
Travel Vaccines and Advice for Malawi

Malawi promises an array of animal adventures and looks into lifestyles that are exclusive to this part of the world. Travelers eager to immerse themselves in an adventure unlike any other often set their sights on Malawi.
Malawi is home to ample culture and wildlife, making it the perfect stop for any tourists hoping to find a truly unique experience on their travels.
Do I Need Vaccines for Malawi?
Yes, some vaccines are recommended or required for Malawi. The CDC and WHO recommend the following vaccinations for Malawi: hepatitis A , hepatitis B , typhoid , cholera , yellow fever , rabies , meningitis , polio , measles, mumps and rubella (MMR) , Tdap (tetanus, diphtheria and pertussis) , chickenpox , shingles , pneumonia and influenza .
COVID-19 vaccination is recommended for travel to all regions, both foreign and domestic. Check with your local Passport Health clinic if immunization is offered in your area.
See the bullets below to learn more about some of these key immunizations:
- COVID-19 – Airborne & Direct Contact – Recommended for all unvaccinated individuals who qualify for vaccination
- Hepatitis A – Food & Water – Recommended for most travelers
- Hepatitis B – Blood & Body Fluids – Accelerated schedule available
- Typhoid – Food & Water – Shot lasts 2 years. Oral vaccine lasts 5 years, must be able to swallow pills. Oral doses must be kept in refrigerator.
- Cholera – Food & Water – Areas of active cholera transmission include: Blantyre, Dedza, Dowa, Karonga, Kasungu, Likoma, Lilongwe, Mulanje, Nkhatabay, Nsanje, Rumphi and Salima
- Yellow Fever – Mosquito – Required if traveling from a country where yellow fever is present.
- Rabies – Saliva of Infected Animals – High risk country. Vaccine recommended for long-term travelers and those who may come in contact with animals.
- Measles Mumps Rubella (MMR) – Various Vectors – Given to anyone unvaccinated and/or born after 1957. One time adult booster recommended.
- TDAP (Tetanus, Diphtheria & Pertussis) – Wounds & Airborne – Only one adult booster of pertussis required.
- Chickenpox – Direct Contact & Airborne – Given to those unvaccinated that did not have chickenpox.
- Shingles – Direct Contact – Vaccine can still be given if you have had shingles.
- Pneumonia – Airborne – Two vaccines given separately. All 65+ or immunocompromised should receive both.
- Influenza – Airborne – Vaccine components change annually.
- Meningitis – Airborne & Direct Contact – Given to anyone unvaccinated or at an increased risk, especially students.
- Polio – Food & Water – Considered a routine vaccination for most travel itineraries. Single adult booster recommended.
See the tables below for more information:
Malaria , dengue and chikungunya are all mosquito-borne infections found in Malawi. It is important to bring mosquito repellents and netting to prevent bites and potential spread. Antimalarials are recommended as well.
In all regions of Liberia, malaria is present. Antimalarial use is strongly recommended. Malaria is chloroquine-resistant in Liberia.
Rabies poses a risk to travelers to Malawi, especially if staying for a long period of time or visiting rural areas. Vaccination should be considered before traveling.
Visit our vaccinations page to learn more. Travel safely with Passport Health and schedule your appointment today by calling or book online now .
Is There Cholera in Malawi?
Cholera outbreaks in Malawi have been confirmed in the central region, southern region and in the northern districts of Karonga and Rumphi.
The best protection against cholera is through vaccination. Passport Health clinics offer the cholera vaccine. Book your cholera vaccination appointment today!
Do I Need a Visa or Passport for Malawi?
Americans planning to visit Malawi will need a visa to enter the country. There is also an exit fee of $30 for U.S. citizens.
Sources: Embassy of Malawi and U.S. State Department
The U.S. Department of State reports that you must declare all foreign currency when entering Malawi as well.
What is the Climate Like in Malawi?
Malawi is a country with sub-tropical climate. This means that the weather is warm and moderate almost all year round. The nation is also dry, and most of its precipitation occurs between November and April. Here is what to expect in a few tourist destinations:
- Lilongwe – The capital city of Malawi enjoys warm summers and milder winters. The high altitude of the city’s location actually keeps the temperatures a little lower, and more pleasant. Lilongwe sees most of its heavy rainfall from December to February and can be prone to downpours during this time.
- Blantyre – Temperatures in this city are considered tropical, it is often warm and sometimes humid. The area’s humidity is at its peak in October and November, the warm months right before the rainy season begins. The weather can also be misty and cool during the cold season in June and July.
- Mulanje – Temperatures also stay fairly warm throughout the year. Mount Mulanje itself experiences different weather patterns, as it cools the higher you climb. Weather on the mountain can also be sporadic, as mist and rainfall can cover Mount Mulanje. The area sees more precipitation around November, December and January.
How Safe is Malawi?
Crime in Malawi is fairly common. Armed residential break-ins are frequent, and break-ins in lodges and hotels have been reported. Robberies and pick-pocketing are also common street crimes.
Carjackings are prevalent in Lilongwe and Blantyre. This most often occurs when entering through a security gate into a home. Always keep doors locked and windows closed, and stay alert when entering or leaving.
Stay off the streets at night, particularly in urban areas. Armed assaults and muggings are becoming more prevalent. Foreigners are especially targeted in Lilongwe. Regardless of how many people you are with, city streets are not safe at night. It is also wise to exercise caution during the day. Make sure to arrange all your transportation in Malawi through your hotel or restaurant.
Be cautious when visiting or staying in isolated, lone areas such as Mount Mulanje. Public security in these areas is often limited. Be weary when visiting remote areas, and do not travel at night or alone.
While in Malawi, it is also crucial to stay alert for public demonstrations and civil disturbances. Avoid crowds, rallies and demonstrations, and always be aware of your surroundings.
Maneuvering Malawi’s Mount Mulanje
Avoid an embarrassing stop, over 70% of travelers will have diarrhea., get protected with passport health’s travelers’ diarrhea kit .
Adventurers and lovers of extreme sports consider Malawi an ideal travel destination. The nations’ terrain offers the perfect chance to test their skills.
One location that attracts hikers, bikers and rock climbers alike is Mount Mulanje. This mountain stands at over 3000 meters (or over 9800 feet) tall. It is a picturesque destination for those wishing to see its rolling green valleys and clear, flowing rivers. But, the mountain’s rugged terrain is what calls to risk-takers from all across the globe.
Even attempting to climb or hike Mount Mulanje if you are not prepared can lead to severe injury. If you plan to climb the mountain, never climb alone. Always have enough food and water, and bring essential equipment like maps, guidebooks and compasses. Stick together with your group and do not push into unknown territory.
There is limited public security at Mount Mulanje. Avoid traveling at night and never travel alone.
What Should I Pack for Malawi?
In addition to all travel documents and medications recommended by a Passport Health Travel Medicine Specialist, here are some items to consider packing:
- Insect Repellent – Since malaria is at risk in Malawi, you should always pack bug spray. Packing a repellent with at least 20%-30% DEET will keep mosquitoes away.
- Water Purifier – Cholera is spread primarily through contaminated water. Having a water purifiers or filter while in Malawi can prevent contact with dirty water. Having a water purifier helps ensure your safety and protects your health.
- Neutral-colored clothing – Wearing neutral clothing, such as beige and gray, prevents contact with mosquitoes. It can also prevent from drawing too much attention to yourself. Avoid bringing too many blue or black articles of clothing. These colors attract tsetse flies, which may carry African sleeping sickness.
- Conservative clothing options – In some areas of Malawi, particularly in some villages, it can be offensive to wear revealing clothing. Islamic areas in southern Malawi require conservative dress. Wearing shorts, small skirts, crop tops and tank tops can be considered rude in many areas in the country.
- Walking shoes – Many adventures in Malawi require you to be on your feet. Hiking and walking through reservations can be uncomfortable, if not dangerous, if you do not have the proper footwear.
U.S. Embassy to Malawi
All Americans visiting Malawi should register with the U.S. Embassy in Lilongwe. This will inform the office of your travel plans and will allow them to reach out in the case of an emergency or evacuation. You can register online, through the Smart Traveler Enrollment Program (STEP) .
U.S. Embassy Lilongwe Area 40, City Center 16 Jomo Kenyatta Road Lilongwe 3, Malawi Mailing Address: PO Box 30016 Lilongwe 3, Malawi Telephone: +(265) 1-773-166, 1-773-342 and 1-773-367 (Dial “0” before the “1” within Malawi) Emergency After-Hours Telephone: +(265) (0)882-960-178 or +265 (0)88 198 0814 Fax: +(265) 1-774-471 (Dial “0” before the “1” within Malawi)
Visit the U.S. Embassy website before your departure to confirm correct contact details for the U.S. Embassy in Malawi.
Ready to start your next journey? Call us at or book online now !
Customer Reviews
Passport health – travel vaccines for malawi.
On This Page: Do I Need Vaccines for Malawi? Is There Cholera in Malawi? Do I Need a Visa or Passport for Malawi? What is the Climate Like in Malawi? How Safe is Malawi? Maneuvering Malawi’s Mount Mulanje What Should I Pack To Malawi? U.S. Embassy to Malawi

- Records Requests
- Passport Health App
- Privacy Center
- Online Store
- Skip to main content
- Skip to "About this site"
Language selection
Search travel.gc.ca.
Help us to improve our website. Take our survey !
COVID-19: travel health notice for all travellers
Malawi travel advice
Latest updates: The Health section was updated - travel health information (Public Health Agency of Canada)
Last updated: April 17, 2024 11:55 ET
On this page
Safety and security, entry and exit requirements, laws and culture, natural disasters and climate, malawi - exercise a high degree of caution.
Exercise a high degree of caution in Malawi due to crime.
Back to top
Petty crime
Petty crime, such as pickpocketing and bag snatching occurs regularly.
Theft is frequent in:
- popular tourist areas including marketplaces and high-density residential areas
- main bus stations, especially in Lilongwe and Blantyre
- the ferry terminals for the Ilhla ferry
- restaurants, including patios located near streets
During your stay in Malawi:
- ensure that your personal belongings, including your passport and your other travel documents are secure at all times
- avoid carrying large sums of cash or unnecessary valuables
- avoid walking at night, either alone or with a group
- pay attention to your surroundings, particularly in crowded and tourist areas
Violent crime
Violent crime occurs, especially in Lilongwe and Blantyre. Incidents include:
- residential burglary
- armed robbery
There are further reports of travellers being targeted in the Mulanje district and facing intimidation and violence.
During your trip:
- always be aware of your surroundings
- always keep your car windows up and doors locked
- be vigilant if approached by strangers befriending you, offering assistance or to become your tour guide
- if you're robbed, hand over cash, electronic devices and valuables without resistance
Road safety
Road safety is poor throughout the country. Fatal vehicle accident rates are high, partly due to the lack of emergency health care availability.
Police rarely conduct road patrols. Hitchhiking and taking matola (informal lifts in the back of open vehicles) are considered dangerous.
Road conditions
Road conditions vary throughout the country. Highways are generally in good condition, but most roads don’t have road shoulders, leaving pedestrians, cyclists, and livestock to use roadways day and night.
Driving can also be dangerous due to:
- insufficient lighting
- unpaved roads
- poorly maintained and abandoned vehicles
Driving habits
Drivers don’t always respect traffic laws and have poor driving skills.
Drinking and driving and cell phone use while driving are common.
Roadside assistance is very limited.
If you choose to drive in Malawi:
- always drive defensively
- avoid driving at night
- plan your trip in advance, especially if you are visiting a rural area
- don't pick up hitchhikers
- ask about insurance coverage options for roadside assistance when you rent a vehicle
Roadblocks are common throughout the country.
You may be asked for identification.
- Make sure your ID documents are up to date
- Do not go through a checkpoint without stopping, even if it appears unattended
- If stopped, follow the instructions of police officers
Demonstrations
Even peaceful demonstrations can turn violent at any time. They can also lead to disruptions to traffic and public transportation.
- Avoid areas where demonstrations and large gatherings are taking place
- Follow the instructions of local authorities
- Monitor local media for information on ongoing demonstrations
Mass gatherings (large-scale events)
Fuel shortages
Fuel shortages occur frequently. This could lead to line-ups and gas stations and a reduction of essential services.
- Plan accordingly
- Keep a supply of fuel on hand
Tourist infrastructure
Tourist infrastructure is limited outside of major centres.
If you’re planning to travel to remote areas:
- plan your trip accordingly
- keep a supply of water, food and fuel on hand
- make sure you always have a complete emergency kit on hand
- bring a cell phone, charger and local emergency numbers
- use a reputable tour operator
Adventure tourism
Outdoor activities, such as kayaking, scuba diving, snorkelling, hiking, mountain biking, etc. and other adventure activities can be dangerous if unprepared. Trails are not always marked, and weather conditions can change rapidly, even during summer.
Tour operators may not always adhere to international safety standards.
If you intend to practice adventure tourism:
- never do so alone, and do not part with your tour companions
- contact the Mountain Club of Malawi for security advice before climbing Mount Mulanje
- obtain detailed information on your activity and on the environment in which you will be setting out
- buy travel insurance that includes helicopter rescue and medical evacuation
- ensure that your physical condition is good enough to tackle the challenges of your activity
- ensure that you’re adequately equipped and bring sufficient water
Wildlife viewing
Wildlife viewing poses risks, particularly on foot or at close range.
- Only use reputable and professional guides or tour operators
- Always maintain a safe distance when observing wildlife
- Only exit a vehicle when a professional guide or warden says it’s safe to do so
- Closely follow park regulations and warden’s advice
Spiked food and drinks
Never leave food or drinks unattended or in the care of strangers. Be wary of accepting snacks, beverages, gum or cigarettes from new acquaintances. These items may contain drugs that could put you at risk of sexual assault and robbery.
Women’s Safety
Women travelling alone may be subject to some forms of harassment and verbal abuse.
Advice for women travellers
Public transportation
Long-distance buses between big cities are generally safe but some operate with standing passengers. Public transport is limited in rural areas. Travel by minibus is not recommended, as the vehicles are overcrowded and poorly maintained.
Some ferries operating on Lake Malawi have poor safety measures. Don’t board a ferry that appears overloaded or unseaworthy.
We do not make assessments on the compliance of foreign domestic airlines with international safety standards.
Information about foreign domestic airlines
Every country or territory decides who can enter or exit through its borders. The Government of Canada cannot intervene on your behalf if you do not meet your destination’s entry or exit requirements.
We have obtained the information on this page from the Malawian authorities. It can, however, change at any time.
Verify this information with the Foreign Representatives in Canada .
Entry requirements vary depending on the type of passport you use for travel.
Before you travel, check with your transportation company about passport requirements. Its rules on passport validity may be more stringent than the country’s entry rules.
Regular Canadian passport
Your passport must be valid at least six months beyond the date you expect to leave Malawi and have a least 2 blank pages.
Passport for official travel
Different entry rules may apply.
Official travel
Passport with “X” gender identifier
While the Government of Canada issues passports with an “X” gender identifier, it cannot guarantee your entry or transit through other countries. You might face entry restrictions in countries that do not recognize the “X” gender identifier. Before you leave, check with the closest foreign representative for your destination.
Other travel documents
Different entry rules may apply when travelling with a temporary passport or an emergency travel document. Before you leave, check with the closest foreign representative for your destination.
