- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games

Traveling while pregnant: Your complete guide
Unless you're nearing your due date or have certain complications, your healthcare provider will generally give you the green light for pregnancy travel. Here's how to safely explore – plus what to consider before making plans.

Is traveling while pregnant safe?
When to avoid pregnancy travel, when is the best time to travel while you're pregnant , can pregnant women travel during covid, when should you stop traveling while pregnant, your pregnancy travel checklist, when to call your doctor while traveling.
Yes, it's generally safe to travel during pregnancy as long as you're not too close to your due date and you're not experiencing any serious pregnancy complications. There are special precautions to take, of course, and you may find yourself stopping to use the bathroom more than you're used to, but that babymoon can be within reach.
Before you pack your suitcase, talk with your healthcare provider to make sure it’s safe for you to travel and that your destination is a good choice. You'll want to avoid places where infectious diseases are prevalent (or there are high outbreaks of Zika or malaria, for example). The COVID-19 pandemic has made people reconsider where they feel safe traveling as well; if you're fully vaccinated, the CDC says you can travel Opens a new window , but it's always best to check with your doctor first.
And bear in mind that the activities you take part in might be different than normal – you'll want to skip the Scuba diving lessons, for example (though snorkeling is okay!).
It's safe to fly when you're pregnant as well, and most airlines will allow you to fly domestically until about 36 weeks of pregnancy. International routes may have different rules, so be sure to check with your airline before booking anything. Your doctor will tell you to avoid flying, however, if you have a health concern that might require emergency care or any other health conditions that aren’t well controlled.
It's best to avoid traveling while pregnant if you have any health conditions that can be life-threatening to both you or your baby. If you have any of the following conditions, your doctor will almost certainly advise you against travel:
- Placental abruption
- Preeclampsia
- You're in preterm or active labor
- Cervical insufficiency (incompetent cervix)
- Premature rupture of membranes (PROM)
- A suspected ectopic pregnancy
- Vaginal bleeding
You might also need to be extra-cautious or skip travel if you're experiencing intrauterine growth restriction , you have placenta previa , or you have other conditions that may place your pregnancy at a higher risk. It’s always a good idea to discuss your concerns with your healthcare provider before travel regarding any medical conditions you have, and they'll be able to advise you on what's best, depending on the trip.
The sweet spot for pregnancy travel is during your second trimester , between 14 weeks and 27 weeks. By the second trimester, any struggles you’ve had with morning sickness and fatigue during the earlier weeks of pregnancy should have hopefully subsided – and after 12 weeks, your risk of miscarriage decreases significantly as well. And you're not too far along to worry about third trimester exhaustion or going into preterm labor yet, either.
Your energy levels are likely to be good during your second trimester too (bring on the sightseeing!), and it will still be relatively easy and comfortable for you to travel and move around at this time. Keep in mind that once you hit that third trimester, pregnancy travel might be more difficult as you find it harder to move around and stay still for long periods of time.
It's complicated (and often a personal decision based on your own risk factors), but the CDC says that if you're fully vaccinated against COVID-19, you can travel. Of course, it's important you still do everything you can to keep yourself and others around you safe, including following all mask-wearing and social distancing guidelines in the destination you visit.
Women are at an increased risk for severe illness if they contract COVID-19 while pregnant , and they're more likely to experience preterm birth and other poor pregnancy outcomes. (This is why the CDC, the American College of Obstetricians and Gynecologists, and the Society for Maternal-Fetal Medicine all recommend that women who are pregnant, breastfeeding, or are planning on becoming pregnant get the COVID vaccine .)
If you're vaccinated and decide to travel, the CDC advises avoiding international destinations that are designated Level 4, due to high rates of local COVID-19 transmission.
Take all this information into account and talk to your doctor before you decide on where and when to travel while you're pregnant. And if you experience any symptoms of COVID-19, whether while traveling or at home, call your healthcare provider as soon as possible.
The guidelines for when to stop traveling while you're pregnant vary based on your mode of travel, but more or less, you should wrap up travel before you're 36 weeks pregnant.
Most airlines will let pregnant women fly domestically until they're 36 weeks pregnant – and many cut that off earlier for international travel. This rule is often enforced on an honor system policy, but some airlines may ask for a doctor’s note – so make sure you have that from your healthcare provider if you're traveling in the third trimester, just in case.
Most cruise ships don't allow travel after 24 weeks of pregnancy. Some cruise lines' cutoff dates vary, so verify policies before booking a cruise.
As for road trips, there's no official deadline for when you need to stop traveling, but your personal comfort level (physically and emotionally) – and your doctor's advice – might help you decide. You can drive while pregnant all the way up until your due date, but things may get considerably less comfortable on longer trips as you approach full term.
Travel of any kind requires advance preparation, but when you're pregnant and traveling, that pre-trip checklist gets a little longer. Give yourself a little more time than usual to plan for a trip – and use the tips below to stay safe and comfortable on your next adventure.
Before you travel
- Talk to your healthcare provider to determine if your trip is safe for you and if there are any medical concerns to consider. It's a good idea to discuss any activities you plan to do while you're away too. If you're planning an international trip, make sure to ask about any vaccines you may need for the areas you're visiting.
- Make sure you know your prenatal test schedule. Plan travels around any prenatal tests you need to schedule, including ultrasounds and other important screening tests.
- Book an aisle seat. You'll likely be more comfortable being able to get up to stretch or go to the bathroom on longer flights.
- Buy travel insurance. You don't need special travel insurance when you're pregnant, but it's never a bad idea to secure a policy. You may want to consider one with a “cancel for any reason” clause that reimburses you for money lost on cancelled trips for reasons (read: any reason) beyond what’s listed on the base policy. Check with your personal health insurance, too, to make sure it covers potential pregnancy complications while traveling internationally (some don’t). Consider adding evacuation insurance as part of a travel insurance plan, too.
- Gather your medical records and health information . If you’re in your second or third trimester, ask your ob-gyn or midwife for a digital copy of your prenatal chart, and have that easily accessible during your trip. Typically, this chart includes your age, your blood type, the name and contact information for your healthcare provider, the date of your last menstrual period, your due date, information about any prior pregnancies, your risk factors for disease, results of pregnancy-related lab tests (including ultrasounds or other imaging tests), your medical and surgical history, and a record of vital signs taken at each visit.
- Keep a list of key names and numbers you may need in the event of an emergency saved on your phone and written on a piece of paper (in case your battery dies).
- Have a contingency plan for doctors and hospitals that will take your insurance where you're going in case you go into labor early or experience pregnancy complications that require urgent care while you're away from home.
- Pack medicines and prenatal vitamins. That might include an extended supply of prescriptions and over-the-counter remedies , too. Bring enough to cover your entire trip and a written prescription that you can fill if you lose anything. It's a good idea to keep prescription medicine in its original container, so if your bags are searched it will be clear that you're not using medication without a prescription.
- Prepare for the unexpected. On a road trip, that might mean an unexpected breakdown, so join an auto club that provides roadside assistance. Download any apps you use for renting cars and accessing boarding passes before you leave so you can easily reschedule things in the event of a last-minute cancellation.
- If you're flying during your third trimester, be sure to call the airline to check about the cutoff week for pregnancy travel. A note from your doctor that says you’re cleared to travel is always good to have when traveling during your third trimester.
During your trip
- Drink plenty of water and continue to eat healthy foods . Keep in mind that many restaurants abroad commonly serve unpasteurized foods (like soft cheeses and milk), which can be dangerous for pregnant women due to the presence of listeria.
- Avoid eating raw or undercooked meat or fish , drinks with ice (which may be contaminated), non-bottled water, and other foods that can cause traveler's diarrhea, which can be more of a problem for pregnant women than other people.
- On long flights and drives, take time to stretch by pulling over for a walk or strolling up and down the airplane aisle. And when seated, always wear your seat belt .
- Maternity compression socks are handy to have along – both in transit and worn under your clothes while you’re out and about exploring – because they can ease the symptoms of swollen feet and legs. These are a few of our favorite pregnancy compression socks .
- Take advantage of help. Many countries have dedicated lines in shops and airports for pregnant travelers, so don't feel any shame taking a shorter wait if you see one.
- Go easy on yourself. Remember, you're growing a baby. You might not have quite the stamina for sightseeing and late nights like you used to pre-pregnancy. Make the most of your vacation but don't fret you miss out on things because you need more downtime from exploring than you usually would.
- Don’t forget to get photos of your bump. When your baby is older, you'll have fun showing them all the places you traveled with them before they were born.
- Go for the comfy shoes. Travel during pregnancy is the best reason ever to forgo those strappy stilettos for your favorite sneakers .
- Pack snacks so you always have something to curb your appetite if there’s a long wait for a restaurant or you get stuck in transit or someplace remote with no food offerings.
- Try to be in the moment with your travel partners as much as possible. Once your baby is born, your attention will be pulled in a whole new direction.
If you have any medical concerns traveling while pregnant, don’t hesitate to pick up the phone and call your doctor for advice. The below are a few symptoms that definitely warrant calling your ob-gyn or health care provider or seeking emergency care while traveling or at home:
- Signs of pre-term labor (including a constant, low dull backache, bleeding, etc.)
- Ruptured membranes (your water breaks)
- Severe cramping
- Spiking blood pressure
- Severe nausea or vomiting
- COVID-19 symptoms
Was this article helpful?
Best compression socks for pregnancy

Is it safe to fly while I'm pregnant?

Is it safe to travel to high altitudes while pregnant?

When can I travel again after giving birth?

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
AAFP. 2020. Ultrasound during pregnancy. American Academy of Family Physicians. https://familydoctor.org/ultrasound-during-pregnancy/ Opens a new window [Accessed April 2023]
ACOG. 2020. FAQ055: Travel during pregnancy. American College of Obstetricians and Gynecologists. https://www.acog.org/womens-health/faqs/travel-during-pregnancy Opens a new window [Accessed April 2023]
CDC. 2019. Pregnant Travelers. https://wwwnc.cdc.gov/travel/yellowbook/2020/family-travel/pregnant-travelers Opens a new window [Accessed April 2023]
CDC. 2022. Domestic Travel During Covid-19. https://www.cdc.gov/coronavirus/2019-ncov/travelers/travel-during-covid19.html Opens a new window [Accessed April 2023]
CDC 2023. International Travel During Covid-19. https://www.cdc.gov/coronavirus/2019-ncov/travelers/international-travel-during-covid19.html Opens a new window [Accessed April 2023]
CDC. 2022. Covid-19: Pregnant and Recently Pregnant People. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/pregnant-people.html Opens a new window [Accessed April 2023]

Terry Ward is a freelance travel, health, and parenting writer who has covered everything from flying with toddlers to why you should travel with your kids even when they're too young to remember it. She lives in Tampa, Florida, with her husband and their young son and daughter, and enjoys camping, sailing, scuba diving, skiing, and almost anything else done in the great outdoors.
Where to go next

Appointments at Mayo Clinic
- Pregnancy week by week
Is it safe to fly during pregnancy?
Generally, air travel before 36 weeks of pregnancy is considered safe for people who aren't dealing with any pregnancy problems. Still, if you're pregnant, it's a good idea to talk with your health care provider before you fly.
Your provider might suggest that you not fly if you have certain pregnancy complications that could get worse because of air travel or that could require emergency care. Examples include a history of miscarriage or vaginal bleeding, severe anemia, and high blood pressure or diabetes that's not well controlled. If you had preeclampsia during a previous pregnancy — a condition that causes high blood pressure and extra protein in urine — flying may not be advised. The same is true if you're pregnant with twins or other multiples.
Tell your provider how far you are flying, as the length of the flight might make a difference. Also, be aware that some airlines may not allow pregnant people on international flights. Check with your airline before you make travel arrangements.
After 36 weeks of pregnancy, your health care provider may advise against flying. And some airlines don't allow pregnant people to fly after 36 weeks. The airline also may require a letter from your health care provider that states how far along in your pregnancy you are and whether flying is advised.
If your health care provider says it's okay for you to fly, and your plans are flexible, the best time to travel by air might be during the second trimester. The risks of common pregnancy emergencies are lowest during that time.
When you fly:
- Buckle up. During the trip, keep your seatbelt fastened when you are seated, and secure it under your belly.
- Drink plenty of fluids. Low humidity in the airplane could cause you to become dehydrated.
- Avoid gassy foods and drinks before you fly. Gases expand during flight, and that could make you uncomfortable. Examples of foods and drinks to avoid include broccoli and carbonated soda.
- Think about medical care. Plan for how you'll get obstetric care during your trip if you need it. Bring copies of your medical information in case you need care while you're away.
Blood clots
Air travel can raise the risk for blood clots in the legs, a condition called venous thrombosis. The risk is higher for pregnant people. Moving your legs may help prevent this problem. Take a walk up and down the aisle every hour during the flight. If you must remain seated, flex and extend your ankles from time to time. In general, it's best to avoid tightfitting clothing, as that can hinder blood flow. Wearing compression stockings can help with blood circulation during a long flight.
Radiation exposure linked to air travel at high altitudes isn't thought to be a problem for most people who fly during pregnancy. But pilots, flight attendants and others who fly often might be exposed to a level of radiation that raises concerns during pregnancy. If you must fly frequently during your pregnancy, talk about it with your health care provider.
Mary Marnach, M.D.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Allergy medications during pregnancy
- AskMayoExpert. Health considerations for air travelers: Pregnancy considerations. Mayo Clinic; 2022.
- Air Travel During Pregnancy: ACOG Practice Bulletin No. 746. American College of Obstetricians and Gynecologists. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/08/air-travel-during-pregnancy. Accessed Dec. 1, 2022.
- Ram S, et al. Air travel during pregnancy and the risk of venous thrombosis. American Journal of Obstetrics and Gynecology. 2022; doi:10.1016/j.ajogmf.2022.100751.
Products and Services
- A Book: Obstetricks
- Available Solutions for Prenatal Nutrition from Mayo Clinic Store
- A Book: Taking Care of You
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- Ankle swelling during pregnancy
- Antibiotics and pregnancy
- Aspirin during pregnancy
- Pregnancy back pain
- Falling during pregnancy: Reason to worry?
- Fetal ultrasound
- Flu shot in pregnancy
- Headaches during pregnancy: What's the best treatment?
- Iron deficiency anemia during pregnancy: Prevention tips
- Leg cramps during pregnancy
- Pregnancy acne
- Pregnancy and fish
- Pregnancy constipation
- Pregnancy diet: Essential nutrients
- Pregnancy due date calculator
- Pregnancy exercises
- Pregnancy nutrition don'ts
- Pregnancy stretches
- Pregnancy weight gain
- Pregnant. Now What Happens?
- Prenatal testing
- Prenatal vitamins and pregnancy
- Sex during pregnancy
- Twin pregnancy
- Vaccines during pregnancy
- Vaping during pregnancy
- Working during pregnancy
- X-ray during pregnancy
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Expert Answers
- Air travel during pregnancy Is it safe
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
Pregnant Travelers

