Shop for Plans
Shop for your own coverage, plans through your employer.
Learn about the medical, dental, pharmacy, behavioral, and voluntary benefits your employer may offer.

Looking for Medicare coverage?
Electronic medical and health records.
There are three types of medical records commonly used by patients and doctors:
- Personal health record (PHR)
- Electronic medical record (EMR)
- Electronic health record (EHR)
PHR, or personal health record
Technically, any medical record you keep for yourself is a personal health record (PHR). You can keep records:
- On a device (a computer or smartphone, for example).
- On the Internet.
But you're most likely to hear the term PHR for records that you keep on the Internet. Your health plan's website or a local hospital's website may have programs you can use for free to do this. And your information is protected so that only people with permission can see it.
The advantage of using a website provided by your health plan is that you can type in information. For example, you can type in results of blood pressure tests you do at home. And when you see your doctor for a checkup or for treatment, the doctor can see those home test results with just a few taps on the keyboard.
Quick access to information like that can help your doctor give you the best care possible.
EMR, or electronic medical record
Electronic medical records (EMRs) are electronic files that a doctor or other provider uses instead of paper files stored on shelves. The doctor types the information into a computer. Those computer files stay in your doctor's computer system.
Keeping records on a computer is a lot easier than keeping paper records. And these systems also handle scheduling and billing. Some doctors are still using paper because it's a lot of work to convert all those paper files into electronic records.
EMRs usually stay in the office computer system. They can't usually be sent to or shared with other providers outside of that system, such as a lab or hospital.
EHR, or electronic health record
Electronic health records (EHRs) are built to be shared with other health care providers who all use the same system. So with an EHR system, your family doctor can instantly send medical records to your heart specialist, your hospital, the lab, your drugstore, and your computer at home.
The goal of EHRs is to improve the coordination of your care by giving providers accurate, up-to-date information. This includes information from you, the patient.
Current as of: August 6, 2023
Author: Healthwise Staff
Clinical Review Board All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use . Learn how we develop our content .
To learn more about Healthwise, visit Healthwise.org .
© 1995-2024 Healthwise, Incorporated. Healthwise, Healthwise for every health decision, and the Healthwise logo are trademarks of Healthwise, Incorporated.
Related Links
Page footer, i want to..., secure member sites, the cigna group information.
Cigna. All rights reserved.
Individual and family medical and dental insurance plans are insured by Cigna Health and Life Insurance Company (CHLIC), Cigna HealthCare of Arizona, Inc., Cigna HealthCare of Illinois, Inc., Cigna HealthCare of Georgia, Inc., Cigna HealthCare of North Carolina, Inc., Cigna HealthCare of South Carolina, Inc., and Cigna HealthCare of Texas, Inc. Group health insurance and health benefit plans are insured or administered by CHLIC, Connecticut General Life Insurance Company (CGLIC), or their affiliates (see a listing of the legal entities that insure or administer group HMO, dental HMO, and other products or services in your state). Accidental Injury, Critical Illness, and Hospital Care plans or insurance policies are distributed exclusively by or through operating subsidiaries of Cigna Corporation, are administered by Cigna Health and Life Insurance Company, and are insured by either (i) Cigna Health and Life Insurance Company (Bloomfield, CT); (ii) Life Insurance Company of North America (“LINA”) (Philadelphia, PA); or (iii) New York Life Group Insurance Company of NY (“NYLGICNY”) (New York, NY), formerly known as Cigna Life Insurance Company of New York. The Cigna name, logo, and other Cigna marks are owned by Cigna Intellectual Property, Inc. LINA and NYLGICNY are not affiliates of Cigna.
All insurance policies and group benefit plans contain exclusions and limitations. For availability, costs and complete details of coverage, contact a licensed agent or Cigna sales representative. This website is not intended for residents of New Mexico.
Selecting these links will take you away from Cigna.com to another website, which may be a non-Cigna website. Cigna may not control the content or links of non-Cigna websites. Details

- Center on Health Equity and Access
- Health Care Cost
- Health Care Delivery
- Value-Based Care
EHR Documentation and the Patient–Physician Visit
The need for physicicans to gather information for electronic health records has changed the nature of the patient visit.
IN 1999 AND 2001, the Institute of Medicine (IOM) issued reports that galvanized the medical community about healthcare quality. The 1999 report, To Err Is Human: Building a Safer Health System highlighted the negative role that medical errors play in healthcare quality. 1 Extrapolating from reviews of adverse events in Colorado, Utah, and New York, the authors concluded that between 44,000 and 88,000 Americans die annually as a result of medical errors; the cost in dollars was likewise very high. The authors reported that “total national costs—lost income, lost household production, disability, and healthcare costs—were estimated to be between $17 billion and $29 billion, of which health care costs represented over one-half.” 1
Stressing the need to adopt a culture of safety within the American healthcare system to improve its quality, the authors noted that blaming individuals for errors was not useful—the focus should be “on preventing future errors by designing safety into the system.” The report further emphasized the importance of information technology and the need for computerized patient records, which would benefit patient care.The following are key highlights from the IOM report:
• The ability to access patient data without delay at any time in any place (eg, in an emergency or when the patient is away from home)
• Ensure that services are obtained and track outcomes of treatment
• Aggregate data from large numbers of patients, both to measure outcomes of treatment and to promptly recognize complications of new drugs, devices, and treatments
To achieve these results, systems would need to be “patient specific, allow population-based analyses, and have systems that manage the case process through reminder, decision support, and guidance grounded in evidence-based knowledge.” 1
In 2001, the IOM published Crossing the Quality Chasm: A New Health System for the 21st Century , which furthered the concept that using information technology would greatly improve healthcare quality. 2 The report stressed “the importance of a strong information infrastructure in supporting efforts to reengineer care processes; manage the burgeoning clinical knowledge base; coordinate patient care across clinicians, settings, and over time; support multidisciplinary team functioning; and facilitate performance and outcome measurements for improvement and accountability.” 2
Despite the IOM’s belief that greater use of information technology and computerized records would improve healthcare quality, adoption of electronic record keeping remained slow. In 2001, only 18% of medical practices in the United States were using some form of an electronic health record (EHR). The HITECH Act of 2009 greatly spurred EHR implementation by offering financial incentives for adoption and penalties for failure to comply. Consequently, 78% of community practices in the United States had started using some form of EHRs by 2013, 3 with the prediction that 90% of practices would have EHRs by 2017. 4
Unintended Consequences
Unfortunately, the significant increase in the amount of data to be collected has created 2 unplanned consequences. For many practices, physicians became responsible for collecting this explosion of required data during the patient visit. This has caused them to spend more time doing data entry and clerical tasks than clinical activities. One study showed that “for every hour a physician spent providing direct clinical care to patients, he or she spent nearly 2 hours on EHR and other desk work, plus another 1 to 2 hours each night.” 5 Another study reported the actual effect on physician well-being when the time allotted for a visit did not meet the actual time required to accomplish all the required tasks. These time pressures increased the following: “stress, satisfaction, burnout and intent to leave practice.” 6 The problem of increased risk of physician burnout with EHR usage was confirmed in a 2016 report. 7
The other unintended consequence for patient care was how the physical task of using computers or other electronic devices during a patient visit could adversely affect the quality of patient—physician communication. In 2005, Ventres et al related that physicians using EHRs were more occupied with data gathering and clarifying clinical information than listening to patients’ own narratives. They were more prone to neglecting patients’ agendas” and less likely to “explore psychosocial and emotional issues or discuss how health problems affect patients’ lives.” Using the computer also created other problems, with physicians spending more time staring at the monitor or intensely keyboarding, rather than interacting with the patient. 8
Nowhere in medicine is effective patient—physician communication more vital than in the relationship between oncologists and their patients. A cancer diagnosis creates great stress and uncertainty. Patients need to be able to understand complex information about their illness and its possible treatments, and they are often required to make life-altering decisions. Patients depend on their oncologists to help them in all these areas. 9
With electronic record keeping, patients are finding themselves sharing the physician’s time and attention with the computer, turning what used to be a “dyadic” relationship between patient and physician to a triadic relationship of patient, physician, and computer. 10 Investigators write that patients across the globe have a “major concern about computers in the office—the fixation of the physician’s eyes on the computer screen.” This fear was not unfounded, as a study by Margalit et al found that physicians spent an average of 24% to 55% of the time gazing at the screen during a patient’s visit. 11
Research has confirmed that the use of the computer during the office visit takes away from the goal of patient-centered care. Even the simple task of introductions and starting a visit was affected by the presence of the computer: investigators found that after a short greeting, physicians walked straight to the computer, rather than interacting with the patient or discussing the patient’s agenda.12 What the physicians saw on the computer screen often prompted their opening statement, failing to ask the patient to share his or her concern(s). 12
Street et al noted that using the computer during the visit led physicians to focus more on information-related tasks and less on psychosocial issues. 13 They also found that physicians busy filling out check boxes in the EHR reduced the number of open-ended questions they asked patients and that multitasking caused physicians to lose focus and compromise effective communication. 13
Interventions to Improve Patient—Physician Computer Interactions
While physicians can control, to a variable extent, their choice of hardware and software and their communication style, they have little to no control over the amount of data collection mandated by external stakeholders (payers, governmental organizations, external review organizations, vendors and suppliers, etc). Recognizing the burden of administrative tasks on physicians, the American College of Physicians’ Medical Practice and Quality Committee issued a white paper on the need for all external stakeholders to review the value and necessity for all the information being collected and whether some of the data can be eliminated or decreased. The paper emphasized that this needs to be an ongoing process, not simply a onetime effort. 14
Unfortunately, physician choice of hardware and software is very much influenced by cost. Purchase of software updates and training on how to use the software are added practice expenses, over and above unforeseen expenses such as changes in computer equipment and exam room layout. computer equipment and exam room layout.
Physicians need to appreciate the effect that EHR charting and documenting has had on physician—patient communication—they need to understand that paying excessive attention to the computer and EHR may cause them to lose focus on their patients. Physicians must recognize that certain behaviors under their control are not acceptable. "Looking predominantly at the computer monitor during office visits, typing while patients are talking about intimate concerns, reading silently from the monitor while patients sit idly, using templates to lead interviewing rather than listening to patient narratives, and having their backs to patients” all work against relationship building. 15
In their 2013 paper, How to Integrate the Electronic Health Record and Patient-Centered Communication Into the Medical Visit: A Skills-Based Approach, Duke et al presented 10 behaviors or interventions physicians should follow when using an EHR. 10
• Changing the location of the EHR’s computer screen is a fairly easy intervention. Ideally, exam room screens should be located in a position that allows physicians to maintain patient eye contact and avoid having their backs to patients.
• Similarly, the ability to share the screen and its information with the patient is another positive for effective communication. 16
• A crucial skill that is under physicians’ control is their ability to type and their familiarity with their own EHR. As less computer-savvy physicians retire, the problems of poor typing and slowness with mouse clicks will disappear. In the meantime, all physicians using EHRs should make every effort to become proficient at typing and using computer hardware and know the capabilities and functionalities of their own EHR program.
• Ideally, physicians should have reviewed their patient’s records before starting any encounter. Upon starting a visit, they should introduce themselves and their role in the patient’s care. It is also useful for the physician to introduce the patient to the electronic record and explain that he or she might be typing into the computer during the course of the visit.
• A major pitfall to avoid is allowing the EHR template to dictate the course of the visit. Physicians need to start with open-ended questions and collaborate with the patient on what is to be accomplished during the course of the visit. Statements such as “Excuse me a second while I type this into the record,” “Just give me a minute while I look at the computer—I want to make sure I get this down correctly,” and “Let me tell you what I am typing” are ways to involve patients in what one is doing when focused on the computer and not the patients. 10 Physicians should explain to the patients when questions specific to templates or required data elements must be entered into the EHR.
• Physicians need to be able to follow patient cues and emotions and know when to interrupt typing and devote their complete attention to their patients. Research has shown that “emotional aspects of the interview are best accomplished when the physician moves her head, eyes, and torso toward the patient; removes her hands from the keyboard or mouse; pushes the monitor away; and gives the patient her undivided attention.” 10 One of the major advantages of the computer for clinical practice and for oncology specialists is the ability to educate patients about their condition and to share information. The physician can point to the screen and offer to visually share test results, lab findings with trends, or x-ray tests. Additionally, information on treatments and possible clinical trials can be found and printed out for the patient. This ability to readily share the information in the EHR is a
major benefit and facilitator of patient engagement.
The transition from paper-based office records to documentation using electronic media has had several unplanned consequences. Physicians are finding themselves spending more time on data entry and looking at computer screens than on focusing on patients. While the EHR has greatly improved the ability to share information and educate patients, it has also had a negative impact on patient centeredness and emotional and psychological communication and the ability to establish a trusting relationship between physicians and patients. This article outlines practical ways to use the computer in a positive way. AUTHOR INFORMATION
Sheree Starrett, MD, MS, is a board-certified hematologist/medical oncologist, recently retired as a medical director with Aetna. She is a member of the National Association of Managed Care Physicians and is currently working as a consultant in managed care. REFERENCES
1. Institute of Medicine. To Err Is Human: Building a Safer Health Care System . Washington, DC: The National Academies Press; 1999.
2. Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century . Washington, DC: The National Academies Press; 2001.
3. Hsiao C-J, Hing E. Use and characteristics of electronic health record systems among office-based physician practices: United States, 2001-2013. NCHS Data Brief No. 143. Hyattsville, MD: National Center for Health Statistics; 2014.
4. Mennemeyer S, Menachemi N, Rahurkar S, Ford EW. Impact of the HITECH Act on physicians’ adoption of electronic health records. J Am Med Inform Assoc . 2016;23(2):375-379. doi: 10.1093/jamia/ocv103.
5. Sinsky C, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med . 2016;165(11):753-760. doi: 10.7326/M16-0961.
6. Babbott S, Manwell LB, Brown R, et al. Electronic medical records and physician stress in primary care: results from the MEMO study. J Am Med Inform Assoc . 2014;21(e1):e100-e106. doi: 10.1136/amiajnl-2013-001875.
7. Shanafelt, TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc . 2016;91(7):836-848. doi: 10.1016/j.mayocp.2016.05.007.
8. Ventres W, Kooienga S, Marlin R, Vuckovic N, Stewart V. Clinician style and examination room computers: a video ethnography. Fam Med . 2005;37(4):276-281.
9. Epstein RM, Street RL Jr; National Cancer Institute. Patient-centered communication in cancer care: promoting healing and reducing suffering.
healthcaredelivery.cancer.gov/pcc/pcc_monograph.pdf. Published October 2007. Accessed October 9, 2017.
10. Duke P, Frankel RM, Reis S. How to integrate the electronic health record and patient-centered communication into the medical visit: a skills-based approach. Teach Learn Med . 2013;25(4):358-365. doi: 10.1080/10401334.2013.827981.
11. Margalit RS, Roter D, Dunevant MA, Larson S, Reis S. Electronic medical record use and physician-patient communication: an observational study of Israeli primary care encounters. Patient Educ Couns . 2006;61(1):134-141. doi: 10.1016/j.pec.2005.03.004.
12. Pearce C, Trumble S, Arnold M, Dwan K, Phillips C. Computers in the new consultation: within the first minute. Fam Pract . 2008;25(3):202-208. doi: 10.1093/fampra/cmn018.
13. Street RL, Liu L, Farber NJ, et al. Provider interaction with the electronic health record: the effects on patient-centered communication in medical encounters. Patient Educ Couns . 2014;96(3):315-319. doi: 10.1016/j.pec.2014.05.004.
14. Erickson S, Rockwern B, Koltov M, McLean R; Medical Practice and Quality Committee of the American College of Physicians. Putting patients first by reducing administrative tasks in health care: a position paper of the American College of Physicians. Ann Intern Med . 2017;166(9):659-661. doi: 10.7326/M16-2697.
15. Ventres W, Kooienga S, Marlin R. EHRs in the exam room: tips on patient-centered care. Fam Pract Manag . 2006;13(3):45-47.
16. Ventres W, Kooienga S, Vuckovic N, Marlin R, Nygren P, Stewart V. Physicians, patients, and the electronic health record: an ethnographic analysis. Ann Fam Med . 2006;4(2):124-131. doi: 10.1370/afm.425.