Useful links
- Foreign Representatives in Canada
- Canadian passports
Tourist visa: not required for stays up to 30 days Business visa: not required for stays up to 30 days Student visa: required
If you wish to extend your stay in Malawi, contact the Department of Immigration and Citizenship of Malawi. You may be fined upon departure if you overstay the 30-day period without proper authorization.
Specific documents are required for Canadians volunteering in Malawi.
Visa information - Department of Immigration and Citizenship Services, Republic of Malawi
Children and travel
Learn more about travelling with children .
Yellow fever
Learn about potential entry requirements related to yellow fever (vaccines section).
Relevant Travel Health Notices
- Global Measles Notice - 13 March, 2024
- COVID-19 and International Travel - 13 March, 2024
- Polio: Advice for travellers - 17 April, 2024
This section contains information on possible health risks and restrictions regularly found or ongoing in the destination. Follow this advice to lower your risk of becoming ill while travelling. Not all risks are listed below.
Consult a health care professional or visit a travel health clinic preferably 6 weeks before you travel to get personalized health advice and recommendations.
Routine vaccines
Be sure that your routine vaccinations , as per your province or territory , are up-to-date before travelling, regardless of your destination.
Some of these vaccinations include measles-mumps-rubella (MMR), diphtheria, tetanus, pertussis, polio, varicella (chickenpox), influenza and others.
Pre-travel vaccines and medications
You may be at risk for preventable diseases while travelling in this destination. Talk to a travel health professional about which medications or vaccines may be right for you, based on your destination and itinerary.
Yellow fever is a disease caused by a flavivirus from the bite of an infected mosquito.
Travellers get vaccinated either because it is required to enter a country or because it is recommended for their protection.
- There is no risk of yellow fever in this country.
Country Entry Requirement*
- Proof of vaccination is required if you are coming from or have transited through an airport of a country where yellow fever occurs.
Recommendation
- Vaccination is not recommended.
- Discuss travel plans, activities, and destinations with a health care professional.
- Contact a designated Yellow Fever Vaccination Centre well in advance of your trip to arrange for vaccination.
About Yellow Fever
Yellow Fever Vaccination Centres in Canada * It is important to note that country entry requirements may not reflect your risk of yellow fever at your destination. It is recommended that you contact the nearest diplomatic or consular office of the destination(s) you will be visiting to verify any additional entry requirements.
There is a risk of hepatitis A in this destination. It is a disease of the liver. People can get hepatitis A if they ingest contaminated food or water, eat foods prepared by an infectious person, or if they have close physical contact (such as oral-anal sex) with an infectious person, although casual contact among people does not spread the virus.
Practise safe food and water precautions and wash your hands often. Vaccination is recommended for all travellers to areas where hepatitis A is present.
Measles is a highly contagious viral disease. It can spread quickly from person to person by direct contact and through droplets in the air.
Anyone who is not protected against measles is at risk of being infected with it when travelling internationally.
Regardless of where you are going, talk to a health care professional before travelling to make sure you are fully protected against measles.
Hepatitis B is a risk in every destination. It is a viral liver disease that is easily transmitted from one person to another through exposure to blood and body fluids containing the hepatitis B virus. Travellers who may be exposed to blood or other bodily fluids (e.g., through sexual contact, medical treatment, sharing needles, tattooing, acupuncture or occupational exposure) are at higher risk of getting hepatitis B.
Hepatitis B vaccination is recommended for all travellers. Prevent hepatitis B infection by practicing safe sex, only using new and sterile drug equipment, and only getting tattoos and piercings in settings that follow public health regulations and standards.
Coronavirus disease (COVID-19) is an infectious viral disease. It can spread from person to person by direct contact and through droplets in the air.
It is recommended that all eligible travellers complete a COVID-19 vaccine series along with any additional recommended doses in Canada before travelling. Evidence shows that vaccines are very effective at preventing severe illness, hospitalization and death from COVID-19. While vaccination provides better protection against serious illness, you may still be at risk of infection from the virus that causes COVID-19. Anyone who has not completed a vaccine series is at increased risk of being infected with the virus that causes COVID-19 and is at greater risk for severe disease when travelling internationally.
Before travelling, verify your destination’s COVID-19 vaccination entry/exit requirements. Regardless of where you are going, talk to a health care professional before travelling to make sure you are adequately protected against COVID-19.
The best way to protect yourself from seasonal influenza (flu) is to get vaccinated every year. Get the flu shot at least 2 weeks before travelling.
The flu occurs worldwide.
- In the Northern Hemisphere, the flu season usually runs from November to April.
- In the Southern Hemisphere, the flu season usually runs between April and October.
- In the tropics, there is flu activity year round.
The flu vaccine available in one hemisphere may only offer partial protection against the flu in the other hemisphere.
The flu virus spreads from person to person when they cough or sneeze or by touching objects and surfaces that have been contaminated with the virus. Clean your hands often and wear a mask if you have a fever or respiratory symptoms.
Malaria is a serious and sometimes fatal disease that is caused by parasites spread through the bites of mosquitoes.
Malaria is a risk to travellers to this destination. Antimalarial medication is recommended for most travellers to this destination and should be taken as recommended. Consult a health care professional or visit a travel health clinic before travelling to discuss your options. It is recommended to do this 6 weeks before travel, however, it is still a good idea any time before leaving. Protect yourself from mosquito bites at all times:
- Cover your skin and use an approved insect repellent on uncovered skin.
- Exclude mosquitoes from your living area with screening and/or closed, well-sealed doors and windows.
- Use insecticide-treated bed nets if mosquitoes cannot be excluded from your living area.
- Wear permethrin-treated clothing.
If you develop symptoms similar to malaria when you are travelling or up to a year after you return home, see a health care professional immediately. Tell them where you have been travelling or living.
In this destination, rabies is commonly carried by dogs and some wildlife, including bats. Rabies is a deadly disease that spreads to humans primarily through bites or scratches from an infected animal. While travelling, take precautions , including keeping your distance from animals (including free-roaming dogs), and closely supervising children.
If you are bitten or scratched by a dog or other animal while travelling, immediately wash the wound with soap and clean water and see a health care professional. In this destination, rabies treatment may be limited or may not be available, therefore you may need to return to Canada for treatment.
Before travel, discuss rabies vaccination with a health care professional. It may be recommended for travellers who are at high risk of exposure (e.g., occupational risk such as veterinarians and wildlife workers, children, adventure travellers and spelunkers, and others in close contact with animals).
Polio (poliomyelitis) is an infectious disease that can be prevented by vaccination. It is caused by poliovirus type 1, 2 or 3. Wild poliovirus (WPV1) and/or circulating vaccine-derived poliovirus (cVDPV1 or cVDPV3)) is/are present in this destination.
This destination is subject to Temporary Recommendations under the World Health Organization’s polio Public Health Emergency of International Concern (PHEIC) .
Polio is spread from person to person and through contaminated food and water. Infection with the polio virus can cause paralysis and death in individuals of any age who are not immune.
Recommendations:
- Be sure that your polio vaccinations are up to date before travelling. Polio is part of the routine vaccine schedule for children in Canada.
- One booster dose of the polio vaccine is recommended as an adult .
- Make sure that the polio vaccinations are documented on the International Certificate of Vaccination or Prophylaxis. This is the only document accepted as proof of vaccination. It is provided at Yellow Fever Vaccination Centres .
- Carry the certificate as proof of vaccination.
Proof of vaccination:
- Travellers who are visiting for longer than 4 weeks may be required to receive a dose of polio vaccine 1 to 12 months before they leave this destination. This may be required even if you have previously received all the recommended polio vaccine doses as part of the routine vaccine schedule in Canada.
- Make sure that the polio vaccination is documented on the International Certificate of Vaccination or Prophylaxis.
Safe food and water precautions
Many illnesses can be caused by eating food or drinking beverages contaminated by bacteria, parasites, toxins, or viruses, or by swimming or bathing in contaminated water.
- Learn more about food and water precautions to take to avoid getting sick by visiting our eat and drink safely abroad page. Remember: Boil it, cook it, peel it, or leave it!
- Avoid getting water into your eyes, mouth or nose when swimming or participating in activities in freshwater (streams, canals, lakes), particularly after flooding or heavy rain. Water may look clean but could still be polluted or contaminated.
- Avoid inhaling or swallowing water while bathing, showering, or swimming in pools or hot tubs.
Cholera is a risk in parts of this country. Most travellers are at very low risk.
To protect against cholera, all travellers should practise safe food and water precautions .
Travellers at higher risk of getting cholera include those:
- visiting, working or living in areas with limited access to safe food, water and proper sanitation
- visiting areas where outbreaks are occurring
Vaccination may be recommended for high-risk travellers, and should be discussed with a health care professional.
Travellers' diarrhea is the most common illness affecting travellers. It is spread from eating or drinking contaminated food or water.
Risk of developing travellers' diarrhea increases when travelling in regions with poor standards of hygiene and sanitation. Practise safe food and water precautions.
The most important treatment for travellers' diarrhea is rehydration (drinking lots of fluids). Carry oral rehydration salts when travelling.
Typhoid is a bacterial infection spread by contaminated food or water. Risk is higher among children, travellers going to rural areas, travellers visiting friends and relatives or those travelling for a long period of time.
Travellers visiting regions with a risk of typhoid, especially those exposed to places with poor sanitation, should speak to a health care professional about vaccination.
There is a risk of schistosomiasis in this destination. Schistosomiasis is a parasitic disease caused by tiny worms (blood flukes) which can be found in freshwater (lakes, rivers, ponds, and wetlands). The worms can break the skin, and their eggs can cause stomach pain, diarrhea, flu-like symptoms, or urinary problems. Schistosomiasis mostly affects underdeveloped and r ural communities, particularly agricultural and fishing communities.
Most travellers are at low risk. Travellers should avoid contact with untreated freshwater such as lakes, rivers, and ponds (e.g., swimming, bathing, wading, ingesting). There is no vaccine or medication available to prevent infection.
Insect bite prevention
Many diseases are spread by the bites of infected insects such as mosquitoes, ticks, fleas or flies. When travelling to areas where infected insects may be present:
- Use insect repellent (bug spray) on exposed skin
- Cover up with light-coloured, loose clothes made of tightly woven materials such as nylon or polyester
- Minimize exposure to insects
- Use mosquito netting when sleeping outdoors or in buildings that are not fully enclosed
To learn more about how you can reduce your risk of infection and disease caused by bites, both at home and abroad, visit our insect bite prevention page.
Find out what types of insects are present where you’re travelling, when they’re most active, and the symptoms of the diseases they spread.
There is a risk of chikungunya in this country. The risk may vary between regions of a country. Chikungunya is a virus spread through the bite of an infected mosquito. Chikungunya can cause a viral disease that typically causes fever and pain in the joints. In some cases, the joint pain can be severe and last for months or years.
Protect yourself from mosquito bites at all times. There is no vaccine available for chikungunya.
- In this country, risk of dengue is sporadic. It is a viral disease spread to humans by mosquito bites.
- Dengue can cause flu-like symptoms. In some cases, it can lead to severe dengue, which can be fatal.
- The level of risk of dengue changes seasonally, and varies from year to year. The level of risk also varies between regions in a country and can depend on the elevation in the region.
- Mosquitoes carrying dengue typically bite during the daytime, particularly around sunrise and sunset.
- Protect yourself from mosquito bites . There is no vaccine or medication that protects against dengue fever.
Onchocerciasis (river blindness) is an eye and skin disease caused by a parasite spread through the bite of an infected female blackfly. Onchocerciasis often leads to blindness if left untreated. Risk is generally low for most travellers. Protect yourself from blackfly bites, which are most common close to fast-flowing rivers and streams. There is no vaccine available for onchocerciasis although drug treatments exist.
African trypanosomiasis (sleeping sickness) is caused by a parasite spread through the bite of a tsetse fly. Tsetse flies usually bite during the day and the bites are usually painful. If untreated, the disease is eventually fatal. Risk is generally low for most travellers. Protect yourself from bites especially in game parks and rural areas. Avoid wearing bright or dark-coloured clothing as these colours attract tsetse flies. There is no vaccine available for this disease.
Animal precautions
Some infections, such as rabies and influenza, can be shared between humans and animals. Certain types of activities may increase your chance of contact with animals, such as travelling in rural or forested areas, camping, hiking, and visiting wet markets (places where live animals are slaughtered and sold) or caves.
Travellers are cautioned to avoid contact with animals, including dogs, livestock (pigs, cows), monkeys, snakes, rodents, birds, and bats, and to avoid eating undercooked wild game.
Closely supervise children, as they are more likely to come in contact with animals.
Anthrax is a serious infectious disease caused by bacteria. People can get sick with anthrax if they come into contact with infected animals or contaminated animal products. Anthrax can cause severe illness in both humans and animals. Travellers to areas where anthrax is common or where an outbreak is occurring in animals can get sick with anthrax if:
- they have contact with infected animal carcasses or eat meat from animals that were sick when slaughtered
- they handle animal parts, such as hides, wool or hair, or products made from those animal parts, such as animal hide drums.
If you are visiting these areas, do not eat raw or undercooked meat and avoid contact with livestock, wildlife, animal products, and animal carcasses.
Person-to-person infections
Stay home if you’re sick and practise proper cough and sneeze etiquette , which includes coughing or sneezing into a tissue or the bend of your arm, not your hand. Reduce your risk of colds, the flu and other illnesses by:
- washing your hands often
- avoiding or limiting the amount of time spent in closed spaces, crowded places, or at large-scale events (concerts, sporting events, rallies)
- avoiding close physical contact with people who may be showing symptoms of illness
Sexually transmitted infections (STIs) , HIV , and mpox are spread through blood and bodily fluids; use condoms, practise safe sex, and limit your number of sexual partners. Check with your local public health authority pre-travel to determine your eligibility for mpox vaccine.
Tuberculosis is an infection caused by bacteria and usually affects the lungs.
For most travellers the risk of tuberculosis is low.
Travellers who may be at high risk while travelling in regions with risk of tuberculosis should discuss pre- and post-travel options with a health care professional.
High-risk travellers include those visiting or working in prisons, refugee camps, homeless shelters, or hospitals, or travellers visiting friends and relatives.
HIV (Human Immunodeficiency Virus) is a virus that attacks and impairs the immune system, resulting in a chronic, progressive illness known as AIDS (Acquired Immunodeficiency Syndrome).
High risk activities include anything which puts you in contact with blood or body fluids, such as unprotected sex and exposure to unsterilized needles for medications or other substances (for example, steroids and drugs), tattooing, body-piercing or acupuncture.
Medical services and facilities
Medical facilities are available in rural and major urban centers. However, most lack supplies, medical equipment, and specialised personnel.
Medical evacuation may be required for serious conditions.
Cash payment is expected and may be required before any service is provided.
Make sure you get travel insurance that includes coverage for medical evacuation and hospital stays.
Travel health and safety
Some prescription medications may not be available in Malawi.
If you take prescription medications, you’re responsible for determining their legality in the country.
- Bring sufficient quantities of your medication with you
- Always keep your medication in the original container
- Pack them in your carry-on luggage
- Carry a copy of your prescriptions
Keep in Mind...
The decision to travel is the sole responsibility of the traveller. The traveller is also responsible for his or her own personal safety.
Be prepared. Do not expect medical services to be the same as in Canada. Pack a travel health kit , especially if you will be travelling away from major city centres.
You must abide by local laws.
Learn about what you should do and how we can help if you are arrested or detained abroad .
