
Create Free Account or
- Acute Coronary Syndromes
- Anticoagulation Management
- Arrhythmias and Clinical EP
- Cardiac Surgery
- Cardio-Oncology
- Cardiovascular Care Team
- Congenital Heart Disease and Pediatric Cardiology
- COVID-19 Hub
- Diabetes and Cardiometabolic Disease
- Dyslipidemia
- Geriatric Cardiology
- Heart Failure and Cardiomyopathies
- Invasive Cardiovascular Angiography and Intervention
- Noninvasive Imaging
- Pericardial Disease
- Pulmonary Hypertension and Venous Thromboembolism
- Sports and Exercise Cardiology
- Stable Ischemic Heart Disease
- Valvular Heart Disease
- Vascular Medicine
- Clinical Updates & Discoveries
- Advocacy & Policy
- Perspectives & Analysis
- Meeting Coverage
- ACC Member Publications
- ACC Podcasts
- View All Cardiology Updates
- Earn Credit
- View the Education Catalog
- ACC Anywhere: The Cardiology Video Library
- CardioSource Plus for Institutions and Practices
- ECG Drill and Practice
- Heart Songs
- Nuclear Cardiology
- Online Courses
- Collaborative Maintenance Pathway (CMP)
- Understanding MOC
- Image and Slide Gallery
- Annual Scientific Session and Related Events
- Chapter Meetings
- Live Meetings
- Live Meetings - International
- Webinars - Live
- Webinars - OnDemand
- Certificates and Certifications
- ACC Accreditation Services
- ACC Quality Improvement for Institutions Program
- CardioSmart
- National Cardiovascular Data Registry (NCDR)
- Advocacy at the ACC
- Cardiology as a Career Path
- Cardiology Careers
- Cardiovascular Buyers Guide
- Clinical Solutions
- Clinician Well-Being Portal
- Diversity and Inclusion
- Infographics
- Innovation Program
- Mobile and Web Apps

Coding and Reimbursement
Coding corner: overview of 2024 coding changes impacting cardiology, acc 2024 medicare physician fee schedule final rule calculator now available, coding solutions for renal denervation, new category iii cpt code for remote programming of subcutaneous cardiac rhythm monitor systems, appropriate use of modifier 25.
- Audit Programs
- Fraud and Abuse
- Provider Enrollment
Decoding the CPT RUC
Documentation.
- Evaluation and Management
- Place of Service Codes
Ordering and Referring Overview
Jacc journals on acc.org.
- JACC: Advances
- JACC: Basic to Translational Science
- JACC: CardioOncology
- JACC: Cardiovascular Imaging
- JACC: Cardiovascular Interventions
- JACC: Case Reports
- JACC: Clinical Electrophysiology
- JACC: Heart Failure
- Current Members
- Campaign for the Future
- Become a Member
- Renew Your Membership
- Member Benefits and Resources
- Member Sections
- ACC Member Directory
- ACC Innovation Program
- Our Strategic Direction
- Our History
- Our Bylaws and Code of Ethics
- Leadership and Governance
- Annual Report
- Industry Relations
- Support the ACC
- Jobs at the ACC
- Press Releases
- Social Media
- Book Our Conference Center
Clinical Topics
- Chronic Angina
- Congenital Heart Disease and Pediatric Cardiology
- Diabetes and Cardiometabolic Disease
- Hypertriglyceridemia
- Invasive Cardiovascular Angiography and Intervention
- Pulmonary Hypertension and Venous Thromboembolism
Latest in Cardiology
Education and meetings.
- Online Learning Catalog
- Products and Resources
- Annual Scientific Session
Tools and Practice Support
- Quality Improvement for Institutions
- Accreditation Services
- Practice Solutions
Heart House
- 2400 N St. NW
- Washington , DC 20037
- Email: [email protected]
- Phone: 1-202-375-6000
- Toll Free: 1-800-253-4636
- Fax: 1-202-375-6842
- Media Center
- ACC.org Quick Start Guide
- Advertising & Sponsorship Policy
- Clinical Content Disclaimer
- Editorial Board
- Privacy Policy
- Registered User Agreement
- Terms of Service
- Cookie Policy
© 2024 American College of Cardiology Foundation. All rights reserved.
- (800) 516-5234
- [email protected]
- 134 N 4th St, Brooklyn, NY 11249
iRCM is an industry leader with innovative technology and an expert team. We are a complete Revenue Cycle Management solution that streamlines reimbursements and delivers remarkable results.
- 134 N 4Th Street Brooklyn, NY 11249
- 718-303-0763
- Terms and Conditions
- Solo/Private Practices
- ASC Billing
- SNF Billing

- View All Services
- View All Specialties
Cardiology CPT Codes – A Quick Reference for Billing and Coding

- Cardiology and Associated CPT Codes in Healthcare
- What is Cardiology in Healthcare?
- Specialized focus on heart and circulatory health.
- In-depth study and treatment of cardiovascular conditions.
- Wide array of medical procedures and diagnostic tests.
- What are Cardiology CPT Codes?
- Specific alphanumeric codes for cardiology procedures.
- Standardization within the Current Procedural Terminology.
- Facilitation of accurate billing and reimbursement in healthcare.
- Commonly Used CPT Codes in Cardiology
Going through the landscape of cardiology coding involves a thorough understanding of commonly used CPT codes for precise billing and reimbursement.

Here’s a brief overview of some key codes:
CPT Code 93010: This code involves the interpretation and reporting of electrocardiograms, providing crucial insights into cardiac health through diagnostic analysis.
CPT Code 93000: A routine electrocardiogram with a minimum of 12 leads, this code serves as a fundamental diagnostic tool for cardiac assessments.
CPT Code 93005: Specifically performed during initial preventive physical examinations, this routine electrocardiogram ensures comprehensive screening with a minimum of 12 leads.
CPT Code 93306: Designated for complete transthoracic echocardiography, this code aids in assessing congenital cardiac anomalies through detailed imaging of the heart.
CPT Code 93798: Includes physician’s cardiovascular stress test interpretation, vital for diagnosing and managing diseases through exercise-induced heart evaluations..
CPT Code 93325: Used for Doppler echocardiography, this code employs pulsed-wave and/or continuous-wave spectral display to provide detailed insights into cardiovascular function.
CPT Code 93296: CPT Code 93296: Focuses on programming implantable devices, ensuring optimal function through iterative adjustment by a qualified healthcare professional.
CPT Code 93015: Encompasses comprehensive cardiovascular stress tests using varied methods, supervised by a physician for a thorough assessment.
CPT Code 93018: Addresses cardiovascular stress tests with exclusive pharmacological stress, offering valuable diagnostic information under physician supervision.
CPT Code 93017 : Involves cardiovascular stress tests with exercise, continuous electrocardiographic monitoring, ensuring a comprehensive evaluation of cardiac function.
Understanding commonly used CPT codes for cardiology evaluation and treatment is crucial for precise billing and reimbursement in healthcare. From interpreting electrocardiograms to overseeing cardiovascular stress tests, these codes play a pivotal role in diagnosing and managing diseases, ensuring accurate evaluations under medical supervision.
- Utilizing Evaluation and Management (E/M) Codes for Cardiology Services
- Effect of Inaccurate CPT Codes in Cardiology Medical Practice
Accurate CPT coding is pivotal in cardiology, yet the implications of inaccuracies reverberate through a medical practice.
Diminished Compensation: Errors in CPT codes impact reimbursement, directly affecting the financial stability.
Scrutiny and Fines: Incorrect coding triggers investigations, leading to financial penalties and resource-intensive resolutions.
Reputation Erosion: Coding mistakes tarnish the practice’s standing with insurers, hampering future reimbursement prospects.
Legal Entanglements : Coding inaccuracies may invite legal issues, fines, and exclusion from government programs.
Non-Compliance Challenges: Coding errors pose compliance issues, attracting financial repercussions and penalties under regulations like HIPAA.
Ensuring precision in CPT coding is not just about financial integrity; it safeguards reputation, compliance, and, most importantly, the standard of patient care.
- Documentation and Coding Guidelines in Cardiology Practice

1.Procedure Clarity:
Clearly articulate details of the performed procedure, specifying the approach, anatomical site, and any notable findings.
2.Clinical Justification:
Document the clinical necessity of the procedure, explaining its vital contribution to the patient’s diagnosis and treatment.
3.Time-Driven Services:
For time-sensitive services like stress tests, record the total duration, covering both service provision and supervision/interpretation time
4.Comprehensive Patient Details:
Capture a thorough overview of the patient’s condition, ensuring all relevant information supports services rendered and justifies specific CPT codes.
5.Thorough Recordkeeping:
Implement meticulous recordkee ping for accurate documentation, creating a transparent foundation for ethical cardiology billing practices.
- Effective Strategies for Maximizing Cardiology Reimbursement
- Accurate coding and documentation
- Proper use of modifiers
- Appealing denied claims
- Negotiating favorable payer contracts
- Staying informed about reimbursement policies
- Final Thoughts
Recent Post

ICD-10 Code for Neck Pain – Essential for Proper Documentation

CO 197 Denial – Understanding and Avoiding Medicare Claim Issues

Chest Pain ICD-10 Code R07.9 – Your Complete Guide

ICD-10 E03.9 : Hypothyroidism – A Detailed Overview
Medical billing services, credentialing & enrollment, medical coding services, quality payment program, front office management, professional staffing solutions, get customized billing quote, our services.
- (718) 303-0763

Follow these four steps to code quickly and accurately, while reducing the need to count up data points.
KEITH W. MILLETTE, MD, FAAFP, RPh
Fam Pract Manag. 2021;28(4):21-26
Author disclosure: no relevant financial affiliations.

