You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.

What is COVID-19?
Who can get covid-19, can i travel if i recently had covid-19, what can travelers do to prevent covid-19, more information.
CDC Respiratory Virus Guidance has been updated. The content of this page will be updated soon.
Coronavirus disease 2019 (COVID-19) is a respiratory illness caused by the virus SARS-CoV-2. The virus spreads mainly from person to person through respiratory droplets and small particles produced when an infected person coughs, sneezes, or talks. The virus spreads easily in crowded or poorly ventilated indoor settings.
People with COVID-19 have reported a wide range of symptoms – ranging from no or mild symptoms to severe illness. Symptoms may appear 2–14 days after exposure to the virus. Possible symptoms include fever, chills, cough, shortness of breath, fatigue, muscle aches, headache, new loss of taste and smell, sore throat, runny nose, nausea, vomiting, or diarrhea.
Anyone can get COVID-19. However, some people are more likely than others to get very sick if they get COVID-19. These include people who are older, are immunocompromised , or have certain disabilities , or have underlying health conditions . Vaccination, past infection, and timely access to testing and treatment can help protect you from getting very sick from COVID-19.
Yes, you can travel once you have ended isolation . Check CDC guidance for additional precautions, including testing and wearing a mask around others. If you recently had COVID-19 and are recommended to wear a mask, do not travel on public transportation such as airplanes, buses, and trains if you are unable to wear a mask whenever around others.
Get up to date with your COVID-19 vaccines before you travel and take steps to protect yourself and others . Consider wearing a mask in crowded or poorly ventilated indoor areas, including on public transportation and in transportation hubs. Take additional precautions if you were recently exposed to a person with COVID-19. Don’t travel while sick.
If you have a weakened immune system or are at increased risk for severe disease talk to a healthcare professional before you decide to travel. If you travel, take multiple prevention steps to provide additional layers of protection from COVID-19, even if you are up to date with your COVID-19 vaccines. These include improving ventilation and spending more time outdoors, avoiding sick people, getting tested for COVID-19 if you develop symptoms, staying home if you have or think you have COVID-19, and seeking treatment if you have COVID-19.
Consider getting travel insurance in case you need medical care abroad .
Consider getting a COVID-19 test if you:
- Develop COVID-19 symptoms before, during, or after travel.
- Will be traveling to visit someone who is at higher risk of getting very sick from COVID-19.
- Were in a situation with a greater risk of exposure during travel (e.g., in an indoor, crowded space like an airport terminal while not wearing a mask).
If you traveled and feel sick, particularly if you have a fever, talk to a healthcare professional, and tell them about your recent travel.
- Masking During Travel
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
CDC updates Covid isolation guidelines for people who test positive

People who test positive for Covid no longer need to isolate for five days , the Centers for Disease Control and Prevention said Friday.
The CDC’s new guidance now matches public health advice for flu and other respiratory illnesses: Stay home when you’re sick, but return to school or work once you’re feeling better and you’ve been without a fever for 24 hours.
The shift reflects sustained decreases in the most severe outcomes of Covid since the beginning of the pandemic, as well as a recognition that many people aren’t testing themselves for Covid anyway.
“Folks often don’t know what virus they have when they first get sick, so this will help them know what to do, regardless,” CDC director Dr. Mandy Cohen said during a media briefing Friday.
Over the past couple of years, weekly hospital admissions for Covid have fallen by more than 75%, and deaths have decreased by more than 90%, Cohen said.
“To put that differently, in 2021, Covid was the third leading cause of death in the United States. Last year, it was the 10th,” Dr. Brendan Jackson, head of respiratory virus response within the CDC’s National Center for Immunization and Respiratory Diseases, said during the briefing.
Many doctors have been urging the CDC to lift isolation guidance for months, saying it did little to stop the spread of Covid.
The experiences of California and Oregon , which previously lifted their Covid isolation guidelines, proved that to be true.
“Recent data indicate that California and Oregon, where isolation guidance looks more like CDC’s updated recommendations, are not experiencing higher Covid-19 emergency department visits or hospitalizations,” Jackson said.
Changing the Covid isolation to mirror what’s recommended for flu and other respiratory illnesses makes sense to Dr. David Margolius, the public health director for the city of Cleveland.
“We’ve gotten to the point where we are suffering from flu at a higher rate than Covid,” he said. “What this guidance will do is help to reinforce that— regardless of what contagious respiratory viral infection you have — stay home when you’re sick, come back when you’re better.”
Dr. Kristin Englund, an infectious diseases expert at the Cleveland Clinic, said the new guidance would be beneficial in curbing the spread of all respiratory viruses.
“I think this is going to help us in the coming years to make sure that our numbers of influenza and RSV cases can also be cut down, not just Covid,” she said.
Latest news on Covid
- Common Covid symptoms follow a pattern now, doctors say.
- Covid during pregnancy can cause health issues in babies.
- How big of a risk is coinfection with Covid and other viruses?
Still, the decision was likely to draw criticism from some clinicians who point to the fact that the U.S. logged 17,310 new Covid hospitalizations in the past week alone.
“It’s something that is likely to draw a wide array of opinions and perhaps even conflicting opinions,” said Dr. Faisal Khan, Seattle’s director of public health. “But [the CDC’s] rationale is sound in that the pandemic is now in a very different phase from where it was in 2021 or 2022 or 2023.”
Though the isolation guidelines have been wiped away, the CDC still encourages people to play it safe for five days after they are feeling better. That includes masking around vulnerable people and opening windows to improve the flow of fresh air indoors.
The majority of viral spread happens when people are the sickest. “As the days go on, less virus spreads,” Cohen said.
People at higher risk for severe Covid complications, such as the elderly, people with weak immune systems and pregnant women, may need to take additional precautions.
Dr. Katie Passaretti, chief epidemiologist at Atrium Health in Charlotte, said it was a “move in the positive direction.”
“We are continuing to edge into what the world looks like after Covid, with Covid being one of many respiratory viruses that are certain that circulate,” she said.
The new guidance is for the general public only, and does not include isolation guidelines in hospital settings, which is generally 10 days.
On Wednesday, the agency said that adults 65 and older should get a booster shot of the Covid vaccine this spring. It’s anticipated that the nation will experience an uptick in the illness later this summer.
Winter and summer waves of Covid have emerged over the past four years, with cases peaking in January and August, respectively, according to the CDC .
Another, reformulated, shot is expected to be available and recommended this fall.
CDC’s main tips for reducing Covid spread:
- Get the Covid vaccine whenever it is available. Cohen said that 95% of people who were hospitalized with Covid this past winter had not received the latest vaccine.
- Cover coughs and sneezes, and wash hands frequently.
- Increase ventilation by opening windows, using air purifiers and gathering outside when possible.
Erika Edwards is a health and medical news writer and reporter for NBC News and "TODAY."
Disclaimer: This translation was last updated on August 2, 2022. For up-to-date content, please visit the English version of this page.
Disclaimer: The Spanish COVID-19 site is currently undergoing significant updates which may lead to a delay in translated content. We apologize for any inconvenience.
Isolation and Precautions for People with COVID-19
If you were exposed to COVID-19, you should start taking precautions.
Isolation and Exposure Calculator
A tool to help you determine if you need to isolate or take other steps to prevent spreading COVID-19.
If you have COVID-19, you can spread the virus to others. There are precautions you can take to prevent spreading it to others: isolation, masking, and avoiding contact with people who are at high risk of getting very sick . Isolation is used to separate people with confirmed or suspected COVID-19 from those without COVID-19.
These recommendations do not change based on COVID-19 hospital admission levels . If you have COVID-19, also see additional information on treatments that may be available to you.
This information is intended for a general audience. Healthcare professionals should see Ending Isolation and Precautions for People with COVID-19 . This CDC guidance is meant to supplement—not replace—any federal, state, local, territorial, or tribal health and safety laws, rules, and regulations.
For Healthcare Professionals: Ending Isolation and Precautions for People with COVID-19
Regardless of vaccination status, you should isolate from others when you have COVID-19 .
You should also isolate if you are sick and suspect that you have COVID-19 but do not yet have test results. If your results are positive, follow the full isolation recommendations below. If your results are negative, you can end your isolation.
You can end your isolation
Follow the full isolation recommendations below
When you have COVID-19, isolation is counted in days, as follows:
If you had no symptoms
- Day 0 is the day you were tested (not the day you received your positive test result)
- Day 1 is the first full day following the day you were tested
- If you develop symptoms within 10 days of when you were tested, the clock restarts at day 0 on the day of symptom onset
If you had symptoms
- Day 0 of isolation is the day of symptom onset , regardless of when you tested positive
- Day 1 is the first full day after the day your symptoms started
If you test positive for COVID-19, s tay home for at least 5 days and isolate from others in your home.
You are likely most infectious during these first 5 days.
- Wear a high-quality mask if you must be around others at home and in public.
- Do not go places where you are unable to wear a mask. For travel guidance, see CDC’s Travel webpage .
- Do not travel .
- Stay home and separate from others as much as possible.
- Use a separate bathroom, if possible.
- Take steps to improve ventilation at home, if possible.
- Don’t share personal household items, like cups, towels, and utensils.
- Monitor your symptoms . If you have an emergency warning sign (like trouble breathing), seek emergency medical care immediately.
- Learn more about what to do if you have COVID-19 .
End isolation based on how serious your COVID-19 symptoms were. Loss of taste and smell may persist for weeks or months after recovery and need not delay the end of isolation.
You may end isolation after day 5.
If you had symptoms and:
Your symptoms are improving.
You may end isolation after day 5 if:
- You are fever-free for 24 hours (without the use of fever-reducing medication).
Your symptoms are not improving
Continue to isolate until:
- Your symptoms are improving. 1
If you had symptoms and had:
Moderate illness (you experienced shortness of breath or had difficulty breathing).
You need to isolate through day 10.
Severe illness (you were hospitalized) or have a weakened immune system
- You need to isolate through day 10.
- Consult your doctor before ending isolation.
- Ending isolation without a viral test may not be an option for you.
If you are unsure if your symptoms are moderate or severe or if you have a weakened immune system, talk to a healthcare provider for further guidance.
Regardless of when you end isolation
Until at least day 11:.
- Avoid being around people who are more likely to get very sick from COVID-19.
- Remember to wear a high-quality mask when indoors around others at home and in public.
- Do not go places where you are unable to wear a mask until you are able to discontinue masking (see below).
- For travel guidance, see CDC’s Travel webpage .
After you have ended isolation, when you are feeling better (no fever without the use of fever-reducing medications and symptoms improving),
- Wear your mask through day 10.
- If you have access to antigen tests, you should consider using them. With two sequential negative tests 48 hours apart, you may remove your mask sooner than day 10.
Note: If your antigen test results 1 are positive, you may still be infectious. You should continue wearing a mask and wait at least 48 hours before taking another test. Continue taking antigen tests at least 48 hours apart until you have two sequential negative results. This may mean you need to continue wearing a mask and testing beyond day 10.
After you have ended isolation, if your COVID-19 symptoms recur or worsen, restart your isolation at day 0. Talk to a healthcare provider if you have questions about your symptoms or when to end isolation.
[1] As noted in the Food and Drug Administration labeling for authorized over-the-counter antigen tests, negative test results do not rule out SARS-CoV-2 infection and should not be used as the sole basis for treatment or patient management decisions, including infection control decisions.
Isolation Print Resource

