--------------------------------

What Is Cost Per Visit (CPV) and How To Calculate It?
Sanja trajcheva.
Marketing | May 06, 2023

As a digital marketer, you probably have a whole stack of KPIs that you’re monitoring on a daily basis. So here is another one for you… Cost per visit, or CPV.
Understanding your cost per visit can help you make sense of how much your advertising is costing you in total. It can also help you identify how effective your ad campaigns are and can even help you spot click fraud .
Sounds super useful, right? OK, so first of all, what is CPV?
Table of Contents
What is Cost per Visit?
The cost per visit (CPV) to your site or business looks at how much you’re paying for your advertising and how much a single visit costs.
This can be applied to both website clicks and physical visits or appointments at your location. Generally, it is used to analyze your PPC campaigns, but once you understand how to work out the cost per visit, you can apply it in different ways.
Unlike ROAS (return on ad spend), which focuses on how much it costs to win one customer, CPV looks more at how much you’re paying for an individual visit. It’s a useful way to work out how effective your ad campaigns are across multiple platforms and strategies.
Cost per visit is also not necessarily a metric used by the ad platforms, so you won’t see it in your dashboard. It is, however, quite useful to know if you want to tally up the results of your ad spend.
Do I need to know Cost Per Visit?
Most businesses are using a mixture of advertising methods online, which can include CPC (cost per click), CPA (cost per acquisition), and CPM (cost per thousand impressions).
And running digital marketing ad campaigns usually means using multiple platforms. You might be using Google Ads to target the bottom-of-funnel (BoFu) market and sell. But you might be using Facebook Ads to increase site visitors and boost your brand visibility.
If you’ve ever looked at your spreadsheets or advertising dashboards and scratched your head, understanding your cost per visit can help make sense of all of your combined metrics.
How to work out Cost Per Visit (CPV)
Let’s say you want to work out your cost per visit in a weekly period.
The first thing to do is tally up your ad spend on all platforms that you’re using and the clicks or site visits that came from each of them.
As we can see from the chart above, our example business has spent $650 on marketing in a week. From that, there have been 125 site visits.
$650 / 125 visits = 5.2
That makes a total of around $5.20 per site visit.
To calculate cost per visit (CPV):
Total Cost (divided by) Total Visits = Cost Per Visit (CPV)
In this instance, we’re not looking at the CPA or ROAS, which will return different figures.
Now, another way to look at your cost per visit is to look at the total site visits you have in a period and divide that by all of your marketing efforts. This might also include the time spent to create organic content, the costs of any freelancers or agencies you’re using to do keyword research or manage your ads, and even the software you pay for to help you do the job.
This might look something like:
- Paid ad spend $650
- In-house marketing team $300
- Freelance contributor $150
- Software package $25
And let’s say you have 800 unique views on your site per week from all sources, including organic, paid search, and your paid social campaigns.
$1125 / 800 = $1.40 per visit
Understanding CPV
With the cost per visit, you can then apply your cost per acquisition or return on ad spend and see where your marketing efforts are most successful.
Of course, those organic results might not seem the most cost-effective in the short term, but they are probably (or should be) part of your overall content marketing strategy.
When looking at your paid search results, you can investigate how effective your PPC ads are at attracting the right kind of site visitors. Looking at that cost per visitor, you can then analyze things like:
- Time spent on site or bounce rate
- Pages viewed
- Average spend per customer
- Lifetime value of a customer
- How PPC fares as a percentage of your marketing spend
What’s in a click?
Each click has a value, even if it’s from an organic source. At some point, you’ve paid money or spent your time (which also has value, right?) to create a clickable resource.
Eventually, with some good marketing strategy, the bulk of your sales and site visitors should come from organic search results. Although not ‘free’ traffic (again, you have paid for it), it doesn’t cost per click or per view.
But pay-per-click is still one of the most effective ways of driving traffic to your business and getting on top of the SERPs.
When it comes to clicks on paid search ads, the issues of click fraud and ad fraud become key. Of those site visitors, how many of them are not genuine potential customers?
Understanding how much click bots or malicious business competitors can cost your business can be an eye-opener for many business owners.
According to research from the University of Baltimore, the volume of click fraud averages around 14% globally. And from our own data, we’ve seen this rising to over 60% for some particularly competitive industries.
Yes, that means that 60% of paid clicks on some ad campaigns are not even real customers (or even people), which in many cases also means a higher cost per visit (CPV).
Check out how much fraudulent traffic there is on your PPC ads with the free trial of our industry-leading anti-click fraud software.

As an experienced content writer, Sanja is a firm believer in the power of storytelling to inspire and educate audiences. In her role at CHEQ, Sanja fearlessly tackles the challenges of the fake web – navigating through fake traffic, ad fraud, and click fraud. When not writing, she enjoys exploring new tastes and planning her next adventures.
Related articles
Unveiling the state of fake traffic 2024: insights, trends, and solutions, the bad actors awards: celebrating the most disruptive bots.
Subscribe to our newsletter!
Recommended articles.
How Retailers Can Use Holiday Shopping Findings to Fuel Growth in 2024
Latest posts.
What is Click Fraud? How it Works, Examples, and Red Flags
Price Scraping Exposed: Who is at Risk and How to Prevent it?

Top 7 Ways to Detect Account Takeover Fraud
OTP Bots: The Achilles’ Heel of Your Digital Defense

How to target bottom of funnel customers with PPC content

Webinar Recap: How Junk Leads Impact Revenue Teams

How Bots and Bad Actors Bypass Web Application Firewalls (WAFs)

Don’t Fall Victim: How to Detect Bot Attack on Your Website
Comparing reCAPTCHA and hCAPTCHA: Are CAPTCHA still worth it?
Block invalid traffic with cheq essentials.
- rankingCoach 360 includes:
- Local Marketing Get found locally
- Google Ads More visitors today
- Search Engine Optimization (SEO) Reach the top of Google
- Reputation management Be at one with your customers
- Social Media Monitoring Track the latest news
- Brand Monitoring Check your presence all over the web
- Features overview
- Local Marketing
- Search Engine Optimization (SEO)
- Reputation management
- Social Media Monitoring
- Brand Monitoring
Cost Per Visit (CPV)
What is cost per visit (cpv).
The term cost per visit is pretty self-explanatory. It means the amount of money you’re paying for an ad and how much a single visit to your web page (through that ad) will cost you.
It can be relevant to both website clicks and physical visits or appointments at your location. However, it’s mainly used to analyze digital PPC (pay-per-click) marketing campaigns and help you understand your ads’ reach and influence.
When looking at your paid search results, you can determine how effective your PPC ads are at attracting the right audience. Looking at that cost per visit, you can then analyze variables such as:
- Bounce rate
- Pages viewed
- Average spend per customer
- The lifetime value of a customer
And learning about these factors can significantly help you in improving your ads and your website. But before that, let’s take a look at how we can calculate the cost per visit.
How to Calculate Cost Per Visit
Let’s say you want to calculate your cost per visit for one week.
The first thing to do is add up your ad spend on all platforms you’ve used in the last week and the site visits or clicks that came from each of them.
So, for example, let’s suppose that a business has spent $450 on marketing in a week. And as a result of investing that money, there have been 125 site visits.
$450 / 125 visits = 3.6
That makes a total of around $3.60 per site visit.
Meanwhile, another way to perceive cost per visit is to divide all your marketing efforts by the number of total site visits you might’ve received in a certain period.
It would include the costs of any freelancers or agencies you might’ve used to conduct keyword research or manage your ads, the time you spent to build organic content, and even the software you pay for to help you do the job.
In the end, it might look something like this:
- Money spent on ads $450
- In-house marketing team $300
- Freelance contributions $260
- Software used in the process $35
And let’s suppose your site had 800 unique views per week from all sources, including organic, paid search, and your paid social campaigns.
The final result would be: $1045 / 800 = $1.30 per visit
Why Is Cost Per Visit Important?
Each click on a web page or advertisement has value, even if it’s from an organic source. Remember that you’ve invested time and money to create spaces that will link to your site and increase your page visits. So, the money you’ve spent should be converting into sales for your business. Otherwise, there’s no point in running paid ads.
Key Takeaway
Overall, cost per visit can be an effective method to help you determine what works and what doesn’t for your digital marketing strategy. If you can calculate and then analyze the figures, you can then determine which ads might be costing you the most and whether your money is being well spent.
- Credit cards
- View all credit cards
- Banking guide
- Loans guide
- Insurance guide
- Personal finance
- View all personal finance
- Small business
- Small business guide
- View all taxes
You’re our first priority. Every time.
We believe everyone should be able to make financial decisions with confidence. And while our site doesn’t feature every company or financial product available on the market, we’re proud that the guidance we offer, the information we provide and the tools we create are objective, independent, straightforward — and free.
So how do we make money? Our partners compensate us. This may influence which products we review and write about (and where those products appear on the site), but it in no way affects our recommendations or advice, which are grounded in thousands of hours of research. Our partners cannot pay us to guarantee favorable reviews of their products or services. Here is a list of our partners .
Understanding Copays, Coinsurance and Deductibles

Many or all of the products featured here are from our partners who compensate us. This influences which products we write about and where and how the product appears on a page. However, this does not influence our evaluations. Our opinions are our own. Here is a list of our partners and here's how we make money .
Coinsurance, copays and deductibles are different out-of-pocket costs for health care, and being familiar with these terms can help you better understand your health coverage and costs. Even after you pay monthly premiums for health insurance , out-of-pocket costs can lead to high medical bills if you get sick or injured.
Here's how health insurance costs work.
Defining some health insurance terms
Before understanding how it all works together, let's brush up on some common health insurance terms.
Coinsurance
Coinsurance is a percentage of a medical charge you pay, with the rest paid by your health insurance plan, which typically applies after your deductible has been met. For example, if you have 20% coinsurance, you pay 20% of each medical bill, and your health insurance will cover 80%.
A copay, or copayment , is a predetermined rate you pay for health care services at the time of care. For example, you may have a $25 copay every time you see your primary care physician, a $10 copay for each monthly medication and a $250 copay for an emergency room visit.
The deductible is how much you pay before your health insurance starts to cover a larger portion of your bills. In general, if you have a $1,000 deductible, you must pay $1,000 for your care out of pocket before your insurer starts covering a higher portion of costs. The deductible resets yearly.
The premium is the monthly payment you make to have health insurance.
You pay the premium each month like a gym membership, even if you don't use the coverage. If you don't pay the premium, you may lose your insurance. If you're fortunate enough to have employer-provided insurance, the company typically picks up part of the premium.
Out-of-pocket maximum
The out-of-pocket maximum is the limit of what you'll pay in one year, out of pocket, for your covered health care before your insurance covers 100% of the bill. The maximum out-of-pocket limit for marketplace health plans (those on the Affordable Care Act health insurance marketplace) is $9,450 for an individual and $18,900 for a family in 2024 . (This amount doesn't include what you spend for services your insurance doesn't cover.)
Coinsurance vs. copay
Copays and coinsurance are different ways your health insurance may require you to pay for covered services. Here are the differences:
Copay vs. deductible
Your health plan may have both copays and deductibles, and whether you pay one or the other may depend on the services you receive. For some services, such as a visit to your primary care doctor, you may owe a fixed copay, such as $10 or $20. For other services, such as an MRI, you may have to pay the approved cost of the service up to your deductible.
Your copay may count toward your deductible, but it doesn't always. And you may owe copays for some services after you meet your deductible.
Coinsurance vs. deductible
Deductibles and coinsurance work together, but usually consecutively. As mentioned, the deductible is the amount you pay before your insurance starts covering the cost of your health care. Once you meet your deductible, you'll typically owe coinsurance (such as 20% of approved charges) on all additional services for the rest of the year.
You'll pay coinsurance on approved medical care until you hit the out-of-pocket maximum on your plan, after which your insurance will cover 100% of the rest of your care for the year.
How it all works together
Health insurance policies can have a variety of cost-sharing options. For example, some policies have low premiums, high deductibles and high maximum out-of-pocket limits, while others have high premiums, lower deductibles and lower max out-of-pocket limits.
In general, it works like this: You pay a monthly premium to have health insurance. Then, when you go to the doctor or the hospital, you pay either full cost for the services or copays as outlined in your policy. Once the total amount you pay for services, not including copays, adds up to your deductible amount in a year, your insurer starts paying a more significant chunk of your medical bills, commonly 80%. The remaining percentage that you pay is called coinsurance.
You'll continue to pay copays or coinsurance until you've reached the out-of-pocket maximum for your policy. At that time, your insurer will start paying 100% of your medical bills until the policy year ends or you switch insurance plans.
The catch: Your health plan's network
Here's the snag: The co-sharing scenario highlighted above works only if you choose doctors, clinics and hospitals within your health plan's provider network. If you use an out-of-network doctor, you could be on the hook for the whole bill, depending on which type of policy you have. This brings us to two related terms:
This is the group of doctors and providers who agree to accept your health insurance. Health insurers negotiate lower rates for care with the doctors, hospitals and clinics in their networks. So when you go in-network, your bills will typically be cheaper, and the costs will count toward your deductible and out-of-pocket maximum.
Out of network
A provider your insurance plan hasn't negotiated a discounted rate with is considered out of network. If you get care from an out-of-network provider, you may have to pay the entire bill yourself, or just a portion, as indicated in your insurance policy summary.
» MORE: What the No Surprises Act means for your medical bills
Doing the math on copays, coinsurance and deductibles
To illustrate with an example, consider a person — let's call her Prudence — who needs some health services. (Your costs would be different based on your policy, so you'll want to do your own calculations.)
Prudence's policy:
Insurance coverage: Single.
Annual deductible: $1,200.
Copays: $20 per office visit, $50 per specialist, $100 per ER visit; these don't count toward her deductible.
Coinsurance: 20% after she meets her deductible.
Scenario: Doctor visits and an MRI
Prudence goes in for an annual checkup. Because she goes to an in-network provider, this is a free preventive care visit. (If it had been an office visit for a medical issue, there would have been a $20 copay.) However, her primary care physician thinks Prudence should see an orthopedist based on her physical exam. The orthopedist later recommends an MRI.
Copays for an in-network specialist on her plan are $50. The MRI provider is in her insurer's network, and the approved insurance charge is $1,000 for the MRI, including the radiologist fees for interpreting the scan.
Imaging scans like this are "subject to deductible" under Prudence's policy, so she must pay for it herself, or out of pocket, because she hasn't met her deductible yet.
Total out-of-pocket costs: $50 for the specialist copay + $1,000 for the scan = $1,050.
Scenario: Trip to the ER
Later that year, Prudence falls while hiking and hurts her wrist. She heads to an in-network emergency room, for which she has a $100 copay. After the copay, ER charges are $3,400. Her deductible will be applied next.
Prudence has already paid $1,000 of her $1,200 deductible for her MRI, so she's responsible for $200 of the ER bill before her insurer pays a larger share. Of the remaining $3,200, her health plan will pay 80%, leaving Prudence with a 20% coinsurance of $640.
Total out-of-pocket costs: $100 for the ER copay + $200 for remaining deductible + 20% coinsurance ($640) = $940.
Prudence has now paid $1,990 toward her medical costs this year, not including premiums. She has also met her annual deductible, so if she needs care again, she'll pay only copays and 20% of her medical bills (coinsurance) until she reaches the out-of-pocket maximum on her plan.
Understanding how your health insurance works can save you money and grief now and down the road.
On a similar note...

