Voice speed
Text translation, source text, translation results, document translation, drag and drop.

Website translation
Enter a URL
Image translation
Patient journey 101: Definition, benefits, and strategies
Last updated
22 August 2023
Reviewed by
Melissa Udekwu, BSN., RN., LNC
Today’s patients are highly informed and empowered. They know they have choices in their healthcare, which can put healthcare providers under a lot of pressure to provide solutions and meet their patients’ expectations.
Just like any customer, patients embark on a journey that begins before they ever contact the provider. This makes understanding the journey and where improvements can be made extremely important. Mapping the patient journey can help practitioners provide better care, retain a solid customer base, and ultimately identify ways to improve patient health.
- What is the patient journey?
The patient journey is best described as the sequence of experiences a patient has from admission to discharge. This includes all the touchpoints between the patient and provider from beginning to end.
The patient journey continues through consultation, where they meet the potential caregiver. That portion of the journey includes interactions with a doctor and support staff, how long they wait to be seen, and the steps taken for diagnosis and treatment.
The patient’s post-care journey includes follow-ups from the healthcare provider, post-treatment care, and billing. For example, if the patient has questions about post-surgery care or how to read their invoice, how quickly their questions are answered and their problems resolved will impact their satisfaction.
Mapping the patient journey helps healthcare providers improve patient satisfaction at every step of the way. By collecting data at each stage and conducting an in-depth analysis, providers can identify patient concerns and make the necessary improvements to meet their patient satisfaction goals.
What is another name for the patient journey?
The term “patient funnel” describes the journey patients take from first learning about a healthcare provider or healthcare product to actually making an appointment or purchase. This “funnel” can be applied to any type of business, describing the stages a customer goes through to obtain a service.
- Understanding the stages of the patient journey
Each stage of the patient journey is essential to a positive patient experience . Gathering and analyzing data can alert healthcare providers to potential issues throughout the journey.
Data collection at each of the following stages will give healthcare providers the information they need to make the necessary improvements:
1. Awareness
Awareness is where the patient journey begins. This is when they first research symptoms and identify the need to see a medical professional.
They may consider at-home remedies and get advice from friends, social media, or websites. Once they identify the need for a healthcare provider, they continue their research via review sites, advertising campaigns, and seeking referrals from friends and family.
Determining the way patients become aware they need healthcare and the sources they use for research is important. The data collected at this stage could suggest your organization has an insufficient social media presence, inadequate advertising, or a website in need of an update.
To remedy these shortcomings, you might consider adding informational blogs to your website, performing a social media analysis, or closely monitoring customer reviews.
This stage in the patient journey is where the patient schedules services with the healthcare provider.
This engagement is essential for acquiring new patients and retaining current patients. Patients will contact you in several ways to schedule an appointment or get information. Most will call on the first attempt to schedule an appointment.
This is a crucial touchpoint in the journey. A new patient may become frustrated and move on if they find it difficult to access your services or are placed on hold for a long period or transferred numerous times.
Patient engagement occurs in other ways, such as your online patient portal, text messages, and emails. Your patients may interact differently, so it’s important to gather data that represents their preferred means of communication. Work to make the improvements required to correct access issues and ensure efficient communication.
The care stage can include everything from your patient’s interaction with the front desk to how long they have to wait in the examination room to see a doctor.
Check-in, check-out, admissions, discharge, billing, and of course, the actual visit with the healthcare provider are other touchpoints in the care stage.
There are a couple of ways to gather and analyze this data. Most organizations choose to analyze it holistically, even if it’s collected separately. For example, you might gather data about the patient’s interaction with the front desk, the clinical visit, and the discharge process, but you may want to analyze the care segment as a whole.
4. Treatment
Treatment may be administered in the office. For example, a patient diagnosed with hypertension may have medication prescribed. That medication is the treatment. Gathering information at this stage is critical to see how your patient views the healthcare provider’s follow-up or responses to inquiries.
In most cases, treatment extends beyond the initial clinical visit. For example, a patient might require additional tests to get a diagnosis. Providing the next steps to a patient in a timely manner and letting them know the test results is crucial to patient satisfaction .
5. Long term
A satisfied patient results in a long-term relationship and referrals to friends and family. Most of the data collected at this stage will be positive since the patient is continuing to use your services.
Gathering data after the treatment stage allows you to expand on the qualities that keep patients returning for your services in the long term.
- Benefits of patient journey mapping
The patient benefits from their healthcare provider understanding their journey and taking steps to improve it. Healthcare providers also reap several benefits, including the following:
1. Efficient patient care
When they understand the patient journey, healthcare providers can provide care more efficiently and spend less time and money on unnecessary, unwanted communications.
2. Proactive patient care
Proactive patient care is aimed at preventing rather than treating disease. For example, women who are over a certain age should have an annual mammogram, smokers may be tested for lung disease, and elderly women may need a bone density study. These preventative measures can help keep disease at bay, improve health outcomes, and build trust with patients.
3. Value-based patient care
Patients don’t want to feel they are being charged unfairly for their healthcare. Focusing on the individual patient promotes satisfaction and yields positive outcomes.
The Center for Medicare and Medicaid Services (CMS) has issued recent guidelines for participants that help offset the costs of high-quality care through a reward system.
4. Retention and referrals
Patients who are happy with their journey will keep returning for healthcare, and happy patients equal voluntary referrals. Many providers offer rewards to incentify referrals.
- How to get started with patient journey mapping
Follow the steps below to start the patient journey mapping process:
Establish your patient personas
Journey mapping is a great way to identify your patient’s characteristics so that their experience can be further enhanced.
Some of the following determinations can help you pinpoint your patient’s persona and establish protocols to provide a better service:
How do your patients prefer to communicate? Are they more comfortable with phone calls, texts, or other methods?
How are most patients finding your services? Are they being referred by friends or family members, or are they seeing advertisements?
Would the patient prefer in-person communication or telecommunication?
What are the patient’s expectations of care?
This data can be complex and widespread, but it can give you the information you need to more effectively and efficiently communicate with your patients.
Understand the entire patient lifecycle
Each patient is unique. Understanding the patient lifecycle can avoid confusion and miscommunication.
To positively engage the patient, you’ll need to gather data not only about communication methods but where they are in the patient journey, their health issue, and their familiarity with the healthcare provider’s procedures and treatment options.
Understand the moments of truth
With a few exceptions, most people seek healthcare services when they are ill or have a healthcare issue. These situations can cause patients to feel stressed and anxious. It’s these moments of interaction where compassion, knowledge, and understanding can provide relief and reassurance.
When patients see their healthcare provider, they are looking for solutions to problems. It’s the provider’s opportunity to identify these moments of truth and capitalize on them.
Get the data you need
Healthcare providers can collect vast amounts of data from patients, but the data collected rarely goes far enough in analyzing and determining solutions.
Your patients have high expectations regarding personalized treatment based on data. They want personalized, easy access to medical information and records, responsive treatments and follow-up, and communication in their preferred format.
You need more than clinical data to give patients what they want. You also need personal data that sets each patient apart and ensures a tailored experience.
For example, it might be challenging for parents of small children to contact the clinic and schedule appointments at certain times of the day. As a healthcare provider, you’ll need to be aware of the best times to contact this individual and offer simple methods for scheduling appointments.
Another example is patients with physical disabilities. You can take steps to improve their access to and experience at the healthcare facility.
Encourage referrals and loyalty
Although engagement on social media and online forums is becoming more and more common, the best way for new patients to find you is through referrals. Referrals stem from satisfactory experiences and trust.
Should you be using a customer insights hub?
Do you want to discover previous research faster?
Do you share your research findings with others?
Do you analyze patient research?
Start for free today, add your research, and get to key insights faster
Editor’s picks
Last updated: 22 July 2023
Last updated: 11 September 2023
Last updated: 10 October 2023
Last updated: 16 November 2023
Last updated: 12 October 2023
Last updated: 25 November 2023
Last updated: 3 July 2023
Last updated: 27 January 2024
Last updated: 27 November 2023
Last updated: 17 January 2024
Latest articles
Related topics, .css-je19u9{-webkit-align-items:flex-end;-webkit-box-align:flex-end;-ms-flex-align:flex-end;align-items:flex-end;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-flex-direction:row;-ms-flex-direction:row;flex-direction:row;-webkit-box-flex-wrap:wrap;-webkit-flex-wrap:wrap;-ms-flex-wrap:wrap;flex-wrap:wrap;-webkit-box-pack:center;-ms-flex-pack:center;-webkit-justify-content:center;justify-content:center;row-gap:0;text-align:center;max-width:671px;}@media (max-width: 1079px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}}@media (max-width: 799px){.css-je19u9{max-width:400px;}.css-je19u9>span{white-space:pre;}} decide what to .css-1kiodld{max-height:56px;display:-webkit-box;display:-webkit-flex;display:-ms-flexbox;display:flex;-webkit-align-items:center;-webkit-box-align:center;-ms-flex-align:center;align-items:center;}@media (max-width: 1079px){.css-1kiodld{display:none;}} build next, decide what to build next.

Users report unexpectedly high data usage, especially during streaming sessions.

Users find it hard to navigate from the home page to relevant playlists in the app.

It would be great to have a sleep timer feature, especially for bedtime listening.

