) over two minutes, or with an intravenously administered beta blocker such as propranolol (Inderal), given in a dose of 0.5 to 1 mg (up to 3 to 5 mg if needed).
A number of medications, including calcium channel blockers, beta blockers, and digoxin (Lanoxin), are effective for maintaining ventricular rates within acceptable ranges. Because calcium channel blockers are associated with better exercise tolerance, they may be preferable to beta blockers. 15 Digoxin is associated with a high degree of exercise intolerance; therefore, it should be reserved for use in patients who are relatively immobile, who cannot tolerate other treatment options, or who have significant ventricular dysfunction.
Paroxysmal Supraventricular Tachycardias
Based on duration, supraventricular tachycardias are usually categorized as paroxysmal, persistent, or chronic. Paroxysmal supraventricular tachycardia (PSVT) is the most common of these arrhythmias and the one that is most often encountered in the primary care setting. Longer-duration supraventricular tachycardias can be treated similarly to PSVT, but cardiology consultation is often required to identify the electrophysiologic mechanism responsible for sustaining the arrhythmia. In contrast to ventricular tachycardias (discussed in part II of this article) and atrial fibrillation, PSVT is usually a narrow-complex tachycardia with a regular rate.
Atrioventricular Nodal Reentry Causing PSVT
Atrioventricular nodal reentry, the most common mechanism of PSVT, occurs when two pathways exist with different conduction rates. A premature atrial complex that is blocked in the fast pathway and redirected through the slow pathway usually triggers the tachycardia ( Figure 1 ) . The electrical signal proceeds down the slow pathway and then reenters the fast pathway in a retrograde direction. By the time the signal has propagated down the slow pathway and back around on the fast pathway, the slow pathway is no longer refractory and is ready to conduct the signal again, completing a continuous circuit.
Reentrant tachycardias usually produce a narrow-complex tachycardia with no discernible P wave. The rate is usually between 160 and 190 beats per minute. In a less common form of atrioventricular nodal reentrant tachycardia, the circulating wavefront proceeds in an antegrade fashion down the fast pathway and in a retrograde fashion up the slow pathway. In this form, inverted P waves ( Figure 2 ) are clearly visible in lead II of the electrocardiogram (ECG).
It is important to note that atrioventricular nodal reentrant tachycardia can result in a wide-complex tachycardia if the patient has preexisting bundle branch block.
Accessory Pathways Causing PSVT
Accessory pathways (Wolff-Parkinson-White syndrome) and other bypass tracts can cause PSVT. In patients with Wolff-Parkinson-White syndrome, a shortened PR interval and a slurred upstrike to the QRS complex “delta wave” on the resting ECG indicate the presence of an accessory pathway ( Figure 3 ) .
It should be noted that the resting ECG may be normal in some patients with Wolff-Parkinson-White syndrome, because of the inability of the accessory pathway to conduct in the antegrade direction. The usual mechanism of PSVT in this setting is antegrade conduction down the normal pathways through the atrioventricular node and retrograde conduction through the accessory pathway.
The ECG in an atrial arrhythmia with an accessory pathway usually shows a narrow-complex tachycardia at rates of 160 to 240 beats per minute. Delta waves are absent because the normal pathways are used for ventricular activation. Inverted P waves may be seen in the inferior leads. In a much less common form of PSVT, antegrade conduction is down the bypass tract and results in a wide-complex tachycardia.
Increased Automaticity Causing PSVT
Increased automaticity usually occurs when the atrium is enlarged, as in patients with chronic lung disease, congestive heart failure, or electrolyte and acid-base disturbances. Usually, the stretched atria fire irregularly, producing multiple premature beats that emanate from different areas of the atria. Because the foci for the ectopic beats are in multiple sites, the P waves vary in morphology, giving rise to the term “multifocal atrial tachycardia.”
The diagnosis of multifocal atrial tachycardia depends on the identification of an irregular rhythm with three or more different P-wave morphologies. The rate is usually between 130 and 180 beats per minute. Treatment is directed at correcting the underlying cause. Antiarrhythmic drugs are usually not helpful.
In most patients, PSVT is benign and self-limited. However, some patients can have angina, hypotension, and intense anxiety. The first step in the management of PSVT is to determine whether the patient is hemodynamically stable. If PSVT is sustained and there is any indication of instability (i.e., angina, shortness of breath, decreased level of consciousness, hypotension, or congestive heart failure), electrical cardioversion should be performed urgently.
