- Find a Doctor

Coding and Billing Guidelines for Emergency Department
- Provider Service: 800-368-2312
- For Medicaid Expansion: 833-777-5779
- Caring Foundation
- Privacy & Legal
- Our Partners in Health:
Fargo (Headquarters) 4510 13th Ave. S. Fargo, N.D., 58121
Blue Cross Blue Shield of North Dakota is an independent licensee of the Blue Cross Blue Shield Association, serving residents and businesses in North Dakota. All rights reserved.
© 2024 Blue Cross Blue Shield of North Dakota
- Non-Discrimination Notice
- العَرَبِيَّة
- Diné Bizaad
Processing...
Please wait while your form is being submitted

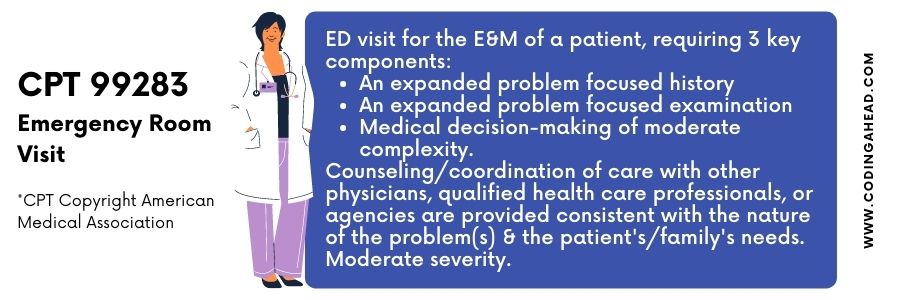
Welcome to our informative guide on the 99283 CPT code for emergency department visits. In this article, we will provide you with a detailed understanding of this code and its significance in healthcare billing and reimbursement. Whether you are a healthcare professional or simply seeking information about ER coding, we’ve got you covered.
When patients visit the emergency department, their medical services are categorized and reported using specific codes. One such code, the 99283 CPT code, is assigned to ER visits that require an expanded problem focused history, an expanded problem focused examination, and medical decision making of moderate complexity. This code is commonly associated with level 3 ER visits, which involve patients with moderate severity presenting problems.
Key Takeaways:
- The 99283 CPT code is used for reporting emergency department visits.
- This code corresponds to level 3 visits, which involve moderate severity presenting problems.
- The code requires an expanded problem focused history, examination, and moderate complexity in medical decision making.
- Accurate coding and documentation are crucial for proper reimbursement.
- Medical Bill Gurus can assist healthcare providers with medical billing services and navigating the reimbursement process for the 99283 code.
Now that we’ve provided you with an overview, let’s dive deeper into the components of the 99283 CPT code and understand its relevance in emergency department visits.
What is a CPT Code?
CPT codes, or Current Procedural Terminology codes, are a set of medical codes used to describe medical procedures and services provided by healthcare professionals. These codes play a crucial role in healthcare billing and reimbursement. They provide a standardized way to communicate the specific procedures and services rendered, allowing for accurate documentation and proper categorization for billing purposes.
One commonly used CPT code in the field of evaluation and management is the 99283 code. This code is specifically assigned to emergency department visits and falls under the category of evaluation and management codes. It is used to report emergency visits that require an expanded problem-focused history, an expanded problem-focused examination, and medical decision making of moderate complexity.
Healthcare providers rely on CPT codes to accurately bill for their services and receive appropriate reimbursement from insurance companies or government programs such as Medicare. These codes serve as a universal language in the healthcare industry, bridging the gap between healthcare providers and payers.
Benefits and Importance of CPT Codes
The utilization of CPT codes offers several benefits:
- Standardization: CPT codes provide a standardized method for documenting and reporting medical procedures and services across various healthcare settings. This uniformity enhances communication and reduces ambiguity.
- Precision in Billing: CPT codes ensure precise billing by accurately representing the complexity and nature of the medical services provided. This helps healthcare providers receive fair and appropriate reimbursement.
- Comparative Analysis: CPT codes allow for comparisons between different procedures and services. These comparisons assist in analyzing healthcare trends, assessing outcomes, and determining the cost-effectiveness of certain treatments.
- Reimbursement: Accurate coding using CPT codes is essential for healthcare providers to receive timely reimbursement for the services they render. Proper documentation and assignment of CPT codes significantly reduce the risk of claim denials.
In summary, CPT codes are a critical component of healthcare billing and reimbursement. They enable accurate representation and communication of medical services, ensure fair reimbursement for healthcare providers, and facilitate efficient analysis of healthcare data. The 99283 code specifically captures the evaluation and management aspects of emergency department visits, providing a well-defined categorization for billing purposes.
Components of the 99283 CPT Code
The 99283 CPT code encompasses three essential components that must be fulfilled for accurate reporting. These components consist of an expanded problem focused history, an expanded problem focused examination, and medical decision making of moderate complexity. Proper documentation should highlight the presence of these components to ensure precise coding and billing.
New Patient Visit – Level 3
When using the 99283 CPT code, the expanded problem focused history involves obtaining a detailed account of the patient’s current condition, symptoms, and medical history. This includes relevant information about the presenting problem, any known allergies or medications, and the patient’s past medical, surgical, and family history.
The expanded problem focused examination requires a systematic assessment of the patient’s affected body areas and organ systems related to the presenting problem. Medical practitioners evaluate the patient’s vital signs, perform targeted physical examinations, and document any observed abnormalities or findings related to the chief complaint.
Medical decision making of moderate complexity involves the evaluation and analysis of the patient’s medical condition, diagnostic test results, and treatment options. The practitioner assesses the information collected during the history and examination to derive a diagnosis, determine the appropriate management plan, and ensure patient safety.
By accurately documenting and fulfilling these three components, healthcare providers can ensure proper coding and billing for emergency department visits that meet the criteria for the 99283 CPT code.
Emergency Department Visits and Coding Guidelines
When it comes to coding emergency department visits, following specific coding guidelines is crucial. According to the Current Procedural Terminology (CPT) definition, an emergency department is a hospital-based facility that provides unscheduled episodic services to patients who require immediate medical attention.
To accurately code an ER visit, it is essential to document the level of history, examination, and medical decision making. This documentation ensures the assignment of the appropriate CPT code, reflecting the complexity of the visit. Proper documentation is essential for accurate coding and compliant billing.
Let’s take a closer look at the key aspects of coding guidelines for emergency department visits.
Documentation Requirements
When coding an emergency department visit, thorough documentation is essential to accurately reflect the level of service provided. The documentation should include:
- A detailed history of the patient’s chief complaint and presenting problems
- A comprehensive examination, including vital signs, physical findings, and any diagnostic tests performed
- Medical decision making that demonstrates the complexity of the patient’s condition and the management involved
By documenting these elements, healthcare providers ensure compliance with coding guidelines and enable accurate coding and billing of emergency department visits.
Coding Guidelines for Emergency Department Visits
When coding an emergency department visit, the key considerations include:
- Selecting the appropriate CPT code based on the complexity of the visit
- Following the CPT guidelines to ensure accurate code assignment
- Adhering to any specific payer requirements or modifiers, if applicable
It is important to note that CPT codes for emergency department visits are categorized based on the level of complexity, such as problem-focused, expanded problem-focused, or detailed examination. Choosing the correct code is crucial for proper reimbursement and compliance with coding guidelines.
Understanding the coding guidelines for emergency department visits is paramount to ensure accurate coding and compliant billing. By carefully documenting the necessary information and selecting the appropriate CPT code, healthcare providers can submit claims that reflect the complexity of the services provided during an emergency department visit.
Reimbursement Process for 99283 CPT Code
Reimbursement for the 99283 CPT code is a critical aspect of the healthcare billing process. The amount of reimbursement received for an emergency department visit depends on various factors, including the payer’s policies and the documentation supporting the level of service provided. Accurate coding and thorough documentation are essential to ensure proper reimbursement for healthcare providers.
At Medical Bill Gurus, we understand the complexities of the reimbursement process and can assist healthcare providers in navigating through the intricacies. Our team of experienced professionals is well-versed in the coding guidelines and documentation requirements for the 99283 CPT code. We can help providers optimize their revenue by ensuring accurate coding and comprehensive documentation.
When it comes to reimbursement, every detail matters. The documentation supporting the level of service provided must align with the assigned CPT code, specifically the expanded problem focused history, expanded problem focused examination, and medical decision making of moderate complexity. By accurately coding and documenting the visit, healthcare providers can maximize their reimbursement and avoid potential claim denials.
Medical Bill Gurus works closely with healthcare providers, offering comprehensive medical billing services tailored to their specific needs. We have extensive experience in navigating the reimbursement process, ensuring that our clients receive the appropriate reimbursement for the services they provide. With our expertise, you can focus on delivering quality patient care while we handle the complex billing and reimbursement processes.
Trust Medical Bill Gurus to be your partner in optimizing revenue and streamlining the reimbursement process. Contact us today to learn more about our medical billing services and how we can assist you in navigating the reimbursement process for the 99283 CPT code.
Medical Bill Gurus – Your Medical Billing Company
At Medical Bill Gurus, we understand the complexities of medical billing and the importance of accurate coding for healthcare providers. Led by President Daniel Lynch, our team specializes in providing comprehensive medical billing services tailored to the unique needs of each provider.
With our expertise in working with all insurance payers, including Medicare, we can help you optimize your revenue through accurate coding and billing practices. Our dedicated team is committed to ensuring your financial success by staying up-to-date with the latest coding guidelines and reimbursement processes.
When you partner with Medical Bill Gurus, you can expect:
- Accurate and timely submission of claims
- Thorough documentation and coding reviews to maximize reimbursement
- Personalized support and guidance throughout the billing process
- Transparent reporting to track your revenue and identify areas for improvement
- Compliance with HIPAA rules and regulations to protect patient confidentiality
Our goal is to streamline your billing operations, reduce administrative burden, and help you focus on providing quality patient care. Trust Medical Bill Gurus to be your dedicated partner in medical billing.
The Importance of Accurate Coding
Accurate coding is crucial for healthcare providers as it directly impacts the reimbursement they receive for their services. Proper coding ensures that the services provided are reflected accurately in billing claims, which in turn affects reimbursement rates. Accurate documentation is essential to support the assigned codes and prevent denial of claims.
Why Accurate Coding Matters
Accurate coding plays a significant role in healthcare billing and reimbursement. When the wrong code is assigned or documented inaccurately, it can result in payment delays, denials, or even potential legal issues. Healthcare providers rely on accurate coding to receive fair compensation for their services and maintain financial stability.
Accurate coding also helps healthcare providers in the following ways:
- Transparent and Consistent Billing: Accurate coding ensures that the services provided are transparently communicated through billing claims. It allows payers, such as insurance companies, to understand the nature and complexity of the services rendered.
- Avoidance of Overbilling or Underbilling: Accurate coding prevents overbilling, which can result in audits, financial penalties, and damaged professional reputation. Conversely, underbilling can lead to revenue loss and unsustainable financial practices.
- Compliance with Regulatory Standards: Proper coding ensures compliance with regulatory standards, such as the Healthcare Common Procedure Coding System (HCPCS) and the International Classification of Diseases (ICD). Adhering to these standards helps healthcare providers avoid legal and compliance issues.
The Role of Documentation
Accurate documentation is a crucial component of accurate coding. It provides evidence to support the assigned codes and justifies the level of service provided. Comprehensive and detailed documentation helps healthcare providers avoid claim denials and provides a clear record of the patient’s condition and treatment.
Documentation should:
- Include relevant patient information, such as medical history, chief complaint, and relevant clinical findings.
- Specify the complexity of the medical decision making involved.
- Outline the extent of the problem-focused history and examination conducted.
Proper documentation should align with the coding guidelines and accurately reflect the services rendered. It is essential to maintain clear and consistent records that can withstand audits or reviews.
