

Family Life

AAP Schedule of Well-Child Care Visits

Parents know who they should go to when their child is sick. But pediatrician visits are just as important for healthy children.
The Bright Futures /American Academy of Pediatrics (AAP) developed a set of comprehensive health guidelines for well-child care, known as the " periodicity schedule ." It is a schedule of screenings and assessments recommended at each well-child visit from infancy through adolescence.
Schedule of well-child visits
- The first week visit (3 to 5 days old)
- 1 month old
- 2 months old
- 4 months old
- 6 months old
- 9 months old
- 12 months old
- 15 months old
- 18 months old
- 2 years old (24 months)
- 2 ½ years old (30 months)
- 3 years old
- 4 years old
- 5 years old
- 6 years old
- 7 years old
- 8 years old
- 9 years old
- 10 years old
- 11 years old
- 12 years old
- 13 years old
- 14 years old
- 15 years old
- 16 years old
- 17 years old
- 18 years old
- 19 years old
- 20 years old
- 21 years old
The benefits of well-child visits
Prevention . Your child gets scheduled immunizations to prevent illness. You also can ask your pediatrician about nutrition and safety in the home and at school.
Tracking growth & development . See how much your child has grown in the time since your last visit, and talk with your doctor about your child's development. You can discuss your child's milestones, social behaviors and learning.
Raising any concerns . Make a list of topics you want to talk about with your child's pediatrician such as development, behavior, sleep, eating or getting along with other family members. Bring your top three to five questions or concerns with you to talk with your pediatrician at the start of the visit.
Team approach . Regular visits create strong, trustworthy relationships among pediatrician, parent and child. The AAP recommends well-child visits as a way for pediatricians and parents to serve the needs of children. This team approach helps develop optimal physical, mental and social health of a child.
More information
Back to School, Back to Doctor
Recommended Immunization Schedules
Milestones Matter: 10 to Watch for by Age 5
Your Child's Checkups
- Bright Futures/AAP Recommendations for Preventive Pediatric Health Care (periodicity schedule)

