You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
- Section 6 - Medical Tourism
- Section 7 - Travel & Breastfeeding

Pregnant Travelers
Cdc yellow book 2024.
Author(s): Romeo Galang, I. Dale Carroll, Titilope Oduyebo
- The Pretravel Consultation
Infectious Disease Concerns
Environmental health concerns, transportation considerations.
Pregnancy can cause physiologic changes that require special consideration during travel. With careful preparation, however, most pregnant people can travel safely.
Pretravel Consultation
The pretravel consultation and evaluation of pregnant travelers ( Box 7-01 ) should begin with a careful medical and obstetric history, specifically assessing gestational age and the presence of factors and conditions that increase risk for adverse pregnancy outcomes. A visit with an obstetric health care provider also should be a part of the pretravel assessment to ensure routine prenatal care and identify any potential problems. Instruct pregnant travelers to carry with them a copy of their prenatal records and physician’s contact information.
Review the pregnant person’s travel itinerary, including accommodations, activities, and destinations, to guide pretravel health advice. Discourage pregnant travelers from undertaking unaccustomed vigorous activity. Swimming and snorkeling during pregnancy generally are safe, but falls during waterskiing have been reported to inject water into the birth canal. Most experts advise against scuba diving for pregnant people because of risk for fetal gas embolism during decompression (see Sec. 4, Ch. 4, Scuba Diving: Decompression Illness & Other Dive-Related Injuries ). Riding animals, bicycles, or motorcycles presents risks for abdominal trauma.
Educate pregnant people on how to avoid travel-associated risks, manage minor pregnancy discomforts, and recognize more serious complications. Advise pregnant people to seek urgent medical attention if they experience contractions or premature labor; symptoms of deep vein thrombosis (e.g., unusual leg swelling and pain in the calf or thigh) or pulmonary embolism (e.g., unusual shortness of breath); dehydration, diarrhea, or vomiting; severe pelvic or abdominal pain; symptoms of preeclampsia (e.g., severe headaches, nausea and vomiting, unusual swelling, vision changes); prelabor rupture of the membranes; or vaginal bleeding.
Box 7-01 Pretravel consultation for pregnant travelers: a checklist for health care providers
☐ Review vaccination history (e.g., COVID-19, hepatitis A, hepatitis B, measles, pertussis, rubella, varicella, tetanus) and update vaccinations as needed (see text for contraindications during pregnancy)
☐ Policies and paperwork
- Discuss supplemental travel insurance, travel health insurance, and medical evacuation insurance; research specific coverage information and limitations for pregnancy-related health issues
- Advise travelers to check airline and cruise line policies for pregnant travelers
- Provide letter confirming due date and fitness to travel
- Provide copy of medical records
☐ Prepare for obstetric care at destination
- Advise traveler to arrange for obstetric care at destination, as needed
☐ Review signs and symptoms requiring immediate care, including
- Contractions or preterm labor
- Deep vein thrombosis or pulmonary embolism symptoms, which include unusual swelling of leg with pain in calf or thigh, unusual shortness of breath
- Pelvic or abdominal pain
- Preeclampsia symptoms (e.g., unusual swelling, severe headaches, nausea and vomiting, vision changes)
- Rupture of membranes
- Vomiting, diarrhea, dehydration
Contraindications to Travel During Pregnancy
Absolute contraindications are conditions for which the potential harm of travel during pregnancy always outweighs the benefits of travel to the pregnant person or fetus. Relative contraindications are conditions for which travel should be avoided if the potential harm from travel outweighs its benefits ( Box 7-02 ).
Although travel is rarely contraindicated during a normal pregnancy, pregnancies that require frequent antenatal monitoring or close medical supervision might warrant a recommendation that travel be delayed. Educate pregnant travelers that the risk of obstetric complications is greatest in the first and third trimesters of pregnancy.
Box 7-02 Contraindications to travel during pregnancy
Absolute contraindications.
- Abruptio placentae
- Active labor
- Incompetent cervix
- Premature labor
- Premature rupture of membranes
- Suspected ectopic pregnancy
- Threatened abortion / vaginal bleeding
- Toxemia, past or present
RELATIVE CONTRAINDICATIONS
- Abnormal presentation
- Fetal growth restriction
- History of infertility
- History of miscarriage or ectopic pregnancy
- Maternal age <15 or >35 years
- Multiple gestation
- Placenta previa or other placental abnormality
Planning for Emergency Care
Obstetric emergencies are often sudden and life-threatening. Advise all pregnant travelers (but especially those in their third trimester or otherwise at high risk) to identify, in advance, international medical facilities at their destination(s) capable of managing complications of pregnancy, delivery (including by caesarean section), and neonatal problems. Counsel against travel to areas where obstetric care might be less than the standard at home.
Many health insurance policies do not cover the cost of medical treatment for pregnancy or neonatal complications that occur overseas. Pregnant people should strongly consider purchasing supplemental travel health insurance to cover pregnancy-related problems and care of the neonate, as needed. In addition, pregnant travelers should consider medical evacuation insurance coverage in case of pregnancy-related complications (see Sec. 6, Ch. 1, Travel Insurance, Travel Health Insurance & Medical Evacuation Insurance ).
Medications
Over-the-counter drugs and nondrug remedies can help a pregnant person travel more comfortably. For instance, pregnant people can safely use a mild bulk laxative for constipation. In addition, several simple available remedies are effective in relieving the symptoms of morning sickness. Nonprescription remedies include ginger, available as a powder that can be mixed with food or drinks (e.g., tea), and as candy (e.g., lollipops). Similarly, pyridoxine (vitamin B6) is effective in reducing symptoms of morning sickness and is available in tablet form, as well as lozenges and lollipops. Antihistamines (e.g., dimenhydrinate, meclizine) often are used in pregnancy for morning sickness and motion sickness and appear to have a good safety record.
Carefully consider appropriate pain management and use of analgesics during pregnancy. Acetaminophen remains the nonopioid analgesic of choice during pregnancy. Although low-dose aspirin has been demonstrated to be relatively safe during pregnancy for certain clinical indications, it should be used cautiously. Aspirin can increase the incidence of abruption, and other anti-inflammatory agents can cause premature closure of the ductus arteriosus.
Various systems are used to classify drugs with respect to their safety in pregnancy . Refer to specific data about the effects of a given drug during pregnancy rather than depending on a classification. Counsel patients to help them make a balanced decision on the use of medications during pregnancy.
Vaccinations
In the best possible scenario, people should be up to date on routine vaccinations before becoming pregnant. The most effective way of protecting the infant against many diseases is to vaccinate the pregnant person. See a summary of current Advisory Committee on Immunization Practices (ACIP) guidelines for vaccinating pregnant people .
Coronavirus Disease 2019
Pregnant people are more likely to become more severely ill from coronavirus disease 2019 (COVID-19) than people who are not pregnant. Having COVID-19 during pregnancy increases a person’s risk of complications that can affect their pregnancy. For these reasons, the Centers for Disease Control and Prevention (CDC) recommends that people who are pregnant, trying to get pregnant, or who might become pregnant in the future get vaccinated against COVID-19 . As of August 2022, the COVID-19 vaccines authorized or approved for use in the United States are nonreplicating vaccines that do not cause infection in the pregnant person or the fetus. Pregnant people may choose to receive any of the COVID-19 vaccines authorized or approved for use in the United States; the ACIP does not state a preference.
COVID-19 vaccination can be safely provided before pregnancy or during any trimester of pregnancy. Available vaccines are highly effective in preventing severe COVID-19, hospitalizations, and deaths; data have shown that the benefits of vaccination during pregnancy, to both the pregnant person and their fetus, outweigh any potential risks. Pregnant people might want to speak with their health care provider before making a decision about receiving COVID-19 vaccine , but a consultation is not required before vaccination. Side effects from COVID-19 vaccination in pregnant people are like those expected among nonpregnant people. Pregnant people can take acetaminophen if they experience fever or other post-vaccination symptoms.
The ACIP recommends that all people who are or who will become pregnant during the influenza season have an annual influenza vaccine using inactivated virus. Influenza vaccines can be administered during any trimester.
The safety of hepatitis A vaccination during pregnancy has not been determined; because hepatitis A vaccine is produced from inactivated virus, though, the risk to the developing fetus is expected to be low. Weigh the risk associated with vaccination against the risk for infection in pregnant people who could be at increased risk for exposure to hepatitis A virus. According to the ACIP, pregnant people traveling internationally are at risk of hepatitis A virus infection; ACIP recommends vaccination during pregnancy for nonimmune international travelers.
Limited data suggest that developing fetuses are not at risk for adverse events resulting from vaccination of pregnant people with hepatitis B vaccine (for details, see Sec. 5, Part 2, Ch. 8, Hepatitis B ). ACIP recommends vaccinating pregnant people identified as being at risk for hepatitis B virus infection during pregnancy; risk factors include >1 sex partner during the previous 6 months, being evaluated or treated for a sexually transmitted infection, recent or current injection drug use, or having a HBsAg-positive sex partner. In November 2021, ACIP recommended vaccination of all adults 19–59 years old.
Japanese Encephalitis
Data are insufficient to make specific recommendations for use of Japanese encephalitis vaccine in pregnant people (see Sec. 5, Part 2, Ch. 13, Japanese Encephalitis ).
Live-Virus Vaccines
Most live-virus vaccines, including live attenuated influenza, measles-mumps-rubella, live typhoid (Ty21a), and varicella, are contraindicated during pregnancy. Postexposure prophylaxis of a nonimmune pregnant person exposed to measles can be provided by administering measles immune globulin (IG) within 6 days of exposure; for varicella exposures, varicella-zoster IG can be given within 10 days. Advise people planning to become pregnant to wait ≥4 weeks after receiving a live-virus vaccine before conceiving.
Yellow Fever
Yellow fever vaccine is the exception to the rule about live-virus vaccines being contraindicated during pregnancy. ACIP considers pregnancy a precaution (i.e., a relative contraindication) for yellow fever vaccine. If travel is unavoidable, and the risk for yellow fever virus exposure outweighs the vaccination risk, it is appropriate to recommend vaccination. If the risks for vaccination outweigh the risks for yellow fever virus exposure, consider providing a medical waiver to the pregnant traveler to fulfill health regulations. Because pregnancy might affect immune responses to vaccination, consider performing serologic testing to document an immune response to yellow fever vaccine. Furthermore, if a person was pregnant (regardless of trimester) when they received their initial dose of yellow fever vaccine, they should receive 1 additional dose before they are next at risk for yellow fever virus exposure (see Sec. 5, Part 2, Ch. 26, Yellow Fever ).
Meningococcal
According to the ACIP , pregnant (and lactating) people should receive quadrivalent meningococcal vaccine, if indicated. Meningococcal vaccine might be indicated for international travelers, depending on risk for infection at the destination (see Sec. 5, Part 1, Ch. 13, Meningococcal Disease ).
No adverse events linked to inactivated polio vaccine (IPV) have been documented among pregnant people or their fetuses. Vaccination of pregnant people should be avoided, however, because of theoretical concerns. IPV can be administered in accordance with the recommended immunization schedule for adults if a pregnant person is at increased risk for infection and requires immediate protection against polio (see Sec. 5, Part 2, Ch. 17, Poliomyelitis ).
Administer rabies postexposure prophylaxis with rabies immune globulin and vaccine after any moderate- or high-risk exposure to rabies; consider preexposure vaccine for travelers who have a substantial risk for exposure (see Sec. 5, Part 2, Ch. 18, Rabies ).
Tetanus-Diphtheria-Pertussis
Tetanus, diphtheria, and acellular pertussis vaccine (Tdap) should be given during each pregnancy irrespective of a person’s history of receiving the vaccine previously. To maximize maternal antibody response and passive antibody transfer to the infant, optimal timing for Tdap administration is between 27 and 36 weeks’ gestation (earlier during this time frame is preferred), but it may be given at any time during pregnancy.
Malaria Prophylaxis
Malaria, caused by Plasmodium spp. parasites transmitted by mosquitoes, can be much more serious in pregnant than in nonpregnant people and is associated with high risks of illness and death for both mother and fetus. Malaria in pregnancy can be characterized by heavy parasitemia, severe anemia, and profound hypoglycemia, and can be complicated by cerebral malaria and acute respiratory distress syndrome. Placental sequestration of parasites might result in fetal loss due to abruption, premature labor, or miscarriage. An infant born to an infected mother is apt to be of low birth weight, and, although rare, congenital malaria is possible.
Because no prophylactic regimen provides complete protection, pregnant people should avoid or delay travel to malaria-endemic areas. If travel is unavoidable, the pregnant person should take precautions to avoid mosquito bites and use an effective prophylactic regimen.
Chloroquine is the drug of choice for pregnant travelers going to destinations with chloroquine-sensitive Plasmodium spp., and mefloquine is the drug of choice for pregnant travelers going to destinations with chloroquine-resistant Plasmodium spp. Doxycycline is contraindicated because of teratogenic effects on the fetus after the fourth month of pregnancy. Primaquine is contraindicated in pregnancy because the infant cannot be tested for glucose-6-phosphate dehydrogenase deficiency, putting the infant at risk for hemolytic anemia. Atovaquone-proguanil is not recommended because of lack of available safety data. A list of the available antimalarial drugs and their uses and contraindications during pregnancy can be found in Sec. 5, Part 3, Ch. 16, Malaria .
Travel Health Kits
In addition to the recommended travel health kit items for all travelers (see Sec. 2, Ch. 10, Travel Health Kits ), pregnant travelers should pack antacids, antiemetic drugs, graduated compression stockings, hemorrhoid cream, medication for vaginitis or yeast infection, prenatal vitamins, and prescription medications. Encourage pregnant travelers to consider packing a blood pressure monitor if travel will limit access to a health center where blood pressure monitoring is available.
Respiratory and urinary infections and vaginitis are more likely to occur and to be more severe during pregnancy. Pregnant people who develop travelers’ diarrhea or other gastrointestinal infections might be more vulnerable to dehydration than nonpregnant travelers. Stress the need for strict hand hygiene and food and water precautions (see Sec. 2, Ch. 8, Food & Water Precautions ). Drinking bottled or boiled water is preferable to chemically treated or filtered water. Pregnant people should not consume water purified by iodine-containing compounds because of potential effects on the fetal thyroid (see Sec. 2, Ch. 9, Water Disinfection ).
As mentioned previously, pregnant people are at increased risk for severe COVID-19–associated illness (e.g., requiring invasive ventilation or extracorporeal membrane oxygenation) and death compared with people who are not pregnant. Underlying medical conditions (e.g., chronic kidney disease, diabetes, obesity) and other factors (e.g., age, occupation) can further increase a pregnant person’s risk for developing severe illness. Additionally, pregnant people with COVID-19 are at greater risk for preterm birth and other adverse outcomes.
Pregnant people, recently pregnant people, and those who live with or visit them should take steps to protect themselves from getting COVID-19. CDC recommends that people (including those who are pregnant) not travel internationally until they are up to date with their COVID-19 vaccines . Additional information for international travelers is available at CDC's International Travel website.
Hepatitis A and hepatitis E are both spread by the fecal–oral route (see Sec. 5, Part 2, Ch. 7, Hepatitis A , and Sec. 5, Part 2, Ch. 10, Hepatitis E ). Hepatitis A has been reported to increase the risk for placental abruption and premature delivery. Hepatitis E is more likely to cause severe disease during pregnancy and could result in a case-fatality rate of 15%–30%; when acquired during the third trimester, hepatitis E is also associated with fetal complications and fetal death.
Listeriosis & Toxoplasmosis
Listeriosis and toxoplasmosis (see Sec. 5, Part 3, Ch. 23, Toxoplasmosis ) are foodborne illnesses of particular concern during pregnancy because the infection can cross the placenta and cause spontaneous abortion, stillbirth, or congenital or neonatal infection. Warn pregnant travelers to avoid unpasteurized cheeses and uncooked or undercooked meat products. Risk for fetal infection increases with gestational age, but severity of infection is decreased.
Other Parasitic Infections & Diseases
Parasitic infections and diseases can be a concern, particularly for pregnant people visiting friends and relatives in low- and middle-income countries. In general, intestinal helminths rarely cause enough illness to warrant treatment during pregnancy. Most, in fact, can be addressed safely with symptomatic treatment until the pregnancy is over. On the other hand, protozoan intestinal infections (e.g., Cryptosporidium , Entamoeba histolytica , Giardia ) often do require treatment. These parasites can cause acute gastroenteritis, severe dehydration, and chronic malabsorption resulting in fetal growth restriction. E. histolytica can cause invasive disease, including amebic liver abscess and colitis. Pregnant people also should avoid bathing, swimming, or wading in freshwater lakes, rivers, and streams that can harbor the parasitic worms (schistosomes) that cause schistosomiasis (see Sec. 5, Part 3, Ch. 20, Schistosomiasis ).
Travelers’ Diarrhea
The treatment of choice for travelers’ diarrhea is prompt and vigorous oral hydration; azithromycin or a third-generation cephalosporin may, however, be given to pregnant people if clinically indicated. Avoid use of bismuth subsalicylate because of the potential impact of salicylates on the fetus. In addition, fluoroquinolones are contraindicated in pregnancy due to toxicity to developing cartilage, as noted in experimental animal studies.
Vectorborne Infections
Pregnant people should avoid mosquito bites when traveling in areas where vectorborne diseases are endemic. Preventive measures include use of Environmental Protection Agency–registered insect repellants , protective clothing, and mosquito nets (see Sec. 4, Ch. 6, Mosquitoes, Ticks & Other Arthropods ). For details on yellow fever vaccine and malaria prophylaxis during pregnancy, see above.
Zika virus is spread primarily through the bite of an infected Aedes mosquito ( Ae. aegypti and Ae. albopictus ) but can also be sexually transmitted. The illness associated with Zika can be asymptomatic or mild; some patients report acute onset of conjunctivitis, fever, joint pain, and rash that last for several days to a week after infection.
Birth defects caused by Zika virus infection during pregnancy include brain, eye, and neurodevelopmental abnormalities. Because of the risk for birth defects, CDC recommends pregnant people avoid travel to areas with a Zika outbreak, and, for the duration of the pregnancy, to avoid sex or use condoms with anyone who has traveled to a risk area.
Advise pregnant people considering travel to areas with Zika to carefully assess the risks of Zika infection during pregnancy; provide information about prevention strategies, signs and symptoms, and the limitations of Zika testing. Pregnant people should strictly follow steps to prevent mosquito bites and sexual transmission. See additional information, including the most current list of countries and territories where Zika is active . Guidance for pregnant people can be found on the CDC Zika website .
Pregnant people should be aware of specific current environmental issues in their international destinations (e.g., natural disasters, special events or gatherings, travel warnings). More information can be found at the CDC Travelers’ Health website and on the destination pages of the US Department of State website.
Air Quality
Air pollution causes more health problems during pregnancy because ciliary clearance of the bronchial tree is slowed, and mucus is more abundant. For more details on traveling to destinations where air quality is poor, see Sec. 4, Ch. 3, Air Quality & Ionizing Radiation .
Extremes of Temperature
Body temperature regulation is not as efficient during pregnancy, and temperature extremes can create more physiological stress on the pregnant person (see Sec. 4, Ch. 2, Extremes of Temperature ). In addition, increases in core temperature (e.g., heat exhaustion, heat stroke), might harm the fetus. The vasodilatory effect of a hot environment and dehydration might cause fainting. For these reasons, then, encourage pregnant travelers to seek air-conditioned accommodations and restrict their level of activity in hot environments. If heat exposure is unavoidable, the duration should be as short as possible to prevent an increase in core body temperature. Pregnant travelers should take measures to avoid dehydration and hyperthermia.
High Elevation Travel
Pregnant people should avoid activities at high elevation unless they have trained for and are accustomed to such activities; those not acclimated to high elevation might experience breathlessness and palpitations. The common symptoms of acute mountain sickness (insomnia, headache, and nausea) frequently are associated with pregnancy, and it might be difficult to distinguish the cause of the symptoms. Most experts recommend a slower ascent with adequate time for acclimatization. No studies or case reports show harm to a fetus if the mother travels briefly to high elevations during pregnancy; recommend that pregnant people not sleep at elevations >12,000 ft (≈3,600 m) above sea level, if possible. Probably the greatest concern is that high-elevation destinations often are inaccessible and far from medical care (see Sec. 4, Ch. 5, High Elevation Travel & Altitude Illness ).
Advise pregnant people to follow safety instructions for all forms of transport and to wear seat belts, when available, on all forms of transportation, including airplanes, buses, and cars (see Sec. 8, Ch. 5, Road & Traffic Safety ). A diagonal shoulder strap with a lap belt provides the best protection. The shoulder belt should be worn between the breasts with the lap belt low across the upper thighs. When only a lap belt is available, pregnant people should wear it low, between the abdomen and across the upper thighs, not above or across the abdomen.
Most commercial airlines allow pregnant travelers to fly until 36 weeks’ gestation. Some limit international travel earlier in pregnancy, and some require documentation of gestational age. Pregnant travelers should check with the airline for specific requirements or guidance, and should consider the gestational age of the fetus on the dates both of departure and of return.
Most commercial jetliner cabins are pressurized to an equivalent outside air pressure of 6,000–8,000 ft (≈1,800–2,500 m) above sea level; travelers might also experience air pressures in this range during travel by hot air balloon or on noncommercial aircraft. The lower oxygen tension under these conditions likely will not cause fetal problems in a normal pregnancy. People with pregnancies complicated by conditions exacerbated by hypoxia (e.g., preexisting cardiovascular problems, sickle cell disease, severe anemia [hemoglobin <8.0 g/dL], intrauterine fetal growth restriction) could, however, experience adverse effects associated with low arterial oxygen saturation.
Risks of air travel include potential exposure to communicable diseases, immobility, and the common discomforts of flying. Abdominal distention and pedal edema frequently occur. The pregnant traveler might benefit from an upgrade in airline seating and should seek convenient and practical accommodations (e.g., proximity to the lavatory). Pregnant travelers should select aisle seating when possible, and wear loose fitting clothing and comfortable shoes that enable them to move about more easily and frequently during flights.
Some experts report that the risk for deep vein thrombosis (DVT) is 5–10 times greater among pregnant than nonpregnant people, although the absolute risk is low. To help prevent DVT, pregnant travelers should stay hydrated, stretch frequently, walk and perform isometric leg exercises, and wear graduated compression stockings (see Sec. 8, Ch. 3, Deep Vein Thrombosis & Pulmonary Embolism ).
Cosmic radiation during air travel poses little threat to the fetus but might be a consideration for pregnant travelers who fly frequently (see Sec. 9, Ch. 3, . . . perspectives: People Who Fly for a Living—Health Myths & Realities ). Older airport security machines are magnetometers and are not harmful to the fetus. Newer security machines use backscatter x-ray scanners, which emit low levels of radiation. Most experts agree that the risk for complications from radiation exposure from these scanners is extremely low.
Cruise Ship Travel
Most cruise lines restrict travel beyond 24 weeks’ gestation (see Sec. 8, Ch. 6, Cruise Ship Travel ). Cruise lines might require pregnant travelers to carry a physician’s note stating that they are fit to travel, including the estimated date of delivery. Pregnant people should check with the cruise line for specific requirements or guidance. For pregnant travelers planning a cruise, provide advice about gastrointestinal and respiratory infections, motion sickness (see Sec. 8, Ch. 7, Motion Sickness ), and the risk for falls on a moving vessel, as well as the possibility of delayed care while at sea.
The following authors contributed to the previous version of this chapter: Diane F. Morof, I. Dale Carroll
Bibliography
Allotey J, Stallings E, Bonet M, Yap M, Chatterjee S, Kew T, et al.; PregCOV-19 Living Systematic Review Consortium. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ. 2020;370:m3320.
Bisson DL, Newell SD, Laxton C; on behalf of the Royal College of Obstetricians and Gynaecologists. Antenatal and postnatal analgesia. BJOG. 2018;126(4):114–24.
Centers for Disease Control and Prevention. Guidelines for vaccinating pregnant women. Atlanta: The Centers; 2014. Available from: www.cdc.gov/vaccines/pregnancy/hcp-toolkit/guidelines.html .
Dotters-Katz S, Kuller J, Heine RP. Parasitic infections in pregnancy. Obstet Gynecol Surv. 2011;66(8):515–25.
Hezelgrave NL, Whitty CJ, Shennan AH, Chappell LC. Advising on travel during pregnancy. BMJ. 2011;342:d2506.
Irvine MH, Einarson A, Bozzo P. Prophylactic use of antimalarials during pregnancy. Can Fam Physician. 2011;57(11):1279–81.
Magann EF, Chauhan SP, Dahlke JD, McKelvey SS, Watson EM, Morrison JC. Air travel and pregnancy outcomes: a review of pregnancy regulations and outcomes for passengers, flight attendants, and aviators. Obstet Gynecol Surv. 2010;65(6):396–402.
Rasmussen SA, Jamieson DJ, Honein MA, Petersen LR. Zika virus and birth defects—reviewing the evidence for causality. N Engl J Med. 2016;374(20):1981–7.
Rasmussen SA, Watson AK, Kennedy ED, Broder KR, Jamieson DJ. Vaccines and pregnancy: past, present, and future. Semin Fetal Neonatal Med. 2014;19(3):161–9.
Roggelin L, Cramer JP. Malaria prevention in the pregnant traveller: a review. Travel Med Infect Dis. 2014;12(3):229–36.
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Altitude Sickness
- Sleeplessness
- Traveler’s Diarrhea
- Motion Sickness
- Malaria Prevention
Top Countries
- South Africa
Have a question?
Runway offers travelers like you, the medications you may need before you go. Email us at anytime.
- Nausea Prevention
- How it works
Email us at anytime at:
Motion Sickness During Pregnancy – Everything to Know
18 Jan 2024
Photographer
Motion sickness during pregnancy can be a challenging aspect of expecting mothers’ lives.
While the experience varies from woman to woman, understanding the causes, symptoms, and potential management strategies is crucial for those dealing with this discomfort.
This article provides a comprehensive overview of motion sickness during pregnancy, covering its definition, common triggers, symptoms, and practical measures to alleviate the unease.
Understanding Motion Sickness in Pregnancy
Motion sickness, often referred to as travel sickness, is a condition where an individual feels nauseous and dizzy when exposed to certain types of motion, such as traveling in a car, airplane, or boat.
During pregnancy, hormonal changes, particularly the increased levels of estrogen, can influence the susceptibility to motion sickness. The combination of altered hormonal balance and the physical changes occurring in the body can contribute to a heightened sensitivity to motion stimuli.
Causes of Motion Sickness During Pregnancy
Hormonal changes.
The primary driver behind motion sickness during pregnancy is the hormonal shift, specifically the rise in estrogen levels. This hormone affects the inner ear, a key component of the body’s balance system, leading to an increased likelihood of experiencing motion-related discomfort.
Physical Changes
As pregnancy progresses, the growing uterus exerts pressure on nearby organs, including the stomach. This physical change can contribute to feelings of nausea and discomfort, especially when subjected to motion.
Increased Sensitivity
Pregnant women may experience heightened sensitivity to various stimuli, including odors and motions. This heightened sensitivity can exacerbate the symptoms of motion sickness when exposed to certain environments or activities.
Symptoms of Motion Sickness in Pregnancy
- Nausea and Vomiting — The hallmark symptoms of motion sickness during pregnancy include nausea and, in some cases, vomiting. These symptoms can range from mild discomfort to more pronounced feelings of queasiness.
- Dizziness — Feelings of dizziness or lightheadedness are common manifestations of motion sickness. The altered balance mechanisms in the inner ear contribute to these sensations when exposed to motion.
- Sweating and Pallor — Some pregnant women experiencing motion sickness may notice increased sweating and a paler complexion. These physiological responses are the body’s reactions to the perceived stress associated with motion discomfort.
Managing Motion Sickness During Pregnancy
Choose the right mode of transportation.
Opting for modes of transportation that allow for a smoother ride can help minimize motion sickness. Consider choosing a larger, more stable vehicle or opting for a seat with minimal motion, such as the front seat in a car.
Stay Hydrated and Maintain a Light Diet
Dehydration can exacerbate feelings of nausea, so staying adequately hydrated is crucial. Additionally, maintaining a light diet and avoiding heavy or greasy meals before travel can help reduce the risk of motion sickness.
Focus on a Fixed Point
When in motion, focusing on a fixed point, such as the horizon, can help stabilize visual input and alleviate symptoms. This technique helps the brain reconcile conflicting signals from the inner ear and eyes.
Take Breaks and Get Fresh Air
Taking breaks during travel, especially on long journeys, allows for brief periods of rest and fresh air. Stepping outside and breathing in fresh air can contribute to a sense of relief from motion sickness.
Consultation with Healthcare Professionals
When to seek medical advice.
- While motion sickness during pregnancy is generally a temporary and manageable condition, seeking medical advice becomes essential in certain situations.
- If the symptoms are severe, persistent, or significantly impacting the well-being of the pregnant woman, consulting with a healthcare professional is advisable.
- Additionally, if there are concerns about the effects of motion sickness on the developing fetus or if there are pre-existing medical conditions, medical guidance should be sought.
Medication Considerations
Healthcare providers may recommend certain medications to alleviate motion sickness symptoms during pregnancy. However, the use of medications like a scopolamine patch prescription should be approached with caution, especially during the first trimester when the fetus is most vulnerable to potential adverse effects. Any medication, whether over-the-counter or prescription, should be discussed with a healthcare professional to ensure it is safe and appropriate for the specific circumstances.
Preventive Measures for Travel During Pregnancy
Plan travel during the second trimester.
The second trimester is often considered the most comfortable time for travel during pregnancy. By this stage, many women have passed the initial period of morning sickness, and the physical discomfort associated with the third trimester has not yet set in. Planning trips during this window can enhance the overall travel experience.
Consider Motion Sickness Bands
Acupressure bands, often worn around the wrists, are a non-invasive option to manage motion sickness. Some pregnant women find relief using these bands, which apply pressure to specific points believed to alleviate nausea and vomiting.
Travel During Off-Peak Hours
Choosing to travel during off-peak hours can contribute to a smoother experience. This may involve avoiding rush hours when traffic is heavy or selecting flights during less crowded times. Less crowded environments can reduce the overall sensory stimuli and minimize the risk of motion sickness.
Inform Travel Companions
Open communication with travel companions is crucial. Informing them about the potential for motion sickness and discussing strategies to make the journey more comfortable can foster understanding and support. Travel companions can play a significant role in creating a supportive environment during the trip.
Next, we will delve into additional considerations for pregnant individuals dealing with motion sickness, including self-care measures, the impact of multiple modes of transportation, and coping strategies that can be implemented during travel. By addressing these aspects comprehensively, pregnant women can equip themselves with practical insights for a smoother journey despite the challenges of motion sickness.
Coping Strategies and Self-Care During Travel
Ensuring proper ventilation during travel can be beneficial for pregnant individuals dealing with motion sickness. Fresh air can help alleviate feelings of nausea and create a more comfortable environment. When possible, open windows or choose modes of transportation with good airflow.
- Engaging in distraction techniques can redirect focus and alleviate symptoms. Bringing along entertainment such as books, music, or podcasts can be helpful.
- Additionally, focusing on conversation with travel companions or observing the surroundings can divert attention away from motion discomfort.
- Incorporating relaxation techniques into the travel routine can contribute to a calmer experience. Techniques such as deep breathing, guided imagery, or meditation can help manage stress and reduce the intensity of motion sickness symptoms.
Choosing loose, comfortable clothing for travel can enhance overall comfort. Tight or constrictive clothing may exacerbate feelings of nausea, so opting for breathable and relaxed attire is advisable.
Impact of Multiple Modes of Transportation
Combination of modes.
Travel itineraries involving a combination of transportation modes, such as a car followed by a boat or a plane, can increase the risk of motion sickness. The cumulative effect of different motions can intensify symptoms. Planning for breaks between modes of transportation and allowing time for the body to adjust can help mitigate this impact.
Choose Direct Routes
Opting for direct routes whenever possible can minimize the duration of travel and exposure to varying motions. Direct flights or non-stop car rides reduce the likelihood of experiencing motion sickness associated with multiple take-offs, landings, or changes in speed and direction.
Final Thoughts: Navigating Motion Sickness During Pregnancy
Motion sickness during pregnancy is a common challenge that many expectant mothers face. By understanding the causes, symptoms, and management strategies, pregnant individuals can navigate their journeys more comfortably. From practical measures like choosing the right mode of transportation and staying hydrated to preventive measures and self-care techniques, there are various strategies to alleviate motion sickness.
As each pregnancy is unique, it’s essential for pregnant individuals to tailor these strategies to their specific needs and consult with healthcare professionals when necessary. The second trimester may offer a more comfortable window for travel, and the use of acupressure bands or medication under medical guidance can provide additional support.
Open communication with travel companions, planning for breaks, and incorporating relaxation techniques are valuable tools for managing motion sickness. By adopting a proactive and informed approach, pregnant women can enhance their overall travel experience and focus on the positive aspects of their journey.

