
What Does a Patient Flow Coordinator Do?
Find out what a Patient Flow Coordinator does, how to get this job, salary information, and what it takes to succeed as a Patient Flow Coordinator.

The Patient Flow Coordinator plays an essential role in managing the movement of patients through healthcare facilities, ensuring that each individual receives timely and efficient care. By overseeing admissions, transfers, and discharges, this position helps to optimize bed availability and resource allocation, contributing to the overall smooth operation of the hospital or clinic. The coordinator works closely with medical, nursing, and administrative staff to monitor patient needs and adjust plans accordingly, aiming to enhance patient satisfaction and care outcomes. Through effective communication and strategic planning, the Patient Flow Coordinator supports the healthcare team’s efforts to provide high-quality care in a dynamic environment.
Patient Flow Coordinator Job Duties
- Monitor and manage patient admissions, discharges, and transfers to optimize bed utilization and patient flow within the facility.
- Coordinate with medical, nursing, and administrative staff to identify and resolve bottlenecks in patient flow processes.
- Implement and oversee the execution of patient placement policies and procedures to ensure compliance with healthcare regulations and standards.
- Analyze patient flow data to identify trends, forecast bed availability, and prepare reports for hospital management.
- Facilitate communication between departments to ensure timely patient transfers and the efficient use of resources.
- Participate in multidisciplinary meetings to discuss complex cases and determine the best course of action for patient placement.
- Train and mentor new staff on patient flow procedures and the use of patient management software systems.
- Develop and maintain relationships with external healthcare facilities and services for patient referrals and transfers.
Patient Flow Coordinator Salary & Outlook
Factors influencing a Patient Flow Coordinator’s salary include years of experience, healthcare facility size, and specialization (e.g., emergency services vs. elective surgery coordination). Additionally, skills in data analysis for optimizing patient throughput and proficiency in healthcare software systems can significantly impact earnings. Leadership roles and responsibilities also play a crucial role.
- Median Annual Salary: $46,725 ($22.46/hour)
- Top 10% Annual Salary: $80,500 ($38.7/hour)
The employment of patient flow coordinators is expected to grow faster than average over the next decade.
This growth is driven by an aging population requiring more healthcare services, increasing patient volumes in hospitals, and the need for efficient patient care coordination to improve healthcare outcomes and reduce wait times, making the role of Patient Flow Coordinators critical in managing healthcare resources effectively.
Patient Flow Coordinator Job Requirements
Education: A Patient Flow Coordinator typically holds a Bachelor’s Degree in Health Administration, Nursing, or a related field, with coursework in healthcare management, patient care protocols, and organizational behavior. Some may have a Post-Secondary Certificate or Associate’s Degree in healthcare-related studies, emphasizing practical skills in medical terminology, patient coordination, and healthcare systems. Advanced education in communication, leadership, and problem-solving is also beneficial for effectively managing patient flow and ensuring efficient healthcare service delivery.
Experience: Patient Flow Coordinators typically come from diverse backgrounds, with a significant portion having some experience in healthcare or administrative roles. On-the-job training is common, allowing newcomers to adapt to the specific systems and protocols of their workplace. Many have previously worked in positions that require strong organizational and communication skills, as these are crucial for managing patient logistics efficiently. Training programs focused on patient care coordination, data management, and interdepartmental communication further prepare individuals for the multifaceted nature of this role.
Certifications & Licenses: Certifications and licenses are not typically required for the role of Patient Flow Coordinator.
Patient Flow Coordinator Skills
Scheduling Optimization: Balancing patient appointments with healthcare provider availability optimizes clinic throughput and minimizes wait times. It involves a comprehensive understanding of healthcare operations and the agility to adapt to changing patient demands, ensuring efficient patient flow.
Patient Triage: Assessing the severity of patients’ conditions to determine the necessary level of care is a primary duty. By effectively allocating resources, patient outcomes and hospital workflow are optimized.
Electronic Health Records Management: Coordinating patient flow necessitates seamless access to and updating of patient information. This capability ensures that healthcare professionals involved in a patient’s care are informed with the latest data, streamlining the process from admission through discharge.
Interdepartmental Coordination: Orchestrating patient transfers between departments requires knowledge of each department’s capabilities, schedules, and care protocols. Smooth transitions are facilitated, reducing wait times and maximizing resource utilization, which positively affects patient satisfaction and care outcomes.
Patient Communication: Engaging in effective and empathetic conversations with patients addresses their needs and concerns, promoting a smoother healthcare experience. This ability allows for accurate patient status assessment and efficient resource management.
Queue Management: Managing the flow of patients through various care stages efficiently reduces wait times and enhances satisfaction. A strategic approach to scheduling and prioritizing needs, while considering staff workload and resources, is essential.
Patient Flow Coordinator Work Environment
A Patient Flow Coordinator typically operates within a healthcare setting, such as a hospital or clinic, where the environment is fast-paced due to the nature of medical care. Their workspace is often a blend of office settings and patient care areas, equipped with computers and communication devices to manage patient admissions, transfers, and discharges efficiently.
Work hours can extend beyond the typical nine-to-five, including nights, weekends, and holidays, to match the 24/7 nature of healthcare facilities. The dress code is usually business casual, with an emphasis on practicality and professionalism.
The role demands high interaction levels with medical staff, patients, and families, requiring strong communication skills and a calm demeanor. The emotional environment can be challenging, given the constant exposure to patient care situations. However, the position offers opportunities for professional development through continuous learning about healthcare operations and patient care coordination. Technology plays a crucial role in their daily tasks, from electronic health records to patient tracking systems, ensuring efficient patient flow and care delivery.
Advancement Prospects
A Patient Flow Coordinator can advance to higher managerial roles within healthcare administration, such as Patient Services Manager or Director of Operations. This progression involves taking on more responsibility for the strategic planning and coordination of patient services across a healthcare facility.
To achieve these advancements, a coordinator should focus on mastering the intricacies of healthcare systems, including patient care standards, healthcare laws, and hospital operational efficiency. Demonstrating an ability to improve patient flow and satisfaction metrics significantly enhances promotion prospects.
Gaining experience in various healthcare settings, such as emergency departments, outpatient clinics, and surgical units, provides a broad perspective necessary for higher-level management roles. This diverse experience equips a coordinator with the skills to handle complex logistical challenges in patient care delivery.
Leadership qualities are crucial. Showing initiative in problem-solving, team management, and process improvement projects can set a Patient Flow Coordinator apart, marking them as a candidate for advancement within the healthcare administration hierarchy.
What Does a Coding Manager Do?
What does a dock master do, you may also be interested in..., what does a passport specialist do, what does a director of surgical services do, how to become a neuropsychology technician: step-by-step guide.
What Does a Junior Network Administrator Do?