- Pharmacology
- Allergy, Immunology, and ENT
- Emergency Medicine
- Endocrinology
- Adolescent Medicine
- Gastroenterology
- Infectious Diseases
- Practice Improvement
- Respiratory
- Dermatology
- Mental, Behavioral and Development Health
- Rheumatology
- Sexual Health
2021 evaluation and management coding update
A new evaluation and management coding system for outpatient visits was implemented earlier this year. This article details the nuances of the new system.
Effective January 1 this year, the Centers for Medicare & Medicaid Services (CMS), with guidance from the American Medical Association (AMA), implemented a new evaluation and management (E/M) coding system for outpatient visits. The first change in 25 years, it was developed to ease the documentation burden on medical providers. This article details the nuances of the 2021 E/M coding system, to help keep office notes in compliance with the new guidelines.
Implications for medical practice
In order to comply with the pre-2021 coding guidelines, physicians were spending too much time writing bloated notes to justify the level of service billed; many were frequently completing their notes at home. This was just one of many factors contributing to physician burnout. Recognizing the burden that documentation was placing on medical providers, CMS launched their “Patients Over Paperwork” initiative in 2017, and finalized guidelines based on the 2020 AMA relative value scale (RVS) Update Committee (RUC) suggestions. A benefit of the updated guidelines is that pediatrician work relative value unit (wRVU) productivity will increase for well visit codes and acute visit codes. As a consequence, compensation will likely increase by as much as 9% for pediatricians whose pay is based predominantly on wRVU output. 1 On December 22, 2020, congress adjusted the Medicare Physician Fee Schedule (MPFS) conversion factor, a change that will likely improve 2021 pediatrician compensation further. 2
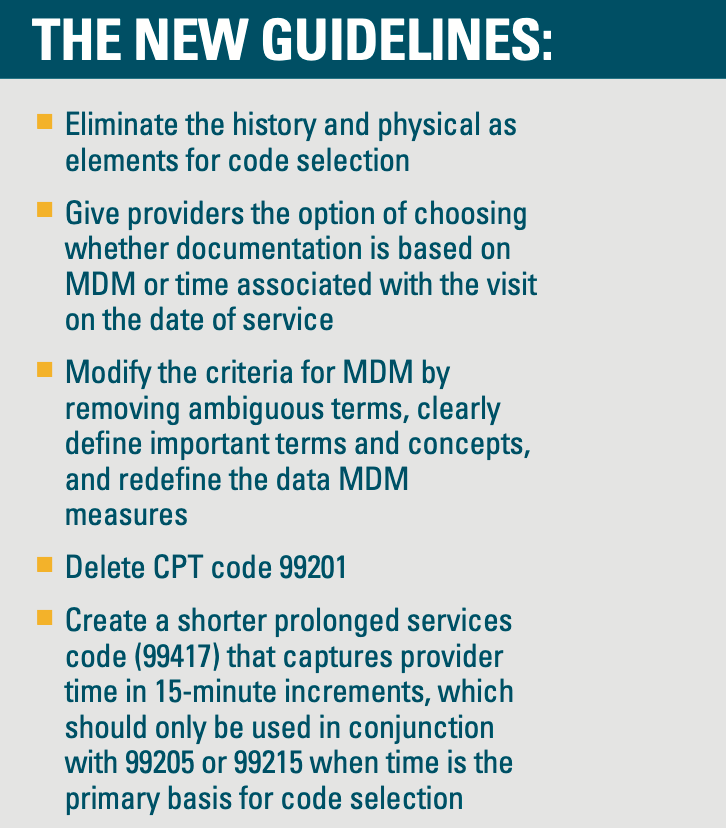
The new guidelines
Prior to 2021, billing for an outpatient visit required a very complicated mixture of documenting appropriate elements of the patient’s history and physical along with the medical decision-making (MDM) associated with the visit or time spent counseling patient or coordinating care. The updated CMS guidelines are based only on 1) a clearer method of assigning MDM or 2) a new methodology for assigning a time component to the visit on the date of service.
Medical decision-making: 2021 guidelines
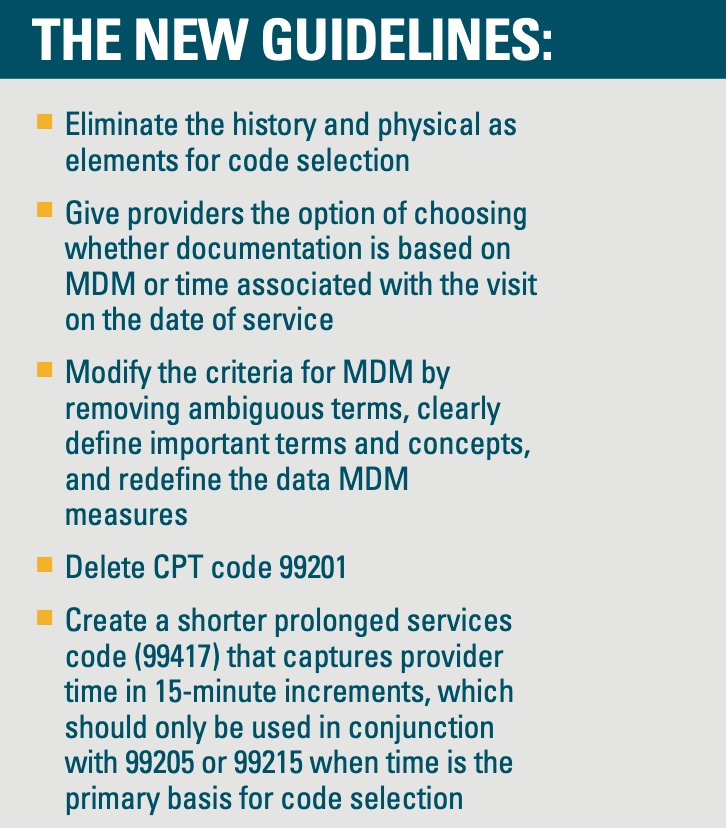
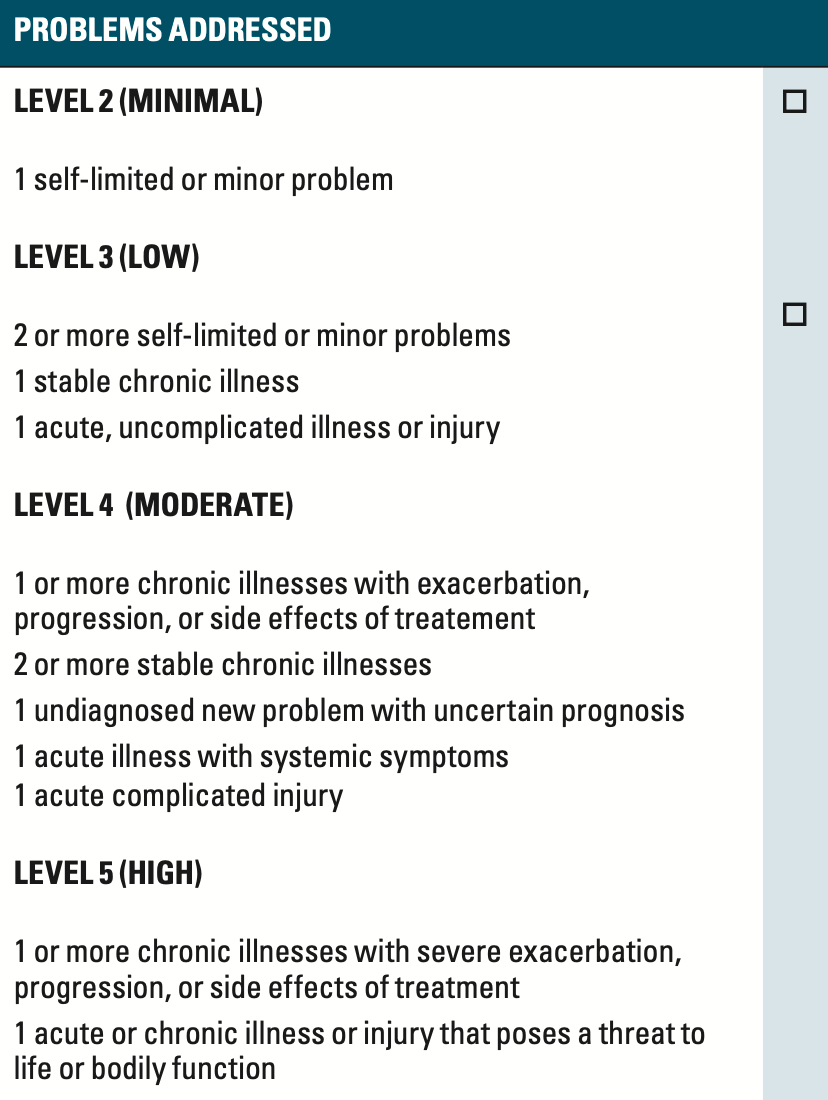
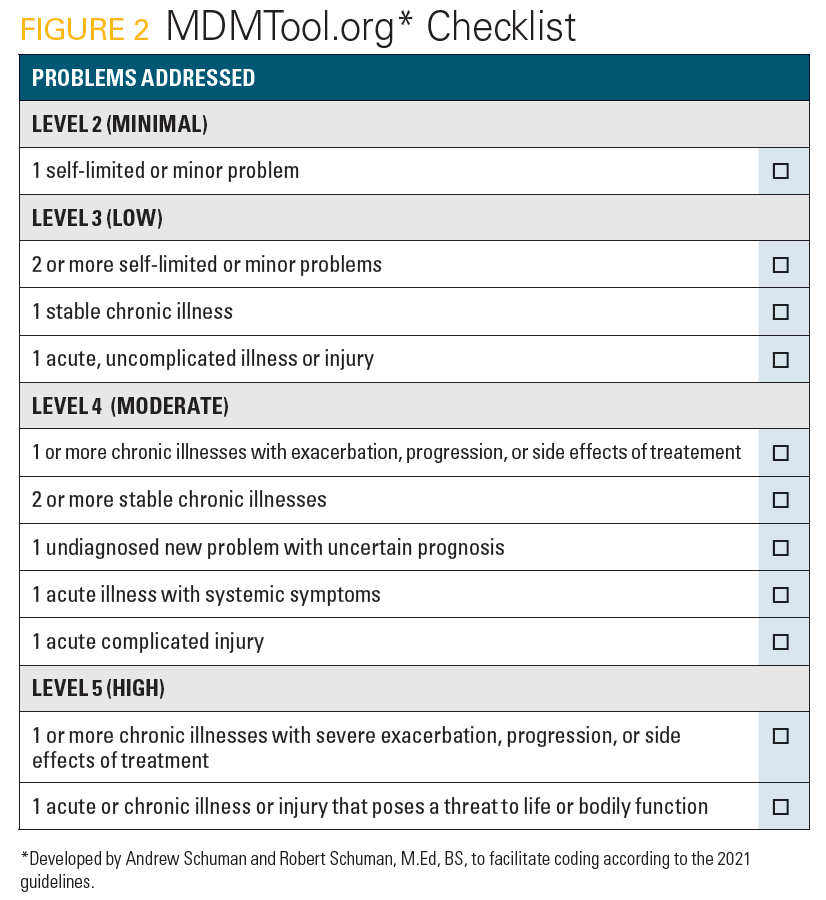
As they did previously, CMS recognizes 4 levels of MDM (straightforward, low complexity, moderate complexity, and high complexity). MDM quantifies the complexity of establishing a diagnosis and/or selecting management options by measuring:
- The number and complexity of problems addressed at the encounter
- The amount and/or complexity of data to be reviewed and analyzed
- The risk of complications and/or morbidity with patient treatment