I need better filters to find the songs or artists I’m looking for.
Log in or sign up
Get started for free
Vitesse de lecture
Traduction de texte, texte source, résultats de traduction, traduction de documents, glisser-déposer.
Traduction de sites Web
Saisissez une URL
Traduction d'image
Enregistrées.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Process mapping the...
Process mapping the patient journey: an introduction
- Related content
- Peer review
- Timothy M Trebble , consultant gastroenterologist 1 ,
- Navjyot Hansi , CMT 2 1 ,
- Theresa Hydes , CMT 1 1 ,
- Melissa A Smith , specialist registrar 2 ,
- Marc Baker , senior faculty member 3
- 1 Department of Gastroenterology, Portsmouth Hospitals Trust, Portsmouth PO6 3LY
- 2 Department of Gastroenterology, Guy’s and St Thomas’ NHS Foundation Trust, London
- 3 Lean Enterprise Academy, Ross-on-Wye, Hertfordshire
- Correspondence to: T M Trebble tim.trebble{at}porthosp.nhs.uk
- Accepted 15 July 2010
Process mapping enables the reconfiguring of the patient journey from the patient’s perspective in order to improve quality of care and release resources. This paper provides a practical framework for using this versatile and simple technique in hospital.
Healthcare process mapping is a new and important form of clinical audit that examines how we manage the patient journey, using the patient’s perspective to identify problems and suggest improvements. 1 2 We outline the steps involved in mapping the patient’s journey, as we believe that a basic understanding of this versatile and simple technique, and when and how to use it, is valuable to clinicians who are developing clinical services.
What information does process mapping provide and what is it used for?
Process mapping allows us to “see” and understand the patient’s experience 3 by separating the management of a specific condition or treatment into a series of consecutive events or steps (activities, interventions, or staff interactions, for example). The sequence of these steps between two points (from admission to the accident and emergency department to discharge from the ward) can be viewed as a patient pathway or process of care. 4
Improving the patient pathway involves the coordination of multidisciplinary practice, aiming to maximise clinical efficacy and efficiency by eliminating ineffective and unnecessary care. 5 The data provided by process mapping can be used to redesign the patient pathway 4 6 to improve the quality or efficiency of clinical management and to alter the focus of care towards activities most valued by the patient.
Process mapping has shown clinical benefit across a variety of specialties, multidisciplinary teams, and healthcare systems. 7 8 9 The NHS Institute for Innovation and Improvement proposes a range of practical benefits using this approach (box 1). 6
Box 1 Benefits of process mapping 6
A starting point for an improvement project specific for your own place of work
Creating a culture of ownership, responsibility and accountability for your team
Illustrates a patient pathway or process, understanding it from a patient’s perspective
An aid to plan changes more effectively
Collecting ideas, often from staff who understand the system but who rarely contribute to change
An interactive event that engages staff
An end product (a process map) that is easy to understand and highly visual
Several management systems are available to support process mapping and pathway redesign. 10 11 A common technique, derived originally from the Japanese car maker Toyota, is known as lean thinking transformation. 3 12 This considers each step in a patient pathway in terms of the relative contribution towards the patient’s outcome, taken from the patient’s perspective: it improves the patient’s health, wellbeing, and experience (value adding) or it does not (non-value or “waste”) (box 2). 14 15 16
Box 2 The eight types of waste in health care 13
Defects —Drug prescription errors; incomplete surgical equipment
Overproduction —Inappropriate scheduling
Transportation —Distance between related departments
Waiting —By patients or staff
Inventory —Excess stores, that expire
Motion —Poor ergonomics
Overprocessing —A sledgehammer to crack a nut
Human potential —Not making the most of staff skills
Process mapping can be used to identify and characterise value and non-value steps in the patient pathway (also known as value stream mapping). Using lean thinking transformation to redesign the pathway aims to enhance the contribution of value steps and remove non-value steps. 17 In most processes, non-value steps account for nine times more effort than steps that add value. 18
Reviewing the patient journey is always beneficial, and therefore a process mapping exercise can be undertaken at any time. However, common indications include a need to improve patients’ satisfaction or quality or financial aspects of a particular clinical service.
How to organise a process mapping exercise
Process mapping requires a planned approach, as even apparently straightforward patient journeys can be complex, with many interdependent steps. 4 A process mapping exercise should be an enjoyable and creative experience for staff. In common with other audit techniques, it must avoid being confrontational or judgmental or used to “name, shame, and blame.” 8 19
Preparation and planning
A good first step is to form a team of four or five key staff, ideally including a member with previous experience of lean thinking transformation. The group should decide on a plan for the project and its scope; this can be visualised by using a flow diagram (fig 1 ⇓ ). Producing a rough initial draft of the patient journey can be useful for providing an overview of the exercise.
Fig 1 Steps involved in a process mapping exercise
- Download figure
- Open in new tab
- Download powerpoint
The medical literature or questionnaire studies of patients’ expectations and outcomes should be reviewed to identify value adding steps involved in the management of the clinical condition or intervention from the patient’s perspective. 1 3
Data collection
Data collection should include information on each step under routine clinical circumstances in the usual clinical environment. Information is needed on waiting episodes and bottlenecks (any step within the patient pathway that slows the overall rate of a patient’s progress, normally through reduced capacity or availability 20 ). Using estimates of minimum and maximum time for each step reduces the influence of day to day variations that may skew the data. Limiting the number of steps (to below 60) aids subsequent analysis.
The techniques used for data collection (table 1 ⇓ ) each have advantages and disadvantages; a combination of approaches can be applied, contributing different qualitative or quantitative information. The commonly used technique of walking the patient journey includes interviews with patients and staff and direct observation of the patient journey and clinical environment. It allows the investigator to “see” the patient journey at first hand. Involving junior (or student) doctors or nurses as interviewers may increase the openness of opinions from staff, and time needed for data collection can be reduced by allotting members of the team to investigate different stages in the patient’s journey.
Data collection in process mapping
- View inline
Mapping the information
The process map should comprehensively represent the patient journey. It is common practice to draw the map by hand onto paper (often several metres long), either directly or on repositionable notes (fig 2 ⇓ ).
Fig 2 Section of a current state map of the endoscopy patient journey
Information relating to the steps or representing movement of information (request forms, results, etc) can be added. It is useful to obtain any missing information at this stage, either from staff within the meeting or by revisiting the clinical environment.
Analysing the data and problem solving
The map can be analysed by using a series of simple questions (box 3). The additional information can be added to the process map for visual representation. This can be helped by producing a workflow diagram—a map of the clinical environment, including information on patient, staff, and information movement (fig 3 ⇓ ). 18
Box 3 How to analyse a process map 6
How many steps are involved?
How many staff-staff interactions (handoffs)?
What is the time for each step and between each step?
What is the total time between start and finish (lead time)?
When does a patient join a queue, and is it a regular occurrence?
How many non-value steps are there?
What do patients complain about?
What are the problems for staff?
Fig 3 Workflow diagram of current state endoscopy pathway
Redesigning the patient journey
Lean thinking transformation involves redesigning the patient journey. 21 22 This will eliminate, combine and simplify non-value steps, 23 limit the impact of rate limiting steps (such as bottlenecks), and emphasise the value adding steps, making the process more patient-centred. 6 It is often useful to trial the new pathway and review its effect on patient management and satisfaction before attempting more sustained implementation.
Worked example: How to undertake a process mapping exercise
South Coast NHS Trust, a large district general hospital, plans to improve patient access to local services by offering unsedated endoscopy in two peripheral units. A consultant gastroenterologist has been asked to lead a process mapping exercise of the current patient journey to develop a fast track, high quality patient pathway.
In the absence of local data, he reviews the published literature and identifies key factors to the patient experience that include levels of discomfort during the procedure, time to discuss the findings with the endoscopist, and time spent waiting. 24 25 26 27 He recruits a team: an experienced performance manager, a sister from the endoscopy department, and two junior doctors.
The team drafts a map of the current endoscopy journey, using repositionable notes on the wall. This allows team members to identify the start (admission to the unit) and completion (discharge) points and the locations thought to be involved in the patient journey.
They decide to use a “walk the journey” format, interviewing staff in their clinical environments and allowing direct observation of the patient’s management.
The junior doctors visit the endoscopy unit over two days, building up rapport with the staff to ensure that they feel comfortable with being observed and interviewed (on a semistructured but informal basis). On each day they start at the point of admission at the reception office and follow the patient journey to completion.
They observe the process from staff and patient’s perspectives, sitting in on the booking process and the endoscopy procedure. They identify the sequence of steps and assess each for its duration (minimum and maximum times) and the factors that influence this. For some of the steps, they use a digital watch and notepad to check and record times. They also note staff-patient and staff-staff interactions and their function, and the recording and movement of relevant information.
Details for each step are entered into a simple table (table 2 ⇓ ), with relevant notes and symbols for bottlenecks and patients’ waits.
Patient journey for non-sedated upper gastrointestinal endoscopy
When data collection is complete, the doctor organises a meeting with the team. The individual steps of the patient journey are mapped on a single long section of paper with coloured temporary markers (fig 2 ⇑ ); additional information is added in different colours. A workflow diagram is drawn to show the physical route of the patient journey (fig 3 ⇑ ).
The performance manager calculates that the total patient journey takes a minimum of 50 minutes to a maximum of 345 minutes. This variation mainly reflects waiting times before a number of bottleneck steps.
Only five steps (14 to 17 and 22, table 2 ⇑ ) are considered both to add value and needed on the day of the procedure (providing patient information and consent can be obtained before the patient attends the department). These represent from 13 to 47 minutes. At its least efficient, therefore, only 4% of the patient journey (13 of 345 minutes) is spent in activities that contribute directly towards the patient’s outcome.
The team redesigns the patient journey (fig 4 ⇓ ) to increase time spent on value adding aspects but reduce waiting times, bottlenecks, and travelling distances. For example, time for discussing the results of the procedure is increased but the location is moved from the end of the journey (a bottleneck) to shortly after the procedure in the anteroom, reducing the patient’s waiting time and staff’s travelling distances.
Fig 4 Workflow diagram of future state endoscopy pathway
Implementing changes and sustaining improvements
The endoscopy staff are consulted on the new patient pathway, which is then piloted. After successful review two months later, including a patient satisfaction questionnaire, the new patient pathway is formally adopted in the peripheral units.
Further reading
Practical applications.
NHS Institute for Innovation and Improvement ( https://www.institute.nhs.uk )—comprehensive online resource providing practical guidance on process mapping and service improvement
Lean Enterprise Academy ( http://www.leanuk.org )—independent body dedicated to lean thinking in industry and healthcare, through training and academic discussion; its publication, Making Hospitals Work 23 is a practical guide to lean transformation in the hospital environment
Manufacturing Institute ( http://www.manufacturinginstitute.co.uk )—undertakes courses on process mapping and lean thinking transformation within health care and industrial practice
Theoretical basis
Bircheno J. The new lean toolbox . 4th ed. Buckingham: PICSIE Books, 2008
Mould G, Bowers J, Ghattas M. The evolution of the pathway and its role in improving patient care. Qual Saf Health Care 2010 [online publication 29 April]
Layton A, Moss F, Morgan G. Mapping out the patient’s journey: experiences of developing pathways of care. Qual Health Care 1998; 7 (suppl):S30-6
Graban M. Lean hospitals, improving quality, patient safety and employee satisfaction . New York: Taylor & Francis, 2009
Womack JP, Jones DT. Lean thinking . 2nd ed. London: Simon & Schuster, 2003
Cite this as: BMJ 2010;341:c4078
Contributors: TMT designed the protocol and drafted the manuscript; TMT, MB, JH, and TH collected and analysed the data; all authors critically reviewed and contributed towards revision and production of the manuscript. TMT is guarantor.
Competing interests: MB is a senior faculty member carrying out research for the Lean Enterprise Academy and undertakes paid consultancies both individually and from Lean Enterprise Academy, and training fees for providing lean thinking in healthcare.
Provenance and peer review: Not commissioned; externally peer reviewed.
- ↵ Kollberg B, Dahlgaard JJ, Brehmer P. Measuring lean initiatives in health care services: issues and findings. Int J Productivity Perform Manage 2007 ; 56 : 7 -24. OpenUrl CrossRef
- ↵ Bevan H, Lendon R. Improving performance by improving processes and systems. In: Walburg J, Bevan H, Wilderspin J, Lemmens K, eds. Performance management in health care. Abingdon: Routeledge, 2006:75-85.
- ↵ Kim CS, Spahlinger DA, Kin JM, Billi JE. Lean health care: what can hospitals learn from a world-class automaker? J Hosp Med 2006 ; 1 : 191 -9. OpenUrl CrossRef PubMed
- ↵ Layton A, Moss F, Morgan G. Mapping out the patient’s journey: experiences of developing pathways of care. Qual Health Care 1998 ; 7 (suppl): S30 -6. OpenUrl
- ↵ Peterson KM, Kane DP. Beyond disease management: population-based health management. Disease management. Chicago: American Hospital Publishing, 1996.
- ↵ NHS Modernisation Agency. Process mapping, analysis and redesign. London: Department of Health, 2005;1-40.
- ↵ Taylor AJ, Randall C. Process mapping: enhancing the implementation of the Liverpool care pathway. Int J Palliat Nurs 2007 ; 13 : 163 -7. OpenUrl PubMed
- ↵ Ben-Tovim DI, Dougherty ML, O’Connell TJ, McGrath KM. Patient journeys: the process of clinical redesign. Med J Aust 2008 ; 188 (suppl 6): S14 -7. OpenUrl PubMed Web of Science
- ↵ King DL, Ben-Tovim DI, Bassham J. Redesigning emergency department patient flows: application of lean thinking to health care. Emerg Med Australas 2006 ; 18 : 391 -7. OpenUrl CrossRef PubMed
- ↵ Mould G, Bowers J, Ghattas M. The evolution of the pathway and its role in improving patient care. Qual Saf Health Care 2010 ; published online 29 April.
- ↵ Rath F. Tools for developing a quality management program: proactive tools (process mapping, value stream mapping, fault tree analysis, and failure mode and effects analysis). Int J Radiat Oncol Biol Phys 2008 ; 71 (suppl): S187 -90. OpenUrl PubMed Web of Science
- ↵ Womack JP, Jones DT. Lean thinking. 2nd ed. London: Simon & Schuster, 2003.
- ↵ Graban M. Value and waste. In: Lean hospitals. New York: Taylor & Francis, 2009;35-56.
- ↵ Westwood N, James-Moore M, Cooke M. Going lean in the NHS. London: NHS Institute for Innovation and Improvement, 2007.
- ↵ Liker JK. The heart of the Toyota production system: eliminating waste. The Toyota way. New York: McGraw-Hill, 2004;27-34.
- ↵ Womack JP, Jones DT. Introduction: Lean thinking versus Muda. In: Lean thinking. 2nd ed. London: Simon & Schuster, 2003:15-28.
- ↵ George ML, Rowlands D, Price M, Maxey J. Value stream mapping and process flow tools. Lean six sigma pocket toolbook. New York: McGraw Hill, 2005:33-54.
- ↵ Fillingham D. Can lean save lives. Leadership Health Serv 2007 ; 20 : 231 -41. OpenUrl CrossRef
- ↵ Benjamin A. Audit: how to do it in practice. BMJ 2008 ; 336 : 1241 -5. OpenUrl FREE Full Text
- ↵ Vissers J. Unit Logistics. In: Vissers J, Beech R, eds. Health operations management patient flow logistics in health care. Oxford: Routledge, 2005:51-69.
- ↵ Graban M. Overview of lean for hospital. Lean hospitals. New York: Taylor & Francis, 2009;19-33.
- ↵ Eaton M. The key lean concepts. Lean for practitioners. Penryn, Cornwall: Academy Press, 2008:13-28.
- ↵ Baker M, Taylor I, Mitchell A. Analysing the situation: learning to think differently. In: Making hospitals work. Ross-on-Wye: Lean Enterprise Academy, 2009:51-70.
- ↵ Ko HH, Zhang H, Telford JJ, Enns R. Factors influencing patient satisfaction when undergoing endoscopic procedures. Gastrointest Endosc 2009 ; 69 : 883 -91. OpenUrl CrossRef PubMed Web of Science
- ↵ Del Rio AS, Baudet JS, Fernandez OA, Morales I, Socas MR. Evaluation of patient satisfaction in gastrointestinal endoscopy. Eur J Gastroenterol Hepatol 2007 ; 19 : 896 -900. OpenUrl CrossRef PubMed Web of Science
- ↵ Seip B, Huppertz-Hauss G, Sauar J, Bretthauer M, Hoff G. Patients’ satisfaction: an important factor in quality control of gastroscopies. Scand J Gastroenterol 2008 ; 43 : 1004 -11. OpenUrl CrossRef PubMed Web of Science
- ↵ Yanai H, Schushan-Eisen I, Neuman S, Novis B. Patient satisfaction with endoscopy measurement and assessment. Dig Dis 2008 ; 26 : 75 -9. OpenUrl CrossRef PubMed Web of Science
- Search Menu
- Advance Articles
- Editor's Choice
- Supplements
- Patient Perspectives
- Methods Corner
- Science for Patients
- Invited Commentaries
- ESC Content Collections
- Author Guidelines
- Instructions for reviewers
- Submission Site
- Why publish with EJCN?
- Open Access Options
- Self-Archiving Policy
- Read & Publish
- About European Journal of Cardiovascular Nursing
- About ACNAP
- About European Society of Cardiology
- ESC Publications
- Editorial Board
- Advertising & Corporate Services
- War in Ukraine
- Journals on Oxford Academic
- Books on Oxford Academic
Article Contents
Introduction, why patient journey mapping, how is patient journey mapping conducted, use of technology in patient journey mapping, future implications for patient journey mapping, conclusions, patient journey mapping: emerging methods for understanding and improving patient experiences of health systems and services.
Lemma N Bulto and Ellen Davies Shared first authorship.
Conflict of interest: none declared.
- Article contents
- Figures & tables
- Supplementary Data
Lemma N Bulto, Ellen Davies, Janet Kelly, Jeroen M Hendriks, Patient journey mapping: emerging methods for understanding and improving patient experiences of health systems and services, European Journal of Cardiovascular Nursing , 2024;, zvae012, https://doi.org/10.1093/eurjcn/zvae012
- Permissions Icon Permissions
Patient journey mapping is an emerging field of research that uses various methods to map and report evidence relating to patient experiences and interactions with healthcare providers, services, and systems. This research often involves the development of visual, narrative, and descriptive maps or tables, which describe patient journeys and transitions into, through, and out of health services. This methods corner paper presents an overview of how patient journey mapping has been conducted within the health sector, providing cardiovascular examples. It introduces six key steps for conducting patient journey mapping and describes the opportunities and benefits of using patient journey mapping and future implications of using this approach.
Acquire an understanding of patient journey mapping and the methods and steps employed.
Examine practical and clinical examples in which patient journey mapping has been adopted in cardiac care to explore the perspectives and experiences of patients, family members, and healthcare professionals.
Quality and safety guidelines in healthcare services are increasingly encouraging and mandating engagement of patients, clients, and consumers in partnerships. 1 The aim of many of these partnerships is to consider how health services can be improved, in relation to accessibility, service delivery, discharge, and referral. 2 , 3 Patient journey mapping is a research approach increasingly being adopted to explore these experiences in healthcare. 3
a patient-oriented project that has been undertaken to better understand barriers, facilitators, experiences, interactions with services and/or outcomes for individuals and/or their carers, and family members as they enter, navigate, experience and exit one or more services in a health system by documenting elements of the journey to produce a visual or descriptive map. 3
It is an emerging field with a clear patient-centred focus, as opposed to studies that track patient flow, demand, and movement. As a general principle, patient journey mapping projects will provide evidence of patient perspectives and highlight experiences through the patient and consumer lens.
Patient journey mapping can provide significant insights that enable responsive and context-specific strategies for improving patient healthcare experiences and outcomes to be designed and implemented. 3–6 These improvements can occur at the individual patient, model of care, and/or health system level. As with other emerging methodologies, questions have been raised regarding exactly how patient journey mapping projects can best be designed, conducted, and reported. 3
In this methods paper, we provide an overview of patient journey mapping as an emergent field of research, including reasons that mapping patient journeys might be considered, methods that can be adopted, the principles that can guide patient journey mapping data collection and analysis, and considerations for reporting findings and recognizing the implications of findings. We summarize and draw on five cardiovascular patient journey mapping projects, as examples.
One of the most appealing elements of the patient journey mapping field of research is its focus on illuminating the lived experiences of patients and/or their family members, and the health professionals caring for them, methodically and purposefully. Patient journey mapping has an ability to provide detailed information about patient experiences, gaps in health services, and barriers and facilitators for access to health services. This information can be used independently, or alongside information from larger data sets, to adapt and improve models of care relevant to the population that is being investigated. 3
To date, the most frequent reason for adopting this approach is to inform health service redesign and improvement. 3 , 7 , 8 Other reasons have included: (i) to develop a deeper understanding of a person’s entire journey through health systems; 3 (ii) to identify delays in diagnosis or treatment (often described as bottlenecks); 9 (iii) to identify gaps in care and unmet needs; (iv) to evaluate continuity of care across health services and regions; 10 (v) to understand and evaluate the comprehensiveness of care; 11 (vi) to understand how people are navigating health systems and services; and (vii) to compare patient experiences with practice guidelines and standards of care.
Patient journey mapping approaches frequently use six broad steps that help facilitate the preparation and execution of research projects. These are outlined in the Central illustration . We acknowledge that not all patient journey mapping approaches will follow the order outlined in the Central illustration , but all steps need to be considered at some point throughout each project to ensure that research is undertaken rigorously, appropriately, and in alignment with best practice research principles.