Follow isolation and precaution recommendations if you have or suspect you have COVID-19. These steps help prevent spreading the virus to others in your household and your community. Take precautions regardless of your vaccination status.
File Details: 705 KB, 1 page
To receive email updates about COVID-19, enter your email address:
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
Understanding the CDC’s Updated COVID Isolation Guidance
The updated recommendations align guidance for COVID infection with that for other common respiratory viruses.
Aliza Rosen
For the first time since 2021, the Centers for Disease Control and Prevention has updated its COVID isolation guidance.
Specifically, it has shifted the recommendation that someone who tests positive for COVID isolate for five days to a timeline based on the progression of the person’s symptoms. The update is part of a larger strategy to provide one set of recommendations for most common respiratory illnesses , including COVID, influenza, and respiratory syncytial virus (RSV).
In this Q&A, virologist Andy Pekosz , PhD, a professor in Molecular Microbiology and Immunology , explains the CDC’s new isolation guidance, the reasons for the update, and why the prevention and treatment strategies we’ve all become accustomed to still play an important part in reducing respiratory virus transmission.
What are the updated recommendations for someone who comes down with a respiratory infection?
The updated guidance from the CDC is to “stay home and away from others (including people you live with who are not sick) if you have respiratory virus symptoms that aren't better explained by another cause.” You can resume normal activities once your symptoms are improving and you’ve been fever-free—without the aid of fever-reducing medications—for at least 24 hours.
For the five days after you resume your normal activities, you should take extra precautions, like wearing a well-fitting mask and maintaining distance from others, gathering outdoors or in well-ventilated areas, cleaning hands and high-touch surfaces often, and testing when possible before gathering with others. If symptoms or fever return, you should start back at square one: staying home and away from others until you’ve been improving and fever-free for at least 24 hours.
What should you do if you’re at higher risk of severe illness?
If you’re at higher risk of severe illness—generally, this is older adults and young children, pregnant people, people with disabilities, and people with compromised immune systems—seek testing and contact your physician. If you test positive for COVID or flu, there are antiviral medications that can be taken within a few days of symptom onset and are extremely effective in reducing the likelihood that your symptoms become severe or that you need to be hospitalized.
How does this differ from previous guidance?
Before this, the CDC recommended that people who test positive for COVID should isolate away from others for five days and wear a well-fitting mask around others for the following five days. This was different from the general guidance for other common respiratory viruses, like flu and RSV.
Now there is no one-size-fits-all duration for how long to isolate; rather, you can resume regular activities—ideally still using other prevention strategies, like masking and distancing—based on when your symptoms have improved and your fever has gone away.
This marks a significant change in guidance for people who test positive for COVID. Why has the guidance changed?
The CDC has simplified its recommendations for how long to stay home and isolate after testing positive or experiencing symptoms to be consistent across COVID-19, influenza, and RSV infections. This way, anyone who develops symptoms can follow the same isolation guidance, irrespective of what respiratory virus they’re infected with.
It’s important to note, though, that this guidance on how long to isolate is just one part of a larger strategy for combating respiratory viruses that includes:
- Being up to date on recommended vaccines.
- Practicing good hygiene regarding hand-washing, sneezing, and coughing.
- Being aware of antiviral treatment options for COVID-19 and influenza.
- Taking steps to improve indoor air quality.
If the guidance is the same for all respiratory viruses, is it still important to test to know what someone is sick with?
Yes, testing is still needed in order to get a prescription for antivirals to treat COVID-19 or influenza. Those antivirals have been shown to reduce disease severity in several different groups, so if you are in a high risk group, be sure to test early and contact your physician so you can get the antiviral prescriptions as soon as possible.
Testing can also play an important role in preventing transmission, particularly if you were recently around someone who has since become sick, or if you plan to spend time with someone who is at higher risk of severe infection.
For COVID in particular, rapid home antigen tests are a great way to determine whether you’re still infectious and able to infect others. Symptom severity can be fairly subjective and a presence or lack of symptoms does not always align with infectiousness , so testing out of isolation for COVID is still good practice if you have access to tests.
Does this new guidance mean that all of these respiratory viruses pose the same risk?
No, COVID-19 is still causing more cases and more severe disease than influenza or RSV. A person’s risk for severe infection will also vary based on a number of factors, including age and health conditions .
The updated guidance acknowledges that we can simplify the recommendations for what to do after becoming infected with a respiratory virus, as part of the larger strategy to address spread.
The CDC also recently recommended that people over age 65 receive an additional dose of this year’s COVID vaccine . What drove that decision?
There are a few reasons behind this new recommendation for older adults . First, most severe COVID infections are occurring in individuals 65 years and older who have not been vaccinated recently. The CDC’s recommendation notes that more than half of COVID hospitalizations between October 2023 and December 2023 occurred in adults over 65.
Second, we know immunity after vaccination wanes over a few months, so an additional dose will provide renewed protection through the spring. New COVID variants like JN.1 that are circulating now have some mutations that improve their ability to evade vaccine-induced immunity, but the antibodies made through vaccination still recognize them. It’s not a perfect match, but a second dose of this year’s vaccine will provide protection against current variants to an age group at increased risk of severe illness, hospitalization, and death.
When should people over 65 get this additional dose of the current COVID vaccine?
The recommendation from the CDC is for people 65 and older who have already received one dose of the 2023-24 COVID vaccine to get a second shot at least four months after their most recent dose .
For people in that age group who haven’t had the 2023-24 vaccine, there’s no need to wait. They can get their shot now to be protected through the spring.
Will there be an updated COVID-19 vaccine for these newer variants?
We can likely expect to see a new COVID-19 vaccine available this fall, just like we see new, updated influenza vaccines each fall. This spring—typically around May—a decision will be made on which variants the updated vaccine will be designed around, and like we saw in 2023, the new vaccine will be available in the fall as we head into the typical respiratory virus season.
Aliza Rosen is a digital content strategist in the Office of External Affairs at the Johns Hopkins Bloomberg School of Public Health.
- More Americans Could Benefit from Paxlovid for COVID Infection
- What to Know About the Updated COVID-19 Vaccine for Fall/Winter 2023
Related Content

Outbreak Preparedness for All

What’s Happening With Dairy Cows and Bird Flu

Decisive Action Needed to Stop Cervical Cancer Deaths

How Dangerous is Dengue?