Pregnant travelers can generally travel safely with appropriate preparation. But they should avoid some destinations, including those with risk of Zika and malaria. Learn more about traveling during pregnancy and steps you can take to keep you and your baby healthy.
Before Travel
Before you book a cruise or air travel, check the airlines or cruise operator policies for pregnant women. Some airlines will let you fly until 36 weeks, but others may have an earlier cutoff. Cruises may not allow you to travel after 24–28 weeks of pregnancy, and you may need to have a note from your doctor stating you are fit to travel.
Zika and Malaria
Zika can cause severe birth defects. The Zika virus is spread through mosquito bites and sex. If you are pregnant, do not travel to areas with risk of Zika . If you must travel to an area with Zika, use insect repellent and take other steps to avoid bug bites. If you have a sex partner who lives in or has traveled to an area with Zika, you should use condoms for the rest of your pregnancy.
Pregnant travelers should avoid travel to areas with malaria, as it can be more severe in pregnant women. Malaria increases the risk for serious pregnancy problems, including premature birth, miscarriage, and stillbirth. If you must travel to an area with malaria, talk to your doctor about taking malaria prevention medicine. Malaria is spread by mosquitoes, so use insect repellent and take other steps to avoid bug bites.
Make an appointment with your healthcare provider or a travel health specialist that takes place at least one month before you leave. They can help you get destination-specific vaccines, medicines, and information. Discussing your health concerns, itinerary, and planned activities with your provider allows them to give more specific advice and recommendations.
Plan for the unexpected. It is important to plan for unexpected events as much as possible. Doing so can help you get quality health care or avoid being stranded at a destination. A few steps you can take to plan for unexpected events are to get travel insurance , learn where to get health care during travel , pack a travel health kit , and enroll in the Department of State’s STEP .
Be sure your healthcare policy covers pregnancy and neonatal complications while overseas. If it doesn’t get travel health insurance that covers those items. Consider getting medical evacuation insurance too.
Recognize signs and symptoms that require immediate medical attention, including pelvic or abdominal pain, bleeding, contractions, symptoms of preeclampsia (unusual swelling, severe headaches, nausea and vomiting, and vision changes), and dehydration.
Prepare a travel health kit . Pregnant travelers may want to include in your kit prescription medications, hemorrhoid cream, antiemetic drugs, antacids, prenatal vitamins, medication for vaginitis or yeast infection, and support hose, in addition to the items recommended for all travelers.
During Travel
Your feet may become swollen on a long flight, so wear comfortable shoes and loose clothing and try to walk around every hour or so. Sitting for a long time, like on long flight, increases your chances of getting blood clots, or deep vein thrombosis. Pregnant women are also more likely to get blood clots. To reduce your risk of a blood clot, your doctor may recommend compression stockings or leg exercises you can do in your seat. Also, see CDC’s Blood Clots During Travel page for more tips on how to avoid blood clots during travel.
Choose safe food and drink. Contaminated food or drinks can cause travelers’ diarrhea and other diseases and disrupt your travel. Travelers to low or middle income destinations are especially at risk. Generally, foods served hot are usually safe to eat as well as dry and packaged foods. Bottled, canned, and hot drinks are usually safe to drink. Learn more about how to choose safer food and drinks to prevent getting sick.
Pregnant women should not use bismuth subsalicylate, which is in Pepto-Bismol and Kaopectate. Travelers to low or middle income destinations are more likely to get sick from food or drinks. Iodine tablets for water purification should not be used since they can harm thyroid development of the fetus.
After Travel

If you traveled and feel sick, particularly if you have a fever, talk to a healthcare provider immediately, and tell them about your travel. Avoid contact with other people while you are sick.
More Information
CDC Yellow Book: Pregnant Travelers
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.

- Pregnancy Classes

Travel During Pregnancy
As long as there are no identified complications or concerns with your pregnancy, it is generally safe to travel during your pregnancy. The ideal time to travel during pregnancy is the second trimester . In most cases, you are past the morning sickness of the first trimester and several weeks from the third stage of pregnancy when you are more easily fatigued .
Is it safe to travel during pregnancy?
Traveling by air is considered safe for women while they are pregnant; however, the following ideas might make your trip safer and more comfortable.
- Most airlines allow pregnant women to travel through their eighth month. Traveling during the ninth month is usually allowed if there is permission from your health care provider.
- Most airlines have narrow aisles and smaller bathrooms, which makes it more challenging to walk and more uncomfortable when using the restroom. Because of potential turbulence that could shake the plane, make sure you are holding on to the seatbacks while navigating the aisle.
- You may want to choose an aisle seat which will allow you to get up more easily to reach the restroom or just to stretch your legs and back.
- Travel on major airlines with pressurized cabins and avoid smaller private planes. If you must ride in smaller planes, avoid altitudes above 7,000 feet.
- Although doubtful, the risk of DVT can be further reduced by wearing compression stockings.
The Royal College of Obstetricians and Gynaecologists and the International Air Travel Association recommend that expecting mothers in an uncomplicated pregnancy avoid travel from the 37th week of pregnancy through birth. Avoiding travel from 32 weeks through birth is recommended for women who have complicated pregnancies with risk factors for premature labor, such as mothers carrying multiples.
Risk factors that warrant travel considerations include the following:
- Severe anemia
- Cardiac disease
- Respiratory disease
- Recent hemorrhage
- Current or recent bone fractures
Traveling by Sea During Pregnancy
Traveling by sea is generally safe for women while they are pregnant; the motion of the boat may accentuate any morning sickness or make you feel nauseous all over again. There are a few considerations to make your trip safer and more comfortable:
- Check with the cruise line to ensure that there is a health care provider on board in case there are any pregnancy complications .
- Review the route and port-of-calls to identify if there is access to any medical facilities if needed.
- Make sure any medications for seasickness are approved for women who are pregnant and that there is no risk to the developing baby.
- Seasickness bands use acupressure points to help prevent upset stomach and maybe a good alternative to medication.
International Travel During Pregnancy
Traveling overseas has the same considerations that local or domestic travel has, but it also has additional concerns that you need to know about before making an international trip. The information below is provided to help you assess whether an international trip is good for you at this time:
- It is important to talk with your health care provider before you take a trip internationally to discuss safety factors for you and your baby.
- Discuss immunizations with your health care provider and carry a copy of your health records with you.
- With international travel, you may be exposed to a disease that is rare here in the United States but is common in the country you visit.
- Contact the Centers for Disease Control and Prevention at (800) 311-3435 or visit their website at www.cdc.gov to receive safety information along with immunization facts related to your travels.
- Diarrhea is a common concern when traveling overseas because you may not be used to the germs and organisms found in the food and water of other countries. This can lead to a problem of dehydration .
Here are some tips to avoid diarrhea and help keep you safe:
- Drink plenty of bottled water
- Used canned juices or soft drinks as alternatives
- Make sure the milk is pasteurized
- Avoid fresh fruits and vegetables unless they have been cooked or can be peeled (such as an orange or a banana)
- Make certain that all meat and fish has been cooked completely; if you are unsure, do not eat it
Travel Tips During Pregnancy
Whether you are going by car, bus, or train, it is generally safe to travel while you are pregnant; however, there are some things to consider that could make your trip safer and more comfortable.
- It is essential to buckle-up every time you ride in a car. Make sure that you use both the lap and shoulder belts for the best protection of you and your baby.
- Keep the airbags turned on. The safety benefits of the airbag outweigh any potential risk to you and your baby.
- Buses tend to have narrow aisles and small restrooms. This mode of transportation can be more challenging. The safest thing is to remain seated while the bus is moving. If you must use the restroom, make sure to hold on to the rail or seats to keep your balance.
- Trains usually have more room to navigate and walk. The restrooms are usually small. It is essential to hold on to rails or seat backs while the train is moving.
- Try to limit the amount of time you are cooped up in the car, bus, or train. Keep travel time around five to six hours.
- Use rest stops to take short walks and to do stretches to keep the blood circulating.
- Dress comfortably in loose cotton clothing and wear comfortable shoes.
- Take your favorite pillow.
- Plan for plenty of rest stops, restroom breaks and stretches.
- Carry snack foods with you.
- If you are traveling any distance, make sure to carry a copy of your prenatal records.
- Enjoy the trip.
Want to Know More?
- How to Treat Jet Lag Naturally During Pregnancy
Compiled using information from the following sources:
1. Planning Your Pregnancy and Birth Third Ed. The American College of Obstetricians and Gynecologists, Ch. 5. William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 8.
2. Royal College of Obstetricians and Gynaecologists, Air Travel and Pregnancy (Scientific Impact Paper No. 1), https://www.rcog.org/uk, May 22, 2013.
BLOG CATEGORIES
- Can I get pregnant if… ? 3
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Breastfeeding 29
- Changes In Your Body 5
- Cord Blood 4
- Genetic Disorders & Birth Defects 17
- Health & Nutrition 2
- Is it Safe While Pregnant 54
- Labor and Birth 65
- Multiple Births 10
- Planning and Preparing 24
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Pregnancy Health and Wellness 149
- Pregnancy Products & Tests 8
- Pregnancy Supplements & Medications 14
- The First Year 41
- Week by Week Newsletter 40
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Paternity Tests 2
- Pregnancy Symptoms 5
- Prenatal Testing 16
- The Bumpy Truth Blog 7
- Uncategorized 4
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Women's Health 34
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
Share this post:
Similar post.

Preconception Wellness - Prepare for the Unexpected

Leg Cramps During Pregnancy

Prenatal Vitamin Limits
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
Placenta previa, for example, happens when the placenta completely or partially covers the cervix. It can cause bleeding during pregnancy, as well as serious complications—like hemorrhage or preterm birth—that would be difficult to navigate in an unfamiliar location.
Additionally, traveling is a risk factor for blood clots, according to the CDC—and pregnant people already have a heightened chance of developing them. Certain conditions and disorders may increase the risk of blood clots too much for long road trips.
2. Plan for Your Second Trimester
The American College of Obstetricians and Gynecologists (ACOG) says the ideal time to travel is during the second trimester, between 14 and 28 weeks. "During these weeks, your energy has returned, morning sickness is improved or gone, and you are still able to get around easily," recommends the organization. "After 28 weeks, it may be harder to move around or sit for a long time."
Not only is the middle of the pregnancy when pregnant people will likely feel the best, but it also carries a lower risk of any complications.
3. Prepare for the Pregnancy Road Trip
Advanced planning can make any road trip easier. This includes thoughtful packing like easy-to-change clothing if you get too hot or too cold and taking healthy foods, snacks, and drinks. Also, make sure your route is accurate to avoid delays and check for safe places to stop.
4. Drink Enough Water
There's a link between dehydration and uterine contractions, so keeping on top of water intake is crucial, says Dr. Gaither. Have a sufficient supply of water readily available in the car and make sure to drink even more if you've been sweating or exercising. Pregnant people should drink eight to 12 cups (or 64 to 96 ounces) of water each day, according to ACOG. This ensures healthy digestion, amniotic fluid formation, and nutrient circulation.
5. Bring Extra Medications or Supplements
Taking the proper medications and supplements while pregnant is imperative, and it's even more important on a road trip. Dr. Gaither says pregnant travelers will want to double-check that they've packed any medications and vitamins they need.
It's also important to bring extra, in case they're on the road longer than originally anticipated. Include over-the-counter medicines approved by your health care provider, so you'll have them if you need them. And, don't forget to pack your prenatal vitamin !
6. Always Wear a Seat Belt
Wearing a seat belt in a car is one of the most important car safety tips, especially when you're pregnant. The myth that a seat belt could harm the fetus is pure fiction, but there's a proper way to wear one if you're pregnant, according to the National Highway Traffic Safety Administration (NHTSA).
Pregnant people should wear the shoulder belt away from their neck and across their chest. The lap belt should be secured below the belly so it fits snugly. Pregnant people should also keep as much distance as possible between their belly and the steering wheel, while still ensuring they can reach the wheel and pedals. Additionally, the NHTSA recommends pregnant people don't disable the airbags.
7. Get Out and Stretch Often
Dr. Gaither says pregnant travelers should stop "at least every two hours" and get out of the car, stretch, and walk around. This increases blood flow to the lower body which helps prevent complications like deep vein thrombosis (DVT) in the legs. These blood clots usually dissolve on their own. However, in rare cases, they can break off, travel to the lungs, and block blood flow. This potentially life-threatening condition is called a pulmonary embolism.
While the risk for DVT is low, it does increase with pregnancy. The CDC recommends knowing the signs of DVT, which include swelling and/or redness in the leg (or arm), unexplained pain or tenderness, and skin that feels warm when touched. Signs of a pulmonary embolism include difficulty breathing, fast or irregular heartbeat, and chest pain or discomfort.
8. Dress Comfortably
Being comfortable during pregnancy is key, and that's especially true during a road trip. Luckily, a few essentials can make the ride more relaxing—and safer. Non-medical compression socks or support hosiery may be a good idea to help support blood flow.
Other helpful travel accessories include a lumbar pillow, comfortable shoes, and a good water bottle (because hydration is key to a healthy pregnancy ). A cooler, sunglasses, and sunscreen also may be helpful. And, avoid wearing too-tight clothing and shoes.
9. Avoid Remote Locations
Nothing is stopping most pregnant people from traveling, but it's always smart to be mindful of where you're going. If possible, maintain a steady speed (instead of speeding up and slowing down) and avoid winding, hilly, bumpy roads, and frequent lane changes. Also, don't travel to extremely remote areas where medical care may be difficult to find in case of an emergency.
10. Have an Emergency Plan in Place
Pregnant travelers will want to have a plan in case any unexpected health concerns pop up, as they can happen quickly during pregnancy. If you don't have access to an electronic health record, take a copy of your medical record with you. If any problems do arise during a road trip, Dr. Gaither recommends pregnant people contact their health care provider and the nearest hospital for advice, evaluation, and possible treatment.
11. Relax and Have Fun
There are lots of things to take into consideration when planning a road trip while pregnant, but always remember to have fun! Advanced planning and a comfortable wardrobe will help make the trip easier. Plan a trip you're excited about and indulge in a little pre-baby R&R.
Pregnant Travelers . Centers for Disease Control and Prevention . 2022.
Blood Clots and Travel: What You Need to Know . Centers for Disease Control and Prevention . 2023.
Travel During Pregnancy . American College of Obstetricians and Gynecologists . 2023.
How Much Water Should I Drink During Pregnancy? . American College of Obstetricians and Gynecologists . 2020.
If You're Pregnant: Seat Belt Recommendations for Drivers and Passengers . National Highway Traffic Safety Administration .
Related Articles
What to expect when traveling in each trimester of pregnancy

