- Pizzazz Sandals
- Leather Naturally
- Bestsellers
- Why HF Journey


Coming Soon
For the classy, sophisticated and fashionable, that enjoy wearing timeless curation in leather, our upcoming collection features classic and high-end products that emulate elegance with distinct and polished detailing. From leather footwear to designer sneakers, our product development team is coming up with exciting new designs and products, for you to wear and enjoy. Stay Tuned.

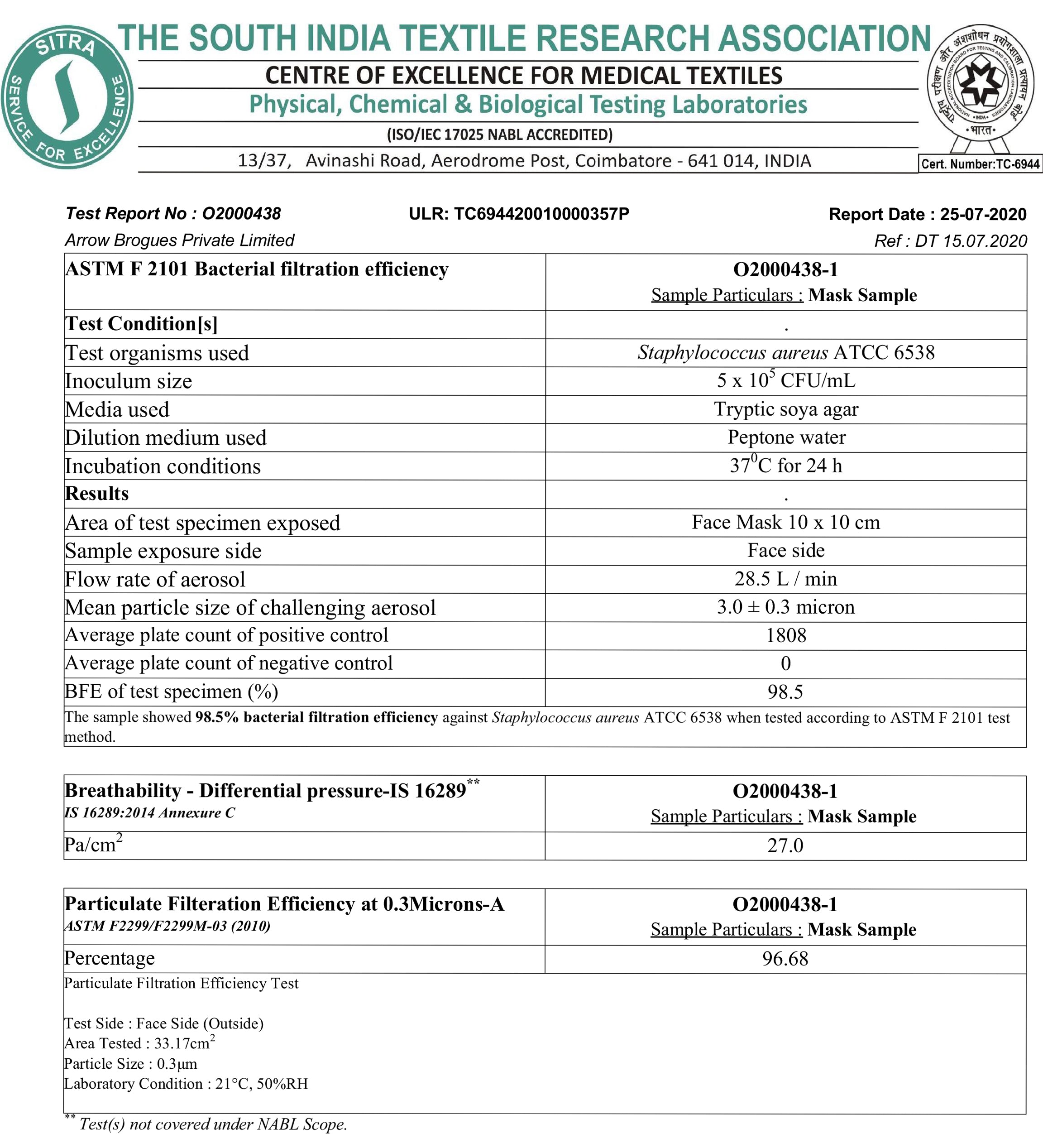
PFE Certification
Managing Heart Failure Hospitalizations
— strategies for decongestion, inotropic support, and optimizing guideline-directed medical therapy.
by Crystal Phend, Contributing Editor, MedPage Today Reviewed By Andrew Perry, MD, Cardiovascular Research Fellow, Vanderbilt Translational and Clinical Research Center, Vanderbilt University Medical Center, Nashville

"Medical Journeys" is a set of clinical resources reviewed by physicians, meant for the medical team as well as the patients they serve. Each episode of this journey through a disease state contains both a physician guide and a downloadable/printable patient resource. "Medical Journeys" chart a path each step of the way for physicians and patients and provide continual resources and support, as the caregiver team navigates the course of a disease.
Hospital admission occurs almost universally at some point in the heart failure (HF) journey. The disease is one of the most common reasons for hospital admission in the United States.