- (214) 295-5890
- [email protected]
Understanding the Role of a Patient Care Coordinator
- March 13, 2024

Have you ever wondered what makes healthcare services seamless, who ensures your journey through diagnosis, treatment, and recovery is as smooth as possible? Enter the Patient Care Coordinator. With the complexity of healthcare services and the nuances of patient needs, the role of a Patient Care Coordinator has never been more vital. This article, backed by CBM Medical Management , with over 40 years of experience in Revenue Cycle Management and Practice Start-Up, aims to demystify the essential functions of a Patient Care Coordinator and underscore their importance in the healthcare continuum.
What is a Patient Care Coordinator?
A Patient Care Coordinator is your go-to person in the healthcare setting. They stand at the intersection of healthcare provision and patient care management, ensuring that both realms communicate effectively for the benefit of the patient. Their role is comprehensive, covering scheduling appointments, providing educational resources, to even navigating the muddy waters of health insurance claims.
Key Responsibilities
Let’s dive deeper into what a Patient Care Coordinator does:
- Appointment Scheduling: They manage your appointments, ensuring you see the right specialist at the right time. This management reduces waiting times and improves healthcare outcomes.
- Patient Education: They provide patients with necessary information about their conditions, treatment plans, and any required preparation for procedures or tests.
- Insurance Navigation: One of the most complex aspects of healthcare is dealing with insurance claims. Patient Care Coordinators help patients understand their coverage and assist in resolving any disputes.
- Follow-Up Care: Post-treatment, they ensure you have the resources and knowledge for at-home care, schedule follow-up appointments, and are available for any questions or concerns.
Why Are They Essential?
Imagine trying to manage your healthcare journey alone. Overwhelming, right? This is where a Patient Care Coordinator becomes your advocate, aiming to make your healthcare experience as stress-free as possible. They are essential because they:
- Bridge Communication Gaps: They ensure clear communication between doctors and patients, which is crucial for effective treatment.
- Enhance Patient Experience: By handling the administrative tasks, they allow patients to focus solely on their recovery and health.
- Improve Healthcare Outcomes: Through timely appointments and follow-up care, they play a critical role in improving overall healthcare results.
How to Leverage a Patient Care Coordinator
If you’re overwhelmed by your healthcare journey, seeking the support of a Patient Care Coordinator can be a game-changer. In today’s digital age, many services, including patient care coordination, can be conducted virtually. Virtual assistant services offered by reputable healthcare management companies like CBM Medical Management are becoming increasingly popular, ensuring you receive uninterrupted high-quality care, regardless of where you are.
In conclusion, the role of a Patient Care Coordinator is invaluable in navigating the complex healthcare landscape. They not only ensure your healthcare journey is seamless but also advocate for your needs, ensuring you get the best possible care. Remember, you don’t have to manage your healthcare journey alone – a Patient Care Coordinator can be your ally every step of the way.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Join our newsletter
Other posts, the importance of malpractice insurance for mental health providers.
- May 9, 2024
The Essential Guide to Credentialing for Solo Practitioners
Selecting the best insurance panels for your mental health practice, understanding insurance credentialing for mental health professionals.
- May 8, 2024

We are a 22 year old company with over 40 years of Medical Billing, Medical Coding, Medical Receivable Recovery and Virtual Front Desk Assistance.
Quick Links
Contact info.
2435 North Central Expressway Ste 1200, Richardson, TX 75080
© 2023 CBM Medical Management. Design & Developed by The WRIGHT Consult

Transforming Outcomes
Insights on skin, infection and patient care
Taking a Holistic View of the Patient Journey: a Transplant Coordinator’s Perspective

Patient experience and patient journey are two terms used in healthcare, often interchangeably, to describe how we thoughtfully interact with patients. However, these two terms refer to very different aspects of patient care. While most clinicians enter the patient’s journey for a moment in time, adding to the experiences that become their overall journey to wellness, there are few roles that allow the nurse to experience the full journey with the patient.
I learned, in one of those roles, that having a holistic view of the patient journey can make all the difference.
As a renal and pancreas transplant coordinator, I was the core touchpoint for all my patients. It was common to care for over 1,000 patients simultaneously, as when you receive an organ transplant the coordinator becomes like a member of your family, often for life. From the point of transplant, I constantly worked to ensure the patient could get labs drawn, reviewing those labs for trends or abnormalities and ensuring they were able to receive their medications without pause and took them correctly. In our complex health care system, doing all this could sometimes mean moving mountains to ensure patients have what they need. This close relationship helps ensure care is done holistically, with the patient at the core of the decision-making process. Eventually, recipients become less dependent on their coordinator, yet will reach out for every medical ailment or question, no matter how unrelated to their transplant it may be.
By closely following the patient journey, the coordinator can pick up on nuances that, ultimately, can be lifesaving. And, for Ron* that was literally the case. Ron was a new renal transplant recipient challenged with a lack of healthcare knowledge and support system as well as extreme comorbidities. Like many patients, I worked with him very closely following his transplant, and I learned that he loved coming into the clinic to learn about his health and how he could continue to improve to become more independent in his care. He enjoyed talking with all the coordinators, nephrologists, and surgeons and looked forward to his appointments. One day, he didn’t show up and when I called, he didn’t answer. Sixty minutes went by and still nothing. Most would leave it at that, with a voicemail to reschedule the appointment. But I knew that while Ron had many challenges, he was dedicated to his health care. When there was no answer from his emergency contact as well, I called 911 for a welfare check.
Ron was found unconscious. He had fallen in the middle of the night and couldn’t get up. He was transported to the hospital where he spent several days and, while he had a serious wound from his fall, he ultimately recovered.
While not all stories will involve literally saving someone’s life, Ron’s story is just one example of the difference a health care advocate following along the patient journey can have on the patient’s experience and outcomes.
Just a few additional ways this style of care can save both resources and money for the facility and patient may include:
- Ensuring the patient does not undergo unnecessary procedures. When we know a patient already had a procedure done, even if in another health system, we can navigate the system to receive the results and reduce extra work.
- Reducing the number of physician visits. The patient can talk to their transplant coordinator about any medical concerns and we can provide them direct access to the correct specialty clinic rather than numerous physician visits to address an issue.
- Faster therapeutic care. When a patient is prescribed a medication they previously reacted poorly to, we can call their physician to have them try something else.
Navigating the complex health care system is never easy, and I often consider how many patients could be helped and how many lives could be saved if they had a health care advocate such as a transplant coordinator. Understanding the full patient journey is key to improving the patience experience and ultimately improving outcomes. Most clinicians enter the patient’s journey for a moment in time, yet when we can put those experiences together, we can support the patient on their journey and provide holistic care that is empowering and effective.
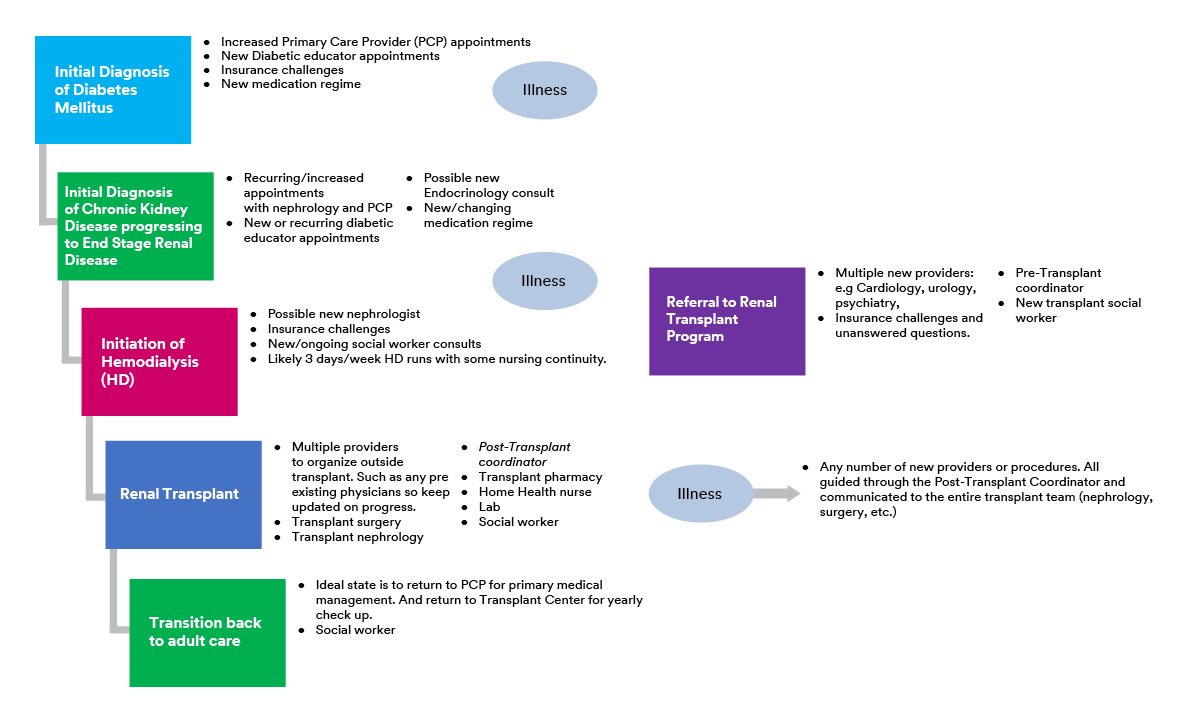
This example of a transplant patient’s experience through the health care system shows how complex and challenging the patient journey can be, with many touchpoints involving various different care providers.
*Name has been changed.