This year, to guide MDM decisions, providers must become familiar with the coding table. As in the past, the table columns list the number and complexity of problems addressed, the data reviewed for the visit, and the risk associated with treating the patient. The performance and interpretation of in-office tests (rapid strep, rapid flu tests, etc.) as well as external tests, such as complete blood count (CBC) or an x-ray done at a hospital are appropriate to consider as data elements. Each test counts as 1, if it is performed or evaluated on the day of service (see Figure 1).
Looking at the coding table, determining the level of MDM associated with a visit depends on 2 of 3 scores associated with elements of care columns. To qualify for an MDM level, 2 of the 3 elements for that level of decision-making must be met or exceeded. Keep in mind that, for pediatricians, the majority of outpatient visits are low complexity (level 3 – 99203 new patient, 99213 established patient) and moderate complexity (level 4 – 99204 new patient, 99214 established patient).
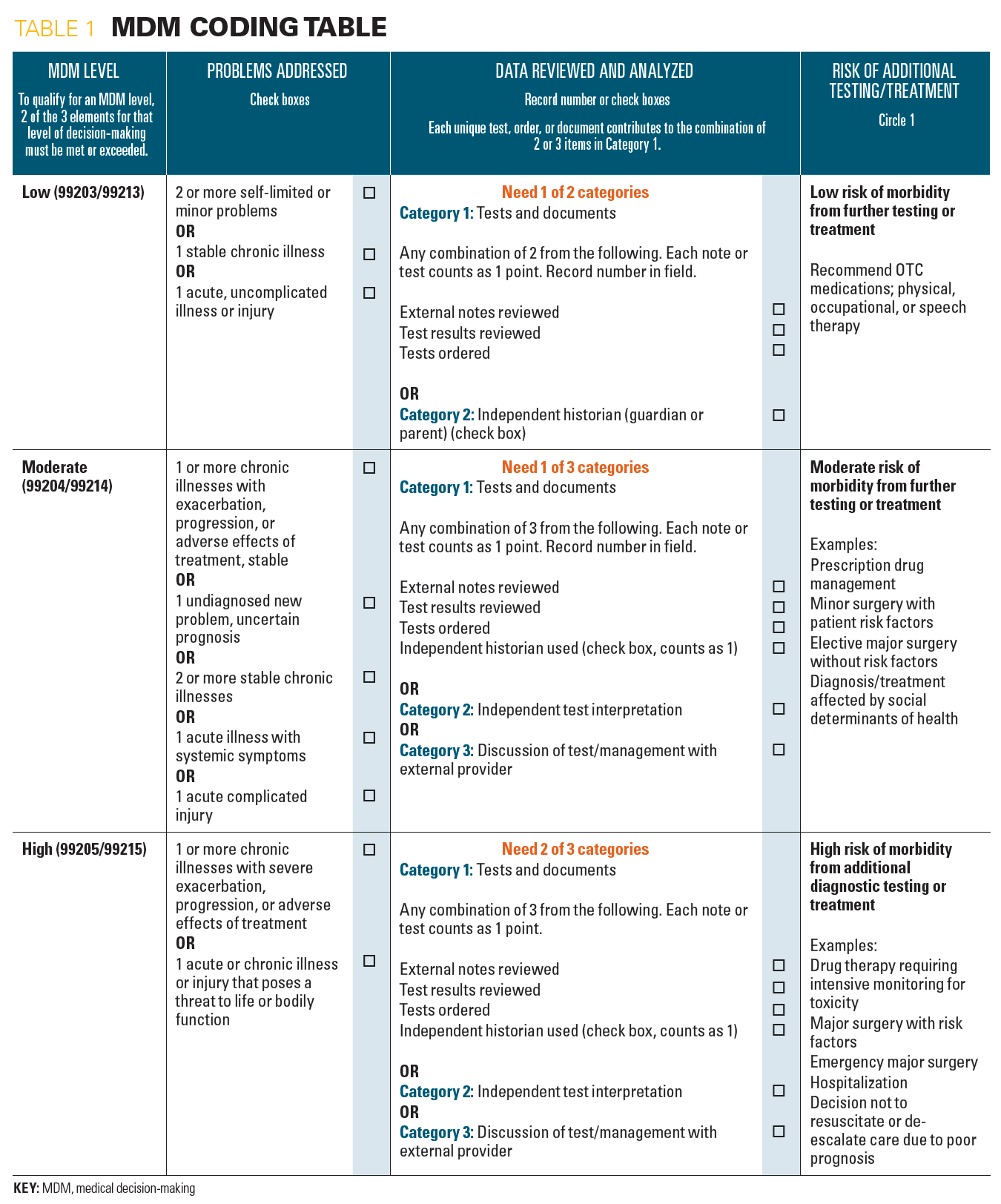
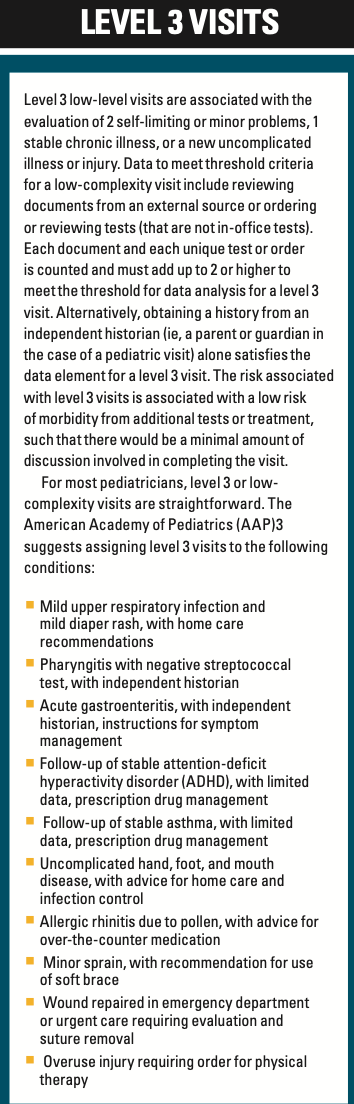
Level 3 visits
Level 3 low-level visits are associated with the evaluation of 2 self-limiting or minor problems, 1 stable chronic illness, or a new uncomplicated illness or injury. Data to meet threshold criteria for a low-complexity visit include reviewing documents from an external source or ordering or reviewing tests (that are not in-office tests). Each document and unique test or order is counted and must add up to 2 or higher to meet the threshold for data analysis for a level 3 visit.
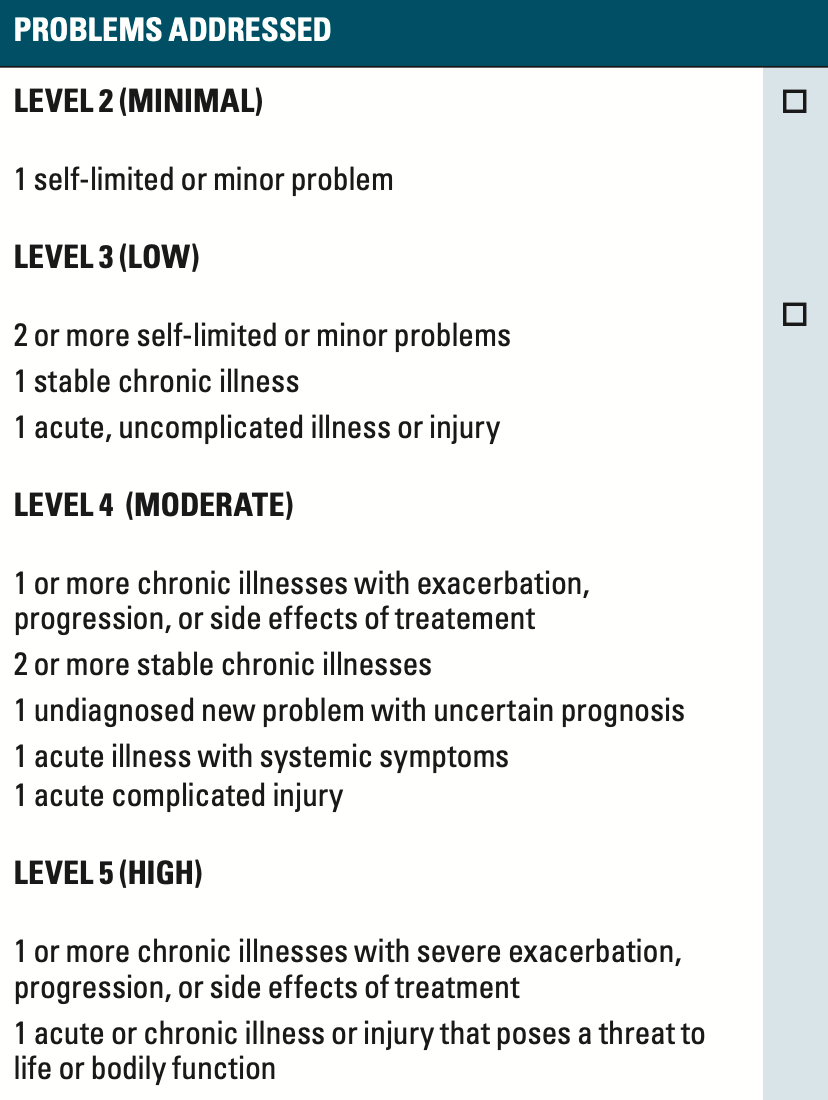
Problems addressed
Alternatively, obtaining a history from an independent historian (ie, a parent or guardian in the case of a pediatric visit) alone satisfies the data element for a level 3 visit. The risk associated with level 3 visits is associated with a low risk of morbidity from additional tests or treatment, such that there would be a minimal amount of discussion involved in completing the visit.
For most pediatricians, level 3 or low-complexity visits are straightforward. The American Academy of Pediatrics (AAP) 3 suggests assigning level 3 visits to the following conditions:
- Mild upper respiratory infection and mild diaper rash, with home care recommendations
- Pharyngitis with negative streptococcal test, with independent historian
- Acute gastroenteritis, with independent historian, instructions for symptom management
- Follow-up of stable attention-deficit/hyperactivity disorder (ADHD), with limited data, drug management
- Follow-up of stable asthma, with limited data, prescription drug management
- Uncomplicated hand, foot, and mouth disease, with advice for home care and infection control
- Allergic rhinitis due to pollen, with advice for over-the-counter medication
- Minor sprain, with recommendation for use of soft brace
- Wound repaired in emergency department or urgent care requiring evaluation and suture removal
- Overuse injury requiring order for physical therapy
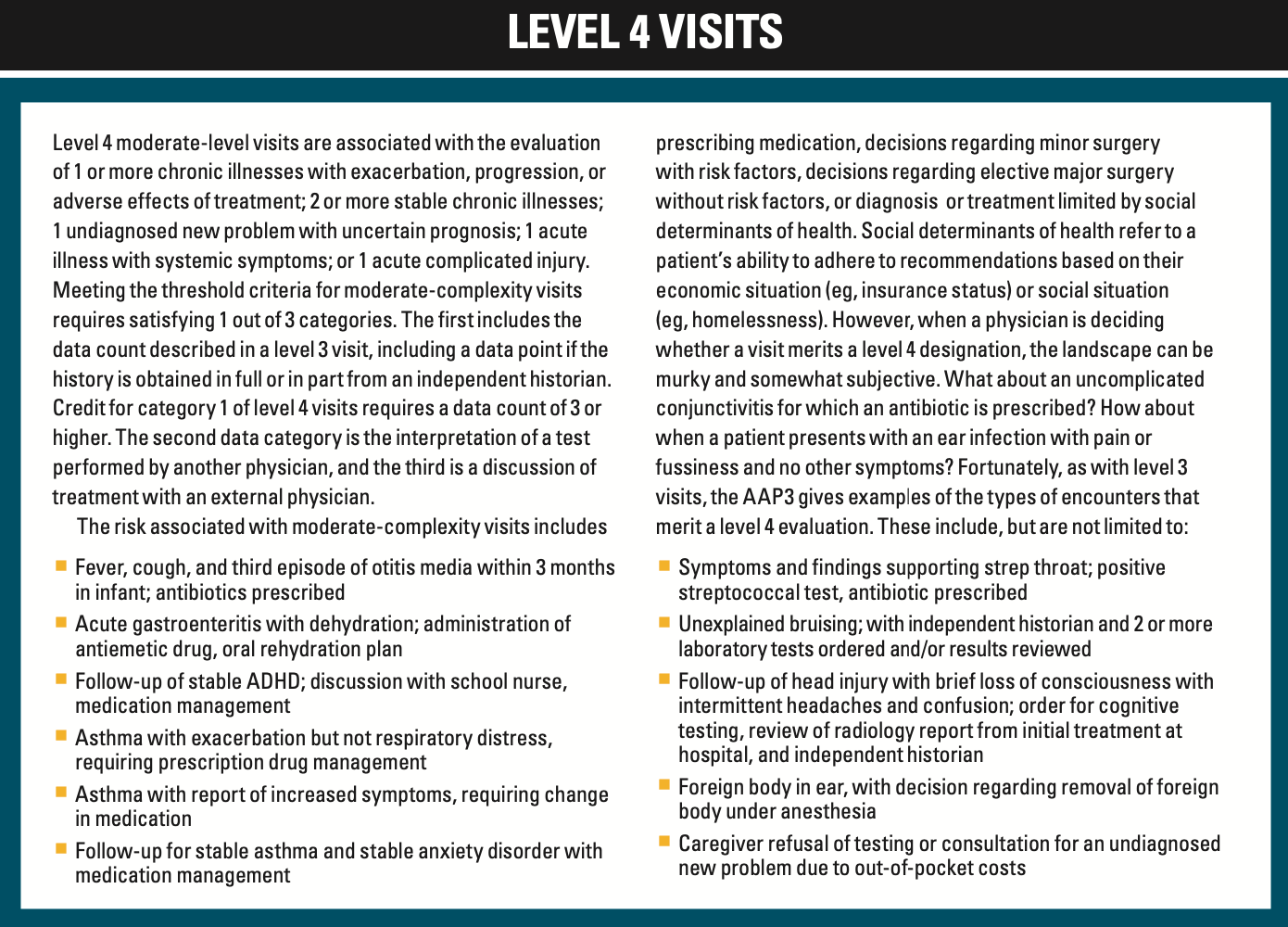
Level 4 visits