Steps for conducing patient journey mapping.
Five cardiovascular patient journey mapping research examples have been included in Figure 1 , 12–16 to provide specific context and illustrate these six steps. For each of these examples, the problem or gap in practice or research, consultation processes, research question or aim, type of mapping, methods, and reporting of findings have been extracted. Each of these steps is then discussed, using these cardiovascular examples.

Examples of patient journey mapping projects.
Define the problem or gap in practice or research
Developing an understanding of a problem or gap in practice is essential for facilitating the design and development of quality research projects. In the examples outlined in Figure 1 , it is evident that clinical variation or system gaps have been explored using patient journey mapping. In the first two examples, populations known to have health vulnerabilities were explored—in Example 1, this related to comorbid substance use and physical illness, 13 and in Example 2, this related to geographical location. 13 Broader systems and societal gaps were explored in Examples 4 and 5, respectively, 15 , 16 and in Example 3, a new technologically driven solution for an existing model of care was tested for its ability to improve patient outcomes relating to hypertension. 14
Consultation, engagement, and partnership
Ideally, consultation with heathcare providers and/or patients would occur when the problem or gap in practice or research is being defined. This is a key principle of co-designed research. 17 Numerous existing frameworks for supporting patient involvement in research have been designed and were recently documented and explored in a systematic review by Greenhalgh et al . 18 While none of the five example studies included this step in the initial phase of the project, it is increasingly being undertaken in patient partnership projects internationally (e.g. in renal care). 17 If not in the project conceptualization phase, consultation may occur during the data collection or analysis phase, as demonstrated in Example 3, where a care pathway was co-created with participants. 14 We refer readers to Greenhalgh’s systematic review as a starting point for considering suitable frameworks for engaging participants in consultation, partnership, and co-design of patient journey mapping projects. 18
Design the research question/project aim
Conducting patient journey mapping research requires a thoughtful and systematic approach to adequately capture the complexity of the healthcare experience. First, the research objectives and questions should be clearly defined. Aspects of the patient journey that will be explored need to be identified. Then, a robust approach must be developed, taking into account whether qualitative, quantitative, or mixed methods are more appropriate for the objectives of the study.
For example, in the cardiac examples in Figure 1 , the broad aims included mapping existing pathways through health services where there were known problems 12 , 13 , 15 , 16 and documenting the co-creation of a new care pathway using quantitative, qualitative, or mixed methods. 14
In traditional studies, questions that might be addressed in the area of patient movement in health systems include data collected through the health systems databases, such as ‘What is the length of stay for x population’, or ‘What is the door to balloon time in this hospital?’ In contrast, patient mapping journey studies will approach asking questions about experiences that require data from patients and their family members, e.g. ‘What is the impact on you of your length of stay?’, ‘What was your experience in being assessed and undergoing treatment for your chest pain?’, ‘What was your experience supporting this patient during their cardiac admission and discharge?’
Select appropriate type of mapping
The methods chosen for mapping need to align with the identified purpose for mapping and the aim or question that was designed in Step 3. A range of research methods have been used in patient journey mapping projects involving various qualitative, quantitative, and mixed methods techniques and tools. 4 Some approaches use traditional forms of data collection, such as short-form and long-form patient interviews, focus groups, and direct patient observations. 18 , 19 Other approaches use patient journey mapping tools, designed and used with specific cultural groups, such as First Nations peoples using artwork, paintings, sand trays, and photovoice. 17 , 20 In the cardiovascular examples presented in Figure 1 , both qualitative and quantitative methods have been used, with interviews, patient record reviews, and observational techniques adopted to map patient journeys.
In a recent scoping review investigating patient journey mapping across all health care settings and specialities, six types of patient journey mapping were identified. 3 These included (i) mapping key experiences throughout a period of illness; (ii) mapping by location of health service; (iii) mapping by events that occurred throughout a period of illness; (iv) mapping roles, input, and experiences of key stakeholders throughout patient journeys; (v) mapping a journey from multiple perspectives; and (vi) mapping a timeline of events. 3 Combinations or variations of these may be used in cardiovascular settings in the future, depending on the research question, and the reasons mapping is being undertaken.
Recruit, collect data, and analyse data
The majority of health-focused patient journey mapping projects published to date have recruited <50 participants. 3 Projects with fewer participants tend to be qualitative in nature. In the cardiovascular examples provided in Figure 1 , participant numbers range from 7 14 to 260. 15 The 3 studies with <20 participants were qualitative, 12 , 14 , 16 and the 2 with 95 and 260 participants, respectively, were quantitative. 13 , 15 As seen in these and wider patient journey mapping examples, 3 participants may include patients, relatives, carers, healthcare professionals, or other stakeholders, as required, to meet the study objectives. These different participant perspectives may be analysed within each participant group and/or across the wider cohort to provide insights into experiences, and the contextual factors that shape these experiences.
The approach chosen for data collection and analysis will vary and depends on the research question. What differentiates data analysis in patient journey mapping studies from other qualitative or quantitative studies is the focus on describing, defining, or exploring the journey from a patient’s, rather than a health service, perspective. Dimensions that may, therefore, be highlighted in the analysis include timing of service access, duration of delays to service access, physical location of services relative to a patient’s home, comparison of care received vs. benchmarked care, placing focus on the patient perspective.
The mapping of individual patient journeys may take place during data collection with the use of mapping templates (tables, diagrams, and figures) and/or later in the analysis phase with the use of inductive or deductive analysis, mapping tables, or frameworks. These have been characterized and visually represented in a recent scoping review. 3 Representations of patient journeys can also be constructed through a secondary analysis of previously collected data. In these instances, qualitative data (i.e. interviews and focus group transcripts) have been re-analysed to understand whether a patient journey narrative can be extracted and reported. Undertaking these projects triggers a new research cycle involving the six steps outlined in the Central illustration . The difference in these instances is that the data are already collected for Step 5.
Report findings, disseminate findings, and take action on findings
A standardized, formal reporting guideline for patient journey mapping research does not currently exist. As argued in Davies et al ., 3 a dedicated reporting guide for patient journey mapping would be ill-advised, given the diversity of approaches and methods that have been adopted in this field. Our recommendation is for projects to be reported in accordance with formal guidelines that best align with the research methods that have been adopted. For example, COREQ may be used for patient journey mapping where qualitative methods have been used. 20 STROBE may be used for patient journey mapping where quantitative methods have been used. 21 Whichever methods have been adopted, reporting of projects should be transparent, rigorous, and contain enough detail to the extent that the principles of transparency, trustworthiness, and reproducibility are upheld. 3
Dissemination of research findings needs to include the research, healthcare, and broader communities. Dissemination methods may include academic publications, conference presentations, and communication with relevant stakeholders including healthcare professionals, policymakers, and patient advocacy groups. Based on the findings and identified insights, stakeholders can collaboratively design and implement interventions, programmes, or improvements in healthcare delivery that overcome the identified challenges directly and address and improve the overall patient experience. This cyclical process can hopefully produce research that not only informs but also leads to tangible improvements in healthcare practice and policy.
Patient journey mapping is typically a hands-on process, relying on surveys, interviews, and observational research. The technology that supports this research has, to date, included word processing software, and data analysis packages, such as NVivo, SPSS, and Stata. With the advent of more sophisticated technological tools, such as electronic health records, data analytics programmes, and patient tracking systems, healthcare providers and researchers can potentially use this technology to complement and enhance patient journey mapping research. 19 , 20 , 22 There are existing examples where technology has been harnessed in patient journey. Lee et al . used patient journey mapping to verify disease treatment data from the perspective of the patient, and then the authors developed a mobile prototype that organizes and visualizes personal health information according to the patient-centred journey map. They used a visualization approach for analysing medical information in personal health management and examined the medical information representation of seven mobile health apps that were used by patients and individuals. The apps provide easy access to patient health information; they primarily import data from the hospital database, without the need for patients to create their own medical records and information. 23
In another example, Wauben et al. 19 used radio frequency identification technology (a wireless system that is able to track a patient journey), as a component of their patient journey mapping project, to track surgical day care patients to increase patient flow, reduce wait times, and improve patient and staff satisfaction.
Patient journey mapping has emerged as a valuable research methodology in healthcare, providing a comprehensive and patient-centric approach to understanding the entire spectrum of a patient’s experience within the healthcare system. Future implications of this methodology are promising, particularly for transforming and redesigning healthcare delivery and improving patient outcomes. The impact may be most profound in the following key areas:
Personalized, patient-centred care : The methodology allows healthcare providers to gain deep insights into individual patient experiences. This information can be leveraged to deliver personalized, patient-centric care, based on the needs, values, and preferences of each patient, and aligned with guideline recommendations, healthcare professionals can tailor interventions and treatment plans to optimize patient and clinical outcomes.
Enhanced communication, collaboration, and co-design : Mapping patient interactions with health professionals and journeys within and across health services enables specific gaps in communication and collaboration to be highlighted and potentially informs responsive strategies for improvement. Ideally, these strategies would be co-designed with patients and health professionals, leading to improved care co-ordination and healthcare experience and outcomes.
Patient engagement and empowerment : When patients are invited to share their health journey experiences, and see visual or written representations of their journeys, they may come to understand their own health situation more deeply. Potentially, this may lead to increased health literacy, renewed adherence to treatment plans, and/or self-management of chronic conditions such as cardiovascular disease. Given these benefits, we recommend that patients be provided with the findings of research and quality improvement projects with which they are involved, to close the loop, and to ensure that the findings are appropriately disseminated.
Patient journey mapping is an emerging field of research. Methods used in patient journey mapping projects have varied quite significantly; however, there are common research processes that can be followed to produce high-quality, insightful, and valuable research outputs. Insights gained from patient journey mapping can facilitate the identification of areas for enhancement within healthcare systems and inform the design of patient-centric solutions that prioritize the quality of care and patient outcomes, and patient satisfaction. Using patient journey mapping research can enable healthcare providers to forge stronger patient–provider relationships and co-design improved health service quality, patient experiences, and outcomes.
None declared.
Farmer J , Bigby C , Davis H , Carlisle K , Kenny A , Huysmans R , et al. The state of health services partnering with consumers: evidence from an online survey of Australian health services . BMC Health Serv Res 2018 ; 18 : 628 .
Google Scholar
Kelly J , Dwyer J , Mackean T , O’Donnell K , Willis E . Coproducing Aboriginal patient journey mapping tools for improved quality and coordination of care . Aust J Prim Health 2017 ; 23 : 536 – 542 .
Davies EL , Bulto LN , Walsh A , Pollock D , Langton VM , Laing RE , et al. Reporting and conducting patient journey mapping research in healthcare: a scoping review . J Adv Nurs 2023 ; 79 : 83 – 100 .
Ly S , Runacres F , Poon P . Journey mapping as a novel approach to healthcare: a qualitative mixed methods study in palliative care . BMC Health Serv Res 2021 ; 21 : 915 .
Arias M , Rojas E , Aguirre S , Cornejo F , Munoz-Gama J , Sepúlveda M , et al. Mapping the patient’s journey in healthcare through process mining . Int J Environ Res Public Health 2020 ; 17 : 6586 .
Natale V , Pruette C , Gerohristodoulos K , Scheimann A , Allen L , Kim JM , et al. Journey mapping to improve patient-family experience and teamwork: applying a systems thinking tool to a pediatric ambulatory clinic . Qual Manag Health Care 2023 ; 32 : 61 – 64 .
Cherif E , Martin-Verdier E , Rochette C . Investigating the healthcare pathway through patients’ experience and profiles: implications for breast cancer healthcare providers . BMC Health Serv Res 2020 ; 20 : 735 .
Gilburt H , Drummond C , Sinclair J . Navigating the alcohol treatment pathway: a qualitative study from the service users’ perspective . Alcohol Alcohol 2015 ; 50 : 444 – 450 .
Gichuhi S , Kabiru J , M’Bongo Zindamoyen A , Rono H , Ollando E , Wachira J , et al. Delay along the care-seeking journey of patients with ocular surface squamous neoplasia in Kenya . BMC Health Serv Res 2017 ; 17 : 485 .
Borycki EM , Kushniruk AW , Wagner E , Kletke R . Patient journey mapping: integrating digital technologies into the journey . Knowl Manag E-Learn 2020 ; 12 : 521 – 535 .
Barton E , Freeman T , Baum F , Javanparast S , Lawless A . The feasibility and potential use of case-tracked client journeys in primary healthcare: a pilot study . BMJ Open 2019 ; 9 : e024419 .
Bearnot B , Mitton JA . “You’re always jumping through hoops”: journey mapping the care experiences of individuals with opioid use disorder-associated endocarditis . J Addict Med 2020 ; 14 : 494 – 501 .
Cunnington MS , Plummer CJ , McDiarmid AK , McComb JM . The patient journey from symptom onset to pacemaker implantation . QJM 2008 ; 101 : 955 – 960 .
Geerse C , van Slobbe C , van Triet E , Simonse L . Design of a care pathway for preventive blood pressure monitoring: qualitative study . JMIR Cardio 2019 ; 3 : e13048 .
Laveau F , Hammoudi N , Berthelot E , Belmin J , Assayag P , Cohen A , et al. Patient journey in decompensated heart failure: an analysis in departments of cardiology and geriatrics in the Greater Paris University Hospitals . Arch Cardiovasc Dis 2017 ; 110 : 42 – 50 .
Naheed A , Haldane V , Jafar TH , Chakma N , Legido-Quigley H . Patient pathways and perceptions of treatment, management, and control Bangladesh: a qualitative study . Patient Prefer Adherence 2018 ; 12 : 1437 – 1449 .
Bateman S , Arnold-Chamney M , Jesudason S , Lester R , McDonald S , O’Donnell K , et al. Real ways of working together: co-creating meaningful Aboriginal community consultations to advance kidney care . Aust N Z J Public Health 2022 ; 46 : 614 – 621 .
Greenhalgh T , Hinton L , Finlay T , Macfarlane A , Fahy N , Clyde B , et al. Frameworks for supporting patient and public involvement in research: systematic review and co-design pilot . Health Expect 2019 ; 22 : 785 – 801 .
Wauben LSGL , Guédon ACP , de Korne DF , van den Dobbelsteen JJ . Tracking surgical day care patients using RFID technology . BMJ Innov 2015 ; 1 : 59 – 66 .
Tong A , Sainsbury P , Craig J . Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups . Int J Qual Health Care 2007 ; 19 : 349 – 357 .
von Elm E , Altman DG , Egger M , Pocock SJ , Gøtzsche PC , Vandenbroucke JP , et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies . Lancet 2007 ; 370 (9596): 1453 – 1457 .
Wilson A , Mackean T , Withall L , Willis EM , Pearson O , Hayes C , et al. Protocols for an Aboriginal-led, multi-methods study of the role of Aboriginal and Torres Strait Islander health workers, practitioners and Liaison officers in quality acute health care . J Aust Indigenous HealthInfoNet 2022 ; 3 : 1 – 15 .
Lee B , Lee J , Cho Y , Shin Y , Oh C , Park H , et al. Visualisation of information using patient journey maps for a mobile health application . Appl Sci 2023 ; 13 : 6067 .
Author notes
- cardiovascular system
- health personnel
- health services
- health care systems
- narrative discourse
Email alerts
Related articles in pubmed, citing articles via.
- Recommend to Your Librarian
- Advertising and Corporate Services
- Journals Career Network
Affiliations
- Online ISSN 1873-1953
- Print ISSN 1474-5151
- Copyright © 2024 European Society of Cardiology
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