Emergency Response to Malaria within Endemic Regions

How Long Does Motion Sickness Last?
Runway offers travelers like you, the medications you may need before you go.
Flying while pregnant? Here’s what you need to know

Editors note: This guide has been updated with the latest information.
During pregnancy, seemingly harmless things like eating deli meat and cleaning your cat's litter box are suddenly off-limits, along with more obvious restrictions on sports like skiing and scuba diving.
But what about "grey area" activities like flying in an airplane?
There's no single set of guidelines governing air travel during pregnancy and every airline has different restrictions, timelines and requirements. Some airlines may also require a medical certificate from a primary attending doctor or midwife for air travel during the final months of pregnancy, though even that varies, with U.S. airlines typically offering more flexibility than international carriers.
For more TPG news delivered each morning to your inbox, sign up for our daily newsletter .
In the absence of clear guidelines, TPG turned to Dr. Nithya Gopal , a board-certified OB-GYN physician and the Director of OB-GYN services at Viva Eve in New York City, for her expert recommendations on safe air travel during pregnancy.
Here's what she had to say:
Is it safe to fly when you are pregnant?
There is no evidence of adverse pregnancy outcomes due to flying, according to Dr. Gopal.
"The general consensus is that it is safest to fly in the first and second trimesters," Dr. Gopal told The Points Guy. "While the first and third trimesters tend to be when the most obstetric emergencies are going to happen, I personally become more cautious with my patients after 32 weeks because of the increased risk for premature labor and the possibility of needing urgent medical attention when you are in the sky."

The most important thing you can do, no matter how far along you are in your pregnancy, is to consult with your healthcare provider before flying.
"Any time you are planning to fly during pregnancy , you should be having that conversation," Dr. Gopal said. Your provider will be familiar with any safety precautions you should take to ensure a safe and healthy flight.
Related: Guide to flying in each trimester of pregnancy
The airline you are flying may have its own cutoff, so you will want to confirm with it beforehand whether you will be allowed to fly if you are in (or nearing) your third trimester. We've included a chart below that outlines the rules for most major airline carriers.
What can you do to stay comfortable on a flight?

When you factor in morning sickness and general pregnancy discomfort with the increased risk for blood clots that all fliers need to be aware of, flying during pregnancy can be uncomfortable even when it is deemed safe.
Dr. Gopal shared her recommendations for addressing these common issues when you take to the (baby-) friendly skies during pregnancy. Her number one tip for staying comfortable while in flight is to wear compression socks to help maintain blood flow and reduce swelling in the legs.
In addition, "I also tell my patients to get up and move at least every hour when they are on the plane," Dr. Gopal said.
To prevent clotting, "some doctors may also prescribe a low-dose aspirin," she added. "It isn't something that is recommended by the American College of Obstetricians and Gynecologists (ACOG), but it isn't harmful, either."
If it's nausea or acid reflux that ail you, there are medications generally considered safe that you can take to alleviate your symptoms. These would be the same ones prescribed by your doctor for morning sickness, so speak with your provider before your flight to ensure you have what you need at the ready.
Dr. Gopal also advises wearing loose, unrestrictive clothing (along with your seatbelt, or course) and drinking extra fluids to counteract the pressurized air in the cabin and keep you hydrated.
"Over-the-counter Gas-X may also help with bloating that can happen as a result of the pressurized air," Dr. Gopal said.
Related: What happens when a baby is born in flight?
Must you speak with your healthcare provider before flying?