Download PDF: EHR Documentation and the Patient–Physician Visit
Galvanizing Community Oncology Through Advocacy, Empowerment, and Stewardship
Coverage from the Community Oncology Alliance Community Oncology Conference, held April 4-5, 2024, in Orlando, Florida.

Examining Low-Value Cancer Care Trends Amidst the COVID-19 Pandemic
On this episode of Managed Care Cast, we're talking with the authors of a study published in the April 2024 issue of The American Journal of Managed Care® about their findings on the rates of low-value cancer care services throughout the COVID-19 pandemic.

Implementing Treatment Escalation Plans in Oncology Care at Admission Boosts Uptake, Study Finds
Treatment escalation plans can successfully be implemented into routine oncology practice, according to one study.

Oncology Onward: A Conversation With Penn Medicine's Dr Justin Bekelman
Justin Bekelman, MD, director of the Penn Center for Cancer Care Innovation, sat with our hosts Emeline Aviki, MD, MBA, and Stephen Schleicher, MD, MBA, for our final episode of 2023 to discuss the importance of collaboration between academic medicine and community oncology and testing innovative cancer care delivery in these settings.

Center on Health Equity and Access: April 2024

Office Procedures for Older Adults by Physician Associates and Nurse Practitioners
The authors probed Medicare Part B data to explore outpatient clinical procedures performed by physician associates and nurse practitioners and report the trends from 2014 through 2021.
2 Commerce Drive Cranbury, NJ 08512
609-716-7777
myPatientVisit Portal
About this app
Data safety.
Ratings and reviews
- Flag inappropriate
What's new
App support.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
You Can Now Access Your Health Records Digitally
Solskin / Getty Images
Key Takeaways
- Under new federal rules from the 21st Century Cures Act, healthcare organizations must give patients access to their health records in an electronic format.
- Experts say this will benefit patients because it will give them information that can help them make informed decisions about their care.
- Provider portals are the main way to request health care records, but there are other ways to get access including through third-party apps and organizations or even via email.
Medical providers and healthcare organizations must now give patients electronic access to their health records under new federal rules that went into effect on Oct. 6.
The rules—passed under the 21st Century Cures Act —was designed to increase access and exchange of electronic healthcare information without delay and allow patients to choose who to share their data with.
Before the new rules, patients may not have been able to see edits or updates to their records, including notes from nurses and doctors regarding surgeries, information on their medication history, images from screenings, or even results for certain procedures.
The new policies will benefit patients and providers who “may need to receive information from across the country from another hospital system,” according to Elise Anthony, JD , executive director of policy at the Office of the National Coordinator for Health Information Technology (ONC).
“We’re really excited to see the progress that’s being made and has been made around the sharing of data and how it supports patients,” Anthony told Verywell.
How Does Better Data Access Benefit Patients?
Patients have had the right to request a copy of their medical records either on paper or electronically since the passage of the HIPAA Privacy Rule in 1966.
However, the purpose of the new rules is to create a better system for information exchange between patients and their providers, according to Ben Teicher, associate director of media relations for the American Hospital Association .
“For many patients with chronic conditions or other reasons for frequent visits to different providers, it is hard to keep everyone up to speed on the latest changes in their health, changes in medications or other developments,” Teicher told Verywell in an email.
But the increased accessibility to digital health records could potentially lead to patient confusion or distress, especially for test results that don’t have any context.
"Test results can come back at any time, including off hours and weekends,” said Karen Bogard, RHIA, MHA , a senior manager in data and record integrity senior manager at Mass General Brigham.
But experts generally agree that accessibility and standardization of medical records are necessary for patients to understand information related to their own health.
“For patients with a long and complex medical history, it may be helpful for them to have access to notes from their care team to help them better understand and make informed decisions about their care,” Bogard said.
How Can You Get Your Health Records Digitally?
According to Kathryn Marchesini, JD , chief privacy officer at the ONC, patients can get their health records from their providers in most cases.
She said some providers will have an online portal that displays lab results, medication summaries, and immunization records. Patients will be able to request their records through these online provider portals.
Patients may also have to fill out a form, often called a health or medical record release form to receive health records. In addition, other providers may require patients to submit a letter via email, mail or fax requesting their records.
“A healthcare provider could require an individual to request access in writing and it could be done through electronic means,” Marchesini told Verywell. It’s important to note that a provider cannot enforce unreasonable barriers that deny or delay access to patient records.
Anthony added that some patients can request their records through a third-party app or organization. In some cases, the records can be sent via email or other ways if both patients and providers agree to that method.
“If some patients see many different providers and would like to see their information in one place and an app can support that, they may prefer that option,” Anthony said.
However, Marchesini warned that some third-party organizations are not HIPAA-covered entities, which means they may not have strict privacy and security standards.
It might take a while for providers to comply with the new rules and establish standardized health data, but the new regulation is the first step in giving patients more control of their own data.
“Having the ability of patients and providers to have that conversation and for that information to move, even if it is not standardized, is important,” Anthony said. “We want to support the ability of patients to receive information in different ways, sometimes it’s a portal, sometimes it’s a third-party app, sometimes it might be another means as well.”
What This Means For You
Health plans and providers including clinics, hospitals and doctor’s offices must provide patients access to their health records in a digital format under the federal law called Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule. Patients can get their records in different ways, mainly through a provider portal.
Department of Health and Human Services. Your rights under HIPAA .
By Alyssa Hui Hui is a health news writer and former TV news reporter. She was the 2020 recipient of the Midwest Broadcast Journalists Association Jack Shelley Award.
- Solutions Solutions
- Who We Serve Who We Serve
- Resources Resources
- Company Company
An all-in-one practice management solution that delivers comprehensive EHR, RCM, and patient engagement software and services.
A connected, tailorable EHR solution that empowers clinicians.
RCM software and services that boost efficiency and profitability.
Communication and care tools that improve patient relationships.
Technology that helps improve patient outcomes and reduce costs.
Expert consulting and support to help improve performance and ROI.
Easily connect to athenaOne and extend its capabilities.
Tailor your athenahealth experience with industry-leading partners.
Enterprise RCM software that maximizes collections with less work.
- Provider Organizations Startup Practices Small Medical Practices Medium to Large Medical Groups Enterprises & Health Systems Federally Qualified Health Centers Member-centric Care Organizations
- Medical Specialties Behavioral Health Orthopedics Pediatrics Primary Care Urgent Care Women's Health View All Specialties
- Other Organizations Healthcare Payers Labs and Imaging Centers
- Partners Marketplace Partners Developers
- Thought Leadership Our Insights
- Resources Case Studies
- About athenahealth Who We Are Leadership athenaGives
- Join Us Contact Us Careers
- In the News Newsroom Press Releases

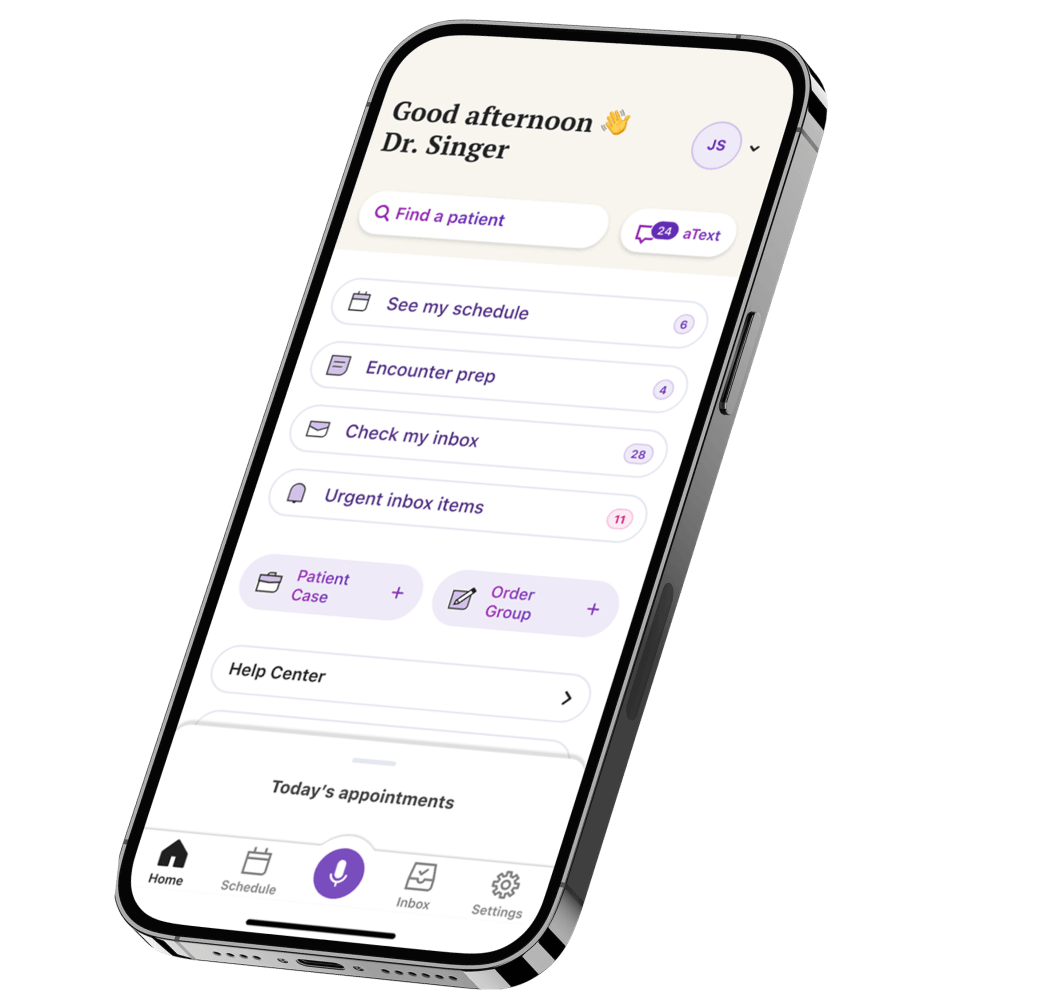
Electronic Health Records
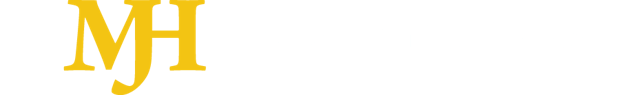
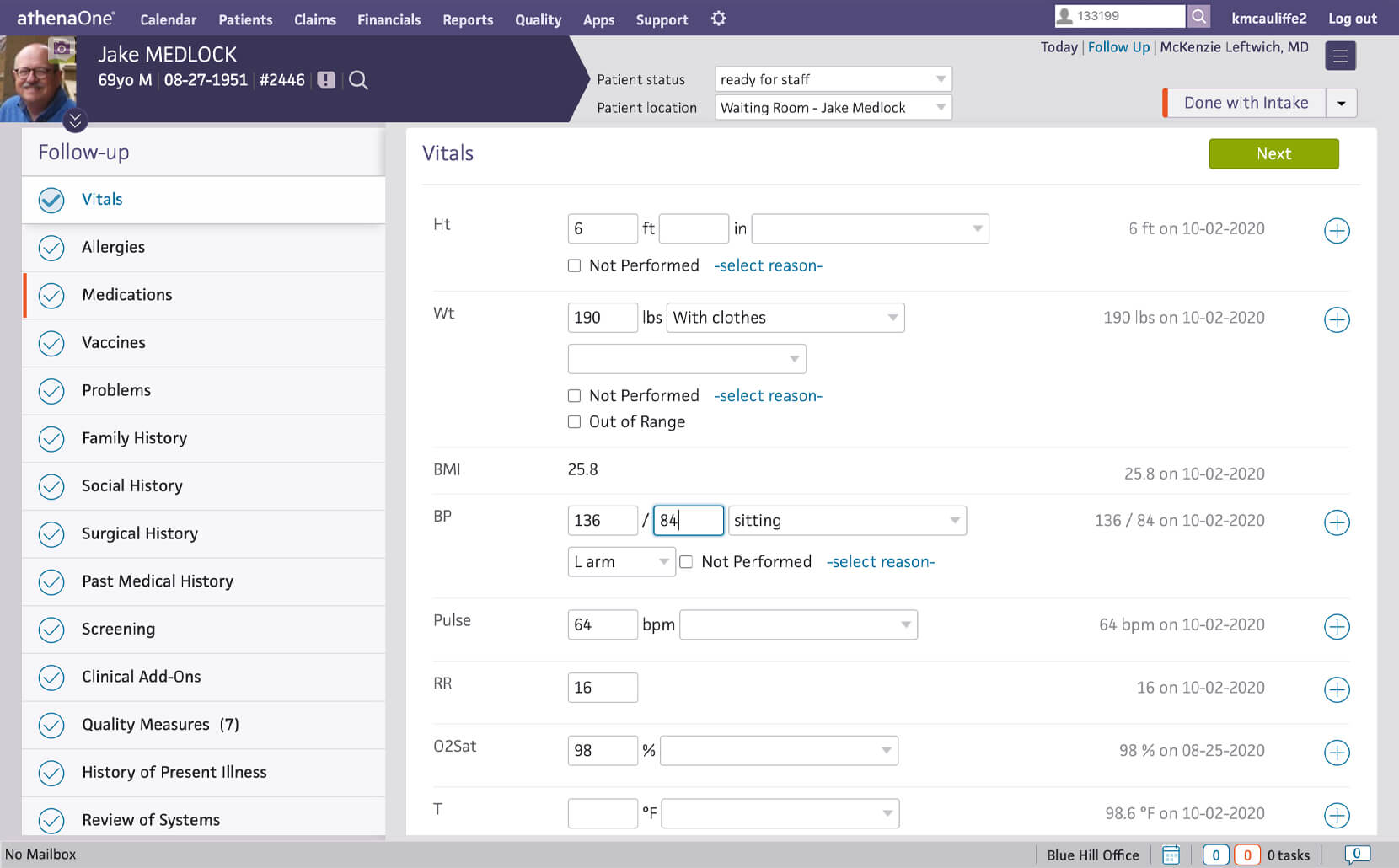
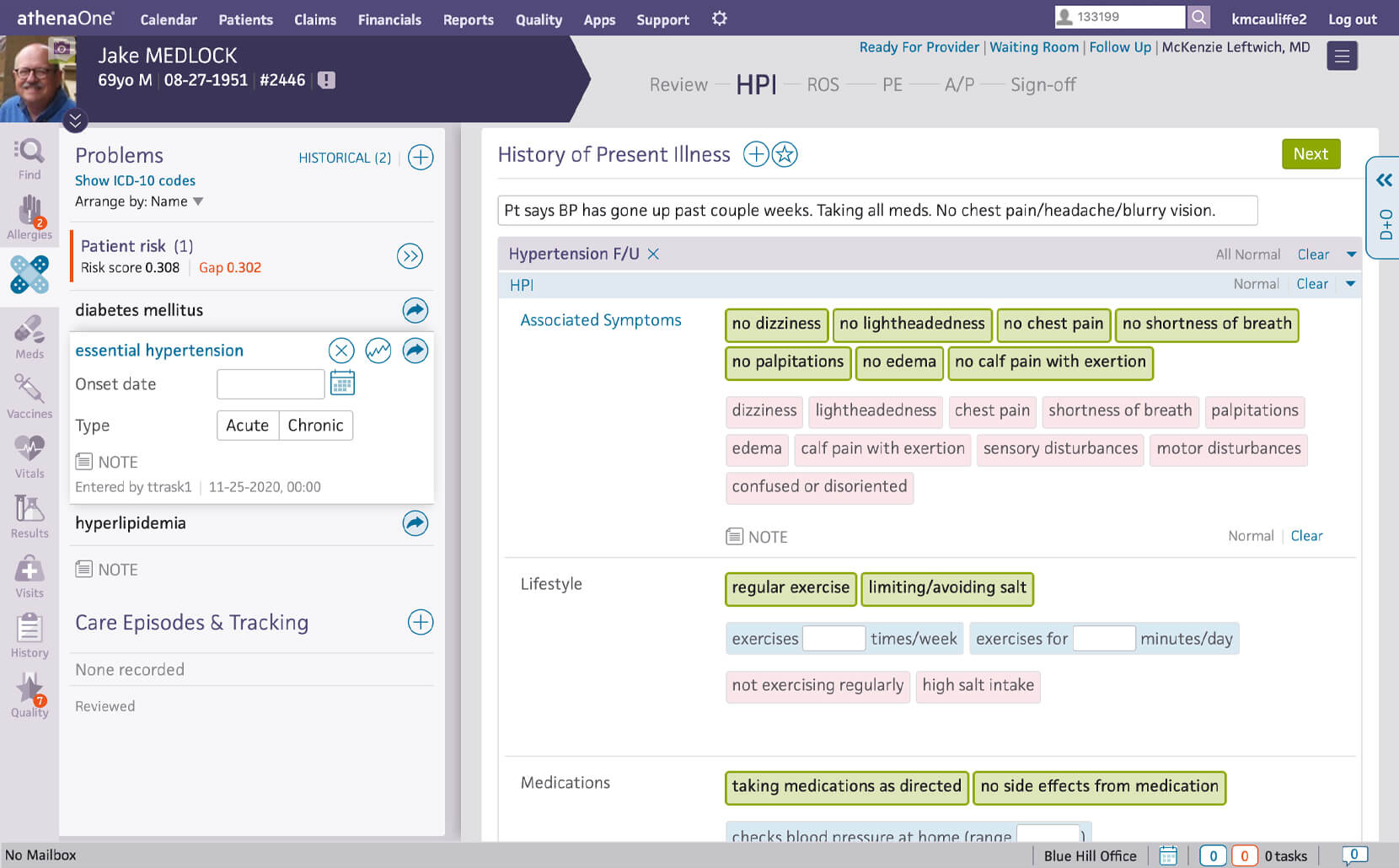
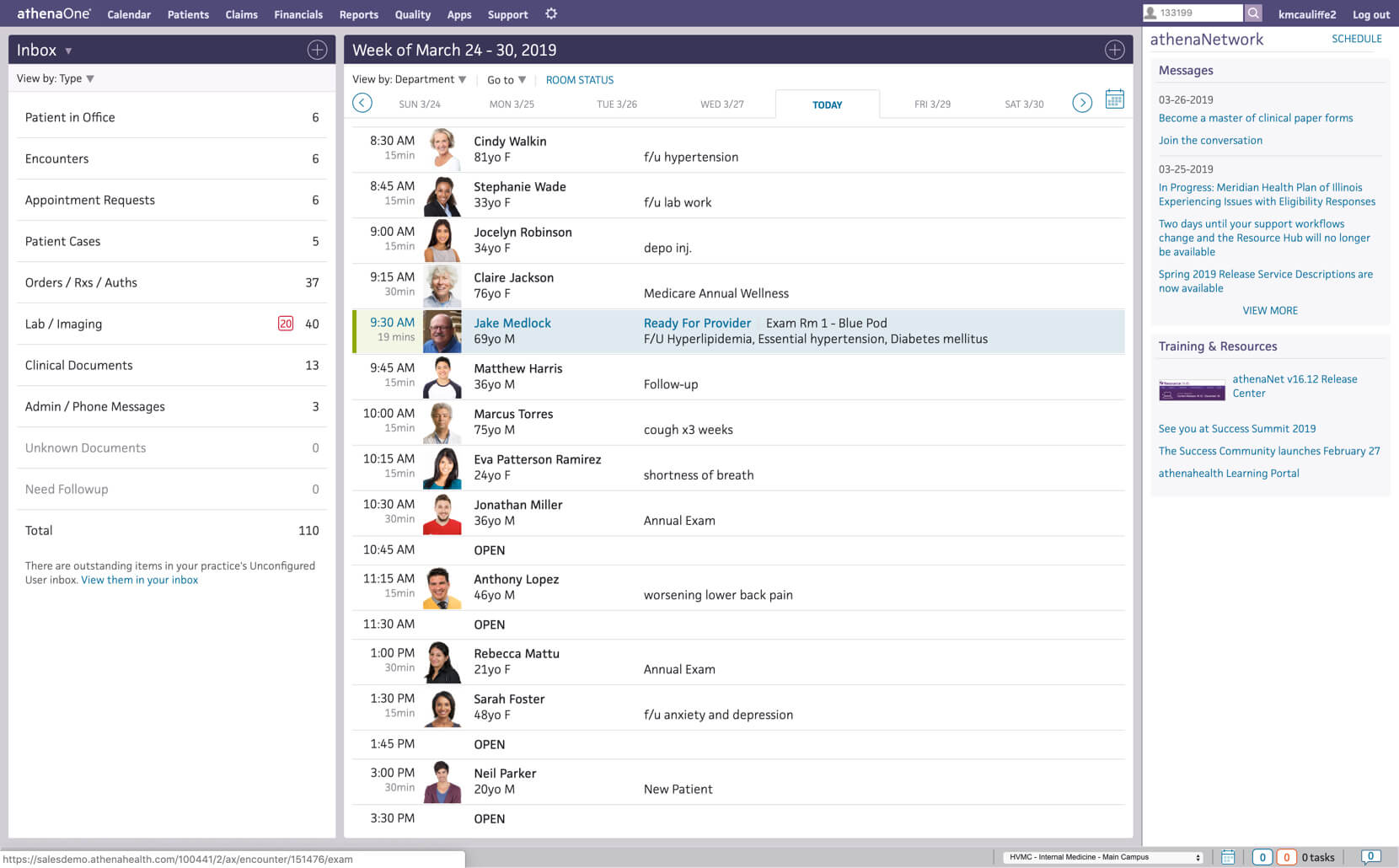
An ehr that lets you focus on delivering care, athenaone’s electronic medical records capabilities make it easier to document patient encounters and deliver exceptional care ., improve the encounter experience for clinicians and patients.