National HF hospitalization rates are on the rise, increasing from 4.4 per 1,000 U.S. adults in 2010 to 4.9 per 1,000 in 2017, according to a study of Nationwide Readmission Database trends. Pandemic impacts on lifestyle and healthcare were expected to contribute to worsening of chronic conditions associated with HF, suggesting the potential for further rise in the rates.
Acute coronary syndrome requiring urgent revascularization and inflammatory heart disease will account for some of these decompensation cases, but the vast majority arise from gradually rising cardiac filling pressures with preexisting structural heart disease.
Hospitalization is recommended for HF patients with hypotension; declining renal function; change in mental status; dyspnea at rest; atrial fibrillation with a rapid heart rate, ventricular tachycardia (including after an implanted cardioverter-defibrillator shock) or other arrhythmia; and acute coronary syndromes.
Inpatient care focuses on hemodynamic stabilization, symptom relief, and preventing short-term morbidity and mortality. Care starts with hemodynamic assessment to determine the severity of congestion and the adequacy of perfusion.
Management is then guided by investigation of the overall patient trajectory and precipitating factors, such as uncontrolled hypertension, acute infection, medication or lifestyle nonadherence, or use of medications that increase sodium retention, such as nonsteroidal anti-inflammatory drugs and steroids.
Decongestion
For acute decompensated HF, reducing congestion is a key goal of inpatient treatment.
Some studies have shown that natriuresis (as measured by urinary sodium output) is associated with a mortality benefit in HF . However, the PUSH-AHF randomized controlled trial did not show a difference in outcomes using a natriuresis-guided strategy versus usual care.
Loop diuretics are the most commonly used, with careful attention to dosing. Higher doses can be required for patients with severe renal insufficiency or low cardiac output to make sure enough of the drug reaches the site where it's needed. Resistance to oral diuretics can also occur because splanchnic congestion leads to bowel wall edema and thus poor gastrointestinal absorption of the medication.
Adding a thiazide diuretic or a mineralocorticoid receptor antagonist (MRA) with diuretic effects can also be effective.
In terms of the diuretic, the DOSE trial did not show an advantage of bolus doses of furosemide rather than continuous infusion, although with some trend for greater diuresis and symptom improvement at the expense of transient worsening of renal function. The TRANSFORM-HF trial showed similar outcomes for furosemide and torsemide. However, the ADVOR trial showed that adding IV acetazolamide to loop diuretics boosted early decongestion.
Guidelines suggest use of IV nitroglycerin or nitroprusside as an option to consider as an add-on to diuretics for dyspnea relief for patients without systemic hypotension.
While the need for IV diuretics has been a leading reason for admission to rapidly reduce congestion, outpatient management with ambulatory or clinic-based diuretic use is gaining support. At-home dosing with an IV-equivalent formulation of furosemide (Furoscix) is also approved for patient self-administration using a pre-filled cartridge for 5-hour subcutaneous injection.
In one retrospective analysis of day-case unit or home IV treatment, only 11 of 79 patients needed to be admitted for higher doses than could be administered on an outpatient basis. The outpatient treatment group actually had a lower rate of 30-day mortality or HF readmission than seen with usual-care inpatient treatment (17.5% vs 32.6%, P =0.02). Another larger observational study showed a similar association.
Medication dose adjustments are guided by daily laboratory testing for serum electrolytes, urea nitrogen, and creatinine concentrations, as well as careful monitoring of fluid intake and output, vital signs, standing body weight, clinical signs and symptoms of congestion, and hypoperfusion.
Residual congestion merits "careful consideration for further intervention before and after discharge, because [these patients] face higher risk for rehospitalization and death," note the 2022 American Heart Association guidelines .
Inotropic Support
While positive inotropes weren't shown to improve survival for hospitalized HF patients overall in the FIRST trial , their role in increasing cardiac output and improving hemodynamics gives short-term use a recommendation as "reasonable" for hospitalized patients with documented severe systolic dysfunction who present with low blood pressure and significantly low cardiac index.
"To minimize adverse effects, lower doses of parenteral inotropic drugs are preferred, although the development of tachyphylaxis should be acknowledged, and the choice of agent may need to be changed during longer periods of support," according to the HF guidelines. "Similarly, the ongoing need for inotropic support and the possibility of discontinuation should be regularly assessed."
In cases of cardiogenic shock, though, IV inotropes have a class 1 recommendation, followed by temporary mechanical circulatory support when that isn't enough to maintain end-organ function.
Despite limited evidence to guide use of IV inotropic agents, the guidelines point to "broad availability, ease of administration, and clinician familiarity favor such agents as the first therapeutic consideration when signs of organ hypoperfusion persist despite empiric volume replacement and vasopressors." Selection can be guided by blood pressure, concurrent arrhythmias, and availability.
Guideline-Directed Medical Therapy
"Hospitalization for HF is a sentinel event that signals worse prognosis and the need to restore hemodynamic compensation but also provides key opportunities to redirect the disease trajectory," the HF guidelines argue.
Central to that effort is optimization of guideline-directed medical therapy (GDMT).
Once diuresis is working, underutilized drugs can be initiated and doses uptitrated toward the target. The CHAMP registry and others have shown that few patients get target doses of GDMT in the community and more than 40% don't get medications prescribed anytime soon after hospitalization. The opportunity is particularly great for MRAs, which 67% of HF patients weren't on in the CHAMP data despite generic availability.