So you're pregnant? Congrats! It's an exciting time but also one in which many aspects of your life will begin to change, including travel. While you'll quickly need to understand the airline industry's rules for flying while pregnant , there are some more personal tips I'd like to share with you based on my experience traveling throughout the first, second and third trimesters of both of my pregnancies.
A few truths about pregnancy
Picky, starving moms need to travel with snacks.
I didn't know I was pregnant when I took the first flight of my second pregnancy. I was on a mileage run from Houston to Los Angeles, and by the time we landed, I was super tired, kinda grumpy and oh-my-so-hungry.
Then began a mad search for food. Luckily, Counter Burger was open and serving up sweet potato fries and burgers. Out of habit, I went for the veggie burger but I quickly regretted my decision, which left me far from satisfied with ground-up veggie mush.
In the early stages of pregnancy, your normal travel habits of going a little hungry for a while, or making due with what's around, may not work well.
Throughout your pregnancy, travel with water to stay hydrated and snacks to stave off hunger pangs and keep you going through travel delays. If you're feeling particularly food sensitive, research the food options at your destination ahead of time. I virtually lived on chicken noodle soup for a whole week early in my pregnancy and then, for a couple of days, all I wanted were hush puppies. I know how to get those items at home but when you are on the road, you either need to do more research or be more flexible -- which is sometimes easier said than done.
Related: 4 tips for planning travel while planning a pregnancy
Research and make choices about inflight radiation and other risks
I'm not an expert, but because I fly often, I have given some thought to inflight radiation exposure , especially during the early stages of pregnancy.
For pregnant flight attendants and pilots, the Federal Aviation Administration recommends a limit of 1 mSv during pregnancy, with no more than 0.5 mSv per month. I don't fly as much as an airline employee, but it doesn't take much research to learn that the amount of radiation you (and your gestating baby) are exposed to in the air varies dramatically from route to route. The highest-level routes are typically longer, higher-altitude polar routes. Here's some information from NASA about polar flights and radiation .
Every expectant mother should discuss the risks of flying during pregnancy with her doctor before getting on a plane. For me, nine months was a tiny moment in my traveling life, so I was OK adjusting my behavior a bit out of an abundance of caution. However, I didn't adjust to the point of never leaving my house. We still flew when I was pregnant, but I was judicious about when and where I would fly.
Check your health insurance policy
If you aren't familiar with your medical insurance coverage for when you travel, brush up on those facts now. Look at in-network and out-of-network benefits, as well as coverage for procedures for medical emergencies in other countries, if relevant. Most likely, if you do have coverage for treatment in other countries, you will still be on the hook to pay for your care up front and then submit for reimbursement from your health insurer. Plan accordingly and plan for the unexpected. If your baby decides to arrive early, for instance, check to make sure your insurance would cover possible extended and expensive care in an intensive care unit in a hospital away from your home.
Be sure to check what your health insurance coverage provides if you deliver at another facility later in your pregnancy. I once had an insurance plan that specifically did not cover out-of-network deliveries after 36 weeks, so that is something you would want to know before venturing away from home late in pregnancy.
Consider travel insurance
Trip insurance can be helpful if you are traveling while pregnant. Read the plan's fine print to determine what might be covered and whether you are covered if you already knew you were pregnant when you purchased the plan. Typically, a normal pregnancy or normal delivery would not be covered but if there are unexpected complications with the pregnancy, then related trip-cancellation or trip-interruption coverage may kick in on certain plans in certain situations.
Here are some travel insurance providers to check out: Allianz Travel Insurance, Travel Guard and Travelex Insurance . You can also compare a variety of plans at a portal like SquareMouth .
Here are some articles that will help you brush up on your travel insurance knowledge:
- The best travel insurance policies and providers
- What is independent travel insurance and when is it worth it?
- When to buy travel insurance versus when to rely on credit card protections
- Is credit card travel insurance sufficient on its own?
- Why I buy travel insurance
Traveling in the first trimester
Traveling in the first trimester can range from "no big deal" to "I think I'm going to die from misery right this very instant." Symptoms in early pregnancy can vary widely and can change by the day. A flight in your first trimester may be no different from any other flight you've ever taken or it may feel like you are flying with the worst hangover of your life.
Unless you are very high risk or have other extenuating medical issues, your doctor will probably give you the green light to travel in early pregnancy. Feeling extra tired, nauseous and queasy doesn't make for the perfect travel experience, so here are some tips to make travel easier:
Pick an aisle seat and move about the cabin
When you do hit the skies early on, choose a seat where you will be the most comfortable, likely an aisle seat so you can get to the restroom easily. I also recommend getting up to walk around and stretch your legs. (Here are tips for credit cards that will defeat basic economy and let you get a seat assignment in advance.)
Room service come to the rescue
In my first trimester of my second pregnancy, I went on a trip with my daughter and parents to New York City to see the Macy's Thanksgiving Day Parade and I was met with another challenge. I was at the point in my pregnancy when I needed food immediately upon waking or I was going to get queasy. Since I was staying in a hotel room with my young daughter, this meant room service. I also had granola bars and fruit on hand, but that was not enough to really do the trick some mornings. Had my husband been there, he could have gone in search of a warm bagel and juice, but since he wasn't on this trip, we had to improvise. Thanks goodness Marriott elite status helped defray the cost of most of the breakfast!

Take it easy when you need to
Once you are further along in your pregnancy and you actually look pregnant, you will sometimes get a little sympathy or, at least, empathy while traveling. Strangers may offer to help with your bag and people may have more patience with you if you're moving slowly. However, in the first trimester nobody can tell you are pregnant, and no one is going to feel sorry for you. If you act queasy on the plane, you will pretty much be treated like you have Ebola, and any other issue or ailment will pretty much not interest anyone. I once told the flight attendant I was pregnant when she was giving me the eye about looking queasy.
Take care of yourself, don't overdo it and know when to say enough is enough. You may be used to very busy travel days, but now find yourself needing a nap during your first trimester, and that's OK. Listen to your body and adjust accordingly.
Traveling in the second trimester
You have probably heard that the second trimester is generally the easiest of the three trimesters for most expecting moms. You usually aren't as sick and or as tired as in the first trimester, and you aren't as large, uncomfortable and exhausted as in the third trimester. From roughly weeks 13 to 27 of a pregnancy, your activity and comfort levels are often good, and this means that it can be a great time to travel. Couples that like to take "babymoons" (one last couples trip before the baby arrives) often try to schedule them in the second trimester.
Related: The best babymoon destinations for every month of the year
The beginning and end of the second trimester are quite different
You will probably enter the second trimester not really looking pregnant, and end it looking quite different. This means that you may feel very different at the beginning and end of the second trimester. The second trimester is when lots of belly growing happens and this can mean that some types of travel will be more uncomfortable toward the end of these few months of pregnancy than at the beginning.

Consider where you are comfortable traveling
A very personal and important decision to make during the second trimester is to determine if there are certain restrictions you will place on yourself in terms of where you're comfortable traveling. Some types of travel will ban women from traveling during the second trimester. For example, many cruise lines will not allow a woman to book a cruise if she will enter her 24th week of pregnancy (or later) while on the voyage.
Royal Caribbean's policy bars pregnant women from sailing at and after the 24th week. It was developed in concert with the Cruise Lines International Association endorsement of the American College of Emergency Physicians Health Care Guidelines for Cruise Ship Medical Facilities .
Many consider unborn fetuses to be viable if born beginning around 24 weeks (though that age threshold is getting earlier and earlier). This means that a baby born at 24 weeks gestation would have anywhere from a 50% to 70% chance of survival outside the womb if (and only if) there is immediate access to advanced medical care. A cruise ship clearly doesn't have an advanced neonatal care unit on board, so presumably the policy is related to why cruise lines draw the line for pregnant passengers.
I personally draw the line for travel at 23 or 24 weeks when talking about destinations that don't have the same level of advanced medical care as the United States -- or long flights or a flight path that could hinder prompt access to advanced medical care if I happened to unexpectedly go into labor. The Maldives is an example of somewhere I would not want to travel in this instance because there would be significant delays in obtaining medical care on these remote islands.
Plan big, but not too big
The second trimester is a great time to squeeze in a pre-baby trip or two since you will probably feel relatively like to your pre-pregnant self much of the time. We went to Aruba when I was 14 weeks pregnant and it was a fantastic trip. I had lots of energy and a normal appetite. Flying was not uncomfortable because my belly was still pretty small and the only real adjustment was to make sure I had a somewhat larger bathing suit before the trip.
At 23 weeks, I traveled to Spain and still felt pretty energetic and "normal." I will admit that the flight in economy wasn't super comfortable since I did have a belly that was hindering curling up in positions that usually help me sleep on the plane, but our time on the ground in Spain wasn't really impacted at all by the pregnancy other than missing out on the Spanish wine.
The great thing about both of those trips was that they were at my own pace. This meant that if I didn't feel like doing much one afternoon, I could take it easy. Even though you may feel great in the second trimester, you can still tire more quickly than normal, so be sure to limit your vacation activities to those you can manage. There are also activities that some doctors might advise against by the second trimester like thrill rides, scuba diving or horseback riding, so double-check any restrictions before planning more adventurous outings.

Traveling in the third trimester
Pregnancy isn't an illness or disease. For many families, it's just a normal phase in a woman's life before a new baby joins the family. Assuming things are going well, it's not a time when you have to cancel all travel. However, once the third trimester rolls around, travel can get a more complicated and does eventually have to stop.
The beginning and end of the third trimester are quite different
Changes come even more quickly in the third trimester. You enter the third trimester about 28 weeks pregnant and end it with a newborn. This means that types of travel that are possible at 27 and 28 weeks pregnant may be inadvisable, or even prohibited, at 37 and 38 weeks pregnant.
Select destinations and activities carefully
In the final months of pregnancy, some activities are probably going to be more comfortable and enjoyable than others. For example, swimming and spa time may be exactly what you need.
I give strong preference to visiting beach and resort destinations in the final trimester. Trust me when I say that few activities are as comfortable in the third trimester as floating in the water! We went to The Phoenician (a Marriott property) in Scottsdale, Arizona, when I was about 31 weeks pregnant and even with my big belly, it was the perfect mix of spa, swimming and fun activities for our 5 year old before both our lives changed.

You are going to get uncomfortable
Maybe this isn't universal and there are some magical creatures out there who never feel uncomfortable during pregnancy, but every mom I know eventually hit a point in her pregnancy when she wasn't comfortable. For many, this means that sitting for an extended time in a small airline seat, standing in long lines or trekking around in the heat to explore a city all day eventually become pretty miserable activities.
No one can tell you when you will hit that point, but it will likely happen in the third trimester. For me, my back started giving me a bunch of trouble at around week 30 or 31. I was incredibly grateful there were no more flights scheduled during that pregnancy beyond that point.
If you are going to fly during the later weeks of your third trimester and have the ability to secure a more comfortable seat up front, or at least one with extra legroom so you can stretch out, it may well be a good investment in your comfort. I brought a tennis ball with me when I flew so I could give myself a bit of a "back massage" against the airplane seat.