Penalties for possession, use or trafficking of illegal drugs are severe. Convicted offenders can expect heavy fines and a lengthy jail sentence.
Drugs, alcohol and travel
Photography
Photography of sensitive installations is prohibited. This includes:
- military sites
- government buildings
- places of worship
Seek permission before taking photos of individuals.
Imports and exports
It's illegal to import and export:
- pornographic material
You must have a licence to import firearms and munitions for hunting.
It’s illegal to purchase or export uncut precious stones.
2SLGBTQI+ travellers
Malawian law prohibits sexual acts between individuals of the same sex.
This law is currently suspended.
However, 2SLGBTQI+ persons could be discriminated against based on their sexual orientation, gender identity, gender expression, or sex characteristics.
2SLGBTQI+ persons should carefully consider the risks of travelling to Malawi.
Travel and your sexual orientation, gender identity, gender expression and sex characteristics
Dual citizenship
Dual citizenship is not legally recognized in Malawi.
If local authorities consider you a citizen of Malawi, they may refuse to grant you access to Canadian consular services. This will prevent us from providing you with those services.
Travellers with dual citizenship
International Child Abduction
The Hague Convention on the Civil Aspects of International Child Abduction is an international treaty. It can help parents with the return of children who have been removed to or retained in certain countries in violation of custody rights. It does not apply between Canada and Malawi.
If your child was wrongfully taken to, or is being held in Malawi by an abducting parent:
- act as quickly as you can
- consult a lawyer in Canada and in Malawi to explore all the legal options for the return of your child
- report the situation to the nearest Canadian government office abroad or to the Vulnerable Children’s Consular Unit at Global Affairs Canada by calling the Emergency Watch and Response Centre.
If your child was removed from a country other than Canada, consult a lawyer to determine if The Hague Convention applies.
Be aware that Canadian consular officials cannot interfere in private legal matters or in another country’s judicial affairs.
- International Child Abduction: A Guidebook for Left-Behind Parents
- Travelling with children
- Canadian embassies and consulates by destination
- Emergency Watch and Response Centre
Identification
Local authorities may request to see your passport and visa at any time.
- Always carry a photocopy of your passport including your visa
- Keep a photocopy of your passport in a safe place in case it’s lost or seized
- Keep a digital copy of your ID and travel documents
You should carry an international driving permit
International Driving Permit
Dress and behaviour
Malawi is generally a conservative society.
To avoid offending local sensitivities:
- dress conservatively
- behave discreetly and avoid public displays of affection
- respect religious and social traditions
The local currency is the Malawi kwacha (MWK). The economy is predominately cash based.
US dollars are widely accepted.
You must declare all foreign currencies upon arrival and departure in Malawi. Local authorities may detain you or confiscate your passport if you do not comply.
Ensure you carry enough currency, as credit and debit cards are not widely accepted outside tourist establishments.
Earthquakes
Malawi is located in a seismic zone. Although infrequent, earthquakes do occasionally occur and may cause landslides. Strong aftershocks are possible up to one week after the initial quake.
Rainy season
The rainy season extends from November to April.
Seasonal flooding can hamper overland travel and reduce the provision of essential services. Secondary roads may become impassable due to mudslides and landslides. Bridges, buildings, and infrastructure may be damaged.
- Monitor local media for the latest updates, including on road conditions
- Stay away from flooded areas
- Monitor weather reports
- Follow the instructions of local authorities, including evacuation orders
Local services
In case of emergency, dial:
- police: 997 / 990
- medical assistance: 998
- firefighters: 999
Consular assistance
Botswana, Malawi
For emergency consular assistance, call the Embassy of Canada to Zimbabwe, in Harare, and follow the instructions. At any time, you may also contact the Emergency Watch and Response Centre in Ottawa.
The decision to travel is your choice and you are responsible for your personal safety abroad. We take the safety and security of Canadians abroad very seriously and provide credible and timely information in our Travel Advice to enable you to make well-informed decisions regarding your travel abroad.
The content on this page is provided for information only. While we make every effort to give you correct information, it is provided on an "as is" basis without warranty of any kind, expressed or implied. The Government of Canada does not assume responsibility and will not be liable for any damages in connection to the information provided.
If you need consular assistance while abroad, we will make every effort to help you. However, there may be constraints that will limit the ability of the Government of Canada to provide services.
Learn more about consular services .
Risk Levels
take normal security precautions.
Take similar precautions to those you would take in Canada.
Exercise a high degree of caution
There are certain safety and security concerns or the situation could change quickly. Be very cautious at all times, monitor local media and follow the instructions of local authorities.
IMPORTANT: The two levels below are official Government of Canada Travel Advisories and are issued when the safety and security of Canadians travelling or living in the country or region may be at risk.
Avoid non-essential travel
Your safety and security could be at risk. You should think about your need to travel to this country, territory or region based on family or business requirements, knowledge of or familiarity with the region, and other factors. If you are already there, think about whether you really need to be there. If you do not need to be there, you should think about leaving.
Avoid all travel
You should not travel to this country, territory or region. Your personal safety and security are at great risk. If you are already there, you should think about leaving if it is safe to do so.
We’re sorry, this site is currently experiencing technical difficulties. Please try again in a few moments. Exception: request blocked
Cookies on GOV.UK
We use some essential cookies to make this website work.
We’d like to set additional cookies to understand how you use GOV.UK, remember your settings and improve government services.
We also use cookies set by other sites to help us deliver content from their services.
You have accepted additional cookies. You can change your cookie settings at any time.
You have rejected additional cookies. You can change your cookie settings at any time.
- Passports, travel and living abroad
- Travel abroad
- Foreign travel advice
Entry requirements
This advice reflects the UK government’s understanding of current rules for people travelling on a full ‘British citizen’ passport from the UK, for the most common types of travel.
The authorities in Malawi set and enforce entry rules. If you’re not sure how these requirements apply to you, contact the Malawi High Commission in the UK .
COVID-19 rules
There are no COVID-19 testing or vaccination requirements for travellers entering Malawi.
Passport validity requirements
Your passport must have an ‘expiry date’ at least 6 months after the day you arrive in Malawi.
Check with your travel provider that your passport and other travel documents meet requirements. Renew your passport if you need to.
You will be denied entry if you do not have a valid travel document or try to use a passport that has been reported lost or stolen.
Visa requirements
If you are travelling to Malawi for a visit of 30 days or less on a British passport you do not need a visa.
If you wish to live, work or study in Malawi, visit the Malawi Immigration website for further information.
Travelling with children from South Africa
If you’re travelling with children aged 17 and under and passing through South Africa, see what documents you need in South Africa travel advice .
Vaccination requirements
At least 8 weeks before your trip, check the vaccinations and certificates you need in TravelHealthPro’s Malawi guide .
Depending on your circumstances, these may include:
- a yellow fever vaccination certificate
- a polio vaccination certificate
Customs rules
There are strict rules about goods you can take into or out of Malawi . You must declare anything that may be prohibited or subject to tax or duty.
Related content
Is this page useful.
- Yes this page is useful
- No this page is not useful
Help us improve GOV.UK
Don’t include personal or financial information like your National Insurance number or credit card details.
To help us improve GOV.UK, we’d like to know more about your visit today. We’ll send you a link to a feedback form. It will take only 2 minutes to fill in. Don’t worry we won’t send you spam or share your email address with anyone.
- Travel Clinic
- Health Checks & Blood Tests
- Family Health
- Sexual Health
- Aesthetic Clinics
- Occupational Health
- Pricing List
- Login / Register
- Online Booking

Find a Clinic
- MK test Home
- Travel vaccinations >
Travel Vaccinations for Malawi
Vaccinations, certificate requirements.
Yellow fever vaccination certificate required for travellers aged 1 year or over arriving from countries with risk of yellow fever transmission and for travellers having transited for more than 12 hours through an airport of a country with risk of yellow fever transmission.
How much will it cost?
Recommended for all travellers.
The vaccines in this section are recommended for all travellers visiting the country.
If you have grown up in the UK, you have received a diphtheria vaccine as a part of your childhood vaccination schedule. Before going to Vietnam you should check whether you need a booster for diphtheria - this is the case if it has been over ten years since your last booster.
Hepatitis A is a viral infection which causes an inflammation of the liver. In countries where hep A is prominent, many people catch it as a child. The infection tends to be mild in children but can occasionally cause complications. In adults, however, it can lead to liver damage or even liver failure. Although infection rates appear to be on the decrease, hepatitis A is endemic to Sri Lanka and the vaccination is recommended for all travellers.
The tetanus vaccine - or a booster - is recommended for all travellers who are planning to visit a country where access to medical assistance may be limited. You can get tetanus when tetanus bacteria get into your bloodstream, usually due to injury or a wound. You need a booster if your last tetanus jab was over ten years ago.
Like hepatitis A and typhoid, cholera is a food- and waterborne disease and you need to practise good food hygiene to reduce your risk of cholera. The cholera vaccine may be relevant for travellers going to rural areas as well as areas with poor sanitation. Your nurse or pharmacist will assess your cholera risk based on where you’re travelling to as well as the activities you have planned and make a recommendation as to whether you should have the vaccine.
Why do I need a consultation?
It is difficult to say which vaccines you need without asking a medical professional. Your itinerary, your medical history and the activities you have planned all affect which vaccinations you need. It is important that a trained travel nurse or pharmacist checks what you need.
Exactly the travel vaccinations you need - no more, no less.
During your consultation, our nurse or pharmacist will talk you through the health risks at your travel destinations to check which vaccines you need. If a vaccine is not essential, we will explain your options so you can decide whether you would like to have it.
Malaria is a serious and sometimes fatal disease transmitted by mosquitoes. You cannot be vaccinated against malaria.
Malaria Precautions
- Malaria risk is high throughout the year in all areas.
- Malaria precautions are essential. Avoid mosquito bites by covering up with clothing such as long sleeves and long trousers especially after sunset, using insect repellents on exposed skin and, when necessary, sleeping under a mosquito net.
- Check with your doctor or nurse about suitable antimalarial tablets.
- See malaria map – additional information can be found by clicking on the Regional Information icon below the map.
- High risk areas: atovaquone/proguanil OR doxycycline OR mefloquine is usually advised.
- If you have been travelling in a malarious area and develop a fever seek medical attention promptly. Remember malaria can develop even up to one year after exposure.
- If travelling to an area remote from medical facilities, carrying standby emergency treatment for malaria may be considered.
Find your nearest clinic
Check which of our 60+ clinics is closest to you

View all clinics
How it works
1 book an appointment.
Book online or call our booking line. Our lines are open every day!
2 Attend Consultation
During your appointment, the nurse or pharmacist will assess which vaccines or medications you need.
3 Get your treatment
Once our health advisor has assessed your needs, you'll receive your vaccinations & treatments straight away.
How it Works
Book an appointment online, attend your consultation, get your treatment, what our customers think, popular destinations, south africa.
This website uses cookies to ensure you get the best experience on our website. Learn more

Information on how to stay safe and healthy abroad. About us.
- Destinations
- Asia (Central)
- Asia (East)
- Australasia & Pacific
- Central America
- Europe & Russia
- Middle East
- North America
- South America & Antarctica

Malawi (Africa)
Advice for all destinations.
Read the information on the COVID-19: Health Considerations for Travel page for advice on travelling during the COVID-19 pandemic.
Vaccinations and malaria risk
Review both the Vaccination and Malaria sections on this page to find out if you may need vaccines and/or a malaria risk assessment before you travel to this country.
If you think you require vaccines and/or malaria risk assessment, you should make an appointment with a travel health professional:
- How to make an appointment with a travel health professional
A travel health risk assessment is also advisable for some people, even when vaccines or malaria tablets are not required.
- Do I need a travel health risk assessment?
Risk prevention advice
Many of the health risks experienced by travellers cannot be prevented by vaccines and other measures need to be taken.
Always make sure you understand the wider risks at your destination and take precautions, including:
- food and water safety
- accident prevention
- avoiding insect bites
- preventing and treating animal bites
- respiratory hygiene
- hand hygiene
Our advice section gives detailed information on minimising specific health risks abroad:
- Travel Health Advice A-Z
Other health considerations
Make sure you have travel insurance before travel to cover healthcare abroad.
Find out if there are any restrictions you need to consider if you are travelling with medicines .
Know how to access healthcare at your destination: see the GOV.UK English speaking doctors and medical facilities: worldwide list
If you feel unwell on your return home from travelling abroad, always seek advice from a healthcare professional and let them know your travel history.
Vaccinations
- Confirm primary courses and boosters are up to date as recommended for life in Britain - including for example, seasonal flu vaccine (if indicated), MMR , vaccines required for occupational risk of exposure, lifestyle risks and underlying medical conditions.
- Courses or boosters usually advised: Diphtheria; Hepatitis A; Poliomyelitis; Tetanus.
- Other vaccines to consider: Hepatitis B; Rabies; Typhoid.
- Selectively advised vaccines - only for those individuals at highest risk: Cholera.
Yellow fever vaccination certificate required for travellers aged 1 year or over arriving from countries with risk of yellow fever transmission and for travellers having transited for more than 12 hours through an airport of a country with risk of yellow fever transmission.
Notes on the diseases mentioned above
Risk is higher during floods and after natural disasters, in areas with very poor sanitation and lack of clean drinking water.
- Diphtheria : spread person to person through respiratory droplets. Risk is higher if mixing with locals in poor, overcrowded living conditions.
Risk is higher where personal hygiene and sanitation is poor.
Risk is higher for long stays, frequent travel and for children (exposed through cuts and scratches), those who may require medical treatment during travel.
- Tetanus : spread through contamination of cuts, burns and wounds with tetanus spores. Spores are found in soil worldwide. A total of 5 doses of tetanus vaccine are recommended for life in the UK. Boosters are usually recommended in a country or situation where the correct treatment of an injury may not be readily available.
- Typhoid : spread mainly through consumption of contaminated food and drink. Risk is higher where access to adequate sanitation and safe water is limited.
Malaria is a serious and sometimes fatal disease transmitted by mosquitoes.You cannot be vaccinated against malaria.
Malaria precautions
- Malaria risk is high throughout the year in all areas.
- Malaria precautions are essential. Avoid mosquito bites by covering up with clothing such as long sleeves and long trousers especially after sunset, using insect repellents on exposed skin and, when necessary, sleeping under a mosquito net.
- Check with your doctor or nurse about suitable antimalarial tablets.
- See malaria map – additional information can be found by clicking on the Regional Information icon below the map.
- High risk areas: atovaquone/proguanil OR doxycycline OR mefloquine is usually advised.
- If you have been travelling in a malarious area and develop a fever seek medical attention promptly. Remember malaria can develop even up to one year after exposure.
- If travelling to an area remote from medical facilities, carrying standby emergency treatment for malaria may be considered.
Other Health Risks
Altitude and travel, schistosomiasis.
There is a risk of exposure to coronavirus (COVID-19) in this country.
Please be aware that the risk of COVID-19 in this country may change at short notice and also consider your risk of exposure in any transit countries and from travelling itself.
- The 'News' section on this page will advise if significant case increases or outbreaks have occurred in this country.
Prior to travel, you should:
- Check the latest government guidance on the FCDO Foreign travel advice and country specific pages for travel to this country and the rules for entering the UK on return.
- Ensure you are up to date with UK recommendations on COVID-19 vaccination.
- You can check this in the FAQ's.