Thus, guidelines recommend not routinely stopping medications despite mild drops in renal function or asymptomatic blood pressure reduction in the hospital. Beta-blockers should be continued unless the patient is in shock. Any GDMT that is stopped during hospitalization due to clinical condition should be restarted and optimized "as soon as possible."
Electronic health record prompts from a virtual care team helped boost optimization of GDMT in the IMPLEMENT-HF trial .
Trials have pointed to outcome advantages to starting medications during HF hospitalizations. For example, the EMPULSE trial showed more than a 15 percentage point reduction in composite all-cause mortality, HF events, and HF symptoms with the SGLT2 inhibitor empagliflozin (Jardiance) started in the hospital.
The COACH trial showed that even for patients discharged from the emergency department, a strategy of protocolized nurse-led rapid outpatient follow-up reduced 30-day all-cause mortality or hospitalization for cardiovascular causes by a relative 12%.
"However, care and attention in both inpatient and outpatient settings need to go beyond stabilization and decongestion if we want to reduce readmissions for any cause," argued an editorial in the New England Journal of Medicine accompanying the COACH publication. "Strategies such as carefully reconciling medication lists to mitigate the risks associated with polypharmacy, improving nutritional status, providing supportive measures when cognitive impairment is present, recruiting services to promote physical function, and activating the social network, possibly augmented by home health care, are all crucial."
Read previous installments of this series:
Part 1: Heart Failure: A Look at Low Ejection Fraction
Part 2: Exploring Heart Failure With Preserved Ejection Fraction
Part 3: Heart Failure With Reduced Ejection Fraction: Diagnosis and Evaluation
Part 4: Case Study: Lightheadedness, Fatigue in Man With Hypertension
Part 5: Heart Failure With Preserved Ejection Fraction: Diagnosis and Evaluation
Part 6: Heart Failure Medical Management
Part 7: Managing Heart Failure Comorbidities
Part 8: Case Study: Heart Failure Exacerbation Due to an Often Overlooked Cause
Part 9: Device-Based Therapies for Heart Failure
- style-guide
HF Journey: New Style Statement In The Mask Era

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- PMC10889710

Inpatient vs. Outpatient: A Systematic Review of Information Needs throughout the Heart Failure Patient Journey
Lisa m. cotie.
1 KITE Research Institute, Toronto Rehabilitation Institute, University Health Network, Toronto, ON M4G 2V6, Canada; [email protected] (L.M.C.);
Maureen Pakosh
Gabriela lima de melo ghisi.
2 Department of Physical Therapy, Temerty Faculty of Medicine, University of Toronto, Toronto, ON M5S 3H2, Canada
Associated Data
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
The objective of this systematic review was to identify and describe information needs for individuals with heart failure (HF) throughout their patient journey. Six databases were searched (APA PsycINFO, CINAHL Ultimate, Embase, Emcare Nursing, Medline ALL, and Web of Science Core Collection) from inception to February 2023. Search strategies were developed utilizing the PICO framework. Potential studies of any methodological design were considered for inclusion through a snowball hand search. Data from the included articles were extracted by a reviewer, and the extraction accuracy was independently cross-checked by another author. Quality appraisal was assessed using the Mixed-Methods Appraisal Tool. A narrative synthesis was used to analyze all the outcomes according to the Synthesis Without Meta-analysis reporting guidelines. Twenty-five studies (15 quantitative and 10 qualitative) were included. Socioeconomic, cultural, and demographic factors influencing information needs were considered. The top three information needs for outpatients included general HF information, signs and symptoms and disease management strategies. For inpatients, medications, risk factors, and general HF were reported as the top needs. These divergent needs emphasize the importance of tailored education at different stages. Additionally, the review identified gaps in global representation, with limited studies from Africa and South America, underscoring the need for inclusive research. The findings caution against overgeneralization due to varied reporting methods. Practical implications call for culturally sensitive interventions to address nuanced HF patients’ needs, while future research must prioritize standardized reporting, consider diverse patient journey timepoints, and minimize biases for enhanced reliability and applicability.
1. Introduction
Heart failure (HF) is a medical condition characterized by the diminished ability of the heart to pump or fill with blood, resulting in a reduced cardiac output due to structural and/or functional abnormalities [ 1 ]. The global prevalence of HF in the general adult population ranges from 1 to 3%, a figure anticipated to rise with ongoing advancements in diagnostic methods and treatment modalities [ 1 ]. HF manifests in various phenotypes, such as HF with a preserved ejection fraction (HFpEF) and HF with a reduced ejection fraction (HFrEF) [ 2 ]. While improvements in treatments are expected to stabilize or decrease the prevalence of HFrEF, there is a steady increase in the occurrence of HFpEF [ 1 ]. The 5-year risk of HF-related mortality remains substantial, reaching approximately 75% [ 3 ]. The economic burden associated with HF is significant, with an estimated annual healthcare cost of around $36,000 CAD per patient in developed countries [ 1 ]. A substantial portion of these costs arise from inpatient care and the occurrence of rehospitalization [ 4 ].