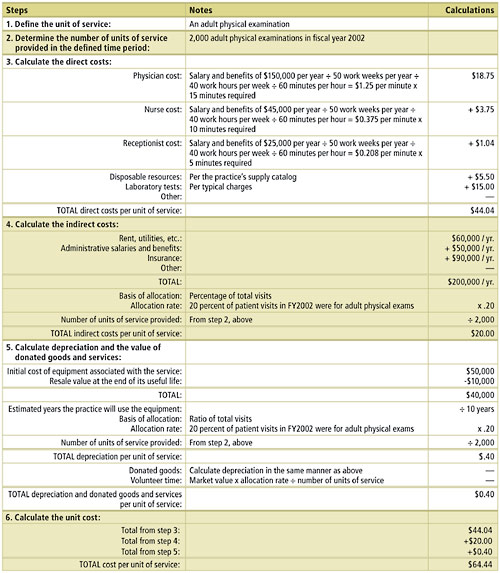
Do you know what it costs your practice to provide an adult physical, a well-child exam or an office procedure? A “unit cost analysis” will tell you that and more .
JEFF KULLGREN, MPH, AND MARIA D. SIBELLA, MA
Fam Pract Manag. 2004;11(4):41-45
A unit cost analysis is one of the most useful yet underused tools for managing a family practice. It takes into account all of the resources associated with providing a particular service and calculates how much it costs to provide that service at the smallest practical unit. 1 – 3 For example, you might want to know the true cost of providing an adult physical exam, a well-child visit or a particular procedure.
Cost-per-unit data can be highly useful to you when developing budgets, setting fees, planning for expansion or negotiating rates with health care insurers. You may find, for example, that the true cost of providing an adult physical exam is significantly higher than the current reimbursement rate of a local health plan. You might then be able to use the data to negotiate a higher reimbursement rate, or at least decide whether the contract is worth renewing. Similarly, you may find that the costs of doing a certain procedure make it unprofitable given the level of reimbursement and the demand for the procedure.
In our recent experience at a medium-sized community health center in the Midwest, the unit cost analysis proved to be an insightful tool. It showed us, for example, that our laboratory expenses for patients with HIV account for about half of the cost of each of their medical visits. When this information was shared with a funding agency, it decided to increase its financial support of the clinic. The analysis also provided a foundation for further inquiries, including a time study of patient and staff work flow that will be used to improve the clinic’s efficiency.
While most physicians would agree on the theoretical utility of unit cost information, they might doubt the practicality of actually performing a unit cost analysis, fearing that it requires vast and expensive resources such as consultants, sophisticated computer systems or accounting training. Fortunately, these elements are not needed to conduct a unit cost analysis. By following the steps provided below, you can acquire valid and actionable cost information about the care you provide regardless of practice size or resources.
Knowing the costs of your services can help you with setting fees, planning for the future and negotiating better rates with health plans.
A unit cost analysis does not require sophisticated computer systems or accounting training.
Family physicians can use a unit cost analysis to determine the true cost of providing an adult physical exam, a well-child visit, a particular procedure, etc.
Six steps to a unit cost analysis
Unit cost analysis is fairly straightforward. The most important thing to remember is that you can and should modify the methodology where necessary for your organization. In doing so, bear in mind that you are not striving to produce a publishable analysis that will stand up under peer review. Instead, you are simply trying to obtain accurate cost information that will enable sound management decisions.
The sample unit cost analysis provided in this article will help illustrate how each of these steps can be applied in the real world. Both the example and this article take a “bottom up” approach (that is, you start by determining all of the individual costs associated with a unit of service and then add them together to determine the cost per unit). Practices with more sophisticated information management systems may be able to take a “top down” approach (that is, you start with the total costs associated with a service and then divide by the number of units of service provided to determine the cost per unit). Each of these methods will lead to the same destination (the cost per unit); they simply have different ways of getting there.
Step 1: Define the unit of service. The first step in a unit cost analysis is to identify the type of service whose cost you want to know. Common units of service are office visits, adult physicals, diabetes check-ups, well-child exams, etc. How you define a unit of a given service should be based on what is meaningful, familiar and useful to your practice. Your staff, for example, may be used to thinking about office visits in 15-minute intervals. This definition will be important when you begin to figure the costs of physician time, nurse time and support staff time associated with the service. Using familiar definitions will make it easier to acquire information, communicate findings with your staff and translate your results into action.
Another consideration in choosing and defining your units of service is your information management system. If your units of service correspond with data already captured by your computer system, it will be easier for you to find the data you need and analyze your practice’s costs. For example, if your computer system tracks claims better than visits, you might choose to calculate the costs of preventive medicine services coded 99381 to 99429.
Units of service can be further segmented, as needed, to provide more detailed cost data about particular types of patients. Patients for whom English is a second language, for example, may require the presence of an interpreter during their regular office visits as well as extra time with their physician. Likewise, patients being treated for chronic diseases may require more time with the physician, more lab tests or more nurse time devoted to patient education. By breaking down your units of service into these smaller components, you can identify costs that might be missed by looking at only the average costs of all patients.
Step 2: Determine the number of units of service provided. In determining the number of units provided, you will need to choose a time period to analyze and must adhere to this period throughout your analysis. Practices with a computerized practice management system should be able to produce the number of units of a particular service provided during a given time period fairly easily. Practices without a computerized system can use a basic chart audit to produce a reasonable estimate. Again, the goal is to acquire the most valid and reliable information available with the staff time and resources available.
Step 3: Calculate the direct costs. Direct costs are expenses you can easily relate to the provision of a specific service. Examples of direct costs include physician and support staff salaries and benefits, medical supplies, lab tests and other resources consumed at the time of the service. Unit costs are likely to be more sensitive to direct costs than any other component of the analysis, so a careful and detailed approach is crucial.
The largest and most important direct cost is often the physician time allocated to one unit of service. This component can be determined through one or a combination of four methods: 1) direct observation of physician activities; 2) time sheets or time diaries that physicians fill out; 3) time sheets or time diaries that patients fill out; or 4) patient cycle times (from check-in to checkout) generated from a practice management system. Support staff time can be determined similarly. For example, by keeping a time diary for one week, a physician may find that he spends an average of eight minutes in the exam room with the typical adult patient. Using his salary or hourly wage as a reference, the physician could then determine his cost for those eight minutes. (See step three of the example .)
Cost information for other resources – such as materials, supplies and laboratory tests – that are consumed during a particular service can be obtained through several different approaches as well. Often a discussion with the physicians or staff familiar with the resources used to provide the service will be sufficient. Reviews of invoices and budgets for the time period or direct observation can also be helpful in tallying the resources directly consumed. For example, to determine the resources associated with a typical office visit, your nurse might simply make a list of the items commonly used and consult the practice’s supply catalog to determine their costs.
Step 4: Calculate the indirect costs. Indirect costs are expenses shared by more than one area of the practice. These costs involve resources that are not directly consumed during the provision of a service, but without them the provision of that service would not be possible. Common examples include administrative staff salaries and benefits, facility costs, insurance premiums, office equipment and supplies, and marketing expenses.
To calculate the indirect costs associated with a particular service, begin by making a list of all indirect costs within the practice (e.g., rent and utilities = $60,000 per year; administrative salaries and benefits = $50,000 per year; malpractice and general liability insurance = $90,000 per year). Then, total these indirect costs (e.g., $200,000 per year). Next, decide how much of the practice’s indirect costs should be allocated to the service in question. Common bases for allocation include the ratio of the selected service to all services provided, the percentage of total revenue attributed to the service, the percentage of practice square-footage devoted to the service, or the percentage of the organization’s total direct costs attributed to the service. For example, the fact that 20 percent of a practice’s visits are adult physical exams can be used as a rationale for attributing 20 percent of the practice’s indirect costs to adult physical exams. (See step four of the example .) Often, more than one potential basis for assigning indirect costs will suggest themselves. In such cases you’ll simply want to decide which one makes the most sense for your practice as a whole.
Step 5: Calculate depreciation and the value of donated goods and services. Before you can figure the full cost of providing the service in question, you must incorporate estimates for depreciation and the value of any donated goods or services. Overlooking these expenses may lead you to underestimate long-term expenses, and it may impede long-range planning. “Straight line depreciation” is one generally accepted – and perhaps the most straightforward – way of calculating this cost. Take the initial cost of the equipment and subtract its estimated resale value at the end of its useful life (e.g, $50,000 - $10,000 = $40,000). Divide this number by the years you expect your practice to use the equipment (e.g., $40,000 ÷ 10 years = $4,000). Using a cost allocation similar to the one used in step 4, determine the amount of depreciation attributable to the service (e.g., $4,000 x .20 = $800). Divide this number by the number of units of service provided in the study time period to arrive at a depreciation cost per unit of service (e.g., $800 ÷ 2,000 adult physical exams per year = $0.40 per adult physical exam).
Some clinics also rely on the use of donated goods or volunteer services, and the market value of these items (i.e., the amount you would have had to pay to acquire the donated goods or services) should be included in your cost calculations. Since these resources may not always be available to a practice, the costs of replacing them to maintain current service levels can be significant. Documenting the financial importance of these donations can also be valuable for organizational fundraising and planning.
To calculate depreciation for donated goods, use the formula described above for depreciation of non-donated equipment. To calculate the cost of donated services, multiply the market value of the services by the allocation rate, and then divide by the number of units of service provided (e.g., $10,000 x .20 ÷ 2,000 adult physical exams provided per year = $1.00 per unit of service).
Step 6: Determine the full cost of the unit of service. This final step is the simplest: Add the costs from steps 3, 4 and 5 to arrive at a total cost per unit of service. In the example , the final cost for an adult physical examination was $64.44.
AN EXAMPLE: CALCULATING THE COST OF PROVIDING AN ADULT PHYSICAL EXAM
Family physicians in a two-person practice would like to know the true cost of providing an adult physical exam in their office. The practice wants to determine whether a private insurer is compensating them adequately and whether they should try to negotiate a better reimbursement rate.
Using data for fiscal year 2002, the physicians completed the following unit cost analysis. The practice also kept time diaries for one week to determine the physician and staff time required for an average adult physical examination.
In the end, the physicians found that an average adult physical examination costs $64.44.
Lessons learned
As family medicine continues to be practiced in a financially hostile health care environment, the need for accurate and actionable cost data has never been greater and will only increase in the future. A unit cost analysis can reliably yield this information and is a valuable tool for any family practice seeking to improve its management, efficiency and planning. By using an effective but realistic approach based on the six steps listed in this article, even the most resource-poor organizations can design and conduct a unit cost analysis that will help managers make the sound decisions needed not only to survive – but to succeed – within this environment.
Health Resources and Services Administration. Determining the Unit Cost of Services: A Guide for Estimating the Cost of Services Funded by the Ryan White CARE Act of 1990 . Rockville, Md: U.S. Department of Health & Human Services; 1993.
Yates BT. Analyzing Costs, Procedures, Processes and Outcomes in Human Services . Thousand Oaks, Calif: Sage Publications; 1996.
Zelman WN. Cost per unit of service. Evaluation and Program Planning . 1987;10:201-207.
Continue Reading
More in fpm, more in pubmed.
Copyright © 2004 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

