

Medicare Wellness Visits Back to MLN Print November 2023 Updates
What’s Changed?
- Added information about monthly chronic pain management and treatment services
- Added information about checking for cognitive impairment during annual wellness visits
- Added information about Social Determinants of Health Risk Assessments as an optional element of annual wellness visits

Quick Start
The Annual Wellness Visits video helps you understand these exams, as well as their purpose and claim submission requirements.
Medicare Physical Exam Coverage
Initial Preventive Physical Exam (IPPE)
Review of medical and social health history and preventive services education.
✔ New Medicare patients within 12 months of starting Part B coverage
✔ Patients pay nothing (if provider accepts assignment)
Annual Wellness Visit (AWV)
Visit to develop or update a personalized prevention plan and perform a health risk assessment.
✔ Covered once every 12 months
Routine Physical Exam
Exam performed without relationship to treatment or diagnosis of a specific illness, symptom, complaint, or injury.
✘ Medicare doesn’t cover a routine physical
✘ Patients pay 100% out-of-pocket
Together we can advance health equity and help eliminate health disparities for all minority and underserved groups. Find resources and more from the CMS Office of Minority Health :
- Health Equity Technical Assistance Program
- Disparities Impact Statement
Communication Avoids Confusion
As a health care provider, you may recommend that patients get services more often than we cover or that we don’t cover. If this happens, help patients understand they may have to pay some or all costs. Communication is key to ensuring patients understand why you’re recommending certain services and whether we cover them.

Initial Preventive Physical Exam
The initial preventive physical exam (IPPE), also known as the “Welcome to Medicare” preventive visit, promotes good health through disease prevention and detection. We pay for 1 IPPE per lifetime if it’s provided within the first 12 months after the patient’s Part B coverage starts.
1. Review the patient’s medical and social history
At a minimum, collect this information:
- Past medical and surgical history (illnesses, hospital stays, operations, allergies, injuries, and treatments)
- Current medications, supplements, and other substances the person may be using
- Family history (review the patient’s family and medical events, including hereditary conditions that place them at increased risk)
- Physical activities
- Social activities and engagement
- Alcohol, tobacco, and illegal drug use history
Learn information about Medicare’s substance use disorder (SUD) services coverage .
2. Review the patient’s potential depression risk factors
Depression risk factors include:
- Current or past experiences with depression
- Other mood disorders
Select from various standardized screening tools designed for this purpose and recognized by national professional medical organizations. APA’s Depression Assessment Instruments has more information.
3. Review the patient’s functional ability and safety level
Use direct patient observation, appropriate screening questions, or standardized questionnaires recognized by national professional medical organizations to review, at a minimum, the patient’s:
- Ability to perform activities of daily living (ADLs)
- Hearing impairment
- Home and community safety, including driving when appropriate
Medicare offers cognitive assessment and care plan services for patients who show signs of impairment.
- Height, weight, body mass index (BMI) (or waist circumference, if appropriate), blood pressure, balance, and gait
- Visual acuity screen
- Other factors deemed appropriate based on medical and social history and current clinical standards
5. End-of-life planning, upon patient agreement
End-of-life planning is verbal or written information you (their physician or practitioner) can offer the patient about:
- Their ability to prepare an advance directive in case an injury or illness prevents them from making their own health care decisions
- If you agree to follow their advance directive
- This includes psychiatric advance directives
6. Review current opioid prescriptions
For a patient with a current opioid prescription:
- Review any potential opioid use disorder (OUD) risk factors
- Evaluate their pain severity and current treatment plan
- Provide information about non-opiod treatment options
- Refer to a specialist, as appropriate
The HHS Pain Management Best Practices Inter-Agency Task Force Report has more information. Medicare now covers monthly chronic pain management and treatment services .
7. Screen for potential SUDs
Review the patient’s potential SUD risk factors, and as appropriate, refer them to treatment. You can use a screening tool, but it’s not required. The National Institute on Drug Abuse has screening and assessment tools. Implementing Drug and Alcohol Screening in Primary Care is a helpful resource .
8. Educate, counsel, and refer based on previous components
Based on the results of the review and evaluation services from the previous components, provide the patient with appropriate education, counseling, and referrals.
9. Educate, counsel, and refer for other preventive services
Include a brief written plan, like a checklist, for the patient to get:
- A once-in-a-lifetime screening electrocardiogram (ECG), as appropriate
- Appropriate screenings and other covered preventive services
Use these HCPCS codes to file IPPE and ECG screening claims:
Initial preventive physical examination; face-to-face visit, services limited to new beneficiary during the first 12 months of medicare enrollment
Electrocardiogram, routine ecg with 12 leads; performed as a screening for the initial preventive physical examination with interpretation and report
Electrocardiogram, routine ecg with 12 leads; tracing only, without interpretation and report, performed as a screening for the initial preventive physical examination
Electrocardiogram, routine ecg with 12 leads; interpretation and report only, performed as a screening for the initial preventive physical examination
Federally qualified health center (fqhc) visit, ippe or awv; a fqhc visit that includes an initial preventive physical examination (ippe) or annual wellness visit (awv) and includes a typical bundle of medicare-covered services that would be furnished per diem to a patient receiving an ippe or awv
* Section 60.2 of the Medicare Claims Processing Manual, Chapter 9 has more information on how to bill HCPCS code G0468.
Report a diagnosis code when submitting IPPE claims. We don’t require you to use a specific IPPE diagnosis code, so you may choose any diagnosis code consistent with the patient’s exam.
Part B covers an IPPE when performed by a:
- Physician (doctor of medicine or osteopathy)
- Qualified non-physician practitioner (physician assistant, nurse practitioner, or certified clinical nurse specialist)
When you provide an IPPE and a significant, separately identifiable, medically necessary evaluation and management (E/M) service, we may pay for the additional service. Report the additional CPT code (99202–99205, 99211–99215) with modifier 25. That portion of the visit must be medically necessary and reasonable to treat the patient’s illness or injury or to improve the functioning of a malformed body part.
CPT only copyright 2022 American Medical Association. All rights reserved.
IPPE Resources
- 42 CFR 410.16
- Section 30.6.1.1 of the Medicare Claims Processing Manual, Chapter 12
- Section 80 of the Medicare Claims Processing Manual, Chapter 18
- U.S. Preventive Services Task Force Recommendations
No. The IPPE isn’t a routine physical that some patients may get periodically from their physician or other qualified non-physician practitioner (NPP). The IPPE is an introduction to Medicare and covered benefits, and it focuses on health promotion, disease prevention, and detection to help patients stay well. We encourage providers to inform patients about the AWV during their IPPE. The Social Security Act explicitly prohibits Medicare coverage of routine physical exams.
No. The IPPE and AWV don’t include clinical lab tests, but you may make appropriate referrals for these tests as part of the IPPE or AWV.
No. We waive the coinsurance, copayment, and Part B deductible for the IPPE (HCPCS code G0402). Neither is waived for the screening electrocardiogram (ECG) (HCPCS codes G0403, G0404, or G0405).
A patient who hasn’t had an IPPE and whose Part B enrollment began in 2023 can get an IPPE in 2024 if it’s within 12 months of the patient’s Part B enrollment effective date.
We suggest providers check with their MAC for available options to verify patient eligibility. If you have questions, find your MAC’s website .
Annual Wellness Visit Health Risk Assessment
The annual wellness visit (AWV) includes a health risk assessment (HRA). View the HRA minimum elements summary below. A Framework for Patient-Centered Health Risk Assessments has more information, including a sample HRA.
Perform an HRA
- You or the patient can update the HRA before or during the AWV
- Consider the best way to communicate with underserved populations, people who speak different languages, people with varying health literacy, and people with disabilities
- Demographic data
- Health status self-assessment
- Psychosocial risks, including, but not limited to, depression, life satisfaction, stress, anger, loneliness or social isolation, pain, suicidality, and fatigue
- Behavioral risks, including, but not limited to, tobacco use, physical activity, nutrition and oral health, alcohol consumption, sexual health, motor vehicle safety (for example, seat belt use), and home safety
- Activities of daily living (ADLs), including dressing, feeding, toileting, and grooming; physical ambulation, including balance or fall risks and bathing; and instrumental ADLs (IADLs), including using the phone, housekeeping, laundry, transportation, shopping, managing medications, and handling finances
1. Establish the patient’s medical and family history
At a minimum, document:
- Medical events of the patient’s parents, siblings, and children, including hereditary conditions that place them at increased risk
- Use of, or exposure to, medications, supplements, and other substances the person may be using
2. Establish a current providers and suppliers list
Include current patient providers and suppliers that regularly provide medical care, including behavioral health care.
- Height, weight, body mass index (BMI) (or waist circumference, if appropriate), and blood pressure
- Other routine measurements deemed appropriate based on medical and family history
4. Detect any cognitive impairments the patient may have
Check for cognitive impairment as part of the first AWV.
Assess cognitive function by direct observation or reported observations from the patient, family, friends, caregivers, and others. Consider using brief cognitive tests, health disparities, chronic conditions, and other factors that contribute to increased cognitive impairment risk. Alzheimer’s and Related Dementia Resources for Professionals has more information.
5. Review the patient’s potential depression risk factors
6. Review the patient’s functional ability and level of safety
- Ability to perform ADLs
7. Establish an appropriate patient written screening schedule
Base the written screening schedule on the:
- Checklist for the next 5–10 years
- United States Preventive Services Task Force and Advisory Committee on Immunization Practices (ACIP) recommendations
- Patient’s HRA, health status and screening history, and age-appropriate preventive services we cover
8. Establish the patient’s list of risk factors and conditions
- A recommendation for primary, secondary, or tertiary interventions or report whether they’re underway
- Mental health conditions, including depression, substance use disorders , suicidality, and cognitive impairments
- IPPE risk factors or identified conditions
- Treatment options and associated risks and benefits
9. Provide personalized patient health advice and appropriate referrals to health education or preventive counseling services or programs
Include referrals to educational and counseling services or programs aimed at:
- Fall prevention
- Physical activity
- Tobacco-use cessation
- Social engagement
- Weight loss
10. Provide advance care planning (ACP) services at the patient’s discretion
ACP is a discussion between you and the patient about:
- Preparing an advance directive in case an injury or illness prevents them from making their own health care decisions
- Future care decisions they might need or want to make
- How they can let others know about their care preferences
- Caregiver identification
- Advance directive elements, which may involve completing standard forms
Advance directive is a general term that refers to various documents, like a living will, instruction directive, health care proxy, psychiatric advance directive, or health care power of attorney. It’s a document that appoints an agent or records a person’s wishes about their medical treatment at a future time when the individual can’t communicate for themselves. The Advance Care Planning fact sheet has more information.