Patient education has a pivotal role in the care of those living with HF [ 5 ]. Management programs for HF, incorporating education as a key element, prove successful in enhancing self-care practices, thereby leading to a decrease in hospital readmission rates [ 6 , 7 , 8 ]. Moreover, these programs have the potential to lower the likelihood of HF-related hospitalization by 20% [ 9 ]. A systematic review of 35 self-management education studies, involving 7413 congestive heart failure patients, demonstrated that structured educational interventions positively impacted disease-related knowledge, self-monitoring, medication adherence, time to hospitalization, and days spent in the hospital [ 10 ].
Educating HF patients before hospital discharge has been shown to reduce readmissions, assist with self-identification of problems earlier, and promote improved self-care [ 11 ]. These initiatives are particularly significant for individuals living with chronic HF, contributing to a minimized need for re-hospitalizations and an overall improvement in quality of life [ 12 ]. Addressing the challenge of hospital admissions and readmissions through improved self-management is crucial for the long-term well-being of HF patients [ 10 ]. It should be a primary focus for clinicians, researchers, and other healthcare stakeholders, aiming to alleviate the burden on the healthcare system while enhancing patient outcomes [ 2 ].
Research indicates a disparity in educational priorities between patients and their healthcare providers [ 13 ]. While both groups recognize the significance of information related to medications and signs and symptoms of HF, clinicians tend to assign greater importance to lifestyle factors, such as diet and weight management, compared to patients [ 14 ]. To bridge this gap, healthcare providers must gain a deeper understanding of the learning needs of HF patients and tailor education to be more patient-centered [ 14 , 15 ].
According to adult learning principles, it is crucial to recognize that adults learn best when the content is personally meaningful to them [ 16 ]. Therefore, understanding the specific information required from the patient’s perspective becomes paramount. Notably, it is essential to acknowledge the differences between patients admitted to the hospital with HF and those receiving outpatient care. Inpatients often present with more severe illness, multiple comorbidities, and higher event rates [ 17 ]. Consequently, the information needs of HF patients evolve throughout their healthcare journey, emphasizing the importance of adapting education to different phases of patient care. Hence, the objective of this systematic review was to identify and describe information needs for individuals living with HF throughout their patient journey. The findings from this review may offer valuable insights into structuring educational interventions that can effectively cater to the varied needs of HF patients, potentially adapting to different settings based on patients’ circumstances, whether in inpatient or outpatient care.
2. Materials and Methods
The reporting of this study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist [ 18 ]. This systematic review was prospectively registered at the Open Science Framework ( https://osf.io/k2egt/ (accessed on 4 October 2023)). Ethical review and approval were waived for this study because this is a systematic review that did not include participants.
2.1. Eligibility Criteria
This review included studies that examined the information requirements reported by individuals with HF, utilizing questionnaires tailored to assess information needs, qualitative data collected via interviews and focus groups, or any patient-reported outcome measures directly evaluating the information sought by HF patients. Information needs reported by family members, caregivers, and/or healthcare providers were not considered for this review. Studies using any methodological design were considered for inclusion in this review (i.e., quantitative, qualitative, and mixed methods). Additionally, narrative, systematic, and scoping reviews were examined as a possible source of additional primary studies. The selection criteria did not impose any restrictions based on language for studies to be eligible for inclusion.

2.2. Information Sources and Search Strategy
Six academic databases were searched, including APA PsycINFO, CINAHL Ultimate, Embase, Emcare Nursing, Medline ALL, and Web of Science Core Collection (Inception to 16 February 2023). The search strategies were developed in collaboration with an Information Specialist (MP) utilizing the PICO (i.e., Population, Intervention, Comparator, Outcome) framework, subject headings as appropriate for each database, and free-text terms relevant to the topical concepts. The full Medline search strategy is available in the Supplementary Material File S1 .
2.3. Selection Process, Data Collection Process and Data Items
Following the removal of duplicates in Covidence (Covidence systematic review software 2023, Veritas Health Innovation, Melbourne, Australia, available at www.covidence.org ), two independent reviewers (LMV and GLMG) screened titles and abstracts of all the records. Full texts of the remaining citations were then independently reviewed to determine whether they met the outlined eligibility criteria (LMC and GLMG). For all stages of the screening, if disagreements between the reviewers existed, consensus was achieved through discussion. The reviewers were not blinded to the authors or journals of the papers throughout the screening process.
One researcher (LMC) independently extracted all relevant data related to the study characteristics (authors, titles, year of publication, journal, country, language, study design, sample size), description of the population (i.e., diagnosis, nationality, sex, mean age/age range), stage of the HF journey (i.e., inpatient, outpatient), and relevant educational needs into an Excel spreadsheet. All extracted data were verified by a second researcher (GLMG). Discrepancies were resolved by consensus.
2.4. Quality Assessment
The quality of the articles was then assessed using the Mixed-Methods Appraisal Tool (MMAT) [ 19 ]. To use the MMAT, the study design (i.e., qualitative, quantitative RCT, quantitative non-randomized, quantitative descriptive, and mixed methods) of each included citation is determined and five criteria are assessed based on the type of study. Each of the five items is rated as present (yes), not present (no), or indeterminant (unable to tell) [ 19 ]. LMC and GLMG separately scored each included study and compared scores upon completion.