Bring your own pillows
Sleep becomes a challenge in the third trimester for many women and a pillow fort of sorts becomes a necessity to get some good shut-eye. Many pregnant moms find that using some sort of body pillow or pillow arrangement helps to keep their bellies supported and comfortable at night. You can't assume that the hotel will have similar pillows, so bring your own if they become essential to good rest in your third trimester. I had no shame in hauling my pillow fort with me on our last road trip at eight months pregnant.
See if you are allowed to fly
Even if your doctor OKs it, many airlines have rules about women flying in the third trimester. Check out airline rules for traveling while pregnant for complete details, but generally speaking, most U.S. airlines don't have many flight restrictions until the last month of pregnancy. However, many international airlines do have restrictions and documentation requirements beginning at 28 weeks. If you are pregnant with more than one baby, the restrictions kick in even earlier.
Decide when to stop traveling
I'm all for traveling while pregnant but, realistically, most women will want to stop traveling at some point in the third trimester. I would imagine by about 36 or 37 weeks, most women will probably decide to stay closer to home. I went on a road trip about three hours from home at 35 weeks and then called it quits for the rest of the pregnancy. There's still a whole new world of travel waiting once a new baby joins the family .

Bottom line
There is usually no reason to stop traveling when you're expecting. During my last pregnancy, I went on 12 trips, 28 flights, visited four countries and I'm very glad I had the opportunity to stay that active. I'm also glad that I grounded myself from flight after 31 weeks and from road trips at 35 weeks because those were the right decisions for my comfort level.
- Skip to main content
- Skip to site information
Language selection
Help us to improve our website. Take our survey !
Travelling while pregnant
Find useful information and considerations to help you prepare for safe and healthy travels outside Canada while pregnant.
With careful preparation, travelling while pregnant can be safe. The decision to travel should be made in consultation with your health care professional, based on your personal health circumstances.
On this page
Before you go, while you're away, if you need help.
Medical practices, health standards and infection control measures vary from country to country. You may not have access to the same level of care, procedures, treatments and medications as you would in Canada.
You could also be at increased risk of getting an infection and/or developing severe complications from certain infections, which could also affect the fetus.
Before leaving Canada:
- consult a health care professional or visit a travel health clinic at least 6 weeks before travelling to get personalized health advice and recommendations
- check our Travel Advice and Advisories for country-specific information, including about possible health risks
- know how to seek medical assistance outside of Canada
- review the policy and the coverage it provides
- most policies do not automatically cover pregnancy-related conditions or hospital care for premature infants
- ask your insurance provider about coverage for medical care during pregnancy, giving birth and intensive care for you and your fetus or newborn
- carry a copy of your prenatal records
- talk to your health care professional about any additional items you may want to bring that are specific to your health needs
Local laws and medical services relating to pregnancy can differ from Canada. Learn the local laws, and how these may apply to you before you travel.
Pre-travel vaccines and medications
Many vaccines can be safely given during pregnancy. Due to a higher risk of more severe outcomes for you and your fetus, some vaccines are recommended specifically during pregnancy, such as tetanus-diphtheria-pertussis (DTaP) and influenza.
Don’t take medications you may still have from prior trips. Tell the health care professional about your pregnancy, or intended pregnancy, before filling any prescriptions. The decision to get any pre-travel vaccinations or medications should be discussed with your health care professional.
The decision can depend on:
- your purpose of travel (e.g., tourism, visiting friends and relatives)
- your planned destination(s)
- the length of your trip
- your risk of getting a disease
- how severe the effect of a disease would be to you and/or your fetus
- your planned activities
- any underlying medical issues and/or pregnancy-related complications
Malaria could cause major health problems for a mother and her unborn baby. A pregnant woman may want to consider avoiding travel to areas where malaria transmission occurs.
Description of malaria risk by country and preventative measures.
If you can’t avoid travelling to an area where malaria is present:
- some medications to prevent or treat malaria may not be safe during pregnancy
- take extra care to protect yourself from mosquito bites
Zika virus infection during pregnancy can pose significant risks to your fetus even if you don’t develop symptoms. While pregnant, you may want to consider avoiding travelling to a country or areas with risk of Zika virus.
Latest travel health advice on Zika virus.
If you choose to travel, take precautions to avoid infection with Zika virus:
- prevent mosquito bites at all times
- protect yourself from contact with semen, vaginal fluid and blood
- always use condoms correctly or avoid sexual contact while in countries or areas with risk of Zika virus
Learn more about Zika virus and pregnancy:
- Zika virus: Pregnant or planning a pregnancy
- Zika virus: Advice for travellers
- Pregnancy and travel (tropical medicine and travel)
Monitor your health and be prepared
Emergencies can happen at any time. Know where the nearest hospital or medical centre is while you are travelling and confirm they will accept your medical insurance.
Seek medical attention immediately if you develop any of the following symptoms while travelling:
- persistent vomiting and/or diarrhea
- dehydration
- vaginal bleeding
- passing tissue or clots
- abdominal pain, cramps or contractions
- your water breaks
- excessive swelling of face, hands or legs
- excessive leg pain
- severe headaches
- visual problems
If you develop these symptoms after your return to Canada, you should see a health care professional immediately and tell them about your recent trip.
Transportation
Always wear a seatbelt when travelling by plane or car. When using a diagonal shoulder strap with a lap belt, the straps should be placed carefully above and below your abdomen. If only a lap belt is available, fasten it at the pelvic area, below your abdomen.
If you have any medical or pregnancy-related complications, discuss with your health care professional whether air travel is safe for you.
Most airlines restrict travel in late pregnancy or may require a written confirmation from a physician. Check this with the airline before booking your flight.
During long flights, you may be at higher risk of developing blood clots, known as deep vein thrombosis (DVT). The risk of deep vein thrombosis can be reduced by:
- getting up and walking around occasionally
- exercising and stretching your legs while seated
- selecting an aisle seat when possible
- wearing comfortable shoes and loose clothing
Your health care professional may recommend additional ways to reduce your risk such as wearing compression stockings.
Always stay well hydrated while travelling.
Land travel
The risk of deep vein thrombosis can be reduced by:
- stopping the vehicle to walk around every couple of hours

Motion sickness
Certain medications used to treat nausea and vomiting during pregnancy may also be effective in relieving motion sickness.
If you think you might experience motion sickness during your trip, speak to your health care professional about the use of these medications.
Environmental and recreational risks
Some activities may not be recommended or may require additional precautions. Discuss your travel plans, including any planned or potential recreational activities with a health care professional.
High altitude
You should avoid travelling to an altitude above 3,658 metres (12,000 feet).
However, if you have a high-risk pregnancy and/or are in the late stages of pregnancy, the highest altitude should be 2,500 metres (8,200 feet).
If you have pregnancy-related complications, you should avoid unnecessary high-altitude exposure.
Keep in mind that most high-altitude destinations are far from medical care services.
Personal protective measures
Food-borne and water-borne diseases.
Eat and drink safely while travelling while travelling. Many food-borne and water-borne illnesses can be more severe during pregnancy and pose a risk to the fetus.
This can include:
- toxoplasmosis
- listeriosis
- hepatitis A and E
To help avoid food-borne and water-borne diseases:
- before eating or preparing food
- after using the bathroom or changing diapers
- after contact with animals or sick people
- before and after touching raw meat, poultry, fish and seafood
- if you’re at a destination that lacks proper sanitation and/or access to clean drinking water, only drink water if it has been boiled or disinfected or if it’s in a commercially sealed bottle
- use ice made only from purified or disinfected water
- this could cause the fetus or newborn to develop thyroid problems
- unpasteurized dairy products, such as raw milk and raw milk soft cheeses
- unpasteurized juice and cider
- raw or undercooked eggs, meat or fish, including shellfish
- raw sprouts
- non-dried deli meats, including bologna, roast beef and turkey breast
- don’t use bismuth subsalicylate (Pepto-Bismol®)
- Information on travellers’ diarrhea
Illnesses acquired from insect and other animals
Protect yourself from insect bites:
- wear light-coloured, loose clothes made of tightly woven materials such as nylon or polyester
- prevent mosquitoes from entering your living area with screening and/or closed, well-sealed doors and windows
- use insecticide-treated bed nets if mosquitoes can’t be prevented from entering your living area
- information on insect bite and pest prevention
Some infections, such as rabies and influenza, can be shared between humans and animals. You should avoid contact with animals including dogs, livestock (pigs, cows), monkeys, snakes, rodents, birds, and bats.
Information for if you become sick or injured while travelling outside Canada.
For help with emergencies outside Canada, contact the:
- nearest Canadian office abroad
- Emergency Watch and Response Centre in Ottawa
More information on services available at consular offices outside Canada.
Related links
- Immunization in pregnancy and breastfeeding: Canadian Immunization Guide
- Advice for Canadians travelling to Zika-affected countries
- Advice for women travellers
- If you get sick before or after returning to Canada
- Receiving medical care in other countries
- Travel vaccinations
- What you can bring on a plane
3 Weeks Pregnant
Medical review policy, latest update:, your baby at week 3, at a glance, 3 weeks pregnant is how many months, how big is my baby at 3 weeks, implantation, boy or girl, your body at week 3.

The corpus luteum and pregnancy hormones
Pregnancy and sense of smell, pregnancy symptoms week 3, tips for you this week.
What to Expect When You’re Expecting , 5th edition, Heidi Murkoff. WhatToExpect.com, Pregnancy Tests , August 2022. WhatToExpect.com, How Much Water Should You Drink During Pregnancy? , November 2022. WhatToExpect.com, How Much Vitamin C Do You Need During Pregnancy? , June 2022. National Institutes of Health, National Library of Medicine, Fetal Development , July 2021. American College of Obstetricians and Gynecologists, Prenatal Genetic Diagnostic Tests , December 2022. KidsHealth From Nemours, All About Genetics , October 2021. National Institutes of Health, National Human Genome Research Institute, X Chromosome Infographic , July 2021. National Institutes of Health, National Library of Medicine, Pregnancy Test , November 2022. Food and Drug Administration, Pregnancy , April 2019. National Institutes of Health, National Library of Medicine, Pregnancy and Olfaction: A Review , February 2014. Mayo Clinic, Symptoms of Pregnancy: What Happens First , December 2021. Society for Endocrinology, Ovaries , March 2021. National Institutes of Health, National Library of Medicine, Vitamin C , January 2023. National Institutes of Health, National Library of Medicine, Iron in Diet , January 2023. American College of Obstetricians and Gynecologists, Nutrition During Pregnancy , June 2023. National Institutes of Health, National Library of Medicine, Pregnancy and Nutrition , January 2021. American College of Obstetricians and Gynecologists, Morning Sickness: Nausea and Vomiting of Pregnancy , December 2021. WhatToExpect.com, Pregnancy Due Date Calculator and Conception Calculator , September 2023. WhatToExpect.com, Has Your Sense of Smell Gotten Stronger During Pregnancy? , January 2023. WhatToExpect.com, How Many Weeks, Months and Trimesters in a Pregnancy? , May 2022. WhatToExpect.com, Your Guide to Pregnancy Hormones , November 2022. WhatToExpect.com, When Does Implantation Occur? Symptoms, What to Expect , May 2023. WhatToExpect.com, Metallic Taste During Pregnancy (Dysgeusia) , September 2022. WhatToExpect.com, Can You Drink Alcohol While Pregnant? , May 2021. WhatToExpect.com, What Is the Two-Week Wait? , August 2023. WhatToExpect.com, What Are Your Chances of Having Twins? , April 2023. WhatToExpect.com, HCG Levels During Pregnancy: What Is Normal? , May 2021. WhatToExpect.com, What Is Fertilization? , July 2023. WhatToExpect.com, Pregnancy Symptoms: 14 Early Signs of Pregnancy , May 2023. WhatToExpect.com, Cramping During Pregnancy: Normal or Something More? , October 2022.
Recommended Products

⚠️ You can't see this cool product because you have ad block enabled.

What Other January 2025 Moms Are Talking About
Recommended reading, signs it's a boy or a girl: predicting the sex of your baby, pregnancy symptoms: 14 early signs of pregnancy, ⚠️ you can't see this cool content because you have ad block enabled., pregnancy "sins" it's okay to commit video, early way day deals: up to 70% off nursery furniture and more at wayfair, how to plan the perfect pregnancy announcement photo session, inclined sleepers are dangerous for babies — here's why, explore more in your pregnancy week-by-week.
Ready Steady Baby
Travelling when pregnant.
Whether you’re doing short journeys in the car or getting on a plane for a holiday abroad, it’s important to take extra care of yourself when you’re pregnant. Making a few small changes and planning ahead will help to make sure you have a comfortable and safe journey.
Wherever you’re going, it’s a good idea to take your maternity notes with you in case you need medical help.