We don’t limit how many times the patient can revisit the ACP during the year, but cost sharing applies outside the AWV.
11. Review current opioid prescriptions
- Review any potential OUD risk factors
- Provide information about non-opioid treatment options
12. Screen for potential SUDs
Review the patient’s potential SUD risk factors, and as appropriate, refer them for treatment. You can use a screening tool, but it’s not required. The National Institute on Drug Abuse has screening and assessment tools. Implementing Drug and Alcohol Screening in Primary Care is a helpful resource .
13. Social Determinants of Health (SDOH) Risk Assessment
Starting in 2024, Medicare includes an optional SDOH Risk Assessment as part of the AWV. This assessment must follow standardized, evidence-based practices and ensure communication aligns with the patient’s educational, developmental, and health literacy level, as well as being culturally and linguistically appropriate.
1. Review and update the HRA
2. Update the patient’s medical and family history
At a minimum, document updates to:
3. Update current providers and suppliers list
Include current patient providers and suppliers that regularly provide medical care, including those added because of the first AWV personalized prevention plan services (PPPS), and any behavioral health providers.
- Weight (or waist circumference, if appropriate) and blood pressure
5. Detect any cognitive impairments patients may have
Check for cognitive impairment as part of the subsequent AWV.
6. Update the patient’s written screening schedule
Base written screening schedule on the:
7. Update the patient’s list of risk factors and conditions
- Mental health conditions, including depression, substance use disorders , and cognitive impairments
- Risk factors or identified conditions
8. As necessary, provide and update patient PPPS, including personalized health advice and appropriate referrals to health education or preventive counseling services or programs
9. Provide advance care planning (ACP) services at the patient’s discretion
10. Review current opioid prescriptions
11. Screen for potential substance use disorders (SUDs)
12. Social Determinants of Health (SDOH) Risk Assessment
Preparing Eligible Patients for their AWV
Help eligible patients prepare for their AWV by encouraging them to bring this information to their appointment:
- Medical records, including immunization records
- Detailed family health history
- Full list of medications and supplements, including calcium and vitamins, and how often and how much of each they take
- Full list of current providers and suppliers involved in their care, including community-based providers (for example, personal care, adult day care, and home-delivered meals), and behavioral health specialists
Use these HCPCS codes to file AWV claims:
Annual wellness visit; includes a personalized prevention plan of service (pps), initial visit
Annual wellness visit, includes a personalized prevention plan of service (pps), subsequent visit
Report a diagnosis code when submitting AWV claims. We don’t require you to use a specific AWV diagnosis code, so you may choose any diagnosis code consistent with the patient’s exam.
Part B covers an AWV if performed by a:
- Medical professional (including health educator, registered dietitian, nutrition professional, or other licensed practitioner) or a team of medical professionals directly supervised by a physician
When you provide an AWV and a significant, separately identifiable, medically necessary evaluation and management (E/M) service, we may pay for the additional service. Report the additional CPT code (99202–99205, 99211–99215) with modifier 25. That portion of the visit must be medically necessary and reasonable to treat the patient’s illness or injury or to improve the functioning of a malformed body part.
You can only bill G0438 or G0439 once in a 12-month period. G0438 is for the first AWV, and G0439 is for subsequent AWVs. Don’t bill G0438 or G0439 within 12 months of a previous G0402 (IPPE) billing for the same patient. We deny these claims with messages indicating the patient reached the benefit maximum for the time period.
Medicare telehealth includes HCPCS codes G0438 and G0439.
ACP is the face-to-face conversation between a physician (or other qualified health care professional) and a patient to discuss their health care wishes and medical treatment preferences if they become unable to communicate or make decisions about their care. At the patient’s discretion, you can provide the ACP during the AWV.
Use these CPT codes to file ACP claims as an optional AWV element:
Advance care planning including the explanation and discussion of advance directives such as standard forms (with completion of such forms, when performed), by the physician or other qualified health care professional; first 30 minutes, face-to-face with the patient, family member(s), and/or surrogate
Advance care planning including the explanation and discussion of advance directives such as standard forms (with completion of such forms, when performed), by the physician or other qualified health care professional; each additional 30 minutes (List separately in addition to code for primary procedure)
Report a diagnosis code when submitting an ACP claim as an optional AWV element. We don’t require you to use a specific ACP diagnosis code as an optional AWV element, so you may choose any diagnosis code consistent with a patient’s exam.
We waive both the Part B ACP coinsurance and deductible when it’s:
- Provided on the same day as the covered AWV
- Provided by the same provider as the covered AWV
- Billed with modifier 33 (Preventive Service)
- Billed on the same claim as the AWV
We waive the ACP deductible and coinsurance once per year when billed with the AWV. If we deny the AWV billed with ACP for exceeding the once-per-year limit, we’ll apply the ACP deductible and coinsurance .
We apply the deductible and coinsurance when you deliver the ACP outside the covered AWV. There are no limits on the number of times you can report ACP for a certain patient in a certain period. When billing this service multiple times, document changes in the patient’s health status or wishes about their end-of-life care.
SDOH is important in assessing patient histories; in assessing patient risk; and in guiding medical decision making, prevention, diagnosis, care, and treatment. In the CY 2024 Medicare Physician Fee Schedule final rule , we added a new SDOH Risk Assessment as an optional, additional element of the AWV. At both yours and the patient’s discretion, you may conduct the SDOH Risk Assessment during the AWV.
Use this HCPCS code to file SDOH Risk Assessment claims as an optional AWV element:
Administration of a standardized, evidence-based social determinants of health risk assessment tool, 5-15 minutes
Report a diagnosis code when submitting an SDOH Risk Assessment claim as an optional AWV element. We don’t require you to use a specific SDOH Risk Assessment diagnosis code as an optional AWV element, so you may choose any diagnosis code consistent with a patient’s exam.
The implementation date for SDOH Risk Assessment claims is July 1, 2024. We waive both the Part B SDOH Risk Assessment coinsurance and deductible when it’s:
We waive the SDOH Risk Assessment deductible and coinsurance once per year when billed with the AWV.
If we deny the AWV billed with SDOH Risk Assessment for exceeding the once-per-year limit, we’ll apply the deductible and coinsurance. We also apply the deductible and coinsurance when you deliver the SDOH Risk Assessment outside the covered AWV.
AWV Resources
- 42 CFR 410.15
- Section 140 of the Medicare Claims Processing Manual, Chapter 18
No. The AWV isn’t a routine physical some patients may get periodically from their physician or other qualified NPP. We don’t cover routine physical exams.
No. We waive the coinsurance, copayment, and Part B deductible for the AWV.
We cover an AWV for all patients who’ve had Medicare coverage for longer than 12 months after their first Part B eligibility date and who didn’t have an IPPE or AWV within those past 12 months. We cover only 1 IPPE per patient per lifetime and 1 additional AWV every 12 months after the date of the patient’s last AWV (or IPPE). Check eligibility to find when a patient is eligible for their next preventive service.
Generally, you may provide other medically necessary services on the same date as an AWV. The deductible and coinsurance or copayment applies for these other medically necessary and reasonable services.
You have different options for accessing AWV eligibility information depending on where you practice. Check eligibility to find when a patient is eligible for their next preventive service. Find your MAC’s website if you have specific patient eligibility questions.
Know the Differences
An IPPE is a review of a patient’s medical and social health history and includes education about other preventive services .
- We cover 1 IPPE per lifetime for patients within the first 12 months after their Part B benefits eligibility date
- We pay IPPE costs if the provider accepts assignment
An AWV is a review of a patient’s personalized prevention plan of services and includes a health risk assessment.
- We cover an annual AWV for patients who aren’t within the first 12 months after their Part B benefits eligibility date
- We cover an annual AWV 12 months after the last AWV’s (or IPPE’s) date of service
- We pay AWV costs if the provider accepts assignment
A routine physical is an exam performed without relationship to treatment or diagnosis for a specific illness, symptom, complaint, or injury.
- We don’t cover routine physical exams, but the IPPE, AWV, or other Medicare benefits cover some routine physical elements
- Patients pay 100% out of pocket
View the Medicare Learning Network® Content Disclaimer and Department of Health & Human Services Disclosure .
The Medicare Learning Network®, MLN Connects®, and MLN Matters® are registered trademarks of the U.S. Department of Health & Human Services (HHS).
CPT codes, descriptions and other data only are copyright 2022 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply. Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability for data contained or not contained herein.

- CCM (Chronic Care Managmenet)
- Care Coordination
- Preventitive and Wellness Programs
- Product Updates
- RHCs / FQHCs
« View All Posts
Annual Wellness Visit | CPT codes
2024 CPT Codes for Annual Wellness Visits
- Share This Article
January 4th, 2024 | 9 min. read

ThoroughCare
Content Team
Print/Save as PDF
An Annual Wellness Visit (AWV) is a preventive screening used to identify gaps in care.
As covered by Medicare Part B, providers should understand what CPT billing codes matter to the service and how to use them. This can help your organization avoid denied claims and enhance care.
AWVs are covered for Medicare Part B patients without a co-pay. This yearly assessment helps patients create personalized care plans that providers can use to improve outcomes.
AWVs are reimbursable under Medicare’s Physician Fee Schedule, paying various rates.
AWV CPT Codes to Know: G0402, G0438, G0439
Different CPT billing codes reflect specific types of Medicare wellness visits. The crucial qualifying determinant is when a certain AWV can be provided and billed for.