Even if your pregnancy is considered low-risk, it's always a smart idea to speak with your healthcare provider before flying. "There are a number of potential risks that go along with flying during pregnancy and those risks can change from week to week and month to month, so it's important to have that honest conversation with your doctor," Dr. Gopal said.
Related: Things You Should Do Before, During and After Flying to Stay Healthy
There are certain pregnancy conditions that may make flying more risky or unadvisable. If you are hypertensive, asthmatic or prone to clotting disorders, it's even more critical to speak with your doctor before flying.
Airline policies differ, but if you need documentation, it never hurts to include enough detail to satisfy the most stringent airline requirements.
"As with many things related to air travel, it's better to be safe than sorry," Dr. Gopal said. "It's definitely worth it, and sometimes necessary, to have medical documentation from your provider's office."
A thorough medical certificate or waiver should state:
- The number of weeks of pregnancy.
- The estimated delivery date.
- Whether the pregnancy is single or multiple.
- Whether there are any complications.
- That you are in good health and fit to travel through the date of your final flight.
Additionally, the certificate should be:
- Written on official clinic or hospital letterhead if possible.
- Signed by the doctor or attending midwife.
- Be dated no later than 72 hours before the departure date.
- Be written in clear, simple English.
Carry this certificate with you on your flight. Some airlines won't ask to see it, but others will. Some airlines also may have their own documentation requirements. See the chart below to find out which airlines require it.
Airline policies for pregnant women
Bottom line.

Even though it may be deemed safe, flying during pregnancy can be uncomfortable — and it is perfectly acceptable to implement your own cutoff for flying with your baby bump in tow. The majority of the time, though, flying is perfectly safe during pregnancy, providing that you follow the guidelines of the airline and your healthcare provider. Read on to learn more about traveling before, during and after pregnancy:
- What to expect in every trimester of pregnancy
- 4 tips for planning travel while planning a pregnancy
- Babymoon boom! These are the top 10 spots for a US getaway before the baby comes
- Flying with a baby checklist
Additional reporting by Katherine Fan and Tarah Chieffi.
Appointments at Mayo Clinic
- Pregnancy week by week
Is it safe to fly during pregnancy?
Generally, air travel before 36 weeks of pregnancy is considered safe for people who aren't dealing with any pregnancy problems. Still, if you're pregnant, it's a good idea to talk with your health care provider before you fly.
Your provider might suggest that you not fly if you have certain pregnancy complications that could get worse because of air travel or that could require emergency care. Examples include a history of miscarriage or vaginal bleeding, severe anemia, and high blood pressure or diabetes that's not well controlled. If you had preeclampsia during a previous pregnancy — a condition that causes high blood pressure and extra protein in urine — flying may not be advised. The same is true if you're pregnant with twins or other multiples.
Tell your provider how far you are flying, as the length of the flight might make a difference. Also, be aware that some airlines may not allow pregnant people on international flights. Check with your airline before you make travel arrangements.
After 36 weeks of pregnancy, your health care provider may advise against flying. And some airlines don't allow pregnant people to fly after 36 weeks. The airline also may require a letter from your health care provider that states how far along in your pregnancy you are and whether flying is advised.
If your health care provider says it's okay for you to fly, and your plans are flexible, the best time to travel by air might be during the second trimester. The risks of common pregnancy emergencies are lowest during that time.
When you fly:
- Buckle up. During the trip, keep your seatbelt fastened when you are seated, and secure it under your belly.
- Drink plenty of fluids. Low humidity in the airplane could cause you to become dehydrated.
- Avoid gassy foods and drinks before you fly. Gases expand during flight, and that could make you uncomfortable. Examples of foods and drinks to avoid include broccoli and carbonated soda.
- Think about medical care. Plan for how you'll get obstetric care during your trip if you need it. Bring copies of your medical information in case you need care while you're away.
Blood clots
Air travel can raise the risk for blood clots in the legs, a condition called venous thrombosis. The risk is higher for pregnant people. Moving your legs may help prevent this problem. Take a walk up and down the aisle every hour during the flight. If you must remain seated, flex and extend your ankles from time to time. In general, it's best to avoid tightfitting clothing, as that can hinder blood flow. Wearing compression stockings can help with blood circulation during a long flight.
Radiation exposure linked to air travel at high altitudes isn't thought to be a problem for most people who fly during pregnancy. But pilots, flight attendants and others who fly often might be exposed to a level of radiation that raises concerns during pregnancy. If you must fly frequently during your pregnancy, talk about it with your health care provider.
Mary Marnach, M.D.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Allergy medications during pregnancy
- AskMayoExpert. Health considerations for air travelers: Pregnancy considerations. Mayo Clinic; 2022.
- Air Travel During Pregnancy: ACOG Practice Bulletin No. 746. American College of Obstetricians and Gynecologists. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/08/air-travel-during-pregnancy. Accessed Dec. 1, 2022.
- Ram S, et al. Air travel during pregnancy and the risk of venous thrombosis. American Journal of Obstetrics and Gynecology. 2022; doi:10.1016/j.ajogmf.2022.100751.
Products and Services
- Available Solutions for Prenatal Nutrition from Mayo Clinic Store
- A Book: Taking Care of You
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- Ankle swelling during pregnancy
- Antibiotics and pregnancy
- Aspirin during pregnancy
- Pregnancy back pain
- Falling during pregnancy: Reason to worry?
- Fetal ultrasound
- Flu shot in pregnancy
- Headaches during pregnancy: What's the best treatment?
- Iron deficiency anemia during pregnancy: Prevention tips
- Leg cramps during pregnancy
- Pregnancy acne
- Pregnancy and fish
- Pregnancy constipation
- Pregnancy diet: Essential nutrients
- Pregnancy due date calculator
- Pregnancy exercises
- Pregnancy nutrition don'ts
- Pregnancy stretches
- Pregnancy weight gain
- Pregnant. Now What Happens?
- Prenatal testing
- Prenatal vitamins and pregnancy
- Sex during pregnancy
- Twin pregnancy
- Vaccines during pregnancy
- Vaping during pregnancy
- Working during pregnancy
- X-ray during pregnancy
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Expert Answers
- Air travel during pregnancy Is it safe
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
Travelling in pregnancy
With the proper precautions such as travel insurance, most women can travel safely well into their pregnancy.
Wherever you go, find out what healthcare facilities are at your destination in case you need urgent medical attention. It's a good idea to take your maternity medical records (sometimes called handheld notes) with you so you can give doctors the relevant information if necessary.
Find out more about getting healthcare abroad .
Make sure your travel insurance covers you for any eventuality, such as pregnancy-related medical care during labour, premature birth and the cost of changing the date of your return trip if you go into labour .
When to travel in pregnancy
Some women prefer not to travel in the first 12 weeks of pregnancy because of nausea and vomiting and feeling very tired during these early stages. The risk of miscarriage is also higher in the first 3 months, whether you're travelling or not.
Travelling in the final months of pregnancy can be tiring and uncomfortable. So, many women find the best time to travel or take a holiday is in mid-pregnancy, between 4 and 6 months.
Flying in pregnancy
Flying isn't harmful to you or your baby, but discuss any health issues or pregnancy complications with your midwife or doctor before you fly.
The chance of going into labour is naturally higher after 37 weeks (around 32 weeks if you're carrying twins), and some airlines won't let you fly towards the end of your pregnancy. Check with the airline for their policy on this.
After week 28 of pregnancy, the airline may ask for a letter from your doctor or midwife confirming your due date, and that you are not at risk of complications. You may have to pay for the letter and wait several weeks before you get it.
Long-distance travel (longer than 4 hours) carries a small risk of blood clots (deep vein thrombosis (DVT)) . If you fly, drink plenty of water and move about regularly – every 30 minutes or so. You can buy a pair of graduated compression or support stockings from the pharmacy, which will help reduce leg swelling.
Travel vaccinations when you're pregnant
Most vaccines that use live bacteria or viruses aren't recommended during pregnancy because of concerns that they could harm the baby in the womb.
However, some live travel vaccines may be considered during pregnancy if the risk of infection outweighs the risk of live vaccination. Ask your GP or midwife for advice about specific travel vaccinations. Non-live (inactivated) vaccines are safe to use in pregnancy.
Malaria tablets
Some anti-malaria tablets aren't safe to take in pregnancy so ask your GP for advice.
Zika virus is mainly spread by mosquitoes found in some parts of the world. For most people it's mild and not harmful, but can cause problems if you're pregnant.
If you are pregnant, it is not recommended to travel to parts of the world where the Zika virus is present, such as parts of:
- South and Central America
- the Caribbean
- the Pacific islands
Check before you travel
It's important to check the risk for the country you're going to before you travel.
Find out more about the Zika virus risk in specific countries on the Travel Health Pro website
Car travel in pregnancy
It's best to avoid long car journeys if you're pregnant. However, if it can't be avoided, make sure you stop regularly and get out of the car to stretch and move around.
You can also do some exercises in the car (when you're not driving), such as flexing and rotating your feet and wiggling your toes. This will keep the blood flowing through your legs and reduce any stiffness and discomfort. Wearing compression stockings while on long car journeys (more than 4 hours) can also increase the blood flow in your legs and help prevent blood clots.
Tiredness and dizziness are common during pregnancy so it's important on car journeys to drink regularly and eat natural, energy-giving foods, such as fruit and nuts.
Keep the air circulating in the car and wear your seatbelt with the cross strap between your breasts and the lap strap across your pelvis under your bump, not across your bump.
Road accidents are among the most common causes of injury in pregnant women. If you have to make a long trip, don't travel on your own. You could also share the driving with your companion.
Sailing in pregnancy
Ferry companies have their own restrictions and may refuse to carry heavily pregnant women (often beyond 32 weeks on standard crossings and 28 weeks on high-speed crossings ). Check the ferry company's policy before you book.
For longer boat trips, such as cruises, find out if there are onboard facilities to deal with pregnancy and medical services at the docking ports.
Food and drink abroad in pregnancy
Take care to avoid food- and water-borne conditions, such as stomach upsets and travellers' diarrhoea . Some medicines for treating stomach upsets and travellers' diarrhoea aren't suitable during pregnancy.
Always check if tap water is safe to drink. If in doubt, drink bottled water. If you get ill, keep hydrated and continue eating for the health of your baby, even if you're not hungry.
Find out about a healthy diet in pregnancy , and foods to avoid in pregnancy .
Page last reviewed: 17 August 2022 Next review due: 17 August 2025
- Skip to main content
- Skip to site information
Language selection
Help us to improve our website. Take our survey !
Travelling while pregnant
Find useful information and considerations to help you prepare for safe and healthy travels outside Canada while pregnant.
With careful preparation, travelling while pregnant can be safe. The decision to travel should be made in consultation with your health care professional, based on your personal health circumstances.
On this page
Before you go, while you're away, if you need help.
Medical practices, health standards and infection control measures vary from country to country. You may not have access to the same level of care, procedures, treatments and medications as you would in Canada.
You could also be at increased risk of getting an infection and/or developing severe complications from certain infections, which could also affect the fetus.
Before leaving Canada:
- consult a health care professional or visit a travel health clinic at least 6 weeks before travelling to get personalized health advice and recommendations
- check our Travel Advice and Advisories for country-specific information, including about possible health risks
- know how to seek medical assistance outside of Canada
- review the policy and the coverage it provides
- most policies do not automatically cover pregnancy-related conditions or hospital care for premature infants
- ask your insurance provider about coverage for medical care during pregnancy, giving birth and intensive care for you and your fetus or newborn
- carry a copy of your prenatal records
- talk to your health care professional about any additional items you may want to bring that are specific to your health needs
Local laws and medical services relating to pregnancy can differ from Canada. Learn the local laws, and how these may apply to you before you travel.
Pre-travel vaccines and medications
Many vaccines can be safely given during pregnancy. Due to a higher risk of more severe outcomes for you and your fetus, some vaccines are recommended specifically during pregnancy, such as tetanus-diphtheria-pertussis (DTaP) and influenza.
Don’t take medications you may still have from prior trips. Tell the health care professional about your pregnancy, or intended pregnancy, before filling any prescriptions. The decision to get any pre-travel vaccinations or medications should be discussed with your health care professional.
The decision can depend on:
- your purpose of travel (e.g., tourism, visiting friends and relatives)
- your planned destination(s)
- the length of your trip
- your risk of getting a disease
- how severe the effect of a disease would be to you and/or your fetus
- your planned activities
- any underlying medical issues and/or pregnancy-related complications
Malaria could cause major health problems for a mother and her unborn baby. A pregnant woman may want to consider avoiding travel to areas where malaria transmission occurs.
Description of malaria risk by country and preventative measures.
If you can’t avoid travelling to an area where malaria is present:
- some medications to prevent or treat malaria may not be safe during pregnancy
- take extra care to protect yourself from mosquito bites
Zika virus infection during pregnancy can pose significant risks to your fetus even if you don’t develop symptoms. While pregnant, you may want to consider avoiding travelling to a country or areas with risk of Zika virus.
Latest travel health advice on Zika virus.
If you choose to travel, take precautions to avoid infection with Zika virus:
- prevent mosquito bites at all times
- protect yourself from contact with semen, vaginal fluid and blood
- always use condoms correctly or avoid sexual contact while in countries or areas with risk of Zika virus
Learn more about Zika virus and pregnancy:
- Zika virus: Pregnant or planning a pregnancy
- Zika virus: Advice for travellers
- Pregnancy and travel (tropical medicine and travel)
Monitor your health and be prepared
Emergencies can happen at any time. Know where the nearest hospital or medical centre is while you are travelling and confirm they will accept your medical insurance.
Seek medical attention immediately if you develop any of the following symptoms while travelling:
- persistent vomiting and/or diarrhea
- dehydration
- vaginal bleeding
- passing tissue or clots
- abdominal pain, cramps or contractions
- your water breaks
- excessive swelling of face, hands or legs
- excessive leg pain
- severe headaches
- visual problems
If you develop these symptoms after your return to Canada, you should see a health care professional immediately and tell them about your recent trip.
Transportation
Always wear a seatbelt when travelling by plane or car. When using a diagonal shoulder strap with a lap belt, the straps should be placed carefully above and below your abdomen. If only a lap belt is available, fasten it at the pelvic area, below your abdomen.
If you have any medical or pregnancy-related complications, discuss with your health care professional whether air travel is safe for you.
Most airlines restrict travel in late pregnancy or may require a written confirmation from a physician. Check this with the airline before booking your flight.
During long flights, you may be at higher risk of developing blood clots, known as deep vein thrombosis (DVT). The risk of deep vein thrombosis can be reduced by:
- getting up and walking around occasionally
- exercising and stretching your legs while seated
- selecting an aisle seat when possible
- wearing comfortable shoes and loose clothing
Your health care professional may recommend additional ways to reduce your risk such as wearing compression stockings.
Always stay well hydrated while travelling.
Land travel
The risk of deep vein thrombosis can be reduced by:
- stopping the vehicle to walk around every couple of hours
Motion sickness
Certain medications used to treat nausea and vomiting during pregnancy may also be effective in relieving motion sickness.
If you think you might experience motion sickness during your trip, speak to your health care professional about the use of these medications.
Environmental and recreational risks
Some activities may not be recommended or may require additional precautions. Discuss your travel plans, including any planned or potential recreational activities with a health care professional.
High altitude
You should avoid travelling to an altitude above 3,658 metres (12,000 feet).
However, if you have a high-risk pregnancy and/or are in the late stages of pregnancy, the highest altitude should be 2,500 metres (8,200 feet).
If you have pregnancy-related complications, you should avoid unnecessary high-altitude exposure.
Keep in mind that most high-altitude destinations are far from medical care services.
Personal protective measures
Food-borne and water-borne diseases.
Eat and drink safely while travelling while travelling. Many food-borne and water-borne illnesses can be more severe during pregnancy and pose a risk to the fetus.
This can include:
- toxoplasmosis
- listeriosis
- hepatitis A and E
To help avoid food-borne and water-borne diseases:
- before eating or preparing food
- after using the bathroom or changing diapers
- after contact with animals or sick people
- before and after touching raw meat, poultry, fish and seafood
- if you’re at a destination that lacks proper sanitation and/or access to clean drinking water, only drink water if it has been boiled or disinfected or if it’s in a commercially sealed bottle
- use ice made only from purified or disinfected water
- this could cause the fetus or newborn to develop thyroid problems
- unpasteurized dairy products, such as raw milk and raw milk soft cheeses
- unpasteurized juice and cider
- raw or undercooked eggs, meat or fish, including shellfish
- raw sprouts
- non-dried deli meats, including bologna, roast beef and turkey breast
- don’t use bismuth subsalicylate (Pepto-Bismol®)
- Information on travellers’ diarrhea
Illnesses acquired from insect and other animals
Protect yourself from insect bites:
- wear light-coloured, loose clothes made of tightly woven materials such as nylon or polyester
- prevent mosquitoes from entering your living area with screening and/or closed, well-sealed doors and windows
- use insecticide-treated bed nets if mosquitoes can’t be prevented from entering your living area
- information on insect bite and pest prevention
Some infections, such as rabies and influenza, can be shared between humans and animals. You should avoid contact with animals including dogs, livestock (pigs, cows), monkeys, snakes, rodents, birds, and bats.
Information for if you become sick or injured while travelling outside Canada.
For help with emergencies outside Canada, contact the:
- nearest Canadian office abroad
- Emergency Watch and Response Centre in Ottawa
More information on services available at consular offices outside Canada.
Related links
- Immunization in pregnancy and breastfeeding: Canadian Immunization Guide
- Advice for Canadians travelling to Zika-affected countries
- Advice for women travellers
- If you get sick before or after returning to Canada
- Receiving medical care in other countries
- Travel vaccinations
- What you can bring on a plane
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
Is it safe to travel to high altitudes while pregnant?

