An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Cochrane Database Syst Rev

Schedules for home visits in the early postpartum period
Maternal complications including psychological and mental health problems and neonatal morbidity have been commonly observed in the postpartum period. Home visits by health professionals or lay supporters in the weeks following the birth may prevent health problems from becoming chronic with long‐term effects on women, their babies, and their families.
To assess outcomes for women and babies of different home‐visiting schedules during the early postpartum period. The review focuses on the frequency of home visits, the duration (when visits ended) and intensity, and on different types of home‐visiting interventions.
Search methods
We searched the Cochrane Pregnancy and Childbirth Group's Trials Register (28 January 2013) and reference lists of retrieved articles.
Selection criteria
Randomised controlled trials (RCTs) (including cluster‐RCTs) comparing different types of home‐visiting interventions enrolling participants in the early postpartum period (up to 42 days after birth). We excluded studies in which women were enrolled and received an intervention during the antenatal period (even if the intervention continued into the postnatal period) and studies recruiting only women from specific high‐risk groups. (e.g. women with alcohol or drug problems).
Data collection and analysis
Study eligibility was assessed by at least two review authors. Data extraction and assessment of risk of bias were carried out independently by at least two review authors. Data were entered into Review Manager software.
Main results
We included data from 12 randomised trials with data for more than 11,000 women. The trials were carried out in countries across the world, and in both high‐ and low‐resource settings. In low‐resource settings women receiving usual care may have received no additional postnatal care after early hospital discharge.
The interventions and control conditions varied considerably across studies with trials focusing on three broad types of comparisons: schedules involving more versus fewer postnatal home visits (five studies), schedules involving different models of care (three studies), and home versus hospital clinic postnatal check‐ups (four studies). In all but two of the included studies, postnatal care at home was delivered by healthcare professionals. The aim of all interventions was broadly to assess the wellbeing of mothers and babies, and to provide education and support, although some interventions had more specific aims such as to encourage breastfeeding, or to provide practical support.
For most of our outcomes only one or two studies provided data, and overall results were inconsistent.
There was no evidence that home visits were associated with improvements in maternal and neonatal mortality, and no consistent evidence that more postnatal visits at home were associated with improvements in maternal health. More intensive schedules of home visits did not appear to improve maternal psychological health and results from two studies suggested that women receiving more visits had higher mean depression scores. The reason for this finding was not clear. In a cluster randomised trial comparing usual care with individualised care by midwives extended up to three months after the birth, the proportions of women with Edinburgh postnatal depression scale (EPDS) scores ≥ 13 at four months was reduced in the individualised care group (RR 0.68, 95% CI 0.53 to 0.86). There was some evidence that postnatal care at home may reduce infant health service utilisation in the weeks following the birth, and that more home visits may encourage more women to exclusively breastfeed their babies. There was some evidence that home visits are associated with increased maternal satisfaction with postnatal care.
Authors' conclusions
Increasing the number of postnatal home visits may promote infant health and maternal satisfaction and more individualised care may improve outcomes for women, although overall findings in different studies were not consistent. The frequency, timing, duration and intensity of such postnatal care visits should be based upon local and individual needs. Further well designed RCTs evaluating this complex intervention will be required to formulate the optimal package.
Plain language summary
Home visits in the early period after the birth of a baby
Health problems for mothers and babies commonly occur or become apparent in the weeks following the birth. For the mothers these include postpartum haemorrhage, fever and infection, abdominal and back pain, abnormal discharge, thromboembolism, and urinary tract complications, as well as psychological and mental health problems such as postnatal depression. Mothers may also need support to establish breastfeeding. Babies are at risk of death related to infections, asphyxia, and preterm birth. Home visits by health professionals or lay supporters in the early postpartum period may prevent health problems from becoming long‐term, with effects on women, their babies, and their families. This review looked at different home‐visiting schedules in the weeks following the birth.
We included 12 randomised trials with data for more than 11,000 women. Some trials focused on physical checks of the mother and newborn, while others provided support for breastfeeding, and one included the provision of practical support with housework and childcare. They were carried out in both high‐resource countries and low‐resource settings where women receiving usual care may not have received additional postnatal care after early hospital discharge.
The trials focused on three broad types of comparisons: schedules involving more versus less postnatal home visits (five studies), schedules involving different models of care (three studies), and home versus hospital clinic postnatal check‐ups (four studies). In all but two of the included studies postnatal care at home was delivered by healthcare professionals. For most of our outcomes only one or two studies provided data and overall results were inconsistent.
There was no evidence that home visits were associated with reduced newborn deaths or serious health problems for the mothers. Women's physical and psychological health were not improved with more intensive schedules of home visits although more individualised care improved women's mental health in one study. Overall, babies were less likely to have emergency medical care if their mothers received more postnatal home visits. More home visits may have encouraged more women to exclusively breastfeed their babies. The different outcomes reported in different studies, how the outcomes were measured, and the considerable variation in the interventions and control conditions across studies were limitations of this review. The studies were of mixed quality as regards risk of bias.
More research is needed before any particular schedule of postnatal care can be recommended
Description of the condition
The postpartum period, defined by the World Health Organization (WHO) as the period from childbirth to the 42nd day following delivery ( WHO 2005 ), is critical for both mothers and newborns. An estimated 529,000 maternal deaths occur worldwide each year because of pregnancy‐related complications in the antenatal, intrapartum, and postpartum periods, especially in resource‐limited settings ( WHO 2005 ).These deaths are often sudden and unpredictable, with 11% to 17% occurring during childbirth itself and 50% to 71% occurring during the postpartum period ( WHO 2005 ). Maternal health problems commonly observed in the postpartum period include postpartum haemorrhage, fever, abdominal and back pain, abnormal discharge, puerperal genital infection, thromboembolic disease, and urinary tract complications ( Bashour 2008 ), as well as psychological and mental health problems such as postnatal depression. The postpartum period is also critical for newborns. Every year approximately 3.7 million babies die in the first four weeks of life. Most of these infants are born in developing countries and most die at home. Nearly 40% of all deaths of children younger than five years old occur within the first 28 days of life (neonatal or newborn period). Just three causes—infections, asphyxia, and preterm birth—account for nearly 80% of these deaths ( WHO/UNICEF 2009 ). Moreover, the postpartum period is a time of transition for women and their families, who are adjusting on physical, psychological, and social levels ( Shaw 2006 ). In most developed countries, postpartum hospital stays are often shorter than 48 hours following a vaginal birth; thus most postpartum care is provided in community and ambulatory‐care settings. Early intervention in the postpartum period may prevent health problems from becoming chronic with long‐term effects on women, their babies, and their families.
Description of the intervention
The purpose of a home‐visiting program is to provide support at home for mothers, babies, and families by health professionals or skilled attendants. However, a single clearly defined methodology for this intervention does not exist. Further, the term "home visiting" is used differently in various contexts ( AAP 2009 ). Since the 1970s, the length of hospital stay after childbirth has fallen dramatically in many high‐resource settings. Early postnatal discharge of healthy mothers and term infants does not appear to have adverse effects on breastfeeding or maternal depression when women are offered at least one nurse‐midwife home visit after discharge ( Brown 2002 ). Home‐visiting programs provide breastfeeding and hygiene education, parenting and child health instruction, and general support to families, successfully addressing many of the barriers to access including transportation issues, initiation of timely care, and completeness of services ( AAP 1998 ; AAP 2009 ). Several trials have assessed the impact of home‐visiting programs, especially effects on child abuse and neglect in vulnerable families ( Donovan 2007 ; Olds 1997 ; Quinlivan 2003 ). Others focused on the effectiveness and cost‐effectiveness of intensive home‐visiting programs ( Barlow 2006 ; Carabin 2005 ; McIntosh 2009 ). Some home‐visiting programs have specifically targeted high risk groups such as women suffering domestic abuse (intimate partner violence) or families that are economically or socially disadvantaged. Home‐visiting programs for high risk groups or those by child health nurses may include components during pregnancy and may continue over many months or years; such programs are outside the scope of this review and have been addressed in other Cochrane reviews ( Bennett 2008 ; Jahanfar 2013 ; Macdonald 2008 ; Turnbull 2012 ). In this review we focus on the early postnatal period following discharge from hospital.
In 2009, WHO and the United Nations Children's Fund recommended home visits by a skilled attendant in resource‐limited settings. In high‐mortality settings and where access to facility‐based care is limited, at least two home visits are recommended for all home births: the first visit should occur within 24 hours of the birth, the second visit on day three, and if possible, a third visit should be made before the end of the first week of life (day seven). For babies born in a healthcare facility, the first home visit was recommended to be made as soon as possible after the mother and baby return home with remaining visits following the same schedule as for home births ( WHO/UNICEF 2009 ).
A recent review demonstrated the effectiveness of community‐based intervention packages in improving neonatal outcomes and reducing maternal and neonatal morbidity and mortality in resource‐limited settings; home visiting is the one of the main components in each of these intervention packages. This review offers encouraging evidence of the value of integrating maternal and newborn care in community settings ( Lassi 2010 ). We, therefore, did not include intervention packages of continuous care with components of antenatal or hospital care in our review.
How the intervention might work
In high‐resource settings healthy women and babies are frequently discharged from hospital within one or two days of the birth, and in low‐resource settings women may be discharged within hours of the birth or give birth at home ( Brown 2002 ). Potentially, home visits in the first few days of the birth by healthcare professions or trained support workers offer opportunities for assessment of the mother and newborn, health education, infant feeding support, emotional or practical support and, if necessary, referral to other health professionals or agencies ( Carabin 2005 ; Donovan 2007 ; Lassi 2010 ; Shaw 2006 ). Postpartum visits may prevent health problems developing or reduce their impact by early intervention or referral. Home visits have improved coverage of key maternal and newborn care practices such as early initiation of breastfeeding, exclusive breastfeeding, skin‐to‐skin contact, delayed bathing, attention to hygiene (e.g. hand washing and water quality), umbilical cord care, infant skin care. In addition, home visits may identify conditions that require additional care or check‐up, as well as counselling regarding when to take the mother and newborn to a healthcare facility ( WHO/UNICEF 2009 ). Home visits may involve not only the assessment of the mother and newborn for physical problems but also assessment of maternal mental health, family circumstances and the home environment.
Depending on the context, home visits may take a non‐judgmental and supportive role or a more directive approach in which the goals are to monitor family compliance with standards of parenting care and ensure the newborn's health and welfare.The type of approach used can influence the ability of the carers to engage mothers and newborns, resulting in acceptance or rejection of the help offered and potential for further disengagement ( Doggett 2005 ).
Why it is important to do this review
Despite many studies and reviews, evidence regarding the effectiveness of different types of home‐visiting programs in the early postnatal period is not sufficient. In some contexts once women have been discharged from hospital there may be no, or very limited postnatal follow‐up. In higher‐resource settings once women are at home, services may be provided by a range of health and social care agencies (newborn health visitors, social workers, paediatricians and general practitioners) and may be fragmented; postnatal home visits potentially allow continuity of care after hospital discharge and for the assessment and referral of the mother and newborn.
This review addresses the following questions: do different schedules of postpartum home‐visiting programs reduce maternal/neonatal mortality and morbidities, and if they do, what is the optimal schedule for postpartum home visits? This review includes reports evaluating the frequency, timing, duration and intensity of home visits.The optimal schedule has been set out by WHO/UNICEF 2009 , however, there was no clear evidence underpinning recommendations.
The primary objective of this review is to assess outcomes (maternal and newborn mortality) of different home‐visiting schedules during the early postpartum period. The review focuses on the frequency of home visits (how many home visits altogether), the timing (when visits started, e.g. within 48 hours of the birth), duration (when visits ended), intensity (how many visits per week), and different types of home‐visiting interventions.
Criteria for considering studies for this review
Types of studies.
We included studies that compared outcomes after home visits with outcomes of no home visits or different types of home‐visiting interventions; studies that used random or quasi‐random allocations of participants; and those in which the unit of allocation was the individual or group (cluster‐randomised). We also planned to include studies available only as abstracts, noting that these studies were awaiting assessment, pending publication of the full report. There was, however, no such study identified.
Types of participants
Eligible studies were ones that enrolled participants in the early postpartum period (up to 42 days after birth). We excluded studies in which women were enrolled and received an intervention during the antenatal period, even those in which the intervention continued into the postnatal period.
We planned to exclude studies that only recruited women from specific high‐risk groups (e.g. women identified with alcohol or drug problems) as interventions to support such women have been addressed elsewhere ( Turnbull 2012 ).
Types of interventions
Interventions included scheduled home visiting in the postpartum period (excluding studies with antenatal home visiting in which the visits continued over many months). Interventions were home visits with various frequency, timings, duration and intensity.
We planned to include studies with co‐intervention(s). Home visits may include outreach visits to non‐healthcare facilities. Trials including a group that did not receive home visits would have been eligible but would have been analysed separately.
Types of outcome measures
Primary outcomes.
- Maternal mortality at 42 days post birth.
- Neonatal mortality.
Secondary outcomes
Maternal outcomes.
- Maternal morbidities (postpartum haemorrhage, puerperal fever, abdominal and back pain, abnormal discharge, puerperal genital infection, thromboembolic disease, and urinary tract complications) within 42 days after birth.
- Maternal mental health (depression, anxiety) and related problems (intimate partner violence, drug use) at 42 days after birth.
- Satisfaction with overall care and service at 42 days after birth.
Neonatal outcomes
- Neonatal morbidities (pneumonia, upper respiratory tract infection, diarrhoea, septic meningitis, encephalopathy or cerebral injury, and jaundice) within 28 days after birth.
- Established feeding regimen (e.g. exclusive breastfeeding) at 28 days after birth.
- Incomplete immunisation.
- Failure to thrive, abuse, neglect, domestic violence from parents for any reason within 28 days after birth.
Search methods for identification of studies
Electronic searches.
We contacted the Trials Search Co‐ordinator to search the Cochrane Pregnancy and Childbirth Group’s Trials Register (28 January 2013).
The Cochrane Pregnancy and Childbirth Group’s Trials Register is maintained by the Trials Search Co‐ordinator and contains trials identified from:
- monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
- weekly searches of MEDLINE;
- weekly searches of Embase;
- handsearches of 30 journals and the proceedings of major conferences;
- weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Details of the search strategies for CENTRAL, MEDLINE and Embase, the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service can be found in the ‘Specialized Register’ section within the editorial information about the Cochrane Pregnancy and Childbirth Group.
Trials identified through the searching activities described above are each assigned to a review topic (or topics). The Trials Search Co‐ordinator searches the register for each review using the topic list rather than keywords.
Searching other resources
(1) references from published studies.
We searched the reference lists of relevant trials and reviews identified.
(2) Unpublished literature
We planned to contact the authors for more details about the published trials/ongoing trials.
We did not apply any language restrictions.
Selection of studies
Two review authors (NY and SN) independently assessed eligibility for inclusion for all studies identified as a result of the search strategy. We resolved discrepancies by discussion and by consulting a third review author (RM).
Data extraction and management
We designed a form to extract data. For eligible studies, two review authors (NY and SN) extracted the data using the agreed form. We resolved discrepancies through discussion. We entered data into the Review Manager (RevMan) software ( RevMan 2012 ) and checked for accuracy.
If information regarding any of the above had been unclear, we planned to contact authors of the original reports to provide further details.
Assessment of risk of bias in included studies
Two review authors (TD and NY) independently assessed the risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions ( Higgins 2011 ). We resolved any disagreement by discussion or by involving an additional assessor (RM).
(1) Sequence generation (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
- low risk of bias (any truly random process, e.g. random number table; computer random number generator);
- high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
- unclear risk of bias.
(2) Allocation concealment (checking for possible selection bias)
We described for each included study the method used to conceal the allocation sequence in sufficient detail and determine whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
- low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
- high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
- unclear risk of bias.
(3) Blinding (checking for possible performance and detection bias)
Blinding study participants and personnel from knowledge of which intervention a participant received is generally not feasible for this type of intervention. It may however, be possible to blind outcome assessment. We considered that studies were at low risk of bias for detection bias if outcome assessors were blinded, or if we judged that the lack of blinding could not have affected the results. We assessed blinding separately for different outcomes or classes of outcomes.
- low, high or unclear risk of bias for outcome assessors.
(4) Incomplete outcome data (checking for possible attrition bias through withdrawals, dropouts, protocol deviations)
We described for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported, the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported we planned to re‐include missing data in the analyses. We were not, however, able to re‐include data, as the data were not available. We assessed methods as:
- low risk of bias (e.g. no missing outcome data; missing outcome data balanced across groups);
- high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; ‘as treated’ analysis done with substantial departure of intervention received from that assigned at randomisation);
- unclear risk of bias.
(5) Selective reporting bias
We described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
- low risk of bias (where it was clear that all of the study’s pre‐specified outcomes and all expected outcomes of interest to the review were reported);
- high risk of bias (where not all the study’s pre‐specified outcomes were reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest were reported incompletely and so could not be used; study failed to include results of a key outcome that would have been expected to have been reported);
(6) Other sources of bias
We described for each included study any concerns we have about other possible sources of bias.
We assessed whether each study was free of other problems that could put it at risk of bias:
- low risk of other bias;
- high risk of other bias;
- unclear whether there is risk of other bias.
(7) Overall risk of bias
We made explicit judgements about whether studies are at high risk of bias, according to the criteria given in the Cochrane Handbook for Systematic Reviews of Interventions ( Higgins 2011 ). With reference to (1) to (6) above, we assessed the likely magnitude and direction of the bias and whether we considered it was likely to impact on the findings. We planned to explore the impact of the level of bias through undertaking sensitivity analyses ‐ see Sensitivity analysis .
Measures of treatment effect
Dichotomous data.
For dichotomous and categorical data, we used risk ratios (RR) with 95% confidence intervals (CI) and used the summary RR to combine trials that measured the same outcome. We had also planned to use the risk difference (RD).
Continuous data
For continuous data, we used the mean difference (MD) with 95% CI if outcomes were measured in the same way between trials. If required, we would have used the standardised mean difference (SMD) to combine trials that measured the same outcome, but used different methods.
Unit of analysis issues
Cluster‐randomised trials.
We included cluster‐randomised trials in the analyses along with individually‐randomised trials. When including cluster trials, we adjusted their sample sizes using the methods described in the Cochrane Handbook for Systematic Reviews of Interventions ( Higgins 2011 ) using an estimate of the intra cluster correlation co‐efficient (ICC) derived from the trial, from a similar trial or from a study of a similar population. Where we used ICCs from other sources, we reported this and planned to conduct sensitivity analyses to investigate the effect of variation in the ICC. We identified both cluster‐randomised trials and individually‐randomised trials, and we synthesised the relevant information provided there was little heterogeneity between the study designs and the interaction between the effect of intervention and the choice of randomisation unit was considered to be unlikely.
Trials with multiple treatment arms
One trial with three arms has been included in this review as two separate studies ( Bashour 2008a ; Bashour 2008b ); to avoid double counting, the control group data (events and sample) were shared between the two study comparisons.
Dealing with missing data
For included studies, we noted levels of attrition as:
- low risk of bias (indicates no or low level of missing data on intention‐to‐treat basis);
- high risk of bias (indicates high level of missing data);
We planned to explore the impact of including studies with high levels of missing data in the overall assessment of treatment effect by using Sensitivity analysis .
For all outcomes, we carried out analyses, as far as possible, on an intention‐to‐treat (ITT) basis, i.e. we attempted to include all participants randomised to each group in the analyses, and all participants were analysed in the group to which they were allocated, regardless of whether or not they received the allocated intervention. The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
Assessment of heterogeneity
We used the T², I² and Chi² statistics to examine heterogeneity among the trials in each analysis.
We regarded heterogeneity as substantial if the I² was greater than 30% and either the T² was greater than zero, or there was a low P value (less than 0.10) in the Chi² test for heterogeneity. If we had identified substantial heterogeneity, we planned to explore it by pre‐specified subgroup analysis.
Assessment of reporting biases
Had there been 10 or more studies in the meta‐analysis, we planned to investigate reporting biases (such as publication bias) using funnel plots. We planned to assess funnel plot asymmetry visually. If asymmetry was suggested by a visual assessment, we planned to perform exploratory analyses to investigate it. In this version of the review, too few trials contributed data to allow us to carry out this planned analyses.
Data synthesis
We carried out statistical analysis using the RevMan software ( RevMan 2012 ). We used a fixed‐effect model for combining data where trials examined the same intervention, and the trials' populations and interventions were judged sufficiently similar. When there was clinical heterogeneity sufficient to expect that the underlying treatment effects differed between trials, or when substantial statistical heterogeneity was detected, we used random‐effects meta‐analysis to produce an overall summary if an average treatment effect across trials was considered clinically meaningful. The random‐effects summary was treated as the average range of possible treatment effects and we discussed the clinical implications of treatment effects differing between trials. When the average treatment effect was not clinically meaningful, we did not combine trials. If we had identified heterogeneity for different types of study designs, we planned to carry out separate meta‐analysis by type of studies (individually‐randomised trial, cluster‐randomised trial).
Subgroup analysis and investigation of heterogeneity
We planned to perform a subgroup analysis according to the following clinically logical predefined groups.
- Initiation of the intervention (within 48 hours after birth or later).
- Duration of the intervention (< three weeks or ≥ three weeks).
- Intensity or frequency of the intervention (< one visit/week versus ≥ one visit/week.).
- Person doing the visit: medical professional versus skilled attendant.
- Parity: primiparity versus multiparity.
However, interventions in included trials were too heterogeneous to conduct subgroup analyses planned as above, and we therefore decided to conduct subgroup analyses by intensity/frequency of the intervention only in the comparison of more versus fewer home visits as below.
- Any number of home visits versus no home visit.
- Four or more home visits versus fewer than four visits.
- More home visits versus fewer home visits (both groups had more than four visits).
We planned subgroup analyses on both the primary and secondary outcomes.
For post hoc analyses, we considered a 99% CI excluding a zero treatment effect as statistically significant.
Also, when we identified substantial heterogeneity, we investigated it using subgroup analyses and sensitivity analyses. We considered whether an overall summary was meaningful, and where it was, used random‐effects analysis to produce it.
We assessed differences between subgroups using interaction tests available in RevMan 2012 .
Sensitivity analysis
We planned to perform sensitivity analyses to explore the effect of trial quality on the primary analysis and primary outcomes.
We planned to explore any risk of bias associated with a particular aspect of study quality (e.g. high risk of bias for allocation concealment) by sensitivity analyses.
Where we included cluster‐randomised trials, we planned to carry out sensitivity analysis using a range of values for intra class correlation coefficients.
Description of studies
Results of the search.
The search of the Cochrane Pregnancy and Childbirth Group's Trials Register identified 21 reports, and our additional searches of reference lists identified eight reports. Some studies resulted in multiple publications and one duplicate report. The 28 unique reports equated to 24 separate studies. After assessing eligibility we included 12 studies (one trial with three arms has been reported in this review as two separate studies ( Bashour 2008a ; Bashour 2008b )). We excluded 10 studies. Two reports are awaiting further assessment pending translation from the original Spanish ( Furnieles‐Paterna 2011 ; Salazar 2011 ) and more information about these trials is set out in Characteristics of studies awaiting classification tables.
Included studies
After assessing eligibility we included 12 randomised trials with a total of 11,287 women.
Three of the trials ( Christie 2011 ; Kronborg 2007 ; MacArthur 2002 ) were cluster‐randomised and health centres or healthcare staff were the units of randomisation. For these trials event rates and, or sample sizes have been adjusted in the analysis to take account of cluster design effect.
One of the trials included three arms; women in the intervention groups received either four or one home visits, while the control group received no visits. In order for us to set out the results for all three groups we have reported this trial as though it was two studies ( Bashour 2008a ; Bashour 2008b ). In the Data and analyses , women receiving four visits versus no visits are entered under Bashour 2008a ; whereas one versus no visits are compared in Bashour 2008b . The events and sample number for the control group have been divided between these comparisons to avoid double counting.
Results of trials were published between 1998 and 2012 although study data may have been collected some years before publication (e.g. in Ransjo‐Arvidson 1998 women were recruited between 1989 and 1992).
The studies were carried out in countries across the globe in both high‐ and low‐resource settings. Three studies were carried out the USA ( Escobar 2001 ; Lieu 2000 ; Paul 2012 ), three in the UK ( Christie 2011 ; MacArthur 2002 ; Morrell 2000 ), two in Canada ( Gagnon 2002 ; Steel 2003 ), and one each in Turkey ( Aksu 2010 ), Syria ( Bashour 2008a ; Bashour 2008b ), Denmark ( Kronborg 2007 ) and Zambia ( Ransjo‐Arvidson 1998 ). It is important to take the time and setting into account when interpreting results as routine practice varied across time and in different settings; for example, in the UK usual care may have involved up to seven home visits, whereas in other settings there may have been no postnatal care after hospital discharge.
The number and type of visits examined varied considerably across these trials, and control conditions also varied. Broadly, trials examined three types of comparisons: schedules involving more versus less postnatal home visits; schedules involving different models of care; and home versus hospital clinic postnatal follow‐up. In view of the complexity of interventions we have set out the main components of interventions and a description of control conditions in Table 4 .
1. Schedules involving more versus fewer home visits
In five of our included studies the main comparison was between women receiving more versus fewer home visits in the postnatal period.
Aksu 2010 examined the effect of one postnatal visit by a trained supporter versus no postnatal visits; Bashour 2008a ; Bashour 2008b compared four or one postnatal home visits from midwives versus no home visits following hospital discharge. Ransjo‐Arvidson 1998 compared four versus one midwife home visits. In these three studies, carried out in low‐resource settings, women may have received no additional postnatal care.
In contrast, Christie 2011 and Morrell 2000 examined the impact of additional care in settings where women already received more than four postnatal visits from midwives as part of usual care. Christie 2011 compared groups receiving six versus one health visitor visits (in addition to midwifery care) and Morrell 2000 examined the impact of up to 10 visits from lay supporters; again visits were provided in addition to routine midwifery care which was available to women in both intervention and control groups. (In the data and analysis tables we have separated studies where women in both groups received more than four home visits as the impact of interventions is likely to be different from that in settings where women received no, or very limited postnatal care.)
2. Schedules comparing different models of postnatal care
Three studies examined different ways of providing postnatal care.
Steel 2003 compared the effects of two visits by public health nurses in the early postnatal period compared with a telephone screening interview with discretionary nurse home visits.
In a cluster‐randomised trial Kronborg 2007 looked at the effects of more structured postnatal visits; women in the intervention group were visited between one and three times by health visitors who had attended special training on promoting and supporting breastfeeding. Women in the control group received usual care by health visitors who had not attended the breastfeeding courses.
MacArthur 2002 compared postnatal care that was adapted to the individual needs of women and home visits extended beyond the usual period of care (flexible visits up to 10 to 12 weeks postpartum). This was compared with usual care which involved a more rigid schedule of midwife home visits confined to the early postnatal period.
3. Home versus hospital postnatal care
Four of the included studies compared outcomes in women attending hospital clinics for postnatal checks and follow‐up (usual care) versus home visits by nurses ( Escobar 2001 ; Gagnon 2002 ; Lieu 2000 ; Paul 2012 ).
For all types of comparisons the purpose of visits was broadly similar: to assess the physical health and wellbeing of mothers and babies (with referral for further care where necessary), to promote and support breastfeeding, to assess maternal emotional wellbeing and to offer health education and support. In some cases the intervention focused on a particular aspect of care (e.g. breastfeeding), whereas other interventions were more general.
The outcomes measured in different studies varied. Most studies included some measure of maternal and infant health (although the particular outcomes measured, the way they were measured, and the time of follow‐up varied considerably between studies). Health service utilisation was also reported in a number of trials. Maternal emotional wellbeing and rates of breastfeeding were reported in some of the studies, and a minority reported maternal satisfaction with postnatal care. In the data and analyses tables we have set up analyses for all prespecified outcomes even where no studies have reported results. We did this in order to illustrate gaps in the evidence, and so that empty tables can be populated in updates of the review as more data become available.
Excluded studies
Ten studies identified by the searches were excluded after assessing the full trial reports. Two trials were excluded as they focused on outcomes in women following early hospital discharge after the birth rather than on different schedules of home visits for women discharged at the same time ( Boulvain 2004 ; Carty 1990 ). Two studies did not specifically examine postnatal home visits ( Gunn 1998 ; Simons 2001 ). One study, which recruited high‐risk women, involved intervention by child health nurses, rather than more general care of the mother and baby in the early postnatal period ( Izzo 2005 ). Quinlivan 2003 also focused on a high‐risk group rather than on the impact of different schedules of care. Three excluded studies examined complex interventions that included components delivered during the antenatal period ( Korfmacher 1999 ; Lumley 2006 ; Olds 2002 ). Finally, Stanwick 1982 was excluded for methodological reasons; there were major protocol deviations in this study, with many women in the intervention group failing to receive the intervention as planned, and analysis was carried out according to treatment received rather than by randomisation group (data were not available to allow us to restore women to their original randomisation group).
Risk of bias in included studies
The included studies were of mixed methodological quality; we were unable to carry out planned sensitivity analysis (temporarily excluding studies at high or unclear risk of bias for allocation concealment) as too few studies contributed data to allow any meaningful additional analysis.
Ten of the 12 included studies used methods to generate the randomisation sequence that we judged were at low risk of bias: seven used computer‐generated sequences or external trial randomisation services ( Aksu 2010 ; Escobar 2001 ; Gagnon 2002 ; Kronborg 2007 ; Lieu 2000 ; MacArthur 2002 ; Paul 2012 ) and three used random number tables ( Christie 2011 ; Morrell 2000 ; Steel 2003 ). In the Bashour 2008a ; Bashour 2008b trial, it was not clear how the randomisation sequence was decided, and the method used by Ransjo‐Arvidson 1998 was assessed as being at high risk of bias.
Concealment of group allocation at the point of randomisation was assessed as being at low risk of bias in nine of the studies; five trials reported using sequentially numbered, sealed envelopes to conceal allocation ( Bashour 2008a ; Bashour 2008b ; Escobar 2001 ; Lieu 2000 ; Morrell 2000 ; Steel 2003 ) and four used external randomisation services ( Christie 2011 ; Gagnon 2002 ; Kronborg 2007 ; MacArthur 2002 ). In the trials by Aksu 2010 , Paul 2012 , and Ransjo‐Arvidson 1998 the methods used to conceal allocation were not described, or were not clear.
Blinding women and care providers to this type of intervention is not generally feasible and no attempts to achieve blinding for these groups were described. All studies were judged to be at high risk of bias for this domain. It is possible that lack of blinding may have been an important source of bias.
In seven of the trials it was reported that outcome assessors were blind to group allocation ( Bashour 2008a ; Bashour 2008b ; Escobar 2001 ; Gagnon 2002 ; Lieu 2000 ; MacArthur 2002 ; Paul 2012 ; Steel 2003 ). However, where outcome data were assessed by interview, women may have revealed their treatment group and it was not clear whether or not blinding was successful; none of the trialists reported checking the success of blinding. Blinding of outcome assessors was either not attempted or not mentioned in the remaining five trials ( Aksu 2010 ; Christie 2011 ; Kronborg 2007 ; Morrell 2000 ; Ransjo‐Arvidson 1998 ).
Incomplete outcome data
In six of the included trials sample attrition and missing data did not appear to be important sources of bias (assessed as low or unclear risk of bias) ( Bashour 2008a ; Bashour 2008b ; Christie 2011 ; Escobar 2001 ; Lieu 2000 ; Paul 2012 ; Steel 2003 ). In some trials, although attrition was balanced across groups there was more than 10% loss to follow‐up; in the Aksu 2010 trial the response rate at four months postpartum was 82%; 16% were lost to follow‐up in the Kronborg 2007 study and 15% in the trials by Gagnon 2002 and Ransjo‐Arvidson 1998 . By four months postpartum more than 20% of the sample were lost to follow‐up in the MacArthur 2002 trial. Loss to follow‐up was not balanced in the intervention and control groups in the Morrell 2000 study; while the response rate was 83% for those women receiving additional postnatal visits it was only 75% in the control group.
Selective reporting
Assessing selective reporting bias is not easy without access to study protocols, and for all studies included in the review, risk of bias was assessed from published study reports. In most, but not all of the studies the primary outcomes were specified in the methods section and trialists reported results for these outcomes. We were unable to carry out planned investigation of possible publication bias by generating funnel plots as too few studies contributed data.
Other potential sources of bias
In most of the studies there were no other obvious sources of bias. In four of the trials there was some imbalance between groups at baseline ( Escobar 2001 ; Gagnon 2002 ; Lieu 2000 ; Morrell 2000 ). In the cluster trial reported by Christie 2011 , health visitors were the unit of randomisation and it appeared that there were differences between health visitors in terms of the number of women recruited to the trial and in their practices; the impact of these differences in individual practices is unclear. In the Steel 2003 study women were recruited in two study areas and usual practice was different in each area and this led to protocol deviations; again, it is not clear how this would affect results. Finally, in the Ransjo‐Arvidson 1998 trial much of the analysis related to the intervention group only, in addition, the nature of the intervention may have affected findings. Midwives asked women about their health as part of the intervention so women in the intervention group were asked repeatedly to identify health problems, whereas women in the control group were only asked as part of follow‐up assessments; this may have affected recall and introduced a risk of response bias.This trial may also have had the potential for publication bias because the publication date was more than six years after study completion.
We have set out the 'Risk of bias' assessments for individual studies in Figure 1 and for overall bias across all studies for different bias domains in Figure 2 .