Journal of Urgent Care Medicine
Practice Management
Understanding Your Cost Per Patient
Urgent message: Assessing the true cost per patient is key to determining which pricing model will generate the most revenue for an urgent care center.
JORDAN TODD RICE, MD A cost-per-patient analysis may not work for every urgent care center owner, but this article is intended to give JUCM readers the basic tools they need to understand the formulas. It can also serve as a baseline for discussions with urgent care center staff, executives, managers, clinicians, and owners.
The goal of the exercise is to help urgent care providers better understand key elements of patient costs so they can determine which pricing model will best serve their organizations, be they for-profit, nonprofit, a single urgent care center or a practice with multiple locations.
How do operators of urgent care centers truly break down the cost for providing care to a single patient for primary care, urgent care or Workers’ Compensation services?
- How can the operator of an urgent care center do a true cost/benefit analysis to find out if it makes sense to switch to a single payment from payors rather than traditional fee-for-service reimbursement?
- How can and will paperless and digital systems affect the answers to the previous two questions?
Overcoming Accounting Obstacles One of the biggest challenges in calculating cost per patient is getting information from an urgent care center’s accounting and practice management systems. This is the most difficult task because such systems are great for generating information about pricing and revenue but not set up to provide costs, unless the Relative Value Unit (RVU) option is switched on. Some providers thought that the advent of all-in-one systems and single databases combing practice management (billing, scheduling, claims follow-up, etc.) and an electronic medical record would make the task easy to accomplish. In fact, automation helps practices do better charge capture, speeds up patient visits (after the normal 3- to 6-month learning curve for the switch from paper to paperless) and may even automate coding. It does not, however, compute the true cost per patient.
The other obstacle is the accounting program. Virtually every transaction in every category can be seen in an urgent care practice’s Chart of Accounts, but calculating the cost of each transaction is not as easy as you might think. For example, if your practice has a 401 (k) plan or your employees pay a portion of their health insurance, is that a true “cost” that needs to be factored into the computation of average cost?
Finally, an urgent care practice must be able to differentiate types of payors and services. For example, if your practice is a hybrid that provides both primary care and urgent care services, payors typically pay the same amount regardless of the type of visit. The main differentiators for most states and payors are factors such as the type of provider (some payors discount a physician extender visit by as much as 15%), use of “s” codes for a particular facility (fee-for-service or global fee) and whether a service was rendered “after hours” compared with the hours of an average practice. All of these factors affect reimbursement and cost, assuming that physician extenders are paid less than MDs and DOs. Even the place of service can affect reimbursement, but it usually does not impact cost. The same is true for treating Workers’ Compensation cases or providing occupational medicine services. The reimbursement levels may be higher or lower than those for a non-work-related injury, but the cost should be relatively similar for treating a 10-cm laceration, an aggravated left ankle sprain, or carpal tunnel syndrome, which is now becoming more and more common outside of the workplace because of the advent of home computers, pads, tablets, and even smartphones.
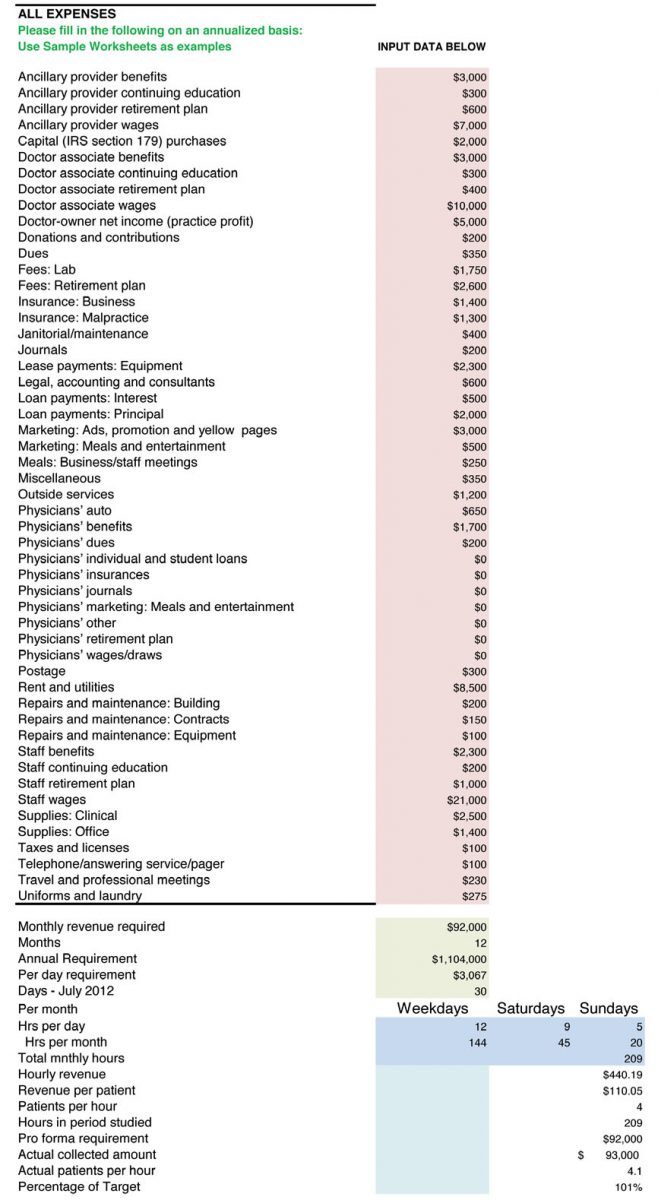
Thus we need to focus on cost only and in this case we will look across the board. Table 1 is a typical chart of accounts for an urgent care practice by category.
Your urgent care practice may have more or less accounts, but the ones listed are typical whether you have one office or 50.
For simplicity, let’s assume that for June 2011, the total for the accounts shown in Table 1 was $100,000. In a very unsophisticated model, we would simply take the number of patients for the month and divide that into $100,000 to get the cost per patient. If the practice saw 50 patients per day for 30 days in June, the total number of patients seen that month would have been 1,500. The cost per patient, then, would be $66.66 ($100,000 divided by 1,500). Net revenue of $120,000 from the 1,500 patients (understanding that most billings would be collected in June, some in July, and the remainder in August) would result in net profit of $20,000.
The collected amount per patient would be $80 and the profit per patient, in our simplistic model, would be $14.34. Continuing with our simplistic example, if a payor were to offer the practice a global fee of $90 per patient, which would typically encompass all services, including on-site laboratory, x-ray, electrocardiography (ECG), spirometry and most other patient costs, the practice would then receive a profit of $24.34 per patient. That is one reason that practices receiving global fees use digital technology for x-rays, ECG, and spirometry and send most laboratory work out to be processed. There are also savings to be had on the billing and collection side because global fees don’t get rejected, don’t have to be re-filed, and co-pays are received at the time of service, so there is little patient follow-up in terms of collections.
Real-World Complications Why, then, do simple cost-per-patient calculations not work in the real world? The factors involved are myriad, some which we’ve already discussed. One issue is how payroll is processed. In a traditional medical model, employees and clinicians are paid every 2 weeks. Some urgent care practices pay employees weekly, whereas others pay twice a month, and others even pay clinicians daily.
Clearly, when employees are paid every 2 weeks, there will be three pay periods in several months every year, which skews costs tremendously. Also, many insurance premiums are paid quarterly, semi-annually or even annually. That, too, affects month-to-month costs. Other factors include benefits payments, such as 401 (k) or retirement contributions, which may happen every pay period, monthly, or annually. Utility, water, sewer, and other costs also fluctuate from month to month. In Maine and Oregon, heating costs may sky rocket in mid-winter, whereas Arizona and Florida may have high cooling costs from mid-spring to mid-fall. Water and sewer costs tend to fluctuate less, but even they can go up and down. Therefore, it might make sense to do computations for your urgent care practice using quarterly, semi-annually, or even annual numbers.
If our model urgent care center has $1.2 million in true costs and 18,000 patients, the cost per patient would be the same: $66.66. But what if the center’s costs were actually $1.4 million and it had only 17,000 patients? Now the cost zooms to $82.35 per patient. Conversely, if the center only had $1 million in costs and 20,000 patients, the cost per patient would be only $50. Again, ANY additional revenues above this would be profits (or surplus for non-profit urgent care centers).
Now, let’s do some addition and subtraction from revenues for your urgent care center. Do you sell products for weight loss or durable medical equipment, or do your physicians dispense drugs? If so, those services usually are not paid by fee-for-services or global contracts. Laboratory services and x-rays typically are included in a global fee, but they usually are separate fees for a payor. Do you bill separately for them? The same question applies to Healthcare Common Procedure Coding System items, which are reimbursed and may be a “carve out” paid in addition to a global fee, depending on the individual contract. Cash-only services such as allergy testing, home sleep studies (elective), Holter or event monitoring are revenue. But their costs should be separated from the equation to compare fee-for-service and global fees and truly understand your actual cost per patient.
Understanding a Cost Benefit Analysis Spreadsheet Next, let’s look at how a cost benefit analysis spreadsheet works. A typical one that includes all costs is available in the Resources section of UCA’s Members Only portal, Uconnect (http://uconnect.ucaoa.org), and can be downloaded for free. A screenshot of what typical data entry looks like is shown in Figure 1.
Please note that annualized numbers were used in our example for the reasons we previously mentioned. There are too many expenses that are not paid on a monthly basis, and payroll can skew the numbers from month to month. What is key is to understand that each provider uses different resources, some of which are reimbursed and some are not. Once again, x-rays could be a profitable venture, but you have to understand the true cost of each x-ray. What is the cost of the unit? Is it leased or purchased? How much developer or fixer does it take if you use plain film for 100 or 1,000 x-rays? Is there a maintenance contract on the development unit? How about on the x-ray tube and collimator?
What cost benefit analysis does is permit the operator of an urgent care center operator to know the exact cost per x-ray, based on ALL costs against ALL revenues. In fact, I have worked with owners of urgent care centers who insisted they made money with a particular payor on a three-view ankle x-ray. But when we looked at all costs, including the cost for the room (rented or owned facility), personnel and over-reads if required, many times those x-rays were costing money not producing revenue. Even digital units have costs associated with them other than just the lease or amortized purchase price, such as the price of replacement cassettes, DVDs, maintenance, and replacement tubes.
The Impact of Variation in Reimbursement The hardest part of determining cost per patient is factoring into the equation varying reimbursements. Unless your urgent care center accepts cash only, you may be receiving 100 different reimbursements for a three-view ankle x-ray. Medicare, Medicaid, Indian Health Service, Tri-Care and some Federally Qualified Health Center fees are all under the Centers for Medicare & Medicaid Services (CMS) umbrella, but each will have a different reimbursement level. And even that number can be affected by the clinician on duty and whether that individual was a physician extender or a physician, for whom discounts of between 10% and 15% might apply. Figure 2 illustrates this computation, focusing on one insurance company.
For our example, we used fictitious numbers and a fictitious payor and chose an arbitrary reimbursement of $35 for a three-view ankle x-ray for Delta employee. From there, we included all costs involved with taking three x-rays. Note that we added every possible cost. Most are inputted as an annual cost and then we worked backward to the cost per x-ray. We can do this working off the annual number or the monthly number. The spreadsheet includes ALL costs for the facility and takes into consideration the total amount of space for x-rays, including the development room, x-ray storage, x-ray room, and operator area. If you pay for over-reads and they are not reimbursed separately or directly by a payor, then that needs to be included. We added all costs associated with the x-ray unit (assuming a lease, in this case), such as maintenance, fixer, developer, film, and any other direct costs. We also added in 15% (every center will be different) for billing and administration to collect and bill for the service. So, after looking at our sample $35 payment and subtracting these expenses, we came out with a profit of $1.64 per three-view ankle x-ray for this particular insurance company.
The same cost can be used when negotiating global fees. You simply need to look at the total number of x-rays you do for that particular payor over a period of time (1 year is safe) and interpolate the same costs minus some administration and billing, because they will be lower. If you receive a global fee of $150, for example, and one out of three patients has an x-ray and the average cost of that x-ray is $33.36, that equals a cost of $11.12 per patient under the global fee. This same calculation can be done for all payors and all x-rays your center offers and for which it bills. This is true of in-house laboratories.
A lot of work? Absolutely! There is no easy way to do a cost benefit analysis. It takes time and effort and requires a complete knowledge of true costs and actual reimbursements net of any write-offs, charge-offs, collection fees, and any other factors that will affect the actual cash that goes into the center’s bank account.
Understanding RBRVS Now we turn to Resource-Based Relative Value Units (RBRVS). Why are these helpful to your practice, if your practice management system allows you to use them? This is a neutral system used by CMS, HMOs, and many payors to determine how much money providers should be paid. All procedures (CPTs) are assigned a base value, which is influenced by three factors: physician work (52%), practice expense (44%), and malpractice expense (4%). The value for a particular CPT code is then further adjusted by a geographic factor because it clearly costs more to deliver services in New York and San Francisco than it would in small towns where there are no physician shortages. And finally, there is an annual conversion factor.
A debate about the issue of payment for effort-based medicine versus outcomes-based medicine is beyond the scope of this article. Reimbursement for urgent care services traditionally has been done based on our efforts and not the actual outcomes because urgent care providers usually do little follow up and are the largest referral source in all of medicine, save the emergency department. An argument can be made for reimbursing hybrid urgent care centers for outcomes-based medicine, but the focus of this article is understanding costs. And costs based on RBRVS can be a helpful indicator of what it should cost to provide a particular procedure coded via CPT for conditions from urinary tract infection, to ankle sprain, to upper respiratory infection.
Weighing Fee-for-Service Versus Global Fees Once you understand the cost per patient for your urgent care center, you can start evaluating whether fee-for-service is better than global fees on a payor-by-payor basis. In other words, the center will have to absorb the cost per x-ray, which will ONLY be affected on the global fee basis (because it is part of the global fee), but the actual cost per x-ray to the center should be a bit lower because there is less administration and the payment is stable from patient to patient. Yes, the comparison between fee-for-service and global fees is apples to organs, but in the end, the issue is which generates more profit or surplus (for non-profits). This article has not addressed hospital-based centers that have a facility fee and professional component, because a global fee for both typically is precluded by regulatory issues at the state and federal level. Physicians employed by a hospital-owned center may want to consider comparing global fees with fee for service. Again, such calculations can take a lot of time and one center may have a global fee with Medicaid but a fee-for-service arrangement with Blue Cross Blue Shield, for example. However, without calculating the true cost per patient, no urgent care center can be in a position to properly to make a case that an insurance company or CMS is underpaying for its providers’ services.
This primer offers basic tools for starting the process of identifying your urgent care center’s cost per patient. More information is available from the following resources to help providers further refine the process:
- http://www.sjsu.edu/faculty/watkins/cba.htm
- http://management.about.com/cs/money/a/CostBenefit.htm
- http://www.mindtools.com/pages/article/newTED_08.htm
- http://www.archives.gov/federal-register/publications/faqs.html
- http://www.physicianpractice.com/rvu/content/article/1462168/1867117
- ← High-Risk Conditions Presenting as Back Pain (Part 2)
- Atypical Appendicitis in the Older Patient →
- Clinical Feature Articles
- Case Reports
- Orthopedic Case Report
- Clinical Image Challenges
- Web Exclusive Images Challenges
- Abstracts in Urgent Care
- JUCM Webinars Archive
- Letters from the Editor-in-Chief
- From the UCA CEO
- Practice Management Articles
- Perspectives
- Occupational Medicine
- Revenue Cycle Management
- Developing Data
- Web Exclusive Articles
- Buyer’s Guide
- Author Bios
- Author Instructions
- Submit An Article
- Individual Articles
- Full Issue PDFs
Remember Me
Lost your password?
Username or E-mail:
Cost per visit
Cost Per Visit indicates the cost incurred by an ecommerce business to attract each visitor to its site.
Cost per visit is a critical metric in ecommerce, representing the amount of money an advertiser spends to garner a single visit to their website through different marketing channels. This metric helps understand the efficiency of an online marketing campaign in terms of attracting potential consumers. It provides an insight into how effectively the advertiser is capitalizing on its digital marketing strategies based on the monetary investment and the traffic drawn to the webpage.
Cost Per Visit = Total Marketing Expenses (in a given period) / Total Website Visits (in that given period)
If an ecommerce business invests $10,000 per month in digital marketing and results in 50,000 site visits, then CPV would be $0.20 ($10,000/50,000).
Why is Cost Per Visit important?
Knowing the Cost per visit helps ecommerce businesses understand the effectiveness of their marketing investments. It enables them to track the cost-effectiveness of different marketing channels, helping them prioritize resources and fine-tune their marketing strategies for maximized returns. Examining Cost per visit can reveal crucial insights into whether a business is spending too much or too little on attracting website visitors.
Which factors impact Cost Per Visit ?
Multiple factors can influence Cost per visit, including the quality of content, SEO effectiveness, the marketing channel's efficiency, targeting precision, frequency of customer interaction, competitor's strategies, and changes in industry trends.
How can Cost Per Visit be improved?
To optimize Cost per visit, it is crucial to improve the conversion rate and drive quality traffic to the website. Ecommerce businesses should focus on effective SEO strategies, high-quality, relevant content, social media marketing, and pay-per-click advertising. A/B testing can also assist in understanding visitor preferences and trends.
What is Cost Per Visit 's relationship with other metrics?
Cost per visit is deeply intertwined with other ecommerce metrics like conversion rate, Cost per Acquisition (CPA), and Return on Marketing Investment (ROMI). A lowered CPV can optimize ROI, indirectly leading to a lower CPA. Enhanced CPV results could indicate improved efficiency in SEO, content, advertising, and overall marketing efforts.
Explore more Glossary terms
Cost of goods sold.
Cost of Goods Sold (COGS) is an accounting metric used to calculate the cost of any goods sold in an ecommerce business.
Coverage Issues
Track SEO health with Coverage Issues metrics. Measure index problems encountered by Googlebot, ensuring website visibil...
Cost Per Completed View
Cost Per Completed View (CPCV) is a digital advertising metric that calculates the cost of a single full video view.
Cost per Email Click
Cost per Email Click (CPC) is a useful email metric that measures the price paid to acquire leads or customers via email...
Clicks per post
Clicks per post refer to the number of times users click on a particular post in an ecommerce environment, offering insi...
CPA fraud refers to dishonest actions undertaken to falsely increase the perceived performance of a CPA campaign.
Cost Per Visit Calculator
Author: Calculator Academy Team
Last Updated: August 1, 2023
Enter the total cost of the marketing campaign and the number of visits generated into the calculator to determine the cost per visit.
- Cost Per Click Calculator
- Cost Per Point Calculator
- Cost Per Impression Calculator
- Cost Per Acquisition Calculator
- Cost Per Reach Calculator
- Cost Per Action Calculator
- Cost Per Result Calculator
- Cost Per User Calculator
- Cost Per Vote Calculator
Cost Per Visit Formula
The following equation is used to calculate the Cost Per Visit.
- Where CPV is the cost per visit ($/visit)
- MC is the total marketing cost ($)
- V is the number of visits generated
To calculate the cost per visit, divide the total cost of the marketing campaign by the total number of visits generated.
What is Cost Per Visit?
Definition:
Cost per visit, or CPV for short, is a measure of the monetary costs it takes a business to generate one visit, typically to a website, but in some cases to a physical store.
Sometimes marketing teams like to look at the cost per visit of other metrics like cost per impression because getting people to visit the store or website is the ultimate goal, not getting an impression.
How to Calculate Cost Per Visit?
Example Problem:
The following example outlines the steps and information needed to calculate the Cost Per Visit.
First, determine the total marketing cost. In this case, the marketing cost is found to be $600.00.
Next, determine the total number of website visits generated. For this example, the number of visits was 20.
Finally, calculate the cost per visit using the formula above:
CPV = MC / #V
CPV = $600.00 / 20
CPV = $30.00 / visit
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
How to Calculate Your Health Plan Coinsurance Payment
Health insurance doesn’t pay all of your healthcare expenses. Instead, you’re expected to foot the bill for part of the cost of your care through your health plan’s cost-sharing requirements like your deductible , copayments , and coinsurance .
This article will explain how coinsurance works, how it differs from deductibles and copays, and how you can know what to expect in terms of the bills you may receive from your medical providers.
Since deductibles and copayments are fixed amounts, it doesn’t take a lot of math to figure out how much to pay. A $30 copayment to fill a prescription or see a doctor will cost you $30 no matter how much the total bill for the prescription or office visit was.
Your health insurance picks up the rest of the tab. Note that this generally only applies if you use an in-network provider and fulfill any prior authorization requirements that your insurance plan has.
However, calculating your health insurance coinsurance payment is trickier. Since coinsurance is a percentage of the total cost for the service, you’ll owe a different amount of coinsurance for each service you receive.
If the healthcare service you received was cheap, your coinsurance won’t be much. However, if the healthcare service was expensive, your coinsurance could wind up being hundreds or even thousands of dollars. Your coinsurance will be limited by your health plan's maximum out-of-pocket limit .
You need to understand how to calculate your health insurance coinsurance payment so you’ll know how much you’ll owe for coinsurance and you can budget for it.
Find Your Coinsurance Rate
You’ll need to find your coinsurance rate for the type of care you’re getting. You should be able to locate this in the Summary of Benefits and Coverage you got when you enrolled in your health plan. Sometimes you can even find it on your health insurance card.
Coinsurance typically kicks in after you've met your deductible, so you'll want to understand how much your deductible is as well. You'll pay your medical bills in full—at the negotiated discounted rate that your insurer has with your medical provider—until you've paid an amount equal to your deductible. Then you'll start to pay coinsurance. Note that some health plans have coinsurance for certain drug tiers even before you've met your deductible.
On some health plans, coinsurance can be the same percentage no matter what type of service you get. For example, 30% coinsurance for hospitalization and 30% coinsurance for specialty drug prescriptions.
In other health plans, you might have a low coinsurance rate for some services and a higher rate for other types of services. For example, you could have 35% coinsurance for hospitalization, but only 20% coinsurance for surgery at an outpatient surgery center.
And it's very common for prescription drug coverage to be structured with copayments for drugs that are in lower-cost tiers, but coinsurance for higher tier or specialty drugs. So you may be accustomed to paying a flat dollar amount at the pharmacy, but then end up having to pay a percentage of the cost of a new prescription—which can get quite expensive, depending on the drug.
Note that prescription costs are generally capped by health plans' maximum out-of-pocket limits, but that's not true for Medicare Part D prescription coverage. However, the Inflation Reduction Act is phasing in a cap on out-of-pocket prescription costs under Medicare Part D, starting in 2024.
Find the Cost of Your Care
Once you know your coinsurance rate, you need to determine the total cost of the healthcare service you received. If you’re using an in-network provider, your health plan has already negotiated discounts from that provider.
Calculate your health insurance coinsurance payment based on the discounted rate, not the standard rate charged to people who don’t belong to your health plan.
Find this in-network discounted amount on your Explanation of Benefits (EOB) listed as “ allowed amount ". The EOB will also show the amount the provider billed, which will generally be higher than the allowed amount.
If you haven’t gotten the healthcare service yet, you won’t have an EOB to check. You can try asking your medical provider or health insurer what the in-network rate for that particular service is.
But know that sometimes you simply won't be able to get an accurate estimate of the total cost of your treatment in advance, either because the information is considered proprietary, as part of the network negotiations between the insurer and the medical provider, or because the medical provider won't know in advance exactly what services need to be performed.
A healthcare transparency rule was phased in starting in mid-2022 (fully in force by 2024), requiring health plans to make pricing and network-approved costs available to consumers upon request.
This rule is controversial, with insurers deriding it as unnecessary and costly, while HHS officials herald it as a big step forward for healthcare price transparency. It is expected to result in lower MLR rebates , as well as higher premiums in the individual/family health insurance market.
A similar, but much less far-reaching rule was finalized in 2019, requiring hospitals to publicize their network-negotiated rates for common services. This rule took effect in January 2021, although enforcement and compliance have proved challenging. In 2023, CMS outlined new rules to make hospital pricing lists more readily available to the public.
If the care you're going to need is a basic service that doesn't vary from case to case (an MRI, for example), the hospital or doctor's office should be able to give you a total price in advance.
But if you're having a surgical procedure, the doctor may not know exactly what will be involved until they actually do the surgery—and no amount of transparency regulations can address that.
You can rest assured that your health plan's maximum out-of-pocket will kick in if the bill becomes substantial, but if your out-of-pocket maximum isn't met, the amount you'll have to pay in coinsurance could be subject to change.
Calculate Your Coinsurance
To calculate the coinsurance you owe, you’ll first convert your percentage figure into a decimal figure by moving the decimal point two spaces to the left like this:
Now, multiply this decimal figure by the network-approved amount for the service you had or will have. Note that this is not the same as the amount that is billed by the medical provider since insurance companies negotiate lower rates and require their in-network medical providers to write off the portion of their bill above that amount.
Assuming you've used an in-network medical provider, the coinsurance amount is calculated based on the network-approved price, NOT the amount that was initially billed.
Coinsurance rate (as a decimal figure) x total cost = coinsurance you owe.
Follow these two examples to see the calculations and results
Antoine’s health plan requires 20% cost-sharing to fill a prescription. The network-negotiated price for his prescription is $150.
0.20 x $150.00 = $30.00 Coinsurance rate x total cost = coinsurance Antoine owes.
Antoine owes $30 coinsurance for this particular prescription.
Kinsey’s health plan requires 35% cost-sharing for hospitalizations. The total network-negotiated cost for her hospital stay, after she pays her deductible, is $12,850.
0.35 x $12,850 = $4,497.50 Coinsurance rate x total cost = coinsurance Kinsey owes.
Kinsey will owe $4,497.50 in coinsurance charges for her hospitalization, in addition to the amount of her deductible. But that's assuming she hasn't yet met her health plan's out-of-pocket maximum yet. If her deductible plus this coinsurance would exceed the out-of-pocket maximum for her plan, her coinsurance amount will be reduced so that her costs won't go over the plan's limit.
Factors Affecting Coinsurance Amount
Don’t forget that you must also pay your deductible. On some health plans, you’ll have to pay the entire deductible before your health plan begins to pay part of the cost of your non-preventive care. Only after you’ve paid your full deductible will you be sharing the cost of your care with your health plan by paying coinsurance.
If you have a really big healthcare bill, your out-of-pocket maximum might kick in and protect you from some of the cost. Once the deductibles, copayments, and coinsurance you’ve paid this year add up to the out-of-pocket maximum, your cost-sharing requirements are finished for the year.
Your health plan picks up 100% of the cost of your covered in-network care for the rest of the year. You don’t have to pay coinsurance, copays, or deductibles again until next year (usually). Note that this isn't how it works with Medicare (inpatient cost-sharing for Original Medicare is based on benefit periods rather than the calendar year).
In 2024, all non-grandfathered, non-grandmothered plans must have out-of-pocket maximums that don't exceed $8,450 for a single individual and $18,900 for multiple family members on the same plan. But many plans have out-of-pocket maximums that are well below these limits. Medicare Advantage plans cannot have out-of-pocket maximums of more than $8,850 in 2024 (not counting drug costs). Original Medicare does not have a cap on out-of-pocket costs, but most enrollees have supplemental coverage that pays some or all of the out-of-pocket costs.
Thanks to the Affordable Care Act , most preventive care must be covered by your health insurance without requiring coinsurance, copayments, or even a deductible, as long as your health plan isn't grandfathered.
This means you won’t have to pay coinsurance on things like your yearly physical exam, yearly mammogram, and routine immunizations. Although it may seem like preventive care is free, it’s not. Instead, the cost of that preventive care is included in your monthly health insurance premium whether or not you actually use the care.
It's also important to note that while some of these services, such as mammograms and colonoscopies, are fully paid for by your health insurance without cost-sharing if they're done on a preventive basis, but subject to your deductible and coinsurance if they're considered diagnostic.
So if you're just going in for your routine annual mammogram, you won't have to pay anything. But if you've found a lump in your breast and are having a mammogram to determine whether it's cause for concern, expect to have to pay your health plan's normal cost-sharing (deductible and/or coinsurance) for the mammogram.
Coinsurance is a form of health care cost-sharing in which the patient pays a percentage of the cost and their health plan pays the rest. Coinsurance typically kicks in after the patient has paid their deductible, but before they have met their annual maximum out-of-pocket limit. Coinsurance typically applies to services that aren't covered with a copay.
Centers for Medicare and Medicaid Services. Transparency in Coverage .
Keith K. Trump Administration finalizes transparency rule for health insurers . Health Affairs. November 1, 2020.
Department of Health and Human Services. Medicare and Medicaid Programs: CY 2020 hospital outpatient PPS policy changes and payment rates and ambulatory surgical center payment system policy changes and payment rates. price transparency requirements for hospitals to make standard charges public .
Lloyd, Travis G.; Hoffmann, Stephanie M. Bradley Insights and Events. The Ongoing Saga of the CMS Hospital Price Transparency Rule .
Centers for Medicare & Medicaid Services. Hospital Price Transparency Fact Sheet .
Centers for Medicare and Medicaid Services. Center for Consumer Information and Insurance Oversight. Premium Adjustment Percentage, Maximum Annual Limitation on Cost Sharing, Reduced Maximum Annual Limitation on Cost Sharing, and Required Contribution Percentage for the 2024 Benefit Year .
Centers for Medicare and Medicaid Services. Final Contract Year (CY) 2024 Standards for Part C Benefits, Bid Review, and Evaluation .
By Elizabeth Davis, RN Elizabeth Davis, RN, is a health insurance expert and patient liaison. She's held board certifications in emergency nursing and infusion nursing.
- Ironstream for Splunk®
- Ironstream for ServiceNow®
- Automate Evolve
- Automate Studio
- Assure Security
- Assure MIMIX
- Assure MIMIX for AIX®
- Assure QuickEDD
- Assure iTERA
- Syncsort MFX
- Syncsort Optimize IMS
- Syncsort Optimize DB2
- Syncsort Optimize IDMS
- Syncsort Network Management
- Syncsort Capacity Management
- Spectrum Context Graph
- Spectrum Global Addressing
- Spectrum Quality
- Trillium Discovery
- Trillium Geolocation
- Trillium Quality
- Data360 Analyze
- Data360 DQ+
- Data360 Govern
- Spectrum Spatial
- Spectrum Spatial Routing
- Spectrum Spatial Insights
- Spectrum Global Geocoding
- Spectrum Enterprise Tax
- MapInfo Pro
- Precisely Addresses
- Precisely Boundaries
- Precisely Demographics
- Precisely Points of Interest
- Precisely Streets
- PlaceIQ Audiences
- PlaceIQ Movement
- EngageOne Communicate
- EngageOne RapidCX
- EngageOne Digital Self-Service
- EngageOne Vault
- EngageOne Compose
- EngageOne Enrichment
- Precisely Data Integrity Suite
- Precisely APIs
- Precisely Data Experience
- Customer engagement
- Digital self-service
- Digital archiving
- Email and SMS
- Print to digital
- Data enrichment
- Data integrity
- Environmental, social and governance (ESG)
- Data integration
- Security Information and Event Management
- Real-time CDC and ETL
- IT Operations Analytics
- IT Operations Management
- Cloud data warehousing
- Data governance
- Data catalog
- Data products
- Data quality
- Address validation/standardization
- CRM & ERP data validation
- Customer 360
- Data matching & entity resolution
- Data observability
- Data reconciliation
- Data validation and enrichment
- IBM systems optimization
- Geo addressing and spatial analytics
- Spatial analytics
- Geocoding and data enrichment
- Master data management
- Process automation
- Amazon Pinpoint
- Compliance with security regulations
- Security monitoring and reporting
- High availability and disaster recovery
- Data privacy
- Access control
- IBM mainframe
- Sort optimization
- Microsoft Azure
- SAP process automation
- Excel to SAP automation
- SAP master data management
- SAP finance automation
- Financial services
- Telecommunications
- Precisely Strategic Services
- Professional services
- Analyst reports
- Customer stories
- Infographics
- Product demos
- Product documentation
- Solution sheets
- White papers
- IBM i security
- Location intelligence
- Master Data Management
- SAP Automation
- Financial service and banking
- Supply Chain
- Global offices
- Careers and Culture
- Diversity, Equity, Inclusion, and Belonging
- Environmental, Social, and Governance (ESG)
- Global Code of Conduct
- Precisely Trust Center
- Press releases
- In the news
- Trust ’23
- Get in touch
Blog > Data Enrichment > The Emergence of Cost-Per-Visitor and What Marketers Need to Know