It’s fine to drive or be a passenger in a car while you’re pregnant.
It’s important to wear a seat belt as you normally would. Make sure the straps don’t go over your bump by:
- placing the lap strap across your hips so it fits comfortably under your bump
- placing the diagonal strap between your breasts and around your bump
Take regular breaks when driving and make sure you bring some water and snacks with you for the journey.
Going on holiday or abroad
If you’re planning a holiday, seek health advice as early as possible.
You should give some thought to where you want to go as:
- the things you may normally love, like hot sunny weather, may not be a great idea if you’re uncomfortable or finding it hard to sleep
- you shouldn’t travel to areas where there’s malaria or the Zika virus if you can avoid it
You should also consider the quality of medical care in the country you plan to visit.
Fitfortravel has more advice for pregnant travellers
Staying safe on holiday
Activities like walking and swimming are fine while you’re pregnant, but it’s not a good idea to do any activity where you might fall.
Take care to avoid coming into contact with water or food that could cause tummy upsets. Some medicines for treating diarrhoea may not be suitable in pregnancy.
Talk to your midwife if you have questions.
Travel vaccinations
You’ll need vaccinations before you travel to certain countries.
There are some vaccinations you shouldn’t have when you’re pregnant, especially in the first 3 months, so always check before you book anything.
Find out which travel vaccinations you might need
Travel insurance
Before you travel, you’ll need special travel insurance that:
- covers any medical costs
- allows you to cancel for any issues with your pregnancy
If you don’t tell your insurer you’re pregnant before you travel, your insurance may not be valid.
If you’re travelling in Europe, the European Health Insurance Card (EHIC) may allow you to use the health services in these countries.
Apply for a European Health Insurance Card
Flying while pregnant
Air travel is generally safe if you’re having an uncomplicated pregnancy.
If you have any pregnancy complications, check with your midwife or GP that there’s no medical reason to stop you flying, such as high blood pressure or a risk of deep vein thrombosis .
Most airlines won’t let you fly if you’re within about a month of your due date. Some will need a letter from your GP or midwife saying you’re fit to fly when you’re 7 months pregnant. Check with the airline before you book.
Having a comfortable flight
When travelling by plane:
- drink plenty of water as you’re much more likely to get dehydration while flying.
- take healthy snacks with you so you can follow your own eating plan
- take whatever makes you more comfortable, such as an extra pillow or warm socks
Be aware it may take you a bit longer than before to recover from jet lag.
Deep vein thrombosis
Deep vein thrombosis (DVT) is a blood clot in a deep vein in your leg, calf or pelvis.
You’re more likely to get DVT if:
- you sit for long periods of time
- do very little activity
If you’re travelling on a long-distance flight or sitting for 4 hours or more, talk to your midwife as you may need medication. F ollow your midwife or doctor’s advice.
More about deep vein thrombosis
Further information, other languages and alternative formats
Translations and alternative formats of this information are available from Public Health Scotland .
If you need a different language or format, please contact [email protected].
- Ready Steady Baby leaflet in Arabic, Polish, Simplified Chinese (Mandarin) and Ukrainian
- Ready Steady Baby leaflet in English (Easy Read)
Source: Public Health Scotland - Opens in new browser window
Last updated: 14 December 2023
Help us improve NHS inform
Your feedback has been received
Don’t include personal information e.g. name, location or any personal health conditions.
Also on NHS inform
- Travel health and vaccinations
Other health sites
- fitfortravel: Advice for pregnant women
- Institute for Health Visiting: Travelling with your baby
- Disabled Living Foundation (DLF)
- Rica: consumer research charity
- Health & Care Professions Council (HCPC)

1, 2, or 3 Weeks Pregnant

Weeks Pregnant
Pregnancy is a much anticipated time in your life, and you may be eagerly watching for those very early signs in weeks 1, 2, or 3. But, did you know that you’re not actually pregnant during these first couple of weeks? We know it’s a little confusing, and it’s also why you might not notice any pregnancy symptoms early on! Keep reading to better understand what’s going on in that body of yours during the first three weeks of pregnancy.
Highlights at 1, 2, and 3 Weeks Pregnant
Before we get into all the details, here are a few highlights to look forward to during these early weeks of your pregnancy:
Watching for symptoms in weeks 1, 2, and 3 of pregnancy. Are you wondering if it's possible to feel pregnant after two days, or during weeks 1 and 2 of pregnancy? You might notice symptoms like light bleeding, spotting, cramps, or bloating around week 3 when the egg implants into your uterus.
Calculating your due date. Most healthcare providers track pregnancy along 40 weeks, starting with the last day of your previous period. That means you aren’t actually pregnant until fertilization occurs and your baby is conceived, between week 2 and 3 of your pregnancy.
Making healthy choices early on. As early as possible in your pregnancy, you’ll want to adopt a healthy lifestyle that supports the development of your baby. Though your healthcare provider may offer specific advice, you'll likely want to incorporate certain vitamins, foods, and exercise into your daily life.
Your First Three Weeks of Pregnancy
Here’s the thing: Because of the way pregnancy is usually measured, you’re not actually pregnant during the first two weeks or so of your pregnancy. Healthcare providers calculate the length of an average pregnancy as 280 days, which is 40 weeks, starting from the first day of your last menstrual period—this is known as the LMP dating method.
So, when you’re 1 week pregnant, you’re having your period. At 2 weeks pregnant, you’re probably ovulating. And since ovulation happens about 14 days after the start of your period (assuming you have a 28-day cycle), with fertilization and conception following, you can’t really become pregnant until around week 3 at the earliest.
It can be mind-boggling—we get it. But, for the sake of calculation, and what you and your healthcare provider will consider as 1 and 2 weeks pregnant, you’re not actually pregnant until week 3. But although at 1, 2, or 3 weeks pregnant you may not notice any of those very early signs of pregnancy, there’s still a lot happening on the inside.
How to Determine Your Due Date
“If I'm 3 weeks pregnant when is my due date?” It's natural to wonder about your due date right away when you find out you’re pregnant, as you’re already looking forward to meeting your new baby!
For an estimate, try our Due Date Calculator , where you can simply enter the first day of your last menstrual period (LMP) or the date of conception.
RELATED PREGNANCY TOOL
Again, healthcare providers use the LMP method to determine your estimated due date. So once you start to notice those early pregnancy signs or have the feeling that you might be pregnant, take a pregnancy test at home or confirm your pregnancy with your healthcare provider so you can calculate your due date!
How Many Months Is 1 to 3 Weeks Pregnant?
Your healthcare provider will refer to your pregnancy in weeks, but you also might hear a reference to months. It gets a little tricky, given that nine months doesn't divide evenly into weeks, but the first month of pregnancy typically includes the first four weeks. So, at 1, 2, or 3 weeks pregnant, you’re in your first month of pregnancy, even if you haven’t noticed any belly bump or symptoms!
Are There Pregnancy Symptoms at 1, 2, or 3 Weeks Pregnant?
Your journey through pregnancy has officially begun, but as mentioned above, you’re not actually pregnant yet. This is a difficult concept to grasp at first, and many people wonder if there are any symptoms during the first 72 hours of pregnancy. Again, because of the way pregnancy is calculated, you won’t feel any symptoms of being pregnant during those first three days—or possibly three weeks. But after two weeks, an exciting series of events starts to take place inside your body:
Egg release. One of your ovaries will release an egg around 14 days after the first day of your last period (assuming you have a typical 28-day cycle).
Fertilization. The egg will travel down one of the fallopian tubes, where it may unite with sperm. If they find each other, they’ll join up in a fallopian tube to create a single cell called a zygote in a process called fertilization. This process determines the sex of a baby .
First DNA. The zygote carries chromosomes from the egg and sperm and sets the first building blocks of your future baby’s genetic makeup.
Development. The zygote then moves down the fallopian tube and toward the uterus as it starts dividing into a larger group of cells. Cells will continue to divide as your baby develops over the course of your pregnancy.
What this all boils down to is that you won’t feel any of those very early signs of pregnancy in weeks 1, 2, or possibly even 3. If you have yet to conceive, then it makes sense that you wouldn’t notice anything! Therefore, things like morning sickness can’t start at 1 week pregnant and you won’t feel symptoms like pregnancy-related belly pain or discharge at 1 or 2 weeks pregnant.
Typical Early Signs of Pregnancy
OK, so now you know that during weeks one, two, or three, you may not even suspect you’re pregnant and you likely won't notice any pregnancy symptoms at all, as it’s still very early (and you might not have even conceived until 3 weeks pregnant). However, there are several signs of pregnancy that you could experience in the following weeks:
A missed period is often the first clue (among other signs and symptoms) that you may be pregnant, but it won’t happen until you’re 4 weeks pregnant, not before. At around the time you miss a period, you may start noticing more early pregnancy symptoms.
Implantation bleeding is another early sign of pregnancy, as it occurs when the tiny ball of cells attaches to the uterine lining. Not everyone experiences it, but this light spotting is normal and can sometimes be mistaken for menstrual blood. Spotting, cramps, or light bleeding usually happens 10 to 14 days after conception, so around when you’re 3 to 4 weeks pregnant.
Morning sickness is another common symptom of early pregnancy, but it usually crops up between weeks 4 and 9.
Other symptoms like gas, fatigue, breast tenderness , moodiness, and frequent urination can also occur during these early weeks.
Now that you know these early signs of pregnancy, take our quiz to test your knowledge!
How Big Is a Pregnant Belly at 1, 2, and 3 Weeks?
Every person and every pregnancy is different, so you could start to show earlier or later than others. It’s safe to say that you won’t see any difference in your pregnant belly’s size at 1, 2, or 3 weeks. Remember that you’re not actually pregnant during those first two weeks and it’s still early during the third week.
How Big Is a Baby at 3 Weeks?
Even though your belly bump won’t be noticeable at 3 weeks pregnant, your baby's development is under way with cells dividing and multiplying. Still, by around 3 weeks in your pregnancy, your little one is just 1/25 of an inch long—too small for a bump just yet.
When Can You Confirm Your Pregnancy?
Can you get a positive pregnancy test at 3 weeks, you may wonder? It’s possible, but it’s always best to wait until after your missed period to take a pregnancy test, as you’ll receive more credible results. That’s because a home pregnancy test responds to the levels of a hormone called human chorionic gonadotropin, or hCG, in your urine, which begin to increase shortly after conception. So, although your hCG levels may be high enough in week 3 to result in a positive test, you’ll want to confirm with your healthcare provider that you’re pregnant.
Think you might be pregnant? Take our Am I Pregnant quiz . It won’t tell you for sure, but it’s all good fun!
How Far Along Are You?
Knowing how far along you are in pregnancy is helpful for both you and your healthcare provider. Your provider will use this information to check on your baby’s growth and development, keep an eye on your health, and schedule tests and exams.
The weeks of pregnancy can be grouped into three trimesters :
First trimester : 1 to 13 weeks (roughly months one to three)
Second trimester : 14 to 27 weeks (months four to seven)
Third trimester : 28 to 40-42 weeks (months seven to nine).
Check out the illustration below to see how far along you are in your pregnancy:
What Precautions Should You Take During Early Pregnancy?
Even though you probably haven’t experienced any signs of pregnancy very early on in weeks 1, 2, or 3, you’ll want to do everything you can to stay healthy and safe. In fact, it’s always wise to take some precautions as soon as you start trying to conceive or learn that you’re pregnant.
Lifestyle Adjustments
Even simple adjustments can help support you as you start your pregnancy! Though you’ll want to consult your healthcare provider to determine what’s best for you, some worthwhile lifestyle changes and precautions include
eating healthily
staying hydrated
reducing stress
getting regular exercise.
When you start trying for a baby or learn that you’re pregnant, folic acid is essential, as it’s a B vitamin that helps reduce the risk of certain birth defects that affect the baby’s brain and spine. Your healthcare provider can recommend a prenatal vitamin that contains at least 400 micrograms of folic acid.
Eliminating Bad Habits
Prepregnancy is also a great time to eliminate some less healthy habits, too, including
exposure to secondhand smoke
drinking alcohol.
In addition, your provider may recommend limiting your daily consumption of caffeine. Consult your healthcare provider to learn the best ways to stay healthy and safe when you’re pregnant.
For more general advice, download our pregnancy guide!
1 to 3 Weeks Pregnant: Your Checklist
Yes, it’s early, but it’s also an exciting time! As you anticipate your new pregnancy, consider the following to-dos:
□ Even if you’ve already taken one, you might want to complete another home pregnancy test after your missed period for the best results.
□ Schedule an appointment with your healthcare provider to confirm your pregnancy with a blood test.
□ Check out our pregnancy calendar to know what to anticipate in the next few weeks.
□ Though you can’t find out your baby’s gender just yet, have a little fun with our Chinese Gender Predictor !
- American College of Obstetricians and Gynecologists. Your Pregnancy and Childbirth: Month to Month, 6th ed. (Washington, DC: American College of Obstetricians and Gynecologists, 2015).
- Mayo Clinic. Guide to a Healthy Pregnancy, 2nd ed. (Rochester, MN: Mayo Clinic Press, 2018).
- Mayo Clinic. “Pregnancy Week by Week.”
- Mayo Clinic. “Symptoms of Pregnancy: What Happens First.”
- Kids Health. “Week 1.”
- National Library of Medicine. “Length of Human Pregnancy and Contributors to its Natural Variation.”
Review this article:
Read more about pregnancy.
- Giving Birth
- Pregnancy Announcement
- Pregnancy Calendar
- Pregnancy Symptoms
- Baby Shower & Registry
- Prenatal Health and Wellness
- Preparing For Your New Baby
- Due Date Calculator

