Blood Clots and Travel: What You Need to Know
More than 300 million people travel on long-distance flights (generally more than four hours) each year. 1 Blood clots, also called deep vein thrombosis (DVT), can be a serious risk for some long-distance travelers. Most information about blood clots and long-distance travel comes from information that has been gathered about air travel. However, anyone traveling more than four hours, whether by air, car, bus, or train, can be at risk for blood clots.


Blood Clots and Travel: What You Should Know
This podcast is designed to help people reduce their risk of blood clots during long-distance travel of four hours or more.
Blood clots can form in the deep veins (veins below the surface that are not visible through the skin) of your legs during travel because you are sitting still in a confined space for long periods of time. The longer you are immobile, the greater is your risk of developing a blood clot. Many times the blood clot will dissolve on its own. However, a serious health problem can occur when a part of the blood clot breaks off and travels to the lungs causing a blockage. This is called a pulmonary embolism, and it may be fatal. The good news is there are things you can do to protect your health and reduce your risk of blood clots during a long-distance trip.
Understand What Can Increase Your Risk for Blood Clots
Even if you travel a long distance, the risk of developing a blood clot is generally very small. Your level of risk depends on the duration of travel as well as whether you have any other risks for blood clots. Most people who develop travel-associated blood clots have one or more other risks for blood clots, such as:
- Older age (risk increases after age 40)
- Obesity ( body mass index [BMI] greater than 30kg/m 2 )
- Recent surgery or injury (within 3 months)
- Use of estrogen-containing contraceptives (for example, birth control pills, rings,patches)
- Hormone replacement therapy (medical treatment in which hormones are given to reduce the effects of menopause)
- Pregnancy and the postpartum period (up to 3 months after childbirth)
- Previous blood clot or a family history of blood clots
- Active cancer or recent cancer treatment
- Limited mobility (for example, a leg cast)
- Catheter placed in a large vein
- Varicose veins
The combination of long-distance travel with one or more of these risks may increase the likelihood of developing a blood clot. The more risks you have, the greater your chances of experiencing a blood clot. If you plan on traveling soon, talk with your doctor to learn more about what you can do to protect your health. The most important thing you can do is to learn and recognize the symptoms of blood clots.

My name is Amaris White and I want to share my personal experience with blood clots. My hope is that by sharing this information, you will learn the signs and symptoms of this potentially fatal condition and know how to protect yourself and others.
Recognize the Symptoms
Deep vein thrombosis (dvt).
About half of people with DVT have no symptoms at all. The following are the most common symptoms of DVT that occur in the affected part of the body (usually the leg or arm):
- Swelling of your leg or arm
- Pain or tenderness that you can’t explain
- Skin that is warm to the touch
- Redness of the skin
If you have any of these symptoms, contact your doctor as soon as possible.
Pulmonary Embolism (PE)
You can have a PE without any symptoms of a DVT. Symptoms of a PE can include:
- Difficulty breathing
- Faster than normal or irregular heartbeat
- Chest pain or discomfort, which usually worsens with a deep breath or coughing
- Coughing up blood
- Lightheadedness, or fainting
If you have any of these symptoms, seek medical help immediately.
For more information on blood clots
Blood Clots and Long Distance Travel: Advising Patients

View this video to learn more about how healthcare providers can advise their patients on long-distance travel and blood clots.
Protect Yourself and Reduce Your Risk of Blood Clots During Travel
- Know what to look for. Be alert to the signs and symptoms of blood clots.
- Talk with your doctor if you think you may be at risk for blood clots. If you have had a previous blood clot, or if a family member has a history of blood clots or an inherited clotting disorder, talk with your doctor to learn more about your individual risks.
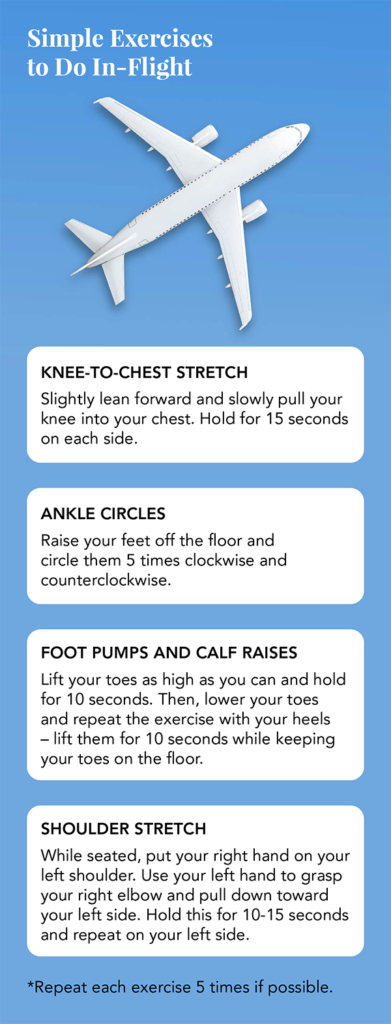
- Move your legs frequently when on long trips and exercise your calf muscles to improve the flow of blood. If you’ve been sitting for a long time, take a break to stretch your legs. Extend your legs straight out and flex your ankles (pulling your toes toward you). Some airlines suggest pulling each knee up toward the chest and holding it there with your hands on your lower leg for 15 seconds, and repeat up to 10 times. These types of activities help to improve the flow of blood in your legs.
- If you are at risk, talk with your doctor to learn more about how to prevent blood clots. For example, some people may benefit by wearing graduated compression stockings.
- If you are on blood thinners, also known as anticoagulants, be sure to follow your doctor’s recommendations on medication use.
1 Gavish I, Brenner B. Air travel and the risk of thromboembolism. Intern Emerg Med 2011 Apr;6(2):113-6.
- Yellow Book chapter on DVT and travel
- World Health Organization
Join the Public Health Webinar Series on Blood Disorders
- Upcoming webinar
- View past webinars
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- ASH Foundation
- Log in or create an account
- Publications
- Diversity Equity and Inclusion
- Global Initiatives
- American Society of Hematology
- Blood Clots
Clots and Travel
- Agenda for Nematology Research
- Precision Medicine
- Genome Editing and Gene Therapy
- Immunologic Treatment
- Research Support and Funding
Blood clots can sometimes form in your legs during air travel because you are immobile for long periods of time, often sitting in cramped spaces with little leg room. The clinical term for this type of blood clot is deep vein thrombosis (DVT). The longer the flight, the more at risk you are for developing a clot. Flights lasting 8 to 10 hours or longer pose the greatest risk.
In some cases, the DVT will dissolve and go away on its own. However, in more serious cases, it can cause pain, swelling, and warmth of the affected leg, or it can break off and travel to the blood vessels of your lungs, causing pulmonary embolism (PE).
DVT and PE, collectively known as venous thromboembolism, are highly preventable (see prevention tips below). The U.S. Surgeon General has issued a Call to Action on DVT and PE to raise public awareness of these blood conditions and increase research on the causes, prevention, and treatment.
There are several symptoms that can be warning signs of blood clots, including the following:
- Swelling of the leg, ankle, or calf
- Redness or discoloration
- Increased warmth over the skin
Am I At Risk?
Your risk of developing a blood clot during air travel is increased by the following:
- Use of oral contraceptives
- Certain cancers
- Certain recent surgeries
- Age (increased risk for people over age 60)
- History of previous blood clots
- Family history of blood clots
- Chronic inflammatory diseases
- High blood pressure
- High cholesterol
- Prior central line placement
How Can I Prevent Blood Clots When I Travel?
There are some simple steps you can take to avoid developing a blood clot while flying. Make sure to stretch your legs and get some exercise. You can do this by walking around the plane every few hours and changing positions in your seat.
If you plan on traveling soon and have concerns about getting a blood clot, talk with your doctor about your risks and prevention. Depending on your physical condition, genetics, and medical history, you may want to see a hematologist, a doctor who specializes in blood conditions.
Deep Vein Thrombosis: A Patient's Journey
Where Can I Find More Information?
If you find that you are interested in learning more about blood diseases and disorders, here are a few other resources that may be of some help:
Results of Clinical Studies Published in Blood
Search Blood , the official journal of ASH, for the results of the latest blood research. While recent articles generally require a subscriber login, patients interested in viewing an access-controlled article in Blood may obtain a copy by e-mailing a request to the Blood Publishing Office .
Patient Groups
A list of Web links to patient groups and other organizations that provide information.