Level 4 moderate-level visits are associated with the evaluation of 1 or more chronic illnesses with exacerbation, progression, or adverse effects of treatment; 2 or more stable chronic illnesses; 1 undiagnosed new problem with uncertain prognosis; 1 acute illness with systemic symptoms; or 1 acute complicated injury. Data required to meet the threshold criteria for moderate-complexity visits require satisfying 1 out of 3 categories. The first includes the data count described in a level 3 visit, including a data point if the history is obtained in full or in part from an independent historian. Credit for category 1 of level 4 visits requires a data count of 3 or higher. The second data category is the interpretation of a test performed by another physician, and the third is a discussion of treatment with an external physician.
The risk associated with moderate-complexity visits includes prescribing medication, decisions regarding minor surgery with risk factors, decisions regarding elective major surgery without risk factors, or diagnosis or treatment limited by social determinants of health. Social determinants of health refer to a patient’s ability to adhere to recommendations based on their economic situation (eg, insurance status) or social situation (eg, homelessness). However, when a physician is deciding whether a visit merits a level 4 designation, the landscape can be murky. What about an uncomplicated conjunctivitis for which an antibiotic is prescribed? How about when a patient presents with an ear infection with pain or fussiness and no other symptoms? Fortunately, as with level 3 visits, the AAP 3 gives examples of the types of encounters that merit a level 4 evaluation. These include, but are not limited to:
- Fever, cough, and third episode of otitis media within 3 months in infant; antibiotics prescribed
- Acute gastroenteritis with dehydration; administration of antiemetic drug, oral rehydration plan
- Follow-up of stable ADHD; discussion with school nurse, medication management
- Asthma with exacerbation but not respiratory distress, requiring prescription drug management
- Asthma with report of increased symptoms, requiring medication change
- Follow-up for stable asthma and stable anxiety disorder with medication management
- Symptoms and findings supporting strep throat; positive streptococcal test, antibiotic prescribed
- Unexplained bruising; with independent historian and 2 or more laboratory tests ordered and/or results reviewed
- Follow-up of head injury with brief loss of consciousness with intermittent headaches and confusion; order for cognitive testing, review of radiology report from initial treatment at hospital, and independent historian
- Foreign body in ear, with decision regarding removal of foreign body under anesthesia
- Caregiver refusal of testing or consultation for an undiagnosed new problem due to out-of-pocket costs
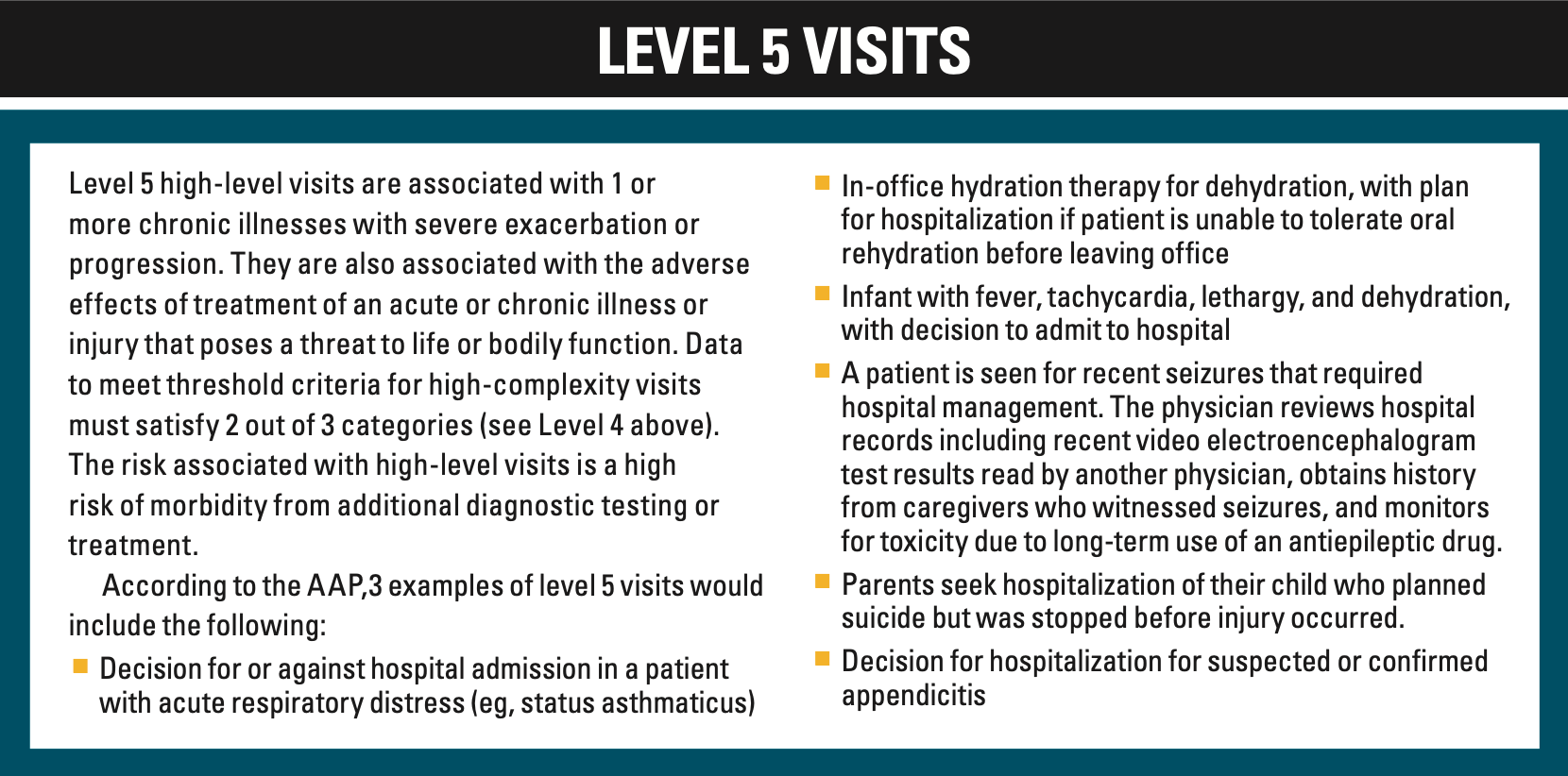
Level 5 visits
Level 5 high-level visits are associated with 1 or more chronic illnesses with severe exacerbation or progression. They are also associated with the adverse effects of treatment of an acute or chronic illness or injury that poses a threat to life or bodily function. Data to meet threshold criteria for high-complexity visits must satisfy 2 out of 3 categories (see Level 4). The risk associated with high-level visits is a high risk of morbidity from additional diagnostic testing or treatment.
According to the AAP, 3 examples of level 5 visits would include:
- Decision for or against hospital admission in a patient with acute respiratory distress (eg, status asthmaticus)