The 1-2-3 Guide to Patient Journey Mapping [Template Inside]
by Gaine Solutions | Feb 28, 2024 | Healthcare , Life Sciences , Master Data Management

Patient journeys in today’s healthcare landscape are complex, spanning a number of platforms, systems, touchpoints, and interactions. As patients engage with healthcare providers through diverse channels, both digital and physical, the need for a structured and comprehensive approach to managing the patient journeys is evident. Patient journey mapping is the solution.
Patient journey mapping creates a high-level and holistic view of the patient journey that empowers healthcare providers to make the most informed and impactful decisions possible about how to enhance operations and care.
In this guide, we’ll walk step-by-step through the process of creating and implementing a patient journey map that drives better performance results and patient outcomes for your healthcare organization.
Key Takeaways:
- Patient journey mapping is crucial for understanding and enhancing the patient experience.
- Patient journey mapping leads to improved patient satisfaction, better clinical outcomes, and increased operational efficiency.
- Developing a patient journey map requires clear objectives, a cross-functional team, and data-driven approaches to gaining insight.
- Improvement strategies should be developed for each critical moment and touchpoint, with changes implemented and continuously monitored for effectiveness over time.
What is Patient Journey Mapping and Why Is It Important?
Patient journey mapping is the process of creating a detailed visualization of a patient’s healthcare journey, from initial contact through treatment and follow-up care, identifying every touchpoint along the way. This methodical approach helps healthcare providers see the care process from the patient perspective, including the highs, lows, and gaps in the patient experience.
The example below is from the U.S. Department of Veteran Affairs, and shows how intricate and complex the patient journey is once it’s mapped completely. This drives home the importance of documenting the journey visually in order to see it in a holistic way.
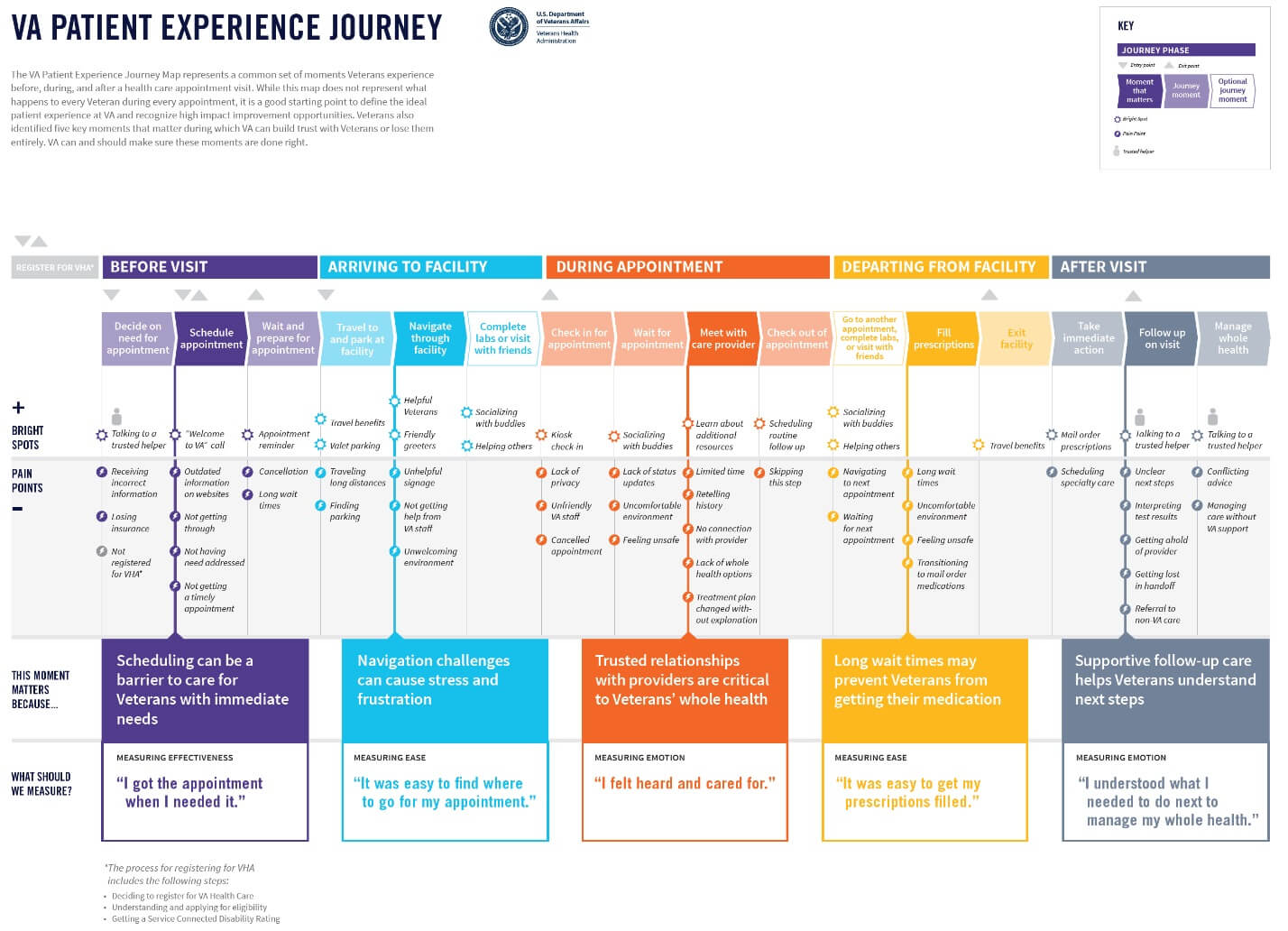
Image Source
When done effectively, patient journey mapping is a valuable tool driving more seamless, integrated, and patient-centered care. Journey mapping also helps healthcare organizations make informed decisions about where to allocate resources, how to streamline operations, and ways to personalize care to meet the unique needs of each patient.
In the end, the benefits of patient journey mapping are threefold:
- Improved Patient Satisfaction : Enhances the overall patient experience by addressing specific needs and preferences, leading to higher satisfaction rates.
- Better Clinical Outcomes : Identifies opportunities for early intervention and personalized care plans, contributing to improved health results.
- Increased Operational Efficiency : Streamlines healthcare processes by pinpointing inefficiencies and redundancies, leading to more effective use of resources.
It leads to 360-degree improvements that enhance clinical, administrative, and operational aspects of both the healthcare system and the patient experience. In the next section, we’ll walk through the steps you can take to develop a patient journey map for your organization.
Your Step-by-Step Patient Journey Mapping Template
1. identify the goals and scope of your map.
Begin by d eve loping a clear vision of what you aim to achieve through patient journey mapping. Whether it’s to enhance patient satisfaction, streamline healthcare delivery, or identify gaps in service, setting specific objectives will direct your mapping efforts. During this step, you should also determine the scope of your map (i.e. whether it focuses on a particular service line or the entire healthcare experience).
2. Gather a Cross-Functional Team
Assemble a team that represents a broad spectrum of roles within your organization, including clinicians, administrative staff, IT professionals, and cust ome r service representatives. Diverse perspectives ensure a holistic view of the patient journey, capturing insights from every facet of patient interaction.
3. Map the Patient Touchpoints
Systematically list every interaction point between the patient and your healthcare system. This includes digital touchpoints like website visits, appointment scheduling portals, and social media interactions, as well as physical touchpoints like clinic visits, phone calls, and direct mail communication. Mapping these touchpoints requires a detailed understanding of the patient’s path through your system, from initial awareness through treatment and follow-up care.
4. Collect and Analyze Data
Leverage diverse data sources to understand patient experiences at each touchpoint. Collect patient feedback through cha nne ls like surveys, interviews, and comment cards. Analyze staff insights and review operational data. Look for patterns in behavior and satisfaction levels, and identify bottlenecks or pain points in the patient journey.
Having a centralized data management platform in place is crucial for this step—it provides a central repository for the data you collect as part of your patient journey mapping exercise, while also giving you seamless access to historical data in one location.
5. Visualize the Journey
Develop a visual representation of the patient journey. Use flowcharts, storyboards, or diagrams to depict the sequence of touchpoints and the patient’s experience at each stage. This visualization should be from the patient’s perspective, highlighting critical interactions, emotions, and decision points.
Tools like customer journey mapping software can facilitate this process, but even simple graphical tools or whiteboards can be effective.
6. Identify Moments of Truth
Highlight key moments in the journey that significantly impact the patient’s perception of care—things like first contact, diagnosis communication, wait times, and billing support. These are opportunities to make a lasting impression on the patient, and identifying them allows your team to prioritize areas for immediate improvement or innovation.
7. Develop Improvement Strategies
For each critical moment and touchpoint, evaluate what’s working effectively as well as areas for potential improvements. Call out specific gaps and pain points that may exist for the patient at every stage on your journey map. Then, brainstorm how to resolve them.
This may happen by introducing new technologies, optimizing existing processes, providing additional training for your staff, enhancing communication strategies, and more.
8. Implement Changes
Prioritize the identified improvements based on their potential impact and feasibility. Create a detailed implementation plan, assigning clear responsibilities and deadlines. Ensure there is a mechanism for tracking progress and measuring the impact of these changes on the patient experience and other goals and objectives you set at the start of the process.
9. Monitor and Adjust
Establish a continuous feedback loop to monitor the effectiveness of implemented changes. Use patient feedback, staff input, and performance metrics to assess progress. Be prepared to make iterative adjustments to your strategies based on this feedback, fostering a culture of continuous improvement.
Putting it All Together
Embarking on patient journey mapping is more than a strategic exercise—it’s a commitment to elevating the standard of care through a deep understanding of the patient’s experience. It represents a pivotal shift toward a more empathetic, patient-centric approach in healthcare, where decisions are informed by the nuanced needs and experiences of those we serve.
Gaine’s Coperor platform is a scalable, ecosystem-wide master data management solution designed for the unique challenges of the healthcare and life sciences industries. It creates a single source of data truth within an organization that makes initiatives like journey mapping possible. Learn more here or start your real-time Coperer demo today.
Opt-in with Gaine for More Insight
Great welcome to the mdm a-team you may unsubscribe at any time., more articles like this.
- Case Studies
- Contracting
- Credentialing
- Data Governance
- Data Quality
- Data Science
- Health Plans
- Interoperability
- Life Sciences
- Master Data Management
- Network Adequacy
- Network Management
- Next-Gen MDM
- Provider Data Management
- Provider Groups
- Provider Network
- Provider Network Management
- Uncategorized
- Whitepapers