The Emergence of Cost-Per-Visitor and What Marketers Need to Know
Location data allows businesses to understand consumer behavior, drive sales, and inform decisions in incredible ways. However, the technology needs for accurate location intelligence are exceedingly complex. Like a Russian doll, there are multiple layers beneath the surface – all working together to collect and interpret massive amounts of data, and determine the best way to deploy intelligence in a dynamic and ever-changing world.
Admittedly, new technologies are inherently complex. Their norms have not been established, and standards compete for consensus. Companies package products in a noble effort to provide a simple interface to promising, powerful, and complex capabilities.
One recent model we’ve taken note of is Cost Per Visit (CPV). On the surface, it seems like a simple way to use location – but when you peel back the layers, there’s a lot that is not immediately clear. The allure of simplicity is concealing some troubling details.
What is Cost Per Visit? CPV is a new metric that aims to charge advertisers only for new store visits that are driven by media. This structure is meant to increase the efficiency of an advertiser’s spend. However, there are many challenges to overcome before CPV can be reliably used as a transactional metric. For now, if you are evaluating CPV, here are three important things to consider:
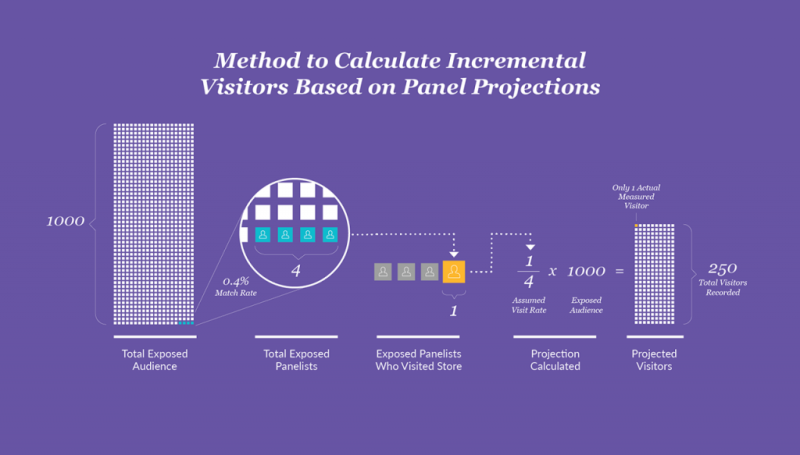
1. Panel projections are used to measure visits – you are not paying for visits, you are paying for projected visits. Current CPV offerings use panel-based projections to validate visitation measurement. While fine for directional insights, limited size panels aren’t ideal when projecting a precise number of visits for locations. This is because panels only measure a very small portion of all visits; the rest of the measured visits (which advertisers are asked to pay for) are assumed to have happened. This all boils down to an alarming fact: advertisers are being charged for projected visits, not actual measured visits.
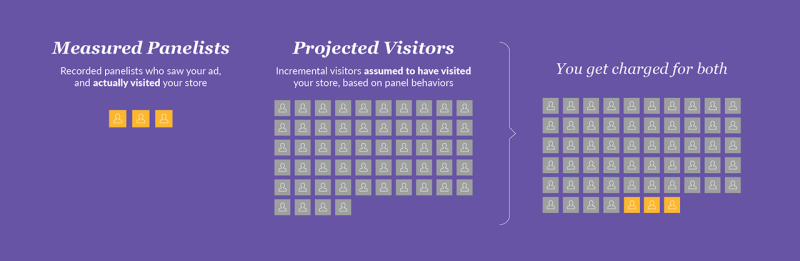
2. Projections account for a majority of visits a media company is taking credit for – between 99.5% and 99.7% of reported visits are projections, not actual visits. Think about it this way – let’s say 1000 people view your ad. With the standard campaign panel match rates we’ve seen (between 0.3-0.5%), that means about 4 panelists (out of the 1,000) will see your ad. If only 1 out of the 4 panelists visited your store, the other 996 ad viewers (non-panelists) would be assumed to visit at the same rate (25%). This means you would be charged for 250 visitors, even though only 1 was measured as a visitor .
3. The control group methodology used to calculate incremental visits is flawed – which means you will pay for visits which would have occurred anyway! To account for an audience’s normal visitation behavior (i.e. loyal customers), it is essential to withhold part of your audience from advertising. This is known as a B control group, and is used as a benchmark to measure expected, predictable behavior. True control groups mirro r the group who do receive ads as closely as possible – typically down to the DMA and demographic level. In addition, a proper B control group will include previous visitation patterns to isolate the incremental visits driven by your campaign. If someone shops at Kroger every week, it would be disingenuous to credit an advertisement with generating their usual weekly grocery run.
Read our Audience Handbook
Precisely PlaceIQ Syndicated Audience Handbook
Read this handbook and explore real-world audiences to discover new and innovative ways to reach high-value consumers.
Unfortunately, available CPV offerings do not use well planned B control groups. This means they are reporting inflated visitation metrics, and advertisers are being charged for visits that would have occurred normally. Think of it this way – let’s say you target frequent store visitors . A portion of this group would have visited anyways – because that is their typical behavior. Without a proper control group in place to account for this, the advertiser will end up paying for normal visits , instead of just incremental visits.
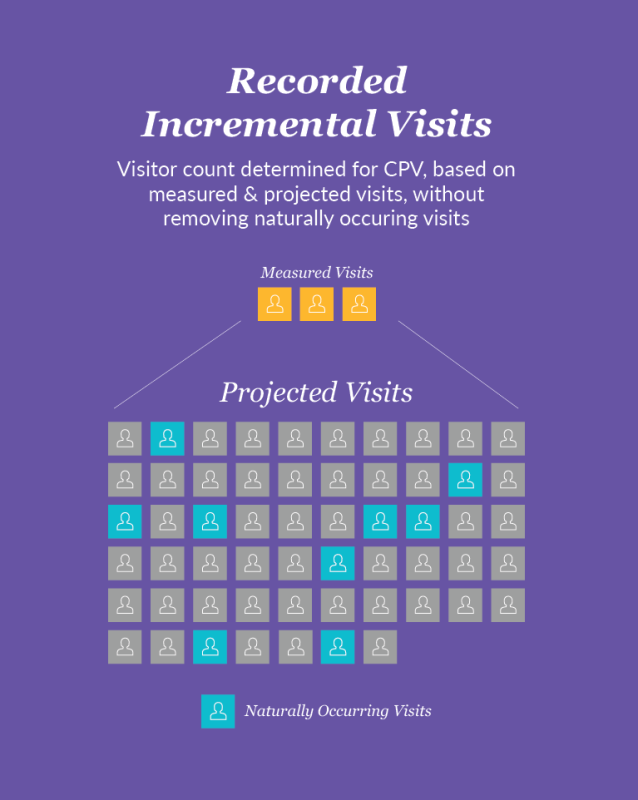
To summarize; with a CPV model as it exists today, you are paying for projected visits, based upon a panel that measures only 0.3% to 0.5% of your audience. To make matters worse, those visits likely aren’t incremental and we have no way of determining ad-driven visits since a true B control isn’t used.
Think of it this way: Would you pay Google for 1000 clicks, after 3 clicks occurred?

Would you declare the winner of a marathon after 138 yards?
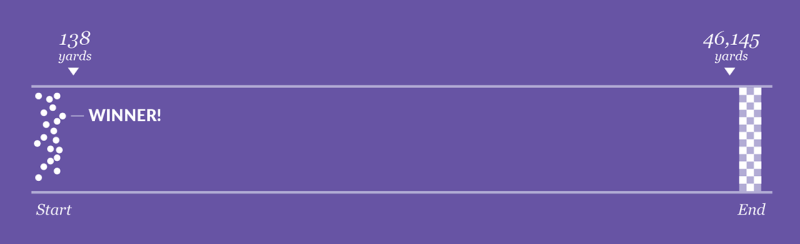
If you answered no to either of these, then CPV probably isn’t for you, as current approaches in-market use the same type of projections.
While one day a proper and accountable CPV system may exist, the structural realities of available data are the natural gating factor. As such, marketers should consider CPV to still be in its primitive stages, with many challenges to address before it can be a reliable metric to transact against. For those testing the waters, it is important to dig deep with your vendor, ask questions, and understand their underlying approach. This will enable you to make the best decision for your campaign, your budget, and your brand.
To learn more, read our Precisely PlaceIQ Syndicated Audience Handbook and explore real-world audiences to discover new and innovative ways to reach high-value consumers.
This post originally appeared as a contributed article on AdAge.com .
Read this audience handbook and explore real-world audiences to discover new and innovative ways to reach high-value consumers.
Related posts

Build the Context You Need Around Your Data
Chances are, we’ve all heard the story of the lighthouse and the naval vessel, in which the captain of a large ship sees a light in the distance and transmits a command that the smaller vessel...

New Year’s Resolutions and Gym Deals: A Catalyst for Changing Consumer Behavior
Consumers kick-started the year by building more health-focused habits, with nearly a 5% increase in visits to gyms and grocery stores, while interest in less healthy options like convenience stores...

B2B Data Enrichment for Beginners
Your competitors use data to target your customers, discover unmet needs, and explore new markets. If you’re not using data to your advantage, you risk falling behind the rest of the pack. In a...