About Post Author
Whitney ficocello, bsn, rn, phn.
- Business of Healthcare
- Innovation and Science
- Patient Experience
- Reducing Preventable Infections
- Think Skin Deeper
- Skin and Wound Management
- Anna A. Kuang
- Caroline Johnson
- Debra M. Thayer
- Dr. Matthew Regulski
- Janet Prust
- Jessica Pehrson
- Kiley Black
- Kimberly Schommer
- Matthew M. Cooper
- Nikki Kluck
- Sarah Isakson
- Whitney Ficocello
- William Leiva
- Share Your Story
Related Post
New study shows 3m™ v.a.c.® therapy is more cost effective compared to competitors, being proactive in the wake of a positive brca2 result: susan’s story, the call for better diabetes care: why i had to amputate my father’s foot, no colon, still rollin’: amber doesn’t let an ostomy slow her down, patient becomes her own advocate for her central line, avoiding bsis for 12 years, meet marla: skin trauma and the patient experience.
Managing Complex Patient Journeys in Healthcare
- First Online: 29 December 2018
Cite this chapter

- Ragnhild Halvorsrud 3 ,
- Annette Lund Lillegaard 4 ,
- Mette Røhne 3 &
- Andreas Momme Jensen 5
3815 Accesses
7 Citations
Healthcare services are increasingly being digitized for greater flexibility and efficient sharing of information. There is also increased awareness among healthcare providers that they must consider their services from the perspective of the patient. To offer a coherent patient journey and efficient treatment, healthcare providers need a structured overview of their service processes and how these affect the patient journey. This chapter introduces customer journey modeling language (CJML) to support the design, management, and analysis of complex patient journeys. Through two case studies, we describe how CJML has been utilized for a shared overview of patient journeys, improvement work, internal training, and knowledge sharing. The first case study was carried out with DIPS, a supplier of eHealth systems to Norwegian hospitals. Here, CJML was used to support the documentation and rollout of a new generation of tools for surgery planning, a complex and resource-intensive process during which critical information is exchanged over time among a range of actors. The second case study was conducted at Oslo University Hospital. Cross-functional teams used CJML to document the patient journey associated with cervical cancer as the basis for improvement work. The two case studies demonstrate how CJML supports healthcare service design through a common understanding of the patient journeys among stakeholders and by visualizing the workflows and actors involved. Although several weaknesses in CJML remain to be resolved, the case studies suggest the benefit of a model-based approach in two regards: first, as an effective communication tool to unite medical, technical, and administrative expertise and second to enhance the patient focus throughout the improvement and digitization of health services.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Ash, J. S., Berg, M., & Coiera, E. (2004). Some unintended consequences of information technology in health care: The nature of patient care information system-related errors. Journal of the American Medical Informatics Association, 11 (2), 104–112.
Article Google Scholar
Ausen, D., Austad, H. O., Svagård, I., Landmark, A. D., Tjønnås, M. S., Rohde, T, et al. (2017). Development and implementation of digital cooperation and support at KAD/Oslo Municipality (2017:00881). Oslo: SINTEF. Retrieved February 22, 2018, from https://www.sintef.no/globalassets/sintef-teknologi-og-samfunn/prosjektwebber/velferdsteknologi/sluttrapport-samkad_sintef-2017-00881.pdf
Bayliss, E. A., Edwards, A. E., Steiner, J. F., & Main, D. S. (2008). Processes of care desired by elderly patients with multimorbidities. Family Practice, 25 (4), 287–293. https://doi.org/10.1093/fampra/cmn040
Berwick, D. M., Nolan, T. W., & Whittington, J. (2008). The triple aim: Care, health, and cost. Health Affairs, 27 (3), 759–769. https://doi.org/10.1377/hlthaff.27.3.759
Brattheim, B. J., Hellesø, R., & Melby, L. (2015). Planning for post-hospital care-local challenges to general benefits of e-messages: Hospital staff’s perspectives. In CEUR workshop proceedings (Vol. 1574, pp. 43–52).
Google Scholar
Bygstad, B., Hanseth, O., Siebenherz, A., & Øvrelid, E. (2017). Process innovation meets digital infrastructure in a high-tech hospital. In Proceedings of the 25th European Conference on Information Systems (ECIS) (pp. 801–814), 5–10 June 2017, Guimarães, Portugal.
de Bruin, S. R., Versnel, N., Lemmens, L. C., Molema, C. C., Schellevis, F. G., Nijpels, G., et al. (2012). Comprehensive care programs for patients with multiple chronic conditions: A systematic literature review. Health Policy, 107 (2–3), 108–145. https://doi.org/10.1016/j.healthpol.2012.06.006
EPA. (2018). Care pathways . European Pathway Association. Retrieved February 22, 2018, from http://e-p-a.org/care-pathways/
France, D. J., Levin, S., Hemphill, R., Chen, K., Rickard, D., Makowski, R., et al. (2005). Emergency physicians’ behaviors and workload in the presence of an electronic whiteboard. International Journal of Medical Informatics, 74 (10), 827–837.
Halvorsrud, R., Haugstveit, I. M., & Pultier, A. (2016). Evaluation of a modelling language for customer journeys. In A. Blackwell, B. Plimmer, & G. Stapleton (Eds.), Proceedings from the 2016 I.E. Symposium on Visual Languages and Human-Centric Computing (VL/HCC) (pp. 40–48), Cambridge, UK, 5–7 September 2016.
Halvorsrud, R., Kvale, K., & Følstad, A. (2016). Improving service quality through customer journey analysis. Journal of Service Theory and Practice, 26 (6), 840–867.
Hertzum, M., & Simonsen, J. (2013). Work-practice changes associated with an electronic emergency department whiteboard. Health Informatics Journal, 19 (1), 46–60. https://doi.org/10.1177/1460458212454024