Take care while traveling to high altitudes while pregnant: It isn't always recommended, depending on where you go and how you respond to being there.
At high altitudes, less oxygen is available, which means you'll tire more easily. It also means your baby will get less oxygen, which can negatively affect growth and development.
There isn't much research on the effects of traveling to high altitudes during pregnancy. One study of about 450 women who frequently traveled to and exercised at high altitudes during pregnancy didn't find increased risk of complications, though the study's authors said further research is needed to be sure it's safe.
The Centers for Disease Control and Prevention recommends that pregnant women who are traveling avoid staying at altitudes at or higher than 8,500 feet above sea level for more than a few days, and if possible, avoid sleeping at altitudes higher than 12,000 feet. (Denver is 5,280 feet above sea level and would probably be fine, for example; but Pikes Peak, at more than 14,000 feet above sea level, might not be safe.)
Women respond differently to high altitudes during pregnancy. The symptoms of altitude sickness are often similar to typical pregnancy symptoms – dizziness , shortness of breath , lightheadedness, headaches , and trouble sleeping – so it can be hard to tell if you're suffering from altitude sickness or just going through pregnancy. But if you're getting less oxygen than you're used to and you can feel it, your baby may not be getting as much oxygen, either.
If you feel sick while traveling at higher altitudes than you're used to, go to a lower altitude. And if you still don't feel well after you descend, seek medical care.
The CDC also recommends avoiding strenuous physical activity while at high altitudes during pregnancy (unless you're already trained for exercise at high altitude), since you may experience breathlessness and palpitations. If you're planning a vacation at a higher elevation, plan extra time to acclimate before you jump into any physical activity, and you may need to avoid some activities altogether , like skiing or hiking.
One of the biggest concerns about traveling to higher altitudes during pregnancy is these locations are often remote and far from medical care. Some pregnant women need to be especially careful in these situations. If you have hypertension , preeclampsia , or any other high-risk pregnancy condition, going to high altitudes may make your condition worse – and you could be far from the care you need in case of an emergency. Talk with your healthcare provider before making travel plans.
Research shows that repeated exposure to hypoxia – not getting enough oxygen – during pregnancy increases your risk of preeclampsia and can impact your baby's growth. But if you're just traveling to a high altitude for a few days during your pregnancy and you don't experience noticeable altitude sickness, there's no need to worry.
As for women who live at altitudes higher than 8,500 feet, their bodies have made adjustments over time, including higher levels of red blood cells (more hemoglobin), increased numbers of small blood vessels, and increased proteins in the muscles that store oxygen. These adaptations help people function at higher altitudes.
Babies born to moms living at high elevations tend to be smaller than babies born at lower altitudes. Pregnant women living at high altitudes are at two to three times greater risk of preeclampsia and intrauterine growth restriction . For women whose ancestors lived at high elevations for thousands of years (such as those in Bolivia, Peru, or Tibet), the risk of growth restriction is reduced due to evolutionary adjustments, although their babies are smaller on average than those at lower altitudes.
Was this article helpful?
Is it safe to fly while I'm pregnant?

Is it safe to travel at high altitudes with a baby?

Can you go to a concert while pregnant?

Traveling while pregnant: Your complete guide

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
CDC. 2019. Pregnant Travelers. http://wwwnc.cdc.gov/travel/yellowbook/2014/chapter-8-advising-travelers-with-specific-needs/pregnant-travelers Opens a new window [Accessed November 2021]
Jean D, et al. 2012. Travel to high altitude during pregnancy: Frequently asked questions and recommendations for clinicians. High Altitude Medicine and Biology 13(2):73-81. http://www.ncbi.nlm.nih.gov/pubmed/22724609 Opens a new window [Accessed November 2021]
Julian CG, et al. 2014. Inhibition of peroxisome proliferator-activated receptor gamma: A potential link between chronic maternal hypoxia and impaired fetal growth. FASEB Journal 28(3):1268-79. http://www.ncbi.nlm.nih.gov/pubmed/24307415 Opens a new window [Accessed November 2021]
Julian, CG. 2011. High altitude during pregnancy. Clinics in Chest Medicine 32(1):21-31. http://www.ncbi.nlm.nih.gov/pubmed/21277446 Opens a new window [Accessed November 2021]
Zamudio, S. 2007. High-altitude hypoxia and preeclampsia. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6428070/ Opens a new window [Accessed November 2021]
Keyes L, et al. 2016. Outdoor Activity and High Altitude Exposure During Pregnancy: A Survey of 459 Pregnancies. Wilderness & Environmental Medicine 27(2):227-35. https://www.wemjournal.org/article/S1080-6032(16)00107-1/fulltext [Accessed November 2021]
Krampl, E. 2002. Pregnancy at high altitude. Ultrasound in Obstetrics & Gynecology 19:535-39. https://obgyn.onlinelibrary.wiley.com/doi/pdf/10.1046/j.1469-0705.2002.00738.x Opens a new window [Accessed November 2021]
Palmer SK, et al. 1999. Altered blood pressure course during normal pregnancy and increased preeclampsia at high altitude (3,100 meters) in Colorado. American Journal of Obstetrics and Gynecology 180(5):1161-68. https://pubmed.ncbi.nlm.nih.gov/10329872/ Opens a new window [Accessed November 2021]
Keyes L, et al. 2003. Intrauterine growth restriction, preeclampsia, and intrauterine mortality at high altitude in Bolivia. Pediatric Research 54:20-25. https://pubmed.ncbi.nlm.nih.gov/12700368/ Opens a new window [Accessed November 2021]
Glyde Julian C, et al. 2009. Augmented uterine artery blood flow and oxygen delivery protect Andeans from altitude-associated reductions in fetal growth. American Journal of Physiology 296(5):1564-75. https://pubmed.ncbi.nlm.nih.gov/19244584/ Opens a new window [Accessed November 2021]

Rebekah Wahlberg is a senior associate editor and baby name trends specialist at BabyCenter, the world's number one digital parenting resource. She lives in Southern California with her silly dog Booger, where she enjoys hiking, yoga, and watching Netflix when she "should" be reading. Wahlberg is passionate about creating content that helps parents and parents-to-be equip themselves with everything they need to succeed.
Where to go next

How to Make Long Flights More Comfortable When You're Pregnant
By Joanna Carrigan

All products featured on Condé Nast Traveler are independently selected by our editors. However, when you buy something through our retail links, we may earn an affiliate commission.
Preparing for a newborn can feel like an exhilarating task; on the one hand, there’s a long-anticipated, already much-loved new arrival making an entrance into your life. On the other, getting yourself into a birthing headspace can feel like a marathon. I’ve already lost count of the amount of stroller reviews , hypno-birthing manuals, crib catalogs, and paint samples I’ve flicked through in my quest for newborn nirvana.
With that in mind, many couples are now opting to take a break from the organizational overload in the form of a long-haul babymoon —a pre-birth couples vacation—as a way of spending those last special moments together as a family of two. And in fact, air travel can generally be considered safe for most expectant mothers , with advice from your doctor recommended.
“All pregnancies and mums have individual needs and varying circumstances,” says Marie Louise, midwife and author of The Modern Midwife’s Guide To Pregnancy . “If mums have any health complications or are close to giving birth, travel should be very carefully considered. Otherwise, mums need a break—it’s good to enjoy and relax on your travels.”
Pregnancy can often feel like a long-haul adventure in itself, and whilst the thought of an extensive flight may not jump out at the top of your to-do list, there are ways to make that coveted trip—and any other air travel during pregnancy that comes up—more comfortable.
Below, I’ve curated an essential list for what to pack in your carry-on for air travel during pregnancy, based in part on my own experience traveling to Europe whilst expecting.
Strategic carry-ons
A great place to start is your carry-on itself, as the right style can help not only to make your essentials more accessible, but the correct product can be re-used as a diaper bag once your pre-baby vacation is a distant happy memory. The key to choosing the perfect carry-on is not only to be mindful of the airline guidelines set out around dimensions and weight restrictions, but to think from your own perspective about what will be easiest for you to carry. If back issues prevail—a common complaint during pregnancy—a stylish rucksack may be more suitable than a tote. And if you’re looking for post-pregnancy practicality, a duffel can tick that cross-functional box.

Pregnancy support bands
Glamour takes a back seat with this essential, but your posture and ligaments will thank me later. If you’re flying internationally or just maneuvering your way through a large airport, you may face long walks between terminals, which can place strain on the lower back. Bump support bands are designed to help relieve the pressure that the additional weight of your bump is putting on your back, and therefore can make a sensible addition to your carry-on packing list.

Anti-nausea pregnancy methods
Not every foray into the world of parenthood is a smooth one, and unfortunately nausea and sickness can play a starring role in pregnancy, especially in the early stages. My first 16 weeks of pregnancy were punctuated with frequent trips to the restroom, and with many flights taken during this time, I became accustomed to having to rely on a few tricks to see me through those difficult moments.
Travel bands can be an excellent way to relieve pregnancy related nausea, and they’ve taken a high-tech turn in recent years. Hypnotherapy podcasts can also be a calming way to reduce feelings of sickness, and are best listened to with noise-canceling headphones and an eye mask .

Hydrating skincare for expectant mothers
Pregnancy can present some interesting skincare dilemmas , with many people experiencing a change at some point across their nine months. Dry patches, oily T-zones, and acne outbreaks are all common complaints. To help skin stay hydrated when flying, there are many pregnancy-safe products out there which can help replenish and restore your skin's natural barrier. La Mer The Mist Facial Spray is a particular favorite of mine—easy to apply, super lightweight, and long-lasting.

Travel pillows
During pregnancy, ligaments in the hips and back loosen in preparation for birth and this can often cause secondary strain across the top of the shoulders and neck which can be very uncomfortable for expectant mothers. If you’re traveling whilst pregnant, I recommend investing in a travel neck pillow , and packing your pregnancy pillow if you’re flying in a seat with a lie-flat bed.

Compression socks
“During pregnancy, you are at an increased risk of developing a blood clot,” Louise says. “That’s why compression socks , hydration, and movement—walking, stretching, and circling ankles—is recommended.”
Again, it’s not the most glamorous addition to your carry-on, but this footwear is important nonetheless. Try to stretch your legs every hour or so if possible, with a walk down the aisle or some lower leg exercises.

While packing a well-stocked carry-on will undoubtedly enhance your flying experience, there are other ways to ensure that you’re prepared for a relaxing trip. Here are my top three tips for flying while pregnant:
Food and beverage choices
Whilst it’s unlikely you’ll be able to see the full on-board menu in advance, it’s often a good idea to pre-select your meal genre if you’re having aversions or preferences during your pregnancy. Being able to rule out meat, dairy, or even opt for a lighter option may be preferable for some mothers-to-be. It could be worth packing a couple of extra snacks in your carry-on, just in case. I’ve been stashing ginger tea bags and plenty of dried fruit and nuts ( dried banana chips are a particular craving of mine) to see me through.
The airport experience
Lounge access can not only be an enjoyable way to kick-off your vacation, it can also be a lifesaver for tired feet. Having access to a clean and comfortable restroom can also often be advantageous, so if your travel tickets don’t include a lounge as standard, it could be worth a pay-for-access option to give you peace of mind that you’ll be spending time in a calm and restful environment before or in between flights.
Your travel outfit
While a stylish airport look is always desirable, comfort should definitely reign supreme during this important period, since your body is already coping with so much. Activewear can provide comfort and support during long-haul travel, and there are plenty of options out there. I look to brands like Alo Yoga and Lululemon for pieces that satisfy both the style and comfort stakes.
This website uses cookies to ensure you get the best experience on our website. Learn more

Information on how to stay safe and healthy abroad. About us.
- General Travel Health Advice
Advice for Pregnant Travellers
Disease risks, maternity notes and medical care, travel insurance, vaccinations, malaria prevention.
Pregnancy creates an altered state of health which requires practical consideration before travel. In the first instance travel plans should be discussed with your GP, practice nurse, midwife or obstetrician, ideally before booking and well in advance of your intended departure date.
Fluctuating hormone levels and the psychological impact of pregnancy, as regards changing routines and responsibilities, may adversely affect your capacity to cope with the stressful nature of travel. It is therefore worth considering if you will have access to sufficient emotional and physical support during travel.
Many diseases have more severe consequences in pregnancy, with significant risk to both mother and unborn baby. For example, malaria in pregnancy is harmful to both you and your unborn baby with an increased risk of severe illness or death for both. Consequently, where possible, you should avoid all non-essential travel to tropical destinations during pregnancy, in particular those with a risk of diseases such as malaria , zika virus or yellow fever .
The association between infection with zika virus and birth defects means that non-essential travel to areas with ongoing high risk of zika virus transmission should be postponed by women who are pregnant or planning pregnancy. For further information see our zika virus page.
Take a copy of your hand held maternity notes in case you need medical care during travel; include information about any pre-existing medical conditions and your blood group.
Carefully consider your intended destinations prior to booking, find out about:
- availability and standard of medical care
- existing health risks in the destination countries
- any other travel warnings.
The Foreign, Commonwealth and Development Office (FCDO) website provides advice on the availability of medical treatment and facilities alongside any travel warnings on an individual country basis.
It is essential that all your early pregnancy examinations are carried out prior to travel in order to rule out potential complications. If travelling after 28 weeks of pregnancy, it is important to ensure that available medical facilities at the destination are suitable to manage complications of pregnancy such as pre-eclampsia and caesarean section.
Be aware that blood supplies may not be safe in some destinations; this can increase the risks of blood borne infections such as hepatitis B , C and HIV .
Misunderstandings due to language barriers or cultural problems could make communication and therefore diagnosis and treatment of any illness more difficult than it would be at home.
Ensure that your travel insurance policy covers both you and your unborn child, and if delivery should occur during travel, that your newborn is insured.
Failure to notify your travel insurance provider that you are pregnant is likely to invalidate your insurance policy.
Additionally, it should be remembered that insurance policies are only as good as the medical facilities available.
Please see our travel insurance page for further information.
Air travel is generally considered safe in uncomplicated pregnancy. However, it is important to discuss your fitness to fly with your GP, practice nurse, midwife or obstetrician before departure.
Be aware that policies vary between each airline but generally:
- Most commercial airlines accept pregnant travellers up to 36 weeks if single pregnancy or up to 32 weeks if a multiple pregnancy. This is because labour is more likely after 37 weeks, or around 32 weeks if carrying an uncomplicated twin pregnancy.
- Some airlines require written documentation from your practice nurse, midwife or obstetrician. This is to confirm you are in good health, that your pregnancy is uncomplicated and your due date.
- Flying during the first 12 weeks of pregnancy may be considered risky as miscarriage is more common during this early stage. Additionally, at this stage pregnant travellers may be suffering from pregnancy induced nausea and fatigue which could make travelling uncomfortable.
- You may be at greater risk of deep vein thrombosis (DVT) during pregnancy and the postpartum period; please refer to our Deep Vein Thrombosis page for further information.
The Royal College of Obstetricians and Gynaecologists have produced an advice leaflet for pregnant women planning to undertake air travel: Air Travel and Pregnancy
Pregnancy does not prevent you from receiving vaccines that can protect the health of you and your unborn baby.
A general rule is that most recommended vaccines can be used if the risk of infection is substantial and if there are serious consequences of infection. However, a careful risk versus benefit analysis is needed for every individual, and the decision on whether to vaccinate should be made in conjunction with an appropriately qualified health care professional.
Inactivated Vaccines in Pregnancy
Inactivated vaccines cannot replicate which means they cannot cause disease in either the mother or her unborn baby. Most inactivated vaccines can be used if the risk of disease is considered high.
Live Vaccines in Pregnancy
The risk of the disease versus the benefit of administering any live vaccine during pregnancy requires expert consideration and expert advice should be sought. This is due to a theoretical concern that vaccinating pregnant women with live vaccines, such as: measles, mumps, rubella, chicken pox (varicella) and yellow fever, could potentially infect the unborn baby. Consequently, live vaccines are usually avoided during pregnancy. However, the use of live vaccines in pregnancy may be appropriate if travel is unavoidable and the risk of the disease is high.
Malaria in pregnancy is associated with miscarriage, premature delivery, low birth weight, severe illness or death, affecting both the mother and unborn baby. Consequently, you should avoid all non-essential travel to known malaria risk areas during your pregnancy.
If travel to a malaria area is unavoidable then it is important that you seek expert advice. In the first instance contact your GP for advice, however, be aware that they may refer you to a specialist travel medicine service.
Mosquito bite avoidance is essential in the prevention of malaria. Pregnant women are more attractive to mosquitoes and should therefore be particularly careful to avoid mosquito bites.
For further information please see our mosquito bite avoidance page.
Malaria Medication in Pregnancy
If antimalarial tablets are recommended then you should seek expert advice about which malaria tablets are safest for you to take.
The choice of malaria tablets will largely be determined by your destination, stage of pregnancy and any other pre-existing medical conditions you may have.
Malaria tablets should always be used in combination with mosquito bite avoidance .
back to top
- Disease Prevention Advice