- In-office hydration therapy for dehydration, with plan for hospitalization if patient is unable to tolerate oral rehydration before leaving office
- Infant with fever, tachycardia, lethargy, and dehydration, with decision to admit to hospital
- A patient is seen for recent seizures requiring hospital management. The physician reviews hospital records including recent video electroencephalogram test results read by another physician, obtains history from caregivers who witnessed seizures, and monitors for toxicity due to long-term use of an antiepileptic drug.
- Parents seek hospitalization of their child who planned suicide but was stopped before injury occurred
- Decision for hospitalization for suspected or confirmed appendicitis
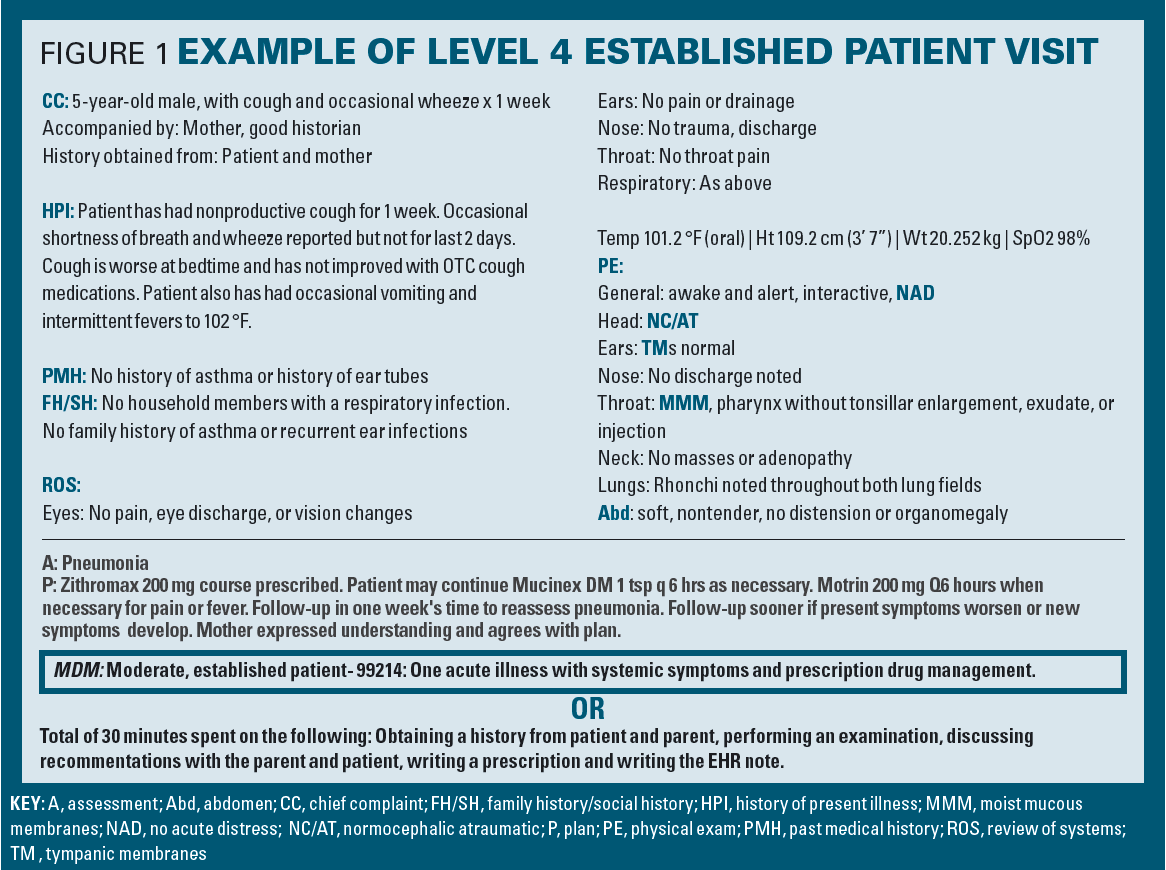
If you use MDM to code, you must accurately determine those elements of MDM that contributed to your determination of the level of service. Usually, your assessment and plan will contain enough details to justify the level of MDM billed for. The prudent pediatrician will conclude a level 4 or 5 note by presenting the MDM elements documented in the note (Figure 1). The note in Figure 1 was presented in table format with invisible borders to conserve space, which enables reading without scrolling. Important components of the note are highlighted to capture the reader’s attention. Documenting MDM at the end of your note reduces the chance of an insurance company audit. It also serves as a reminder to document the elements needed to justify the level of service you submit.
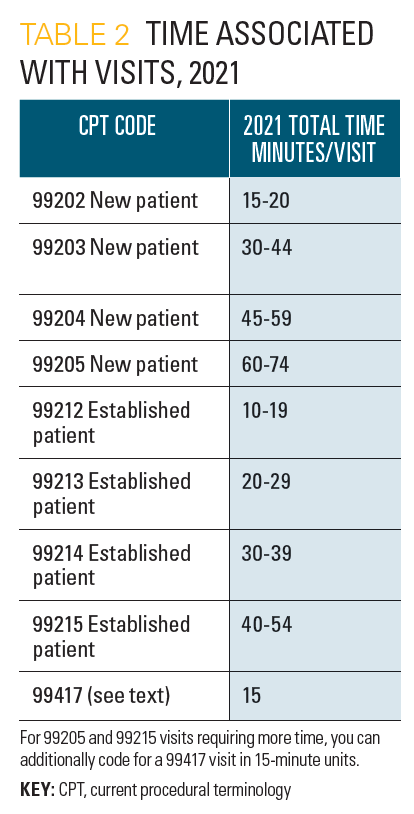
Coding by time
Using time to determine a level of service can be less confusing compared to assigning a level of service using MDM. Time now consists of:
- Preparing to see the patient, reviewing tests and external notes
- Obtaining a history from the parent
- Performing an examination
- Ordering medication or tests
- Referring to and possibly communicating with other health care providers on management
- Documenting in the health record
- Communicating results (on day of service) with the patient
- Time spent in care coordination
Coding by time is dependent on providers being honest in their determination of time elements during a visit. As such, visits coded by time are quite difficult for insurance companies to reject.
A brief webinar on the guidelines is available on the medgizmos.com website. You can also visit MDMTool.org (Figure 2) which helps providers code more accurately.
- 2021 evaluation and management CPT Codes. Sullivan Cotter. Accessed January 26, 2021. https://sullivancotter.com/2021-evaluation-and-management-cpt-codes/
- Rules Committee print 116-68: text of the house amendment to the senate amendment to H.R.133. House Committee on Rules. December 21, 2020. Accessed February 2, 2021. https://rules.house.gov/sites/democrats.rules.house.gov/files/BILLS-116HR133SA-RCP-116-68.pdf
- American Academy of Pediatrics. Office E/M 2021: examples of pediatric medical decision-making for office evaluation and management services. AAP Pediatric Coding Newsletter . 2021; 16(4):9-11.
The problem with patient portals (and how to resolve them)
How pediatricians can best manage electronic health records without compromising patient care.