2.5. Synthesis Methods
The results were analyzed accordingly to the Synthesis Without Meta-analysis (SWiM) reporting guidelines [ 20 ]. A narrative synthesis was used to analyze all the outcomes that could not be meta-analyzed. Information needs were considered across the patient journey and ultimately were categorized into inpatient vs. outpatient needs. Only those identified as the primary needs (i.e., endorsed by the majority of participants, exceeding 50%) were incorporated into this review. Due to the nature of the data included in this review, a formal meta-analysis was not possible.
The initial database search yielded 55,301 records. After the initial and secondary screenings, a total of 51 full-text articles were assessed for eligibility. Overall, 25 studies were included in the review. This study selection process is illustrated in the PRISMA flow diagram ( Figure 1 ).

PRISMA flow diagram.
3.1. Characteristics of the Included Studies
Table 1 summarizes the characteristics of the 25 included studies, published between 1994 and 2022. Studies were conducted in Europe ( n = 8) [ 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 ], North America ( n = 7) [ 29 , 30 , 31 , 32 , 33 , 34 , 35 ], Asia ( n = 6) [ 14 , 36 , 37 , 38 , 39 , 40 ], Australia ( n = 3) [ 41 , 42 , 43 ], and Africa ( n = 1) [ 44 ]. Twenty three of the studies were published in English [ 14 , 21 , 22 , 23 , 24 , 25 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 ], one in French [ 26 ], and one in Italian [ 27 ]. In total, 56% percent of the studies included patients from an outpatient perspective [ 14 , 21 , 22 , 23 , 25 , 27 , 28 , 30 , 33 , 35 , 36 , 37 , 39 , 43 ], 32% of studies were from an inpatient perspective [ 26 , 29 , 31 , 32 , 34 , 38 , 40 , 42 ], and 12% of studies included both inpatient and outpatient stages of the patient journey [ 24 , 41 , 44 ]. Overall, 15 of the 25 studies had a quantitative descriptive design [ 14 , 21 , 22 , 23 , 28 , 29 , 30 , 31 , 32 , 34 , 36 , 37 , 38 , 40 , 41 ], while the remaining 10 were qualitative in nature [ 24 , 25 , 26 , 27 , 33 , 35 , 39 , 42 , 43 , 44 ].
Study characteristics.
* Mixed Methods Appraisal Tool.
The sample sizes of the included studies ranged from 10 [ 25 ] to 347 [ 38 ] (median = 50), with a total of 1687 heart failure patients across all studies. Fourteen studies provided information related to the New York Heart Association (NYHA) functional classification (I–IV) [ 14 , 22 , 24 , 28 , 29 , 34 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 44 ], which included participants from all classifications. Of the 1687 participants, 38% were women. Age was presented differently across studies, including range, mean ± SD, and percent above a specified cut-off. All age data can be found in Table 1 .
Table 1 also shows the quality appraisal of the included studies. In total, 10 of the 25 studies had “yes” responses for all five categories (i.e., score of 5/5, which indicates “good” quality) [ 14 , 24 , 27 , 34 , 35 , 37 , 38 , 40 , 42 , 44 ], 10 had one “no” or “can’t tell” responses [ 22 , 25 , 26 , 28 , 29 , 30 , 31 , 32 , 41 , 43 ] and the remaining 5 had two or more “no” or “can’t tell” responses out of five, indicating low quality [ 21 , 23 , 33 , 36 , 39 ]. No studies were excluded due to low quality.
In total, 11 [ 14 , 29 , 30 , 31 , 32 , 34 , 36 , 37 , 38 , 40 , 41 ] of the 25 included studies used a variety of adaptations of the cardiac patient learning needs inventory (CPLNI) [ 45 ] to measure patients HF learning needs. The CPLNI asks users to rank the importance, from 1 (not important) to 5 (very important) of having knowledge about 43 items categorized into 8 domains. These domains include general disease information, anatomy and physiology, psychological factors, risk factors, medication information, diet information, physical activity and other pertinent information. Ten studies used interviews or focus groups [ 24 , 25 , 26 , 27 , 33 , 35 , 39 , 42 , 43 , 44 ], four used questionnaires design specifically for the study (two used Likert scales, one multiple choice and one used a question prompt list) [ 21 , 23 , 26 , 43 ], and the remaining studies used other surveys [ 22 , 28 ].
3.2. Information Needs of Heart Failure Patients in Outpatient Settings
Fourteen of the twenty-five included studies had HF patients that were not admitted to hospital at the time of the study [ 14 , 21 , 22 , 23 , 25 , 27 , 28 , 30 , 33 , 35 , 36 , 37 , 39 , 43 ]. Among the various learning needs of these patients, the top three included general HF information (e.g., definition of HF, how it is diagnosed, prognosis), signs and symptoms, and disease management strategies. Specifically, 6 of the 14 “outpatient” studies listed general information related to HF [ 21 , 23 , 25 , 27 , 36 , 43 ] and signs and symptoms of HF [ 14 , 27 , 28 , 30 , 33 , 37 ] among the top three learning needs. Five of the studies listed various disease management strategies (i.e., behaviour/lifestyle, daily salt intake, fluid intake/weight management) as a top learning need rated by the patients [ 21 , 27 , 33 , 36 , 39 ]. Two studies focused on information needs specifically related to sexuality after HF diagnosis. Patients in these studies described information related to communication with their partner, relaxation and comfort in their relationship and sexual environment, and finally, the role of HF symptoms in and during sexual activity as the most important [ 22 , 28 ].