- Students & Professionals
How to Avoid Blood Clots When Flying: Advice from a Vascular Surgeon

What You Should Know About Traveling Blood Clots
A blood clot in a deep vein that breaks off and travels to your lungs could be life-threatening. Here’s what you need to know about this type of traveling blood clot.
Deep vein thrombosis (DVT) is a medical condition that occurs when a blood clot develops deep in a vein. These clots typically occur in the leg, thigh, or pelvis, but may also develop in the arm.
DVT can become dangerous if the blood clot breaks off and travels through the bloodstream to the lungs. This causes a blockage called a pulmonary embolism (PE) and can be life-threatening.
The Connection Between DVT and PE
Think of pulmonary embolism as a complication of deep vein thrombosis , explains Roy Silverstein, MD , a professor and chair in the Medical College of Wisconsin’s division of hematology and oncology in Milwaukee. Some important things to know about DVT and PE:
- You can have DVT and not know it, especially if the clot is small.
- The most common symptoms of DVT are swelling in an arm or leg, tenderness that isn’t from an injury, and skin that feels warm and is red in the area of the clot.
- A clot usually forms in just one leg or arm, not both.
- You’re at a greater risk for a PE if you have deep vein thrombosis or a history of DVT.
Like DVT, you can have a PE and not know it.
“With a PE, one of three things happens,” says Andrea Obi, MD , a vascular surgeon at University of Michigan Health in Ann Arbor. “Sometimes it will plug up just a very small blood vessel in the lung, and the remainder of the lung will compensate and the person may not even know it happened.”
A second scenario, she says, is that “the clot will break off and travel to the lung and block a slightly larger blood vessel that impairs the ability of the lung to exchange blood that’s returning for blood that’s oxygenated.” This will cause oxygen saturation levels to drop.
Signs of PE might include the following:
- Shortness of breath
- A rapid heartbeat
- Chest pain or discomfort that gets worse when you breathe deeply or cough
- Coughing up blood
- Feeling lightheaded or faint
- Feeling anxious or sweating
- Having clammy or discolored skin
“The third scenario is sudden death, and that’s really what we’re trying to prevent when we talk about making a timely diagnosis of DVT and getting patients on blood thinners right away,” Dr. Obi says.
Diagnosing DVT and PE
DVT and PE aren’t always detected for what they are. “The symptoms are quite subtle, and sometimes it’s a nagging pain in the leg that people don’t pay much attention to,” Dr. Silverstein says. “You think you pulled a muscle — you don’t think it could be a clot.”
However, because PE can lead to sudden death, it’s critical to seek medical treatment right away if you think you might be experiencing any of the telltale symptoms.
According to the Centers for Disease Control and Prevention , as many as 900,000 people in the United States develop DVT, PE, or both every year. An estimated 60,000 to 100,000 of them die, and most are sudden deaths because the fatal PE goes unrecognized. In fact, sudden death is the first symptom for a quarter of the people who have a pulmonary embolism, the CDC notes.
That need not be the case, however. “As long as we make a prompt diagnosis and treat it, patients do extremely well,” Silverstein says.
Most often, DVT can be diagnosed with duplex ultrasound. A sonographer uses an ultrasound machine, sending sound waves through the leg, to observe blood flow in your veins.
To diagnose PE, doctors may order a computed tomography (CT) scan or a specialized X-ray of your lungs, called a ventilation/perfusion scan; it can also show how much blood is getting to your lungs, notes Johns Hopkins Medicine . During the ventilation part of the scan, you inhale a small amount of a radioactive gas. Radioisotopes are injected into your bloodstream to allow doctors to see where blood flows to your lungs.
A blood test known as D-dimer measures a substance found in your blood when a clot dissolves, according to MedlinePlus . High levels may suggest blood clots. If your level is normal and you have few risk factors for PE, it could indicate that you don’t have PE.
Managing DVT and PE Blood Clot Disorders
Sitting while traveling long distances in a plane or car can increase your risk for DVT and PE, and the longer the trip, the higher the risk, Silverstein says.
Women who take hormones, whether birth control pills or estrogen therapy, are also at an increased risk, as are pregnant women and women in the six weeks after childbirth. People who have to spend an extended amount of time in bed, most often because of hospitalization and recovery from an illness or surgery, have a heightened risk, too.
Treatment involves medications that thin your blood and slow its ability to clot. Blood thinners won’t break up clots, Silverstein says, but they will stop the clot from growing and prevent further clots. “The body has a natural way of healing itself, and eventually the clot disappears on its own,” he says.
If a pulmonary embolism is life-threatening, your doctor can administer a thrombolytic, an agent that will dissolve the clot quickly. Because thrombolytics can cause you to bleed, they’re used only when your life is in danger. “Thrombolytic therapy has to be done in a hospital setting,” notes Silverstein.
Sometimes, though not often, surgery is required to remove the blood clot.
“If the blockage is big enough where it’s causing really severe deficits in oxygen or strain on the heart, then in those patients we do try to treat them by removing the blood clot,” Obi says.
Silverstein adds that the most worrisome complication of PE is death. If you have repeated clots, over time they can damage your lungs, and that can lead to chronic heart disease. Most of the time, that doesn’t happen, he says.
Once you’ve had a PE, you are at a greater risk of having more. Other factors that could further increase your risk, per Johns Hopkins Medicine :
- Being sedentary or bedridden
- Being overweight
- Undergoing surgery or breaking a bone
- Having a history of a stroke, chronic heart disease, high blood pressure, chronic obstructive pulmonary disease (COPD), or paralysis
In addition, research has also noted a link between DVT, PE, and COVID-19. A 2022 study concluded there was an increased risk of developing either DVT or PE in the months following a COVID-19 infection , although the researchers noted that the risk seemed to be higher during the first wave of the pandemic, and especially in people with multiple other chronic health conditions.
Age is also a risk factor. “The older you are, the higher your risk,” Silverstein says, “particularly after age 55.”
Never ignore DVT or PE symptoms, thinking they will go away, especially if you have risk factors. Because the signs — if any — will be subtle, err on the side of caution.
Editorial Sources and Fact-Checking
Everyday Health follows strict sourcing guidelines to ensure the accuracy of its content, outlined in our editorial policy . We use only trustworthy sources, including peer-reviewed studies, board-certified medical experts, patients with lived experience, and information from top institutions.
- Data and Statistics on Venous Thromboembolism. Centers for Disease Control and Prevention . June 28, 2023.
- Lung Scan. Johns Hopkins Medicine .
- D-Dimer Test. MedlinePlus . November 8, 2021.
- Pulmonary Embolism. Johns Hopkins Medicine.
- Katsoularis I, Fonseca-Rodríguez O, Farrington P, et al. Risks of Deep Vein Thrombosis, Pulmonary Embolism, and Bleeding After COVID-19: Nationwide Self-Controlled Cases Series and Matched Cohort Study. BMJ . April 6, 2022.

- May 27, 2022
Traveling and Blood Clots
Traveling for long distances by car poses a number of challenges to individuals due to long periods of time sitting behind the wheel or being cramped in the passenger seat. What if you’re flying? Same thing – sitting in a cramped, upright position with little legroom. Both modes of travel make it difficult to get up to walk or stretch.
A few simple exercises you can do when traveling in a car, a plane, or a train can help reduce cramping, and numbness, and even prevent a blood clot from forming. It’s about awareness, planning ahead, and being proactive before you climb into that car, or board that flight, or train.
Prevent blood clots while traveling
Blood clots are formed when blood is sluggish or constricted, such as when seated in an upright position with the knees bent and the hips stuck at 90-degree angles for extended periods of time. This leads to slowing and even pooling of the blood, especially in the abdomen and lower extremities.
While most individuals travel without any complications, some travelers are at an increased risk of developing blood clots. Those with a family history of clotting issues, obesity, smoking, and immobility place a person at an increased risk for the formation of blood clots due to poor circulation, limited mobility, and strain on the heart muscle overall.
Prevention is key. If you’re concerned about a long journey ahead of you, speak with your physician about exercise, hydration, and activity that may be coordinated to your mode of transportation. For example, if you travel by bus or plane, it’s often difficult to just get up and walk around. If driving, rest stops are the only way to get out and walk and stretch.
Several exercises to promote blood flow can be done in small or tight spaces, such as an airplane or bus seat to increase comfort and decrease the potential for pooling of blood. Some examples include:
- Slide your feet under the seat in front of you (or on the car floor well) and straighten your legs as much as you can, then circle your ankles
- Pressing your toes to the floor, lift your heels, contract, release, and repeat
- Seated ‘marching in place is a good way to keep the blood moving in the lower extremities
Perform exercises like these at least once an hour, more often if possible. When driving, frequent rest stops encourage walking and stretching that improve circulation.
Before traveling, be aware of the dangers associated with blood clots. No matter what type of travel is planned, plan and prepare.
Related Posts