7 Data-Driven Strategies to Improve Star Ratings

Closing HEDIS Care Gaps through Effective Data Management

CMS Prior Authorization Final Rule: A Guide For Payers and Providers
The Patient Journey
- Open Access
- First Online: 15 December 2020
Cite this chapter
You have full access to this open access chapter

- Elena Beleffi 5 ,
- Paola Mosconi 6 &
- Susan Sheridan 7
41k Accesses
2 Citations
The wide implementation of patient safety improvement efforts continues to face many barriers including insufficient involvement of all stakeholders in healthcare, lack of individual and organizational learning when medical errors occur and scarce investments in patient safety. The promotion of systems-based approaches offers methods and tools to improve the safety of care. A multidisciplinary perspective must include the involvement of patients and citizens as fundamental contributors to the design, implementation, and delivery of health services.
The patient journey is a challenging example of using a systems approach. The inclusion of the patient’s viewpoint and experience about their health journey throughout the time of care and across all the care settings represents a key factor in improving patient safety. Patient engagement ensures that the design of healthcare services are aligned with the values, the preferences, and needs of the patient community and integrates the real-life experience and the skills of the people to enhance patient safety in the patient journey.
The utmost priority to implement patient engagement is the training of patients. Therefore, training for both patients/families/advocates and health professionals is the foundation on which to build active engagement of patients and consequently an effective and efficient patient journey.
The chapter offers examples of successful training courses designed to foster strategic alliances among healthcare professionals and researchers with patients and their organizations. Training of patients constitutes the first step to develop shared knowledge, co-produced projects, and the achievement of active multilevel participation of patients for the implementation of patient safety in the patient journey.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others

Patient Experiences of Safety in Care Transitions
Top 10 interventions in paediatric patient safety.