- Industry News
- Law & Malpractice
- Coding & Documentation
- Practice Management
- Patient Engagement & Communications
- Billing & Collections
- Staffing & Salary
A Metric to Quantify the Cost of Patient Visits
What is time-driven activity based cost accounting and how does it help your practice understand the cost of seeing a patient?
One of my favorite questions to ask is “how much does it cost to see a patient?” I know it's a generic question, but it is a starting point for today’s medical practice. Understanding the cost of doing business is essential with value based and other payment models emerging.
The simple way to start is to identify total visits (all E&M codes) for a period and divide by total expenses (typically without the physician). If you have 6,250 annual visits as a solo provider and your total costs are $365,761, the cost per visit is $58.52. You can then decide to break this down further for new patients vs. established patients. Or you could chose to identify costs per total relative value unit, tRVU.
There are other options as well. Eventually you will want to break the cost idea into smaller, workable parts.
One of the most interesting approaches is to identify how much it costs for each category of care provided in the patient visit cycle (e.g., check in, triage, provider time, follow up, and check out). You can look at the cost associated with the triage area: Vital signs, questions on prescriptions, documentation for the visit, and the like. Let’s assume that it takes 10 minutes for this to occur.
If you are paying the medical assistant $15.00 an hour and there is a $2.00 additional cost per hour for benefits, the total cost per minute needs to be calculated. At 2,080 hours worked per year, the total cost at $17.00 per hour would be $35,360. The total minutes worked would be $124,800. The cost per minute is $0.28. The cost for triage is $2.80 just for time. Add in the direct cost for supplies and allocate costs for space and equipment, and it adds up. If this process is done for each category of service in the cycle you gain a better understanding of the cost for the visit. Once this is understood, you can begin to ask if there are activities done at the time by the right individual and is it worth the cost of doing that activity. Further, is it best to do that activity at that time.
This approach is called time-driven activity based cost accounting (TBABC). It may seem like a lot of work but in our experience an exercise of this nature creates an awareness that results in improving the management of the patient visit cycle. The improved management of that flow produces several options for management to consider.
First, the support is more efficient for the provider which allows the provider to spend more valuable time with the patient, either relationship building or specific to the treatment plan development. More efficiency may lead to seeing one additional patient per day for that provider, which will net at current Medicare rates additional income of ~$18,000 with very little expense. Better control of staff time leads to reduction in overtime. Better control of all times contributes to all getting out of the office on time, which leads to a better work-life balance.
Step one is to accept that there is a need to understand the cost of providing service to the patient. Once a basic understanding is arrived at, taking a page for other industries, utilizing TDABC, as initially complex as it may seem is an effort that produces some important results.

Time-sensitive threats to physicians wealth: Spring 2024
Don't wait! Make sure your wealth is protected.

Asset Protection and Financial Planning
Asset protection attorney and regular Physicians Practice contributor Ike Devji and Anthony Williams, an investment advisor representative and the founder and president of Mosaic Financial Associates, discuss the impact of COVID-19 on high-earner assets and financial planning, impending tax changes, common asset protection and wealth preservation mistakes high earners make, and more.

Putting fun in the practice: Hire for attitude, train for skills
Health care could use some hiring tips from Southwest Airlines.

Avoiding Claims Denials in Your Practice
Physicians Practice® spoke with Terry Blessing III, Senior Vice President of Client Development at VisiQuate, about how practices can work to reduce the likelihood of encountering denied claims.
9 Tips for collecting from patients
Collecting copayments and coinsurance can be challenging.

Why providers need to consider generational differences in the payment process
Generation Z is driving changes to patient engagement and payment.
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

Cost Per View (CPV)
Assess engagement.
CPV offers insights into how well the video resonates with the audience.
Expand Reach
A lower CPV aids in extending awareness campaigns to a larger pool of people.
Spot Issues
An uptick in CPV is a red flag calling for immediate changes in the campaign.
Client Reports
Low CPV metrics highlight the effective use of budget in reports and dashboards.
Why Cost Per View Is Important
Cost per View serves as a precise measure of the financial efficiency of any video advertising campaign, including Facebook Ads, YouTube TrueView video ads, programmatic ads, and more.
When budgets are constrained, knowing the Cost per View offers a direct metric for evaluating how well advertising spend translates into actual views.
Furthermore, a low Cost per View often indicates more than just cost-effectiveness; it points to the video's relevance and appeal to the target audience.
Stop Wasting Time on Reports. Get Marketing Insights Faster & Drive Results.
How CPV Interacts with Other KPIs
CPV frequently operates in concert with Total Video Views, Click-through Rate (CTR), and Conversion Rate. A campaign with a low CPV but a high CTR often means that the video content captures attention cost-effectively and persuades viewers to take the next step.
Because the max CPV bid directly impacts ad rank, consider CPV alongside Return on Advertising Spend (ROAS) or Customer Lifetime Value (CLV). These advertising metrics provide a more holistic view of campaign performance and maximize the use of an advertising budget. For example, if a video ad doesn't contribute to a satisfactory ROAS, then the maximum CPV bid should likely be reduced.
Video is the ultimate first impression for a product, brand, or concept! You can share more information more effectively and creatively, driving significantly more engagement than any text or static visual.
How To Calculate CPV
Understanding CPV helps determine whether the investment in a particular video ad is justified by the audience engagement it generates. To calculate Cost per View, take the total cost of the video advertisement and divide it by the total number of views it receives.
CPV Formula Example

What Is a Good CPV?
A good average CPV for video ads typically ranges between $0.10 and $0.50 for most industries. At this level, the video advertisement is not only reaching a broad audience but doing so cost-effectively.
What Is a Bad CPV?
CPV figures above $0.60 for video ad campaigns are generally considered high , suggesting that the ad is not resonating with the target audience or that ad placement needs refinement to improve efficiency.
How To Set CPV Benchmarks & Goals
Because industry or platform CPV calculator averages can be misleading, agencies often rely on past video campaigns to set future CPV benchmarks. By examining historical data across multiple campaigns or clients, they better predict a realistic Cost per View for similar campaigns.
Digging Deeper into CLV Data
To dig out more granular insights into Cost per View performance, consider segmenting data by viewer demographics, device types, or time of day. This allows for tailored adjustments to specific campaign elements.
Report Smarter, Not Harder.
Better, faster & easier client reports are just a few clicks away, why cpv matters to clients.
Cost per View offers a transparent way to track the effectiveness of a video advertising campaign by placing a value on each time users watch an ad. Clients are particularly interested in CPV because it tells them how much bang they get for their advertising buck and the maximum amount they are willing to pay for a view of a video ad.
A low CPV translates to how much less the advertisers pay to reach a broader audience. This is especially compelling when comparing Cost per View with other forms of advertising, like Cost per Thousand (CPM), where costs can escalate quickly without achieving the same level of engagement. CPV provides a straightforward way to link budget spend directly to the number of views, making it easier to evaluate the ROI of the campaign.
Why CPV Matters to Agencies
Agencies see CPV as a dynamic tool for campaign and video ad optimization. They use CPV to tailor targeting options according to the specific objectives of the campaign to reach engaged viewers in the most cost-effective way possible.
For example, if the goal is to raise brand awareness, agencies focus on lowering Cost per View on in-stream ads to reach broader audiences. On the other hand, if the goal is lead generation, agencies may be willing to accept a higher max CPV bid on a particular video ad if it means reaching a more qualified audience.

Save Time and Money By Automating Your Client Reporting
Cost per View Analysis & Reporting Best Practices
Analyzing CPV helps sharpen the focus and efficiency of a video ad campaign. This deeper understanding equips advertisers to tweak various components for better results.
CPV Over Time
Examining CPV over a specific time frame allows for an accurate evaluation of online advertising performance and to understand how seasonal trends or particular events influence Cost per View.
CPV by Channel
Evaluating CPV across different platforms or channels. From YouTube Ads to Facebook Ads to StackAdapt, each channel may offer a different pricing model–as well as unique targeting options–which impact the CPV averages.
CPV by Campaign
With CPV advertising, not all campaigns are created equal. Comparing Cost per View across various campaigns helps identify which strategies are more cost-effective than others, especially when measured against other pricing models like Cost per Impression.
CPV Audience Insights
CPV marketing data also varies across audience segments. Identifying which demographics, geographics, or interest groups respond better to ads helps advertisers refine targeting, potentially lowering Cost per View and elevating engagement.
Put CPV in Context
When a video ad campaign is in play, it's vital to contextualize Cost per View with other performance indicators. Say a user watches an in-stream ad; what actions do they take afterward? Just like other forms of online advertising, a completed view should be a gateway to further engagement.
Visualize CPV Performance
Graphics and charts show how well a video ad or series of CPV ads are performing. These visuals illustrate trends over time or how Cost per View varies when a user views content across different platforms. This makes it easier for clients to grasp the impact of their ad spend.
Facebook Ads Dashboard Example
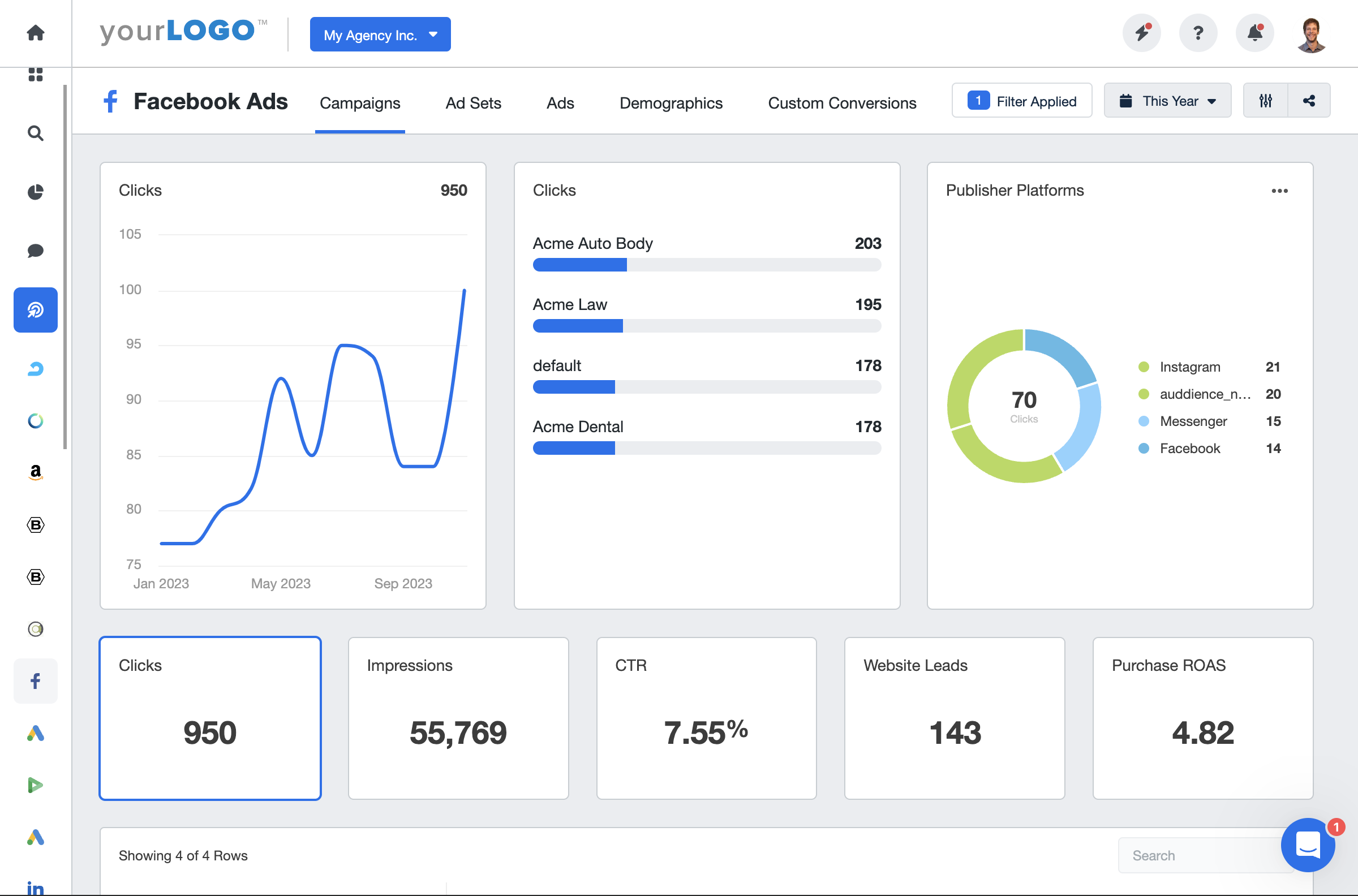
Related Integrations
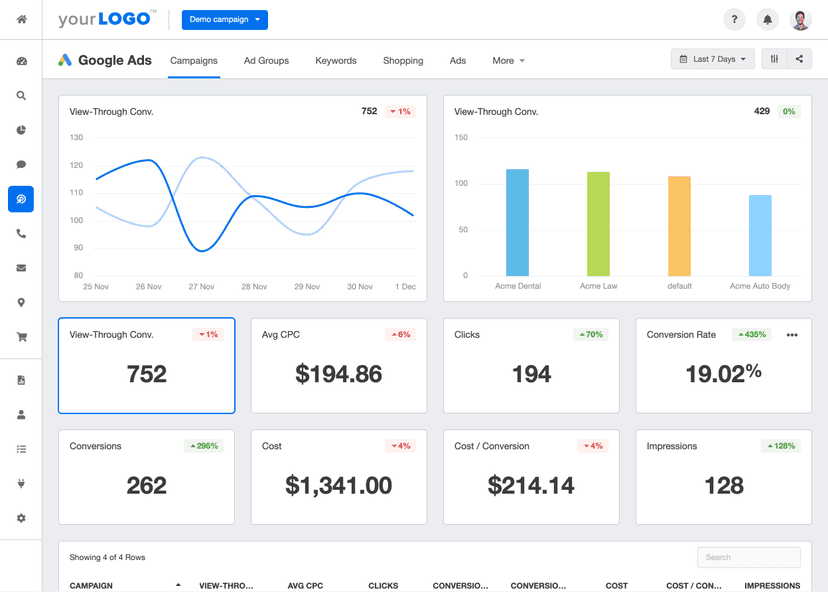
How To Improve Cost Per View
Improving Cost per View isn't just about cutting costs but maximizing impact. Here are some actionable tips to lower CPV and enhance the efficiency and reach of video campaigns.
Refine Targeting
Pinpoint the audience more effectively. Utilize demographic data, dayparting, and audience interests to reduce wasted views and thus lower the CPV.
Test Creative Elements
Don't settle for the first video. A/B test variations in visuals and messaging to discover what really captivates the audience and encourages more cost-effective views.
Check Ad Placements
Not all ad locations are created equal. Evaluate where ads are displayed and cut out the less effective placements to improve CPV.
Related Blog Posts
The Ultimate Agency Guide to Video Ads Marketing
Ready to take your agency’s video marketing strategy to new heights? This comprehensive guide has got you covered! Learn how to create attention-grabbing video ads, pinpoint your target audience, and measure your campaign’s success. Let’s dive in and supercharge your video ads marketing game today.
YouTube SEO: A How-To Guide for Ranking Videos
In this guide, we’ll walk you through some SEO tips, from keyword research to video content creation, and show you how to use end cards, descriptions, and hashtags for the best results.
Powerful Programmatic Advertising Strategies For Your Clients
Looking for best practices for your programmatic advertising? Read these so your agency runs its programmatic campaigns more smoothly, and ensure that they reach their intended audience for your clients.
Agency Growth Tips, Delivered to Your Inbox.
The must-have reporting software for agencies. AgencyAnalytics has revolutionized our client reporting. I couldn’t recommend it enough.

ProVance Media
You wouldn’t think the little things make that big of an impact, but AgencyAnalytics has fundamentally changed our internal process for the better.

Squeeze Marketing
AgencyAnalytics has saved us hours every month in reporting time. Now we can provide far more thorough reporting for our clients, and it’s faster and easier to pull together. It also gives our agency a much more professional touch.