The new rules for coding evaluation and management (E/M) office visits are a big improvement but still a lot to digest. 1 , 2 To ease the transition, previous FPM articles have laid out the new American Medical Association/CPT medical decision making guide 3 and introduced doctor–friendly coding templates (see “ Countdown to the E/M Coding Changes ,” FPM , September/October 2020), explained how to quickly identify level 4 office visits (see “ Coding Level 4 Visits Using the New E/M Guidelines ,” FPM , January/February 2021), and applied the new guidelines to common visit types (see “ The 2021 Office Visit Coding Changes: Putting the Pieces Together ,” FPM , November/December 2020).
After several months of using the new coding rules, it has become clear that the most difficult chore of coding office visits now is assessing data to determine the level of medical decision making (MDM). Analyzing each note for data points can be time-consuming and sometimes confusing.
That being the case, it's important to understand when you can avoid using data for coding, and when you can't. I've developed a four-step process for this (see “ A step-by-step timesaver ”).
The goal of this article is to clarify the new coding rules and terminology and to explain this step-by-step approach to help clinicians code office visits more quickly, confidently, and correctly.
The new evaluation and management office visit coding rules have simplified many things but are still a lot to digest, especially when it comes to counting data.
There are different levels of data and different categories within each level, which can make using data to calculate the visit level time-consuming and confusing.
By calculating total time, and then moving on to assessing problems and prescription drug management, most visits can be optimally coded without dealing with data at all.
OFFICE VISIT CODING RULES AND TERMINOLOGY
To make full use of the step-by-step process, we have to first understand the new rules, as well as coding terminology. Here is a brief summary.
Medically appropriate . Physicians and other qualified health care professionals may now solely use either total time or MDM to determine the level of service of an office visit. That means the “history” and “physical exam” components are no longer needed for code selection, which simplifies things. But your patient note must still contain a “medically appropriate” history and physical. So continue to document what is needed for good medical care.
New patient . A new patient is a patient who has not been seen by you or one of your partners in the same medical specialty and the same group practice within the past three years.
Total time and prolonged services . Total time includes all the time you spend on a visit on the day of the encounter (before midnight). It includes your time before the visit reviewing the chart, your face-to-face time with the patient, and the time you spend after the visit finishing documentation, ordering or reviewing studies, refilling medications, making phone calls related to the visit, etc. It does not include your time spent performing separately billed services such as wellness visits or procedures. Total time visit level thresholds differ for new patients vs. established patients. (See the total times in “ The Rosetta Stone four-step template for coding office visits .”)
The prolonged services code comes into play when total time exceeds the limits set for level 5 visits by at least 15 minutes.
Medical decision making . MDM is made up of three components: problems, data, and risk. Each component has different levels, which correspond to levels of service (low/limited = level 3, moderate = level 4, and high/extensive = level 5). The highest level reached by at least two out of the three components determines the correct code for the level of service. MDM criteria is the same for new and established patients.
Problems addressed . This includes only the problems you address at that specific patient visit. It does not include all the patient's diagnoses and does not include problems that are exclusively managed by another clinician. Problems addressed are separated into low-complexity problems (level 3), moderate-complexity problems (level 4), and high-complexity problems (level 5). To code correctly, you need to know the coding value of the problems you address. It is helpful to think of problems in terms of levels of service (e.g., a sinus infection is usually a level 3 problem, and pneumonia or uncontrolled diabetes are usually level 4 problems).
The simplest way to summarize problems is this: Life-threatening problems are level 5; acute or chronic illnesses or injuries are level 3 or 4 depending on how many there are, how stable they are, and how complex they are; and if there's just one minor problem, it's level 2.
(For more specifics see “ What level of problem did I address? ”)
Risk . Risk is also separated into “low” (level 3), “moderate” (level 4), and “high” (level 5) categories.
Level 3 risk includes the use of over-the-counter (OTC) medications.
Level 4 risk includes the following:
Prescription drug management: starting, stopping, modifying, refilling, or deciding to continue a prescription medication (and documenting your thought process),
Social determinants of health that limit diagnosis or treatment (this is when patients' lack of finances, insurance, food, housing, etc., affects your ability to diagnose, manage, and care for them as you normally would).
Level 5 risk includes the following:
Decisions about hospitalization,
Decisions about emergency major surgery,
Drug therapy that requires intensive toxicity monitoring,
Decisions to not resuscitate or to de-escalate care because of poor prognosis.
Data analyzed . For purposes of MDM, data is characterized as “limited” (level 3 data), “moderate” (level 4 data), or “extensive” (level 5 data). But each level of data is further split into Categories 1, 2, and 3. This can make calculating data complicated, confusing, and time-consuming. Here are the data components and terms you need to know.
Category 1 data includes the following:
The ordering or reviewing of each unique test , i.e., a single lab test, panel, X-ray, electrocardiogram (ECG), or other study.
Ordering and reviewing the same lab test or study is worth one point, not two; a lab panel (e.g., complete blood count or comprehensive metabolic panel) is worth one point,
Reviewing a pertinent test or study done in the past at your own facility or another facility,
Reviewing prior external notes from each unique source, including records from a clinician in a different specialty or from a different group practice or facility as well as each separate health organization (e.g., reviewing three notes from the Mayo Clinic is worth one point, not three, but reviewing one note from Mayo and one from Johns Hopkins is worth a total of two points),
Using an independent historian, which means obtaining a history from someone other than the patient, such as a parent, spouse, or group home staff member. (This is included in Category 2 for level 3 data, but falls into Category 1 for level 4 and 5 data.)
Category 2 data includes the following:
Using an independent historian (for level 3 data only),
Independent interpretation of tests, which is your evaluation or reading of an X-ray, ECG, or other study (e.g., “I personally reviewed the X-ray and it shows …”) and can include your personal evaluation of a pertinent study done in the past at your or another facility. It does not include reviewing another clinician's written report only, and it does not include studies for which you are also billing separately for your reading.
Category 3 data includes the following:
Discussion of patient management or test interpretation with an external physician, other qualified health care professional, or appropriate source. An external physician or other qualified health care professional is someone who is not in your same group practice or specialty. Other appropriate sources could include, for example, consulting a patient's teacher about the patient's attention deficit hyperactivity disorder.
A STEP-BY-STEP TIMESAVER
The majority of office visits can be optimally coded by using time or by looking at what level of problems were addressed (see Steps 1 and 2 below) and whether a prescription medication was involved.
A level 3 problem can be coded as a level 3 visit if you address it with an OTC or prescription medication. A level 4 problem can be coded as a level 4 visit if you order prescription medication or perform any other type of prescription drug management (modifying, stopping, or deciding to continue a medication). Most level 2 and level 5 office visits are straightforward, and most level 5 visits will be coded by time. They will typically be visits in which you address multiple problems or complicated problems and the total time exceeds 40 minutes for established patients. This is much more common than seeing critically ill patients who may require admission, which is another level 5 scenario. The few remaining patient visits that have not already been coded require analyzing data (Steps 3 and 4). (See “ The Rosetta Stone four-step template for coding office visits .”)
Step 1: Total time . Think time first. If your total time spent on a visit appropriately credits you for level 3, 4, or 5 work, then document that time, code the visit, and be done with it. But if it does not, go to Step 2.
Step 2: “Problems plus.” Don't be afraid to move on from time-based coding if you believe you performed a higher level visit using MDM. Many visits can be coded with MDM just by answering these two questions: What was the highest-level problem you addressed during the office visit? And did you order, stop, modify, or decide to continue a prescription medication?
If you addressed a level 2 problem and your total time was less than 20 minutes (or less than 30 for a new patient), then code level 2.
If you addressed a level 3 problem, plus you recommended an OTC medication or performed prescription drug management, then code level 3.
If you addressed a level 4 problem, plus you performed prescription drug management, then code level 4.
Chronic disease management often qualifies as level 4 work. For documentation, think “P-S-R”: problem addressed, status of the problem (stable vs. unstable), and prescription drug management (Rx). This trio should make it clear to coders, insurance companies, and auditors that level 4 work was performed.
For instance, if a patient has controlled hypertension and diabetes and you document that you decided to continue the current doses of losartan and metformin, that's level 4 (two stable chronic illnesses plus prescription drug management). If you see a patient with even one unstable chronic illness and document prescription drug management to address it, that's also level 4.
For a level 5 problem, if you see a really sick patient and decide to admit or consider admission (and you document your thought process in your note), then code level 5.
By starting with total time and, if necessary, moving on to “problems plus,” you will probably be able to optimally code 90% of your office E/M visits. But on the rare occasions when you see a patient for level 4 or 5 problems for less than the required time and don't do any prescription drug management, you may have to proceed to Steps 3 and 4.
Step 3: Level 4 problem with simple data or social determinants of health concerns . Code level 4 if you saw a patient for a level 4 problem and did any of the following:
Personally interpret a study (e.g., X-ray),
Discuss management or a test with an external physician,
Modify your workup or treatment because of social determinants of health.
Step 4: Level 4 or 5 problem with complex data . If you saw a patient for a level 4 problem and still haven't been able to code the visit at this point, you have to tally Category 1 data points:
Review/order of each unique test equals one point each,
Review of external notes from each unique source equals one point each,
Use of an independent historian equals one point.
Once you reach three points, code it as level 4.
For a level 5 problem, if you see a really sick patient, order/interpret an X-ray or ECG, and review/order two lab tests, then code level 5.
Following these steps should allow you to quickly identify the optimal level to code most any E/M office visit (for pre-op visits, see “ Coding pre-ops template .”)
Here's a catchy rhyme to remember the basic outline of the steps:
To finish fast ,
code by time and problems first ,
and save data for last .
By mastering the new coding rules and terminology and applying this four-step approach, you can code office visits more quickly, accurately, and confidently — and then spend more time with your patients and less time at the computer.
CPT Evaluation and Management (E/M) Office or Other Outpatient and Prolonged Services Code and Guideline Changes . American Medical Association. Accessed June 10, 2021. https://www.ama-assn.org/system/files/2019-06/cpt-office-prolonged-svs-code-changes.pdf
E/M Office Visit Compendium 2021. American Medical Association; 2020.
Table 2 – CPT E/M office revisions level of medical decision making. American Medical Association. Accessed June 10, 2021. https://www.ama-assn.org/system/files/2019-06/cpt-revised-mdm-grid.pdf
Continue Reading

More in FPM
More in pubmed.
Copyright © 2021 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

Phone: (888) 454-4325
(888) 454-4325
- Coding Made Simple: A Breakdown of Cardiology CPT Codes
- Posted on September 14, 2023
- Leave a comment
Cardiology is a medical specialty that relies heavily on different diagnostic tests, imaging studies, and interventional procedures to assess and treat conditions related to the heart and circulatory system. Many CPT codes apply specifically to the types of services performed by cardiologists and cardiology practices. Properly using these cardiology CPT codes is crucial for appropriate reimbursement and to convey the complexity of care provided.
This blog post will overview the most frequently used CPT codes in cardiology. We’ll describe the codes with their application and any special billing tips or recent changes. Whether you are a cardiologist, work in a cardiology practice, or are responsible for cardiology medical billing and coding, understanding these key cardiology CPT codes is essential for your reimbursement and compliance.
Most Common Cardiology CPT Codes
Some of the most common cardiology CPT codes relate to electrocardiograms (EKGs), echocardiograms, cardiac catheterization, and stress testing. However, new codes are introduced over time with advancements in the field. Cardiology providers and medical coders must stay up-to-date on CPT codes and billing guidelines.
Electrocardiograms (EKGs) CPT Codes
93000 is one of the most commonly used codes in cardiology. It is used for routine EKG tracing and interpretation. This basic EKG code is used for routine annual exams, pre-operative clearance, and evaluating cardiac symptoms like chest pain, heart palpitations, dizziness, or syncope.
93005 is used for electrocardiogram tracing only, without interpretation and report. It allows separate billing for the EKG trace, which a cardiologist sometimes interprets later. The tracing-only code can be used when one provider performs the EKG trace recording, and another interprets it separately.
93010 is used when an interpretation is done from an already performed tracing. The interpretation and report code is used when a provider reviews and analyzes a tracing that was already completed. This often occurs when a cardiologist is consulted on an EKG done elsewhere.
93040 (rhythm ECG, one to three leads, with report) is used for enhanced rhythm EKGs that monitor cardiac rhythms over an extended time.
Echocardiogram CPT Codes
CPT code 93306 (Echocardiography, transthoracic) is the most common echocardiogram code for imaging the heart’s structure and function using ultrasound waves passed over the chest wall. CPT code 93306 is used for evaluating heart function, looking for valve disorders, assessing chamber size, calculating ejection fraction, and detecting abnormalities in heart structure.
93307 (Echocardiography, complete, without spectral Doppler) is for a full transthoracic echocardiogram without the Doppler assessment. 93308 (Echocardiography, limited, without spectral Doppler) code is used for focused or limited imaging of certain heart structures. 93307 and 93308 are often used to quickly assess known issues like post-surgery or post-MI evaluation of heart function.
Cardiac Catheterization
93452 (Left heart catheterization including imaging) involves catheterization of the left side of the heart, often coupled with angiography.
93453 (Combined right and left heart catheterization) code includes catheterization of both sides of the heart in the same procedure.
93456 (Left heart catheterization for congenital disabilities) is used for patients with congenital heart defects.
93458 (Left heart catheterization for acquired defects) is used for patients with acquired defects like coronary artery disease.
Stress Testing
93015 (Cardiovascular stress test using exercise and EKG monitoring) is the most common type of cardiac stress test. Exercise stress testing is commonly done to induce ischemia in patients with coronary artery disease and evaluate EKG changes.
93017 (Cardiovascular stress test with EKG monitoring and administration of the drug) is for pharmacologic stress testing. Pharmacologic stress testing is preferred for patients unable to exercise adequately on the treadmill.