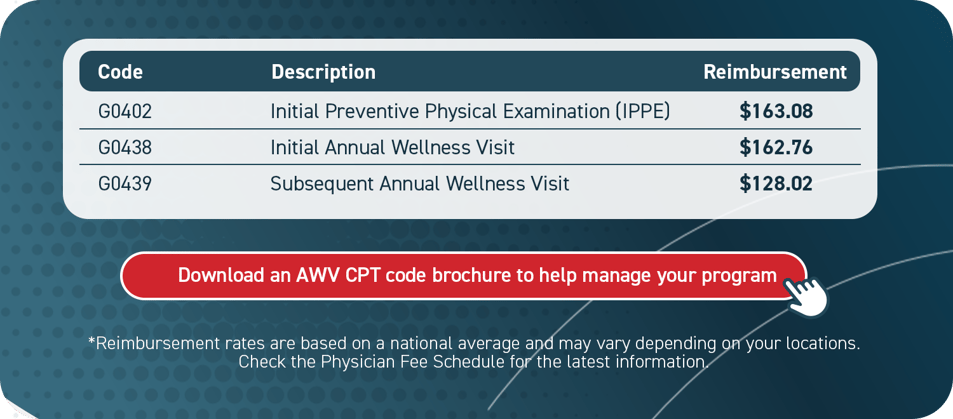
There are three types of wellness visits : Initial Preventive Physical Examination (IPPE), an Initial Annual Wellness Visit, and the Subsequent Annual Wellness Visit. Each entails a different billing code as well as specific qualifiers for each program.
- Initial Preventive Physical Examination (G0402) : Patients may only receive this benefit within the first 12 months of their Medicare enrollment. Commonly referred to as the “welcome to Medicare visit,” it is considered a once in a lifetime assessment and after the initial eligibility period, the patient cannot receive an Initial Preventive Physical Examination. It is also dependent on the health risk assessment .
- Initial Annual Wellness Visits (G0438) : Similar to an Initial Preventive Physical Examination, except it is available to a patient after 11 months of Medicare enrollment. This is for patients that miss their window for an Initial Preventive Physical Examination. However, if the patient does complete an Initial Preventive Physical Examination, they must still complete the Initial Annual Wellness Visit. This screening also includes an optional cognitive exam and end-of-life planning.
- Subsequent Annual Wellness Visit (G0439) : Is the yearly follow-up to an Initial Annual Wellness Visit. Eleven full months after the Initial Annual Wellness Visit, a patient can attend these visits to modify and maintain their preventive care plan, based on how their health is at any given time.
About AWVs and Their Billing Requirements
Medicare’s wellness visit is a yearly assessment of a patient’s health used to identify risks and create a personalized care plan. AWVs are different from yearly physical examinations. They offer a more complete review of a patient’s medical history and current lifestyle to suggest care goals that close gaps .
Wellness visits can be of particular importance for patients living with chronic conditions.
With an AWV, a personalized care plan is designed to help manage chronic illnesses , as well as schedule preventive screenings to improve early detection of disease.
Who Can Provide AWVs?
AWV billing must be directed by a provider with an NPI number. However, clinical staff can administer most of the assessment, saving physician time and involvement. Eligible providers include:
- Physician assistants
- Nurse practitioners
- Certified nurse midwives
- Clinical nurse specialists
- Pharmacists
AWV Billing Requirements
The following components must be included in a patient’s wellness visit:
- A health risk assessment
- A review and update of medical and family history
- A review of current providers, prescriptions/medications, and durable medical equipment suppliers
- Height, weight, blood pressure, BMI, and other routine measurements
- Personalized health advice, health education, and preventative counseling
- A list of identified risk factors, current medical and mental health conditions, and recommended treatment options
- A cognitive impairment screening
- A five to 10-year screening schedule for appropriate preventive services
- A review of the patient’s functional ability and level of safety, including screening for hearing impairments, risk of falling, activities of daily living, and level of home safety
- Identification of patients at risk for alcohol, tobacco, and opioid abuse
- Advance care planning
Submitting Claims to Medicare
Five items are required when submitting a Medicare claim :
- A CPT Code for the specific type of AWV provided
- An ICD-10 code for a general adult medical examination (Z00.00)
- Date of service
- Place of service (most office in-office or telehealth)
- Submit NPI number
It is helpful to know the staff care coordinator assigned to a patient in case of an audit.
Three Steps to Bill for AWVs:
- Verify CMS requirements were met
- Submit claims to CMS annually (or when best for your organization)
- Determine there are no conflicting billing codes

Additional AWV Billing Opportunities
Medicare supports additional CPT codes for optional, add-on services related to AWVs. These include Advance Care Planning and a social determinants of health screening.
Advance Care Planning with AWVs
Advance Care Planning helps patients prepare for future medical decision-making in case of serious illness or they are unable to communicate their care preferences. Specifically, Advance Care Planning includes two primary documents:
- A living will
- A durable healthcare power of attorney
An AWV assessment asks patients whether they have Advance Care Planning documents in place. If not, the provider can use the AWV to discuss advance care options and schedule time to complete a plan.
CPT Code 99497
The average billing rate is $80.56. To accurately bill for code 99497, services must:
- Allow for 30 minutes of a face-to-face consultation with the patient, their family member(s), and/or a surrogate (with a minimum of 16 minutes of service time documented)
- Be provided by a physician or other qualified healthcare professional
- Include an explanation and review of advance care directives and options for completing them
Documentation to account for at least 16 minutes of service time should record that the ACP conversation was voluntary on behalf of the patient, encapsulate what was talked about, record who was present for the conversation, and note the length of time for the consultation.
Again, it is not required to complete an advance care directive during ACP. Completion is only required if you’ve noted in your documentation that you’ve performed this task. However, when ACP is completed with an AWV, it is entirely covered for the patient .
CPT Code 99498
This is simply an add-on billing code to allow for an additional 30 minutes of ACP services. The average reimbursement rate is $69.75. Requirements for billing this code include:
- Listing this billing claim separately in addition to the code for the primary consultation
- That a minimum of 16 minutes past the first 30 minutes is documented using the same documentation requirements noted above.
Social Determinants of Health Assessment with AWVs
Providers can collect social determinants of health ( SDOH ) data while performing an AWV. SDOH discussions should be between 5 and 15 minutes in length, and cover food and housing insecurities, transportation needs, and utility difficulties.
The SDOH risk assessment addresses factors that influence the diagnosis and treatment of patients’ medical conditions. While not designed as a screening, the assessment is tied to one or more known or suspected SDOH needs.
CPT Code G0136
Providers can receive an additional $18.66 for assessing SDOH during an AWV. For the patient, this assessment is fully covered by Medicare when provided with an AWV.
To claim this CPT code, providers must:
- Deliver 5-15 minutes of SDOH discussion
- Not assess a patient more than every 6 months
- Administer a standardized, evidence-based SDOH risk assessment
Medicare stresses the importance of following up with patients about SDOH and working to connect them with available resources.
AWVs for Federally Qualified Health Centers
Federally Qualified Health Centers (FQHC) can bill for AWVs, but they utilize additional codes.
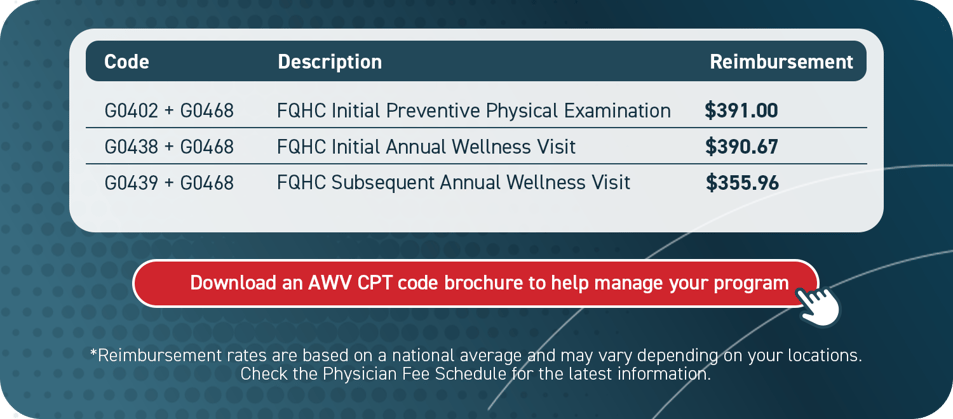
In addition to the standard CPT codes associated with AWVs, an FQHC may use a special add-on code (G0468) that will support additional reimbursement.
For example, if an FQHC were to provide an Initial Preventive Physical Examination, the clinic would bill for G0402 + G0468. This coding indicates to Medicare that the service is being provided through an FQHC.
These organizations receive much higher average reimbursement rates.
AWVs Promote Value-based Care
AWVs ask about lifestyle, social history, mental health and home environment. Documenting these details can help providers risk-stratify patient populations and develop comprehensive, personalized care plans that can close gaps.
This can help clinicians better coordinate services, streamline collaborative decision-making and support value-based care delivery. AWVs have been shown to build stronger provider-patient relationships, secure additional revenue and contribute to cost savings.
ThoroughCare Simplifies Annual Wellness Visits
ThoroughCare offers end-to-end workflow for Annual Wellness Visits.
We simplify the process, so providers can focus on engaging patients. Guided interviews help ask the right questions and ensure all service requirements are met. ThoroughCare includes digital solutions, such as:
- An interactive health risk assessment
- Screening tools, such as ADL, CAGE, DAST-10, GAD-7, MDQ, PAC, PHQ-2, and a mini cognitive exam
- A care gaps summary with recommended interventions
- A full report of Personalized Prevention Plan Services
- Comprehensive care planning tools
- Automated CPT code assignment for accurate billing

*Reimbursement rates are based on a national average and may vary depending on your location.
Check the Physician Fee Schedule for the latest information.
License for Use of "Physicians' Current Procedural Terminology", (CPT) Fourth Edition
End User/Point and Click Agreement: CPT codes, descriptions and other data only are copyright 2009 American Medical Association (AMA). All Rights Reserved (or such other date of publication of CPT). CPT is a trademark of the AMA.
You, your employees and agents are authorized to use CPT only as contained in the following authorized materials including but not limited to CGS fee schedules, general communications, Medicare Bulletin , and related materials internally within your organization within the United States for the sole use by yourself, employees, and agents. Use is limited to use in Medicare, Medicaid, or other programs administered by the Centers for Medicare & Medicaid Services (CMS). You agree to take all necessary steps to insure that your employees and agents abide by the terms of this agreement.