Blood Clot Formation: A Hidden Danger of Dog Bites
Dog bites, while often considered in terms of immediate physical trauma and infection risk, carry another, less commonly discussed danger: the potential to cause blood clot formation. This post explores the complex relationship between dog bites and blood clots, aiming to raise awareness and understanding of this serious health risk. Understanding How a Dog Bite

The Link Between Falls and Blood Clots
When we think of the aftermath of a fall, bruises and perhaps a broken bone come to mind. However, there’s another less obvious but potentially dangerous consequence: blood clots. While a fall might seem like an isolated incident, its implications can extend far beyond immediate injuries, potentially leading to the development of blood clots. Understanding

Understanding Blood Clot Risks After a Hysterectomy
Understanding Blood Clot Risks After a Hysterectomy A hysterectomy, the surgical removal of the uterus, can be a life-changing procedure for many women, offering relief from various medical conditions such as chronic pain, heavy bleeding, or cancer. However, like any major surgery, it comes with its set of post-operative risks, including the development of blood

Managing Blood Clot Concerns After Your C Section
**Managing Blood Clot Concerns After Your C Section** Bringing a new life into the world is a momentous event, and for many, a C-section is a vital part of the journey. While it’s a common and generally safe procedure, like any surgery, it comes with its set of complications and risks, including the potential for

The Risk of Blood Clots After a Car Accident
Car accidents are traumatic events that can have lasting physical effects, some of which may not be immediately apparent. Among these potential post-accident complications, the risk of developing blood clots is significant yet often overlooked. Blood clots can pose serious health risks, including the potential for life-threatening conditions such as deep vein thrombosis (DVT) and

Is It a Blood Clot or Just a Muscle Cramp? Know the Difference
Experiencing leg pain or discomfort can be concerning, especially when trying to determine if it’s a blood clot or just a muscle cramp. Both conditions share similarities in their manifestation but have distinctly different causes and risks associated with them. Understanding these differences is crucial for addressing the issue appropriately and ensuring your health and
North American Thrombosis Forum
Home / Patients / Patients Are Asking: Does Flying I…
Patients Are Asking: Does Flying Increase My Risk for a Clot
Last updated on July 17, 2023
FULL SUMMARY
- When we travel far away from home, we may worry about getting a blood clot.
- The chance of getting a blood clot from traveling is small, but some have a higher risk, like those who are overweight, older, pregnant, have a history of blood clots, or have limited mobility.
- Airplanes have unique factors that can affect risk, like sitting in a tight seat and not being able to move around much.
- To lower the risk, try to move around every 1-2 hours, drink lots of water, and avoid sleeping or sitting in awkward positions for too long.
- Experts recommend these commonsense measures for most people, but those at higher risk may need to wear compression stockings or talk to their healthcare provider about taking medicine to prevent blood clots.

Home is where the heart is, though you might have to travel a long way to get there for the holidays. Long-distance travel may raise your stress level, but can it also raise your risk of getting a blood clot? Dr. Susan Kahn, a Professor of Medicine at McGill University and a Canada Research Chair in venous thromboembolism (VTE), weighs in.
Blood clots affect about 1-2 in 1,000 U.S. adults per year, and the risk may double or triple after a flight that’s 4+ hours. One study estimates that 1 in 4,600 travelers will have a blood clot within 4 weeks of a long flight. According to Dr. Kahn, “the actual risk of a travel-related blood clot is quite small, and the average traveler doesn’t need to worry about it. Billions of people travel by plane every year, and most of them don’t get a blood clot.”
However, those who already have risk factors for a clot may have a higher risk of developing travel-related VTE. These risk factors include:
- Age over 40
- Use of birth control pills or hormone therapy
- Recent injury or surgery
- Limited mobility
- A personal or family history of blood clots
- Active cancer or recent cancer treatment
It’s unclear if long-distance air travel is any riskier than car or train travel, but there are factors unique to airplanes that can affect risk:
- Air travelers sit in tight quarters with the back of the knee pressed against the seat. The vein behind the knee is a common area for clots to form.
- Immobility can raise the risk of a clot, but your seat assignment, turbulence, etc. can make it difficult to move around the plane.
- Your body takes in less oxygen when air pressure is lower, and some data suggest that lower oxygen levels can trigger the body’s clotting response.
- Dehydration may also increase the risk of a clot and drinking coffee or alcohol on a flight can fast-track dehydration.
- Many people sleep on flights – but if you’re sleeping, you aren’t moving or hydrating.
The good news is that there are several commonsense methods that can help lower your risk:
- Choose a bulkhead seat or see if your flight offers extra-legroom seating. If not, avoid putting a bag under the seat in front of you so you have more space for your legs and feet.
- Try to move around the plane every 1-2 hours. Selecting an aisle seat can make it easier to get up and walk.
- Avoid sleeping in awkward positions for long periods of time.
- Try not to cross your legs.
- Avoid wearing tight clothing.
- Drink lots of water and avoid alcohol, caffeine, and sedatives.
- Do some simple exercises in your seat to improve blood flow. (See picture at bottom.)
WHAT DO THE GUIDELINES SAY?
2012 american college of chest physicians (accp) guidelines.
Low-risk travelers should frequently move, perform calf exercises, and sit in an aisle seat if possible.
It’s suggested that high-risk travelers wear properly fitted, below-knee compression stockings while in flight.
Preventive blood thinners or aspirin are not recommended for long-distance travelers.
2018 American Society of Hematology (ASH) Guidelines
Compression stockings or anticoagulants/aspirin are not recommended for low-risk travelers.
“For the average healthy person taking a long flight, we don’t recommend anything other than commonsense measures, like walking around the plane and staying hydrated,” explains Dr. Kahn, who helped write the guideline.
ASH suggests that high-risk passengers use graduated compression stockings or a preventive dose of low-molecular-weight heparin (LMWH) for flights over 4 hours, If these measures aren’t practical, travelers can consider taking aspirin.
Because there’s still a limited amount of data on travel-related VTE, the ASH recommendations are conditional, meaning that the right course of action may be different for each patient.
The bottom line:
- Travel-related blood clots are rare.
- Moving around and staying hydrated are two ways to stay healthy – both in flight and on the ground.
- Travel-related VTE is an area that needs more research. Clear-cut evidence is lacking.
- Talk to your healthcare provider if you’re concerned about developing a blood clot while traveling.
References :
Blood Clots and Travel: What You Need to Know. Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/dvt/travel.html . Updated February 1, 2019.
Kahn SR, et al. Chest. 2012;141(2):e195s-e226s.
Planes, Trains, and VTE. American Society of Hematology Clinical News. https://www. ashclinicalnews.org/features/feature-articles/planes-trains-vtes/. Updated March 1, 2019.
*Originally published in The Beat – December 2019. Read the full newsletter here .
Blood Clot Blood Clots Blood Thinner Deep Vein Thrombosis Exercise Prevention Risk Risk Factors Travel
Related Articles

About Blood Clots
What Is My Risk of Getting a Blood Clot, Really?
How Your Body Makes a Clot: The Coagulation Cascade