Venture into the Sky and Beyond With These 4 Travel Tips for Expecting Mothers
Last Updated on June 12, 2023
Traveling is an activity that promotes broadened horizons, cultural understanding, and memories that last a lifetime. But what if you’re pregnant? Should the adventure stop? The answer is a resounding ‘no.’ During pregnancy, life is filled with preparations, adjustments, and, of course, excitement. Many women wonder whether traveling while carrying their little bundle of joy is safe. The good news is that it’s safe and can add value to your pregnancy experience.
The first trimester is usually marked by morning sickness and fatigue. Therefore, the ideal time to travel during pregnancy, as suggested by health experts, typically falls within the second trimester, when expecting mothers often feel their best. However, this doesn’t mean flying in the first or third trimester is a complete no-go; extra precautions and consultations with healthcare providers are needed.
Traveling while pregnant offers numerous benefits that contribute to a healthy and vibrant pregnancy experience. It allows mothers-to-be to relax, break free from routine, and enjoy their time before welcoming their little ones. It can also help foster a positive mindset, which is essential during this phase. One major value addition of traveling during pregnancy is connecting with different cultures and their pregnancy rituals. Experiencing how different societies celebrate the beauty of motherhood can be an enriching experience. Moreover, it could also provide some inspiration for your birthing traditions. Lastly, traveling during pregnancy can strengthen the bond between couples. Pregnancy is a journey that is not just about the mother but also about the father-to-be. Traveling together can create beautiful memories and bring couples closer, preparing them emotionally for parenthood.
Packing the Right Travel Essentials for Women
Packing appropriately is crucial when you’re pregnant. Carrying the right items can make a significant difference in the comfort and ease of your journey. A checklist of travel essentials for women , particularly pregnant women, is a must. Start with comfortable maternity clothing. Opt for loose, breathable clothes and comfortable walking shoes. Remember maternity undergarments that offer support and comfort.
Health essentials are a priority. Include a basic first-aid kit, prenatal vitamins, prescribed medications, and copies of your medical records or important health information. It’s also good to carry a list of emergency contacts. Ensure you pack healthy snacks, considering your dietary needs and cravings. Hydrating fluids like a refillable water bottle should be included as well. Consider travel comfort items like neck pillows, compression socks, and noise-canceling headphones. These can make your travel experience much smoother and more enjoyable.
Choosing the Right Destination and Accommodation
When selecting a destination, consider the medical facilities available there. Choose a place where quality healthcare is accessible. Additionally, think about the climate and terrain. You don’t want to be caught where the weather conditions might affect your comfort and health. Your accommodation should prioritize comfort and safety. Ensure it’s close to a hospital or a clinic. Check whether they offer amenities like a comfortable bed, access to nutritious food, and a serene environment.
Tips for Flying with Pregnancy
Flying with pregnancy can be a concern for many. Airlines often have different policies for pregnant passengers, so checking them beforehand is essential. Always inform the airline about your pregnancy when booking. Stay hydrated and walk around the cabin when possible to help with circulation. Choose an aisle seat for easy movement. Also, consider investing in travel insurance that covers pregnancy-related issues. Ensure you have the necessary protection for any unforeseen circumstances during your journey.
Embracing Babymoons
A concept that is gaining popularity among couples is the “ babymoon .” It’s a pre-baby getaway dedicated to enjoying the couple’s time together before their life changes with the baby’s arrival. Babymoons are a great way to celebrate pregnancy. They can be a quiet retreat in the countryside, a beach holiday, or even a city break – whatever appeals to your preferences. The focus is on relaxation, connection, and making memories. When planning your babymoon, consider your comfort and convenience. The destination should not involve arduous travel, and the activities should be pregnancy-friendly.
Remember, the purpose of a babymoon isn’t just to travel but to take a break from the hustle of pregnancy preparations, connect with your partner, and enjoy this special phase of life.
Pregnancy is a beautiful journey filled with anticipation, joy, and a fair share of challenges. Embracing travel during this period is possible and can enhance your pregnancy experience, offering you memories that will be treasured long after your child comes into the world.
Motherhood doesn’t need to limit your horizons; it can be an opportunity to expand them. Allow your pregnancy to be a chapter of personal and global exploration, connection, and growth. Traveling while pregnant can empower you, giving you strength and courage as you prepare to bring a new life. It reassures you that pregnancy is not a pause but a stretch of the journey where you continue to enjoy and embrace life with a growing love inside you.
Every expecting mother has a story to tell, and travel can add colorful pages to this chapter of your life. Remember that your strength as a mother begins long before the labor room. It begins with every decision you make to enrich your life and the life of the unborn. So go ahead, pack your bags, board that flight, and let the adventure of motherhood take you places you’ve never been. The world is waiting to celebrate this beautiful journey with you.
The pregnancy journey is transformative, and adding travel into the mix can make it an unforgettable voyage. Remember, the world is your oyster, and your pregnancy is the pearl within. Treasure it, celebrate it, and above all, enjoy the journey!
Related posts:
- Top Ten Nepal Travel Tips
- How much does it cost to travel in Chile (and tips for traveling Chile on a shoestring)
- How much does it cost to travel in the Philippines (+ money-saving tips)
- Three Tips to Find the Best Car Rental in Tampa

June 1, 2020
Due to travel restrictions, plans are only available with travel dates on or after
Due to travel restrictions, plans are only available with effective start dates on or after
Ukraine; Belarus; Moldova, Republic of; North Korea, Democratic People's Rep; Russia; Israel
This is a test environment. Please proceed to AllianzTravelInsurance.com and remove all bookmarks or references to this site.

Use this tool to calculate all purchases like ski-lift passes, show tickets, or even rental equipment.

Travel During Pregnancy: What Does Travel Insurance Cover?

Some of the most common questions we get at Allianz Global Assistance are about traveling while pregnant. While most pregnant women can safely travel without incident, sometimes complications arise and customers wonder, "What does travel insurance cover?"
Here’s the quick answer: Travel insurance can cover certain situations that result from unforeseen pregnancy complications, or a pregnancy that occurs after you’ve purchased your plan. Travel insurance typically does not cover trip cancellations or other travel losses resulting from normal pregnancy.
Like any other kind of insurance, travel insurance includes specific coverage definitions and restrictions. Read your agreement carefully, and if you have any questions about coverage, call. Pregnant women should consult their doctors with concerns and questions about safe travel.
If you’re pregnant, or you might be soon, it’s wise to protect upcoming trips. Maximize your coverage window by purchasing travel protection as soon as possible. Our most popular plan is OneTrip Prime , which includes substantial benefits for trip cancellation/interruption and medical emergencies.
Read on for a detailed guide to travel insurance and pregnancy from Allianz Global Assistance.
Pregnancy Complications: What Does Travel Insurance Cover?
You're in the first trimester of your pregnancy and feeling fine — until you begin feeling extremely nauseous a week before you're supposed to fly to New York on business. Your doctor diagnoses you with hyperemesis gravidarum, a severe and serious form of morning sickness, and you end up in the hospital on the day of your scheduled flight. Can travel insurance reimburse you for the canceled trip?
Yes. Travel insurance from Allianz Global Assistance can cover losses resulting from unforeseen pregnancy complications, such as pre-eclampsia, gestational diabetes or hyperemesis gravidarum. That means your travel insurance may reimburse you for nonrefundable trip costs lost if you must cancel or interrupt your trip because of pregnancy complications. The illness, injury, or medical condition you’re experiencing must be disabling enough to make a reasonable person cancel their trip, and a doctor must advise you to cancel it. For example, normal morning sickness would not be a covered reason for trip cancellation. When you’re filing a claim for trip cancellation/interruption related to a pregnancy complication, you’ll need documentation from your physician.
All travel insurance plans from Allianz Global Assistance include access to 24-Hour Emergency Assistance . If you experience a medical emergency while traveling, or any other problem, contact our hotline via phone or the TravelSmart TM app for rapid assistance. If your plan includes emergency medical benefits, your insurance may reimburse you for the cost of emergency medical care that you received for covered pregnancy complications while traveling.
Please note that travel insurance does not cover the chance that a complication might occur. For example, if you delivered prematurely with your first two pregnancies, your doctor might advise you to cancel the trip to Paris you planned for the sixth month of your third pregnancy. However, this is still considered a normal pregnancy because no complication has been diagnosed. Travel insurance would not cover the trip cancellation.
Surprise Pregnancy and Trip Cancellation
You and your spouse are planning a week-long European river cruise to celebrate your third anniversary. Tickets are hard to come by, so you book your trip a year in advance. You schedule the flights and purchase your travel insurance — and two months later, you discover you're pregnant. Will travel insurance cover your trip cancellation?
On some plans, Allianz Global Assistance lists pregnancy as a covered reason for trip cancellation if you find out you are pregnant after purchasing your policy. For your trip cancellation to be covered, you must provide medical records to verify the pregnancy occurred after that date. Please see your policy documents for your plan’s specific coverage. And if you’re planning a trip now, don’t wait to buy travel insurance! Get a quote today.

Late-Term Pregnancy and Trip Cancellation
You decide to plan a babymoon getaway so you and your sweetie can enjoy some time together before the baby arrives. You book your plane tickets and a bed-and-breakfast on the beach. You're feeling fine and getting excited. Then your doctor advises you, as a precaution, not to travel in the eighth month of pregnancy. Will travel insurance cover this pregnancy-related trip cancellation?
No. In this scenario, there are no medical complications with your pregnancy, so the cancellation will not be covered. Please understand that Allianz Global Assistance is not disagreeing with your doctor's recommendation not to travel — you should do what's best for you and your baby's health. However, most travel insurance plans from Allianz Global Assistance do not include normal pregnancy as a covered reason for trip cancellation (except as described above.)
Airline Rules for Flying While Pregnant
You're flying to Los Angeles to see your sister one last time before the baby's born. But when you get to the gate, the airline won't let you on board because you're too close to your due date. Will your travel insurance plan reimburse you for the missed flight?
No. Being refused service by a carrier because of normal pregnancy is not a covered reason for trip cancellation. Cruise ships and airlines have very specific rules about travel while pregnant. Here are selected airline pregnancy policies, but you should also call your travel supplier to check before you book your trip. Please note that this information is subject to change.
- American Airlines: A medical certificate is required to fly within four weeks of your delivery date in a normal, uncomplicated pregnancy. Travel is not permitted within seven days of your due date on domestic flights under five hours, or within four weeks of your due date on international flights, unless you get a medical certificate and clearance from a Special Assistance Coordinator. 1
- Delta: Delta does not impose restrictions on flying for pregnant women. However, ticket change fees and penalties cannot be waived for pregnancy. 2
- JetBlue: Pregnant passengers expecting to deliver within seven days are prohibited from travel, unless they provide a doctor's certificate dated no more than 72 hours prior to departure stating that the passenger is physically fit for air travel and that the estimated date of delivery is after the date of the last flight. 3
- Southwest: Southwest has no pregnancy prohibitions, but recommends against air travel beginning at the 38th week of pregnancy. 4
- United: To fly in or after your 36 th week of pregnancy, you must provide the original and two copies of an obstetrician’s certificate, dated within three days (72 hours) prior to your flight departure, that says you’re fit to fly. 5
Travel Insurance and Childbirth
You're enjoying your babymoon vacation in Cozumel when suddenly you feel the first twinge of labor. Twelve hours later, you're the proud mother of a baby girl. Will travel insurance cover the cost of labor and delivery?
No. Normal childbirth is not covered by travel insurance from Allianz Global Assistance. However, if complications arise in delivery, the costs of emergency medical care may be covered. Also, attending the childbirth of a family member can be a covered reason for trip cancellation, depending on your plan.
While travel insurance from Allianz Global Assistance can't cover every possible pregnancy scenario, we want to do our best to help! Our Assistance team is available 24 hours a day to provide expert advice and aid.
Related Articles
- Traveling While Pregnant: Key Considerations
- The Essential Packing Checklist for Flying With An Infant
- Great Babymoon Destinations in the US
- JetBlue.com
- Southwest.com

Get a Quote
{{travelBanText}} {{travelBanDateFormatted}}.
{{annualTravelBanText}} {{travelBanDateFormatted}}.
If your trip involves multiple destinations, please enter the destination where you’ll be spending the most time. It is not required to list all destinations on your policy.
Age of Traveler
Ages: {{quote.travelers_ages}}
If you were referred by a travel agent, enter the ACCAM number provided by your agent.
Travel Dates
{{quote.travel_dates ? quote.travel_dates : "Departure - Return" | formatDates}}
Plan Start Date
{{quote.start_date ? quote.start_date : "Date"}}
Share this Page
- {{errorMsgSendSocialEmail}}
Your browser does not support iframes.
Popular Travel Insurance Plans
- Annual Travel Insurance
- Cruise Insurance
- Domestic Travel Insurance
- International Travel Insurance
- Rental Car Insurance
View all of our travel insurance products
Terms, conditions, and exclusions apply. Please see your plan for full details. Benefits/Coverage may vary by state, and sublimits may apply.

Insurance benefits underwritten by BCS Insurance Company (OH, Administrative Office: 2 Mid America Plaza, Suite 200, Oakbrook Terrace, IL 60181), rated “A” (Excellent) by A.M. Best Co., under BCS Form No. 52.201 series or 52.401 series, or Jefferson Insurance Company (NY, Administrative Office: 9950 Mayland Drive, Richmond, VA 23233), rated “A+” (Superior) by A.M. Best Co., under Jefferson Form No. 101-C series or 101-P series, depending on your state of residence and plan chosen. A+ (Superior) and A (Excellent) are the 2nd and 3rd highest, respectively, of A.M. Best's 13 Financial Strength Ratings. Plans only available to U.S. residents and may not be available in all jurisdictions. Allianz Global Assistance and Allianz Travel Insurance are marks of AGA Service Company dba Allianz Global Assistance or its affiliates. Allianz Travel Insurance products are distributed by Allianz Global Assistance, the licensed producer and administrator of these plans and an affiliate of Jefferson Insurance Company. The insured shall not receive any special benefit or advantage due to the affiliation between AGA Service Company and Jefferson Insurance Company. Plans include insurance benefits and assistance services. Any Non-Insurance Assistance services purchased are provided through AGA Service Company. Except as expressly provided under your plan, you are responsible for charges you incur from third parties. Contact AGA Service Company at 800-284-8300 or 9950 Mayland Drive, Richmond, VA 23233 or [email protected] .
Return To Log In
Your session has expired. We are redirecting you to our sign-in page.

Is it safe to take anti-sickness medication when pregnant?
Are anti-sickness drugs such as Metoclopramide and Cyclizine OK to take during pregnancy and why are some people scared of using them?

- Susannah Osborne
- Share on facebook
- Share on twitter
- Share on pinterest
- Share on whatsapp
- Share on reddit
- Share on tumblr
In a nutshell
Most anti-sickness (anti-emetic) medication is safe to take during pregnancy but a doctor should always prescribe anti-emetic drugs, and it’s worth trying natural alternatives first.
The expert view
If you're really struggling with sickness during your pregnancy, there’s good news: anti-sickness medications are safe to take during pregnancy if prescribed by a doctor. Anti-sickness drugs have had a difficult history - see more below - but rest assured, there is medicine you can take which won't harm your baby.
“There is medication that is safe to use in pregnancy,” confirms midwife Anne Richley, “but it should always be prescribed by a doctor, not bought over the counter.”
The NHS commonly prescribes antihistamines like Promethazine and Cyclizine to treat pregnancy sickness and taking anti-emetic drugs, like Prochlorperazine (Stemetil) or Metoclopramide, is another way of easing pregnancy nausea.
These drugs work either by blocking the signals from and to your the part of your brain that controls the sickness mechanism, or by encouraging your stomach to empty faster, so there’s nothing to bring up. You may also be prescribed vitamin B6, which may help relieve pregnancy nausea for some women, though it doesn't reduce vomiting.
More like this
So when might you need to take anti-sickness drugs.
While more than half of pregnant women suffer with morning sickness, most mums-to-be are able to get through it and find the sickness eases by around week 12.
However, some women have really severe sickness, called hyperemesis gravidarum . This affects around 0.1% of pregnancies, and became well known when Kate Middleton, the Duchess of Cambridge, suffered from it when she was pregnant with Prince George .
According to Patient.co.uk, if your symptoms are, “persistent, severe and preventing daily activities" and typically last beyond week 20 of your pregnancy, you may need treatment with drugs.
If you feel you're not coping with pregnancy nausea, do talk to your midwife or doctor.
There are also more serious sickness symptoms, which mean you should contact your GP or midwife immediately. These are:
- if you're unable to keep food or any fluids down for 24 hours
- you don't wee for more than 8 hours and your urine is dark coloured
- you feel very weak, dizzy or faint when you stand up
- you have stomach pains
- you have a high temperature - 38°C (100.4°F) or above
- your sick contains blood
But aren’t anti-sickness drugs dangerous in pregnancy?
In the 60s a drug called Thalidomide was used to treat morning sickness. This did prove to be dangerous to unborn babies and was banned from use to treat pregnancy sickness.
The medications doctors now prescribe are largely considered safe and effective, although as with all medicines there can be side effects and it’s generally best to avoid medication when you’re pregnant if you can.
One study of more than 200,000 women found babies born to mums who had taken an antihistamine during their pregnancy were no more likely to have something wrong with them than babies whose mothers had not taken one. And another study of 40,000 women proved that taking metoclopramide didn’t increase the risks birth defects or miscarriage.
How can I cope without taking medication?
There are also lots of ways to stop feeling and being sick that don’t involve a visit to the pharmacy.
“There are various things that you can try to reduce the symptoms before using drugs,” says Anne. “Try eating little and often. Also, acupressure bands, often used for travel sickness, can work wonders.”
Other suggested natural treatments include including more ginger in your diet, eating dry, bland foods first thing in the morning, acupuncture and wearing clothes that don't feel tight around the waist.
Mums writing in our forum say:
"I was given Prochlorperazine when I was 10 wks pregnant with my DD. I had suffered from about 5 weeks and lost almost a stone. I visited my GP every week and begged them to help me but it took until 10 weeks for them to prescribe them (they worked great once I got them). I had to take anti sickness tablets until I was 26wks." baby_blaylock
"Have had really bad case of hyperemesis gravidarum since 6 weeks pregnant. Got medication from doctor but nothing seemed to really kick it but......last few days have become increasingly better and without jinxing myself I don't feel sick today! Am hoping that this is the start of me turning a corner. Fingers crossed!" tiger2004
"I had Hyperemesis and lost 2 stone in a matter of weeks. Everyone kept saying it's just morning sickness you have to force yourself to eat but I couldn't even keep water down. When I saw my consultant my urine sample was neon orange and she said she'd never seen anything like it and wanted me on a drip now. I was put on medication and luckily it stopped me being sick but the nausea was there throughout the pregnancy. There are a lot of foods I still can't eat because of it. There's only so many times you can throw something up and still want to eat it." Lucian3
Read more...
- When will my morning sickness stop
- Do I have hyperemesis gravidarum (extreme morning sickness)?
- Four breakfasts to help morning sickness