If the symptoms are restricted to discomfort (e.g., palpitations and anxiety), conservative measures should be applied. Conservative management of PSVT can include both nonpharmacologic and pharmacologic measures ( Table 3 ) . 16
Vagal maneuvers to increase parasympathetic tone and slow conduction through the atrioventricular node should be the first approach. Patients should be taught some of these maneuvers for use in future episodes. They should also be instructed to avoid inciting factors, such as caffeine, tobacco, alcohol, pseudoephedrine, and stress. Carotid sinus massage can be attempted, but its role hasbecome more limited because of the effectiveness of drug therapy and the risk of embolism from carotid pressure in some patients.
The goal of pharmacologic management is to slow or block atrioventricular nodal conduction. Agents used for this purpose include adenosine (Adenocard), calcium channel blockers (verapamil [Calan] or diltiazem), and beta blockers (e.g., esmolol [Brevibloc]).
Adenosine is an ultra–short-acting agent that is cleared quickly (half-life of 1 to 6 seconds). This agent is given intravenously in an initial dose of 6 mg, which is followed by one or two 12-mg boluses. Adenosine works by reducing conductance along the slow antegrade pathway. Side effects include flushing, dyspnea, and chest pain. Because of the short half-life of adenosine, these effects are usually very brief and do not ordinarily result in complications.
One advantage of adenosine is that it lacks the negative inotropic effects of calcium channel blockers. Adenosine can also decrease the sinus rate transiently and produce a “rebound” sinus tachycardia. Adenosine should not be used in patients with heart transplants, because such patients may be too sensitive to its effects. 17
Calcium channel blockers can also be used to disrupt a reentrant pathway. Verapamil can be given in a 5- to 10-mg bolus over 2 minutes, followed by 10 mg in 15 to 30 minutes if the initial dose does not convert the arrhythmia. 18 Verapamil and other calcium channel blockers should not be used in patients with an undiagnosed wide-complex tachycardia, because of the risk of fatal hypotension or ventricular fibrillation if the arrhythmia is actually ventricular tachycardia and not PSVT. 19
Intravenously administered diltiazem is also effective. 20 Initial treatment consists of a bolus of 0.25 mg per kg administered over two minutes. A repeat bolus of 0.35 mg per kg given over two minutes can be administered 15 minutes later.
Esmolol, a short-acting beta blocker, can be given in an intravenous bolus of 0.5 mg per kg over 1 minute or in an infusion at a rate of 0.5 mg per kg per minute after an initial loading dose of 0.5 mg per kg. An advantage of esmolol over other beta blockers is its short half-life (four to five minutes), compared with the much longer half-lives (three hours or more) of most other beta blockers. Because of a similar depressive effect on left ventricular contractility, esmolol should be used with caution if initial treatment with a calcium channel blocker is not successful.
Other antiarrhythmic drugs, including quinidine, procainamide, flecainide (Tambocor), and amiodarone, may be used in patients who do not respond to initial medications. However, selective radiofrequency ablation is rapidly becoming the treatment of choice in this situation.
Long-term control of recurrent PSVT caused by atrioventricular nodal reentry may be achieved with pharmacologic therapy or radiofrequency ablation. Patients who have infrequent, well-tolerated recurrences may manage these episodes with self-administered physiologic maneuvers.
Radiofrequency ablation is now used early in the management of patients with PSVT caused by an accessory pathway (Wolff-Parkinson-White syndrome), atrioventricular nodal reentrant tachycardia, or atrial tachycardia. 21 The success rate for radiofrequency ablation is 95 percent in patients with an accessory pathway or atrioventricular nodal reentrant tachycardia, and approximately 80 percent in patients with atrial tachycardia. 21
Other Atrial Arrhythmias
Sinus arrhythmia.
Sinus arrhythmia is usually a normal event in young persons and athletes. In fact, it occurs with such high frequency that it may considered a normal variant rather than a true arrhythmia.
There are two forms of sinus arrhythmia. In the “respiratory” form, the RR interval shortens during inspiration and slows during expiration. Breath-holding eliminates the variation. In the “nonrespiratory” form, the same phasic variation is seen in the RR interval but is not related to respirations. This form of sinus arrhythmia occurs in elderly patients, patients with digoxin overdose, and patients with increased intracranial pressure.
Sinus arrhythmia is usually asymptomatic. Sometimes, however, the long pauses can cause dizziness or syncope. Treatment is usually unnecessary.
WANDERING ATRIAL PACEMAKER
Patients with wandering atrial pacemaker are usually not symptomatic. The condition is most often an isolated finding on the ECG and requires no treatment. Sometimes it is noted on physical examination as an irregularly irregular rhythm.
With wandering atrial pacemaker, the ECG shows variable P-wave morphology and PR intervals. The atrial impulses conduct in a 1:1 fashion and usually control the rhythm for several beats before shifting to another focus. The normal heart rate in wandering atrial pacemaker differentiates this condition from multifocal atrial tachycardia.