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Effects of interventions
Comparison 1: schedules involving more versus fewer home visits (five trials with 2102 women).
In five included studies the main comparison was between women receiving more versus less home visits in the postnatal period ( Aksu 2010 ; Bashour 2008a ; Bashour 2008b ; Christie 2011 ; Morrell 2000 ; Ransjo‐Arvidson 1998 ). One trial included three arms and to allow us to report findings for two different intervention groups this trial has been treated as two separate studies in this review ( Bashour 2008a ; Bashour 2008b ). One of the trials ( Christie 2011 ) was a cluster‐randomised trial and in the data and analyses tables we have used the effective sample size and event rates (adjusted for cluster design effect).
Aksu 2010 examined the effect of one postnatal visit versus no postnatal visits; Bashour 2008a ; Bashour 2008b four or one home visits versus none; Ransjo‐Arvidson 1998 four versus one home visits. Christie 2011 and Morrell 2000 examined the impact of additional care in settings where women already received more than four visits as part of usual care. Christie 2011 compared groups receiving six versus one health visitor visits (in addition to midwifery care) and Morrell 2000 up to 10 lay supporter visits versus no additional visits with routine midwifery care available to women in both intervention and control groups. (In the data and analysis tables we have separated studies where women in both groups received more than four home visits.)
For many of our prespecified outcomes only one or two studies contributed data and results were not always available for all women randomised. For each result we have specified the number of studies and women for whom data were available (for cluster‐randomised trials these are the adjusted figures). We anticipated that the treatment effect might differ in trials comparing different numbers of visits, we therefore used a random‐effects model for all analyses in this comparison.
Maternal mortality up to 42 days postpartum
Only one trial reported this outcome ( Christie 2011 ). There was no evidence of differences in maternal mortality between groups receiving additional health visitor visits compared with controls, with only one death in 951 women (risk ratio (RR) 2.46, 95% confidence interval (CI) 0.10 to 60.14, one study with 951 women) ( Analysis 1.1 ).

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 1 Maternal mortality within 42 days post birth.
Neonatal mortality
Two trials reported on neonatal death ( Bashour 2008a ; Bashour 2008b ; Ransjo‐Arvidson 1998 ); there was no strong evidence that more visits were associated with fewer deaths. Pooled results showed no evidence of differences between intervention and control groups (average RR 0.99, 95% CI 0.26 to 3.69, two studies, 1281 women), similarly women receiving four or one visits versus none, or four visits versus one had similar numbers of neonatal deaths (RR 3.06, 95% CI 0.37 to 25.39, one study, 873 women; and, RR 0.48, 95% CI 0.09 to 2.60, one study, 408 women, respectively) ( Analysis 1.2 ).

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 2 Neonatal mortality.
Severe maternal morbidity
Two studies reported this outcome, Bashour 2008a ; Bashour 2008b reported the number of women seeking medical help for a health problem and Ransjo‐Arvidson 1998 the number of women where a doctor had identified a problem up to 42 days. The numbers of women with problems were very similar in intervention and control groups and there was no evidence of differences between groups either overall, or for women receiving different patterns of visits (overall RR 0.96, 95% CI 0.81 to 1.15, two studies, 1228 women; four or one visits versus none RR 0.97, 95% CI 0.80 to 1.17, one study, 876 women; and, four visits versus one RR 0.90, 95% CI 0.52 to 1.54, one study, 352 women) ( Analysis 1.3 ).

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 3 Severe maternal morbidity.
Maternal health problems up to 42 days
Only one study reported results for most of our pre‐specified outcomes relating to maternal postpartum health problems up to 42 days after the birth ( Bashour 2008a ; Bashour 2008b ). There was no evidence of differences between women receiving four or one postnatal home visits versus none for secondary postpartum haemorrhage (RR 0.78, 95% CI 0.49 to 1.26); abdominal pain (RR 1.06, 95% CI 0.83 to 1.34); back pain (RR 0.96, 95% 0.83 to 1.11); urinary tract complications (RR 0.83, 95% CI 0.63 to 1.10); fever (RR 1.30, 95% CI 0.93 to 1.82) or dyspareunia (RR 1.18, 95% CI 0.90 to 1.55). No studies reported on thromboembolic disease or puerperal genital tract infections.
One study reported mean scores on a scale measuring maternal perceptions of their general health at six weeks postpartum ( Morrell 2000 ). There was no strong evidence of differences between women receiving additional postnatal support and controls (mean difference (MD) ‐1.60, 95% CI ‐4.72 to 1.52) ( Analysis 1.12 ).

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 12 Maternal perception of general health at 6 weeks (mean SF36).
Postnatal depression and anxiety
None of the studies included in this comparison reported the number of women with a diagnosis of depression in the postnatal period. Two studies looked at mean scores on the Edinburgh postnatal depression scale (EPDS) at six weeks ( Morrell 2000 ) and eight weeks postpartum ( Christie 2011 ). In the Morrell 2000 study women received additional support from lay people, and in Christie 2011 , women received additional health visitor support as well as routine midwife home visits. The intervention did not appear to have a positive effect in either study, and overall, women receiving the additional visits had slightly higher mean depression scores (MD 1.05, 95% CI 0.27 to 1.82) ( Analysis 1.14 ).

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 14 Mean postnatal depression score (last assessment up to 42 days postpartum).
Christie 2011 reported mean anxiety scores at eight weeks postpartum; there was no strong evidence of a difference between groups (MD 3.80, 95% CI ‐0.44 to 8.04) ( Analysis 1.16 ).

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 16 Mean maternal anxiety score (last assessment up to 42 days postpartum).
Maternal satisfaction with care in the postnatal period
Women were asked about their satisfaction with postnatal care in two studies. In one study the number of women saying they were "happy" with their postnatal experience was reported ( Bashour 2008a ; Bashour 2008b ) ( Analysis 1.17 ). Women receiving no formal postnatal care were slightly more satisfied with their experience, but there was no evidence of difference between groups, and in all groups most women reported satisfaction (RR 0.96, 0.90 to 1.02). In a second study ( Christie 2011 ), the additional support provided by health visitors was associated with increased mean satisfaction scores (MD 14.70, 95% CI 8.32 to 21.08) ( Analysis 1.18 ).

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 17 Maternal satisfaction with postnatal care.

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 18 Mean satisfaction score with postnatal care.
Infant outcomes
Neonatal health service use.
Three studies reported the number of babies requiring urgent health care during the postnatal period although the way this outcome was defined varied in the three studies ( Bashour 2008a ; Bashour 2008b reported hospital visits up to four months; Ransjo‐Arvidson 1998 doctor‐identified infant health problem at six weeks; and Christie 2011 use of emergency medical services up to eight weeks). Overall, babies were less likely to have emergency medical care if their mothers received more postnatal home visits (average RR 0.65, 95% CI 0.45 to 0.95, three studies with 1370 infants) ( Analysis 1.19 ).

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 19 Serious neonatal morbidity up to 6 months.
Breastfeeding
Exclusive breastfeeding at up to six weeks was reported in three studies. Women receiving additional support at home were more likely to be exclusively breastfeeding their babies at six weeks postpartum, and at the last assessment up to six months postpartum (average RR 1.17, 95% CI 1.01 to 1.36, three studies 960 women, and, average RR 1.38, 95% CI 1.10 to 1.73, three studies 1309 women respectively) ( Analysis 1.20 ; Analysis 1.21 ).

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 20 Exclusive breastfeeding (last assessment up to 6 weeks).

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 21 Exclusive breastfeeding (last assessment up to 6 months).
For any breastfeeding there was no evidence of differences between women receiving additional postnatal visits and controls at either six weeks or up to six months postpartum (average RR 0.89, 95% CI 0.57 to 1.38, two studies 813 women, and, average RR 1.01, 95% CI 0.99 to 1.03, two studies 1315 women, respectively) ( Analysis 1.22 ; Analysis 1.23 ).

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 22 Any breastfeeding (up to 6 weeks).

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 23 Any breastfeeding (last assessment up to 6 months).
Aksu 2010 reported mean duration of breastfeeding (months) in 54 women who had received one versus no postnatal care at home. In both groups women on average breast fed their babies for approximately a year or more, but the mean duration was increased by three months in women receiving a home visit (MD 3.00, 95% CI 2.33 to 3.67) ( Analysis 1.24 ).

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 24 Mean duration of any breastfeeding (months).
Neonatal morbidity
Two studies reported infant respiratory tract infections up to eight weeks postpartum, although the condition was not defined in the same way in the two trials. In Bashour 2008a ; Bashour 2008b the number of babies suffering a cough or cold was reported, whereas in the Ransjo‐Arvidson 1998 trial infants appeared to have more serious illness. Overall, and in individual studies there was no clear evidence of difference between groups (pooled RR 0.99, 95% CI 0.84 to 1.17, two studies 1217 infants) ( Analysis 1.25 ).

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 25 Infant respiratory tract infection within 42 days.
A single study reported on the number of infants with jaundice (not defined); very similar numbers of infants had jaundice in both intervention and control groups (RR 1.04, 95% CI 0.85 to 1.26, 861 infants) ( Analysis 1.26 ). In the same study, approximately half of the babies were reported to have had diarrhoea, however, more infants in the group receiving no visits were reported to suffer from diarrhoea compared to those whose mothers received postnatal home visits (RR 0.85, 95% CI 0.74 to 0.98, 861 infants) ( Analysis 1.27 ).

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 26 Infant jaundice.

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 27 Infant diarrhoea up to 42 days postpartum.
There were no clear differences between groups in the number of infants receiving immunisations; the vast majority of infants were immunised whether or not their mothers received postnatal care at home (RR 0.99, 95% CI 0.96 to 1.01) ( Analysis 1.28 ).

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 28 Infant immunisation took place.
Non‐prespecified outcomes
One study reported on contraceptive use at 42 days postpartum; no clear differences between groups were identified (RR 0.98, 95% CI 0.82 to 1.16) ( Analysis 1.29 ).

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 29 Non prespecified ‐ Contraceptive use.
Comparison 2: Schedules comparing different models of postnatal care (three studies with 4394 women)
Three studies are included in this comparison; each examined a different type of intervention and control condition and we have not pooled findings in meta‐analyses. In brief, Steel 2003 compared two home visits compared with a telephone screening interview with discretionary nurse home visits. In Kronborg 2007 , health visitors (HVs) were randomised, and women were visited between one and three times by HVs who had attended special training on supporting breastfeeding compared with usual care by HVs who had been specially trained. MacArthur 2002 compared individualised postnatal care up to 10 to 12 weeks postpartum with usual care, which involved a more rigid schedule of midwife home visits in the early postnatal period.
For most of our prespecified outcomes no data were reported in any of the three trials.
None of the studies reported on maternal mortality.
In the study by MacArthur 2002 there were only three neonatal deaths from a sample of 2064 women, and no significant differences between treatment groups were identified.
None of the studies reported on maternal general morbidity although MacArthur 2002 reported on the number of women with EPDS scores greater than 12 (the cut‐off used to denote high risk of postnatal depression) at four months postpartum. Women receiving individualised extended postnatal care were less likely to have EPDS scores ≥ 13 compared with women receiving routine care (RR 0.68, 95% CI 0.53 to 0.86) ( Analysis 2.9 ).

Comparison 2 Studies comparing different ways of offering postnatal care at home, Outcome 9 Postnatal depression (EPDS ≥ 13 at 4 months postpartum).
Steel 2003 reported the number of babies with health problems up to four weeks; there was no strong evidence of any difference between groups (RR 0.97, 95% CI 0.85 to 1.12) ( Analysis 2.15 ).

Comparison 2 Studies comparing different ways of offering postnatal care at home, Outcome 15 Neonatal morbidity up to 28 days.
The cluster‐randomised trial by Kronborg 2007 examined the impact of care from HVs with special training to promote and support breastfeeding. In this study there was no evidence of difference in the number of women who had stopped exclusive breastfeeding at six weeks (RR 0.81, 95% CI 0.58 to 1.14) ( Analysis 2.16 ). Few women in either group continued to exclusively breastfeed at six months and there was no evidence of difference between groups identified (RR 1.47, 95% CI 0.81 to 2.69) ( Analysis 2.17 ).

Comparison 2 Studies comparing different ways of offering postnatal care at home, Outcome 16 Stopped exclusive breastfeeding (last assessment up to 6 weeks).

Comparison 2 Studies comparing different ways of offering postnatal care at home, Outcome 17 Exclusive breastfeeding (last assessment up to 6 months).
In the study comparing home visits versus telephone screening by Steel 2003 most women in both groups were breastfeeding their babies at six weeks postpartum (any breastfeeding) and there was no clear difference between groups (RR 1.03, 95% CI 0.99 to 1.08) ( Analysis 2.18 ).

Comparison 2 Studies comparing different ways of offering postnatal care at home, Outcome 18 Any breastfeeding (up to 6 weeks).
None of our other prespecified infant outcomes were reported in any of these studies.
Comparison 3: Home versus hospital postnatal care (four studies with 3917 women)
Four studies compared women attending hospital clinics for postnatal checks (usual care) versus home visits by nurses ( Escobar 2001 ; Gagnon 2002 ; Lieu 2000 ; Paul 2012 ).
None of these studies reported on maternal or neonatal mortality.
Maternal morbidity
All four studies reported on maternal use of emergency health care in the postnatal period although there were some differences in definitions; Escobar 2001 and Lieu 2000 reported on the number of women making an urgent hospital visit up to two weeks, and Paul 2012 the number of women seeking unplanned emergency health care up to two weeks, whereas Gagnon 2002 reported hospital admissions up to eight weeks postpartum. Pooled results from these studies revealed no evidence of differences between women receiving hospital clinic versus home postnatal care (RR 1.04, 95% CI 0.85 to 1.26, four studies, 3755 women) ( Analysis 3.3 ).

Comparison 3 Postnatal visit at home vs hospital clinic visit, Outcome 3 Severe maternal morbidity.
Maternal anxiety and depression
Two studies reported on the number of women with depressive symptoms at two weeks postpartum; similar numbers of women in the intervention and control groups had symptoms (RR 1.10, 95% CI 0.93 to 1.30, two studies with 2177 women) ( Analysis 3.10 ).

Comparison 3 Postnatal visit at home vs hospital clinic visit, Outcome 10 Postnatal depression (last assessment up to 42 days postpartum).
Gagnon 2002 reported mean scores on the State Trait Anxiety Inventory (STAI) at two weeks. There were no evidence of differences between groups (MD 0.30, 95% CI ‐1.08 to 1.68, 513 women) ( Analysis 3.13 ).

Comparison 3 Postnatal visit at home vs hospital clinic visit, Outcome 13 Mean maternal anxiety score (last assessment up to 42 days postpartum).
Data on depression and anxiety were also collected in the Paul 2012 study. However, while the MDs between groups were set out, mean scores for women in the home and hospital groups were not reported and we were unable to enter data from this trial in our data and analyses tables. The authors reported no statistically significant differences in mean EPDS or STAI scores at two weeks, two months and six months postpartum.
Satisfaction with care
In two studies, women seemed to prefer home rather than hospital clinic care; postnatal care was rated as good or excellent by 68% of women in the home care group compared with 55% in the clinic group (unweighted percentages). This difference between groups was statistically significant (there was high heterogeneity for this outcome and we used a random‐effects model; average RR 1.26, 95% CI 1.09 to 1.45) ( Analysis 3.14 ). Gagnon 2002 identified no evidence of difference in mean scores for satisfaction with postnatal care at eight weeks (MD ‐0.10, 95% CI ‐0.88 to 0.68) ( Analysis 3.15 ).

Comparison 3 Postnatal visit at home vs hospital clinic visit, Outcome 14 Maternal satisfaction with postnatal care.

Comparison 3 Postnatal visit at home vs hospital clinic visit, Outcome 15 Mean satisfaction score with postnatal care.
All four studies examined at least one outcome relating to breastfeeding. Gagnon 2002 reported the number of women exclusively breastfeeding at two weeks. There was no strong evidence of differences between groups (RR 1.05, 95% CI 0.93 to 1.18) ( Analysis 3.16 ). Escobar 2001 and Lieu 2000 reported the number of women who had discontinued any breastfeeding at two weeks; again, there were no clear differences between groups (RR 0.93, 95% CI 0.78 to 1.12) ( Analysis 3.18 ). Paul 2012 examined the number of women breastfeeding at eight weeks postpartum and while slightly more women in the home visit group were still breastfeeding at this time, the difference between groups did not reach statistical significance (RR 1.09, 95% CI 1.00 to 1.18) ( Analysis 3.19 ).

Comparison 3 Postnatal visit at home vs hospital clinic visit, Outcome 16 Exclusive breastfeeding (last assessment up to 6 weeks).

Comparison 3 Postnatal visit at home vs hospital clinic visit, Outcome 18 Discontinued breastfeeding (up to 6 weeks).

Comparison 3 Postnatal visit at home vs hospital clinic visit, Outcome 19 Any breastfeeding (last assessment up to 6 months).
Infant severe morbidity and health care use
All four studies reported on infant use of emergency health care; Escobar 2001 and Lieu 2000 reported on the number of infants re‐hospitalised within two weeks of initial discharge, and Paul 2012 the number of infants requiring unplanned emergency health care up to two weeks. Gagnon 2002 reported infant hospital admissions up to eight weeks postpartum. Pooled results revealed no evidence of differences in infant health service use for women receiving hospital clinic versus home postnatal care (RR 1.11, 95% CI 0.86 to 1.43, four studies 3770 infants) ( Analysis 3.21 ).

Comparison 3 Postnatal visit at home vs hospital clinic visit, Outcome 21 Severe infant morbidity up to 6 weeks.
Planned subgroup and sensitivity analysis
For our primary outcomes we had planned subgroup analysis by when visits were initiated, by the duration and intensity of the intervention, by the person carrying out the visit (medical professional versus skilled attendant), by content of the visit, by parity, and by other potential modifying factors (e.g. study in developed versus developing country). However, within each comparison, data for our primary outcomes were scarce. For maternal mortality only one study reported findings and for neonatal mortality, within the different comparisons, at most two studies contributed data. For both of our primary outcomes event rates were low and within studies there were no significant differences between groups, nor was there evidence of heterogeneity between studies where more than one study contributed data. For these reasons, we did not think that in this version of the review subgroup analysis would throw any further light on findings. In future updates of the review, as more data become available we will carry out planned additional analysis.
Similarly, planned sensitivity analysis by risk of bias was not performed; again, too few studies contributed data to any particular analysis to make such additional analyses meaningful.
Summary of main results
In this review we have included data from 12 randomised trials with data for more than 11,000 women. The trials were carried out in countries across the world, and in both high‐ and low‐resource settings. In low‐resource settings, women receiving usual care may have received no additional postnatal care after early hospital discharge.
The interventions and control conditions varied considerably across studies with trials focusing on three broad types of comparisons: schedules involving more versus fewer postnatal home visits (five studies), schedules involving different models of care (three studies), and home versus hospital clinic postnatal check‐ups (four studies). In all but two of the included studies, postnatal care at home was delivered by healthcare professionals. The broad aims of all interventions were to assess the wellbeing of mothers and babies, and to provide education and support, although some interventions had more specific aims such as to encourage breastfeeding or to provide practical support.
In the five studies comparing more versus less postnatal home visits there was no evidence of differences between groups for maternal and neonatal mortality. Only one study (which reported a large number of outcomes overall) reported results for most of our outcomes relating to maternal morbidity, and there was no strong evidence that more postnatal visits at home were associated with improvements in maternal health.
Two studies examining maternal depression compared mean scores on the EPDS and results suggested that women receiving more visits had higher mean scores, denoting an increased risk of depression. The reason for this finding is not clear. It is possible that women who had more contact with healthcare professionals may have been more willing to disclose their feelings. The authors of one trial ( Morrell 2000 ), also speculated that increased provision of support may somehow disrupt women's usual support networks, or that the withdrawal of services may result in increased depression.
Two studies reported on maternal satisfaction with postnatal care and in one of these, additional health visitor support was associated with increased satisfaction scores. There was some evidence that postnatal care at home may reduce infant health service utilisation in the weeks following the birth, and that more home visits may encourage more women to exclusively breastfeed their babies. The evidence regarding any breastfeeding was less clear, although one study with a small sample size suggested that a home visit may encourage women to continue to breastfeed for longer. There was no strong evidence that infant morbidity including jaundice and respiratory tract infections was affected by home visits, although episodes of diarrhoea were reported less often by women in the groups receiving visits in a single study (this study reported a large number of outcomes and as findings were not consistent it is possible that this finding occurred by chance).
For the three studies comparing different ways of offering care involving postnatal home visits it was not clear that interventions had a consistent effect, and many of our prespecified outcomes were not reported. There did not appear to be strong evidence from two studies that experimental interventions increased the number of women breastfeeding their babies. In one study, women in the experimental groups receiving an extended programme of home visits by midwives appeared to have lower EPDS scores at four months postpartum.
Four studies examined home versus hospital clinic postnatal checks. There were no data reported for most of our outcomes. There were no clear differences between groups for maternal emergency healthcare utilisation or maternal anxiety or depression. In two studies women seemed to prefer home rather than hospital care, while a third study examining satisfaction with care did not identify any clear difference between groups. There was no strong evidence that home care was associated with an increase in breastfeeding, or that infant emergency healthcare utilisation differed between groups.
Overall completeness and applicability of evidence
The studies included in the review examined different sorts of interventions in different types of settings and drawing clear conclusions is not simple. The trials had a variety of aims with some focusing on physical checks of the mother and newborn, while others specifically aimed to provide support for breastfeeding, and one included the provision of more practical support with housework and childcare; under these circumstances it is not surprising that results from studies were not entirely consistent. This variation in aims was reflected in the choice of outcomes reported in different studies, and for most of our outcomes there were very few data. Further, for outcomes such as breastfeeding there were differences in how outcomes were measured and when. Important clinical outcomes relating to maternal and infant health were mainly not reported, and for these outcomes results were dominated by a single study. Perhaps surprisingly, not all of the studies reported maternal satisfaction with different schedules or ways of offering care; those studies that did, provided some evidence that women preferred care at home. Improved maternal satisfaction with care involving home visits may be related to women's increased health awareness, support for behavioural change, and improved access to health‐care services, however, the evidence on maternal views is still limited. There was some evidence from two studies carried out in high‐resource settings that maternal depression scores were increased in women receiving more postnatal visits; the reasons for this finding are not clear, and this finding warrants further research attention in future trials and qualitative research.
Quality of the evidence
The studies included in the review were of mixed quality as regards risk of bias. Most of the studies used methods to generate the randomisation sequence and to conceal allocation at the point of randomisation that we judged were at low risk of bias. On the other hand, blinding women and healthcare staff to this type of intervention is not generally feasible, and in many of the studies the experimental and control interventions may have been delivered by quite different staff. Although in eight of the 12 studies it was stated that outcome assessors were blind to treatment group, many of the data on breastfeeding and maternal depression, for example, were derived from interviews and it is possible that women disclosed their allocation. It is also possible that the interventions themselves led to a response bias; women in the groups receiving more care were asked to discuss their health (physical and psychological) as part of the intervention, and it is possible that this may have affected reporting of health problems as part of study assessments. Loss to follow‐up was a further problem in half of these trials. Even relatively low sample attrition (less than 5%) may mean it is more difficult to interpret results for outcomes that occur infrequently (such as serious maternal morbidity) as those with health problems may be less likely to respond. We were unable to investigate possible publication bias as too few studies contributed data.
Most of the results in the review are derived from one or two studies and several of the studies had small sample sizes; we were unable to pool many of the data in meta‐analysis; there was a lack of consistency between studies in terms of the outcomes reported, and the time and way in which outcomes were measured. In addition, there was considerably diversity in terms of the aims of interventions and the way they were delivered. These differences mean that for any one outcome there were few data and most of our results were inconclusive.
Potential biases in the review process
We are aware that authors carrying out a review may themselves introduce bias. We took a number of measures to try to reduce bias; at least two review authors carried out data extraction and assessed risk of bias. All data were checked after entry. Nevertheless, assessing risk of bias for example, requires individual judgements and it is possible that a different review team may have made different assessments.
Agreements and disagreements with other studies or reviews
Generally, postnatal home visits seem likely to increase maternal satisfaction, and may promote breastfeeding, and reduce infant morbidities, but these effects are very much dependent upon the aims of the package of the postnatal interventions. The findings are in line with what the previous literature has shown.
Implications for practice
Generally, postnatal home visits have been recommended where mothers and their newborns are discharged early to promote infant health and maternal satisfaction. However, the results of this review are inconclusive and in the absence of strong or consistent evidence the frequency, timing, duration and intensity of such postnatal care visits should be determined by individual and local needs, and where possible, should take account of maternal preferences.
Implications for research
Further well designed randomised controlled trials or any other studies evaluating this complex intervention will be required to formulate the optimal package. The design of interventions in such a trial should be based upon postpartum health priorities in each context, which would determine the intensity and content of postnatal care visits.
Feedback from MacArthur and Bick, 12 March 2015
The findings of our study ( MacArthur 2002 ) have been included in this review in the opposite direction to the results reported in our Lancet paper. The review states that the intervention group had worse (higher) EPDS scores than the control group, which is opposite to the actual findings.
The review concludes "Significantly more women receiving extended postnatal care had high EPDS scores (RR 1.47, 95% CI 1.13 to 1.92) (Analysis 2.9)". This is completely wrong as it was significantly FEWER, not more.
Similarly, the Discussion states “For the three studies comparing different ways of offering care involving postnatal home visits it was not clear that interventions had a consistent or positive effect, and many of our prespecified outcomes were not reported. There did not appear to be strong evidence from two studies that experimental interventions increased the number of women breastfeeding their babies. In one study, women in the experimental groups receiving an extended programme of home visits by health visitors appeared to have higher EPDS scores. The reason for this finding is not clear". Again this is incorrect.
This serious inaccuracy should be rectified, and the conclusions of the overall review amended.
Comment submitted by Christine MacArthur and Debra Bick, March 2015
Thanks to Professors MacArthur and Bick for this feedback. The feedback is correct ‐ in a previous version of this review data on postnatal depression scores for the MacArthur 2002 trial was entered the wrong way around and appeared to favour the control group. The review team apologises for this serious data entry mistake and the data have now been corrected. The text has also been amended in the abstract, the plain language summary, the main results section and the discussion, so that it is now clear that results from this trial show a reduction in depression scores in the group receiving an extended programme of home visits by health visitors.
Contributors
Reply from Naohiro Yonemo, Therese Dowswell, Shuko Nagai, and Rintaro Mori, April 2017
Protocol first published: Issue 9, 2011 Review first published: Issue 7, 2013
Acknowledgements
The authors would like to acknowledge the help received from the Cochrane Pregnancy and Childbirth Group and Thai Cochrane Network.
As part of the pre‐publication editorial process, this review has been commented on by three peers (an editor and two referees who are external to the editorial team), a member of the Pregnancy and Childbirth Group's international panel of consumers and the Group's Statistical Adviser
The National Institute for Health Research (NIHR) is the largest single funder of the Cochrane Pregnancy and Childbirth Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, NHS or the Department of Health.
Edited (no change to conclusions), comment added to review
Data and analyses
Comparison 1.

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 4 Secondary postpartum haemorrhage.

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 5 Abdominal pain up to 42 days postpartum.

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 6 Back pain up to 42 days postpartum.

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 9 Urinary tract complications up to 42 days postpartum.

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 10 Maternal fever up to 42 days postpartum.

Comparison 1 Schedules involving more vs fewer postpartum visits, Outcome 11 Dyspareunia.
Comparison 2