Simplified documentation
Reduce distractions and documentation time during patient encounters with an EHR that up-levels the clinician experience.
Customizable features like best-practice templates, macros, accelerators, Pre-Encounter Prep, and Focused Encounter help reduce documentation time.
The documentation process can be easily tailored to support the needs of specialties.
Give physicians the ability to document encounters on the go using their existing customized macros, templates, and order sets with the athenaOne app.
Get real-time patient data and insights from our network surfaced in your standard workflows.
Perform clinical work on the go
Give physicians the ability to perform meaningful clinical work from their mobile devices with this fully integrated extension of our EHR.
View your day through our EHR workflows
Review your patient’s history at a glance
Get an easy-to-read summary of your patient’s record so you’re fully prepared for the encounter.
Designed to help you focus on the patient
Get support from your staff in areas like vitals with smart workflow delegation.
Document encounters your way
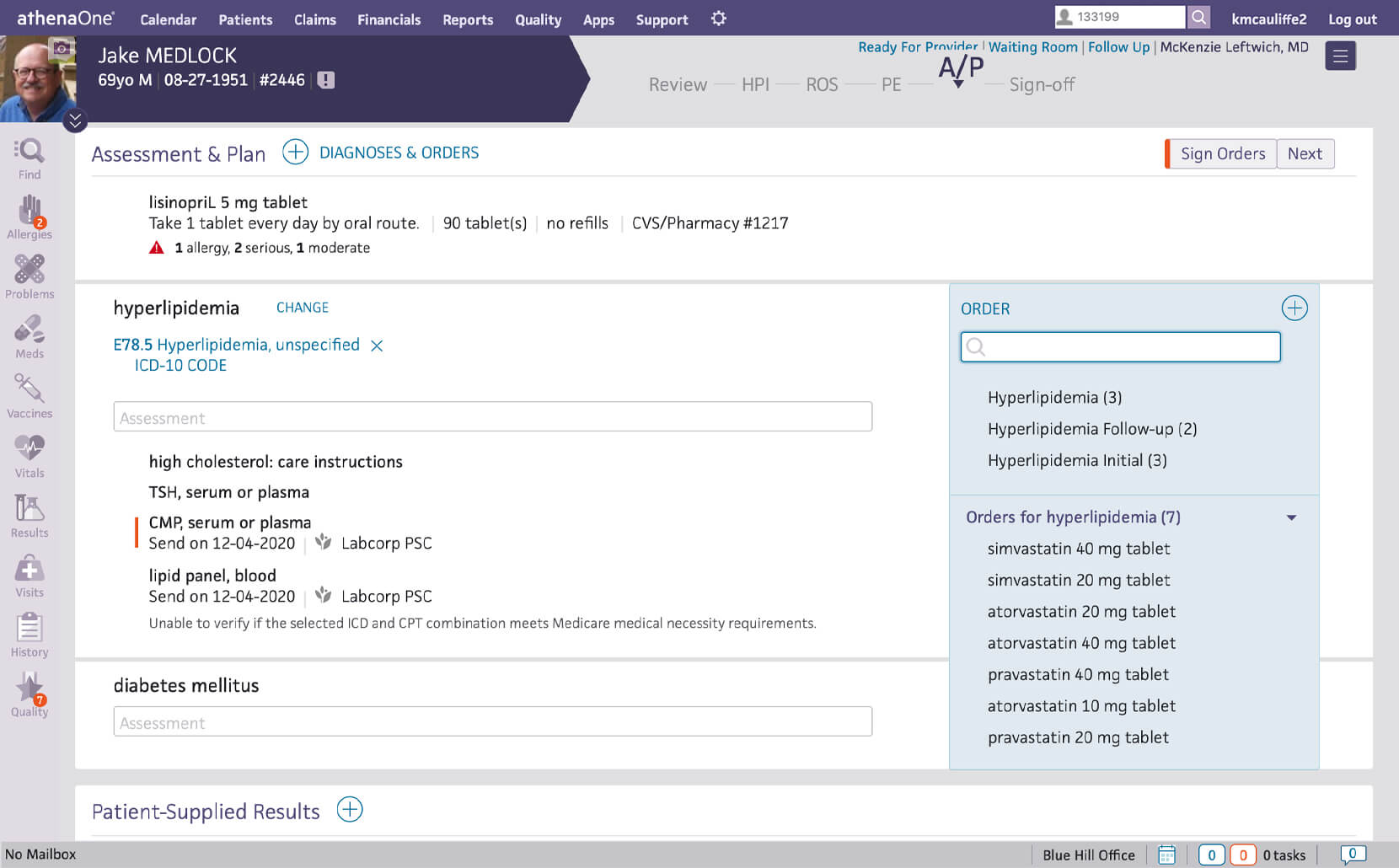
Write and save notes the way you prefer for typical encounters and diagnoses.
Ordering made easy
Add diagnoses and orders during the patient encounter. Everything flows into a cart for your review at the end.
See our EHR in action
Get an inside look at how athenaOne organizes the visit and helps you document faster and more accurately.
These fully integrated services build on athenaOne’s EHR software, enabling more efficient daily workflows and extraordinary care delivery.
Dr. Ashish Parikh, Chief Quality Officer,
Summit Health
Here’s how customers rate us

athenaOne—the solution to healthcare complexity and performance
Explore how athenaOne’s comprehensive EHR, RCM, and patient engagement capabilities simplify clinical complexity while helping drive organizational success.
Patient Portal
myPatientVisit Login
The myPatientVisit login portal is an online service portal that will allow you 24/7 access to your health information made available to your by the practice. Once logged in to your personal account, you will be able to request a new appointment, Pay your medical bills, see your upcoming appointments, access reports, lab results, Clinical Document Architecture (CDA) and your demographic information.
Many providers now offer patient portals. For access to the myPatientVisit Login Portal, you will need to set up an account. The service is free. A password is used so that all of your information is private and secure.
How Does myPatientVisit Patient Portal Work?
myPatientVisit Patient Portal eliminates time-consuming phone calls and provides you with 24/7 online access to your doctor’s office. It’s easy, secure, and safe to use myPatientVisit. Your information will be accessible only to you. Use secure email to communicate with your provider online.
How Your Account is Protected
Nextech have taken extra steps to ensure that your private health information remains confidential. Your records are safe from unauthorized access because the My Patient Visit patient portal is password-protected and information is delivered via an encrypted connection.
All communication between you and Nextech using My Patient Visit is carried over a secure, encrypted connection. Encryption means the information is encoded in such a way that no one can read it during transmission. Also, your health records are stored behind a firewall to prohibit unauthorized access.
In addition, My Patient Visit access requires a unique username and password. The MyPatientVisit patient portal is owned and operated by Nextech and is fully compliant with federal and state laws pertaining to your privacy. Your name and email address will be kept private and confidential and will never be sold or released by Nextech.
If you learn or suspect that your username or password has been wrongfully used or disclosed, you should promptly notify us and immediately reset your password. To help ensure the security of your password or account, please sign out of your account at the end of each session.
The myPatientVisit Login portal is available 24 hours a day, seven days a week for patients. Each patient will be given their user account credentials through which all the administrative matters can be accessed and managed.
If you are a new user and have not yet created an account, please select the option at the bottom of the initial login screen for “Create an account”. You will then be guided through creating a login for our site. You can either register using your email address that you provided to the office or you can register by creating a username and entering a security code provided to you from the office.