Billing Tips and Modifiers
Modifiers are essential for delineating professional vs. technical components and bypassing bundling issues when performing multiple cardiac procedures—accurate use of modifiers results in better claim reimbursement.
Herein are some tips regarding the modifier’s usage in cardiology billing:
Electrocardiograms
- Modifier 59 can be added to cardiology CPT codes 93000 or 93010 when an EKG is performed in addition to an E/M service on the same day. This avoids bundled payment.
- Modifier 26 is used with 93005 when only the professional component of an EKG trace is being billed separately.
Echocardiograms
- Modifier 26 is added for professional component billing only.
- Modifier TC is only applied for technical component billing by the facility/equipment with an echocardiogram CPT code.
- Modifier 59 may be needed if a diagnostic Cath is bundled with a surgical intervention.
- Modifiers LC, LD, RC, and LD define vessel(s) imaged during angiography.
- Modifier 22 is used to indicate increased complexity for congenital disabilities.
- 93015 and 93017 need modifier 26 when only the professional component is billed.
- Modifier TC is used if only the facility billed the technical component.
- Modifier 59 may be required if a stress test is done with other cardiac procedures.
Recent Changes to Codes
Staying current with new and updated CPT codes is essential in cardiology to capture reimbursement for the latest procedures and technology improvements. Regular code updates from the AMA and CMS keep cardiology billing aligned with the rapid pace of advancement.
Code 93X34 was introduced for prolonged external ECG patch monitoring exceeding 48 hours. This new code reflects the extended EKG monitoring now possible with patch devices. January 2022 added codes for cardiac magnetic resonance imaging (MRI) with contrast – 75561, 75563, and 75564. This provides more specific coding for cardiac MRIs beyond the previous broad MRI codes. Code 93356 was created in 2022 for transesophageal echocardiography for congenital cardiac anomalies. This includes differentiation from the standard TEE code 93355. January 2022 introduced +93600 intracardiac echocardiography during therapeutic/diagnostic intervention. This reflects the increasing use of ICE during procedures like Ablation.
See Also: Mental Health Billing: A Complete Guide
Proper application of CPT codes is vital for cardiology medical billing and reimbursement. As cardiology is a fast-evolving medical specialty, new codes are introduced frequently to keep pace with technological advances. Some of the most common cardiology CPT codes relate to EKGs, echocardiography, cardiac catheterization, and stress testing. However, there are many specific codes for emerging techniques like cardiac MRI, CT angiography, intracardiac echocardiography, and newer interventional procedures. Accurate coding requires understanding what each code represents and when to apply the correct code.
Keeping up with cardiology CPT code changes, additions, billing tips, and modifier usage is essential but challenging. This is where the experienced medical billing and coding team at Precision Hub can help. Our team specializes in cardiology and is up-to-date on the latest coding protocols. We handle all aspects of cardiology medical billing. With Precision Hub as your cardiology medical billing partner, you can rest assured your practice is coding properly and optimizing revenue. Our team stays on top of updates related to cardiology CPT codes so you can focus on delivering excellent patient care. Contact us today to learn more about our medical billing and coding services.

CPT Codes for Urgent Care: Guidelines 2023
My name is Simon and I hold a PhD in Medical Sciences. I bring to Precision Hub my seven years of exposure. As a medical writer, I have contributed to industries as vast as medical devices & med-tech, pharmaceuticals, healthcare agencies, hospitals, health tech firms and healthcare communication agencies.
No comment yet, add your voice below!
Add a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Schedule a Demo
Monthly Collection <$5000 $5001 - $9999 $25000 - $49999 $50000 - $74999 $750000 - $99999 >100000
Submit application
- Billing , Coding
Cardiology Medical Coding Cheat Sheet: Common Mistakes and Pitfalls
Melanie Graham
Although treatment has advanced leaps and bounds in the last few decades, heart disease remains the leading cause of death for U.S. adults. And with more than 20 million U.S. adults facing coronary artery disease, cardiology remains one of the busiest and highest-paid specialties .
But high demand and top-tier salaries won’t matter much if your private cardiology practice has a problematic revenue cycle. Cardiology is a complex field with ever-changing treatments and procedures. That means keeping track of new cardiology medical billing guidelines and medical coding best practices, which can sometimes vary across payers. Even a solid claim scrubbing process may not catch every slip-up.
Fortunately, following a few crucial cardiology billing tips (like those outlined in the cheat sheet below) can help your practice reduce costly errors and ensure a healthy revenue cycle management (RCM) process .
Cardiology Billing Guidelines and Coding Cheat Sheet
Keeping track of cardiology CPT codes and billing best practices is far from easy. We’ve put together this short cheat sheet with a few basics for cardiology medical billing. You can download the full cheat sheet here .
Common Mistakes and Pitfalls in Cardiology Billing and Coding
Like many medical specialties, cardiology coding, claims and reimbursement can get complex. Below are some of the common cardiology billing challenges your team may encounter.
Not Checking Coverage Guidelines Before Procedures and Tests
One of the most common mistakes with cardiology billing is forgetting to check a patient’s specific coverage guidelines for a procedure or test. Missing this important step can pose problems for the patient and the practice. Reimbursement could be at stake, and patients may feel confused or frustrated when they receive a surprise bill for their care.
Beyond insurance eligibility , it’s also important for your team to check coverage guidelines before a cardiology procedure or test. You’ll need to make sure all prior authorizations, referrals or pre-certifications are in place before the scheduled procedure. Each payer will have specific guidelines, so understanding the intricacies of the patient’s plan is critical for a smooth claim filing process.
Not Coding for Comorbidities
Cardiology patients often face more than one diagnosis, also called comorbidity. Common heart disease comorbidities include diabetes, high blood pressure (hypertension) and COPD.
When it comes to cardiology billing and coding, it’s important to document these comorbidities to help ensure your practice gets reimbursed as much as possible. You can document diseases separately or use ICD-10-CM combination codes.
ICD-10-CM stands for the International Classification of Diseases, Tenth Edition, Clinical Modification . Like CPT codes, ICD-10-CM allows physicians to speak a common language for diagnoses.
When documenting different diagnoses, check the coding instructions and read the code descriptions carefully. In some cases, you may need a combination code. A combination code helps classify multiple diagnoses, a diagnosis with a complication, or a diagnosis with a secondary manifestation. For example, a patient whose heart failure was caused by hypertension.
Schedule a Risk-Free Medical Billing & Revenue Cycle Analysis Today!
Not adding the proper modifiers.
Cardiology codes often include modifiers at the end. Modifiers are two-digit codes that show you’ve somehow altered the service in the original five-digit CPT code.
For example, you may add modifier 25 to a patient visit where the clinician determined the patient needed a stress test at the end of the visit. Modifier 25 is for “significant and separate evaluation and management (E/M) on the same day as another procedure or service.” You would add “-25” to the end of the CPT code for the patient visit.
Not using modifiers properly could result in lost revenue for your practice. In the example above, forgetting the “25” modifier may mean you miss out on reimbursement for the patient visit. Instead, the payer may lump together the visit with the stress test procedure.
Other common cardiology modifiers include:
- 22 – Increased procedural services
- 51 – Multiple procedures done at the same time
- 52 – Reduced services
- 53 – Discontinued procedure
For more information on modifiers, download our Cardiology Billing Cheat Sheet .
Not Being Specific with Your Coding
Every cardiology condition has various options for diagnosis code. Coding mistakes often happen when you choose a code that isn’t specific enough for the diagnosis.
For example, the ICD code for unspecified systolic congestive heart failure (150.2) differs from the code for combined systolic and diastolic congestive heart failure (150.4).
Coding for the Symptoms and Not the Diagnosis
Often, cardiology coders submit symptom codes in addition to or instead of diagnosis codes. For the best possible reimbursement, only submit symptom codes if they are unrelated to the diagnosis. For example, if a patient is diagnosed with angina, you don’t need to submit a code for chest pain.
How to Prevent Cardiology Claim Denials
A claim rejection or denial will slow down your cardiology practice’s RCM process, which ultimately means a longer time to get paid. Avoiding these issues on the front end of your RCM can make a big difference to your bottom line.
Here are a few tips on how to prevent cardiology claim denials.
Know Payers’ Billing Guidelines and Set Up Rules for Unique Edits
Every payer is different, so you must understand the billing and coding intricacies for each. Understanding the unique guidelines can help avoid denials and delays in payments.
If you have a payer with a unique billing protocol or code edit that your team is repeatedly entering, find an RCM tool that can automate this process. With the Gentem platform , for example, you can work with our team to create edits for specific claims or payers, which saves time and reduces the chance of manual error.
Keep Thorough Documentation
It’s always a good idea to keep detailed documentation for each patient, including symptoms, diagnoses, comorbidities, tests and treatments. Make sure you keep track of all patient encounters and avoid waiting too long between the date of service (DOS) and entering charges (also called charge lag).
Having thorough notes will help your practice with pre-authorizations or certifications, as some payers require comprehensive patient notes. The notes will also help your practice if needs to appeal any claim rejections or denials.
Modernize Your Billing and RCM
Learn how Gentem’s technology can save your organization time and increase revenue. Schedule a demo with our team today.
Create an Accurate Eligibility Check Routine
Verifying a patient’s insurance eligibility is an essential first step in the RCM and claim submission process. Your claim may not get very far if a patient doesn’t have an active insurance plan.
It’s a good idea to set up a process where you can automatically check upcoming appointments. For example, the workflow could check eligibility for the following week’s schedule, giving your team plenty of time to reach out to patients if there are insurance issues. A tool with batch eligibility check features can save your team time, too.