- If you are at increased risk of severe COVID-19 you should carefully consider your travel plans and consider seeking medical advice prior to making any decisions.
For further information, see Coronavirus disease (COVID-19) and COVID-19: Health Considerations for Travel pages.
Polio Vaccination Exit Recommendations
If you are visiting this country for longer than 4 weeks, you may be advised to have a booster dose of a polio-containing vaccine if you have not had one in the past 12 months. You should carry proof of having had this vaccination. Please speak to a travel health professional to discuss.
- 65 additional items in the news archive for this country
back to top
Featured on

- What is a visa?
- Electronic Visa (eVisa)
- Visa on Arrival
- Appointment Required Visa
- Invitation Letter
- Arrival Card
- Passport Renewal
- Project Kosmos: Meet the man with the world's most challenging travel schedule
- Australia Visa and ETA requirements for US citizens explained
- Brazil eVisa for US citizens
- India Tourist Visa for UK citizens
- Possible B1/B2 Visa questions during the interview
Select Your Language
- Nederlandse
- 中文 (Zhōngwén), 汉语, 漢語
Select Your Currency
- AED United Arab Emirates Dirham
- AFN Afghan Afghani
- ALL Albanian Lek
- AMD Armenian Dram
- ANG Netherlands Antillean Guilder
- AOA Angolan Kwanza
- ARS Argentine Peso
- AUD Australian Dollar
- AWG Aruban Florin
- AZN Azerbaijani Manat
- BAM Bosnia-Herzegovina Convertible Mark
- BBD Barbadian Dollar
- BDT Bangladeshi Taka
- BGN Bulgarian Lev
- BIF Burundian Franc
- BMD Bermudan Dollar
- BND Brunei Dollar
- BOB Bolivian Boliviano
- BRL Brazilian Real
- BSD Bahamian Dollar
- BWP Botswanan Pula
- BZD Belize Dollar
- CAD Canadian Dollar
- CDF Congolese Franc
- CHF Swiss Franc
- CLP Chilean Peso
- CNY Chinese Yuan
- COP Colombian Peso
- CRC Costa Rican Colón
- CVE Cape Verdean Escudo
- CZK Czech Republic Koruna
- DJF Djiboutian Franc
- DKK Danish Krone
- DOP Dominican Peso
- DZD Algerian Dinar
- EGP Egyptian Pound
- ETB Ethiopian Birr
- FJD Fijian Dollar
- FKP Falkland Islands Pound
- GBP British Pound Sterling
- GEL Georgian Lari
- GIP Gibraltar Pound
- GMD Gambian Dalasi
- GNF Guinean Franc
- GTQ Guatemalan Quetzal
- GYD Guyanaese Dollar
- HKD Hong Kong Dollar
- HNL Honduran Lempira
- HTG Haitian Gourde
- HUF Hungarian Forint
- IDR Indonesian Rupiah
- ILS Israeli New Sheqel
- INR Indian Rupee
- ISK Icelandic Króna
- JMD Jamaican Dollar
- JPY Japanese Yen
- KES Kenyan Shilling
- KGS Kyrgystani Som
- KHR Cambodian Riel
- KMF Comorian Franc
- KRW South Korean Won
- KYD Cayman Islands Dollar
- KZT Kazakhstani Tenge
- LAK Laotian Kip
- LBP Lebanese Pound
- LKR Sri Lankan Rupee
- LRD Liberian Dollar
- LSL Lesotho Loti
- MAD Moroccan Dirham
- MDL Moldovan Leu
- MGA Malagasy Ariary
- MKD Macedonian Denar
- MNT Mongolian Tugrik
- MOP Macanese Pataca
- MUR Mauritian Rupee
- MVR Maldivian Rufiyaa
- MWK Malawian Kwacha
- MXN Mexican Peso
- MYR Malaysian Ringgit
- MZN Mozambican Metical
- NAD Namibian Dollar
- NGN Nigerian Naira
- NIO Nicaraguan Córdoba
- NOK Norwegian Krone
- NPR Nepalese Rupee
- NZD New Zealand Dollar
- OMR Omani Rial
- PAB Panamanian Balboa
- PEN Peruvian Nuevo Sol
- PGK Papua New Guinean Kina
- PHP Philippine Peso
- PKR Pakistani Rupee
- PLN Polish Zloty
- PYG Paraguayan Guarani
- QAR Qatari Rial
- RON Romanian Leu
- RSD Serbian Dinar
- RUB Russian Ruble
- RWF Rwandan Franc
- SAR Saudi Riyal
- SBD Solomon Islands Dollar
- SCR Seychellois Rupee
- SEK Swedish Krona
- SGD Singapore Dollar
- SHP Saint Helena Pound
- SLL Sierra Leonean Leone
- SOS Somali Shilling
- SRD Surinamese Dollar
- SVC Salvadoran Colón
- SZL Swazi Lilangeni
- THB Thai Baht
- TJS Tajikistani Somoni
- TOP Tongan Pa anga
- TRY Turkish Lira
- TTD Trinidad and Tobago Dollar
- TWD New Taiwan Dollar
- TZS Tanzanian Shilling
- UAH Ukrainian Hryvnia
- UGX Ugandan Shilling
- USD United States Dollar
- UYU Uruguayan Peso
- UZS Uzbekistan Som
- VND Vietnamese Dong
- VUV Vanuatu Vatu
- WST Samoan Tala
- XAF CFA Franc BEAC
- XCD East Caribbean Dollar
- XOF CFA Franc BCEAO
- XPF CFP Franc
- YER Yemeni Rial
- ZAR South African Rand
- ZMW Zambian Kwacha
We've updated our app!
Download it now
Malawi Vaccination Requirements: Do I need a vaccine to travel to Malawi?
Please note: All Covid-19 entry protocols have been removed.
Going to Malawi is a fantastic plan if you want to have a great time with your family or friends and start an adventure. To stay in the country, you will need some health requirements for your safety and the local’s safety. If you wonder about the Malawi Vaccination Requirements: Do I need a vaccine to travel to Malawi? Do not worry because iVisa.com will explain it to you.
Besides, you will also need other travel requirements that you must fulfill before your country’s departure. If you do not know which you will need based on your nationality, iVisa.com will help you with it, and you will also obtain it easily with us. You will not spend long hours completing a questionnaire, but you can complete it in just ten minutes from your sofa’s comfort. Try the Visa Checker tool .

Find out more about the Malawi Vaccination Requirements: Do I need a vaccine to travel to Malawi? in the following lines.
How to apply for a travel document with iVisa.com?
Follow the process below to get your travel documents easily with our services:
- Fill in the online form by offering your private information.
- Review all your answers to make sure that they're correct, then select your favored processing time and pay the appropriate fee.
- Upload and attach any document required , then click the submit button. The document will be sent to your inbox once approved and processed.
That's all! iVisa.com makes it simple for you.
Get started here .
Frequently Asked Questions
Do i need a vaccine to travel to malawi.
Yes, you will need to get some vaccines before you visit Malawi. To make it simple for you, we prepared the following vaccines that you must consider before your departure to Malawi.
- Chickenpox.
- Diphtheria.
You might also need other vaccines as well, but they are not mandatory to get. However, you should bear them in mind: Hepatitis A, Typhoid, and Malaria. We recommend you keep reading to find out more about other travel requirements and how you can get them with iVisa.com .
Apply right away with iVisa.com .
Do I need a COVID-19 vaccine to visit Malawi?
No, you don't. COVID vaccionations are not mandatory to enter Malawi at this time. Now, if you are a COVID vaccine certificate holder, you won't need to present a negative PCR test.
Since information may change quickly, we advise you to follow up on the latest Malawi travel updates and/or contact your local embassy.
Is it mandatory to present a negative result from a COVID-19 test to enter Malawi?
- COVID test prior to arrival: PCR within 72 hours, for unvaccinated travelers.
- COVID test exemptions: Fully vaccinated travelers and children under 12.
Do I have to self-isolate even if I have a negative result from the COVID-19 PCR Test?
- Quarantine requirements: There are no quarantine requirements in Malawi.
Can iVisa.com help me get my travel documents?
Yes, we can help you process most of the electronic documents required to enter Malawi. Click here to check the process and start the application.
Do I need other travel documents to visit Malawi?
Yes, you do. If you want to know which travel documents you will need to visit and stay in Malawi, we recommend using the iVisa.com website. You will also have the opportunity to get all you need for your trip with us while you avoid any tedious paperwork. Bear in mind the Malawi Vaccination Requirements: Do I need a vaccine to travel to Malawi? Before your departure.
Most of the time, we only ask you to have the following list of items:
- Email address.
- Payment options (debit/credit card) .
Start right away with iVisa.com! .
Can you speed up my process if I have an emergency?
Yes, we can help you with this! Please notice that the price you have to pay for the document will vary depending on how fast you want it. Here are your options:
- Standard Procedure: USD $111.99 - 10 days
- Rush Procedure: USD $149.99 - 9 days
- Super Rush Procedure: USD $204.99 - 7 days
Apply right now
Should I trust iVisa.com?
Yes, you should! iVisa.com is an excellent alternative to obtain the travel documents you need to visit Malawi. Our fantastic team will help you with most of the paperwork while completing the application form on our user-friendly platform. Still, have doubts about it? Do not hesitate and check the reviews section from our satisfied clients.
Apply right now and avoid all the paperwork with our help.
I have more doubts about it; how can I get in touch with you?
Feel free to reach our customer service agents who will clarify all your questions whenever you need answers about the Malawi Vaccination Requirements: Do I need a vaccine to travel to Malawi? We also suggest you take a look at the iVisa.com website to find different tools explaining a bit further about it.
Do not think twice and apply with iVisa.com .
iVisa.com Recommends
Malawi is a small country that is divided into northern, central, and southern areas. Northern Malawi is the smallest settlement in the country, with Mzuzu as the region’s capital. Central Malawi, on the other side, is one of the places that preserve different natural areas that you should visit. If you still have doubts about where to go, and how to reach there, we recommend you some places to start and know about it.
In Northern Malawi, you will find Chintheche, which is close to Lake Malawi’s, and you will have the opportunity to go to the beach there. In fact, you will love it because it will remind you that you are in the Caribbean. It has one of the clearest waters in the region, making it the perfect place to visit and relax in the meantime with your family and friends. The native people are the most welcoming, and you will feel right at home.
In Central Malawi, you will find five national parks that will make your travel experience even more exciting. You will love it. In fact, these are fascinating places to stay. Find out more at iVisa.com .
Related Articles

Malawi e-Visa for Citizens of Curaçao

Malawi e-Visa for Citizens of Yemen

Malawi e-Visa for Citizens of Western Sahara
- iVisa is NOT affiliated with any government agency. This site does not provide legal advice and we are not a law firm. None of our customer service representatives are lawyers and they also do not provide legal advice. We are a private, internet-based travel and immigration consultancy provider dedicated to helping individuals travel around the world. You may apply by yourself directly on the various government websites. The source of information: https://www.immigration.gov.mw/
Update April 12, 2024
Information for u.s. citizens in the middle east.
- Travel Advisories |
- Contact Us |
- MyTravelGov |
Find U.S. Embassies & Consulates
Travel.state.gov, congressional liaison, special issuance agency, u.s. passports, international travel, intercountry adoption, international parental child abduction, records and authentications, popular links, travel advisories, mytravelgov, stay connected, legal resources, legal information, info for u.s. law enforcement, replace or certify documents.
Share this page:
Malawi Travel Advisory
Travel advisory october 10, 2023, malawi - level 2: exercise increased caution.
Reissued with updates to civil unrest information.
Exercise increased caution in Malawi due to crime and civil unrest.
Country Summary: Violent Crime such as theft, burglary, armed robbery, assault, and carjacking is common. The capabilities of the Malawi Police Service are growing but its resources and abilities to deter and investigate crimes, assist victims, and apprehend criminals are limited.
Demonstrations may occur and increase in frequency around political issues and events such as elections. Teargas is frequently deployed at demonstrations and roads may be blocked.
Read the country information page for additional information on travel to Malawi.
If you decide to travel to Malawi:
- Avoid demonstrations and crowds.
- Monitor local media for breaking events and be prepared to adjust your plans.
- Keep travel documents up to date and easily accessible.
- Enroll in the Smart Traveler Enrollment Program ( STEP ) to receive security messages and make it easier to locate you in an emergency.
- Follow the Department of State on Facebook and Twitter .
- Review the Country Security Report for Malawi.
- U.S. citizens who travel abroad should always have a contingency plan for emergency situations. Review the Traveler’s Checklist .
- Visit the CDC page for the latest Travel Health Information related to your travel.
- U.S. citizens are reminded to avoid all gatherings, even peaceful ones, that could turn violent with little or no warning.
Travel Advisory Levels
Assistance for u.s. citizens, search for travel advisories, external link.
You are about to leave travel.state.gov for an external website that is not maintained by the U.S. Department of State.
Links to external websites are provided as a convenience and should not be construed as an endorsement by the U.S. Department of State of the views or products contained therein. If you wish to remain on travel.state.gov, click the "cancel" message.
You are about to visit:
Major step in malaria prevention as three West African countries roll out vaccine
Cotonou/Freetown/Monrovia — In a significant step forward for malaria prevention in Africa, three countries—Benin, Liberia and Sierra Leone—today launched a large-scale rollout of the life-saving malaria vaccine targeting millions of children across the three West African nations. The vaccine rollout, announced on World Malaria Day, seeks to further scale up vaccine deployment in the African region.
Today’s launch brings to eight the number of countries on the continent to offer the malaria vaccine as part of the childhood immunization programmes, extending access to more comprehensive malaria prevention. Several of the more than 30 countries in the African region that have expressed interest in the vaccine are scheduled to roll it out in the next year through support from Gavi, the Vaccine Alliance, as efforts continue to widen its deployment in the region in coordination with other prevention measures such as long-lasting insecticidal nets and seasonal malaria chemoprevention.
Benin, which received 215 900 doses, has added the malaria vaccine to its Expanded Programme on Immunization. The malaria vaccine should be provided in a schedule of 4 doses in children from around 5 months of age.
“The introduction of the malaria vaccine in the Expanded Programme on Immunization for our children is a major step forward in the fight against this scourge. I would like to reassure that the malaria vaccines are safe and effective and contribute to the protection of our children against this serious and fatal diseases,” said Prof Benjamin Hounkpatin, Minister of Health of Benin.
In Liberia, the vaccine was launched in the southern Rivercess County and will be rolled out afterwards in five other counties which have high malaria burden. At least 45 000 children are expected to benefit from the 112 000 doses of the available vaccine.
"For far too long, malaria has stolen the laughter and dreams of our children. But today, with this vaccine and the unwavering commitment of our communities, healthcare workers and our partners, including GAVI, UNICEF and WHO, we break the chain. We have a powerful tool that will protect them from this devastating illness and related deaths, ensuring their right to health and a brighter future. Let's end malaria in Liberia and pave the way for a healthier, more just society," said Dr Louise Kpoto, Liberia’s Minister of Health.
Two safe and effective vaccines — RTS,S and R21 — recommended by World Health Organization (WHO), are a breakthrough for child health and malaria control. A pilot malaria vaccine programme in Ghana, Kenya and Malawi reached over 2 million children from 2019 to 2023, showing a significant reduction in malaria illness and a 13% drop in overall child mortality and substantial reductions in hospitalizations.