Pregnancy Week by Week

3 Weeks Pregnant

Key Takeaways at 3 Weeks Pregnant
- Guess what? Fertilization has just occurred. Yes, that means you’re officially pregnant—you probably just don’t know it yet!
- What’s on the cusp of happening next? Implantation ! If you notice a little bit of spotting, it might be an embryo burrowing itself in your uterus. Then again, you may not experience any bleeding or you might think it’s your period.
- If you’ve been trying to get pregnant, then you’ve likely started making some lifestyle changes. If not, there’s no time like the present. Make sure you’re taking a prenatal vitamin, getting moderate exercise and avoiding alcohol.
Sperm met egg last week, and voila—you've made a baby! It’s so early that when you’re 3 weeks pregnant, you may have no idea that you’re actually pregnant. Conception just happened a few days ago, and there probably hasn't been time for you to miss a period yet at week 3 of pregnancy.
Baby at Week 3
Your now-fertilized egg (yay!) is on a journey through a fallopian tube, dividing and re-dividing into identical cells on its way to your uterus.
3 week ultrasound
At 3 weeks pregnant, an ultrasound may not detect your soon-to-be-baby. That super-teeny fertilized egg (called a morula) is smaller than a grain of salt and is on the move, but as early as week 4 your doctor may be able to see your uterine lining get thicker, a sign that the little morula has reached their destination for the rest of pregnancy (you guessed it: your uterus).
Pregnancy Symptoms at Week 3
When you’re 3 weeks pregnant, symptoms may not have appeared yet. That’s because most early pregnancy symptoms are caused by pregnancy hormones, and you probably don’t have a very high level of those in your body yet. (Oh, but you’ll get there!) Some signs of pregnancy at 3 weeks—and the few weeks following—are:
Implantation bleeding
If your little soon-to-be-embryo has already made it to their new home, you may see a bit of spotting as the fertilized egg burrows into the lining of your uterus.
As the pregnancy hormone hCG begins to make its way through your newly pregnant body, you may notice some feelings of queasiness—or nausea so bad it makes you puke. Morning sickness should really be called all-day sickness since it doesn’t discriminate by time of day. If you’re feeling this symptom of pregnancy at this point, you may be further along than you thought. (Or you may even be 3 weeks pregnant with twins! That’s because twin moms-to-be often have higher levels of pregnancy hormones and therefore worse nausea.)
Breast changes
Your breasts can start to get sore and your nipples may darken as your body starts prepping to make milk.
Missed period
If your cycle is typically shorter than 28 days, you may realize toward the end of this week that you could be pregnant. The only way to know for sure is to take a pregnancy test .
Positive home pregnancy test
Check the box of your home pregnancy test to see how accurate its results are before your missed period. Most are over 99 percent accurate once you’ve missed it, and some brands promise to detect pregnancy hormones in your urine sooner than that. (For example, when you’re 3 weeks 5 days pregnant or even 3 weeks 4 days pregnant.) Here’s the thing: The amount of pregnancy hormone hCG in your body might not be enough for the test to detect right away—but it doubles every 48 hours. If you get a negative result, follow up a few days and then a week later with another pregnancy test and then another, to be sure it wasn’t just too early to tell.
Positive blood pregnancy test
In some cases—like if you’re at risk for miscarriage or ectopic pregnancy—your doctor may ask you to come into the office for a blood draw. Blood tests can detect smaller amounts of hCG than urine tests can, so you may find out that you’re pregnant sooner with a blood test than you would with an at-home test.
Can you tell you’re pregnant at 3 weeks?
While some people feel no difference at all at this early stage, others may start to notice 3 weeks pregnant symptoms. The experience at 3 weeks pregnant can really vary, so don’t fret if you don’t feel anything out of the ordinary. However, if you feel nauseous and your breasts are sore, that’s normal too. Everything changes quickly in early pregnancy, so no matter how you feel, be prepared to feel different in a week!

Your Pregnant Belly at 3 Weeks
You may be excited to start noticing something different about your appearance, but at 3 weeks pregnant, a belly isn’t really a thing. Though you may feel a bit bloated , most pregnant women don’t start to show until around week 12 or later, so you’ve got quite a way to go before you actually look pregnant.
Before you start eating for two, know that doctors only recommend most women gain one to five pounds total in the first trimester—that’s the first 13 weeks. So you definitely don’t have license to start majorly indulging at this point. In fact, you shouldn’t really do anything different except try to eat a healthy, well-rounded diet and take a daily prenatal vitamin with at least 400 micrograms of folic acid in it. Doctors don’t recommend increasing your daily calorie intake until the second trimester. Once you hit week 14 , you’ll want to add about 300 (healthy) calories per day.
How many weeks are you at implantation?
Implantation occurs soon, at about 4 weeks pregnant. For implantation to happen, the cells in the fertilized egg, now a morula, will continue to divide until it becomes a blastocyst. About five to eight days after fertilization, the blastocyst will have arrived, where it will begin to implant in the wall of the uterus. What a journey!
Pregnancy tests have come a long way and can even detect pregnancy before you’ve missed your period. That can work for you and also against you. For the truest result, I'd recommend testing a few days after you’ve missed your period with first morning urine. If negative and still no period, repeat this process every two to three days—always first thing in the morning.
Heather Bartos
MD, ob-gyn and medical director of Be. Women’s Health & Wellness
Tips for 3 Weeks Pregnant
Trying to conceive can be daunting, and perpetually wondering if you’re expecting can further cause stress. Here’s what you can do to prioritize your physical and mental health.
First things first: You’re probably chomping at the bit to officially find out that you’re pregnant, but be patient. A pregnancy test might not be able to detect a pregnancy just yet. Wait until the test you’ve purchased says it can detect a pregnancy—probably at the end of the week. Once you start testing, if you get a negative result, feel free to keep testing every couple days until you get your period.
Ace that test
When it’s time to take the pregnancy test at the end of the week, take it first thing in the morning. Your first morning pee is the most concentrated, making it the most likely to have a high enough concentration of hCG for the test to detect. Follow the directions exactly for the most accurate results.
Continue taking care of yourself
You should still be taking your prenatal vitamins every day, drinking plenty of water and eating healthy, balanced meals. Continue to get regular moderate exercise and practice self-care.
Focus on foods that are high in calcium and iron to help support the extra blood your body is making. If you’re nauseous or vomiting, try making ginger tea, drinking some clear broth or eating a banana (yay, potassium!). Even ice cream can be a good compromise when you’re struggling to eat but still need protein and calcium. Make it a banana split with a few nuts and you’re covering your bases pretty well!
I bought every test on the store shelf. Strips, dips, digital, you name it. It was like a scene out of a sitcom. I needed a definitive answer—over and over again.
Emily M., mom of two
Pregnancy Checklist at Week 3
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
American College of Obstetricians and Gynecologists, Morning Sickness: Nausea and Vomiting During Pregnancy , December 2021
American Pregnancy Association, 3 Weeks Pregnant
American Pregnancy Association, 12 Weeks
American Pregnancy Association, Are You Pregnant?
American Pregnancy Association, Diet During Pregnancy
American Pregnancy Association, Early Fetal Development
American Pregnancy Association, Folate and Folic Acid When Pregnant
American Pregnancy Association, Pregnancy Nutrittion
American Pregnancy Association, Pregnancy Tests
American Pregnancy Association, Pregnancy Weight Gain
Centers for Disease Control and Prevention, Planning for Pregnancy , February 2023
Cleveland Clinic, Am I Pregnant? , July 2022
Cleveland Clinic, Fetal Development , March 2023
Cleveland Clinic, Pregnancy Tests , November 2022
March of Dimes, Pregnancy Week by Week
Mayo Clinic, Fetal Development: The 1st Trimester , June 2022
Mayo Clinic, Is Nausea During Pregnancy a Good Sign? , October 2021
NPR, The Surprising Science of How Pregnancy Begins , April 2023
Planned Parenthood, Pregnancy Tests
Planned Parenthood, Month by Month
Planned Parenthood, When do Pregnancy Symptoms Start? , June 2020
UNICEF, What to Eat Before, During and After Pregnancy
Learn how we ensure the accuracy of our content through our editorial and medical review process .
Navigate forward to interact with the calendar and select a date. Press the question mark key to get the keyboard shortcuts for changing dates.
- Share full article
Advertisement
Supported by
The First Six Weeks of Pregnancy, Explained
Florida is set to ban abortions after six weeks. Experts explain how that can often be before a woman knows she is pregnant.

By Alisha Haridasani Gupta
By the time a woman is considered six weeks pregnant, she would have had two weeks, at most, to realize it.
That’s because the gestational age of a fetus is counted not from the moment that sperm fertilizes an egg or from the moment you have a positive pregnancy test, but weeks earlier, on the first day of the previous menstrual cycle. This means that just two weeks after a missed period, a woman is six weeks pregnant, said Dr. Dawnette Lewis, director of Northwell Health’s Center for Maternal Health in New York and a maternal fetal medicine specialist.
That’s if someone has a typical menstrual cycle, which lasts about four weeks. But several factors — including stress, perimenopause and certain health conditions — can make the menstrual cycle so unpredictable that it could take longer than six weeks for someone to realize they might be pregnant.
“People come in and they’re like, ‘I’ve always had irregular periods and I just thought I was gaining weight’ and lo and behold, they are pregnant,” said Dr. Shruthi Mahalingaiah, a fertility doctor at Massachusetts General Hospital and professor of environmental and reproductive health at Harvard T.H. Chan School of Public Health.
The question of how soon it’s possible to detect and confirm a pregnancy has come into focus as new abortion restrictions have been enacted in 21 states , including in Florida, where a ban on abortion after six weeks is set to take effect May 1, making it the third state to do so.
We asked experts to explain how the first six weeks of pregnancy unfold, and what factors might make a pregnancy hard to detect.
Weeks 1 to 2:
If an egg isn’t fertilized, the uterus sheds its lining. The first day of bleeding is considered Day 1 of a menstrual cycle. Typically, this bleeding lasts between three and seven days, Dr. Lewis said.
As the bleeding subsides, estrogen and another hormone, called follicle stimulating hormone or F.S.H., begin to rise. Together, they nudge the ovaries to produce a mature egg and create a fresh uterine lining for a potential fertilized egg.
At or around Day 14 of a cycle, the ovary would typically release an egg. If an egg is released and sperm is present, fertilization can occur in the fallopian tube a day or two after ovulation.
Weeks 3 to 4:
If an egg has been fertilized, it becomes an embryo, which typically travels into the uterus and implants itself on the lining. This can take around a week or more, Dr. Belmonte said.
Once this happens, the body begins producing a hormone called human chorionic gonadotropin, also known as the pregnancy hormone. This tells the ovaries to hold off producing another egg.
At implantation, a woman would technically be considered about four weeks pregnant, based on how gestational age is calculated. But she would likely not have any physical symptoms of pregnancy, like nausea or fatigue. HCG levels may also be too low to be detected by an at-home pregnancy test; it is only detectable about a week after implantation, said Dr. Michael Belmonte, an obstetrician-gynecologist and fellow at the American College of Obstetricians and Gynecologists.
It is impossible to know if the embryo will keep developing normally or whether it even implanted in the uterus, said Dr. Mahalingaiah. About half of fertilized embryos do not end up implanting at all. In an estimated 2 percent of pregnancies, the embryo implants elsewhere, like the fallopian tube. This is known as an ectopic pregnancy and can be life-threatening, requiring medical or surgical intervention.
If you are pregnant, this is, roughly speaking, the earliest that you might be able to detect a pregnancy at home. If you have a regular four-week cycle, have missed your period and think you might be pregnant, you might take a urine test at home at the tail end of this week, which would pick up elevated hCG levels.
But there are several reasons to expect a period to be irregular and not think to take a pregnancy test at this point. Polycystic ovarian syndrome , which affects as many as five million women in the United States, can disrupt ovulation and cause irregular menstrual cycles, as can other endocrine disorders like thyroid disease. Significant amounts of stress in the first two weeks of your cycle can delay ovulation or menstruation, said Dr. Mahalingaiah, as can a bad case of the flu. Those who are in perimenopause, the transition to menopause, experience increasingly irregular ovulation as they approach the end of their reproductive years. This means that their menstrual cycles can change in length every month , often by several weeks.
Even if you did suspect you were pregnant around week 5, a health care provider would not be able use an ultrasound to confirm that a pregnancy is viable, because there would be no fetal cardiac activity yet. The pregnancy may also turn out to have been what is known as a biochemical pregnancy, Dr. Mahalingaiah said. When this happens, someone might test positive on an early home pregnancy test, but the fetus doesn’t develop further. This results in a pregnancy loss that simply looks like a late period. Some research suggests an estimated 22 percent of pregnancies end this way.
This is approximately when an ultrasound could pick up fetal cardiac activity, which can sound like a heartbeat. Some states require an ultrasound before a woman can obtain an abortion, including a medication abortion. Florida requires two in-person visits, 24 hours apart, including an ultrasound. The new law also prohibits telehealth providers from prescribing medication to end a pregnancy.
That timing, Dr. Belmonte said, leaves women with “a very small window” in which to confirm a pregnancy and obtain an abortion.
Alisha Haridasani Gupta is a Times reporter covering women’s health and health inequities. More about Alisha Haridasani Gupta
Pregnancy, Childbirth and Postpartum Experiences
‘A Chance to Live’: Cases of trisomy 18 may rise as many states restrict abortion. Some women have chosen to have these babies , love them tenderly and care for them devotedly.
Teen Pregnancies: A large study in Canada found that women who were pregnant as teenagers were more likely to die before turning 31 .
Weight-Loss Drugs: Doctors say they are seeing more women try weight-loss medications in the hopes of having a healthy pregnancy. But little is known about the impact of those drugs on a fetus.
Premature Births: After years of steady decline, premature births rose sharply in the United States between 2014 and 2022. Experts said the shift might be partly the result of a growing prevalence of health complications among mothers .
Depression and Suicide: Women who experience depression during pregnancy or in the year after giving birth have a greater risk of suicide and attempted suicide .
A Long Awaited Breakthrough: Scientists said they had pinpointed the cause of severe morning sickness — a discovery could lead to better treatments for severe nausea and vomiting during pregnancy.