3.3. Information Needs of Heart Failure Patients in Inpatient Settings
Eight of the studies had patients admitted to the hospital at the time of data collection [ 26 , 29 , 31 , 32 , 34 , 38 , 40 , 42 ]. The top information needs reported in these studies were related to medications, risk factors, and general HF ( Table 2 ). Seventy-five percent of the studies had medication information in the top three learning needs of patients [ 26 , 29 , 31 , 32 , 34 , 42 ]. Fifty percent of the eight inpatient studies had general HF information [ 34 , 39 , 40 , 42 ] and risk factors [ 31 , 32 , 38 , 40 ] ranked as top learning needs.
Top 3 ranked information needs reported in the included studies ( n = 25).
HF: heart failure; NR: not reported.
Three studies included both in- and outpatients as participants [ 24 , 41 , 44 ]. Signs and symptoms of HF were amongst the highest ranked learning needs in two of the three studies [ 24 , 41 ], while prognosis [ 41 ], risk factors [ 41 ] and disease management (lifestyle changes) [ 44 ] were other important educational topics listed in these studies. The top information needs in outpatients and inpatients are illustrated as a word cloud in Figure 2 .

Top information needs in outpatients ( blue ) and inpatients ( pink ).
4. Discussion
This review identified 25 studies aimed at characterizing the information needs of individuals throughout their patient journey with HF. Employing a patient journey mapping approach [ 46 ], we categorized the outcomes to delineate information needs for both inpatients and outpatients. Patients in the outpatient stage prioritized general HF information, signs and symptoms, and disease management strategies as their top three information needs. Conversely, those in the inpatient stage of their HF journey highlighted information about medications, risk factors, and general HF information as their primary priorities. Three studies encompassed both in- and outpatients, identifying signs and symptoms of HF, prognosis, risk factors, and disease management (lifestyle changes) as crucial information needs. Additionally, two studies focused on information needs related to sexuality, revealing that patients emphasized communication with their partner, comfort in their relationship and environment, and the impact of sexual activity on their symptoms as top priorities.
It is unsurprising that individuals in the outpatient stage of HF prioritized general HF information, signs and symptoms, and disease management as their top informational needs. When patients are at home, without the constant care and assistance provided by hospital staff, the onus of managing their disease falls upon themselves [ 47 ]. Consequently, a crucial aspect of their self-management revolves around a comprehensive understanding of the signs and symptoms associated with HF, particularly those that may signify serious conditions leading to potential readmission to the hospital [ 48 ]. In terms of disease management, patients expressed a keen interest in obtaining information related to their daily salt and fluid intake. Additionally, they sought guidance on the significance of monitoring their daily body weight, which is aligned with practical management recommendations for this patient population [ 47 ]. This emphasis on disease management underscores the critical role patients play in their own care, necessitating a thorough comprehension of key aspects to enhance their ability to manage HF effectively within a home environment.
Interestingly, there was a notable trend in which information pertaining to physical activity restrictions, psychological factors, and general food intake ranked as the least important among study participants. It is crucial to highlight that cardiac rehabilitation (CR) stands as a class IA recommendation for HF patients [ 2 , 49 ], as its participation has been demonstrated to enhance functional capacity [ 50 , 51 ], improve quality of life [ 50 , 51 ], and significantly reduce the risk of hospital readmission [ 52 ], particularly for those with HFrEF [ 51 , 53 ]. Despite these well-established benefits, unfortunately, patients with HF are largely excluded from CR programs [ 54 ]. Regrettably, studies reveal a concerning gap in CR referrals for HF patients, with as few as one quarter of eligible individuals receiving such referrals upon discharge following hospitalization for HF and less than 5% of those referred ultimately participating in CR [ 55 ]. This dearth in referrals might elucidate why HF outpatients ranked information related to physical activity, psychological factors, dietary considerations beyond salt intake, as well as lifestyle factors like alcohol intake and smoking as low priorities in their informational needs. This underscores the need for increased awareness and integration of CR into the overall care plan for HF patients, considering its proven benefits for both functional outcomes and the reduction in hospital readmissions.
Individuals who were inpatients for these studies ranked information about medications, risk factors and general disease information as their highest learning needs. Specifically, inpatients displayed a keen interest in understanding the potential side effects of medications and how to address issues that might arise in connection with their medication regimen. This is important as studies have shown the implementation of guideline-directed medical therapy remains below optimal levels [ 56 ]. Research shows that clinicians consistently underscore the significance of medications as a crucial component of chronic disease management for individuals with HF [ 31 ]. Frequently, hospital readmissions and clinic visits are strategically scheduled around adjustments, additions, or removals to the medication regimen, aiming to better control symptoms [ 57 ]. It is possible that when patients receive information that directly influences their well-being, improves their symptoms, and reduces the likelihood of hospitalization, they exhibit a heightened motivation to retain such knowledge [ 31 ]. As patients prepare for discharge, understanding the risk factors that may exacerbate their condition becomes paramount [ 34 ]. Notably, individuals with HF who are inpatients generally exhibit a higher level of illness severity and experience higher event rates compared to their outpatient counterparts [ 17 ]. Consequently, the information needs for these distinct groups diverge, necessitating tailored educational approaches to address the unique challenges and requirements of inpatient and outpatient populations.