American Heart Month: How to Keep Active During the Colder Months
The Procedure Playbook: A New Educational Resource from NATF
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
- Section 8 - Perspectives : Responding to Medical Emergencies When Flying
- Section 8 - Jet Lag
Deep Vein Thrombosis & Pulmonary Embolism
Cdc yellow book 2024.
Author(s): Nimia Reyes, Karon Abe
Pathogenesis
Air travel–related venous thromboembolism, risk factors, clinical presentation, preventive measures, recommendations.
Deep vein thrombosis (DVT) is a condition in which a blood clot develops in the deep veins, usually in the lower extremities. A pulmonary embolism (PE) occurs when a part of the DVT clot breaks off and travels to the lungs, which can be life-threatening. Venous thromboembolism (VTE) refers to DVT, PE, or both. VTE is often recurrent and can lead to long-term complications (e.g., post-thrombotic syndrome after a DVT, chronic thromboembolic pulmonary hypertension after a PE).
Extended periods of limited mobility inherent to long-distance travel could increase a traveler’s risk for VTE. An association between VTE and air travel was first reported in the early 1950s; since then, long-distance air travel has become more common, leading to increased concerns about travel-related VTE.
Virchow’s classic triad for thrombus formation is venous stasis, vessel wall damage, and a hypercoagulable state. Prolonged, cramped sitting during long-distance travel interferes with venous flow in the legs, creating venous stasis. Seat-edge pressure to the popliteal area of the legs can aggravate venous stasis and contribute to vessel wall damage. Coagulation activation can result from an interaction between air cabin conditions (e.g., hypobaric hypoxia) and individual risk factors for VTE. Studies of the pathophysiologic mechanisms for the increased risk of VTE after long-distance travel have not produced consistent results, but venous stasis appears to play a major role. Other factors specific to air travel might increase coagulation activation, particularly in travelers with preexisting risk factors for VTE.
The annual incidence of VTE in the general population is estimated to be 0.1% but is greater in subpopulations with risk factors for VTE ( Box 8-03 ). The actual incidence of travel-related VTE is difficult to determine because there is no national surveillance for VTE and no consensus on the definition of travel-related VTE, particularly regarding duration of travel and period of observation after travel.
Box 8-03 Venous thromboembolism (VTE) risk factors
- Cancer (active)
- Estrogen use (hormonal contraceptives or hormone replacement therapy)
- Hospitalization, surgery, or trauma (recent)
- Limited mobility (e.g., prolonged bed rest, paralysis, extended period of restricted movement [such as wearing a leg cast])
- Obesity (Body Mass Index [BMI] ≥30 kg/m2)
- Older age (increasing risk after age 40)
- Pregnancy and the postpartum period
- Previous VTE
- Serious medical illness
- Thrombophilia (inherited or acquired) or a family history of VTE
Studies estimating the incidence of air travel–related VTE have used various criteria to determine risk factors and end points. For example, investigators have defined long-distance air travel as lasting anywhere from >3 hours to >10 hours. Although no standard definition exists, >4 hours is most often used. Post-flight observation period is similarly inconsistent and ranges from “hours after landing” to ≥8 weeks; 4 weeks, however, is most common. Finally, study outcomes range from asymptomatic DVT to symptomatic DVT/PE to severe or fatal PE. Asymptomatic DVT was estimated to be 5–20 times more common than symptomatic events, but asymptomatic DVT is of uncertain clinical significance and often resolves spontaneously.
In general, the incidence of air travel–related VTE appears to be low. For flights >4 hours, one study reported an absolute risk for VTE of 1 in 4,656 flights; another reported an absolute risk of 1 in 6,000 flights. People who travel on long-distance flights generally are healthier and therefore at a lower risk for VTE than the general population. Five prospective studies conducted to assess the incidence of DVT after travel >8 hours among travelers at low to intermediate risk for VTE yielded an overall VTE incidence of 0.5%; the incidence of symptomatic VTE was 0.3%.
Studies indicate that long-distance air travel might increase a person’s overall risk for VTE by 2- to 4-fold. Some studies found that long-distance air travel increased the risk of VTE occurring, while others either found no definitive evidence of increased risk, or found that risk increased only if ≥1 additional VTE risk factors were present. Level of risk correlates with duration of travel and with preexisting risk factors for VTE. Risk decreases with time after air travel and returns to baseline by 8 weeks; most air travel–related VTE occurs within the first 1–2 weeks after the flight.
A similar increase in risk for VTE is noted with other modes of long-distance travel (bus, car, train), which implies that increased risk is due mainly to prolonged limited mobility rather than by the air cabin environment.
Most travel-related VTE occurs in travelers with preexisting risk factors for VTE (Box 8-03). The combination of air travel with preexisting individual risk factors might synergistically increase risk. Some studies have shown that 75%–99.5% of people who developed travel-related VTE had ≥1 preexisting risk factor; one study showed that 20% had ≥5 risk factors. For travelers without preexisting risk factors, the risk of travel-related VTE is low.
For air travelers, height appears to be an additional risk factor; people <1.6 m (5 ft, 3 in) and those >1.9 m (6 ft, 3 in) tall were at increased risk. Because airline seats are higher than car seats and cannot be adjusted to a person’s height, air travelers <1.6 m (5 ft, 3 in) tall might be more prone to seat-edge pressure to the popliteal area. Air travelers >1.9 m (6 ft, 3 in) tall are also at increased risk, possibly because taller travelers have less leg room.
Signs and symptoms of DVT/PE are nonspecific. Typical signs or symptoms of DVT in the extremities include pain or tenderness, swelling, warmth in the affected area, and redness or discoloration of the overlying skin. The most common signs or symptoms of acute PE include unexplained shortness of breath, pleuritic chest pain, cough or hemoptysis, and syncope.
Imaging studies are needed for diagnosis. Duplex ultrasonography is the standard imaging procedure for DVT diagnosis. Computed tomographic pulmonary angiography is the standard imaging procedure for diagnosis of PE. Ventilation-perfusion scan is the second-line imaging procedure.
Anticoagulant medications commonly are used to treat DVT or PE; anticoagulants also are used for VTE prophylaxis. Bleeding can be a complication of anticoagulant therapy. The most frequently used injectable anticoagulants are unfractionated heparin, low molecular weight heparin (LMWH), and fondaparinux. Oral anticoagulants include apixaban, betrixaban, dabigatran, edoxaban, rivaroxaban, and warfarin.
The American College of Chest Physicians (ACCP) and the American Society of Hematology (ASH) each provide guidelines on the prevention of VTE in long-distance travelers.
American College of Chest Physicians Guidelines
ACCP 2012 guidelines (Grade 2C: weak recommendations, low- or very low-quality evidence): for long-distance travelers (>6 hours travel) at increased risk of VTE, the ACCP recommends frequent ambulation, calf muscle exercise, sitting in an aisle seat if feasible, and use of properly fitted below-the-knee graduated compression stockings (GCS) providing 15–30 mmHg of pressure at the ankle during travel. For long-distance travelers not at increased risk of VTE, use of GCS is not recommended. ACCP suggests against the use of aspirin or anticoagulants to prevent VTE in long-distance travelers.
American Society of Hematology Guidelines
ASH 2018 guidelines (conditional recommendations, very low certainty in the evidence of effects): for long-distance travelers (>4 hours travel) at substantially increased VTE risk (e.g., recent surgery, prior history of VTE, postpartum, active malignancy, or ≥2 risk factors, including combinations of the above with hormone replacement therapy, obesity, or pregnancy) the ASH guideline panel suggests GCS or prophylactic low molecular weight heparin (LMWH). If GCS or LMWH are not feasible, ASH suggests using aspirin rather than no VTE prophylaxis. For travelers without risk factors, ASH suggests not using GCS, LMWH, or aspirin for VTE prophylaxis.
Graduated Compression Stockings & Pharmacologic Prophylaxis
GCS appear to reduce asymptomatic DVT in travelers and are generally well tolerated. Decisions regarding use of pharmacologic prophylaxis for long-distance travelers at high risk should be made on an individual basis. When the potential benefits of pharmacologic prophylaxis outweigh the possible adverse effects, anticoagulants rather than antiplatelet drugs (e.g., aspirin) are recommended. People at increased risk should be evaluated with enough time before departure so that they understand how to take the medication; evaluate whether the traveler could have potential adverse effects from the combination of pharmacologic prophylaxis with any other medications they are taking.
No evidence exists for an association between dehydration and travel-related VTE. Furthermore, no direct evidence exists to support the concept that drinking plenty of nonalcoholic beverages to ensure adequate hydration or avoiding alcoholic beverages has a protective effect. Therefore, maintaining hydration is reasonable and unlikely to cause harm, but it cannot be recommended specifically to prevent travel-related VTE.
In-Flight Mobility & Seat Assignment
Immobility while flying is a risk for VTE. Indirect evidence suggests that maintaining mobility could prevent VTE. In view of the role that venous stasis plays in the pathogenesis of travel-related VTE, recommending frequent ambulation and calf muscle exercises for long-distance travelers is reasonable.
An aisle seat also might be a protective factor to reduce the risk of developing VTE. In one study, travelers seated in window seats experienced a 2-fold increase in general risk for VTE compared with passengers in aisle seats; travelers with a body mass index ≥30 kg/m2 who sat in window seats had a 6-fold increase in risk. Conversely, aisle seats are reported to have a protective effect compared with window or middle seats, probably because travelers are freer to move around.
General protective measures for long-distance travelers include calf muscle exercises, frequent ambulation, and aisle seating when possible. Additional protective measures for long-distance travelers at increased risk of VTE include properly fitted below-the-knee GCS and anticoagulant prophylaxis, but only in particularly high-risk cases where the potential benefits outweigh the risks.
The following authors contributed to the previous version of this chapter: Nimia L. Reyes, Michele G. Beckman, Karon Abe
Bibliography
Aryal KR, Al-Khaffaf H. Venous thromboembolic complications following air travel: what’s the quantitative risk? A literature review. Eur J Vasc Endovasc Surg. 2006;31(2):187–99.
Bartholomew JR, Schaffer JL, McCormick GF. Air travel and venous thromboembolism: minimizing the risk. Cleve Clin J Med. 2011;78(2):111–20.
Chandra D, Parisini E, Mozaffarian D. Meta-analysis: travel and risk for venous thromboembolism. Ann Intern Med. 2009;151(3):180–90.
Eklöf B, Maksimovic D, Caprini JA, Glase C. Air travel–related venous thromboembolism. Dis Mon. 2005;51(2–3):200–7.
Kahn SR, Lim W, Dunn AS, Cushman M, Dentali F, Akl EA, et al. Prevention of VTE in nonsurgical patients: antithrombotic therapy and prevention of thrombosis, 9th edition: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012;141(2 Suppl):e195S–226S.
Schobersberger W, Schobersberger B, Partsch H. Travel-related thromboembolism: mechanisms and avoidance. Expert Rev Cardiovasc Ther. 2009;7(12):1559–67.
Schreijer AJ, Cannegieter SC, Caramella M, Meijers JC, Krediet RT, Simons RM, et al. Fluid loss does not explain coagulation activation during air travel. Thromb Haemost. 2008;99(6):1053–9.
Schreijer AJ, Cannegieter SC, Doggen CJ, Rosendaal FR. The effect of flight-related behaviour on the risk of venous thrombosis after air travel. Br J Haematol. 2009;144(3):425–9.
Schünemann HJ, Cushman M, Burnett AE, Kahn SR, Beyer-Westendorf J, Spencer FA, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: prophylaxis for hospitalized and nonhospitalized medical patients. Blood Adv. 2018;2(22):3198–225.
Watson HG, Baglin TP. Guidelines on travel-related venous thrombosis. Br J Haematol. 2011;152(1):31–4.
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.