This product includes CPT which is commercial technical data and/or computer data bases and/or commercial computer software and/or commercial computer software documentation, as applicable which were developed exclusively at private expense by the American Medical Association, 515 North State Street, Chicago, Illinois, 60610. U.S. Government rights to use, modify, reproduce, release, perform, display, or disclose these technical data and/or computer data bases and/or computer software and/or computer software documentation are subject to the limited rights restrictions of DFARS 252.227-7015(b)(2)(June 1995) and/or subject to the restrictions of DFARS 227.7202-1(a)(June 1995) and DFARS 227.7202-3(a)June 1995), as applicable for U.S. Department of Defense procurements and the limited rights restrictions of FAR 52.227-14 (June 1987) and/or subject to the restricted rights provisions of FAR 52.227-14 (June 1987) and FAR 52.227-19 (June 1987), as applicable, and any applicable agency FAR Supplements, for non-Department Federal procurements.
AMA Disclaimer of Warranties and Liabilities.
CPT is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. AMA warrants that due to the nature of CPT, it does not manipulate or process dates, therefore there is no Year 2000 issue with CPT. AMA disclaims responsibility for any errors in CPT that may arise as a result of CPT being used in conjunction with any software and/or hardware system that is not Year 2000 compliant. No fee schedules, basic unit, relative values or related listings are included in CPT. The AMA does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this file/product is with CGS or the CMS and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
CMS Disclaimer
The scope of this license is determined by the AMA, the copyright holder. Any questions pertaining to the license or use of the CPT must be addressed to the AMA. End Users do not act for or on behalf of the CMS. CMS DISCLAIMS RESPONSIBILITY FOR ANY LIABILITY ATTRIBUTABLE TO END USER USE OF THE CPT. CMS WILL NOT BE LIABLE FOR ANY CLAIMS ATTRIBUTABLE TO ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION OR MATERIAL CONTAINED ON THIS PAGE. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information or material.
This license will terminate upon notice to you if you violate the terms of this license. The AMA is a third party beneficiary to this license.
POINT AND CLICK LICENSE FOR USE OF "CURRENT DENTAL TERMINOLOGY", ("CDT")
End User License Agreement
These materials contain Current Dental Terminology, Fourth Edition (CDT), copyright © 2002, 2004 American Dental Association (ADA). All rights reserved. CDT is a trademark of the ADA.
THE LICENSE GRANTED HEREIN IS EXPRESSLY CONDITIONED UPON YOUR ACCEPTANCE OF ALL TERMS AND CONDITIONS CONTAINED IN THIS AGREEMENT. BY CLICKING BELOW ON THE BUTTON LABELED "I ACCEPT", YOU HEREBY ACKNOWLEDGE THAT YOU HAVE READ, UNDERSTOOD AND AGREED TO ALL TERMS AND CONDITIONS SET FORTH IN THIS AGREEMENT.
IF YOU DO NOT AGREE WITH ALL TERMS AND CONDITIONS SET FORTH HEREIN, CLICK BELOW ON THE BUTTON LABELED "I DO NOT ACCEPT" AND EXIT FROM THIS COMPUTER SCREEN.
IF YOU ARE ACTING ON BEHALF OF AN ORGANIZATION, YOU REPRESENT THAT YOU ARE AUTHORIZED TO ACT ON BEHALF OF SUCH ORGANIZATION AND THAT YOUR ACCEPTANCE OF THE TERMS OF THIS AGREEMENT CREATES A LEGALLY ENFORCEABLE OBLIGATION OF THE ORGANIZATION. AS USED HEREIN, "YOU" AND "YOUR" REFER TO YOU AND ANY ORGANIZATION ON BEHALF OF WHICH YOU ARE ACTING.
- Subject to the terms and conditions contained in this Agreement, you, your employees, and agents are authorized to use CDT-4 only as contained in the following authorized materials and solely for internal use by yourself, employees and agents within your organization within the United States and its territories. Use of CDT-4 is limited to use in programs administered by Centers for Medicare & Medicaid Services (CMS). You agree to take all necessary steps to ensure that your employees and agents abide by the terms of this agreement. You acknowledge that the ADA holds all copyright, trademark and other rights in CDT-4. You shall not remove, alter, or obscure any ADA copyright notices or other proprietary rights notices included in the materials.
- Applicable Federal Acquisition Regulation Clauses (FARS)\Department of Defense Federal Acquisition Regulation Supplement (DFARS) Restrictions Apply to Government use. Please click here to see all U.S. Government Rights Provisions .
- ADA DISCLAIMER OF WARRANTIES AND LIABILITIES. CDT-4 is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. No fee schedules, basic unit, relative values or related listings are included in CDT-4. The ADA does not directly or indirectly practice medicine or dispense dental services. The sole responsibility for the software, including any CDT-4 and other content contained therein, is with (insert name of applicable entity) or the CMS; and no endorsement by the ADA is intended or implied. The ADA expressly disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this file/product. This Agreement will terminate upon notice to you if you violate the terms of this Agreement. The ADA is a third-party beneficiary to this Agreement.
- CMS DISCLAIMER. The scope of this license is determined by the ADA, the copyright holder. Any questions pertaining to the license or use of the CDT-4 should be addressed to the ADA. End users do not act for or on behalf of the CMS. CMS DISCLAIMS RESPONSIBILITY FOR ANY LIABILITY ATTRIBUTABLE TO END USER USE OF THE CDT-4. CMS WILL NOT BE LIABLE FOR ANY CLAIMS ATTRIBUTABLE TO ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION OR MATERIAL COVERED BY THIS LICENSE. In no event shall CMS be liable for direct, indirect, special, incidental, or consequential damages arising out of the use of such information or material.
The license granted herein is expressly conditioned upon your acceptance of all terms and conditions contained in this agreement. If the foregoing terms and conditions are acceptable to you, please indicate your agreement by clicking below on the button labeled "I ACCEPT". If you do not agree to the terms and conditions, you may not access or use the software. Instead, you must click below on the button labeled "I DO NOT ACCEPT" and exit from this computer screen.

Initial Preventive Physical Examination (IPPE)
As part of the Affordable Care Act, Medicare provides coverage for an IPPE for patients who have been enrolled in Medicare for less than one year. It is a one-time service, intended to help provide an introduction to insurance coverage, benefits, and give appropriate screening for disease detection and preventive promotion of health. The IPPE must be performed within the first 12 months after the effective date of the beneficiary's Medicare Part B coverage.
An IPPE includes the following seven components:
- A review of the beneficiary's medical and social history
- Review of the beneficiary's potential risk factors for mood disorders
- Review of the beneficiary's functional ability and level of safety
- An examination
- End-of-life planning
- Education, counseling, and referral based on the previous five components
- Education, counseling, and referral for other preventive services
Annual Wellness Visit (AWV)
As part of the Affordable Care Act, Medicare provides coverage for an AWV for patients who are enrolled in Medicare. This service may be covered as often as once per year. There are two specific types of AWV: initial and subsequent. Required elements for the initial AWV include:
- A self-reported health risk assessment
- Establishment of the beneficiary's medical/family history
- A health assessment within the office
- Establishment of current providers and suppliers of service
- Detection of any cognitive impairment that the beneficiary may have
- Establishment of a written screening schedule for the beneficiary
- Establishment of a list of risk factors and conditions for which the primary, secondary, or tertiary interventions are recommended for the beneficiary
- Furnishing of personalized health advice to the beneficiary, and a referral for further care, if appropriate
The subsequent AWV visit will be updating the patient's past history as established during the initial visit, as well as a new assessment to establish any needed additional treatment. This is a shorter established service. Required elements for subsequent AWVs include:
- Update of the self-reported risk assessment
- An update of the beneficiary's medical/family history
- Update of the list of current providers and suppliers of service
- Update of the written screening schedule for the beneficiary
- Update of the list of risk factors and conditions for which the primary, secondary, or tertiary interventions are recommended for the patient
- Furnishing of personal health advice to the beneficiary, and a referral for further care, if appropriate
Stay Connected
People With Medicare
Working with us
Existing health care professionals, patient care programs & quality assurance.
- Medicare resources
Patient's mental health
Education, trainings and manuals, regulations, news and insights, annual wellness visit (awv) documentation and coding.
A Medicare Annual Wellness Visit (AWV) is not a typical physical exam. Rather, it’s an opportunity to promote quality, proactive, cost-effective care. AWVs help you engage with your patients and increase revenue.
A physician, PA, NP, certified clinical nurse specialist or a medical professional under the direct supervision of a physician (including health educators, registered dietitians and other licensed practitioners) can perform AWVs.
AWV documentation
Document all diagnoses and conditions to accurately reflect severity of illness and risk of high-cost care.
An ICD-10 Z code is the first diagnosis code to list for wellness exams to ensure that member financial responsibility is $0.
- Z00.00 — encounter for general adult medical examination without abnormal findings
- Z00.01 — encounter for general adult medical examination with abnormal findings
The two CPT® codes used to report AWV services are:*
- G0438 — initial visit**
- G0439 — subsequent visit (no lifetime limits)
Additional services (lab, X-rays, etc.) ordered during an AWV may be applied toward the patient’s
deductible and/or be subject to coinsurance. Before performing additional services, discuss them
with the patient to verify that the patient understands their financial responsibilities.
More information
For additional information and education, contact us at [email protected] .
*CPT® is a registered trademark of the American Medical Association.
**Code G0438 is for the first AWV only. The submission of G0438 for a beneficiary for which a claim code of G0438 has already been paid will result in a denial.
Legal notices
Aetna is the brand name used for products and services provided by one or more of the Aetna group of companies, including Aetna Life Insurance Company and its affiliates (Aetna).
Health benefits and health insurance plans contain exclusions and limitations.
Also of interest:
You are now being directed to the AMA site
Links to various non-Aetna sites are provided for your convenience only. Aetna Inc. and its affiliated companies are not responsible or liable for the content, accuracy or privacy practices of linked sites, or for products or services described on these sites.
You are now being directed to the Give an Hour site
Links to various non-Aetna sites are provided for your convenience only. Aetna Inc. and its affiliated companies are not responsible or liable for the content, accuracy or privacy practices of linked sites, or for products or services described on these sites.

You are now being directed to the CVS Pharmacy® site
You are now being directed to the cdc site.
Links to various non-Aetna sites are provided for your convenience only. Aetna Inc. and its its affiliated companies are not responsible or liable for the content, accuracy or privacy practices of linked sites, or for products or services described on these sites.
Aetna® is proud to be part of the CVS Health family.
You are now being directed to the CVS Health site.
You are now being directed to the Apple.com COVID-19 Screening Tool
Links to various non-Aetna sites are provided for your convenience only. Aetna Inc. and its affiliated companies are not responsible or liable for the content, accuracy, or privacy practices of linked sites, or for products or services described on these sites.