Accurate coding and documentation are essential components of efficient healthcare billing and reimbursement. By ensuring the right codes are assigned and supported by comprehensive documentation, healthcare providers can maximize their revenue, maintain compliance, and provide quality care to their patients.
Understanding the Level 3 ER Visit
When a patient presents with moderate severity problems in the emergency department, it is typically categorized as a level 3 ER visit. The 99283 CPT code is commonly assigned to these visits, as it reflects the expanded problem focused history, expanded problem focused examination, and medical decision making of moderate complexity involved in the evaluation and management of the patient.
Coding Reminder and HIPAA Rules
When it comes to coding and reimbursement processes, it is crucial to stay updated with the ever-evolving coding rules and guidelines. At our company, we prioritize compliance with the Health Insurance Portability and Accountability Act (HIPAA) rules, which govern medical code sets such as CPT, HCPCS, and ICD-9-CM. By adhering to these regulations, we ensure the privacy and security of patient health information while accurately documenting and coding medical services.
It is essential to use valid codes that are relevant to the date of service. Submitting or accepting only valid codes prevents coding errors and promotes accurate billing and reimbursement. We are continuously monitoring coding changes and updates to provide our clients with the most up-to-date coding practices and ensure compliance with HIPAA guidelines.
As coding guidelines continue to evolve, it is crucial for healthcare providers to partner with a trusted medical billing company that has a deep understanding of these changes and can navigate through the coding process effectively. At Medical Bill Gurus, we are committed to providing reliable and accurate medical billing services while adhering to the latest coding guidelines and HIPAA rules.
Stay informed and compliant with our expert team of medical billers who are well-versed in coding practices and HIPAA regulations. Let us handle your medical coding and billing needs, allowing you to focus on delivering exceptional patient care. Trust our expertise and experience in maximizing your revenue while ensuring compliance with coding rules and HIPAA guidelines.
Key Features of Our Coding Reminder and HIPAA Compliance:
- Regular updates on coding changes and guidelines
- Awareness of HIPAA rules and regulations
- Adherence to coding standards and best practices
- Accurate documentation and coding of medical services
- Secure handling of patient health information
Let us help you navigate the complex world of medical coding and reimbursement, ensuring compliance with HIPAA rules and optimizing your revenue. Contact us today to learn more about our comprehensive medical billing services.
Contact Medical Bill Gurus
If you have any questions or need assistance with medical billing services, you can contact our provider services at the following phone numbers:
- (651) 662-5200
- Toll-free: 1-800-262-0820
Our dedicated team at Medical Bill Gurus is ready to address any inquiries you may have. Whether you need help with coding, billing, or navigating the reimbursement process, we are here to assist you. Contact us today to learn more about our comprehensive medical billing services.
Medicare Guidelines for the 99283 CPT Code
When it comes to the 99283 CPT code, Medicare follows specific guidelines for reimbursement and documentation. It’s important to understand these guidelines in order to ensure proper reimbursement for Medicare patients. Here are some key points to keep in mind:
Reimbursement Rates
The reimbursement rates for the 99283 code may vary for Medicare patients. Medicare sets national facility and non-facility total payment rates for this code. It’s essential to check the specific reimbursement rates applicable to your region to ensure accurate billing. The table below provides an overview of the Medicare reimbursement rates for the 99283 code:
Note: The reimbursement rates provided in the table are for illustrative purposes only and may not reflect current rates. Please refer to the official Medicare documentation for the most up-to-date reimbursement rates.
Proper documentation is crucial when coding and billing for Medicare patients. Medicare has specific documentation requirements that must be met to support the level of service provided. It’s essential to accurately document the expanded problem focused history, expanded problem focused examination, and medical decision making of moderate complexity. Failure to meet these documentation requirements may result in claim denials or audits.
We understand the importance of adhering to Medicare guidelines, which is why at Medical Bill Gurus, we stay up-to-date with the latest coding and billing regulations. Our team of experts can assist you in navigating the Medicare reimbursement process, ensuring accurate coding and maximizing your revenue. Contact us today to learn more about our medical billing services.
Reimbursement Rates for 99283 CPT Code
The reimbursement rates for the 99283 CPT code can vary depending on the payer and geographic location. It is crucial to understand these rates to ensure accurate billing and reimbursement. Medicare, for example, sets national facility and non-facility payment rates for the 99283 code.
Here is an overview of the reimbursement rates for the 99283 CPT code:
Please note that these rates are for illustrative purposes only and may not represent the current reimbursement rates. It is essential to check with each specific payer to determine the accurate rates for the 99283 CPT code.
Global Days and CPT Coding
The concept of global days does not apply to the 99283 CPT code. Global periods are timeframes during which all related services for a procedure or surgery are considered part of the initial service and are not billed separately. However, this concept does not apply to the 99283 code since ER visits are typically standalone services.
When it comes to the 99283 CPT code, there is no need to worry about global periods or bundled services. This code specifically captures the evaluation and management of patients in the emergency department, and each visit is treated as a separate entity. It means that all the services provided during an ER visit, from the history and examination to the medical decision-making, can be coded and billed independently.
Unlike surgical procedures that have healing periods and post-operative care included in global periods, ER visits are not subject to the same rules. Therefore, you can confidently report and code the 99283 CPT code without considering any global days or bundled services.
Next, we’ll dive into more details about the bundled services and related CPT codes for emergency department visits. Stay tuned!
Bundling Information for 99283 CPT Code
The 99283 CPT code encompasses bundled services that are included in the reporting of this code. These bundled services should not be reported separately when the main code, 99283, is used. Included services range from laboratory tests and procedures to counseling and coordination of care with other healthcare professionals.
When using the 99283 CPT code, it’s important to understand which services are bundled and should not be reported separately. This helps ensure accurate coding and billing, preventing potential claim denials and ensuring proper reimbursement. The bundled services for the 99283 code vary depending on the specific circumstances and the medical necessity of the services provided.
To illustrate the bundled services within the 99283 CPT code, the following table provides an overview:
It’s crucial to understand that these bundled services are not reported separately when the 99283 CPT code is used. Proper documentation of the bundled services provided during the ER visit is essential for accurate coding and billing.
Related CPT Codes
When coding for emergency department visits, healthcare providers should be familiar with several related CPT codes. These codes encompass various levels of visits, procedures, and counseling services. It is crucial to carefully review the documentation and select the most appropriate code based on the level of service provided. By accurately coding the services, healthcare providers can ensure proper reimbursement and compliance with billing guidelines.
Commonly Used Related CPT Codes
Below are some commonly used related CPT codes for emergency department visits:
These are just a few examples of the related CPT codes used for emergency department visits. It is essential to consult the complete CPT code set and any applicable coding guidelines to ensure accurate coding and billing.
In conclusion, understanding the 99283 CPT code is crucial for accurate coding and billing of emergency department visits. This code, commonly assigned to level 3 ER visits, reflects the expanded problem focused history, examination, and medical decision making of moderate complexity involved in evaluating and managing patients. By following coding guidelines and accurately documenting the services provided, healthcare providers can ensure proper reimbursement for their efforts.
At Medical Bill Gurus, we offer comprehensive medical billing services to assist healthcare providers in optimizing their revenue and navigating the complex coding and reimbursement process. Our team, led by President Daniel Lynch, specializes in working with all insurance payers, including Medicare. We can help healthcare providers streamline their billing practices and maximize their reimbursement rates.
If you need assistance with your medical billing needs, whether it’s understanding the 99283 CPT code or navigating the reimbursement process, contact Medical Bill Gurus. Our provider services team is available at (651) 662-5200 or toll-free at 1-800-262-0820 to address your inquiries and provide further information about our services. Let us help you optimize your revenue and ensure accurate coding and billing practices.
What is the 99283 CPT code?
The 99283 CPT code is used for reporting emergency department visits that require an expanded problem focused history, an expanded problem focused examination, and medical decision making of moderate complexity. It is often assigned to level 3 ER visits.
What is a CPT code?
CPT codes, or Current Procedural Terminology codes, are a set of medical codes used to describe medical procedures and services provided by healthcare professionals. The 99283 code falls under the category of evaluation and management codes, specifically for emergency department visits.
What are the components of the 99283 CPT code?
The 99283 CPT code requires an expanded problem focused history, an expanded problem focused examination, and medical decision making of moderate complexity.
What are the coding guidelines for emergency department visits?
Emergency department visits have specific coding guidelines that must be followed. It is important to document the level of history, examination, and medical decision making in order to assign the appropriate CPT code.
How does the reimbursement process work for the 99283 CPT code?
Reimbursement for the 99283 CPT code is dependent on various factors, including the payer’s policies and the documentation supporting the level of service provided. Accurate coding and documentation are essential for proper reimbursement.
Who is Medical Bill Gurus?
Medical Bill Gurus is a medical billing company led by President Daniel Lynch. They specialize in providing medical billing services for healthcare providers, assisting with the coding, billing, and reimbursement process.
Why is accurate coding important?
Accurate coding is crucial for healthcare providers as it directly impacts the reimbursement they receive for their services. Proper coding ensures that the services provided are reflected accurately in billing claims, which affects reimbursement rates.
What is a level 3 ER visit?
When a patient presents with moderate severity problems in the emergency department, it is typically categorized as a level 3 ER visit. The 99283 CPT code is commonly assigned to these visits.
What are the coding reminder and HIPAA rules to follow?
All coding and reimbursement processes are subject to changes, updates, and other requirements of coding rules and guidelines. It is important to stay up to date with coding changes and follow the HIPAA rules governing medical code sets.
How can I contact Medical Bill Gurus?
If you have any questions or need assistance with medical billing services, you can contact Medical Bill Gurus’ provider services at (651) 662-5200 or toll-free at 1-800-262-0820.
What are the Medicare guidelines for the 99283 CPT code?
Medicare follows specific guidelines for the 99283 CPT code. Reimbursement rates and documentation requirements may vary for Medicare patients. It is important to adhere to their guidelines when coding and billing for Medicare.
What are the reimbursement rates for the 99283 CPT code?
The reimbursement rates for the 99283 CPT code may vary depending on the payer and the geographic location. Medicare sets national facility and non-facility total payment rates for this code. It is important to check specific reimbursement rates for each payer.
Does the concept of global days apply to the 99283 CPT code?
No, the concept of global days does not apply to the 99283 CPT code. ER visits are typically standalone services and are not subject to global periods.
What bundled services are included in the 99283 CPT code?
The 99283 CPT code has bundled services that are included in the reporting of this code. These bundled services should not be reported separately when the main code, 99283, is used.
Are there any related CPT codes for emergency department visits?
Yes, there are several related CPT codes that healthcare providers should be aware of when coding for emergency department visits. These codes include different levels of visits, procedures, and counseling services.
What is the significance of understanding the 99283 CPT code?
Understanding the 99283 CPT code is essential for accurate coding and billing of emergency department visits. Medical Bill Gurus offers medical billing services to assist healthcare providers in optimizing their revenue and navigating the coding and reimbursement process.
Leave a Comment Cancel Reply
Your email address will not be published. Required fields are marked *