‘The big buzz’: a qualitative study of how safe care is perceived, understood and improved in general practice
- Patient journey
- Patient engagement
- Patient empowerment
- Patient safety
- Healthcare ergonomics
- Co-production
- Knowledge creation
1 Introduction
Almost 20 years after publication “To Err is Human: Building a Better Health System” (Kohn et al. 1999), patient safety is still not widely implemented. This report from the Institute of Medicine is the milestone that constituted a turning point for improving quality of care and patient safety identifying the need to rethink healthcare delivery to provide safe, effective, and efficient care.
The barriers of implementing patient safety as a driving force for change towards more effective healthcare include multiple factors: insufficient involvement of all stakeholders contributing to the care process, lack of willingness of organizations and individuals to learn from errors and scarce investments in patient safety improvement and research.
There is a growing need to promote systems approaches to finding solutions in healthcare to improve the safety of care, the quality of healthcare delivery, patients’ health and citizens’ well-being.
The discussion paper “Bringing a Systems Approach to Health” defines the systems approach as one “that applies scientific insights to understand the elements that influence health outcomes; models the relationships between those elements; and alters design, processes, or policies based on the resultant knowledge in order to produce better health at lower cost” [ 1 ].
A multidisciplinary approach must include the involvement of citizens and patients as fundamental contributors to the design, implementation, delivery, and evaluation of health services.
This means that citizen participation plays an essential role, bringing the unique point of view of patients and family members into the debate on patient safety and quality of care.
Patients and more generally citizens, when actively and systematically engaged, bring ideas and experiences which can support a collaborative and reciprocal learning process among the healthcare stakeholders. This produces knowledge that leads to improved practices, a real knowledge creation process where the dynamic participation of all actors in healthcare systems contribute to an active learning environment where the identification, the investigation, and the planning of solutions related to health incidents is a cyclic process enabling healthcare knowledge creation.
The added value of involving patients in healthcare is, respect to other more complex interventions, a low cost opportunity to take into consideration unconventional points of view creating and building knowledge and providing original insights and ideas that otherwise would not be considered.
Health professionals and patients’ skills and knowledge are acquired through individual experience or education and transferred to the health organizations in a perspective of co-production of healthcare. It is a merging of the efforts of those who produce and those who use the solutions to address health problems. It serves to establish a strengthened and long-term relationship in terms of trust and effectiveness and to distribute the responsibilities among all stakeholders [ 2 ].
In light of these arguments, the systems approach—inspired by the fundamentals of ergonomics and human factors (HFE)—creates new alliances between healthcare and engineering, of which patient journey is a challenging example [ 3 ].
Applying the systems approach to patient safety allows the analysis of the factors that characterize the encounters and the interactions between healthcare professionals and patients during the entire course of care. The observation of possible critical issues to the individual and specific encounter between clinician and patient is crucial in widening the scope of observation and research of the entire “journey” of the patient, taking into consideration the complexity of patient, their values and needs, their preferences, the economic and social context in which they live, and language and communication issues.
These observations and research should be carried out considering the interconnections and interactions together with the components of the processes; importance should be given to the context, and to manage the complexity, the value of a holistic approach.
2 The Patient Journey
A modern health system looks to the future in the context of the challenges imposed by the real world. It must manage the gap between guidelines and health protocols and what effectively happens and how reality is perceived by patients and family members.
It is more and more necessary to bring the patient’s point of view in the analysis of the care process, in the incident reporting and analysis, in the design and implementation of solutions and guidelines in healthcare.
Vincent and Amalberti in “Safer Healthcare” (2016) [ 4 ] stated that the incident analysis should broaden the class of events having consequences on patient safety. Incidents reported from the patient’s point of view should be included in addition to those suggested by health professionals. Additionally, when analyzing an incident, it should be done in the context of the patient journey rather than a single episode.
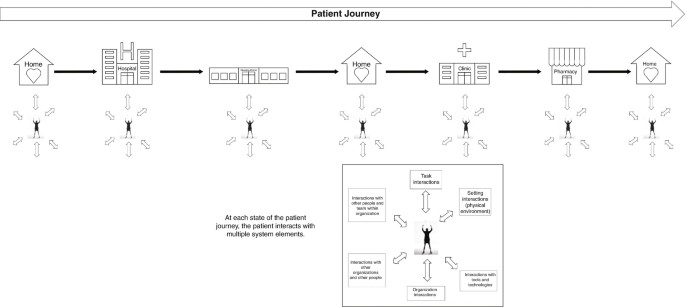
Instead of focusing on the individual encounter, it is necessary to extend the observation timeframe by applying the examination of contributing factors to each of the encounters that compose the patient journey (temporal series of encounters with healthcare facilities, a hospital unit, a specialist visit, a primary care clinic, a home health agency), considering both the negative and positive events and the points for improvement that were revealed (Fig. 10.1 ).
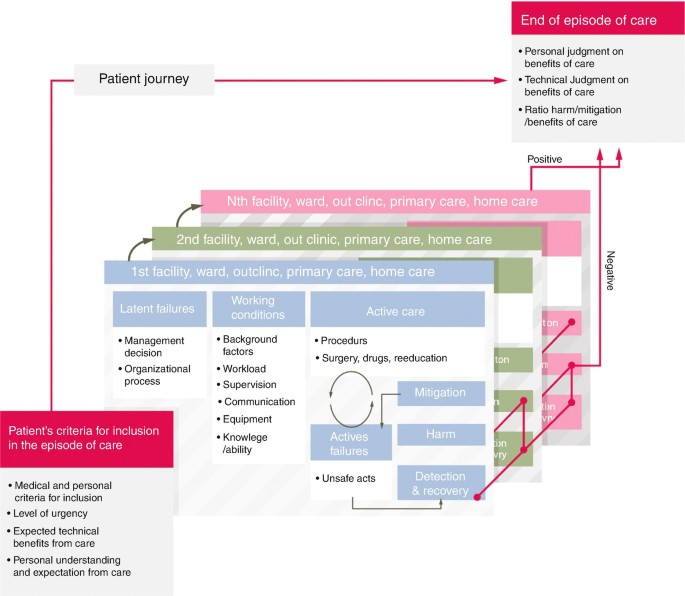
Analysis of safety along the patient journey
The adoption of this wider approach is unique in that it incorporates the patient’s perspective of safety and includes new features in the incident analysis such as asking patients to recount the episode of care, including patient and family in the investigation team when possible, asking patients the contributory factors from their point of observation and perception and involving patients and families in the reflections and comments on the disclosure process [ 4 ].
The episodes patients and families can highlight are often different from those that professionals are more accustomed to reporting. However, patients could be involved in further ways in incident reporting and assessment, and today patient-derived information constitutes a free and little used resource.
As per McCarthy’s definition, “patient journey mapping describes the patient experience, including tasks within encounters, the emotional journey, the physical journey, and the various touch points” [ 5 ]. Carayon and Woldridge define “patient journey as the spatio-temporal distribution of patients’ interactions with multiple care settings over time” [ 3 ], where at each point of touch with each healthcare service along the patient journey, the patient interacts with several system elements (task interaction, physical environment, interaction with tools and technologies, organization interaction, interaction with other organizations and other people, interaction with other people and teams within the organization) (Fig. 10.2 ).
The patient journey as a set of interactions and transitions
The patient journey represents the time sequence of what happens to the patient, especially during transitions of care, in particular considering that the health professional who takes care of the patient only sees the portion of care for which he is responsible and in which he has an active role. Conversely, the patient is the only person who has a continuously active and first-hand role during their health journey. They alone are in possession of information that characterizes the entire care experience.
Moreover, when patients navigate their journey, they contact and interface with multiple work systems at several time points, where the sequence of interactions in the work systems determine the outcome experienced by patients and families, healthcare professionals, and health organizations. (Fig. 10.3 ). Each local work system is influenced by a wider socio-organizational context, which can be formal healthcare organization (such as hospital, primary care facility, nursing home) or informal (home).
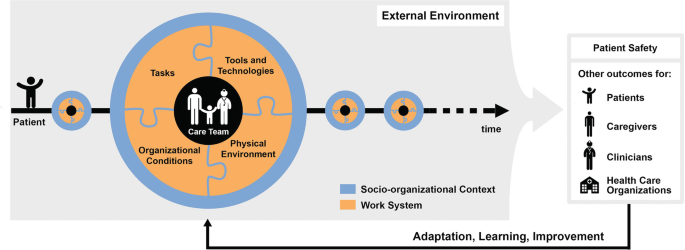
SEIPS 3.0 model: sociotechnical systems approach to patient journey and patient safety
Every point of the patient journey offers data on health outcomes and patient experience outcomes that should be used as feedback to redesign healthcare work systems in terms of adaptation, learning, improvement.
Patient’s experience represents an important resource in participatory collaborative design, especially in the patient journey where this experience is the result of multiple interactions across space and time.
3 Contextualizing Patient Safety in the Patient Journey
Many of the incidents or near-misses during healthcare are not due to serious errors, but to the combination of small failures, such as limited experience of a recently qualified doctor, use of obsolete equipment, an infection difficult to diagnose or inadequate communication within a team.
We know that the analysis of an incident requires looking back to the succession of events that have occurred and that led to the problematic episode, considering both active and latent errors, and all the aspects connected directly or indirectly. It is fundamental to examine the safety of the entire patient journey, all the encounters that make up the entire care process, to study the whole medical history of the patient in an attempt to reconstruct all the elements that characterize the “health journey”, not only from the viewpoint of the health professionals, but also from that of the patient and family.
In light of these arguments, new concepts, tools, models, and methods need to be embraced to support patient safety in the patient journey.
A significant contribution in terms of concepts, frameworks, and models is offered by Industrial and Systems Engineering, and often human factors and systems engineering (HF/SE) have an approach to include the preferences and the needs of stakeholders when designing solutions to address the critical aspects of a health process.
Human factors and ergonomics are described as “the scientific discipline concerned with the understanding of interactions among humans and other elements of a system, and the profession that applies theory, principles, data and methods to design in order to optimize human well-being and overall system performance. Practitioners of ergonomics and ergonomists contribute to the design and evaluation of tasks, jobs, products, environments and systems in order to make them compatible with the needs, abilities and limitations of people. Ergonomics helps harmonize things that interact with people in terms of people’s needs, abilities and limitations” [ 6 ].
Process models have found widespread use in drug management, visit planning, care transition, to name a few, and can offer tools and methods to investigate interprofessional and physician–patient communication, interruptions and health information handover.
Drawing from the finding of Carayon’s studies [ 3 ], the Systems Engineering Initiative for Patient Safety (SEIPS) model gives a description of five work system elements which when applied to a definite patient journey model should outline who (person) is doing what (tasks) with tool and technologies, taking into consideration the physical and organizational environment where all these activities take place. All these factors have to be examined for both patients and workers and the process analysis and modelling have to consider what patients and families/caregivers, healthcare professionals and workers actually do ( work-as-done versus work-as-imaginated ).
Patients, families, and caregivers are deeply involved in the healthcare process due to the tasks they carry out in the intermediate sectors of care between encounters. Away from direct interactions with professionals, they have to perform multiple actions requiring understanding of what behaviour to adopt, which instructions to follow, how to administer a medication and how to communicate with hospital doctors, general practitioner, and home healthcare professionals [ 3 ].
Taking into account what has been highlighted so far, one of the leading and most challenging keys to success in improving patient safety is to adopt a systems approach to patient safety which includes the patient’s perspective about their health journey throughout the time of care and across all the care settings.
This assumption highlights that patients and their families are valuable resources and can play an important role in patient safety improvement efforts. Viewing health systems as “co-producing systems”, patients can engage as partners in co-producing patient safety improvement activities individually, in groups and collectively. Individual patient and family member participation/co-production of safer care is fundamental. Equally as important is the co-management and co-governance of healthcare services, in addition to the engagement of communities in policy definition and designing activities.
In fact, patient engagement directs the design of healthcare systems towards the preferences, the values, the real-life experiences, and—not less important—the skills of the people to enhance patient safety in the patient journey.
Such a change of perspective involves multiple dimensions of interactions and relationship between patients and professionals, encompassing cooperation, dialogue and listening, trust, reciprocity and peer-to-peer work [ 2 ].
It follows that on the one hand the healthcare organizations have to demonstrate the willingness to support health professionals to effectively engage patients in the patient journey to achieve the common goal of reducing the risk of patient harm or incidents as well as the willingness to integrate patients and family members as partners into quality and safety improvement efforts. On the other hand, it is necessary to motivate and encourage patients and families/caregivers to actively participate during the individual care process for safer care as well as partner in organizational patient safety improvement efforts to ensure safer care for others.
The working group Patient and Family Involvement for the delivery of Safe and Quality Care [ 7 ] stated that the utmost priority to realize the patient involvement is the training of patients, followed by the promotion of interdisciplinary training programmes for healthcare professionals to promote patient and family engagement, the implementation of multilevel structures that allow for participatory processes by patients and smarter allocation of resources in healthcare that supports involving citizens in patient safety improvement efforts for better healthcare.
This working group was part of the activities of the “1st International Meeting about Patient safety for new generations—Florence, 31st August and 1st September 2018” organized by the Centre for Clinical Risk Management and Patient Safety, Tuscany Region—WHO Collaborating Centre for in Human Factors and Communication for the Delivery of Safe and Quality care [ 7 ].
Therefore, training for both patients/families/advocates and health professionals is a pillar on which to build active engagement of patients and consequently an effective and efficient patient journey. From this perspective, the participation of patients (i.e. representatives of patients’ associations and organizations, patient and citizen advocates) in training courses—specifically designed for this target audience of trainees and aimed to encourage co-production of care—is an essential and effective activity to co-produce a better healthcare system in terms of quality and safety of care.
Sharing a common language, promoting citizens’ and patients’ awareness of importance of co-production of care, teaching the key role that patients can play in making treatments safer (investments in health literacy), learning to work together and within a network (locally, regionally, and nationally/internationally) on priority safety and quality of care issues: these are some of the main strengths of training courses aimed to be at the basis of active engagement of patients and citizens.
Examples of successful training courses include “PartecipaSalute” and “Accademia del Cittadino” organized in Italy by Laboratory for Medical Research and Consumers Involvement of the Istituto di Ricerche Farmacologiche Mario Negri IRCCS and the Centre for Clinical Risk Management and Patient Safety, Tuscany Region. The following paragraph describes this educational experience which is specifically designed for citizens and patients to improve their knowledge and skills in patient safety and quality of care, with the aim of co-producing better healthcare services.
4 From PartecipaSalute to the Accademia del Cittadino: The Importance of Training Courses to Empower Patients
Over the last few years in the field of health and research and with regard to participation and involvement of citizens and patients, we have witnessed the transition from a paternalist to a partnership model. Individual citizens and those citizens involved in patients’ associations or groups have acquired a new role: no longer passive but actively involved in decision-making regarding health, healthcare, and research in the health field [ 8 , 9 ].
This is a progressive step-by-step process based on the recognition and implementation of the key concepts such as health literacy and empowerment. Health literacy, more properly used at individual level is defined as the capacity to obtain, read, understand, and use healthcare information in order to make appropriate health decisions and follow instructions for treatment [ 10 ]. Empowerment, more used at the community level, is a process that, starting from the acquisition of accurate knowledge and skills, enables groups to express their needs and more actively participate to request better assistance, care, and research. At this level, the availability of organized independent and evidence-based training courses is essential to allow people to be able to critically appraise and use information about the effects of healthcare interventions. Consequently, they will have the skills to participate in the multidisciplinary working groups (composed of researchers, health professionals, patient and citizen advocates, institutional representatives).
In the late 1990s, the Istituto di Ricerche Farmacologiche Mario Negri IRCCS held the first training courses of this kind focused at breast cancer associations. Some years later, within the project PartecipaSalute—a not-for-profit research project designed to foster a strategic alliance among healthcare professionals, patients, and their organizations—an ad hoc training programme for representatives of citizens’ and patients’ organizations was defined with a multimodule format [ 11 , 12 ]. This was an innovative approach, at least in the Italian setting in that period.
PartecipaSalute training programme has combined different experiences: the Mario Negri Institute IRCCS experience in collaborative research activities with patients’ associations, the Italian Cochrane Centre with the activities aimed at promoting the principles of evidence-based medicine, and Zadig long-term experience in health communication. The above promoters jointly developed the PartecipaSalute training programme on the belief that data are more important than opinions, and that every decision should be supported by well-conducted research data.
The spread of this belief to patients and citizens with the purpose of stronger involvement was a key point of PartecipaSalute training courses.
Therefore, patient, family, and community knowledge of the principles of how evidence is developed through clinical research is essential to make or support decisions in the health debate, to promote better clinical research, or to convey correct information. The strength of the PartecipaSalute programme was based on the exchange of experiences in an interactive way aimed at creating opportunities for discussion, overcoming the teacher–learner model. Each session started with an interactive discussion of a real situation—such as a screening, vaccination, therapy—and after sharing data, opinions or articles from media, evidence was presented and discussed, underlining significant methodological aspects. The programme offered the opportunity to debate the value and significance of the methodology offering critical appraisal tools. Each participant was invited to take an active part, starting from direct personal or associative experience. Table 10.1 presents the topics considered in the first three editions of the training programme. The participation was free, and different types of materials were provided including an ad hoc manual published by PartecipaSalute, copies of the PowerPoint presentation and articles.
Considering the characteristics of the programme and its modular structure, the PartecipaSalute training programme could be adapted to specific contexts. In fact, the experience of PartecipaSalute was adopted at the regional level by Regione Toscana (Centre for Clinical Risk Management and Patient Safety and the Quality of healthcare and Clinical pathways of Health Department, Tuscany Region) developing a more specific training programme called PartecipaSalute-Accademia del Cittadino (Academy of Citizen), focused on patient safety and risk management. In particular, after some modules on methods related to evidence-based medicine, uncertainties in medicine and information and communication in health, the training was mainly dedicated to regional and local activities on clinical risk management, the role of patients’ associations to improve patient safety and to support the implementation of best practices, the analysis and data of adverse events and risk assessment in terms of quality and safety in the care processes (Table 10.2 ).
The PartecipaSalute-Accademia del Cittadino joint training programme has been implemented in three editions over the last decade and has trained about 100 members of patient and citizen advocates representing 38 patients’ associations. The courses ranged from 5 to 3 modules of 2 days each in residential mode to allow participants to get to know each other and create a network of associations committed to be engaged in clinical research, quality, and healthcare safety issues.
The entire educational experience was characterized by the use of participatory training methods, based on working groups, practical exercises, lectures from experts with opportunities for discussions. As a result of this training course model, the participants were recognized as “expert patients” and were regularly involved in basic activities for promoting patient safety as auditors on significant events and helping to define policies on patient safety at the Tuscany regional level. In addition, they have participated in patient safety walkarounds in hospitals and in developing eight cartoons intended to promote the education of citizens for the prevention of the most diffused risks (such as prevention of infections, prevention of falls and handovers).
Feedback on the satisfaction on tutors, topics discussed and knowledge gained was regularly requested from participants through questionnaires distributed before and after the programme. In general, positive feedback was received; participants appreciated the interactive methods of work, the clarity of the language, and the effort to make difficult problems easy to understand. An ad hoc questionnaire was provided to the participants regarding the methodology of clinical research, always showing an improvement in the self-evaluated knowledge before and after the course. Feedback of the results of the evaluation was also shared with each participant. Most of participants reported their experience to other members of the organization. In particular, in the case of the Regione Toscana training, the possibility of immediately transferring what was learned in the course in all the activities in collaboration with the health institutions, policy makers, and health professionals—such as working groups on patient safety best practices, participation to audits, development of tools to improve health literacy—was appreciated.
Some limitations emerged from these experiences. The selection of participants is the first issue, not only because the training course is accessible to a small number of participants (in general no more than 30 participants), but also because the groups comprised of middle-aged and retired participants, with few younger ones. Additionally, there were few individual patient or family member representatives from patient associations. The majority of those representing patient associations were in managerial or leadership positions. Furthermore, it is difficult to choose between small, local, or bigger regional associations. Residential training courses also restricted the participation for geographical reasons.
The PartecipaSalute and ParteciaSalute-Accademia del Cittadino training experiences show that patients and citizens are willing to get actively involved in healthcare and the research debate. There is a real desire to improve their knowledge and skills on health and research issues and allow some general considerations regarding the active engagement of citizens representing associations and advocacy groups.
In conclusion, it is very important to invest in a process of empowerment aimed to have well-trained activists involved vigorously and constructively in the debate, design, and assessment of health and research. Switching from tokenism to active participation is necessary to effectively partner with patients and the general population to design, plan, and co-produce safer more effective healthcare, while also supporting better more patient-centred research [ 13 , 14 ].
Also, the training courses are feasible and useful, as has recently been discovered also by pharma or other groups that organize courses mainly focused on drugs and drug development, thus directing the participation of the groups more to market needs than to public health.
Furthermore, this training initiative facilitates the networking among associations in part overcoming the difficulties that derive from personalization and division among the associations representing citizens and patients.
Finally, this illustrates the importance of the design and promotion of training courses with institutions, such as the Regione Toscana, in order to be able to implement projects of real collaboration between institutions, healthcare professionals, and consumers’ and patients’ representatives.
5 Recommendations
A systemic approach to health can provide valuable models for wider implementation of patient safety. A multidisciplinary approach includes the involvement of citizens and patients as unique stakeholders in the design, implementation, delivery, and assessment of health services.
Involving patients in healthcare is an opportunity to bring uncommon points of view into policy making and to create shared knowledge between healthcare professionals and patients.
The implementation of patients’ and families’/caregivers’ perspectives in the patient journey is the golden opportunity to leverage crucial input, such as experiential knowledge, safer care, patient motivation, and trust and social cohesion into the co-production of safety solutions in healthcare. This represents a way to get closer to person-centred care, to create opportunities for patients to meet and share information and knowledge, to develop structures and policies for patient involvement at different levels (with healthcare systems, universities, and policy makers).
However, little has been done to overcome some healthcare systems barriers: the power imbalance between the doctor and patient, language differences, the lack of diffusion of non-technical skills and, last but not least, the lack of evidence about the value of patient involvement.
To be widely implemented, patient engagement in the patient journey requires courageous leadership, organizational efforts, a wider culture of safety of care, the implementation of multilevel structures for the engagement of patients and resources from smarter spending in healthcare.
Education is the landmark to integrate meaningful patient and citizen engagement in healthcare. Training of patients is the fundamental starting point to develop shared knowledge, co-produce projects, and implement an active multilevel participation of patients and families for the improvement of quality and safety of care.
Kaplan G, Bo-Linn G, Carayon P, Pronovost P, Rouse W, Reid P, Saunders R. Bringing a systems approach to health, Discussion Paper. Institute of Medicine and National Academy Engineering. 2013.
Google Scholar
Palumbo R. Contextualizing co-production of health care: a systematic literature review. Int J Public Sect Manag. 2016;29(1):72–90. https://doi.org/10.1108/IJPSM-07-2015-0125 .
Article Google Scholar
Carayon P, Wooldridge AR. Improving patient safety in the patient journey: contributions from human factors engineering. In: Smith AE, editor. Women in industrial and systems engineering. Key advances and perspective in emerging topics, Women in engineering and science, vol. 12. Cham: Springer; 2019. p. 275–99.
Vincent C, Amalberti R. Safer healthcare-strategies for the real world, vol. 5. Cham: Springer Open; 2016. p. 47–57.
Book Google Scholar
McCarthy S, O’Raghallaigh P, Woodworth S, Lim YL, Kenny LC, Adam F. An integrated patient journey mapping tool for embedding quality in healthcare service reform. J Decis Syst. 2016;25(Suppl 1):354–68. https://doi.org/10.1080/12460125.2016.1187394 .
International Ergonomics Association (IEA). Definition and domains of ergonomics. https://www.iea.cc/whats/ . Accessed 23 Dec 2019.
International Meeting about Patient safety for new medical generations—Florence, 31 Aug and 1 Sept 2018. http://iea2018.org/?page_id=4373 . Accessed 23 Dec 2019.
Castro EM, Van Regenmortel T, Vanhaecht K, Sermeus W, Van Hecke A. Patient empowerment, patient participation and patient-centeredness in hospital care: a concept analysis based on a literature review. Patient Educ Couns. 2016;99(12):1923–39. https://doi.org/10.1016/j.pec.2016.07.026 . Epub 2016 Jul 18.
Article PubMed Google Scholar
Coulter A, Ellins J. Effectiveness of strategies for informing, educating, and involving patients. Br Med J. 2007;335:24–7.
IOM. Health literacy: a prescription to end confusion. Washington DC: National Academies Press, 2004; Am J Prev Med. 2009;36(5):446–51.
Mosconi P, Colombo C, Satolli R, Liberati A. PartecipaSalute, an Italian project to involve lay people, patients’ associations and scientific-medical representatives on the health debate. Health Expect. 2007;10:194–204.
Mosconi P, Satolli R, Colombo C, Villani W. Does a consumer training work? A follow-up survey of the PartecipaSalute training programs. Health Res Policy Syst. 2012;10:27. https://doi.org/10.1186/1478-4505-10-27 .
Article PubMed PubMed Central Google Scholar
Ocloo J, Matthews R. From tokenism to empowerment: progressing patient and public involvement in healthcare improvement. BMJ Qual Saf. 2016;25:626–32. https://doi.org/10.1136/bmjqs-2015-004839 .
Chalmers I, Bracken MB, Djulbegovic B, Garattini S, Grant J, Gülmezoglu AM, Howells DW, Ioannidis JP, Oliver S. How to increase value and reduce waste when research priorities are set. Lancet. 2014;383:156–65. https://doi.org/10.1016/S0140-6736(13)62229-1 .
Download references
Author information
Authors and affiliations.
Centre for Clinical Risk Management and Patient Safety, Tuscany Region—WHO Collaborating Centre in Human Factors and Communication for the Delivery of Safe and Quality Care, Florence, Italy
Elena Beleffi
Laboratory for Medical Research and Consumers Involvement, Public Health Department, Istituto di Ricerche Farmacologiche Mario Negri IRCCS, Milan, Italy
Paola Mosconi
The Society to Improve Diagnosis in Medicine, Evanston, IL, USA
Susan Sheridan
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Elena Beleffi .
Editor information
Editors and affiliations.
London School of Hygiene and Tropical Medicine, London, UK
Liam Donaldson
Department of Hygiene and Public Health, Catholic University of the Sacred Heart, Rome, Italy
Walter Ricciardi
Italian Network for Safety in Healthcare, Florence, Italy
Riccardo Tartaglia
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Reprints and permissions
Copyright information
© 2021 The Author(s)
About this chapter
Beleffi, E., Mosconi, P., Sheridan, S. (2021). The Patient Journey. In: Donaldson, L., Ricciardi, W., Sheridan, S., Tartaglia, R. (eds) Textbook of Patient Safety and Clinical Risk Management . Springer, Cham. https://doi.org/10.1007/978-3-030-59403-9_10
Download citation
DOI : https://doi.org/10.1007/978-3-030-59403-9_10
Published : 15 December 2020
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-59402-2
Online ISBN : 978-3-030-59403-9
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Patient Journey Mapping: What it is and Why it Matters