Exploring the 2021 evaluation and management coding update: Part 2
Contemporary Pediatrics sat down with Andrew J. Schuman, MD, FAAP, to discuss the levels of Medical Decision Making and offers examples of what types of visits would account for those levels.

Why your practice needs an internet contingency plan
Doctors and staff should know how to respond if internet goes down for prolonged periods.

Exploring the 2021 evaluation and management coding update: Part 1
Contemporary Pediatrics sat down with Andrew J. Schuman, MD, FAAP, to discuss what went into the new system.

The Great Resignation: Survival strategies for pediatric practice
Despite significant staffing shortages and increased workloads, medical practices can thrive by learning how best to do more with less.

How to recognize and help a physician colleague in emotional distress
Although it may be hard for us to admit, physicians face the same types of mental health conditions as our patients.
2 Commerce Drive Cranbury, NJ 08512
609-716-7777
Disclaimer » Advertising
- HealthyChildren.org

- ‹ Prev
- Next ›
The 27th edition of the AAP cornerstone coding publication has been completely updated to include all changes in pediatric-specific Current Procedural Terminology (CPT) and ICD-10-CM codes for 2022—complete with expert guidance for their application. The book's many clinical vignettes and examples, as well as the many coding pearls throughout, provide the added guidance needed to ensure accuracy and payment. (NOTE: This book features a full text reading experience. Click a chapter title to access content.)
Appendix II: Quick Reference to 2022 CPT ® Pediatric Code Changes
- Published: January 2022
- Split-Screen
- Chapter Contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the Chapter PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
"Quick Reference to 2022 CPT ® Pediatric Code Changes", Coding for Pediatrics 2022 : A Manual for Pediatric Documentation and Payment , Committee on Coding and Nomenclature (COCN), American Academy of Pediatrics, Linda D. Parsi, MD, MBA, CPEDC, FAAP, Cindy Hughes, CPC, CFPC, Becky Dolan, MPH, CPC, CPEDC
Download citation file:
- Ris (Zotero)
- Reference Manager
We have made every effort to include changes to procedures and services that are applicable to pediatric practices in this appendix. However, revisions and/or additional codes may have been published subsequent to the date of this printing. This list does not include all changes made to Current Procedural Terminology ( CPT ) 2022. Also, not all codes included in the quick reference table are further discussed in this publication (typically due to limited use by most pediatricians). Codes not discussed elsewhere are shaded in gray. Always refer to CPT 2022 for a complete listing of new codes, complete descriptions, and revisions. For questions or additional information on codes not discussed in this publication, please contact the American Academy of Pediatrics Coding Hotline ( https://form.jotform.com/Subspecialty/aapcodinghotline ). Any errata to CPT 2022 will be posted to the American Medical Association website, https://www.ama-assn.org/practice-management/cpt/errata-technical-corrections . These changes take effect January 1, 2022. Do not report the changes or codes prior to that date.
●=New code ▲=Revised code # =Re-sequenced code + =Add-on code ★=Telemedicine
Related Chapters
Related articles.
Advertising Disclaimer »

Affiliations
- Books by Subject
- Institutional Collections
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations, advertising.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account

Follow these four steps to code quickly and accurately, while reducing the need to count up data points.
KEITH W. MILLETTE, MD, FAAFP, RPh
Fam Pract Manag. 2021;28(4):21-26
Author disclosure: no relevant financial affiliations.