In Sierra Leone, the first doses were administered to children at a health centre in Western Area Rural where the authorities kicked off the rollout of 550 000 vaccine doses. The vaccine will then be delivered in health facilities nationwide.
“With the new, safe and efficacious malaria vaccine, we now have an additional tool to fight this disease. In combination with insecticide-treated nets, effective diagnosis and treatment, and indoor spraying, no child should die from malaria infection,” said Dr Austin Demby, Minister of Health of Sierra Leone.
Malaria remains a huge health challenge in the African region, which is home to 11 countries that carry approximately 70% of the global burden of malaria. The region accounted for 94% of global malaria cases and 95% of all malaria deaths in 2022, according to the World Malaria Report 2023.
“The African region is advancing in the rollout of the malaria vaccine – a game-changer in our fight against this deadly disease,” said Dr Matshidiso Moeti, WHO Regional Director for Africa. “Working with our member states and partners, we’re supporting the ongoing efforts to save the lives of young children and lower the malaria burden in the region.”
Aurelia Nguyen, Chief Programme Officer at Gavi, the Vaccine Alliance, noted: “Today we celebrate more children gaining access to a new lifesaving tool to fight one of Africa’s deadliest diseases. This introduction of malaria vaccines into routine programmes in Benin, Liberia, and Sierra Leone alongside other proven interventions will help save lives and offer relief to families, communities and hard-pressed health systems.”
Progress against malaria has stalled in these high-burden African countries since 2017 due to factors including climate change, humanitarian crises, low access to and insufficient quality of health services, gender-related barriers, biological threats such as insecticide and drug resistance and global economic crises. Fragile health systems and critical gaps in data and surveillance have compounded the challenge.
To put malaria progress back on track, WHO recommends robust commitment to malaria responses at all levels, particularly in high-burden countries; greater domestic and international funding; science and data-driven malaria responses; urgent action on the health impacts of climate change; harnessing research and innovation; as well as strong partnerships for coordinated responses. WHO is also calling attention to addressing delays in malaria programme implementation.
Communications and marketing officer Tel: + 242 06 520 65 65 (WhatsApp) Email: boakyeagyemangc [at] who.int
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
- Section 2 - Interactions Between Travel Vaccines & Drugs
- Section 2 - Travelers’ Diarrhea
Yellow Fever Vaccine & Malaria Prevention Information, by Country
Cdc yellow book 2024.
Author(s): Mark Gershman, Rhett Stoney (Yellow Fever) Holly Biggs, Kathrine Tan (Malaria)
The following pages present country-specific information on yellow fever (YF) vaccine requirements and recommendations, and malaria transmission information and prevention recommendations. Country-specific maps are included to aid in interpreting the information. The information in this chapter was accurate at the time of publication; however, it is subject to change at any time due to changes in disease transmission or, in the case of YF, changing entry requirements for travelers. Updated information reflecting changes since publication can be found in the online version of this book and on the Centers for Disease Control and Prevention (CDC) Travelers’ Health website. Recommendations for prevention of other travel-associated illnesses can also be found on the CDC Travelers’ Health website .
Yellow Fever Vaccine
Entry requirements.
Entry requirements for proof of YF vaccination under the International Health Regulations (IHR) differ from CDC’s YF vaccination recommendations. Under the IHR, countries are permitted to establish YF vaccine entry requirements to prevent the importation and transmission of YF virus within their boundaries. Certain countries require proof of vaccination from travelers arriving from all countries ( Table 5-25 ); some countries require proof of vaccination only for travelers above a certain age coming from countries with risk for YF virus transmission. The World Health Organization (WHO) defines areas with risk for YF virus transmission as countries or areas where YF virus activity has been reported currently or in the past, and where vectors and animal reservoirs exist.
Unless issued a medical waiver by a yellow fever vaccine provider, travelers must comply with entry requirements for proof of vaccination against YF.
WHO publishes a list of YF vaccine country entry requirements and recommendations for international travelers approximately annually. But because entry requirements are subject to change at any time, health care professionals and travelers should refer to the online version of this book and the CDC Travelers’ Health website for any updates before departure.
CDC Recommendations
CDC’s YF vaccine recommendations are guidance intended to protect travelers from acquiring YF virus infections during international travel. These recommendations are based on a classification system for destination-specific risk for YF virus transmission: endemic, transitional, low potential for exposure, and no risk ( Table 2-08 ). CDC recommends YF vaccination for travel to areas classified as having endemic or transitional risk (Maps 5-10 and 5-11 ). Because of changes in YF virus circulation, however, recommendations can change; therefore, before departure, travelers and clinicians should check CDC’s destination pages for up-to-date YF vaccine information.
Duration of Protection
In 2015, the US Advisory Committee on Immunization Practices published a recommendation that 1 dose of YF vaccine provides long-lasting protection and is adequate for most travelers. The recommendation also identifies specific groups of travelers who should receive additional doses, and others for whom additional doses should be considered (see Sec. 5, Part 2, Ch. 26, Yellow Fever ). In July 2016, WHO officially amended the IHR to stipulate that a completed International Certificate of Vaccination or Prophylaxis is valid for the lifetime of the vaccinee, and YF vaccine booster doses are not necessary. Moreover, countries cannot require proof of revaccination (booster) against YF as a condition of entry, even if the traveler’s last vaccination was >10 years ago.
Ultimately, when deciding whether to vaccinate travelers, clinicians should take into account destination-specific risks for YF virus infection, and individual risk factors (e.g., age, immune status) for serious YF vaccine–associated adverse events, in the context of the entry requirements. See Sec. 5, Part 2, Ch. 26, Yellow Fever , for a full discussion of YF disease and vaccination guidance.
Table 2-08 Yellow fever (YF) vaccine recommendation categories 1
Malaria prevention.
The following recommendations to protect travelers from malaria were developed using the best available data from multiple sources. Countries are not required to submit malaria surveillance data to CDC. On an ongoing basis, CDC actively solicits data from multiple sources, including WHO (main and regional offices); national malaria control programs; international organizations; CDC overseas offices; US military; academic, research, and aid organizations; and the published scientific literature. The reliability and accuracy of those data are also assessed.
If the information is available, trends in malaria incidence and other data are considered in the context of malaria control activities within a given country or other mitigating factors (e.g., natural disasters, wars, the coronavirus disease 2019 pandemic) that can affect the ability to control malaria or accurately count and report it. Factors such as the volume of travel to that country and the number of acquired cases reported in the US surveillance system are also examined. In developing its recommendations, CDC considers areas within countries where malaria transmission occurs, substantial occurrences of antimalarial drug resistance, the proportions of species present, and the available malaria prophylaxis options.
Clinicians should use these recommendations in conjunction with an individual risk assessment and consider not only the destination but also the detailed itinerary, including specific cities, types of accommodations, season, and style of travel, as well as special health conditions (e.g., pregnancy). Several medications are available for malaria prophylaxis. When deciding which drug to use, consider the itinerary and length of trip, travelers’ previous adverse reactions to antimalarials, drug allergies, medical history, and drug costs. For a thorough discussion of malaria and guidance for prophylaxis, see Sec. 5, Part 3, Ch. 16, Malaria .
Entry requirements : Required for travelers ≥1 year old arriving from countries with risk for YF virus transmission; this includes >12-hour airport transits or layovers in countries with risk for YF virus transmission. 1
CDC recommendations : Not recommended
- Chloroquine
- P. falciparum (primarily)
- P. malariae , P. ovale , and P. vivax (less commonly)
- Atovaquone-proguanil, doxycycline, mefloquine, tafenoquine 3
Other Vaccines to Consider
See Health Information for Travelers to Malawi .
1 Current as of November 2022. This is an update of the 2010 map created by the Informal WHO Working Group on the Geographic Risk of Yellow Fever.
2 Refers to Plasmodium falciparum malaria, unless otherwise noted.
3 Tafenoquine can cause potentially life-threatening hemolysis in people with glucose-6-phosphate-dehydrogenase (G6PD) deficiency. Rule out G6PD deficiency with a quantitative laboratory test before prescribing tafenoquine to patients.
4 Mosquito avoidance includes applying topical mosquito repellant, sleeping under an insecticide-treated mosquito net, and wearing protective clothing (e.g., long pants and socks, long-sleeve shirt). For additional details on insect bite precautions, see Sec. 4, Ch. 6, Mosquitoes, Ticks & Other Arthropods.
5 Primaquine can cause potentially life-threatening hemolysis in people with G6PD deficiency. Rule out G6PD deficiency with a quantitative laboratory test before prescribing primaquine to patients.
6 P. knowlesi is a malaria species with a simian (macaque) host. Human cases have been reported from most countries in Southwest Asia and are associated with activities in forest or forest-fringe areas. P. knowlesi has no known resistance to antimalarials.
Yellow Fever Maps
2 In 2017, the Centers for Disease Control and Prevention (CDC) expanded its YF vaccination recommendations for travelers going to Brazil because of a large YF outbreak in multiple states in that country. Please refer to the CDC Travelers’ Health website for more information and updated recommendations.
3 YF vaccination is generally not recommended for travel to areas where the potential for YF virus exposure is low. Vaccination might be considered, however, for a small subset of travelers going to these areas who are at increased risk for exposure to YF virus due to prolonged travel, heavy exposure to mosquitoes, or inability to avoid mosquito bites. Factors to consider when deciding whether to vaccinate a traveler include destination-specific and travel-associated risks for YF virus infection; individual, underlying risk factors for having a serious YF vaccine–associated adverse event; and destination entry requirements.
The following authors contributed to the previous version of this chapter: Mark D. Gershman, Emily S. Jentes, Rhett J. Stoney (Yellow Fever) Kathrine R. Tan, Paul M. Arguin (Malaria)
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Open access
- Published: 17 April 2024
Factors associated with malaria vaccine uptake in Nsanje district, Malawi
- Atusaye J. Simbeye 1 ,
- Save Kumwenda 2 na1 ,
- Lauren M. Cohee 3 , 4 na1 ,
- Dickens Omondi 1 ,
- Peninah K. Masibo 5 ,
- Hesborn Wao 6 &
- Shehu S. Awandu 1 na1
Malaria Journal volume 23 , Article number: 105 ( 2024 ) Cite this article
684 Accesses
17 Altmetric
Metrics details
Malaria remains a significant global health burden affecting millions of people, children under 5 years and pregnant women being most vulnerable. In 2019, the World Health Organization (WHO) endorsed the introduction of RTS,S/AS01 malaria vaccine as Phase IV implementation evaluation in three countries: Malawi, Kenya and Ghana. Acceptability and factors influencing vaccination coverage in implementing areas is relatively unknown. In Malawi, only 60% of children were fully immunized with malaria vaccine in Nsanje district in 2021, which is below 80% WHO target. This study aimed at exploring factors influencing uptake of malaria vaccine and identify approaches to increase vaccination.
In a cross-sectional study conducted in April–May, 2023, 410 mothers/caregivers with children aged 24–36 months were selected by stratified random sampling and interviewed using a structured questionnaire. Vaccination data was collected from health passports, for those without health passports, data was collected using recall history. Regression analyses were used to test association between independent variables and full uptake of malaria vaccine.
Uptake of malaria vaccine was 90.5% for dose 1, but reduced to 87.6%, 69.5% and 41.2% for dose 2, 3, and 4 respectively. Children of caregivers with secondary or upper education and those who attended antenatal clinic four times or more had increased odds of full uptake of malaria vaccine [OR: 2.43, 95%CI 1.08–6.51 and OR: 1.89, 95%CI 1.18–3.02], respectively. Children who ever suffered side-effects following immunization and those who travelled long distances to reach the vaccination centre had reduced odds of full uptake of malaria vaccine [OR: 0.35, 95%CI 0.06–0.25 and OR: 0.30, 95%CI 0.03–0.39] respectively. Only 17% (n = 65) of mothers/caregivers knew the correct schedule for vaccination and 38.5% (n = 158) knew the correct number of doses a child was to receive.
Only RTS,S dose 1 and 2 uptake met WHO coverage targets. Mothers/caregivers had low level of information regarding malaria vaccine, especially on numbers of doses to be received and dosing schedule. The primary modifiable factor influencing vaccine uptake was mother/caregiver knowledge about the vaccine. Thus, to increase the uptake Nsanje District Health Directorate should strengthen communities’ education about malaria vaccine. Programmes to strengthen mother/caregiver knowledge should be included in scale-up of the vaccine in Malawi and across sub-Saharan Africa.
Malaria continues to pose a significant global health challenge. Globally, an estimated 249 million cases of malaria occurred in year 2022 which was 2 million more cases than in 2021 [ 1 ]. Sub-Saharan African countries facing the hardest hit contributing 93.6% (233 million) of total malaria cases and 95.4% (580,000) of total malaria deaths [ 1 ]. In Africa, about 78.1% (453,000) of the total deaths in 2022 were children below 5 years [ 1 ]. Malawi is among the 15 countries with the highest burden of malaria reporting over 4 million estimated malaria cases were reported in 2022 [ 1 ].
To control malaria, the National Malaria Control Programme (NMCP) within the Malawi Ministry of Health (MOH) currently supports the following interventions: long-lasting insecticidal nets (LLINs), prompt diagnosis with effective treatment with artemisinin-based combination therapy (ACT), and indoor residual spraying (IRS). The RTS,S/AS01 malaria vaccine is a new addition to malaria control tools [ 2 ]. In 2021, the World Health Organization (WHO) recommended RTS,S/AS01 for children at risk of malaria in sub-Saharan African regions of moderate to high malaria transmission [ 3 ]. The successful deployment of a malaria vaccine could substantially reduce the burden of malaria-related morbidity and mortality in under five children 4 , 5 , 6 . However, vaccines cannot achieve their anticipated benefits if the uptake is low. It is estimated that 1 out of every 5 children do not receive basic vaccines which contributes to more than 30 million under five years children suffering from Vaccine Preventable Disease (VPDs) each year [ 5 ]. For instance, the 2023 measles outbreak in South Africa was caused due to low coverage of measles vaccine [ 7 ]. Similarly, there was an outbreak of Polio in Cameroon due to low coverage of Oral Polio Vaccine (OPV) [ 8 ], low vaccine coverage has contributed to infectious disease outbreaks in vulnerable population [ 9 ]. Vaccine hesitancy also contributes to low vaccination coverage in many Africa countries [ 10 ].
In 2019, a Phase IV implementation study of the RTS,S/AS01 vaccine delivered through routine EPI platforms was conducted in Malawi. The four required doses of malaria vaccine were delivered at 5, 6, 7, and 22 months. The implementation study took place in 11 districts, including Nsanje. The effectiveness and impact of malaria vaccine relies not only on its introduction to the country but also on its widespread acceptance and uptake. This research study aimed to quantify the uptake of malaria vaccine in Nsanje district and investigate the factors associated with malaria vaccine uptake, including sociodemographic, mother/caregiver-related factors, and health care system factors. Identification of these factors may help to develop approaches to accelerate high levels of uptake of malaria vaccines, thereby advancing the global agenda towards malaria eradication.
All the 4 contacts for malaria vaccine are new and are not given with any other EPI interventions (Table 1 ). The only other vaccine that is given in the second year of life is measles and rubella vaccine dose 2, which is given at 15 months.