Take Steps to Avoid Human Error
With so many twists and turns to cardiology billing, it comes as no surprise that simple human error is often the biggest hurdle to a clean claim process. With that in mind, make sure you:
- Work with a billing and coding team that has experience in cardiology
- Audit your RCM and billing process often to find patterns and errors that may be affecting your cash flow
- Set up a thorough review and claim scrubbing process
- Partner with a smart RCM software solution that provides automated workflows to reduce the likelihood of human error
Get additional best practices in our full Cardiology Billing Cheat Sheet.
Cardiology CPT Codes
The CPT codes for cardiovascular procedures typically range from 92920 to 93793. Some common cardiology CPT codes include:
- 93010: Electrocardiogram (ECG or EKG), routine with at least 12 leads
- 93798: Physician services for outpatient cardiac rehabilitation; with continuous ECG monitoring (per session)
- 93015: Cardiovascular stress test using treadmill or bicycle exercise, continuous ECG monitoring with supervision, interpretation and report
- 93306: Echocardiogram (Echo) where the provider uses a transducer to get a 2D picture of the heart through the chest wall (transthoracic).
Get more cardiology CPT code ranges in our Cardiology Billing Cheat Sheet .
Find a Partner Who Can Modernize Your Cardiology RCM and Billing Process
Efficient and accurate coding is one piece of healthy revenue cycle management and crucial to the success of your cardiology practice. Billing and coding mistakes can get expensive and ultimately affect the viability of your practice.
Keeping up with CPT and ICD code changes is helpful, as well as having experienced and knowledgeable coding staff. Efficient and effective billing processes can also go a long way in helping your bottom line.
If you’re finding it difficult to get full reimbursements for your cardiology care, Gentem’s AI-powered revenue cycle management (RCM) platform can help you improve your billing process and submit cleaner claims. We’ve helped cardiology practices increase collections, allowing them to expand staff and care for more patients.
Book a demo today to learn more about our powerful RCM and billing tools .

WATCH: Revenue Cycle Tips for Staying Independent
Many physicians are leaving private practice due to rising costs, lower reimbursement rates and staffing shortages. But staying independent is possible with a healthy revenue cycle.
Learn how to run a successful private practice with tips from this 20-minute webinar session.
5 Must-Know Metrics To Build A Thriving Medical Practice
With this free guide, you’ll learn the key metrics that inform your practice’s financial performance and how best to optimize them to support practice growth.
Subscribe To Our Newsletter
Related articles.

What Is Healthcare Revenue Cycle Management (RCM)?