You are now being directed to the US Department of Health and Human Services site
You are now being directed to the cvs health covid-19 testing site, you are now being directed to the fight is in us site.
Links to various non-Aetna sites are provided for your convenience only. Aetna Inc. and its affiliated companies are not responsible or liable for the content, accuracy, or privacy practices of linked sites, or for products or services described on these sites.
You are now leaving the Aetna® website
Please log in to your secure account to get what you need.
You are now leaving the Aetna Medicare website.
The information you will be accessing is provided by another organization or vendor. If you do not intend to leave our site, close this message.
Get a link to download the app
Just enter your mobile number and we’ll text you a link to download the Aetna Health℠ app from the App Store or on Google Play.
Message and data rates may apply*
This search uses the five-tier version of this plan
Each main plan type has more than one subtype. Some subtypes have five tiers of coverage. Others have four tiers, three tiers or two tiers. This search will use the five-tier subtype. It will show you whether a drug is covered or not covered, but the tier information may not be the same as it is for your specific plan. Do you want to continue?
Applied Behavior Analysis Medical Necessity Guide
By clicking on “I Accept”, I acknowledge and accept that:
The Applied Behavior Analysis (ABA) Medical Necessity Guide helps determine appropriate (medically necessary) levels and types of care for patients in need of evaluation and treatment for behavioral health conditions. The ABA Medical Necessity Guide does not constitute medical advice. Treating providers are solely responsible for medical advice and treatment of members. Members should discuss any matters related to their coverage or condition with their treating provider.
Each benefit plan defines which services are covered, which are excluded, and which are subject to dollar caps or other limits. Members and their providers will need to consult the member's benefit plan to determine if there are any exclusions or other benefit limitations applicable to this service or supply.
The conclusion that a particular service or supply is medically necessary does not constitute a representation or warranty that this service or supply is covered (i.e., will be paid for by Aetna) for a particular member. The member's benefit plan determines coverage. Some plans exclude coverage for services or supplies that Aetna considers medically necessary.
Please note also that the ABA Medical Necessity Guide may be updated and are, therefore, subject to change.
Medical necessity determinations in connection with coverage decisions are made on a case-by-case basis. In the event that a member disagrees with a coverage determination, member may be eligible for the right to an internal appeal and/or an independent external appeal in accordance with applicable federal or state law.
Aetna® is proud to be part of the CVS® family.
You are now being directed to CVS Caremark ® site.
ASAM Terms and conditions
By clicking on “I accept”, I acknowledge and accept that:
Licensee's use and interpretation of the American Society of Addiction Medicine’s ASAM Criteria for Addictive, Substance-Related, and Co-Occurring Conditions does not imply that the American Society of Addiction Medicine has either participated in or concurs with the disposition of a claim for benefits.
This excerpt is provided for use in connection with the review of a claim for benefits and may not be reproduced or used for any other purpose.
Copyright 2015 by the American Society of Addiction Medicine. Reprinted with permission. No third party may copy this document in whole or in part in any format or medium without the prior written consent of ASAM.
Precertification lists
Should the following terms and conditions be acceptable to you, please indicate your agreement and acceptance by selecting the button below labeled "I Accept".
- The term precertification here means the utilization review process to determine whether the requested service, procedure, prescription drug or medical device meets the company's clinical criteria for coverage. It does not mean precertification as defined by Texas law, as a reliable representation of payment of care or services to fully insured HMO and PPO members.
- Applies to: Aetna Choice ® POS, Aetna Choice POS II, Aetna Medicare ℠ Plan (PPO), Aetna Medicare Plan (HMO), all Aetna HealthFund ® products, Aetna Health Network Only ℠ , Aetna Health Network Option ℠ , Aetna Open Access ® Elect Choice ® , Aetna Open Access HMO, Aetna Open Access Managed Choice ® , Open Access Aetna Select ℠ , Elect Choice, HMO, Managed Choice POS, Open Choice ® , Quality Point-of-Service ® (QPOS ® ), and Aetna Select ℠ benefits plans and all products that may include the Aexcel ® , Choose and Save ℠ , Aetna Performance Network or Savings Plus networks. Not all plans are offered in all service areas.
- All services deemed "never effective" are excluded from coverage. Aetna defines a service as "never effective" when it is not recognized according to professional standards of safety and effectiveness in the United States for diagnosis, care or treatment. Visit the secure website, available through www.aetna.com, for more information. Click on "Claims," "CPT/HCPCS Coding Tool," "Clinical Policy Code Search."
- The five character codes included in the Aetna Precertification Code Search Tool are obtained from Current Procedural Terminology (CPT ® ), copyright 2023 by the American Medical Association (AMA). CPT is developed by the AMA as a listing of descriptive terms and five character identifying codes and modifiers for reporting medical services and procedures performed by physicians.
- The responsibility for the content of Aetna Precertification Code Search Tool is with Aetna and no endorsement by the AMA is intended or should be implied. The AMA disclaims responsibility for any consequences or liability attributable or related to any use, nonuse or interpretation of information contained in Aetna Precertification Code Search Tool. No fee schedules, basic unit values, relative value guides, conversion factors or scales are included in any part of CPT. Any use of CPT outside of Aetna Precertification Code Search Tool should refer to the most Current Procedural Terminology which contains the complete and most current listing of CPT codes and descriptive terms. Applicable FARS/DFARS apply.
LICENSE FOR USE OF CURRENT PROCEDURAL TERMINOLOGY, FOURTH EDITION ("CPT ® ")
- CPT only Copyright 2023 American Medical Association. All Rights Reserved. CPT is a registered trademark of the American Medical Association. You, your employees and agents are authorized to use CPT only as contained in Aetna Precertification Code Search Tool solely for your own personal use in directly participating in health care programs administered by Aetna, Inc. You acknowledge that AMA holds all copyright, trademark and other rights in CPT. Any use not authorized herein is prohibited, including by way of illustration and not by way of limitation, making copies of CPT for resale and/or license, transferring copies of CPT to any party not bound by this agreement, creating any modified or derivative work of CPT, or making any commercial use of CPT. License to sue CPT for any use not authorized herein must be obtained through the American Medical Association, CPT Intellectual Property Services, 515 N. State Street, Chicago, Illinois 60610. Applications are available at the American Medical Association Web site, www.ama-assn.org/go/cpt.
U.S. Government Rights
This product includes CPT which is commercial technical data and/or computer data bases and/or commercial computer software and/or commercial computer software documentation, as applicable which were developed exclusively at private expense by the American Medical Association, 515 North State Street, Chicago, Illinois, 60610. U.S. Government rights to use, modify, reproduce, release, perform, display, or disclose these technical data and/or computer data bases and/or computer software and/or computer software documentation are subject to the limited rights restrictions of DFARS 252.227-7015(b)(2) (June 1995) and/or subject to the restrictions of DFARS 227.7202-1(a) (June 1995) and DFARS 227.7202-3(a) (June 1995), as applicable for U.S. Department of Defense procurements and the limited rights restrictions of FAR 52.227-14 (June 1987) and/or subject to the restricted rights provisions of FAR 52.227-14 (June 1987) and FAR 52.227-19 (June 1987), as applicable, and any applicable agency FAR Supplements, for non-Department of Defense Federal procurements.
Disclaimer of Warranties and Liabilities.
CPT is provided "as is" without warranty of any kind, either expressed or implied, including but not limited to the implied warranties of merchantability and fitness for a particular purpose. No fee schedules, basic unit, relative values or related listings are included in CPT. The American Medical Association (AMA) does not directly or indirectly practice medicine or dispense medical services. The responsibility for the content of this product is with Aetna, Inc. and no endorsement by the AMA is intended or implied. The AMA disclaims responsibility for any consequences or liability attributable to or related to any use, non-use, or interpretation of information contained or not contained in this product.
This Agreement will terminate upon notice if you violate its terms. The AMA is a third party beneficiary to this Agreement.
Should the foregoing terms and conditions be acceptable to you, please indicate your agreement and acceptance by selecting the button labeled "I Accept".
The information contained on this website and the products outlined here may not reflect product design or product availability in Arizona. Therefore, Arizona residents, members, employers and brokers must contact Aetna directly or their employers for information regarding Aetna products and services.
This information is neither an offer of coverage nor medical advice. It is only a partial, general description of plan or program benefits and does not constitute a contract. In case of a conflict between your plan documents and this information, the plan documents will govern.
Dental clinical policy bulletins
- Aetna Dental Clinical Policy Bulletins (DCPBs) are developed to assist in administering plan benefits and do not constitute dental advice. Treating providers are solely responsible for dental advice and treatment of members. Members should discuss any Dental Clinical Policy Bulletin (DCPB) related to their coverage or condition with their treating provider.
- While the Dental Clinical Policy Bulletins (DCPBs) are developed to assist in administering plan benefits, they do not constitute a description of plan benefits. The Dental Clinical Policy Bulletins (DCPBs) describe Aetna's current determinations of whether certain services or supplies are medically necessary, based upon a review of available clinical information. Each benefit plan defines which services are covered, which are excluded, and which are subject to dollar caps or other limits. Members and their providers will need to consult the member's benefit plan to determine if there are any exclusions or other benefit limitations applicable to this service or supply. Aetna's conclusion that a particular service or supply is medically necessary does not constitute a representation or warranty that this service or supply is covered (i.e., will be paid for by Aetna). Your benefits plan determines coverage. Some plans exclude coverage for services or supplies that Aetna considers medically necessary. If there is a discrepancy between this policy and a member's plan of benefits, the benefits plan will govern. In addition, coverage may be mandated by applicable legal requirements of a State or the Federal government.
- Please note also that Dental Clinical Policy Bulletins (DCPBs) are regularly updated and are therefore subject to change.
- Since Dental Clinical Policy Bulletins (DCPBs) can be highly technical and are designed to be used by our professional staff in making clinical determinations in connection with coverage decisions, members should review these Bulletins with their providers so they may fully understand our policies.
- Under certain plans, if more than one service can be used to treat a covered person's dental condition, Aetna may decide to authorize coverage only for a less costly covered service provided that certain terms are met.
Medical clinical policy bulletins
- Aetna Clinical Policy Bulletins (CPBs) are developed to assist in administering plan benefits and do not constitute medical advice. Treating providers are solely responsible for medical advice and treatment of members. Members should discuss any Clinical Policy Bulletin (CPB) related to their coverage or condition with their treating provider.