PREMATURE ATRIAL COMPLEXES
A premature atrial complex is generated from an ectopic focus in the atria. Therefore, the P wave is usually different in morphology from the usual sinus P wave. The impulse conducts along the normal pathways, generating a narrow QRS complex followed by a pause. Sometimes the premature atrial complex is not conducted and can mimic heart block ( Figure 4 ) .
Premature atrial complexes are found in a variety of settings, including the excessive consumption of caffeine or alcohol and the use of sympathomimetic drugs. These complexes can also be present in patients with structural heart disease.
Patients with premature atrial complexes are usually asymptomatic and require no treatment. A beta blocker given in a low dosage can be tried in patients with uncomfortable symptoms, but no studies of efficacy have been reported. Patients should be counseled to decrease their intake of caffeine, tobacco, and alcohol, and their use of over-the-counter sympathomimetic substances, which are often present in cold medicines and weight-loss preparations.
It is important to note that premature atrial complexes sometimes precipitate supraventricular tachycardia, atrial flutter, or atrial fibrillation.
Sinus Nodal Arrhythmias
Sinus pause and sinoatrial exit block.
Sinus pause or arrest occurs when the sinoatrial node fails to discharge. The ECG shows a pause in the sinus rhythm, with no preceding P wave. Patients usually have no symptoms, but if the pause is prolonged, they may have lightheadedness, palpitations, syncope, and falls. In sinus arrest, the length of the pause has no relationship to the PP interval. Sinoatrial exit block is recognized by the pauses being multiples of PP intervals.
Sinus node dysfunction is usually caused by drugs such as digoxin, quinidine, or procainamide. It can also be caused by ischemia, myocarditis, or fibrosis.
From a therapeutic standpoint, it is probably not important to distinguish between sinus arrest and sino-atrial exit block. Both can occur in well-trained athletes 22 and can be a factor in sick sinus syndrome. 23
SICK SINUS SYNDROME
The term “sick sinus syndrome” encompasses a number of abnormalities, including sinus bradycardia, sinus arrest or exit block, combinations of sinoatrial and atrioventricular nodal conduction disturbances, and atrial tachyarrhythmias. More than one of these arrhythmias may be recorded in the same patient (bradycardia-tachycardia syndrome).
The abnormalities in sick sinus syndrome are usually due to ischemia, fibrosis, or drug-induced or autonomic dysfunction. Signs and symptoms are related to cerebral hypoperfusion and reduced cardiac output.
Treatment of recurrent symptomatic bradycardia or prolonged pauses requires implantation of a permanent pacemaker. 24
Levy S. Epidemiology and classification of atrial fibrillation. J Cardiovasc Electrophysiol. 1998;9(8 suppl):S78-82.
Ryder KM, Benjamin EJ. Epidemiology and significance of atrial fibrillation. Am J Cardiol. 1999;84(9A):R131-8.
Benjamin EJ, Levy D, Vaziri SM, D'Agostino RB, Belanger AJ, Wolf PA. Independent risk factors for atrial fibrillation in a population-based cohort. The Framingham Heart Study. JAMA. 1994;271:840-4.
Golzari H, Cebul RD, Bahler RC. Atrial fibrillation: restoration and maintenance of sinus rhythm and indications for anticoagulation therapy. Ann Intern Med. 1996;125:311-23.
Pritchett EL. Management of atrial fibrillation. N Engl J Med. 1992;326:1264-71.
Sudlow M, Thomson R, Thwaites B, Rodgers H, Kenny RA. Prevalence of atrial fibrillation and eligibility for anticoagulants in the community. Lancet. 1998;352:1167-71.
Falk RH. Atrial fibrillation. N Engl J Med. 2001;344:1067-78.
Manning WJ, Silverman DI, Keighley CS, Oettgen P, Douglas PS. Transesophageal echocardiographically facilitated early cardioversion from atrial fibrillation using short-term anticoagulation: final results of a prospective 4.5-year study. J Am Coll Cardiol. 1995;25:1354-61.
Santos AL, Aleixo AM, Landieri J, Luis AS. Conversion of atrial fibrillation to sinus rhythm with amiodarone. Acta Med Port. 1979;1:15-23.
Management of new onset atrial fibrillation. Summary, evidence report/technology assessment: no. 12. Rockville, Md.: Agency for Healthcare Research and Quality, May 2000; AHRQ publication no. 00-E006. Retrieved April 23, 2002, from www.ahcpr.gov/clinic/epcsums/atrialsum.htm .