The U.S. Syphilis Spike Has Been Brewing for Decades
- COVID-19 travel advice
Considering travel during the pandemic? Take precautions to protect yourself from COVID-19.
A coronavirus disease 2019 (COVID-19) vaccine can prevent you from getting COVID-19 or from becoming seriously ill due to COVID-19 . But even if you're vaccinated, it's still a good idea to take precautions to protect yourself and others while traveling during the COVID-19 pandemic.
If you've had all recommended COVID-19 vaccine doses, including boosters, you're less likely to become seriously ill or spread COVID-19 . You can then travel more safely within the U.S. and internationally. But international travel can still increase your risk of getting new COVID-19 variants.
The Centers for Disease Control and Prevention (CDC) recommends that you should avoid travel until you've had all recommended COVID-19 vaccine and booster doses.
Before you travel
As you think about making travel plans, consider these questions:
- Have you been vaccinated against COVID-19 ? If you haven't, get vaccinated. If the vaccine requires two doses, wait two weeks after getting your second vaccine dose to travel. If the vaccine requires one dose, wait two weeks after getting the vaccine to travel. It takes time for your body to build protection after any vaccination.
- Have you had any booster doses? Having all recommended COVID-19 vaccine doses, including boosters, increases your protection from serious illness.
- Are you at increased risk for severe illness? Anyone can get COVID-19 . But older adults and people of any age with certain medical conditions are at increased risk for severe illness from COVID-19 .
- Do you live with someone who's at increased risk for severe illness? If you get infected while traveling, you can spread the COVID-19 virus to the people you live with when you return, even if you don't have symptoms.
- Does your home or destination have requirements or restrictions for travelers? Even if you've had all recommended vaccine doses, you must follow local, state and federal testing and travel rules.
Check local requirements, restrictions and situations
Some state, local and territorial governments have requirements, such as requiring people to wear masks, get tested, be vaccinated or stay isolated for a period of time after arrival. Before you go, check for requirements at your destination and anywhere you might stop along the way.
Keep in mind these can change often and quickly depending on local conditions. It's also important to understand that the COVID-19 situation, such as the level of spread and presence of variants, varies in each country. Check back for updates as your trip gets closer.
Travel and testing
For vaccinated people.
If you have been fully vaccinated, the CDC states that you don't need to get tested before or after your trip within the U.S. or stay home (quarantine) after you return.
If you're planning to travel internationally outside the U.S., the CDC states you don't need to get tested before your trip unless it's required at your destination. Before arriving to the U.S., you need a negative test within the last day before your arrival or a record of recovery from COVID-19 in the last three months.
After you arrive in the U.S., the CDC recommends getting tested with a viral test 3 to 5 days after your trip. If you're traveling to the U.S. and you aren't a citizen, you need to be fully vaccinated and have proof of vaccination.
You don't need to quarantine when you arrive in the U.S. But check for any symptoms. Stay at home if you develop symptoms.
For unvaccinated people
Testing before and after travel can lower the risk of spreading the virus that causes COVID-19 . If you haven't been vaccinated, the CDC recommends getting a viral test within three days before your trip. Delay travel if you're waiting for test results. Keep a copy of your results with you when you travel.
Repeat the test 3 to 5 days after your trip. Stay home for five days after travel.
If at any point you test positive for the virus that causes COVID-19 , stay home. Stay at home and away from others if you develop symptoms. Follow public health recommendations.
Stay safe when you travel
In the U.S., you must wear a face mask on planes, buses, trains and other forms of public transportation. The mask must fit snugly and cover both your mouth and nose.
Follow these steps to protect yourself and others when you travel:
- Get vaccinated.
- Keep distance between yourself and others (within about 6 feet, or 2 meters) when you're in indoor public spaces if you're not fully vaccinated. This is especially important if you have a higher risk of serious illness.
- Avoid contact with anyone who is sick or has symptoms.
- Avoid crowds and indoor places that have poor air flow (ventilation).
- Don't touch frequently touched surfaces, such as handrails, elevator buttons and kiosks. If you must touch these surfaces, use hand sanitizer or wash your hands afterward.
- Wear a face mask in indoor public spaces. The CDC recommends wearing the most protective mask possible that you'll wear regularly and that fits. If you are in an area with a high number of new COVID-19 cases, wear a mask in indoor public places and outdoors in crowded areas or when you're in close contact with people who aren't vaccinated.
- Avoid touching your eyes, nose and mouth.
- Cover coughs and sneezes.
- Wash your hands often with soap and water for at least 20 seconds.
- If soap and water aren't available, use a hand sanitizer that contains at least 60% alcohol. Cover all surfaces of your hands and rub your hands together until they feel dry.
- Don't eat or drink on public transportation. That way you can keep your mask on the whole time.
Because of the high air flow and air filter efficiency on airplanes, most viruses such as the COVID-19 virus don't spread easily on flights. Wearing masks on planes has likely helped lower the risk of getting the COVID-19 virus on flights too.
However, air travel involves spending time in security lines and airport terminals, which can bring you in close contact with other people. Getting vaccinated and wearing a mask when traveling can help protect you from COVID-19 while traveling.
The Transportation Security Administration (TSA) has increased cleaning and disinfecting of surfaces and equipment, including bins, at screening checkpoints. TSA has also made changes to the screening process:
- Travelers must wear masks during screening. However, TSA employees may ask travelers to adjust masks for identification purposes.
- Travelers should keep a distance of 6 feet apart from other travelers when possible.
- Instead of handing boarding passes to TSA officers, travelers should place passes (paper or electronic) directly on the scanner and then hold them up for inspection.
- Each traveler may have one container of hand sanitizer up to 12 ounces (about 350 milliliters) in a carry-on bag. These containers will need to be taken out for screening.
- Personal items such as keys, wallets and phones should be placed in carry-on bags instead of bins. This reduces the handling of these items during screening.
- Food items should be carried in a plastic bag and placed in a bin for screening. Separating food from carry-on bags lessens the likelihood that screeners will need to open bags for inspection.
Be sure to wash your hands with soap and water for at least 20 seconds directly before and after going through screening.
Public transportation
If you travel by bus or train and you aren't vaccinated, be aware that sitting or standing within 6 feet (2 meters) of others for a long period can put you at higher risk of getting or spreading COVID-19 . Follow the precautions described above for protecting yourself during travel.
Even if you fly, you may need transportation once you arrive at your destination. You can search car rental options and their cleaning policies on the internet. If you plan to stay at a hotel, check into shuttle service availability.
If you'll be using public transportation and you aren't vaccinated, continue physical distancing and wearing a mask after reaching your destination.
Hotels and other lodging
The hotel industry knows that travelers are concerned about COVID-19 and safety. Check any major hotel's website for information about how it's protecting guests and staff. Some best practices include:
- Enhanced cleaning procedures
- Physical distancing recommendations indoors for people who aren't vaccinated
- Mask-wearing and regular hand-washing by staff
- Mask-wearing indoors for guests in public places in areas that have high cases of COVID-19
- Vaccine recommendations for staff
- Isolation and testing guidelines for staff who've been exposed to COVID-19
- Contactless payment
- Set of rules in case a guest becomes ill, such as closing the room for cleaning and disinfecting
- Indoor air quality measures, such as regular system and air filter maintenance, and suggestions to add air cleaners that can filter viruses and bacteria from the air
Vacation rentals, too, are enhancing their cleaning procedures. They're committed to following public health guidelines, such as using masks and gloves when cleaning, and building in a waiting period between guests.
Make a packing list
When it's time to pack for your trip, grab any medications you may need on your trip and these essential safe-travel supplies:
- Alcohol-based hand sanitizer (at least 60% alcohol)
- Disinfectant wipes (at least 70% alcohol)
- Thermometer
Considerations for people at increased risk
Anyone can get very ill from the virus that causes COVID-19 . But older adults and people of any age with certain medical conditions are at increased risk for severe illness. This may include people with cancer, serious heart problems and a weakened immune system. Getting the recommended COVID-19 vaccine and booster doses can help lower your risk of being severely ill from COVID-19 .
Travel increases your chance of getting and spreading COVID-19 . If you're unvaccinated, staying home is the best way to protect yourself and others from COVID-19 . If you must travel and aren't vaccinated, talk with your health care provider and ask about any additional precautions you may need to take.
Remember safety first
Even the most detailed and organized plans may need to be set aside when someone gets ill. Stay home if you or any of your travel companions:
- Have signs or symptoms, are sick or think you have COVID-19
- Are waiting for results of a COVID-19 test
- Have been diagnosed with COVID-19
- Have had close contact with someone with COVID-19 in the past five days and you're not up to date with your COVID-19 vaccines
If you've had close contact with someone with COVID-19 , get tested after at least five days. Wait to travel until you have a negative test. Wear a mask if you travel up to 10 days after you've had close contact with someone with COVID-19 .
- How to protect yourself and others. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html. Accessed Feb. 4, 2022.
- Domestic travel during COVID-19. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/travel-during-covid19.html. Accessed Feb. 4, 2022.
- Requirement for face masks on public transportation conveyances and at transportation hubs. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/face-masks-public-transportation.html. Accessed Feb. 4, 2022.
- International travel. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/international-travel/index.html. Accessed Feb. 4, 2022.
- U.S citizens, U.S. nationals, U.S. lawful permanent residents, and immigrants: Travel to and from the United States. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/international-travel-during-covid19.html. Accessed Feb. 4, 2022.
- Non-US. citizen, non-U.S. immigrants: Air travel to the United States. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/noncitizens-US-air-travel.html. Accessed Feb. 4, 2022.
- People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed Feb. 4, 2022.
- Stay up to date with your vaccines. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/stay-up-to-date.html. Accessed Feb. 4, 2022.
- Pack smart. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/page/pack-smart. Accessed Feb. 4, 2022.
- Travel: Frequently asked questions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/travelers/faqs.html. Accessed Feb. 7, 2022.
- Coronavirus (COVID-19) information. Transportation Security Administration. https://www.tsa.gov/coronavirus. Accessed Feb. 7, 2022.
- WHO advice for international traffic in relation to the SARS-CoV-2 Omicron variant (B.1.1.529). World Health Organization. https://www.who.int/news-room/articles-detail/who-advice-for-international-traffic-in-relation-to-the-sars-cov-2-omicron-variant. Accessed Feb. 7, 2022.
- VRHP/VRMA Cleaning guidelines for COVID-19. Vacation Rental Management Association. https://www.vrma.org/page/vrhp/vrma-cleaning-guidelines-for-covid-19. Accessed Feb. 7, 2022.
- Safe stay. American Hotel & Lodging Association. https://www.ahla.com/safestay. Accessed Feb. 7, 2022.
- Khatib AN, et al. COVID-19 transmission and the safety of air travel during the pandemic: A scoping review. Current Opinion in Infectious Diseases. 2021; doi:10.1097/QCO.0000000000000771.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- A Book: Future Care
- Antibiotics: Are you misusing them?
- COVID-19 and vitamin D
- Convalescent plasma therapy
- Coronavirus disease 2019 (COVID-19)
- COVID-19: How can I protect myself?
- Herd immunity and coronavirus
- COVID-19 and pets
- COVID-19 and your mental health
- COVID-19 antibody testing
- COVID-19, cold, allergies and the flu
- COVID-19 drugs: Are there any that work?
- Long-term effects of COVID-19
- COVID-19 tests
- COVID-19 in babies and children
- Coronavirus infection by race
- COVID-19 vaccine: Should I reschedule my mammogram?
- COVID-19 vaccines for kids: What you need to know
- COVID-19 vaccines
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- COVID-19: Who's at higher risk of serious symptoms?
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Extracorporeal membrane oxygenation (ECMO)
- Fever: First aid
- Fever treatment: Quick guide to treating a fever
- Fight coronavirus (COVID-19) transmission at home
- Honey: An effective cough remedy?
- How do COVID-19 antibody tests differ from diagnostic tests?
- How to measure your respiratory rate
- How to take your pulse
- How to take your temperature
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Loss of smell
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Multisystem inflammatory syndrome in children (MIS-C)
- Nausea and vomiting
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Shortness of breath
- Thermometers: Understand the options
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
- Vaccine guidance from Mayo Clinic
- Watery eyes
U.S. travel resources
- Check CDC recommendations for travel within the U.S.
- Review testing requirements for travel to the U.S.
- Look up restrictions at your destination .
- Review airport security measures .
Related resources
Make twice the impact.
Your gift can go twice as far to advance cancer research and care!
What to Do If You Test Positive for COVID-19 While Traveling
A fter two years of pandemic living, Americans are collectively ready for a vacation. About 85% of people in the U.S. expect to travel this summer, according to data from the industry trade group U.S. Travel Association. Many others aren’t even waiting that long. Almost 2.3 million people passed through U.S. Transportation Security Administration checkpoints on April 10, only slightly fewer than on that date in 2019.
No matter how much we might like to, though, it’s not always possible to take a vacation from COVID-19. The virus is still circulating widely , including in popular tourist destinations like the U.K., Germany, France, and Italy. That means getting sick while traveling is a real possibility—and one that can turn into an expensive and stressful logistical headache.
What happens if you get COVID-19 while traveling internationally?
To enter the U.S., international travelers currently need either a negative COVID-19 test result obtained within one day of their flight or proof that they have recovered from COVID-19 in the last 90 days. (This policy applies to both U.S. citizens and non-citizens, but children younger than 2 are exempt.) Without one of those documents, you cannot board a U.S.-bound flight. If you test positive, you should isolate and delay travel for 10 days , according to the U.S. Centers for Disease Control and Prevention (CDC).
But where do you stay if you need to quarantine abroad? And who pays for extended accommodations and rescheduled flights?
Specifics vary from country to country, but the short answer is that travelers are often on the hook. Exceptions to the test-to-return policy may be granted on an “extremely limited” basis, such as in the event of an emergency medical evacuation or humanitarian crisis, the CDC says—but the average vacationer won’t have many options beyond paying to extend their stay.
“Have a plan in case you have to remain overseas longer than anticipated,” the U.S. Department of State writes on its website . “This includes being ready to cover additional lodging costs, flight ticket change fees, and any other additional expenses they may incur due to the unexpected extension.”
Some travel insurance covers extra expenses incurred because of a COVID-19 case, but policies may not cover all costs related to an extension, according to a spokesperson for the U.S. Travel Insurance Association. “Travelers concerned about this potential disruption in their travels should first look for a policy that includes sickness or quarantine as a covered reason, and then determine which benefits quarantine falls under and the limits of those benefits,” they wrote in a statement.
A spokesperson for the State Department said travelers who must isolate should contact their hotels and airlines to arrange accommodations and re-book travel, and, if necessary, seek assistance from their nearest U.S. embassy or consulate. The spokesperson added that U.S. citizens traveling abroad are subject to local quarantine rules, which may differ from those of the U.S. CDC.
Certain countries maintain “quarantine hotels” where travelers can quarantine upon arrival (if required by that country) or ride out their isolation periods. USA Today reports that some resorts even offer discounted rates to guests who have to extend their stays to isolate. It’s smart to check ahead of time, however, as these hotels aren’t available in all areas and their costs vary widely.
Aliya Waldman, who is 29 and lives in Missouri, stayed in a quarantine hotel after catching COVID-19 during a March trip with the Birthright program, which organizes visits to Israel for Jewish young adults. Waldman was required to stay in the hotel for a full week, even though she tested negative after five days in isolation. She believes the costs of her stay and new return flight were covered by Birthright, but says the experience has made her think twice about traveling abroad independently during the pandemic. “I won’t be able to afford getting stuck in another country,” she says.
It’s not clear how long international travelers will have to abide by the CDC’s testing requirement. Four trade groups—the U.S. Travel Association, Airlines for America, American Hotel and Lodging Association, and U.S. Chamber of Commerce—recently urged the White House’s coronavirus czar to suspend that policy, since many Americans have some immunity to the virus from vaccination and prior exposure , and are thus at lower risk than they were earlier in the pandemic. “While providing little health benefit, this requirement discourages travel by imposing an additional cost and the fear of being stranded overseas,” they wrote in a joint letter .
What happens if you get COVID-19 while traveling within the U.S.?
There is no negative test requirement for most domestic transportation, only a mask mandate that the CDC said will be in place through at least May 3 . But that doesn’t mean you should get on a plane, train, or bus if you’re sick. The CDC says not to travel if you have symptoms of COVID-19 or have tested positive and not yet completed an isolation period. Without a testing requirement in place, though, that guideline depends heavily on the honor system.
Nonetheless, travelers who test positive for COVID-19 within the U.S. should self-isolate where they are, if there’s no way to get home via private transportation. Finding a place to do so can be tricky, though. Some U.S. cities with hotel quarantine programs, including New York City and Philadelphia , are winding them down, and Airbnb says guests should not check into a listing if they have COVID-19. Competing rental platform Vrbo, however, told Condé Nast Traveler that its private properties can be “an ideal lodging option for guests who need to quarantine or self-isolate.”
More Must-Reads From TIME
- The 100 Most Influential People of 2024
- Coco Gauff Is Playing for Herself Now
- Scenes From Pro-Palestinian Encampments Across U.S. Universities
- 6 Compliments That Land Every Time
- If You're Dating Right Now , You're Brave: Column
- The AI That Could Heal a Divided Internet
- Fallout Is a Brilliant Model for the Future of Video Game Adaptations
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Write to Jamie Ducharme at [email protected]
2-FOR-1 GA TICKETS WITH OUTSIDE+
Don’t miss Thundercat, Fleet Foxes, and more at the Outside Festival.
GET TICKETS
BEST WEEK EVER
Try out unlimited access with 7 days of Outside+ for free.
Start Your Free Trial

I Just Tested Positive for COVID. Should I Get on the Plane Anyway?
This is an ethical dilemma many of us are now facing: Is it OK to fly when I’ve got COVID? Outside’s travel expert weighs in.