It is noteworthy to highlight that 21 of the 25 included studies were published before 2020. Assessing the information needs of patients in the current time period is of paramount importance, especially considering the significant changes that have occurred in the healthcare landscape with the advent of the COVID-19 pandemic [ 58 ]. The unprecedented challenges posed by the pandemic have introduced new dimensions to the healthcare system, impacting patients with HF who also contracted the COVID-19 virus. The coexistence of HF and COVID-19 may introduce pharmacological and symptomatic implications that need careful consideration in understanding the holistic needs of these patients [ 58 , 59 ]. Additionally, as knowledge and treatment options improve over time, understanding the needs of patients with respect to education is important to understand. Regularly updated data understanding the information needs of HF patients are necessary to ensure the most current information is shared with patients.
There are many factors related to HF that can influence sexuality, including pharmacological treatments, physiological aspects, and the broader psychological and emotional ramifications of receiving a diagnosis of HF [ 60 , 61 , 62 ]. Research indicates that over half of patients with HF encounter sexual challenges, ranging from difficulties to a complete cessation of sexual activity due to their diagnosis [ 22 , 28 ]. However, reassuringly, evidence suggests that despite a decline or cessation in sexual activity, there appears to be little to no impact on other aspects of relationships [ 22 ]. Historically, sexual counseling has been surrounded by stigma, perceived as shameful, embarrassing, and anxiety-provoking [ 63 , 64 ]. Additionally, the topic of sexuality is taboo in many cultures [ 63 , 65 , 66 ], necessitating a culturally sensitive approach when providing information to patients. The results from this systematic review highlight the need for sexual information by HF individuals. Research suggests that sexual information should be discussed at a variety of times through the patient journey and thus falls to the responsibility of the entire clinical team [ 22 , 28 ]. A better understanding of the specific information needs of HF patients can help guide these discussions [ 22 , 28 ].
When identifying the information needs of HF patients, it is crucial to take into account variables such as sex and gender, age, socioeconomic status, and cultural differences [ 5 ] Each of these factors is likely to exert a substantial influence on the unique information requirements of patients. Socioeconomic status, for example, can play a pivotal role in determining patients’ access to various treatment options, including pharmacotherapy and CR [ 67 ]. Cultural considerations are equally significant, encompassing the need to comprehend and adapt information related to food intake, treatment options, and sensitive topics such as sexuality and relationships [ 68 ]. Moreover, sex, gender, and age are important factors that may significantly shape the information needs of HF patients. Notably, four studies included in this review reported differences in information needs between men and women, underscoring the importance of considering these demographic variables in tailoring educational strategies [ 21 , 22 , 28 , 30 ].
The results from this review should be interpreted with caution. One notable limitation arises from the diverse methods employed to describe patient characteristics across the included studies. This variability in reporting hindered our ability to create a more nuanced and detailed mapping of the patient’s journey. While we presented results from the distinct inpatient and outpatient stages of the HF journey, it is essential to acknowledge that information needs may vary at other critical junctures in a patient’s trajectory, such as the time of diagnosis, during treatment (including device interventions), or in the context of end-of-life care. Future studies are needed—given that only four included studies are dated during or after 2020—and should endeavor to provide a more comprehensive understanding of information needs across each stage of the HF patient journey to capture potential changes over time. Another limitation stems from the geographical scope of the studies, with a notable absence of research conducted in certain regions of the world, particularly Africa and South America. Consequently, the generalizability of the results may be constrained, and caution should be exercised when applying these findings globally. Cultural differences may lead to differences in information needs between regions. A comprehensive understanding of information needs in HF necessitates a global perspective that considers the influence of cultural nuances and regional disparities.
Furthermore, it is important to recognize that our analysis was strictly descriptive, and a formal assessment of potential bias was not conducted.
In conclusion, this review offers valuable insights into the information needs of individuals navigating the complex journey of HF, and what clinicians must consider to ensure they understand patients’ information needs at each stage. The main information needs vary by different stages of HF, with patients in the outpatient stage prioritizing signs and symptoms and disease management strategies, while those in the inpatient stage prioritize information about medications and risk factors. Both groups are keen to learn general information about their condition, which highlights the need to include education throughout their patient journey. It is likely these differences are more granular than the outpatient vs. inpatient stages of the patient journey, and therefore it is the responsibility of clinicians to assess patient information needs multiple times throughout their HF journey. Providing important information to patients can help to decrease hospital readmissions, ultimately leading to better patient outcomes and decreased healthcare costs.
The findings of this review bear significant practical implications for healthcare providers, policymakers, and researchers. Firstly, the recognition of varied information needs throughout the HF journey underscores the importance of tailoring patient education interventions to meet specific requirements and enhance HF management. This personalized approach holds potential to enhance self-management, diminish hospital readmissions, and improve overall patient outcomes [ 69 , 70 ]. Additionally, the review underscores the importance of cultural sensitivity, highlighting the necessity for healthcare professionals to tailor information delivery to diverse cultural norms. Integrating sexual counseling and addressing taboos surrounding certain topics can foster a more supportive and patient-centered care environment. Moving forward, there is a need for discussions regarding future directions for improving HF management, considering implementation science studies and/or pragmatic trials to bridge the gap between guidelines and real-world practices.