Falk RH, Knowlton AA, Bernard SA, Gotlieb NE, Battinelli NJ. Digoxin for converting recent-onset atrial fibrillation to sinus rhythm. A randomized, double-blinded trial. Ann Intern Med. 1987;106:503-6.
Pappone C, Rosanio S, Oreto G, Tocchi M, Gugliotta F, Vicedo-mini G, et al. Circumferential radiofrequency ablation of pulmonary vein ostia: a new anatomic approach for curing atrial fibrillation. Circulation. 2000;102:2619-28.
Swerdlow CD, Schsls W, Dijkman B, Jung W, Sheth NV, Olson WH, et al. Detection of atrial fibrillation and flutter by a dual-chamber implantable cardioverter-defibrillator. For the Worldwide Jewel AF Investigators. Circulation. 2000;101:878-85.
Physicians' desk reference. 56th ed. Montvale, N.J.: Medical Economics, 2002.
Segal JB, McNamara RL, Miller MR, Kim N, Goodman SN, Powe NR, et al. The evidence regarding the drugs used for ventricular rate control. J Fam Pract. 2000;49:47-59.
Myerburg RJ, Kessler KM, Castellanos A. Recognition, clinical assessment, and management of arrhythmias and conduction disturbances. In: Alexander RW, Schlant RC, Fuster V, eds. Hurst's The heart, arteries and veins. 9th ed. New York: McGraw-Hill, Health Professions Division, 1998:873–942.
O'Nunain S, Jennison S, Bashir Y, Garratt C, McKenna W, Camm AJ. Effects of adenosine on atrial repolarization in the transplanted human heart. Am J Cardiol. 1993;71:248-51.
Rinkenberger RL, Prystowsky EN, Heger JJ, Troup PJ, Jackman WM, Zipes DP. Effects of intravenous and chronic oral verapamil administration in patients with supraventricular tachyarrhyth-mias. Circulation. 1980;62:996-1010.
Stewart RB, Bardy GH, Greene HL. Wide complex tachycardia: misdiagnosis and outcome after emergent therapy. Ann Intern Med. 1986;104:766-71.
Betriu A, Chaitman BR, Bourassa MG, Brevers G, Scholl JM, Bruneau P, et al. Beneficial effect of intravenous diltiazem in the acute management of paroxysmal supraventricular tach-yarrhythmias. Circulation. 1983;67:88-94.
Morady F. Radio-frequency ablation as treatment for cardiac arrhythmias. N Engl J Med. 1999;340:534-44.
Bjornstad H, Storstein L, Meen HD, Hals O. Ambulatory electrocardiographic findings in top athletes, athletic students and control subjects. Cardiology. 1994;84:42-50.
Wu DL, Yeh SJ, Lin FC, Wang CC, Cherng WJ. Sinus automaticity and sinoatrial conduction in severe symptomatic sick sinus syndrome. J Am Coll Cardiol. 1992;19:355-64.
Haywood GA, Katritsis D, Ward J, Leigh-Jones M, Ward DE, Camm AJ. Atrial adaptive rate pacing in sick sinus syndrome: effects on exercise capacity and arrhythmias. Br Heart J. 1993;69:174-8.
Continue Reading
More in afp, more in pubmed.
Copyright © 2002 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Wandering Atrial Pacemaker EKG Interpretation with Rhythm Strip
Ekg features, wandering atrial pacemaker ekg interpretation example.
This website is only for professional medical education. Contact your doctor for medical care. 2024 © MedEdu LLC. All Rights Reserved. Terms & Conditions | About Us | Privacy | Email Us

- Mobile Apps
- Journal Club
- Antibiotics
- Quick Critical Care
- Residency Directory
- Recent Changes
- About WikEM
- Getting Started
- Creating & Editing
- Needed Pages
- Editorial Levels
- Contribution Score
- Elective Guide
- Citing WikEM
- What links here
- Related changes
- Special pages
- Printable version
- Permanent link
- Page information
- Browse properties

- View source
- View history
- Create account

We need you! See something you could improve? Make an edit and help make WikEM better for everyone.
- Wandering atrial pacemaker
- 2 Clinical Features
- 3.1 Palpitations
- 4.2 Diagnosis
- 5 Management
- 6 Disposition
- 8 External Links
- 9 References
- Three or more ectopic foci within the atrial myocardium serve as the pacemaker
- Rate is less than 100bpm (in contrast to MAT )
- Is irregularly irregular therefore sometimes confused with atrial fibrillation and sinus arrhythmia
- Intrinsic cardiac or pulmonary disease
- Metabolic derangements
- Drug toxicity (including Digoxin )
Clinical Features
- Often seen in the extremes of age and in athletes
- Rarely causes symptoms
Differential Diagnosis
Palpitations.