OhMyDigital
See More KPI Examples
Cost per thousand (cpm).
Cost Per Thousand (CPM) represents the cost an advertiser pays for 1,000 impressions of an ad.
Cost Per Lead (CPL)
Cost Per Lead (CPL) is a digital marketing metric that quantifies a company's cost to acquire a new lead.
Conversion Rate
Conversion Rate measures the percentage of leads or visitors to a website or application who take a desired action, such as making a purchase or filling out a form.
Return on Ad Spend (ROAS)
Return on Ad Spend (ROAS) calculates the total revenue generated for each dollar spent on advertising.
Cost Per Acquisition (CPA)
Cost per Acquisition (CPA) calculates the average spend on advertising for acquiring one customer.
Cost Per Reach
Cost Per Reach refers to the cost of reaching each individual in a target audience during an ad campaign.
Get Started for Free
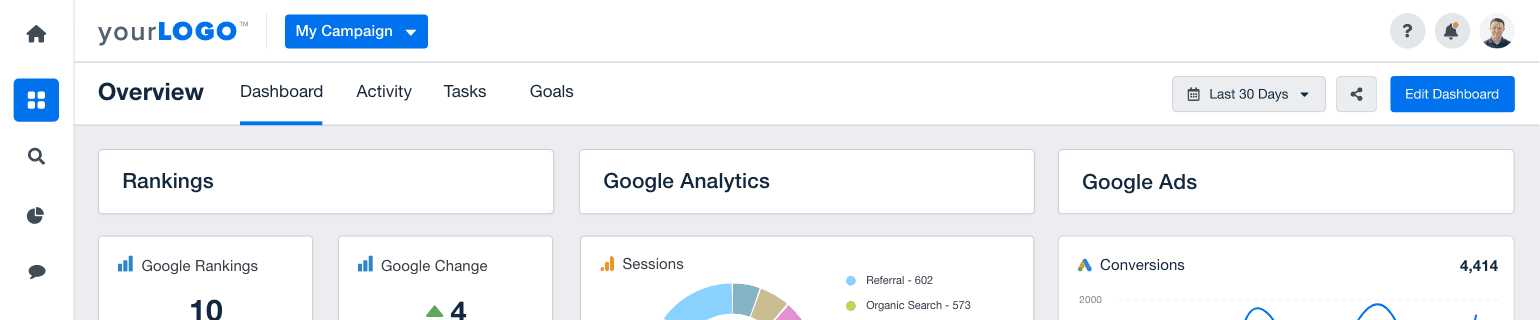
- KPI Examples
Cost per view (CPV)
The cost per view is an important PPC metric helping you have an idea of your advertising costs per number of views.
TRACK YOUR COST PER VIEW!
Templates using this KPI
Integrations using this KPI
What is cost per view?
The cost per view (CPV) , also called average CPV, CPV cost or cost per completed view CPCV is a video marketing term used to know the cost per completed views. It’s a pricing model for video campaigns where you pay for a view of your video ad. A view is counted when a viewer watches at least 30 seconds of your ad (or the complete duration if shorter) or if the viewer interacts with the ad.
How to calculate cost per view
To calculate CPV, divide the cost of a video advertisement by the total number of views. For example, if you spend $5,000 on your video ad campaign and your total number of views is 10,000, then the CPV is 5,000/10,000= .05
Cost per view formula (CPV calculator)
Cost per view = total cost / number of views
What is a good cost per view?
A good average cost per view goes anywhere between 3 cents to 30 cents per view, of course, it all depends on the industry, the campaigns, the type of video ad you have, etc.
What is a bad cost per view?
A bad cost per view would probably be more than what your advertising budget allows. Keep in mind that a view is not a sale, so if you’re doing video ads to get conversions, cost per views are not your number one metric to track and the cheaper the better. However if you track cost per views for your brand awareness, the question to ask yourself is how much you’re prepared to pay for each pair of eyes to look at your ad.
Cost per view best practices
Optimize your cost per view with these best practices.
Track alongside other metrics
It’s important to track other digital marketing metrics alongside your CPV such as cost per mille (CPM) click-through rate (CTR), average cost, cost per click, average CPM, ad spend, and conversion rate. This way you can have a better overview of what works best and why. For example a video ad campaign can have a very low cost per view, but also a very low click-through rate, or low video views which doesn’t mean great results for your bottom line.
Optimize your video ad campaigns
Make sure your video advertising campaigns are directed to the right target audience and demographic, that you have a good call to action, that the format works well for the type of ads, that you optimize the landing page etc. Make sure you also post ads on the right channels from display ads to social media, YouTube, Adwords, google search display network, Linkedin, so that a large number of people from your target audience can be reached.
Take brand awareness into consideration
When it comes to video views, brand awareness is one of the major components. So of course the cost per view in that case is even more important than the cost per click (CPC). Online advertising is filled with different metrics and you may be tempted to only take ROI or clicks as performance indicators to know if your ads worked. In the case of video views however, having eyes on your ad is just as important, so this metric should be used with brand awareness in mind.
Want to track all your KPIs in one easy-to-use dashboard?
Ressources about cost per view
Learn to use this kpi in our help center.
- How to create a dashboard with Google Ads?
- How to create reports and dashboards using Bing Ads (Microsoft Advertising)?
- How to create an Instagram Ads dashboard?
- How to create a dashboard using Facebook Ads?
Read about this KPI on our blog
- A Quick Guide to PPC Metrics
- 7 PPC KPIs You Should Be Tracking
KPIs you may also like
Conversion Rate
Customer lifetime value (CLV)
Customer acquisition cost (CAC)
Return on marketing investment
Traffic sources
Cost per acquisition (CPA)
Cost per lead (CPL)
Unique visitor
Bounce rate
Average time on page
Keyword Difficulty
Domain rating
Domain authority
Referring domains
Get Started Today!
Made in Canada
DashThis is a brand owned by Moment Zero inc
Copyright © 2011-2024
DEMYSTIFIED
Average cost per visitor.
Visitor acquisition costs often spiral out of control when left untracked. While tracking these costs can be difficult in the long run the effort is worth it.
Definition A function of the total sum of marketing costs, the average cost per visitor is defined as:
Total Acquisition Marketing Costs / Visitors = Average Cost per Visitor
For most companies the tricky piece is summing acquisition marketing costs, owing to the fact that few companies are accurately tracking these numbers on anything more granular than a quarterly basis. It is recommended that you limit the summation to online marketing activities only unless you strongly brand your URL in offline marketing materials. By adding up the costs of search, email, banner, partner and feed-based marketing activities a fairly useful KPI can be generated. This indicator is a good candidate for segmentation by marketing channel. For example, you may want to calculate the average cost per visitor for your email, banner and search based marketing efforts.
Presentation Because this KPI is dollar-based little usually needs to be done regarding presentation to attract stakeholder interest. Especially if the average cost per visitor is high, most executives and managers will pay close attention to this indicator.
Expectation Ideally visitor acquisition costs are low and contribute to a well-run, high margin business. Unfortunately the ideal case is rarely observed. It is worthwhile to set the expectation that the company will work diligently to lower visitor acquisition costs and carefully critique each marketing channel.
Action If cost per visitor suddenly increases it is worthwhile to compare this increased cost to average revenue per visitor and relevant conversion rates. If cost per visitor is going up but revenue or conversion are flat or decreasing something has gone awry. The converse is also true: if your acquisition costs drop suddenly you want to make sure that this fortuitous event has not happened at the expense of revenue or other measured value.
Leave a Reply Cancel reply
Discover more from analytics.
Subscribe now to keep reading and get access to the full archive.
Type your email…
Continue reading
Effective Cost Per Visit (eCPV)
What is effective cost per visit (ecpv).
Effective Cost Per Visit (eCPV) is calculated by dividing the total store revenue during a given period by the number of visitors for that same period. For example, if a store had 10,000 visitors driven from its location-based marketing efforts and the store’s revenue for the same period was $100,000, then the eCPV would be $10.
Learn how you can improve your eCPV with GroundTruth’s groundbreaking CPV marketing solutions and only pay when a visitor actually visits your store from an advertisement.
Sign up for Ads Manager
Learn how to buy and manage all of our available advertising products in our easy-to-use self-serve platform.
Subscribe to our Newsletters
Stay on top of the latest location marketing news, strategies, tips and tricks.
See what location can do for you.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Health Care Financ Rev
- v.16(1); Fall 1994