Haugstveit, I.M., Halvorsrud, R., & Karahasanovic, A. (2016). Supporting redesign of C2C services through customer journey mapping. In N. Morelli, A. de Götzen, & F. Grani (Eds.), ServDes. 2016 Service Design Geographies. Proceedings of the fifth Service Design and Service Innovation Conference (pp. 215–227). Aalborg University Copenhagen, Denmark, 24–26 May, 2016. Linköping University Electronic Press.
Kaplan, K. (2016). Journey mapping in real life: A survey of UX practitioners . Nielsen Norman Group. Retrieved February 22, 2018, from https://www.nngroup.com/articles/journey-mapping-ux-practitioners/
Løvlie, L., Polaine, A., & Reason, B. (2013). Service design: From insight to implementation . New York: Rosenfeld Media.
Melby, L., Brattheim, B. J., & Helleso, R. (2015). Patients in transition: Improving hospital-home care collaboration through electronic messaging: Providers’ perspectives. Journal of Clinical Nursing, 24 (23–24), 3389–3399.
Meld.St.9. (2012–2013). One citizen – one patient record. Digital services in the health and care sector. 11/2012 . Report 9 (2012–2013) from Ministry of Health and Care Services (in Norwegian). Accessed October 18, 2018, from https://www.regjeringen.no/no/dokumenter/meld-st-9-20122013/id708609/
Meld.St.47. (2008–2009). The coordination reform: Proper treatment – at the right place and right time . Report 47 (2008–2009) from Ministry of Health and Care Services. Accessed October 18, 2018, from https://www.regjeringen.no/en/dokumenter/report.no.-47-to-the-storting-2008-2009/id567201/
NDH. (2014). One citizen – one journal. ICT challenges in the health care sector . Report Norwegian Directorate of Health. Retrieved February 22, 2018, from https://www.regjeringen.no/contentassets/355890dd2872413b838066702dcdad88/ikt_utfordringsbilde_helse_omsorgssektoren.pdf
NDH. (2016). Administration of patient journeys across treatment institutions . Report from Norwegian Directorate of Health (IS-2393), Version 1.0, 04/2016. Retrieved February 22, 2018, from https://ehelse.no/Documents/E-helsekunnskap/Administrasjon%20av%20pasientforløp%20på%20tvers%20av%20behandlingssteder_pdf
NDH. (2018). National guidelines for patient pathway given by Norwegian Directorate of Health . Retrieved February 22, 2018, from https://helsedirektoratet.no/retningslinjer/rehabilitering-habilitering-individuell-plan-og-koordinator/seksjon?Tittel=pasientforlop-i-habilitering-og-6901
NDeH. (Ed.). (2017). National eHealth strategy for 2017–2022 . Norwegian Directorate of eHealth. Retrieved February 22, 2018, from https://ehelse.no/Documents/Nasjonal%20e-helsestrategi%20og%20handlingsplan/Nasjonal%20e-helsestrategi%202017-2022%20%28PDF%29.pdf
OMG. (2011). Business process model and notation. In version 2.0: Object Management Group (OMG) . Retrieved from https://www.omg.org/spec/BPMN/2.0/About-BPMN/
Øvrelid, E., & Halvorsen, M. (2016). Improving patient flow through lightweight technology. In NOKOBIT, Norwegian Conference for Organizations’ Use of IT , 24(1). ISSN 1892-0748.
Øvrelid, E., Sanner, T., & Siebenherz, A. (2017). From admission to discharge: Informating patient flow with “lightweight IT”. In NOKOBIT, Norwegian Conference for Organizations’ Use of IT , 25(1). ISSN 1892-0748.
Scott, I. A., Shohag, H., & Ahmed, M. (2014). Quality of care factors associated with unplanned readmissions of older medical patients: A case-control study. Internal Medicine Journal, 44 (2), 161–170.
Shannon, C. E., & Weaver, W. (1963). Mathematical theory of communication . Urbana, IL: University of Illinois Press.
Shostack, G. L. (1982). How to design a service. European Journal of Marketing, 16 (1), 49–63.
Stickdorn, M., Schneider, J., Andrews, K., & Lawrence, A. (2011). This is service design thinking: Basics, tools, cases (Vol. 1). Hoboken, NJ: Wiley.
Svagård, I., Boysen, E. S., Fensli, R., & Vatnøy, T. (2016). Response center services in health care services: Needs and future scenarios (A27689) . Oslo: SINTEF. Retrieved February 22, 2018, from https://www.sintef.no/globalassets/sintef-teknologi-og-samfunn/prosjektwebber/velferdsteknologi/sintef-a27689.pdf
Syal, R. (2013). Abandoned NHS IT system has cost £10bn so far. The Guardian . Accessed October 18, 2018, from https://www.theguardian.com/society/2013/sep/18/nhsrecords-system-10bn
Tax, S. S., McCutcheon, D., & Wilkinson, I. F. (2013). The service delivery network (SDN): A customer-centric perspective of the customer journey. Journal of Service Research, 16 (4), 454–470. https://doi.org/10.1177/1094670513481108
Vogeli, C., Shields, A. E., Lee, T. A., Gibson, T. B., Marder, W. D., Weiss, K. B., et al. (2007). Multiple chronic conditions: Prevalence, health consequences, and implications for quality, care management, and costs. Journal of General Internal Medicine, 22 , 391–395. https://doi.org/10.1007/s11606-007-0322-1
Download references
Author information
Authors and affiliations.
SINTEF Digital, Oslo, Norway
Ragnhild Halvorsrud & Mette Røhne
DIPS AS, Bodø, Norway
Annette Lund Lillegaard
Sykehuspartner HF, Oslo, Norway
Andreas Momme Jensen
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Ragnhild Halvorsrud .
Editor information
Editors and affiliations.
Department of Healthcare Management, Neu Ulm University of Applied Sciences, Neu-Ulm, Germany
Mario A. Pfannstiel
Management, Professional Services and Sports Economics, University of Potsdam, Potsdam, Germany
Christoph Rasche
Rights and permissions
Reprints and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Halvorsrud, R., Lillegaard, A.L., Røhne, M., Jensen, A.M. (2019). Managing Complex Patient Journeys in Healthcare. In: Pfannstiel, M.A., Rasche, C. (eds) Service Design and Service Thinking in Healthcare and Hospital Management. Springer, Cham. https://doi.org/10.1007/978-3-030-00749-2_19
Download citation
DOI : https://doi.org/10.1007/978-3-030-00749-2_19
Published : 29 December 2018
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-00748-5
Online ISBN : 978-3-030-00749-2
eBook Packages : Business and Management Business and Management (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Talk to an Expert
Empower your patients through Chronic Care Management. Click Here