- Narrow-complex tachycardias
- Wide-complex tachycardias
- Second Degree AV Block Type I (Wenckeback)
- Second Degree AV Block Type II
- Third Degree AV Block
- Premature atrial contraction
- Premature junctional contraction
- Premature ventricular contraction
- Sick sinus syndrome
- Acute coronary syndrome
- Cardiomyopathy
- Congenital heart disease
- Congestive heart failure (CHF)
- Mitral valve prolapse
- Pacemaker complication
- Pericarditis
- Myocarditis
- Valvular disease
- Panic attack
- Somatic Symptom Disorder
- Drugs of abuse (e.g. cocaine )
- Medications (e.g. digoxin , theophylline )
- Thyroid storm
- Pulmonary embolism
- Dehydration
- Pheochromocytoma

- ECG should show three distinct P wave morphologies with a ventricular rate <100bpm
- Rarely requires treatment

Disposition
- Outpatient management
- Multifocal atrial tachycardia
- Dysrhythmia
External Links
- Richard Cunningham
- fardis tavangary
- Ross Donaldson
- Privacy policy
- Disclaimers
We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

Day 6: Ectopic Arrhythmias and Triggered Activity
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Day 6: ectopic arrhythmias and triggered activity.
- Interpretations of Sample Tracings
- Full Chapter
- Supplementary Content
Ectopy—a disorder of impulse formation
Mechanisms of ectopic arrhythmias
Ectopic arrhythmias require:
Default—slowing of the normal dominant sinus pacemaker which allows a slower focus to take control, or
Usurpation—an acceleration of a lower pacemaker which takes control by virtue of being faster than the sinus rate
Disorders of the sinus node, such as SA arrest, SA exit block, or excessive vagal tone may allow a lower focus to take control by default
A variety of factors, including digitalis toxicity, hypoxia, electrolyte disturbances, ischemia, or chronic lung disease may stimulate an ectopic focus to accelerate and usurp control from the SA node
Properties of ectopic arrhythmias
Ectopic arrhythmias usually start and stop gradually ( non-paroxysmally )
They are not usually initiated by a premature beat
They may be somewhat irregular
They are not terminated by vagal maneuvers, although AV block may be increased
AV block of varying degrees is frequently present (particularly if digitalis toxicity is the cause)
These arrhythmias are usually quite resistant to treatment with standard class I or III agents
Catheter ablation may be effective if a causative agent cannot be identified or treated
The major ectopic arrhythmias
Wandering atrial pacemaker
Mechanisms and causes
There are three or more ectopic atrial pacemakers
This arrhythmia is typically seen in young healthy persons, particularly athletes
The etiology is uncertain
Heart rate—the heart rate is 60–100 and is usually irregular
ECG morphology ( Day 6-01 )
There are at least three P wave morphologies with varying PR intervals
There is usually moderate variation in the heart rate
Multifocal atrial tachycardia
Caused by multiple ectopic atrial foci
Chronic lung disease is typically the underlying clinical abnormality, although it can also occur in the setting of hypoxia, electrolyte abnormalities, acid-base disturbances, and ischemia (i.e., frequently in the intensive care setting)
ECG morphology ( Day 6-02 )
The rate is 100–140
There is typically 1:1 AV conduction
This arrhythmia is frequently confused with atrial fibrillation; the distinction is an important one since management is usually very different
Ectopic atrial rhythms
A single ectopic atrial focus accelerates and usurps control from the sinus node, or the sinus node slows down and allows an ectopic focus to appear
Digitalis toxicity, electrolyte abnormalities, ischemia, hypoxia, and chronic lung disease are typical causes
ECG morphology ( Day 6-03 ) ( Day 6-04 )
The P waves are of the same morphology but have an abnormal axis, indicating their ectopic origin
The atrial rate may be slightly irregular
AV block of varying degrees is sometimes present (particularly if digitalis toxicity is the cause)
Atrial tachycardia with AV block should be considered a manifestation of digitalis toxicity until proven otherwise ( Day 6-05 )
The atrial rate in atrial tachycardia is usually 140–200
Sign in or create a free Access profile below to access even more exclusive content.
With an Access profile, you can save and manage favorites from your personal dashboard, complete case quizzes, review Q&A, and take these feature on the go with our Access app.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait

Multifocal Atrial Tachycardia (MAT)
- Ed Burns and Robert Buttner
- Jun 4, 2021
Multifocal Atrial Tachycardia (MAT) Overview
- A rapid, irregular atrial rhythm arising from multiple ectopic foci within the atria.