Comparison 2 Studies comparing different ways of offering postnatal care at home, Outcome 2 Neonatal mortality.
Comparison 3
Characteristics of studies, characteristics of included studies [ordered by study id].
EPDS: Edinburgh Postnatal Depression Scale ITT: intention to treat MCS: mental health score PCS: physical health score NA: not applicable RhoGAM: Rh (D) immunoglobulin SF‐36: short 36 STAI: State‐Trait Anxiety Inventory vs: versus
Characteristics of excluded studies [ordered by study ID]
Characteristics of studies awaiting assessment [ordered by study id], differences between protocol and review.
In the objectives and types of interventions sections, we changed the description of interventions. The interventions and control conditions varied considerably across studies with trials focusing on three broad types of comparisons: schedules involving more versus fewer postnatal home visits, schedules involving different models of care, and home versus hospital clinic postnatal check‐ups.
Contributions of authors
Naohiro Yonemoto, Shuko Nagai and Rintaro Mori contributed to conceptualisation of this review and development of the protocol. Naohiro Yonemoto and Shuko Nagai screened and reviewed the identified studies, and contributed to data entry. Naohiro Yonemoto contributed to the analyses. Therese Dowswell also reviewed the identified studies and contributed to analyses and preparation of the manuscript. Rintaro Mori also contributed to writing and advised on the analyses. All the review authors approved the final version of the review.
Sources of support
Internal sources.
- National Centre of Neurology and Psychiatry, Japan.
External sources
- Health and Labour Sciences Research Grants, Japan.
TD is supported by the NIHR NHS Cochrane Collaboration Programme grant scheme award for NHS‐prioritised centrally‐managed, pregnancy and childbirth systematic reviews: CPGS 10/4001/02
Declarations of interest
None known.
References to studies included in this review
Aksu 2010 {published data only}.
- Aksu H, Kucuk M, Duzgun G. The effect of postnatal breastfeeding education/support offered at home 3 days after delivery on breastfeeding duration and knowledge: a randomized trial . Journal of Maternal‐Fetal and Neonatal Medicine 2011; 24 ( 2 ):354‐61. [ PubMed ] [ Google Scholar ]
Bashour 2008a {published data only}
- Bashour HN, Kharouf MH, Abdulsalam AA, Asmar K, Tabbaa MA, Cheikha SA. Effect of postnatal home visits on maternal/infant outcomes in Syria: a randomized controlled trial . Public Health Nursing 2008; 25 ( 2 ):115‐25. [ PubMed ] [ Google Scholar ]
Bashour 2008b {published data only}
Christie 2011 {published data only}.
- Christie J, Bunting B. The effect of health visitors' postpartum home visit frequency on first‐time mothers: cluster randomised trial . International Journal of Nursing Studies 2011; 48 ( 6 ):689‐702. [ PubMed ] [ Google Scholar ]
Escobar 2001 {published data only}
- Escobar G, Braveman P, Ackerson L, Odouli R, Coleman‐Phox K, Lieu T. Home visits vs. hospital‐based group follow‐up visits after early postpartum discharge [abstract] . Pediatric Academic Societies Annual Meeting; 2001 April 28‐May 1; Baltimore, USA . 2001:Abstract no: 1111. [ PubMed ]
- Escobar GJ, Braveman PA, Ackerson L, Odouli R, Coleman‐Phox K, Capra AM, et al. A randomized comparison of home visits and hospital‐based group follow‐up visits after early postpartum discharge . Pediatrics 2001; 108 :719‐27. [ PubMed ] [ Google Scholar ]
Gagnon 2002 {published data only}
- Gagnon AJ, Dougherty G, Jimenez V, Leduc N. Randomized trial of postpartum care after hospital discharge . Pediatrics 2002; 109 ( 6 ):1074‐80. [ PubMed ] [ Google Scholar ]
Kronborg 2007 {published data only}
- Kronborg H, Vaeth M, Olsen J, Iversen L, Harder I. Effect of early postnatal breastfeeding support: a cluster‐randomized community based trial . Acta Paediatrica 2007; 96 ( 7 ):1064‐70. [ PubMed ] [ Google Scholar ]
Lieu 2000 {published data only}
- Lieu TA, Braveman PA, Escobar GJ, Fischer AF, Jensvold NG, Capra AM. A randomized comparison of home and clinic follow‐up visits after early postpartum hospital discharge . Pediatrics 2000; 105 :1058‐65. [ PubMed ] [ Google Scholar ]
MacArthur 2002 {published data only}
- MacArthur C, Winter HR, Bick DE, Knowles H, Lilford R, Henderson C, et al. Effects of redesigned community postnatal care on womens' health 4 months after birth: a cluster randomised trial . Lancet 2002; 359 :378‐85. [ PubMed ] [ Google Scholar ]
Morrell 2000 {published data only}
- Morrell CJ, Spiby H, Stewart P, Walters S, Morgan A. Costs and effectiveness of community postnatal support workers: randomised controlled trial . BMJ 2000; 321(7261) :593‐8. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Paul 2012 {published data only}
- Paul IM, Beiler JS, Schaefer EW, Hollenbeak CS, Alleman N, Sturgis SA, et al. A randomized trial of single home nursing visits vs office‐based care after nursery/maternity discharge: the Nurses for Infants Through Teaching and Assessment After the Nursery (NITTANY) Study . Archives of Pediatrics & Adolescent Medicine 2012; 166 ( 3 ):263‐70. [ PubMed ] [ Google Scholar ]
Ransjo‐Arvidson 1998 {published data only}
- Ransjo‐Arvidson AB, Chintu K, Ng'andu N, Eriksson B, Susu B, Christensson K, et al. Maternal and infant health problems after normal childbirth: a randomised controlled study in Zambia . Journal of Epidemiology & Community Health 1998; 52 :385‐91. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Steel 2003 {published data only}
- Steel O'Connor KO, Mowat DL, Scott HM, Carr PA, Dorland JL, Young Tai KF. A randomized trial of two public health nurse follow‐up programs after early obstetrical discharge: an examination of breastfeeding rates, maternal confidence and utilization and costs of health services . Canadian Journal of Public Health. Revue Canadienne de Sante Publique 2003; 94 ( 2 ):98‐103. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Young Tai KFW, O'Connor KO, Scott HM, Mowat DL, Carr PA. Do community follow‐up programs improve infant outcome after early obstetrical discharge? A randomized controlled trial. [abstract] . Pediatric Research 2000; 47 ( 4 ):161A. [ Google Scholar ]
References to studies excluded from this review
Boulvain 2004 {published data only}.
- Boulvain M, Perneger TV, Othenin‐Girard V, Petrou S, Berner M, Irion O. Home‐based versus hospital‐based postnatal care: a randomised trial . BJOG: an international journal of obstetrics and gynaecology 2004; 111 ( 8 ):807‐13. [ PubMed ] [ Google Scholar ]
Carty 1990 {published data only}
- Carty EM, Bradley CF. A randomized, controlled evaluation of early postpartum hospital discharge . Birth 1990; 17 :199‐204. [ PubMed ] [ Google Scholar ]
Gunn 1998 {published data only}
- Gunn J, Lumley J, Chondros P, Young D. Does an early postnatal check‐up improve maternal health: results from a randomised trial in Australian general practice . British Journal of Obstetrics and Gynaecology 1998; 105 ( 9 ):991‐7. [ PubMed ] [ Google Scholar ]
Izzo 2005 {published data only}
- Izzo CV, Eckenrode JJ, Smith EG, Henderson CR, Cole R, Kitzman H, et al. Reducing the impact of uncontrollable stressful life events through a program of nurse home visitation for new parents . Prevention Science 2005; 6 ( 4 ):269‐74. [ PubMed ] [ Google Scholar ]
Korfmacher 1999 {published data only}
- Korfmacher J, O'Brien R, Hiatt S, Olds D. Differences in program implementation between nurses and paraprofessionals providing home visits during pregnancy and infancy: a randomized trial . American Journal of Public Health 1999; 89 ( 12 ):1847‐51. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Lumley 2006 {published data only}
- Lumley J, Small R, Brown S, Watson L, Gunn J, Mitchell C, et al. Prism (program of resources, information and support for mothers) protocol for a community‐randomised trial [isrctn03464021] . BMC Public Health 2003; 3 :36. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lumley J, Watson L, Small R, Brown S, Mitchell C, Gunn J. Prism (program of resources, information and support for mothers): a community‐randomised trial to reduce depression and improve women's physical health six months after birth . BMC Public Health 2006; 6 :37. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Willis K, Small R, Brown S. Using documents to investigate links between implementation and sustainability in a complex community intervention: the PRISM study . Social Science & Medicine 2012; 75 ( 7 ):1222‐9. [ PubMed ] [ Google Scholar ]
Olds 2002 {published data only}
- Olds DL, Robinson J, O'Brien R, Luckey DW, Pettitt LM, Henderson CR Jr, et al. Home visiting by paraprofessionals and by nurses: a randomized, controlled trial. [Comment] . Pediatrics 2002; 110 ( 3 ):486‐96. [ PubMed ] [ Google Scholar ]
Quinlivan 2003 {published data only}
- Quinlivan JA, Box H, Evans SF. Postnatal home visits in teenage mothers: a randomised controlled trial . Lancet 2003; 361 ( 9361 ):893‐900. [ PubMed ] [ Google Scholar ]
Simons 2001 {published data only}
- Simons J, Reynolds J, Morison L. Randomised controlled trial of training health visitors to identify and help couples with relationship problems following a birth . British Journal of General Practice 2001; 51 :793‐9. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Stanwick 1982 {published data only}
- Stanwick RS, Moffat MEK, Robitaille Y, Edmond A, Dok C. An evaluation of the routine postnatal public health nurse home visit . Canadian Journal of Public Health 1982; 73 :200‐5. [ PubMed ] [ Google Scholar ]
References to studies awaiting assessment
Furnieles‐paterna 2011 {published data only}.
- Furnieles‐Paterna E, Hoyuelos‐Camara H, Montiano‐Ruiz I, Penalver‐Julve N, Fitera‐Lamas L. Randomized comparative study of the puerperal visits in the mothers house and in the health center [Spanish] [Estudio comparativo y aleatorizado de la visita puerperal en el domicilio de la madre y en el centro de salud]. Matronas Profesion 2011; 12 ( 3 ):65‐73. [ Google Scholar ]
Salazar 2011 {published data only}
- Salazar I, Sainz JA, Garcia E, Marrugal V, Garrido R. Influence of early postpartum home visits on the detection and clinical course of postpartum depression . Progresos de Obstetricia y Ginecologia 2011; 54 ( 2 ):65‐70. [ Google Scholar ]
Additional references
- American Academy of Pediatrics. Council on Child and Adolescent Health. The role of home‐visitation programs in improving health outcomes for children and families . Pediatrics 1998; 101 ( 3 ):486‐9. [ PubMed ] [ Google Scholar ]
- American Academy of Pediatrics. Council on Child and Adolescent Health. The role of preschool home‐visiting programs in improving children's developmental and health outcomes . Pediatrics 2009; 123 ( 2 ):598‐603. [ PubMed ] [ Google Scholar ]
Barlow 2006
- Barlow J, Davis H, McIntosh E, Jarrett P, Mockford C, Stewart‐Brown S. Role of home visiting in improving parenting and health in families at risk of abuse and neglect: results of a multicentre randomised controlled trial and economic evaluation . Archives of Disease in Childhood 2007; 92 ( 3 ):229‐33. [ PMC free article ] [ PubMed ] [ Google Scholar ]
Bashour 2008
Bennett 2008.
- Bennett C, Macdonald G, Dennis JA, Coren E, Patterson J, Astin M, et al. Home‐based support for disadvantaged adult mothers . Cochrane Database of Systematic Reviews 2008, Issue 1 . [DOI: 10.1002/14651858.CD003759.pub3] [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brown S, Small R, Faber B, Krastev A, Davis P. Early postnatal discharge from hospital for healthy mothers and term infants . Cochrane Database of Systematic Reviews 2002, Issue 3 . [DOI: 10.1002/14651858.CD002958] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Carabin 2005
- Carabin H, Cowan LD, Beebe LA, Skaggs VJ, Thompson D, Agbangla C. Does participation in a nurse visitation programme reduce the frequency of adverse perinatal outcomes in first‐time mothers? . Paediatric and Perinatal Epidemiology 2005; 19 ( 3 ):194‐205. [ PubMed ] [ Google Scholar ]
Doggett 2005
- Doggett C, Burrett S, Osborn DA. Home visits during pregnancy and after birth for women with an alcohol or drug problem . Cochrane Database of Systematic Reviews 2005, Issue 4 . [DOI: 10.1002/14651858.CD004456.pub2] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Donovan 2007
- Donovan EF, Ammerman RT, Besl J, Atherton H, Khoury JC, Altaye M, et al. Intensive home visiting is associated with decreased risk of infant death . Pediatrics 2007; 119 ( 6 ):1145‐51. [ PubMed ] [ Google Scholar ]
Higgins 2011
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011 . Available from www.cochrane‐handbook.org .
Jahanfar 2013
- Jahanfar S, Janssen PA, Howard LM, Dowswell T. Interventions for preventing or reducing domestic violence against pregnant women . Cochrane Database of Systematic Reviews 2013, Issue 2 . [DOI: 10.1002/14651858.CD009414.pub2] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lassi ZS, Haider BA, Bhutta ZA. Community‐based intervention packages for reducing maternal and neonatal morbidity and mortality and improving neonatal outcomes . Cochrane Database of Systematic Reviews 2010, Issue 11 . [DOI: 10.1002/14651858.CD007754.pub2] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Macdonald 2008
- Macdonald G, Bennett C, Dennis JA, Coren E, Patterson J, Astin M, et al. Home‐based support for disadvantaged teenage mothers . Cochrane Database of Systematic Reviews 2008, Issue 1 . [DOI: 10.1002/14651858.CD006723.pub2] [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
McIntosh 2009
- McIntosh E, Barlow J, Davis H, Stewart‐Brown S. Economic evaluation of an intensive home visiting programme for vulnerable families: a cost‐effectiveness analysis of a public health intervention . Journal of Public Health 2009; 31 ( 3 ):423‐33. [ PubMed ] [ Google Scholar ]
- Olds DL, Eckenrode J, Henderson CR Jr, Kitzman H, Powers J, Cole R, et al. Long‐term effects of home visitation on maternal life course and child abuse and neglect. Fifteen‐year follow‐up of a randomized trial . JAMA 1997; 278 ( 8 ):637‐43. [ PubMed ] [ Google Scholar ]
RevMan 2012 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan) . Version 5.2. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2012.
- Shaw E, Levitt C, Wong S, Kaczorowski J, McMaster University Postpartum Research Group. Systematic review of the literature on postpartum care: effectiveness of postpartum support to improve maternal parenting, mental health, quality of life, and physical health . Birth 2006; 33 ( 3 ):210‐20. [ PubMed ] [ Google Scholar ]
Turnbull 2012
- Turnbull C, Osborn DA. Home visits during pregnancy and after birth for women with an alcohol or drug problem . Cochrane Database of Systematic Reviews 2012, Issue 1 . [DOI: 10.1002/14651858.CD004456.pub3] [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- World Health Organization. Make every mother and child count . The World Health Report 2005.
WHO/UNICEF 2009
- WHO/UNICEF. Joint statement. Home visits for the newborn child: a strategy to improve survival . WHO/FCH/CAH/09.02 2009. [ PubMed ]
References to other published versions of this review
Yonemoto 2011.
- Yonemoto N, Nagai S, Mori R. Schedules for home visits in the early postpartum period . Cochrane Database of Systematic Reviews 2011, Issue 9 . [DOI: 10.1002/14651858.CD009326] [ PubMed ] [ CrossRef ] [ Google Scholar ]
Home visits by midwives in the early postnatal period
The postnatal period is a vulnerable time that involves reorientation and new experiences. Early visits by a midwife may therefore help enhance the women’s perception of coping.
Background: Postnatal care has changed over the years. The period spent in the maternity ward has gradually been reduced from five to six days to approximately two days. According to health policy, women’s and their families’ experience of pregnancy, childbirth and maternity should be coherent and holistic and provide a sense of security.
Objectives: The aim of the study is to shed light on women's experiences with home visits by a local midwife in the early postnatal period.
Method: The study is qualitative. We conducted nine semi-structured individual interviews. We analysed data by using a qualitative content analysis inspired by hermeneutic interpretation and a systematic condensation of text. The study is based on the theory of health promotion, empowerment, coping, autonomy and the relationship between the midwife and the mother.
Main results: Three main categories describe the women’s experiences:
- having control themselves,
- knowledge and support, and
- continuity and relationship with the midwife.
Conclusion: This study indicates that home visits by local midwives may contribute to women being able to cope with the new circumstances in their lives. Being able to meet women’s individual needs seems to enhance empowerment. Midwives and health visitors have different skills that can complement each other and contribute to promoting health in the postpartum period.
Postnatal care has gradually changed over recent years. Previously, the mother and child would spend five or six days in the maternity ward after a normal birth. Now, they generally go home after one or two days, depending on the woman’s health condition (1). The programme for follow-up in the early postnatal period has not been organised to keep pace with these changes. Most pregnant women are followed up by a midwife and doctor in the municipality throughout the pregnancy and give birth in a hospital with the assistance of a midwife employed at the hospital. The woman then moves to a maternity hotel or ward, where she meets other midwives whom she does not know from before.
The health visitor is usually the first person to establish contact with the woman after her return home, seven to fourteen days after the birth. The postnatal period is a vulnerable time of reorientation and new experiences, during which most women may feel a need for information and support. As a result of the pregnancy and birth, the bodily, mental and social changes may represent challenges for the women concerned (2, 3).
Guidelines for postnatal care
The national professional guidelines for postnatal care were published in 2014 to help ensure appropriate and predictable postnatal care. The municipalities provide maternity services that vary in scope and content, and the Board of Health Supervision has pointed out that the time elapsing from the women’s discharge from hospital until they contact the public health centre represents a critical period (1). The Coordination Reform provides instructions for more effort in health promotion and disease prevention. The reform proposes to bestow a key role on the municipal midwife services in the follow-up of mother and child during the first days after birth (4).
The objective of postnatal care is to help the woman establish a better sense of coping and enable her to take charge of her new life situation to the greatest possible extent, in the best interests of herself and her family (1). The midwife and the health visitor possess different skills, but in their follow-up in the early postnatal period their focus in overlapping. The national professional guidelines for postnatal care recommend that both of them undertake home visits (1).
Before the publication of the national professional guidelines for postnatal care, only very few women were visited at home by the midwife immediately after giving birth, since home visits were not included in the tasks of municipal midwives. At the time of writing, only a few municipalities have made provisions for early home visits by a midwife, and there are few studies available of postnatal care practices in Norway (1, 5).
The importance of home visits
Searches for previous research on this topic show that some studies investigate postnatal care in hospitals, while others focus on women and post-partum depression. A number of studies conclude that home visits by a midwife are important. These conclusions are based on investigations of the differences between provision of postnatal care in hospitals and in the home (6, 7), women’s experience of early discharge (8) and parents’ perception of relational continuity when midwifery students provided follow-up during the antenatal, perinatal and postnatal period (9). This study details women’s perceptions and experiences with home visits by a municipal midwife immediately after being discharged following childbirth.
Our research questions are the following:
- What could be the importance of early visits by a midwife with regard to the woman’s perception of coping in her new life situation?
- How can the midwife help in accommodating the woman’s needs in the context of home visits?
- What significance does it have for the woman that the home visit is undertaken by a midwife?
The study is based on theories of empowerment, in the sense of having as much control as possible over issues that may affect personal health. The study emphasised co-determination, redistribution of power and recognition of the woman’s competence in relation to herself (11). The correlation between relational work, perception of coping and autonomy can be regarded as fundamental for health promotion.
The research design is descriptive, with some explorative elements. We chose to use a qualitative methodology to elucidate the research question (12, 13).
We conducted nine semi-structured individual interviews. The interview guide focused on the woman’s perception of her new life situation, the experience of coping in the early postnatal period, perceptions and experiences associated with the home visit by a midwife and the relationship to the midwife.
Regional committees for medical and health research ethics (REC) have determined that the study falls outside of their mandate (reference number 2013/1140 A). The study has been reported to the Norwegian Centre for Research Data (NSD) (project number 34872) and has been implemented in compliance with guidelines for research ethics (14).
Participants
Since the first author was familiar with the field, she contacted the director of the health services and midwives in the three municipalities that conducted projects on early home visits by a midwife. Most of the visits were undertaken by the same midwife. The women were recruited through convenience sampling (15). The first author requested the municipal midwives to recruit participants consecutively after having undertaken the visit, in order to avoid selective recruitment. All the women who were asked consented to participate in the study.
The inclusion criteria were the following: a healthy child born at full term, home visit by a midwife from one to six days after birth, Norwegian-speaking, and the participation should not represent an undue burden. The participants included six primiparous and three multiparous women. The home visits were undertaken by four different midwives.
Data collection
The first author, who had no previous knowledge of the women involved, was responsible for the collection of data. She interviewed the women in their homes in the period from November 2013 to January 2014. Only the mother and child were present during the interviews, which lasted for an average of one hour. The interviews were recorded on an audio device and transcribed verbatim.
We analysed the data with inspiration from hermeneutic content interpretation and systematic text condensation (12, 16). The systematic procedure for text condensation helped achieve an appropriate handling of the large amount of text. In addition, the principles for hermeneutic content interpretation helped elicit valid interpretations in a hermeneutic perspective. This perspective implies that any interpretation depends on the prior understanding on which it is based (12).
Table 1 shows the four stages of the analysis process.
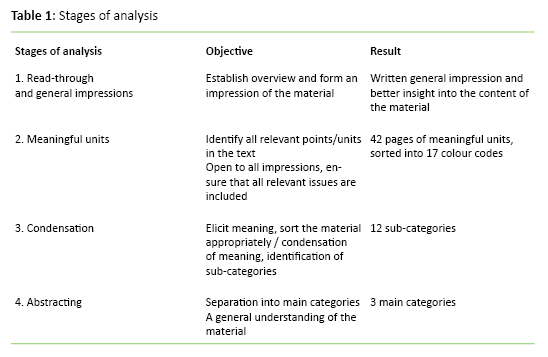
The first author repeatedly read through the entire material. She made notes of reflections and ideas along the way, before writing down the general impression. The condensation took place in an iterative process that involved all the authors, back and forth between the research questions, general impressions and units of meaning. The abstracting took place in the same way. Research questions, general impressions and sub-categories were assessed in light of each other until the categorisation became meaningful on the basis of findings and research questions. During the analysis process we focused on being aware of our preconceptions, using notes and discussions as an aid, in order to ensure valid interpretations.
Table 2 shows the categories that emerged during the analysis.
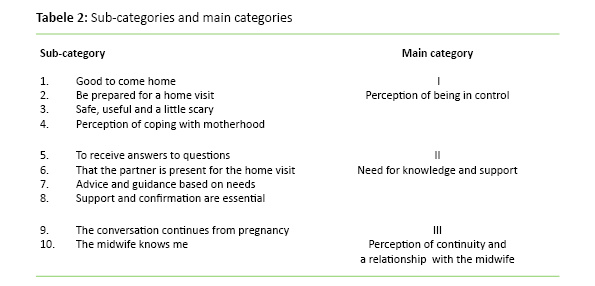
The perception of being in control
The women felt that the home visit helped provide security and calm in a hectic postnatal period. Many of them told us that they looked forward to the midwife’s visit. The women were aware of what the midwife could provide, and that the visit was voluntary and agreed beforehand. The women thus felt that they were prepared for the visit and in control of the situation:
‘When you come home, it’s much calmer than being in the hospital, it’s easier to think through the things that you wonder about or questions to be asked.’
‘It was very good that we were prepared ... that way, the entire process becomes natural and informal.’
The women felt more secure when receiving support and confirmation from the midwife.
Prior to the home visit, many of the women had believed that the visit would entail checking or assessment of the home and of them as parents. One of the mothers described it as ‘scary’. All the women described the sense of security and the advantage of receiving help based on their own needs as the key element of the home visit:
‘The impression that I had beforehand, what I learned from others, was that they come to check that everything is in order in the house and all that, but certainly also because it was the midwife, it felt just like having a friend visiting, a friend who also has the knowledge.’
The women described various experiences of coping associated with matters being as expected, and that they were able to cope with new roles and tasks. One woman had a strong perception of coping in the context of the birth itself. She described it as important for her to share this experience with the midwife during the home visit:
‘So that was really great, because now I can finally do it, and had the confirmation that I can’ (breastfeeding).
‘We did everything ourselves ... I really felt that sense of coping.’
The need for knowledge and support
During the home visit, it is crucial that the women receive answers to their questions, advice and guidance. The participants described the conversation with the midwife about the pregnancy and birth as essential for their understanding and confirmation:
‘We had prepared ourselves ... made notes of questions and such, so that we could ask about what we were unsure of.’
‘Then we talked a lot about the birth ... I really needed that – that it was her I told what I felt about or what my hopes were before the birth ... because she had been involved all the way, even though she hadn’t been present during the birth itself.’
The partner’s role in the home visit was underscored as essential, because the partner could support the woman. The partner’s questions and experiences were considered:
‘It was good that he could be there too, then we receive the same information, and he also had some questions.’
Many reported that preparing adequately for the postnatal period was difficult, and that manoeuvring through the available information could present problems:
‘No matter how well one prepares, one can never prepare enough, because one cannot know what lies ahead.’
The women’s need for counselling and guidance varied from simple advice and confirmation of normality to more comprehensive guidance regarding matters such as breastfeeding, the birth or how to cope with overwhelming emotions. The women reported feeling safer in their new role after having been provided with support and confirmation by the midwife:
‘I feel quite a lot more trust in the midwife, it’s because I know that she’s a midwife, she knows about me too, not just the baby.’
‘It’s important to hear when one is so uncertain and emotional and very fearful of doing something wrong’ (about confirmation).
Perception of continuity and the relationship to the midwife
The home visit was described as meaningful and informal. The continuity in the relationship between the woman and the midwife emerged when the woman reported that the midwife was familiar with her condition during pregnancy and that the conversation ‘flowed’ immediately. Many described how they continued the conversation with the midwife during the consultations at the public health centre:
‘With the midwife it’s like: “Hello, how did the birth go?” and then we just start chatting.’
‘After all, the midwife knows how things have gone from day one, that makes it a different conversation.’
Many of the women reported that they felt confident in discussing their emotions and experiences. The relationship to the midwife was important and appeared to help reinforce the woman’s sense of coping. One of the women was previously unfamiliar with the midwife, but described how she felt the visit was useful because of the help and support that it provided to her:
‘It wouldn’t have been as easy to sit there and be open about emotions and the birth experience with someone who does not know you a little from before.’
‘When we were talking and I was telling her about it all, I could breathe, I felt relieved.’
The women felt confident about their early discharge from the maternity ward when knowing that the midwife would come in a couple of days. Because information about the visit was provided beforehand, the woman could take control of the situation and choose whether or not to make use of this option. We interpret this to mean that predictability was important to the women. A Norwegian study confirms that being able to choose for oneself inspires confidence (17). Pursuant to the Patients’ and Users’ Rights Act, the woman is entitled to choose whether or not to accept a home visit (18).
The fact that the women believed that the visit involved being checked, can be seen as indicating that the women were in a vulnerable situation in their new role. The asymmetry of the situation, in which the woman was in need of the midwife’s help, may also have had an effect. Ruyter and collaborators claim that autonomy is not a constant, but varies in light of the condition and situation of the individual (19). The postpartum woman is in a vulnerable situation, and it may therefore be said that her autonomy may be limited. Establishing a good relationship may help the party involved in the relationship reinforce and regain her autonomy (20, 21). After the visit, none of the women felt that it had constituted a control measure. This might be associated with the fact that the relationship between the woman and the midwife was known, and that the midwife was skilled in building relationships.
All the women felt a need to discuss issues associated with the child’s weight and breastfeeding.
Other research shows that women who have received home visits are more satisfied than those who have been in a maternity ward. This is most likely due to the busy environment at the hospital and the perceived importance of continuity and relational interaction between the midwife and the woman (7, 8). When the woman feels accommodated and trusts the midwife and her skills, she can work to enhance her own insight and self-confidence through this relationship. Thereby, she obtains a better opportunity to make correct and autonomous decisions for herself and her child. This is crucial in the formation of a secure basis for the ties between mother and child, as well as for the child’s health in later life (20).
At the stage when breastfeeding had barely started, guidance in breastfeeding and feeding was essential. Breastfeeding is appropriate both in terms of child nutrition and bonding. Guidance on breastfeeding in the early postnatal period, combined with home visits, may help sustain breastfeeding over time (22, 23). All the women felt the need to discuss issues associated with the child’s weight and breastfeeding. Other important topics included how to understand the child’s signals, sleep balance and the woman’s own health.
This study shows that the ability to accommodate the child’s needs may help the women to feel a sense of coping. Other studies confirm that the child’s health and well-being are crucial for the mothers’ feeling of confidence (6, 24, 25). Seemingly, when the women felt confident about the condition of the child, they could start thinking of themselves and their own needs. Talking about the birth was important to the women. We interpret this to mean that a discussion of expectations and actual experiences could help enhance the understanding of the birth process. Most of the women described it as appropriate and natural to have this conversation with the midwife, whom they knew from before. However, one woman described it as rewarding despite her not having previous acquaintance with the midwife.
The women felt confident in talking to a midwife they knew from their pregnancy period.
Aune et al. found that during the home visit, attention was focused on perceptions and experiences from pregnancy and birth, more than on future events (9). These findings may confirm that the perception of coherence and understanding of the process are important to the women. This may corroborate the argument that midwifery skills are crucial in the early postnatal period. The women expressed difficulty in preparing adequately for the postnatal period, and felt secure when the midwife could contribute her knowledge and skills. Women may need support to take care of themselves during the first week of the postnatal period (26, 10).
The objective of the guidance is to support the woman and to provide her with better knowledge and skills to enhance her self-confidence and self-efficacy. She can thus better address her new life situation and have power, influence and control of the situation (27, 28). The study appears to show that attention to individual needs and the ability to cope helped promote empowerment in the woman, which is consistent with other studies (8, 9, 29).
Having their partner present during the home visit was important for the majority of the women. Giving both of them the opportunity to discuss their questions and thoughts may help bolster the chances of a positive and equal collaboration in their new family setting (30, 31). If the woman is provided with information to be shared later with her partner, this may result in an asymmetric relationship (19, 20).
Perception of continuity and the relationship with the midwife
The study shows that the women felt confident in speaking with a midwife they knew from their pregnancy period and who had competence with regard to the newborn child as well to them as women. The continuity in the relationship is claimed to help bolster the women’s trust in the midwife’s expertise, advice and guidance, and in addition, the midwife can reinforce the women’s trust in their own resources (9, 32).
Many of the women described how they were overwhelmed by the initial period. The postnatal period is a vulnerable time for the woman because of the major changes that occur in her life (20, 33, 34). The midwife’s skills in communication and relationship-building appear to have an impact on the benefits that the woman derives from the home visit. Razurel et al. emphasise that emotional and social support is more crucial than practical knowledge during the early postnatal period (35). Whether the women were facing challenges or a normal process appeared to have little bearing on the need to obtain support or confirmation from the midwife. The support and confirmation that the midwife gave regarding the women’s choices or understanding of the situation could provide them with confidence, self-efficacy and a sense of coping. These are the main elements of empowerment thinking and can thus be interpreted as evidence that the midwife may help promote empowerment in the woman (11, 28).
The midwife may use her skills and previous relationship with the mother to accommodate her individual needs (32, 36). This could be an opportunity for continuity, even if the woman and the midwife are not known to each other from the pregnancy period. The midwife’s professional skills may help the woman perceive consistency and continuity in her understanding of the process. Studies show that women are greatly satisfied with the information and guidance provided by the midwife during the home visit (7, 8).
Whether the women were facing challenges or a normal process appeared to have little bearing on the need to obtain support or confirmation from the midwife.
The tasks of the midwife and the health visitor overlap during the home visit; for example, both may provide guidance on breastfeeding. They both focus on health promotion and include the family, the woman and the newborn child, but they possess different skills. The midwife’s skills include maternal health, pregnancy, birth and the postnatal period (37). She makes a home visit one to six days after the woman’s discharge from hospital, when she mainly focuses on the woman and the newborn child. The midwife may, for example, help strengthen the woman in her new life situation, which may assist in developing her skills as a mother. The health visitor has competence with regard to children, adolescents and their families (38). She makes a home visit six days to two weeks after discharge, focusing on the child’s health and development within the family. The health visitor may, for example, help in establishing positive bonding and good family relationships.
Better collaboration and understanding between health visitors and midwives during home visits may help better adapt the follow-up options for the early postnatal period to the woman, the child and the individual needs of the family. Moreover, it is likely that better interdisciplinary collaboration and familiarity with each other’s competencies may help ensure a better utilisation of resources and competencies.
Validity of the study
The study elucidates the perceptions and experiences of women from home visits by a municipal midwife in the early postnatal period. This topic has not previously been highlighted in Norwegian studies. The first author is a midwife with experience from community midwifery services. She is familiar with the conditions related to the topic that the study seeks to explore. This knowledge may help lend considerable relevance to the questions in the interview guide, but may also entail the risk that certain elements are overlooked or underestimated. We attempted to reduce this risk by clarifying our preconceptions throughout the research process (12, 16, 39).
The fact that the first author is a midwife may have influenced the women, causing them not to report any negative aspects out of fear of appearing unfriendly. To reduce the risk of such an effect, the first author informed the participants about her role as a researcher prior to the interview. No questions related to midwifery were brought up during or after the interview. Reflections were noted immediately after the interview and used for purposes of validation during the analysis. We believe that undertaking the interviews in the woman’s home environment helps reinforce the validity and credibility of the study (40). The women were recruited by locally employed midwives on the basis of availability, which may have had an effect, in that the women’s attitude to home visits by a midwife was known in advance (15). Efforts were made to reduce this effect by recruiting the women consecutively after the home visits had been undertaken. This may help enhance the validity of the study.
The study shows that a community midwife may help establish a perception of consistency and continuity by maintaining regular contact with the woman throughout the pregnancy until the home visit. The visit may provide an opportunity to accommodate the women’s individual needs, in light of the previously established relationship and the midwife’s competence in maternal health, pregnancy, birth and the postnatal period. When the woman feels that she is regarded as ‘an expert on her own situation’, is permitted to participate in the process of identifying the best solutions and thus remain in control of her own life situation, this may help reinforce her empowerment.
Home visits by a midwife may thus help advance the woman’s perception of coping and reinforce her empowerment, which will promote the health of the woman, the child and the family. The midwife and the health visitor possess different skills, and home visits by both may be appropriate in terms of health promotion. Interdisciplinary collaboration is important, and more research on how best to make use of resources and skills is needed.
1. Helsedirektoratet. Nasjonal retningslinje for barselomsorgen. Nytt liv og trygg barseltid for familien. Oslo. 2014. Available at: https://helsedirektoratet.no/retningslinjer/nasjonal-faglig-retningslinje-for-barselomsorgen-nytt-liv-og-trygg-barseltid-for-familien . (Downloaded 18.06.2015).
2. Venheim MA. Barselomsorg : Plager og komplikasjoner. In: Tegnander E, Brunstad A. (ed). Jordmorboka: ansvar, funksjon og arbeidsområde. Oslo: Akribe; 2010.
3. Lundgren I, Berg M. Central concepts in the midwife-woman relationship. Scandinavian journal of caring sciences. 2007;21(2):220–8.
4. Helse- og omsorgsdepartementet. Samhandlingsreformen: rett behandling – på rett sted – til rett tid. Oslo: Regjeringen. 2009.
5. Den norske jordmorforening. Høringssvar. 2015. Availabe at: http://www.jordmorforeningen.no/Media/Filer/Hoeringssvar/Dnj_hoeringsvar_prioteringer_helsetjenesten_2015 . (Downloaded 15.05.15).
6. Hildingsson IM, Sandin-Bojö A-K. «What is could indeed be better» – Swedish women’s perceptions of early postnatal care. Midwifery. 2011;27(5):737–44.
7. Fenwick J, Butt J, Dhaliwal S, Hauck Y, Schmied V. Western Australian women's perceptions of the style and quality of midwifery postnatal care in hospital and at home. Women and Birth. 2010;23(1):10–21.
8. Johansson K, Aarts C, Darj E. First-time parents' experiences of home-based postnatal care in Sweden. Uppsala Journal of Medical Sciences. 2010;115(2):131–7.
9. Aune I, Dahlberg MU, Ingebrigtsen O. Parents’ experiences of midwifery students providing continuity of care. Midwifery. 2012;28(4):432–8.
10. Hjälmhult E, Lomborg K. Managing the first period at home with a newborn: a grounded theory study of mothers’ experiences. Scandinavian journal of caring sciences. 2012;26(4):654–62.
11. Tveiten S. Empowerment og veiledning : sykepleierens pedagogiske funksjon i helsefremmende arbeid. I: Gammersvik Å, Larsen T. (red). Helsefremmende sykepleie – i teori og praksis. Bergen: Fagbokforlaget Vigmostad & Bjørke. 2012.
12. Kvale S, Brinkmann S. Det kvalitative forskningsintervju. 2. ed. Oslo: Gyldendal Akademisk. 2009.
13. Polit DF, Beck CT. Nursing research. Generating and assessing evidence for nursing practice. 9. ed. Wolters Kluwer Health Lippincott Williams & Wilkins. 2012.
14. De nasjonale forskningsetiske komiteer. Forskningsetiske retningslinjer for samfunnsvitenskap, humaniora, juss og teologi. 2006. Available at: https://www.etikkom.no/forskningsetiske-retningslinjer/Samfunnsvitenskap-jus-og-humaniora/ . (Downloaded 18.06.2015).
15. Thagaard T. Systematikk og innlevelse. En innføring i kvalitativ metode. 4. ed. Bergen: Fagbokforlaget Vigmostad & Bjørke. 2013.
16. Malterud K. Kvalitative metoder i medisinsk forskning. En innføring. Oslo: Universitetsforlaget. 2013.
17. Henriksen L. Hva betyr helhet og kontinuitet i svangerskap, fødsel og barselomsorg for kvinner? En evaluering av Barsel hjemme, et prosjekt fra Oslo. 2010.
18. Lovdata. Lov om pasient- og brukerrettigheter. 2. juli 1999; nr. 63. [Pasient- og brukerrettighetsloven].
19. Ruyter KW, Førde R, Solbakk JH. Medisinsk og helsefaglig etikk. Oslo: Gyldendal Akademisk. 2014.
20. Schibbye A-LL. Relasjoner: et dialektisk perspektiv på eksistensiell og psykodynamisk psykoterapi. Oslo: Universitetsforlaget. 2012.
21. Goering S. Postnatal reproductive autonomy: promoting relational autonomy and self-trust in new parents. Bioethics. 2009;23(1):9–19.
22. Hansen MN. Barseltiden og amming. In: Tegnander E, Brunstad A. (ed). Jordmorboka: ansvar, funksjon og arbeidsområde. Oslo: Akribe. 2010.
23. Kronborg H, Vaeth M, Kristensen I. The effect of early postpartum home visits by health visitors: a natural experiment. Public health nursing (Boston, Mass). 2012;29(4):289–301.
24. Forster DA, McLachlan HL, Rayner J, Yelland J, Gold L, Rayner S. The early postnatal period: exploring women's views, expectations and experiences of care using focus groups in Victoria, Australia. BMC Pregnancy & Childbirth. 2008;8:27.
25. Persson EK, Fridlund B, Kvist LJ, Dykes A-K. Mothers’ sense of security in the first postnatal week: interview study. Journal of Advanced Nursing. 2011;67(1):105–16.
26. Fahey JO, Shenassa E. Understanding and meeting the needs of women in the postpartum period: The perinatal maternal health promotion model. Journal of Midwifery & Women's Health. 2013;58(6):613–21.
27. Tveiten S. Veiledning: mer enn ord. Bergen: Fagbokforlaget. 2013.
28. Askheim OP. Empowerment i helse- og sosialfaglig arbeid: floskel, styringsverktøy, eller frigjøringsstrategi? Oslo: Gyldendal Akademisk. 2012.
29. Askelsdottir B, Lam-de Jonge W, Edman G, Wiklund I. Home care after early discharge: impact on healthy mothers and newborns. Midwifery. 2013;29(8):927–34.
30. Rudman A, Waldenstrom U. Critical views on postpartum care expressed by new mothers. BMC Health Serv Res. 2007;7:178.
31. Ellberg L, Högberg U, Lindh V. «We feel like one, they see us as two»: new parents’ discontent with postnatal care. Midwifery. 2010;26(4):463–8.
32. Hunter B, Berg M, Lundgren I, Ólafsdóttir ÓÁ, Kirkham M. Relationships: The hidden threads in the tapestry of maternity care. Midwifery. 2008;24(2):132–7.
33. Brodén M. Graviditetens muligheder: en tid hvor relationer skabes og udvikles. København: Akademisk Forlag. 2004.
34. Reinar L,M. Barselomsorg; Plager og komplikasjoner. In: Tegnander E, Brunstad A. Jordmorboka: ansvar, funksjon og arbeidsområde. Oslo: Akribe. 2010.
35. Razurel C, Bruchon-Schweitzer M, Dupanloup A, Irion O, Epiney M. Stressful events, social support and coping strategies of primiparous women during the postpartum period: a qualitative study. Midwifery. 2011;27(2):237–42.
36. Aune I, Dahlberg U, Ingebrigtsen Or. Relational continuity as a model of care in practical midwifery studies. British Journal of Midwifery. 2011;19(8):515–23.
37. Rammeplan for jordmorutdanningen. Oslo: Regjeringen. 2005. Available at: https://www.regjeringen.no/globalassets/upload/kilde/kd/pla/2006/0002/ddd/pdfv/269373-rammeplan_for_jordmorutdanning_05.pdf . (Downloaded 18.06.2015).
38. Rammeplan for helsesøsterutdanningen. Oslo: Regjeringen. 2005. Available at: https://www.regjeringen.no/globalassets/upload/kilde/kd/pla/2006/0002/ddd/pdfv/269386-rammeplan_for_helsesosterutdanning_05.pdf . (Downloaded 18.06.2015).
39. Fog J. Med samtalen som udgangspunkt: det kvalitative forskningsinterview. København: Akademisk Forlag. 2004.
40. Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Education Today. 2004;24(2):105–12.