Heading out the door? Read this article on the Outside app available now on iOS devices for members! >","name":"in-content-cta","type":"link"}}'>Download the app .
I’m about to go on spring break, and if I test positive for COVID before flying home, I can’t afford to isolate for five days in a place or miss extra work. It seems like everyone is coughing and sneezing on planes these days, and folks are opting to fly anyway. As much as I want to be a conscientious traveler, why should I pay another thousand bucks to stay in a hotel and quarantine for five days when nobody else appears to be doing that? —Weary of the Pandemic
You’re right. Most Americans are tired of dealing with pandemic rules and regulations—including the government. On January 30, President Biden announced that, as of May 11, the administration would officially shift away from treating COVID as a national public-health crisis and instead begin to manage it more like the flu or other seasonal respiratory disease. But does that mean we should be flying if we’re infected?
If you travel, even infrequently, and haven’t yet grappled with this question, chances are you will. I found myself in the throes of such a predicament right before the holidays. I was on assignment in Antarctica on a 100-passenger cruise ship, and although cruises were considered a hotbed for the coronavirus in the early days of the pandemic, almost two years later, any fear of catching the virus had faded from my mind. I should have known better and read the obvious signs: namely, being welcomed aboard by masked staff.
In hindsight, I probably should have taken a COVID test before flying home to New Jersey for Christmas to see my virus-phobic mom and immune-compromised aunt. But I’d been vaccinated, did not feel sick, and assumed that if anyone on the ship had gotten sick, we would have been alerted.
On the ten-hour leg of my flight from Buenos Aires to Houston, I sat next to a lovely elderly couple from the cruise, both of whom were vigilant about keeping on their N95 masks. Two days after I returned, I received an email from a passenger I’d befriended, who reported that at least a dozen people on the cruise had come down with COVID—including the couple I sat next to on the plane.
“Yes, I felt like an asshole,” a friend of mine who recently flew home when she thought she might have COVID admits. “Yes, I worried that I could’ve infected someone with a weak immune system. But people are coughing and sniffling on planes and in airports all the time.”
Thankfully, I tested negative, but the incident made me realize how easily I could have unknowingly gotten my family sick, perhaps with serious consequences. It also made me consider what the travel repercussions of testing positive might have been: missing Christmas with my family and having to quarantine alone in Ushuaia, Argentina, for at least five days (as recommended by the Centers for Disease Control and Prevention).
When I mentioned the situation to a friend, she admitted she’d recently taken a flight to Oahu, even though she knew she had COVID. “It’s so unethical, but I honestly was adamant about this trip,” she confided. “I needed a vacation, and I felt totally fine. I wore a mask, obviously.”
With Relaxed COVID Requirements, Many Sick Travelers Have Opted to Fly
We all have our reasons for traveling while sick. For better or for worse, sidestepping COVID guidelines has become much easier for travelers. For more than a year, providing timely proof of a negative COVID test ahead of your flight was a pricey, stressful hassle. So, as a road warrior, I was relieved when the CDC dropped this mandate for domestic travel last June. (Regulations for international travel have largely followed suit, with very few nations still requiring testing or proof of vaccination for inbound passengers; a full list of country-specific entry requirements can be found here .)
Quarantining while traveling has also been a costly and inconvenient part of the pandemic, as anyone who has been required to do it can attest. Now given the choice of traveling with COVID or hunkering down and isolating, which could cost thousands of dollars in hotel fees, room-service meals, missed work, and child care, many choose to fly infected with the coronavirus. And there are no rules stopping them from boarding a plane.
Last August, Ellen (not her real name) started to feel a tickle in her throat on the final day of her weeklong trip to Kauai. “I thought, Oh shit, I cannot get COVID right now,” she recalls. Her first vacation since pandemic travel restrictions had relaxed was, it turns out, anything but relaxing: The town of Hanalei felt super crowded. Restaurants averaged two-hour waits for dinner. And everything, from her Airbnb to meals, was expensive.
In this transitional period of the pandemic, many people are already treating COVID like the flu or a cold, says Henry Wu, director of the Emory TravelWell Center in Atlanta.
“By the last day of the trip, I started feeling run-down, and I really wanted to get home,” she says. “I didn’t want to be isolated in a last-minute, overpriced hotel room for five more days on the island and deal with flight-change costs. Not to mention my partner and I were due back at work.”
Ellen decided not to test before her flight back to the mainland, rationalizing that germs were everywhere and other passengers on her flight likely had COVID, too. She took extra precautions to assuage her guilt, double-masking with N95’s and sanitizing her hands more frequently than she normally would. But by the time she got home from the red-eye flight, she had a fever and sore throat, and when she finally took a COVID test, it was positive. Her partner, who had been around her unmasked at the height of contagion, never got sick.
“Yes, I felt like an asshole,” she admits. “Yes, I worried that I could’ve infected someone with a weak immune system. But people are coughing and sniffling on planes and in airports all the time.”
Amid the height of cold and flu season, it can seem like everyone traveling has a sniffle and the majority of people aren’t letting any illness—a common cold, COVID, or RSV among the top three this year and difficult to discern, based on symptoms—cancel big plans. In mid-January, Jamie DeLancey flew from Denver to San Francisco to watch the 49ers play in the NFL’s wild-card championship game, with what he assumed was a bad cold. He’d come down with COVID before and this felt different, so he did not test, noting that he hasn’t found such tests to be reliable. While he wore a mask on his flights, he didn’t wear one at the game.
In this transitional period of the pandemic, many people are already treating it like the flu or a cold, says Henry Wu, director of the Emory TravelWell Center in Atlanta. “In a way, that’s a logical rationale if you’re vaccinated and unlikely to get sick,” he says. “But that’s not the reality for some people who are elderly or immune-compromised. In many ways, things haven’t changed. If you’re sick and in contact with them, you could put them in the hospital.”
The CDC continues to advise avoiding travel if you are sick with or have tested positive for COVID, and isolating for at least five days after your positive test if you’re either asymptomatic or your symptoms first appear; following these guidelines, you should test again on day six and then wear a high-quality mask, such as an N95, when outdoors between days six and ten if you are around others, including on a plane. Whether the masses of travelers adhere to these is another thing altogether, as we’ve all seen play out on airlines.
How to Avoid Frustration, Fees, and Questionable Choices if You Get COVID Before or During a Trip
When Ross Holbrook flew from Denver to San José del Cabo, Mexico, with his wife and two young daughters last May, he watched his seatmate chug a bottle of DayQuil cold medicine. Holbrook was vaccinated and wearing a mask, but on day three of their family vacation, he tested positive for COVID; by day eight, his wife and one of the girls were also positive. Their Airbnb had a pool, so they made the best of things, but due to the mandatory quarantine rules in effect at the time, the family estimates they spent nearly $3,000 extending their car and Airbnb rentals. “We did consider driving home,” he says, but that idea was abandoned as impractical.
Five extra days in a destination like Mexico or Hawaii can cost a small fortune, not to mention difficult to find a room at the height of spring break or summer travel. What if you can’t afford to isolate and stay extra days in a place if you get COVID? Should you put off travel completely? Not necessarily, but you should have a COVID game plan that protects others, says Richard Martinello, the medical director of infection prevention at Yale New Haven Health in Connecticut.
“We all have busy lives, but as part of society, we have responsibilities not to put others in harm’s way, like not driving drunk,” he says. “Putting yourself in prolonged close contact with fellow travelers when you are knowingly sick, whether with COVID or any other contagious virus, is irresponsible. You never know who you’re sitting next to on a plane. If they’re immune-compromised, even a cold could push them over the edge to serious illness.”
Martinello acknowledges that the average traveler can’t afford to miss five additional days from work and home, so if you must travel sick, he suggests driving rather than flying or another form of public transportation. That said, if a partner or friend will be driving with you, they should be aware that you’re sick, he says, so they are consenting and can test and isolate appropriately.
Stuck somewhere like Hawaii, where flying home is the only option? Take every precaution to limit contagion spread. Wear an N95 mask. Paper surgical masks are the next best option, and homemade cloth masks even have some value in preventing the spread of germs, he says. You can also request to be moved next to an empty seat.
Check Your Airline’s COVID Policies
Several airlines, including Delta and United, continue to waive change fees for travelers looking to rebook due to COVID. Hawaiian Airlines will allow a one-time ticket change (with the difference in fares charged) for the same circumstances. Purchasing travel insurance for a flight also covers most COVID cancellations and rebookings.
Such thoughtful policies have prompted some travelers to make the morally conscious decision when illness sets in. Carmino DeMecurio was one of those people. He was booked to fly from New York City to Fort Lauderdale, Florida, for a business trip on January 19, but tested positive for COVID on January 16. He canceled the entire trip and said Delta immediately issued him an e-credit for a future flight. He was able to call in remotely for his meeting. “It wasn’t ideal to be the only person on a screen, but out of respect for others, it seemed like the right decision,” he says.
Consider Getting Travel Insurance
While airlines can be accommodating, quarantine lodging accommodations can be the real zinger for travelers. According to a spokesperson for the American Hotel and Lodging Association, it’s up to individual hotels to decide whether to offer a discounted rate if a guest must extend a stay due to quarantine. If you’ve splurged on a big trip, or you’re traveling far from home, trip insurance might be a smart investment. Allianz Travel Insurance recently added an Epidemic Coverage Endorsement to some of its plans. Under this new policy, if you have proof—a PCR test or a physician’s note—that you’ve tested positive for COVID during a trip, you can be reimbursed for unused, prepaid, nonrefundable trip costs, as well as additional accommodation and transportation costs incurred, depending on which situation applies.
Allianz’s OneTrip Basic policy, for example, offers up to $10,000 in trip cancellation and trip-interruption benefits per insured person, while the OneTrip Prime , the company’s most comprehensive policy, covers up to $100,000 in trip cancellation and up to $150,000 in trip-interruption benefits, with the option to tack on what’s called a Cancel Anytime upgrade, an option that reimburses travelers for up to 80 percent of prepaid, nonrefundable expenses for a trip that must be canceled for almost any reason not already covered by the policy.
According to an Allianz spokesperson, travelers can typically expect to pay 5 to 6 percent of the cost of their vacation for a standard travel-insurance policy. Actual prices will fluctuate based on a traveler’s age, state of residence, primary destination, length of stay, and total cost of their trip. For example, a 34-year-old from California traveling to Africa for a $9,700 three-week safari would pay $443 for a policy.
So should you travel with COVID if you come down with it on your upcoming spring-break trip? That depends on how prepared you are with a contingency plan, an adequate insurance policy, and the risk you’re willing to take when it comes to your personal health and the health of others, as you can still be hospitalized and even die from the virus. Not least is the ethical consideration of it all. Martinello advises travelers to follow the simple golden rule of “do unto others as you would have them do unto you.” And if you don’t trust your fellow air passengers—which, as this article reflects, are generally as eager to get away or get home as you are—do everyone a favor and wear a mask.
Any number of concerns are on our radar as we plan our next trip, from serious issues like how destinations are working to mitigate tourists’ environmental impact to inconveniences like months-long passport wait times. In this column, our travel expert Jen Murphy will be addressing your questions about how to navigate the world. Check out her previous column, on how to avoid bed bugs during your next hotel stay, here .
- United States
Popular on Outside Online
>", "path": "https://www.outsideonline.com/adventure-travel/destinations/north-america/the-best-trails-around-asheville-according-to-a-local-hiker/", "listing_type": "recirc", "location": "list", "title": "the best trails around asheville, according to a local hiker"}}'> the best trails around asheville, according to a local hiker, >", "path": "https://www.outsideonline.com/outdoor-gear/cars-trucks/guide-2025-4runner/", "listing_type": "recirc", "location": "list", "title": "an inside look into the 2025 toyota 4runner, tacoma, and land cruiser"}}'> an inside look into the 2025 toyota 4runner, tacoma, and land cruiser, >", "path": "https://www.outsideonline.com/outdoor-adventure/everest/mount-everest-season-preview/", "listing_type": "recirc", "location": "list", "title": "everest season kicks off with new rules, big crowds, and poop bags"}}'> everest season kicks off with new rules, big crowds, and poop bags, >", "path": "https://www.outsideonline.com/adventure-travel/destinations/reasons-to-love-running-in-austin/", "listing_type": "recirc", "location": "list", "title": "reasons to love running in austin"}}'> reasons to love running in austin.

How soon can you travel after testing positive for COVID-19?

A positive COVID-19 test during a trip can throw all your travel plans into limbo . But even a positive test in the weeks before you travel can be cause for concern.
If you're wondering when you'll be cleared to travel again after testing positive for COVID-19 , it's an important question: Here's everything you need to know.
For more TPG news delivered each morning to your inbox, sign up for our free daily newsletter .
What are the rules on flying back to the US?

If you've traveled internationally in the past year, you're likely familiar with the rules to fly back to the United States, but they've changed several times .
All travelers coming to the U.S., vaccinated or not, must produce a negative COVID-19 test taken within one calendar day of their departure. (The previous policy allowed vaccinated international travelers to show a negative test taken within three days before departure.) Additionally, international foreign travelers can enter the U.S. with proof of vaccination and a negative COVID-19 test .
If you have a positive test, does that mean you're banned from flying back to the U.S.? Not quite — but the rules can be a little confusing even if you're a seasoned traveler. If you recently had COVID-19 but recovered from the virus, you can still travel back to the U.S., but you'll need the proper paperwork. Let's break it down.
What paperwork do I need to travel after testing positive?

People who recovered from COVID-19 may continue to test positive for the virus up to three months after infection, even after they've recovered.
According to the U.S. Centers for Disease Control and Prevention, travelers who recently recovered from COVID-19 can fly back to the U.S. with proof that they've recovered from COVID-19 instead of a negative test. This proof can include your positive COVID-19 viral test result, but it has to be taken no more than 90 days before your flight's departure from a foreign country.
Additionally, you will also need a signed letter from a licensed healthcare professional stating that you're cleared to travel back to the U.S. According to the CDC, the letter from a healthcare provider must include:
- Information that identifies you personally (such as your name and date of birth) and matches your passport.
- The letter must be signed and dated by the healthcare provider.
- The letter must be on official letterhead that contains the name, address and phone number of the healthcare provider or public health official who signed the letter.
The CDC says the positive test result and letter together are referred to as "documentation of recovery." If you tested positive, that's the only way to be able to fly back to the U.S. if you've recovered from the virus but don't have a negative test result.
Proof of recovery is also acceptable for certain destinations, so you may be able to use this documentation to travel abroad after you're cleared by a doctor to travel.
What if I can't show proof of recovery?
The CDC is pretty strict on this rule: You either need a negative COVID-19 test or proof of recovery. The agency says, "If you have recovered from COVID-19 but are not able to obtain documentation of recovery that fulfills the requirements, you will need to show a negative COVID-19 viral test result from a sample taken no more than one day before your flight to the US departs."
How soon can I leave my destination after a positive COVID-19 test?