Do Preset per Visit Payment Rates Affect Home Health Agency Behavior?
This article reports on preliminary impacts during the first year of a demonstration in which home health agencies (HHAs) were paid a prospectively set rate for each Medicare home health visit rendered, rather than being reimbursed for costs. Forty-seven agencies in five States participated. The evaluation compared the experiences of randomly assigned treatment agencies and their patients with those of control agencies and their patients and found no compelling evidence of any demonstration impact on agency cost per visit, the volume of home health services, agency revenue and profit, patient selection and retention, quality of care, or use and cost of Medicare services.
Introduction
In recent years, home health care has been the fastest growing Medicare benefit. Medicare home health spending was estimated at $10.2 billion in fiscal year (FY) 1993—a 42-percent increase over FY 1992 and a 298-percent increase over FY 1989 ( U.S. House of Representatives, 1993 ).
As one of its many initiatives to make provision of Medicare services more cost effective, HCFA has implemented a demonstration program of prospective payment for home health care. The major goal of introducing prospective payment to home health care is to minimize public expenditures by providing care more efficiently while ensuring that access to care and the quality of care are adequate.
During the first phase of this demonstration, participating agencies were paid a prospectively determined rate for each home health visit rendered to Medicare beneficiaries. Under the second phase of the demonstration, agencies will be paid a prospectively determined rate for each episode of home health care they render. In both phases of the demonstration, agencies retain most of any reasonable surplus of payments over costs and are at risk for shortfalls, giving them a financial incentive to provide home care in a more cost-efficient manner than they might under the current method of cost reimbursement. HHAs are currently reimbursed for reasonable costs incurred. Costs are judged to be reasonable if they do not exceed specified limits. During the per visit demonstration, the limits in effect for freestanding agencies were set at 112 percent of the mean cost per visit incurred by all agencies in the same geographic area. The limits for hospital-based agencies were 13 to 16 percent higher than those for freestanding agencies. The limits are applied in the aggregate; costs that are above the limit for one type of visit may be offset by lower costs for another type of visit.
This article reports on our early estimates of the impacts of per visit prospective payment, estimated on data from the first year of the per visit home health prospective payment demonstration. We examine impacts on per visit costs, use of home health services, agency financial performance, selection and retention of patients, and quality of care. These preliminary findings are not necessarily indicative of program impacts during the life of the demonstration.
The Per Visit Demonstration
According to the terms of the per visit demonstration, the prospectively set rates that an agency received for the six types of home health visits covered by Medicare (skilled nursing, physical therapy, occupational therapy, speech therapy, medical social services, and home health aide) were based on the agency's own costs during a base year (the year immediately preceding its entry into the demonstration), adjusted annually for local increases in the prices of inputs required to produce health services.
In recognition of the inverse relationship between volume and average per visit costs for home health services, the demonstration also included provisions to adjust the payment rate downward (from base-year costs) for agencies that grew appreciably and upward for those that shrank. Rates were decreased 1 percent for every 10-per-centage-point increase in the number of Medicare visits rendered (relative to the base year) and increased 1 percent for every 10-percentage-point decrease in the number of such visits. Although research indicates that average cost per visit varies inversely with the volume of home health visits rendered and average cost per visit for home health care, there is considerable uncertainty about their exact relationship. Cross-sectional analyses (which investigate the differences in average cost per visit for agencies that render different volumes of output during a given period and which assume that the underlying cost structure of the home health industry is in economic equilibrium) have generally concluded that smaller agencies experience economies of scale as they grow. However, the results of these studies differ with respect to the magnitude of these economies and the range over which they apply ( Hay and Mandes, 1984 ; Kass, 1987 ; Nyman and Svetlik, 1989 ; Schmitz, 1990 ; Chu, Brown, and Phillips, 1993 ). Longitudinal analyses investigating the relationship between the year-to-year change in the average cost per visit and the change in the volume of output ( Schmitz, 1989 ; Chu, Brown, and Phillips, 1993 ) suggest much larger changes in average cost per visit as volume changes than do the cross-sectional analyses.
The demonstration included provisions for HCFA to share profits and absorb losses that exceeded certain levels. At the end of each year, HCFA shared in any profits greater than 5 percent of an agency's Medicare-allowable cost of providing the prospectively paid services. HCFA also reimbursed agencies for any losses greater than 5 percent of these costs, provided the payment did not exceed the cost limits.
The demonstration also included procedures to ensure that the number of visits rendered was appropriate and that the quality of care was adequate. The number of visits was monitored through a medical review process identical to that under cost reimbursement, and an independent organization reviewed a sample of cases from each prospectively paid agency to assess the quality of care rendered. Forty-seven agencies in the five demonstration States (California, Florida, Illinois, Massachusetts, and Texas) participated in the per visit demonstration for at least 1 year, entering between October 1990 and October 1991, as their FYs began. (Two other agencies dropped out before the end of their first year.) Each agency operates under the demonstration for a total of 3 years; thus, demonstration operations will be completed at the end of September 1994.
As Table 1 indicates, the agencies participating in the demonstration represented a broad mix of HHAs. They operated under a mix of auspices, with most being proprietary. A little more than one-fourth were members of a chain. The majority of demonstration agencies had been in operation for more than 6 years. 1 They predominantly served Medicare patients, and most demonstration agencies offered all six home health services covered by Medicare. The demonstration agencies varied in size, from more than 240,000 Medicare visits during their base year to only 122 Medicare visits during that year. Most of the demonstration agencies had been growing prior to entering the demonstration; more than one-half of them had experienced rapid growth prior to entering the demonstration, increasing the number of Medicare visits rendered by 30 percent or more. Four out of every five of the demonstration agencies had base-year costs that were below the limits, and more than one-third had base-year costs that were less than 85 percent of the limits.
SOURCE: Data on auspice and chain membership were obtained from the demonstration contractor, Abt Associates, Inc. Data on related organizations and years of operation were obtained from the Initial agency survey for the demonstration. All other data were obtained from Medicare Cost Reports. Data are for 26 treatment agencies and 21 control agencies.
The participating agencies were randomly assigned to either a treatment group, which was paid under the demonstration's prospective ratesetting mechanism, or a control group, which was paid under Medicare's normal cost-reimbursement procedure. Because the number of agencies participating in the demonstration was small, the treatment and control groups differed somewhat despite randomization. Although not statistically significant, there were material predemonstration differences between treatment and control agencies that may have affected the outcome we examined, including differences in agency size and costs. Table 1 provides descriptive statistics on treatment and control agencies.
Research Issues
Paying HHAs a fixed, predetermined amount per visit creates a number of incentives. Because agencies retain profits (or surpluses), they will benefit from selecting the most efficient way to deliver their services, perhaps altering direct care or administrative operations. Agencies may also want to increase the volume of services rendered to benefit from economies of scale. In addition, agencies that are able to reduce their costs below the per visit payment have an incentive to increase the number of visits provided because each visit generates additional net revenue.
Patient care may be affected by these incentives. The fixed rate of payment per visit could encourage agencies to avoid or drop certain patients who require lengthy or expensive visits or to make operational changes (such as requiring staff to make more visits per day or reducing supervisory staff) that might result in a poorer quality of care and, perhaps, in higher use of other Medicare services. On the other hand, an increase in volume of visits rendered could lead to better care for beneficiaries and, as a result, could reduce the use of other Medicare services.
Thus, a full understanding of the effects of prospective ratesetting for home health care requires that a number of potential program outcomes be addressed. In this article, we examine data from the first year of demonstration operations to test hypotheses about the possible effects of prospective ratesetting on:
- Cost per visit, by type of visit and type of cost.
- The use of home health services (including the volume of visits rendered by agencies) and characteristics of episodes (including duration, intensity, and number of visits).
- Agencies' net revenues and profits.
- Patient selection and retention.
- Quality of care.
- Use and costs of all Medicare-covered services by agency patients.
We tested a number of hypotheses under each of these areas, most of which stated that prospective ratesetting had no effect on the outcome examined. The only directional hypotheses tested were for cost per visit; these stated that prospective ratesetting did not reduce per visit costs. Many of the specific hypotheses examined will be evident from the tables to be presented.
When data for all 3 years of the demonstration become available, we will examine the same issues for the demonstration in its entirety and will also examine impacts on the use of services not covered by Medicare. (Data on the use of these services were collected only once during the second demonstration year.)
Data and Methodology
The analysis relies on data from many sources and from a number of samples, some of which are based on agency-level data. Most of the agency-level analyses rely on data for the 3 predemonstration years and for the first demonstration year, with the agency-year as the unit of analysis. The number of agency-years for which data were available varies from 134 to 189, depending on the analysis. Other analyses of agency-level data are limited to the first demonstration year only and data for 41 to 49 agencies, depending on the analysis.
Many analyses use data on individual home health patients in the treatment and control agencies during the first demonstration year. For these analyses, the unit of analysis is the home health episode, as defined by agency-reported start and end dates. 2 In general, the number of episodes included varies from 24,366 to 25,339, depending on the analysis.
Our samples are for virtually the entire population of agencies participating in the demonstration and all of the episodes they rendered during the first demonstration year. However, it is useful to consider the statistical power that would be available for testing hypotheses if they were random samples of agencies and episodes. Only substantial differences can be detected with the agency-level data. For cost per visit, a key dependent variable, the unit of analysis is agency-year. For a range of assumptions about the correlation of observations across years and the amount of variance of the dependent variable explained by our regression models, we estimate that we can detect differences in cost per visit of about one-third to one-half a standard deviation, or about 15 to 25 percent of the mean, with 80-percent power. 3 The statistical power of the episode-level analysis is sufficient (even with conservative assumptions) to allow us to detect a difference of approximately 10 percent of the standard deviation of the dependent variable (equivalently, about 5 percentage points in a binary variable) with 80-percent power. 4
Data to construct variables were drawn from a number of sources. A great deal of the data on agencies were obtained from Medicare Cost Reports; Medicare claims constituted the primary data source for the episode-level analyses. Other key data sources included the demonstration-agency survey, home health certification (HCFA 485 and 486) forms, patient intake forms developed for this evaluation, Medicare eligibility file, and reviews of case records by the quality assurance contractor, New England Research Institute (NERI). Some variables also were developed from the Provider of Service File, section 223 limit file, Area Resource File, agency financial statements, and predemonstration agency characteristics data collected by Abt Associates Inc., the technical assistance contractor for the demonstration.
The basic methodology of all of our analyses is to compare the experiences of the treatment and control agencies and their patients to estimate the impact of per visit ratesetting. In virtually all of the impact analyses, we control for differences between treatment and control agencies that arose by chance, using ordinary least squares regression (for continuous dependent variables) and logit analysis (for binary dependent variables). To account for the correlation between observations on a given agency across years in those analyses using the agency-year as the unit of analysis, we estimated two specifications: (1) a fixed-effects model (which controls for time-invariant, agency-specific factors by including a series of binary variables representing agencies) 5 and (2) a random-effects model (which includes an agency-specific component in the error term). The random-effects model provides more precise estimates; however, these will be biased if unmeasured agency characteristics are correlated with treatment status. The fixed-effects model, on the other hand, yields unbiased but less precise estimates.
We present the estimated impacts of per visit ratesetting obtained from our multivariate models. To help put the magnitude of an impact estimate in perspective, we also present the treatment group mean for the demonstration period.
Regardless of the issue examined, we find no compelling evidence that prospective ratesetting had any impact during the first year of the demonstration.
Cost per Visit
Our estimates suggest that prospective ratesetting has not led to lower costs per visit among treatment agencies, for any type of visit, than would have occurred in the absence of the demonstration. This finding holds for both total cost per visit, which includes allocated overhead expenses, and direct cost per visit, which excludes such expenses. Using data from the 3 years preceding agencies' entry into the demonstration and from the year after entry, average cost per visit for each type of visit was regressed on time and treatment-status interaction terms, plus agency and area characteristics. The impacts on costs were estimated from the model coefficients as the predicted difference between treatment and control agencies in the change in average cost per visit between the 3-year predemonstration period and the postdemonstration year, controlling for the various agency and area characteristics.
The findings are not sensitive to the econometric specification used to account for the correlation of an agency's costs across years (that is, a random- or fixed-effects model) nor to the set of control variables used to account for possible pre-existing differences between treatment and control agencies. Because there were material predemonstration differences between the treatment and control agencies in agency size and costs, we included concurrent measures of volume and case mix as control variables in some of the models. Concurrent measures of volume and case mix could be affected by treatment status, however, and their inclusion could possibly bias our estimates of the full impact of prospective ratesetting. Therefore, we also estimated models that included only predemonstration agency characteristics as control variables.
Of the 48 estimates obtained (6 visit types, 2 types of costs, 2 sets of control variables, and 2 econometric specifications), none was significantly different from 0. Furthermore, the estimates were as likely to show a cost increase as they were to show the hypothesized cost decrease. To illustrate, Table 2 presents impact estimates for total cost per visit for each of the six visit types from the fixed-effects model, excluding control variables for volume and case mix.
NOTES: Numbers in parentheses are t -statistics. The estimated impact of per visit ratesetting is computed as the expected value of the treatment-control difference in the demonstration year minus the average treatment-control difference in the predemonstration period, estimated from the coefficients of the fixed-effects model. The unit of analysis is the agency-year. The sample size varies by type of visit (not all agencies offered all types of visits). The maximum number of agency-years is 189, and the minimum is 134. The maximum number of agencies in any given year is 48 (27 treatment and 21 control), and the minimum is 32 (19 treatment and 13 control).
SOURCE: Authors' calculations from Medicare Cost Report data.
Use of Home Health Services
The opportunity to retain savings and the greater risk of losses under prospective payment provide treatment agencies with incentives to reduce their cost per visit by shifting the total volume toward a more efficient level and to increase net revenue by shifting toward the types of visits or patients for which profit margins are the greatest. In general, the incentives are to increase the volume of visits rendered. However, because prospective rates are set at the agency's own base-year average cost, different shifts in volume may be appropriate for different agencies, depending on their own size and cost structures.
Despite the incentives under the demonstration, we find no compelling evidence that during the first demonstration year treatment agencies have either increased or decreased total visits, Medicare visits, or Medicare visits as a proportion of total visits, relative to control agencies. This finding is not sensitive to the econometric specification (that is, a fixed- or random-effects model) nor to the set of control variables. Some models included only predemonstration agency and area characteristics. Other models included variables describing the mix of patients served by each agency during the first demonstration year. To illustrate, Table 3 presents impact estimates for Medicare visits for each of the six visit types from the random-effects model, controlling for predemonstration agency characteristics and case mix during the first demonstration year.
NOTES: Numbers In parentheses are t -statistics. The unit of analysis is the agency-year. The sample size varies by type of visit (not all agencies offered all types of visits). The maximum number of agency-years is 189, and the minimum is 138. The maximum number of agencies in a given year is 48 (27 treatment and 21 control), and the minimum is 32 (19 treatment and 13 control).
Treatment agencies appear to have treated their patients differently, or served a different mix of patients, than did control agencies. After controlling for observed differences in patient characteristics, agency predemonstration behavior concerning episode duration and intensity, and agency characteristics, we estimate that the patients of treatment agencies received significantly fewer visits per episode and significantly more visits per week than did the patients of control agencies, although the duration of episodes did not differ for the two groups ( Table 4 ). Given the lack of evidence of program effects on total agency volume and the demonstration incentive to increase the number of visits, it is difficult to plausibly explain how prospective rate-setting might be responsible for a reduction in visits per episode. Moreover, these estimates are internally inconsistent Visits per episode equals visits per week multiplied by episode duration (in weeks); therefore, the estimated percent change in visits per episode should equal the estimated percent change in duration plus the estimated percent change in visits per week. Our results controlling for patient characteristics, predemonstration behavior, and agency characteristics, however, indicate a sizable percent reduction in visits per episode (-9.5 percent), which is not consistent with the small percent reduction in duration (-3.4 percent) and the increase in visits per week observed (+2.8 percent). Finally, the sign of the estimate on visits per week is sensitive to the control variables included in the model, reversing direction when agency characteristics were added.
NOTES: Numbers in parentheses are t -statistics. The sample size Is 25,339 (19,029 treatment and 6,310 control) episodes.
SOURCE: Authors' calculations from Medicare claims data.
Given the anomalies, we conclude that the estimated treatment-control differences are probably not due to the effects of prospective payment. They are more likely to result from failure of the regression models to accurately reflect the true effect of observed preexisting differences on outcome measures or unmeasured predemonstration differences between treatment and control agencies or their patients.
Agency Revenues and Surplus
We also found no evidence that agencies increased their revenues or probability of generating a surplus (equivalently, a profit for the for-profit agencies) as a result of the demonstration. This finding is not surprising, given the absence of any demonstration effects on costs.
The overall pattern observed during the 4-year period examined is one of change and uncertainty. Revenues increased rapidly during the predemonstration period, and about one-half of the 41 non-hospital-based agencies lost money on their overall (combined Medicare and non-Medicare) operations during that period. (Hospital-based agencies do not report revenues separately for their home health business; therefore, they were excluded from this analysis.)
Prospective ratesetting does not appear to have induced treatment agencies to change the mix of their Medicare and non-Medicare business during the first demonstration year. The regression-adjusted mean proportion of visits paid for by Medicare is 62 percent for the control group, compared with 64 percent for the treatment group.
Although both treatment and control agencies fared somewhat better during the first demonstration year than during the preceding years, more than one-third of all agencies lost money on their overall operations during that year. Controlling for agency and area characteristics, logit analysis indicates that control agencies were slightly more likely to have generated an overall surplus (70 percent, compared with 59 percent for treatment agencies), but the difference was not statistically significant Because HHAs cannot generate a surplus on Medicare-covered visits under the current cost-reimbursement system, any surplus realized by control agencies during the demonstration period (and by all agencies during the predemonstration period) came solely from their non-Medicare business and other sources of income.
As Table 5 indicates, treatment agencies may have been somewhat more likely than control agencies to reduce their costs relative to their predemonstration level, after adjustment for inflation and any change in the volume of visits rendered. 6 Controlling for agency and area characteristics, logit analysis indicates that about one-half (48 percent) of the treatment agencies generated surpluses on their Medicare business by holding per visit costs below their adjusted base-year rates, whereas only 29 percent of the control agencies did so. (This difference is statistically significant at the 0.10 level.) The ratio of demonstration costs to adjusted base-year costs, however, was much more variable for treatment agencies. Also, as described above, we found that the control agencies were more likely to have overall surpluses, and that prospective rate-setting did not reduce per visit costs significantly. Taken together, these results suggest that treatment agencies may have been somewhat successful in holding cost increases for their Medicare operations below those experienced by control agencies, but the difference, if any, was slight.
NOTES: Numbers in parentheses are t -statistics. Control agencies did not earn surpluses from Medicare home health visits. However, we have adjusted their base-year per-visit costs for inflation and change in volume to estimate the per-visit rates they would have received if they had been paid prospectively according to the procedures used to pay treatment agencies and then computed their hypothetical revenues and surpluses under these rates.
SOURCE: Authors' calculations from Medicare Cost Reports from 48 agencies (27 treatment and 21 control) for the first demonstration year.
Patient Selection and Retention
Although financial incentives exist for treatment agencies to avoid serving or to drop patients who are particularly costly to serve, we found no compelling evidence of these behaviors. This issue is of particular importance to those considering national conversion to prospective ratesetting, because such behaviors could result in restricted access to home care services for certain types of patients and to greater use of and costs for other health care services, including hospitals and skilled nursing facilities.
We examined the issue of program effects on agencies' selection and retention of patients by comparing the characteristics of patients in the treatment and control agencies. Using logit analysis for the binary dependent variables and ordinary least squares for the continuous variables, each of a series of patient characteristics was regressed on treatment status, controlling for predemonstration agency and area characteristics. The patient characteristics were those associated with the severity of patient condition and with diagnoses likely to require home health visits that are longer (more expensive) or shorter than average. Controlling for predemonstration agency and area characteristics, we also estimated the impact of per visit ratesetting on the number of visits per episode for subgroups of patients having characteristics associated with long visits. We also compared the regression-adjusted proportions of patients who were transferred and who resided in areas that were expensive to serve because the agencies considered them unsafe and provided escorts for staff.
As Table 6 indicates, we found a number of statistically significant differences between the treatment and control groups with respect to patient characteristics. The differences were often small in magnitude, however, and did not always indicate that treatment agencies were more likely than control agencies to avoid high-cost patients. On the one hand, treatment-agency patients were significantly less likely than control-agency patients to have had various types of functional impairments and comorbidities at the beginning of their home health episode. On the other hand, treatment-agency patients were less likely to be clinically stable and to have caregivers.
NOTES: Numbers in parentheses are t -statistics. The sample size is 24,555 (18,402 treatment and 6,153 control) episodes.
SOURCE: Authors' calculations from the demonstration patient Intake form, HCFA certification forms 485 and 486, and Medicare claims.
We found no convincing evidence that patients admitted to treatment agencies were less likely than those admitted to control agencies to require treatments typically associated with long home health care visits. 7 The treatment-control difference was statistically significant for only one of the nine variables examined (intravenous therapy). Furthermore, after controlling for predemonstration agency and area characteristics, we found no treatment-control difference in the number of visits per episode delivered to those patients requiring any of the treatments typically associated with expensive home health visits. Treatment-agency patients were also no more likely than control-agency patients to be transferred to another HHA or to reside in unsafe areas. Thus, we found no evidence that the program incentives induced treatment agencies to “dump” patients who were expensive to serve.
Quality of Care
We found no evidence that the treatment agencies altered their behavior in ways that affect the quality of home health care. Although demonstration incentives could induce agencies to make changes (for example, to reduce the length of visits or amount of supervisor time), such changes, if they occurred, did not result in poorer outcomes for patients of treatment agencies relative to those of control agencies. We also found no evidence that the incentive to increase visits led to improved quality of care by treatment agencies.
No differences between the treatment and control agencies were found in any of the agency structure or process characteristics that might be linked to quality of care. The 18 measures examined reflected nurses' workloads, hiring practices, training procedures, staff competency (based on a federally mandated test for home health aides), changes in care planning, amount of supervision, accreditation, and number of patient complaints. Because we had so few observations on these structure and process measures (44 agencies), this analysis was limited to comparison of treatment and control group means.
In our logit analysis of the six quality assurance review indicators, we observed only one statistically significant difference in quality problems. As Table 7 indicates, controlling for predemonstration agency, area, and patient characteristics, treatment agencies were significantly more likely than control agencies to fail to address all acute problems immediately. However, we observed no significant difference on the key quality assurance variable examined—the existence of confirmed quality problems with the potential to affect patients adversely. 8
NOTES: Numbers in parentheses are t -statistics. The sample size is 650 (407 treatment and 243 control) episodes.
SOURCE: Authors' calculations from New England Research Institute quality assurance review assessments, completed as of November 1992.
Controlling for agency, area, and patient characteristics, we observed no differences between the patients of treatment and control agencies in our logit analysis of post-discharge patient outcome measures: death within 30 days, admitted to a hospital within 30 days for the same or any diagnosis, or readmitted to a HHA within 30 days for the same or any diagnosis.
Use of Medicare-Covered Services
Treatment-agency patients received significantly fewer Medicare-covered services than did control-agency patients during their home health care episodes. Although this difference could have resulted from improvements in the quality of home care under the demonstration, our analysis of quality of care produced no evidence of such an impact. We conclude that the observed difference in the use of Medicare-covered services is due to differences in the case mixes of the two groups of agencies (rather than a program impact), with the treatment agencies having more acutely ill patients and the control agencies treating a higher proportion of chronically ill patients.
Using ordinary least squares or logit analysis and controlling for patient characteristics at home health admission and for predemonstration agency characteristics, we found no significant differences in overall Medicare reimbursements or in hospital use. We did find, however, that treatment-agency patients had significantly lower home health use (and costs), durable medical equipment use, practitioners' service use, and other Part B service costs during their home health care episodes ( Table 8 ). Treatment-agency patients' shorter average length of episode partly explained these differences. When the utilization and cost measures for Medicare-covered services were expressed in terms of per day of episode, to standardize for this difference, we found that relative to control-agency patients, treatment-agency patients had higher Part A and Part B reimbursements per day of episode.
NOTES: Numbers in parentheses are t -statistics. The sample size is 24,396 (18,298 treatment and 6,098 control) episodes.
We conclude from this pattern of shorter episodes and higher cost per day and from the results of the analysis of patient characteristics at admission that treatment-agency patients were more likely than control-agency patients to have an acute problem (such as a broken limb) resulting in the need for a relatively brief home care episode, consisting mainly of nursing or therapy (rather than aide visits), until their recovery. Conversely, control-agency patients appear to have had more functional impairments, increasing their need for aide-intensive home health care over a longer period. This difference in care needs would account for the higher cost per day observed for treatment-agency patients, because aide visits, on average, cost only about one-third as much as nursing or therapy visits.
Limitations and Implications
The findings from this preliminary analysis are limited by the data. Only 47 agencies participated for the entire first year of the demonstration, and only data for the first year of the 3-year demonstration period were available for the study. With the limited number of agencies, there may well be important pre-existing differences between the treatment and control agencies, despite randomization, possibly leading to differences in outcome measures between the two groups that cannot be attributed to prospective ratesetting. Thus, we are more dependent on the statistical models to control for these differences than one might expect in a study with random assignment of participants. The small number of agencies also means that relatively few such variables can be used in the statistical models to account for the effects of these pre-existing differences, and that the parameters of the models cannot be estimated with a high level of precision. Furthermore, in addition to these potential biases in the estimates, one must recognize that there is very little statistical power to detect moderate-size effects of the demonstration on agency-level outcomes of interest, such as costs and profits. That is, even if prospective rate-setting did affect agencies' behavior, the effects would have to be fairly large in order to have a high probability of detecting them with our sample because of the natural variation across agencies. Having data for only the first year of the demonstration also limits the precision of our estimates; more important, prospective ratesetting may have impacts that do not occur or that are not reflected in our outcome measures until after the first year of the demonstration. It is also possible that the impact of per visit ratesetting may differ depending on the characteristics of agencies and patients. For this preliminary analysis, we did not conduct subgroup analyses.
Despite these limitations, our results are reasonably consistent across the different study areas and with the results of our study of agency operations under the demonstration ( Thornton et al., 1993 ). A finding of no demonstration impacts on costs is consistent with our interviews with participating HHAs, in which treatment agencies reported having made few modifications to their operations in response to the demonstration. Thus, we should see little or no impact on agencies' costs, on the quality of care, or on patient selection—and that is essentially what we observed. The lack of effects on quality of care, in turn, suggests that we should see no impacts on the use and costs of Medicare services by treatment-agency patients. Although we observed some differences, these appear to result from differences in the mix of patients served by treatment and control agencies, rather than from a program effect We will re-investigate all of these issues in the final reports on the per visit home health evaluation, in which we will analyze data from all three demonstration years and will consider results for subgroups defined by agency and patient characteristics.
To date, our overall finding is that per visit prospective payment did not stimulate the expected responses. In addition to the limitations of the analysis discussed previously, several factors may explain this outcome ( Thornton et al., 1993 ). First, the incentives of per visit ratesetting were diluted to some extent because the demonstration procedures were not entirely prospective: Volume adjustment was applied retrospectively and final per-visit rates could not be established until base-year cost reports could be audited, many months after agencies entered the demonstration. Second, the control agencies were also likely to be seeking ways to operate more efficiently. The demonstration took place in a national policy environment that emphasizes the efficient production of health care, and where all HHAs look for ways to ease the paperwork burden on their staff. Third, the opportunity to reduce clinical costs is limited by the requirements for participation in the Medicare program, State regulations, accrediting bodies, the demands of referral sources, and the professional standards of staff. Finally, agencies face incentives to control costs under cost reimbursement (particularly, the section 223 limits), which appears to have induced agencies to restrain cost increases. During the last decade, the increase in the average cost for a Medicare home health visit has been only marginally greater than the increases in the general Consumer Price Index.
Under per episode ratesetting, agencies will face stronger incentives to change their behavior than under per visit ratesetting and may have greater opportunity to do so. Reimbursed a fixed, predetermined amount for each episode of care rendered, agencies will face incentives to reduce the number of visits per episode, as well as cost per visit, perhaps giving them a greater opportunity than under per visit ratesetting to increase their operational efficiency and realize a financial advantage.
This article is derived from material first produced under Contract Number 500-90-0047 from the Health Care Financing Administration (HCFA) to Mathematica Policy Research, Inc., and the Bigel Institute for Health Policy, Brandeis University. Barbara R. Phillips, Randall S. Brown, Craig V. Thornton, Amy C. Klein, and Jennifer L. Schore are with Mathematica Policy Research, Inc. Christine E. Bishop, Grant A Ritter, and Kathleen C Skwara are with the Bigel Institute for Health Policy, Brandeis University. The opinions expressed are those of the authors and do not necessarily reflect the views or policy positions of Mathematica Policy Research, Inc., Brandeis University, or HCFA.
1 Agencies that had been operating for fewer than 3 years (as of the base year) were excluded from the demonstration.
2 The end date used is the closing date of the final bill submitted by an agency for a given episode.
3 In our sample, the correlation in the total cost of a skilled nursing visit between the base year and the previous year is 0.8, and our models explain about 70 percent of the variance in total cost of a skilled nursing visit. The minimum detectable difference is about one-third of the standard deviation ($38 in our sample), or about 16 percent of the sample mean of $80.
4 This estimate is for a one-tailed test of differences in simple means; the minimum detectable difference will be smaller for regression-adjusted means. We have assumed that the proportion of variance that is agency-specific is .07, which is the observed value in our sample for the number of visits per episode, and that the variance of the binary variable is .25 (the maximum possible).
5 Or, equivalently, by transforming each dependent and independent variable into deviations around its agency-specific mean during the 4 observed years.
6 We adjusted the base-year per visit costs of control agencies for inflation and change in volume under the procedures applied to the treatment group.
7 The patient characteristics associated with the need for long visits are: daily intravenous/infusion therapy planned, administration of intravenous therapy, diagnosis of serious cancer, diagnosis of complicated wounds, diagnosis of decubiti, terminal illness noted at admission, and decreased within 90 days of admission.
8 Only one episode, for a patient of a treatment agency, was found to have had a quality problem that actually had a significant adverse effect on the patient In our analysis, this case is included with those with a problem with the potential to affect patients adversely.
Reprint Requests: Barbara R. Phillips, Ph.D., Mathematica Policy Research, Inc., P.O. Box 2393, Princeton, New Jersey 08543-2393.
- Chu D, Brown RS, Phillips BR. Economies of Scale and Volume Adjustment for Medicare-Certified, Free-Standing Home Health Agencies. Princeton, NJ.: Mathematica Policy Research; Jan, 1993. Report submitted to the Health Care Financing Administration. [ Google Scholar ]
- Kass DI. Economies of Scale and Scope in the Provision of Home Health Services. Journal of Health Economics. 1987; 6 :129–146. [ PubMed ] [ Google Scholar ]
- Hay JW, Mandes G. Home Health Cost-Function Analysis. Health Care Financing Review. 1984 Spring; 5 (3):111–116. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nyman J, Svetlik MA. Does the Average Cost of Home Health Care Vary with Case Mix? Public Health Reports. 1989 Jul-Aug; 104 :335–341. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schmitz RJ. Unpublished Memorandum to William Saunders. Health Care Financing Administration; Jan 23, 1989. [ Google Scholar ]
- Schmitz RJ. Estimating the Costs of Home Health Care. Cambridge, MA.: Abt Associates Inc.; 1990. [ Google Scholar ]
- Thornton C, Leutz W, Phillips BR, Schore JL. Changing Incentives in Changing Times: A Case Study of Selected Home Health Agencies Participating in the Per-visit Prospective Payment Demonstration. Report submitted to the Health Care Financing Administration; Princeton, NJ.: Mathematica Policy Research, Inc.; Aug, 1993. [ Google Scholar ]
- U.S. House of Representatives, Committee on Ways and Means. 1993 Green Book: Background Material and Data on Programs within the Jurisdiction of the Committee on Ways and Means. Washington, DC.: U.S. House of Representatives; Jul 7, 1993. Report WMCP:103-18. [ Google Scholar ]
- Search Search Please fill out this field.
What Is Cost Per Click (CPC)?
Understanding cost per click (cpc).
- How Is It Calculated?
How to Lower Cost Per Click
- Alternatives
CPC vs. CPM
- Pros and Cons
- Cost Per Click FAQs
The Bottom Line
Cost per click (cpc) explained, with formula and alternatives.
:max_bytes(150000):strip_icc():format(webp)/Group1805-3b9f749674f0434184ef75020339bd35.jpg)
Yarilet Perez is an experienced multimedia journalist and fact-checker with a Master of Science in Journalism. She has worked in multiple cities covering breaking news, politics, education, and more. Her expertise is in personal finance and investing, and real estate.
:max_bytes(150000):strip_icc():format(webp)/YariletPerez-d2289cb01c3c4f2aabf79ce6057e5078.jpg)
Investopedia / Mira Norian
Cost per click (CPC) is an online advertising revenue model that websites use to bill advertisers based on the number of times visitors click on a display ad attached to their sites.
The primary alternative is the cost per mille (CPM) model, which charges 1,000 ad impressions—or views—of the display ad, regardless of whether or not a viewer clicks on the ad.
The cost-per-click model is also known as pay-per-click (PPC),
Key Takeaways
- Websites bill advertisers based on cost per click, which is an online advertising revenue model.
- Content publishers often use a third-party company to create matches with advertisers.
- Google's AdSense platform is one of the largest cost per click models.
Advertisers commonly use cost per click with a set daily budget for a campaign. When the advertiser's budget is reached, the ad is automatically removed from the website's rotation for the remainder of the billing period. For example, a website with a cost-per-click rate of $.10 would bill an advertiser $100 for 1,000 click-throughs.
Most publishers use a third party to match them with advertisers. The largest such entity is Google Ads , which uses a platform called Google AdSense.
How Much Does a Click Cost?
A click costs no more than you're willing to pay through a bidding system. For example, you could bid a maximum of $1 per click on Google Ads. The system runs through algorithms that evaluate your ads and charges you no more than your bid. However, there are some caveats.
The Google Ads system applies discounts to advertisers with higher ad Quality Scores. This score is determined by the relevance of the ad and the advertiser's content to the search terms used. You'll also be dinged in the position of your ad the lower you bid, again adjusting for the other factors evaluated by the platform.
How Is Cost Per Click Calculated?
A formula may be used to determine the rate you pay per click. One of the most popular ways to calculate your CPC is:
Advertising Campaign Cost / Number of Clicks
Some publishers or platforms like Google Ads use a bidding process to set their rates. For instance, Google Ads asks you to select the maximum amount you're willing to pay per click. Google's platform then uses Ad Rank thresholds to determine the actual cost when your ad is clicked.
This means your cost varies up to your maximum because the platform ranks your bid, ad quality, position, user signals, search topics, and related auctions and sets the cost per click. You can even have Google automate the bids for you to increase your click-through.
The platform then positions your ad based on your maximum amount, with higher maximums achieving a higher placement on the page.
Because advertising can become very expensive when paying by clicks, you need to have a plan to keep from paying too much per click. This means researching and creating a strategy with keywords to raise your Quality Score, a large measure of how your ads compete with others.
Raise Your Quality Score
Your Quality Score is crucial to increasing your clicks and decreasing your costs. You can improve your Quality Score by making adjustments to your:
- Expected clickthrough rate : You can edit the ad to make it more appealing to your targeted consumer base, highlight features and benefits, and above all, ensure your ad details match your keywords.
- Ad relevance : Your ad should appeal to your audience and their search intent. Look at search results for different phrases and analyze the results.
- Landing page experience : Landing pages should be relevant to the audience that clicks the ad. For instance, an advertisement for a widget shouldn't lead to a landing page featuring gadgets. Additionally, the speed of your landing page loads should be fast enough on mobile devices and computers so that potential customers don't need to wait.
Keyword Research
Keywords drive internet searches, so it makes sense to ensure you have keywords in your ads that lead people to your website. Some techniques you can try are:
- Targeting : You should try to target your audience by matching your ad text with what they are searching for.
- Splitting : You can split your ads into groups with different keywords and match them to other searches.
- Grouping : Grouping involves creating themes for your products and services, which you then make group names for and use keywords that match searches. For instance, if you are marketing headphones, you could group them into over-the-ear and in-ear headphones and target your audience with matching keywords.
Cost Per Click Alternatives
There are plenty of alternatives to Google AdSense, including Media.net, Infolinks, Amazon Advertising, and Bidvertiser, to name a few.
Some specialize in small or large publishers, and some offer a better deal than Google AdSense to stay competitive.
Amazon Advertising is designed to allow Amazon website affiliates to place ads that reach shoppers on and off the website when searching for specific products.
Meta Ads Manager allows advertisers to run campaigns on Facebook and Instagram.
In the print world, advertisers choose publications that match their customer profiles and place ads in them. They pay more for bigger ads and more prominent placement, but the effectiveness of those ads can usually only be implied by tracking before-and-after sales numbers. Coupons and contests are among the strategies that help them track their ads' effectiveness better.
In the online world, advertisers know how many people are at least interested enough to click on their ads. That has led to two of the primary ways to reach consumers through web advertising:
- Cost per mille (CPM) or cost per thousand is a pricing model that charges advertisers for the number of times their ads were displayed to a consumer.
- CPC charges advertisers only for the number of times a consumer clicks on their ads to get further information on a product.
Advantages and Disadvantages of CPC Advertising
Higher value
Drives website traffic
More expensive than CPM
Prices vary widely
Less effective for brand and product awareness
Pros Explained
- Higher value : Cost-per-click advertising is more highly valued than CPM advertising because it indicates that an ad has gotten a prospective customer to take the first step towards taking action, whether it is making a purchase or getting more information.
- Drives website traffic : Cost per click is generally considered more effective because it drives traffic to the advertiser's site.
Cons Explained
- More expensive : CPC is more costly than CPM
- Prices vary widely : Because prices vary due to other factors, you may pay less or more depending on your Quality Score, bidding, sponsorship, and other factors.
- Less effective for brand and product awareness : CPM is better for brand recognition and product awareness, assuming that page visitors at least see the logo and, however unconsciously, absorb the message.
What Does Cost Per Click Mean?
Cost per click is how much it costs you when a propective customer clicks on your ad.
How Do You Calculate Cost Per Click?
Cost per click is generally calculated by dividing the overall cost of your ads by the number of clicks your ads received.
What Is CPC and CPM?
Cost per click is a measurement of the amount of money you pay when a consumer clicks your ads, and cost per mille is the cost you pay per 1,000 ad impressions—or 1,000 loads of a page with your ad on it.
Why Is Cost Per Click Important?
Cost per click is significant because it shows you how much you're paying for your advertising and how effective your campaign is.
Demographic targeting of advertising was created offline, primarily by the print magazine industry. It allowed advertisers to choose a specialty magazine that reached the audience that was most likely to be interested in their product.
The cost-per-click advertising model emerged with the internet. It added an actionable element in the ability to immediately click on a link to get more information, place an order, claim a coupon, or download an app.
The software for creating ads and buying ad space is growing increasingly sophisticated. However, the primary concern of advertisers in using either the cost-per-click or cost-per-impression models is accuracy in reporting the actual numbers that the ad reaches.
Google. " Google Adsense ."
Google. " Maximum CPC Bid: Definition. "
Google. " Ad Rank Thresholds: Definition. "
Google. " About Automated Bidding. "
Google. " About Quality Score. "
Google. " 5 Ways To Use Quality Score To Improve Your Perfomance. "
Amazon Advertising. " Grow your business with Amazon Advertising ."
Meta. " Ads Manager. "
:max_bytes(150000):strip_icc():format(webp)/CPM-edit-e635f4dfe70c4749986100b8429533dc.jpg)
- Terms of Service
- Editorial Policy
- Privacy Policy
- Your Privacy Choices