You can access the Portal through these means:
- Log in and create account through text message or email sent at time of scheduling.
- Go to https://www.mypatientvisit.com/#/login to your browser.
- Enter your username and password.
- Click on login
When you select the “ Remember Me ” check box and then log in, your username is encrypted and stored on the computer you are currently using. The next time you log in, the system will prefill your username and you only need to enter your password (which, for security reasons, is never saved) to log in.
Important: Because “ Remember Me ” stores your username on the computer you’re using, do not use this feature on public computers (such as those in a library or internet cafe).
On the Dashboard:
- See your Upcoming Appointments – Date & Time, Provider and Purpose of Visit
- Pre-Register – Click the button to fill out the Patient Demographics Information & Insurance Information
- Send a Message – Click the Send a Message button to send secure message to your practice.
- Add a profile picture by clicking on the Camera icon
- See your account balance
- See your last visit and upcoming visit dates
- Patient Information: Fill out your Patient Demographic information
- Insurance Information: Fill out your insurance information
myDocuments:
- Clinical Summary Documents on file
- Patient Documents on file
- Forms: Fill out and complete forms required for patient visit.
myMessages:
- Send and Review Messages: A way to securely send and receive messages from you care provider(s)
myAccounts:
- Connect to a different practice: Allows you to connect to your other care provider that is using MPV
MyPatientVisit Bill Pay
Bill Payments made convenient! This is a service which provides businesses with the ability to generate bills for their customers to make payment of what is due. ExpressPay provides bill pay services to Banks, Utility services providers and more.
Want to Pay a Bill?
- Go to the MyPatientVisit login page
- Click/Tap on ” Bill Pay“
- Practice ID
- Patient Account #
- Patient Last Name
- $ Payment Amount
- Accept Terms of Use
myPatientVisit App
The myPatientVisit mobile app is a patient-centered platform that allows patients to access their healthcare information and communicate with their provider’s staff from their mobile devices. The app is optimized for mobile use and provides a user-friendly interface for patients to check their balance, view upcoming appointments, and chat with their provider’s team.
The myPatientVisit App for iPhone and iPad also includes a new feature called “ I’m Here, ” which allows patients to inform the office staff that they have arrived for their appointment and begin a chat with their provider’s team.
Need help with Your Login?
What if I don’t know my username? From the Login Page, Click the link “Need help with Login?” From the “FORGOT LOGIN CREDENTIALS” Page > Select the “Forgot Username”. Follow prompts to complete. If you are still having issues please contact care provider’s office
What if I forgot my password? From the Login Page, Click the link “Need help with Login?” From the “FORGOT LOGIN CREDENTIALS” Page > Select the “Forgot Password”. Follow prompts to complete. If you are still having issues please contact care provider’s office.
What if I forgot my Username & Password? From the Login Page, Click the link “Need help with Login?” From the “FORGOT LOGIN CREDENTIALS” Page > Select the “Forgot Username & Password”. Follow prompts to complete. If you are still having issues please contact care provider’s office.
Why can’t I login? Please read the error messages carefully and complete the required information. If the issue continues, please contact your practice.
On this Page
Appointments at Mayo Clinic
- Consumer health
- Personal health records and patient portals
Personal health records and patient portals are powerful tools for managing your health.
If you're like most people, you have a number of health concerns and may visit multiple doctors and pharmacies. Keeping track of it all can be a challenge. With a personal health record, you can gather — and manage — all that information in one easily accessible location.
What is a personal health record?
A personal health record is simply a collection of information about your health. If you have a shot record or a folder of medical papers, you already have a basic personal health record.
And you've probably encountered the big drawback of paper records: You rarely have them with you when you need them.
Electronic personal health records (PHRs) remedy that problem by making your information accessible to you anytime via web-enabled devices, such as computers, smartphones and tablets.
What information goes into a PHR?
In general, your PHR needs to include anything that helps you and your doctors manage your health — starting with the basics:
- Your doctor's names and phone numbers
- Allergies, including drug allergies
- Your medications, including dosages
- List and dates of illnesses and surgeries
- Chronic health problems, such as high blood pressure
- Living will or advance directives
- Family history
- Immunization history
You can also add information about what you're doing to stay healthy and prevent disease, such as:
- Home blood pressure readings
- Exercise and dietary habits
- Health goals, such as stopping smoking or losing weight
PHRs, EHRs and patient portals
PHRs are not the same as electronic health records (EHRs), also called electronic medical records (EMRs), which are owned and maintained by doctors' offices, hospitals or health insurance plans.
EHRs typically contain the same basic information you would put in a PHR , such as your date of birth, medication list and drug allergies. But EHRs contain more extensive information because they're used by health care providers to store visit notes, test results and much more.
A PHR that is tied to an EHR is called a patient portal. In some but not all cases you can add information, such as home blood pressure readings, to your record via a patient portal. If that's the case, you may not want to create a separate, standalone PHR .
However, you may want to consider having at least some basic information on hand in case of emergency, including advance directives, which outline your decisions about health care, such as whether to use life-support machines.
You could use an app such as the Health app for iPhones, which includes Medical ID, which makes critical information available via the lock screen for use by first responders in an emergency. Medical ID can display medical conditions, allergies, medications, blood type and emergency contacts. You can also use it to indicate if you're registered to be organ donor.
It is important to make sure any apps you use are secure so that your information is kept private. Make sure any app you use requires you to enter a password and that your phone has a firewall or encryption software. Research all apps before you download them to your phone and enter your personal information.
Similar apps are available for other smartphones as well. Or you could go low tech and keep a card in your wallet or wear a medical alert bracelet.
What are the benefits of a PHR?
Having a PHR can be a lifesaver, literally. In an emergency you can quickly give first responders vital information, such as diseases you're being treated for, medications you take, drug allergies, and contact information for your doctor.
If you see multiple doctors and they don't use the same EHR system, a PHR is a good way to keep all of your health information in one place.
A PHR also empowers you to manage your health between visits. For example, a PHR enables you to:
- Track and assess your health. Record and track your progress toward your health goals, such as lowering your cholesterol level.
- Make the most of doctor visits. Be ready with questions for your doctor and information you want to share, such as blood pressure readings since your last visit.
- Manage your health between visits. Upload and analyze data from home-monitoring devices such as a blood pressure cuff. And remind yourself of your doctor's instructions from your last appointment.
- Get organized. Track appointments, vaccinations, medications and preventive or screening services, such as mammograms. In fact, studies have shown when parents use personal health records for their children, the children are more likely to get their preventive well-child checkups on time.
Are there drawbacks to PHRs?
Building a complete health record takes some time. You have to collect and enter all your health information. Only a minority of doctors, hospitals, pharmacies and insurance companies can send information electronically to a PHR that isn't part of a patient portal.
In most cases, you will have to update your PHR manually each time you see the doctor, fill a prescription, have a test or go to the hospital.
Even if you use a patient portal, you still need to review the information that's added to it. The process of transferring health data electronically isn't always perfect and mistakes can happen.
Will my information be kept private?
Perhaps the most common concerns about PHRs are about privacy and security. To address these issues, reputable PHR systems follow industry best practices, such as making their privacy policies public and submitting to monitoring by independent organizations. In addition, federal laws have been put in place to protect the security of personal health information.
How do I get started?
If your primary care doctor offers a patient portal, use it. The staff at the front desk should be able to tell you how to register for it. (If your doctor doesn't offer one, ask if one will be available in the future.) Then start taking advantage of its features. Most portals offer the following:
- Appointment reminders
- Medication list
- Appointment summaries, sometimes with associated educational material
- Secure messaging with your provider
- Test results
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Individuals' right under HIPAA to access their health information. U.S. Department of Health and Human Services. https://www.hhs.gov/hipaa/for-professionals/privacy/guidance/access/index.html. Accessed Dec. 12, 2019.
- What are the benefits of personal health records? HealthIT.gov. https://www.healthit.gov/faq/what-are-benefitspersonal-health-records. Accessed Dec. 12, 2019.
- What are the differences between electronic medical records, electronic health records, and personal health records? HealthIT.gov. https://www.healthit.gov/faq/what-are-differences-between-electronic-medical-recordselectronic-health-records-and-personal. Accessed Dec. 12, 2019.
- Device software functions including mobile medical applications. U.S. Food and Drug Administration. https://www.fda.gov/medical-devices/digital-health/device-software-functions-including-mobile-medicalapplications. Accessed Dec. 12, 2019.
- How can you protect and secure health information when using a mobile device? HealthIT.gov. https://www.healthit.gov/topic/privacy-security-and-hipaa/how-can-you-protect-and-secure-health-information-whenusing-mobile-device. Accessed Dec. 12, 2019.
- Empower your patients with health records on iPhone. Apple. https://www.apple.com/healthcare/health-records/. Accessed Dec. 12, 2019.
- McBride S, et al., eds. Personal health records and patient portals. In: Nursing Informatics for the Advanced Practice Nurse: Patient, Quality, Outcomes, and Interprofessionalism. 2nd ed. Springer; 2019.
- Grossman LV, et al. Interventions to increase patient portal use in vulnerable populations: A systematic review. Journal of the American Medical Informatics Associations: JAMIA. 2019; doi:10.1093/jamia/ocz023.
- Abd-Alrazaq AA, et al. Factors that affect the use of electronic personal health records among patients: A systematic review. International Journal of Medical Informatics. 2019; doi:10.1016/j.ijmedinf.2019.03.014.
- Mobile devices and health. New England Journal of Medicine. 2019; doi:10.1056/NEJMra1806949.
Products and Services
- The Mayo Clinic Diet Online
- Assortment of Health Products from Mayo Clinic Store
- A Book: Mayo Clinic Family Health Book, 5th Edition
- A Book: The Mayo Clinic Diet Bundle
- A Book: Live Younger Longer
- A Book: Mayo Clinic Book of Home Remedies
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- A Book: Mayo Clinic on Digestive Health
- Myths about cancer causes
- Emergency essentials: Putting together a survival kit
- Emergency health information
- Kidney donation: Are there long-term risks?
- Living wills
- Organ donation: Don't let these myths confuse you
- Osteopathic medicine
- Telehealth: Technology meets health care
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Make twice the impact
Your gift can go twice as far to advance cancer research and care!

Applying even one of these 10 strategies can help you reduce frustration, improve productivity, and get home earlier.
JAY WINNER, MD, FAAFP
Fam Pract Manag. 2020;27(4):5-10
Author disclosure: no relevant financial affiliations disclosed.
© 2020 Jay Winner, MD, FAAFP
INSIDE: Computer setups for exam rooms and televisits
Many physicians consider electronic health record (EHR) documentation to be a main source of burnout. 1 In fact, recent increases in physician burnout have coincided with the widespread adoption and use of EHRs. Even among those who aren't experiencing burnout, it's rare to find a doctor who is not experiencing some degree of frustration with the EHR. Poorly designed and poorly implemented EHRs are to blame, and continued advocacy is needed to improve these problems. In the meantime, there are strategies all physicians can use to become more efficient with electronic documentation — strategies that can help reduce frustration, improve productivity, and reduce work after clinic.
While not every strategy described in this article may be applicable to your practice, and you may already use others, if you find even one or two new strategies to help you get home a little earlier every day, reading this article will be time well spent.
Electronic health records (EHRs) are a major source of frustration and even burnout for physicians, but there are strategies physicians can use to make EHR documentation more efficient.
The overarching goal is to finish most, if not all, documentation during the visit so that you have little or no work after clinic.
Strategies include adopting a more efficient EHR setup in the exam room, using templates, smart phrases, and patient questionnaires, and writing shorter notes.
THE GOAL: FINISH MOST (IF NOT ALL) DOCUMENTATION DURING THE VISIT
Before I began using my current EHR system, my documentation routine was to take handwritten notes during a visit. At some point after the visit, I would dictate the visit, which would later be transcribed for documentation. If I was running behind, it was very easy for those dictations to stack up. At the end of a shift, I might have a half day of documentation to complete. At the end of particularly busy days, I might have almost an entire day of dictations left to do. Seeing a tall stack of charts and many undictated notes on my desk was, by far, my least favorite part of thsse day. Completing those notes was the task I most dreaded.
Today, when I finish the visit, my note is done. Those days of stacks of unfinished records are just bad memories. I spend less time documenting, and I get paid for more of my work. In the past, if I used CPT time-based coding, I could not count the extra five minutes of dictating that I completed after the patient left. Now, because I do all my documentation with the patient in the exam room, any time that I do spend is potentially billable.
Here are 10 strategies that have helped me become more efficient and could help you too, no matter which EHR system you use.
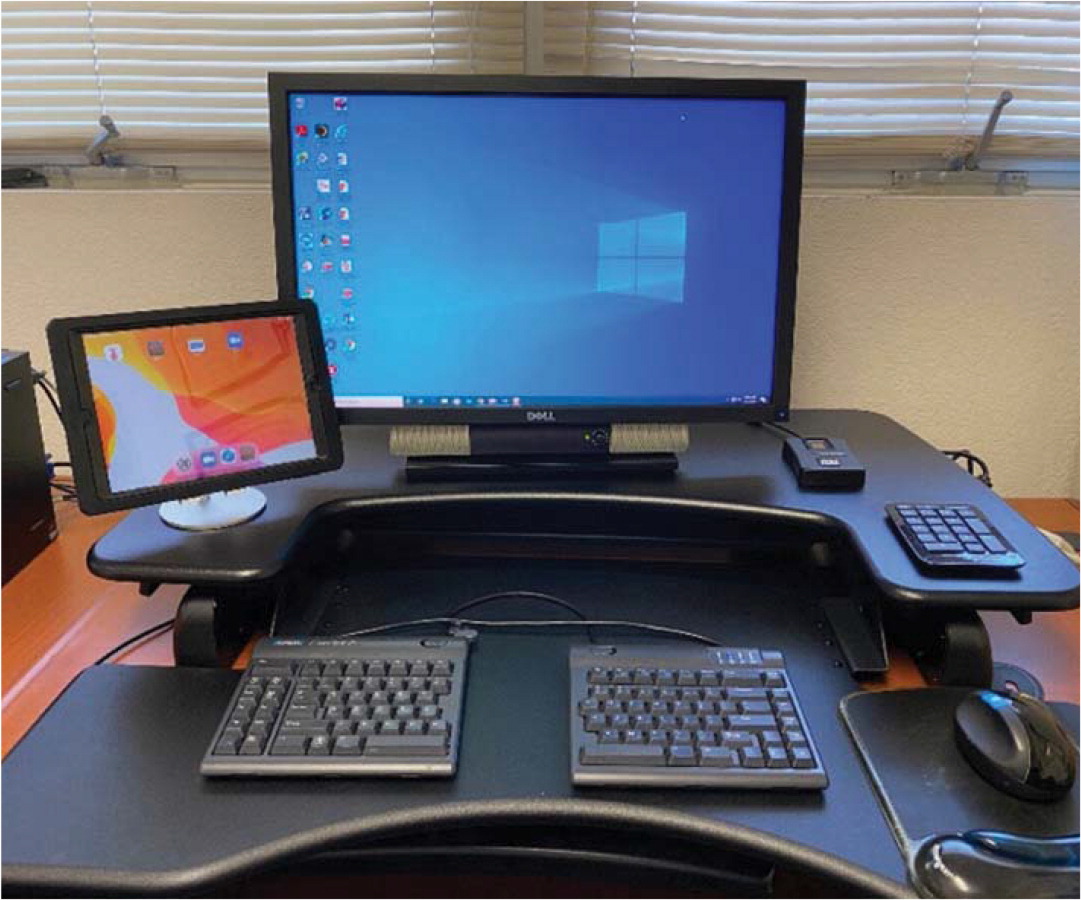
1. Rethink your exam room setup . Ideally, you should place the computer where you can alternate between looking at the screen and looking at the patient with only a small shift in your gaze. There are a variety of exam room setups that will work ( see the first photo below ). The key is to avoid setting up the room so that your back is to the patient, because you'll lose the ability to pick up important nonverbal communication and you'll potentially get a sore neck from frequently turning your head. Having a laptop computer or a monitor that swivels makes it easier to show the patient information on the computer screen. Some practices even put their computer workstations on wheels and make them wireless so the entire setup can be moved around as needed.
When you are doing a televisit, the best setup involves two screens — one screen (perhaps a tablet) that displays the patient and a larger screen that displays the EHR for documentation ( see the second photo below ). Again, with only a small shift in your gaze, you should also be able to change your focus back and forth between the patient and the EHR.
COMPUTER SETUPS FOR EXAM ROOMS AND TELEVISITS
For a face-to-face visit, place the computer in a location where you can easily see your patient and your EHR screen without having to turn your head. Do not place the computer in a location where your back would be facing the patient. With the setup shown below, note that whether the patient is seated in the chair or on the exam table, only a small shift in gaze is needed to document in the EHR. I usually ask the patient to sit in the chair at first (further away) until the exam, which has been helpful during the pandemic.