Barselomsorgen er til å gråte av
De fødende blir sendt hjem nesten før de er ferdige med fødselen, skriver leg

Kvinner med barseltraumer må ikke overlates til psykiatrien
Oppfølgingen av den nybakte morens mentale helse er helt tilfeldig, skriver G

Jordmødre etterlyser mobilvettregler for kvinner i barsel
Mange barselkvinner er ikke klar over hvor mye tid de bruker på mob
– Dette er vårt siste varsel, nå vil vi ha bedre barsel
Barselomsorgen er kampsak på årets 8. mars.

Her blir ingen barselkvinner skrevet ut etter seks timer
I Helse Nord-Trøndelag får barselkvinner være på sykehuset så lenge de har be

Jordmorforbundet kritisk til ny foreldrepermisjon
Jordmorforbundet frykter at det nye forslaget om en tredelt foreldrepermisjon

– Jordmorstillinger må øremerkes
Halvparten av landets kommuner mangler kommunal jordmortjeneste. De siste fir

Desperasjon fra barsel
Kristin Storrusten fikk et barn som skrek. Mye. Så fikk hun et barn til.

Må øke barselpermisjonen for kvinnen
Norge har for kort permisjon for mor etter fødsel ifølge EUs barseldirektiv,

Bekymret for barsel
Når Marte-Kari Løve har født, får hun være på barsel i 48 timer.

4 om barselomsorgen
Tre jordmødre og en helsesøster sier hva de mener.

Prioriter jordmødre, nå!

Jordmødre får ikke gjort det de skal
En av fire jordmødre avviser fødende kvinner.

Sykepleier klaget inn etter møte med pasient på byen

Sykepleier gikk fra demenssyk pasient utendørs i 19 minus

Ledelsesekspert: Helse må få større lønnsøkning enn alle andre

Barn døde under operasjon i Stavanger: Familien er helt knust, sier bistandsadvokat

Regjeringen går inn for å droppe karakterkrav til sykepleie

– Jeg blir nesten berusa når jeg ser vanskelige sår heles

Sykepleier/vernepleier - Enhet for sikkerhetspsykiatri


Administrativ leder for radiologer ved SUS
Operasjonssykepleier - dagkirurgi.
Bli med i det jordmorfaglige arbeidet i NSF

Spesialsykepleier operasjon i seksjonens fagteam

Seksjonsleder
Sykepleier/spesialutdannet sykepleier -akuttenhet a.

Sykepleiere til en godt krydret arbeidshverdag? Her er en PSYKT god mulighet!
Er du en trygg og positiv avdelingssykepleier.

Anestesisykepleier
Avdelingssjef - aio-avdelingen, book reviews.
Heseblesende om et rotløst og omflakkende liv
Se mennesket bak diagnosen
Ensidig om KI som helsevesenets redning
Sykepleieridentitet forklart mellom to permer

Test deg selv
Har du full kontroll? Test deg selv med Sykepleiens fagquiz'er.

Demens-sykepleier Anna Marie ble selv rammet av demens
Your baby after the birth
Having skin-to-skin contact with your baby straight after the birth can help keep her or him warm and can help with getting breastfeeding started.
First feed, weight gain and nappies
Some babies feed immediately after birth and others take a little longer.
The midwives will help you whether you choose to:
- feed with formula
- combine breast and bottle feeds
It's normal for babies to lose some weight in the first few days after birth. Putting on weight steadily after this is a sign your baby is healthy and feeding well.
Read more about your baby's weight , and your baby's nappies, including healthy poo .
Tests and checks for your baby
A children's doctor (paediatrician), midwife or newborn (neonatal) nurse will check your baby is well and will offer him or her a newborn physical examination within 72 hours of birth.
In the early days, the midwife will check your baby for signs of:
- infection of the umbilical cord or eyes
- thrush in the mouth
On day 5 to 8 after the birth, you'll be offered the blood spot (heel prick) test for your baby.
Before you baby is 5 weeks old you should be offered a newborn hearing screening test .
If your baby is in special care , these tests may be done there. If your baby is at home, the tests may be done at your home by the community midwife team.
Learn how to tell when a baby is seriously ill .
Safe sleeping for your baby
Make sure you know how to put your baby to sleep safely to reduce the risk of sudden infant death syndrome (SIDS) .
2 weeks and beyond
You don't need to bathe your baby every day. You may prefer to wash their face, neck, hands and bottom carefully instead.
Most babies will regain their birthweight in the first 2 weeks. Around this time their care will move from a midwife to a health visitor.
The health visitor will check your baby's growth and development at regular appointments and record this in your baby's personal child health record (PCHR) , also known as their "red book".
You after the birth
The maternity staff caring for you will check you're recovering well after the birth.
They will take your temperature, pulse and blood pressure.
They'll also feel your tummy (abdomen) to make sure your womb is shrinking back to its normal size.
Some women feel tummy pain when their womb shrinks, especially when they're breastfeeding. This is normal.
Seeing a midwife or health visitor
Midwives will agree a plan with you for visits at home or at a children's centre until your baby is around 10 days old. This is to check that you and your baby are well and support you in these first few days.
Bleeding after the birth (postnatal bleeding)
You'll have bleeding (lochia) from your vagina for a few weeks after you give birth.
The bleeding usually stops by the time your baby is 12 weeks old.
Non-urgent advice: Speak to your GP, midwife or health visitor if you've got postnatal bleeding and any of these:
- a high temperature over 38C
- the bleeding smells unusual for you
- tummy pain that gets worse
- the bleeding gets heavier or doesn't get any less
- lumps (clots) in the blood
- pain between the vagina and anus (perineum) that gets worse
It could be a sign of infection.
Make sure you know the signs of a serious heavy bleed after giving birth (postpartum haemorrhage, or PPH). This is rare and needs emergency care.
Immediate action required: Call 999 if you've got postnatal bleeding and:
- the bleeding suddenly gets heavier
- you feel faint, dizzy or have a pounding heart
This could mean you're having a very heavy bleed (postpartum haemorrhage) and need emergency treatment.
Read more about your body after the birth , including when you might need urgent medical attention.
Feeding your baby
When you're breastfeeding in the early days , breastfeed your baby as often as they want. This may be every 2 hours.
Let your baby decide when they've had enough (this is called baby-led feeding).
You can express your breast milk if you're having problems with breastfeeding . Problems can include breast engorgement or mastitis .
Get breastfeeding and bottle feeding advice .
Your baby's crying
Crying is your baby's way of telling you they need comfort and care. It can be hard to know what they need, especially in the early days.
There are ways you can soothe your crying baby .
How you feel
Find out how to cope if you feel stressed after having a baby . There are support services for new parents that may help.
You may feel a bit down, tearful or anxious in the first week after giving birth. This is normal.
If these feelings start later or last for more than 2 weeks after giving birth, it could be a sign of postnatal depression .
Postnatal depression and anxiety are common, and there is treatment. Speak to your midwife, GP or health visitor as soon as possible if you think you might be depressed or anxious.
Sex and contraception
You can have sex as soon as you feel ready after having a baby.
There are no rules about when to have sex after giving birth. Every woman's physical and emotional changes are different.
You can get pregnant from 3 weeks (21 days) after giving birth. This can happen before you have a period, even if you're breastfeeding.
You need to start using contraception from 21 days after the birth every time you have sex if you don't want to get pregnant again.
Talk to your doctor, midwife or contraception (family planning) nurse about contraception after having a baby . They can arrange contraception before you have sex for the first time.
Being active may feel like a challenge when you're tired, but gentle exercise after childbirth can help your body recover and may help you feel more energetic.
You should also do pelvic floor exercises to strengthen the muscles around your bladder, vagina and anus.
Page last reviewed: 8 July 2022 Next review due: 8 July 2025
- Research article
- Open access
- Published: 29 August 2018
Early postnatal home visits: a qualitative study of barriers and facilitators to achieving high coverage
- Yared Amare 1 ,
- Pauline Scheelbeek 2 ,
- Joanna Schellenberg 2 ,
- Della Berhanu 2 &
- Zelee Hill 3
BMC Public Health volume 18 , Article number: 1074 ( 2018 ) Cite this article
4776 Accesses
11 Citations
1 Altmetric
Metrics details
Timely interventions in the postnatal period are important for reducing newborn mortality, and early home visits to provide postnatal care are recommended. There has been limited success in achieving timely visits, and a better understanding of the realities of programmes is needed if improvements are to be made.
We explored barriers and facilitators to timely postnatal visits through 20 qualitative interviews and 16 focus group discussions with families and Health Extension Workers in four Ethiopian sites.
All sites reported some inaccessible areas that did not receive visits, but, Health Extension Workers in the sites with more difficult terrain were reported to make more visits that those in the more accessible areas. This suggests that information and work issues can be more important than moderate physical issues. The sites where visits were common had functioning mechanisms for alerting workers to a birth; these were not related to postnatal visits but to families informing Health Extension Workers of labour so they could call an ambulance. In the other sites, families did not know they should alert workers about a delivery, and other alert mechanisms were not functioning well. Competing activities reducing Health Extension Worker availability for visits, but in some areas workers were more organized in their division of their work and this facilitated visits. The main difference between the areas where visits were reported as common or uncommon was the general activity level of the Health Extension Worker. In the sites where workers were active and connected to the community visits occurred more often.
Conclusions
If timely postnatal home visits are to occur, CHWs need realistic catchment areas that reflect their workload. Inaccessible areas may need their own CHW. Good notification systems are essential, families will notify CHWs if they have a clear reasons to do so, and more work is needed on how to ensure notification systems function. Work ethic was a clear influencer on whether home visits occur, studies to date have focused on understanding the motivation of CHWs as a group, more studies on understanding motivation at an individual level are needed.
Peer Review reports
Approximately 2.9 million neonates die every year, which accounts for 44% of deaths among children under five years of age. 73% of these deaths are in the first week of life, and 36% on the first day [ 1 , 2 ]. This highlights the importance of timely intervention in this vulnerable period [ 2 ]. Several life saving newborn behaviours can be promoted, and interventions delivered, through early postnatal care (PNC). These include an assessment of the baby and treatment or referral, and counselling on breastfeeding, thermal care, hygiene, cord care and on danger signs [ 3 , 4 ].
Evidence shows that home visits by community health workers (CHWs) can be an effective means of delivering postnatal care in high mortality settings, and can reduce mortality [ 5 , 6 ], and this strategy has been adopted by 59 of the 75 countries in the Countdown to 2015 report [ 7 ]. Observational data suggest that these visits need to occur within 2 days of delivery to be effective [ 8 ]. The World Health Organization recommends that those who deliver at home should receive a home visit within 24 h of delivery, and those who deliver in a facility should receive PNC in the facility for the first 24 h and home visits from day three [ 3 ].
There have been mixed results in achieving timely visits. Data from sub-Saharan Africa show modest coverage of postnatal care home visits by CHWs, even in study and pilot program settings. In Malawi only 11% of women received a PNC visit within 3 days of delivery, in Tanzania only 15% within 2 days, in Uganda 26% received a visit on day 1, and in Ghana 38% received a visit on day 1 or 2 (figures calculated from authors data) [ 6 , 9 , 10 , 11 , 12 ]. Data from government programmes show even lower coverage levels [ 7 ]. Given the timing of newborn deaths and the importance of early visits, the need for research in this area has been acknowledged [ 13 ]. We identified only three quantitative studies exploring factors affecting the coverage of postnatal care home visits. A meta-analysis of quantitative data from Bangladesh, Malawi and Nepal found that early visits were more likely if a mother had been visited in pregnancy, if they had notified the CHW about the birth, and if the birth had been at home. In Ethiopia attending ANC, having more than two family meetings in pregnancy with a CHW, delivering with a CHW or skilled attendant, and having the CHW’s phone number were associated with receiving early home visits [ 14 ]. No association with maternal socio-demographic characteristics were found in any of the studies [ 10 , 11 , 14 ]. A program review that conducted qualitative interviews with government policy makers and technical specialists identified the need for a functioning primary health care system, a feasible PNC visit schedule, community demand, a functioning system to notify CHWs of a birth, and a cadre of CHWs who are qualified, motivated, have adequate time, access and transport [ 7 ]. We identified no qualitative studies at community level. Such research could provide evidence on why visits may, or may not, occur based on the experiences of the providers and beneficiaries. This paper reports the findings of a study, conducted in Ethiopia, on factors affecting early postnatal home visits by CHWs - Health Extension Workers. This is particularly timely as a Community Based Newborn Care program is currently being rolled out across the country, which includes early postnatal contacts to identify and manage neonatal sepsis at community level, and to provide counselling to families on newborn care [ 15 ].
Program description
The Health Extension Program was introduced in 2003, and has provided one year of training to over 30,000 female Health Extension Workers (HEW). Two salaried workers, educated to at least grade 10, are selected by local councils to serve an area of around 5000 people. They are stationed in health posts and are supported by a network of community volunteers, called the Health Development Army (HDA). HEWs provide health promotion, and disease prevention and treatment, both in the community and at the Health Post [ 16 , 17 , 18 ]. In 2009 a program to equip HEWs with the skills to provide essential newborn care was introduced, which included early post natal visits [ 19 ], and Community Based Newborn Care (CBNC) was added in 2014 including the identification and treatment of sepsis at community level.
Study setting selection and characteristics
The study was conducted in the Amhara and Southern Nations, Nationalities and Peoples (SNNP) regions of Ethiopia. The study was conducted in areas where the Health Extension Program, including CBNC activities, are supported by The Last Ten Kilometers programme (L10 K), a project implemented by JSI Research & Training Institute, Inc. In addition to routine HEW activities, L10 K has implemented a Community Based Data for Decision Making platform that includes tracking pregnant women, recording their service needs and linking them with the health system, and Family Conversations to promote key maternal and newborn health messages [ 20 , 21 , 22 , 23 ].
We were interested in understanding barriers and facilitators to early postnatal care within a reasonably functioning system, and L10 K provided us with a list of woreda (districts) and kebeles (lowest administrative units) that they considered had a functioning HEW and HDA system. From this list we selected two typical woreda in each region, and one kebele in each woreda that was reasonably accessible to the data collection team. We refer to the selected kebele s as kebele “A-D” to maintain anonymity. Table 1 shows the characteristics of the selected kebeles , all of which had a predominantly subsistence farming based economy. There were no reports of the use of the private sector by any study participants and we did not identify any private providers of PNC in the study areas.
Data collection
Data were collected from end of March, 2015 to May, 2015. Ethical approval was gained from the research ethics committees of the London School of Hygiene and Tropical Medicine, and from the Ministry of Science and Technology in Ethiopia. Written informed consent was obtained from all respondents. Data were collected using pre-tested semi structured guides developed by the authors. Data were collected as part of a wider study on the mechanisms of behaviour change related to key maternal and newborn care practices.
Data were collected from recent mothers, grandmothers, fathers, HEWs and HDA members using narrative and in-depth interviews, friendship pair interviews and focus group discussions. Collecting data from several respondent groups, and using a range of methods, ensured we captured a range of views and allowed for data triangulation. Sample sizes, respondent groups, the rationale for using each method, and the content related to early PNC visits are shown in Table 2 . Sample sizes were based on prior experience of when saturation was likely to be reached. The possibility of conducting additional interviews and FGDs was built into the data collection plan in case saturation was not reached as anticipated.
The recent mothers and grandmothers were identified with the assistance of HEWs and HDAs and through snowball sampling. They were eligible for inclusion if they, or their daughter/daughter in law, received at least one home visit by an HEW or HDA in the ante or postnatal period. Recent mothers were purposively selected to ensure a range of ages, educational levels, parities, sex of newborn and socio-economic status that reflected the variation within the study site. For example, less than 14% of women in the study regions had secondary school education [ 24 ], and our purposive sampling focused on women with no or primary education. Place of delivery was also set as a selection criteria but it proved difficult to get many respondents who delivered at home. Fathers were recruited through the local authorities or through the HEWs and HDAs. All HDAs in a kebele were invited for the HDA FGDs. As there were only 2 HEWs per kebele , HEWs from neighbouring health posts were invited to the HEW FGDs. Selected respondents were approached in their home or place of work by the interviewers who explained the study, answered questions and took consent. Three participants refused: one wanted to attend a funeral, and the other two were too busy with their household chores to be able to participate.
Data were collected by four trained interviewers in the local language, with translators used in SNNPR. Interviews lasted from 1 to 2 h and took place in respondents’ houses. FGDs consisted of 3–7 participants and lasted from 1.5 to 2.5 h. They were conducted in neutral locations such as community centres. Interviews and FGDs were audio-recorded and fully transcribed in English within a week of data collection. During data collection, interviewers received regular feedback from senior researchers on their transcripts, interview techniques and to discuss emerging themes. The research team met twice during data collection to ‘pre-analyse’ the data in-order to document emerging themes and identify areas that needed to be explored in subsequent interviews and focus groups and to determine if saturation had been reached.
Data analysis
We conducted a thematic analysis, this consisted of multiple readings of the postnatal care sections of the transcripts to ensure familiarity with the data, to get an understanding of the data as a whole, to begin to identify recurring ideas, and core, a-typical or notable ideas, − these were captured in reflective notes. General themes were derived deductively from the research aims, these were: Timing and content of PNC visits, reactions to PNC visits, and factors influencing the occurrence of visits. Analysis for the timing of, content and reaction to PNC was semantic/descriptive, while coding for factors influencing the occurrence of visits included examining the data for latent constructs. Interviews and focus groups were coded within the broad themes using NVIVO. Coding consisted of reading each transcript and identifying the underlying meaning of each segment of text. For each segment we considered what the segment was about, what message it was giving, what stuck out, and how it was different or similar to others segments, each segment was then given one or more code related to its underlying meaning. Codes that contained similar concepts were sorted and placed into themes. Themes and codes were refined and adjusted by looking for patterns, links and contradictions within themes. Data credibility was checked by triangulating data between respondent groups and between data collection methods. Data analysis was done by two of the senior researchers who discussed their coding regularly to enhance conceptual thinking and increased coding rigor.
There was considerable variability in the reported occurrence and timing of post-natal care (PNC) visits by HEW among the four study kebele . Respondents from all respondent groups consistently reported that HEWs in kebele A and B in Amhara visit most mothers within 3 days of giving birth. But the replacement of two longstanding HEWs by temporary workers in kebele B was reported to have led to a recent decline in visits. Visits were reported as occurring late or not at all in kebele C in SNNPR, and were said to be largely non-existent in kebele D in SNNPR. Reflecting their reportedly frequent occurrence, PNC visits in the Amhara kebeles were described as ‘ordinary’, while in kebele D respondents had ‘never heard’ of this type of visit.
Through our inductive coding three main interlinked themes related to why early PNC visit may or may not occur emerged. These were physical issues related to accessibility and transport issues; information issues related to whether the HEW knew about the delivery; and work issues related to HEW availability, HEW performance and organization. We found no pattern in relation to PNC visits and maternal education level, with nearly all of the mothers interviewed having no or primary education levels.
Physical issues
The main physical barriers to early PNC visits were related to accessibility (distance, spread of villages and topography) and to transport. In all study areas, there were households that were classed as inaccessible by all participants due to time or terrain issues. For example, in kebele A, there were some areas that were accessible only by ladders or only in the dry season, and these were difficult for the HEWs to visit:
‘Some of the places are quite mountainous, and other places can only be accessed using a ladder to descend a ravine….There are places that we can’t access in the wet season…. Those that are nearer are not problematic. We get them within 24 hours’ [ kebele A, Amhara, HEW – FGD].
Generally a flat topography and clustered settlements were seen to facilitate visits and a hilly terrain and scattered settlements were seen as a barrier. A flat terrain meant that households were generally accessible by transportation, which was facilitated by the few HEWs that had bicycles: ‘The topography of this kebele is flat like …. no ups and downs It is accessible for cars and walking’ [ kebele D, SNNPR, Fathers – FGD].
Although extreme distances and terrains were limiting factors for PNC visits, moderate difficulties were not a limiting factor. Kebele A and B had the most difficult terrain overall, but these kebele are where community members reported that early PNC visits were most common. In contrast kebele D was generally flat and accessible but PNC visits were reported by community members as not occurring at all suggesting that information and work issues can be more important barriers than moderate physical difficulties.
Information issues
Whether the HEWs’ knew a birth had occurred was a key theme in whether early PNC visits occurred. The main sub-themes were whether there was a functioning alert mechanism; and minor sub themes were place of delivery, migration in pregnancy and whether the pregnancy carried any stigma.
In the Amhara kebeles (A and B), where visits were reported as being common, mothers reported that HEWs knew they had delivered because they were involved in the delivery or in calling the ambulance. Women in these kebeles reported that they were told to inform the HEW when they went into labor, and few women had the ambulance number themselves: ‘ I directly went to their office [health post] when I felt labor pain, and it is the HEWs who called for Ambulance services’ [ kebele A, Amhara, mother-narrative]. In the difficult to access areas of these kebeles , HEWs reported that they relied on the HDAs informing them of the delivery, which was hampered by accessibility issues as HDAs went in person or sent a messenger to inform an HEW of a delivery:
‘The problem is that we do not get the feedback through the HDAs on time. They have to go a lot of distance and they sometimes send the feedback through students…….because of that we visit them after 7 days. So that is our major problem’ [ kebele A Amhara, HEW-FGD].
In the SNNP kebeles (C and D), where PNC visits were reported as occurring late or not at all, women were given the ambulance number directly, often by the HDA. The HEWs thus relied on the HDA leaders informing them that a woman had given birth, and this did not always occur. In particular, HDAs in kebele D (where PNC visits were rare) reported that they did not always tell the HEWs about a delivery ‘The problem may be with us [HDA].….for example there was a mother that had delivered; I did go and visit her but I have not come and tell the HEW about it’ [ kebele D, SNNPR, HDA – FGD]. This lack of provision of information was not linked to a lack of HDA activity, which was high in these kebele . Instead, there were some reports that the HDAs were tasked by the HEWs to conduct their visits and did not see any benefit of informing them of a delivery.
Other means of identifying delivered women were using the expected date of delivery, word of mouth and being informed by the family. Using the expected date of delivery was reported as problematic as the date were not accurate, and word of mouth was only useful where HEWs were very active in the community and made regular visits. In kebele A, in Amhara, and kebele C, in SNNPR, HEWs reported that the women themselves were meant to inform the HEW of the delivery, but mothers did not know that they should inform the HEW, and this mechanism was not functioning.
At the time of the study, few women in the study Kebles reported delivering at home, with major efforts from HEWs and HDAs to ensure all women delivered in a facility. Delivering at home was reported as shameful, with threats of sanctions and a fear that the HEW and HDA would be angry. Respondents from the mother, father and HEW/HDA FGDs all reported that HEWs would not know about women who delivered at home ‘If a woman gives birth at home, the HEWs won’t hear about it. Nobody tells them that she has given birth’ [ kebele A, Amhara, Mother – FGD]. In the few cases we found where the HEWs knew about a home delivery, the women felt that they were denied PNC visits as a sanction for not delivering at a facility or not attending ANC, and this was reiterated in a mothers in the FGDs: ‘ If she [mother] refused and decided to stay at home, they [HEW] will never visit her and she just sit at her house alone….they won’t be at her side [kebele A, Amhara, Mother- FGD]. In general attending ANC was a proactive decision by the family, while the families’ roles in receiving PNC visits was passive, with no active care seeking decisions in relation to the home visits. We found no pattern or link between attending ANC and receiving a PNC visit.
Other minor themes related to HEWs being unaware of deliveries, that were reported in the HEW/HDA FGDs, were that some first time mothers travel to their own mother in another kebele to deliver, and that unmarried ‘teenagers’ keep their pregnancies and deliveries secret due to the stigma attached to them.
Work issues
Two main sub themes related to work issues that affected whether timely PNC visits were made were: HEW availability and HEW work ethic and organization. Mothers, HEWs and HDAs reported workload and HEW availability as barriers to making timely PNC visits. Issues included being unavailable for visits as they were escorting women for delivery, multiple women delivering in different locations at the same time, staff absences, and participation in training workshops, meetings and health campaigns: ‘There are only two HEWs. They have lots of activities, which they are expected to perform. Therefore, they cannot cover all mothers in the three days after delivery’ [ kebele C, SNNPR, Mother – FGD]. Some HEWs were more organized in terms of dividing up the community and having a clear plan for visiting communities, and these plans facilitated early visits.
Differences in HEW work ethic was also identified as a reason for no or late PNC visits, and the main differences between the kebele with reported high and low levels of early PNC visits was the general level of activity of the HEWs. In kebeles with low PNC visits HEWs were reported as only coming to the community for vaccinations, being rarely at the health post, or rarely leaving the health post: ‘They [HEWs] spend the whole day here [at health post] but no one come to here…..they didn’t go inside the village’ [ kebele D, SNNPR, Father - FGD]. Temporary HEWs were reported as having particular issues with poor links with the community and with the HDA. This translated into few PNC visits being made: ‘Such staff [temporary] have a feeling that they will not be there in the kebele for long and show some sort of reluctance. They will not take their job … they believe that another person will take over from them very soon’ [ kebele A, Amhara, HEW – FGD]. In kebeles with low PNC coverage the HEWs sometimes relied on strong HDA teams to conduct activities, or were reported as only being interested in ensuring facility deliveries occurred.
In contrast, in those kebeles with reported high PNC coverage, community members described a general high level of HEW activity and a sense of connectedness between the community and the HEW:
‘ They themselves live with us. They are with us when the baby is delivered. They visit us every day. They do not do only visiting within three days. They call for Ambulance; they escort us to the health facility and assist us in delivery’ [ kebele B, Amhara, Mother - FGD].
Home visits by community health workers to provide postnatal care have the potential to reduce newborn mortality [ 5 , 6 ], but observational data suggest that these need to occur within 24 h to be effective [ 8 ]. Despite the importance of PNC visits, achieving early visits in sub Saharan African settings has proved difficult [ 6 , 9 , 10 , 11 , 25 ], and there has been little research on why early visits are not achieved. We found that visits were affected by three inter-linked issues: physical issues (accessibility and transport), information issues (whether the HEW knows about the delivery), and work issues (HEW availability and performance).
Accessibility as a barrier to CHW performance has been found in several settings [ 26 ], and there were areas in all the study sites that were inaccessible due to topography or distance constraints. We found that moderate accessibility issues were not barriers to early visits if HEWs were active, organized and well connected to the community. Care should be taken when demarcating work areas to exclude areas that are unreachable; such areas may require their own CHW for timely visits to occur. The demarcation of small and realistic catchment areas was hypothesized as a reason why Village Health Workers (VHW) in a study in Bangladesh achieved a coverage of early home visits of 87% [ 13 ].
Knowing that a delivery has occurred was essential for HEWs making a timely PNC visit, and no or late notification of a delivery has been identified as a barrier to early home visits in other settings [ 8 , 10 , 13 ]. In the study areas formal notification strategies existed through HDAs informing HEWs of a delivery, although this did not always occur despite the existence of enhanced tracking of pregnant women through L10Ks’ Community Based Data for Decision Making platform. Timely notification by HDAs was hindered by distance, and HDAs did not report using mobile phones for notification. Providing mobile phones or air time could improve notification rates, with an association between having the HEWs phone number and receiving an early PNC visit found in a previous Ethiopian study [ 14 ]. Evidence suggests that using mobile phones to increase communication is highly valued by CHWs because it reduces travel time and enhances efficiency [ 27 ], however, this may be difficult where mobile phone coverage levels are low.
In two of the study kebeles families notified the HEWs directly when they went into labour, and HEWs played an active role in calling an ambulance or assisting with the delivery. This demonstrates that when families are aware of the need to notify a HEW, and have a reason to do so, then they are able and willing to do this. Our study suggests that family led notification, especially if done in labor, may result in earlier PNC visits than HDA led notification. Family led notification is likely to be enhanced by HEWs making pregnancy visits, especially if family members are included [ 10 , 14 ], as this may improve links between the HEW and the family, and helps ensure that families know their role in notification. Facilities did not play a role in the notification process in the study kebeles . As rates of facility delivery increase facilities could play an important role in notification, particularly for newborns identified as high risk who may benefit most from early visits. The passive role that families currently play in PNC home visits may explain why we saw no pattern in visits by education levels, mirroring the lack of association between socio demographic characteristics and PNC visits found in other studies [ 10 , 11 , 14 ].
Issues with HEW availability were also reported as affecting PNC coverage, with competing tasks meaning that HEWs were not always available for timely visits. Such factors are largely out of control of the HEWs, and care needs to be taken to ensure that CHW tasks are feasible and take into account travel time. There was some evidence that HEWs and HDAs were focusing on facility deliveries to the detriment of their other activities.
The greatest difference between kebeles with high and low PNC coverage was the general activity level of the HEW. This affected notification issues and was more important than moderate physical barriers. In some kebeles , HEWs were reported as rarely coming to the community or relying on active HDAs to perform tasks, whilst in others they were reported as making frequent visits and were clearly well connected to the community. There was a particular problem with temporary workers. The role of motivation in performance is well recognized and numerous studies have reported on general motivators of CHWs. Few studies have explored variability in motivation across areas, nor the role of contextual issues, although these appear to be important [ 26 ]. We identified only one study that aims to rigorously evaluate methods of improving CHW motivation: the results of this study are yet to be reported and more research is needed [ 28 ].
We found little evidence of socio-cultural barriers from the community side for early visits, except that home delivery may be a barrier for notifying HEWs for fear for sanctions, and that some first time mothers travel to their home community for delivery. The use of sanctions for those who deliver at home may lead to vulnerable families not receiving vital services. There is much attention now being paid to the disrespect and abuse of women in facilities [ 29 , 30 ]: there is also the potential for this to occur during home visits.
During this study we took several steps to maximize data quality and data transferability such as the use of multiple study sites, methods and respondent groups; the use of methods that aimed to overcome social desirability bias; purposive sampling to saturation; regular meetings and feedback during data collection to enhance reflective thinking; triangulation of data and team analysis. Despite this there is the potential for reporting and recall bias. Data were collected from small geographic areas that were accessible to the study teams and had reasonably functioning HEW systems, the findings may not apply to other areas with significantly different contextual issues, however the study findings suggest several issues that could be explored and considered when exploring issues related to PNC coverage in other settings. Studies in other settings in Ethiopia would further enhance transferability.
If timely postnatal home visits are to occur, programs need to ensure that CHWs have realistic catchment areas that reflect their workload. Inaccessible areas may need their own CHW. Good notification systems are essential, families will notify CHWs if they have a clear reasons to do so, and more work is needed on how to ensure other potential notification systems function. Work ethic was a clear influencer on whether home visits occur, studies to date have tended to explore the motivation of CHWs as a group rather than exploring differences between CHWs, more studies on understanding motivation at an individual level are needed.
Darmstadt GL, Kinney MV, Chopra M, Cousens S, Kak L, Paul VK, et al. Who has been caring for the baby? Lancet. 2014;384(9938):174–88.
Article PubMed Google Scholar
Lawn JE, Blencowe H, Oza S, You D, Lee AC, Waiswa P, et al. Every newborn: progress, priorities, and potential beyond survival. Lancet. 2014;384(9938):189–205.
World Health Organization. WHO recommendations on postnatal care of the mother and newborn. Geneva: World Health Organization; 2013. Report No.: 978 92 4 150664 9
Google Scholar
World Health Organization and UNICEF. Home visits for the newborn child: a strategy to improve survival. Geneva: World Health Organization and UNICEF; 2009.
Gogia S, Sachdev HS. Home visits by community health workers to prevent neonatal deaths in developing countries: a systematic review. Bull World Health Organ. 2010;88(9):658–666B.
Article PubMed PubMed Central Google Scholar
Kirkwood BR, Manu A, ten Asbroek AH, Soremekun S, Weobong B, Gyan T, et al. Effect of the Newhints home-visits intervention on neonatal mortality rate and care practices in Ghana: a cluster randomised controlled trial. Lancet. 2013;381(9884):2184–92.
McPherson R, Hodgins S. Postnatal home visitation: lessons from country programs operating at scale. J Glob Health. 2018;8(1):010422.
Baqui AH, Ahmed S, El Arifeen S, Darmstadt GL, Rosecrans AM, Mannan I, et al. Effect of timing of first postnatal care home visit on neonatal mortality in Bangladesh: a observational cohort study. BMJ. 2009;339:b2826.
Waiswa P, Pariyo G, Kallander K, Akuze J, Namazzi G, Ekirapa-Kiracho E, et al. Effect of the Uganda newborn study on care-seeking and care practices: a cluster-randomised controlled trial. Glob Health Action. 2015;8:24584.
Sitrin D, Guenther T, Murray J, Pilgrim N, Rubayet S, Ligowe R, et al. Reaching mothers and babies with early postnatal home visits: the implementation realities of achieving high coverage in large-scale programs. PLoS One. 2013;8(7):e68930.
Article PubMed PubMed Central CAS Google Scholar
Callaghan-Koru JA, Nonyane BA, Guenther T, Sitrin D, Ligowe R, Chimbalanga E, et al. Contribution of community-based newborn health promotion to reducing inequities in healthy newborn care practices and knowledge: evidence of improvement from a three-district pilot program in Malawi. BMC Public Health. 2013;13:1052.
Hanson C, Manzi F, Mkumbo E, Shirima K, Penfold S, Hill Z, et al. Effectiveness of a home-based counselling strategy on neonatal care and survival: a cluster-randomised trial in six districts of rural southern Tanzania. PLoS Med. 2015;12(9):e1001881.
Shah R, Munos MK, Winch PJ, Mullany LC, Mannan I, Rahman SM, et al. Community-based health workers achieve high coverage in neonatal intervention trials: a case study from Sylhet. Bangladesh J Health Popul Nutr. 2010;28(6):610–8.
PubMed Google Scholar
Tesfaye S, Barry D, Gobezayehu AG, Frew AH, Stover KE, Tessema H, et al. Improving coverage of postnatal care in rural Ethiopia using a community-based, collaborative quality improvement approach. J Midwifery Womens Health. 2014;59(Suppl 1):S55–64.
The Last Ten Kilometers. Community based newborn care. In: Kilometers TLT, editor. News from the last ten kilometers. Addis Ababa: The Last Ten Kilometers; 2014.
Banteyerga H. Ethiopia's health extension program: improving health through community involvement. MEDICC Rev. 2011;13(3):46–9.
Koblinsky M, Tain F, Gaym A, Karim A, Carnell M, Tesfaye S. Responding to the maternal health care challenge: The Ethiopian Health Extension Program. Ethiop J Health Dev. 2010;24(Special Issue 1):105–9.
Legesse H, Degefie T, Hiluf M, Sime K, Tesfaye C, Abebe H, et al. National scale-up of integrated community case management in rural Ethiopia: implementation and early lessons learned. Ethiop Med J. 2014;52(Suppl 3):15–26.
Karim AM, Admassu K, Schellenberg J, Alemu H, Getachew N, Ameha A, et al. Effect of ethiopia’s health extension program on maternal and newborn health care practices in 101 rural districts: a dose-response study. PLoS One. 2013;8(6):e65160.
The Last Ten Kilometers. Improving maternal and newborn health care practices. The role of community based data for decision making in: kilometers TLT, editor. News from the last ten kilometers. The Last Ten Kilometers: Addis Ababa; 2013.
Betemariam B, Karim A, Getachew N. Evidence based scaling-up an innovative community-based maternal and newborn health strategy in Ethiopia. In: 141st American Public Health Assocition annual meeting. Boston, USA; 2013.
Darmstadt GL, Marchant T, Claeson M, Brown W, Morris S, Donnay F, et al. A strategy for reducing maternal and newborn deaths by 2015 and beyond. BMC Pregnancy Childbirth. 2013;13:216.
Karim A. Effectiveness evaluation of a large-scale community-based program: Lessons from Ethiopia. Annals of Global Health. 2015;81(1):192.
Article Google Scholar
Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland: CSA and ICF. p. 2016.
Penfold S, Manzi F, Mkumbo E, Temu S, Jaribu J, Shamba DD, et al. Effect of home-based counselling on newborn care practices in southern Tanzania one year after implementation: a cluster-randomised controlled trial. BMC Pediatr. 2014;14:187.
Kok MC, Kane SS, Tulloch O, Ormel H, Theobald S, Dieleman M, et al. How does context influence performance of community health workers in low- and middle-income countries? Evidence from the Literature Health Res Policy Syst. 2015;13:13.
Thondoo M, Strachan DL, Nakirunda M, Ndima S, Muiambo A, Kallander K, et al. Potential roles of Mhealth for community health workers: formative research with end users in Uganda and Mozambique. JMIR Mhealth Uhealth. 2015;3(3):e76.
Kallander K, Strachan D, Soremekun S, Hill Z, Lingam R, Tibenderana J, et al. Evaluating the effect of innovative motivation and supervision approaches on community health worker performance and retention in Uganda and Mozambique: study protocol for a randomised controlled trial. Trials. 2015;16:157.
Bohren MA, Vogel JP, Hunter EC, Lutsiv O, Makh SK, Souza JP, et al. The Mistreatment of Women during Childbirth in Health Facilities Globally: A Mixed-Methods Systematic Review. PLoS Med 2015;12(6):e1001847; discussion e1001847.
Freedman LP, Kruk ME. Disrespect and abuse of women in childbirth: challenging the global quality and accountability agendas. Lancet. 2014;384(9948):e42–4.
Download references
The study was funded by the Bill and Melinda Gates foundation as part of the IDEAS study.
Availability of data and materials
The datasets generated and analysed during the current study are not publicly available due to issues of confidentiality and privacy. Although respondents’ names are not included in transcripts they do include place names and any names mentioned by respondents, for example, names of Health Extension Workers.
Author information
Authors and affiliations.
Consultancy for Social Development, PO Box 70196, Addis Ababa, Ethiopia
Yared Amare
London School of Hygiene and Tropical Medicine, Keppel Street, London, WC1E 7HT, UK
Pauline Scheelbeek, Joanna Schellenberg & Della Berhanu
University College London, 30 Guilford Street, London, WC1N 1EH, UK
You can also search for this author in PubMed Google Scholar
Contributions
ZH and JS conceived the study; ZH, YA and PA designed the study and the data collection tools. YA, PA and DB were responsible for the acquisition of data. ZH, PS and YA were responsible for analysing and interpreting the data. ZH and YA prepared the first draft of the paper and all authors commented on the paper and approved the final version.
Corresponding author
Correspondence to Zelee Hill .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval was obtained from the Institutional Review Boards of the London School of Hygiene and Tropical Medicine and the Ministry of Science and Technology in Ethiopia. Written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Amare, Y., Scheelbeek, P., Schellenberg, J. et al. Early postnatal home visits: a qualitative study of barriers and facilitators to achieving high coverage. BMC Public Health 18 , 1074 (2018). https://doi.org/10.1186/s12889-018-5922-7
Download citation
Received : 29 August 2017
Accepted : 01 August 2018
Published : 29 August 2018
DOI : https://doi.org/10.1186/s12889-018-5922-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Community health worker
- Qualitative
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Jump to navigation
- Bahasa Malaysia