Appointments at Mayo Clinic
Foot swelling during air travel: a concern, what causes leg and foot swelling during air travel.
Leg and foot swelling during air travel is common. It's usually harmless. The most likely reason for it is sitting for a long time without moving during a flight.
Sitting with the feet on the floor for a long time causes blood to pool in the leg veins. The position of the legs while seated also increases pressure in the leg veins. This plays a role in swelling by causing fluid to leave the blood and move into the surrounding soft tissues.
A dangerous blood clot called deep vein thrombosis (DVT) sometimes causes leg swelling. But the risk of getting DVT on an airplane is very low for healthy people, especially on flights that last under four hours. In general, the chance of getting DVT starts to rise on flights over 12 hours.
You can reduce foot and leg swelling, and lower your risk of blood clots, by wearing compression stockings on a long flight. The stockings apply pressure to the lower legs.
If you notice swelling in one leg that doesn't go away or starts within two weeks of a long flight, get a health care checkup right away. The swelling might be a symptom of DVT or another condition that needs treatment. If you have a higher risk of blood clots, talk with a member of your health care team before you fly.
John M. Wilkinson, M.D.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Hand swelling during exercise: A concern?
- Clarke MJ, et al. Compression stockings for preventing deep vein thrombosis in airline passengers (review). Cochrane Database of Systematic Reviews. 2021; doi:10.1002/14651858.CD004002.pub4.
- Douketis JD, et al. Prevention of venous thromboembolism in adult travelers. https://www.uptodate.com/contents/search. Accessed June 27, 2023.
- Blood clots and travel: What you need to know. Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/dvt/travel.html. Accessed June 27, 2023.
- AskMayoExpert. Health considerations for air travelers. Mayo Clinic; 2022.
- Jong EC. Jet health. Travel and Tropic Medicine Manual. Elsevier; 2017. https://www.clinicalkey.com. Accessed June 27, 2023.
- Smith CC. Clinical manifestations and evaluation of edema in adults. https://www.uptodate.com/contents/search. Accessed June 27, 2023.
- The effect of compression stocking on leg edema and discomfort during a 3-hour flight: A randomized controlled trial. European Journal of Internal Medicine. 2019; doi:10.1016/j.ejim.2019.01.013.
- Nishmura N, et al. Gravity-induced lower-leg swelling can be ameliorated by ingestion of α-glucosyl hesperidin beverage. Frontiers in Physiology. 2021; doi:10.3389/fphys.2021.670640.
- Wilkinson JM (expert opinion). Mayo Clinic. July 4, 2023.
Products and Services
- Available Compression Products from Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Mitral valve clip to treat mitral regurgitation: Bob's story
- Mitral valve overview
- Chronic sinusitis
- Cold urticaria
- Compression bandaging
- Mitral valve regurgitation
- Myocarditis
- Robotic heart surgery treats mitral regurgitation: Ed's story
- Scleroderma
- Symptom Checker
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Foot swelling during air travel A concern
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
How to tell if you're getting a blood clot while flying

Travelers have never been more aware of their health and safety when flying. But for some people, the novel coronavirus isn't the only health risk they're worried about on airplanes.
According to the National Blood Clot Alliance , an average of 274 people die from blood clots every day and 600,000 nonfatal blood clots occur every year. Air travel can increase this risk as you're sitting for long periods with little room to move your legs. This can cause a particular type of blood clot called deep vein thrombosis (DVT).

"DVT's are more likely to form when there is venous stasis, which means that the blood is pooling in the veins," Dr. Mehmet Oz (of "The Dr. Oz Show") told The Points Guy. "This is more likely to happen in people who are sedentary for long periods, like on a long plane ride, because part of the way the blood in the leg veins gets back up to the heart is when muscles contract."
In 2018, Dr. Rajiv Narula, MD — founder of the International Travel Health Consultants — told TPG that "on flights more than eight hours, [there's an] increased risk of DVT." And certain studies say this condition can occur on flights as short as four hours.
While the condition can resolve itself, in some cases people experience a pulmonary embolism: when the clot travels to the lungs and blocks blood flow there. The blocked blood flow in the lung prevents the body from getting oxygen.
So, how can you tell if you have a blood clot on a plane ? We chatted with a couple of experts to learn the symptoms, find out who is most susceptible and what to do if you develop one during a flight.
Related: It's flu season — Here's how to avoid getting sick on a plane
Know if you're at risk
According to Dr. Narula, travelers with certain "underlying medical issues" are typically more prone to DVT.
Several factors can make a person more susceptible to developing a blood clot.
"Things that put you at risk for blood clots include certain genetic clotting disorders, being immobilized because of surgery or injury, chronic diseases like heart failure and cancer, smoking and older age," said Dr. Oz.

Dr. Nathan Favini, medical lead at Forward , a new technology-based healthcare startup, added that oral birth control pills and pregnancy also make a blood clot more likely. "Estrogen is thought to be the cause," he said. "So, forms of birth control that don't contain estrogen, like IUDs, are safer in this regard."
If you fall into one of these categories, you should take extra precautions to help prevent blood clots and be aware if you start to develop any symptoms.
Related: What happens if you get sick during a flight?
Symptoms of a blood clot
Knowing you have a blood clot can be tricky, as you can often write off the symptoms as something else, but there are a few key warning signs to pay attention to when traveling. If you experience these symptoms, you should seek medical help immediately.
"If you develop pain, tenderness, swelling, warmth and/or redness in your legs during a flight, those may be signs of a deep vein thrombosis or blood clot," said Dr. Favini. "If you have more than one or many of those symptoms, it becomes more likely that you're experiencing a clot."
When TPG's former social media director developed a blood clot during a six-hour flight home from Iceland, she woke up with sore and aching calves and felt dizzy, hot and light-headed.