Revenue Cycle KPI Glossary: Definitions and Benchmarks You Should Know

7 Ways to Prevent Medicaid Claim Denials
Eliminate your medical billing headaches today..
Guide to Billing, Coding, and Reimbursement for Interventional Cardiology
Learn the Basics of Getting Reimbursed for Your Services
Current Procedural Terminology, or CPT, is the coding system for physician-performed procedures. The code set is maintained by the CPT Editorial Panel. This 21-member panel is authorized to revise, update, or modify CPT. The Panel meets three times a year to review Code Change Applications. Stay abreast of new and revised CPT codes through the CPT Editorial Panel Summary of Panel Actions released after every meeting.
Evaluation and management CPT codes fall under different categories based on place of service. There are codes for office visits, hospital visits, nursing facility visits, home or residence visits, and emergency room visits. All visit types follow the same basic guidelines and require history, an examination, and medical decision-making. A medically appropriate history and examination must be documented, but specific components are no longer required for coding purposes. Medically appropriate is determined by the provider. The level of service is determined by either medical decision-making or time.
Medical Decision-Making: The three components of medical decision-making are the number and complexity of problems addressed, assessing and reviewing data, and risk. Two out of three must meet the level of service to bill that level.
Time: Any visit can be documented based on the total time spent on the date of the encounter. Time can include activities both before and after the actual visit as long as they are performed by the physician on the date of the encounter. Time spent must be documented in the chart note in order to bill based on time. Time requirements are listed in the CPT book under the code descriptions.
For more detailed information on determining the correct level of service, see SCAI’s educational videos:
2021 Office Visit Coding Changes
Evaluation and Management: 2023 Changes to Non-Office Visit Codes
The catheterization codes have lots of guidelines that can be confusing. Use these tip sheets to understand what guidelines apply to which codes.
General Coding Guidelines for Catheterizations
General Coding Guidelines for Congenital Catheterizations
The PCI codes have lots of guidelines that can be confusing. Use this tip sheet to understand what guidelines apply to which codes.
General Coding Guidelines for PCI
Use this tool to select the appropriate PCI CPT codes and modifiers.
PCI Selection Tool
ICD-10-CM codes are used to document the diagnosis for which the patient was treated. Diagnosis codes establish medical necessity in claims processing and provide key information for risk adjustment. Always select the most specific diagnosis code available that most appropriately represents the patient's condition. Avoid unspecified codes whenever possible.
ICD-10-CM Browser Tool
Moderate sedation is separately reimbursable by accurately and appropriately reporting the moderate sedation codes (99152, 99153) that went into effect on January 1, 2017. The physician's role is commonly that of an “administrator" or supervisor directing another practitioner, such as an RN. The physician doesn’t have to administer the moderate sedation drug(s); the physician can supervise the administration of the moderate sedation drug(s), and the physician is still considered to be performing the service.
Coding Q&A—Moderate Sedation with Cardiac Catheterization
A modifier is two digits appended to a CPT code that provides additional information that can be used for payment or tracking purposes. Modifiers also enable healthcare professionals to respond effectively to payment policy requirements. For accurate reimbursement, be sure you understand how to use payment modifiers. Always review payer policy to be sure of what the payer requires.
Using Modifiers for Reimbursement
The AMA/Specialty Society RVS Update Committee (or “RUC”) makes annual recommendations to the Centers for Medicare & Medicaid Services (or “CMS”) on the relative value units (or “RVUs”) to be assigned to new, revised and existing CPT codes. This 32-member panel represents the entire medical profession, with 28 seats appointed by national medical specialty society organizations and three appointed by the AMA. The RUC process also includes specialty society representatives from each of the approximately 125 specialty societies seated in the AMA House of Delegates.
Medicare is a federal insurance program that provides benefits for beneficiaries age 65 or older and for those with certain disabilities, end-stage renal disease (ESRD), and amyotrophic lateral sclerosis (ALS).
Medicare has four parts:
- Part A or hospital insurance, which covers inpatient and post-acute care services. Part A is paid by payroll taxes and has no premium, but beneficiaries pay a deductible for hospitalizations.
- Part B covers physician services and other out-patient ancillary services. Enrollment is voluntary and requires a monthly premium. Beneficiaries must also pay a yearly deductible and twenty percent co-insurance for all services.
- Part C is also known as Medicare Advantage, where private payers manage Part A and B benefits. Enrollment is voluntary and may require a monthly premium in excess of the Part B premium. Additional benefits, such as dentistry, may be included, and many services have a copay rather than co-insurance.
- Part D is prescription drug coverage.
Understanding the Basics of Medicare
To become a Medicare provider, you must enroll. The easiest way to enroll is by using the online enrollment system, PECOS. Enrollment is required for all types of Medicare participation.
Medicare Enrollment for Providers and Suppliers
To be a participating provider in the Medicare program, you must agree to accept assignment. That means you accept the Medicare fee schedule amount as payment in full and will file a claim for the beneficiary. In return, you will be paid at the full fee schedule rate and receive payments directly from Medicare.
Another option is to be a non-participating provider. Being non-PAR gives you the right to bill the patient up to 115% of the limiting charge. However, you must collect the entire balance from the patient because Medicare will send the payment to the patient. In addition, if you decide to accept assignment on a claim to receive direct payment, Medicare will only reimburse 95% of the physician fee schedule rate.
Opt Out: Physicians can choose to opt out of Medicare participation. This is the only option that allows the physician to bill the patient in full for services rendered. The physician must sign an affidavit on the PECOS site and sign a contract with the patient to provide services on a cash basis. The patient and the provider cannot seek reimbursement from Medicare. Opt-out lasts for two years.
Opt-Out Affidavit
The only time a PAR or nonPAR provider can bill the patient for services is when the services are not covered by the Medicare program. To do so, the provider must give the patient an advanced beneficiary notice prior to the service being rendered. The notice must be specific to the service being rendered and clearly state why Medicare will not cover the service. A blanket ABN is not acceptable. The patient then has the choice to refuse or pay for the service.
ABN Instructions
The Medicare Benefit Policy Manual provides detailed information on Medicare payment policy and can be found on the CMS website.
Medicare Benefit Policy Manual
The Medicare Claims Processing Manual provides more specific details about claims submission and payment and can be found on the CMS website.
Medicare Claims Processing Manual
The Centers for Medicare and Medicaid Services or CMS is in charge of managing the Medicare program, but they contract out the claims processing operations to private insurers. There are 6 Medicare Administrative Contractors, or MACs, each responsible for a different region of the country. The MACs are responsible for all claims processing and payment. MACs can also make their own policies known as 'local coverage decisions'. Refer to your MAC’s website for the most up-to-date information.
Who are the MACS
Medicare Administrative Contractors by State
Medicare does not require prior authorization. Instead, CMS has pre- and post-payment audits to ensure claims are being billed appropriately. A Comprehensive Error Rate Testing (CERT) audit is done to review for improper payment. CMS will request documentation about a billed service. The Targeted Probe and Educate program (TPE) assists specific providers with high rejection rates or unusual billing practices in correcting those errors.
Medicare Claim Review Programs
Comprehensive Error Rate Testing (CERT)
Targeted Probe and Educate Program
Anyone knowingly submitting false claims to the government under Medicare can trigger the False Claims Act and be is liable for treble damages for each claim. The False Claims Act applies to the Medicare program and anyone knowingly submitting claims for services not provided. The act allows for whistleblowers to bring cases to the government.
Fraud and Abuse Laws
Medicare Fraud & Abuse: Prevent, Detect, Report
The False Claims Act
Section 1877 of the Social Security Act prohibits referrals to healthcare entities where the physician (or their immediate family) has a financial interest in services that may be paid by Medicare. Exceptions exist, so it is important for physicians to discuss any financial arrangements with a healthcare attorney. Penalties include a $15,000 per service civil penalty as well as claims denial.
Limitation on Certain Physician Referrals—Section 1877
CMS is statutorily required to keep the Medicare Physician Fee Schedule budget neutral under MACRA. All increases until 2026 are to come from MIPS. Therefore, any increases to some codes must be paid for by decreases to other codes. For example, increases made to the Evaluation and Management codes reduced procedure reimbursement.
Every year, CMS creates the conversion factor, which determines the payment rate for the fee schedule for that year. Multiply the RVU for the procedure by the conversion factor to determine the payment rate for that code for that year.
National Coverage Determinations (NCDs) are payment policies established by CMS that apply nationally to all Medicare Administrative Carriers (MACs).
National Coverage NCD Report Results
Local Coverage Determinations are payment policies that apply specifically to one particular MAC or jurisdiction. Local Coverage Articles (LCAs) include additional information, such as applicable CPT and diagnosis codes.
Local Coverage Determinations
The National Correct Coding Initiative (NCCI) is a program developed by the Center for Medicare and Medicaid Services (CMS) to ensure that CPT codes are used correctly when more than one service is provided on the same day. There are two types of edits: procedure to procedure (PTP) and medically unlikely (MUE) edits. PTP edits indicate when two codes cannot be billed together on the same day. MUE edits indicate the number of units that can be billed on the same day. NCCI edit changes are released quarterly. NCCI edits are specific to Medicare and Medicaid, but most payers either follow NCCI edits or have their own similar edit system.
Understanding NCCI Edits
MIPS is a quality-based payment program with four components: quality, improvement activities, promoting interoperability, and cost measures. All physicians enrolled in the Medicare program are required to participate in MIPS if they have been a participating provider for over a year and exceed the low volume threshold. Participation is important because it affects your Medicare reimbursement. Not participating can result in up to a 9% payment penalty applied to your Medicare reimbursement two years after the reporting year. By participating, you can share in up to a 9% payment bonus. Even if you leave your current practice, the bonus or penalty for that payment year will follow the physician.
Quality Payment Program Resource Library
MIPS Value Pathways What Does MIPS Participation Mean for Your Practice
An Alternative Payment Model is a value-based care model that gives added incentive payments to provide high-quality and cost-efficient care. APMs can apply to a specific clinical condition, a care episode, or a population. APMs are part of CMS’ Quality Payment Program (QPP).
APMs Overview
The inpatient-only list lists procedures published in the Outpatient Prospective Payment System (OPPS) final rule. The list is updated yearly. Medicare will not bill any procedure on the list unless billed as an in-patient service.
Changes to the List
In 2022, the Centers for Medicare and Medicaid Services (CMS) reversed course on a previous policy to remove 298 codes from the in-patient-only (IPO) list. In the 2022 Outpatient Prospective Payment System final rule released in November 2021, CMS stated that they would be reinstating the codes to the list and they would not be moving forward with the stages removed of additional codes as previously indicated. CMS also established a new policy for removing codes from the list in the future.
The list will be reviewed annually as a part of the rule-making process, and a procedure must meet at least one of the following criteria to be considered for removal.
- Most out-patient departments are equipped to provide the service or procedure to the Medicare population.
- The simplest service or procedure described by the code may be performed in most outpatient departments.
- The service or procedure is related to CMS codes already removed from the In-patient Only List.
- CMS determines that the service or procedure is being performed in numerous hospitals on an outpatient basis.
- CMS determines that the service or procedure can be appropriately and safely performed in an ambulatory surgical center and is specified as a covered ambulatory surgical procedure, or CMS has proposed to specify it as a covered ambulatory surgical procedure.
To find the full list, you need to download the Addenda of the final rule.
How Do I Bill for Services on the IPO List?
Codes on the in-patient-only list are not subject to the two-midnight rule, but the patient must be admitted as an in-patient. If the procedure is done in an out-patient setting, the service can be billed as an in-patient if the service is provided on the date of an in-patient admission, provided within three days of an in-patient admission, or deemed related to the in-patient admission.
Does the List Only Apply to Medicare Patients?
No. Many payers, especially Medicaid, follow CMS policies. If the payer follows the IPO list, an in-patient authorization may be required. The hospital should also be aware that the status of the procedure is in-patient.
The Inpatient Only List: What You Need to Know
Documentation is essential for patient care and reimbursement. Each patient encounter should be documented completely and accurately.
Documentation Matters Toolkit
Medicare defines accountable care organizations as “groups of doctors, hospitals, and other health care providers, who come together voluntarily to give coordinated, high-quality care to the Medicare patients they serve.” Many large group practices and hospitals participate in ACOs. Even if specialists are omitted, it is important to understand how participation impacts the organization as a whole.
Accountable Care Organizations (ACOs): General Information
Accountable Care Organizations: Understanding the New Frontier of Physician Payment—Webinar
Medicaid provides health coverage to millions of Americans, including eligible low-income adults, children, pregnant women, elderly adults, and people with disabilities. States administer Medicaid according to federal requirements. The program is funded jointly by states and the federal government. Check with your state for specific programs and requirements.
Medicare Advantage
Medicare Part C or Medicare Advantage is the other program that pays for physician services. Beneficiaries choose to enroll in a plan run by a private insurer. Be aware that these plans can have the same requirements as private insurance, such as prior authorizations and referrals, so be sure to check the plan’s policies. Medicare Advantage plans must offer the same benefits as Medicare but can also include additional benefits. Medicare Advantage plans pay Medicare fee schedule rates.
Reimbursement
Most insurance companies require credentialing for a physician to become a part of their provider network. Most group practices and hospitals will have existing contracts already negotiated. But, if you are starting a private practice, you will need to review the contracts and weigh the costs and benefits of participating. Review fee schedules, billing requirements, and coverage policies to determine if participation makes sense.
In vs. Out of Network : If you decide to contract with an insurance company, you will be considered an in-network provider. That means plan members will be able to locate you in their directory, and you must accept the negotiated contract rate set by the insurance company and abide by the plan’s coverage guidelines. If you decide not to contract with the insurance company, you remain out-of-network. As an out-of-network provider, the patient remains responsible for the full billed amount, and payment from the insurance company may be made directly to the patient.
Insurance plans have different levels of benefits and coverage requirements. A health maintenance organization (HMO) is more restrictive, requiring the patient to see only in-network providers and requiring referrals for specialist care. A preferred provider organization (PPO) allows the patient more freedom, usually offering both in- and out-of-network benefits and allowing the patient to see any provider within the network without a referral.
Most insurance plans require some type of prior authorization or precertification. What services require prior authorization are plan-specific and usually addressed in the plan’s benefit manual. Services that require prior authorization must be reviewed by the insurance company prior to the service being rendered. Failure to obtain prior authorization results in zero payment for the service.
When a service is denied, either through prior auth or after claim submission, most insurance companies have a mechanism to appeal the decision. Check policy manuals for the appeals process. It usually includes up to three levels of appeal.
Each insurance company has its own policy regarding the use of telehealth. Be sure to review the policy for the originating site location (i.e., may the patient be in their home), the requirement for synchronous audio and visual communication, and which services are allowed.
The No Surprises Act went into effect on January 1, 2022, despite litigation in multiple states. In Texas, a federal judge ruled in favor of the Texas Medical Association’s case regarding the appropriate out-of-network rate for arbitration. The Department of Health and Human Services (HHS) is moving forward with updating guidance on the arbitration process to meet the requirements of the court’s decision.
What Does it Mean for My Practice?
Overall, the No Surprises Act applies to out-of-network providers practicing in in-network facilities. Therefore, if your practice participates in the same health plans as your facility, the act does not apply to you. However, the second interim final rule included a provision that applies to all providers in all settings. A good faith estimate must be given to all self-pay patients.
Good Faith Estimate
The good faith estimate (GFE) must be given to all uninsured and self-pay patients (who elect not to use insurance for services). The estimate must also be provided for all other providers involved in the procedure. So, the interventional cardiologist is also required to request an estimate from the facility and any other treating providers.
A notice of the availability of a good faith estimate should be posted both in the office and online in accessible formats for all patients. Uninsured patients should also be told verbally of the availability of the GFE, but the estimate must be provided in writing.
The GFE must be given to the patient no later than three business days after an appointment is scheduled if the appointment is more than ten days out. If an appointment is scheduled between three and ten days out, the GFE must be given no later than one business day after an appointment is scheduled. When requested without an appointment, the response should be no more than three business days after the request is made. If changes to the expected services occur, a new GFE must be provided no later than one business day before services are rendered.
The Written Document
The written GFE requires the following components and CMS has provided a template.
- Patient name and date of birth
- A clear description of service and date scheduled (if applicable)
- List of all items and services (including those to be provided by co-providers)
- CPT code, diagnosis code, and charge per item of service
- Name, NPI, and TIN of all service providers and the state where the services will be rendered
- List of items from other providers that will require separate scheduling
- Disclaimer that separate GFEs will be issued upon request for services listed in number six and that items in number four will be provided in those separate GFEs
- Disclaimer that there may be other services required that must be scheduled separately during treatment and are not included in the GFE
- Disclaimer that this is only an estimate and actual services, and charges may differ
- Disclaimer informing the patient of their rights to a patient-provider dispute resolution process if actual billed charges are substantially above the estimate, as well as where to find information on how to start the dispute process
- Disclaimer that GFE is not a contract, and the patient is not required to obtain services from the provider
Patient-Provider Resolution Process
If billed charges exceed the GFE by $400, the patient may initiate a dispute resolution process. The patient has 120 days from receipt of the bill to initiate the dispute process with HHS.
Good Faith Estimate for Patients with Insurance The Act also requires a good faith estimate to be provided for patients with insurance, but this provision has been deferred to future rule-making. Additional information will be provided as it becomes available.
Out of Network Provisions The following provisions only apply to out-of-network providers performing services in participating facilities for patients with commercial healthcare plans:
- Cannot balance bill the patient for emergency services
- Cannot balance bill the patient for non-emergency services performed in a participating facility unless requirements for notice and consent are met
- Must disclose protections against balance billing
- Ensure continuity of care when provider ends contract with payor
These provisions do not apply to Medicare, Medicaid, Indian Health Services, Veterans Affairs, or Tricare beneficiaries.
Relative Value Units (RVUs) were established as a means to value services based on the resources required. RVUs are established for the following three categories of resources:
Physician Work: The physician’s individual effort in providing a service, which includes time, technical difficulty of the procedure, severity of patient’s condition, and the physical and mental effort required to provide the service.
Practice Expense: There are direct and indirect practice resources involved in furnishing each service. Direct expense categories include clinical labor, medical supplies, and medical equipment. Indirect expenses include physician practice overhead and all other expenses.
Professional Liability Insurance: Insurance to protect a physician against professional liability.
When a physician signs an employment agreement with a hospital, the physician agrees to re-assigning all payment for services rendered to the hospital, so an employed physician may be unaware of RVUs. However. RVUs are also used as a means of tracking productivity in employment agreements.
Information provided here by the Society for Cardiovascular Angiography and Interventions (SCAI) reflects a consensus of informed opinion regarding proper use of CPT codes. These comments and opinions are based on limited knowledge of the medical and factual circumstances of an individual case and should be used for general purposes only. These materials may not be copied or disseminated without the express written consent of SCAI.
Neither SCAI nor its employees or representatives are qualified to make clinical judgments or to render legal advice and counsel regarding the proper code for any given procedure, nor the consequences of use of any code including use of codes for purposes of reimbursement. For legal advice, recipients of such information should consult their own counsel.
CPT © 2024 American Medical Association. All rights reserved. CPT® is a registered trademark of the American Medical Association
© Society for Cardiovascular Angiography & Interventions
SCAI ® is a registered trademark of the Society for Cardiovascular Angiography & Interventions.
All content found on the Society for Cardiovascular Angiography & Interventions website (www.scai.org) including text, images, audio, video, or other formats is created for informational purposes only. Links to other content are to be taken at your own risk. SCAI is not responsible for the content or claims of external websites.
Get in touch
Follow us on social media.