- While the Clinical Policy Bulletins (CPBs) are developed to assist in administering plan benefits, they do not constitute a description of plan benefits. The Clinical Policy Bulletins (CPBs) express Aetna's determination of whether certain services or supplies are medically necessary, experimental and investigational, or cosmetic. Aetna has reached these conclusions based upon a review of currently available clinical information (including clinical outcome studies in the peer-reviewed published medical literature, regulatory status of the technology, evidence-based guidelines of public health and health research agencies, evidence-based guidelines and positions of leading national health professional organizations, views of physicians practicing in relevant clinical areas, and other relevant factors).
- Aetna makes no representations and accepts no liability with respect to the content of any external information cited or relied upon in the Clinical Policy Bulletins (CPBs). The discussion, analysis, conclusions and positions reflected in the Clinical Policy Bulletins (CPBs), including any reference to a specific provider, product, process or service by name, trademark, manufacturer, constitute Aetna's opinion and are made without any intent to defame. Aetna expressly reserves the right to revise these conclusions as clinical information changes, and welcomes further relevant information including correction of any factual error.
- CPBs include references to standard HIPAA compliant code sets to assist with search functions and to facilitate billing and payment for covered services. New and revised codes are added to the CPBs as they are updated. When billing, you must use the most appropriate code as of the effective date of the submission. Unlisted, unspecified and nonspecific codes should be avoided.
- Each benefit plan defines which services are covered, which are excluded, and which are subject to dollar caps or other limits. Members and their providers will need to consult the member's benefit plan to determine if there are any exclusions or other benefit limitations applicable to this service or supply. The conclusion that a particular service or supply is medically necessary does not constitute a representation or warranty that this service or supply is covered (i.e., will be paid for by Aetna) for a particular member. The member's benefit plan determines coverage. Some plans exclude coverage for services or supplies that Aetna considers medically necessary. If there is a discrepancy between a Clinical Policy Bulletin (CPB) and a member's plan of benefits, the benefits plan will govern.
- In addition, coverage may be mandated by applicable legal requirements of a State, the Federal government or CMS for Medicare and Medicaid members.
See CMS's Medicare Coverage Center
- Please note also that Clinical Policy Bulletins (CPBs) are regularly updated and are therefore subject to change.
- Since Clinical Policy Bulletins (CPBs) can be highly technical and are designed to be used by our professional staff in making clinical determinations in connection with coverage decisions, members should review these Bulletins with their providers so they may fully understand our policies.
- While Clinical Policy Bulletins (CPBs) define Aetna's clinical policy, medical necessity determinations in connection with coverage decisions are made on a case by case basis. In the event that a member disagrees with a coverage determination, Aetna provides its members with the right to appeal the decision. In addition, a member may have an opportunity for an independent external review of coverage denials based on medical necessity or regarding the experimental and investigational status when the service or supply in question for which the member is financially responsible is $500 or greater. However, applicable state mandates will take precedence with respect to fully insured plans and self-funded non-ERISA (e.g., government, school boards, church) plans.
See Aetna's External Review Program
- The five character codes included in the Aetna Clinical Policy Bulletins (CPBs) are obtained from Current Procedural Terminology (CPT®), copyright 2015 by the American Medical Association (AMA). CPT is developed by the AMA as a listing of descriptive terms and five character identifying codes and modifiers for reporting medical services and procedures performed by physicians.
- The responsibility for the content of Aetna Clinical Policy Bulletins (CPBs) is with Aetna and no endorsement by the AMA is intended or should be implied. The AMA disclaims responsibility for any consequences or liability attributable or related to any use, nonuse or interpretation of information contained in Aetna Clinical Policy Bulletins (CPBs). No fee schedules, basic unit values, relative value guides, conversion factors or scales are included in any part of CPT. Any use of CPT outside of Aetna Clinical Policy Bulletins (CPBs) should refer to the most current Current Procedural Terminology which contains the complete and most current listing of CPT codes and descriptive terms. Applicable FARS/DFARS apply.
LICENSE FOR USE OF CURRENT PROCEDURAL TERMINOLOGY, FOURTH EDITION ("CPT®")
CPT only copyright 2015 American Medical Association. All Rights Reserved. CPT is a registered trademark of the American Medical Association.
You, your employees and agents are authorized to use CPT only as contained in Aetna Clinical Policy Bulletins (CPBs) solely for your own personal use in directly participating in healthcare programs administered by Aetna, Inc. You acknowledge that AMA holds all copyright, trademark and other rights in CPT.
Any use not authorized herein is prohibited, including by way of illustration and not by way of limitation, making copies of CPT for resale and/or license, transferring copies of CPT to any party not bound by this agreement, creating any modified or derivative work of CPT, or making any commercial use of CPT. License to use CPT for any use not authorized herein must be obtained through the American Medical Association, CPT Intellectual Property Services, 515 N. State Street, Chicago, Illinois 60610. Applications are available at the American Medical Association Web site, www.ama-assn.org/go/cpt.
Go to the American Medical Association Web site
You are now leaving the Aetna® website.
We're working with 3Won to process your request for participation. Please select "Continue to ProVault to begin the contracting and credentialing process.
Links to various non-Aetna sites are provided for your convenience only. Aetna Inc. and its affiliates are not responsible or liable for the content, accuracy or privacy practices of linked sites, or for products or services described on these sites.
FOR 20% OFF CVS HEALTH BRAND PRODUCTS:
Excludes sale and promo items, alcohol, prescriptions and copays, pseudoephedrine/ephedrine products, pre-paid, gift cards, and items reimbursed by any health plan. Not combinable with other offers. 20% discount is not valid on other CVS brands such as CVS Pharmacy, Beauty 360®, CVS, Gold Emblem® or Gold Emblem abound®. CVS reserves the right to apply the 20% discounts to qualifying items in any order within the transaction. For in-store use only.
Links to various non-Aetna sites are provided for your convenience only. Aetna Inc. and its subsidiary companies are not responsible or liable for the content, accuracy, or privacy practices of linked sites, or for products or services described on these sites.
Healthcare.gov
For a complete list of participating walk-in clinics, use our provider lookup. Walk in appointments are based on availability and not guaranteed. Online scheduling is recommended. Includes select MinuteClinic services. Not all MinuteClinic services are covered. Please consult benefit documents to confirm which services are included. Members enrolled in qualified high deductible health plans must meet their deductible before receiving covered non preventative MinuteClinic services at no cost share. However, such services are covered at negotiated contract rates. This benefit is not available in all states.

Billing Annual Wellness Visits Under Medicare, Part III
July 24, 2023
Last week, we delved deeper into the second of three types of wellness visits—Annual Wellness Visits (AWVs)—covered by Medicare. Now, let’s shift our focus to Subsequent Wellness Visits (along with addressing some of your questions).
Subsequent Wellness Visits (SWVs)
The first Annual Wellness Visit focuses on gathering information to create a Health Risk Assessment. During Subsequent Wellness Visits, which are also conducted annually, the aim is to update this information and the Health Risk Assessment. The code for Subsequent Wellness Visits is G0439, and it includes the same set of questions as the AWV. The patient is required to complete the same questionnaire as the previous year, and all the provided information must be reviewed and documented as updated. It is important to update the medication lists and prior diagnoses as well. If a health condition no longer exists or is not current (e.g., cancer, cold, ear infection), it should be either removed or marked with a HISTORY status.
Here are the complete CMS guidelines for Wellness visits:
https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/preventive-services/medicare-wellness-visits.html
Now let’s address some frequently asked questions regarding AWVs and SWVs.
- Yes, but there are certain considerations. You can bill the PHQ-9 mental health screening using code G0444 (59) with both the AWV and SWV, but only if the patient answers all nine questions, meeting the required 15 minutes for billing the screening. If the patient stops at question 2, it is not billable as it does not meet the requirements. Additionally, MOLST 99497 can be separately billed for a duration of >16 to 30 minutes.
- The billing eligibility depends on the patient’s insurance. According to Medicare regulations, routine physicals are not covered. If Medicare is the patient’s primary insurance and they have a commercial insurance policy as secondary, then bill for the AWV/SWV.
- The billing eligibility depends on the patient’s insurance. According to Medicare. regulations, routine physicals are not covered. If Medicare is the patient’s primary insurance and they have a commercial insurance policy as secondary, then bill for the AWV/SWV.
- If the senior adult has a Medicare replacement plan (such as Tufts Medicare Preferred, HMO Blue Medicare, or similar plans), either can be billed. Depending on the insurance, the patient can receive both the Medicare AWV and a routine physical, but not on the same day. Typically, these two visits would be scheduled at least six months apart.
- As always, the answer depends on the specific circumstances. Medicare wellness visits, including IPPEs, AWVs, and SWVs, are considered “hands-off” physical examinations. These visits primarily involve conversations, questions, and information gathering. They also include counseling and referrals to specialists.
- In the case of these visits, the answer is yes: You can add an additional “sick” visit to the AWV if the patient addresses new or ongoing health issues and the healthcare provider addresses chronic or new issues.
- However, when it comes to routine 99397 physicals for patients aged 65 or older, the situation becomes more complex. You can bill for an additional office visit only if (a) the health issue or problem is new or (b) a current issue is worsened or exacerbated. It is not permissible to add charges for stable health issues during the routine physical.
To revisit the beginning of this insightful journey, click the link below:
Billing Wellness Visits Under Medicare, Part I
Confused about the 2023 medical coding changes?
Register for our mid-year e/m coding check-up webinar.
Reserve your spot now: https://bit.ly/43lsWWZ
Boost your revenue cycles with the knowledge and insights shared by Nancy Entwistle, one of our medical coding experts.
Download PDF
More Coffee & Coding
More pro tips & tricks.
Apr 15, 2024
More Pro Tips & Tricks April 15, 2024 Back by popular demand: We received such a positive response to our “tips and tricks” edition of Coffee & Coding that we’ve decided to make it a recurring feature each quarter. So, we invite you to grab a fresh cup of...
The Problem with Independent Historians
Apr 8, 2024
The Problem with Independent Historians April 8, 2024 In most cases, we know who independent historians are: mothers, fathers, guardians, grandparents, or adult children. But we still see many instances when the term is incorrectly applied in the documentation—mostly,...