Travelers have to consider the possibility of testing positive for COVID-19 while abroad. What happens after the positive test depends entirely on the destination and, in some cases, your vaccination and booster status.
For instance, if you test positive while in France , you'll have to quarantine for seven days if you're fully vaccinated with a booster dose. However, you can leave quarantine after five days with a negative antigen or RT-PCR test result and if you've had no symptoms in 48 hours. If you are not fully vaccinated (France will soon require travelers to have a booster to be considered fully vaccinated ) or not vaccinated and test positive, you must isolate for 10 days, though the quarantine can be shortened.
So if you have international travel planned, you'll need to read up on the rules around how long you'll have to stay in quarantine and the documentation you'll need for your flight back to the U.S.

Explaining the New CDC Guidance on What To Do if You Have COVID-19
By Kate Yandell
Posted on March 15, 2024
Q: Is one day isolation sufficient to stop forward transmission of COVID-19?
A: People with COVID-19 could potentially transmit it to others well beyond a day after developing symptoms or testing positive. New guidance from the CDC advises people to isolate until they have been fever-free and with symptoms improving for at least 24 hours, and then take precautions for five days, which covers the period when “most people are still infectious.”
FULL ANSWER
The Centers for Disease Control and Prevention on March 1 updated its guidance on preventing the spread of respiratory viruses, consolidating advice on a range of common respiratory illnesses including COVID-19, flu and respiratory syncytial virus, or RSV.
Since December 2021 , the agency had recommended individuals isolate for at least five days after developing symptoms of COVID-19, or after a positive test if asymptomatic. After five days, the agency recommended various symptom-based criteria for leaving isolation combined with additional continued precautions, such as masking.

The new guidance drops the standard minimum of five days of isolation in favor of a symptom-based approach. The agency advises people to stay home and away from others when they are sick with a respiratory virus. People can cease isolation if, over a period of 24 hours, their overall symptoms have been improving and they have been fever-free without using fever-reducing medications.
Many people have had questions about what the new guidance means for people who have COVID-19. Some, like our reader, have referred to the idea that the guidance means only one day of isolation is needed. “do you agree with Biden that one day isolation for covid is fine and dandy??” asked one person on X, formerly known as Twitter.
But that’s not what Biden or the CDC is recommending.
“It’s not saying isolate for 24 hours,” epidemiologist Ronit Dalmat , a research scientist at the University of Washington, told us, referring to the CDC guidance. “It’s saying if you have a fever, absolutely stay home” until it has been gone for 24 hours, and also stay home until other symptoms are improving.
Nor does the CDC say people are guaranteed not to spread COVID-19 or other respiratory illnesses after their symptoms have improved. “Keep in mind that you may still be able to spread the virus that made you sick, even if you are feeling better,” the guidance says. “You are likely to be less contagious at this time, depending on factors like how long you were sick or how sick you were.”
The guidance recommends continuing to take precautions for five days after resuming normal activities. These include physical distancing, testing, improving air quality, using good hygiene and wearing a well-fitting mask, such as an N95 or KN95.
“The total number of days of precautions when sick, that is, a period of staying home and away from others plus 5 days of additional actions, covers the period during which most people are still infectious,” the CDC wrote in an FAQ.
“That whole period could be quite a while,” Dalmat said. “That could be 10 days for some people.”
The CDC said in background materials accompanying the new guidance that it looked at data from countries and states that had adopted similar policies for COVID-19 isolation and had not seen “clear increases in community transmission or hospitalization rates.”
“The updated guidance on steps to prevent spread when you are sick particularly reflects the key reality that many people with respiratory virus symptoms do not know the specific virus they are infected with,” the CDC said. The agency noted that its survey data indicated less than half of people with cold or cough symptoms would take an at-home COVID-19 test.
Some on social media have misinterpreted the guidance as an admission that it was always reasonable to liken COVID-19 to the flu, as was done early in the pandemic despite the marked difference in the diseases’ severity.
But the new CDC guidance acknowledges the continued seriousness of COVID-19 while also detailing the ways in which treatments, vaccines and population immunity have improved outcomes for people with the disease.
“COVID-19 remains a greater cause of severe illness and death than other respiratory viruses, but the differences between these rates are much smaller than they were earlier in the pandemic,” the CDC said . The agency explained that the risks are reduced due to the availability of COVID-19 treatments and population immunity to the virus, both from vaccination and prior infection. The agency also said that long COVID remains a risk, although the prevalence appears to be falling.
The Science on COVID-19 Transmission
Whether someone transmits COVID-19 depends on multiple factors . These include a person’s infectious viral load, but also the susceptibility of the people the infected person encounters and the precautions taken.
There’s no one-size-fits-all answer to how long a particular individual will shed infectious virus and how much they will shed. “Everybody has a slightly different ability to control the amount of virus in their system, which is a part of what makes the virus shed,” Dalmat said. Variation in how people’s bodies fight a virus affects “how much virus you are putting in the world that is infectious.”
There’s evidence that a relatively small number of people who shed particularly high levels of the virus over the course of their infections have been responsible for a disproportionate number of COVID-19 cases, and many people with COVID-19 do not infect others.
However, according to the CDC, the data on the typical overall length of shedding has not significantly changed, even as new variants of SARS-CoV-2 — the virus that causes COVID-19 — have arisen. “Even as the SARS-CoV-2 virus has continued to evolve, the duration of shedding infectious virus has remained relatively consistent, with most individuals no longer infectious after 8-10 days,” the agency said .
The CDC accompanied this statement with a figure showing data collected by the Respiratory Virus Transmission Network from five U.S. sites between November 2022 and May 2023 (see below). One line on the graph (light blue) shows how often researchers were able to isolate and grow — or culture — virus from people with COVID-19.
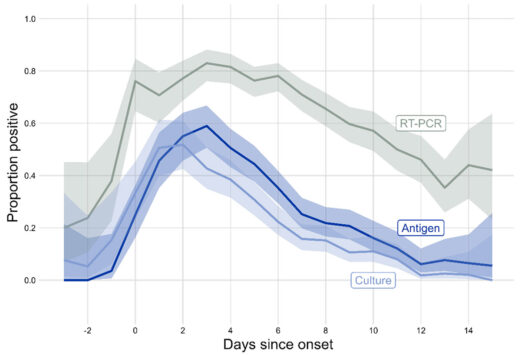
Trying to culture the virus that causes COVID-19 from a respiratory sample — a laborious process used in research — indicates whether someone is carrying infectious virus. The figure shows that the proportion of people with culturable virus began to increase two days before symptoms begin, or before a positive test for those who were asymptomatic, peaking around one to two days after symptom onset. After that, the rate began falling, with around one-third of people having culturable virus at day five. By day 10, the percentage had dropped to around 10%.
A different study , published in 2023 in the International Journal of Infectious Diseases, combined data from multiple studies done in people diagnosed with COVID-19 in 2021 and 2022. The average duration of shedding of culturable virus was just over five days from symptom onset or first positive PCR test, whichever came first.
Another metric for assessing infectiousness in people with COVID-19 is viral load, often measured as the amount of viral materials, such as RNA or proteins, found in a respiratory sample. A 2023 study published in Clinical Infectious Diseases found that median viral load for people diagnosed with COVID-19 peaked around three or four days after symptoms started. The study assessed people seeking testing for respiratory infections between April 2022 and April 2023.
Someone who is shedding infectious virus may or may not transmit it to others. One factor is that the average person is less susceptible to infection today than they were early in the pandemic, Dalmat said.
“Even if the person is producing the exact same amount of virus today as they could have three years ago, the people on the other end on average are less likely to get infected,” Dalmat said, explaining that today more than 98% of the population has had some exposure to COVID-19 itself, COVID-19 vaccines or both.
When people do get infected, the cases tend to be less severe. “Among the people who get infected with COVID these days, on average it is much rarer that it turns into a very serious illness,” Dalmat said, while also acknowledging that a lot of individuals “are still very vulnerable.” People at elevated risk for severe disease include those who are elderly or immune compromised.
While the CDC guidance harmonizes suggested precautions for COVID-19 and other common respiratory viruses, there are differences in the details of how COVID-19 and other respiratory viruses are spread.
The new guidance is meant to be a general rule of thumb but does not apply to health care settings or cases where there is an outbreak of a disease that requires special instructions, the CDC said. The CDC also said the agency is working on specific guidance for schools, which should be available prior to the 2024/2025 school year.
Masks, Tests and Other Precautions
Isolating from other people when sick is a key way to reduce one’s risk of spreading COVID-19. But the CDC guidance lists additional ways to reduce the chances of spreading a respiratory illness.
Masks can help prevent the wearer from spreading a respiratory virus. They can also protect others from inhaling a virus, particularly well-fitting masks such as N95 or KN95 respirators, the guidance says. Individuals can take measures to improve their hygiene and the air quality in their surroundings and maintain physical distance from others, such as by avoiding crowded spaces.
The CDC still recommends testing to help high-risk people who are sick determine whether to seek treatment for a specific virus. For instance, someone with COVID-19 may benefit from receiving Paxlovid within five days of when their symptoms start. The guidance also lists tests as a tool that can help people decide when they need to take precautions to avoid spreading disease.

At-home rapid antigen tests can be helpful for people who are recovering from COVID-19 and want to see if they still have infectious virus, Dalmat said. In their research, she and her colleagues found that among people who tested positive for COVID-19 on a rapid antigen test, subsequent negative antigen test results were “very, very highly correlated to whether you had infectious virus or not,” she said. That means people with COVID-19 who start to test negative on rapid antigen tests as they get better likely are no longer at risk of infecting others.
However, the CDC cautions that rapid antigen tests early in the course of a person’s infection often miss COVID-19. People who are sick should be taking precautions regardless of test results, Dalmat said. “They shouldn’t test and have a negative test be the end of it,” she said.
The authors of the Clinical Infectious Diseases study , which measured viral loads over the course of infection, wrote that “our data in combination with others’ suggest that symptomatic individuals testing positive for SARS-CoV-2 by PCR currently may not reliably test positive on a rapid antigen test until the third, fourth, or even fifth day of symptoms.”
The CDC guidance says people can end isolation when they have been fever-free and their symptoms have been improving for at least 24 hours. Dalmat cautioned that the definition of improving symptoms is somewhat ambiguous.
“Symptoms improving can mean different things to different people,” Dalmat said, adding that people should make sure their symptoms are truly getting better. “If your symptoms are not really improving – not kind of plateauing but really improving — you should continue to stay home and continue to take whatever measures you are taking in your household.”
Editor’s note: SciCheck’s articles providing accurate health information and correcting health misinformation are made possible by a grant from the Robert Wood Johnson Foundation. The foundation has no control over FactCheck.org’s editorial decisions, and the views expressed in our articles do not necessarily reflect the views of the foundation.
Branswell, Helen. “ CDC Eases Isolation Guidance for Covid and Other Respiratory Illnesses .” STAT. 1 Mar 2024.
“ Preventing Spread of Respiratory Viruses When You’re Sick .” CDC website. Updated 1 Mar 2024.
“ CDC’s Updated Respiratory Virus Guidance: What to Do When You Are Sick .” CDC website. 1 Mar 2024.
“ CDC Updates and Shortens Recommended Isolation and Quarantine Period for General Population .” CDC website. 27 Dec 2021.
“ Isolation and Precautions for People with COVID-19 .” CDC website. Updated 11 Mar 2023.
Cali Dreaming NaphiSoc (@NaphiSoc). “ Prof Hotez: do you agree with Biden that one day isolation for covid is fine and dandy?? ” X. 2 Mar 2024.
Dalmat, Ronit. Interview with FactCheck.org.
“ Respiratory Virus Guidance Update FAQs .” CDC website. Updated 1 Mar 2024.
“ Background for CDC’s Updated Respiratory Virus Guidance .” CDC website. Updated 1 Mar 2024.
Matt Kim 🇰🇷🇺🇸 (@mattattack009). “ Zero Accountability .” Instagram. 4 Mar 2024.
DiedSuddenly (@DiedSuddenly_). “ Turns out everything they told you about Covid was a lie. Of course they knew this 3 years ago, and they’ll show zero remorse for what they have done .” X. 2 Mar 2024.
Citizen Free Press (@CitizenFreePres). “ … and then one day, four years later on a Friday afternoon when no one was looking, the CDC admitted that the great conspiracy theory about Covid was true .” X. 1 Mar 2024.
Rieder, Rem. “ Trump’s Deceptive Comparison of the Coronavirus to the Flu .” FactCheck.org. 9 Sep 2020.
“ How is COVID-19 transmitted? ” FactCheck.org. Updated 11 Feb 2022.
Puhach, Olha et al. “ SARS-CoV-2 Viral Load and Shedding Kinetics .” Nature Reviews Microbiology. 2 Dec 2022.
Wu, Yu et al. “ Duration of Viable Virus Shedding and Polymerase Chain Reaction Positivity of the SARS-CoV-2 Omicron Variant in the Upper Respiratory Tract: A Systematic Review and Meta-Analysis .” International Journal of Infectious Diseases. 18 Feb 2023.
Frediani, Jennifer K. et al. “ The New Normal: Delayed Peak SARS-CoV-2 Viral Loads Relative to Symptom Onset and Implications for COVID-19 Testing Programs .” Clinical Infectious Diseases. 28 Sep 2023.
Cevik, Muge and Kalil, Andre C. “ Omicron Variant: Assessing the Duration of Viral Shedding and Its Implications .” Clinical Microbiology and Infection. 25 Nov 2022.
“ Risk Factors for Severe Illness from Respiratory Viruses .” CDC website. Updated 1 Mar 2024.
Wu, Katherine J. “ Why Are We Still Flu-Ifying COVID? ” The Atlantic. 28 Feb 2024.
“ Masks and Respiratory Viruses Prevention .” CDC website. Updated 1 Mar 2024.
“ Hygiene and Respiratory Viruses Prevention .” CDC website. Updated 1 Mar 2024.
“ Taking Steps for Cleaner Air for Respiratory Virus Prevention .” CDC website. Updated 1 Mar 2024.
“ About Physical Distancing and Respiratory Viruses .” CDC website. Updated 1 Mar 2024.
“ Preventing Respiratory Viruses .” CDC website. Updated 1 Mar 2024.
“ COVID-19 Treatments and Medications .” CDC website. Updated 15 Mar 2024.
“ Testing and Respiratory Viruses .” CDC website. Updated 1 Mar 2024.
Drain, Paul K. et al. “ Duration of Viral Infectiousness and Correlation with Symptoms and Diagnostic Testing in Non-Hospitalized Adults during Acute SARS-CoV-2 Infection: A Longitudinal Cohort Study .” Journal of Clinical Virology. 3 Mar 2023.
Advertisement
Supported by
What to Know About the C.D.C. Guidelines on Vaccinated Travel
In updated recommendations, the federal health agency said both domestic and international travel was low risk for fully vaccinated Americans. But travel remains far from simple.
- Share full article