- Patient line (727) 771-1300
- Questions (727) 499-0355

Patient line
Questions about our services
Update on Cardiology Medical Billing Codes
- April 8, 2022
PracticeForces Blog

Cardiology medical billing is undoubtedly one of the most complex areas of medical billing. Regular changes to fundamental procedure rules, difficult contractual adjustments and codes, and cardiology’s very nature make cardiology medical billing a complex science to master. It would explain why most cardiology providers prefer to outsource cardiology medical billing.
However, if you own a cardiology practice or work as an office manager in a cardiology practice, it’s essential that you understand cardiology medical billing guidelines. We shared six tips on boosting cardiology medical billing revenues and improving patient satisfaction in a previous blog. Today let’s talk about the cardiology medical billing codes to help your cardiology practice avoid underquoting and misquoting medical conditions.
Here is what you need to know to ensure cardiology medical billing and coding accuracy in your practice.
Codes for Continuous Cardiac Monitoring and Detection
Codes 93241-93248 have been added to code and document the advances in the field of continuous cardiac monitoring and detection. Codes 93241, 93242, 93243, and 93244 are for external electrocardiographic recording for more than 48 hours up to seven days. The codes 93245, 93246, 93247, and 93248 are for external electrocardiographic recording for more than seven days up to fifteen days. These codes were introduced for dates of service on or after Jan 1, 2021. Category 3 codes 0295T, 0296T, 0297T, and 0298T have been deleted.
Codes for Congenital Cardiac Anomalies
New codes were introduced in 2021 for congenital cardiac anomalies. These are:
- 33741 for transcatheter atrial septostomy.
- 33745 for TIS creation by stent placement
- 33746 for each additional intracardiac shunt location.
- 33995 for insertion of ventricular assist device.
- 33997 for removal of right heart ventricle assist device.
- 33992 for removal of left heart ventricle assist device.
- 33990 for arterial-only access.
- 33991 for both arterial and venous access.
Cardiology Medical Billing for total time spent on patient encounters or MDM
From 2021, codes 99202 to 99215 were introduced to define time as the total time spent on patient encounters (pre, during, and post-meeting time) rather than just the face-to-face interaction. As per the new guidelines, the total billable time on the date of the visit includes:
- Time spent preparing for the patient visit (including review of the test results).
- Time spent to obtain and review medical history.
- Time spent performing a medical examination.
- Time spent in counseling and informing the patient or the patient’s family.
- Time spent ordering medication, tests, and procedures.
- Coordinating with other health care providers.
- Information capture in the patient’s HER.
The codes to be used will be determined by the total time spent. For instance, for the time slot of 15 to 29 minutes, the code is 99202. For 10-19 minutes, the code is 99212.
As a coding example, if a patient visits the cardiologist’s office for a follow-up visit and the doctor spends five minutes reviewing the lab results and another nine minutes on the vital signs, the code 99212 will be used to bill this patient encounter.
Alternatively, the cardiology medical billing can be done basis the level of medical decision making (MDM). The criterion for MDM includes
(a) the number and complexity of problems addressed during the encounter,
(b) the complexity of data to be reviewed, and
(c) the risk of complications and or mortality of patient management. The E/M codes include four types of MDM: straightforward (code (99202; time 15-29 mins.), low complexity (99203, time 30-44 mins), moderate complexity (99204; time 45-59 mins), and high complexity (99205; time 60-74 mins).
As revenue cycle management specialists, we understand the challenges of cardiology medical billing and coding. We have many cardiology practices whom we work have been working with for years. Our clients focus on delivering the best patient care while we take care of the documentation standards and cardiology medical billing to the highest degree of specificity.
Contact us to know how we can help you grow revenues and improve the patient experience with your cardiology practice.

Parul Garg, CEO and co-founder of PracticeForces, has significantly contributed to the growth of over 1,000 U.S. medical practices through her expertise in medical billing and coding since the company’s inception in 2003. With a background in Computer Science and an MBA in Human Resources, her leadership and AAPC-certified coding skills have been pivotal in managing the company’s operations effectively.
Related Posts
Onshore vs. offshore medical billing – which is better.
When you decide to outsource medical billing, the two most popular options are – onshore and offshore medical billing. As the name suggests, ‘onshore’ refers
Enhancing RCM for Multispecialty Practices: A Compilation
This section provides a concise overview of Revenue Cycle Management (RCM) and its vital role in healthcare practices, particularly in multispecialty settings. Multispecialty practices face
Ready to improve your cash flow without sacrificing patient care?
Mon-fri 8:30am-5:30pm.
Patient Line
*Women Owned Business
2410 Northside Dr, Clearwater, FL 33761
Get Directions
Quick Links