AVAILABLE MON-FRI
From 8 am to 8 pm mst, houston office:.
525 N Sam Houston Pkwy E, Suite #246 Houston, Texas, 77060
Denver Office:
3000 Lawrence Street Suite #15 Denver, CO 80205
Tampa Office:
260 1st Ave S, #34 St Petersburg, Florida 33701
Phoenix Office:
7042 E Indian School Rd #100 Scottsdale, AZ 85251
Copyright © 2024 | All Rights Reserved | Medical Billing Company | XML Sitemap | Privacy Policy | Cookie Policy | HIPPA Compliance Policy
Digital Marketing by Denver Digital Marketing Agency

Free Online Medical Billing and Coding Certification Programs | onlinemedicalcodingandbilling.com
Find medical billing and coding Certification programs and more. Explore videos, curriculum, Books, salary information, and the top online schools.
CPT Code 99283: When To Assign ED Level 3
CPT code 99283 is used to describe a Level 3 Emergency Department (ED) visit. This code is assigned when the patient presents with a problem that requires urgent evaluation by a physician, but the severity of the problem is not life-threatening.
According to the Centers for Medicare and Medicaid Services (CMS), the following criteria must be met in order to assign a Level 3 ED code:
- A detailed history must be obtained, including information about the patient’s chief complaint, the duration and severity of the problem, and any associated symptoms.
- A detailed examination must be performed, including a focused examination of the affected body system(s).
- Medical decision-making of moderate complexity must be involved, which includes consideration of the patient’s presenting problem, the complexity of any necessary diagnostic tests, and the risk of complications or morbidity.
If these criteria are met, then CPT code 99283 can be assigned to the ED visit. It’s important to note that the decision of which ED level to assign should always be based on the medical necessity of the services provided, and not on the patient’s diagnosis or the services rendered.