- CCM for Primary Care
- CCM for Specialties
- CCM for RHCs
- CCM for FQHCs
- Annual Wellness Visits
- RPM Enrollment Service
- Quality Improvement Services
- Press Releases
- White Papers
- Case Studies
- About ChartSpan
- Join Our Team
- For Patients

Talk with a ChartSpan Representative Today!
Our team is ready to help you improve patient care and outcomes.
Explore by Topic
- Chronic Care Management
- Annual Wellness Visit
- Remote Patient Monitoring Enrollment As a Service (RPM EaaS)
- MIPS & Quality Improvement
Explore by Type
- Research & Education
- Patient Stories
- White Paper
Chart-Markers: The CCM Patient Journey

If you’re considering offering Medicare’s Chronic Care Management program to your patients, you probably have questions about the journey a CCM patient will go through. CCM can help increase practice revenue and close gaps in care , but these benefits are only meaningful if patients have a positive experience.
At ChartSpan, we call our patient roadmap “Chart-Markers.” Our clinical team uses Chart-Markers to guide patients’ flow through a structured CCM program and to ensure they have the support they need to manage their chronic conditions. Conversations with their care coordinator lead to assessments and screenings that uncover where a patient may need help, and care coordinators provide resources to patients who need them.
Chart-Markers is not a rigid system, since every patient’s journey varies based on their individual needs. But the structured clinical roadmap helps patients consistently work on relevant care goals, so they can improve their health outcomes and manage their chronic conditions.
Want to learn more about how Chart-Markers works? We’ve put together this framework to show the patient’s journey.

Step 1: Enrollment Call
Every patient journey begins with their enrollment call. Enrollment specialists must follow CMS guidelines for the call and must explain:
- What Chronic Care Management is
- That patients may have a copay
- How participants can unenroll at any time
- That patients may only enroll under one provider
The enrollment specialist must receive verbal consent from the patient that they want to enroll, record the call, and archive the recording for 10 years.
Step 2: Welcome Call for CCM Patients
Once a patient gives their consent to enroll in Chronic Care Management, they will receive a welcome call from a care coordinator. The care coordinator will review what care management is and get to know the patient and the health outcomes they would like to accomplish.
If patients are ready to discuss their chronic conditions and their care goals, the coordinator can jump into those processes as well.

Step 3: Discussion of Chronic Conditions
During monthly touchpoint calls, care coordinators engage in an in-depth discussion of the chronic conditions that led to the patient being enrolled in Chronic Care Management. The patient can share how they’re currently managing their conditions, what concerns they have, and what goals they would like to reach.
For example, a patient with high blood pressure and diabetes might discuss their current blood pressure readings and A1C levels, whether they’re happy with those levels, and concerns about whether they’re eating well or getting enough exercise. This discussion empowers personal care coordinators to write relevant, achievable care goals for patients.
Care coordinators can also obtain and review medical records from various providers that are involved in the care of the patient. With these records, the coordinator can ensure the patient’s care goals match their provider’s recommendations and meet their current health needs.
Step 4: Care Goals
Care goals are one of the most vital elements of Chronic Care Management. Every CCM patient will have a few care goals at a time, created by the patient in collaboration with their personal care coordinator.
Some goals may be introduced by patients first, while others will be suggested by the care coordinator based on the patient’s conditions and current health status. Care goals follow SMART goal standards:
- Relevant
For example, a patient with hypertension might set a goal to lower their blood pressure to 130/80 by the end of the month. The care coordinator will record that this goal is related to a patient’s hypertension, then help the patient come up with a plan to achieve the goal. The coordinator might:
- Provide recipes that are low in salt
- Suggest exercises approved by the patient’s provider
- Share stress management techniques
Qualities of an Effective Care Goal
An effective care goal includes:
- The problem that needs to be addressed
- The goal created following the SMART standard
- Steps that could help the patients achieve the goal
- The actions the patient takes each month
- Evaluations by the coordinator of how well the goal is going
- How often the goal should be reviewed
If a patient achieves their goal, or if a goal becomes irrelevant, the patient and the care coordinator can work together to create a new care goal. If a patient isn’t interested in addressing a particular condition, the care coordinator can also set a goal of educating the patient about their condition and the benefits of better managing it.
Care coordinators can also serve as health advocates–not only setting goals, but holding patients accountable to them by checking in regularly and offering encouragement or advice.
Step 5: Assessments
Assessments are an important aspect of Chart-Markers. Care coordinators are trained to provide assessments when your practice asks for them or when patients demonstrate that an assessment might be helpful.
For example, if a patient mentions they fell recently, the coordinator should conduct a fall risk screening. If the patient seems confused during the call, the coordinator might perform a cognitive assessment.
A CCM program could include assessments for:
- Cognitive abilities
- Functional skills
- Durable medical equipment needs
- Medication adherence
- Condition awareness
- Daily health
Based on the assessment’s results, the care coordinator can determine whether the patient needs to see their provider and what educational content or video resources could help them manage their health.
Step 6: Social Determinants of Health
Social Determinants of Health (SDOH) have a dramatic impact on patient health , accounting for roughly 50% of county-level variations in health outcomes. SDOH has therefore become a priority for many practices. In response, CCM vendors have embraced SDOH screenings and started providing socioeconomic resources.
During an SDOH screening, care coordinators ask whether patients have access to:
- Clean, safe housing
- Reliable transportation
- Work, volunteer, or social opportunities
- Nutritious food
- Safe relationships
- Financial resources
If a patient is facing SDOH hardships, their care coordinator can connect them to local resources like housing agencies, car services, food pantries, grocery delivery, and support groups. The care coordinator can also report to your practice on where the patient needs support and follow up with the patient each month to ensure they’ve found the resources they need.
Step 7: Quality Improvement
Quality scores are critically important to many healthcare practices, especially those who are members of ACOs or have entered into value-based contracts. To increase their quality scores, providers need patients to complete their screenings and make appointments to close care gaps.
Chronic Care Management makes closing care gaps easier and faster for overworked providers. At your practice’s request or based on patient needs, care coordinators can perform assessments for:
- Mental health
- High blood pressure
- Influenza immunizations
- Pneumonia immunizations
- Breast cancer screenings
- Colorectal cancer screenings
- Diabetic eye exams
- Diabetes hemoglobin A1C control
Identifying and Closing Care Gaps
If a patient reports that they’re missing screenings, exams, or immunizations, the care coordinator can share education on why specific forms of preventive care are important. When a patient agrees they need the screening, the CCM coordinators can quickly reach out to your practice to schedule it.
Coordinators can also note when patients have received immunizations or screenings at pharmacies or mobile screening facilities. They can capture information about where and when the screening took place and then share this information with you to help close the care gap for your practice.
Additionally, CCM can aid patients struggling with A1C levels, high blood pressure, BMI, or other health indicators. Care coordinators can make appointments at your practice or give the patient strategies and resources to improve their health at home.
Finally, with growing rates of loneliness and depression among older adults , mental health screenings have become a critical component of CCM. If care coordinators notice a mental health concern after a screening, they’ll alert your practice about the patient’s mental health challenges and direct them to resources like therapists and support groups.
Improving Quality Scores
Identifying and closing care gaps plays an essential role in improving patients’ health and in increasing practices’ quality scores. The average ChartSpan CCM customer managed to earn an 88.4 Merit-Based Incentive Payment (MIPS) score from Medicare, making them eligible for reimbursement increases and payment bonuses.
While helping patients remains at the core of CCM, increased Medicare revenue can benefit many struggling healthcare practices.