The other thing to look out for, according to Dr. Favini, is the rapid onset of shortness of breath. This can be a sign that a clot has formed in, or traveled to, your lungs.
"If you're experiencing these symptoms, especially shortness of breath, let the staff on your airplane know right away," said Dr. Favini.
Related: I got food poisoning before my long-haul flight
How to prevent a blood clot
So, now you know what to look for if you're developing a blood clot. But, there are certain critical steps you can take to avoid one in the first place.
"Drink lots of fluids, but not with caffeine, which makes you pee more so [there's] less fluid in your blood ... And avoid alcohol," said Dr. Oz. "Then, move around every two hours and move [your] feet like stepping on a gas pedal more frequently."
When TPG spoke to Daniel Giordano, co-founder of Bespoke Treatments Physical Therapy in New York City, about movements and stretches travelers can easily perform on an airplane to promote blood circulation, Giordano said he recommends his clients travel with a device such as a Firefly knee strap . This can gently stimulate the peroneal nerve to promote circulation while performing simple exercises like, as Dr. Oz suggested, pumping your legs.
And for Dr. Narula, the key is anti-embolism socks. These knee-high stockings are specifically designed to put graduated pressure on your legs, which can improve circulation.
Additional reporting by Melanie Lieberman.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
The Ultimate Guide to Compression Socks for Flying
- How They Work
- Choosing the Right Socks
- How to Wear Them
- Side Effects
- Who Should Avoid Them?
- Seeking Medical Care
Compression socks (also called compression stockings) are a type of foot and leg covering that squeezes (compresses) the legs and increases blood flow. Compression socks can be helpful while flying as they can lower your risk for blood clots, especially if you have circulation issues.
This article discusses how compression socks work, their benefits, how to choose the most effective pair for your needs, and the potential side effects.
nito100 / Getty Images
How Compression Socks Work for Air Travel
If you're at a higher risk for blood clots based on your health history, a healthcare provider may recommend compression socks when flying. Compression socks are tighter than regular socks and boost blood circulation by squeezing the legs. This can help lower the chance of leg swelling, pain, and blood clots.
During air travel, you usually have to sit in one place for an extended period—typically longer than you would otherwise sit throughout the day. This prolonged sitting can affect blood flow throughout the body, raising the risk of blood clots . The risk of a blood clot while flying is a more significant concern during long-distance flights, considered four hours or longer.
Compression socks offer varying compression levels, depending on your needs.
Graduated Compression Socks
Graduated compression socks, also called medical compression socks or stockings, place the most pressure around the ankles and less pressure as the socks go up the legs. This encourages better blood flow toward the heart.
Nonmedical Support Hosiery
Nonmedical support hosiery provides a uniform amount of pressure around the full stocking. Nonmedical support hosiery is inexpensive and usually easy to find at pharmacies. You can buy them without a prescription. They may be helpful if you commonly have tired, achy legs.
Anti-Embolism Stockings
Anti-embolism stockings provide uniform pressure throughout the stocking. They also provide less pressure than graduated compression stockings. They are geared toward someone who is not moving a lot and may be recovering from surgery.
Benefits of Compression Socks for Flying
Wearing compression socks while flying offers several potential benefits, such as:
- Encouraging better circulation, which helps lower the risk of blood clots
- Reducing or preventing leg swelling
- Preventing dull, achy legs
- Lowering your risk for deep vein thrombosis (DVT)
A healthcare provider may recommend that you wear compression socks while flying if you:
- Are pregnant
- Had recent surgery
- Have a clotting disorder
- Have varicose veins, which can impede your blood flow
- Often get a heavy, achy feeling in your legs or swelling
A healthcare provider may also recommend using compression socks while flying, even if you have none of these issues. The socks can help anyone by encouraging better circulation, particularly when you're not moving around as much as usual, such as during a flight.
Choosing the Right Compression Socks for Flying
If you want to choose the right compression socks for flying, consider the following factors:
Compression Levels
You'll want to choose socks that are the right compression level for you. The level of compression in these stockings is measured by millimeters of mercury, or mmHg (the same measurement used for blood pressure). A higher number indicates more compression. Information on the different levels of compression is as follows:
You can check with a healthcare provider to determine which compression level is best for your health needs while flying. Some compression socks are available over the counter (OTC) at drugstores, while prescription stockings mush be ordered by a healthcare provider. Which type you use depends on your health needs and whether your health insurance covers them.
How to Stay Comfortable During a Long Flight
In addition to wearing compression socks, try the following to stay comfortable and encourage blood circulation during a long flight:
- Ask for an aisle seat so it's easier for you to get up and walk around regularly.
- Do in-seat exercises to improve circulation, such as ankle circles, leg extensions, lifting your knee toward your chest, and holding it there for 15 seconds.
- Know the symptoms of a blood clot in the leg , including pain, warmth, and redness.
- Stay hydrated and avoid alcohol, which dehydrates you.
- Wear comfortable, loose-fitting clothing.
If you have a heart condition, check with a healthcare provider to ensure it's OK to fly.
Other Considerations When Choosing Compression Socks
Compression socks come in a variety of sizes and materials. Some are knee-high (usually the most comfortable), some go up to the thighs, and some are full-length (like pantyhose). They're also made with different materials. Sock length will be determined by your health requirements as recommended by your healthcare provider.
Tips to keep in mind when choosing compression socks are:
- Aim for compression socks with a firm fit that aren't too tight. They shouldn't hurt.
- Medical equipment stores often carry prescription socks and staff are able to assign you an accurate fit.
- If you can, buy two pairs to have some available while washing and drying the other pair.
If you wear compression socks regularly—not just while flying—replace them every six months. They lose elasticity over time and become less effective.
How to Wear Compression Socks While Flying
If you've settled on a pair of compression socks that suit you, the next thing you'll want to consider is how to wear them when flying.
When to Put Them On
Try on the compression stockings before flying to be sure they fit properly. Don't wait until directly before your flight to try them on for the first time. If you can, do a test run at the time of day that you have the least amount of swelling, such as in the morning. On the day of the flight, put them on before you board.
How Long to Wear Compression Socks
It's usually OK to wear compression socks all day but always check the label first. Most of the time, you can wear them comfortably during the duration of your flight. While some brands suggest nighttime wear as well, compression socks typically are designed to be worn during the day and taken off before bedtime.
Potential Side Effects of Wearing Compression Socks While Flying
It's important to wear compression socks that fit you properly. You may experience side effects such as the following if the socks aren't a perfect fit:
- Chafing and bruising (the risk for this increases if you have dry skin on your legs or if you're more prone to cuts)
- Cutting off your circulation
- Redness around the skin
Always follow the recommendation of your healthcare provider on whether compression socks may benefit you the next time you fly.
Who Should Avoid Compression Socks for Flying?
Compression socks are safe for most people. However, check with a healthcare provider first if you have peripheral artery disease (PAD) or diabetes.
You should avoid compression socks if you're allergic to the material that they're made from. You can ask your healthcare provider about alternatives to compression socks for flying.
When to Contact a Healthcare Provider
Let a healthcare provider know if you experience any of the following symptoms:
- A rash on your legs or feet
- Discomfort in your legs or feet while wearing your socks compared to the last time you wore them
- New pain or swelling
- Numbness in your legs or feet/toes
- Redness or warmth in your legs or feet
Compression socks help encourage blood flow toward the heart. They can reduce the risk of blood clots, leg swelling, and aching. Compression socks have different compression levels, ranging from a low level if you want extra support to a firm level if you have severe leg pain or previous blood clot problems.
Wear well-fitting compression socks while flying to avoid side effects such as redness, chafing, or cutting off circulation.
MedlinePlus. Compression stockings .
Centers for Disease Control and Prevention. Blood clots: what you need to know .
Lim CS, Davies AH. Graduated compression stockings . CMAJ . 2014;186(10):E391-8. doi:10.1503/cmaj.131281.
Ochsner Health. Who should wear compression socks?
Centers for Disease Control & Prevention. Deep vein thrombosis and pulmonary embolism .
University of Michigan Health. Compression stockings: How to use them .
NHS. How long should I wear compression socks to improve my circulation .
Rother U, Grussler A, Griesbach C, Almasi-Sperling V, Lang W, Meyer A. Safety of medical compression stockings in patients with diabetes mellitus or peripheral arterial disease . BMJ Open Diabetes Res Care. 2020;8(1):e001316.
NHS. Anti-embolic stockings .
By Vanessa Caceres Caceres is a Florida-based health journalist with 15 years of experience. She holds a bachelor's degree in journalism and psychology and a master's degree in linguistics.
Exercises to Stop Your Legs From Clotting on Airline Flights