(2023) CPT Code 99283 | Description, Guidelines, Reimbursement, Modifiers & Examples
CPT code 99283 bills for services performed by the physician in the emergency department (ED). ED visits do not differentiate between new and established patients and reports per day. ED visits bills with five category CPT codes (99281-99285).
CPT codes 99281-99285 require three key components of evaluation and management CPT codes such as history, exam, and medical decision making (MDM).
The lowest CPT code is 99281 , including problem-focused history and exam and straightforward MDM.
CPT 99282 and CPT code 99283 describe an expanded problem-focused history and exam with MDM of low or moderate complexity, respectively, represented by 99282 and 99283.
The encounter typically addresses common to reasonable severity health concerns at these service levels.
The last two levels of service in this category represent high-severity problems.
Code 99284 describes a high-severity health concern that does not pose an immediate threat to life or physiologic function; a detailed history and exam in conjunction with moderate complexity MDM needs for reporting this level of service.
The highest level of service, 99285 , requires a comprehensive history and examination with high complexity MDM for high-severity health issues that pose an immediate threat to the life or physiologic function of the patient.
Time does not write as a descriptor for these CPT codes (99281-99285) due to the complex nature of the patient’s condition, and the physician sees multiple patients simultaneously.
However, it is unable to determine face-to-face time accurately.
CPT Code 99283 Description
CPT code 99283 reports by the physician; or other qualified health professionals when service renders at the emergency department for the evaluation and management of a patient.
It typically requires 3 out of 3 key components:
- An expanded problem-focused history
- An expanded problem-focused examination
- Medical decision-making of moderate complexity
The nature of presenting the problem must reflect the patient’s current condition and or family needs.
CPT Code 99283 Reimbursement
A maximum of one unit of CPT code 99283 is allowed to bill on the same day.
In contrast, a maximum of three times are allowed when documentation supports the medical necessity of CPT code 99283.
The CPT 99283 cost and RUVS are as follows when performed in the facility, it will be $76.16 and 2.20081, respectively.
In contrast, non-facility will be $76.16 and 2.20081, respectively.
Telehealth services are provided to patients most frequently due to COVID 19 situation.
In this case, it is appropriate to attach modifier 95 with CPT code 99283.
If it performs at the hospital due to some emergency, then it will be billed Q3014 for reporting telehealth services provided at the hospital.
CPT Code 99283 Modifiers
The most frequent modifiers used with 99283 CPT code are 24, 25, 57, and 95.
Modifier 25 will be appended with 99283 CPT code when it performs in conjunction with other services that are not allowed to be billed together on the same day.
For instance, the physician saw the patient with a headache and had shoulder surgery on the same day by the same physician.
In contrast, modifier 24 will be attached to CPT code 99283 when performed in the postoperative period with unrelated procedures or services.
Modifier 95 will be attached to 99283 CPT code if the service visits as a telehealth visit.
Modifier 57 will be attached to CPT 99283 if the physician plans to do surgery the same day the E/M visit performs.

CPT Code 99283 | Billing Guidelines
Documentation supports the medical necessity of service and should be medically appropriate to reflect the patient’s current condition.
CPT 99283 reports with the place of service 23 for a hospital emergency room.
Q3014 is applicable when the hospital provides telemedicine service as an origin site to other outpatient hospital patients.
CPT code 99283 requires 3 out of 3 key components (history, exam, and medical decision making) to meet the criteria or exceed the level of service, which are as follows:
Detailed history: It requires at least 4 HPI elements, 10 ROS systems, and one history component is needed 2 out of 3 components (PFSH).
Detailed Exam: It requires eight-plus systems as per 95 documentation, and nine-plus systems with two-plus bullets require 97 documentation.
High MDM : It requires at least 2 out of three components of MDM that must be met on that basis of risk, diagnostic or treatment, Data management services like Medicine, Laboratory, review, counseling, Interpretation of services.
If time is mentioned in the medical notes, it is appropriate to bill based on time instead of MDM, typically requiring 35 minutes on the patient’s hospital floor or unit.
Critical care services (99291-99292) are not allowed to be billed together in conjunction with ED code (CPT 99283).
CPT code 99283 cannot be billed together on the same date in combination with Observation services (99217-99220, 99234-99236)
99283 CPT code has no time limitations because it is difficult to determine the time during multiple encounters with patients simultaneously in ED.
In addition, ED care does not differentiate between new and established patients.
CPT Code 99283 Examples
The following are examples of CPT 99283 when this service will be billed:
58 y/o male with a PMH of HTN, HLD, hypothyroidism presenting to the hospital outpatient setting because of a headache and high blood pressure before arrival.
The patient lays down in bed at 10 pm and begins having a gradual onset pulsating frontal and occipital headache.
He reports that the pain was very severe. His headaches are usually associated with HTN.
The blood pressure shows a value of 210/100 and denies associated dizziness, chest pain , shortness of breath , motor weakness , numbness/tingling, abdominal pain, nausea/vomiting.
The physician ordered a series of diagnostic tests CT, MRI , and EKG .
EKG was independently interpreted and reviewed by the doctor. Patient reports improvement in HA with Tylenol.
A 51-year-old-female presents to the emergency with syncope . The patient applies a nicotine patch earlier.
The patient had a brief episode of feeling hot, numbness, and tingliness in her b/l hands, “gas discomfort” in her stomach, headache.
When she tried to get up, she lost consciousness(witnessed by her partner, who I spoke to for more history).
Partner states she was only out for a few seconds before perking up to routine.
Pt states she has had episodes like this in the past but several years ago. No known cardiac history.
Physicians plan to order CBC , CMP, mg, phos, trop, EKG, Tylenol, Pepcid, Zofran.
EKG: Normal sinus rhythm. 70 bpm. No ST elevation or T wave inversions.
CXR: My interpretation showed no acute abnormalities.
36-year-old male presents to the emergency department with PMH HTN, HLD, Afib (on eliquis), Mitral valve replacement, and gout presenting to the Office today for dark blood stools for two days.
He states that he started having diarrhea yesterday and has had 4 BM in the past two days.
The patient denies nausea, vomiting, CP, SOB, dizziness, fevers, chills, took eliquis this morning.
The physician also notes worsening bilateral lower extremity edema for which he takes Lasix.
He took Indomethacin for four days for a presumed gout flare. The colonoscopy was done three years ago, found benign polyp but otherwise WNL.
Physician plan to admit and Plan Labs, EKG, CT abdomen , and Pelvis, and prescribed Medicine.
70-year-old female presents to ED with a history of HLD presenting to the OPD for substernal chest pain.
The patient worked out daily, was a very healthy, active senior, lived at home, and worked out today.
After the workout, she took a sip of water, and she had substernal chest pain, none radiating, associated with weakness.
However, Gatorate helped with the substernal chest pain. She had no chest pain shortly after.
However, her trainer told her to see a provider. She went to urgent care with asymptomatic resolved chest pain; they sent her over here because she had a family history of MI in her family.
Her brother died of MI at age 48 EKG without ischemic changes. Low suspicion for ACS. HEART score 3.
38-year-old female past medical history of chronic gastritis diagnosed on endoscopic two weeks ago presenting with one month of on and off palpitations and lightheadedness.
The patient states that she has been feeling off for the last month and describes her symptoms as when she wakes up in the morning and feels fogginess has bouts of palpitations with associated lightheadedness without syncope.
The patient cannot pinpoint a trigger and states her symptoms resolve independently.
Palpitations last anywhere from seconds to minutes.
The patient endorses that she has a healthy diet and does not do any narcotics drink alcohol or smoke.
The patient otherwise denies fevers, chills, syncope, headaches, neck pain, chest pain, shortness of breath, back pain , abdominal pain, nausea, vomiting, diarrhea, constipation.
The physician decided will obtain EKG labs chest x-ray reassess.
EKG normal sinus rhythm at 74 bpm with a QTC of 426 no ST elevations or depressions.
Emergency department visit for a sexually active female complaining of vaginal discharge who is afebrile and denies experiencing abdominal or back pain.
Emergency department visit for a well-appearing 8-year-old who has a fever , diarrhoea, and abdominal cramps; is tolerating oral fluids and is not vomiting.
Emergency department visit for a patient with an inversion ankle injury, who is unable to bear weight on the injured foot and ankle.
Emergency department visit for a patient who has a complaint of acute pain associated with a suspected foreign body in the painful eye.
Emergency department visit for a healthy for a healthy, young adult patient who sustained a blunt head injury with local swelling and bruising without subsequent confusion, loss of consciousness, or memory deficit.
Similar Posts
How to use cpt code 27041.
CPT 27041 describes the procedure for performing a biopsy of the deep subfascial or intramuscular soft tissue in the pelvis and hip area. This article will cover the description, official description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code 27041? CPT 27041 is used…
How To Use CPT Code 76512
CPT 76512 describes the diagnostic procedure of ophthalmic ultrasound, specifically B-scan, with or without a non-quantitative A-scan superimposed. This article will cover the description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information, similar codes and billing examples. 1. What is CPT Code 76512? CPT 76512 can be used to describe the diagnostic…
How To Use CPT Code 27397
CPT 27397 describes the transfer or transplant of multiple muscle tendons in the thigh. This article will cover the description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code 27397? CPT 27397 can be used to describe a surgical procedure in which the provider transfers…
How To Use CPT Code 37650
CPT 37650 describes the ligation of the femoral vein, a procedure commonly performed to address varicose veins. This article will cover the description, official details, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code 37650? CPT 37650 is used to describe the ligation of the…
(2023) CPT Codes For PSA (Prostate-Specific Antigen)
The CPT codes for PSA are CPT 0359U, CPT 3268F and CPT 81539. Below you can find the long and short descriptions of these procedures. CPT Code 0359U Long description : Oncology [prostate cancer], analysis of all prostate-specific antigen [PSA] structural isoforms by phase separation and immunoassay, plasma, algorithm reports risk of cancer. Short description:…
How To Use CPT Code 50520
CPT 50520 describes the closure of nephrocutaneous or pyelocutaneous fistulas, which are abnormal communications between the skin and the kidney or between the skin and the renal pelvis. This article will cover the description, procedure, qualifying circumstances, appropriate usage, documentation requirements, billing guidelines, historical information and billing examples. 1. What is CPT Code 50520? CPT…
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Skip to main content
- Skip to primary sidebar
- Skip to footer
Efficient MD
Improving physician efficiency
Efficient MD / December 17, 2018
A Simplified Explanation of Emergency Department E/M Coding