How can healthcare organizations make every stage of the patient journey better?
How was your last experience in a healthcare facility? Think about every step of that patient care journey - the phone calls, in person meetings, wait times, communication and all of the healthcare professional/ patient interactions. It’s a lot.
Healthcare organizations are working diligently to improve patient satisfaction and quality of care by asking, “How can we make the patient experience better?” But that’s no mean feat, trying to capture the multitude of challenges patients face when navigating a healthcare journey. That makes improving it even more difficult.
A first, fundamental step to improving patient experience is understanding what that experience looks like today. This is where patient journey mapping comes into play. You can use patient journey maps to understand the highs and lows, pain points and gaps to begin pinpointing which interventions will be most impactful. Then you can assess which changes you have the power to make.
As a result, you’ll be better able to manage your patient’s journey, improve care pathways and meet—and exceed—patient expectations, needs, and wants.
What is Patient Journey Mapping?
Patient journey mapping works to identify and understand the details of all patient touchpoints within a specific healthcare experience. It helps you visualize the process patients go through to receive care, complete a treatment plan, and/or reach a desired outcome. When done correctly, patient journey maps make it easier for you to identify pain points, discover opportunities and re-align treatment and care approaches across the entire healthcare system.
What makes up a patient’s journey?
A patient’s journey represents the entire sequence of events or touchpoints that a patient experiences within a given health system, with a specific provider, or within a specific facility. These touchpoints are either virtual or in-person. They range from the mundane to the nerve-wracking or life-changing. They comprise events from scheduling an appointment online to reviewing post-surgery instructions with a doctor.
It’s key for healthcare professionals and clinicians to recognize the patient journey extends well beyond the most obvious in-person interactions at a treatment facility. The patient journey happens before, during and after a healthcare service: pre-visit, during-visit, and post-visit. These include but are not limited to:
- Finding the right service or practitioner
- Scheduling an appointment
- Submitting a list of current medications
- Arriving at the medical facility
- Identifying where to check-in.
These experiences can instil a sense of reassurance or unease before a patient even receives care. In essence, they set the tone and expectations for the physical visit. A frustrating or confusing experience during the pre-visit stage will impact the emotional state of the patient and family for the rest of their interactions.
During-visit
- Checking in at the front desk
- Waiting in the lobby to be called
- Discussion with nurses before speaking to a doctor
- Family waiting for updates in the lobby during a procedure
- Care from doctor and staff.
There are an infinite number of touchpoints during the delivery of healthcare. Each one will have a different level of impact on the patient’s experience.
- Post-care instructions at hospital
- Hospital discharge process
- Completing a patient feedback survey
- Paying for the medical treatment
- Post-surgery calls or online messages from the nurse or doctor.
The patient experience after a hospital visit plays a vital role in either reinforcing a positive experience or mitigating a negative one. Actions such as post-appointment follow-ups extend the care relationship and may help the likelihood of the patient sticking to the treatment plan
All these individual touchpoints are crucial to understand. Altogether, these positive and negative experiences — no matter how big or small — comprise the patient journey.
Who are the stakeholders?
The healthcare ecosystem is complex, involving multiple stakeholders and a wide range of internal and external factors, including:
- People (patients, their families and caregivers, doctors, nurses, administration, parking attendants, volunteers)
- Technology and systems (online registration, parking tickets, surgery updates, mobile app, website, social media)
- Facilities (hospital campus navigation, parking availability, building accessibility).
Investigation of all players and systems involved is essential to seeing the multidimensional layers impacting the experience. To do this, patient journey maps should include the perspectives of patients, providers, and staff - and those perspectives must be of the same journey. Often, an interaction that occurs from one point of view will show only one reality. However, further investigation will show the many contributing factors across the care delivery process. This is only apparent by examining multiple perspectives.
Once you understand the entire journey, with pain points, you’ll be able to identify patterns across patient personas and different demographics, and any gaps within the healthcare process. You can then begin asking important questions like:
- Which moments are most painful?
- Why do they happen?
- What must we change in order to improve the experience?
- Who must we impact?
- Which do we have the power to change?
Benefits of patient journey mapping
Patient journey mapping provides the opportunity to turn the healthcare experience from a primarily reactive experience to a proactive one. By building out care journeys for your patients, you can close any gaps in provision and establish robust preventative routines that ultimately help your patients stay healthier for as long as possible. Engaging consumers and patients based on where they are and what they want, builds trust and confidence. That retains patients in your system and encourages them to make friends and family referrals.
But how does the process work?
- Streamline patient processes and workflows: upgrading the usability and functionality of online patient portals, websites and mobile apps can put more control in the patients’ hands, increasing patient flow and cutting operational expenses.
- Increase staff efficiency : enhancing internal online tools and creating automation within systems can assist hospital staff in implementing protocols and schedules and help them anticipate and solve problems more easily. It can help to align the expected service delivery with the actual one.
- Clear routes and direction across medical facilities: hospitals can be incredibly complicated to navigate - whether it’s using the right entrance, finding parking or making your way to the cafeteria for a snack. Improving signage, making visible pathways, and using landmarks to help orient users can help patients and families readily access the resources they need.
- Improve communication between patients and providers: exchanging patient information and coordinating care can be a challenge for providers and a frustration for patients. This misalignment can be due to silos within organizations, incompatible technology systems or many other factors. Working to bridge the appropriate organizational or technological gap can help alleviate stress and anxiety.
- Develop seamless and timely patient and family updates: waiting while a family member is in surgery or communicating with a doctor to secure care for a child is typically an extremely stressful process. Families wait anxiously for updates which can be infrequent and lacking detail. Implementing a seamless system for families to communicate directly and receive regular updates, through an app or text, can help ease these pain points.
- Better ‘in-between visit’ care and check-ins with patients and families: communication between patients, including families and caregivers and providers can feel ‘hit or miss.’ Patients may be scrambling to answer phone calls or missing phone calls only to find themselves unable to get hold of the provider when they call back. Alternatively, providers are challenged to communicate critical information to a wide range of patients. Establishing better communication systems can improve patient engagement, build the patient’s confidence in the care they receive, and ease the care provider’s job.
In short, we’re talking happier patients who experience better communication and levels of empathy at every stage of the patient journey.
What tools and methods are used for creating a patient journey map in healthcare?
There are many ways to undertake patient journey mapping, but doing it well isn’t always as simple as it may seem. It’s not a single exercise, moving from A to B. It’s more complex, involving a series of tools.
Our team at Highland has helped a lot of our clients create their first journey map . Grab a bunch of sticky notes and pens to start your map. Our process tends to go like this:
- Chart the course -work out what you want to achieve (your goal); determine whose journey you’re mapping, the start and end points; create the persona(s); think about what the stages of the journey may be.
- Prepare to interview - list your potential questions being mindful that you want the interviewee to recount events rather than share opinions. Schedule interviews with a tool like Calendly. Look into other available data (such as patient feedback).
- Interviews and coding - we interview in pairs so that one can speak whilst the other takes notes. With permission, record the interviews. Afterwards, code the responses according to thoughts, actions, experience etc. We use a simple Google Sheet to do this.
- Building blocks - go through the interviews and notes. Start mapping. Use a specific color of sticky note for each Building Block and add points to the wall in their themes.
- Identify opportunities - “mine” the wall for opportunities, presenting ideas to the team. Together, prioritise the top three or four to tackle.
Repeat this whole process with another persona or goal to examine.
Explore this journey mapping process in more detail
The outcome of this process should be that healthcare professionals can look after patients better. Using patient data collection to underpin your decision-making can transform your organization’s culture to one of continuous improvement. By referring constantly to patient data, you can identify the key areas to amend and improve to better the patient experience. Satisfied customers, those who’ve experienced a near seamless patient journey, will rate your facility highly and they’ll be more likely to generate new referrals.
Improve your customer experience with Highland Solutions’ help
You may know your healthcare facility like the back of your hand, but you only know it from your informed perspective. Getting a 360º view of the patient experience is the first step to improving it. A huge challenge for healthcare leaders like you is to recognize, understand and address the fact that the overall experience is created by the cumulative interactions across the various touchpoints in the healthcare journey: pre-visit, during-visit, and post-visit.
Despite years of expertise, it’s easy for healthcare providers and leaders to develop blind spots for persistent issues in the care process. Partnering with a knowledgeable research team to conduct patient journey mapping will bring expertise and a fresh perspective to your quality of care. It’s not only about uncovering in-depth insights via patient journey maps, but also translating them into actionable strategies to help you bridge any gaps between current and emerging patient needs and the present state of your healthcare organization.
Once on the right track, you’ll be enabled to manage and grow relationships at every stage of the patient journey. The more patient-centric you become, the better experience you build, reaching a higher quality of patient care, patient retention and loyalty, and improved health outcomes and overall well-being.
Get in touch to find out more about how we can help you with patient journey mapping
“Working with Highland is a really powerful experience for a company to be able to gain insights. To have real conversations with patients unlocks new pathways, ones that may be uncomfortable and uncover change, but they empower you to move forward in a way that feels really constructive.”
Chris Whitworth, Vice President, Treatment
Download “The Essential Guide to Launching a Digital Product for Experts & Expert Firms”