By Ceylan Yeginsu
The Centers for Disease Control and Prevention updated its guidance for fully vaccinated Americans in April, saying that traveling both domestically and internationally was low risk.
The long-awaited recommendations were issued by federal health officials after a series of studies found that vaccines administered in the United States were robustly effective in preventing infections in real-life conditions.
One is considered fully vaccinated two weeks after receiving the single dose of the Johnson & Johnson vaccine, or two weeks after receiving the second dose of the Pfizer-BioNTech or Moderna shots.
If you decide to travel, you might still have some questions. Here are the answers.
Will I still need to wear a mask and socially distance while traveling?
Yes. Under federal law, masks must be worn at airports in the United States, onboard domestic flights and in all transport hubs. The C.D.C. says that as long as coronavirus measures are taken in these scenarios, including mask wearing, fully vaccinated Americans can travel domestically without having to take a test or quarantine, although the agency warns that some states and territories may keep their local travel restrictions and recommendations in place.
For those wishing to travel internationally, a coronavirus test will not be required before departure from the United States unless mandated by the government of their destination. Vaccinated travelers are still required to get tested three days before travel by air into the United States, and are advised to take a test three to five days after their return, but will not need to self-quarantine.
Can I go abroad?
Yes, but only to countries that will have you.
More than half the world’s countries have reopened to tourists from the United States, including the countries of the European Union , which on June 18 added the United States to its “safe list” of countries, meaning that American travelers can now visit. While the European Union aims to take a coordinated approach to travel this summer, member states will be allowed to set their own requirements for travelers from individual countries based on their own epidemiological criteria, which means they may require testing or vaccination.
Some places like Turkey, Croatia and Montenegro had already been welcoming Americans with negative test results. Greece joined that growing list in May, ahead of most European countries, opening to fully vaccinated tourists and other foreigners with a negative test.
Many Caribbean nations have reopened to American tourists, but each has its own coronavirus protocols and entry requirements.
Here’s a full list of countries Americans can currently travel to.
What about domestic travel? Is it free and clear to cross state borders?
If you are fully vaccinated, the C.D.C. says you can travel freely within the United States and that you do not need to get tested, or self-quarantine, before or after traveling. But some states and local governments may choose to keep travel restrictions in place, including testing, quarantine and stay-at-home orders. Hawaii , for instance, still has travel restrictions in place.
Before you travel across state lines, check the current rules at your destination.
How are they going to check that I’m fully vaccinated?
Right now, the best way to prove that you have been vaccinated is to show your vaccine card .
Digital vaccine and health certificates showing that people have been vaccinated or tested are in various stages of development around the world and are expected, eventually, to be widely used to speed up travel.
The subject of “ vaccine passports ” is currently one of the most hotly debated topics within the travel industry, with questions over the equity of their use and concerns over health and data privacy.
In early April, Gov. Ron DeSantis of Florida issued an executive order that would ban local governments and state businesses from requiring proof of vaccination for services.
And in March, the European Union endorsed its own vaccine certificate , which some countries are already using, with more expected to adopt it by July 1.
But what about my kids? What’s the guidance on traveling with unvaccinated people?
The C.D.C. advises people against travel unless they have been vaccinated. If you must travel, the agency recommends testing one to three days before a trip and following all coronavirus guidance at your destination.
In May, the F.D.A. expanded its emergency use authorization of the Pfizer-BioNTech coronavirus vaccine to include adolescents between 12 and 15 years of age.
All air passengers aged two and older coming into the United States, including fully vaccinated people, are required to have a negative Covid-19 test result taken no more than three days before they board their flight.
What is my moral obligation to the places I visit where most people are not vaccinated?
The United States inoculation rollout has been among the fastest in the world, but there is a stark gap between its rapid rollout and the vaccination programs in different countries. Some nations have yet to report a single dose being administered.
Many countries are currently seeing a surge in new cases and are implementing strict coronavirus protocols, including mask mandates in public spaces, capacity limits at restaurants and tourist sites and other lockdown restrictions.
It is important to check coronavirus case rates, measures and medical infrastructure before traveling to your destination and not to let your guard down when you get there. Even though you are fully vaccinated, you may still be able to transmit the disease to local communities who have not yet been inoculated.
You can track coronavirus vaccination rollouts around the world here.
Follow New York Times Travel on Instagram , Twitter and Facebook . And sign up for our weekly Travel Dispatch newsletter to receive expert tips on traveling smarter and inspiration for your next vacation.
Ceylan Yeginsu is a London-based reporter. She joined The Times in 2013, and was previously a correspondent in Turkey covering politics, the migrant crisis, the Kurdish conflict, and the rise of Islamic State extremism in Syria and the region. More about Ceylan Yeginsu
CDC says people exposed to COVID-19 don't have to isolate. What does that mean for travel?
Unvaccinated Americans don’t have to quarantine anymore if they’ve been exposed to COVID-19, according to newly relaxed guidelines from the Centers for Disease Control and Prevention. Also, people who test positive can end isolation sooner if they are asymptomatic or their symptoms improve quickly.
CDC spokesperson Tom Skinner told USA TODAY on Friday that additional guidance for travel would be coming soon. He did not provide a timeline for those updates.
"CDC is in the process of updating guidance for K-12/ECE, healthcare settings, high-risk congregate, and travel," Skinner said in an email. "So as of now, there are no changes to guidance for travel."
I got COVID while traveling: Here's what I wish I knew (and what I needed) to go back home
First vacation since the pandemic?: What to bring – and what to leave behind
Learn more: Best travel insurance
With limited exceptions , only vaccinated foreign nationals may enter the U.S., but U.S. citizens may enter without being vaccinated. Pre-departure testing has not been required for entry into the country since mid-June.
Here's what all travelers should know about entering the U.S. by air, land and sea.
Can I travel if I am not up-to-date on COVID-19 vaccines and was exposed to COVID-19?
The CDC now recommends people mask up for 10 days and test after five days if they are not fully vaccinated but are exposed to someone who is COVID-19 positive. This is in line with existing recommendations for people who are fully vaccinated.
Regardless of vaccination status, the CDC advises people who test positive to quarantine at least five days , instead of the previous 10.
"On Day 6, or later, when they are fever-free for 24 hours and their other symptoms have improved, they can end isolation and wear a mask indoors at home and in public," said Greta Massetti, an author of the CDC guidelines.
Traveling by plane to the US
Air travel is pretty much back to normal now for U.S. citizens. There are no pre-departure testing requirements for any travelers, and Americans arriving from abroad do not need to show proof of vaccination. The same applies to immigrants and lawful permanent residents as well.
The CDC does still recommend pre-departure testing for all passengers flying to the U.S., but it is not required.
Foreign nationals, however, are still required to show proof of vaccination to enter the U.S. before boarding their flight.
WHO and world leaders: How we're building better, more equitable vaccine systems
Here's what the CDC counts as fully vaccinated for the purposes of international visitors:
- Two weeks (14 days) after your dose of an accepted single-dose vaccine
- Two weeks (14 days) after your second dose of an accepted two-dose series
- Two weeks (14 days) after you received the full series of an accepted COVID-19 vaccine (not placebo) in a clinical trial
- Two weeks (14 days) after you received two doses of any “mix-and-match” combination of accepted COVID-19 vaccines administered at least 17 days apart.
According to industry trade group Airlines for America, as of June, airlines were still carrying almost 20% fewer transatlantic travelers than they were in 2019.
I took a CO2 detector on a flight: It showed me when I was most likely exposed to COVID
Can US citizens travel to Canada and Mexico by land or ferry?
The borders between the U.S., Canada and Mexico are open, but some restrictions remain.
With few exceptions, only fully vaccinated foreign nationals may enter Canada.
There are no entry restrictions for U.S. citizens entering Mexico, but travelers may be subject to health screenings upon arrival .
Vaccination is not required for U.S. citizens returning to the U.S. by land or ferry, but it is required for foreign nationals .
COVID-19 testing is not required for anyone entering the U.S. or Mexico, nor is it required for fully vaccinated travelers entering Canada.
U.S. Customs and Border Protection notes that "all testing requirements for travel fall under the authority and purview of the CDC."
"CBP is currently operating under the Secretary of Homeland Security’s Notification of Temporary Travel Restrictions Applicable to Land Ports of Entry and Ferries Service Between the United States and Canada/Mexico," a spokesman for the federal agency said in a statement to USA TODAY. "CBP will continue to enforce these restrictions until they are lifted or rescinded by the Secretary of Homeland Security."
What does the new guidance mean for cruise lines?
The CDC issued updated COVID-19 guidance for cruise ships last month, including recommended protocols for symptomatic passengers, crew and their close contacts.
As part of those guidelines, the agency said all symptomatic travelers should be isolated and tested as soon as they report symptoms to medical personnel. In addition to identifying and testing the close contacts of those infected, the CDC said cruise ships may consider a number of measures, including quarantine “until at least 5 full days after their last exposure,” among other steps, according to its website .
Travelers can check with their cruise line for its latest protocols.
“Passengers sailing on CLIA-member cruise lines will continue to see health and safety protocols in place that evolve commensurate with the public health situation,” Anne Madison, spokesperson for Cruise Lines International Association, told USA TODAY.
Carnival Cruise Line, for instance, requires passengers who are “in close contact with or exposed to any guest or crew member who tests positive for COVID-19” or who have symptoms to get tested, along with their close contacts, according to its website . Those travelers may need to quarantine in their staterooms until they are cleared by the medical team.
Royal Caribbean International also requires guests who test positive to isolate, and close contacts “will need to meet necessary quarantine and/or testing requirements based on their vaccination status,” according to the line’s website .
Contributing: Associated Press
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
- Considerations Ahead of Testing
- At-Home Test Accuracy
- PCR vs. Rapid Tests
- Testing Options for Breakthrough Cases
- Positive Result: What to Do Next
- Does Insurance Cover At-Home COVID Tests?
- Best At-Home Tests
- Retesting After Having COVID
What to Do If You Get a Positive At-Home COVID-19 Test Result
Take these steps to avoid spreading the virus
- Test Options
- Next in At-Home COVID Test Guide Does Health Insurance Cover At-Home COVID Tests?
A positive at-home COVID-19 test result may appear to answer one concerning question ("Do I have the virus?") but lead to others ("Now what?"). So it can help to know more about what a positive test means and what to do next if you have a fever, cough, loss of smell, or other COVID-19 symptoms .
It's just as important to understand the limits of a test. The availability of a fast, at-home COVID-19 test is helpful to anyone with symptoms or who's been exposed to the virus. But an at-home test can give incorrect results too. Notably, the rapid antigen at-home tests can give a false negative, saying you don't have COVID when you really do.
This article explains how at-home COVID-19 tests work, their accuracy, and what to do with a positive test result . It also presents precautions that are still necessary, even if you take frequent at-home tests.
Verywell / Ellen Lindner
Which COVID Test Is More Accurate?
At-home COVID tests can be purchased from a pharmacy, retail store, or online. Look for a label denoting Food and Drug Administration (FDA) authorization, since these tests have been evaluated by the FDA for reliability.
As of November 2022, there were 27 different at-home tests authorized by the FDA and sold over the counter, most of them antigen tests. All of these tests rely on a nasal swab from the nostrils and deliver results within 10 to 60 minutes. The most common time frame is 15 or 20 minutes.
These at-home tests are different from those mailed to a laboratory for analysis after you collect the sample at home. There are dozens of those PCR tests as well, with a longer delay until you receive results.
Regardless of the type of test, at-home tests are a great option for those experiencing COVID-19 symptoms who want to test before going to an in-person testing center.
Types of COVID-19 Tests
Diagnostic COVID-19 tests are meant for diagnosing an active COVID-19 infection. They require specimen collection from the nose or saliva. The two types of diagnostic tests are:
- PCR (polymerase chain reaction) tests , also known as molecular tests. They look for viral DNA and are highly accurate, but take longer and are more expensive. PCR COVID-19 tests are considered the gold standard. Most at-home PCR tests require mailing the sample to a lab, with results in 24–48 hours.
- Antigen tests , also known as rapid tests, look for viral proteins, give results within minutes, and are less expensive. However, antigen tests are less accurate than PCR tests and have more false negative results. Depending on the likelihood of infection, a negative antigen test may need to be followed up with a PCR.
Another type of test for COVID-19 is the antibody test, which requires a blood specimen. Self-tests do not detect antibodies, and this test should not be performed to diagnose an active COVID-19 infection.
Antibody tests demonstrate prior infection by testing for antibodies, which are proteins made by the body that remain in the blood after infection.
Some antibody tests may be positive in vaccinated people, since their bodies have also created certain antibodies.
Is a Positive At-Home Result Accurate?
During cold and flu season, symptoms like nasal congestion and fatigue don't necessarily mean COVID-19. But it can be challenging to tell the illnesses apart, since they share certain symptoms.
A negative result from an at-home test can be very reassuring, but know that certain situations and types of tests may require repeat or follow-up testing. As with any kind of medical testing, false negatives and false positives can happen. These decrease the accuracy of a test.
A false negative test means that the test result shows up as negative when the person actually does have COVID-19. This situation is more common with antigen tests, compared with PCR tests.
False negatives can happen due to improper specimen collection, which is why it's important to perform the test exactly as instructed by the kit. Keep in mind that COVID-19 variants may have mutations that make them undetectable by the specific test.
A false positive test means that the test shows a positive result when the person is not actually infected with COVID-19. False positive results are much less common and can happen due to a problem with the test kit itself. They can also occur for a period of time after a person has recovered from COVID-19.
A positive result should not be assumed to be a false positive, and action must be taken when a positive result is received.
In some cases when COVID-19 infection is unlikely, a confirmatory PCR test can be considered after a positive result on the antigen test.
False Negatives and At-Home COVID Tests
COVID-19 rapid antigen at-home tests can give a false negative result. It's possible when the viral load is low, such as when testing is done too soon after exposure and you don't yet have symptoms. That's why rapid antigen tests for COVID-19 are most accurate at least five days after exposure. Contact your healthcare provider for additional guidance.
Next Steps After a Positive COVID Test
At-home COVID tests are very specific, making false positive rates low. For this reason, a positive test result should not be considered a false positive, and you should take steps after receiving a positive test to decrease the chances of passing the virus to other people.
To reduce the chances of spreading COVID, the Centers for Disease Control and Prevention (CDC) recommends that you:
- Isolate at home until you've been fever-free for 24 hours (without taking fever-reducing medication) AND your symptoms are mild and improving.
- Take additional precautions for five days following isolation , such as wearing a well-fitting mask, keeping a distance from others, and washing your hands often.
If you need to isolate at home, take the following measures:
- Stay home unless you require medical care.
- If you live with others, try to avoid contact as much as possible by staying in a separate room, and use a separate bathroom, if possible.
- Don't share personal items like cups or towels.
- Improve ventilation in your home, if possible.
Positive Tests and Treatment
A positive at-home COVID-19 test doesn't necessarily require hospitalization or in-person treatment. Most cases of COVID-19 do not.
At-home care should include lots of rest and plenty of fluids to prevent dehydration.
Over-the-counter fever-reducing medication, such as Tylenol (acetaminophen) and NSAIDs like Advil or Motrin (ibuprofen), can lower fever and ease body aches and headache. Cold and flu medications like decongestants and expectorants can also help relieve symptoms.
Stay in contact with your healthcare provider and let them know if you are experiencing worsening symptoms or have any questions. While most people do not experience severe symptoms, some have mild symptoms initially that worsen several days later.
When to Seek Immediate Medical Care
If you experience concerning symptoms such as shortness of breath, chest pain, and blue or gray skin or lips, you should seek medical care immediately.
Your healthcare provider may recommend certain treatments approved for treating COVID-19, particularly if you have underlying conditions that increase your risk for severe complications.
For example, the antiviral treatment Paxlovid can be given in an outpatient setting and is effective at reducing hospitalization and death in people with COVID-19. People who may benefit include those who:
- Are aged 65 and older
- Live with a compromised immune system
- Have heart or lung diseases
- Are diagnosed with diabetes
- Live with obesity
This medication is most effective when given as early as possible, within five days of when symptoms begin.
The information in this article is current as of the date listed. As new research becomes available, we’ll update this article. For the latest on COVID-19, visit our coronavirus news page .
Centers for Disease Control and Prevention. Self-testing.
Food and Drug Administration. List of authorized at-home OTC COVID-19 diagnostic tests .
Centers for Disease Control and Prevention. Guidance for Antigen Testing for SARS-CoV-2 for Healthcare Providers Testing Individuals in the Community .
Food and Drug Administration. At-Home COVID-19 Antigen Tests-Take Steps to Reduce Your Risk of False Negative: FDA Safety Communication .
Centers for Disease Control and Prevention. Respiratory virus guidance .
Centers for Disease Control and Prevention. COVID-19 Treatments and Medications .
By Angela Ryan Lee, MD Dr. Lee is an Ohio-based board-certified physician specializing in cardiovascular diseases and internal medicine.
Disclaimer: This translation was last updated on August 2, 2022. For up-to-date content, please visit the English version of this page.
Disclaimer: The Spanish COVID-19 site is currently undergoing significant updates which may lead to a delay in translated content. We apologize for any inconvenience.
What to Do if You Have Been Around Someone With COVID-19
Stay away from people who have covid-19.
Stay away from people who are sick with COVID-19. People can spread COVID-19 when they talk. People can spread COVID-19 when they cough. People can spread COVID-19 when they sneeze.
Some people with COVID-19 feel fine. People can spread COVID-19 even if they feel fine. Stay away from people with COVID-19 even if they feel fine.
What to Do If You Were Around Someone Who Has COVID-19
Get tested if you were around someone with COVID-19. Take a COVID-19 test at least 5 days after you were around that person. Take a COVID-19 test even if you feel fine.
Watch for symptoms if you were around someone with COVID-19. Watch for COVID-19 symptoms for 10 days.
Be cautious if you were around someone with COVID-19. Wear a mask for 10 days around others in your home. Wear a mask for 10 days around others in public. Be extra careful around people who are likely to get very sick from COVID-19.
What to Do If Someone With COVID-19 Visited Your Home Recently
Let in air from outside to clear the air in your home. Open doors to let in air from outside. Open windows to let in air from outside. Use fans to clear the air in your home. Use a portable air cleaner to help filter the air in your home. The best portable air cleaners are called “HEPA” cleaners.
To receive email updates about COVID-19, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Virgin Voyages Help & Support for Health and Safety
- Help & Support
- / Before You Sail
- / Health and Safety
Health and Safety
- Any Sailor who has signs of COVID will receive complimentary medical care on board via our onboard Medical Team — our medical center is equipped with the latest PCR testing capabilities to test for COVID-19 and other viral diseases.
- In case of a positive PCR test, those Sailors will be isolated under Virgin Voyages Infection Prevention & Control protocols.
- The medical team will follow up with any close contact.
- Our highly trained medical team will treat impacted Sailors with the best care until we arrive back and are in port, and the impacted Sailors can be transferred to local medical facility or has indicated by Port Regulations
- If negative, we will test for other viral infections as well, for example, influenza A & B, etc., and if any of those tests are confirmed, treatment is administered accordingly.
- Isolation may not be required for the above cases, but our medical doctors on board will determine on a case by case basis.
Other topics related to "Health and Safety"
- Accessibility
- Travel Requirements
- Voyage Protection
Need help getting the As to your Qs?
Hit the big, red button below and reach out to our sailor services crew..
Free COVID Home Test Kits Are Still Available: Here's How to Get Them
If you think you might have COVID, don't panic: You have plenty of options for free testing and treatments.