The way medical charts are coded and billed is unnecessarily convoluted, and you have the Centers for Medicare & Medicaid (CMS) to thank for that. They are the ones who created the coding system that is used to assign an Evaluation & Management (E/M) level to our charts. Each chart is billed using a Current Procedure Terminology (CPT) code based on E/M levels 1-5.
Billing and coding is an extraordinarily boring topic. I’m actually impressed that you’ve read this far. But I think it’s worth taking a little time to understand the basics in order to chart as efficiently as possible. A level 5 chart does not necessarily require that you write a novel to meet the coding criteria. It is also possible to write a very long, thorough chart and still only get credit for a level 3 or 4 chart. Unless you know the elements of the chart that count towards that level of coding, you may end up doing a lot of unnecessary work.
Rather than review the criteria for every component of each of the 5 CPT codes, which would be time-consuming and painful for you to read, I thought it would be most beneficial to go through a sample level 5 (CPT code 99285) ED visit, pointing out the potential pitfalls where your chart could possibly be down-coded to a level 4.

There are only 3 components that determine the E/M level:
1. HISTORY
2. PHYSICAL EXAM
3. MEDICAL DECISION MAKING
As I go through this sample case I will demonstrate the minimum amount of documentation needed for the chart to be coded as a level 5 chart. I’m certainly not telling you to only document the minimum just to hit the level 5 criteria, as you should thoroughly chart everything that is necessary for each patient. This is simply an exercise to illustrate the minimum documentation that would be needed solely for coding purposes. Next to each of these 3 components, I will list in parentheses the minimum criteria required for that particular component. Keep in mind that the lowest scoring of the 3 components will determine the E/M level for the entire chart.
HISTORY ( HPI: Chief Complaint, 4+ elements, ROS: 10+ elements, PFSH: 2 of 3 elements)
The history component consists of 4 elements: chief complaint (CC), History of present illness (HPI), Review of systems (ROS), and Past medical, family and social history (PFSH). A level 5 chart is designated “comprehensive” and includes 4+ HPI elements, 10+ ROS elements, and 2 of the 3 PFSH elements. What do you do if the patient is unable to provide a history because they are altered or intubated? Or what if the patient refuses to give a history? Add a qualifier describing the reason for the limitation, such as “patient is unable to provide history secondary to…”. This will apply to all elements of the history component.
- CC – This is a mandatory element for all charts, regardless of CPT level.
- Modifying Factors
- Associated Signs/Symptoms
*In lieu of the HPI elements you could also document the status of 3 chronic or inactive conditions.
- Constitutional
- Ears, Nose, Mouth, Throat
- Cardiovascular
- Respiratory
- Gastrointestinal
- Genitourinary
- Musculoskeletal
- Integumentary (skin and/or breast)
- Neurological
- Psychiatric
- Hematologic/Lymphatic
- Allergic/Immunologic
A level 5 chart must document at least 10 organ systems. Your EMR may have a button you can click that states something to the effect “all other systems reviewed and are negative.” Clicking this button will technically satisfy the 10+ organ system ROS criteria, but doing so attests that you actually reviewed every organ system with the patient. A word of caution: don’t document something that you didn’t do!
- Past Medical History (PMH) – Includes experiences with illnesses, operations, injuries, and treatments.
- Family History (FH) – Review of medical events, diseases, and hereditary conditions that may place the patient at risk.
- Social History (SH) – Includes sexual history, alcohol/drug use, employment, and education.
A level 5 chart must include at least one item each from 2 of the 3 components . These are often documented by another staff member, such as the triage nurse. If these are documented by another staff member they still counts toward your coding as long as you attest that their notes were “reviewed and verified by me.”
Let’s get to the sample case:
John Doe is a 60yo male with a history of hypertension and diabetes who presents to the emergency department complaining of chest pain . He describes the pain as a “pressure” sensation in his left chest that began at 4pm today while walking . He notes that his father died of an MI at age 65 .
This brief paragraph includes the chief complaint (chest pain), 4 HPI elements: quality (“pressure”), location (left chest), duration (began at 4pm), and context (while walking); past medical history (history of hypertension and diabetes) and family history (father died of an MI at age 65). As long as you include your 10 ROS elements, you’ve met the minimum level 5 criteria for the HISTORY component of the chart! If this were a real patient you would clearly want to include more details regarding his presentation, but again, I’m using this example just to illustrate that you don’t need to write a novel for your chart to be coded at a level 5.
Pitfall – Keep in mind that the PFSH consists of 3 distinct components: PMH, FH and SH. You could list 10 medical conditions that the patient is suffering from but these all only count for 1 of these elements, the PMH. If the entire chart meets criteria for a level 5 chart but only 1 of these 3 elements is documented, such as failing to document that the patient is a smoker or has a significant FH of heart disease, the HISTORY component of the chart will be downcoded to a level 4, which means the entire chart is downcoded to a level 4.
PHYSICAL EXAM ( 9 systems, with 2 bullets per system )
A level 5 chart requires a “comprehensive” physical exam, which consists of 9 systems, with 2 bullets per system. CMS recognizes the following 14 systems as part of the physical exam:
- Ears, Nose, Mouth and Throat
- Chest (Breasts)
If you’d like to see the bullets that are within each of these systems, they can be found at the CMS website here . I’ve found that the most efficient way to ensure that your chart meets level 5 coding criteria is to create a “normal” templated exam that includes the minimum 9 systems with 2 bullets per system and modifying it as needed. However, if you choose to do this, be cautious! You need to know exactly what is in your templated exam and you must review it for each patient to ensure that you have not documented something that you did not actually do. Again, don’t document something that you didn’t do .
MEDICAL DECISION MAKING ( High )
The MDM section of your note is the most nebulous of the 3 components when it comes to understanding how it is coded. There are 3 elements that are considered here, with the final code being based upon the highest 2 of the 3 following elements:
- The number of possible diagnoses and/or the number of management options that must be considered (I will refer to this as DIAGNOSES )
- The amount and/or complexity of medical records, diagnostic tests, and/or other information that must be obtained, reviewed and analyzed (I will refer to this as DATA )
- The risk of significant complications, morbidity and/or mortality, as well as comorbidities, associated with the patient’s presenting problem(s), the diagnostic procedure(s) and/or the possible management options (I will refer to this as RISK )
DIAGNOSES – The highest score for this category is “extensive,” which is needed to bill as a level 5 chart. If you are seeing a patient who is presenting with a problem that is new to you , the provider, and you are pursuing a workup of the presenting problem, this fulfills the “extensive” criteria. If you are seeing the same patient, but not pursuing any workup, this component would be categorized as “multiple” rather than “extensive” and coded as a level 4 rather than a level 5. As an emergency provider, nearly every patient you treat will be presenting with a problem that is new to you . A rare exception to this may be someone who is returning for a scheduled re-check.
DATA – Again, the highest score for this category is “extensive,” which corresponds to a level 5 chart. This section is calculated using a scoring system, with a score of 4 or greater needed to be considered “extensive.” Here is the breakdown of the scoring :
- Review and/or order of clinical lab tests – ( 1 point )
- Review and/or order of radiology tests (excluding cardiac cath and echo) – ( 1 point )
- Review and/or order of medical tests (PFTs, colonoscopy, cath, echo) – ( 1 point )
- Discuss tests with performing physician (e.g., You discussed a colonoscopy result with the gastroenterologist. You must document this discussion in your note.) – ( 1 point )
- Independent review of image, tracing, specimen* – ( 2 points )
- Reviewed and summarized old records or history from a person other than the patient (e.g., If you spoke with a consultant, even informally, this counts! Just be sure to document the conversation in your note.) – ( 2 points )
* If documenting an ECG, your interpretation must include at least 3 of the 6 elements: rate/rhythm, axis, intervals, ST-segment changes, comparison to prior, summary of the patient’s clinical condition
RISK – Level of risk is scored from “minimal” to “high,” with a score of “high” needed to bill as a level 5 chart. The risk score is calculated using a risk table, which is unwieldy and probably not worth your time to study. For our purposes, to understand what qualifies as a level 5 chart in the ED, suffice it to say that a patient who is sick and requires urgent intervention typically qualifies as a “high” level of risk. Conditions that fall under this category include acute MI, pulmonary embolism, severe COPD exacerbation, multiple trauma, seizure, CVA, and psychiatric patients who are a threat to themselves or others. Also note that any patient who receives a parenteral-controlled substance qualifies as “high” risk .
Let’s revisit our patient who is presenting to the ED with chest pain. His chief complaint is a problem that is new to us . If we decide to pursue a workup for his chest pain (e.g., labs, ekg, cxr, etc.), the DIAGNOSES component of the MDM would meet the “extensive” criteria. Now, in order for the MEDICAL DECISION MAKING element of the chart to qualify for level 5 billing, we just need either the DATA or RISK component to also meet the threshold for a level 5 chart. Remember, you need 2 of the 3 components of the MDM ( DIAGNOSES, DATA and RISK ) to satisfy the highest level of billing in order for the MDM element to be billed as a level 5 chart.
Remember, the DATA component of the MDM is calculated based on points derived from various elements of the workup. We need at least 4 points to satisfy the “extensive” level of billing required for a level 5 chart. For this patient, if we order labs ( 1 point ), a chest x-ray ( 1 point ), and then document our interpretation of the chest x-ray ( 2 points ) we have a total of 4 points, which is sufficient to reach the “extensive” level of billing for the DATA component.
At this point the MDM element of the chart satisfies the billing criteria for a level 5 E/M code because 2 of the 3 elements of the MDM , the DIAGNOSES and DATA components, meet the maximum level of billing. The RISK component of the MDM does not even need to be considered because the MDM can be billed as a level 5 chart without it. However, if you had treated your patient’s chest pain with morphine during the encounter, this would have automatically bumped the RISK component to the maximum level, “high.” If this were the case, all 3 of the MDM elements would satisfy the criteria for a level 5 chart, though only 2 of these 3 are needed.
To recap, a level 5 E/M chart requires that all 3 components of the chart, the HISTORY, PHYSICAL EXAM, and MDM, meet their respective maximum coding criteria. Here are the 3 components with their respective level 5 billing criteria and the items from the chart that fulfill them:

CRITICAL CARE TIME
Critical care documentation is a special snowflake that warrants its own section. CMS defines critical care as a medical condition that “impairs one or more vital organ systems” and is one in which “there is a high probability of imminent or life-threatening deterioration in the patient’s condition.” They further note that the physician should provide “frequent personal assessment and manipulation” of the patient’s condition.
Here is a list of diagnoses that suggest critical care billing may be appropriate:
- Active seizures
- Acute altered mental status
- Acute GI bleed
- Acute psychosis with agitation
- Acute stroke
- Cardiac arrest
- Delirium tremens
- Ectopic pregnancy
- Hyperkalemia requiring treatment
- Hypovolemic shock
- Intracerebral hemorrhage
- Moderate to severe asthma
- Moderate to severe CHF
- Overdose requiring antidotes or reversal agents
- Pneumothorax
- Pulmonary embolus
- Rapid atrial fibrillation
- Respiratory distress requiring non-invasive positive pressure ventilation
- Respiratory distress requiring intubation
- Severe anemia requiring blood transfusion
- Suicidal ideation immediate threat
- Unstable angina
In addition to the patient having a critical condition, in order to bill for critical care time, you need to have spent 30 minutes or more on patient care . This includes time spent on direct patient care, as well as time spent on indirect patient care. Indirect patient care may include documentation, reviewing prior records, and speaking with consultants, paramedics, and family members. It is important to note that critical care time does not include time spent on procedures that are billed separately, such as intubations and central lines.
Some critically-ill patients may not qualify for critical care billing . If a patient with a STEMI is brought in by ambulance and then whisked off to the cath lab within 10 minutes of arrival, they would typically not qualify for critical care billing, regardless of how unstable they were. At least 30 minutes of time must be spent on patient care to bill for critical care.
If you care for a patient who meets the criteria for critical care billing and document it as such, these CPT codes ( 99291 for the first 30-74 minutes, 99292 for each additional 30 minutes beyond the first 74 minutes) supercede all of the elements discussed above for coding a E/M level 5 chart. Meaning, if you didn’t document a social history and your ROS only includes 8 organ systems instead of the 10 required for a level 5 chart, it will still be billed as a critical care chart.
Keep in mind that some patients may appear clinically stable but still qualify for critical care billing. The hyperkalemic patient who requires treatment, monitoring and frequent reassessments may qualify. As may the asthmatic who requires BiPAP and frequent reassessments.
Congrats on making it to the end! I hope this has been helpful. If you have any feedback for me regarding this article please contact me at [email protected] .
Disclaimer: This article was written for informational purposes only. I cannot guarantee the accuracy of the information provided. Payment policies can vary from payer to payer. I assume no responsibility for, and expressly disclaim liability for, damages of any kind arising out of, or relating to, the use, non-use, interpretation of, or reliance on information contained here. Specific coding or payment related issues should be directed to the payer.
Share this:
- Click to print (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on Reddit (Opens in new window)
2023 Documentation Guideline Changes for ED E/M Codes 99281-99285

On July 1, 2022, the American Medical Association (AMA) released a preview of the 2023 CPT Documentation Guidelines for Evaluation and Management (E/M) services. These changes reflect a once-in-a-generation restructuring of the guidelines for choosing a level of emergency department (ED) E/M visit impacting roughly 85 percent of the relative value units (RVUs) for typical members. Since 1992, a visit level was based on a combination of history, physical exam, and medical decision-making elements. Beginning in 2023, the emergency department E/M services will be based only on medical decision making.
You Might Also Like
- Documentation Pearls for Navigating Abscess Incision/Drainage Codes
- ICD-10 Diagnosis Codes to Use for Zika Virus Documentation
- Avoid Patient History Documentation Errors in Medical Coding
Explore This Issue
The American College of Emergency Physicians (ACEP) represents the specialty in the AMA current procedural technology (CPT) and AMA/Specialty Society RVS Update Committee (RUC) processes. In fact, they are your only voice in those arenas. The AMA convened a joint CPT/RUC work group to refine the guidelines based on accepted guiding principles. Although the full CPT code set for 2023 has not yet been released, the AMA recognized that specialties needed to have access to the documentation guidelines changes early to educate both their physicians on what to document and their coders on how to extract the elements needed to determine the appropriate level of care based on chart documentation. Additionally, any electronic medical record or documentation template changes will need to be in place prior to January 1, 2023, to maintain efficient cash flows and ensure appropriate code assignment.
ACEP was able to convince the Joint CPT/RUC Workgroup that time should not be a descriptive element for choosing ED levels of service because emergency department services are typically provided on a variable intensity basis, often involving multiple encounters with several patients over an extended period of time. It would be nearly impossible to track accurate times spent on every patient under concurrent active management.
The prior requirements to document a complete history and physical examination will no longer be deciding factors in code selection in 2023, but instead the 2023 Guidelines simply require a medically appropriate history and physical exam. That leaves medical decision making as the sole factor for code selection going forward. These changes are illustrated by the 2023 ED E/M code descriptors, which will appear as follows:
The 2023 E/M definitions have been updated to reflect simply Medical Decision Making determining the level.
- 99281: ED visit for the evaluation and management of a patient that may not require the presence of a physician or other qualified health care professional.
- 99282: ED visit for the evaluation and management of a patient, which requires a medically appropriate history and/or examination and straightforward medical decision making.
- 99283: ED visit for the evaluation and management of a patient, which requires a medically appropriate history and/or examination and low medical decision making.
- 99284: ED visit for the evaluation and management of a patient which requires a medically appropriate history and/or examination and moderate medical decision making.
- 99285: ED visit for the evaluation and management of a patient, which requires a medically appropriate history and/or examination and high medical decision making.
Pages: 1 2 3 | Single Page
Topics: 2023 guidelines Coding CPT guidelines Practice Management Reimbursement & Coding

Medicare’s Reimbursement Updates for 2024

Workplace Violence and Mental Health in Emergency Medicine

Maryland Implements Value-Based Alternative Payment Model
Current issue.