The new rules for coding evaluation and management (E/M) office visits are a big improvement but still a lot to digest. 1 , 2 To ease the transition, previous FPM articles have laid out the new American Medical Association/CPT medical decision making guide 3 and introduced doctor–friendly coding templates (see “ Countdown to the E/M Coding Changes ,” FPM , September/October 2020), explained how to quickly identify level 4 office visits (see “ Coding Level 4 Visits Using the New E/M Guidelines ,” FPM , January/February 2021), and applied the new guidelines to common visit types (see “ The 2021 Office Visit Coding Changes: Putting the Pieces Together ,” FPM , November/December 2020).
After several months of using the new coding rules, it has become clear that the most difficult chore of coding office visits now is assessing data to determine the level of medical decision making (MDM). Analyzing each note for data points can be time-consuming and sometimes confusing.
That being the case, it's important to understand when you can avoid using data for coding, and when you can't. I've developed a four-step process for this (see “ A step-by-step timesaver ”).
The goal of this article is to clarify the new coding rules and terminology and to explain this step-by-step approach to help clinicians code office visits more quickly, confidently, and correctly.
The new evaluation and management office visit coding rules have simplified many things but are still a lot to digest, especially when it comes to counting data.
There are different levels of data and different categories within each level, which can make using data to calculate the visit level time-consuming and confusing.
By calculating total time, and then moving on to assessing problems and prescription drug management, most visits can be optimally coded without dealing with data at all.
OFFICE VISIT CODING RULES AND TERMINOLOGY
To make full use of the step-by-step process, we have to first understand the new rules, as well as coding terminology. Here is a brief summary.
Medically appropriate . Physicians and other qualified health care professionals may now solely use either total time or MDM to determine the level of service of an office visit. That means the “history” and “physical exam” components are no longer needed for code selection, which simplifies things. But your patient note must still contain a “medically appropriate” history and physical. So continue to document what is needed for good medical care.
New patient . A new patient is a patient who has not been seen by you or one of your partners in the same medical specialty and the same group practice within the past three years.
Total time and prolonged services . Total time includes all the time you spend on a visit on the day of the encounter (before midnight). It includes your time before the visit reviewing the chart, your face-to-face time with the patient, and the time you spend after the visit finishing documentation, ordering or reviewing studies, refilling medications, making phone calls related to the visit, etc. It does not include your time spent performing separately billed services such as wellness visits or procedures. Total time visit level thresholds differ for new patients vs. established patients. (See the total times in “ The Rosetta Stone four-step template for coding office visits .”)
The prolonged services code comes into play when total time exceeds the limits set for level 5 visits by at least 15 minutes.
Medical decision making . MDM is made up of three components: problems, data, and risk. Each component has different levels, which correspond to levels of service (low/limited = level 3, moderate = level 4, and high/extensive = level 5). The highest level reached by at least two out of the three components determines the correct code for the level of service. MDM criteria is the same for new and established patients.
Problems addressed . This includes only the problems you address at that specific patient visit. It does not include all the patient's diagnoses and does not include problems that are exclusively managed by another clinician. Problems addressed are separated into low-complexity problems (level 3), moderate-complexity problems (level 4), and high-complexity problems (level 5). To code correctly, you need to know the coding value of the problems you address. It is helpful to think of problems in terms of levels of service (e.g., a sinus infection is usually a level 3 problem, and pneumonia or uncontrolled diabetes are usually level 4 problems).
The simplest way to summarize problems is this: Life-threatening problems are level 5; acute or chronic illnesses or injuries are level 3 or 4 depending on how many there are, how stable they are, and how complex they are; and if there's just one minor problem, it's level 2.
(For more specifics see “ What level of problem did I address? ”)
Risk . Risk is also separated into “low” (level 3), “moderate” (level 4), and “high” (level 5) categories.
Level 3 risk includes the use of over-the-counter (OTC) medications.
Level 4 risk includes the following:
Prescription drug management: starting, stopping, modifying, refilling, or deciding to continue a prescription medication (and documenting your thought process),
Social determinants of health that limit diagnosis or treatment (this is when patients' lack of finances, insurance, food, housing, etc., affects your ability to diagnose, manage, and care for them as you normally would).
Level 5 risk includes the following:
Decisions about hospitalization,
Decisions about emergency major surgery,
Drug therapy that requires intensive toxicity monitoring,
Decisions to not resuscitate or to de-escalate care because of poor prognosis.
Data analyzed . For purposes of MDM, data is characterized as “limited” (level 3 data), “moderate” (level 4 data), or “extensive” (level 5 data). But each level of data is further split into Categories 1, 2, and 3. This can make calculating data complicated, confusing, and time-consuming. Here are the data components and terms you need to know.
Category 1 data includes the following:
The ordering or reviewing of each unique test , i.e., a single lab test, panel, X-ray, electrocardiogram (ECG), or other study.
Ordering and reviewing the same lab test or study is worth one point, not two; a lab panel (e.g., complete blood count or comprehensive metabolic panel) is worth one point,
Reviewing a pertinent test or study done in the past at your own facility or another facility,
Reviewing prior external notes from each unique source, including records from a clinician in a different specialty or from a different group practice or facility as well as each separate health organization (e.g., reviewing three notes from the Mayo Clinic is worth one point, not three, but reviewing one note from Mayo and one from Johns Hopkins is worth a total of two points),
Using an independent historian, which means obtaining a history from someone other than the patient, such as a parent, spouse, or group home staff member. (This is included in Category 2 for level 3 data, but falls into Category 1 for level 4 and 5 data.)
Category 2 data includes the following:
Using an independent historian (for level 3 data only),
Independent interpretation of tests, which is your evaluation or reading of an X-ray, ECG, or other study (e.g., “I personally reviewed the X-ray and it shows …”) and can include your personal evaluation of a pertinent study done in the past at your or another facility. It does not include reviewing another clinician's written report only, and it does not include studies for which you are also billing separately for your reading.
Category 3 data includes the following:
Discussion of patient management or test interpretation with an external physician, other qualified health care professional, or appropriate source. An external physician or other qualified health care professional is someone who is not in your same group practice or specialty. Other appropriate sources could include, for example, consulting a patient's teacher about the patient's attention deficit hyperactivity disorder.
A STEP-BY-STEP TIMESAVER
The majority of office visits can be optimally coded by using time or by looking at what level of problems were addressed (see Steps 1 and 2 below) and whether a prescription medication was involved.
A level 3 problem can be coded as a level 3 visit if you address it with an OTC or prescription medication. A level 4 problem can be coded as a level 4 visit if you order prescription medication or perform any other type of prescription drug management (modifying, stopping, or deciding to continue a medication). Most level 2 and level 5 office visits are straightforward, and most level 5 visits will be coded by time. They will typically be visits in which you address multiple problems or complicated problems and the total time exceeds 40 minutes for established patients. This is much more common than seeing critically ill patients who may require admission, which is another level 5 scenario. The few remaining patient visits that have not already been coded require analyzing data (Steps 3 and 4). (See “ The Rosetta Stone four-step template for coding office visits .”)
Step 1: Total time . Think time first. If your total time spent on a visit appropriately credits you for level 3, 4, or 5 work, then document that time, code the visit, and be done with it. But if it does not, go to Step 2.
Step 2: “Problems plus.” Don't be afraid to move on from time-based coding if you believe you performed a higher level visit using MDM. Many visits can be coded with MDM just by answering these two questions: What was the highest-level problem you addressed during the office visit? And did you order, stop, modify, or decide to continue a prescription medication?
If you addressed a level 2 problem and your total time was less than 20 minutes (or less than 30 for a new patient), then code level 2.
If you addressed a level 3 problem, plus you recommended an OTC medication or performed prescription drug management, then code level 3.
If you addressed a level 4 problem, plus you performed prescription drug management, then code level 4.
Chronic disease management often qualifies as level 4 work. For documentation, think “P-S-R”: problem addressed, status of the problem (stable vs. unstable), and prescription drug management (Rx). This trio should make it clear to coders, insurance companies, and auditors that level 4 work was performed.
For instance, if a patient has controlled hypertension and diabetes and you document that you decided to continue the current doses of losartan and metformin, that's level 4 (two stable chronic illnesses plus prescription drug management). If you see a patient with even one unstable chronic illness and document prescription drug management to address it, that's also level 4.
For a level 5 problem, if you see a really sick patient and decide to admit or consider admission (and you document your thought process in your note), then code level 5.
By starting with total time and, if necessary, moving on to “problems plus,” you will probably be able to optimally code 90% of your office E/M visits. But on the rare occasions when you see a patient for level 4 or 5 problems for less than the required time and don't do any prescription drug management, you may have to proceed to Steps 3 and 4.
Step 3: Level 4 problem with simple data or social determinants of health concerns . Code level 4 if you saw a patient for a level 4 problem and did any of the following:
Personally interpret a study (e.g., X-ray),
Discuss management or a test with an external physician,
Modify your workup or treatment because of social determinants of health.
Step 4: Level 4 or 5 problem with complex data . If you saw a patient for a level 4 problem and still haven't been able to code the visit at this point, you have to tally Category 1 data points:
Review/order of each unique test equals one point each,
Review of external notes from each unique source equals one point each,
Use of an independent historian equals one point.
Once you reach three points, code it as level 4.
For a level 5 problem, if you see a really sick patient, order/interpret an X-ray or ECG, and review/order two lab tests, then code level 5.
Following these steps should allow you to quickly identify the optimal level to code most any E/M office visit (for pre-op visits, see “ Coding pre-ops template .”)
Here's a catchy rhyme to remember the basic outline of the steps:
To finish fast ,
code by time and problems first ,
and save data for last .
By mastering the new coding rules and terminology and applying this four-step approach, you can code office visits more quickly, accurately, and confidently — and then spend more time with your patients and less time at the computer.
CPT Evaluation and Management (E/M) Office or Other Outpatient and Prolonged Services Code and Guideline Changes . American Medical Association. Accessed June 10, 2021. https://www.ama-assn.org/system/files/2019-06/cpt-office-prolonged-svs-code-changes.pdf
E/M Office Visit Compendium 2021. American Medical Association; 2020.
Table 2 – CPT E/M office revisions level of medical decision making. American Medical Association. Accessed June 10, 2021. https://www.ama-assn.org/system/files/2019-06/cpt-revised-mdm-grid.pdf
Continue Reading