Home visits in the early period after the birth of a baby
What is the issue?
Health problems for mothers and babies commonly occur or become apparent in the weeks following the birth. For the mothers these include postpartum haemorrhage (substitute excessive blood loss), fever and infection, abdominal and back pain, abnormal discharge (heavy or smelly vaginal discharge), thromboembolism (a blood clot), and urinary tract complications (being unable to control the urge to pee), as well as psychological and mental health problems such as postnatal depression. Mothers may also need support to establish breastfeeding. Babies are at risk of death related to infections (babies may be badly affected by infections), asphyxia (difficulties in breathing, caused by lack of oxygen), and preterm birth (being born prematurely).
Why is this important?
Home visits by health professionals or lay supporters in the early postpartum period may prevent health problems from becoming long-term, with effects on women, their babies, and their families. This review looked at different home-visiting schedules in the weeks following the birth.
What evidence did we find?
We included 16 randomised trials with data for 12,080 women. Some trials focused on physical checks of the mother and newborn, while others provided support for breastfeeding, and one included the provision of practical support with housework and childcare. They were carried out in both high-resource countries and low-resource settings where women receiving usual care may not have received additional postnatal care after early hospital discharge.
The trials focused on three broad types of comparisons: schedules involving more versus fewer postnatal home visits (five studies), schedules involving different models of care (three studies), and home versus facility postnatal check-ups (eight studies). In all but four of the included studies, postnatal care at home was delivered by healthcare professionals. For most of our outcomes, only one or two studies provided data. Overall, our results were inconsistent.
The evidence was very uncertain about whether home visits reduced newborn deaths or serious health problems with the mother. Women's physical and psychological health were not improved with more intensive schedules of home visits although more individualised care improved women's mental health in one study and maternal satisfaction was slightly better in two studies. Overall, babies may be less likely to have additional medical care if their mothers received more postnatal home visits. More home visits may have encouraged more women to exclusively breastfeed their babies and women to be more satisfied with their postnatal care. The different outcomes reported in different studies, how the outcomes were measured, and the considerable variation in the interventions and control conditions across studies were limitations of this review. The certainty of the evidence was generally found to be low or very low according to the GRADE criteria.
What does this mean?
Increasing the number of postnatal home visits may promote infant health and exclusive breastfeeding and more individualised care may improve outcomes for women. More research is needed before any particular schedule of postnatal care can be recommended.
The evidence is very uncertain about the effect of home visits on maternal and neonatal mortality. Individualised care as part of a package of home visits probably improves depression scores at four months and increasing the frequency of home visits may improve exclusive breastfeeding rates and infant healthcare utilisation. Maternal satisfaction may also be better with home visits compared to hospital check-ups. Overall, the certainty of evidence was found to be low and findings were not consistent among studies and comparisons. Further well designed RCTs evaluating this complex intervention will be required to formulate the optimal package.
Maternal complications, including psychological/mental health problems and neonatal morbidity, have commonly been observed in the postpartum period. Home visits by health professionals or lay supporters in the weeks following birth may prevent health problems from becoming chronic, with long-term effects. This is an update of a review last published in 2017.
The primary objective of this review is to assess the effects of different home-visiting schedules on maternal and newborn mortality during the early postpartum period. The review focuses on the frequency of home visits (how many home visits in total), the timing (when visits started, e.g. within 48 hours of the birth), duration (when visits ended), intensity (how many visits per week), and different types of home-visiting interventions.
For this update, we searched the Cochrane Pregnancy and Childbirth Group's Trials Register, ClinicalTrials.gov, the WHO International Clinical Trials Registry Platform (ICTRP) (19 May 2021), and checked reference lists of retrieved studies.
Randomised controlled trials (RCTs) (including cluster- , quasi-RCTs and studies available only as abstracts) comparing different home-visiting interventions that enrolled participants in the early postpartum period (up to 42 days after birth) were eligible for inclusion. We excluded studies in which women were enrolled and received an intervention during the antenatal period (even if the intervention continued into the postnatal period), and studies recruiting only women from specific high-risk groups (e.g. women with alcohol or drug problems).
Two review authors independently assessed trials for inclusion and risk of bias, extracted data and checked them for accuracy. We used the GRADE approach to assess the certainty of the evidence.
We included 16 randomised trials with data for 12,080 women. The trials were carried out in countries across the world, in both high- and low-resource settings. In low-resource settings, women receiving usual care may have received no additional postnatal care after early hospital discharge.
The interventions and controls varied considerably across studies. Trials focused on three broad types of comparisons, as detailed below. In all but four of the included studies, postnatal care at home was delivered by healthcare professionals. The aim of all interventions was broadly to assess the well-being of mothers and babies, and to provide education and support. However, some interventions had more specific aims, such as to encourage breastfeeding, or to provide practical support.
For most of our outcomes, only one or two studies provided data, and results were inconsistent overall. All studies had several domains with high or unclear risk of bias.
More versus fewer home visits (five studies, 2102 women)
The evidence is very uncertain about whether home visits have any effect on maternal and neonatal mortality (very low-certainty evidence). Mean postnatal depression scores as measured with the Edinburgh Postnatal Depression Scale (EPDS) may be slightly higher (worse) with more home visits, though the difference in scores was not clinically meaningful (mean difference (MD) 1.02, 95% confidence interval (CI) 0.25 to 1.79; two studies, 767 women; low-certainty evidence). Two separate analyses indicated conflicting results for maternal satisfaction (both low-certainty evidence); one indicated that there may be benefit with fewer visits, though the 95% CI just crossed the line of no effect (risk ratio (RR) 0.96, 95% CI 0.90 to 1.02; two studies, 862 women). However, in another study, the additional support provided by health visitors was associated with increased mean satisfaction scores (MD 14.70, 95% CI 8.43 to 20.97; one study, 280 women; low-certainty evidence). Infant healthcare utilisation may be decreased with more home visits (RR 0.48, 95% CI 0.36 to 0.64; four studies, 1365 infants) and exclusive breastfeeding at six weeks may be increased (RR 1.17, 95% CI 1.01 to 1.36; three studies, 960 women; low-certainty evidence). Serious neonatal morbidity up to six months was not reported in any trial.
Different models of postnatal care (three studies, 4394 women)
In a cluster-RCT comparing usual care with individualised care by midwives, extended up to three months after the birth, there may be little or no difference in neonatal mortality (RR 0.97, 95% CI 0.85 to 1.12; one study, 696 infants). The proportion of women with EPDS scores ≥ 13 at four months is probably reduced with individualised care (RR 0.68, 95% CI 0.53 to 0.86; one study, 1295 women). One study suggests there may be little to no difference between home visits and telephone screening in neonatal morbidity up to 28 days (RR 0.97, 95% CI 0.85 to 1.12; one study, 696 women). In a different study, there was no difference between breastfeeding promotion and routine visits in exclusive breastfeeding rates at six months (RR 1.47, 95% CI 0.81 to 2.69; one study, 656 women).
Home versus facility-based postnatal care (eight studies, 5179 women)
The evidence suggests there may be little to no difference in postnatal depression rates at 42 days postpartum and also as measured on an EPDS scale at 60 days. Maternal satisfaction with postnatal care may be better with home visits (RR 1.36, 95% CI 1.14 to 1.62; three studies, 2368 women). There may be little to no difference in infant emergency health care visits or infant hospital readmissions (RR 1.15, 95% CI 0.95 to 1.38; three studies, 3257 women) or in exclusive breastfeeding at two weeks (RR 1.05, 95% CI 0.93 to 1.18; 1 study, 513 women).
Women's experiences of home visits by midwives in the early postnatal period
Affiliations.
- 1 St. Olavs University Hospital, Department of Women's Health, Olav Kyrres gt. 17, 7006 Trondheim, Norway. Electronic address: [email protected].
- 2 Department of Nursing Science and Center for Health Promotion Research, Norwegian University of Science and Technology, Trondheim, Norway.
- 3 Department of Nursing Science, Midwifery Education, Faculty of Health and Social Science, Norwegian University of Science and Technology, Trondheim, Norway.
- PMID: 27321721
- DOI: 10.1016/j.midw.2016.05.003
Objective: The aim of the present study is to gain a deeper understanding of women's experiences of midwifery care in connection with home visits during the early postnatal period.
Research design/setting: A qualitative approach was chosen for data collection, and the data presented are based on six focus group interviews (n: 24). The women were both primiparous and multiparous, aged 22-37, and lived with their partners. All participants had given birth at a maternity unit responsible for about 4000 births a year. The transcribed interviews were analysed through systematic text condensation.
Findings: The findings are reflected in three main themes: 'The importance of relational continuity', 'The importance of a postpartum talk' and 'Vulnerability in the early postnatal period'. When the woman had a personal relationship with the midwife responsible for the home visit she experienced predictability, availability and confidence. The women wanted recognition and time to talk about their birth experience. They also felt vulnerable in their maternal role in the early postnatal period and the start of the breast-feeding process.
Conclusions: It is important to promote relational continuity models of midwifery care to address the emotional aspects of the postnatal period. Women generally wish to discuss their birth experience, preferably with the midwife who was present during the birth. Due to the short duration of postnatal care in hospitals, the visit from the midwife a few days after childbirth becomes all the more important.
Keywords: Continuity of care; Home visit; Postnatal care; Postpartum talk.
Copyright © 2016 Elsevier Ltd. All rights reserved.
- Focus Groups
- House Calls*
- Midwifery / standards*
- Mothers / psychology*
- Patient Satisfaction*
- Postnatal Care / standards*
- Qualitative Research
- Open access
- Published: 09 August 2022
Whole genome non-invasive prenatal testing in prenatal screening algorithm: clinical experience from 12,700 pregnancies
- Elena E. Baranova 1 , 2 ,
- Olesya V. Sagaydak 1 ,
- Alexandra M. Galaktionova 1 ,
- Ekaterina S. Kuznetsova 1 ,
- Madina T. Kaplanova 1 ,
- Maria V. Makarova 1 ,
- Maxim S. Belenikin 1 ,
- Anton S. Olenev 3 &
- Ekaterina N. Songolova 4
BMC Pregnancy and Childbirth volume 22 , Article number: 633 ( 2022 ) Cite this article
3375 Accesses
6 Citations
1 Altmetric
Metrics details
A fast adoption of a non–invasive prenatal testing (NIPT) in clinical practice is a global tendency last years. Firstly, in Russia according a new regulation it was possible to perform a widescale testing of pregnant women in chromosomal abnormality risk. The aim of the study—to assess efficiency of using NIPT as a second-line first trimester screening test in Moscow.
Based on the first trimester combined prenatal screening results 12,700 pregnant women were classified as a high-risk (cut-off ≥ 1:100) and an intermediate-risk (cut-off 1:101 – 1:2500) groups followed by whole genome NIPT. Women from high-risk group and those who had positive NIPT results from intermediate-risk group were considered for invasive prenatal diagnostic.
258 (2.0%) samples with positive NIPT results were detected including 126 cases of trisomy 21 (T21), 40 cases of T18, 12 cases of T13, 41 cases of sex chromosome aneuploidies (SCAs) and 39 cases of rare autosomal aneuploidies (RAAs) and significant copy number variations (CNVs). Statistically significant associations ( p < 0.05) were revealed for fetal fraction (FF) and both for some patient’s (body mass index and weight) and fetus’s (sex and high risk of aneuploidies) characteristics. NIPT showed as a high sensitivity as specificity for common trisomies and SCAs with an overall false positive rate 0.3%.
Conclusions
NIPT demonstrated high sensitivity and specificity. As a second-line screening test it has shown a high efficiency in detecting fetus chromosomal anomalies as well as it could potentially lower the number of invasive procedures in pregnant women.
Peer Review reports
Infant mortality is a major medical and social problem, reflecting the quality of the public health system and the future of the country. The main unfavorable factors promoting to high infant mortality are low socioeconomic status of the country, low quality and availability of medical care, severe maternal, fetal or placental conditions, advanced maternity age [ 1 ]. The evolution of reproductive technologies over the last few decades has contributed to an advanced maternal age, which is associated with an increased fetal chromosomal anomaly rates and congenital diseases [ 2 ]. Among other reasons congenital diseases lead to as much as 20% of all infant deaths [ 3 ].
To evaluate and prevent fetus congenital disease, including chromosomal abnormalities, traditional first trimester screening is performed. It includes blood screening combined with an ultrasound examination in the first trimester of pregnancy. Fetus congenital disease can be well diagnosed by ultrasound examinations only from the 11th gestational week. Biochemical blood pregnancy marker risk assessment of chromosomal fetus anomalies is based on the human chorionic gonadotrophin (hCG), the free-β subunit of hCG, and the pregnancy-associated plasma protein (PAPP-A) blood tests. Though widely used biochemical assessment combined with ultrasound is still an indirect evaluation of chromosomal anomalies and results in a false positive rate of up to 5%, leading to increases number of invasive prenatal diagnostic (IPD) procedures [ 4 , 5 ].
To address these limitations, a new screening method, known as a non-invasive prenatal testing (NIPT), was introduced [ 6 ]. The method is based on the massive parallel sequencing of cell-free DNA (cfDNA) fragments derived from a maternal plasma [ 7 ]. The sensitivity of NIPT for most common trisomies including trisomies 21 (T21), 18 (T18), and 13 (T13) is high and reaches up to 99, 96 and 91%, respectively [ 8 ] with a false-positive results rate as low as 0.08% compared to traditional prenatal screening [ 9 ].
There are several types of NIPT – tests targeted on chromosomes of interest (usually 21, 18 and 13) and a whole genome NIPT, that allows to assess all chromosomes and its anomalies. Whole genome NIPT can be used to detect sex chromosome abnormalities and other anomalies, including rare autosomal aneuploidies (RAAs) and significant copy number variations (CNVs), though accuracy of the test for these anomalies is a bit lower due to the fact that RAAs are usually present as a placental mosaicism or a true fetal mosaicism. That could be associated with adverse pregnancy outcomes such as early miscarriage, intrauterine growth restriction, and in-utero fetal demise [ 10 ]. In nonmosaic form these chromosomal anomalies usually lead to a fetus death [ 11 ].
The American College of Obstetricians and Gynecologists (ACOG) originally suggested the use of NIPT for women previously determined to be in a high-risk group by traditional screening [ 12 ]. But it has been shown that the sensitivity and specificity of the test among all pregnant women are similar to those in the high-risk population [ 13 ]. Therefore, current international guidelines recommend the use of NIPT for prenatal screening during pregnancy for all women, regardless of the predetermined risk of fetal anomalies [ 5 , 13 ].
Until recently, in Russia NIPT was primarily a commercially available test used to supplement other screening approaches. On March 13, 2020, NIPT was included as a standard method for prenatal screening as part of a pilot project in Moscow [ 14 ]. The large-scale project was run by the Moscow City Healthcare Department with the participation of 23 prenatal care hospitals and one genetic laboratory. Since the beginning, work on national standards and clinical guidelines for NIPT has been ongoing. The aim of the study was to assess the efficiency of NIPT as a second-line first trimester screening test in Moscow. Preliminary results were published before [ 15 ]. The project is finished now, and its first results are presented.
Recruitment criteria
Pregnant women at high-risk of fetus chromosomal anomalies (cut-off ≥ 1:100) after the traditional prenatal screening were referred for genetic counseling, a IPD and a blood sampling for NIPT according the local regulation [ 14 ]. Blood test for NIPT was performed in the same day of the IPD (Fig. 1 ).
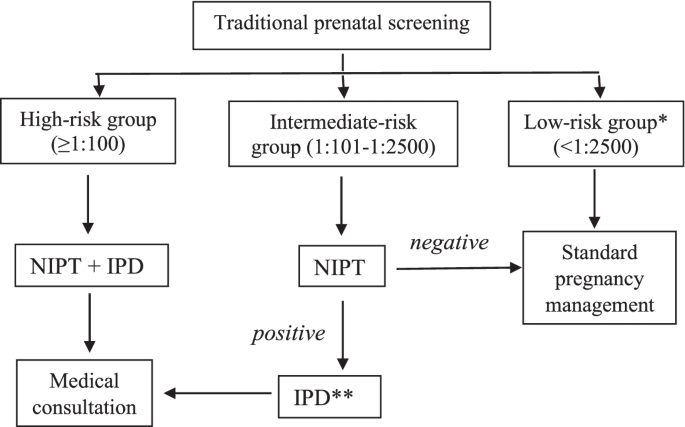
Recruitment criteria for samples that were able to undergo NIPT. *Low-risk group samples were not included into the study. **IPD is obligatory for a high-risk group of pregnant women and is optional for an intermediate-risk group. Abbreviations: NIPT, non–invasive prenatal testing; IPD, invasive prenatal diagnostic
Pregnant women at group of risk 1:101–1:2500 were as well offered to perform NIPT. When receiving a positive (high-risk) NIPT result, pregnant women were considered to undergo a genetic consulting and IPD.
Sample’s collection and blood preparation for sequencing
To perform NIPT 10.0 ml pregnant women peripheral blood samples were collected in STRECK (Cell-Free DNA BCT CE) tubes before IPD. Plasma was separated within 8 h following a double-centrifugation protocol. Tubes were stored temporarily (up to one week) at -20 °C before further processing or stored at – 80 °C for a long-term storage.
The cfDNA isolation, sample library preparation and DNA sequencing were performed according to manufacturer’s protocols. Each sample was sequenced using a BGISEQ-500 (China) platform. Sequencing reads were trimmed and aligned to a universal unique read set incised from the human reference genome (hg19, NCBI build 37). Combined GC-correction and z-score testing methods were used to identify fetal autosomal aneuploidies. The quality control parameters were as follows: the library concentration was higher than 4 ng/μL; the unique mapped reads number was higher than 6 × 106; the GC content was 38%–42%; and the fetal DNA fraction was higher than 3.5%. The original BGI proprietary software (HALOS NIFTY-2.3.2.1011) was used for a bioinformatic data processing.
Fetal fraction calculation
The fetus fetal fraction (FF) was calculated using the FF-QuantSC method, that employs neural network model and utilizes differential genomic patterns between fetal and maternal genomes [ 16 ].
NIPT results
The final report included a risk assessment for T21, T18, T13 and SCAs. Whole genome results for RAAs and clinically significant CNVs were included in the report optionally for women who consented to receive that information.
Invasive prenatal diagnostics
Pregnant women from the high-risk group as well as women with a fetal chromosomal abnormalities risk revealed by NIPT («positive» NIPT results) from the intermediate-risk group were advised to undergo IPD by amniocentesis or chorionic villus sampling (CVS) with a subsequent karyotyping and/or array-based comparative genomic hybridization (aCGH). IPD was also recommended for pregnant women with abnormalities during their second trimester ultrasound examination. CVS or amniocentesis were performed under sterile conditions and an ultrasound guidance in specialized medical hospitals in Moscow.
Karyotype analysis
For karyotype analysis, 10–20 ml of amniotic fluid was obtained by amniocentesis. The amniotic fluid cells with 4.5 ml medium (RPMI-1640, Paneco, Russia) were cultured in a 37 °C incubator with 5% carbon dioxide. The cells were harvested at 10–12 days. After colchicine treatment for 2 h, the cells were digested using 1:250 trypsin, and incubated with 0.075 M KCl for 30 min. The prefixation, fixation, dropping, baking, and G-band staining were performed next. A total of 100 dividing phases were counted using an all-chromosome image analysis system based on the “An International System for Human Cytogenetic Nomenclature, ISCN2016”.
Agilent SurePrint G3 human aCGH array 8*60 K chips were used for aCGH. DNA from amniotic fluid or chorionic villus after IPD was extracted (New iGENatal Kit, igen biotech, Spain). Agilent CytoGenomics (version 5.0) was used for data analyses. CNVs were classified through Online Mendelian Inheritance in Man (OMIM), Database of Genome Variants (DGV) and Decipher databases. Pathogenic, likely pathogenic, variant of uncertain significance (VUS), likely benign, and benign categories were used for CNVs’ allocation. For VUS aCGH was further performed for parents to verify whether the CNVs were inherited from the parents with a normal phenotype. Inherited CNVs from the parents with a normal phenotype were considered as benign.
Statistical analysis was performed as described earlier [ 15 ]. The statistical software package Wizard 2 Version 2.0.4 (250) was used for data analyses.
All in all, 12,700 pregnant women blood samples were analyzed during the Apr.1, 2020 till Apr. 5, 2021 period (Fig. 2 ). The average pregnant women age was 34.4 ± 4.3 years. 53.2% (6756/12700) of pregnant women were in the advanced maternal age (35 and older). The average gestation period was 14 weeks and 1 day ± 1 week and 3 days. 36.7% (4655/12700) of pregnant women had a body mass index (BMI) above 25 kg/m 2 . The majority of pregnancies were spontaneous (96.1%, 12,198/12700) and singleton (98.5%, 12,512/12700) (Table 1 ).