- Most commonly seen in patients with severe COPD or congestive heart failure.
- It is typically a transitional rhythm between frequent premature atrial complexes (PACs) and atrial flutter / fibrillation.
AKA “Chaotic atrial tachycardia”
Electrocardiographic Features
- Heart rate > 100 bpm (usually 100-150 bpm; may be as high as 250 bpm).
- Irregularly irregular rhythm with varying PP, PR and RR intervals.
- At least 3 distinct P-wave morphologies in the same lead.
- Isoelectric baseline between P-waves (i.e. no flutter waves).
- Absence of a single dominant atrial pacemaker (i.e. not just sinus rhythm with frequent PACs).
- Some P waves may be nonconducted; others may be aberrantly conducted to the ventricles.
There may be additional electrocardiographic features suggestive of COPD.
Clinical Relevance
- Usually occurs in seriously ill elderly patients with respiratory failure (e.g. exacerbation of COPD / CHF).
- Tends to resolve following treatment of the underlying disorder.
- The development of MAT during an acute illness is a poor prognostic sign, associated with a 60% in-hospital mortality and mean survival of just over a year. Death occurs due to the underlying illness; not the arrhythmia itself.
Arises due to a combination of factors that are present in hospitalised patients with acute-on-chronic respiratory failure:
- Right atrial dilatation (from cor pulmonale )
- Increased sympathetic drive
- Hypoxia and hypercarbia
- Beta-agonists
- Theophylline
- Electrolyte abnormalities: Hypokalaemia and hypomagnesaemia (e.g. secondary to diuretics / beta-agonists)
The net result is increased atrial automaticity.
ECG Examples
Multifocal atrial tachycardia:
- Rapid irregular rhythm > 100 bpm.
- At least 3 distinctive P-wave morphologies (arrows).
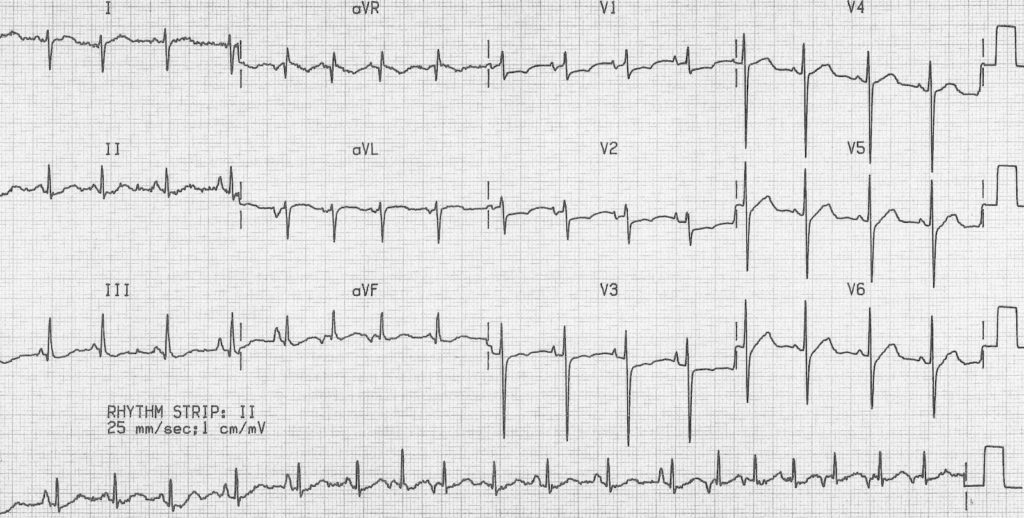
MAT with additional features of COPD :
- Rapid, irregular rhythm with multiple P-wave morphologies (best seen in the rhythm strip).
- Right axis deviation, dominant R wave in V1 and deep S wave in V6 suggest right ventricular hypertrophy due to cor pulmonale.
Related Topics
- The ECG in COPD
- Right atrial enlargement (P pulmonale)
- Right ventricular hypertrophy
Advanced Reading
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course : Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop . Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog .
- Zimmerman FH. ECG Core Curriculum . 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations , 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine . 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care . 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG . 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |

Robert Buttner
MBBS (UWA) CCPU (RCE, Biliary, DVT, E-FAST, AAA) Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Editor-in-chief of the LITFL ECG Library . Twitter: @rob_buttner
Leave a Reply Cancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Privacy Overview
- Find in topic
INTRODUCTION
This topic will review the definition, pathogenesis, etiology, and treatment of MAT in adults. Other tachycardias of atrial origin, as well as the discussion of this arrhythmia in children, are reviewed separately. (See "Focal atrial tachycardia" and "Atrial tachyarrhythmias in children" and "Atrioventricular nodal reentrant tachycardia" and "Atrioventricular reentrant tachycardia (AVRT) associated with an accessory pathway" and "Atrial fibrillation: Overview and management of new-onset atrial fibrillation" .)