More in FPM
More in pubmed.
Copyright © 2021 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
- Why PhysicianXpress
- What to Expect
- FAQ’s
- Our History
- Our Purpose & People
- Our Technology
- Our Partners
- ONC Certified EHR
- PediatricXpress
- VaccineXpress
- RevenueXpress
- Real World Testing Plan
- Privacy Policy
- White Papers
Pediatric Provider Coding Review: ADHD Coding Example

Related Posts


IMAGES
VIDEO
COMMENTS
sick visit (99202-99215). . Codes . 99406-99409. may be reported in addition to the preventive. medicine service codes. CPT. Codes. 99406. moking and tobacco use cessation counseling visit; S ntermediate, greater than 3 minutes up to 10 minutesi. 99407. ntensive, greater than 10 minutesi. 99408. lcohol or substance (other than tobacco ...
If the insurers list differs from that recommended by the AAP, report the insurer to the AAP, which will follow up on your behalf. Some practices have trouble with reimbursement on a three- or four-day visit for newborns discharged 24 hours after birth. In this case, it is recommended that you use office-visit codes 99212-99215 for this three ...
To bill for a well-child visit: Use the age-based preventive visit CPT code and appropriate ICD-10 Code listed in Table 1. Bill for each separate assessment/screening performed using the applicable CPT code from Table 2. If a screening or assessment is positive, use ICD-10 code Z00.121. If it is an issue that requires follow-up or a referral ...
Outpatient to Inpatient Crossover. • Critical care in the ED of patient five years or. younger (99291 -99292) that results in an inpatient admission by the same provider are reported with neonatal or pediatric critical care codes (99468-99472) because these codes are per day and cannot be billed more than once per day.
A child has a well-child visit EPSDT (99381 - 99461), with a well child diagnosis code (Z-code) in the first position; the sick visit code (99211 - 99215) with the modifier 25 and with the illness diagnosis CPT code in the second position. To bill this way, there must be enough evidence in the medical record documentation to support a stand ...
Well-Child Visits in the First 30 Months of Life (W30)* Ages 0-30 Months The percentage of children who had the following number of well-child visits with a PCP during the last 15 months. The following rates are reported: 1.Well-Child Visits in the First 15 Months: Six or more well-child visits 2. Well-Child Visits for Age 15-30 Months: Two or more
Coding Follow-up Visits. Question: Are there any diagnosis codes used when a child comes in for a re-check and the problem is resolved? For example, for otitis media or bronchitis, we usually use 99213 for an office visit. And for the diagnosis we use 382.9 for otitis media, and 466.0 for bronchitis. Are there any resolved codes we should be using?
AAP recommends use preventive medicine codes 99381-99397. If not covered due to previous preventive visit in same year, will be billed to parent. Office visit codes 99211-99215 only if problem uncovered. 99241-99245 outpt. consult if coach or school nurse requests visit due to medical concern.
Follow-up care and aftercare codes describe these reasons for encounters. Note, however, that aftercare of injuries is reported with the appropriate injury code and a seventh character indicating care during a healing phase (subsequent encounter) and/or for sequela of the injury (eg, S53.411D , radiohumeral [joint] sprain of right elbow ...
The preventive medicineservices codes for new patients are 99381 (under 1 year old), 99382 (1 through 4), 99383 (5 through 11), 99384 (12 through 17), and 99385 (18 through 39). The office-visit codes are 99201 through 99205. Note that the sick diagnosis code goes only on the office visit, and the well-care diagnosis code, V20.2, goes only on ...
The Bright Futures/American Academy of Pediatrics (AAP) developed a set of comprehensive health guidelines for well-child care, known as the "periodicity schedule." It is a schedule of screenings and assessments recommended at each well-child visit from infancy through adolescence. Schedule of well-child visits. The first week visit (3 to 5 ...
Changes or corrections may occur prior to official release of Current Procedural Terminology ( CPT ®) 2021. In this issue, we explore example scenarios that might be reported with codes at level 5 of the office E/M services ( 99205 and 99215) for dates of service on and after January 1, 2021. As previously noted, for each level of office E/M ...
Changes or corrections may occur prior to the official release of Current Procedural Terminology ( CPT ®) 2021. In this issue, we review example scenarios that might be reported with codes at level 3 of the office E/M services ( 99203 and 99213) for dates of service on and after January 1, 2021. As previously noted, for each level of office E ...
(CPT ®) code 96110 (Developmental screening). Code 96110 is reported when performed in the context of preventive medicine services. This code also may be reported when screening is performed with other evaluation and management (E/M) services such as acute illness or follow-up office visits. If multiple standardized* screens are
A new evaluation and management coding system for outpatient visits was implemented earlier this year. This article details the nuances of the new system. ... Follow-up of head injury with brief loss of consciousness with intermittent headaches and confusion; order for cognitive testing, review of radiology report from initial treatment at ...
The 27th edition of the AAP cornerstone coding publication has been completely updated to include all changes in pediatric-specific Current Procedural Terminology (CPT) and ICD-10-CM codes for 2022—complete with expert guidance for their application. The book's many clinical vignettes and examples, as well as the many coding pearls throughout, provide the added guidance needed to ensure ...
Step 1: Total time. Think time first. If your total time spent on a visit appropriately credits you for level 3, 4, or 5 work, then document that time, code the visit, and be done with it. But if ...
she asks. 1. Use a Sick Visit Code. First, you should consider the above real-world coding scenario a sick visit. "Our providers say this is not a normal well-child exam," Bibian says. The visit is to check for specific problems. "The encounter is for a follow-up of the hospital visit and to ensure the transition home has gone well," says ...
The provider uses a time-based approach for the selection of the appropriate CPT code for follow-up ADHD visits. If the visit and data analysis review takes between 20-29 minutes, the provider will select CPT code 99213. If the visit and data analysis review takes between 30-39 minutes, the provider will select CPT code 99214. Above is one ...
• Your date of service will be the date the initiation of the e-visit began or the range of dates it took place because this service is cumulative time over 7 days. 99421 Online digital evaluation and management service, for an established patient, for up to 7 days, cumulative time during the 7 days; 5-10 minutes 99422 11-20 minutes