Making Complexity of Problems a Little Less Complex
Apr 1, 2024
Making Complexity of Problems a Little Less Complex April 1, 2024 We see a lot of questions (and confusion) over what constitutes an “acute illness with systemic symptoms.” In fact, according to the American Academy of Pediatrics, “Of the three elements that make up...
Making the Right Choice Between Level 3 and Level 4: Part Two
Mar 25, 2024
Making the Right Choice Between Level 3 and Level 4: Part Two March 25, 2024 In last week’s Coffee & Coding, we provided a refresher on key points to remember about coding appropriately for Level 3. This week let’s do the same for Level 4. Level 4 can be a little...
Level 3 or Level 4: Getting It Right
Mar 18, 2024
Level 3 or Level 4: Getting It Right March 18, 2024 Guidelines notwithstanding, deciding whether to apply Level 3 or Level 4 to a patient encounter isn’t always easy. In fact, we see a lot of inconsistency and confusion on this point. While many clinicians accurately...
Ending Confusion over Modifier 25
Mar 11, 2024
Ending Confusion over Modifier 25 March 11, 2024 It’s a big week here in Boston (my hometown). Sunday, of course, is St. Patrick’s Day. Here in Boston, we also remember March 17 as Evacuation Day—marking the anniversary of the British army leaving the city in 1776....
MDM Level 5: A Quick Refresher on a Complex Subject
Mar 4, 2024
MDM Level 5: A Quick Refresher on a Complex Subject March 4, 2024 We continue to see that, across all medical specialties, physicians are still nervous about billing for Level 5 office visits. I consistently find that many (if not most) providers code for Level 4 even...
HIPAA Compliance: Make sure you know ALL the rules
Feb 26, 2024
HIPAA Compliance: Make sure you know ALL the rules February 26, 2024 The Health Insurance Portability and Accountability Act (HIPAA) of 1996 is a federal law restricting access to individuals' private medical information. That much, I’m sure, our readers already knew....
Making sense of the new coding-by-time rules for 2024
Feb 19, 2024
Making sense of the new coding-by-time rules for 2024 February 19, 2024 We all know that the new year brings changes (some years, more than others). As it turns out, no sooner had we gotten clinicians on track with how much time belongs to the E/M CPT code set than...
How do you code a broken heart?
Feb 12, 2024
How do you code a broken heart? Plus: We answer your questions about toxicity monitoring. February 12, 2024 First things first: While remembering to apply the proper codes and include sufficient documentation, providers and coders must not lose sight of one essential...
Documentation Tips and Tricks: How to Avoid Common Mistakes
Feb 5, 2024
Documentation Tips and Tricks: How to Avoid Common Mistakes February 5, 2024 Every day we see coding mistakes that affect the accuracy of E/M coding levels. Some of them can be costly. So, in this issue of Coffee & Coding, we’ll look more closely at some of these...
Toxic diagnosis coding: What you may be missing
Jan 29, 2024
Toxic diagnosis coding: What you may be missing January 29, 2024 Three quick questions: When did you last look in that little section towards the back of your ICD-10 coding book called the Drug Table? How often have you coded an adverse reaction to a bug bite as...
Why and how to use the new SDOH codes
Jan 22, 2024
Why and how to use the new SDOH codes January 22, 2024 Social Determinants of Health (SDOH) have become increasingly important in determining the needs of patients and directing them to the help they need. For 2024, we have both a new diagnosis code as well as a new...
The long-awaited G2211 code: What you need to know
Jan 15, 2024
The long-awaited G2211 code: What you need to know January 15, 2024 There’s an important new code for 2024, and it pays (literally*) for you to know how and when to use it. Up to this point, E/M coding has failed to take into account the resources, time, and cost...
What’s changed in telehealth services?
Jan 8, 2024
What’s changed in telehealth services? January 8, 2024 The other day, another coder asked me whether post-operative services could be performed under telehealth. It occurred to me that there are probably more coders with the same questions. So, we’re devoting this...
Subscribe to Our Weekly Coffee & Coding Newsletter

Our previous issue described the requirements and introduced an encounter form for documenting these visits. Now we answer your questions about this newest Medicare benefit.
CINDY HUGHES, CPC
Fam Pract Manag. 2011;18(2):13-15
Cindy Hughes is the AAFP's coding and compliance specialist, a contributing editor to Family Practice Management and co-author of FPM 's Getting Paid blog at http://blogs.aafp.org/fpm/gettingpaid/ . Author disclosure: nothing to disclose.
The expansion of Medicare preventive services coverage that took effect on Jan. 1 of this year provides a valuable opportunity for you and your patients to focus on preventive screening and wellness, particularly in the context of an annual wellness visit (AWV), the newest Medicare benefit. However, providing and billing for such visits is, of course, complicated. Our January/February issue cover story provided an overview of Medicare preventive services and two tools to help you deliver, document and bill for them, but a single article could not cover all the details associated with these benefits. You responded with a number of good questions, the answers to which are given below.
What ICD-9 codes should be used with the HCPCS codes for annual wellness visits (G0438 and G0439)?
The Centers for Medicare & Medicaid Services (CMS) did not specify the ICD-9 codes that should be used. Individual Part-B contractors may designate specific codes, but typically ICD-9 codes in the V70 range have been accepted.
Do I understand correctly that, other than measuring vital signs, no physical exam is required?
The following vitals – height, weight, BMI or waist circumference, blood pressure and other measurements as appropriate – are the minimum requirements. Physicians must determine the level of physical examination necessary to create a personalized prevention plan based on the patient's risk factors and health goals and to encourage patient utilization of other preventive services, as this is the purpose of the AWV. Remember that you may provide other covered Medicare preventive services at the same encounter if indicated and your schedule permits, although you should check with the Medicare administrative contractor in your region to confirm that you will be paid for the additional service, as described in the next question.
If I perform the clinical breast and pelvic exam (G0101) at the same encounter as the AWV, will Medicare pay for the breast and pelvic exam in addition to the AWV?
CMS has yet to address this issue. It would be best to direct this question to your Medicare administrative contractor. For example, WPS, the contractor for Kansas, Missouri, Nebraska and Iowa, says, “Medicare can allow both services. However, you must carve out of your pricing for the AWV any services that may be duplicated in the screening breast or pelvic exam.”
In other words, because WPS considers the breast and pelvic exam to overlap with the exam portion of the AWV, physicians must subtract the amount charged for the breast and pelvic exam from their usual charge for the AWV. The Pap smear collection and handling (Q0091) could probably be charged without a reduction of the AWV fee.
Does documenting that a patient was “alert and oriented × 3” (to person, place and time) cover the requirement to “review and document the detection of any cognitive impairment that the individual may have”?
No. CMS defines the assessment as follows: “Detection of any cognitive impairment, for purposes of this section, means assessment of an individual's cognitive function by direct observation, with due consideration of information obtained by way of patient report, concerns raised by family members, friends, caretakers, or others.”
Therefore, your documentation should include an assessment gained from observation, patient interview and input from caregivers present at the encounter. CMS does not require that physicians use a specific assessment tool, but the documentation should include evidence of assessment, such as notations of the patient's general appearance, affect, speech, memory and motor skills.
Does the initial annual wellness visit (HCPCS code G0438) apply only to patients who are new to my practice?
No. The AWV codes do not distinguish between new and established patients. Rather, the initial AWV is billed the first time a Medicare beneficiary receives an AWV that includes all of the elements required by CMS. The subsequent AWV code is reported for patients who have previously received an AWV service, whether at your practice or elsewhere.
It will be difficult to be certain whether one year has elapsed since the Welcome to Medicare visit or initial AWV if the patient is new to my practice. Is it necessary to provide patients with an Advance Beneficiary Notice (ABN) so that we can bill them should they receive the subsequent service prior to their eligibility?
No ABN is required, but it is a good idea to verify the patient's preventive services eligibility and provide those who request the service prior to eligibility with an ABN confirming their agreement to pay. Based on CMS instructions to Medicare contractors, claims for an AWV provided before 11 full months have passed since the last AWV will be denied with a “PR” code, indicating patient responsibility. Note that knowledge of the patient's past preventive services, such as last colonoscopy or the onetime benefit for the pneumococcal vaccination, will facilitate development of the preventive care plan at the annual wellness visits. If your practice is not using the 270/271 electronic eligibility transactions or another Medicare eligibility inquiry program, you may wish to consider options for incorporating this into your scheduling or pre-visit preparation processes.
Where can we learn about conducting electronic eligibility inquiries to determine our patient's eligibility for Medicare preventive services?
You may contact your Medicare administrative contractor, your practice management software vendor or your claims clearinghouse for specific information on options available to you. These will likely include the 270/271 electronic inquiries that are conducted like electronic claims submissions, with the 270 sending your inquiries and the 271 returning the report to you. Another option may be to use the online provider-service portal offered by the Medicare administrative contractor; this may be less expensive and meet your needs if you don't expect to make daily inquiries. However, the 270/271 transactions likely allow for batch inquiries that could save time and effort when inquiries for multiple patients are necessary. These resources can also help determine which patients have Medicare Advantage coverage or have Medicare as a secondary payer.
What is the definition of a “health professional” or “health educator,” both of which may provide AWVs if working under the supervision of a physician, according to the regulations? Do these individuals need to have received formal education leading to a specific degree, or can they be trained?
Neither the legislation that expanded the preventive services benefits (the Affordable Care Act) nor the regulations that CMS created and implemented provide an answer to this question. Given that, the criteria may boil down to whether the person is licensed in the state, working within the scope of practice allowed by the state and, as you said, under the direct supervision of a physician. The concept of team care should enable physicians to include the licensed professionals who are best suited to provide a portion of the AWV service, based on individual patients' needs. Remember that “direct supervision” requires the physician to be in the office suite and readily available to offer assistance and direction as needed. The AWV should be billed by the supervising physician.
Note that the regulations allow physician assistants, nurse practitioners and clinical nurse specialists to provide the AWV. Physician supervision of these health care providers should align with state requirements. For instance, where direct supervision of nurse practitioners is not required, the nurse practitioner may provide and bill for the AWV under his or her NPI number.
Can I still provide a preventive service as described by CPT codes 99387 and 99397 to Medicare patients who wish to have a routine physical that doesn't include all the elements of an AWV?