Flowchart of non-invasive prenatal test (NIPT) results and invasive prenatal diagnostics outcomes of pregnant women undergoing screening for aneuploidies between 1 April 2020 and 5 April 2021. Abbreviations: T, trisomy; SCA, sex chromosomal aneuploidy; RAA, rare autosomal aneuploidy; CNV, copy number variation; aCGH, array comparative genomic hybridization
Blood samples of 502 (3.9%) women in the high-risk group and of 12,198 (96.1%) women in the intermediate-risk group were evaluated. Out of 12,700 samples in 346 (2.7%) cases blood retesting was recommended due to a low FF (below 3.5%).
NIPT results in high-risk pregnant women
Out of 502 women in the high-risk group (≥ 1:100) 148 (29.5%) were considered positive (high risk) by NIPT, and 347 women were considered negative (low risk) (Fig. 2 ). IPD results data is available only for 144 cases: 140 case was confirmed by IPD, 4 cases were not confirmed.
The following anomalies were confirmed by IPD in 140 cases: T21 (Down syndrome) in 93 cases, T18 (Edward syndrome) in 35 cases, T13 (Patau syndrome) in 4 cases, X-monosomy (Turner syndrome) in 3 cases, X-chromosome disomy with Y-chromosome monosomy (Klinefelter syndrome) in 1 case and Y-chromosome disomy (XYY syndrome) in 1 case, RAAs in 2 cases (T7 and T22), CNVs in 1 case (del7p14.1p11.2). In 2 cases different chromosomal anomaly was shown by IPD: in 1 case balanced translocation between chromosomes 14 and 22 was shown by IPD, when NIPT showed high risk for T22; in 1 case X triploidy by IPD was shown, when NIPT was positive for T18 and monosomy X.
NIPT results were not confirmed in 1 case for T18, in 1 case for T13 and 2 cases for trisomy of chromosome 16 (Fig. 2 ).
NIPT results in intermediate-risk pregnant women
Of the 12,198 cases in the intermediate-risk group (1:101 – 1:2500), 110 (0,9%) cases were considered NIPT positive. IPD results data is available for the group: 58 cases were confirmed by IPD, 52 cases were not confirmed.
The following anomalies were confirmed by IPD in 58 cases: T21 in 31 cases, T18 – in 3 case, T13 in 3 cases, X-chromosome monosomy (Turner syndrome) in 5 cases, X-chromosome disomy with Y-chromosome monosomy (Klinefelter syndrome) in 6 cases, X-chromosome monosomy with Y-chromosome disomy (XYY syndrome) in 2 cases, trisomy of X-chromosome in 1 case, RAA in 1 case (T8), CNVs in 6 cases.
NIPT results were not confirmed in 2 cases of T21, 4 cases of T13, 21 cases of SCAs and 19 cases of RAAs and 6 CNVs.
In the risk group, IPD was performed in 24 patients with negative NIPT due to their abnormal 2nd trimester ultrasound results: congenital malformations or ultrasound markers of fetus chromosomal pathology. According to the IPD results: 23 received a normal karyotype in the fetus, in 1 case a pathology was detected—46,XX,del (18)(p11.2)—a deletion of the short arm of chromosome 18 (false-negative result) (Fig. 2 ).
Secondary findings
Thirty-nine cases were considered positive for RAAs or CNVs by NIPT (7 cases in the high-risk group and 32 cases in the intermediate-risk group). The most common were T7 ( n = 6), T16 ( n = 4), T8 ( n = 3) and T22 ( n = 3). Thirty-seven women (5 cases in the high-risk group and 32 cases in the intermediate-risk group) proceeded with IPD, and chromosomal pathology was confirmed only in 10 cases (Fig. 2 ). These chromosomal anomalies are rare and are not detectable by widely used NIPT techniques.
NIPT performance
All in all, the following chromosomal abnormalities have been identified and confirmed: T21 in 124 cases; T18 in 38 cases; T13 in 7 cases; SCAs in 19 cases; RAAs or CNVs – in 10 cases. Comparison of NIPT and IPD results in detection of chromosomal abnormalities is presented in Table 2 . Totally, the rate of false-positive results was 0.3%.
IPD results and/or pregnancy outcomes are available for 9941 women, of whom 9737 had no fetal chromosomal abnormalities and 199 had prenatal and/or postnatal chromosomal abnormalities confirmation. On the basis of the NIPT results and the outcome data available, we calculated the performance of the test in detection of chromosomal anomalies. For T21, T18 and 13, SCAs, RAAs and CNVs the sensitivity was 100%, 100%, 100%, and 92.86%; specificity was 99.50%, 99.15%, 97.47% and 96.88%; positive predictive value (PPV) was 98.26%, 91.67%, 57.14% and 44.83%; negative predictive value (NPV) was 100%, 100%, 100% and 99.80%, respectively (Table 3 ).
To calculate NIPT performance parameters the “true positive” results were defined as positive NIPT results that were confirmed by IPD. The “false positive” results were defined as positive NIPT results for chromosomal anomaly that were shown to be negative by follow‐up IPD. The “true negative” results were defined as negative NIPT results confirmed by karyotyping or aCGH results. The “false negative” results were defined as negative NIPT results with an aneuploidy karyotype confirmed by IPD.
Association of results with fetal fraction
It was shown that FF differs between gestational weeks, p < 0.001 (Fig. 3 ).
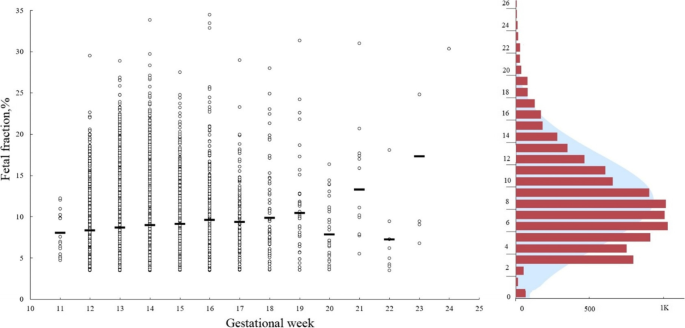
A density distribution of fetal fraction and its relationship with gestational weeks of pregnant women. The average fetal fraction in each week is shown by a black line
Also, it was revealed that samples with low FF (< 3.5%) were observed in women with significantly higher weight and BMI in comparison with women with normal FF: 77.5 kg [62.3;91.1] for low FF and 64.0 kg [58.2;74.4] for normal, ( p < 0.001), BMI – 28.2 kg/m 2 [23.1;33.6] for low FF and 23.4 kg/m 2 [21.0;26.8] for normal, p < 0.001 (Fig. 4 a).
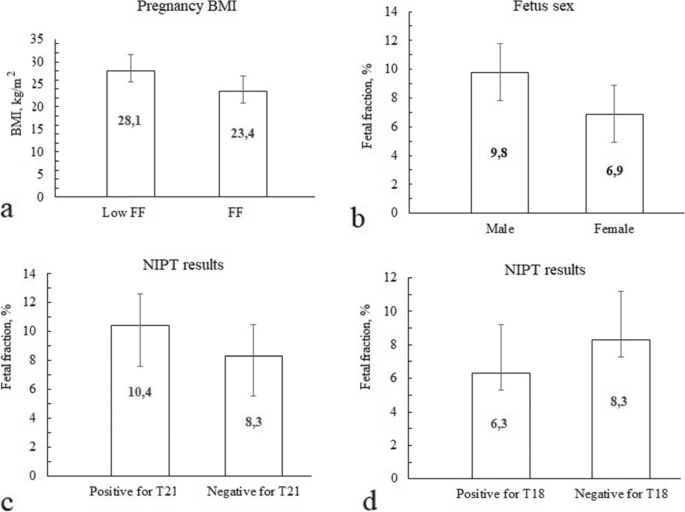
The average level of fetal fraction for patients depending on the BMI ( a ), fetus sex ( b ) and NIPT results: risk of T21 ( c ) and T18 ( d ). Abbreviations: NIPT, non-invasive prenatal testing; T, trisomy; BMI, body mass index.
It was also shown, that the FF is significantly higher in women with male fetus, than female: 9.9% [7.4;13.2] and 6.8% [4.9;8.9], p < 0.001 (Fig. 4 b).
It was also shown, that T21 positive NIPT results were associated with a higher FF, than samples with negative results: 10.4% [7.1;14.4] and 8.3% [6.0;11.2], p < 0.001 (Fig. 4 c). The cut point for significant difference was 9.0% FF, p < 0.001. For T18 it was shown vice versa – T18 positive NIPT results were associated with a lower FF, than samples with negative results: 7.1% [4.4;10.9] and 8.3% [6.0;11.3], p = 0.048 (Fig. 4 d). The same tendency was not revealed for T13 probably due to a small number of samples.
NIPT results according to age and mode of conception
We found a significant difference between the age of women with positive and negative NIPT results for T21: 37 yr [33;40] for high T21 risk and 35 yr [31;38] for low risk, p = 0.017. Summarizing all the positive NIPT results for all anomalies showed, that these were significantly higher in older women. Mean age of women with a high risk was 37 yr [32;40], and for women with a low risk – 35 yr [31;38], p < 0.001.
There was no significant difference in frequency of positive NIPT results in spontaneous and in vitro fertilization pregnancies, p = 0.212.
NIPT was first released in Hong Kong in August 2011 and soon after was introduced commercially in the US in October 2011 [ 17 , 18 , 19 ]. Afterward, in many countries, multiple companies and their distribution partners offered several NIPT tests to pregnant women, either in a commercial or in a state-regulated setting [ 20 ].
The current standard of care for prenatal screening in many high-income countries involves a ultrasound examination combined with biomarker serum screens in the first and/or second trimesters of pregnancy. Despite the fact that in some countries NIPT is performed as a commercial test, or with partial government funding, there is a certain international strategy for introducing NIPT into the structure of prenatal diagnostics. NIPT could be implemented into prenatal testing pipeline in different ways. The most commonly used are as a replacement for serum screening – a first-line test, and as an intermediate step between screening and invasive procedures – a second-line test. The most commonly used implementation model is a combined prenatal screening with the formation of high, intermediate and low risk groups, followed by NIPT in the high and/or intermediate risk group [ 21 ]. NIPT as a first-line test is performed to all pregnant women before an expert ultrasound in the first trimester of pregnancy and successfully used in Belgium and the Netherlands [ 22 , 23 , 24 , 25 ]. NIPT as a second-line test for pregnant women in high or intermediate risk groups determined by the results of combined prenatal screening implemented in some European countries (Germany, Great Britain, France, Italy etc.) [ 26 ]. The main advantage of introducing NIPT precisely as a second-line test is economic feasibility.
In Russia the effectiveness of NIPT integration in traditional prenatal screening as a second-line test was shown in the current study. NIPT showed clear accuracy and revealed 37 additional positive (high risk) cases in the intermediate group of pregnant women at risk, compared to traditional prenatal screening. These results included clinically significant CNVs, that were detected only because NIPT was based whole genome sequencing. CNVs are of particular importance because 20 to 30% of congenital diseases are associated with microdeletions and microduplications, which are not detected by traditional prenatal screening and standard cytogenetic studies [ 27 ].
The main NIPT advantages are its high sensitivity and specificity for common aneuploidies – T21, T18, T13. Multiple validation studies have reported NIPT high sensitivity (98.6%-100%) and specificity (99.7%-100%) for T21 in different populations [ 28 , 29 ]. Our results revealed high sensitivity and specificity both for the common trisomies, SCAs and RAAs/CNVs, which is comparable to other studies as well [ 30 , 31 ].
NIPT shows a very low rate of false-positive and false-negative results compared to traditional prenatal screening results. Several conditions have been known to contribute to false-positive and negative NIPT results: low FF, maternal CNVs and fetal/placental mosaicism are among them [ 32 ]. False-negative results are rare for NIPT, with a frequency of only 0.08% [ 22 ]. In our study we didn’t have false-negative results for common trisomies, SCAs and RAAs. CNVs false-negative rates was 0.008%.
The false-positive rate for common trisomies in our study reached 0.05%, that is much lower than that reported in other studies [ 33 ]. False-positive rate for RAAs and CNVs in our study was 0,09% and 0,04%, respectively. It is assumed that low positive predictive values as well as false-positive rate for CNVs detection are connected with their low frequencies in population.
More over to proven effects there is also one potential effect – decreasing the number of IPD performed in pregnant women. Among 366 women considered to be high risk by traditional prenatal screening, only 105 were confirmed to be high risk by NIPT. That means that 366 women were advised to undergo IPD, although only one third needed these invasive procedures. Currently, the decrease in the number of IPDs is only theoretical, since the regulation of prenatal screening in Russia does not take into account the results of NIPT, and all women at high risk after traditional prenatal screening are considered to undergo IPD.
NIPT has clinical, social and economic benefits. We found social NIPT benefits in its methodology and sample collection. NIPT is safe in blood sampling. Any surgical interventions for are not required. All these can diminish the patient’s anxiety level, which is quite important for pregnant women who may experience hormone-related emotional changes. Moreover, the low false-positive and false-negative rates results reported here and in previous studies [ 34 ], suggests that pregnant women can have high confidence in their NIPT results. In our study, we assessed women’s approaches towards NIPT. The results are processing.
Although NIPT is expensive to perform, its economic benefit manifests over an extended period. NIPT can decrease the direct and indirect costs by decreasing budget payments for the maintenance of people with disabilities.
However, despite the obvious advantages of NIPT adoption, there is a downside. The adoption of NIPT in many countries has led to a decrease in IPD procedures, which has had negative consequences, as some authors have proposed [ 35 ]. One report has suggested that a decline in IPD procedures causes a downturn in opportunities for physicians to practice the skills needed for IPD procedures, leading to significantly higher miscarriage rates associated with these procedures.
The accuracy of NIPT is affected by numerous factors both biological and technical and include the number of sequencing tags, FF, GC base content, and others. FF is a crucial quality control parameter for NIPT interpretation [ 36 ]. Low FF can result in a test failure or a “no call” result. In our study in 2.7% (346/12700) of cases FF was less than 3.5% and a blood sample redraw was required. Any biological factors that increase the maternal contribution and/or reduce the placental contribution may lower the FF [ 37 ]: feto-placental – gestational age, crown rump length, mosaicism, fetal aneuploidy, triploidy, multiple pregnancy, and maternal – maternal age, maternal weight, maternal autoimmune disease, low molecular weight heparin, ethnicity, mode of conception [ 38 , 39 ]. Maternal characteristics such as BMI and gestational age are the main factors that influence FF [ 40 ]. Previous data showed that FF below 4% increased with maternal weight from < 1% at 60 kg to > 50% at 160 kg [ 41 ]. Therefore, the clinical application of NIPT is limited by low FF of cfDNA in obese women. The rate of increase in FF is not constant across gestational age. From 10–12.5 weeks, 12.5–20 weeks, and > 20 weeks, the FF increases at rates of 0.44%, 0.083%, and 0.821% per week, respectively [ 42 ]. Waiting for a later gestational age and repeating blood sampling is not a reliable approach to overcome the low FF in subjects with higher BMIs and earlier gestational ages [ 43 ].
In our study, we analyzed the influence of some available parameters on FF and observed no significant differences between FF and maternal age, gestational age, mode of conception and type of pregnancy. However, we noticed a statistically significant decrease in FF with increased BMI and maternal weight.
In our study it was also shown, that higher FF was more common for male fetuses and for fetuses with high risk for T21, lower FF – for fetuses with high risk for T18. The same was also published in some other studies, showing that euploid male fetus pregnancies with high risk of T21 had higher FF [ 44 ]. For T18, T13 and monosomy X, vice versa other studies has shown lower FF. Higher FF in fetuses with T21 may be one of the reasons the test performance is better for T21 than for T18 and T13. In our study the cut-off for high T21 risk was 9.0% FF. We didn’t find any significant difference in FF for T13 and monosomy X, that is probably due to low incidence yet.
Pregnant women aged over 35 years are usually categorized as advanced maternal age [ 42 ]. It is reported that advanced maternal age is associated with various pregnancy complications, including infant chromosomal anomalies. It is known that such chromosomal abnormalities as T21, T18, T13, triple X syndrome, and XYY syndrome have a close association with maternal age [ 7 ]. However, pathogenic chromosomal deletions and duplications also occur de novo, and the risk of microdeletions and microduplications is the same for all pregnancies regardless of maternal age [ 45 ]. In our study, we detected a significantly higher risk of the genetic abnormalities in women aged 39 and older.
Some studies have also reported that even when the NIPT result was negative, many other chromosomal anomalies could be detected by other technical methods [ 46 ]. The major types of missed fetal abnormalities include structural (balanced or unbalanced) rearrangements, mosaic and triploidies [ 47 ]. Chena et al. declare that 12.4% of fetal chromosomal abnormalities will be missed if NIPT completely replaces IPD in advanced aged pregnant women [ 46 ]. In 2020 ACOG proposed prenatal screening for aneuploidy for all pregnant women, regardless of age or baseline risk factors [ 48 ], but NIPT cannot completely replace IPD in advanced maternal aged women.
NIPT as a second-line test in Moscow, Russia have shown its effectiveness. The major advantage of NIPT was safety, detection of additional chromosomal anomalies and reduction in false-positive rates. Moreover, our findings suggest that NIPT merits serious consideration as a primary screening method for fetal autosomal aneuploidy. NIPT should be recommended for all pregnant women in risk groups, but using it as a first-tier screening and diagnostic tool requires further study.
Limitations of the present study
Main limitations are lack of data due to women refused to undergo IPD and lack of information about pregnancies outcomes.
Availability of data and materials
The datasets generated during and analyzed during the current study are not publicly available due to prohibition of sending raw sequencing data to foreign repositories but are available from the corresponding author on reasonable request.
Abbreviations
Array-based comparative genomic hybridization
American College of Obstetricians and Gynecologists
Body mass index
Cell-free DNA
Copy umber variants
Chorionic villus sampling
Deoxyribonucleic acid
Fetal fraction
False negative
False positive
Glyceraldehyde-3-phosphate dehydrogenase
Human chorionic gonadotrophin
Invasive prenatal diagnosis
Non–invasive prenatal testing
Negative predictive value
Pregnancy-associated plasma protein A
Positive predictive value
Rare autosomal aneuploidies
True positive
True negative
Sex chromosomal aneuploidy
MacDorman MF. Race and ethnic disparities in fetal mortality, preterm birth, and infant mortality in the United States: an overview. Semin Perinatol. 2011;35(4):200–8.
Article PubMed Google Scholar
Baranov AA, Namazova-Baranova LS, Belyaeva IA, Bombardirova EP, Smirnov IE. Medical and social problems of assisted reproductive technologies from the perspective of pediatrics. Vestn Ross Akad Med Nauk. 2015;3:307–14.
Article Google Scholar
Baranov AA, Namazova-Baranova LS, Albitskiy V, Terletskaya RN. Tendencies of infantile and child mortality in the conditions of implementation of the modern strategy of development of health care of the Russian Federation. Vestnic RAMN. 2017;72(5):375–82.
Google Scholar
Sukhikh GT, Karetnikova NA, Baranova EE, Shubina ES, Korostin DO, Evdokimov AN, et al. Noninvasive prenatal diagnosis of aneuploidies by high-throughput sequencing (NGS) in a group of high-risk women. Obstet Gynecol (Moscow). 2016;6:129–57.
Gregg AR, Skotko BG, Benkendorf JL, Monaghan KG, Bajaj K, Best RG, et al. Noninvasive prenatal screening for fetal aneuploidy, 2016 update: a position statement of the American College of Medical Genetics and Genomics. Genet Med. 2016;18(10):1056–65.
Article CAS PubMed Google Scholar
Benn P, Cuckle H, Pergament E. Non-invasive prenatal testing for aneuploidy: current status and future prospects. Ultrasound Obstet Gynecol. 2013;42(1):15–33.
Pös O, Budiš J, Szemes T. Recent trends in prenatal genetic screening and testing. F1000Res. 2019;8:F1000 Faculty Rev-764.
Article PubMed PubMed Central Google Scholar
Taylor-Phillips S, Freeman K, Geppert J, Agbebiyi A, Uthman OA, Madan J, Clarke A, Quenby S, Clarke A. Accuracy of non-invasive prenatal testing using cell-free DNA for detection of Down, Edwards and Patau syndromes: a systematic review and meta-analysis. BMJ Open. 2016;6(1):e010002.
Mackie FL, Hemming K, Allen S, Morris RK, Kilby MD. The accuracy of cell-free fetal DNA based non-invasive prenatal testing in singleton pregnancies: a systematic review and bivariate meta-analysis. BJOG. 2017;124(1):32–46.
Neofytou M. Predicting fetoplacental mosaicism during cfDNA-based NIPT. Curr Opin Obstet Gynecol. 2020;32(2):152–8.
Pertile MD. Chapter 7: Genome-wide cell-free DNA-based prenatal testing for rare autosomal trisomies and subchromosomal abnormalities. In: PageChristiaens L, Klein H-G, editors. Noninvasive prenatal testing (NIPT) [Internet]. London, United Kingdom: Academic Press; 2018. p. 97–123.
Chapter Google Scholar
Noninvasive Prenatal Testing for Fetal Aneuploidy. Available from: http://www.acog.org/Resources-And-Publications/Committee-Opinions/Committee-on-Genetics/Noninvasive-Prenatal-Testing-for-Fetal-Aneuploidy . Accessed July 28, 2014.
Porreco RP, Garite TJ, Maurel K, Marusiak B, Ehrich M, van den Boom D, et al. Noninvasive prenatal screening for fetal trisomies 21, 18, 13 and the common sex chromosome aneuploidies from maternal blood using massively parallel genomic sequencing of DNA. Am J Obstet Gynecol. 2014;211(4):365.e1-12.
Article CAS Google Scholar
Prikaz Minzdrava goroda Moscow № 199 ot 13.03.2020 «Ob organizatsii provedeniya neinvasivnogo prenatalnogo testa v gorode». https://www.mos.ru/dzdrav/documents/department-acts/view/237308220/ .
Olenev AS, Baranova EE, Sagaidak OV, Galaktionova AM, Kuznetsova ES, Kaplanova MT, et al. Adoption of a non-invasive prenatal test (NIPT) in prenatal screening in Moscow: first results. Rus Open Med J. 2021;10:e0110.
Yuan Y, Chai X, Liu N, Gu B, Li S, Gao Y, et al. FF-QuantSC: accurate quantification of fetal fraction by a neural network model. Mol Genet Genomic Med. 2020;8:e1232.
CAS PubMed PubMed Central Google Scholar
Lau TK, Chan MK, Lo PS, et al. Clinical utility of noninvasive fetal trisomy (NIFTY) test – early experience. J Matern Fetal Neonatal Med. 2012;25(10):1856–9.
Agarwal A, Sayres LC, Cho MK, Cook-Deegan R, Chandrasekharan S. Commercial landscape of noninvasive prenatal testing in the United States. Prenat Diagn. 2013;33(6):521–31.
Chandrasekharan S, Minnear MA, Hung A, Allyse M. Noninvasive prenatal testing goes global. Sci Transl Med. 2014;6(231):231fs15.
Bianchi DW, Chiu RWK. Sequencing of circulating cell-free DNA during pregnancy. N Engl J Med. 2018;379:464–73.
Gil MM, Revello R, Poon LC, Akolekar R, et al. Clinical implementation of routine screening for fetal trisomies in the UK NHS: cell-free DNA test contingent on results from first-trimester combined test. Ultrasound Obstet Gynecol. 2016;47(1):45–52.
Bianchi DW, Wilkins-Haug L. Integration of noninvasive DNA testing for aneuploidy into prenatal care: what has happened since the rubber met the road? Clin Chem. 2014;60(1):78–87.
van Schendel RV, van El CG, Pajkrt E, Henneman L, Cornel MC. Implementing non-invasive prenatal testing for aneuploidy in a national healthcare system: global challenges and national solutions. BMC Health Serv Res. 2017;17(1):670.
Karuna RM, van der M, Sistermans EA, Macville MVE, Stevens SJC, Bax CJ, et al. TRIDENT-2: National implementation of genome-wide non-invasive prenatal testing as a first-tier screening test in the Netherlands. AJHG. 2019;105:1091–101.
Neyt M, Hulstaert F, Gyselaers W. Introducing the non-invasive prenatal test for trisomy 21 in Belgium: a cost-consequences analysis. BMJ Open. 2014;4(11):e005922.
UK National Screening Committee non-invasive prenatal testing (NIPT) recommendation. January 2016; Department of Health and Social Care. The UK Strategy for Rare Diseases. 2020 update to the Implementation Plan for England. Published: 26 February 2020. https://www.gov.uk/government/publications/uk-strategy-for-rarediseases-2020-update-to-the-implementation-plan-for-england .
Hongtai L, Gao Y, Hu Z, Lin L, Yin X, Wang J, et al. Performance evaluation of NIPT in detection of chromosomal copy number variants using low-coverage whole-genome sequencing of plasma DNA. PLoS ONE. 2016;11(7):e0159233.
Liang D, Lin Y, Qiao F, Li H, Wang Y, Zhang J, et al. Perinatal outcomes following cell-free DNA screening in >32 000 women: clinical follow-up data from a single tertiary center and has relative lower sensitivities and specificities for T18, T13 and SCAs. Prenat Diagn. 2018;38(10):755–64.
Petersen AK, Cheung SW, Smith JL, Bi W, Ward PA, Peacock S, et al. Positive predictive value estimates for cell-free noninvasive prenatal screening from data of a large referral genetic diagnostic laboratory. Am J Obstet Gynecol. 2017;217(6):691.e1-691.e6.
Luo Y, Hu H, Jiang L, Ma Y, Zhang R, Xu J, et al. A retrospective analysis the clinic data and follow-up of non-invasive prenatal test in detection of fetal chromosomal aneuploidy in more than 40,000 cases in a single prenatal diagnosis center. Eur J Med Genet. 2000;6(9):104001.
Ramdaney A, Hoskovec J, Harkenrider J, Soto E, Murphy L. Clinical experience with sex chromosome aneuploidies detected by noninvasive prenatal testing (NIPT): Accuracy and patient decision-making. Prenat Diagn. 2018;38(11):841–8.
Samura O, Okamoto A. Causes of aberrant non-invasive prenatal testing for aneuploidy: a systematic review. Taiwan J Obstet Gyn. 2020;59:16–20.
Wang Y, Li S, Wang W, Dong Y, Zhang M, Wang X, Yin C. Cell-free DNA screening for sex chromosome aneuploidies by non-invasive prenatal testing in maternal plasma. Mol Cytogenet. 2020;13:10.
Article PubMed PubMed Central CAS Google Scholar
Beaudet AL. Using fetal cells for prenatal diagnosis: History and recent progress. Am J Med Genet C Semin Med Genet. 2016;172(2):123–7.
Hui L, Tabor A, Walker SP, Kilby MD. How to safeguard competency and training in invasive prenatal diagnosis: ‘the elephant in the room.’ Ultrasound Obstet Gynecol. 2016;47(1):8–13.
Kinnings SL, Geis JA, Almasri E, Wang H, Guan X, McCullough RM, et al. Factors affecting levels of circulating cell-free fetal DNA in maternal plasma and their implications for noninvasive prenatal testing. Prenat Diagn. 2015;35(8):816–22.
Hui L, Bianchi DW. Fetal fraction and noninvasive prenatal testing: what clinicians need to know. Prenat Diagn. 2020;40(2):155–63.
Lau TK, Zhao L, Yi X, Yin Y, Wang W. Noninvasive prenatal testing for trisomies 21, 18 and 13: clinical experience from 146,958 pregnancies. Ultrasound Obstet Gynecol. 2015;45:530–8.
Livergood MC, LeChien KA, Trudell AS. Obesity and cell-free DNA “no calls”: is there an optimal gestational age at time of sampling? Am J Obstet Gynecol. 2017;216:413.
PubMed Google Scholar
Qiao L, Zhang Q, Liang Y, Gao A, Ding Y, Zhao N, et al. Sequencing of short cfDNA fragments in NIPT improves fetal fraction with higher maternal BMI and early gestational age. Am J Transl Res. 2019;11(7):4450–9 eCollection 2019.
Ashoor G, Syngelaki A, Poon LC, Rezende JC, Nicolaides KH. Fetal fraction in maternal plasma cell-free DNA at 11–13 weeks’ gestation: relation to maternal and fetal characteristics. Ultrasound Obstet Gynecol. 2013;41:26–32.
Ahkam GK, Abdurrahman Hİ, Emrah B, Suriye Ö, Adnan B. Effect of advanced maternal age on pregnancy outcomes: a single-centre data from a tertiary healthcare hospital. J Obstet Gynaecol. 2019;39(8):1104–11.
Wang E, Batey A, Struble C, Musci T, Song K, Oliphant A. Gestational age and maternal weight effects on fetal cell-free DNA in maternal plasma. Prenat Diagn. 2013;33:662–6.
Goldenberg P. An update on common chromosome microdeletion and microduplication syndromes. Pediatr Ann. 2018;47(5):e198–203.
Chena Y-P, Heb Z-Q, Shia Ye, Zhoua Q, Caia Z-M, Bin Yu, et al. Not all chromosome aberrations can be detected by NIPT in women at advanced maternal age: a multicenter retrospective study. Clin Chim Acta. 2018;486:232–6. https://doi.org/10.1016/j.cca.2018.08.018 .
Zhu Y, Shiming Lu, Bian X, Wang He, Zhu B, Wang H, et al. A multicenter study of fetal chromosomal abnormalities in Chinese women of advanced maternal age. Taiwan J Obstet Gynecol. 2016;55(3):379–84. https://doi.org/10.1016/j.tjog.2016.01.002 .
Palomaki GE, Kloza EM. Prenatal cell-free DNA screening test failures: a systematic review of failure rates, risks of down syndrome, and impact of repeat testing. Genet Med. 2018;20(11):1312–23.
Download references
Acknowledgements
The authors thank the members of Evogen genome sequencing team for help with sequencing.
This study is funded by grant № 01–04-410 from 06.02.2020.
Author information
Authors and affiliations.
LLC “Evogen”, Moscow, Russian Federation
Elena E. Baranova, Olesya V. Sagaydak, Alexandra M. Galaktionova, Ekaterina S. Kuznetsova, Madina T. Kaplanova, Maria V. Makarova & Maxim S. Belenikin
Federal State Budgetary Educational Institution of Further Professional Education “Russian Medical Academy of Continuous Professional Education” of the Ministry of Healthcare of the Russian Federation, Moscow, Russian Federation
Elena E. Baranova
Moscow City Health Department, City clinical hospital №24, Moscow, Russian Federation
Anton S. Olenev
Moscow City Health Department, City clinical hospital №67 named after L.A. Vorokhobova, Moscow, Russian Federation
Ekaterina N. Songolova
You can also search for this author in PubMed Google Scholar
Contributions
EEB, OVS, ASO, ESK were involved in conception and design of the study. MSB, MTK and AMG performed the observations and the data collection. ESK and OVS performed a statistical data processing. ESK drafted the manuscript, MVM, OVS and EEB assisted with the manuscript and ASO and ENS revised the manuscript. All authors edited the manuscript and read and approved the final draft.
Corresponding author
Correspondence to Ekaterina S. Kuznetsova .
Ethics declarations
Ethics approval and consent to participate.
All participants signed informed written consent before a blood collection. The study received ethical approval from Moscow Independent Ethical Committee (MGEC). All methods were carried out in relevant regulations and guidelines.
Consent for publication
Not required.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Baranova, E.E., Sagaydak, O.V., Galaktionova, A.M. et al. Whole genome non-invasive prenatal testing in prenatal screening algorithm: clinical experience from 12,700 pregnancies. BMC Pregnancy Childbirth 22 , 633 (2022). https://doi.org/10.1186/s12884-022-04966-8
Download citation
Received : 10 March 2022
Accepted : 03 August 2022
Published : 09 August 2022
DOI : https://doi.org/10.1186/s12884-022-04966-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Non-invasive prenatal testing
- Prenatal screening
- Fetal aneuploidy
- Amniocentesis
- Rare autosomal trisomies
BMC Pregnancy and Childbirth
ISSN: 1471-2393
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Research article
- Open access
- Published: 16 October 2023
Association of breastfeeding with mental disorders in mother and child: a systematic review and meta-analysis
- Polina Bugaeva 1 na1 ,
- Inna Arkusha 2 , 3 na1 ,
- Rinat Bikaev 3 na1 ,
- Igor Kamenskiy 4 ,
- Aleksandra Pokrovskaya 5 ,
- Yasmin El-Taravi 6 ,
- Valeria Caso 7 ,
- Alla Avedisova 2 ,
- Derek K. Chu 8 ,
- Jon Genuneit 9 , 10 ,
- Gabriel Torbahn 11 , 12 ,
- Timothy R. Nicholson 13 ,
- Dina Baimukhambetova 14 ,
- Aigun Mursalova 14 ,
- Anastasia Kolotilina 14 ,
- Svetlana Gadetskaya 14 ,
- Elena Kondrikova 14 ,
- Mikhail Zinchuk 3 ,
- Renat Akzhigitov 3 ,
- Robert J. Boyle 15 ,
- Alla Guekht 3 &
- Daniel Munblit ORCID: orcid.org/0000-0001-9652-6856 15 , 16 , 17 , 18
BMC Medicine volume 21 , Article number: 393 ( 2023 ) Cite this article
4724 Accesses
2 Citations
24 Altmetric
Metrics details
Breastfeeding has long been associated with numerous benefits for both mothers and infants. While some observational studies have explored the relationship between breastfeeding and mental health outcomes in mothers and children, a systematic review of the available evidence is lacking. The purpose of this study is to systematically evaluate the association between breastfeeding and mental health disorders in mothers and children.
We systematically searched MEDLINE and EMBASE from inception to June 2, 2023. The inclusion criteria consisted of all studies evaluating links between breastfeeding and development of mental health disorders in children and mothers. Risk of bias was assessed using the Newcastle–Ottawa Scale (NOS) while grading of Recommendations Assessment, Development and Evaluation (GRADE) was used to assess the certainty of evidence. A random-effects meta-analysis was used if possible, to estimate the odds ratio for the association between breastfeeding and mental health outcomes. The Mantel–Haenszel method was utilised for pooling ORs across studies. Study heterogeneity was assessed using the I 2 statistic.
Our review identified twenty-one original study. Of these, 18 focused on the association between breastfeeding and child health, assessing depressive disorders, schizophrenia, anxiety disorders, eating disorders and borderline personality disorder. Three studies evaluated the associations between breastfeeding and maternal mental health disorders. Three studies looking at outcomes in children showed no significant association between breastfeeding and occurrence of schizophrenia later in life (OR 0.98; 95% CI 0.57–1.71; I 2 = 29%). For depressive disorders (5 studies) and anxiety disorders (3 studies), we found conflicting evidence with some studies showing a small protective effect while others found no effect. The GRADE certainty for all these findings was very low due to multiple limitations. Three studies looking at association between breastfeeding and maternal mental health, were too heterogeneous to draw any firm conclusions.
Conclusions
We found limited evidence to support a protective association between breastfeeding and the development of mental health disorders in children later in life. The data regarding the association between breastfeeding and maternal mental health beyond the postnatal period is also limited. The methodological limitations of the published literature prevent definitive conclusions, and further research is needed to better understand the relationship between breastfeeding and mental health in mothers and children.
Peer Review reports
Introduction
Mental health disorders continue to be a major global medical and societal burden, affecting individuals of all ages. These disorders are linked to significant morbidity, disability, and mortality rates [ 1 , 2 ]. Prior to the COVID-19 pandemic, the Global Burden of Disease Study estimated that 264 million people worldwide suffered from depression, while bipolar disorder and schizophrenia affected 45 million and 20 million individuals respectively [ 3 ]. The COVID-19 pandemic additionally resulted in increase in prevalence of major depressive disorder and anxiety disorders [ 4 ]. Individuals residing in regions with political, social, and humanitarian problems are particularly susceptible to mental health disorders [ 2 ]. In developed countries, patients often face stigmatisation and neglect by society [ 2 , 5 , 6 ].
The aetiology and mechanisms of mental disorders are complex and not fully understood with multiple factors, hereditary, social and environmental, proposed among the main contributors to their development which limits potential for preventive measures [ 7 ]. Potential exposures during infancy and early childhood were extensively investigated and associations with mental health disorders development were reported [ 8 ].
Breastfeeding is associated with multiple beneficial effects for maternal and child health. Leading local and international organisations, such as the World Health Organization (WHO) [ 9 ], the European Commission for Public Health (ECPH) [ 10 ] and the American Academy of Pediatrics (AAP), produced guidelines recognising exclusive breastfeeding as an optimal feeding method during the first 6 months of life [ 11 ]. Breastfeeding is a well-established contributor both to child socioemotional and neurocognitive development [ 12 , 13 ]. The reason commonly named behind this association is presence of potentially beneficial constituents, such as immunological biomarkers and long-chain polyunsaturated fatty acids (LC-PUFAs), that cannot be fully replaced by human milk substitutes [ 14 , 15 , 16 ], association between breastfeeding and attachment [ 17 ], skin-to-skin contact and socio-emotional aspects [ 14 ].
Although some attempts to investigate associations between breastfeeding and mental disorders were made, comprehensive assessment of available evidence is still lacking. Therefore, the aim of this systematic review is to comprehensively assess available up to date evidence on the associations between breastfeeding and development of mental health disorders in children and mothers to provide an impetus for further research in the field and improve our understanding of the topic.
This systematic review is reported in accordance with the recommendations set forth by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [ 18 ]. The review protocol was registered with the National Institute for Health Research’s PROSPERO a priori (PROSPERO 2019 CRD42019134214).
Search and screening
Studies were identified through searches of two electronic databases (Medline and Embase via OVID) from inception to June 3, 2021, using both free text and medical subject headings (MeSH) terms. Additional search was performed on June 2, 2023, to screen for recent papers. The search strategies are presented in Additional file 1 : Box S1. In addition, the publications cited in the reference lists of the included studies and previously published review articles were carefully screened to ensure that no original published data had been missed.
Pairs of authors (PB, IA, DB, AM and RB) independently conducted the title and abstract screening. Any disagreements between the screeners were resolved via consensus or a third reviewer (DM).
Eligibility criteria
Types of studies.
Any randomised controlled trials (RCTs), quasi-RCTs, as well as cohort (prospective or retrospective) studies, nested case–control studies, other case–control studies and cross-sectional studies (including those with retrospective data) were included.
Types of participants
No restrictions to specific population and high-risk groups (e.g. cohorts of patients with family history of mental illnesses) were applied.
Types of interventions or exposures
Type/duration of breastfeeding. Our systematic review encompassed all infants who were fed breast milk, irrespective of whether it was delivered directly through breastfeeding or administered via a bottle of expressed milk.
The comparison was made with the individuals who were not breastfed (any other type of feeding) and/or breastfeeding of varying duration.
Outcomes of interest
The outcomes of interest are as follows: depressive disorders, bipolar disorder, anxiety disorders, phobia, social anxiety disorders, panic disorder, obsessive–compulsive disorder, separation anxiety disorder, personality disorders, neuroticism, feeding and eating disorders, anorexia, bulimia, binge eating disorder, posttraumatic stress disorder, dysphoria, dissociative disorders, schizophrenia, anaclitic depression, attachment, suicide, alcohol addiction. We did not apply any restrictions pertaining to the diagnosis of the condition.
This systematic review delved into the associations between breastfeeding and designated mental health outcomes, separately assessing these relationships for (a) children and (b) mothers.
Studies with follow-up period less than 12 months since birth were excluded. Manuscripts investigating associations between breastfeeding and autism spectrum disorders (ASD) and attention deficit hyperactivity disorders (ADHD) were excluded, as systematic reviews regarding these conditions were published recently [ 19 , 20 ]. Premature infants are at an increased risk for chronic medical conditions and developmental outcomes, including mental health disorders [ 21 ]. However, the underlying factors that contribute to these risks may differ from those in full-term infants. Therefore, including studies that focus specifically on premature infants may introduce heterogeneity into the analysis, making it difficult to draw conclusions about the association between breastfeeding and mental health outcomes in a general population. To ensure the validity and generalisability of the results, we excluded research papers in which the subjects were premature infants from this systematic review. We also excluded studies providing no specific diagnosis in patients within the cohort of interest. As this topic has been addressed in a previous systematic review, studies examining the relationship between breastfeeding and postnatal maternal depression were excluded [ 22 ].
Data extraction
Pairs of authors (PB, IA, DB, AM, AP and RB) independently conducted the data extraction. The extracted data included study design, country of the study, population characteristics, age of children or/and follow-up period, sample size and follow-up rate, number of cases and controls in exposed and non-exposed group, definition of exposure and outcome, methods of outcome assessment, effect estimates with 95% Cis and confounders included in the analysis.
Data synthesis
All studies included in the systematic review were grouped by the outcome of interest and study type and then further grouped according to the type and/or duration of breastfeeding and effect measure (e.g. odds ratio, hazard ratio). Final groups with three or more studies with comparable exposure and outcome definition were considered suitable for meta-analysis. For outcomes where the original studies did not report both the number of participants in the exposed and non-exposed groups and the odds ratios, meta-analysis was not conducted. This is because such information is necessary to calculate the weights of the studies and estimate the overall effect size.
A random-effects meta-analysis was conducted to estimate the odds ratio (OR) and corresponding 95% confidence interval for the association between breastfeeding and mental health outcomes. The Mantel–Haenszel method was used to pool the Ors across studies. The results were considered statistically significant if the 95% CI did not include the null value of 1.0. Heterogeneity across studies was assessed using the I -squared ( I 2 ) statistic.
Risk of bias assessment
Risk of bias assessment was performed by two authors (PB and RB or YET) independently using Newcastle–Ottawa Scale (NOS), which provides different assessment strategies for case–control and cohort studies [ 23 ]. Assessment according to NOS total score was reported as follows: very good = 9–10, good = 7–8, satisfactory = 5–6, unsatisfactory = 0–4. Selection of NOS instead of Risk Of Bias In Non-randomised Studies—of Interventions (ROBINS-I) was based on similar reliability but better applicability [ 24 ]. Results of NOS evaluation are outlined in Additional file 1 : Tables S1–S3.
The grading of Recommendations, Assessment and Evaluation (GRADE) approach was used to evaluate the certainty of evidence for diseases of interest where pooled analyses and/or narrative synthesis was possible. As per suggested approach it was classified into high, moderate, low and very low [ 25 ]. Data from observational studies were considered low-quality evidence unless there was plausible evidence which would suggest upgrade of evidence certainty [ 26 ].