DEFINITION, PATHOGENESIS, AND PREVALENCE
Terminology — A number of authors have used the term "chaotic" to describe MAT [ 3-5 ]. However, chaos in modern usage in nonlinear dynamics and mathematics implies there is order in what appear to be random events [ 6 ]. A more accurate term for this arrhythmia is probably "multiform" as there is no proof that the arrhythmia is actually multifocal, although multifocal remains the commonly used term [ 1 ].
The tachycardic threshold for multifocal atrial tachycardia (MAT) has traditionally been set at 100 bpm, but a review of 60 patients with multifocal atrial arrhythmias found a stronger association between the incidence of COPD exacerbations and the diagnosis of MAT if a threshold of 90 bpm was used [ 7 ]. The definition of MAT also requires the presence of at least three distinct P-wave morphologies.
To continue reading this article, you must sign in . For more information or to purchase a personal subscription, click below on the option that best describes you:
- Medical Professional
- Resident, Fellow or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
Print Options
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Indian J Anaesth
- v.60(6); 2016 Jun
Intraoperative wandering atrial pacemaker with isoflurane anaesthesia
Sulagna bhattacharjee.
Department of Anaesthesiology, All India Institute of Medical Sciences, New Delhi, India
Puneet Khanna
Sumit bansal, souvik maitra, associated data.
Wandering atrial pacemaker is an arrhythmia originating from the shifting pacemaker sites from the sinoatrial node to the atria and/or atrioventricular node and back to the sinoatrial node.[ 1 ] We report an incident of wandering atrial pacemaker occurring intraoperatively during surgery for testicular torsion.
A 10-year-old boy, American Society of Anesthesiologists (ASA) physical status I, undergoing surgery for a right-sided testicular torsion had received fentanyl, propofol and atracurium for anaesthesia management. After securing his airway with a ProSeal™ laryngeal mask airway, anaesthesia was maintained with isoflurane, air and oxygen under standard ASA monitoring. During manipulation of the testis, he had an episode of bradycardia with heart rate decreasing from 88/min to 54/min without any hypotension or oxygen desaturation that persisted for about 15 s. This was followed by an arrhythmia with rate of 74–78/min having varyingP wave morphology and PR interval that resolved spontaneously [ Figure 1 and Video 1 ]. We diagnosed it to be a case of wandering atrial pacemaker as the heart rate was between 60 and 100/min, with slight irregularity, beat to beat changing shape and size ofP wave of at least three different forms, varying PR interval but normally appearing QRS complexes.[ 2 ] The likely cause of occurrence of arrhythmia was vagal stimulation caused by testicular manipulation. All commonly used volatile anaesthetic agents including isoflurane are known to cause enhanced automaticity of subsidiary atrial pacemakers,[ 3 ] thereby predisposing to the development of atrial arrhythmias and wandering pacemaker phenomenon. Monitoring and recognising this event for possible haemodynamic compromise are important.

Variant morphology of P wave in lead II
Video available on www.ijaweb.org
Financial support and sponsorship, conflicts of interest.
There are no conflicts of interest.

IMAGES
VIDEO
COMMENTS
Wandering atrial pacemaker (WAP) is an atrial rhythm where the pacemaking activity of the heart originates from different locations within the atria. This is different from normal pacemaking activity, where the sinoatrial node (SA node) is responsible for each heartbeat and keeps a steady rate and rhythm. Causes of wandering atrial pacemaker are unclear, but there may be factors leading to its ...
A wandering atrial pacemaker is a relatively rare condition that is often mistaken as atrial fibrillation, or AFib. ... When that happens and your heart continues to beat at a normal rate, you ...
Wandering Atrial Pacemaker (WAP) is a cardiac rhythm disorder that causes irregular and variable heartbeats. Learn the Heart - Healio provides a comprehensive ECG review of this condition ...
Wandering atrial pacemaker (multifocal atrial rhythm) is an irregularly irregular rhythm caused by the random discharge of multiple ectopic atrial foci. By definition, heart rate is ≤ 100 beats/minute. Except for the rate, features are the same as those of multifocal atrial tachycardia. Treatment is directed at causes.
This rhythm and multifocal atrial tachycardia are similar except for heart rate. The other possible explanation is that there is significant respiratory sinus arrhythmia, with uncovering of latent foci of pacemaker activity. Usually, it is associated with underlying lung disease. In the elderly, it may be a manifestation of sick sinus syndrome.