ACEP Now: Vol 43 – No 04 – April 2024
Download PDF
No Responses to “2023 Documentation Guideline Changes for ED E/M Codes 99281-99285”
Leave a Reply Cancel Reply
Your email address will not be published. Required fields are marked *


Popular Keywords
No Record Found
Level 3 Chart
Suggested E/M Coding Level: 3, 99283
This level has been selected based on the 2023 CPT guidelines for E/M codes in the Emergency Department based on 2/3 of the following.
- This patient has the following 2 or more self-limited or minor problems: []
OR
- This patient has the following stable chronic illness: []
- This patient has the following acute uncomplicated injury: []
- I reviewed or ordered at least two unique tests or external notes as following: []
OR
- The assessment required the following independent historian: []
- This patient has a low risk of morbidity due to further diagnostic testing or treatment
- Last updated January 21, 2023
Charting Tips
- This note is intended to be placed at the end of your chart to facilitate coders in selecting the correct E/M level for the visit.
- If you bill greater than 30 minutes of critical care time this note is no longer necessary because an E/M level is not billed with critical care time
- It may be 15 extra seconds to dictate the disease in exacerbation or specify that you reviewed hospitalist records and two labs but that may be the difference between coding as a 3 instead of a 2.
- Remember you only have to meet “low” MDM for 2/3 sections so you can delete the unnecessary section.
- There really isn’t much given by CMS as far as what constitutes “low” risk MDM other than low “low risk of morbidity from additional testing or treatment.”

Three common reasons for level 5 E/M office visits in primary care
Keith W. Millette, MD, FAAFP, RPH
If you’ve read the January/February issue of FPM , you know how to identify level 4 office visits under the new evaluation and management (E/M) guidelines and avoid losing money by under-coding them. But what about level 5 visits?
While not as common, level 5 visits do occur in primary care, and under-coding them can also have serious financial ramifications. To quickly identify and correctly code most level 5 office visits, keep in mind these three common reasons for level 5 work:
Reason No. 1: Time
The new guidelines allow coding of outpatient E/M office visits based solely on either total time on the date of service or medical decision making (MDM). Many level 5 office visits billed by family physicians will be based on time. If your total time is at least 40 minutes for an established patient or 60 minutes for a new patient, code that visit as a level 5.
Remember that total time includes all time spent caring for that patient on the day of the encounter. That means you count your prep time reviewing the chart before the visit, your face-to-face time during the visit, and the time you spend after the visit (as long as it occurs before midnight) reviewing studies, making phone calls, documenting your note, etc. (See these tips for tracking time .)
You must document your total time in the note. Because patients may read your notes, consider writing: “Total time was XX minutes. That includes chart review before the visit, the actual patient visit, and time spent on documentation after the visit.” This helps patients understand that you spend a lot of time behind the scenes caring for them, and it may even prevent confused patients from falsely accusing you of fraud (e.g., “He only spent 20 minutes with me, not the 40 minutes he listed in his note”) . Time spent on separately billed procedures done during an E/M visit does not count toward total time, so adding a statement such as “Time excludes procedure” is also helpful.
Reason No. 2: Pre-op visits for major surgery
To code a level 5 office visit using MDM you need at least two out of these three elements: high complexity problems, high risk, or extensive data review. Pre-op visits before elective major surgery in patients who have risk factors or require labs, X-rays, or electrocardiograms (ECGs) for evaluation/preoperative clearance often check these boxes.
There are two types of risk you can consider when it comes to pre-op visits: procedure risk and patient risk. Major surgery involves high procedure risk, including general anesthesia and the procedure itself (e.g., coronary artery bypass, total hip replacement, and abdominal surgery). Patient risk factors include morbid obesity, heart disease, diabetes, lung disease, etc. It is important to document both the patient risk factors and the procedure risk in your note.
The data portion of MDM is split into three categories:
1. Tests, documents, or independent historian(s); any combination of three from the following:
- Review of prior external note(s) from each unique source,
- Review of the result(s) of each unique test,
- Ordering of each unique test,
- Assessment requiring independent historian(s).
2. Independent interpretation of a test performed by another physician/other qualified health care professional (not separately reported).
3. Discussion of management or test interpretation with an external physician or other qualified health professional/appropriate source (not separately reported).
A visit must include at least two out of those three categories to qualify as level 5 “data” work. For level 5 pre-op visits, this commonly involves ordering/reviewing a minimum of three tests (e.g., labs , ECG, and chest X-ray) and interpreting at least one study (e.g., ECG or X-ray). To get credit for interpretation it must be clear in the note that you evaluated the study (e.g., “I personally evaluated the chest X-ray and it shows … ”) and did not just look at the report. Remember, if your health system is billing separately for the interpretation, you cannot count it toward your E/M visit level (for more tips on counting MDM data, click here ).
For practical purposes, the minimum criteria for coding level 5 pre-ops would look something like this as a simple equation: Level 5 pre-op = major surgery + risk factors + order/review three tests + interpret one study.
Reason No. 3: Very sick patients who require work up and/or admission decision
Very sick patients often require level 5 work if they have a high complexity problem such as acute respiratory distress, depression with suicidal ideation, or any new life-threatening illness or severe exacerbation of an existing chronic illness. It is common for these visits to qualify as high risk or require extensive data review, thereby pushing them into level 5 territory. Examples include the following:
1. Seeing a very sick patient (such as one with severe exacerbation or progression of their chronic condition, or side effects of treatment of their chronic condition) in the office who requires hospital admission (and you are not doing the admitting yourself) or requires you to contemplate admission (make sure to document your thought process in the note). This combines a high-complexity problem (or problems) with high risk.
2. Seeing a very sick patient (such as one with an acute or chronic condition that poses a threat to life or bodily function) who requires an office work up that qualifies as level 5 data review (e.g., ordering/reviewing a minimum of three tests and interpreting one study). This combines a high complexity problem (or problems) with extensive data.
To summarize, here are the three common reasons to code a level 5 office visit:
These are only a few useful examples of level 5 work. Less common scenarios may also qualify, such as visits that include decisions to de-escalate care or initiate do-not-resuscitate orders, decisions about emergency major surgery, and decisions about the use of drugs that require intensive monitoring. Referring to a coding template can be helpful for those scenarios. But for the three types of visits outlined above, you should not be afraid to think level 5 if your documentation supports it.
— Keith W. Millette, MD, FAAFP, RPH, is a family physician in Grand Forks, N.D.
- Chronic care
- Medicare/Medicaid
- Physician compensation
- Practice management
- Reimbursement
- Value-based payment
Other Blogs
- Quick Tips from FPM journal
- AFP Community Blog
- Fresh Perspectives
- In the Trenches
- Leader Voices
- RSS ( About RSS )
Disclaimer: The opinions and views expressed here are those of the authors and do not necessarily represent or reflect the opinions and views of the American Academy of Family Physicians. This blog is not intended to provide medical, financial, or legal advice. Some payers may not agree with the advice given. This is not a substitute for current CPT and ICD-9 manuals and payer policies. All comments are moderated and will be removed if they violate our Terms of Use .
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

- Find a Doctor
- Patients & Visitors
- ER Wait Times
- For Medical Professionals
- Piedmont MyChart