A total of 17,887 items were identified through initial searches, and 40 articles met the inclusion criteria after duplicate removal and title/abstract screening (Fig. 1 ). Full-text manuscripts were assessed, and 19 articles were excluded, resulting in 21 articles included in the qualitative synthesis, with 18 investigating association between breastfeeding and child health and three looking at maternal health outcomes. Of these, three studies were included in the quantitative synthesis for the outcome of schizophrenia. The included studies were published between 1997 and 2023 and were all observational, comprising of 6 case–control studies [ 27 , 28 , 29 , 30 , 31 , 32 ], 5 retrospective studies [ 33 , 34 , 35 , 36 , 37 ] and 9 prospective cohort studies [ 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 ] and one cross-sectional study with retrospective assessment of the exposure [ 47 ].
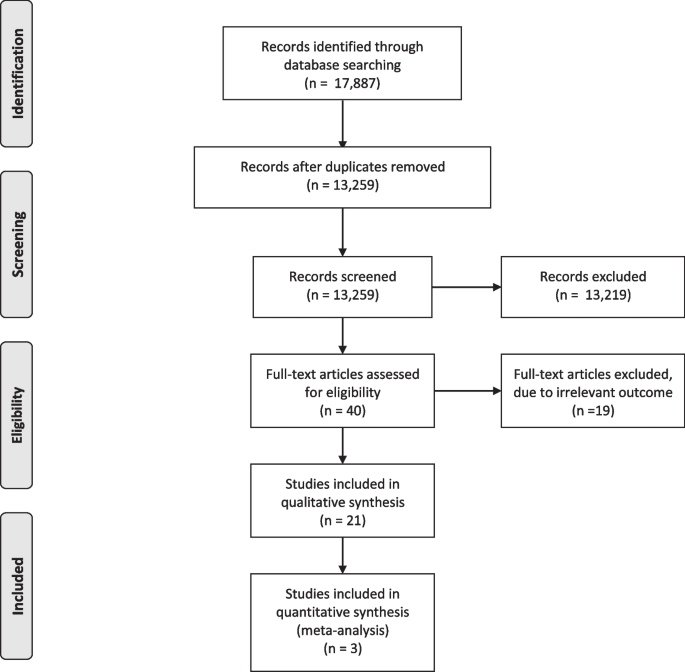
PRISMA flow diagram
The studies investigated associations between breastfeeding and mental health disorders in children and maternal mental health disorders. Specifically, eight studies assessed depressive disorders [ 33 , 34 , 36 , 40 , 41 , 43 , 45 , 47 ], six investigated schizophrenia [ 28 , 29 , 30 , 32 , 37 , 38 ] and five looked at anxiety disorders [ 31 , 41 , 43 , 45 , 47 ], while eating disorders [ 42 ] and borderline personality disorder [ 27 ] were assessed in one study each. In one study, the prevalence of mental health disorders in children was described without specifying the outcome [ 44 ].
Three studies evaluated the associations between breastfeeding and maternal mental health disorders [ 35 , 39 , 46 ].
Participant characteristics
Studies were carried out in twelve different countries, with the majority of the research being conducted in the European and Australasian regions. There were three studies conducted in China [ 33 , 34 , 40 ], three in the USA [ 36 , 39 , 42 ], three in Australia [ 41 , 43 , 46 ], and in the United Kingdom [ 32 , 37 , 47 ], two in Brazil [ 44 , 45 ] and one each in South Korea [ 35 ], Japan [ 29 ], South Africa[ 28 ], Italy [ 30 ], Turkey [ 31 ], Denmark [ 38 ] and Germany [ 27 ].
Sample size ranged from 160 [ 39 ] to 186,452 [ 25 ] participants in cohort studies and between 100 [ 28 ] and 450 [ 31 ] in case–control studies. Most of the studies followed children up to the adolescence with the maximum follow-up duration of 40 years.
Breastfeeding definition and reporting
There was a substantial variation in breastfeeding reporting and definitions used. Some studies collected already predefined data from the registries [ 46 ], others used structured standardised (e.g. Pre-/Postnatal Stress Questionnaire (NPQ-PSQ) [ 27 ], Growing Up Today Study (GUTS) questionnaire [ 42 ]) and non-standardised questionnaires and interviews [ 28 , 30 , 41 , 44 , 45 , 47 , 31 , 32 , 33 , 34 , 36 , 37 , 39 , 40 ] obtaining the data prospectively or retrospectively. Exclusive breastfeeding was usually defined as breastfeeding without intake of “any other food”.
Association between breastfeeding and mental health in children
- Schizophrenia
Six studies investigated schizophrenia, with four using case–control design [ 28 , 29 , 30 , 32 ], and two cohort studies, a prospective [ 38 ] and a retrospective [ 37 ] (Table 1 ). The outcome of interest was defined in accordance with Diagnostic and Statistical Manual of Mental Disorders (DSM)-III [ 32 ], DSM-IV [ 28 , 29 , 30 ], ICD 9 [ 37 ], International Classification of Diseases (ICD)-8 code 295 or ICD-10 code F20 [ 28 ]. In a single study, Sorensen and co-authors defined schizophrenia as bizarre delusions, delusions of control, abnormal affect, autism, hallucinations and disorganised thinking [ 38 ].
The study risk of bias determined by means of NOS was good in cohort studies, while case–control studies were generally of satisfactory risk of bias (range satisfactory to good). The common flaw was lack of adjustment for potentially significant confounders such as family history of schizophrenia, with four studies presenting crude data only [ 28 , 29 , 30 , 37 ]. Exposure to breastfeeding was self-reported by parents, and for several case–control studies, the recall period exceeded 20 years [ 32 , 37 , 38 ].
All but one study [ 38 ] found no association between breastfeeding and schizophrenia, Sorensen et al. reported an association between breastfeeding for two weeks or less and increased risk of schizophrenia adjOR 1.73 (95% CI 1.13–2.67) upon adjustment for maternal schizophrenia, single mother status, sex and parental social status at 1 year of age.
Heterogeneity in methodology and lack of relevant outcome reporting did not allow for meta-analysis of the data from cohort studies. The pooled data from three case–control studies ( n = 528) showed no significant association between breastfeeding and schizophrenia later in life OR 0.98 (95% CI 0.57–1.71) [ 28 , 29 , 30 ] (Fig. 2 ). In the sensitivity analysis, addition of another study [ 37 ] which used siblings as a control group did not change the results OR 0.89 (95% CI 0.58–1.38). The GRADE certainty of evidence was very low due to risk of bias and serious imprecision (Table 2 ).
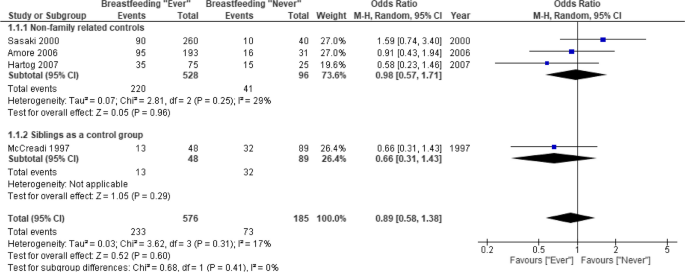
Meta-analysis of case–control studies. Breastfeeding (ever vs. never) and risk of schizophrenia. 1.1.1. Primary analysis, which includes studies using non-family related subjects as a control group. 1.1.2. Sensitivity analysis, which included McCreadi et al. study, which used siblings as a control group
- Depressive disorders
Five studies (three retrospective [ 33 , 34 , 36 ], two prospective cohorts [ 31 , 36 ] and one cross-sectional study with retrospective assessment of the exposure which derived data from the UK biobank cohort [ 47 ]) investigated depressive disorders (Table 3 ).
A wide range of instruments was used across the studies for outcome assessment: Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID) 5.0 [ 33 , 45 ], Child Behaviour Check List (CBCL) which is very consistent with DSM-V diagnostic categories [ 34 ]. Other scales included PHQ-9 (self-reported Patient Health Questionnaire-9) that is consistent with DSM-IV [ 40 , 47 ] and Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS) which is compatible with DSM-III [ 36 ]. According to PHQ-9, depression was defined as having a total score of 11 or more mapping on to DSM-IV [ 40 ]. De Mola et al. used Beck’s Depression Inventory (BDI-II) validated for Brazilian population to assess severity of depressive symptoms [ 45 ].
The study risk of bias was satisfactory on average, ranging between 4 and 7 as per NOS.
Kwok et al. and De Mola et al. reported no association between breastfeeding and depressive disorders development [ 40 , 45 ] upon adjustment for multiple potential confounders. Other two studies showed that absence of any breastfeeding was associated with an increased risk (adjOR 1.88 (95% CI 1.28–2.49 and adjOR 1.71 (95% CI 1.14–2.56) respectively) of depressive disorders later on in life (6–16 years of age) [ 33 , 36 ]. Huang et al. reported a protective effect of breastfeeding only in children who were breastfed longer than 6 months compared to those who have never been breastfed adjOR 0.45 (95% CI 0.23–0.91), while shorter duration of breastfeeding was not associated with any protective effect adjOR 0.79 (95% CI 0.37–1.67) [ 34 ]. A very recent cross-sectional study from Liu et al., based on the data from the UK Biobank cohort suggested protective effect of breastfeeding in mothers smoking adjOR 0.86 (95% CI 0.82–0.91) and not smoking adjOR 0.82 (95% CI 0.79–0.84) during pregnancy [ 47 ]. The overall GRADE certainty of evidence was very low due to potential risk of bias, serious inconsistency and indirectness (Table 2 ).
There was a lack of studies reporting the number of participants in the exposed and non-exposed groups to conduct meta-analysis.
- Anxiety disorders
Three studies (one case–control [ 31 ], one prospective cohort study [ 36 ] and one cross-sectional study with retrospective assessment of the exposure using the data from the UK biobank cohort [ 47 ]) investigated association between breastfeeding and anxiety disorders [ 22 , 36 ] (Table 4 ).
For the primary outcome assessment, Orengul et al. investigated social anxiety disorder, unspecified anxiety disorders, generalised anxiety disorder, specific phobias, separation anxiety disorder and panic disorder using Schedule for affective disorders and schizophrenia for school-age children, present version (K-SADS-P), and the Revised Child Anxiety and Depression Scale (RCADS), total anxiety subscale [ 31 ], while De Mola et al. studied generalised anxiety disorder and social anxiety disorder using Mini International Neuropsychiatric Interview version 5.0 validated for Brazil [ 45 ].
The risk of bias of the studies varied from unsatisfactory to good.
De Mola and co-authors in their cohort study found no association between breastfeeding or its’ duration and anxiety disorders development [ 45 ], while a case–control study from Orengul et al. [ 31 ] found reduced risk in breastfed children when compared with those who have never been exposed to breast milk OR 0.17 (95% CI 0.05–0.60). Liu et al. found that breastfeeding in mothers smoking adjOR 0.87 (95% CI 0.79–0.87) and not smoking adjOR 0.83 (95% CI 0.79–0.87) during pregnancy being associated with less anxiety in a cross-sectional study based on the data from the UK Biobank cohort [ 47 ]. The overall GRADE certainty of evidence was very low due to potential risk of bias and serious inconsistency (Table 2 ).
Depressive/anxiety disorders as a composite outcome
Two cohort studies assessed anxiety and depression as a composite outcome. Hayatbakhsh and co-authors used the Youth Self Report (YSR) of the Child Behaviour Check List (CBCL) which has the same format as the CBCL but with questions paraphrased in the first person [ 41 ]. Oddy et al. reported composite outcome “internalising complaints” that included withdrawn, somatic complaints, anxiety, and depression [ 43 ]. Hayatbakhsh et al. found breastfeeding for at least 4 months to be associated with lower scores of CBCL “anxiety/depression” domain at 14 years of age, while Oddy et al. reported breastfeeding for less than 6 months being associated with higher risk of internalising complaints OR 1.21 (95% CI 1.0–1.46).
Other mental health disorders
Other conditions investigated in the reviewed manuscripts included borderline personality disorder (BPD) [ 27 ] and eating disorders [ 42 ] (Table 5 ).
In a case–control study, Schwarze et al. investigated BPD defined as a pervasive pattern of impulsivity, emotional instability, identity disturbance and dysfunctional interpersonal relationships and diagnosed according to DSM-IV criteria for BPD [ 27 ]. Authors reported increased odds of BPD in those who have never been breastfed adjOR 4.68 (95% CI 1.88–11.66).
In a cohort study, Iron-Segev et al. assessed a broad range of eating disorders, including bulimic behaviours like purging, binge eating and other self-reported eating disorders like anorexia nervosa and bulimia nervosa. Purging was defined as using laxatives or force vomiting to lose weight or keep from gaining weight more than one time a month. The patient was considered as binge eater if eating binge at least once a month and feeling out of control while doing so was reported [ 42 ]. The study did not find any associations between breastfeeding duration (< 4 months, 4–9 months, > 9 months) and any eating disorder.
Association between breastfeeding and maternal mental health
Three studies (a retrospective [ 35 ] and two prospective cohorts [ 39 , 46 ]) investigated associations between breastfeeding and long-term development of maternal mental health outcomes post lactation (Table 6 ). Among them, one looked at a variety of mental disorders, including schizophrenia, unipolar depression, bipolar affective disorder and anxiety disorders [ 46 ] and two assessed associations with maternal depression [ 35 , 39 ].
For depression assessment, instruments used included Patient Health Questionnaire 9 (PHQ-9), with scores of 10 or higher indicating depression [ 35 ], Edinburgh Postnatal Depression Scale (EPDS), with a cut-off of 10 scores being considered a minor depression [ 39 ] and ICD-10 codes at admission for each diagnosis of interest [ 46 ].
The study risk of bias determined by means of NOS varied from satisfactory to good.
Xu et. al reported association between absence of breastfeeding at the time of hospital discharge and higher risk of schizophrenia adjOR 2.0 (95% CI 1.3–3.1) and bipolar affective disorder adjOR 1.9 (95% CI 1.1–3.5) 12 months after delivery but found no protective effect against anxiety disorders and unipolar depression [ 46 ].
Park et al. reported protective effect of prolonged (> 47 months) breastfeeding against maternal depression in the postmenopausal period adjOR 0.33 (95% CI 0.16–0.68) [ 35 ].
Hahn-Holbrook and co-authors suggested that women who breastfed more frequently at 3 months postpartum showed greater subsequent declines in depressive symptomatology over time compared to women who breastfed less frequently and lower absolute levels of depressive symptoms by 24 months since birth [ 39 ].
Heterogeneity in outcome assessment did not allow for meta-analysis.
Breastfeeding has been shown to have a number of benefits for both mother and child. This systematic review assessed up-to-date evidence regarding breastfeeding association with mental health disorders in mother and child. Overall, the current evidence suggests that there is very weak or no association between breastfeeding and the development of mental health disorders. This conclusion is supported by the findings from several studies, including three studies that reported no association between breastfeeding and schizophrenia development in later life (very low evidence). There is conflicting evidence when it comes to associations between breastfeeding and the development of depressive and anxiety disorders, with some studies showing a small protective effect and others reporting no effect. Published literature on this topic has substantial methodological limitations that make it difficult to draw firm conclusions. As it is very hard to randomise breastfeeding exposure, particularly from the ethical perspective, all available evidence comes from observational research only. The GRADE assessment we provide serves a reflection of this limitation and possible biases.
In the published literature, several studies have examined the potential associations between breastfeeding and mental health disorders in both children and mothers. Among studies looking at outcomes in offspring, the majority assessed depressive disorders, schizophrenia and anxiety disorders. Single studies evaluated eating and borderline personality disorders. A small number of studies evaluated associations between breastfeeding and maternal mental health disorders, such as schizophrenia, bipolar affective disorder, anxiety disorders and depression.
Schizophrenia was the outcome most often reported, with six studies investigating the potential association between breastfeeding and this disease using a variety of methodologies including case–control and cohort designs. The risk of bias of these studies was generally good for the cohort studies and satisfactory to good for the case–control studies, although several studies did not adequately adjust for potentially significant confounders such as family history of schizophrenia. Exposure to breastfeeding was self-reported by parents in most of these studies, and the recall period in some of the case–control studies exceeded 20 years. Overall, most of the studies found no significant association between breastfeeding and schizophrenia. Our meta-analyses of case–control studies demonstrated null effect. However, it is worth noting that a major limitation of case–control studies was lack of adjustment for confounding factors. Due to a small number of cohort studies reporting breastfeeding and schizophrenia, and heterogeneity in outcome reporting, we were unable to perform a meta-analysis. The only study reporting protective effect of breastfeeding for more than two weeks was the Copenhagen Perinatal Cohort [ 38 ].
Five cohort studies have investigated the potential association between breastfeeding and the development of depressive disorders in children. The risk of bias of these studies was satisfactory on average, according to the NOS. Two large cohort studies reported no effect, upon adjustment for multiple potential confounders. Two other studies found that an absence of exposure to breastfeeding was associated with an increased risk of developing depressive disorders later in life [ 33 , 36 ]. The fifth study reported a protective effect of breastfeeding on the development of depressive disorders, but only in children who were breastfed for longer than 6 months, while shorter duration of breastfeeding was not associated with any protective effect [ 34 ]. We noted a substantial heterogeneity in approaches to the data collection, differing confounding factors used for adjustment and the outcome assessment with a variety of instruments used which may partially explain contrasting results. A large cross-sectional study with retrospective assessment of the exposure using the data from the UK biobank cohort found that breastfeeding is associated with a lower risk of depression development later in life. The major limitation of this study was related to collection of the data on breastfeeding with participants been asked of whether they were breastfed in their infancy [ 47 ]. Such data, based on individuals’ memories in their adulthood, is associated with a substantial risk of recall bias.
Three studies of varied methodologies and potential bias investigated the relationship between breastfeeding and anxiety disorders. The studies used different assessment tools and focused on various forms of anxiety disorders. De Mola et al. cohort study found no correlation between breastfeeding (or its duration) and the development of anxiety disorders [ 45 ]. In contrast, the case–control study by Orengul et al. found a decreased risk of anxiety disorders in children who were breastfed as opposed to those who were not [ 31 ]. In another cross-sectional study using data from the UK Biobank cohort, Liu et al. discovered an association between breastfeeding and reduced anxiety, irrespective of whether the mothers smoked during pregnancy or not [ 47 ], but study design was prone to substantial risk of bias described in a previous paragraph.
Very limited data are available regarding breastfeeding associations with eating disorders and borderline personality disorders. Iron-Segev and co-authors analysed data from the large prospective cohort study of children who are the offspring of female registered nurses participating in the Nurses’ Health Study II (NHS II) and found no associations between breastfeeding and eating disorders. Participant enrolment in the study at the child’s age of at least 9 years, lack of the data regarding infancy and childhood factors are among the primary limitations of this study. The selected sample represents nurses, predominantly white, from a middle and high socioeconomic status, which limit generalisability of the results. One small case–control study showed association between lack of breastfeeding exposure and development of borderline personality disorder development later in life. Reported confidence intervals were very wide and reflect small sample size which restricts extrapolation of these results to other populations.
A recent systematic review found an association between breastfeeding and a reduced risk of postpartum depression [ 22 ], but it is unclear if this effect persists beyond the first few months of a child’s life. Our review identified only three studies that examined the long-term effects of breastfeeding on maternal mental health. These studies were all cohort studies and used different methods to assess breastfeeding exposure and examined a range of mental health disorders. One large cohort study from Australia found that never breastfeeding was associated with a higher risk of hospitalisation for schizophrenia, bipolar affective disorders and substance-induced mental illness in the first year postpartum compared to women who breastfed their children [ 46 ]. Two other studies focused on breastfeeding duration. A small study from the USA found that women who breastfed more frequently at 3 months postpartum experienced a greater decline in depressive symptoms over time [ 39 ]. However, it is unclear if the sample size was sufficient for the analyses used and the study had limitations, including the use of self-report measures and a predominantly white, upper-middle class and married sample. A study in South Korea found that a longer cumulative duration of breastfeeding was associated with a decreased risk of postmenopausal depression [ 35 ]. However, this study also had limitations, including self-report measures. There is an apparent lack of understanding about the potential association between breastfeeding and long-term maternal mental health. There is a need for more high-quality research to examine the potential association between breastfeeding and long-term maternal mental health. This research should use rigorous methods to assess breastfeeding exposure and control for potential confounders, as well as examine a range of mental health outcomes. Additionally, research should consider the potential moderating factors that may influence the relationship between breastfeeding and maternal mental health, such as individual characteristics, social support and parenting stress.
The GRADE certainty of evidence for all the studied outcomes was very low. This means that there is a high degree of uncertainty about the results, and more high-quality research is needed to confirm these findings. Primary factors that can contribute to a very low GRADE certainty of evidence include risk of bias, serious imprecision, serious inconsistency and indirectness. The very low GRADE certainty suggests that there is a high degree of uncertainty about the results, and more research is needed to confirm these findings.
Limitations
While the current evidence suggests that there is very weak or no association between breastfeeding and the development of mental health disorders, the review has several limitations that should be considered. First, there is a limited availability of high-quality studies that can provide conclusive evidence of the association between breastfeeding and mental health disorders. The current evidence base is primarily based on observational studies, which are subject to a higher risk of bias and confounding factors than randomised controlled trials. Additionally, there is heterogeneity in the study designs and outcomes, making it difficult to compare results across studies. Second, the studies included in this review may be subject to potential biases and confounding factors, such as recall bias or unmeasured confounding variables that were not accounted for in the studies. The studies may also have limitations in the way they assessed and reported breastfeeding exposure. It is also worth noting that the studies included may not be representative of all populations or settings, as the majority of the studies included predominantly white, middle and high socio-economic status individuals. Third, there is a lack of consistent evidence for some mental health outcomes, such as eating disorders and borderline personality disorder. There is also limited evidence available regarding the long-term effects of breastfeeding on maternal mental health. The GRADE certainty of evidence for all the studied outcomes was very low, indicating a high degree of uncertainty about the results and a need for more high-quality research to confirm these findings. Fourth, potential gaps may be associated with our exclusive focus on Medline and Embase databases, without incorporating insights from other relevant databases such as Scopus, CINHAL and PsycINFO, which might offer a broader perspective from allied health and social sciences. Abovementioned limitations should be carefully considered when interpreting the results presented in this manuscript.
Potential directions for future research
Future work in the field may focus on the standardisation of definitions of breastfeeding and the use of consistent, validated tools for the assessment of mental health outcomes. Ideally, future research should consider prioritising cohort studies with larger sample sizes and longer, more regular, follow-up periods, to better understand the long-term implications of breastfeeding on mental health. As most studies lack comprehensive data pertaining to infant exposure to colostrum, and the definition of breastfeeding is frequently imprecise or unclear, there is an area for improvement. Consideration of potential confounding factors, such as family history of mental health disorders, is also crucial to ensure the validity of the findings, as lack of control for confounders was apparent in some of the published research.
Further research is particularly needed in relation to less frequently investigated mental health disorders, as well as in relation to maternal mental health outcomes. There is also a need for more diverse research populations, as most of existing studies were conducted in European and Australasian regions, potentially limiting the generalisability of the findings. Although very costly, development of international consortia focused on prospective, register-oriented data collection could improve the knowledge in the field. A policy-driven, comprehensive data registry for breastfeeding and associated health outcomes could be instrumental for future research.
Despite limited evidence, potential benefits of breastfeeding on the mental health outcomes of both mother and child are apparent due to other known benefits. More efforts should be made that policies should promote and support breastfeeding practices, incorporating robust postpartum mental health screenings and targeted assistance programs for mothers.
There is a lack of consistent evidence to support a relationship between breastfeeding and mental health outcomes in mothers and children. Some studies have found statistically significant associations between breastfeeding and mental health, while others have found no such associations. The quality and methods of these studies are inconsistent, making it difficult to draw conclusions about the relationship between breastfeeding and mental health. Further research is necessary to fully understand any potential associations and potential underlying mechanisms. While breastfeeding may have various benefits for both mothers and children, more research is needed to determine whether it can protect against the development of mental health disorders in both parties.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author, DM, upon reasonable request.
Abbreviations
American Academy of Pediatrics
Attention deficit hyperactivity disorders
Adjusted odds ratio
Autism spectrum disorders
Beck’s Depression Inventory
Borderline personality disorder
Child Behaviour Check List
Diagnostic and Statistical Manual of Mental Disorders
European Commission for Public Health
Edinburgh Postnatal Depression Scale
Grading of Recommendations, Assessment and Evaluation
Growing Up Today Study
International Classification of Diseases
Schedule for Affective Disorders and Schizophrenia for School-Age Children
Long-chain polyunsaturated fatty acids
Medical subject headings
Mini International Neuropsychiatric Interview for Children and Adolescents
Newcastle-Ottawa Scale
Pre-/Postnatal Stress Questionnaire
Patient Health Questionnaire-9
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Revised Child Anxiety and Depression Scale
Randomised controlled trial
Risk Of Bias In Non-randomised Studies—of Interventions
United Kingdom
World Health Organization
Youth Self Report
Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications a systematic review and meta-analysis. JAMA Psychiat. 2015;72(4):334–41.
Article Google Scholar
Mental GBD, Collaborators D. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9(2):137–50. https://doi.org/10.1016/S2215-0366(21)00395-3 .
James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392(10159):1789–858.
Santomauro DF, Mantilla Herrera AM, Shadid J, Zheng P, Ashbaugh C, Pigott DM, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700–12.
Sickel AE, Seacat JD, Nabors NA. Mental health stigma update: a review of consequences. Adv Ment Heal. 2014;12(3):202–15.
Das J, Do QT, Friedman J, McKenzie D, Scott K. Mental health and poverty in developing countries: revisiting the relationship. Soc Sci Med. 2007;65(3):467–80.
Article PubMed Google Scholar
Solmi M, Radua J, Olivola M, Croce E, Soardo L, Salazar de Pablo G, et al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry. 2022;27(1):281–95.
Article CAS PubMed Google Scholar
Moreno JL, Kurita M, Holloway T, López J, Cadagan R, Martínez-Sobrido L, et al. Maternal influenza viral infection causes schizophrenia-like alterations of 5-HT2Aand mGlu2 receptors in the adult offspring. J Neurosci. 2011;31(5):1863–72.
Article CAS PubMed PubMed Central Google Scholar
WHO. Protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services . World Health OrganizationWHO. 2017. p. 1–136. Available from: https://apps.who.int/iris/bitstream/handle/10665/259386/9789241550086-eng.pdf .
Cattaneo A, Yngve A, Koletzko B, Guzman LR. Protection, promotion and support of breastfeeding in Europe. Public Health Nutr. 2005;8(1):39–46.
Meek JY, Noble L. Policy statement: breastfeeding and the use of human milk. Pediatrics. 2022;150(1):1–15.
Google Scholar
Bar S, Milanaik R, Adesman A. Long-term neurodevelopmental benefits of breastfeeding. Curr Opin Pediatr. 2016;4:559.
Turner S, Mayumi Maruyama J, Matijasevich A, Pastor-Valero M. Breastfeeding and the development of socio-emotional competencies: a systematic review. Breastfeed Med. 2019;14(10):691–704.
Krol KM, Grossmann T. Psychological effects of breastfeeding on children and mothers. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2018;61:977.
Article PubMed PubMed Central Google Scholar
Devlin AM, Chau CMY, Dyer R, Matheson J, McCarthy D, Yurko-Mauro K, et al. Developmental outcomes at 24 months of age in toddlers supplemented with arachidonic acid and docosahexaenoic acid: results of a double blind randomized, controlled trial. Nutrients. 2017;9:975.
Lassek WD, Gaulin SJC. Maternal milk DHA content predicts cognitive performance in a sample of 28 nations. Matern Child Nutr. 2015;11:773.
Linde K, Lehnig F, Nagl M, Kersting A. The association between breastfeeding and attachment: a systematic review. Midwifery. 2020;81:102592. https://doi.org/10.1016/j.midw.2019.102592 .
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, The PRISMA, et al. statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021:372.
Tseng PT, Yen CF, Chen YW, Stubbs B, Carvalho AF, Whiteley P, et al. Maternal breastfeeding and attention-deficit/hyperactivity disorder in children: a meta-analysis. Eur Child Adolesc Psychiatry. 2019;28(1):19–30. https://doi.org/10.1007/s00787-018-1182-4 .
Tseng PT, Chen YW, Stubbs B, Carvalho AF, Whiteley P, Tang CH, et al. Maternal breastfeeding and autism spectrum disorder in children: a systematic review and meta-analysis. Nutr Neurosci. 2019;22(5):354–62. https://doi.org/10.1080/1028415X.2017.1388598 .
Singh GK, Kenney MK, Ghandour RM, Kogan MD, Lu MC. Mental health outcomes in US children and adolescents born prematurely or with low birthweight. Depress Res Treat. 2013;2013:7–18.
Alimi R, Azmoude E, Moradi M, Zamani M. The association of breastfeeding with a reduced risk of postpartum depression: a systematic review and meta-analysis. Breastfeed Med. 2022;17(4):290–6. https://doi.org/10.1089/bfm.2021.0183 .
GA Wells, B Shea, D O’Connell, J Peterson, V Welch, M Losos PT. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available from: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp .
Zhang Y, Huang L, Wang D, Ren P, Hong Q, Kang D. The ROBINS-I and the NOS had similar reliability but differed in applicability: a random sampling observational studies of systematic reviews/meta-analysis. J Evid Based Med. 2021;14(2):112–22.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJGWG. GrADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6.
Morche J, Freitag S, Hoffmann F, Rissling O, Langer G, Nußbaumer-Streit B, et al. GRADE guidelines: 18. How ROBINS-I and other tools to assess risk of bias in nonrandomized studies should be used to rate the certainty of a body of evidence. Z Evid Fortbild Qual Gesundhwes. 2020;150–152:124–33.
Schwarze CE, Hellhammer DH, Stroehle V, Lieb K, Mobascher A. Lack of Breastfeeding: A Potential Risk Factor in the Multifactorial Genesis of Borderline Personality Disorder and Impaired Maternal Bonding. J Pers Disord. 2015;29(5):610–26. https://doi.org/10.1521/pedi_2014_28_160 .
Hartong M, Oosthuizen P, Emsley R. Longer duration of breastfeeding associated with risk of developing schizophrenia. S Afr J Psychiatry. 2007;13(2):4. https://doi.org/10.4102/sajpsychiatry.v13i2.30 .
Sasaki T, Okazaki Y, Akaho R, Masui K, Harada S, Lee I, et al. Type of feeding during infancy and later development of schizophrenia. Schizophr Res. 2000;42(1):79–82. https://doi.org/10.1016/s0920-9964(99)00102-4 .
Amore M, Balista C, McCreadie RG, Cimmino C, Pisani F, Bevilacqua G, Ferrari G. Can breast-feeding protect against schizophrenia? Case-control Study. Biol Neonate. 2003;83(2):97–101. https://doi.org/10.1159/000067960 .
Orengul AC, Tarakcioglu MC, Gormez V, Akkoyun S, Zorlu A, Aliyeva N, et al. Duration of Breastfeeding, Bottle-Feeding, and Parafunctional Oral Habits in Relation to Anxiety Disorders Among Children. Breastfeed Med. 2019;14(1):57–62. https://doi.org/10.1089/bfm.2018.0013 .
Leask SJ, Done DJ, Crow TJ, Richards M, Jones PB. No association between breast-feeding and adult psychosis in two national birth cohorts. Br J Psychiatry. 2000;177:218–21. https://doi.org/10.1192/bjp.177.3.218 .
Zhong BL, Ding J, Chen HH, Li Y, Xu HM, Tong J, et al. Depressive disorders among children in the transforming China: an epidemiological survey of prevalence, correlates, and service use. Depress Anxiety. 2013;30(9):881–92. https://doi.org/10.1002/da.22109 .
Huang T, Yue Y, Wang H, Zheng J, Chen Z, Chen T, et al. Infant Breastfeeding and Behavioral Disorders in School-Age Children. Breastfeed Med. 2019;14(2):115–20. https://doi.org/10.1089/bfm.2018.0151 .
Park S, Choi NK. Breastfeeding reduces risk of depression later in life in the postmenopausal period: A Korean population-based study. J Affect Disord. 2019;248:13–7. https://doi.org/10.1016/j.jad.2018.12.081 .
Allen NB, Lewinsohn PM, Seeley JR. Prenatal and perinatal influences on risk for psychopathology in childhood and adolescence. Dev Psychopathol. 1998;10(3):513–29. https://doi.org/10.1017/s0954579498001722 .
McCreadie RG. The Nithsdale Schizophrenia Surveys. 16. Breast-feeding and schizophrenia: preliminary results and hypotheses. Br J Psychiatry. 1997;170:334–7. https://doi.org/10.1192/bjp.170.4.334 .
Sørensen HJ, Mortensen EL, Reinisch JM, Mednick SA. Breastfeeding and risk of schizophrenia in the Copenhagen Perinatal Cohort. Acta Psychiatr Scand. 2005;112(1):26–9. https://doi.org/10.1111/j.1600-0447.2005.00548.x .
Hahn-Holbrook J, Haselton MG, Dunkel Schetter C, Glynn LM. Does breastfeeding offer protection against maternal depressive symptomatology?: A prospective study from pregnancy to 2 years after birth. Arch Womens Ment Health. 2013;16(5):411–22. https://doi.org/10.1007/s00737-013-0348-9 .
Kwok MK, Leung GM, Schooling CM. Breast feeding and early adolescent behaviour, self-esteem and depression: Hong Kong's 'Children of 1997' birth cohort. Arch Dis Child. 2013;98(11):887–94. https://doi.org/10.1136/archdischild-2013-304250 .
Hayatbakhsh MR, O'Callaghan MJ, Bor W, Williams GM, Najman JM. Association of breastfeeding and adolescents' psychopathology: a large prospective study. Breastfeed Med. 2012;7(6):480–6. https://doi.org/10.1089/bfm.2011.0136 .
Iron-Segev S, Peterson KE, Gillman MW, Williams CM, Austin SB, Field AE. Associations of breastfeeding with bulimic behaviors and eating disorders among adolescents. Int J Eat Disord. 2013;46(8):834–40. https://doi.org/10.1002/eat.22165 .
Oddy WH, Kendall GE, Li J, Jacoby P, Robinson M, de Klerk NH, et al. The long-term effects of breastfeeding on child and adolescent mental health: a pregnancy cohort study followed for 14 years. J Pediatr. 2010;156(4):568–74. https://doi.org/10.1016/j.jpeds.2009.10.020 .
Delgado CA, Munhoz TN, Santos IS, Barros FC, Matijasevich A. Prolonged breastfeeding for 24 months or more and mental health at 6 years of age: evidence from the 2004 Pelotas Birth Cohort Study, Brazil. Child Adolesc Ment Health. 2017;22(4):209–15. https://doi.org/10.1111/camh.12224 .
Loret de Mola C, Horta BL, Gonçalves H, Quevedo Lde A, Pinheiro R, Gigante DP, et al. Breastfeeding and mental health in adulthood: A birth cohort study in Brazil. J Affect Disord. 2016;202:115–9. https://doi.org/10.1016/j.jad.2016.05.055 .
Xu F, Li Z, Binns C, Bonello M, Austin MP, Sullivan E. Does infant feeding method impact on maternal mental health? Breastfeed Med. 2014;9(4):215–21. https://doi.org/10.1089/bfm.2013.0142 .
Liu L, Cheng S, Wen Y, Jia Y, Cheng B, Meng P, et al. Maternal smoking around birth may lower the protective effects of breastfeeding on anxiety, depression and neuroticism in adult offspring: a UK biobank study. Eur Arch Psychiatry Clin Neurosci. 2023;273(2):481–92. https://doi.org/10.1007/s00406-022-01477-7 .
Download references
Acknowledgements
Not applicable.
This study received no external funding.
Author information
Polina Bugaeva, Inna Arkusha, and Rinat Bikaev contributed equally to this work.
Authors and Affiliations
Charité – Universitätsmedizin Berlin, Einstein Center for Neurosciences, Berlin, Germany
Polina Bugaeva
V. Serbsky Federal Medical Research Center for Psychiatry and Narcology of the Ministry of Health of the Russian Federation, Moscow, Russia
Inna Arkusha & Alla Avedisova
Moscow Research and Clinical Centre for Neuropsychiatry, Moscow, Russia
Inna Arkusha, Rinat Bikaev, Mikhail Zinchuk, Renat Akzhigitov & Alla Guekht
Moscow City Clinical Hospital After V.M. Buyanov, Moscow, Russia
Igor Kamenskiy
Department of Brain Sciences, Faculty of Medicine, Dementia Research Institute UK, Imperial College London, London, UK
Aleksandra Pokrovskaya
Endocrinology Research Centre, Moscow, Russia
Yasmin El-Taravi
Stroke Unit, Santa Maria Della Misericordia Hospital, University of Perugia, Perugia, Italy
Valeria Caso
Division of Clinical Immunology & Allergy, Department of Medicine, and Department of Health Research Methods, Evidence & Impact, McMaster University, Hamilton, Canada
Derek K. Chu
Department of Pediatrics, Pediatric Epidemiology, Medical Faculty, Leipzig University, Leipzig, Germany
Jon Genuneit
German Center for Child and Youth Health, Leipzig, Germany
Department of Pediatrics, Paracelsus Medical University, Klinikum Nürnberg, Universitätsklinik Der Paracelsus Medizinischen Privatuniversität Nürnberg, Nuremberg, Germany
Gabriel Torbahn
Department of Pediatrics, Paracelsus Medical University, Salzburg, Austria
Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, UK
Timothy R. Nicholson
Department of Paediatrics and Paediatric Infectious Diseases, Institute of Child’s Health, I.M. Sechenov First Moscow State Medical University, Sechenov University, Moscow, Russia
Dina Baimukhambetova, Aigun Mursalova, Anastasia Kolotilina, Svetlana Gadetskaya & Elena Kondrikova
National Heart and Lung Institute, Imperial College London, London, UK
Robert J. Boyle & Daniel Munblit
Care for Long Term Conditions Division, Florence Nightingale Faculty of Nursing, Midwifery and Palliative Care, King’s College London, London, UK
Daniel Munblit
I.M. Sechenov First Moscow State Medical University, Sechenov University, Moscow, Russia
Department of Infectious Disease, Faculty of Medicine, Imperial College London, London, United Kingdom
You can also search for this author in PubMed Google Scholar
Contributions
PB, IA and RB contributed to the work equally and should be regarded as co-first authors. DM and RJB contributed to the work equally and should be regarded as co-last authors. PB: data curation, methodology, writing—original draft preparation, writing—reviewing and editing. IA: data curation, methodology, writing—reviewing and editing. RB: data curation, methodology, writing—reviewing and editing. IK: data curation, methodology, writing—reviewing and editing. AP: data curation, writing—reviewing and editing. YET: data curation, writing—reviewing and editing. VC: conceptualisation, writing—reviewing and editing. AA: conceptualisation, writing—reviewing and editing. DKC: methodology, writing—reviewing and editing. JG: methodology, writing—reviewing and editing. GT: methodology, writing—reviewing and editing. TN: methodology, writing—reviewing and editing. DB: data curation, writing—reviewing and editing. AM: data curation, writing—reviewing and editing. AK: writing—reviewing and editing. SG: writing—reviewing and editing. EK: writing—reviewing and editing. MZ: conceptualisation, methodology, writing—reviewing and editing. RA: conceptualisation, writing—reviewing and editing. RJB: methodology, writing—reviewing and editing. AG: conceptualisation, methodology, writing—reviewing and editing. DM: conceptualisation; data curation; formal analysis; methodology; project administration; writing-original draft; writing-review and editing. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Robert J. Boyle or Daniel Munblit .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was not required for this study as it is a systematic review of previously published literature.
Consent for publication
Competing interests.
The authors declare no support from any organisation for the submitted work. Outside of the submitted work, JG benefit from unrestricted research grants from Danone Nutricia Research to Leipzig University for research into human milk composition within the Ulm Birth Cohort Studies—this work is not related to the present publication; author RJB declares consultancy payment from Cochrane, Wiley and the British Society for Allergy and Clinical Immunology for editorial work and payment for expert witness work in cases involving food anaphylaxis and a disputed infant formula health claim.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: box s1..
Search strategies. Table S1. Newcastle Ottawa Scale (NOS) scoring for the cohort studies. Table S2. Newcastle Ottawa Scale (NOS) scoring for the case-control studies. Table S3. Newcastle Ottawa Scale (NOS) scoring for cross-sectional studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Bugaeva, P., Arkusha, I., Bikaev, R. et al. Association of breastfeeding with mental disorders in mother and child: a systematic review and meta-analysis. BMC Med 21 , 393 (2023). https://doi.org/10.1186/s12916-023-03071-7
Download citation
Received : 07 March 2023
Accepted : 06 September 2023
Published : 16 October 2023
DOI : https://doi.org/10.1186/s12916-023-03071-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breastfeeding
- Child health
- Maternal health
- Mental health
- Systematic review
BMC Medicine
ISSN: 1741-7015
- Submission enquiries: [email protected]
- General enquiries: [email protected]