For a televisit, use two screens (one with the patient and the other with the EHR) so you can easily shift your gaze back and forth as needed. In the setup shown below, the iPad is being used for video-conferencing. Note that the camera lens of the iPad is nearest to the computer used for documentation, so only a minimal shift in gaze is needed to look into the camera.
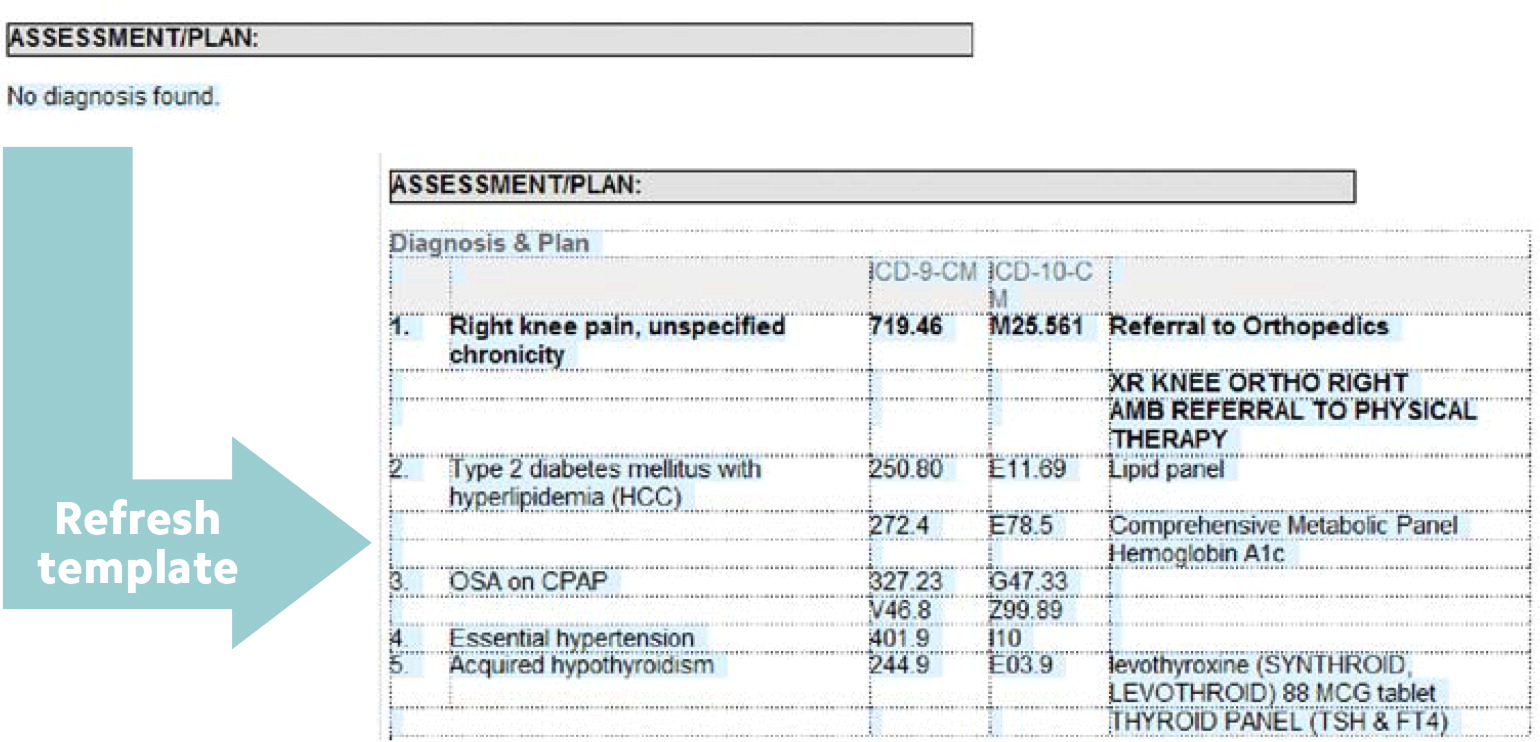
2. Maximize your use of templates and smart phrases . Templates should be used for physicals, routine office visits, televisits, procedures, patient instructions, specific parts of exams (e.g., knee exams), and lists of numbers (e.g., most recent blood pressure readings, weights, A1Cs, thyroid stimulating hormone levels). This eliminates the need to type out words or phrases that you use repeatedly. Learn how to quickly turn part of a note into a template, or how to insert smart phrases into your notes. Ask to use your colleagues' templates, download FPM 's spreadsheet of smart phrases , or browse the sample templates and phrases I've created, all of which you can copy or modify for your practice.
One of my favorite templates provides an automatic list of the patient's diagnoses and associated orders. I use Epic, but many other EHRs have this function as well. I can insert this template into the assessment/plan, and then I only have to type in a few details at the end to complete this part of the note (see “ A sample template ”).
A SAMPLE TEMPLATE
The author's EHR offers a template that provides an automatic list of the patient's diagnoses and associated orders, which he inserts into the assessment/plan to reduce the amount of typing needed to complete this part of the note.
3. Learn to type quickly or use a typing assistant in the exam room . Typing skills allow you to document electronic notes as quickly as handwritten notes — with no additional time spent dictating after the visit. There are free online typing games to help you get faster and more accurate (just Google “free online typing game”). If you don't want to type, consider using a scribe or an extra medical assistant to help with documentation (more on that later in the article).
4. Document the history of present illness (HPI) with understandable notes . Do not type long paragraphs. It takes far too long to write the detailed histories many of us were taught as medical students, and your colleagues do not want to spend time reading your lengthy prose. Sentences are for novels and prisons, not for documenting a medical visit. Instead, for each complaint, type short phrases separated by a semicolon (the key directly under your right pinky finger on the keyboard), and when you need to document a separate complaint, move your pinky over two spaces and hit the enter/return key. (See the example, “ Documenting the HPI: 637 characters vs. 153 characters .”)
DOCUMENTING THE HPI: 637 CHARACTERS VS. 153 CHARACTERS
5. Use the problem list to quickly document your follow-up of chronic problems . My templates for both office visits and physicals contain a problem list at the end of the HPI. Above the problem list is a short phrase: “Interval history in bold” (for the office visit template) or “In addition to preventive health, we discussed the following problems (in bold)” (for the physical template). If I need to take an interval history to follow up on a chronic problem, I make the problem list editable (a right-click with my EHR) and type brief phrases in bold. For instance, for the problem “diabetes with CKD III,” I might write “fasting FS ave 125; AC lunch ave 130; diet has been good except for Thanksgiving; brisk walking 30 min 4 days/wk.” I'll then type in my smart phrase that will pull up the patient's last few A1C results. Another option, if you cannot make the problem list editable or if you are only covering a couple of the items on a long list, is to write the documentation above the problem list. And if you don't have smart phrases for inserting recent A1Cs or other numerical data, you can simply copy and paste the data from the results section of your EHR. It is not necessary to cover everything on the problem list in a particular visit, of course, but these hints will help with documentation of the chronic problems that you do need to cover. (See the examples in “ Strategies for HPI documentation .”)
STRATEGIES FOR HPI DOCUMENTATION
6. Use patient questionnaires to gather data . For a review of systems (ROS) or other common scenarios (PHQ-9, sleep apnea, adult ADHD screenings, etc.), instead of asking patients every question yourself, have your staff provide them with a brief questionnaire that gathers the data. For example, I use an ROS questionnaire that correlates with my ROS documentation template (both are available for free at https://stressremedy.com/primarycare ). If patients have positive responses, I simply update the template, writing in the positives in bold so they are easy to see. I also use an online questionnaire that allows patients to submit updates to their medical history that I then approve. Online questionnaires, as opposed to paper-based questionnaires, are preferable because they can be used for both televisits and office visits.
7. If you use dictating software, take the time to train it . With a little training, the software will be much more accurate. For example, if the software consistently misrecognizes a word or a command, you can teach it the correct pronunciation or add words or phrases to its vocabulary. You can even train the software to add templates using voice commands. It's time well spent.
8. Streamline patient education . One way to do this is with “copy and paste.” Simply copy parts of the plan (written in lay language) and paste them into the patient instructions. This saves you the time of having to restate and retype the information. Some doctors also speak their instructions out loud to the patient as they type the plan, which provides additional reinforcement.
Another time-saving strategy is to utilize audio or video patient education materials during the visit. For example, if a patient is anxious and I've recommended meditation, I might have the patient listen to a short meditation (see https://stressremedy.com/audio/ or https://www.youtube.com/watch?v=8HYLyuJZKno ) while I finish writing the medical orders. Or if a patient is suffering from panic attacks and I've recommended a video on dealing with panic and anxiety (see https://stressremedy.com/videos ), I might have the patient watch the video while I see my next patient. Then I can come back and finish the visit by answering the patient's questions and collaborating on a final plan.
9. Get help from a superuser or EHR staff . When you feel like you're drowning in computer work, the last thing you might want to do is spend more time working on the computer. However, a little investment in technical education, optimizing your system, or learning the hints that others use can really pay off.
10. Consider using a scribe or team documentation . Primary care offices have typically employed one medical assistant per physician, but some practices have begun utilizing additional staff to help with electronic documentation. Depending on your practice style, practice setting, and comfort with your EHR, using a scribe or team documentation may be extremely helpful. Physicians who use a scribe or team documentation generally are more productive (and get home earlier), and the increase in productivity outweighs the extra staffing costs. For more information, see the FPM article “ Team-Based Care: Saving Time and Improving Efficiency ,” the American Academy of Family Physicians TIPS resource on team documentation , and the American Medical Association's Steps Forward module on team documentation .
PICK ONE STRATEGY
Some of the strategies I've suggested in this article can be implemented immediately in your practice, while others will require more effort. Don't get overwhelmed thinking you have to implement all of the strategies at once. Just pick one to get started. Any time and effort you spend now will pay off later, and eventually you'll have the satisfaction of ending each visit and each workday with your documentation complete.
Landi H. Survey: physicians cite EHRs as biggest contributor to burnout. Healthcare Innovation . July 21, 2018. Accessed May 14, 2020. https://www.hcinnovationgroup.com/clinical-it/news/13030577/survey-physicians-cite-ehrs-as-biggest-contributor-to-burnout
Continue Reading

More in FPM
More in pubmed.
Copyright © 2020 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
- (469) 305-7171
- Request Demo
PRACTICE EHR HELP CENTER
Help center > patient.

Patient Chart Overview
Review most recent visits, upcoming and past appointments, start a new clinical note, or enter charges for a patient visit.
Clinical Workflow Overview
Learn the primary workflows for documenting a patient visit.
Modifying Templates
Learn how to modify a template during a visit or make changes to an existing template.
View the outstanding balance for an individual patient, review statements sent, manage the Advanced Payments received, and post patient payments to the outstanding balance or individual visit.
Review all documents scanned, faxed, migrated, or created within Practice EHR.
Review lab orders and results in Practice EHR.
Ordering Labs/Imaging
Learn the primary ways for ordering ancillary services.
Demographics
Manage patient contact information, referring providers, pharmacy, and other contact information necessary for patient care. Patient forms, letters, and access to the patient portal can also be managed from this tab.
Enter information to assist with claim submission and reimbursement. Case management is initiated and updated from this tab as well as the ability to manually verify insurance eligibility for a given date of service.
Read and respond to all patient messages entered by a staff member or the patient via the portal. Clinical and financial alerts are also managed from this tab.
Medication Overview
Review the medications tab within the patient chart.
Ordering Medications
Learn how to electronically prescribe medications for the patient and review past medications and allergies.
Using an Order Set
Review the primary clinical workflow for an order set.
ADDITIONAL RESOURCES
Latest updates.
The ONE with the latest product enhancements, features and fixes.
The ONE place where all your most common questions are answered.
The ONE source you need for medical industry insights, trends and thought leadership.
Why Practice EHR
Contact client support (469) 305-7171 x 2, help center.
- Latest Updates
- Case Studies
5345 Towne Square Drive Suite 125, Plano, TX 75024
Copyright © 2024 Practice EHR. All rights reserved.
- Privacy Policy

Certification of Health IT
Health information technology advisory committee (hitac), health equity, hti-1 final rule, information blocking, interoperability, patient access to health records, clinical quality and safety, health it and health information exchange basics, health it in health care settings, health it resources, laws, regulation, and policy, onc funding opportunities, onc hitech programs, privacy, security, and hipaa, scientific initiatives, standards & technology, usability and provider burden, what are electronic health records (ehrs), ehrs are, at their simplest, digital (computerized) versions of patients' paper charts. but ehrs, when fully up and running, are so much more than that..
EHRs are real-time, patient-centered records. They make information available instantly, "whenever and wherever it is needed". And they bring together in one place everything about a patient's health. EHRs can:
- Contain information about a patient's medical history, diagnoses, medications, immunization dates, allergies, radiology images, and lab and test results
- Offer access to evidence-based tools that providers can use in making decisions about a patient's care
- Automate and streamline providers' workflow
- Increase organization and accuracy of patient information
- Support key market changes in payer requirements and consumer expectations
One of the key features of an EHR is that it can be created, managed, and consulted by authorized providers and staff across more than one health care organization.
A single EHR can bring together information from current and past doctors, emergency facilities, school and workplace clinics, pharmacies, laboratories, and medical imaging facilities.
Open Survey
- (469) 305-7171
- Request Demo
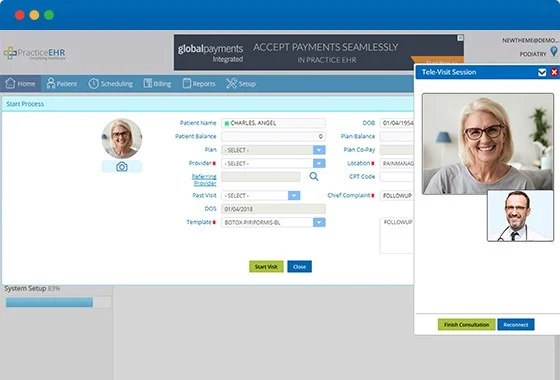
The ONE that offers secure, real-time telehealth visits – anytime, anywhere.

Cost-And-Time Effective
The one that saves time and money..
Telehealth video visits are more efficient and use less resources than in person appointments. Connect with patients through our secure, real-time video technology or a video platform of your choosing, such as Skype, FaceTime or WhatsApp. Practice EHR TeleVisit allows you to provide care anytime, anywhere. Patients can schedule an appointment at their convenience and pay with ease online, reducing the administrative burden on your staff and saving them time.
Animated Text
Integrated patient experience, the one with more satisfied patients..
Give patients the convenient and secure healthcare they want - when and where they want it. TeleVisit also includes an online patient portal for patient appointment requests, messaging, bill pay and more – making the experience easy and convenient for patients and practices, alike. For added convenience, a clinical summary is available at the end of the session on the patient portal.
Simple & Seamless
The one that makes telehealth simple..
With Practice EHR’s TeleVisit feature, adding telemedicine software has never been easier. Your practice can get up and running seamlessly with a telemedicine-specific workflow, templates, check-in process and more – all ready to go with a flip of a switch. Providers can use TeleVisit from within Practice EHR, or as a stand-alone solution.

The ONE that streamlines your workflow.
Practice EHR TeleVisit offers secure, real-time telehealth video sessions integrated with your Practice EHR software. Seamlessly conduct a patient telehealth visit anytime that’s convenient utilizing our intuitive workflow. Providers can conduct video sessions with patients and easily chart the note, prescribe medications and code encounters simultaneously within a single screen, reducing the time spent charting.

What Our Clients Are Saying
I cannot begin to describe how this EHR system has improved my medical practice. Besides being so efficient, I am able to spend quality time with my patients instead of worrying about handwritten notes, appointment mistakes and missing documents. I highly recommend this system to any busy medical practice!
Dr. Ellen Sue Ginsberg, D.O., P.C.
Pain Management Specialist, Bronx, NY
We have been using Practice EHR since January 2016 and are very happy with the program. Practice EHR has enabled us to capture all patient information and billing we may have missed in the past. It has eliminated large amounts of time-consuming paperwork, and it has given me greater control over the practice.
Dr. Henry Hall, D.C.
Co-op City Chiropractic, Bronx, NY
A great EMR and customer service is awesome. From sales on down, working with Practice EHR has been fantastic. I would have no reservations about recommending Practice EHR to anyone looking to start a practice or switch from their current EMR system.
Dr. Justin Rivera, DPM
Valley Foot & Ankle Specialists, Grass Valley, California
Practice EHR is a very efficient EHR system. Very user-friendly and easy to learn. Highly recommended.
Dr. Salman Hassan, M.D. (Pediatrician)
Morris Medical Office, Bronx, NY
The Practice EHR team is very pleasant to work with and they offer an excellent and affordable solution for billing companies and their clients.
David Swiercz, President
HealthCare Automations Inc., Frankfort, IL
We have had a great experience with Practice EHR so far. We switched to Practice EHR 8 months ago and are extremely satisfied with their practice management software. What distinguishes Practice EHR from the rest is its useful training, intuitive interface, and cooperative support team. The onboarding was straightforward, thanks to the support team. I highly recommend Practice EHR to anyone looking for an inexpensive yet efficient EHR system.
Hospital & Health Care
We have recently kicked off our business, and our main concern was to find easy-to-use and inexpensive EHR software. We switched to Practice EHR for its affordable plan that seemed suitable for our new business. Our staff has found their software pleasing to the eyes and simple to use. I will recommend Practice EHR to new practices!
Medical Practice

THE LATEST FROM PRACTICE EHR LottieInteractivity.create({ mode: "scroll", player: "#sixLottie", container: "#sixLottiecontent", actions: [ { visibility: [0, 0.8], type: "seek", frames: [0, 646] } ] });

The Impact of EHR on Cardiology Practice Management
The Electronic Health Records (EHR) are changing how cardiologists work, making complex medical tasks simpler and safer. Imagine this: recent...

Primary Reasons Why Practices Should Be Using a Patient Portal
Healthcare setups are increasingly adopting patient portals to facilitate their patients. Research supports the narrative that patients consider the...

Streamlining Patient Data Management with EHR in Bariatric Clinics
Obesity, a pandemic that has long been overlooked, is rapidly spreading across the globe. Currently, 30% of the global population, or approximately...

How to Navigate the Insurance Reimbursement Process Successfully
The insurance reimbursement process involves hectic paperwork, policies, and patient-testing wait times. Whether you're a healthcare provider or a...

Transform your practice today.
Practice EHR. It’s the ONE.

Or contact our sales team at (469) 305-7171
WHY PRACTICE EHR?
Call us today (469) 305-7171.
- Electronic Health Record
- Practice Management
- Revenue Cycle Management
- Specialty Specific
- Clearinghouse
- e-Prescribing with EPCS
- Electronic Eligibility Verification
- Patient Portal
- Integrated Practice Management and Clearinghouse
- Reports and KPIs
- Patient Check-in Kiosk
- Integrations/Marketplace
- Case Studies
- Why Practice EHR
- Become a Channel Partner
- Become a Reseller
5345 Towne Square Drive Suite 125, Plano, TX 75024
Copyright © 2024 Practice EHR. All rights reserved.