An official website of the United States government
Here's how you know
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
What the New Overtime Rule Means for Workers

One of the basic principles of the American workplace is that a hard day’s work deserves a fair day’s pay. Simply put, every worker’s time has value. A cornerstone of that promise is the Fair Labor Standards Act ’s (FLSA) requirement that when most workers work more than 40 hours in a week, they get paid more. The Department of Labor ’s new overtime regulation is restoring and extending this promise for millions more lower-paid salaried workers in the U.S.
Overtime protections have been a critical part of the FLSA since 1938 and were established to protect workers from exploitation and to benefit workers, their families and our communities. Strong overtime protections help build America’s middle class and ensure that workers are not overworked and underpaid.
Some workers are specifically exempt from the FLSA’s minimum wage and overtime protections, including bona fide executive, administrative or professional employees. This exemption, typically referred to as the “EAP” exemption, applies when:
1. An employee is paid a salary,
2. The salary is not less than a minimum salary threshold amount, and
3. The employee primarily performs executive, administrative or professional duties.
While the department increased the minimum salary required for the EAP exemption from overtime pay every 5 to 9 years between 1938 and 1975, long periods between increases to the salary requirement after 1975 have caused an erosion of the real value of the salary threshold, lessening its effectiveness in helping to identify exempt EAP employees.
The department’s new overtime rule was developed based on almost 30 listening sessions across the country and the final rule was issued after reviewing over 33,000 written comments. We heard from a wide variety of members of the public who shared valuable insights to help us develop this Administration’s overtime rule, including from workers who told us: “I would love the opportunity to...be compensated for time worked beyond 40 hours, or alternately be given a raise,” and “I make around $40,000 a year and most week[s] work well over 40 hours (likely in the 45-50 range). This rule change would benefit me greatly and ensure that my time is paid for!” and “Please, I would love to be paid for the extra hours I work!”
The department’s final rule, which will go into effect on July 1, 2024, will increase the standard salary level that helps define and delimit which salaried workers are entitled to overtime pay protections under the FLSA.
Starting July 1, most salaried workers who earn less than $844 per week will become eligible for overtime pay under the final rule. And on Jan. 1, 2025, most salaried workers who make less than $1,128 per week will become eligible for overtime pay. As these changes occur, job duties will continue to determine overtime exemption status for most salaried employees.
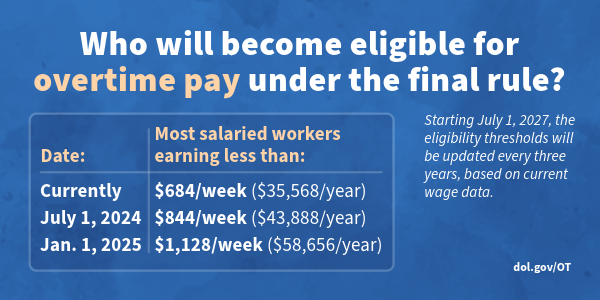
The rule will also increase the total annual compensation requirement for highly compensated employees (who are not entitled to overtime pay under the FLSA if certain requirements are met) from $107,432 per year to $132,964 per year on July 1, 2024, and then set it equal to $151,164 per year on Jan. 1, 2025.
Starting July 1, 2027, these earnings thresholds will be updated every three years so they keep pace with changes in worker salaries, ensuring that employers can adapt more easily because they’ll know when salary updates will happen and how they’ll be calculated.
The final rule will restore and extend the right to overtime pay to many salaried workers, including workers who historically were entitled to overtime pay under the FLSA because of their lower pay or the type of work they performed.
We urge workers and employers to visit our website to learn more about the final rule.
Jessica Looman is the administrator for the U.S. Department of Labor’s Wage and Hour Division. Follow the Wage and Hour Division on Twitter at @WHD_DOL and LinkedIn . Editor's note: This blog was edited to correct a typo (changing "administrator" to "administrative.")
- Wage and Hour Division (WHD)
- Fair Labor Standards Act
- overtime rule
SHARE THIS:

- United States
- United Kingdom
Travel insurance: Pregnancy
Find the right pregnancy travel insurance – you can secure cover during your third trimester. however, very few providers will offer insurance after 30 weeks..
In this guide
Compare travel insurance for pregnancy
What is pregnancy travel insurance, does travel insurance cover pregnancy complications, what isn't covered by pregnancy travel insurance, how do travel insurers cover pregnancy, how to find the best travel insurance for pregnancy, when can i get travel insurance for pregnancy, risks for pregnant women while travelling, any more questions.
Destinations
What you need to know
- Travel insurers can offer cover up to 30 weeks of pregnancy, with a select few offering cover up to 36 weeks
- You may need to let the travel insurer know that you are expecting
- Cover may differ if you are expecting twins or have conceived through IVF
Enter your trip details, filter by "Pregnancy", and select 'More info' to see each travel insurers maximum gestation period.
Use a comma or space to separate ages. Add kids under the age of 1 by typing a “0” 0 traveller(s)
Include travel deals and helpful personal finance content from Finder
By submitting this form, you agree to our Privacy & Cookies Policy and Terms of Service
Pregnancy travel insurance is a policy that will cover you for pregnancy-related expenses while you travel. It's most handy for unexpected medical expenses and cancellation. While it's not usually a specific type of policy, you can get covered by choosing the right travel insurance for your trip.
It can cover you for;
- Financial support for unexpected medical complications
- Emergency childbirth
- Cancellation cover if your doctor says it's not safe to travel
- Additional expenses to fly your partner or a relative to support you in case of emergency
- Your repatriation to Australia in case of emergency (this usually won't cover the repatriation of your baby if it's born overseas)
- Daily hospital cash allowance to cover things like TV use and magazines in the hospital
Yes, travel insurance may cover claims that arise from complications that include:
- gestational diabetes
- gestational hypertension
- pre-eclampsia
- ectopic pregnancy
- molar pregnancy or hydatidiform mole
- post-partum haemorrhage
- retained placenta membrane
- placental abruption
- hyperemesis gravidarum
- placenta praevia
- miscarriage
- emergency caesarean section
- a termination due to medical reasons
- premature births (insurers may have a gestation limit)
There are certain situations and circumstances when pregnancy simply will not be covered by your travel insurance . Your insurer may not provide any cover if:
- Your claim is for antenatal care, childbirth or the care of a newborn child
- Your claim is for standard pregnancy symptoms such as morning sickness, breast tenderness, fatigue, frequent urination, constipation and heartburn
- The purpose of your trip is to undergo fertility treatment
- You've experienced pregnancy complications prior to your policy being issued
- Your pregnancy was conceived through assisted reproduction services such as IVF
- You travel against medical advice
- Your pregnancy will pass the maximum period of gestation allowed by the insurer during your trip
- Your claim is for medical expenses incurred in Australia
- Your claim is for regular antenatal care and routine pregnancy check-ups, for example standard ultrasounds, blood tests or pregnancy tests
This list isn't exhaustive. If there's something specific that you're worried about, check directly with your chosen insurer.
Here's a more detailed breakdown of how some of Australia's most popular travel insurers cover pregnancy.
Ask your doctor if it's safe to travel
Figure out your gestation period
Compare your options and choose a brand that will cover your gestation period
Make sure you have cover for pregnancy-related complications and cancellations
Buy the travel insurance policy as early as possible
Most insurers can cover you if you're between 20-26 weeks pregnant. The risk of complications, including giving birth, increases as you move towards the end of your third trimester. But, you can still get cover outside of these times in some cases.
Be aware that some domestic travel policies won't include pregnancy cover. Also, insurers will likely set strict conditions about what they'll cover – and what they won't – in relation to your pregnancy.
Why Sarah got travel insurance
I have actually planned international travel around pregnancy in the past to give me peace of mind. The last thing I ever wanted was to end up giving birth in a foreign country without the same access to affordable healthcare we have in Australia. Different countries have different laws around 'viability' too, which is awful to think about – the gestation at which doctors think the baby being born is viable with life - but it's really important. In Australia viability is 24 weeks, but in other countries it's 26 weeks. Most recently I flew at 15 weeks pregnant and I read my policy that came free with my credit card before I travelled, and confirmed that as long as I spend at least $500 on travel using my card, I was covered for pregnancy up to 23 weeks.

Sarah Megginson Head of editorial at Finder
While travel can be relaxing, memorable and fun, it also comes with a number of risks attached. Before hitting the road, make sure you’re aware of what can go wrong, and the complications it could cause for you and your unborn child:
- Illness. Falling ill on the road is not only unpleasant, it can also cause serious issues for pregnant women. Due to the increased risk of disease, travel to developing countries is not recommended. You should also be very wary of visiting any country where malaria is present, as malaria can cause miscarriage, premature labour and stillbirth.
- Food poisoning. Some infections can harm your baby or even lead to miscarriage, so be careful what you eat and drink if visiting a country with poor hygiene standards. Avoid undercooked meats and soft cheeses, wash your hands thoroughly, and don’t eat from dodgy street food vendors. If you’re not sure about the quality of the water supply, make sure to only drink bottled water.
- Medications. Pregnant women need to be wary of taking any medications during pregnancy. Some medications, including some products commonly used to treat traveller’s diarrhoea, are dangerous during pregnancy. Make sure you only take medication recommended by a doctor who is aware of your pregnancy.
- Stress. Battling crowds, rushing to make it to the airport on time and dealing with unexpected delays can all cause stress on a holiday. Try to just take it easy and go with the flow at all times, and avoid situations or experiences that are likely to cause stress. While piloting a scooter through the manic city streets of Hanoi might have been the perfect holiday experience when you were younger, a lazy beach holiday is a much better idea at this time of your life.
- Deep vein thrombosis (DVT). Extended periods without moving, such as on a plane or in a car, can cause clots to form in the deep veins of the leg. DVT can potentially be fatal, and pregnant women have a higher risk of developing it.
- Overheating. Overheating during pregnancy can cause serious problems, so take care if travelling in hot weather. Take it easy, stay hydrated at all times, avoid the hottest part of the day, wear plenty of sunscreen and avoid overexerting yourself.
When is the best time to travel when pregnant?
According to pregnancybirthbaby.org, it's best to travel within the second trimester - between 13-26 weeks. At this time, you're at the lowest risk of complications. It's also helpful to note that some airlines have a restriction on gestation periods for your own safety. Make sure to check this before you travel, if you're denied boarding for being too far long in your prgenancy, travel insurance is unlikely to cover you.
Do I have to pay extra for pregnancy cover?
Not usually. Most insurers will automatically cover single, uncomplicated pregnancies at no extra cost. If you're having twins, have had fertility treatments (like IVF) or have pre-existing conditions related to your pregnancy, you may have to pay an additional premium.
Can I get cover if I'm having twins or triplets?
Yes. There are a fair few travel insurance brands that will cover multiple pregnancies. You may have to take an online medical assessment when applying and pay for any additional premiums for cover.
Does travel insurance cover giving birth?
Some travel insurers will cover emergency childbirths, but not all. Make sure to check directly with your insurer. If it's a planned overseas birth, your travel insurance probably won't cover the costs as it's usually for unexpected medical care.
Will the baby be covered?
It really depends on the insurer. There are many insurers who will not provide any cover for the cost of childbirth or expenses related to the medical care of a newborn baby. If you select such a policy and your baby is born overseas, keep in mind that you will most likely face extensive out-of-pocket expenses and, depending on where you're travelling, may not be able to access the best possible level of care for your baby.
However, some insurers will provide cover if your baby arrives early, as long as your little bundle of joy is born inside the insurer's maximum weeks of pregnancy permitted time limit. As always, check the PDS closely to read the full terms and conditions and contact the insurer directly if there's anything you're unsure about.
What if I hit 32 weeks after I've already commenced travel?
If you reach the 32-week mark halfway through your holiday, don't expect your travel insurance to continue providing pregnancy cover all the way through until you return to Australia. In fact, many will refuse to provide any pregnancy cover for your trip unless you're due to return to Australia before the gestation limit has been reached. Once you've reached the insurer's maximum coverable gestation, you will most likely be unable to claim for anything related to your pregnancy or its complications. We recommend making sure your trip ends before you hit the 32-week mark to ensure your whole holiday is covered.
What if I have to cancel my trip due to pregnancy
If you're advised against travelling by your doctor, the good news is that your travel insurance policy can provide cover for the cost of cancelling your holiday. This includes cover for any cancellation fees you're required to pay, as well as any pre-paid deposits for accommodation, tours and the like that are non-refundable. You can also take advantage of trip interruption cover from your travel insurer. For example, if an unexpected complication develops during your journey and treating doctors recommend that the best course of action is for you to return home and rest, travel insurance can cover the cost of your forfeited pre-paid expenses and also the additional flights needed to get you home safely.

Worried you might have to cancel your trip?