Yes. The CPT preventive service codes could be submitted when the elements required for an AWV are not provided but the service meets CPT's definition of an age- and gender-appropriate preventive medicine service. These services are still not covered by Medicare Part B and as such are an out-of-pocket expense to the patient. If you provide a Medicare-covered service (such as a breast or pelvic exam) on the same date, you must subtract the Medicare payment for the covered service from your usual charge for the preventive service before billing the patient.
If a patient requests a head-to-toe physical and the AWV, may I bill for both?
CMS stated in the final rule for the 2011 Medicare Physician Fee Schedule that both services may be billed but also noted that “it would be difficult to distinguish an AWV from another preventive medicine E/M service furnished in the same encounter that would be reported under a preventive medicine services E/M CPT code as there is substantial overlap in the components of CPT codes 99381 through 99397 and HCPCS codes G0438 and G0439 reported for the AWV.” If you choose to provide and bill for both services on the same date, you should take into account the overlap of elements such as history and counseling when determining what to charge the patient for the non-covered preventive service (99381–99397).
How does payment for the AWV compare to payment for a preventive service described by CPT codes 99387 or 99397?
Since there is no Medicare coverage for the preventive services visits described by CPT, these codes are not priced in the Medicare Physician Fee Schedule. However, CMS does assign relative value units (RVUs) to them. The RVUs for the initial annual wellness visit are higher than the RVUs for either of the preventive services visits, and the RVUs for the subsequent annual wellness visit are lower than these. Here are the total RVUs assigned to each of the relevant services: G0438 – 4.74, G0439 – 3.16, 99387 – 4.16, and 99397 – 3.48. In general, the higher the RVUs, the higher the payment.
We hope these answers will make it a bit easier to provide your patients with the preventive services they need.
Continue Reading

More in FPM
More in pubmed.
Copyright © 2011 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Yearly "Wellness" visits
If you’ve had Medicare Part B (Medical Insurance) for longer than 12 months, you can get a yearly “Wellness” visit to develop or update your personalized plan to help prevent disease or disability, based on your current health and risk factors. The yearly “Wellness” visit isn’t a physical exam.
Your first yearly “Wellness” visit can’t take place within 12 months of your Part B enrollment or your “Welcome to Medicare” preventive visit. However, you don’t need to have had a “Welcome to Medicare” preventive visit to qualify for a yearly “Wellness” visit.
Your costs in Original Medicare
You pay nothing for this visit if your doctor or other health care provider accepts assignment .
The Part B deductible doesn’t apply.
However, you may have to pay coinsurance , and the Part B deductible may apply if your doctor or other health care provider performs additional tests or services during the same visit that Medicare doesn't cover under this preventive benefit.
If Medicare doesn't cover the additional tests or services (like a routine physical exam), you may have to pay the full amount.
Your doctor or other health care provider will ask you to fill out a questionnaire, called a “Health Risk Assessment,” as part of this visit. Answering these questions can help you and your doctor develop a personalized prevention plan to help you stay healthy and get the most out of your visit. Your visit may include:
- Routine measurements (like height, weight, and blood pressure).
- A review of your medical and family history.
- A review of your current prescriptions.
- Personalized health advice.
- Advance care planning .
Your doctor or other health care provider will also perform a cognitive assessment to look for signs of dementia, including Alzheimer’s disease. Signs of cognitive impairment include trouble remembering, learning new things, concentrating, managing finances, and making decisions about your everyday life. If your doctor or other health care provider thinks you may have cognitive impairment, Medicare covers a separate visit to do a more thorough review of your cognitive function and check for conditions like dementia, depression, anxiety, or delirium and design a care plan.
If you have a current prescription for opioids, your doctor or other health care provider will review your potential risk factors for opioid use disorder, evaluate your severity of pain and current treatment plan, provide information on non-opioid treatment options, and may refer you to a specialist, if appropriate. Your doctor or other health care provider will also review your potential risk factors for substance use disorder, like alcohol and tobacco use , and refer you for treatment, if needed.
Related resources
- Preventive visits
- Social determinants of health risk assessment
Is my test, item, or service covered?

IMAGES
VIDEO
COMMENTS
Annual Wellness Visit (AWV) Visit to develop or update a personalized prevention plan and perform a health risk assessment. Covered once every 12 months. Patients pay nothing (if provider accepts assignment) Routine Physical Exam. Exam performed without relationship to treatment or diagnosis of a specific illness, symptom, complaint, or injury.
Learn 2023 CPT billing codes for annual wellness visits (AWVs) and understand requirements to maximize the value of G0402, G0438, G0439, 99497, and G0468. ... Subsequent Annual Wellness Visit: Is the yearly follow-up to an Initial Annual Wellness Visit. Eleven full months after the Initial Annual Wellness Visit, a patient can attend these ...
Annual Wellness Visits can be for either new or established patients as the code does not differentiate. The initial AWV, G0438, is performed on patients that have been enrolled with Medicare for more than one year. A patient is eligible for his subsequent AWV, G0439, one year after his initial visit. Remember that during the first year a ...
AWV Coding. The two CPT codes used to report AWV services are: G0438 initial visit; G0439 subsequent visit; Requirements and Components for AWV. Requirements and components for G0438 (initial ...
2. Billing for a Medicare AWV when the patient only has Medicare Part A. They must have Part B coverage as well. 3. Using the wrong primary diagnosis code. If the primary diagnosis code is problem ...
EXAMPLES. Let's look at some examples of when it would be appropriate to bill for a problem-oriented E/M code (CPT 99202-99215) along with a preventive or wellness visit. Patient 1: A 70-year-old ...
Coding and Billing AWV The two CPT codes used to report AWV services are: G0438 initial visit G0439 subsequent visit G0438: Billable for the first AWV only. Patient is eligible after the first 12 months of Medicare coverage. For services within the first 12 months, conduct the Initial Preventive Physical Exam (IPPE), also referred to as the
Medicare established two codes for billing and reimbursement of an annual wellness visit (AWV), effective for services provided on or after January 1, 2011. There are two types of AWVs: an initial visit and a subsequent visit. The initial AWV is a once-in-a-lifetime benefit, allowed after the first 12 months of Medicare enrollment have elapsed ...
Learn 2024 annual wellness visits (AWVs) CPT billing codes. Understand requirements and maximize the value of G0402, G0438, G0439, 99497, and G0468. Learn 2024 annual wellness visits (AWVs) CPT billing codes. ... Subsequent Annual Wellness Visit (G0439): Is the yearly follow-up to an Initial Annual Wellness Visit. Eleven full months after the ...
HCPCS/CPT Codes. G0438 - Initial visit; G0439 - Subsequent visit; Frequency. G0438 - Once in a lifetime; G0439 - Annually; Coverage. ... Annual Wellness Visit Educational Tool; CMS Internet Only Manual (IOM), Publication 100-02, Medicare Benefit Policy Manual, Chapter 15, Section 280.5;
Annual Wellness Visit (AWV) As part of the Affordable Care Act, Medicare provides coverage for an AWV for patients who are enrolled in Medicare. This service may be covered as often as once per year. There are two specific types of AWV: initial and subsequent. Required elements for the initial AWV include: A self-reported health risk assessment
The first Annual Wellness Visit (AWV) service must be identified with HCPCS code G0438 and subsequent AWV services with HCPCS code G0439. Documentation. Providers may scan the patient's clock-drawing test (CDT), but it is not required. At a minimum, the interpretation and scoring of the drawing must be documented.
The two CPT® codes used to report AWV services are:*. G0438 — initial visit**. G0439 — subsequent visit (no lifetime limits) Additional services (lab, X-rays, etc.) ordered during an AWV may be applied toward the patient's. deductible and/or be subject to coinsurance. Before performing additional services, discuss them.
Annual Wellness Visits "AWV" Coding Guidelines ... The Medicare Annual Wellness Visit is a valuable opportunity to build strong relationships with patients, identify and document health risks, and complete ... established office visit, IPPE Initial Subsequent G0402 G0438 G0439 The Subsequent AWV is the yearly follow-up to an IAWV. Eleven months
AWV Coding Guide 8750-9695 R3 (F) Annual Wellness Visit Coding Guide For office use only. Codes to file claims for an Annual Wellness Visit. Code Type Definition G0438 HCPCS Annual Wellness Visit - initial visit. Includes a personalized prevention plan of service (PPS). G0439 HCPCS Annual Wellness Visit - subsequent visit.
The Medicare Annual Wellness Visit (AWV) is available to patients with Medicare coverage for more than one year.* ... Subsequent Comprehensive Preventive Medicine Visit. Annual Comprehensive Visits . CPT-99391-99397. Age Group: < 1 year - 65 years and older (New Patient) Description: Subsequent comprehensive preventive care (e.g., well -child ...
The code for Subsequent Wellness Visits is G0439, and it includes the same set of questions as the AWV. The patient is required to complete the same questionnaire as the previous year, and all the provided information must be reviewed and documented as updated. It is important to update the medication lists and prior diagnoses as well.
Annual wellness visits (AWV) 1. When is an E/M service separately payable on the same DOS as the AWV? The AWV has been designed as an annual overview of the patient's health status, including elements of physical and mental health and general safety. It may be performed by clinical staff under physician or NPP supervision and includes a ...
The Affordable Care Act of 2010 created the Medicare annual wellness visit (AWV) as a way to provide patients with comprehensive preventive care services at no cost. ... A subsequent AWV can then ...
G0468. Federally qualified health center (FQHC) visit, IPPE or AWV; a FQHC visit that includes an initial preventive physical examination (IPPE) or annual wellness visit (AWV) and includes a typical bundle of Medicare-covered services that would be furnished per diem to a patient receiving an IPPE or AWV. Reporting G0468 and FQHC can be hairy ...
HCPCS Code for Annual wellness visit, includes a personalized prevention plan of service (PPPS), subsequent visit G0439 HCPCS code G0439 for Annual wellness visit, includes a personalized prevention plan of service (PPPS), subsequent visit as maintained by CMS falls under Counseling, Screening, and Prevention Services.
Cindy Hughes is the AAFP's coding and compliance specialist, ... and the RVUs for the subsequent annual wellness visit are lower than these. Here are the total RVUs assigned to each of the ...
for longer than 12 months, you can get a yearly "Wellness" visit to develop or update your personalized plan to help prevent disease or disability, based on your current health and risk factors. The yearly "Wellness" visit isn't a physical exam. Your first yearly "Wellness" visit can't take place within 12 months of your Part B ...