- Privacy Policy

- Getting Started
- Appointment Scheduling
- Prescriptions
- Secure Messaging
- Medical Billing and Claims
- Payment Gateway
- Patient Check-In Kiosk
- Facility / Member Management
- Patient Engagement
Patient Portal
- What is Charm PHR for?
- How do I add a new member to my existing Charm PHR account?
- How do I change the username of my account?
- What is the maximum size of the document that I can upload to my PHR account?
- How do I add another practice to my PHR account?
- How to retrieve my Charm PHR account password?
- Can I create my Charm PHR account?
- How do I communicate with my physician?
- I could not log in to PHR even after providing the proper username/password.
- How do I assist Patients in resetting their passwords?
- I am getting a 'DOB Mismatch' message while registering with the Patient Portal.
- How can a Patient share their lab records from PHR to EHR?
- Why is the Patient unable to fill out a questionnaire from PHR?
What is Charm PHR for? Charm Personal Health Record (PHR) enables users to access and track health records online. Patients and their family members can store and manage their health records under a single PHR account.
Users can access Charm PHR features to:
- Add and manage health records like allergies, clinical problems, and other medical histories.
- Communicate with their Practice or Provider effectively.
- Share their health records with Practice members or others through the mail.
- Book appointments and request medicine or supplement refills.
- Track ailments and the treatment's progress.
- Monitor health vitals and fitness goals.
Charm PHR's HIPAA compliance ensures data protection and accessibility.
How do I add a new member to my existing Charm PHR account? Users can add multiple family members to their PHR account using the following steps:
- Have your family members update the same email ID as yours with their Practices. (These Practices should also be Charm registered)
- Accept their Practice invite.
- Enter their date of birth (mm-dd-yyyy format).
- Click on the 'Next' button to complete their user verification.
- Enter the same 'Username or Email ID' and 'Password' you created previously.
- A warning message with the 'Patient Name' confirming their addition to your PHR account will pop up.
- Click on the 'Submit' button.
Note: The linked family members can view and access each other's clinical information within the account.
How do I change the username of my account? Following our recent update, new users cannot create usernames, and old users cannot edit existing names. However, you can edit your email address if need be.
What is the maximum size of the document that I can upload to my PHR account? You can upload documents that are under 50 MB.
How do I add another practice to my PHR account? You need to register your existing PHR account with multiple Practices using the invitation link received. Please follow the steps below to associate multiple Practices with your PHR account
- Submit the same email-id to the new Practice or Facility registered with Charm.
- Click on the invite link sent to your mail.
- Fill in your date of birth (mm-dd-yyyy format).
- Click on the 'Next' button to complete the user verification.
- A warning message with the 'Practice Name' confirming the addition will pop up.
Note: The Practice should be registered with Charm EHR for this purpose.
How to retrieve my Charm PHR account password? You cannot retrieve old passwords from Charm PHR. Alternatively, you can use the “Forgot Password” link on the login page to create a new password. Click on this link for more info.
Can I create my Charm PHR account? As of now, registration for the Charm PHR account is possible only through the invitation link sent by the Practice. Click on this link for further information.
How do I communicate with my physician? You can communicate with physicians through the ' Messages ' section of the PHR account. Here, you can click 'Compose' to write a message and send it to the Provider.
I could not log in to PHR even after providing the proper username/password. For logging into Charm PHR, you should enable cookies in the browser. The URL available below allows you to confirm if cookies are enabled or not. http://www.whatarecookies.com/cookietest.asp
If you see a message stating 'Cookies are DISABLED in this browser' after connecting, you need to enable cookies to access Charm PHR.
How do I assist Patients in resetting their passwords? You can guide Patients to use the Forgot Password link available on the PHR login page or navigate to https://charmphr.com
- Click on Forgot Password link
- Enter your registered email Address
- Click on the 'Submit' button
Check your inbox for a password reset email and use the link to reset your password.
I am getting a 'DOB Mismatch' message while registering with the Patient Portal. To register for the Patient Portal successfully, please ensure that the date of birth (DOB) you enter matches the DOB recorded in your Practice's records. You can contact your Practice to check if there is any difference in the DOB on the EHR records if need be.
How can a Patient share their lab records from PHR to EHR? The Patient can upload their lab records in the PHR and share them using the 'Share Section' feature. Visit this link for detailed steps on sharing PHR data.
Providers can view the shared data under the 'Patient dashboard > "PHR Data" section.
Note: Ensure the EHR settings allows Patients to share data under the 'Settings > PHR Settings > Preferences' section.
Why is the Patient unable to fill out a questionnaire from PHR? Patients may be unable to fill in questionnaires in CharmHealth PHR for the following reasons:
- Questionnaire Section: Only questionnaires available under the "Current Questionnaires" section are fillable. Questionnaires in the "Past Questionnaires" section are not fillable.
- Reconciliation by Providers: If providers have already reconciled the Allergies, Medications, Supplements, or Subjective sections of the questionnaire, Patients cannot fill it in the PHR.
- Signed Encounter: Patients cannot fill out questionnaires if the associated encounter for the questionnaire is already signed.
- Expired Appointment: Patients cannot fill out the questionnaire if the associated appointment date has already passed.
- Open access
- Published: 26 April 2024
Clinician and staff experiences with frustrated patients during an electronic health record transition: a qualitative case study
- Sherry L. Ball 1 ,
- Bo Kim 2 , 3 ,
- Sarah L. Cutrona 4 , 5 ,
- Brianne K. Molloy-Paolillo 4 ,
- Ellen Ahlness 6 ,
- Megan Moldestad 6 ,
- George Sayre 6 , 7 &
- Seppo T. Rinne 2 , 8
BMC Health Services Research volume 24 , Article number: 535 ( 2024 ) Cite this article
22 Accesses
Metrics details
Electronic health record (EHR) transitions are known to be highly disruptive, can drastically impact clinician and staff experiences, and may influence patients’ experiences using the electronic patient portal. Clinicians and staff can gain insights into patient experiences and be influenced by what they see and hear from patients. Through the lens of an emergency preparedness framework, we examined clinician and staff reactions to and perceptions of their patients’ experiences with the portal during an EHR transition at the Department of Veterans Affairs (VA).
This qualitative case study was situated within a larger multi-methods evaluation of the EHR transition. We conducted a total of 122 interviews with 30 clinicians and staff across disciplines at the initial VA EHR transition site before, immediately after, and up to 12 months after go-live (September 2020-November 2021). Interview transcripts were coded using a priori and emergent codes. The coded text segments relevant to patient experience and clinician interactions with patients were extracted and analyzed to identify themes. For each theme, recommendations were defined based on each stage of an emergency preparedness framework (mitigate, prepare, respond, recover).
In post-go-live interviews participants expressed concerns about the reliability of communicating with their patients via secure messaging within the new EHR portal. Participants felt ill-equipped to field patients’ questions and frustrations navigating the new portal. Participants learned that patients experienced difficulties learning to use and accessing the portal; when unsuccessful, some had difficulties obtaining medication refills via the portal and used the call center as an alternative. However, long telephone wait times provoked patients to walk into the clinic for care, often frustrated and without an appointment. Patients needing increased in-person attention heightened participants’ daily workload and their concern for patients’ well-being. Recommendations for each theme fit within a stage of the emergency preparedness framework.
Conclusions
Application of an emergency preparedness framework to EHR transitions could help address the concerns raised by the participants, (1) mitigating disruptions by identifying at-risk patients before the transition, (2) preparing end-users by disseminating patient-centered informational resources, (3) responding by building capacity for disrupted services, and (4) recovering by monitoring integrity of the new portal function.
Peer Review reports
Electronic health record (EHR) transitions present significant challenges for healthcare clinicians and staff. These transitions require adjustments in care delivery and may threaten care quality and value. It is critical that healthcare organizations undergoing these changes learn from others who have undergone similar transitions [ 1 , 2 ]. However, the current literature lacks adequate guidance on navigating EHR transitions, especially as they relate to how clinicians and staff interact with patients [ 3 ].
Embedded within EHRs, patient portals facilitate complete, accurate, timely, and unambiguous exchange of information between patients and healthcare workers [ 4 , 5 ]. These portals have become indispensable for completing routine out-of-office-visit tasks, such as medication refills, communicating laboratory results, and addressing patient questions [ 6 ]. In 2003, the VA launched their version of a patient portal, myHealtheVet [ 7 ] and by 2017 69% of Veterans enrolled in healthcare at the VA had registered to access the patient portal [ 8 ]. Similar to other electronic portals, this system allows Veterans to review test results, see upcoming appointments, and communicate privately and securely with their healthcare providers.
EHR transitions can introduce disruptions to patient portal communication that may compromise portal reliability, impacting patient and clinician satisfaction, patients’ active involvement in self-management, and ultimately health outcomes [ 9 ]. During an EHR transition, patients can expect reductions in access to care even when clinician capacity and IT support are increased. Patients will likely need for more assistance navigating the patient portal including and using the portal to communicate with their providers [ 10 ]. Staff must be prepared and understand how the changes in the EHR will affect patients and safeguards must be in place to monitor systems for potential risks to patient safety. Building the capacity to respond to emerging system glitches and identified changes must be included in any transition plan. Although portal disruptions are likely to occur when a new EHR is implemented, we know little about how these disruptions impact healthcare workers’ interactions and care delivery to patients [ 11 , 12 ].
Due to an urgency to raise awareness and promote resolution of these patient portal issues,, we utilized existing data from the first EHR transition site for the Department of Veterans Affairs (VA)’s enterprise-wide transition. We focused on end users’ responses to the question “How Veterans were affected by the transition?”. We used qualitative methods to begin to understand how provider and patient interactions were affected during and by the EHR transition. We explored the impact of the EHR transition on patients through healthcare workers’ vicarious and direct experiences with patients. Due to the high level of disruption in care delivery we draw on insights from an emergency preparedness framework [ 13 ] to generate a set of recommendations to improve healthcare workers’ experiences during EHR transitions. The emergency preparedness framework includes 4 phases of an iterative cycle that include: (1) building capacity to mitigate issues, (2) preparing for the inevitable onset of issues, (3) responding to issues as they emerge, and (4) strategies to recover from any damage incurred.
In early 2020, the VA embarked on an EHR transition from a homegrown, legacy EHR system, developed by VA clinicians and used since the 1990s, to a new commercial system by the Oracle-Cerner Corporation. The primary objectives of this transition were to standardize care and improve interoperability between VA Medical Centers nationwide and the Department of Defense (DoD). Spanning over a decade, this transition plan is scheduled to roll out to all VA medical centers and outpatient clinics.
In this manuscript, we present data from the Mann-Grandstaff VA Medical Center in Spokane, WA, VA’s first EHR transition site. The study uses qualitative methods with clinician and staff interviews as part of a larger multi-method evaluation of the EHR transition. Our overarching goal is to identify and share recommendations to improve VA’s EHR transition efforts; rather than be guided by a theoretical framework our study design including the interview guides [ 14 , 15 ] were based primarily on what was being experienced. An experienced team of ten qualitative methodologists and analysts conducted the study.
This evaluation was designated as non-research/quality improvement work by the VA Bedford Healthcare System Institutional Review Board deeming it exempt from needing an informed consent. Study materials, including interview guides with verbal consent procedures, were reviewed and approved by labor unions and by the VA Bedford Healthcare System Institutional Review Board; all methods were carried out in accordance with local and national VA guidelines and regulations.
Interview guides and an outline of the data collection plans were reviewed and approved by relevant national unions before beginning recruitment.
Recruitment
Recruitment began in July 2020, before the first site implemented the new EHR. Prior to collecting data, we met with site leadership to get buy-in and support for the study, understand local context, determine how the site was approaching the transition, and to obtain the names of clinicians and staff for potential interviews. All potential participants were invited by email to participate in a one-hour voluntary interview conducted on Microsoft Teams® about their experiences with this transition; we used snowball sampling during interviews to expand the pool of interviewees. Verbal permission for audio recording of interviews was obtained immediately prior to the interview. Interview participants were informed that they could skip any questions, pause or stop the recording, and stop the interview at any time and were invited to ask questions before beginning the interview.
Most participants were interviewed at multiple timepoints; these included pre-implementation interviews, brief check-ins, and post-implementation interviews (Table 1 ). At the end of the pre-implementation interview, participants were invited to participate in 3–4 additional, shorter (15–20 min), check-in interviews where information about any changes in the transition process, context, or experience could be discussed. Most initial interviewees, in addition to three new participants, participated in post-implementation interviews (35–60 min; approximately 2–3 months and 10–12 months after the implementation) to reflect on the entire transition process.
Data collection
Experienced qualitative interviewers included PhD trained qualitative methodologist and masters level qualitative analysts (JB, SB, AC, EK, MM, GS) conducted individual interviews with clinicians and staff, aligning to a semi-structured interview guide with follow-up probes using the participant’s words to elicit rich responses grounded in the data [ 16 ]. The guide was designed to inform ongoing efforts to improve the rollout of the new EHR. Six main categories were covered in our interview guides, including (1) attitudes toward the new software, (2) information communicated about the transition, (3) training and education, (4) resources, (5) prior experience with EHRs, and (6) prior experiences with EHR transitions. After piloting the interview guide with a clinician, initial interviews were completed between September and October 2020 and averaged ∼ 45 min in duration. Two-month and one-year post-implementation interview guides included an additional question, “Has the Cerner transition affected Vets?”; data presented here largely draw from responses to this question. Check-ins (October 2020– December 2020) took ∼ 15 min; two-month post-implementation interviews (December 2020– January 2021) and one-year post-implementation interviews (October 2020 - November 2021) took ∼ 45 min. Audio recordings of all interviews were professionally transcribed. To ensure consistency and relationship building, participants were scheduled with the same interviewer for the initial and subsequent interviews whenever feasible (i.e., check-ins and post-implementation interviews). Immediately following each interview, interviewers completed a debrief form where highlights and general reflections were noted.
Throughout the data collection process, interviewers met weekly with the entire qualitative team and the project principal investigators to discuss the recruitment process, interview guide development, and reflections on data collection. To provide timely feedback to leadership within the VA, a matrix analysis [ 17 ] was conducted concurrently with data collection using the following domains: training, roles, barriers, and facilitators. Based on these domains, the team developed categories and subcategories, which formed the foundation of an extensive codebook.
Data analysis
All interviewers also coded the data. We used inductive and deductive content analysis [ 18 ]. Interview transcripts were coded in ATLAS.ti qualitative data analysis software (version 9). A priori codes and categories (based on the overall larger project aims and interview guide questions) and emergent codes and categories were developed to capture concepts that did not fit existing codes or categories [ 18 ]. Codes related to patient experience and clinician interactions with patients were extracted and analyzed using qualitative content analysis to identify themes [ 18 ]. Themes were organized according to their fit within the discrete stages of an emergency preparedness framework to generate recommendations for future rollout. In total, we examined data from 111 interviews with 24 VA clinicians and staff (excluding the initial 11 stakeholder meetings (from the 122 total interviews) that were primarily for stakeholder engagement). We focused on participants’ responses related to their experiences interacting with patients during the EHR transition.
Exemplar quotes primarily came from participants’ responses to the question, “Has the Cerner transition affected Vets?” and addressed issues stemming from use of the patient portal. This included both clinicians’ direct experiences with the portal and indirect experiences when they heard from patients about disruptions when using the portal. We identified four themes related to clinicians’ and staff members’ reported experiences: (1) stress associated with the unreliability of routine portal functions and inaccurate migrated information; (2) concern about patients’ ability to learn to use a new portal (especially older patients and special populations); (3) frustration with apparent inadequate dissemination of patient informational materials along with their own lack of time and resources to educate patients on use of the new portal; and (4) burden of additional tasks on top of their daily workload when patients needed increased in-person attention due to issues with the portal.
Stress associated with the unreliability of routine portal functions and inaccurate migrated information
One participant described the portal changes as, “It’s our biggest stress, it’s the patients’ biggest stress… the vets are definitely frustrated; the clinicians are; so I would hope that would mean that behind the scenes somebody is working on it” (P5, check-in).
Participants expressed significant frustration when they encountered veterans who were suddenly unable to communicate with them using routine secure messaging. These experiences left them wondering whether messages sent to patients were received.
Those that use our secure messaging, which has now changed to My VA Health, or whatever it’s called, [have] difficulty navigating that. Some are able to get in and send the message. When we reply to them, they may or may not get the reply. Which I’ve actually asked one of our patients, ‘Did you get the reply that we took care of this?’ And he was like, ‘No, I did not (P11, 2-months post)
Participants learned that some patients were unable to send secure messages to their care team because the portal contained inaccurate or outdated appointment and primary site information.
I’ve heard people say that the appointments aren’t accurate in there… veterans who have said, ‘yeah, it shows I’m registered,’ and when they go into the new messaging system, it says they are part of a VA that they haven’t gone to in years, and that’s the only area they can message to, they can’t message to the [site] VA, even though that’s where they’ve actively being seen for a while now. (P20, 2-months post)
After the EHR transition, participants noted that obtaining medications through the portal, which was once a routine task, became unreliable. They expressed concern around patients’ ability to obtain their medications through the portal, primarily due to challenges with portal usability and incomplete migration of medication lists from the former to the new EHR.
I think it’s been negative, unfortunately. I try to stay optimistic when I talk to [patients], but they all seem to be all having continued difficulty with their medications, trying to properly reorder and get medications seems to still be a real hassle for them. (P17, one-year post) …the medications, their med list just didn’t transfer over into that list [preventing their ability to refill their medications]. (P13, 2-months post)
Concern about patients’ ability to learn to use a new portal
Clinicians and staff expressed concerns around veterans’ ability to access, learn, and navigate a new portal system. Clinicians noted that even veterans who were adept at using the prior electronic portal or other technologies also faced difficulties using the new portal.
They can’t figure out [the new portal], 99% of them that used to use our [old] portal, the electronic secure messaging or emailing between the team, they just can’t use [the new one]. It’s not functioning. (P13, one-year post) Apparently, there’s a link they have to click on to make the new format work for them, and that’s been confusing for them. But I still am having a lot of them tell me, I had somebody recently, who’s very tech savvy, and he couldn’t figure it out, just how to message us. I know they’re still really struggling with that. (P5, 2-months post) And it does seem like the My Vet [my VA Health, new portal], that used to be MyHealtheVet [prior portal], logging on and getting onto that still remains really challenging for a large number of veterans. Like they’re still just unable to do it. So, I do think that, I mean I want to say that there’s positive things, but really, I struggle (P17, one-year post)