The limited global representation in the current body of research signals a call for more inclusive studies. Understanding information needs across cultures and regions is essential for providing equitable care. Policymakers should advocate for and support research initiatives that span the globe, fostering a comprehensive understanding of HF patients’ information needs. In summary, the practical implications involve adopting a patient-centered, culturally sensitive, and globally inclusive approach to address the multifaceted information needs of heart failure patients. This, in turn, can lead to more effective healthcare strategies, improved patient outcomes, and a higher quality of life for individuals grappling with this chronic condition.
Acknowledgments
We would like to acknowledge Lais Vanzella for partially supporting the initial screening of records.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm13041085/s1 , File S1: Medline Search Strategy.
Funding Statement
This research received no external funding.
Author Contributions
Conceptualization: G.L.d.M.G.; Methodology: L.M.C. and G.L.d.M.G.; Formal Analysis: L.M.C. and G.L.d.M.G.; Resources: M.P.; Data Curation: L.M.C. and G.L.d.M.G.; Writing—Original Draft Preparation: L.M.C. and G.L.d.M.G.; Writing—Review and Editing: M.P. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Given the nature of this study as a systematic review, ethical review and approval were exempted. The study did not involve participants directly; rather, it systematically reviewed existing literature. As such, there were no interventions, interactions, or data collection from individual participants.
Informed Consent Statement
In the context of this systematic literature review, the need for patient consent is not applicable. Systematic reviews of literature involve the comprehensive examination and synthesis of findings from previously conducted studies, making patient consent unnecessary.
Data Availability Statement
Conflicts of interest.
The authors declare no conflicts of interest.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.

IMAGES
VIDEO
COMMENTS
ONE TREE FOR ONE FOOTWEAR. We plant one tree for every purchase of a footwear. Your step to better environment starts here. HF JOURNEY - Your journey to adventure starts here. Shop from a wide range of premium fashion products with unmatched style and comfort.
About us. About us - HF JOURNEY. Our Story. The beginning of a thousand miles starts with a single step. And thus our's began several years ago. It all started over a trip to a Volcano in the islands of Indonesia which led us to HFJourney materializing in 2020. As part of the Arrow family and with an experience of over 20 years, we're ...
Discover new-season women's sandals from HF Journey. Choose from strappy sandals, casual, smart, or summer sandals with heels for special occasions. Shop now!
HF JOURNEY - Your journey to adventure starts here. Shop from a wide range of premium fashion products with unmatched style and comfort.
HF Journey. 569 likes · 38 talking about this. An innovative combination of traditional and contemporary design techniques to make products that de
HF JOURNEY women's footwear is made of 100% real leather, ethically sourced from the food industry. All our footwear is crafted with passion, care, and atten...
Miles to go, my friend. Let us join your adventure! Together let's EXPLORE. FEEL. LIBERATE
The HF journey adversely impacts patient and caregiver physical, mental, and social well-being and can bring about fear, uncertainty, depression, anxiety, and isolation. Understanding and addressing the totality of these experiences is a first step to improving patients' and caregivers' symptom ramifications.
My HF Journey My hf state is 70% down ! My constipation and urine stream is like 100% ! Brain fog is far far better. I can easily kegal . I have some bloated belly but its way better . Now about erection quality. 100% okay !!! I took cialis 5 mg and the erection lasted 50 minutes in standing position. Before i took 15 mg cialis couldnt even ...
There's an issue and the page could not be loaded. Reload page. 3,577 Followers, 41 Following, 295 Posts - See Instagram photos and videos from HF JOURNEY (@hfjourney)
Shop genuine HF Journey collection at best offers online from Nykaa Fashion. Explore wide range of style & designs with convenience of COD and easy returns!
National HF hospitalization rates are on the rise, increasing from 4.4 per 1,000 U.S. adults in 2010 to 4.9 per 1,000 in 2017, according to a study of Nationwide Readmission Database trends ...
The HF journey's Hi-Gen mask, engineered seamlessly for high fashion trend, has four layers that offer protection along with comfort. The inner and outer layer fabric made of 100% cotton ensures ...
HF Journey Square Buckle Tan Leather Casual Sandal For Women|8197006||8197006| 5.0 out of 5 stars 1 ₹995 ...
3,655 Followers, 46 Following, 310 Posts - See Instagram photos and videos from HF JOURNEY (@hfjourney)
Buy HF Journey Solid Tan Sandal online at best prices on Nykaa Fashion. Uncover the perfect blend of style and savings & avail fast delivery with great offers.
HF Journey. Black Leather Casual Wear Sandals For Women |08179001| ₹1,745 ...
HF JOURNEY. Zeno Cam Casual wear Leather Sandal For Men|1222| 1.0 out of 5 stars 1 ₹3,290 ...
Consequently, the information needs of HF patients evolve throughout their healthcare journey, emphasizing the importance of adapting education to different phases of patient care. Hence, the objective of this systematic review was to identify and describe information needs for individuals living with HF throughout their patient journey.
HF Journey Videos, HEMA FOUNDATION