According to the WHO, it is recommended that the first dose of RTS,S vaccine should be received at 5 months, with the successive doses being received at 1 month apart and the 4th dose to be received at 15–18 months after the third dose. However, the WHO also states that vaccination programmes may choose to give the first dose at a later or slightly earlier age based on operational considerations. At 11 months, is the latest month a child can receive the first dose of malaria vaccine and at 36 months is the latest month for a child to receive dose 4.
Nsanje district is located in the southern region of Malawi. It is situated at the tip of the country along latitude 16°45′00″S and longitude 35°10′00″E. The district is a flatland in the lower Shire valley covering 1,942 square kilometres with an estimated population of 299,168 11 , 12 .The district has 23 health facilities (3 hospitals, 12 health centres and 8 health posts) which are divided into five clusters for health administration purposes. The malaria vaccine was implemented in four out of the five clusters. This study was conducted in the catchment areas of health facilities within each implementation cluster: Mlolo cluster (Mlolo, Trinity, Masenjere, Makhanga, Sankhulani and Mchacha), Kalemba cluster (Kalemba, Phokera, Sorgin, Misamvu, Kanyimbi), Tengani cluster (Tengani, Nyamithuthu and Mkango) and Boma cluster (Nsanje district Hospital and Chididi) [ 12 ]. Cluster sampling was performed.
Study design
This was a cross-sectional study utilizing structured questionnaires together with checklists to collect data on the uptake of malaria vaccine and factors that influence uptake. Data on child vaccination status were obtained by reviewing their health passport. Mothers/caregivers were asked demographic questions about themselves and their children and also about factors that were associated with the uptake of the malaria vaccine.
Study population
In February 2023, names of the mothers/caregivers of children 24–36 months old were extracted from village registers with the help of Health Surveillance Assistants. Children in this age group were eligible to have received all four doses of the vaccine. After all the names were extracted from the village registers, the participants were selected using stratified random sampling. Mothers/caregivers of the selected children were contacted and eligibility assessment was conducted. The eligibility criteria were: a mother/caregiver responsible for the selected child aged 24–36 months by the time of data collection, and the child was a permanent resident of Nsanje district by birth.
Sample size calculation
Using Cochrane’s formula to estimate proportion of children receiving vaccine (prior estimate of dose 4 = 60%) with a margin of error of 5% assuming a normal distribution of the margin of error, the minimum sample was calculated to be 369 participants. After adjustment for a 10% non-response rate and rounding the target sample size was 410.
The total population in the four target clusters is 245,620 including an estimated 12,281 mothers/caregivers. Stratified sampling technique proportionate to size of the cluster population was used in selecting participants for the study. Table 2 shows the sample proportions.
Sampling individual participants
To sample individual respondents in this study, firstly, systematic sampling technique was used to selected respondents from each sub-cluster. The Village Health Registers were used as source of the names for mothers/caregivers. The names of all mothers/caregivers who met the eligibility criteria in each cluster were numbered and written down, thus forming the sampling frame. A formula was used to determine a sampling interval from each cluster. The formula that was used was i = N/n where i was the sampling interval, N was the total number of eligible mothers/caregivers in the sampling frame whereas n was sample size of the cluster. The names and the villages of the mothers/caregivers counting from one to the sampling frame were written on a piece of paper, folded, mixed thoroughly and put in a box then a simple random sampling technique was used to select the first sample. After the first sample was drawn, the initial list that was written down was used to select the subsequent participant. The subsequent participants were selected by adding the sampling interval to the number of the initial sample until the required samples were drawn for that cluster.
Data collection
Questionnaires were administered by research assistants to the study participants. Questions included mothers/caregiver socio-demographic characteristics, child factors (e.g. history of vaccine adverse reactions), community level factors and health care system factors. Information on vaccine uptake and timeliness was extracted from the health passport of the child. For mothers/caregivers who did not have health passports for the children, data was recorded using recall history. The questions were adopted from previous validated questionnaires used in Malaria Indicator surveys and Demographic and Health surveys. Mothers/caregivers were contacted in their homes depending on when they were available to respond to the questionnaire; interviews were not conducted at health facilities or at the vaccination point. Ethical approval was obtained from Jaramogi Oginga Odinga University of Science and Technology, approval number ERC 37/04/23-5/05 and from Malawi National Health Sciences Research Committee, protocol number 23/02/3167. Informed consent was sought from each study participant.
Data analysis
Data from paper-based questionnaires were entered in Microsoft Excel by a single study team member. A second team member double-checked data entry by comparing the questionnaires and the data entered in Microsoft Excel. The cleaned data set was imported to STATA version 16 for analysis. Descriptive statistics were calculated for binary, categorical, and continuous variables. Logistic regression was used to evaluate the association between the independent variables (for example socio-demographic) and the level of malaria vaccine uptake (dependent variable). Malaria vaccine uptake was divided into three categories: no uptake (child has not received any dose of malaria vaccine), partial uptake (child has received first, second or third dose) and full uptake (child has received all four doses). After the univariate analysis, a multivariate analysis was performed on those independent variables with significant p-values of 0.05 in the first stage. The binary regression involved the comparing between full malaria vaccine uptake against partial uptake and no uptake. Final model selection was based on having the lowest Akaike’s Information Criteria (AIC).
Socio-demographics characteristics of mothers/caregiver and their children
A total of 410 mothers/caregivers with children aged 24 to 36 months participated in this study. Participants were most commonly married females (79.8%, n = 327) who were 20–29 years old (54.2%, n = 222), self-employed (58.8%, n = 241), Christians (95.1%, n = 390), and were most often parents as opposed to caregivers (Table 3 ). Education level varied with more than half having no formal education (22%, n = 90) or only primary school (36%, n = 149). Most had at least four antenatal care visits during pregnancy (56.2%, n = 168). Out of the 410 participants, 82.4% (338) had their children’s health passports present whereas 17.6% (72) had no health passports for their children. The median age of the children whose data was collected was 29 months (IQR 26–33), half were male, and almost all were delivered at a health facility (98.8%, n = 405) (Table 4 ).
Uptake of malaria vaccine
The crude uptake was used for this study (vaccinations from health passport plus mothers/caregivers recall). Out of the 410 children, 9.5% of children did not receive any doses of the malaria vaccine. Among those who received the vaccine, coverage was relatively high for dose 1 and 2 (90.5% and 87.6%, respectively), but declined for dose 3 and 4 (69.5% and 41.2%, respectively) (Fig. 1 ). Thus, the levels of malaria vaccine uptake were 9.5% (n = 39) for no uptake , 49.3% (n = 202) for partial uptake and full uptake 41.2% (n = 169) (Table 5 ). Children of the 72 mothers/caregivers who had no health passports of their children had the following levels of uptake of malaria vaccine (no uptake, 33.3%, n = 24), while 40.3% (n = 29) had partial uptake, and 26.4% (n = 19) had taken all the doses of malaria vaccine (full uptake).
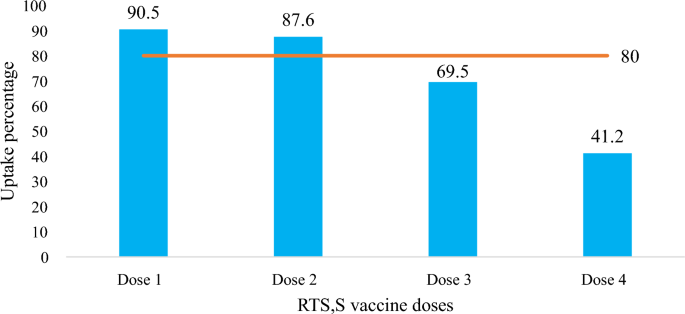
Uptake of malaria vaccine among children aged 24–36 months in Nsanje district. Blue bars: uptake (%), Orange bar: recommended target
Reasons for incomplete vaccination
Among the 39 participants whose child did not receive any dose of malaria vaccine, 26 (67%) did not know their child was eligible, nine (23%) said their religious belief prohibited them from taking the vaccine, and four (10.3%) made a personal decision to refuse the vaccine. Out of the 202 participants who had partial uptake of the vaccine, 70.4% did not know the next date when the vaccination was due and 15 (4%) were not comfortable with issues surrounding vaccines. In total 28 participants reported vaccine hesitancy with their reasons being complete refusal (n = 4), religious reasons (n = 9) and not comfortable with issues surrounding vaccine (n = 15) leading to no or partial uptake (Table 6 ).
Mother/caregiver and child characteristics associated with vaccine uptake
Mothers/caregivers who had secondary or higher education had increased odds of having full uptake of malaria vaccine compared to their counterparts (OR = 2.43, 95% CI 1.43–4.12, p = 0.001). Having attended four or more antenatal visits was associated with full uptake of malaria vaccine (OR = 1.89, 95% CI 1.18–3.02, p = 0.008). However, there was no statistically significant association between sex, religion, occupation of the mother/caregiver and full uptake of malaria vaccine. Children aged 32 to 36 months had increased odds of full malaria vaccine uptake compared to those aged 24 to 27 months (OR = 1.72, 95% CI 1.11–2.69, p = 0.008) whereas sex and place of delivery was not statistically associated.
General knowledge about the malaria vaccine was associated with increased vaccination rates; mothers/caregivers who had heard about malaria vaccine prior this study had increased odds of full malaria vaccine uptake compared to those who never heard about it (OR = 4.47, 95%CI 1.29–15.41). Those who received messaging about the malaria vaccine from under 5 clinic had increased odds to having full malaria vaccine uptake compare to those who learned about the vaccine from the radio (OR = 3.15, 95% CI 1.22–8.11, p = 0.018). However, detailed knowledge about the vaccine, for example, knowing the number of malaria doses to be received and the specific age at which those doses should be received, was not associated with full uptake of malaria vaccine.
Children who ever suffered side effects following immunization were associated with reduction in full uptake of malaria vaccine (OR = 0.36, 95% CI 0.24–0.54, p < 0.001).
Mode of transport was associated with full uptake of malaria vaccine. Those mothers/caregivers who used motorbikes/bikes to go the vaccination point had increased odds (OR = 2.79, 95% CI 1.50–5.18, p = 0.001).
Having heard negative rumours about the malaria vaccine, for example that children were being used for experiments or that the vaccine will affect child development, reduced the odds of full uptake by 25% (OR = 0.25, 95% CI 0.14–044, p ≤ 0.001). Mothers/caregiver who had no problem with the introduction of malaria vaccine had increased odds to full uptake of the vaccine (OR = 3.47, 95% CI 1.29–9.39, p = 0.014).
Multivariate analysis of associations between full uptake of malaria vaccine and mother/caregiver and child factors
Multivariate logistic regression showed that the odds of malaria vaccine uptake was 26.56 times to those who ever heard of malaria vaccine than those who did not. Further, it showered that distance to vaccination point reduced the odds of full uptake by 24% whereas child ever suffered side effects following immunization reduced the odds by 23%. Table 7 below shows the details of multivariate logistic regression.
This study found that only the uptake of the first and the second doses of the RTS,S malaria vaccine met target of coverage for childhood vaccines set by the WHO [ 13 ]. Coverage for the subsequent doses fell below the target with the 4th dose reaching few than half of eligible children. This result means that the malaria vaccine cannot meet its intended purpose of averting childhood malaria morbidity and mortality unless its uptake for full vaccination can be improved. Decreasing coverage after the first dose of a multi-dose vaccine is common and has been reported for RTS,S in Ghana [ 14 ] as well as other childhood vaccine studies on vaccine uptake 15 , 16 , 17 .
The high coverage of RTS,S doses 1 and 2 could have been achieved due to of the campaign conducted during the launch of the vaccine in the routine vaccination system in Nsanje district. This possibly created a lot of demand for the vaccine and it made the communities aware of the vaccine. The district health directorate created demand through risk communication during community engagement. Later after the launch campaigns, the demand could have been reducing which could lead to reduction of the subsequent doses.
The data for coverages of other vaccines offered in the district the same period when this study was conducted was high. Then coverage for BCG was at 99.5%, MR 1 was at 97%, MR 2 was at 92%, Rota 1 was at 98.6% and for Rota 2 was at 94.3%. No vaccine was below 80% whether it was administered once or had several numbers of doses. This showed that only the malaria vaccine had the lowest coverage for full uptake.
Knowledge of the mothers/caregivers on the childhood vaccines, ages at which those vaccines are received and the number of vaccines doses a child should receive to be fully vaccinated is important in order to increase the uptake levels of the vaccine. Although the majority of the mothers/caregivers had ever heard about malaria vaccine, only a few knew the vaccination schedule and number of doses to be received for a child to be fully vaccinated. This poor knowledge could have contributed to the reduction of subsequent doses observed in this study. This indicated that health education and promotion on malaria vaccine is not adequately done in Nsanje district. Similarly, a study conducted by Biset et al . [ 16 ] found that low knowledge about childhood vaccine was associated negatively with full vaccination coverage. Most mothers/caregivers relied on the community health volunteer or the Health Surveillance Assistant to remind them about the next day of vaccination hence there was no association between having knowledge on vaccine schedule and ages with full uptake of malaria vaccine. However, it is very important that the mothers/caregivers should know the ages and the vaccination schedule in cases whereby the community health volunteer or Health Surveillance Assistant did not remind them about the next visit day, they should be able to remember by themselves. In doing so, the coverages could be high. In a study conducted by Victoria et al . [ 18 ], in Ghana, concluded that health education is important because fears and concerns about malaria vaccine are addressed. Addressing the mothers/caregivers concerns through health education may enable the mothers/caregivers to encourage other mothers/caregivers in their communities to get their children vaccinated hence increasing the vaccine coverage. Additionally, some systematic reviews conducted in Africa on childhood vaccination also found that full uptake of childhood vaccines was influenced by mothers knowledge on vaccines 19 , 20 .
In this study, few children did not take any malaria dose. The main reason was that their mother/caregiver not knowing that their children were eligible while some did not take any dose of malaria vaccine because of religious beliefs. In Nsanje district there are certain religions that prohibits its member to go to the hospital or access any other health services. Since mothers/caregivers from these religions are likely not be found at under 5 clinic to learn the importance of malaria vaccines, even if they are willing to vaccinate their children, their religious leader will prevent them from accessing the health services. This was also evidenced in a study conducted by Adeyanju et al . [ 21 ] in Malawi, which reported that religious groupings, for example Zion and Apostolic faith, were prohibiting their members from visiting the hospital and accessing vaccines.
A majority of the children in this study had no or partial uptake of malaria vaccine. The main reason for no/partial uptake being low levels of knowledge and awareness on next visit date and knowing if their child was eligible. This finding is similar to reports by Price et al . [ 22 ] which reported that in first three implementing countries of malaria vaccine, information barrier contributed to no or partial uptake of malaria vaccine. Additionally, in Kenya, a recent study by Hoyt et al . [ 23 ] found that lack of awareness on malaria vaccine was a factor that led to lower coverage of malaria vaccine. Another study by Yeboah et al . [ 24 ] in Ghana recommended that mothers should understand the importance of their children getting the vaccine even during their second year of life, to help increase the uptake of dose 4 of malaria vaccine.
Furthermore, this study showed that the education level of mothers/caregivers was associated with full uptake of malaria vaccine. Mothers/caregivers who had secondary education and above managed to fully vaccinate their children with malaria vaccine. The high uptake of malaria vaccine by those mothers/caregiver that are more educated is because as they can easily understand the importance of malaria vaccine to their children, but also they could have greater access to information regarding malaria vaccines and other vaccines in general. This finding is consistent with the findings from a study conducted in Malawi [ 25 ]. In additional, a study conducted in Burkina Faso reported that level of education was a determinant in the uptake of childhood vaccines [ 26 ]. A systematic review conducted in Sub-Saharan Africa by Tekle et al . [ 27 ] and another study conducted by Touray et al . [ 27 ] found that level of education of a mother/caregiver was associated with full uptake of childhood vaccine.