Do you want to streamline your reimbursements?
Subscribe for actionable tips and insights to grow your medical practice >
- 99233 CPT Code, Level 3 Hospital Followup Note –Dummies Guide 2017-2018
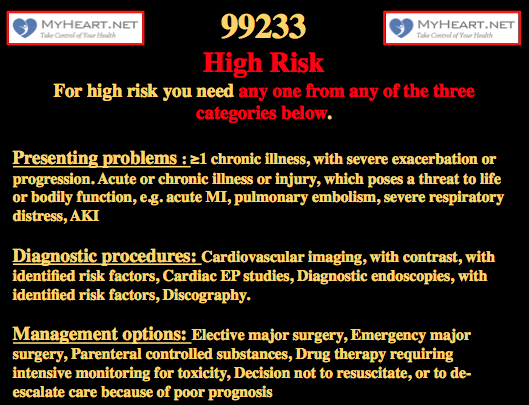
99233 CPT code 7 high risk
A 99233 CPT code explanation, 99223 examples, 99233 example note, 99233 RVU amount, 99233 wRVU / work RVU amount and a 99233 template for EMR.
What is cpt code 99233.
CPT code 99233 is assigned to a level 3 hospital subsequent care (follow up) note. 99233 is the highest level of non-critical care daily progress note. When it comes to 99233 documentation is critical, however understanding of the documentation required is even more critical. WorK RVU (wRVU) for cpt code 99233 is of course higher than that for 99232.
How many work RVU (wRVU) are given for a 99233?
A 99233 CPT code is associated with 2.0 work RVU’s also known as wRVU.
A 99223 = 2 wRVU
In general when is a 99223 code appropriate?
When it comes to coding, documentation is key and you would be surprised to see just how little writing is required to ensure all the key criteria. My personal rule however is that common sense should prevail as opposed to trying to game a system with documentation.
If a patient is improving or remains stable CPT code 99233 is probably not appropriate. Many times, rounds are made on patients where it is essentially a continue meds, continue monitoring, improving basis, essentially a courtesy visit. These are not meant to be 99233’s.
Often, for example the day after a patient is admitted, many management decisions continue to evolve and treatment changes are made. For example blood pressure control or heart failure would require specific medication adjustment and tests that need to be reviewed. Development of renal failure for example that would require holding meds, getting tests, following them and potentially arranging consultation and discussing with specialists. This would be a classic 99233 CPT code type situation. In general, as the patient improves to a state where they are improved and awaiting final stabilization for discharge, CPT code 99232 rather than 99233 would be appropriate.
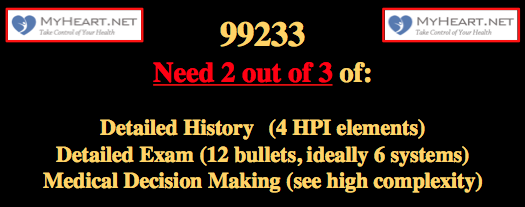
Example of hospital days where CPT code 99233 may be appropriate as long as the documentation is correct
Admission – Patient with shortness of breath and chest pain, comorbidities present, diagnosed with congestive heart failure and known ischemic cardiomyopathy treated medically, IV meds given, complexity is high.
CPT code 99223
Day 2 – Patient improved, meds changed to PO, home meds restarted, no invasive tests planned, continuing to monitor.
CPT code 99232
Day 3 – Kidney function worsens, meds held and changed appropriately, concern for cardiac output being low, nephrology consulted, situation worsened from prior day.
CPT code 99233
Day 4 – Echo reviewed, cardiac function worse than thought, thinking about right heart cath, dobutamine started on floor, IV diuresis ongoing, discussed with consultants.
Day 4 – Situation improves, renal function stabilizes with inotropic support and renal recommendations, breathing improved, meds regimen stable, labs and CXR stable, patient likely to be discharged in next few days.
Documentation is critical when it comes to a 99233
Since 99233 is higher levels of billing when it comes to inpatient follow up, it is likely to come under more scrutiny and therefore documentation and understanding of requirements is critical. In general, many inpatients are truly sick and if there is genuinely high complexity in terms of the patient and the situation the documentation will take care of it by itself. When we take a deeper dive in to the guidelines for documentation it becomes ridiculously convoluted and takes an investment of time to truly develop an understanding to where it can be applied. Once that understanding is developed the whole thing becomes much easier. Unfortunately a note becomes like a point system where a certain number of points are required for a certain number of categories. That can be advantageous however when it comes to efficiency in documentation for those that understand how it works.
The key Components of a 99233
To bill a 99233 you need at least 2 of the 3 key components .
Detailed interval history
Detailed examination.
High complexity decision making
See below for a more detailed breakdown of these categories
Typically one would also:
Coordinating care with other providers
Counseling patient and family
Alternatively a 99233 can be billed on the basis of time as described below.
Time based 99233
The 99233 represent what would typically be 35 minutes of care at the patient bedside or on the patient’s floor or unit.
If 35 minutes was spent with a patient, if there is specific documentation, it is felt that the time alone may justify the 99233. That documentation must include 1) Total time spent (>35mins) 2) Description of the counseling and care coordination 3) State that over half the time was spent on counseling and coordinating specifics of care.
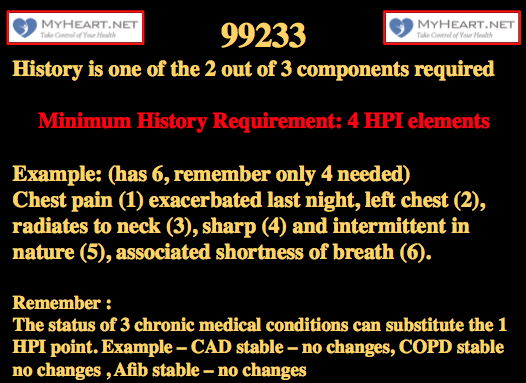
4 HPI elements (locations/severity/duration/associated symptoms etc.) or the status of 3 chronic problems
99233 Examples of interval history:
Chest pain (1) exacerbated last night, left chest (2), radiates to neck (3), sharp (4) and intermittent in nature (5), associated shortness of breath (6).
Shortness of breath (1) noted last night, intermittent (2) and occurring at rest, no relation to exertion (3), no chest pain (4), no nausea (5) or diaphoresis (6).
These examples contain more than the 4 elements required for the HPI element of the 99233. If a patient has a worsening of a condition and it is described appropriately then this should be easily fulfilled.
Note that if there isn’t a 4 point interval HPI, documentation of the status of 3 chronic medical conditions and 2 review of systems are reportedly acceptable surrogates for this in a 99233.
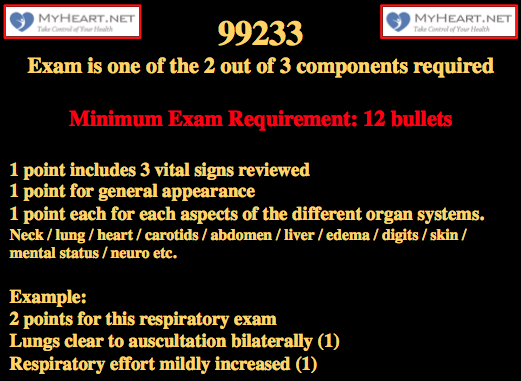
12 bullet points from any organ system
Also described as 6 areas with 2 bullets each, or 2+ areas with 12 total bullets
1 point includes 3 vital signs reviewed
1 point for general appearance
1 point each for Neck / lung / heart / carotids / abdomen / liver / edema / digits / skin / mental status / neuro etc.
In general I would say include 6 organ systems regardless.
99233 examples of detailed exam:
In this cardiac strong exam we have 9 different ‘systems’ which fulfills the 6 suggested, we have 15 bullets, this exceeds the required 12.
1 point for these 3 vital signs
BP 127/84, HR 75, 02sat 96% on air (1 point for the 3 vitals)
1 point for this general exam
Laying in bed, mild increase work of breathing
1 point for this mental status exam
Alert and oriented, can follow instruction
5 points for this cardiovascular exam
Regular rhythm, soft systolic murmur, no added sounds (auscultation of heart)
Forceful apical beat (palpation of the heart)
Normal carotid upstrokes (palpation of carotid)
2+ femoral and radial pulses (examination of peripheral arteries)
1+ bilateral pitting edema (exam of periphery cardiovascular)
1 point for this musculoskeletal exam
No cyanosis or clubbing noted in the digits
1 point for this exam of neck
JVP 10cm, elevated, bed at 45 degrees
2 points for this respiratory exam
Lungs clear to auscultation bilaterally
Respiratory effort mildly increased
2 points for this abdominal exam
Soft and non tender, No masses felt
Auscultation normal bowel sounds
1 point for skin
No new rashes or ulceration noted
High complexity decision making – For a 99233, documentation needs to include at least 2 out of 3 of the following
Extensive management options for diagnosis / treatment
Extensive data to be reviewed
Labs / Radiology tests / PT/OT notes / Consultants notes / Tests to be ordered documented
High risk of complications or comorbidity
Comorbidity documentation that pertains to presenting issues
Risks associated with tests ordered or performed
Risks associated with management issues
For a 99233 typically a combination (2 out of 3 needed) of 4 problem points, 4 data points, and documentation of high risk.
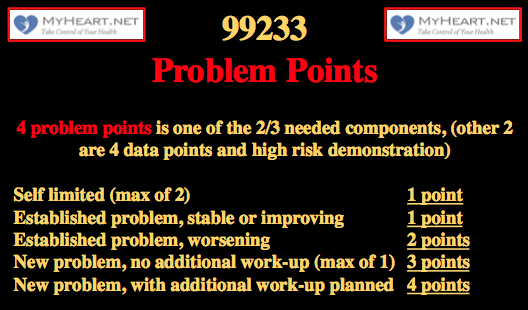
99233 high complexity decision making – 4 problem points
Minor problem points (maximum of 2) = 1 point
Established problem that is stable or demonstrates improvement =1 point
Established problem that worsens = 2 points
New problem with no further work up planned (max of 1) = 3 points
New problem, with additional work-up needed =4 points
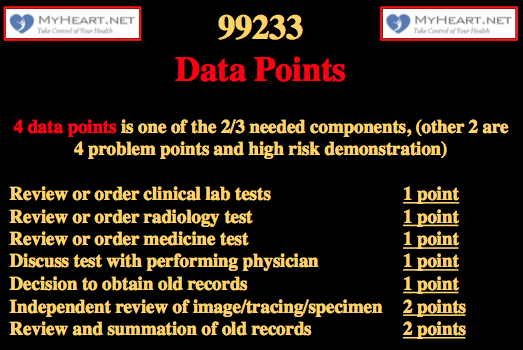
99233 high complexity decision making – 4 Data Points
Review or order labs =1 point
Review or order imaging =1 point
Discuss test with performing physician =1 point
Independently review image / tracing / specimen =2 points
Decide to obtain old records =1 point
Review and summarize old records =2 points
99233 high complexity decision making -Demonstration of High Risk
Needs one of the following 3 elements
Presenting problems
Diagnostic procedures, management options.
One or more chronic illness with exacerbation or progression
Acute or chronic illness posing a threat to life or organ system (resp distress / pulmonary embolism / myocardial infarction / acute kidney injury etc..)
Contrasted cardiac studies
Elective or emergency major surgery
IV controlled therapy
Drug therapy requiring monitoring for toxicity
DNR or establishment of supportive care only
Comprehensive templates for 99233
Here is a comprehensive template for a 99233. I’m sure people will argue that its overkill and takes a lot of time, however I disagree. If these elements are reviewed it clearly improves patient care as multiple pertinent and often ignored elements will be reviewed and taken in to account and can influence decision making. The documentation is comprehensive and in reality not overly time consuming in the era of EMR, particularly if auto-population is used and you are familiar with the patient. If a significant portion of these elements is followed you will much more than fulfill the documentation criteria for a 99233. For those learning the specifics of documentation I would suggest starting comprehensive like this then when you feel comfortable the note can be trimmed significantly and tailored to needs.
Interval HPI;
(If new issue has arisen then state here and if possible describe with 4 points and associated symptoms)
Lab review;
(Pull in lab values if desired)
(Comment on any changes on the review)
Test Review;
(Pull in radiology testing) New radiology tests include
(CXR reading and review) CXR was reviewed and demonstrated
(EKG 12 lead reading and review) 12 lead EKG was reviewed and demonstrated
(Telemetry review and comment) Telemetry was reviewed and demonstrated
(Pull in meds if required)
Physical Exam;
(Pull in BP, HR, temp, 02sat)
(Laying in bed / sitting in chair / ambulating)
(Comfortable / uncomfortable / other comment)
(Alert and oriented, able to answer questions)
(JVP is not elevated, carotid exam normal)
(Regular rate and rhythm, no murmurs noted, no added heart sounds, normal apical pulsation)
(2+ radial pulses bilateral, 2+ femoral/tibial pulses bilaterally)
(no edema in the lower extremities)
(no clubbing or cyanosis)
(Lungs clear to auscultation bilaterally, respiratory effort normal)
(Abdomen soft and non tender, normal bowel sounds)
(No new rashes or ulceration noted)
(Problem list being actively managed)
(Significant new problems interval – work up ordered, treatment started)
(Problem 1 – stable / treating, – management)
(Problem 2 – stable / treating, – management)
(Problem 3 – stable / treating, – management)
(Problem 4 – stable / treating, – management)
Specifics to the 99233
(Discussion with other consultants)
(Discussion with patient and family)
(Review of other notes)
(Obtain old records / summarize old records)
(New studies ordered)
(Code status review)
(IV controlled therapy)
(Drugs being monitored for toxicity)
Comprehensive cardiology centered template example for 99233 – see below for a detailed breakdown and discussion
Shortness of breath worsened overnight, caused to wake from sleep, worse with exertion and lying flat, no further chest pain, no nausea or diaphoresis.
Lab review;
Labs reviewed
BNP is elevated
Cr increased from 1.1 to 1.6
Troponin trend 0.11 to 0.13
ABG showed some hypoxemia
CXR was reviewed and demonstrated findings consistent with worsening of pulmonary edema
12 lead EKG was reviewed and demonstrated sinus rhythm at a rate of 90
Telemetry was reviewed and demonstrated sinus rhythm rate 80-110
Medication list or can simply say was reviewed
BP 100/70, HR 90, temp 98.0, 92% 02sat on 4 liters
Alert and oriented and able to answer questions
Laying in bed
Mildly increased work of breathing
JVP elevated to 10cm at 45degrees, carotid upstroke normal
Cardiac exam, irregular rhythm, no murmurs noted, no added heart sounds, normal apical pulsation
2+ radial pulses bilateral, 2+ femoral bilaterally
1+ bilateral pitting edema in the lower extremities
No clubbing or cyanosis
Lungs have mild creps at bases bilaterally, respiratory effort normal
Abdomen soft and non tender, normal bowel sounds
NSTEMI, s/p PCI
Atrial fibrillation, chronic
Hypertension, chronic, controlled
Diabetes Mellitus, controlled
CHF, acute on chronic systolic
AKI on likely CKD
Interval new issues
CHF / AKI – Interval development of respiratory distress and acute kidney injury. Likely congestive heart failure exacerbation, will order echocardiogram to assess LV function, intravenous Lasix administered, will hold ACE inhibitor in the setting of AKI, continue other meds as stated, monitor renal function closely
Ongoing Issues
NSTEMI / CAD – s/p PCI to RCA 4 days ago, continue aspirin and Plavix, continue BB, holding ACE due to AKI, checking echocardiogram to assess LV function
Hypertension – currently normotensive, holding ACE, continue other meds listed
Atrial fibrillation – rate controlled, continue beta blocker, continue Coumadin for anticoagulation, INR is 1.8 aiming for 2.0-2.5. Will discuss with pharmacy.
Discussed with general medicine team
Discussed with patient who understands issues and daughter at bedside
General medicine note reviewed
Old echo reviewed, EF was 55%, repeat pending
New echocardiogram ordered
Remains Full Code
No IV controlled therapy started
Monitoring Coumadin with INR, co-managing with pharmacy
Detailed Breakdown of the 99233 note template and example.
The example above is a relatively extensive documentation, it would take some people a long time to do that and others could run through it relatively quickly. In my opinion, if there is truly a higher level of care such as a 99233, the time and documentation should reflect that. It can, if methodically done, be in an efficient manner.
By no means is all the documentation above needed. The note basically scores top points in every requirement, and remember only 2 out of the 3 are needed.
Interval HPI
This has already hit over the 4 points required . Theoretically only 1 of the other 2 categories (physical exam and complex decision making) is now needed.
Note that if there isn’t a 4 point interval HPI, documentation of the status of 3 chronic medical conditions and 2 review of systems are acceptable surrogates.
The review of the labs contribute a point to the data point section of the medical decision making section. Remember, 4 data points are needed. Also the increase in creatinine supports the AKI as a new critical diagnosis, the BNP supports CHF acute exacerbation and the hypoxemia supports respiratory distress. Remember, a new significant problem with additional work up planned fulfills 4 points and already qualifies for high risk .
Personally reviewing the radiology test CXR is 2 point. Independent review of the EKG is 2 points (If we had decided to review old records and summarized that would have been 2 points). Later we order an echo, that’s a further point. We had already reviewed the lab above, that’s a further point. In total here we have 6 data points that exceeds the 4 data points required for the 99233. That’s already one of the 2 requirements of the complex medical decision making out the way. Remember it has to be 2 out of the 3 of 4 problem points, 4 data points and high risk. We already have evidence for the new significant diagnosis / problem point above so in theory this note already qualifies for a 99233.
BP 100/70, HR 90, temp 98.0, 92% 02sat on 4 liters (1 point)
Alert and oriented and able to answer questions (1 point)
Laying in bed (1 point)
Mildly increased work of breathing in general (1 point)
JVP elevated to 10cm at 45degrees, carotid upstroke normal (1 point)
Cardiac exam, irregular rhythm, no murmurs noted, no added heart sounds, normal apical pulsation (2 points)
2+ radial pulses bilateral, 2+ femoral bilaterally (1 point)
1+ bilateral pitting edema in the lower extremities (1 point)
No clubbing or cyanosis (1 point)
Lungs have mild creps at bases bilaterally, respiratory effort normal (1 point)
Abdomen soft and non tender, normal bowel sounds (2 points)
No new rashes or ulceration noted (1 point)
Remember that a total of 12 bullets are needed. Ideally 6 organ systems at least. Can be 12 bullets from at least 2 technically. 3 vital signs are 1 point and general appearance is 1 point. In the exam above we have a total of 14 points, we have 6 organ systems, it easily fulfills requirements.
NSTEMI, s/p PCI (established problem, stable 1 point)
Atrial fibrillation, chronic (established problem, stable, 1 point)
Hypertension, chronic, controlled (established problem, stable, 1 point)
Diabetes Mellitus, controlled (established problem, stable, 1 point)
These 4 stable points are ok as they are issues that significantly impact treatment.
CHF, acute on chronic systolic (established problem, worsening (2 points) vs. new problem significantly threatening issue with further work up planned (4 points)
AKI on likely CKD (new problem, significantly threatening issues, further work up planned (4 points).
Once again, our documentation here is basically worth 12 problem points, remember we only need 4; the acute CHF or the AKI would alone have been enough to suffice.
Ongoing Issues
In the section above we have simply bolstered our documentation above. We have laid out the problems that are new and significantly threatening and demonstrated the further work up planned. We have reported the management of the chronic issues. We have documented tests planned and discussions had.
General medicine and PT note reviewed
The discussion with the other physicians involved and also the discussion with the family is a supporting factor for complexity. The review of the medical and the PT notes can act as a point in data. The old echo review can act as a point in data.
The ordering of the new echo acts as a data point also. If this had been a CT angiogram, cath, or other contrasted cardiac scan, or endoscopy for example, it would have actually fulfilled the entire criteria for high risk. If there was IV parenteral therapy, i.e IV pain meds that are controlled, then that also would have acted as high risk. The INR monitoring for the Coumadin, given its significantly high risk for toxicity and need for monitoring can act as a high risk feature also.
Brief note example that fulfills the criteria for a 99233
I’m not a fan of minimalist notes, I think it can breed complacency and doesn’t help with the thought process. The following shows however that when sticking to the criteria for a 99233 we can still achieve what we need to with a minimal note.
Interval history
Shortness of breath worsened overnight, PND, worse with exertion and lying flat, no chest pain, nausea or diaphoresis.
4 interval HPI points satisfied with a worsening shown
Objective points
Alert and oriented, anxious, mildly increased WOB, JVP 10cm, carotid normal, irregular rhythm, no heart murmurs noted, normal apical pulsation, 2+ femoral bilaterally, 1+ bilateral pitting edema in the lower extremities, No clubbing or cyanosis, lungs have mild creps at bases bilaterally, respiratory effort normal
Abdomen soft and non tender, normal bowel sounds No new rashes or ulceration noted
Theoretically we could stop here, we have 2 of the 3 main sections with all criteria fulfilled, interval HPI has 4 points and the physical exam has 12 bullets with 6 systems. This highlights how knowledge of what’s required can allow focus on main issues if that is the aim. In reality the note will continue thought.
Assessement
New respiratory distress, CHF acute exacerbation
Acute Kidney injury
INR is 1.8, patient on coumadin
Both of the above are 4 points each, just one of them would suffice for the medical decision making high complexity requirement. The INR and Coumadin and need for monitoring demonstrate a high risk. In theory this is all that’s needed, you could even take out the physical exam section and still have fulfilled 2/3 requirements as needed.
IV diuresis, repeat echocardiogram, stop ACE inhibitor, monitor renal function
This note was very short, but still way over the requirement in terms of points needed, essentially its point system dense and easily fulfills the documentation needs for a 99233.
Even briefer note example that fulfills the criteria for a 99233
Technically the exam isn’t required
4 data points can be; EKG reviewed no significant ST-T changes (2 points). CXR discussed with radiology concern for pulmonary edema (1 point). Creatinine elevated to 1.6 (1 point). INR is 1.7 on Coumadin, will discuss with pharmacy regarding dose and monitoring ( this is monitoring of a high risk drug and fulfills the criteria for high risk )
4 data points already and high risk demonstration, theoretically the note can stop here and the 99233 criteria have been fulfilled, we have 2 out of the 3 needed, we skipped the exam here remember.
IV diuresis, hold ACE, order echo, monitor renal function
This note was very very short, but still met the requirement in terms of points needed, essentially its highly point system based and despite the brevity of the note fulfills the documentation needs for a 99233.
- Cardiology Coding Center
- Combined Right and Left Heart Catheterization CPT Codes and RVU
- Coronary Intervention CPT Codes and RVU
- Echocardiography CPT Codes and RVU
- Left Heart Catheterization CPT Codes and RVU
- Left Heart Catheterization Miscellaneous CPT Codes and RVU
- Right Heart Catheterization CPT Codes and RVU
- Structural Heart Intervention CPT Codes and RVU
- Coronary Artery Imaging CPT Codes and RVU
- 99232 CPT Code, Level 2 Hospital Followup Note –Dummies Guide 2017-2018
Skip to main content
- Skip to main menu
- Skip to user menu
Certified Medical Coder (CARDIOLOGY & PULMONARY CODING EXPERIENCE)
4 days left
- Save You need to sign in or create an account to save
- Apply (This will open in a new window from which you will be automatically redirected to an external site after 5 seconds)
- An active AAPC, AHIMA, CPC, CCS-P, CPC-H, or related specialty credential.
- 3+ Years of recent coding experience.
- Knowledge of medical terminology and ICD-10 and CPT/HCPCS code sets.
- Excellent interpersonal and problem-solving skills with all levels internal and external customers.
- Outstanding organization skills and time management required.
More searches like this
- Billing / Coding Staff Full Time jobs in New York City