Step 8: Re-evaluating and Adjusting Goals
Every CCM patient’s journey is different. A patient might see dramatic improvements in their condition or experience an emergency that gives them new, more urgent health needs. Sometimes these changing conditions make care goals hard or impossible to adhere to.
CCM coordinators must be able to to reassess and readjust patients’ care goals as needed. During monthly check-ins, the care coordinator can ask about changes in patients’ health or living conditions and alter the goals and the resources they receive accordingly.
For example, a patient who has recently suffered a fall might need information on making their home safer or more accessible, even if they were previously focusing on their A1C levels.
Another patient might currently be working on a blood pressure goal but find themselves struggling with loneliness and boredom. The care coordinator would respond to the patient’s needs and search for resources like volunteering or exercise groups in the patient’s city.
A good Chronic Care Management plan includes comprehensive care goals and screenings without sacrificing attentiveness to patients’ needs and the ability to listen.
Mapping the CCM Patient Journey
While knowing the general roadmap a CCM program will follow is valuable, a good CCM vendor will work with your practice and your patients to provide personalized care. ChartSpan uses Chart-Markers to ensure we meet the most important requirements of a CCM program, like providing care goals, assessments, and SDOH screenings.
However, our care coordinators are flexible and willing to adjust their monthly check-ins to address quality needs, gaps in care, and, most importantly, any patient needs that arise. Their goal is to ensure your patients are receiving the preventative care they need to live healthier, more fulfilling lives.
If you’d like to learn more about Chronic Care Management, check out our free guide to choosing the best CCM vendor for your practice .
Subscribe for More Insights
Get valuable resources delivered straight to your inbox.
" * " indicates required fields
By providing your information, you agree to receive marketing emails from ChartSpan.
You Might Also Like

What is Preventive Care? Benefits, Examples, & Services

The Role of Personalized Healthcare

Medicare Physician Fee Schedule 2024: What You Need to Know
Why measuring patient satisfaction is critical to your Chronic Care Management program
Empower your providers and delight your patients!
Proactively address patient health with preventive care programs that provide more revenue for your practice and more personalized care for your patients..

- News and announcements
Discover how to enhance the patient experience with patient journeys
- By Umesh Rustogi, General Manager, Microsoft Cloud for Healthcare
Microsoft Cloud for Healthcare provides trusted, integrated capabilities that make it easier for health organizations to improve the patient’s experience. The series of experiences and interactions that a patient has with a healthcare organization, from initial contact to post-treatment follow-up, can be described as patient journeys. For health organizations, understanding patient journeys is crucial to their success. By understanding and optimizing each touchpoint in a patient’s experience, providers can improve patient satisfaction, retention, and loyalty, while payors can address efficiencies and the return on investment of their health plans. The ability to effectively map and analyze patient journeys is becoming increasingly important in the competitive healthcare landscape. Patients have more options and are seeking more personalized care; healthcare organizations can differentiate themselves in how they understand and address the patient journey to provide improved, holistic care.
As part of our ongoing commitment to enhancing patient engagement, we recently updated our Patient Outreach solution to include patient journeys.
Reach out to patients for personalized care
Engage in patient care decisions with personalized patient engagement solutions.

Personalized patient journeys
Patient journey application (preview ) enables healthcare organizations to orchestrate personalized journeys across patient touchpoints to automate repetitive tasks and allow patients to get personalized care faster. The patient journey feature extends the customer journey orchestration engine from Microsoft Dynamic 365 Marketing to support more than just outreach specialist.
Providers can orchestrate actions and information flow across multiple touchpoints and people. Interacting with patients throughout their journey removes the disconnect patients often feel while interacting with different people in the healthcare organizations. By automating repetitive tasks, patient journey frees up time and resources, allowing healthcare providers to better focus on delivering the best possible care to patients and allows patients to receive personalized tasks and actions for care from their caregivers, faster. Improving patient experiences is associated with improved clinical outcomes, reduced malpractice risks and greater employee satisfaction, reducing turnover. 1
The first step in understanding patient journeys is to map out the various touchpoints that patients have with your organization. This can include everything from online research to scheduling appointments, from medical procedures to post-treatment follow-up. By identifying these touchpoints, healthcare organizations can pinpoint areas for improvement and ensure that patients have a seamless experience at every stage of their journey.
Once touchpoints have been identified, healthcare providers and payors can use patient and member feedback and data to optimize each interaction. By understanding the patient journey, healthcare organizations can optimize their services and tailor their efforts to attract and retain patients and members.
To enhance patient journeys, new additions to Microsoft Cloud for Healthcare include:
- Trigger-based journeys: The addition of trigger-based journeys in the Patient outreach solution will enhance the system’s ability to respond quickly to patient interaction and changes. By initiating journeys based on specific events, such as the patient being discharged from the hospital or finished being checked in, organizations can streamline their processes and improve their overall responsiveness and ensure patients’ get personalized information quickly.
- New ways to connect and surface: The integration with Microsoft Cloud for Healthcare and Microsoft applications allows for a seamless experience. Providers and payors now have the ability to send messages through Microsoft Teams , surface to-dos in the patient interaction timeline, and allow for secure messaging through Patient Access Portal. The Patient journey feature extends communication channels beyond email to include text messaging and push notifications.

- Patient discharge: The purpose of this journey is to make sure patients get their post-discharge information by looking at the risk factors and communication preferences. This reduces workload from the contact center so they can focus on high-risk patients and automating communication for others.
- Care plan goal overdue: Notify the patient that they have a care plan goal that is overdue so that they can get back on track.
- Initial pregnancy appointment/Pregnancy appointment and education: Remind patients who are pregnant about their appointments and provide them with educational material.
- Annual diabetes eye exam/Diabetes eye exam follow-up scheduling: Remind diabetic patients about their annual eye exam and then automate tasks based off the results of the appointment.
- Teams message for overdue care plan goal: The goal of this journey is to notify a care manager that their patient has an overdue care plan goal. It will then allow the care manager to either update the care plan goal due date or add a task for themself to follow up with the patient.