The last federal shipment of free COVID tests ended in March, but you can still get free tests.
Even if you're vaccinated against COVID-19, you could still be one of the hundreds of millions of people who continue to get infected by the virus. If you have any COVID symptoms, you should get tested as soon as possible. Luckily, there are plenty of free COVID tests and treatments still available.
Recently, the Federal Government halted the US Postal Service's free COVID program, which would allow you to order free COVID-19 tests through the USPS. The end of the free COVID-19 testing program comes on the heels of the Centers for Disease Control and Prevention shifting its official COVID isolation guidelines. Instead of the typical five-day isolation period, the CDC now recommends that you be fever-free and have improving symptoms for 24 hours before returning to normal activities.
Read more: Are Your COVID Tests Really Expired? How to Find Out
However, hope is not lost when it comes to finding free tests. Read on to find out the ways you can still get free COVID testing, as well as how to get your hands on free treatments and COVID vaccines .
For more, here's what to know about long COVID , and how to tell if it's COVID, allergies or something else .
What are my free COVID-19 testing options?
Now that you can no longer receive tests from the Postal Service, you have three main avenues to find free COVID-19 testing locations across the US: HRSA health centers, Test to Treat locations and ICATT testing sites. These options function similarly, but we'll break down the specific steps to find your nearest free testing location.
HRSA health centers offer free COVID-19 testing
HRSA health centers offer free COVID-19 testing.
The Health Resources and Services Administration funds health centers across the US. At these HRSA health centers, you will be able to receive free COVID-19 testing. You can use HRSA's locator tool to find a center near you.
First, select the language you would like to receive your results in. Then simply enter the location you wish to search into the box labeled Location . The locator also allows you to widen your search radius, so you can see all the options your area has to offer.
Once you've found a center that works for you, click through to that particular location's website and follow their specific instructions for obtaining a free COVID-19 test.
Test to Treat locations have COVID testing and medicine
The Test to Treat program makes COVID testing and therapeutics more accessible.
Test to Treat is a federally funded health care initiative that provides more accessible COVID-19 care. This option differs from the others in this article as you can use the Test to Treat centers to receive both COVID testing and treatment for infections. Like the other COVID-19 free testing options, Test to Treat has a locator tool that you can use to find an eligible Test to Treat center near you.
The Test to Treat center locator works like the other COVID testing search tools. Enter your location into the search bar and the tool will display Test to Treat locations in your area. A sliding bar lets you resize the search radius to capture all of the Test to Treat centers within your area.
Within the Test to Treat locator results, you'll be able to see each location's address, which COVID-19 therapeutics they offer and other special instructions you might need to know to get tested. If there's not an option to schedule a COVID test online through your chosen site, you may need to call.
Increasing Community Access to Testing provides COVID testing for the uninsured
ICATT offers free testing to uninsured patients who are showing symptoms of COVID-19 or who have recently been exposed.
Increasing Community Access to Testing , or ICATT, is another free testing program that you can use if you need access to free COVID-19 testing. ICATT works a bit differently than the other programs on this list.
ICATT is specifically designed for uninsured patients who have been exposed to COVID-19 or are experiencing symptoms of COVID-19. Anyone can get an ICATT test at one of the program's locations, regardless of insurance status. If you are uninsured and you wish to be tested at an ICATT-eligible site, you will not need to pay for your test. If you are insured, you might need to pay a fee.
The ICATT locator tool works just like the other locator tools for free COVID testing -- input your address or your ZIP code to find ICATT locations near you. There is a search radius adjuster in this locator to tweak your searches to capture the entire area that you want to search.
Once you've found a location, follow your testing site's steps for scheduling your appointment.
How can I get free COVID-19 vaccines and booster shots?
COVID-19 vaccines and boosters are an important protection against contracting or getting seriously ill from the virus. Since the CDC has recommended updated COVID-19 booster shots for everyone 6 months or older, you might be wondering how to find free COVID-19 vaccines.
If you don't have insurance or a health provider, don't worry. The Department of Health and Human Services website says, "COVID-19 vaccines are 100% free for every individual living in the United States."
On Sept. 14, the Department of Health and Human Services launched the Bridge Access Program , which will continue to provide free vaccines to those who are uninsured through local health departments and HRSA centers. CDC has also partnered with "more than 20,000 retail pharmacy locations nationwide" to provide free vaccines by modifying the existing ICATT program mentioned above.
The Bridge Access Program will end in December 2024, but until then, you'll be able to access free COVID-19 vaccines. To use it, go to vaccines.gov , choose which shot you want, and then click the "search" button. On the next page, select the option that says "Bridge Access Program Participant" to show which locations offer no-cost vaccines.
For more, learn how your blood type could make you more susceptible to COVID and everything to know about the updated COVID-19 boosters .
Correction, Sept. 21, 2023 : An earlier version of this story contained incorrect information about the cost of vaccines for people without insurance. It has been updated with information about how people can get free vaccines.
Other Wellness Guides
- Best Places to Buy Glasses Online
- Best Places to Buy Contacts Online
- Best Prescription Sunglasses
- Best Place to Buy Replacement Prescription Lenses
- Best Blue Light Blocking Glasses
- Best Electric Toothbrush
- Best Invisible Braces
- Best Sunscreen
- Best Mattress
- Best Mattress for Back Pain
- Best Adjustable Mattress
- Purple Mattress
- Saatva Mattress
- Best Headphones for Sleeping
- Best Pillow
- Best Sheets
- Best Elliptical
- Best Treadmill
- Best Rowing Machine
- Best Peloton Alternative
- Best Adjustable Dumbbells
- Best Weightlifting Shoes
- Best Massage Gun
- Theragun Review
- Best Meal Kit Delivery Service
- Best Healthy Meal Delivery Service
- Best Cheap Meal Delivery Service
- Best Plant-Based Meal Delivery Service
- Best Keto Meal Delivery
- Best DNA Test
- Ancestry vs 23 and Me
- Best Continuous Glucose Monitors
- Best Blood Pressure Monitor
- Best Prescription Delivery Services
- Best Portable Humidifiers
- Best Mental Health Apps
- Best Teas for Stress and Anxiety
- Best Fidget Toys for Anxiety
- Best Online Therapy
- Amazon Promo Codes
- Air Up Coupons
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
USDA Actions to Protect Livestock Health From Highly Pathogenic H5N1 Avian Influenza
Federal Order to assist with developing a baseline of critical information and limiting the spread of H5N1 in dairy cattle
WASHINGTON, April 24, 2024 – To further protect the U.S. livestock industry from the threat posed by highly pathogenic H5N1 avian influenza, USDA is sharing a number of actions that we are taking with our federal partners to help us get ahead of this disease and limit its spread.
Today, USDA’s Animal and Plant Health Inspection Service (APHIS) announced a Federal Order requiring the following measures, effective Monday, April 29, 2024:
Mandatory Testing for Interstate Movement of Dairy Cattle
- Prior to interstate movement, dairy cattle are required to receive a negative test for Influenza A virus at an approved National Animal Health Laboratory Network (NAHLN) laboratory.
- Owners of herds in which dairy cattle test positive for interstate movement will be required to provide epidemiological information, including animal movement tracing.
- Dairy cattle moving interstate must adhere to conditions specified by APHIS.
- As will be described in forthcoming guidance, these steps will be immediately required for lactating dairy cattle, while these requirements for other classes of dairy cattle will be based on scientific factors concerning the virus and its evolving risk profile.
Mandatory Reporting
- Laboratories and state veterinarians must report positive Influenza A nucleic acid detection diagnostic results (e.g. PCR or genetic sequencing) in livestock to USDA APHIS.
- Laboratories and state veterinarians must report positive Influenza A serology diagnostic results in livestock to USDA APHIS.
USDA has identified spread between cows within the same herd, spread from cows to poultry, spread between dairies associated with cattle movements, and cows without clinical signs that have tested positive. On April 16, APHIS microbiologists identified a shift in an H5N1 sample from a cow in Kansas that could indicate that the virus has an adaptation to mammals. Centers for Disease Control and Prevention (CDC) conducted further analysis of the specimen sequence, which did not change their overall risk assessment for the general public, because the substitution has been seen previously in other mammalian infections and does not impact viral transmission. Additionally, APHIS’ National Veterinary Services Laboratories found H5N1 in a lung tissue sample from an asymptomatic cull dairy cow that originated from an affected herd and did not enter the food supply.
The novel movement of H5N1 between wild birds and dairy cows requires further testing and time to develop a critical understanding to support any future courses of action. This Federal Order is critical to increasing the information available for USDA. Requiring positive test reporting will help USDA better under this disease and testing before interstate movement will limit its spread.
While we are taking this action today, it is important to remember that thus far, we have not found changes to the virus that would make it more transmissible to humans and between people. While cases among humans in direct contact with infected animals are possible, our partners at the U.S. Centers for Disease Control and Prevention (CDC) believe that the current risk to the public remains low.
Additionally, we continue to see affected cows recover after supported care with little to no associated mortality. We also continue to work with our partners in the states and industry to emphasize the critical importance biosecurity plays in limiting disease spread for all livestock and poultry.
You may view the Federal Order , which is effective on Monday, April 29, 2024.
Further, in an effort to maximize understanding and research on H5N1 in dairy cattle, on April 21, APHIS made publicly available 239 genetic sequences from the U.S. H5N1 clade 2.3.4.4b influenza virus recently found in samples associated with the ongoing HPAI outbreak in poultry and wild birds, and the recent H5N1 event in dairy cattle. APHIS has also offered virus samples to interested researchers to facilitate epidemiological study. Increasing our understanding of this disease and how it spreads is critical to stopping it. This is why APHIS is urging dairy cattle producers and those who work in or with the industry to share epidemiological information from affected farms, even if they are not planning to move cattle interstate. APHIS further urges producer participation in public health assessments to continue to confirm worker safety and monitor for any potential changes in the virus that could impact transmissibility.
In addition, our partners in the U.S. Food and Drug Administration released an update on the ongoing work to ensure continued effectiveness of the federal-state milk safety system. It is important to emphasize that, based on the information and research available to us at this time, the U.S. Food and Drug Administration and USDA believe that our commercial milk supply is safe because of both the pasteurization process and the required diversion or destruction of milk from sick cows. Pasteurization has continuously proven to inactivate bacteria and viruses in milk. The FDA and USDA continue to work closely to collect and evaluate additional data and information specific to avian influenza in dairy cattle and to support state counterparts as this emerging disease in dairy cattle is managed.
As USDA continues to take steps to protect the health of livestock, the Department continues to work closely with federal partners at the CDC on protecting the health of people and FDA on protecting the safety of the food supply. The U.S. government is committed to addressing this situation with urgency.
To learn more about USDA’s response to HPAI in dairy cattle, visit www.aphis.usda.gov/livestock-poultry-disease/avian/avian-influenza/hpai-detections/livestock .
USDA is an equal opportunity provider, employer, and lender.