Participants recognized difficulties with the new system and expressed empathy for the veterans struggling to access the portal.
I think that a lot of us, individually, that work here, I think we have more compassion for our veterans, because they’re coming in and they can’t even get onto their portal website. (P24, one-year post)
Participants acknowledged that learning a new system may be especially difficult for older veterans or those with less technology experience.
But, you know, veterans, the general population of them are older, in general. So, their technologic skills are limited, and they got used to a system and now they have to change to a new one. (P13, 2-months post) So, for our more elderly veterans who barely turn on the computer, they’re not getting to this new portal. (P8, check in) And you know, I do keep in mind that this is a group of people who aren’t always technologically advanced, so small things, when it’s not normal to them, stymie them.(P13, one-year post)
Concerns were heightened for veterans who were more dependent on the portal as a key element in their care due to specific challenges. One participant pointed out that there may be populations of patients with special circumstances who depend more heavily on the prior portal, MyHealtheVet.
I have veterans from [specific region], that’s the way they communicate. Hearing impaired people can’t hear on the phone, the robocall thing, it doesn’t work, so they use MyHealtheVet. Well, if that goes away, how is that being communicated to the veteran? Ok? (P18, Check-in)
Frustration with inadequate dissemination of information to veterans about EHR transition and use of new portal
Participants were concerned about poor information dissemination to patients about how to access the new portal. During medical encounters, participants often heard from patients about their frustrations accessing the new portal. Participants noted that they could only give their patients a phone number to call for help using the new system but otherwise lacked the knowledge and the time to help them resolve new portal issues. Some clinicians specifically mentioned feeling ill-equipped to handle their patients’ needs for assistance with the new portal. These experiences exacerbated clinician stress during the transition.
Our veterans were using the MyHealtheVet messaging portal, and when our new system went up, it transitioned to My VA Health, but that wasn’t really communicated to the veterans very well. So, what happened was they would go into their MyHealtheVet like they had been doing for all of these years, to go in and request their medications, and when they pulled it up it’d show that they were assigned to a clinician in [a different state], that they have no active medications. Everything was just messed up. And they didn’t know why because there was no alert or notification that things would be changing. (P8, check in) I field all-day frustration from the veterans. And I love my job, I’m not leaving here even as frustrated as I am, because I’m here for them, not to, I’m here to serve the veterans and I have to advocate for them, and I know it will get better, it can’t stay like this. But I constantly field their frustrations.… So, I give them the 1-800 number to a Cerner help desk that helps with that, and I’ve had multiple [instances of] feedback that it didn’t help. (P13, one-year post) And [the patients are] frequently asking me things about their medication [within the portal], when, you know, I can’t help them with that. So, I have to send them back up to the front desk to try to figure out their medications. (P17, one-year post)
Veteran frustration and the burden of additional tasks due to issues with the portal
Clinicians reported that veterans expressed frustration with alternatives to the portal, including long call center wait times. Some veterans chose to walk into the clinic without an appointment rather than wait on the phone. Clinicians noted an increase in walk-ins by frustrated veterans, which placed added workload on clinics that were not staffed to handle the increase in walk-ins.
It’s been kind of clunky also with trying to get that [new portal] transitioned. And then that’s created more walk-ins here, because one, the vets get frustrated with the phone part of it, and then MyHealtheVet (prior portal) not [working], so they end up walking [into the clinic without an appointment]. (P19, check-in) In terms of messages, they can’t necessarily find the clinician they want to message. We had a veteran who came in recently who wanted to talk to their Rheumatologist, and it’s like, yeah, I typed in their name, and nothing came up. So, they have to try calling or coming in. (P20, 2-months post)
In summary, participants described the new patient portal as a source of stress for both themselves and their patients.
In addition to their own direct experience using a new EHR to communicate with their patients, clinicians and staff can be affected by perceptions of their patients’ experiences during an EHR transition [ 19 ]. At this first VA site to transition to the new EHR, clinicians and staff shared their concerns about their patients’ experiences using the portal. They were particularly troubled by unreliability of the secure messaging system and challenges patients faced learning to use the new system without proper instruction. Moreover, clinicians were alarmed to hear about patients having to make in-person visits– especially unplanned (i.e., walk in) ones– due to challenges with the new portal. Each of these issues needs to be addressed to ensure veteran satisfaction. However, the only solution participants could offer to frustrated patients was the telephone number to the help desk, leaving them with no clear knowledge of a solution strategy or a timeline for resolution of the issues.
We propose applying emergency preparedness actions to future EHR rollouts: mitigate, prepare, respond, and recover (Fig. 1 ) [ 13 ]. By applying these actions, patient portal disruptions may be alleviated and patients’ communication with their clinicians and access to care can be maintained. For example, issues stemming from a disruption in the portal may be mitigated by first identifying and understanding which patients typically use the portal and how they use it. Sites can use this information to prepare for the transition by disseminating instructional materials to staff and patients on how to access the new portal, targeting the most common and critical portal uses. Sites can respond to any expected and emerging portal disruptions by increasing access to alternative mechanisms for tasks disrupted by and typically completed within the portal. After the transition, recovery can begin by testing and demonstrating the accuracy and reliability of functions in the new portal. These actions directly address reported clinician concerns and can help maintain patient-clinician communication, and access to care.
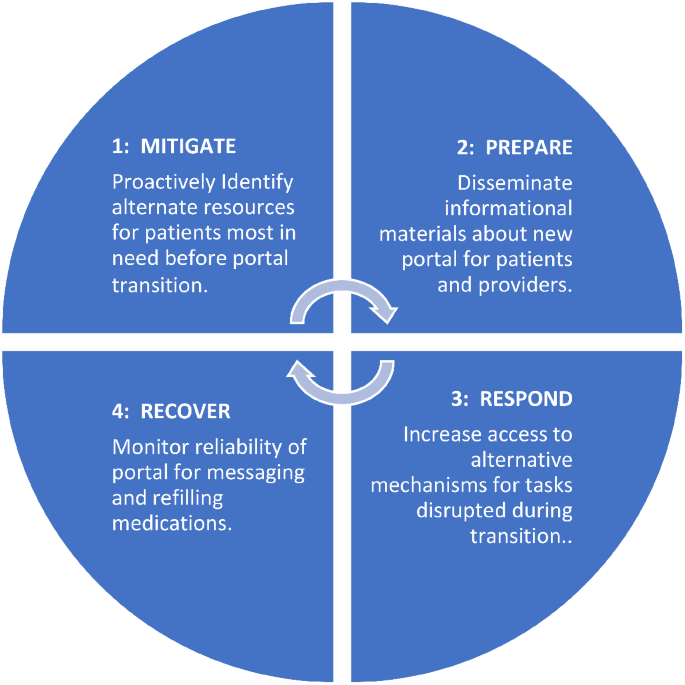
The emergency preparedness framework was applied. This framework includes 4 actions: (1) mitigate, (2) prepare, (3) respond, and (4) recover. These actions can be repeated. Recommendations for how each action (1–4) can be applied to a portal transition are included in each blue quadrant of the circle
Sites could mitigate issues by first understanding which patients will be most affected by the transition, such as those who rely heavily on secure messaging. Reliable use of secure messaging within the VA facilitates positive patient-clinician relationships by providing a mechanism for efficient between-visit communication [ 20 , 21 , 22 , 23 ]. During the EHR transition, clinicians and staff became concerned about the well-being of patients from whom they weren’t receiving messages and those who depended on the portal to complete certain tasks. Since secure messaging is often initiated by patients to clinicians [ 23 ], clinicians will likely be unaware that messages are being missed. Understanding how and which patients currently use the portal and anticipating potential portal needs is a first step toward mitigating potential issues.
Despite efforts to inform Veterans of the EHR transition and patient portal [ 24 ] including information sent to a Veteran by email, direct mail, postings on VA websites, and a town hall, our findings agree with those of Fix and colleagues [ 10 ] and suggest that many Veterans were unprepared for the transition. Our findings suggest that end users heard that more is needed to improve the dissemination of knowledge about the transition and how to navigate the new patient portal to both VA employees and the patients they serve.
Preparations for the transition should prioritize providing VA clinicians and staff with updated information and resources on how to access and use the new portal [ 25 ]. VA clinicians deliver quality care to veterans and many VA employees are proud to serve the nation’s veterans and willing to go the extra mile to support their patients’ needs [ 26 ]. In this study, participants expressed feeling unprepared to assist or even respond to their patients’ questions and concerns about using the new portal. This unpreparedness contributed to increased clinician and staff stress, as they felt ill-equipped to help their patients with portal issues. Such experiences can negatively affect the patient-clinician relationship. Preparing clinicians and patients about an upcoming transition, including technical support for clinicians and patients, may help minimize these potential issues [ 10 , 27 ]. Specialized training about an impending transition, along with detailed instructions on how to gain access to the new system, and a dedicated portal helpline may be necessary to help patients better navigate the transition [ 23 , 28 ].
In addition to a dedicated helpline, our recommendations include responding to potential changes in needed veteran services during the transition. In our study, participants observed more veteran walk-ins due to challenges with the patient portal. Health systems need to anticipate and address this demand by expanding access to in-person services and fortifying other communication channels. For example, sites could use nurses to staff a walk-in clinic to handle increases in walk-in traffic and increase call center capacity to handle increases in telephone calls [ 29 ]. Increased use of walk-in clinics have received heightened attention as a promising strategy for meeting healthcare demands during the COVID-19 pandemic [ 30 ] and can potentially be adapted for meeting care-related needs during an EHR transition. These strategies can fill a gap in communication between clinicians and their patients while patients are learning to access and navigate a new electronic portal.
Finally, there is a need for a recovery mechanism to restore confidence in the reliability of the EHR and the well-being of clinicians and staff. Healthcare workers are experiencing unprecedented levels of stress [ 31 ]. A plan must be in place to improve and monitor the accuracy of data migrated, populated, and processed within the new system [ 2 ]. Knowing that portal function is monitored could help ease clinician and staff concerns and mitigate stress related to the transition.
Limitations
This study has several limitations. First, data collection relied on voluntary participation, which may introduce self-selection response bias. Second, this work was completed at one VA medical center that was the first site in the larger enterprise-wide transition, and experiences at other VAs or healthcare systems might differ substantially. Third, we did not interview veterans and relied entirely on secondhand accounts of patient experiences with the patient portal. Future research should include interviews with veterans during the transition and compare veteran and VA employee experiences.
Despite a current delay in the deployment of the new EHR at additional VA medical centers, findings from this study offer timely lessons that can ensure clinicians and staff are equipped to navigate challenges during the transition. The strategies presented in this paper could help maintain patient-clinician communication and improve veteran experience. Guided by the emergency preparedness framework, recommended strategies to address issues presented here include alerting those patients most affected by the EHR transition, being prepared to address patients’ concerns, increasing staffing for the help desk and walk-in care clinics, and monitoring the accuracy and reliability of the portal to provide assurance to healthcare workers that patients’ needs are being met. These strategies can inform change management at other VA medical centers that will soon undergo EHR transition and may have implications for other healthcare systems undergoing patient portal changes. Further work is needed to directly examine the perspectives of veterans using the portals, as well as the perspectives of both staff and patients in the growing number of healthcare systems beyond VA that are preparing for an EHR-to-EHR transition.
Data availability
Deidentified data analyzed for this study are available from the corresponding author on reasonable request.
Abbreviations
Electronic health record
Department of Veterans Affairs
VA Medical Centers
Department of Defense
Huang C, Koppel R, McGreevey JD 3rd, Craven CK, Schreiber R. Transitions from one Electronic Health record to another: challenges, pitfalls, and recommendations. Appl Clin Inf. 2020;11(5):742–54.
Article Google Scholar
Penrod LE. Electronic Health Record Transition considerations. PM R. 2017;9(5S):S13–8.
Article PubMed Google Scholar
Cogan AM, Haltom TM, Shimada SL, Davila JA, McGinn BP, Fix GM. Understanding patients’ experiences during transitions from one electronic health record to another: a scoping review. PEC Innov. 2024;4:100258. https://doi.org/10.1016/j.pecinn.2024.100258 . PMID: 38327990; PMCID: PMC10847675.
Article PubMed PubMed Central Google Scholar
Powell KR. Patient-perceived facilitators of and barriers to Electronic Portal Use: a systematic review. Comput Inf Nurs. 2017;35(11):565–73.
Google Scholar
Wilson-Stronks A, Lee KK, Cordero CL, et al. One size does not fit all: meeting the Health Care needs of diverse populations. Oakbrook Terrace, IL: The Joint Commission; 2008.
Carini E, Villani L, Pezzullo AM, Gentili A, Barbara A, Ricciardi W, Boccia S. The Impact of Digital Patient Portals on Health outcomes, System Efficiency, and patient attitudes: updated systematic literature review. J Med Internet Res. 2021;23(9):e26189.
Home -. My HealtheVet - My HealtheVet (va.gov).
Nazi KM, Turvey CL, Klein DM, Hogan TP. A decade of veteran voices: examining patient Portal Enhancements through the Lens of user-centered design. J Med Internet Res. 2018;20(7):e10413. https://doi.org/10.2196/10413 .
Tapuria A, Porat T, Kalra D, Dsouza G, Xiaohui S, Curcin V. Impact of patient access to their electronic health record: systematic review. Inf Health Soc Care. 2021;46:2.
Fix GM, Haltom TM, Cogan AM, et al. Understanding patients’ preferences and experiences during an Electronic Health Record Transition. J GEN INTERN MED. 2023. https://doi.org/10.1007/s11606-023-08338-6 .
Monturo C, Brockway C, Ginev A. Electronic Health Record Transition: the patient experience. CIN: Computers Inf Nurs. 2022;40:1.
Tian D, Hoehner CM, Woeltje KF, Luong L, Lane MA. Disrupted and restored patient experience with transition to New Electronic Health Record System. J Patient Exp. 2021;18:8.
Emergency management programs for healthcare facilities. the four phases of emergency management. US Department of Homeland Security website: https://www.hsdl.org/?view&did=765520 . Accessed 28 Aug 2023.
Ahlness EA, Orlander J, Brunner J, Cutrona SL, Kim B, Molloy-Paolillo BK, Rinne ST, Rucci J, Sayre G, Anderson E. Everything’s so Role-Specific: VA Employee Perspectives’ on Electronic Health Record (EHR) transition implications for roles and responsibilities. J Gen Intern Med. 2023;38(Suppl 4):991–8. Epub 2023 Oct 5. PMID: 37798577; PMCID: PMC10593626.
Rucci JM, Ball S, Brunner J, Moldestad M, Cutrona SL, Sayre G, Rinne S. Like one long battle: employee perspectives of the simultaneous impact of COVID-19 and an Electronic Health Record Transition. J Gen Intern Med. 2023;38(Suppl 4):1040–8. https://doi.org/10.1007/s11606-023-08284-3 . Epub 2023 Oct 5. PMID: 37798583; PMCID: PMC10593661.
Sayre G, Young J. Beyond open-ended questions: purposeful interview guide development to elicit rich, trustworthy data [videorecording]. Seattle (WA): VA Health Services Research & Development HSR&D Cyberseminars; 2018.
Averill JB. Matrix analysis as a complementary analytic strategy in qualitative inquiry. Qual Health Res. 2002;12:6855–66.
Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62:1107–15.
Haun JN, Lind JD, Shimada SL, Simon SR. Evaluating Secure Messaging from the veteran perspective: informing the adoption and sustained use of a patient-driven communication platform. Ann Anthropol Pract. 2013;372:57–74.
Kittler AF, Carlson GL, Harris C, Lippincott M, Pizziferri L, Volk LA, et al. Primary care physician attitudes toward using a secure web-based portal designed to facilitate electronic communication with patients. Inf Prim Care. 2004;123:129–38.
Shimada SL, Petrakis BA, Rothendler JA, Zirkle M, Zhao S, Feng H, Fix GM, Ozkaynak M, Martin T, Johnson SA, Tulu B, Gordon HS, Simon SR, Woods SS. An analysis of patient-provider secure messaging at two Veterans Health Administration medical centers: message content and resolution through secure messaging. J Am Med Inf Assoc. 2017;24:5.
Jha AK, Perlin JB, Kizer KW, Dudley RA. Effect of the transformation of the Veterans Affairs Health Care System on the quality of care. N Engl J Med. 2003;348:22.
McAlearney AS, Walker DM, Gaughan A, Moffatt-Bruce S, Huerta TR. Helping patients be better patients: a qualitative study of perceptions about Inpatient Portal Use. Telemed J E Health. 2020;26:9.
https://www.myhealth.va.gov/mhv-portal-web/transitioning-to-my-va-health-learn-more .
Beagley L. Educating patients: understanding barriers, learning styles, and teaching techniques. J Perianesth Nurs. 2011;26:5.
Moldestad M, Stryczek KC, Haverhals L, Kenney R, Lee M, Ball S, et al. Competing demands: Scheduling challenges in being veteran-centric in the setting of Health System initiatives to Improve Access. Mil Med. 2021;186:11–2.
Adusumalli J, Bhagra A, Vitek S, Clark SD, Chon TY. Stress management in staff supporting electronic health record transitions: a novel approach. Explore (NY). 2021;17:6.
Heponiemi T, Gluschkoff K, Vehko T, Kaihlanen AM, Saranto K, Nissinen S, et al. Electronic Health Record implementations and Insufficient Training Endanger nurses’ Well-being: cross-sectional survey study. J Med Internet Res. 2021;23:12e27096.
Laurant M, van der Biezen M, Wijers N, Watananirun K, Kontopantelis E, van Vught AJ. Nurses as substitutes for doctors in primary care. Cochrane Database Syst Rev. 201;7(7):CD001271.
Elnahal S, Kadakia KT, Gondi S, How, U.S. Health systems Can Build Capacity to Handle Demand Surges. Harvard Business Review. 2021. https://hbr.org/2021/10/how-u-s-health-systems-can-build-capacity-to-handle-demand-surges/ Accessed 25 Nov 2022.
George RE, Lowe WA. Well-being and uncertainty in health care practice. Clin Teach. 2019;16:4.
Download references
Acknowledgments
We acknowledge and thank members of the EMPIRIC Evaluation qualitative and supporting team for their contributions to this work including Ellen Ahlness, PhD, Julian Brunner, PhD, Adena Cohen-Bearak, MPH, M.Ed, Leah Cubanski, BA, Christine Firestone, Bo Kim, PhD, Megan Moldestad, MS, and Rachel Smith. We greatly appreciate the staff at the Mann-Grandstaff VA Medical Center and associated community-based outpatient clinics for generously sharing of their time and experiences participating in this study during this challenging time.
The “EHRM Partnership Integrating Rapid Cycle Evaluation to Improve Cerner Implementation (EMPIRIC)” (PEC 20–168) work was supported by funding from the US Department of Veterans Affairs, Veterans Health Administration, Health Services Research & Development Quality Enhancement Research Initiative (QUERI) (PEC 20–168). The findings and conclusions in this article are those of the authors and do not necessarily reflect the views of the Veterans Health Administration, Veterans Affairs, or any participating health agency or funder.
Author information
Authors and affiliations.
VA Northeast Ohio Healthcare System, 10701 East Blvd., Research Service 151, 44106, Cleveland, OH, USA
Sherry L. Ball
Center for Healthcare Organization and Implementation Research, VA Boston Healthcare System, Boston, MA, USA
Bo Kim & Seppo T. Rinne
Department of Psychiatry, Harvard Medical School, Boston, MA, USA
Center for Healthcare Organization and Implementation Research, VA Bedford Healthcare System, Bedford, MA, USA
Sarah L. Cutrona & Brianne K. Molloy-Paolillo
Division of Health Informatics & Implementation Science, Department of Population and Quantitative Health Sciences, University of Massachusetts Chan Medical School, Worcester, MA, USA
Sarah L. Cutrona
Seattle-Denver Center of Innovation for Veteran-Centered and Value-Driven Care, VHA Puget Sound Health Care System, Seattle, WA, USA
Ellen Ahlness, Megan Moldestad & George Sayre
University of Washington School of Public Health, Seattle, WA, USA
George Sayre
Geisel School of Medicine at Dartmouth, Hannover, NH, USA
Seppo T. Rinne
You can also search for this author in PubMed Google Scholar
Contributions
S.R. designed the larger study. G.S. was the qualitative methodologist who led the qualitative team. S.B., E.A., and M.M. created the interview guides and completed the interviews; Data analysis, data interpretation, and the initial manuscript draft were completed by S.B. and B.K. S.C. and B.M. worked with the qualitative team to finalize the analysis and edit and finalize the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Sherry L. Ball .
Ethics declarations
Ethics approval and consent to participate.
This evaluation was designated as non-research/quality improvement by the VA Bedford Healthcare System Institutional Review Board. All methods were carried out in accordance with local and national VA guidelines and regulations for quality improvement activities. This study included virtual interviews with participants via MS Teams. Employees volunteered to participate in interviews and verbal consent was obtained to record interviews. Study materials, including interview guides with verbal consent procedures, were reviewed and approved by labor unions and determined as non-research by the VA Bedford Healthcare System Institutional Review Board.
Consent for publication
Not applicable.
The findings and conclusions in this paper are those of the authors and do not necessarily represent the official position of the Department of Veterans Affairs.
Prior presentations
Ball S, Kim B, Moldestad M, Molloy-Paolillo B, Cubanski L, Cutrona S, Sayre G, and Rinne S. (2022, June). Electronic Health Record Transition: Providers’ Experiences with Frustrated Patients. Poster presentation at the 2022 AcademyHealth Annual Research Meeting. June 2022.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ball, S.L., Kim, B., Cutrona, S.L. et al. Clinician and staff experiences with frustrated patients during an electronic health record transition: a qualitative case study. BMC Health Serv Res 24 , 535 (2024). https://doi.org/10.1186/s12913-024-10974-5
Download citation
Received : 29 August 2023
Accepted : 09 April 2024
Published : 26 April 2024
DOI : https://doi.org/10.1186/s12913-024-10974-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- EHR transition
- Patient experience
- Clinician experience
- Qualitative analysis
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
UnitedHealth paid ransom in Change Healthcare cyberattack, says patient data was compromised