Get the right cover for pre-existing medical conditions

Looking for top level cover? Get comprehensive travel insurance

Jessica Prasida
Jessica Prasida is a travel insurance expert for Finder. She lives and breathes travel, having worked as a travel agent and branch manager at STA Travel for over 4 years, then writing about travel insurance with Finder for another 5 years. Jess has a Bachelor of Business from the University of Technology, Sydney and a Tier 1 General Insurance qualification.
More guides on Finder
Want to make sure you're covered in case your relative falls ill or passes away at home while you're travelling? Read more.
Ask a Question
Click here to cancel reply.
You are about to post a question on finder.com.au:
- Do not enter personal information (eg. surname, phone number, bank details) as your question will be made public
- finder.com.au is a financial comparison and information service, not a bank or product provider
- We cannot provide you with personal advice or recommendations
- Your answer might already be waiting – check previous questions below to see if yours has already been asked
12 Responses
Some of the insurance companies you have listed above show they cover for IVF and Multiple pregnancies but when I go to their sites one or both of these conditions isn’t covered. Is this table up to date? Thanks
Thanks for your question. I have gone through the table to make sure the information is correct. A couple of the providers have indeed updated their information. The data contained in the table reflects the information available in the product disclosure statements (PDS) available from each insurance brand and is up to date.
I hope this was helpful, Richard
Your table is still out of date. Already been through three of the companies you listed as being ok to cover pregnancies as a result of IVF and none so far actually cover this.
Thanks for getting in touch. I’ve reviewed the table and amended those policies which have been updated. It looks like for the majority, you’ll need to provide a pre-existing medical declaration. Also, Worldcare does offer this cover.
All the best, Richard
Hi, I am planning to travel to Fiji for 1week, returning in my 32nd week of pregnancy. Obstetrician is happy for me to go. Single, unassisted and healthy pregnancy. I have found some providers that will cover me, but not the baby if it is born prematurely. Can you provide any advice on who would cover the costs for both me and the baby? Thank you, Rebecca
Hi Rebecca,
Thanks for your question.
There are a lot of travel insurance brands that include pregnancy cover as part of their standard policy. While a fair few insurers cover emergency births, some insurers do not cover childbirth at any stage of the pregnancy.
If the policy you are going to take out covers pregnancy, then there’s a good chance it will cover emergency births. If this is something you’re worried about, make sure you confirm directly with your insurer.
You may see the list of insurers on the pregnancy travel insurance and speak to insurers that includes emergency childbirth.
Dear Will, I would like to ask you, if you can recommend me some travel insurance. I will travel to Israel on 2.July till 13.July and will be in my 31./32. week of pregnancy. Im from Czech rep. and here we have travel insurance covering pregnancy issues just till 28.week. Thanks for your answer
Thanks for your question. finder.com.au is a comparison service and we are not permitted to provide personalised advice. The travel insurers in our panel provide policies for Australian citizen and those in Australia on certain visas.
Will anyone cover a refund of paid for bookings if I get pregnant after paying and therefore have to cancel because the destination is not safe during pregnancy (such as Cusco in Peru)?

Generally Pregnancy will be only covered up to 26 weeks inclusive, if it is a single, natural and no complications and cover will only be provided if it is an emergency. General check ups are not covered under the policy.You would not covered if it is unsafe to travel, you are only covered for cancellation if case there is a complication that has been certified by a medical practitioner.
I hope this helps,
Hi can I check if a 26 week 5 day pregnancy would be covered under the ’26 week inclusive’ clause? Thanks very much.
Thanks for your inquiry.
This extension provides cover from the 26th week of pregnancy for unexpected pregnancy-related complications, childbirth, and care of new-born during the trip, provided:
– Your trip does not extend beyond the 30th week of pregnancy
– You’re not traveling against the advice of your doctor or midwife
– There have been no complications with your pregnancy
– It’s not a multiple pregnancy
– The pregnancy did not result from assisted reproductive programs
Note: if you have any non-pregnancy related medical conditions you will need to apply for this extension by phone
Hope this information helped.
Cheers, Arnold
How likely would you be to recommend finder to a friend or colleague?
Our goal is to create the best possible product, and your thoughts, ideas and suggestions play a major role in helping us identify opportunities to improve.
Important information about this website
Advertiser disclosure.
finder.com.au is one of Australia's leading comparison websites. We are committed to our readers and stands by our editorial principles
We try to take an open and transparent approach and provide a broad-based comparison service. However, you should be aware that while we are an independently owned service, our comparison service does not include all providers or all products available in the market.
Some product issuers may provide products or offer services through multiple brands, associated companies or different labeling arrangements. This can make it difficult for consumers to compare alternatives or identify the companies behind the products. However, we aim to provide information to enable consumers to understand these issues.
How we make money
We make money by featuring products on our site. Compensation received from the providers featured on our site can influence which products we write about as well as where and how products appear on our page, but the order or placement of these products does not influence our assessment or opinions of them, nor is it an endorsement or recommendation for them.
Products marked as 'Top Pick', 'Promoted' or 'Advertisement' are prominently displayed either as a result of a commercial advertising arrangement or to highlight a particular product, provider or feature. Finder may receive remuneration from the Provider if you click on the related link, purchase or enquire about the product. Finder's decision to show a 'promoted' product is neither a recommendation that the product is appropriate for you nor an indication that the product is the best in its category. We encourage you to use the tools and information we provide to compare your options.
Where our site links to particular products or displays 'Go to site' buttons, we may receive a commission, referral fee or payment when you click on those buttons or apply for a product. You can learn more about how we make money .
Sorting and Ranking Products
When products are grouped in a table or list, the order in which they are initially sorted may be influenced by a range of factors including price, fees and discounts; commercial partnerships; product features; and brand popularity. We provide tools so you can sort and filter these lists to highlight features that matter to you.
Terms of Service and Privacy Policy
Please read our website terms of use and privacy policy for more information about our services and our approach to privacy.
Florida abortion clinics and funds face uncertain future on eve of six-week ban
- Medium Text

CASH CRUNCH
Sign up here.
Reporting by Gabriella Borter and Joseph Ax; editing by Paul Thomasch and Bill Berkrot
Our Standards: The Thomson Reuters Trust Principles. New Tab , opens new tab

Thomson Reuters
Gabriella Borter is a reporter on the U.S. National Affairs team, covering cultural and political issues as well as breaking news. She has won two Front Page Awards from the Newswomen’s Club of New York - in 2020 for her beat reporting on healthcare workers during the COVID-19 pandemic, and in 2019 for her spot story on the firing of the police officer who killed Eric Garner. The latter was also a Deadline Club Awards finalist. She holds a B.A. in English from Yale University and joined Reuters in 2017.
World Chevron

Yellen: US negotiating R&D tax credit as part of global tax deal
Treasury Secretary Janet Yellen said on Tuesday that the United States is in talks with other countries to carve out an allowance for the U.S. research and development tax credit as part of the 15% global minimum tax deal.

Postpartum weight loss: how much how soon?

i gained 55 lbs. i lost 35 by 2 weeks PP so i still have a ways to go. the last 20 lbs were stubborn in my last pregnancy so im assuming it won’t be coming off anytime soon.
I lose it that fast. I’ve lost all 25 pounds gained during pregnancy at 3 weeks pp. I’ve also lost a few more pounds.
You May Also Like
Planning visitors during hospital stay, you’re pregnant how these moms reacted, jump to your week of pregnancy, trending on what to expect, moms share home remedies for pregnancy morning sickness, 8 expensive products moms say are worth the money, ⚠️ you can't see this cool content because you have ad block enabled., 14 moms on what labor really feels like, what are your go-to healthy snacks, things they don't tell you about: mom edition, pregnancy brain moments let's have a laugh, help keep our community safe, to create a safe place, please, on our end, we will.

IMAGES
VIDEO
COMMENTS
Download any apps you use for renting cars and accessing boarding passes before you leave so you can easily reschedule things in the event of a last-minute cancellation. If you're flying during your third trimester, be sure to call the airline to check about the cutoff week for pregnancy travel. A note from your doctor that says you're ...
In most cases, pregnant women can travel safely until close to their due dates. ... The best time to travel is mid-pregnancy (14 to 28 weeks). During these weeks, your energy has returned, morning sickness is improved or gone, and you are still able to get around easily. After 28 weeks, it may be harder to move around or sit for a long time.
Most people can safely travel by airplane during pregnancy, but talk to your healthcare provider ahead of time to make sure you don't have any medical conditions that could cause a complication ...
Answer From Mary Marnach, M.D. Generally, air travel before 36 weeks of pregnancy is considered safe for people who aren't dealing with any pregnancy problems. Still, if you're pregnant, it's a good idea to talk with your health care provider before you fly. Your provider might suggest that you not fly if you have certain pregnancy ...
Before you book a cruise or air travel, check the airlines or cruise operator policies for pregnant women. Some airlines will let you fly until 36 weeks, but others may have an earlier cutoff. Cruises may not allow you to travel after 24-28 weeks of pregnancy, and you may need to have a note from your doctor stating you are fit to travel.
Pregnancy and Flying: Your Trimester by Trimester Guide. As a general rule of thumb, most airlines will allow pregnant people to fly right up until week 36 of pregnancy, but you should absolutely ...
Travel During Pregnancy. As long as there are no identified complications or concerns with your pregnancy, it is generally safe to travel during your pregnancy. The ideal time to travel during pregnancy is the second trimester. In most cases, you are past the morning sickness of the first trimester and several weeks from the third stage of ...
Stand up and stretch. Pregnant women are at higher risk for developing blood clots, so it's important to avoid sitting still for long periods of time. Wear loose clothes and keep the blood flowing in your legs: Whether you're flying or driving, take breaks to get up, walk around and stretch every half hour or so.
Virgin Australia. No restrictions. Travel permitted; requires a medical certificate dated within 10 days of departure date once you reach 28 weeks. For flights longer than four hours, travel is not permitted after 36 weeks of pregnancy (32 weeks if pregnant with multiples), or within 48 hours of normal vaginal delivery.
When to travel in pregnancy. Some women prefer not to travel in the first 12 weeks of pregnancy because of nausea and vomiting and feeling very tired during these early stages. The risk of miscarriage is also higher in the first 3 months, whether you're travelling or not. Travelling in the final months of pregnancy can be tiring and uncomfortable.
Learn the ins and outs of traveling safely during pregnancy -- whether you're flying, driving, or going on a cruise. ... "I always tell my patients no travel after 32 weeks, because if she ...
Dr. Gaither says pregnant travelers should stop "at least every two hours" and get out of the car, stretch, and walk around. This increases blood flow to the lower body which helps prevent ...
Whether you're trying for a baby or not, it's natural to be full of questions during the early weeks of pregnancy. At 3 weeks pregnant, you're probably wondering whether you can get pregnancy symptoms before a missed period — or whether it's worth taking a pregnancy test yet.. The 3-week mark is an exciting and important time in your pregnancy because this is when fertilization and ...
Yes. You can choose to travel in the first trimester of pregnancy if you feel well and your pregnancy is healthy. There are, however, important considerations when planning a trip during your pregnancy. In most cases, you can safely travel in your first trimester of pregnancy. The risk for a miscarriage is higher in the early months of ...
Changes come even more quickly in the third trimester. You enter the third trimester about 28 weeks pregnant and end it with a newborn. This means that types of travel that are possible at 27 and 28 weeks pregnant may be inadvisable, or even prohibited, at 37 and 38 weeks pregnant. Select destinations and activities carefully
You should avoid travelling to an altitude above 3,658 metres (12,000 feet). However, if you have a high-risk pregnancy and/or are in the late stages of pregnancy, the highest altitude should be 2,500 metres (8,200 feet). If you have pregnancy-related complications, you should avoid unnecessary high-altitude exposure.
As long as you and your fetus are healthy, and you get your doctor's approval, it is generally considered safe to travel until you are 36 weeks pregnant. However, travelling during pregnancy is not recommended if you have certain pregnancy complications like preeclampsia, gestational diabetes, prelabour rupture of membranes, and the ...
At 3 weeks pregnant, you've officially conceived and are in month 1 of your pregnancy — though it will be a few weeks until you can confirm the news with a pregnancy test. This week, the tiny cluster of cells (soon to become your baby!) are rapidly growing. Meanwhile, surging hormone levels may trigger a heightened sense of smell, one of ...
Talk to your midwife if you have questions. Travel vaccinations. You'll need vaccinations before you travel to certain countries. There are some vaccinations you shouldn't have when you're pregnant, especially in the first 3 months, so always check before you book anything. Find out which travel vaccinations you might need. Travel ...
It can be mind-boggling—we get it. But, for the sake of calculation, and what you and your healthcare provider will consider as 1 and 2 weeks pregnant, you're not actually pregnant until week 3. But although at 1, 2, or 3 weeks pregnant you may not notice any of those very early signs of pregnancy, there's still a lot happening on the inside.
While some people feel no difference at all at this early stage, others may start to notice 3 weeks pregnant symptoms. The experience at 3 weeks pregnant can really vary, so don't fret if you don't feel anything out of the ordinary. However, if you feel nauseous and your breasts are sore, that's normal too. Everything changes quickly in ...
Weeks 3 to 4: If an egg has been fertilized, it becomes an embryo, which typically travels into the uterus and implants itself on the lining. This can take around a week or more, Dr. Belmonte said.
We tell our family this weekend and I can't wait! How are you doing? ... Pregnancy Week 3. Pregnancy Week 4. Pregnancy Week 5. Pregnancy Week 6. Pregnancy Week 7. Pregnancy Week 8. ... What Are Your Go-To Healthy Snacks? Things They Don't Tell You About: Mom Edition. Pregnancy Brain Moments? Let's Have a Laugh!
Any success stories when measuring behind in early ultrasound? I am 6 weeks 3 days but ob wasn't able to measure crown to rump or heartbeat because it was too small . However you could see heartbeat and yolk sac and embryo. I'm scared because with my previous pregnancy a heartbeat was measured at 5 weeks...
My baby is exactly 3 months old and seems to be regressing in sleep the last week, I'm wondering if anyone can shed any insight or experience :( I just feel so bad for her and I don't know how to help herShe had been sleeping through the night for about 8-10 hours for about two weeks.
The department's final rule, which will go into effect on July 1, 2024, will increase the standard salary level that helps define and delimit which salaried workers are entitled to overtime pay protections under the FLSA. ... Starting July 1, most salaried workers who earn less than $844 per week will become eligible for overtime pay under ...
Find the right pregnancy travel insurance - you can secure cover during your third trimester. However, very few providers will offer insurance after 30 weeks. ... Most insurers can cover you if ...
Florida's ban on abortions past six weeks of pregnancy takes effect this week, threatening the future of the state's clinics and abortion funds and forcing patients to travel hundreds of miles to ...
Around how much weight have you lost 3 weeks postpartum with one baby? I feel like I'm losing too fast but not sure. Gained 44 lbs during pregnancy. I lost 30 lbs so far. ... I've lost about 20-25 lbs, I have my final 8ish lbs to go till I'm at pre pregnancy weight. I probably gained about 28-30 lbs. it always differs day to day. If I ...