How NatPat's wellness patches may help your family
NatPat's range of wellness patches and stickers aim to tackle everything from allergies to lack of focus. We take a closer look at the range.
Advertisement feature with NatPat
- Credit cards
- View all credit cards
- Banking guide
- Loans guide
- Insurance guide
- Personal finance
- View all personal finance
- Small business
- Small business guide
- View all taxes
You’re our first priority. Every time.
We believe everyone should be able to make financial decisions with confidence. And while our site doesn’t feature every company or financial product available on the market, we’re proud that the guidance we offer, the information we provide and the tools we create are objective, independent, straightforward — and free.
So how do we make money? Our partners compensate us. This may influence which products we review and write about (and where those products appear on the site), but it in no way affects our recommendations or advice, which are grounded in thousands of hours of research. Our partners cannot pay us to guarantee favorable reviews of their products or services. Here is a list of our partners .
Travel Insurance and Pregnancy: What to Know
Many or all of the products featured here are from our partners who compensate us. This influences which products we write about and where and how the product appears on a page. However, this does not influence our evaluations. Our opinions are our own. Here is a list of our partners and here's how we make money .
There’s a lot to think about when you’re pregnant — especially if you plan to travel. You’ll want to make sure your health care and your trip costs are covered if something goes wrong.
And while travel insurance for pregnancy may sound like a must-have, remember that not all plans will cover your specific needs. At the moment, there isn't a specific insurance option for those who are pregnant. Rather, pregnant people will need to consider travel insurance that includes coverage for trip cancellation and interruption, as well as emergency medical and evacuation costs.
Your decision to buy travel insurance while pregnant will depend on how much of your trip is nonrefundable, where you’re going and what coverages you already have. These coverages may include trip interruption insurance from your credit card issuer or emergency medical coverage from your current health insurer.
Here’s what you need to know to choose the best travel insurance for pregnancy.
Trip cancellation or interruption due to pregnancy
Most travel insurance policies will reimburse you for all or a portion of your nonrefundable travel costs if you have to cancel your trip for a covered reason. But for pregnant people, covered reasons are a little more complicated.
For most policies, normal pregnancy is not a valid reason to cancel your trip if you already knew you were pregnant when you purchased the insurance. But pregnancy may be a valid reason to cancel if you learn you're pregnant after you’ve booked your trip and paid for an insurance policy.
For example, if you prepay for a trip a year in advance, purchase Allianz travel insurance, and a few months later find out you’re pregnant and need to cancel your trip, the company will likely reimburse you for all or a portion of your lost travel costs. But you’ll have to prove that you learned about your pregnancy after you purchased the policy.
On the other hand, if you knew you were pregnant when you purchased the policy, you will likely not get reimbursed if you canceled your flight due to morning sickness, for example.
» Learn more: Can you fly while pregnant? It depends.
Trip cancellation or interruption due to complications of pregnancy
If you have complications during your pregnancy, travel insurance may cover your trip costs regardless of when you learned you were pregnant.
Keep in mind that only specific complications — like gestational diabetes, preeclampsia, hyperemesis gravidarum or miscarriage — are eligible, and a doctor must advise you not to travel due to your diagnosed condition.
» Learn more: What to know about Cancel For Any Reason (CFAR) travel insurance
Medical coverage for pregnant travelers
If you’re traveling domestically, your regular health insurance may be all the coverage you need. Check with your provider. If you’re going abroad, there’s a good chance your health insurance will not reimburse you for medical expenses while traveling. So for pregnant people traveling internationally, travel medical insurance is probably a good idea.
Secondary travel health insurance can be surprisingly affordable. Secondary plans kick in after you’ve used any applicable primary insurance coverage from your current health insurer.
Searching InsureMyTrip.com, we found secondary international medical insurance plans starting at $14 for a 30-year-old California resident traveling to France for 12 days in September. For this price, you receive coverage up to $50,000.
Want higher coverage limits? They’re available. For the same 30-year-old California-based traveler headed to France, GeoBlue 's Voyager Essential plan offers $1 million in travel medical coverage with a $0 deductible for $27 — again, that’s for the whole trip, not per day. This plan is not secondary coverage, meaning you can buy it even if you don’t have a primary health insurer.
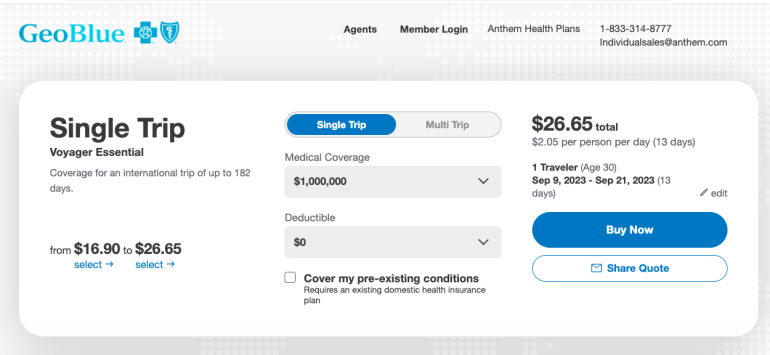
» Learn more: Can I get travel insurance for pre-existing medical conditions?
Emergency medical evacuation due to pregnancy
If you’re traveling to large city, a health care facility is likely a short drive away. But if you’re traveling someplace remote, emergency transportation coverage , like a helicopter, can be a literal lifesaver. Covering this service with an insurance plan can save you a bundle.
Some credit cards give you automatic emergency medical evacuation when you use the card to book your trip, like the Chase Sapphire Reserve® . But if you didn’t use a credit card with emergency evacuation coverage or need higher limits, you may want to buy travel insurance. Most comprehensive plans include emergency medical evacuation insurance, but make sure it’s covered before you purchase your plan.
» Learn more: The best credit cards for travel insurance benefits
Where to buy insurance for traveling while pregnant
Different travel insurance companies have a variety of plans with varying coverage.
A policy from Travel Guard that was perfect for your nonpregnant friend when she traveled to Machu Picchu may not be as good as a policy from Travelex or Nationwide if you’re pregnant and cruising through Europe. Comparison shop and carefully note what’s covered and the deductible limits before you buy.
» Learn more: The best travel insurance companies
Travel insurance while pregnant recapped
You may not need travel insurance for pregnancy, especially if you’re traveling domestically and your trip is fully refundable — but don’t assume that’s always the case.
Read up on your existing coverage from your health plan and any insurance offered by your credit card . Then you can explore a little more of the world before baby arrives, knowing you’re covered for any scenario.
How to maximize your rewards
You want a travel credit card that prioritizes what’s important to you. Here are our picks for the best travel credit cards of 2024 , including those best for:
Flexibility, point transfers and a large bonus: Chase Sapphire Preferred® Card
No annual fee: Bank of America® Travel Rewards credit card
Flat-rate travel rewards: Capital One Venture Rewards Credit Card
Bonus travel rewards and high-end perks: Chase Sapphire Reserve®
Luxury perks: The Platinum Card® from American Express
Business travelers: Ink Business Preferred® Credit Card

on Chase's website
1x-10x Earn 5x total points on flights and 10x total points on hotels and car rentals when you purchase travel through Chase Travel℠ immediately after the first $300 is spent on travel purchases annually. Earn 3x points on other travel and dining & 1 point per $1 spent on all other purchases.
60,000 Earn 60,000 bonus points after you spend $4,000 on purchases in the first 3 months from account opening. That's $900 toward travel when you redeem through Chase Travel℠.

1x-5x 5x on travel purchased through Chase Travel℠, 3x on dining, select streaming services and online groceries, 2x on all other travel purchases, 1x on all other purchases.
60,000 Earn 60,000 bonus points after you spend $4,000 on purchases in the first 3 months from account opening. That's $750 when you redeem through Chase Travel℠.

1x-2x Earn 2X points on Southwest® purchases. Earn 2X points on local transit and commuting, including rideshare. Earn 2X points on internet, cable, and phone services, and select streaming. Earn 1X points on all other purchases.
50,000 Earn 50,000 bonus points after spending $1,000 on purchases in the first 3 months from account opening.

Healthdirect Free Australian health advice you can count on.
Medical problem? Call 1800 022 222. If you need urgent medical help, call triple zero immediately
healthdirect Australia is a free service where you can talk to a nurse or doctor who can help you know what to do.
Motion sickness
7-minute read
Share via email
There is a total of 5 error s on this form, details are below.
- Please enter your name
- Please enter your email
- Your email is invalid. Please check and try again
- Please enter recipient's email
- Recipient's email is invalid. Please check and try again
- Agree to Terms required
Error: This is required
Error: Not a valid value
- Motion sickness is also known as travel sickness, car sickness or sea sickness.
- If you have motion sickness, you are likely to have nausea and may vomit and feel clammy.
- You can help prevent motion sickness by looking outside of the vehicle or focusing on the horizon.
- Symptoms usually end once the motion stops.
- You can try travel sickness treatments to help prevent motion sickness.
What is motion sickness?
Motion sickness is feeling unwell when moving on any type of transport. It is also known as ‘travel sickness’, 'car sickness' or 'sea sickness'. It is a normal response to certain types of movement.
There are a few ways to prevent and manage motion sickness.
What are the symptoms of motion sickness?
Nausea is the main symptom of motion sickness. But you might also experience other symptoms, including:
- vomiting or retching
- cold sweating
- lack of appetite
- dry mouth or excess saliva
- increased sensitivity to smell
If you are prone to motion sickness, you may quickly feel sick if you read a book or look at your phone when in a moving vehicle.
You might feel better after vomiting, and symptoms will generally improve once you stop moving. But you can also feel the after-effects of motion sickness for a few hours or a few days before fully recovering.
What causes motion sickness?
Motion sickness is thought to be caused by your senses being confused when what you see is different to the signals felt by your inner ear balance system .
If you are feeling anxious about travel, this can make motion sickness worse.
You can get motion sick when:
- travelling by car, bus, boat, train or aeroplane
- on amusement park rides
- playing virtual reality video games or simulations
Motion sickness is a common problem. It is most frequent in children aged between 2 and 12 years. If other family members get motion sickness, it is more likely that you will too.

If you already have a condition that causes nausea, such as morning sickness or migraines , you may be more likely to experience motion sickness.
How is motion sickness diagnosed?
You don’t need to see a doctor or get any tests for a diagnosis of motion sickness. There is a pattern of feeling unwell during travel or movement, so you will probably know if you have it.
If you often feel dizzy or nauseous at other times too, discuss this with your doctor.
ASK YOUR DOCTOR — Preparing for an appointment? Use the Question Builder for general tips on what to ask your GP or specialist.
How is motion sickness treated and prevented?
Practical tips.
Here are some tips for preventing motion sickness:
- Look out of the window, and focus on the horizon instead of looking at a book or a screen.
- Try to sit or lie still and rest your head on a pillow or headrest.
- Sit close to the front of a car, bus or train.
- If flying, sit still and close your eyes during take-off and landing.
- Listen to music and breathe mindfully .
- Open the window or air vent for fresh air.
- Eat lightly before and during the trip and avoid alcohol. Sip water instead.
Pressure bands worn on your wrists may help prevent motion sickness in some people.
If you are travelling by sea, after a few days of exposure to the motion you will likely adapt and get used to it.
You can try taking travel sickness medicines to prevent motion sickness. These may include:
- antihistamines
- antiemetics (medications to prevent and treat nausea and vomiting)
There might be side effects, such as drowsiness. Ask your pharmacist or doctor for advice on what to take. Getting advice is especially important:
- for children
- if you are taking other medicines
- if you are pregnant
If you are using a travel sickness medicine, you should take it about half an hour before travel. If you have motion sickness and you already feel nauseous, it is probably too late to take a medicine. Eating a few plain crackers or having a clear, fizzy drink may help.
If you or your child regularly suffer from motion sickness, make sure you have a container, plastic bags and wipes handy. Take a break for some fresh air when needed.
Resources and support
Ask your doctor or pharmacist how to prevent and treat motion sickness.
Visit the Australian Government Smart Traveller website for more travel health advice.
You can also call the healthdirect helpline on 1800 022 222 (known as NURSE-ON-CALL in Victoria). A registered nurse is available to speak with 24 hours a day, 7 days a week.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
Learn more here about the development and quality assurance of healthdirect content .
Last reviewed: October 2023
Search our site for
- Travel Medicine
Need more information?
These trusted information partners have more on this topic.
Top results
Motion sickness - MyDr.com.au
Many people eventually grow out of motion sickness (travel sickness), but for those who don’t there are treatments available and things you can do to help prevent it and ease the symptoms.
Read more on myDr website

Travel with kids: car, plane, bus & train | Raising Children Network
Family travel with kids sometimes involves long journeys by car, plane, bus or train. Our practical tips can help take the stress out of travel with kids.
Read more on raisingchildren.net.au website

Motion sickness - Better Health Channel
Motion sickness may occur in anyone, but some people are particularly sensitive.
Read more on Better Health Channel website

Travel sickness self-care - MyDr.com.au
Travel or motion sickness may occur in any type of moving vehicle, such as a car, boat or plane. Find out what products are available for travel sickness.
Travelling with kids
Travelling with your child can sometimes be challenging. It helps to plan for your travel and give yourself a longer time to get there.
Read more on Pregnancy, Birth & Baby website

Travelling with kids: sleep routines | Raising Children Network
Travel with kids sometimes means adjusting their sleep routines. Here are ideas for making changes in sleep routines easier for your children.
Travel and pregnancy
With the proper precautions, and armed with information on when to travel, vaccinations and insurance, most women can travel safely well into their pregnancy.
Travelling during Pregnancy
Many women will travel during pregnancy for work, recreation and visiting friends and relatives. In general, the second trimester is the safest and most comfortable time to travel. The chance of miscarriage is very small, nausea and vomiting are likely to have settled and physical constraints have not yet begun to limit your movement.
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website

Travellers' diarrhoea - MyDr.com.au
Contaminated food and drink are the major sources of travellers' diarrhoea. High-risk regions for an attack include the majority of Asia, the Middle East, Africa, Mexico, Central and South America.
Travel medical kit checklist - MyDr.com.au
Stay safe when you are travelling with this checklist of handy health supplies and find a list of what to take in your travel medical kit on myDr.com.au.
An Overview of Nausea and Vomiting in Adults | Ausmed
Nausea and vomiting are not conditions themselves - rather, they are non-specific symptoms associated with a variety of conditions. Nausea describes a feeling of unease in the stomach, chest or throat. Vomiting (emesis) is the physical act of forcibly ejecting stomach contents through the mouth.
Read more on Ausmed Education website