Implementing patient journey solutions in healthcare organizations can greatly improve patient outcomes and satisfaction. The sample patient journeys serve as accelerator templates that can be easily customized based on specific organizational needs. With the growing demand for patient-centric care, patient journey solutions will be a key factor in ensuring the success of healthcare organizations in the future.
“The Patient journey feature is remarkably effective. It enables us to personalize outreach to specific cohorts at specific touchpoints and better communicate key messages to patients. We can send a series of customized messages about everything from E-visits and virtual care to appointments and treatment specific follow-up. The Patient journey feature and included sample data is a game changer for us and our customers.” —Deepak Goyal, Partner, Provider Customer Transformation, PwC
Try the Patient journey application preview
Existing Microsoft Cloud for Healthcare customers can sign up now in Solution Center to try our preview. New features are available in the preview section of Patient outreach solution, under the personalized care capabilities card.

- Explore the provided sample patient journeys or follow this step-by-step guide to learn how to Create a simple patient journey .
- Read how to configure patient journey (preview) .
1 The CAHPS Ambulatory Care Improvement Guide, AHRQ .

Related posts

2024 release wave 1: New copilot features to enhance Microsoft Industry Clouds capabilities
![patient journey coordinator [4:56 PM] Jordan Davis (Wipro Designit Services, Inc.) Green background with colored swoops on the top and an image of a young adult helping older adult with a computer.](https://www.microsoft.com/en-us/industry/blog/wp-content/uploads/2024/04/MSFT_Azure_APR08_328468_Blog_Blogheader_240408_V01-1-300x169.webp)
Generative AI and the path to personalized medicine with Microsoft Azure

Streamline controls with Microsoft Cloud for Sovereignty

Advance your carbon reduction strategy with intelligent forecasting and data analysis
Understanding the Distinction Between Care Navigation and Care Coordination
Executive Summary: In the face of increasing complexity within the healthcare system, care navigation and care coordination have emerged as pivotal solutions to guide patients through their healthcare journeys, ensuring they receive personalized and timely care. While care navigation and care coordination share similarities, it’s helpful to distinguish between the two:
- Care navigation centers on keeping individual patients on the right clinical pathways for their unique needs . It’s a protocol-driven, patient-facing function that provides clinical guidance and support, with care navigators acting as knowledgeable guides through the medical system and treatment management plan.
- Care coordination focuses on the administrative and logistical aspects of healthcare , where care coordinators work to ensure that a patient’s care is well-organized and coordinated across various providers and settings.
In this blog, we’ll explore care navigation and how solutions like Preveta’s care navigation platform can enable organizations to deliver tailored support to drive better outcomes.
What is Care Navigation?
Care navigation involves guiding patients through evidence-based clinical care pathways, ensuring they receive the right interventions and care at the right time. It is about keeping individual patients on track through customized protocols based on their unique physiology and disease progression.
Care navigators act as knowledgeable guides, steering patients through the often-confusing medical system and care protocols associated with cancer care, chronic disease management, and other complex medical cases. Navigators advocate for patients, help address barriers, and provide targeted support driven by clinical guidelines and the individual’s response to treatment.
Common activities undertaken by a care navigator include:
- Helping patients understand their condition and their care plans, including assisting with interpreting test results and ‘translating’ complex medical terminology.
- Identifying gaps in a patient’s care and issues that require intervention so that the patient can stay on their care pathway.
- Arranging follow-up appointments, lab work, referrals, and other activities as part of the patient’s care plan.
- Monitoring patient-reported side effects and symptoms, including between provider visits, which is associated with increased survival.
- Liaising with physicians to support any adjustment to treatment based on a patient’s symptoms or side effects, for example, changing chemotherapy dosing, which can help patients tolerate and continue treatment.
- Providing emotional support and a knowledgeable listening ear to patients.
Care navigation can significantly impact the survival rate for common cancers, with Harvard Business Review finding that care navigation increased 5-year prostate cancer survival rates by an impressive 31%.
As well as being great news for patients, care navigation also has significant benefits for providers and physicians, including:
- Generating additional revenue of approximately $150k per care navigator per year.
- Ensuring physicians have access to the data they need by identifying missing lab results, scans, and other data ahead of appointments so they can be obtained, or appointments rescheduled if needed.
- Proactively engaging patients so that they can meet their health goals.
- Reducing no-show and cancellation rates to ensure fewer patients are lost to follow-up.
What is Care Coordination?
On the other hand, care coordination focuses on the administrative and logistical aspects of healthcare to help ensure healthcare professionals can deliver integrated, patient-centered care.
Some common care coordination activities include:
- Coordinating a patient’s care across multiple providers and settings and managing the transition of care from one setting to another, such as when a patient is discharged from hospital.
- Sharing health records and care plans across providers and sites.
- Providing patient and family education for self-care.
- Linking patients with community resources and support services.
The primary focus of care coordination is on optimizing the healthcare system’s efficiency, minimizing redundancies, and providing better integrative care. While it is crucial in improving healthcare outcomes, it predominantly focuses on the system’s operational aspects.
Why is this Distinction Important?
The distinction between care navigation and care coordination is crucial because it recognizes the multifaceted nature of patient care. Moreover, by clearly differentiating care navigation from care coordination, the healthcare industry can unlock new possibilities. It paves the way for technology platforms like Preveta to create a significant impact, revolutionizing the patient journey.
How Technology Can Help with Care Navigation
While many practices are aware of the benefits of care navigation, recruiting, training, and managing care navigators can be challenging. That’s why Preveta has developed a ground-breaking digital care navigation platform that combines technology with a human touch to improve outcomes. By using Preveta, practices can empower Medical Assistants and other staff to become care navigators, significantly enhancing patient experience and outcomes while also adding an additional revenue stream.
Preveta allows practices to make care truly patient-centric by offering:
- Proactive Outreach and Follow-Up: Preveta enables navigators to proactively monitor patients at scale and intervene when care plans fall off track before issues escalate. The system automatically tracks critical data events and care milestones to prompt outreach. Patients receive a caring human touch made possible by giving the navigator full technical support and direction.
- A Holistic, Patient-Centered Approach: Preveta supports patient navigators to take a patient-centered approach by providing them with comprehensive data and systemized, evidence-backed support to enable them to address any obstacles to a patient’s care pathway that may arise.
- Cross-Continuum Connectivity : Preveta centralizes data points from multiple sources, previously siloed, to identify gaps and put in motion additional orders. This eliminates bottlenecks between navigators and clinicians.
- Improved Access and Compliance : Preveta leverages AI and advanced analytics to identify at-risk patients, predict needs, and drive timely interventions for better compliance and outcomes.
By blending compassionate human relationships with data-driven technology, Preveta enables organizations to scale high-touch care navigation that engages patients, resolves barriers, and drives better health outcomes.
Learn more about Preveta today or schedule a free demo to see how you can add care navigation to your practice.
See how Preveta can support your practice
Learn how Preveta can operationalize your care pathways and help facilitate CCM reimbursement
You are using an outdated browser. Please upgrade your browser to improve your experience.
Skip to Site Navigation Skip to Page Content
- Physician Referrals
- Patient Resources
- Why UT Southwestern
Refine your search: Find a Doctor Search Conditions & Treatments Find a Location