Number of antenatal visits was a factor affecting full uptake of malaria vaccine. The children whose mothers/caregivers went for ante natal clinic 4 times or more had increased odds of getting fully vaccinated. This could be due to their health seeking behavior but also because they could have heard about the introduction of malaria vaccine at ANC and being told the importance of vaccinating their children. Similar results were reported in studies conducted by in Malawi, Ghana and Kenya [ 23 , 24 , 25 ].
This study showed that mothers/caregivers whose children ever suffered side effects following immunization had decreased odds of completing all the four doses of malaria vaccine. These mothers/caregivers could have been afraid of taking their children for vaccination in fear of the side effects. Studies conducted in Nigeria, Burkina Faso and Ethiopia also reported side effects following immunization affected the uptake of childhood vaccines [ 21 , 25 , 26 ]. Since malaria vaccine was being newly introduced in Nsanje district mothers/caregivers could think that the vaccine may have worst adverse effects after immunization hence hesitating in the uptake. This could have contributed to the low coverage of fully vaccinated children with malaria vaccine.
Mothers/caregivers who were living near the vaccination point had increased odds in getting their children receiving all the doses than those mothers who were living far. Similar results were observed in studies conducted in Malawi . Three systematic reviews conducted in Ethiopia, Nigeria and in sub-Saharan African systematic also found that distance to the vaccination site was a determinant for full uptake of childhood vaccines 16 , 20 , 28 Furthermore, mode of transport was found to be a significant factor associated with full uptake of malaria vaccine. This study observed that those mothers/caregivers who used commercial motorbikes or bikes were finding it easy to reach the vaccination points hence most of them had their children full vaccinated. Similar findings were reported in a study conducted in Togo [ 29 ].
The study found that having attended vaccination site and failed to vaccinate the child was significantly associated with malaria vaccine uptake. The reasons for mothers/caregivers not vaccinating their child while already at the vaccination site could be vaccine stock-outs, cancellation of the vaccination clinic, arriving at the clinic late while it has already been closed. This could have made some mothers/caregivers not to go to the vaccination site again as they think they may just waste their time to go to the vaccination site and never vaccinate their children hence leading to low coverage of malaria vaccine. Similarly, Lee et al . [ 30 ] found that vaccine stock-outs were significantly associated with low coverage of vaccines. Additionally, a study conducted in Ethiopia in 2021 reported that mothers/caregivers unsatisfied with health care workers was a determinant for incomplete childhood vaccination [ 31 ].
Limitations of the study
Some of the mothers/caregivers had no health passports for their children and consequently the researcher only relied on the word of mouth to re-call some information. This study did not collect qualitative data using Focus Group Discussions (FGDs), this would have thrown more light on the health system factors affecting the uptake of malaria vaccine it could also have given more understanding on perceptions, experiences and challenges faced by mothers/caregivers getting their children to receive malaria vaccine.
In order to reach WHO vaccine targets and increase the effectiveness of the malaria vaccine, district and national level agencies, e.g. Nsanje Directorate of Health and Social Services and Malawi Ministry of Health, should intensify and sustain information, education and communication in the communities about the malaria vaccine. Engaging religious leaders may also enhance these messages.
Availability of data and materials
Relevant datasets for this study are availability from the corresponding author upon request.
Abbreviations
Adverse event following immunization
Ante-natal care
Expanded programme on immunization
Long lasting insecticidal nets
Ministry of Health
National Malaria Control Programme
Piperonyl butoxide
- Malaria vaccine
Vaccine preventable diseases
World Health Organization
WHO. World malaria report. Geneva: World Health Organization; 2023.
Google Scholar
WHO. Malaria: the malaria vaccine implementation programme (MVIP). Geneva: World Health Organization. 2023. https://www.who.int/news-room/questions-and-answers/item/malaria-vaccine-implementation-programme . Accessed 12 June 2022.
WHO. Full Evidence Report on the RTS,S/AS01 Malaria Vaccine. Geneva, World Health Organization, 2021. https://cdn.who.int/media/docs/default-source/immunization/mvip/full-evidence-report-on-the-rtss-as01-malaria-vaccine-for-sage-mpag . Accessed 8 Sept 2022.
Penny MA, Verity R, Bever CA, Saubouin C, Galactionova K, Flasche S, et al. Public health impact and cost-eff effectiveness of the RTS, S/AS01 malaria vaccine: a systematic comparison of predictions from four mathematical models. Lancet. 2016;387:367–75.
Article PubMed PubMed Central Google Scholar
WHO. Business case for WHO immunization activities on the African continent. Geneva: World Health Organization; 2018.
Greenwood BM. Efficacy and safety of RTS, S/AS01 malaria vaccine with or without a booster dose in infants and children in Africa: final results of a phase 3, individually randomised, controlled trial. Lancet. 2015;386:31–45.
Article Google Scholar
Oduoye MO, Zuhair V, Marbell A, Olatunji GD, Khan AA, Farooq A, et al. The recent measles outbreak in South African Region is due to low vaccination coverage: what should we do to mitigate it ? New Microbes New Infect. 2023;54:101164.
Russo G, Miglieta A, Pezzotti P, Biguioh RM, Mayaka GB, Sobze MS, et al. Vaccine coverage and determinants of incomplete vaccination in children aged 12–23 months in Dschang, West Region, Cameroon: a cross-sectional survey during a polio outbreak. BMC Public Health. 2015;15:630.
Hamson E, Forbes C, Wittkopf P, Pandey A, Mendes D, Kowalik J, et al. Impact of pandemics and disruptions to vaccination on infectious diseases epidemiology past and present. Hum Vaccin Immunother. 2023;19:2219577.
Cooper S, Betsch C, Sambala EZ, Mchiza N. Vaccine hesitancy: a potential threat to the achievements of vaccination programmes in Africa. Hum Vaccin Immunother. 2018;14(10):2355–7.
National Statistical Office. Malawi population and housing census report. Zomba, Malawi, 2018. http://www.nsomalawi.mw/images/stories/data_on_line/demography/census_2018/2018%20Malawi%20Population%20and%20Housing%20Census%20Main%20Report.pdf . Accessed 22 Aug 2022
Republic of Malawi. Nsanje District Council socio-economic profile 2017–2022. Lilongwe, Malawi. 2020.
WHO. Immunization Agenda 2030 (IA2030). Geneva, World Health Organization, 2021. https://www.who.int/immunization/ia2030_Draft_One_English.pdf?ua=1 . Accessed 15 June 2022.
Tabiri D, Claude J, Pingdwindé R, Nortey PA. Factors associated with malaria vaccine uptake in Sunyani Municipality, Ghana. Malar J. 2021;20:325.
Acharya P, Kismul H, Mapatano MA, Hatl A. Individual- and community-level determinants of child immunization in the Democratic Republic of Congo: a multilevel analysis. PLoS ONE. 2018;13: e0202742.
Biset G, Woday A, Mihret S, Tsihay M. Full immunization coverage and associated factors among children age 12–23 months in Ethiopia: systematic review and meta-analysis of observational studies. Hum Vaccines Immunother. 2021;17:2326–35.
Adedire EB, Ajayi I, Fawole OI, Ajumobi O, Kasasa S, Nguku P. Immunisation coverage and its determinants among children aged 12–23 months in Atakumosa-west district, Osun State Nigeria: a cross-sectional study. BMC Public Health. 2016;16:905.
Bam V, Mohammed A, Kusi-amponsah A, Armah J, Lomotey AY, Budu HI, et al. Caregivers’ perception and acceptance of malaria vaccine for Children. PLoS ONE. 2023;18: e0288686.
Article CAS PubMed PubMed Central Google Scholar
Bangura JB, Xiao S, Qiu D, Ouyang F, Chen L. Barriers to childhood immunization in sub-Saharan Africa: a systematic review. BMC Public Health. 2020;20:1108.
Galadima AN, Zulkefli AM, Said SM, Ahmad N. Factors influencing childhood immunisation uptake in Africa: a systematic review. BMC Public Health. 2021;21:1475.
Adeyanju GC, Betsch C, Adamu AA, Gumbi KS, Head MG, Aplogan A, et al. Examining enablers of vaccine hesitancy toward routine childhood and adolescent vaccination in Malawi. Glob Health Res Policy. 2022;7:28.
Price J, Gurley N, Gyapong M, Ansah EK, Awusabo-asare K, Cyasi SF, et al. Acceptance of and adherence to a four-dose RTS, S/AS01 schedule: findings from a longitudinal qualitative evaluation study for the malaria vaccine implementation programme. Vaccines. 2023;11:1801.
Hoyt J, Okello G, Bange T, Kariuki S, Jalloh MF, Webster J, et al. RTS, S/AS01 malaria vaccine pilot implementation in western Kenya: a qualitative longitudinal study to understand immunisation barriers and optimise uptake. BMC Public Health. 2023;23:2283.
Yeboah D, Marfo JO, Agyeman YN. Predictors of malaria vaccine uptake among children 6–24 months in the Kassena Nankana Municipality in the Upper East Region of Ghana. Malar J. 2022;21:339.
Mvula H, Heinsbroek E, Chihana M, Crampin AC, Kabuluzi S, Chirwa G, et al. Predictors of uptake and timeliness of newly introduced pneumococcal and rotavirus vaccines, and of measles vaccine in rural Malawi: a population cohort study. PLoS ONE. 2016;11: e0154997.
Kagoné M, Yé M, Nébié E, Sie A, Schoeps A, Becher H, et al. Vaccination coverage and factors associated with adherence to the vaccination schedule in young children of a rural area in Burkina Faso. Glob Health Action. 2017;10:1399749.
Tekle F, Asante A, Woldie M, Dawson A, Hayen A. Child vaccination in sub-Saharan Africa: increasing coverage addresses inequalities. Vaccine. 2022;40:141–50.
Obasohan PE, Mustapha MA, Makada A, Obasohan DN. Evaluating the reasons for partial and non-immunization of children in Wushishi local government area, Niger state, Nigeria: methodological comparison. Afr J Reprod Health. 2018;22:113–22.
PubMed Google Scholar
Ekouevi DK, Gbeasor-komlanvi FA, Yaya I, Zida-compaore WI, Boko A, Sewu E, et al. Incomplete immunization among children aged 12–23 months in Togo: a multilevel analysis of individual and contextual factors. BMC Public Health. 2018;18:952.
Lee D, Lavayen MC, Kim TT, Legins K, Seidel M. Association of vaccine stockout with income immunisation coverage in low-income countries: a retrospective cohort study. BMJ Open. 2023;13: e072364.
Mebrat A, Dube L, Kebede A, Aweke Z. Determinants of incomplete childhood vaccination among children aged 12–23 months in Gambela region, Southwest Ethiopia: a case control study. Ethiop J Health Sci. 2021;31:63.
PubMed PubMed Central Google Scholar
Download references
Acknowledgements
I would like to express my sincere gratitude to Nsanje Directorate of Health and Social Services for giving me clearance to conduct the study in their Health Catchment areas. We would also like to thank village heads who gave permission for us to interview the participants in their villages. We thank Mr. Jomo Sumani, Mr. Mphatso William, Mr. Ben Chilongo, Mr. Wilson Ntchembere, Mr. Doubtful Thete and Mrs. Edina Sadik who participated in data collection. I special thanks should also go to Mr. Jekiyala Kalonga (Nsanje District Malaria Coordinator), Mr. Willy Magwira (Nsanje Health Management Information System Officer), Mr. Fred Minyaliwa (Nsanje District Environmental Health Officer) for their logistical and technical assistance during the implementation of this study.
This work was supported by the Capacity Development of Applied Epidemiologists in Eastern Africa Region (CDAE), a project which is part of European and Developing Countries Clinical Trials Partnership II (EDCPT2) Programme supported by the European Union. CDAE is jointly implemented by the Africa Population and Health Research Center (APHRC), the Amref International University (AMIU) and the Jaramogi Oginga Odinga University of Science and Technology (JOOUST) and funded by the EDCPT2 (Grant: CSA2020E-3139) awarded to AJS.
Author information
Save Kumwenda, Lauren M. Cohee and Shehu S. Awandu shares the final authorship, having contributed equally to the study.
Authors and Affiliations
Department of Biomedical Sciences, School of Health Sciences, Jaramogi Oginga Odinga University of Science and Technology, P. O. Box 210-40601, Bondo, Kenya
Atusaye J. Simbeye, Dickens Omondi & Shehu S. Awandu
Department of Public and Environmental Health Sciences, School of Science and Technology, Malawi University of Business and Applied Sciences, Chichiri, Private Bag 303, Blantyre, Malawi
Save Kumwenda
Department of Pediatrics, Division of Infectious Disease and Tropical Pediatrics, Center for Vaccine Development and Global Health, University of Maryland School of Medicine, 655 B Baltimore St S, Baltimore, MD, 21201, USA
Lauren M. Cohee
Department of Clinical Sciences, Liverpool School of Tropical Medicine, Pembroke Place, Liverpool, L3 5QA, UK
School of Public Health, Amref International University, P. O. Box 27691-00506, Nairobi, Kenya
Peninah K. Masibo
African Population and Health Research Centre (APHRC), P. O. Box 10787-00100, Nairobi, Kenya
Hesborn Wao
You can also search for this author in PubMed Google Scholar
Contributions
AJS, SK, LMC and SSA conceived the study and developed study protocol. AJS conducted data collection supervision. AJS, LMC and SSA conducted data analysis. AJS wrote the first draft of the manuscript. SK, LMC, DO, PKM, HW and SSA revised the manuscript and all authors approved the final manuscript prior to submission. All authors approved the final manuscript.
Corresponding author
Correspondence to Atusaye J. Simbeye .
Ethics declarations
Ethics approval and consent to participate.
Permision to conduct this study was obtained from Jaramogi Oginga Odinga University of Science and Technology ethical review committee (JOOUST-ERC), reference number: JOOUST/DVC-RIO/E4, approval number: ERC 37/04/23-5/05 and from Malawi National Health Sciences Research Committee (NHSRC), protocol number: 23/02/3267, approval number: 3267. Clearance was obtained from Nsanje District Health Directorate before commencement of the study activities. Permission was also sought from local leaders verbally before entering in their villages. Before data collection, informed consent was sought from each study to ensure voluntary participation in the study. All necessary information about the study was explained to the participants. The purpose, risks, and benefits of the study was explained to each study participant. Further, the study participants were told that they have right to withdraw from the study at any point during the study period. Those participants who agreed to be interviewed were requested to either sign or thumbprint the informed consent form.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Simbeye, A.J., Kumwenda, S., Cohee, L.M. et al. Factors associated with malaria vaccine uptake in Nsanje district, Malawi. Malar J 23 , 105 (2024). https://doi.org/10.1186/s12936-024-04938-7
Download citation
Received : 20 February 2024
Accepted : 06 April 2024
Published : 17 April 2024
DOI : https://doi.org/10.1186/s12936-024-04938-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Vaccine uptake
- Vaccine coverage
- Factors influencing vaccine uptake
Malaria Journal
ISSN: 1475-2875
- Submission enquiries: [email protected]
Travel Vaccines and Advice for Malawi

Malawi promises an array of animal adventures and looks into lifestyles that are exclusive to this part of the world. Travellers eager to immerse themselves in an adventure unlike any other often set their sights on Malawi.