Nobody likes long airline flights. Unless you're flying first class, the limited leg room in coach class can lead to stiff and cramped legs. For many people, this won't result in long-term consequences; however, for certain populations, it can be life-threatening if blood clots form in the legs.
Advertisement
If you're at high-risk for clotting, your doctor can prescribe medication. However, moving about the cabin frequently and doing DVT prevention exercises on an airplane can also help prevent a miles-high catastrophe.
Video of the Day
What Is DVT?
The National Heart, Lung, and Blood Institute states that deep vein thrombosis, or DVT, is a condition in which blood clots form in the body's deep veins, especially in those of the legs. In some cases, DVT can lead to a pulmonary embolism — and sudden death — if a blood clot breaks off and gets lodged in a lung.
Dehydration from the dry air of a plane cabin can cause the blood to thicken. Combine that with the immobility created by cramped seats and low cabin pressure, and you have a recipe for blood clotting in the legs.
Not everyone is at risk. According to the American Council on Exercise , those predisposed to clotting include:
- Individuals with cancer, or those who have chronic heart or respiratory failure
- People with a predisposition to clotting, obesity or varicose veins
- People who have recently had major surgery, been bed ridden or endured a leg injury
- Women who are pregnant or who have recently given birth; women who take contraceptives or those undergoing hormone replacement therapy
- People who are 40 years old and older
Read more: Long Flight? Here's How to Stay Healthy and Sane
Exercises in Flight
A frequently cited review published in 2011 by the Cleveland Clinic Journal of Medicine suggests getting up and walking around for about five minutes every hour on long flights of four hours or more. While you're seated, promote circulation with these exercises:
Ankle circles: Raise your feet off the floor. Point your toes and move them around in a circle, moving one foot clockwise and the other counter clockwise.
Foot lifts: Start with your feet flat on the floor. Keeping your heels on the floor, lift your toes up as high as they can go. Return both feet flat on the floor; then keeping your toes on the floor, lift your heels up as high as you can. Continue to alternate back and forth.
Knee lifts: Bend one knee and raise that leg off the seat. Contract the thigh muscles. Lower the leg and switch sides. Alternate back and forth for 20 to 30 repetitions.
Knee-to-chest: Bend forward slightly. Interlace your hands around the top of your shin, just below your knee. Pull the knee into your chest. Hold the position for 15 seconds; then slowly lower the leg back down. Switch sides. Repeat several times.
Read more: Exercises to Stop Your Legs From Clotting on Airline Flights
Standing Plane Exercises
When you're safely able to move about the cabin, get up and walk around. If that is discouraged, you can often stand in the aisle by your seat or in the areas near the bathrooms. Take these opportunities to do some standing DVT prevention exercises on the plane to promote circulation.
Calf raises: Hold on to a seat back or other sturdy object for support. Stand with your feet hip-distance apart and slowly rise up onto your toes. Hold for a second or two; then slowly lower down. Repeat 10 to 20 times.
Marching in place: Bend one knee, bringing it up as high as you can. Return to standing and switch sides. Repeat 10 to 20 times.
Quadriceps stretch: Bend one knee bringing the foot up toward your butt. Keep your knees in line and take hold of the ankle of your lifted foot with the same-side hand. Pull the foot into your butt. Hold for 15 seconds, Release and switch sides.
Forward fold: Separate your feet and fold forward at your hips. Keep a slight bend in your knees. Reach your fingers to your shins or the floor. Hold for 15 seconds. Slowly roll up to standing vertebra by vertebra to avoid lightheadedness.
- American Council on Exercise: "How to Avoid Deep Vein Thrombosis on Long Plane Flights"
- National Institutes of Health: "What Is Deep Vein Thrombosis?"
- Cleveland Clinic Journal of Medicine: "Air Travel and Venous Thromboemolism: Minimizing the Risk"
- American Council on Exercise: Standing Calf Raises - Wall
- MayoClinic.com: Pulmonary Embolism: Risk Factors
Report an Issue
Screenshot loading...
Premium Content

What do long flights do to our bodies?
From dehydration and muscle soreness to nausea and indigestion, the typical discomfort and pain can all be explained by unnatural conditions on long flights.
If you’ve taken a long flight in a seat with limited recline recently, the discomfort of the experience is likely still painfully fresh.
While airline seat size and pitch (aka legroom) have shrunk since the 1990s , time passengers spend in the air is noticeably increasing.
When Qantas launches its nonstop Sydney to London route in late 2025, it will be the longest flight in the world at 20 hours of flying time. Current honors go to Singapore Airlines’ New York to Singapore route, which clocks in at over 18 hours.
The discomfort of long flights goes beyond cramped positions—there’s also dry air that can make your throat, nose, and skin feel dry, and air pressure changes while ascending and descending that can affect your sinuses. Worst case, flying could become deadly if a blood clot forms in your extremities and moves to your lungs.
But experts say most of us don’t have to worry. “Generally, flying is safe for everybody and the problems only occur when you have an underlying condition,” says Explorers Club fellow Michael J. Manyak , a physician specializing in urology and expedition medicine.
Experts break down how your body reacts to long flight times, and what you can do to mitigate discomfort.
Dry air and changes in air pressure
About 50 percent of the air circulating in-flight is pulled in from outside the plane at high and dry altitudes—so it’s generally far less humid than what you’re used to breathing on the ground, Manyak says. This environment can cause your eyes, nose and mouth to feel excessively dry.
“Your mucosal areas are drying out,” he says. “The dry air contributes to a lack of lubrication in your body’s systems.” Drinking plenty of water before and during your flight will help to keep you more comfortable and improve your circulation, too.
And while some respiratory conditions like asthma can be exacerbated by cold, dry air, most people don’t have to worry about symptoms beyond discomfort, Manyak adds.
Air pressure changes during take off and landing cause air in the sinuses to change and can result in pain in the nose and ears for some people, says Laleh Gharahbaghian , physician and clinical professor of emergency medicine at Stanford University.
“This is true for those experiencing sinus disease most profoundly, and felt only mildly as ‘ears needing to pop’ for healthy folks,” she says.
Gharahbaghian recommends taking decongestants before your flight, drinking water, and taking anti-inflammatory medicine if you have a cold or congestion.
Speaking of colds—while it might feel like you get sick or catch a cold every time you fly, Manyak says airports, “where everyone is mingling in waiting areas and there are no air filters,” are more likely where the real exposure occurs. According to the IATA, air in the cabin is half HEPA filtered , half fresh from outside the plane, and also renewed 20-30 times an hour.
( How clean is the air on planes ?)
Muscle soreness
If you don’t get the opportunity to move around, you’re holding a position—that means prolonged engagement of your muscles, which leads to soreness.
You May Also Like

The scandal of 'ghost flights': are empty planes haunting our skies?