Appointment New Patient Appointment or Call 214-645-8300
Kidney Transplant
Patient Journey
Appointment New Patient Appointment or 214-645-8300
Explore Kidney Transplant
We understand the road to transplant can seem overwhelming for patients. So we’ve created a series of videos to help explain the transplant journey from evaluation to waitlisting, and from pre- to post-transplant. Our dedicated team is here for you every step of the way. Hear from our experts on what to expect.
Kidney Transplant Overview
Learn how UT Southwestern approaches kidney transplantation in a multidisciplinary way. Discover how we make your path from evaluation to surgery as smooth as possible.
Hospital Course
Our Surgical Director, Dr. Parsia Vagefi , explains what to expect before, during, and after your kidney transplantation surgery.
Deceased-Donor Options
Our Medical Director, Dr. David Wojciechowski , explains the different types of deceased-donor options available once you are listed for transplant. Our team is dedicated to providing you with the best possible outcomes by finding innovative options to decrease your wait time.
The Benefit of Living Donors
Learn about the advantages of a living-donor kidney transplant, the different types of living-donor options, and how to talk to potential donors.
Nutrition and Transplant
Hear from our transplant dietitian about the importance of nutrition before and after your transplant in order to ensure the best recovery and long-term health maintenance. We talk about the support UT Southwestern offers you every step of the way.
Post-Transplant Medications
After your transplant, you will be on several medications. Our transplant pharmacist discusses the different types of medications and our team’s role after your transplant.
Basics of Transplant Finance
Learn about the basics of transplant finance and the role of our dedicated financial coordinator, who will help you navigate the financial aspects of transplantation and all phases of care.

IMAGES
COMMENTS
2,179 Patient Journey Coordinator jobs available on Indeed.com. Apply to Care Advocate, Practice Manager, Records Coordinator and more!
57 Patient Care Coordinator Journey Clinical jobs available in Remote on Indeed.com. Apply to Care Coordinator, Patient Care Coordinator, Care Advocate and more!
Published Feb 20, 2024. The Patient Flow Coordinator plays an essential role in managing the movement of patients through healthcare facilities, ensuring that each individual receives timely and efficient care. By overseeing admissions, transfers, and discharges, this position helps to optimize bed availability and resource allocation ...
5.0. Patient Care Coordinator. Remote. Here's what you'll do day-to-day: Manage day-to-day patient questions and requests through a shared mailbox and member support across multiple channels (SMS, phone, emails) Provide support to patients to ensure success along their treatment journey. Bring feedback and share insights with the team to ...
A Patient Care Coordinator is your go-to person in the healthcare setting. They stand at the intersection of healthcare provision and patient care management, ensuring that both realms communicate effectively for the benefit of the patient. Their role is comprehensive, covering scheduling appointments, providing educational resources, to even ...
As a Patient Coordinator, you will play a vital role in assisting patients with their medical needs throughout their journey in our medical facility. Your responsibilities will involve developing personalized care plans, coordinating various patient care services, and collaborating closely with patients and their families to ensure they receive ...
Patient Access Coordinator - Remote. Ali'i Health Center. Remote. From $21.75 an hour. Full-time. Monday to Friday + 1. Easily apply. Must possess excellent communication and interpersonal skills to communicate with patients over the phone. Maintains responsibility for: obtaining pre-defined….
Join our team as the new Patient Care Coordinator and make a difference in the lives of our patients. Apply today to embark on an exciting career in healthcare administration! Job Type: Full-time. Pay: $80,000.00 - $90,000.00 per year. Benefits: 401(k) Dental insurance;
Responsibilities: Assist with coordination of scheduling, rescheduling, and canceling patient appointments as required. Confirming completion of patient required forms and authorizations. Manages ...
By closely following the patient journey, the coordinator can pick up on nuances that, ultimately, can be lifesaving. And, for Ron* that was literally the case. Ron was a new renal transplant recipient challenged with a lack of healthcare knowledge and support system as well as extreme comorbidities. Like many patients, I worked with him very ...
Patient Journey Coordinator. Dermacare, San Diego San Diego, CA 2 weeks ago ...
The term patient journey (also referred to as patient pathway, clinical pathway, patient flow, and care pathway) has become a key topic when addressing the challenges in healthcare. ... A personal coordinator is assigned as a contact point between the patient and the health service to increase predictability and ensure the efficient flow of ...
Patient Journey Coordinators (PJCs) Our goal Success measures Improved patient flow: Earlier discharges, reduced LoS, reduced bed occupancy and reduction in crowding in the Emergency Department Improved patient experience: Focused on experience on discharge from hospital - survey data Improved staff experience: Staff feedback and survey data
ChartSpan uses Chart-Markers to ensure we meet the most important requirements of a CCM program, like providing care goals, assessments, and SDOH screenings. However, our care coordinators are flexible and willing to adjust their monthly check-ins to address quality needs, gaps in care, and, most importantly, any patient needs that arise.
The sample patient journeys serve as accelerator templates that can be easily customized based on specific organizational needs. With the growing demand for patient-centric care, patient journey solutions will be a key factor in ensuring the success of healthcare organizations in the future. "The Patient journey feature is remarkably effective.
Care coordination focuses on the administrative and logistical aspects of healthcare, where care coordinators work to ensure that a patient's care is well-organized and coordinated across various providers and settings. In this blog, we'll explore care navigation and how solutions like Preveta's care navigation platform can enable ...
Trauma coordinators are currently seen to play a key role in the case management of trauma patients. They provide a link to ensure good communication and support to the patient and between disciplines, timely discharge and transfer, liaise with post discharge services (for example, housing and social services) and generally act as an advocate for patients throughout the patient journey.
123 Journey Clinical Patient Care Coordinator jobs available in Remote on Indeed.com. Apply to Care Coordinator, Service Coordinator, Utility Manager and more! Skip to main content. ... LPN Patient Care Coordinator - Cleveland Hybrid Remote. Hiring multiple candidates. Cosan Group 3.0. Remote in Independence, OH 44131.
activities that promoted links and good understanding between the coordinator and other professionals: Category 3: Non-coordination activities: actions that do not coordinate the patient pathway. E.g., Clinical activity, time visiting patients, training/expertise, ward management, and journey planning
Patient Journey. New Patient Appointment or 214-645-8300. New Patient Appointment ... Learn about the basics of transplant finance and the role of our dedicated financial coordinator, who will help you navigate the financial aspects of transplantation and all phases of care. The future of medicine, today.
Introduction. Ensuring coordinated care between health and social care services has become a well-established policy and practice concern in most developed countries [].Indeed, care coordination has been identified as a key strategy that has the potential to improve the effectiveness, safety, and efficiency of healthcare systems [].However, and despite the proven benefits, care coordination is ...
1,372 Journey Clinical Patient Care Coordinator jobs available on Indeed.com. Apply to Care Coordinator, Clinic Coordinator, Practice Manager and more!
How much does a Patient Care Coordinator make at Journey Clinical in the United States? The estimated average pay for Patient Care Coordinator at this company in the United States is $20.67 per hour, which is 12% above the national average. Disclaimer.