UnitedHealth Group on Monday said it paid ransom to cyberthreat actors to try to protect patient data, following the February cyberattack on its subsidiary Change Healthcare . The company also confirmed that files containing personal information were compromised in the breach.
“This attack was conducted by malicious threat actors, and we continue to work with the law enforcement and multiple leading cyber security firms during our investigation,” UnitedHealth told CNBC in a statement. “A ransom was paid as part of the company’s commitment to do all it could to protect patient data from disclosure.”
The company did not specify the ransom payment amount.
UnitedHealth, which has more than 152 million customers, said it has also determined that the cyberthreat actors accessed files containing protected health information and personally identifiable information, according to a release Monday .
The files “could cover a substantial proportion of people in America,” the release said.
Change Healthcare offers payment and revenue cycle management tools. The company facilitates more than 15 billion transactions annually, and 1 in every 3 patient records passes through its systems. This means even patients who are not UnitedHealth customers could have been affected by the attack.
UnitedHealth said in the release that 22 screenshots, allegedly of the compromised files, have been uploaded to the dark web. The company said no other data has been published, and it has not seen evidence that doctors’ charts or full medical histories were accessed in the breach.
“We know this attack has caused concern and been disruptive for consumers and providers and we are committed to doing everything possible to help and provide support to anyone who may need it,” UnitedHealth CEO Andrew Witty said in the release.
UnitedHealth said that concerned patients can visit a dedicated website for access to resources. The company has launched a call center that will offer free identity theft protections and credit monitoring for two years, the release said.
The call center will not be able to offer any details about individual data impact given the “ongoing nature and complexity of the data review,” UnitedHealth said.

IMAGES
VIDEO
COMMENTS
Are you a patient who wants to manage your health online? Log in to myPatientVisit.com, the secure and easy way to communicate with your doctor, view your medical history, request appointments, and more. If you don't have an account yet, you can sign up for free and start enjoying the benefits of myPatientVisit.com.
Dermatology Group of the Carolinas - mypatientvisit.com
Step 1: Go to the myPatientVisit login portal. Step 2: Log in with the information you used when you registered. For more information contact: Wyn Partington. Chief Revenue Officer, Nextech. (813) 425-9260. [email protected]. Nextech is the complete healthcare technology solution for specialty providers.
Easy access to your health records puts you in control of decisions regarding your health and well-being. You can monitor your health conditions better, understand and stay on track with treatment plans, and find and fix errors in your record. The resources and videos below will help you understand your rights under the Health Insurance ...
An electronic health record (EHR) is a digital version of a patient's paper chart. EHRs are real-time, patient-centered records that make information available instantly and securely to authorized users. While an EHR does contain the medical and treatment histories of patients, an EHR system is built to go beyond standard clinical data collected in a provider's office and can be inclusive ...
So with an EHR system, your family doctor can instantly send medical records to your heart specialist, your hospital, the lab, your drugstore, and your computer at home. The goal of EHRs is to improve the coordination of your care by giving providers accurate, up-to-date information. This includes information from you, the patient.
How to integrate the electronic health record and patient-centered communication into the medical visit: a skills-based approach. Teach Learn Med . 2013;25(4):358-365. doi: 10.1080/10401334.2013. ...
EHRs Support Provider Decision Making. EHRs can help providers make efficient, effective decisions about patient care, through: Improved aggregation, analysis, and communication of patient information. Clinical alerts and reminders. Support for diagnostic and therapeutic decisions. Built-in safeguards against potential adverse events.
The myPatientVisit™ mobile app is designed with the patient's ease of use in mind, providing a place to check your balance and upcoming appointments quickly, and chat with your provider's staff all from your phone. Ask your provider for an invitation to create your account on myPatientVisit.com. Once your account is created, you will be able ...
Provider portals are the main way to request health care records, but there are other ways to get access including through third-party apps and organizations or even via email. Medical providers and healthcare organizations must now give patients electronic access to their health records under new federal rules that went into effect on Oct. 6.
An all-in-one practice management solution that delivers comprehensive EHR, RCM, and patient engagement software and services. athenaOne Solutions. Electronic Health Record. A connected, tailorable EHR solution that empowers clinicians. ... Get an inside look at how athenaOne organizes the visit and helps you document faster and more accurately
The myPatientVisit mobile app is a patient-centered platform that allows patients to access their healthcare information and communicate with their provider's staff from their mobile devices. The app is optimized for mobile use and provides a user-friendly interface for patients to check their balance, view upcoming appointments, and chat ...
PHRs, EHRs and patient portals. PHRs are not the same as electronic health records (EHRs), also called electronic medical records (EMRs), which are owned and maintained by doctors' offices, hospitals or health insurance plans. EHRs typically contain the same basic information you would put in a PHR, such as your date of birth, medication list ...
Here are 10 strategies that have helped me become more efficient and could help you too, no matter which EHR system you use. 1. Rethink your exam room setup. Ideally, you should place the computer ...
Designed with you in mind, Practice EHR works with any specialty to streamline the entire patient visit, from check-in to check-out, billing to claim submission, and scheduling to follow up - all in one place. Our intuitive EHR software design is easy-to-use, and because it's cloud-based, you have the freedom to work anywhere and everywhere ...
The study looked at about 100 million patient visits to 155,000 U.S. physicians and found they spend an average of 16 minutes and 14 seconds per patient encounter using EHRs, with chart review (33 ...
The ONE with the latest product enhancements, features and fixes. The ONE place where all your most common questions are answered. The ONE source you need for medical industry insights, trends and thought leadership. Watch videos about the patients' charts, flow sheets, financials, demographics, referring providers, insurance, documents ...
EHRs can: Contain information about a patient's medical history, diagnoses, medications, immunization dates, allergies, radiology images, and lab and test results. Offer access to evidence-based tools that providers can use in making decisions about a patient's care. Automate and streamline providers' workflow.
Practice EHR TeleVisit offers secure, real-time telehealth video sessions integrated with your Practice EHR software. Seamlessly conduct a patient telehealth visit anytime that's convenient utilizing our intuitive workflow. Providers can conduct video sessions with patients and easily chart the note, prescribe medications and code encounters ...
To access the MHS GENESIS Patient Portal visit: https://my.mhsgenesis.health.mil. There are three ways you can log in to MHS GENESIS Patient Portal: Logging in with your Department of Defense Self-Service (DS) Logon (see FAQ - DS LOGON) Logging in with your common access card (CAC) Logging in using a Personal Identity Verification (PIV)
Even after deactivating Patients in the EHR, their PHR account remains active. The Patients can continue using it, but they will not be able to send messages, request an appointment or share records with the Practice. Can patients access the visit summary from their patient portal?
patients to get and stay healthy. Access MyChart. Stay ahead of COVID-19 ... Make appointments at your convenience, complete pre-visit tasks from home, and find the nearest urgent care or emergency room when you need it. Connect with a doctor no matter where you are Send a message, get online diagnosis and treatment, talk face-to-face over ...
Enter their date of birth (mm-dd-yyyy format). Click on the 'Next' button to complete their user verification. Enter the same 'Username or Email ID' and 'Password' you created previously. A warning message with the 'Patient Name' confirming their addition to your PHR account will pop up. Click on the 'Submit' button.
Electronic health record (EHR) transitions are known to be highly disruptive, can drastically impact clinician and staff experiences, and may influence patients' experiences using the electronic patient portal. Clinicians and staff can gain insights into patient experiences and be influenced by what they see and hear from patients. Through the lens of an emergency preparedness framework, we ...
After your VAMC changes to the new electronic health record, you will have to manage VA prescriptions from that VAMC on a new patient portal, called My VA Health. Before the change to the new electronic health record: Request your refills in one of these ways: Online with the My HealtheVet prescription refill and tracking tool, or
UnitedHealth said it paid ransom to protect patient data, following the cyberattack on its subsidiary Change Healthcare. But personal data was compromised anyway.