Malawi is home to ample culture and wildlife, making it the perfect stop for any tourists hoping to find a truly unique experience on their travels.
Do I Need Vaccines for Malawi?
Yes, some vaccines are recommended or required for Malawi. The PHAC and WHO recommend the following vaccinations for Malawi: COVID-19 , hepatitis A , hepatitis B , typhoid , cholera , yellow fever , rabies , meningitis , polio , measles, mumps and rubella (MMR) , Tdap (tetanus, diphtheria and pertussis) , chickenpox , shingles , pneumonia and influenza .
See the bullets below to learn more about some of these key immunizations:
- COVID-19 – Airborne – Recommended for all travellers
- Hepatitis A – Food & Water – Recommended for most travellers
- Hepatitis B – Blood & Body Fluids – Accelerated schedule available
- Typhoid – Food & Water – Shot lasts 2 years. Oral vaccine lasts 5 years, must be able to swallow pills. Oral doses must be kept in refrigerator.
- Cholera – Food & Water – Areas of active cholera transmission include: Blantyre, Dedza, Dowa, Karonga, Kasungu, Likoma, Lilongwe, Mulanje, Nkhatabay, Nsanje, Rumphi and Salima
- Yellow Fever – Mosquito – Required if travelling from a country where yellow fever is present.
- Rabies – Saliva of Infected Animals – High risk country. Vaccine recommended for long-term travellers and those who may come in contact with animals.
- Measles Mumps Rubella (MMR) – Various Vectors – Given to anyone unvaccinated and/or born after 1957. One time adult booster recommended.
- TDAP (Tetanus, Diphtheria & Pertussis) – Wounds & Airborne – Only one adult booster of pertussis required.
- Chickenpox – Direct Contact & Airborne – Given to those unvaccinated that did not have chickenpox.
- Shingles – Direct Contact – Vaccine can still be given if you have had shingles.
- Pneumonia – Airborne – Two vaccines given separately. All 65+ or immunocompromised should receive both.
- Influenza – Airborne – Vaccine components change annually.
- Meningitis – Airborne & Direct Contact – Given to anyone unvaccinated or at an increased risk, especially students.
- Polio – Food & Water – Considered a routine vaccination for most travel itineraries. Single adult booster recommended.
See the tables below for more information:
Malaria , dengue and chikungunya are all mosquito-borne infections found in Malawi. It is important to bring mosquito repellents and netting to prevent bites and potential spread. Antimalarials are recommended as well.
Rabies poses a risk to travellers to Malawi, especially if staying for a long period of time or visiting rural areas. Vaccination should be considered before travelling.
Visit our vaccinations page to learn more. Travel safely with Passport Health and schedule your appointment today by calling or book online now .
Do I Need a Visa or Passport for Malawi?
Canadians planning to visit Malawi will need a visa to enter the country. There is also an exit fee of $30 USD for all travellers.
Sources: Embassy of Malawi and Canadian Travel and Tourism
The Canadian Government reports that you must declare all foreign currency when entering Malawi as well.
Visit the Canadian Travel and Tourism website for more information on entry and exit requirements.
What is the Climate Like in Malawi?
Malawi is a country with sub-tropical climate. This means that the weather is warm and moderate almost all year round. The nation is also dry, and most of its precipitation occurs between November and April. Here is what to expect in a few tourist destinations:
- Lilongwe – The capital city of Malawi enjoys warm summers and milder winters. The high altitude of the city’s location actually keeps the temperatures a little lower, and more pleasant. Lilongwe sees most of its heavy rainfall from December to February and can be prone to downpours during this time.
- Blantyre – Temperatures in this city are considered tropical, it is often warm and sometimes humid. The area’s humidity is at its peak in October and November, the warm months right before the rainy season begins. The weather can also be misty and cool during the cold season in June and July.
- Mulanje – Temperatures also stay fairly warm throughout the year. Mount Mulanje itself experiences different weather patterns, as it cools the higher you climb. Weather on the mountain can also be sporadic, as mist and rainfall can cover Mount Mulanje. The area sees more precipitation around November, December and January.
How Safe is Malawi?
Crime in Malawi is fairly common. Armed residential break-ins are frequent, and break-ins in lodges and hotels have been reported. Robberies and pick-pocketing are also common street crimes.
Carjackings are prevalent in Lilongwe and Blantyre. This most often occurs when entering through a security gate into a home. Always keep doors locked and windows closed, and stay alert when entering or leaving.
Stay off the streets at night, particularly in urban areas. Armed assaults and muggings are becoming more prevalent. Foreigners are especially targeted in Lilongwe. Regardless of how many people you are with, city streets are not safe at night. It is also wise to exercise caution during the day. Make sure to arrange all your transportation in Malawi through your hotel or restaurant.
Be cautious when visiting or staying in isolated, lone areas such as Mount Mulanje. Public security in these areas is often limited. Be weary when visiting remote areas, and do not travel at night or alone.
While in Malawi, it is also crucial to stay alert for public demonstrations and civil disturbances. Avoid crowds, rallies and demonstrations, and always be aware of your surroundings.
Maneuvering Malawi’s Mount Mulanje
Adventurers and lovers of extreme sports consider Malawi an ideal travel destination. The nations’ terrain offers the perfect chance to test their skills.
One location that attracts hikers, bikers and rock climbers alike is Mount Mulanje. This mountain stands at over 3,000 meters tall. It is a picturesque destination for those wishing to see its rolling green valleys and clear, flowing rivers. But, the mountain’s rugged terrain is what calls to risk-takers from all across the globe.
Even attempting to climb or hike Mount Mulanje if you are not prepared can lead to severe injury. If you plan to climb the mountain, never climb alone. Always have enough food and water, and bring essential equipment like maps, guidebooks and compasses. Stick together with your group and do not push into unknown territory.
There is limited public security at Mount Mulanje. Avoid travelling at night and never travel alone.
What Should I Pack for Malawi?
In addition to all travel documents and medications recommended by a Passport Health Travel Medicine Specialist, here are some items to consider packing:
- Insect Repellent – Since malaria is at risk in Malawi, you should always pack bug spray. Packing a repellent with at least 20%-30% DEET will keep mosquitoes away.
- Water Purifier – Cholera is spread primarily through contaminated water. Having a water purifiers or filter while in Malawi can prevent contact with dirty water. Having a water purifier helps ensure your safety and protects your health.
- Neutral-colored clothing – Wearing neutral clothing, such as beige and grays, prevents contact with mosquitoes. It can also prevent from drawing too much attention to yourself. Avoid bringing too many blue or black articles of clothing. These colors attract tsetse flies, which may carry African sleeping sickness.
- Conservative clothing options – In some areas of Malawi, particularly in some villages, it can be offensive to wear revealing clothing. Islamic areas in southern Malawi require conservative dress. Wearing shorts, small skirts, crop tops and tank tops can be considered rude in many areas in the country.
- Walking shoes – Many adventures in Malawi require you to be on your feet. Hiking and walking through reservations can be uncomfortable, if not dangerous, if you do not have the proper footwear.
Canadian Embassy to Malawi
Canadian consular services can help travellers with many issues they may face including passport services. There are no consular services in Malawi. For any consular needs, contact the Canadian Embassy of Zimbabwe:
High Commission of Canada in Zimbabwe 45 Baines Avenue, Harare, Zimbabwe Telephone: +263 86 7700 8600
Ready to start your next journey? Call us at or book online now !
Customer Reviews
Passport health – travel vaccines for malawi.
On This Page: Do I Need Vaccines for Malawi? Do I Need a Visa or Passport for Malawi? What is the Climate Like in Malawi? How Safe is Malawi? Maneuvering Malawi’s Mount Mulanje What Should I Pack To Malawi? Canadian Embassy to Malawi

- PIPEDA Policy and Consent Form
- Privacy Policy
- Automatic Data Collection Statement

IMAGES
COMMENTS
All international travelers should be fully vaccinated against measles with the measles-mumps-rubella (MMR) vaccine, including an early dose for infants 6-11 months, according to CDC's measles vaccination recommendations for international travel. In Malawi poliovirus has been identified in the past year.
Specific. Advice. Travelers'. Diarrhea Kits. Available. Malawi promises an array of animal adventures and looks into lifestyles that are exclusive to this part of the world. Travelers eager to immerse themselves in an adventure unlike any other often set their sights on Malawi. Malawi is home to ample culture and wildlife, making it the ...
Yes. VACCINATIONS: Yellow fever, COVID-19. CURRENCY RESTRICTIONS FOR ENTRY: Must declare all foreign currency upon arrival. Doing so helps to ensure travelers will be allowed to depart Malawi with foreign currency. CURRENCY RESTRICTIONS FOR EXIT: $5,000 is the maximum amount of foreign currency with which travelers may exit the country.
Check our Traveler Information Center for more information if you are a traveler with specific health needs, such as travelers who are pregnant, immune compromised, or traveling for a specific purpose like humanitarian aid work. Remember to pack extras of important health supplies in case of travel delays. Prescription medicines. Your prescriptions
Prevention modalities: vaccination, medication, consultation. Hepatitis A. Contaminated food & water. Vaccination (2-dose vaccine): Recommended for most travelers. --Administer 2 doses, at least 6 months apart. --At least 1 dose should be given before travel. Consultation: Advise patient to wash hands frequently and avoid unsafe food and water.
Visit the Department of Homeland Security's website on the latest travel restrictions to the United States. Assistance: U.S. Embassy Lilongwe, Malawi, Area 40, City Center Lilongwe, Malawi. U.S. citizens with emergencies: +265-1-773-166 Ext. 3431. Outside of office hours: +265-999-960-178. E-mail: [email protected].
Some of these vaccinations include measles-mumps-rubella (MMR), diphtheria, tetanus, pertussis, polio, varicella (chickenpox), influenza and others. ... 2SLGBTQI+ persons should carefully consider the risks of travelling to Malawi. Travel and your sexual orientation, gender identity, gender expression and sex characteristics.
All tests require a fee; the average cost is 40,000 MWK for Malawian citizens and 80,000 MWK for foreign nationals. Rapid COVID-19 Tests. Open Monday - Friday from 0800-1700, closed on public holidays. Results are available within 15 minutes. Open Monday - Friday from 0800-1200 and 1300-1600.
Vaccinations and health risks. At least 8 weeks before your trip check: the latest information on vaccination recommendations and health risks in TravelHealthPro's Malawi guide. where to get ...
Providing the following information to the Ministry of Health is required under the Public Health Act of Malawi Chapter 34:01 and is being collected as part of the public health surveillance and response to infectious diseases of international concern. The information will be used by Malawi public health authorities and other international, or local agencies for public health purposes. The ...
FCDO travel advice for Malawi. Includes safety and security, insurance, entry requirements and legal differences. ... At least 8 weeks before your trip, check the vaccinations and certificates you ...
Certificate Requirements. Yellow fever vaccination certificate required for travellers aged 1 year or over arriving from countries with risk of yellow fever transmission and for travellers having transited for more than 12 hours through an airport of a country with risk of yellow fever transmission. Yellow Fever vaccination £69 per dose.
MenACWY (Meningococcal vaccine against serotypes A+C+W+Y) MenB (Meningococcal B vaccine) Typh (Typhoid vaccine) These vaccines are recommended for some travellers visiting this country. The recommendation depends on the duration of the stay, type of travel/activity, the traveller's health etc., and should be assessed by a doctor.
Malawi has received its first 360,000 doses of Astra Zeneca/Oxford vaccines from COVAX. Chiponda said they expect to rollout the vaccinations within five days, starting with the most-at-risk, who include health workers, those with underlying medical conditions, the elderly from age 60 and others. "COVID-19 brought us a cultural shock.
Highlights. Learn about CDC's Traveler Genomic Surveillance Program that detects new COVID-19 variants entering the country. Sign up to get travel notices, clinical updates, & healthy travel tips. CDC Travelers' Health Branch provides updated travel information, notices, and vaccine requirements to inform international travelers and provide ...
Advice for All Destinations COVID-19. Read the information on the COVID-19: Health Considerations for Travel page for advice on travelling during the COVID-19 pandemic.. Vaccinations and malaria risk. Review both the Vaccination and Malaria sections on this page to find out if you may need vaccines and/or a malaria risk assessment before you travel to this country.
Vaccinations The CDC and WHO recommend the following vaccinations for Malawi: hepatitis A, hepatitis B, typhoid, cholera, yellow fever, rabies, meningitis, polio, measles, ... Malawi Travel Facts October 2023 Potable Water Opt for bottled water International Driving Permit
Advice. Travellers'. Diarrhea Kits. Available. Malawi promises an array of animal adventures and looks into lifestyles that are exclusive to this part of the world. Travellers eager to immerse themselves in an adventure unlike any other often set their sights on Malawi. Malawi is home to ample culture and wildlife, making it the perfect stop ...
Yes, you will need to get some vaccines before you visit Malawi. To make it simple for you, we prepared the following vaccines that you must consider before your departure to Malawi. Chickenpox. Measles. Influenza. Polio. Tetanus. Mumps. Diphtheria.
Reissued with updates to civil unrest information. Exercise increased caution in Malawi due to crime and civil unrest.. Country Summary: Violent Crime such as theft, burglary, armed robbery, assault, and carjacking is common. The capabilities of the Malawi Police Service are growing but its resources and abilities to deter and investigate crimes, assist victims, and apprehend criminals are ...
Find out which travel vaccines you may need to help you stay healthy on your trip. Before Travel. Make sure you are up-to-date on all of your routine vaccines. Routine vaccinations protect you from infectious diseases such as measles that can spread quickly in groups of unvaccinated people. Many diseases prevented by routine vaccination are not ...
Today's launch confirms eight countries on the African continent have the opportunity to offer malaria vaccinations. ... A pilot malaria vaccine program in Ghana, Kenya, and Malawi reached over two million children from 2019 to 2023, showing a significant reduction in malaria illness, a 13% drop in overall child mortality, and substantial ...
Two safe and effective vaccines — RTS,S and R21 — recommended by World Health Organization (WHO), are a breakthrough for child health and malaria control. A pilot malaria vaccine programme in Ghana, Kenya and Malawi reached over 2 million children from 2019 to 2023, showing a significant reduction in malaria illness and a 13% drop in ...
CDC Yellow Book 2024. Preparing International Travelers. Author (s): Mark Gershman, Rhett Stoney (Yellow Fever) Holly Biggs, Kathrine Tan (Malaria) The following pages present country-specific information on yellow fever (YF) vaccine requirements and recommendations, and malaria transmission information and prevention recommendations.
Malaria continues to pose a significant global health challenge. Globally, an estimated 249 million cases of malaria occurred in year 2022 which was 2 million more cases than in 2021 [].Sub-Saharan African countries facing the hardest hit contributing 93.6% (233 million) of total malaria cases and 95.4% (580,000) of total malaria deaths [].In Africa, about 78.1% (453,000) of the total deaths ...
Advice. Travellers'. Diarrhea Kits. Available. Malawi promises an array of animal adventures and looks into lifestyles that are exclusive to this part of the world. Travellers eager to immerse themselves in an adventure unlike any other often set their sights on Malawi. Malawi is home to ample culture and wildlife, making it the perfect stop ...