IMAGES
VIDEO
COMMENTS
That makes a total of around $5.20 per site visit. To calculate cost per visit (CPV): Total Cost (divided by) Total Visits = Cost Per Visit (CPV) In this instance, we're not looking at the CPA or ROAS, which will return different figures. Now, another way to look at your cost per visit is to look at the total site visits you have in a period ...
And as a result of investing that money, there have been 125 site visits. $450 / 125 visits = 3.6. That makes a total of around $3.60 per site visit. Meanwhile, another way to perceive cost per visit is to divide all your marketing efforts by the number of total site visits you might've received in a certain period.
Copays, coinsurance and deductibles are types of out-of-pocket costs for health care, but details vary by health plan. ... $20 per office visit, $50 per specialist, $100 per ER visit; these don't ...
Step 6: Determine the full cost of the unit of service. This final step is the simplest: Add the costs from steps 3, 4 and 5 to arrive at a total cost per unit of service. In the example, the ...
The cost per patient, then, would be $66.66 ($100,000 divided by 1,500). Net revenue of $120,000 from the 1,500 patients (understanding that most billings would be collected in June, some in July, and the remainder in August) would result in net profit of $20,000. The collected amount per patient would be $80 and the profit per patient, in our ...
Cost per visit is a critical metric in ecommerce, representing the amount of money an advertiser spends to garner a single visit to their website through different marketing channels. This metric helps understand the efficiency of an online marketing campaign in terms of attracting potential consumers.
To calculate the cost per visit, divide the total cost of the marketing campaign by the total number of visits generated. What is Cost Per Visit? Definition: Cost per visit, or CPV for short, is a measure of the monetary costs it takes a business to generate one visit, typically to a website, but in some cases to a physical store.
Calculate Your Coinsurance. To calculate the coinsurance you owe, you'll first convert your percentage figure into a decimal figure by moving the decimal point two spaces to the left like this: Percentage. Corresponding Decimal Figure. 15%. 0.15. 20%. 0.20.
The Emergence of Cost-Per-Visitor and What Marketers Need to Know. Location data allows businesses to understand consumer behavior, drive sales, and inform decisions in incredible ways. However, the technology needs for accurate location intelligence are exceedingly complex. Like a Russian doll, there are multiple layers beneath the surface ...
Coinsurance means you and the plan share the cost once you meet your deductible. If your plan features 20% coinsurance and a prescription costs $100, you pay $20 and the plan pays $80. A copay is a flat dollar amount you pay each time you go for health care services. You might have a $20 copay doctor visits, a $50 copay for specialists, and a ...
CPV (Cost Per Visit) is a guaranteed performance buying model in which marketers only pay for ads that result in a store visit. Introduced to the market by GroundTruth in Spring of 2017, the Cost Per Visit buying model removes the risk or guesswork of traditional media buying and shifts accountability from buyer to partner, bringing improved ...
The total minutes worked would be $124,800. The cost per minute is $0.28. The cost for triage is $2.80 just for time. Add in the direct cost for supplies and allocate costs for space and equipment, and it adds up. If this process is done for each category of service in the cycle you gain a better understanding of the cost for the visit.
Cost per View offers a transparent way to track the effectiveness of a video advertising campaign by placing a value on each time users watch an ad. Clients are particularly interested in CPV because it tells them how much bang they get for their advertising buck and the maximum amount they are willing to pay for a view of a video ad.
The cost per view (CPV), also called average CPV, CPV cost or cost per completed view CPCV is a video marketing term used to know the cost per completed views.It's a pricing model for video campaigns where you pay for a view of your video ad. A view is counted when a viewer watches at least 30 seconds of your ad (or the complete duration if shorter) or if the viewer interacts with the ad.
Definition. A function of the total sum of marketing costs, the average cost per visit is defined as: Sum of Acquisition Marketing Costs / Visits = Average Cost per Visit. Challenges associate with calculating this key performance indicator are the same as average cost per visitor. Presentation.
Definition. A function of the total sum of marketing costs, the average cost per visitor is defined as: Total Acquisition Marketing Costs / Visitors = Average Cost per Visitor. For most companies the tricky piece is summing acquisition marketing costs, owing to the fact that few companies are accurately tracking these numbers on anything more ...
Three methods performed comparatively well estimating mean cost per visit. The method using an overall cost‐to‐charge ratio (CCR) for all ancillary cost centers without regression adjustment (ANC‐CCR) performed the worst, overestimating "true" costs by $63-$113 per visit. The other three methods, which used CCRs computed from ...
Define Cost Per Visit. shall refer to the amount Company charges for each Visit. Business agrees that the Cost per Visit will vary by Publisher as well as many other variables, including but not limited to: (i) the time of day the Ad is clicked; (ii) the number of other advertisers purchasing advertising with Publisher; (iii) the nature of the products & services Business wishes to promote.
Effective Cost Per Visit (eCPV) is calculated by dividing the total store revenue during a given period by the number of visitors for that same period. For example, if a store had 10,000 visitors driven from its location-based marketing efforts and the store's revenue for the same period was $100,000, then the eCPV would be $10. Learn how you ...
Specifically, we estimated treatment cost per ED visit, mean and total costs by patient and hospital characteristics, and compound annual growth rate in costs and patient volumes. Results During 2012-2019, ED treatment costs increased from $54 billion to $88 billion, a 5.4% annual growth rate—with 4.4 percentage points attributable to ...
Figure 1 plots the predicted values from the outpatient model against the unit cost data and the level of GDP per capita, for all level 1 facilities for the countries included in the sample. The line represents the predicted values of the cost per visit (in natural logs), estimated for a public facility using assumptions outlined in Table 3.
During the per visit demonstration, the limits in effect for freestanding agencies were set at 112 percent of the mean cost per visit incurred by all agencies in the same geographic area. The limits for hospital-based agencies were 13 to 16 percent higher than those for freestanding agencies. The limits are applied in the aggregate; costs that ...
Cost Per Click - CPC: Cost per click (CPC) is a method websites use to bill based on the number of times a visitor clicks on an advertisement. The alternative is cost per thousand (CPM), which is ...