- Medical Professionals
- Find Doctors
- Find Locations
Receive helpful health tips, health news, recipes and more right to your inbox.
Sign up to receive the Living Real Change Newsletter
What to expect in the emergency department
“The emergency department is an area in the hospital where we can quickly assess patients, make them better, or decide they’re going to need additional testing or management and admit them to the hospital,” says Jeffrey Oyler, M.D. , an emergency medicine physician at Piedmont Atlanta Hospital .
Every patient who visits the emergency department (ED) will go through triage, which allows the ED team to establish the severity of that person’s condition. Triage takes into account the patient’s vital signs, as well as his or her complaint. Dr. Oyler says measuring the patient’s vital signs is the most crucial component of triage because these signs are essential to assessing the patient and are something that cannot be faked. The patient is then categorized based on the Emergency Severity Index:
- Level 1 – Immediate: life-threatening
- Level 2 – Emergency: could be life-threatening
- Level 3 – Urgent: not life-threatening
- Level 4 – Semi-urgent: not life-threatening
- Level 5 – Non-urgent: needs treatment as time permits
“It’s hugely important for us to establish who is the sickest, so we can provide the interventional care they need immediately, then work our way down the list as fast as we can,” says Dr. Oyler. Based on the assessment by the triage nurse, the patient will either be:
- Taken to an exam room. If all rooms are full, that person will be next in line for a room. Dr. Oyler emphasizes that patients are not seen in the order of arrival, but based on the severity of their condition.
- Offered a fast-track service. The fast track does not have all of the capabilities of the emergency department, but is intended to help patients with minor emergencies get through the system. People in the waiting room may see other patients with minor injuries being called back before those with more serious injuries, but they are actually being treated in the fast-track area, Dr. Oyler explains.
Behind the waiting room doors
“A quiet waiting room is something we ideally love to have, but it is not a reflection of what is going on in the back,” says Dr. Oyler. “You can have one person or 20 people in your waiting room, but you could have complete chaos in the back with very, very sick patients.” Although the ED waiting room may not seem busy, the behind-the-scenes ambulance bay can bring in patients at all hours of the day. “You can have an incredibly long wait in our emergency department if you show up with a non-life-threatening condition that could have waited for treatment at your primary care physician’s office the next day,” he says. “We are sensitive to the fact that you are waiting,” says Dr. Oyler. “We want you to get back to a room and be seen as fast as possible, but we’re also prioritizing care for people who absolutely have to have it right then and there.” Dr. Oyler stresses the importance of patience if your illness or injury is not life-threatening. “We know you’re suffering and it’s not what we desire, but when your time comes, you’re going to get the service you wanted.” If your condition is not an emergency, you can save time and money by visiting an urgent care center or your primary care physician’s office. Insurance co-pays are usually more expensive at the emergency department compared to co-pays at other facilities. For more information on emergency services throughout the Piedmont system, visit our locations map to choose an emergency room near you .
Need to make an appointment with a Piedmont physician? Save time, book online .
- emergency department
- Emergency Medicine
- Jeffrey Oyler
- urgent care
Related Stories

Schedule your appointment online
Schedule with our online booking tool
*We have detected that you are using an unsupported or outdated browser. An update is not required, but for best search experience we strongly recommend updating to the latest version of Chrome, Firefox, Safari, or Internet Explorer 11+
Share this story
Download the Piedmont Now app
- Indoor Hospital Navigation
- Find & Save Physicians
- Online Scheduling
Download the app today!

IMAGES
VIDEO
COMMENTS
According to CPT, a typical level-II visit lasts 10 minutes, while a typical level-III visit lasts 15 minutes. If counseling or coordination of care account for more than 50 percent of the visit ...
Date. Updates. 1/7/2021. Coding & Billing Guideline created. 9/22/2021. Updated format. 11/21/2022. Removed references to level of history and examination as these references will be deleted 1/1/2023 and only the level of medical decision-making will be used when selecting the appropriate code and added information about time not being a descriptive component for the emergency department ...
The 99283 CPT code is used for reporting emergency department visits. This code corresponds to level 3 visits, which involve moderate severity presenting problems. The code requires an expanded problem focused history, examination, and moderate complexity in medical decision making. Accurate coding and documentation are crucial for proper ...
These are listed under the matrix example of level 4, and result in coding of 99284 Emergency department visit for the evaluation and management of a patient, which requires these 3 key components: A detailed history; A detailed examination; and Medical decision making of moderate complexity. ... One example of level 3 (99283) under possible ...
Each level provides facility intervention examples that align with the evaluation and management (E&M) service. The table below, although not an all-inclusive, provides criteria that our health plan will apply to determine the level of reimbursement, for ED services. ... Emergency Room visits that result in an Inpatient submission will follow ...
The ACEP facility coding model provides an easy to use methodology for assigning visit levels in an Emergency Department (ED). There are three columns in the guidelines. The far left column indicates the facility codes and corresponding APC levels which are justified by the "Possible Interventions" listed in the middle column.
CPT code 99283 is used to describe a Level 3 Emergency Department (ED) visit. This code is assigned when the patient presents with a problem that requires urgent evaluation by a physician, but the severity of the problem is not life-threatening. ... cpt code 99283 modifier 25, level 3 emergency room code, level 3 er visit examples. April 13 ...
C. Leveling Adjustments. When a physician bills a Level 4 (99284) or Level 5 (99285) emergency room E/M service, with a diagnosis indicating a lower level of acuity, complexity, or severity, the service will automatically be reimbursed at the Level 3 (99283) reimbursement rate. The submitted procedure code will be changed to 99283 in the claims ...
The CPT 99283 cost and RUVS are as follows when performed in the facility, it will be $76.16 and 2.20081, respectively. In contrast, non-facility will be $76.16 and 2.20081, respectively. Telehealth services are provided to patients most frequently due to COVID 19 situation. In this case, it is appropriate to attach modifier 95 with CPT code 99283.
The nature of a patient's presenting problem is key to determine the appropriate level of risk under MDM. Choosing between 99283 Emergency department visit for the evaluation and management of a patient, which requires these 3 key components: An expanded problem focused history; An expanded problem focused examination; and Medical decision making of moderate complexity and 99284 Emergency ...
For example, administrating oral meds to a patient is worth three points, and a bandage application is worth five points. The coder adds up the points to determine the appropriate level. One possible point system is: 0-20 points = Level 1 (99281) 21-35 points = Level 2 (99282) 36-60 points = Level 3 (99283)
The codes have not changed, but the code descriptors have been revised. In November 2019, CMS adopted the AMA's revisions to the Evaluation and Management (E/M) office visit CPT codes (99201-99215), code descriptors, and documentation standards.
There are only 3 components that determine the E/M level: 1. HISTORY. 2. PHYSICAL EXAM. 3. MEDICAL DECISION MAKING. As I go through this sample case I will demonstrate the minimum amount of documentation needed for the chart to be coded as a level 5 chart.
These changes are illustrated by the 2023 ED E/M code descriptors, which will appear as follows: The 2023 E/M definitions have been updated to reflect simply Medical Decision Making determining the level. 99281: ED visit for the evaluation and management of a patient that may not require the presence of a physician or other qualified health ...
HPI flushes out the chief complaint in grea t er d e t a il. There are two types of HPI identified for the purpose of coding. A brief HPI consists of 1-3 elements (99281-99283) An extended HPI consists of at least 4 elements (99284-99285) 27. Brief- 32 year old male with left shoulder. injury, occurred 4 hours ago.
The first visit resulted in a level 5 (99285) code and a $9,817.07 facility charge. The second visit resulted in a level 3 (99283) code. Westfall's records don't show how much the facility ...
Attendees at AAPC's AUDITCON, Nov. 3-4, 2022, came loaded with questions about the coding and guideline changes for evaluation and management (E/M) services in CPT® 2023. The conference offered several sessions on the subject, including the ED session, "Changes in 2023: Emergency Department," presented by AAPC Chief Product Officer ...
OR. OR. OR. Suggested E/M Coding Level: 3, 99283 This level has been selected based on the 2023 CPT guidelines for E/M codes in the Emergency Department based on 2/3 of the following. COPA: This patient has the following 2 or more self-limited or minor problems: [] OR This patient has the following stable chronic illness: [] OR This patient has ...
There are four levels of MDM to support the five ED E/M codes: Straight forward (99281) Low (99282) Moderate (99283 and 99284) High (99285) Determine the MDM level by reviewing three distinct components. The entire record must be reviewed and all information considered. CPT® references the following three components for MDM:
Summary. To summarize, here are the three common reasons to code a level 5 office visit: Total time. ≥ 40 minutes for established patients; ≥ 60 minutes for new patients. Pre-op visit. Major ...
Every patient who visits the emergency department (ED) will go through triage, which allows the ED team to establish the severity of that person's condition. Triage takes into account the patient's vital signs, as well as his or her complaint. Dr. Oyler says measuring the patient's vital signs is the most crucial component of triage ...