IMAGES
COMMENTS
Consider getting a COVID-19 test if you: Develop COVID-19 symptoms before, during, or after travel. Will be traveling to visit someone who is at higher risk of getting very sick from COVID-19. Were in a situation with a greater risk of exposure during travel (e.g., in an indoor, crowded space like an airport terminal while not wearing a mask).
March 1, 2024, 10:01 AM PST. By Erika Edwards. People who test positive for Covid no longer need to isolate for five days, the Centers for Disease Control and Prevention said Friday. The CDC's ...
Isolation. If you test positive for COVID-19, stay home for at least 5 days and isolate from others in your home. You are likely most infectious during these first 5 days. Wear a high-quality mask if you must be around others at home and in public. Do not go places where you are unable to wear a mask. For travel guidance, see CDC's Travel ...
Before this, the CDC recommended that people who test positive for COVID should isolate away from others for five days and wear a well-fitting mask around others for the following five days. This was different from the general guidance for other common respiratory viruses, like flu and RSV.
Wear a mask around other people when you have COVID-19. Wear a mask for 10 days after you start feeling sick. Wear a mask for 10 days after you test positive. Wear a mask with extra protection. The mask must cover your nose and mouth. The mask must fit under your chin. The mask must be snug on your face.
People with a positive test result should follow CDC's COVID-19 isolation guidance. Testing people who have recently tested positive, and recovered from COVID-19 If someone has had exposure to someone with COVID-19 and is asymptomatic, but has had COVID-19 within the past 30 days*, testing to identify a new infection is generally not recommended.
Testing before and after travel can lower the risk of spreading the virus that causes COVID-19. If you haven't been vaccinated, the CDC recommends getting a viral test within three days before your trip. Delay travel if you're waiting for test results. Keep a copy of your results with you when you travel.
The CDC says not to travel if you have symptoms of COVID-19 or have tested positive and not yet completed an isolation period. Without a testing requirement in place, though, that guideline ...
The CDC continues to advise avoiding travel if you are sick with or have tested positive for COVID, and isolating for at least five days after your positive test if you're either asymptomatic or ...
This proof can include your positive COVID-19 viral test result, but it has to be taken no more than 90 days before your flight's departure from a foreign country. Additionally, you will also need a signed letter from a licensed healthcare professional stating that you're cleared to travel back to the U.S. According to the CDC, the letter from ...
A: People with COVID-19 could potentially transmit it to others well beyond a day after developing symptoms or testing positive. New guidance from the CDC advises people to isolate until they have ...
What to Know About the C.D.C. Guidelines on Vaccinated Travel. In updated recommendations, the federal health agency said both domestic and international travel was low risk for fully vaccinated ...
Starting on December 6, all air passengers traveling to the United States must show a negative COVID-19 test from within one day of departure before boarding their flight. The Centers for Disease Control and Prevention (CDC) shortened the testing window from three days to one. All travelers two years or older are required to show a negative ...
The CDC now recommends people mask up for 10 days and test after five days if they are not fully vaccinated but are exposed to someone who is COVID-19 positive. This is in line with existing ...
If you're traveling without being fully vaccinated, you can take some steps to protect yourself and the people around you: Get a COVID test 1 to 3 days before you leave. Wear a mask on public ...
Diagnostic COVID-19 tests are meant for diagnosing an active COVID-19 infection. They require specimen collection from the nose or saliva. The two types of diagnostic tests are: PCR (polymerase chain reaction) tests, also known as molecular tests. They look for viral DNA and are highly accurate, but take longer and are more expensive.
Open doors to let in air from outside. Open windows to let in air from outside. Use fans to clear the air in your home. Use a portable air cleaner to help filter the air in your home. The best portable air cleaners are called "HEPA" cleaners. Easy to read information about what to do if you have been around someone with COVID-19.
Before the voyage: If you test positive for COVID, or were exposed to COVID within 10 days of departure, Virgin Voyages will allow you to change your voyage date, or provide a full future voyage credit to use toward a booking at a later time. Taxes and fees and bookable amounts are refunded to the original form of payment. At the terminal: While all Sailors no longer require COVID-19 testing ...
Since the CDC has recommended updated COVID-19 booster shots for everyone 6 months or older, you might be wondering how to find free COVID-19 vaccines. If you don't have insurance or a health ...
WASHINGTON, April 24, 2024 - To further protect the U.S. livestock industry from the threat posed by highly pathogenic H5N1 avian influenza, USDA is sharing a number of actions that we are taking with our federal partners to help us get ahead of this disease and limit its spread. Today, USDA's Animal and Plant Health Inspection Service (APHIS) announced a Federal Order requiring the ...