The Comprehensive Guide to Moscow Nightlife
- Posted on April 14, 2018 July 26, 2018
- by Kings of Russia
- 8 minute read

Moscow’s nightlife scene is thriving, and arguably one of the best the world has to offer – top-notch Russian women, coupled with a never-ending list of venues, Moscow has a little bit of something for everyone’s taste. Moscow nightlife is not for the faint of heart – and if you’re coming, you better be ready to go Friday and Saturday night into the early morning.
This comprehensive guide to Moscow nightlife will run you through the nuts and bolts of all you need to know about Moscow’s nightclubs and give you a solid blueprint to operate with during your time in Moscow.
What you need to know before hitting Moscow nightclubs
Prices in moscow nightlife.
Before you head out and start gaming all the sexy Moscow girls , we have to talk money first. Bring plenty because in Moscow you can never bring a big enough bankroll. Remember, you’re the man so making a fuzz of not paying a drink here or there will not go down well.
Luckily most Moscow clubs don’t do cover fees. Some electro clubs will charge 15-20$, depending on their lineup. There’s the odd club with a minimum spend of 20-30$, which you’ll drop on drinks easily. By and large, you can scope out the venues for free, which is a big plus.
Bottle service is a great deal in Moscow. At top-tier clubs, it starts at 1,000$. That’ll go a long way with premium vodka at 250$, especially if you have three or four guys chipping in. Not to mention that it’s a massive status boost for getting girls, especially at high-end clubs.
Without bottle service, you should estimate a budget of 100-150$ per night. That is if you drink a lot and hit the top clubs with the hottest girls. Scale down for less alcohol and more basic places.
Dress code & Face control
Door policy in Moscow is called “face control” and it’s always the guy behind the two gorillas that gives the green light if you’re in or out.
In Moscow nightlife there’s only one rule when it comes to dress codes:
You can never be underdressed.
People dress A LOT sharper than, say, in the US and that goes for both sexes. For high-end clubs, you definitely want to roll with a sharp blazer and a pocket square, not to mention dress shoes in tip-top condition. Those are the minimum requirements to level the playing field vis a vis with other sharply dressed guys that have a lot more money than you do. Unless you plan to hit explicit electro or underground clubs, which have their own dress code, you are always on the money with that style.
Getting in a Moscow club isn’t as hard as it seems: dress sharp, speak English at the door and look like you’re in the mood to spend all that money that you supposedly have (even if you don’t). That will open almost any door in Moscow’s nightlife for you.
Types of Moscow Nightclubs
In Moscow there are four types of clubs with the accompanying female clientele:
High-end clubs:
These are often crossovers between restaurants and clubs with lots of tables and very little space to dance. Heavy accent on bottle service most of the time but you can work the room from the bar as well. The hottest and most expensive girls in Moscow go there. Bring deep pockets and lots of self-confidence and you have a shot at swooping them.
Regular Mid-level clubs:
They probably resemble more what you’re used to in a nightclub: big dancefloors, stages and more space to roam around. Bottle service will make you stand out more but you can also do well without. You can find all types of girls but most will be in the 6-8 range. Your targets should always be the girls drinking and ideally in pairs. It’s impossible not to swoop if your game is at least half-decent.
Basic clubs/dive bars:
Usually spots with very cheap booze and lax face control. If you’re dressed too sharp and speak no Russian, you might attract the wrong type of attention so be vigilant. If you know the local scene you can swoop 6s and 7s almost at will. Usually students and girls from the suburbs.
Electro/underground clubs:
Home of the hipsters and creatives. Parties there don’t mean meeting girls and getting drunk but doing pills and spacing out to the music. Lots of attractive hipster girls if that is your niche. That is its own scene with a different dress code as well.

What time to go out in Moscow
Moscow nightlife starts late. Don’t show up at bars and preparty spots before 11pm because you’ll feel fairly alone. Peak time is between 1am and 3am. That is also the time of Moscow nightlife’s biggest nuisance: concerts by artists you won’t know and who only distract your girls from drinking and being gamed. From 4am to 6am the regular clubs are emptying out but plenty of people, women included, still hit up one of the many afterparty clubs. Those last till well past 10am.
As far as days go: Fridays and Saturdays are peak days. Thursday is an OK day, all other days are fairly weak and you have to know the right venues.
The Ultimate Moscow Nightclub List
Short disclaimer: I didn’t add basic and electro clubs since you’re coming for the girls, not for the music. This list will give you more options than you’ll be able to handle on a weekend.
Preparty – start here at 11PM
Classic restaurant club with lots of tables and a smallish bar and dancefloor. Come here between 11pm and 12am when the concert is over and they start with the actual party. Even early in the night tons of sexy women here, who lean slightly older (25 and up).
The second floor of the Ugolek restaurant is an extra bar with dim lights and house music tunes. Very small and cozy with a slight hipster vibe but generally draws plenty of attractive women too. A bit slower vibe than Valenok.
Very cool, spread-out venue that has a modern library theme. Not always full with people but when it is, it’s brimming with top-tier women. Slow vibe here and better for grabbing contacts and moving on.

High-end: err on the side of being too early rather than too late because of face control.
Secret Room
Probably the top venue at the moment in Moscow . Very small but wildly popular club, which is crammed with tables but always packed. They do parties on Thursdays and Sundays as well. This club has a hip-hop/high-end theme, meaning most girls are gold diggers, IG models, and tattooed hip hop chicks. Very unfavorable logistics because there is almost no room no move inside the club but the party vibe makes it worth it. Strict face control.
Close to Secret Room and with a much more favorable and spacious three-part layout. This place attracts very hot women but also lots of ball busters and fakes that will leave you blue-balled. Come early because after 4am it starts getting empty fast. Electronic music.
A slightly kitsch restaurant club that plays Russian pop and is full of gold diggers, semi-pros, and men from the Caucasus republics. Thursday is the strongest night but that dynamic might be changing since Secret Room opened its doors. You can swoop here but it will be a struggle.

Mid-level: your sweet spot in terms of ease and attractiveness of girls for an average budget.
Started going downwards in 2018 due to lax face control and this might get even worse with the World Cup. In terms of layout one of the best Moscow nightclubs because it’s very big and bottle service gives you a good edge here. Still attracts lots of cute girls with loose morals but plenty of provincial girls (and guys) as well. Swooping is fairly easy here.
I haven’t been at this place in over a year, ever since it started becoming ground zero for drunken teenagers. Similar clientele to Icon but less chic, younger and drunker. Decent mainstream music that attracts plenty of tourists. Girls are easy here as well.
Sort of a Coyote Ugly (the real one in Moscow sucks) with party music and lots of drunken people licking each others’ faces. Very entertaining with the right amount of alcohol and very easy to pull in there. Don’t think about staying sober in here, you’ll hate it.
Artel Bessonitsa/Shakti Terrace
Electronic music club that is sort of a high-end place with an underground clientele and located between the teenager clubs Icon and Gipsy. Very good music but a bit all over the place with their vibe and their branding. You can swoop almost any type of girl here from high-heeled beauty to coked-up hipsters, provided they’re not too sober.
Afterparty: if by 5AM you haven’t pulled, it’s time to move here.
Best afterparty spot in terms of trying to get girls. Pretty much no one is sober in there and savage gorilla game goes a long way. Lots of very hot and slutty-looking girls but it can be hard to tell apart who is looking for dick and who is just on drugs but not interested. If by 9-10am you haven’t pulled, it is probably better to surrender.
The hipster alternative for afterparties, where even more drugs are in play. Plenty of attractive girls there but you have to know how to work this type of club. A nicer atmosphere and better music but if you’re desperate to pull, you’ll probably go to Miks.
Weekday jokers: if you’re on the hunt for some sexy Russian girls during the week, here are two tips to make your life easier.
Chesterfield
Ladies night on Wednesdays means this place gets pretty packed with smashed teenagers and 6s and 7s. Don’t pull out the three-piece suit in here because it’s a “simpler” crowd. Definitely your best shot on Wednesdays.
If you haven’t pulled at Chesterfield, you can throw a Hail Mary and hit up Garage’s Black Music Wednesdays. Fills up really late but there are some cute Black Music groupies in here. Very small club. Thursday through Saturday they do afterparties and you have an excellent shot and swooping girls that are probably high.
Shishas Sferum
This is pretty much your only shot on Mondays and Tuesdays because they offer free or almost free drinks for women. A fairly low-class club where you should watch your drinks. As always the case in Moscow, there will be cute girls here on any day of the week but it’s nowhere near as good as on the weekend.

In a nutshell, that is all you need to know about where to meet Moscow girls in nightlife. There are tons of options, and it all depends on what best fits your style, based on the type of girls that you’re looking for.
Related Topics
- moscow girls
- moscow nightlife

The Top 3 Cities in Ukraine for First Timers
- Posted on July 7, 2018 August 4, 2019
You May Also Like

- Uncategorized
The Best Expat Blogs for Moscow
- Posted on May 31, 2020 June 1, 2020

Finding a Russian Bride: How and Where to Meet Her
- Posted on August 9, 2019 August 9, 2019

Meeting Women in Moscow: Dating Perspectives on the World’s Most Beautiful Women
- Posted on August 5, 2019 August 9, 2019

Meeting Russian Women: Top 5 Locations
- Posted on August 3, 2019 June 1, 2020
Moscow vs St. Petersburg – Which One to Visit?
- Posted on July 31, 2019 August 3, 2019

Hot Russian Girls – Where to Find & Date Them
- Posted on March 30, 2019 March 30, 2019
A Guide to Teaching English in Russia
- Posted on August 11, 2018 October 9, 2019

How to Attract Russian Girls
- Posted on July 15, 2018 August 4, 2019
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Input your search keywords and press Enter.
Shooter Files by f.d. walker
Street Photography Tips, Interaction, Travel, Guides
Apr 24 2017
City Street Guides by f.d. walker: A Street Photography Guide to Moscow, Russia

*A series of guides on shooting Street Photography in cities around the world. Find the best spots to shoot, things to capture, street walks, street tips, safety concerns, and more for cities around the world. I have personally researched, explored and shot Street Photography in every city that I create a guide for. So you can be ready to capture the streets as soon as you step outside with your camera!
At over 12 million people, Moscow is the largest city in Russia and second largest in Europe by population ( Istanbul is #1). An urban, cosmopolitan metropolis with more than enough glitz and glam to cater to the elite, but without losing its fair share of Soviet era roughness around the edges. It can be fast paced, brash, busy, and trendy like other big cities, but it has its blend of West meets Russia atmosphere and beauty that provides plenty of unique interest. The Red Square is as famous as it gets, but there’s so much more to this city, including the most beautiful subway system you’ve ever seen. It would take years to capture all of Moscow, but that means you have an endless amount of areas to discover.

So here’s a Street Photography guide so you can be ready to capture all that Moscow has to offer before you even arrive!
- Patriarch’s Pond
- Old Arbat Street
- Maroseyka Street
- Tverskoy Boulevard
Top 5 Street Spots:
1. red square.
The Red Square is the most famous square in not just Russia, but all of Eastern Europe. The name actually doesn’t come from the color of the bricks or communism, but from the name in Russian, Krásnaya, once meaning “beautiful” before its meaning changed to “red.” This large plaza is what you see on the cover of guide books and magazines for Moscow, with St. Basil’s Cathedral being the center piece next to Lenin’s Mausoleum surrounded by the Kremlin Wall. Of course, the Red Square attracts hordes of tourist due to the main attractions, but all that activity around an interesting atmosphere does provide street photo opportunities. It’s also the central square connecting to the city’s major streets, providing a good starting point to explore outward.

You’ll also find the popular pedestrian only Nikolskaya Street connecting the Red Square to Lubyanka Square. This line of expensive shops includes plenty of activity, while also leading you to another popular square. Filled with history rivaling any city, the Red Square and surrounding areas are the heart and soul of Russia.

2. Patriarch’s Ponds
Patriarch’s Ponds is one of the most exclusive neighborhoods in Moscow. Despite the name being plural, there’s only one large pond, but it’s worth a visit with your camera. It’s a popular spot for locals and expats to come relax or take a stroll around the pond. You get an interesting mix of young and old too, from young love to “babushkas” feeding pigeons. It’s a very peaceful park atmosphere in one of the nicer areas within the city center, while bringing enough activity for street photography.

The pond is shallow and in the winter becomes a popular spot for ice-skating too. The area is also well-known for the location in the famous Russian novel, The Master and Margarita.
3. Old Arbat (Stary Arbat)
Old Arbat is the most famous pedestrian street in Moscow, and dating back to the 15th century, also one of its oldest. Originally, it was an area of trade, but soon became the most prestigious residential area in Moscow. During the 18th century, Arbat started attracting the city’s scholars and artists, including Alexander Pushkin. Cafes lined the streets and impressive homes filled the neighborhood. Since then, New Arbat street was created as a highway in the area, while Old Arbat was paved for a 1km pedestrian only walkway.

Due to the historic buildings, famous artists that lived here, and the bohemian atmosphere, Old Arbat has become a big attraction for tourists today. Now, there’s a mix of cafes, restaurants, souvenir shops, street performers, street merchants and other attractions for visitors, and some locals, to come enjoy. It can get really busy here and there’s usually something interesting going on so it’s a good street to come walk with your camera for guaranteed life.
4. Gorky Park
One of the most famous places in Moscow is Gorky Park. The official name is Maxim Gorky’s Central Park of Culture & Leisure, which gives you an idea of what goes on here. When built, it was the first of its kind in the Soviet Union. Divided into two parts, it stretches along Moscow River. One end contains fair rides, foods stands, tennis courts, a sports club, a lake for boat rides, and more. This end brings more active life due to its number of attractions, while the other end is more relaxed, where you’ll find gardens, trees, older buildings, and an outdoor amphitheater.

Gorky Park attracts mostly locals so it’s a good spot to capture the non-tourist side of Moscow life. Muscovites come here to escape the city and unwind in a picturesque setting. The park remains alive outside of the warmer months too, especially when the lake turns into the city’s largest outdoor skating rink. I’d recommend taking the metro out here to spend at least half a day exploring the massive park’s life with your camera.
5. Maroseyka Street
Maroseyka Street is a popular area not too far from the Red Square. The long, winding street turns into Pokrovka and is lined with restaurants, cafes, bars and places to stay. It’s actually where I like to stay when I’m in Moscow due to its location and solid street photography opportunities itself. You have Kitay-gorod station near and if you keep walking southwest, you’ll get to the Red Square. But if you walk northwest, as it changes to Pokrovka, you can find a long street of activity for photography with its own interesting atmosphere.

6. Tverskoy Boulevard
Tverskoy Boulevard is the oldest and longest boulevard in Moscow, beginning at the end of Nikitsky Boulevard, and finishing at Pushkin Square, a spot to come for activity itself. The boulevard is made up of two avenues, with pedestrian walkways in-between. You’ll find grass, shrubbery, trees, benches and more walking it’s almost kilometer length. Many people come here to enjoy some relaxation, walk their dog, or just to use it to walk wherever they’re going. Its center location also provides a nice place to walk with your camera near plenty of other spots you’ll want to check out anyway.
Sample Street Walk:
For a full day of Street Photography, covering some of the best spots, you can follow this sample street walk for Moscow:
- Start your morning walking around the Red Square (1), while exploring the surrounding area, including Nikolskaya Street
- Then walk northwest to Patriarch’s Ponds (2) and slowly walk the pond and surrounding area with your camera
- Next, walk east to the Pushkin Monument and stroll down Tverskoy Boulevard (6)
- Once Tverskoy Boulevard (6) ends, it will turn into Nikitsky Boulevard. Follow this down until you get to the start of Old Arbat Street (3), across from Arbatskaya station
- After you’re done walking down Old Arbat Street (3) for more street photography, spend some time checking out Moscow’s beautiful metro stations
- To finish off the day with more street photography, get off the metro near Red Square (1) again, Maroseyka Street (5) or wherever you’re staying for the night.

3 Things I’ll Remember about Shooting in Moscow:
1. museum metro.
The Moscow metro system was the first underground railway system in the Soviet Union and today includes 203 stations across 340km of routes. The elaborate system has some of the deepest stations in the world too, with escalators that seem to go on forever. None of this is what makes it so special, though. Many of its stations feel like stepping inside a museum, making it without a doubt the most interesting and beautiful metro system I’ve been in.

When built, Stalin wanted to make the metro stations “palaces for the people” with marble, chandeliers, and grand architecture. The best part is the variety of architecture and styles used, making many of the stations a completely different experience visually. You could easily spend a whole day traveling the stations and there are even tours available for people who wish to do just that. My advice, though, would be just to buy a ticket and hop on and off at different stations, while exploring different lines. The museum-like surrounding mixed with the crowds of characters can make for a great photography experience.

Since there are so many stations, here are some of my favorites to check out:
- Novoslobodskaya
- Mayakovskaya
- Elektrozavodskaya
- Komsomolskaya
- Ploschad Revolyutsii
- Dostoyevskaya
- Prospekt Mira

2. Moscow is Big
It’s no secret that Moscow is a big city, but it can feel even bigger with how spread out much of it is. This is especially true if you compare it to cities outside of Asia. If I compared it to cities in Europe, I’d probably say only Istanbul would warrant more time to really discover the depths of this city. Most only explore around the Red Square and surrounding area, but that is such a small part of the city. Although, that central area does give you plenty to see on its own.

Fortunately, I had a good friend living in the city to show me around, but it opened up my eyes even more to how much there is to discover in Moscow. It’s a big city with a variety of atmosphere that can take you from “east” to “west” and trendy to rugged depending on where you go. I’d imagine you’d have to live here a while to really know the city.
3. Cosmopolitan Mix of East meets West
Modern skyscrapers mixed with amazing architecture, a world-class metro system with museum-like beauty, trendy fashion and chic clubs, Moscow is a rich mix of Russian culture and history in a more western cosmopolitan package. There is a push to keep the Russian culture, while also pushing forward with a modern metropolis the whole world will envy. This comes with an impressive skyline, that continues to grow, and endless modernities, but with soviet nostalgia and atmosphere mixed in for good measure.

Mixed in with this grand western cosmopolitan atmosphere, is a strong national pride in Russia. This includes their famous leader, Vladimir Putin. Maybe no other place will you see a country’s leader more often. All over, from the pricey tourist shops to the underground walkway stalls, you’ll find goods with Putin’s likeness covering them. From t-shirts to magnets to Matryoshka dolls. There’s a strong national pride that can be seen around the city, which also extends to their leader. Moscow is many things. It’s East meets West, modernizations meets Soviet era, and a whole lot more.
What To Do For a Street Photography Break?:
Eat at a stolovaya.
Stolovayas are Russian cafeterias that became popular in the Soviet days. You grab a tray and walk down the line of freshly prepared local dishes, and select whatever you want from the chefs. They’re usually inexpensive and a much better value than restaurants, while giving you the opportunity to try from a wide selection of everyday Russian food. They’re also very tasty. I always include some borsch on my tray and go from there. The places themselves are all over Moscow and usually come with Soviet-era aesthetics to complete the experience.

Street Safety Score: 7
*As always, no place is completely safe! So when I talk about safety, I’m speaking in general comparison to other places. Always take precaution, be smart, observe your surroundings and trust your instincts anywhere you go!
Being the 2nd largest city in Europe with over 12 million people, you’re going to have your dangerous areas, but for the most part, it feels safe walking around. Russia is statistically higher in crime compared to most of Europe, but this generally doesn’t apply to tourists and visitors. Around the Red Square and surrounding city center, you should feel completely safe walking around. Pick pocketing can happen, but no more than other touristic places. I always explore Moscow freely without coming across too much to worry about. It’s a spread out city, though, so of course it matters where you are. Just use basic street smarts, know where you are and Moscow shouldn’t give you a problem.

People’s Reaction Score: 7
Moscow is fast paced, big city life, which usually means people aren’t too concerned with you, or your camera. I don’t find people notice or pay much attention to me when I’m out taking photos in Moscow. For the most part, people just go about their day. You shouldn’t get too many looks or concern. But it can depend on the area you are in. The more you stick out, the more you might get noticed with suspicions. I’ve never had any problems in Moscow, or Russia, but just be careful who you’re taking a photo of if you get out of the city center. Other than that, it’s about average for reactions.

Street Tips:
Learn the alphabet .
Much of Moscow, including the metro system, doesn’t use english. The Russian alphabet uses letters from the Cyrillic script, which if you aren’t familiar with it and don’t know the sounds, can be hard to decipher the words. This is most important for street names and metro stops when trying to get around. It can save confusion and make it easier getting around if you learn the basic alphabet. At the very least then, you can sound out the words to see which are similar in the english conversion, which can help matching them to maps. When out shooting street photography, getting around is as important as anything. So save yourself some time and frustration by learning the Russian Alphabet.

Use the metro
While Saint-Petersburg feels very walkable for a city its size, Moscow can feel very spread out, even for its bigger size. Outside of the Red Square area, you can have plenty of walking before getting anywhere very interesting, so you’ll need to take the metro a lot if you really want to explore the city. Maps are deceiving here too, it will always be further than it looks.

Another reason it’s less walkable than Saint-Petersburg is its completely different set-up. Moscow’s streets are mostly contstructed in rings with narrow, winding streets in-between. This is common with medieval city cities that used to be confined by walls, but you usually don’t have it in a city this massive. Saint-Petersburg has a more grid-like pattern that also uses the canals to help you know your way around. When it comes to navigating on foot in Moscow, it can be more difficult, so bring a map and take the metro when needed. It’s why Moscow’s metro carries more passengers per day than the London and Paris subways combined.
Explore other areas if you have time
Moscow is really big. While most people stay around the Red Square within the Boulevard Ring, there’s so much more to the city. I covered some other spots outside of this circle, but if you really want to see the city, you’ll need time. If you do have time, some other areas I’d check out first are Zamoskvarechye, along some of the south and western Moscow.

Inspiration:
For some more inspiration, you can look through the Street Photography of Moscow photographer Artem Zhitenev and check out 33 of my photos taken in Moscow .
Conclusion:
Moscow’s name brings a certain mystique, but once you’re there it might bring a different atmosphere than you expect. It’s big and sprawling, but beautiful in many ways. It can feel like a European capital on a grand scale, but you can definitely find its Russian side in there.

The urban sprawl of Moscow can be intimidating, but give it enough time and you’ll be rewarded with plenty to discover. All with the world’s best metro system to take you around.
I hope this guide can help you start to experience some of what Moscow contains. So grab your camera and capture all that Moscow has to offer for Street Photography!
If you still have any questions about shooting in Moscow, feel free to comment below or email me!
(I want to make these guides as valuable as possible for all of you so add any ideas on improvements, including addition requests, in the comment section!)
Click Here For More City Street Guides!
(A New Guide Posted Every Other Wednesday)

Comment Here! Cancel reply
For patreon exclusive educational content:.

Limited Edition Postcard Prints!
Street Photography Workshops
Donations Always Appreciated
I'll always keep Shooter Files free for everyone, but any donations would be greatly appreciated and help me keep it going. Many thanks to everyone following along!
Cheers! -f.d. walker
Search the Files

For Exclusive Patron Content:

IMAGES
COMMENTS
Single home visit in first 48 hours after discharge plus routine check up at hospital vs single hospital visit: ... Bashour 2008b compared four or one postnatal home visits from midwives versus no home visits following hospital discharge. Ransjo‐Arvidson 1998 compared four midwife home visits versus one midwife home visit. In these three ...
For babies born in a healthcare facility, the first home visit was recommended to be made as soon as possible after the mother and baby return home with remaining visits following the same schedule as for home births ... 1 postnatal home visit by registered midwives; on day 3. (3) Group C (n = 301):
The perception of being in control. The women felt that the home visit helped provide security and calm in a hectic postnatal period. Many of them told us that they looked forward to the midwife's visit. The women were aware of what the midwife could provide, and that the visit was voluntary and agreed beforehand.
2 1.1.4 Consider arranging the first postnatal health visitor home visit to take 3 place between 7 and 14 days after transfer of care from midwifery care so 4 that the timing of postnatal contacts is evenly spread out. 5 1.1.5 If a woman did not receive an antenatal health visitor visit, consider 6 arranging an additional early postnatal health ...
A children's doctor (paediatrician), midwife or newborn (neonatal) nurse will check your baby is well and will offer him or her a newborn physical examination within 72 hours of birth. In the early days, the midwife will check your baby for signs of: jaundice. infection of the umbilical cord or eyes. thrush in the mouth.
The services in the postnatal period have until recently consisted of a home visit from a public health nurse 7-14 days after birth. The care provided to the woman during pregnancy, birth and the postnatal period has been widely debated in Norway. The maternity care is fragmented and the women interact with several different midwives and other ...
Timely interventions in the postnatal period are important for reducing newborn mortality, and early home visits to provide postnatal care are recommended. There has been limited success in achieving timely visits, and a better understanding of the realities of programmes is needed if improvements are to be made. We explored barriers and facilitators to timely postnatal visits through 20 ...
In all but four of the included studies, postnatal care at home was delivered by healthcare professionals. ... In a cluster-RCT comparing usual care with individualised care by midwives, extended up to three months after the birth, there may be little or no difference in neonatal mortality (RR 0.97, 95% CI 0.85 to 1.12; one study, 696 infants). ...
Objective: The aim of the present study is to gain a deeper understanding of women's experiences of midwifery care in connection with home visits during the early postnatal period. Research design/setting: A qualitative approach was chosen for data collection, and the data presented are based on six focus group interviews (n: 24). The women were both primiparous and multiparous, aged 22-37 ...
The services in the postnatal period have until recently consisted of a home visit from a public health nurse 7-14 days after birth. The care provided to the woman during pregnancy, birth and the postnatal period has been widely debated in Norway. The maternity care is fragmented and the women interact with several different midwives and other ...
The first postnatal visit is the most critical visit undertaken by a public health nurse (PHN), community midwife or health visitor with a mother and her infant in the early postnatal period ...
1.1.14 Ensure that the first postnatal visit by a midwife takes place within 36 hours after transfer of care from the place of birth or after a home birth. The visit should be face-to-face and usually at the woman's home, depending on her circumstances and preferences.
This program is available to first-time parents under the age of 20. The programme includes home visits from a family nurse while you're pregnant, and after your baby's born. These visits help: to have a healthy pregnancy. you and your baby grow and develop together. you to be the best parent you can be.
The main theme explored, 'The home-based postnatal care model facilitated a smooth succession into motherhood', is explained by the themes: 1) Mothers felt 'not left adrift' when cared for by the home- based postnatal midwives; 2) Professional midwives with authority guided the way intoMotherhood; and 3) The home, a safe and secure space for new mothers.
1.1.4. When caring for a baby, remember that those with parental responsibility have the right be involved in the baby's care, if they choose. 1.1.5. When giving information about postnatal care, use clear language and tailor the timing, content and delivery of information to the woman's needs and preferences.
Background A fast adoption of a non-invasive prenatal testing (NIPT) in clinical practice is a global tendency last years. Firstly, in Russia according a new regulation it was possible to perform a widescale testing of pregnant women in chromosomal abnormality risk. The aim of the study—to assess efficiency of using NIPT as a second-line first trimester screening test in Moscow. Methods ...
Background Breastfeeding has long been associated with numerous benefits for both mothers and infants. While some observational studies have explored the relationship between breastfeeding and mental health outcomes in mothers and children, a systematic review of the available evidence is lacking. The purpose of this study is to systematically evaluate the association between breastfeeding and ...
Moscow nightlife starts late. Don't show up at bars and preparty spots before 11pm because you'll feel fairly alone. Peak time is between 1am and 3am. That is also the time of Moscow nightlife's biggest nuisance: concerts by artists you won't know and who only distract your girls from drinking and being gamed.
The Moscow metro system was the first underground railway system in the Soviet Union and today includes 203 stations across 340km of routes. The elaborate system has some of the deepest stations in the world too, with escalators that seem to go on forever. None of this is what makes it so special, though.