Welcome to The Patient Journey Course
Unlock the secrets to skyrocketing your case acceptance rates with our comprehensive online course. Learn how to confidently communicate with your patients, handle objections, and present treatment plans in a way that resonates with their personality type. With our proven strategies, you'll see a significant increase in your case acceptance, leading to a higher monthly income, a successful practice brand and most importantly satisfied patients. Don't let another potential case slip through your fingers
The first impression is everything, and that's especially true when it comes to patient consultations. If you want to make a good impression and increase your case acceptance rate, you need to deliver the perfect consultation. In this course, you will learn how to: - Build rapport with your patients - Ask the right questions Present your treatment plan in a clear and concise way - Overcome objections - Close the sale By the end of this course, you will be able to deliver consultations that are both informative, persuasive and fun.
Whether you're dealing with NHS or private patients, effective communication is key. Our course offers tailored strategies for both sectors, helping you navigate the presentation of both options and converting more patients to private treatment. Learn how to build trust, manage expectations, and deliver exceptional patient care, regardless of the setting.
Take the guesswork out of patient communication with our tried-and-tested frameworks and scripts. We provide you with the tools to handle any scenario, from tricky patients to complex treatment discussions. With our course, you'll never be at a loss for words again.
We believe in the power of learning from real-world examples. That's why we've included an exclusive archive of real patient journeys I have filmed (as Dental Hype) over the years, shared by successful clinicians You'll learn from their experiences, their mistakes, their highly converting tactics. These are the insider secrets you won't find anywhere else. Our courses will be available to you anytime, with unlimited access. Disclaimer: CPD Certificates will be sent after 6 months from launch upon full course module release.
Learn how to create comprehensive, understandable, and premium treatment plans that your patients will readily accept. We'll teach you how to effectively communicate the value of your services and how to actually price your treatments irrespective of what your competition is doing.

Course Curriculum
You want to build a great patient journey? It starts with great foundations. This module will teach you the building blocks of what the highest converting clinicians do, day-in day-out in their surgeries.
Want to learn how to persuade your patients effectively? To talk their language? To read their personality types? This cutting edge, psychometric framework has not been taught in dentistry before. This module will teach an efficient method to be able to read patients fast and mould your patient journey and treatment plan presentation in a way that will be help your case acceptance increase exponentially without needing to "hard sell!"
Learn the ultimate patient journey framework. Bring your patients through the six phases of dental communicative excellence. Transform your patient journey forever and create an eager waiting list of patients built on amazing word of mouth referrals. Warning - This module will change your career (and potentially your life).
"I don't know how to discuss prices with patients" - Every Dentist Ever. The most common complaint we hear with regards to treatment planning is about price. We are looking to make this complaint a myth with this module. By the end of this module we will have your treatment planning process optimised, taking your presentations from "high stress selling" to "low stress conversations" that convert high end treatment with ease.
Are you tired of constantly under-pricing your high quality work to match your local competitions prices? Do you want the confidence to be able to charge a premium? From pricing strategies and price psychology to treatment planning frameworks and presentation tips & tricks - this module has it all.
In Module 6 of our patient journey course, we dive into the intricacies of operating a mixed practice and achieving patient journey perfection within the NHS system. This module is designed to equip you with the necessary knowledge and skills to seamlessly convert NHS patients to private patients while presenting both options in a persuasive and compelling manner. We understand that navigating the complexities of the NHS system can be challenging, and our aim is to empower you with practical strategies to optimize the patient experience and facilitate a smooth transition from public to private care. Throughout this module, you will gain invaluable insights into the key factors that influence patient decisions and learn effective techniques to engage and educate them about the benefits of private healthcare. We will delve into various topics, including: 1. Understanding the NHS Patient Journey: You will explore the entire patient journey within the NHS system, from initial contact to post-treatment follow-up. By comprehending the intricacies of this process, you will be better equipped to identify opportunities for presenting private care as a valuable alternative. 2. Tailoring the Patient Experience: Creating a seamless and personalized patient experience is paramount in ensuring patient satisfaction and loyalty. We will provide you with practical tips and strategies to enhance the patient journey, including effective communication techniques, active listening, and fostering a sense of trust and rapport. 3. Presenting Private Care Options: Converting NHS patients to private patients requires a delicate balance of presenting the advantages of private healthcare while respecting the existing system. We will guide you through the process of showcasing the unique benefits of private care, emphasizing personalized attention, reduced wait times, access to advanced treatments, and the overall enhanced patient experience. 4. Overcoming Patient Objections: Addressing patient concerns and objections is a crucial aspect of the conversion process. We will equip you with proven techniques to handle objections effectively, emphasizing the value proposition of private care and highlighting the long-term benefits that patients can enjoy. By the end of this module, you will possess the tools and knowledge to navigate the challenges of operating a mixed practice successfully. You will be able to present both NHS and private care options in a persuasive and compelling manner, ultimately helping patients make informed decisions that align with their healthcare needs and aspirations.
The anxiety you face dealing with a difficult patient. The gut wrenching moment you get a complaint. We have you covered. We have multiple, step-by-step, tried and tested frameworks to not only avoid or mitigate against complaints but also turn those difficult patients into your biggest fans! Unbelievable right? You might want to hear us out.
We walk the walk in this course. You are about to see BTS footage of Dr Raabiha Maan with a myriad of different patients. Watch how she communicates, educates, handles objections, treatment plans, manages difficult patients, puts them at ease, wins their hearts, converts high end treatment with ease and has her patient returning for years to come! It's our Patient Journey Framework in action. Once you see this module, you won't practice day-to-day dentistry the same way again.
Implementation. That is what separates a "good" clinician from a "great" one! A "good" course from a "great" one! A "good" patient journey from a "great" one! You are here for a transformation so this module teaches you how to implement everything you have learnt in this course. We made this course for a reason. To help Clinicians Create a personalised, repeatable and unique patient journey that you feel confident and comfortable delivering. Your patients leave with absolute faith in you and talk about you to their friends as “the best experience in a dental practice I've ever had”. So we'll be damned if you don't go ahead and get that outcome for yourself.
Ever wondered what other clinicians patient journeys look like in real life? Never been done in any online course before ... This is our behind the scenes "Fly on the wall content" with real patients and real clinicians that we have filmed over the last 6 years. Finally understand what makes other clinicians so good and learn from what they say/do to close their patients.
Testimonials

Lorem ipsum dolor sit amet, consectetur adipiscing elit. Nullam et lacinia mi. Proin in sagittis dolor. Curabitur et quam id mauris.
“Amazing content. Really impressed/inspired by your story!”
"One of the best online courses I have purchased. Dr Rhona is an amazing teacher and really makes you feel empowered to implement all the ideas, tactics and workflows that she reveals in the course. As a practice owner, I was blown away by the efficiency at which she manages her Invisalign volume. Learning her workflows and social media strategies were worth way more than the price of admission - I was so impressed I've upgraded onto her mentorship programme so I can shadow her and learn first hand. Thank you Rhona."
“Hey Rhona! I did my first composite bonding case today! Still needs adjustments and polishing but watched your module on composite last night and it helped so much thank you!! Made the treatment flow so much better than I expected and i loved it so much! Hopefully much more to come✨”

Get started today
DentalHype © 2023

IMAGES
VIDEO
COMMENTS
Sentean donne un visage à de nombreux services existants -et autonomes- et rend le processus clair, compréhensible, pertinent et concret pendant le « parcours patient ». Traductions en contexte de "patient journey" en anglais-français avec Reverso Context : Our advanced solutions improve the patient journey and optimize operations for ...
Google's service, offered free of charge, instantly translates words, phrases, and web pages between English and over 100 other languages.
Many translated example sentences containing "a patient journey" - French-English dictionary and search engine for French translations.
Parce que le parcours d' un patient dépend du nôtre. Go on a patient's journey through the health system. Faites ici le parcours d' un patient dans le système de santé. A patient's journey to recovery begins upon arrival. Le cheminement du patient dans la voie menant au rétablissement commence dès son arrivée.
Schwannomatosis. A "Patient Journey" is a personal testimony that reflects the needs of patients in two key reference documents—an accessible visual overview, supported by a detailed ...
Healthcare providers also reap several benefits, including the following: 1. Efficient patient care. When they understand the patient journey, healthcare providers can provide care more efficiently and spend less time and money on unnecessary, unwanted communications. 2. Proactive patient care.
Le service sans frais de Google traduit instantanément des mots, des expressions et des pages Web entre le français et plus de 100 autres langues.
26.1 Topic List: The Patient Journey and Quality of Care. 1. Patient mapping or patient journey, definition and importance in highlighting patient experience, link with good care from patient's perspective. 2. Patient journey within quality of care, indicating the route of a patient through healthcare system. 3.
Patient Journey is divided in several stages that are con-. " ". sidered inherent to the speci c disease. Each stage in the. fi. journey is referenced under three levels: clinical presenta ...
Therefore, hospitals can significantly improve the quality of the service provided by exploring and understanding the individual patient journey [ 12 - 14 ]. Many tools may be used to measure and understand patient experience [ 15, 16 ]. Surveys are the methods mainly used to capture the patient experience and to evaluate the quality and ...
The patient journey is a challenging example of using a systems approach. The inclusion of the patient's viewpoint and experience about their health journey throughout the time of care and across all the care settings represents a key factor in improving patient safety. Patient engagement ensures that the design of healthcare services are ...
Process mapping enables the reconfiguring of the patient journey from the patient's perspective in order to improve quality of care and release resources. This paper provides a practical framework for using this versatile and simple technique in hospital. Healthcare process mapping is a new and important form of clinical audit that examines how we manage the patient journey, using the ...
A "Patient Journey" is a personal testimony that reflects the needs of patients in two key reference documents—an accessible visual overview, supported by a detailed information matrix. The journey shows in a comprehensive way the goals that are recognized by both patients and clinical experts. Therefore, it can be used by both these ...
Patient journey mapping is an emerging field of research that uses various methods to map and report evidence relating to patient experiences and interactions with healthcare providers, services, and systems. This research often involves the development of visual, narrative, and descriptive maps or tables, which describe patient journeys and ...
Patient journey maps can be generated using a variety of techniques (8,9), can be used to identify problems, and can suggest improvements to the care process . The effectiveness of these maps has been researched in a range of care settings, including chronic care . As a result of analyzing the patient journey, 3 critical needs were identified ...
The patient journey is a chain of events a patient experiences when engaging with your practice. It includes a variety of encounters, ranging from seeking medical care to scheduling appointments to follow-up care instructions. Generally, you divide the patient journey into three major categories pre-visit, visit, and post-visit.
1. Identify The Goals and Scope of Your Map. Begin by developing a clear vision of what you aim to achieve through patient journey mapping. Whether it's to enhance patient satisfaction, streamline healthcare delivery, or identify gaps in service, setting specific objectives will direct your mapping efforts.
A Patient Journey functions both as a method and as a dynamic document. As a method, they involve charting the needs and experiences of patients and caregivers from the clinical presentation and throughout key stages of their healthcare journey, encompassing both medical and psychological aspects. As a document, they offer a visual and
The promotion of systems-based approaches offers methods and tools to improve the safety of care. A multidisciplinary perspective must include the involvement of patients and citizens as fundamental contributors to the design, implementation, and delivery of health services. The patient journey is a challenging example of using a systems approach.
A patient's journey represents the entire sequence of events or touchpoints that a patient experiences within a given health system, with a specific provider, or within a specific facility. These touchpoints are either virtual or in-person. They range from the mundane to the nerve-wracking or life-changing.
Traducción de "patient journey" en español. patient journey. experiencia del paciente. viaje del paciente. trayecto del paciente. camino del paciente. recorrido del paciente. Mostrar más. Defining the key stages of the process through a patient journey and identifying patient profiles.
Welcome to The Patient Journey Course. This course will help you Masterfully Communicate With Each Patient You See, Everyday, In Any Scenario, With Confidence, Authority And No Hesitation. - Your Income, Patient Experience & Career Fulfillment. Increase Your Case Acceptance Today Whilst Dealing With Any Tricky Patients Or Avoiding Litigative ...