Healthdirect Australia is not responsible for the content and advertising on the external website you are now entering.
Healthdirect 24hr 7 days a week hotline
24 hour health advice you can count on
1800 022 222
Government Accredited with over 140 information partners
We are a government-funded service, providing quality, approved health information and advice
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
© 2024 Healthdirect Australia Limited
Support for this browser is being discontinued
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
- Search Please fill out this field.
- Newsletters
- Sweepstakes
Taking Unisom and Vitamin B6 During Pregnancy for Morning Sickness Relief
Over-the-counter options like Unisom and vitamin B6 can help relieve morning sickness. Here's what you need to know about taking Unisom and B6 during pregnancy.
- How Do Unisom and Vitamin B6 Help Morning Sickness?
- Are Unisom and Vitamin B6 Safe?
- Taking Unisom and Vitamin B6
Other Morning Sickness Remedies
When to consult a health care provider.
Morning sickness affects almost 75% of pregnant people. While home remedies and prevention strategies can be effective, sometimes they just aren't enough. Many people find relief by taking Unisom (doxylamine) and vitamin B6 (pyridoxine) for nausea and vomiting during pregnancy. Both Unisom and B6 are considered safe throughout pregnancy, including in the first trimester.
Morning sickness can start as early as 6 weeks into pregnancy and can last up to 14 weeks, or even longer. And the term “morning sickness” is a misnomer—it’s more like “morning, noon, and night sickness” for many pregnant people.
If that's you, talk to a health care provider about trying Unisom and B6. Here's how they work to ease morning sickness during pregnancy.
Vesna Andjic / Getty Images
How Do Unisom and Vitamin B6 Help Morning Sickness?
The American College of Obstetricians and Gynecologists (ACOG) says that the combination of Unisom and vitamin B6 is an effective remedy for morning sickness, and can be used safely during pregnancy if recommended by your health care provider.
The effectiveness is due to how the ingredients work together, says Diana E. Ramos, MD , an OB-GYN and adjunct assistant clinical professor at the University of Southern California's Keck School of Medicine. Doxylamine, the active ingredient in Unisom, is a type of antihistamine that is known to help with vomiting. B6 is a vitamin shown to relieve nausea in pregnant people. Together, Unisom and B6 are known to treat cases of moderate morning sickness when at-home remedies don’t seem to be working.
Always Read the Label
Doxylamine is often sold over-the-counter as Unisom (a sleep aid), and this medication is what most doctors recommend for morning sickness. It’s important to check the labels when you purchase Unisom, however, as doxylamine isn’t the active ingredient in all Unisom brand products. In some Unisom products, the active ingredient is diphenhydramine.
Are Unisom and Vitamin B6 Safe for Pregnant People?
Unisom and vitamin B6 are safe. Both drugs, whether taken alone or together, are safe to take during pregnancy and have no harmful effects on the fetus, according to the ACOG.
While these medications are considered safe to take throughout pregnancy, it's always to speak with a health care provider before starting any medications, says Lynn L. Simpson, MD , an OB-GYN and the chief of the maternal-fetal medicine division at Columbia University's Irving Medical Center in New York. Your provider can also help you determine the best dosage for you and how to take Unisom and vitamin B6 for morning sickness relief.
How To Take Unisom and Vitamin B6 During Pregnancy
Once you and your health care provider have decided that Unisom and B6 are a good treatment choice for you, you will likely have many questions about the ins and outs of taking the medication. Here is what you need to know.
Is it safe to combine Unisom and vitamin B6 during pregnancy?
While using this medication and supplement together is considered safe, the ACOG recommendations suggest a conservative approach: Trying vitamin B6 supplements alone first, and adding Unisom if needed.
While combining over-the-counter products is an option, experts say that it is also safe for pregnant people to take a prescription medication that combines both vitamin B6 and doxylamine. This is usually a prescription medication called Diclegis (doxylamine and pyridoxine).
“[Prescription combination pills such as Diclegis have been] shown to be more effective than taking Unisom and vitamin B6 separately,” says Dr. Simpson. Dr. Simpson says that taking 10 to 25 milligrams of vitamin B6 every 6 to 8 hours for mild cases of morning sickness may be helpful.
How long do Unisom and B6 take to work?
Unisom is generally fast-acting, says Dr. Ramos. “In general, doxylamine works shortly after ingesting,” she says. “So, if you have nausea now, you will get relief shortly after taking it.”
If you are taking a prescription like Diclegis, relief will be slower but longer-lasting. “The prescription combination is an extended relief formulation. If you take it at night, by morning it will be taking effect,” says Dr. Ramos.
Will taking Unisom make you sleepy?
Unisom is an over-the-counter sleep aid, so it may make you drowsy. Some providers even recommend it for occasional insomnia during pregnancy , but talk to a health care before taking it for that purpose.
“You may want to try it at night to see how you react to the medication,” Dr. Ramos offers. At the same time, she says, all people are different and react differently to medications. Drowsiness might not be an issue for you.
How long can you take Unisom and vitamin B6 during pregnancy?
You can take Unisom and B6 for as long as you need them to treat morning sickness , which for most people is throughout their first trimester, as morning sickness symptoms tend to decrease after that. For some people, morning sickness lasts beyond the first trimester, and you may need to continue taking Unisom and vitamin B6 to find relief.
Do I need to wean off of Unisom and B6?
There is no need to wean off Unisom and vitamin B6, says Dr. Simpson. “Patients can discontinue Unisom and pyridoxine abruptly—no need to taper these medications prior to stopping them,” she says. “Usually patients can stop their medications when they have been asymptomatic for more than a week and are beyond the first trimester.”
Although Unisom and vitamin B6 are considered safe, most health care providers recommend other remedies before taking medication for morning sickness. Combining these at-home remedies with Unisom and vitamin B6 can be helpful too. Dr. Simpson’s favorite non-pharmacologic remedies for morning sickness include dietary changes and avoiding common nausea triggers.
Dietary changes to try
- Eating more often
- Eating smaller amounts
- Eating slowly
- Eating more bland food
- Drinking fluids separately from solids
- Try taking ginger or peppermint
Common nausea triggers to avoid
- Offensive odors
- Excessive heat
For some pregnant people, the combination of Unisom and vitamin B6 isn’t enough to make morning sickness more manageable. If this is the case, you may be dealing with a more severe case of morning sickness called hyperemesis gravidarum , and you should talk to your doctor or midwife about other medications or options for treating it.
Whatever the case, always speak to your health care before taking any medications during pregnancy, including over-the-counter options like Unisom and vitamin B6. And never hesitate to reach out to your provider with questions or concerns along the way: That’s what they are there for.
Nausea and vomiting of pregnancy . Am Fam Physician. 2014.
Place de la vitamine b6 dans le traitement des nausees et vomissements gravidiques [Interest of vitamin b6 for treatment of nausea and/or vomiting during pregnancy] . Gynecol Obstet Fertil Senol . 2020.
ACOG Practice Bulletin No. 189: Nausea And Vomiting Of Pregnancy . Obstetrics & Gynecology. 2018.
Morning sickness: Nausea and vomiting of pregnancy . American College of Obstetricians and Gynecologists . 2023.
Maternal safety of the delayed-release doxylamine and pyridoxine combination for nausea and vomiting of pregnancy; a randomized placebo controlled trial . BMC Pregnancy Childbirth . 2015.
Related Articles
- Mattress Toppers
- Sheets & Bedding
- Sleep Products
- Cleaning & Laundry
- Heating & Cooling
- Home Office
- Kitchen & Dining
- Storage & Organization
- Wine & Bar
- Accessories
- Handbags & Purses
- Lingerie & Sleepwear
- Outdoor & Fitness Apparel
- Kids Clothes & Accessories
- Pregnancy & Postpartum
- Toys & Books
- Apparel & Accessories
- Camping & Hiking
- Fishing & Hunting
- Tennis & Racket Sports
- Tools & Tech
- Training & Recovery
- Water Sports
- Winter Sports
- Personal Products
- Wellness & Self Care
- Computers, Tablets & Accessories
- Online Tools
- Smart Home Devices
- Smartphones, Smartwatches & Accessories
- Hotels & Lodging
- Travel Products
- Father's Day
- Mother's Day
- Valentine's Day
- Amazon Prime Day
- Beauty & Grooming
- Tech & Electronics
- Travel Deals
- Mattress & Sleep
The Best Pregnancy Compression Socks To Soothe Swelling
- Share to Facebook
- Share to Twitter
- Share to Linkedin
Your body goes through so many changes during pregnancy, with many women experiencing increased swelling—especially in the feet and legs—as you near your due date. The best pregnancy compression socks can help you get back on your feet comfortably, boosting blood circulation, reducing swelling and helping prevent blood clots, so you can work, travel, chill or exercise pain-free. When shopping for a great pair of pregnancy compression socks, it’s important to factor in fit, material, comfort, pressure level and ease of use, especially during the third trimester when getting any socks and shoes on can be a pain.
We found the best pregnancy compression socks, according to health experts and pregnant people.
Dr. Laura Purdy, M.D., a board-certified family medicine physician, suggests gentle compression, a soft, breathable fabric and keeping it below the knee as far as fit goes. “Since swelling happens typically later in pregnancy, which is also the time it is harder to put on socks, I would recommend looking for a pair that is easy to put on and doesn't cause you more strain.” Nurse practitioner Christina DeJesus says “compression socks should be snug, but not overly tight, as improper fit can restrict blood flow rather than enhance it.” She also recommends socks with graduated compression, featuring “the most compression at the ankle and gradually decreasing upwards to optimize circulation and support blood flow back toward the heart.”
The pregnancy compression socks below all come highly recommended by Purdy and receive rave reviews from expecting moms.
- Best Pregnancy Compression Socks Overall: Kindred Bravely Premium Maternity Compression Socks
- Best Budget Pregnancy Compression Socks: Charmking Compression Socks
- Best Pregnancy Compression Socks For Travel: Comrad Knee-High Compression Socks
- Best Pregnancy Compression Socks For Exercise: Lululemon Micropillow Compression Knee-High Running Socks
- Best Pregnancy Compression Socks On Amazon: Blueenjoy Copper Compression Socks
- Most Comfortable Pregnancy Compression Socks: Pear Cotton Crew Compression Socks
- Best Stylish Pregnancy Compression Socks: Bombas Women's Everyday Compression Socks
Best Pregnancy Compression Socks Overall
Cute, cushioned and made for moms with graduated compression.
Kindred Bravely
Kindred Bravely Premium Maternity Compression Socks
Popular maternity brand Kindred Bravely nails it with these super soft and stylish high-compression socks. They feature a snug fit for more pain relief and “the sole is cushioned for ultimate comfort,” says Purdy, who loves that this brand is “by moms for moms—so in other words, they get it.” The socks are moisture-wicking and odor-reducing, are available in two calf sizes to achieve the best fit, and come in a pack of two so you can rotate on laundry days. At $15 a per pair, the cost less hard to swallow when you’re knee deep in buying baby gear too.
“I wear these at work or during the day on weekends and it really helps prevent what I call sausage feet,” writes one pregnant mom. “They are also very cute. The colors are subtle and I like the sparkle stripes at the top. I wear them as knee high socks with dresses and get lots of compliments.” We do want to point out though that some moms may find the fit and high compression of these socks too tight.
Best Budget Pregnancy Compression Socks
Enough pairs for the whole week at under $3 each, charmking compression socks.
If you hate laundry and want to stock up on compression socks without breaking the bank, Charmking’s value pack of eight is the way to go. With over 50,000 five-star reviews and an impressive 4.5-average star rating, moms-to-be say they work, well, like a charm to reduce foot and ankle swelling for a fraction of the cost of comparable brands. They’re also breathable and moisture-wicking so you can hit the gym, hike or run in these without worry. Purchase a pack of all black, get an assortment of solid colors or opt for some of the more fun and quirky printed options.
One mom calls them a “godsend” and “super comfy” with the “cutest designs.” Another was surprised at how well they work, noting “they weren’t too hard to get on and the top part doesn’t cut into my legs like my prescription socks did.” They gently hug the legs staying up, even after being worn all day, without constant pulling or tugging.
Best Pregnancy Compression Socks For Travel
Stylish socks frequent fliers and flight attendants swear by, comrad knee-high compression socks.
Purdy and plenty of other women, from flight attendants to moms all over the Internet (just visit any online pregnancy forum asking about the best pregnancy compression socks), praise Comrad’s Knee-High Compression Socks, which are frequently sold out due to their popularity. “They’re made from moisture-wicking nylon, which is a breathable fiber,” says Purdy. “So, the fabric is not overly thick and hot, making them ideal for those who are pregnant and trying to stay cool.” Silver antimicrobial keeps feet fresh for long travel days, while terry cushioning at the heel and a super-soft toe increase comfort so you can enjoy your destination without dying to put your feet up.
“The snug fit provides excellent support and comfort, especially during long hours of standing or travel,” writes one reviewer. Perhaps the best part about these pregnancy compression socks is that they don’t look like compression socks; they’re actually stylish.
Best Pregnancy Compression Socks For Exercise
Working out is a joy in these breathable socks, lululemon micropillow compression knee-high running socks.
These cushioned Lululemon socks offer lightweight compression to keep your legs and feet happy, whether you’re hitting the pavement or the gym. They’re made of breathable mesh in high-sweat areas so your feet stay dry, and are treated with “No-Stink Zinc” to hinder the growth of odor-causing bacteria. For those who like to walk or run in evenings, these socks also have reflective run stripes on the back of the calf to make you more visible to drivers.
“They are the perfect length, are thin enough to go under any pants and stay up where they should,” writes one reviewer. Another reviewer with severe varicose veins, who has tried many brands including pricy medical grade ones, calls these socks “the best for the money.” She says the compression is “firm but comfortable” and the wide band “prevents them from cutting in the back of the knee.”
Best Pregnancy Compression Socks On Amazon
Cloud-like comfort and copper compression at incredible value, blueenjoy copper compression socks.
These bestselling copper compression socks have over 40,000 positive reviews on Amazon and come in a value pack of six, making easier to keep a clean pair on hand. They’re moisture-wicking and infused with copper to help prevent smelly odors, germs and bacteria growth, according to the manufacturer. As an added bonus, there are so many colors and styles to choose from. Reviewers especially love how comfortable they are, which is key when you’re uncomfortable everywhere else.
“I am 30 weeks pregnant and these have been like a cloud to my legs,” writes one. “They don't squeeze my calf muscles too much, but just enough and has helped a lot with my feet swelling.” The socks also have unique temperature regulating properties so you can wear them anytime of year, even in the height of summer. “These are thin enough to wear in Arizona in summer without hating them,” says one reviewer. “The toe box is roomy but not baggy, I didn't pull them once to give my toes relief. They didn't fall down or roll.”
Most Comfortable Pregnancy Compression Socks
Supremely soft and perfect for everyday wear.
Pear Compression
Pear Cotton Crew Compression Socks
These buttery-soft Cotton Crew Compression Socks are truly a dream to wear, especially if you’re like me and prefer something more minimalist and well below the knee you can easily pair with shorts or maternity dresses . They come in three different sizes and three neutral hues: black, gray or white to go with anything.
I like that they feature targeted 360 degree ankle and calf compression to alleviate swelling and increase circulation, as well as toe and heel cushioning for maximum comfort. They’re gentle on even the most sensitive skin, thanks to Standard 100 by Oeko-Tex certification, meaning the materials are verified to be free of chemicals and materials known to be toxic or otherwise harmful.
Best Stylish Pregnancy Compression Socks
Quality, cult-fave compression socks in the cutest colors, bombas women's everyday compression socks.
Cute isn’t a word that typically comes to mind when you think of compression socks, but Bombas Everyday Compression Socks are just that. Purdy loves all the fun color choices and the brand in general, as do I. “They are a medium level of compression, so if that is your preference it's perfect since they will not feel too tight but will be supportive,” she says.
They have a graduated compression that’s tighter around the ankle and looser in the calf, so your legs aren’t being squeezed too much. Other thoughtful details include arch support and no annoying toe seams that can get uncomfortable. They’re also just super soft and high-quality socks that wash well and will hold up over time. I don’t own this pair, but my regular Bombas socks still look great (no holes or pilling) after tons of wear and countless runs and washes.
The 10 Best Hotels In Sedona
The best ipads, according to an apple expert, why trust forbes vetted.
Our editors and writers have spent countless hours researching, testing and reviewing the best baby gear for parents and their little ones, from maternity leggings to the best gifts for expecting moms .
- We are constantly monitoring the industry (it’s our job, after all), and are deeply familiar with many maternity and fashion brands mentioned here.
- The writer of this article is a professional parenting commerce writer, mom of three kids ages 7 and under and a fashion copywriter with a background in fashion public relations, who stays up-to-date on the latest trends in maternity and fashion.
- We consult with highly knowledgable and respected experts in their field. For this story, we interviewed nurse practitioner Christina DeJesus, COO and Co-founder of Orange County’s premier postnatal retreat Ahma & Co , as well as board-certified family medicine physician and medical director of Swell, Dr. Laura Purdy , M.D., M.B.A.
- We regularly update our lists of recommendations to ensure accuracy and freshness. This article was most recently updated in April 2024.
How We Chose The Best Pregnancy Compression Socks
To choose the best pregnancy compression socks, we sought the expertise of a board-certified family medicine physician and a nurse practitioner. Moreover, we know that moms-to-be prioritize insight from other parents, so we only include products well-reviewed and recommended by fellow expecting moms.
- All of the picks on this list were handpicked and recommended by Dr. Purdy herself, each with plenty of reviews from parents to back them up.
- We personally tried most of the brands on this list and can vouch for their quality.
- We analyzed factors like fit, comfort, breathability, compression strength, practicality (how easy they were to get on and off), style and budget when curating this list.
More Recommended Pregnancy Products
- Best Pregnancy Pillows
- Best Shoes For Pregnancy
- Best Maternity Swimsuits
- Best Books To Read During Pregnancy

- Editorial Standards
- Reprints & Permissions
- Investigates
- Houston Life
- Newsletters
WEATHER ALERT
13 warnings, 2 watches and 5 advisories in effect for 27 regions in the area
Morning sickness prenatal check-ups what to know about new rights for pregnant workers.
Alexandra Olson And Claire Savage
Associated Press
Pregnant employees have the right to a wide range of accommodations under new federal regulations for enforcing the Pregnant Workers Fairness Act that supporters say could change workplace culture for millions of people.
The Equal Employment Opportunity Commission, the agency in charge of enforcing the law, adopted an expansive view of conditions related to pregnancy and childbirth in its proposed regulations, including a controversial decision to include abortion, fertility treatment and birth control as medical issues requiring job protections.
Recommended Videos
The rules, which were adopted on a 3-2 vote along partisan lines, were published Monday and offer extensive guidelines for addressing more routine difficulties of pregnancy, such as morning sickness, back pain and needing to avoid heavy lifting. Labor advocates say the law will be especially transformative for pregnant women in low-wage jobs, who are often denied simple requests like more bathroom breaks.
Here's what to know about the law and the EEOC regulations.
WHAT IS THE PREGNANT WORKERS FAIRNESS ACT?
Congress passed the law with bipartisan support in December 2022 following a decade-long campaign by women's rights and labor advocates, who argued that the 1978 Pregnancy Discrimination Act did little to guarantee women would receive the accommodations they might need at work.
The law stated only that pregnant workers should be treated the same as other employees, not that they deserved special consideration. To get their requests met, many pregnant workers therefore needed to demonstrate they had physical limitations covered under the Americans With Disabilities Act, often creating insurmountable hurdles.
The new law treats pregnancy and related conditions as themselves deserving of “reasonable accommodations” and places the burden on employers to prove “undue hardships” for denying any requests.
The law applies to employers of at least 15 workers . The EEOC estimates it will cover roughly 1.5 million pregnant workers in any given year. The EEOC regulations published April 15 are set to go into effect in June.
WHAT ARE WORKERS ENTITLED TO?
The EEOC's 400-page document encompasses a wide array of conditions and relevant advice for employers.
It states that workers are entitled to unpaid time off for situations such as prenatal appointments , fertility treatments, abortion, miscarriage, postpartum depression and mastitis, an infection that arises from breastfeeding. This includes workers who are not covered by federal family leave laws and those who have not been on the job long enough to accrue time off.
Workers can ask for flexible working arrangements to deal with morning sickness, such as a later start time, clearance to work from home or permission to carry snacks in workplaces where eating is typically prohibited. If they can't sit or stand for extended periods due to sciatica, which is common in late pregnancy, they can request a schedule adjustment so their commutes happen during less crowded hours.
The regulations also allow workers to be exempted from tasks such as climbing ladders or heavy lifting. If those duties are essential to their jobs, they can still request a temporary dispensation, according to the EEOC.
Employers don’t have to accommodate workers exactly as requested but they must offer reasonable alternatives. They cannot deny a request without clearing a high bar to prove doing so would cause “undue hardships” for the organization’s finances or operations. They cannot force workers to take unpaid leave if a reasonable accommodation is available.
HOW SHOULD WORKERS REQUEST ACCOMMODATIONS?
The EEOC emphasizes that it “should not be complicated or difficult” for pregnant workers to request accommodations. Workers don't have to make requests in writing, use specific words, cite any laws, or in most cases, provide documentation such as doctors' notes. Employers must respond quickly and have a conversation about how to reasonably accommodate a worker’s needs.
Still, legal experts advise both workers and employers to document the process. A Better Balance, the non-profit that spearheaded the 10-year campaign for the law's passage, advises workers to familiarize themselves with their legal rights and be as specific as possible about their limitations and the changes they they need.
Workers who believe a request was denied illegally can file a complaint with the EEOC . They have 180 days to do so, though the deadline can be extended in some states.
WHAT DO THE EEOC RULES SAY ABOUT ABORTION?
The EEOC included abortion among the conditions covered under the law. The rules state, however, that employers are not obligated to cover expenses related to the procedure or to offer health insurance that does.
The EEOC regulations argue that including abortion is consistent with the agency's longstanding interpretation of other laws under Title VII of the 1964 Civil Rights Act, including the Pregnancy Discrimination Act.
But the decision drew condemnation from Republican lawmakers who had championed the law's passage. The five-member EEOC's two Republican members voted against the regulations.
In a statement explaining her dissent, Commissioner Andrea Lucas said the agency broadened the scope of the law “to reach virtually every condition, circumstance, or procedure that relates to any aspect of the female reproductive system" in ways that "cannot reasonably be reconciled with the text" of the law.
Melissa Losch, a labor and employment attorney at the New Orleans-based firm McGlinchey Stafford, said she expects the regulations to give rise to further litigation. Losch cited the example of a worker living in a state with a restrictive abortion law requesting time off to undergo the procedure in another state. The EEOC rules provide “no good answer” about whether granting such a request would conflict with restrictive state abortion laws, she added.
ARE WORKERS IN TEXAS COVERED?
On February 27, a federal judge blocked enforcement of the Pregnant Workers Fairness Act for Texas state employees, a ruling that came in response to a lawsuit filed by Texas Attorney General Ken Paxton. Paxton argued the law was unconstitutional because it was part of a spending bill that passed in the House without a majority of members present, and the judge ruled in his favor.
Gedmark, of A Better Balance, said she was optimistic the Biden administration would prevail in its expected appeal of the ruling. In the meantime, federal and private sectors workers in Texas are covered by the law.
But in her dissenting statement, Lucas warned that if the Texas case or any future lawsuits succeed in overturning the law, the EEOC's divisive rules have “all but extinguished” the chances of a bipartisan effort to reenact it.
WHAT HAS THE LAW'S IMPACT BEEN SO FAR?
Employers have been obligated to abide by the Pregnant Workers Fairness Act since it took effect on June 27, 2023, though the EEOC regulations provided guidance on how to do so.
The law swiftly made a difference to many low-wage workers, according to Gedmark.
A Better Balance, which operates a helpline, has “heard an overwhelmingly positive experience from workers,” she said. Last summer, the organization worked with some women whose employers stopped resisting requests for accommodations as soon as the law took effect, Gedmark said.
Some workers reported their employers were still operating under the old legal framework, handing them pages of disability paperwork to fill out in response to requests.
The EEOC said it received almost 200 complaints alleging violations of the law by the time the fiscal year ended on Sept. 30, 2023.
Gedmark said the success of the law will depend on enforcement and raising awareness.
“If workers don’t know about the law and don’t know about their rights, then it really undermines the purpose of the law,” she said.
The Associated Press’ women in the workforce and state government coverage receives financial support from Pivotal Ventures. AP is solely responsible for all content. Find AP’s standards for working with philanthropies, a list of supporters and funded coverage areas at AP.org.
Copyright 2024 The Associated Press. All rights reserved. This material may not be published, broadcast, rewritten or redistributed without permission.
Nearly 200 people sick in norovirus outbreaks on Princess, Royal Caribbean ships