The normal heart rate in wandering atrial pacemaker differentiates this condition from multifocal atrial tachycardia. PREMATURE ATRIAL COMPLEXES A premature atrial complex is generated from an ...
Wandering atrial pacemaker (WAP) ( Fig. 3.12) is an atrial rhythm with multiple P-wave morphologies (three or more), often occurring in a repetitive pattern at a rate of less than 100 bpm. The pattern may be dependent on autonomic tone and the respiratory phase (with competing activation from the sinus node, AV node, and other areas in the atria).
A wandering atrial pacemaker is a specific arrhythmia that can affect the heart. A condition that affects the rhythm or rate of the heartbeat is known as an arrhythmia. There are wide varieties of arrhythmia, including an irregular beat, an extra beat, and a fast or slow heart rate.
Wandering atrial pacemaker (WAP) is a benign atrial arrhythmia that has been observed in this case study. WAP and multifocal atrial tachycardia (MAT) differ only with the heart rate - WAP has a heart rate less than 100 bpm whereas MAT has a heart rate greater than 100 bpm. In the WAP rhythm, the pacemaker wanders with the impulses originating ...
Rate: Normal (60-100 bpm) Rhythm: May be irregular P Wave: Changing shape and size from beat to beat (at least three different forms) ... Wandering atrial pacemaker is an arrhythmia originating in shifting pacemaker sites from the SA node to the atria and back to the SA node. On an ECG, the p-waves reflect the pacemaker shifts by shape variations.
Wandering atrial pacemaker. Non-arrhythmic cardiac causes: Acute coronary syndrome. Cardiomyopathy. Congenital heart disease. Congestive heart failure (CHF) Mitral valve prolapse. Pacemaker complication. Pericarditis.
The wandering atrial pacemaker has nothing to do with extrinsic cardiac hardware. The sino-atrial node is the natural pacemaker of the heart. Remember also that if P waves all appear similar and they're arriving at a rate of 60 - 100 beats per minute we assume them to be sinus.
Interpretation: Wandering atrial pacemaker. Wandering atrial pacemaker (WAP) occurs when the pacemaker site shifts back and forth between the sinus node and ectopic atrial sites. ... If the heart rate is slow and the patient is symptomatic, treatment of the rhythm is the same as for symptomatic sinus bradycardia with a pulse. When WAP is ...
The pacemaker is activated and delivers a stimulus only when the intrinsic ventricular rate falls below a predetermined lower limit; pacemaker activity is suppressed when …. ECG tutorial: Basic principles of ECG analysis. … block; multifocal atrial rhythm (wandering atrial pacemaker) when the rate is <100 or multifocal atrial tachycardia ...
When the heart rate is less than 100 beats per minute, the arrhythmia is called "wandering atrial pacemaker." Symptoms. Some people may have no symptoms. When symptoms occur, they can include: Chest tightness; Fainting; Lightheadedness; Sensation of feeling the heart is beating irregularly or too fast (palpitations)
It is usually seen in young adults without structural heart disease or ischemic heart disease, and >60% of cases are observed in women. 49 The ventricular rate is often 180 bpm to 200 bpm but ranges from 110 bpm to >250 bpm (and in rare cases, the rate can be <100 bpm). 54 The anatomic substrate of AVNRT is dual AV nodal physiology .
Wandering atrial pacemaker. Mechanisms and causes. There are three or more ectopic atrial pacemakers. This arrhythmia is typically seen in young healthy persons, particularly athletes. The etiology is uncertain. Heart rate—the heart rate is 60-100 and is usually irregular. ECG morphology
Heart rate > 100 bpm (usually 100-150 bpm; may be as high as 250 bpm). Irregularly irregular rhythm with varying PP, PR and RR intervals. At least 3 distinct P-wave morphologies in the same lead. Isoelectric baseline between P-waves (i.e. no flutter waves). Absence of a single dominant atrial pacemaker (i.e. not just sinus rhythm with frequent ...
Patients with multiple P-wave morphologies but a normal heart rate (60 to 100 bpm) are considered to have a wandering atrial pacemaker, since the heart rate does not meet criteria for a tachycardia. (See 'Terminology' below.) This topic will review the definition, pathogenesis, etiology, and treatment of MAT in adults.
We diagnosed it to be a case of wandering atrial pacemaker as the heart rate was between 60 and 100/min, with slight irregularity, beat to beat changing shape and size ofP wave of at least three different forms, varying PR interval but normally appearing QRS complexes. The likely cause of occurrence of arrhythmia was vagal stimulation caused by ...