IMAGES
VIDEO
COMMENTS
The latest information on coding and reimbursement, including documentation and compliance updates. ... Coding Corner: Overview of 2024 Coding Changes Impacting Cardiology ACC 2024 Medicare Physician Fee Schedule Final Rule Calculator Now Available Coding Solutions For Renal Denervation.
Here's a brief overview of some key codes: CPT Code 93010: This code involves the interpretation and reporting of electrocardiograms, providing crucial insights into cardiac health through diagnostic analysis. CPT Code 93000: A routine electrocardiogram with a minimum of 12 leads, this code serves as a fundamental diagnostic tool for cardiac ...
• Cardiac Catheterization ... CPT CODE(S): (1) 78452-26, (2) 93016 (3) 93018 14. 9/13/2011 8 Treadmill and Myocardial Nuclear Perfusion Study--Example INDICATION: Chest Pain FINDINGS: Patient underwent treadmill nuclear perfusion study for suspected coronary artery disease. The patient exercised on the
Phrenic Nerve Stimulation System. 93224-93278. Cardiovascular Monitoring Services. 93279-93298. Implantable, Insertable, and Wearable Cardiac Device Evaluations. 93303-93356. Echocardiography Procedures. 93451-93598. Cardiac Catheterization Procedures.
The E/M 2021 changes will only apply to specific codes: new and established office/outpatient E/M codes 99202-99215. For example, if your cardiologist sees patients in the hospital, their office, and a nursing facility, only the visits in the cardiologist's office will be held to the new guidelines. Codes in the other E/M categories will not ...
Step 1: Total time. Think time first. If your total time spent on a visit appropriately credits you for level 3, 4, or 5 work, then document that time, code the visit, and be done with it. But if ...
93000 is one of the most commonly used codes in cardiology. It is used for routine EKG tracing and interpretation. This basic EKG code is used for routine annual exams, pre-operative clearance, and evaluating cardiac symptoms like chest pain, heart palpitations, dizziness, or syncope. 93005 is used for electrocardiogram tracing only, without ...
Shunting for Congenital Cardiac Anomalies. You'll find five new codes in the Cardiovascular System section of your 2021 CPT® code book, including three new shunting procedure codes for congenital cardiac anomalies: 33741 Transcatheter atrial septostomy (TAS) for congenital cardiac anomalies to create effective atrial flow, including all ...
INSIDE THIS GUIDE • Hospital Inpatient Codes and 2024 Payments • Outpatient Codes and 2024 Payments (Hospital, OBL, ASC) • Physician 2024 Payment and RVUs
ICD-10-PCS codes for inpatient procedure coding became effective October 1, 2015. This change does not impact CPT coding for physician and hospital outpatient procedure services. Physician and outpatient procedures will continue to use CPT coding to report procedures and all diagnosis coding will be reported using ICD-10-CM.
Cardiology codes often include modifiers at the end. Modifiers are two-digit codes that show you've somehow altered the service in the original five-digit CPT code. For example, you may add modifier 25 to a patient visit where the clinician determined the patient needed a stress test at the end of the visit.
2021 Office Visit Coding Changes. Evaluation and Management: 2023 Changes to Non-Office Visit Codes. CPT Code: Risk: 99202/99212: Minimal risk of morbidity from additional diagnostic testing or treatment. 99203/99213: ... Coding Q&A—Moderate Sedation with Cardiac Catheterization. Modifiers +
CPT code 99214 is an established patient visit code often reported by cardiology practices, and usually it is completely justifiable because of the nature and complexity of the problems patients with cardiovascular conditions present. Some cardiologists, however, fearful of tossing up a red flag or uncertain about the documentation requirements
33997 for removal of right heart ventricle assist device. 33992 for removal of left heart ventricle assist device. 33990 for arterial-only access. 33991 for both arterial and venous access. Cardiology Medical Billing for total time spent on patient encounters or MDM. From 2021, codes 99202 to 99215 were introduced to define time as the total ...
CPT code 99233 is assigned to a level 3 hospital subsequent care (follow up) note. 99233 is the highest level of non-critical care daily progress note. When it comes to 99233 documentation is critical, however understanding of the documentation required is even more critical. WorK RVU (wRVU) for cpt code 99233 is of course higher than that for ...
your coding selections compare with your peers' coding. l. Access quick references from CMS and medical and trade associations View in-depth webcasts for and by medical professionals. To get on the Road to 10 and find out more about ICD-10, visit: cms.gov/ICD10 roadto10.org. Official CMS Industry Resources for the ICD-10 Transition www.cms ...
Do this: If you're billing an E/M visit solely on the basis of time, you can assign +99417 only after 15 minutes have elapsed beyond the minimum time required for the highest-level primary service. In the cases of office/outpatient consultations, you cannot assign +99417 until 15 minutes have passed after the initial 55 minutes of the 99245 ...
Must have experience coding Cardiology and Pulmonary office, hospital visits, non-invasive testing, PFT testing, Electrocardiograms, Pacer Interrogations, Cardiac Monitoring, Cardiac Cath, and Electrophysiology procedure billing. SCHEDULE: 7a - 4p / 8a - 4p Monday - Friday (Long temporary Contract) PAY RATE: $29 - $30 / H.
Cardiology Coding Alert - 2024; Volume 27, Number 4. Hint: Never report +37185 alone on a claim. When your physician removes a blood clot (th... Read more. Hint: Report I71.12 for a ruptured aneurysm of the aortic arch. If your practice performs... Read more. Focus on new CMS prolonged service G codes.