Nearly 200 people got sick in norovirus outbreaks on Princess Cruises and Royal Caribbean International ships.
The Centers for Disease Control and Prevention said 94 of the 2,532 guests on Sapphire Princess reported being ill during its April 5 cruise, along with 20 crew members. The round-trip cruise, which left from Los Angeles with stops in Hawaii and the South Pacific, will end on May 7, according to CruiseMapper .
On Royal Caribbean’s Radiance of the Seas, 67 of its 1,993 guests reported being ill in addition to two crew members during a cruise that ended April 22, according to the CDC . The two-week voyage sailed from Tampa, Florida to Los Angeles with stops in countries like Colombia and Panama, according to CruiseMapper .
In both outbreaks, the guests and crew members’ main symptoms were diarrhea and vomiting.
Princess, Royal Caribbean and the ships’ crews implemented heightened cleaning and disinfection measures and isolated those who were sick, among other steps, the health agency said.
"At the first sign of an increase in the numbers of passengers reporting to the medical center with gastrointestinal illness, we immediately initiated additional enhanced sanitation procedures to interrupt the person-to-person spread of this virus," a Princess spokesperson told USA TODAY in an emailed statement. "Our sanitation program, developed in coordination with the CDC, includes disinfection measures, isolation of ill passengers and communication to passengers about steps they can take to stay well while onboard."
Royal Caribbean did not immediately respond to a request for comment.
The CDC has logged six outbreaks of gastrointestinal illness on cruise ships that met its threshold for public notification since the beginning of the year. Norovirus was listed as the causative agent in five, while one was unknown.
The illness is often associated with cruise ships but outbreaks occur in communities on land as well, according to Dr. Sarah E. Hochman, a hospital epidemiologist and the section chief of infectious diseases at NYU Langone Health’s Tisch Hospital.
“There's not something special or unique about cruise ships,” she said. “It's really any type of congregate setting, but it's also happening out in the community on a much smaller scale among households and household contacts. It just doesn't come to the attention of public health as much as it does for larger congregate settings.”
Hochman said the virus is “incredibly infectious” and congregate settings tend to have many shared surfaces, such as handrails in cruise ship stairwells or elevators. “And so, if you just have one person who's shedding the virus and touches the surface and then someone else touches it and then touches their mouth, that's how it can spread in those types of settings.”
Cruise ship medical facilities: What happens if you get sick or injured (or bitten by a monkey)
Alcohol-based hand sanitizer isn't as effective against norovirus, and Hochman emphasized that washing hands with soap and water “will do a lot to prevent the spread.”
The news comes after more than two dozen Silversea Cruises guests got sick in a gastrointestinal illness outbreak on the luxury line’s Silver Nova ship during a sailing that began in late March.
Nathan Diller is a consumer travel reporter for USA TODAY based in Nashville. You can reach him at [email protected].
- Election 2024
- Entertainment
- Newsletters
- Photography
- Personal Finance
- AP Investigations
- AP Buyline Personal Finance
- AP Buyline Shopping
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Election Results
- Delegate Tracker
- AP & Elections
- Auto Racing
- 2024 Paris Olympic Games
- Movie reviews
- Book reviews
- Personal finance
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
Morning sickness? Prenatal check-ups? What to know about new rights for pregnant workers
FILE - The emblem of the U.S. Equal Employment Opportunity Commission is shown on a podium in Vail, Colo., Tuesday, Feb. 16, 2016, in Denver. Pregnant workers have the right to a wide range of accommodations under new federal regulations for implementing the Pregnant Workers Fairness Act. The regulations take an expansive view of conditions related to pregnancy, from fertility treatments to abortion and post-childbirth complications. (AP Photo/David Zalubowski, File)
- Copy Link copied
Pregnant employees have the right to a wide range of accommodations under new federal regulations for enforcing the Pregnant Workers Fairness Act that supporters say could change workplace culture for millions of people.
The Equal Employment Opportunity Commission, the agency in charge of enforcing the law, adopted an expansive view of conditions related to pregnancy and childbirth in its proposed regulations, including a controversial decision to include abortion, fertility treatment and birth control as medical issues requiring job protections.
The rules, which were adopted on a 3-2 vote along partisan lines, were published Monday and offer extensive guidelines for addressing more routine difficulties of pregnancy, such as morning sickness, back pain and needing to avoid heavy lifting. Labor advocates say the law will be especially transformative for pregnant women in low-wage jobs, who are often denied simple requests like more bathroom breaks.
Here’s what to know about the law and the EEOC regulations.
WHAT IS THE PREGNANT WORKERS FAIRNESS ACT?
Congress passed the law with bipartisan support in December 2022 following a decade-long campaign by women’s rights and labor advocates, who argued that the 1978 Pregnancy Discrimination Act did little to guarantee women would receive the accommodations they might need at work.
The law stated only that pregnant workers should be treated the same as other employees, not that they deserved special consideration. To get their requests met, many pregnant workers therefore needed to demonstrate they had physical limitations covered under the Americans With Disabilities Act, often creating insurmountable hurdles.
The new law treats pregnancy and related conditions as themselves deserving of “reasonable accommodations” and places the burden on employers to prove “undue hardships” for denying any requests.
The law applies to employers of at least 15 workers . The EEOC estimates it will cover roughly 1.5 million pregnant workers in any given year. The EEOC regulations published April 15 are set to go into effect in June.
WHAT ARE WORKERS ENTITLED TO?
The EEOC’s 400-page document encompasses a wide array of conditions and relevant advice for employers.
It states that workers are entitled to unpaid time off for situations such as prenatal appointments , fertility treatments, abortion, miscarriage, postpartum depression and mastitis, an infection that arises from breastfeeding. This includes workers who are not covered by federal family leave laws and those who have not been on the job long enough to accrue time off.
Workers can ask for flexible working arrangements to deal with morning sickness, such as a later start time, clearance to work from home or permission to carry snacks in workplaces where eating is typically prohibited. If they can’t sit or stand for extended periods due to sciatica, which is common in late pregnancy, they can request a schedule adjustment so their commutes happen during less crowded hours.
The regulations also allow workers to be exempted from tasks such as climbing ladders or heavy lifting. If those duties are essential to their jobs, they can still request a temporary dispensation, according to the EEOC.
Employers don’t have to accommodate workers exactly as requested but they must offer reasonable alternatives. They cannot deny a request without clearing a high bar to prove doing so would cause “undue hardships” for the organization’s finances or operations. They cannot force workers to take unpaid leave if a reasonable accommodation is available.
HOW SHOULD WORKERS REQUEST ACCOMMODATIONS?
The EEOC emphasizes that it “should not be complicated or difficult” for pregnant workers to request accommodations. Workers don’t have to make requests in writing, use specific words, cite any laws, or in most cases, provide documentation such as doctors’ notes. Employers must respond quickly and have a conversation about how to reasonably accommodate a worker’s needs.
Still, legal experts advise both workers and employers to document the process. A Better Balance, the non-profit that spearheaded the 10-year campaign for the law’s passage, advises workers to familiarize themselves with their legal rights and be as specific as possible about their limitations and the changes they they need.
Workers who believe a request was denied illegally can file a complaint with the EEOC . They have 180 days to do so, though the deadline can be extended in some states.
WHAT DO THE EEOC RULES SAY ABOUT ABORTION?
The EEOC included abortion among the conditions covered under the law. The rules state, however, that employers are not obligated to cover expenses related to the procedure or to offer health insurance that does.
The EEOC regulations argue that including abortion is consistent with the agency’s longstanding interpretation of other laws under Title VII of the 1964 Civil Rights Act, including the Pregnancy Discrimination Act.
But the decision drew condemnation from Republican lawmakers who had championed the law’s passage. The five-member EEOC’s two Republican members voted against the regulations.
In a statement explaining her dissent, Commissioner Andrea Lucas said the agency broadened the scope of the law “to reach virtually every condition, circumstance, or procedure that relates to any aspect of the female reproductive system” in ways that “cannot reasonably be reconciled with the text” of the law.
Melissa Losch, a labor and employment attorney at the New Orleans-based firm McGlinchey Stafford, said she expects the regulations to give rise to further litigation. Losch cited the example of a worker living in a state with a restrictive abortion law requesting time off to undergo the procedure in another state. The EEOC rules provide “no good answer” about whether granting such a request would conflict with restrictive state abortion laws, she added.
ARE WORKERS IN TEXAS COVERED?
On February 27, a federal judge blocked enforcement of the Pregnant Workers Fairness Act for Texas state employees, a ruling that came in response to a lawsuit filed by Texas Attorney General Ken Paxton. Paxton argued the law was unconstitutional because it was part of a spending bill that passed in the House without a majority of members present, and the judge ruled in his favor.
Gedmark, of A Better Balance, said she was optimistic the Biden administration would prevail in its expected appeal of the ruling. In the meantime, federal and private sectors workers in Texas are covered by the law.
But in her dissenting statement, Lucas warned that if the Texas case or any future lawsuits succeed in overturning the law, the EEOC’s divisive rules have “all but extinguished” the chances of a bipartisan effort to reenact it.
WHAT HAS THE LAW’S IMPACT BEEN SO FAR?
Employers have been obligated to abide by the Pregnant Workers Fairness Act since it took effect on June 27, 2023, though the EEOC regulations provided guidance on how to do so.
The law swiftly made a difference to many low-wage workers, according to Gedmark.
A Better Balance, which operates a helpline, has “heard an overwhelmingly positive experience from workers,” she said. Last summer, the organization worked with some women whose employers stopped resisting requests for accommodations as soon as the law took effect, Gedmark said.
Some workers reported their employers were still operating under the old legal framework, handing them pages of disability paperwork to fill out in response to requests.
The EEOC said it received almost 200 complaints alleging violations of the law by the time the fiscal year ended on Sept. 30, 2023.
Gedmark said the success of the law will depend on enforcement and raising awareness.
“If workers don’t know about the law and don’t know about their rights, then it really undermines the purpose of the law,” she said.
The Associated Press’ women in the workforce and state government coverage receives financial support from Pivotal Ventures. AP is solely responsible for all content. Find AP’s standards for working with philanthropies, a list of supporters and funded coverage areas at AP.org.


IMAGES
VIDEO
COMMENTS
Before you book a cruise or air travel, check the airlines or cruise operator policies for pregnant women. Some airlines will let you fly until 36 weeks, but others may have an earlier cutoff. Cruises may not allow you to travel after 24-28 weeks of pregnancy, and you may need to have a note from your doctor stating you are fit to travel.
Motion sickness is a relatively common problem encountered when people travel by car, by airplane, and particularly by boat. It occurs when your body's balance-sensing system - which includes your inner ear, your eyes, and the sensory nerves in your skin, muscles, and joints - sends conflicting messages to the brain.
Antihistamines (e.g., dimenhydrinate, meclizine) often are used in pregnancy for morning sickness and motion sickness and appear to have a good safety record. Carefully consider appropriate pain management and use of analgesics during pregnancy. Acetaminophen remains the nonopioid analgesic of choice during pregnancy.
The best time to travel is mid-pregnancy (14 to 28 weeks). During these weeks, your energy has returned, morning sickness is improved or gone, and you are still able to get around easily. After 28 weeks, it may be harder to move around or sit for a long time. Preparing for a Trip Expand All.
Motion sickness during pregnancy can be a challenging aspect of expecting mothers' lives. While the experience varies from woman to woman, understanding the causes, symptoms, and potential management strategies is crucial for those dealing with this discomfort. ... Motion sickness, often referred to as travel sickness, is a condition where an ...
Most people can safely travel by airplane during pregnancy, but talk to your healthcare provider ahead of time to make sure you don't have any medical conditions that could cause a complication ...
Travel During Pregnancy. As long as there are no identified complications or concerns with your pregnancy, it is generally safe to travel during your pregnancy. The ideal time to travel during pregnancy is the second trimester. In most cases, you are past the morning sickness of the first trimester and several weeks from the third stage of ...
Virgin Australia. No restrictions. Travel permitted; requires a medical certificate dated within 10 days of departure date once you reach 28 weeks. For flights longer than four hours, travel is not permitted after 36 weeks of pregnancy (32 weeks if pregnant with multiples), or within 48 hours of normal vaginal delivery.
Generally, air travel before 36 weeks of pregnancy is considered safe for people who aren't dealing with any pregnancy problems. Still, if you're pregnant, it's a good idea to talk with your health care provider before you fly. Your provider might suggest that you not fly if you have certain pregnancy complications that could get worse because ...
Some women prefer not to travel in the first 12 weeks of pregnancy because of nausea and vomiting and feeling very tired during these early stages. The risk of miscarriage is also higher in the first 3 months, whether you're travelling or not. Travelling in the final months of pregnancy can be tiring and uncomfortable.
ABSTRACT: In the absence of obstetric or medical complications, occasional air travel is safe for pregnant women. Pregnant women can fly safely, observing the same precautions for air travel as the general population. Because severe air turbulence cannot be predicted and the subsequent risk for trauma is significant should this occur, pregnant women should be instructed to use their seat belts ...
You should avoid travelling to an altitude above 3,658 metres (12,000 feet). However, if you have a high-risk pregnancy and/or are in the late stages of pregnancy, the highest altitude should be 2,500 metres (8,200 feet). If you have pregnancy-related complications, you should avoid unnecessary high-altitude exposure.
Travel in Pregnancy MotherSafe - Royal Hospital for Women Updated February 2023 ... sickness or nausea and vomiting —that combined with the increased risk of falls on a moving vessel may lead many pregnant women to postpone sea travel until after the baby is born, particularly if they haven't travelled by sea before. Respiratory and food ...
If you feel sick while traveling at higher altitudes than you're used to, go to a lower altitude. And if you still don't feel well after you descend, seek medical care. ... Jean D, et al. 2012. Travel to high altitude during pregnancy: Frequently asked questions and recommendations for clinicians. High Altitude Medicine and Biology 13(2):73-81.
Compression socks. "During pregnancy, you are at an increased risk of developing a blood clot," Louise says. "That's why compression socks, hydration, and movement—walking, stretching ...
Most commercial airlines accept pregnant travellers up to 36 weeks if single pregnancy or up to 32 weeks if a multiple pregnancy. This is because labour is more likely after 37 weeks, or around 32 weeks if carrying an uncomplicated twin pregnancy. Some airlines require written documentation from your practice nurse, midwife or obstetrician.
Drink more water than you think you need. This one holds true regardless of whether you're pregnant or not: Drink lots of water on your flight. Staying hydrated while flying is one of the best ...
The first trimester is usually marked by morning sickness and fatigue. Therefore, the ideal time to travel during pregnancy, as suggested by health experts, typically falls within the second ...
Travel insurance from Allianz Global Assistance can cover losses resulting from unforeseen pregnancy complications, such as pre-eclampsia, gestational diabetes or hyperemesis gravidarum. That means your travel insurance may reimburse you for nonrefundable trip costs lost if you must cancel or interrupt your trip because of pregnancy complications.
The expert view. If you're really struggling with sickness during your pregnancy, there's good news: anti-sickness medications are safe to take during pregnancy if prescribed by a doctor. Anti-sickness drugs have had a difficult history - see more below - but rest assured, there is medicine you can take which won't harm your baby.
Rather, pregnant people will need to consider travel insurance that includes coverage for trip cancellation and interruption, as well as emergency medical and evacuation costs. Your decision to ...
Key facts. Motion sickness is also known as travel sickness, car sickness or sea sickness. If you have motion sickness, you are likely to have nausea and may vomit and feel clammy. You can help prevent motion sickness by looking outside of the vehicle or focusing on the horizon. Symptoms usually end once the motion stops.
If you are sick while pregnant, there are some steps you can take to get well. Rest - As noted above, a rested bo dy helps your immune system work better. A healthy immune system can help shorten your sick period. Stay Hydrated - Fluids are also essential to a healthy body. Fluids also help wash out your system.
Drowsiness, constipation, blurred vision, or dry mouth /nose/throat may occur. If any of these effects last or get worse, tell your doctor or pharmacist promptly. To relieve dry mouth, suck ...
Morning sickness affects almost 75% of pregnant people. While home remedies and prevention strategies can be effective, sometimes they just aren't enough. Many people find relief by taking Unisom ...
The best pregnancy compression socks can help you get back on your feet comfortably, boosting blood circulation, reducing swelling and helping prevent blood clots, so you can work, travel, chill ...
Pregnant employees have the right to a wide range of accommodations under new federal regulations for enforcing the Pregnant Workers Fairness Act that supporters say could change workplace culture ...
Pregnant employees have the right to a wide range of accommodations under new federal regulations for enforcing the Pregnant Workers Fairness Act that supporters say could change workplace culture ...
Nearly 200 people got sick in norovirus outbreaks on Princess Cruises and Royal Caribbean International ships. The Centers for Disease Control and Prevention said 94 of the 2,532 guests on ...
Pregnant employees have the right to a wide range of accommodations under new federal regulations for enforcing the Pregnant Workers Fairness Act that supporters say could change workplace culture for millions of people.. The Equal Employment Opportunity Commission, the agency in charge of enforcing the law, adopted an expansive view of conditions related to pregnancy and childbirth in its ...