How exercise can help—or hurt—your digestion

These 4 medicinal herbs may help keep men healthy
Gharahbaghian says it’s not unusual for people to feel stiffness in their back, neck, or even their thighs while enduring the same position for a long period of time.
Getting up to walk up and down the aisle when it’s safe or even adjusting your body and doing things like heel raises while seated can help, she says.
Most injuries can feel worse after sitting for a long period, since inflammation can build without movement to flush it out, says Kevin Lees, director of chiropractic operations at The Joint Chiropractic . Back injuries are no different, of course, and prolonged flexion (sitting for hours) can create pressure on the disks, rubbery cushions between the vertebrae of your spine—especially your lower back.
Slowed digestion, difficulty breathing
By sitting for too long, your digestive system is also affected, Lees says, as the movement of food slows on its way through the intestines.
“If you are sedentary, you do not get the physical stimulation to the intestines,” says Manyak. “This is one of the reasons why we try to get patients up and walking soon after surgery. It is also good for circulation and wound healing.”
( Jet lag doesn’t have to ruin your trip. Here’s what you can do .)
A slumped posture can restrict movement of the ribs, leading to slower and shallower breathing, too, Lees says. “Shallow breathing can lead to decreased oxygen intake…This can cause foggy thinking, dizziness, and even fatigue.”
Gastric reflux can result from a slumped posture, too, and has the potential to cause nausea, says Lees.
Manyak says any potential nausea or motion sickness from turbulence tends to be short-lived, since pilots try to divert from turbulent areas as soon as possible. “Motion sickness goes away almost immediately with stabilization of the environment,” he says.
DVT and blood clots on planes
By far, the biggest risk to your body on a long-haul flight is something that can also affect you on the ground when you remain for too long in a restricted position.
“The worst thing is deep venous thrombosis (DVT), or getting a blood clot in the legs,” Gharahbaghian says. “If a blood clot goes from your legs to your lungs, it can become a life-threatening problem.”
Signs of DVT include swelling, throbbing, or pain in one leg, says Manyak. “The pain occurs because you have impeded the blood supply and its return to the heart…The veins involved swell, causing pain.”
There’s a litany of factors that could predispose fliers to DVT, says Manyak, who himself learned he had a hereditary blood-clotting disorder after experiencing a clot after a trans-Atlantic flight.
These factors include a family history of blood clots, being pregnant or having recently given birth, having cancer or undergoing active or recent cancer treatment, taking birth control, says Manyak.
Getting up to walk the aisles every hour or so during a flight, doing heel raises while at your seat and wearing compression socks, which improve circulation in the legs, are a few of the things you can do to keep blood from pooling in your lower extremities on long flights, Manyak says.
It’s good advice for anybody who feels stir-crazy just thinking about their next long haul flight. “The biggest thing that causes discomfort for travelers during a long haul flight is the fact that you’re not moving,” Manyak says.
Related Topics
- DIGESTIVE SYSTEM

Inflammation isn't always bad. Here's how we can use it to heal.

Why women are more prone to autoimmune diseases

There’s another biome tucked inside your microbiome—here’s why it’s so important

Is ‘leaky gut’ real? It’s more complicated than you’d think.

What your fitness level says about your risk of cancer
- Environment
- Paid Content
History & Culture
- History & Culture
- History Magazine
- Gory Details
- 2023 in Review
- Mind, Body, Wonder
- Terms of Use
- Privacy Policy
- Your US State Privacy Rights
- Children's Online Privacy Policy
- Interest-Based Ads
- About Nielsen Measurement
- Do Not Sell or Share My Personal Information
- Nat Geo Home
- Attend a Live Event
- Book a Trip
- Inspire Your Kids
- Shop Nat Geo
- Visit the D.C. Museum
- Learn About Our Impact
- Support Our Mission
- Advertise With Us
- Customer Service
- Renew Subscription
- Manage Your Subscription
- Work at Nat Geo
- Sign Up for Our Newsletters
- Contribute to Protect the Planet
Copyright © 1996-2015 National Geographic Society Copyright © 2015-2024 National Geographic Partners, LLC. All rights reserved

IMAGES
VIDEO
COMMENTS
More than 300 million people travel on long-distance flights (generally more than four hours) each year. 1 Blood clots, also called deep vein thrombosis (DVT), can be a serious risk for some long-distance travelers. Most information about blood clots and long-distance travel comes from information that has been gathered about air travel.
Clots and Travel. Blood clots can sometimes form in your legs during air travel because you are immobile for long periods of time, often sitting in cramped spaces with little leg room. The clinical term for this type of blood clot is deep vein thrombosis (DVT). The longer the flight, the more at risk you are for developing a clot.
Drink water before and during the flight. The air you breathe inside a plane is often dry because the same air circulates around the cabin. When you're dehydrated, your blood gets thicker. Avoid ...
Prevent Blood Clots During Travel. Take steps to prevent blood clots. Stand up or walk occasionally. Select an aisle seat when possible so you can walk around every 2-3 hours. If traveling by car, include breaks in your travel schedule to stretch and walk around. Exercise your calf muscles and stretch your legs while you're sitting.
People who have severe symptoms of COVID-19 have an increased risk of pulmonary embolism. Bed rest. Being confined to bed for an extended period after surgery, a heart attack, leg fracture, trauma or any serious illness puts you at risk of blood clots. When your legs lie flat for long periods of time, the flow of blood through your veins slows ...
Doing exercises and staying hydrated are really the best tools we have on long flights.". If you've had DVTs in the past or are at high risk of recurrent blood clots, Dr. Bajakian recommends you talk to your doctor before taking a flight longer than 4 to 6 hours. In some extremely high-risk cases, she may prescribe a course of low-dose ...
Here's what you need to know about this type of traveling blood clot. Deep vein thrombosis (DVT) is a medical condition that occurs when a blood clot develops deep in a vein. These clots ...
Blood clots are formed when blood is sluggish or constricted, such as when seated in an upright position with the knees bent and the hips stuck at 90-degree angles for extended periods of time. This leads to slowing and even pooling of the blood, especially in the abdomen and lower extremities. While most individuals travel without any ...
Blood clots affect about 1-2 in 1,000 U.S. adults per year, and the risk may double or triple after a flight that's 4+ hours. One study estimates that 1 in 4,600 travelers will have a blood clot within 4 weeks of a long flight. According to Dr. Kahn, "the actual risk of a travel-related blood clot is quite small, and the average traveler ...
A blood clot, also called a thrombus, is a semi-solid mass of blood that forms in a vein or artery. Blood clots may be stationary and block blood flow, or they may be loose and travel to different ...
Summary. The risk of a blood clot traveling around the body is highest within the first 4 weeks after it initially forms. However, health experts are unsure of exactly how long it takes for a ...
Preventing Travel-Related Blood Clots: A "Passport to Safety". As holidays or vacation time approaches, it is never too early to think about protecting yourself from the risk of blood clots when you travel for more than four hours - whether it is by plane, train, car or bus. The National Blood Clot Alliance has published a one page ...
What to Know About Air Travel if You Have Peripheral Vascular Disease. ... If you stay sitting for the entire flight, your risk of blood clots in your legs increases. This is a risk for anyone ...
Deep vein thrombosis (DVT) is a condition in which a blood clot develops in the deep veins, usually in the lower extremities. A pulmonary embolism (PE) occurs when a part of the DVT clot breaks off and travels to the lungs, which can be life-threatening. Venous thromboembolism (VTE) refers to DVT, PE, or both.
If a person does not receive treatment for a blood clot in the leg, it can pose serious risks. The blood clot can dislodge from the vein and travel through the bloodstream to the lungs ...
A dangerous blood clot called deep vein thrombosis (DVT) sometimes causes leg swelling. But the risk of getting DVT on an airplane is very low for healthy people, especially on flights that last under four hours. In general, the chance of getting DVT starts to rise on flights over 12 hours.. You can reduce foot and leg swelling, and lower your risk of blood clots, by wearing compression ...
Embolisms are blood clots that break free and travel to other parts of your body. Less common, thankfully, are arterial clots. ... The most common signs of a blood clot in your leg include: Swelling.
It is perhaps fitting that of the multitudes of studies presented, several concerned the association of air travel as a risk factor for deep venous thrombosis (DVT). Symington and Stack, who reported an apparent increase in DVT in air travelers compared to non-travelers, first described "Economy Class Syndrome" or "Traveler's Thrombosis ...
According to the National Blood Clot Alliance, an average of 274 people die from blood clots every day and 600,000 nonfatal blood clots occur every year. Air travel can increase this risk as you're sitting for long periods with little room to move your legs. This can cause a particular type of blood clot called deep vein thrombosis (DVT).
Compression socks are tighter than regular socks and boost blood circulation by squeezing the legs. This can help lower the chance of leg swelling, pain, and blood clots. During air travel, you usually have to sit in one place for an extended period—typically longer than you would otherwise sit throughout the day.
Knee-to-chest: Bend forward slightly. Interlace your hands around the top of your shin, just below your knee. Pull the knee into your chest. Hold the position for 15 seconds; then slowly lower the leg back down. Switch sides. Repeat several times. Read more: Exercises to Stop Your Legs From Clotting on Airline Flights.
Experts break down how your body reacts to long flight times, and what you can do to mitigate discomfort. Dry air and changes in air pressure. About 50 percent of the air circulating in-flight is ...