Thanks for visiting! GoodRx is not available outside of the United States. If you are trying to access this site from the United States and believe you have received this message in error, please reach out to [email protected] and let us know.
Home > Blog > The IVF journey and what to expect

The IVF journey and what to expect
IVF is often referred to as a journey. It’s not just a single procedure, but a process, involving multiple hospital visits, a variety of medication, physical and emotional challenges and a lot of waiting.
It’s therefore important to be mentally and physically prepared before you begin your IVF cycle, as feeling informed about what you can expect is a great way to start.
Is IVF the right treatment for me?
Your GP may have referred you to a fertility specialist, if you have been trying unsuccessfully to conceive or there are reasons why conceiving naturally is not an option for you.
You may have tried IUI already, without success, or you may have damaged or blocked fallopian tubes, making IVF your best option.
Your specialist will conduct a variety of tests and assessments of you (and your partner if heterosexual) which may include blood tests, an ultrasound to assess your ovaries and a semen analysis. They will also ask about your family history and any known genetic problems or fertility issues.

What can I do before I start my IVF cycle?
Counselling may be recommended before you start. You should also consider your lifestyle, as having a healthy diet and a healthy lifestyle in general, can have a positive impact on your fertility and the future health of your child. We have blog posts on our site which provide useful information about fertility diets and guidelines on what to do and what not to do for your best chance of conceiving.
You will also need to make sure that you are available to attend all appointments, often at relatively short notice. As IVF treatment depends very much on how and when your body reacts to the drugs, the timetable is individual to you and flexibility is important.
When will my treatment start?
Your IVF cycle will start on the first day of your period.
How does the IVF process start?
Usually, the process starts with fertility drugs to stimulate your ovaries to release more eggs. The medication will be administered by self-injection at home. Your fertility specialist will show you how to do the injections.
You will be asked to have scans and possibly blood tests during the stimulation stage, to observe how the follicles are responding to the medication.
When your follicles are ready, you will have an injection to mature the eggs, so they will be ready for collection.
What happens during egg collection?
Egg collection takes place 36-40 hours after the trigger injection. You will be given a light sedative to make you sleepy during the egg removal procedure, which will take around half an hour.
Eggs are collected using a fine needle, which is passed through the vaginal wall, with the help of a scanning probe.
Due to the sedation, you will need to rest after the procedure and have someone with you. Your clinic will advise you on any other possible precautions, which include not driving and not operating machinery for 24 hours.
What happens with sperm collection?
If you are using a sperm donor, the sample will have been produced much earlier and frozen, to allow time to assess for any genetic abnormalities or infections.
If you are using your partner’s sperm, a sample will need to be produced at the clinic on the same day as egg collection and a private room will be provided to do this.
After egg collection, you may be advised to take medication, to help to prepare the lining of your uterus ready for potential embryo transfer, if viable embryos are produced.
What happens in the insemination process?
The best sperm are selected and added to the eggs in a special dish. If you are having ICSI, the sperm will be injected into each egg. The dishes are then put into an incubator to enable fertilisation.
What happens next?
In the laboratory, experts will check to see if fertilisation has taken place and how any embryos are developing.
Your fertility clinic will keep you informed on the development of any embryos.
What happens during embryo transfer?
If any of the embryos are viable, five days after egg collection, you will need to go to the clinic for embryo transfer.
A catheter will be used to transfer either one or two embryos into your uterus. Only one or two embryos are transferred, to reduce the risk of multiple births. You may choose to have any other viable embryos stored to use in a later IVF cycle.
When will I know if the IVF has worked?
Your clinic will invite you in for a pregnancy test, at least 7 days after embryo transfer. It is advisable to wait for the clinic to do a test, rather than being tempted to do a test at home, as due to the medication and the timing, you may otherwise get either a false positive, or a false negative.
Pregnancy test results
The clinic will tell you whether or not the treatment has resulted in pregnancy.
If the test is positive, you will be told when to attend the clinic for a scan and given any further advice that you need for your pregnancy.
If you have a negative test, your clinic will be able to support you and talk about what your next steps may be.
Here at the IVF network, we know how challenging the IVF process can be, so we provide information and advice through our dedicated channel, blog posts and website, to help you to make informed choices throughout your fertility journey.
&w=384&q=75)
0808 1961942
A typical IVF journey
&w=1920&q=75)
A typical IVF journey, whether it is for the first time or trying again, can also be called a ‘stimulated cycle’. This is because your treatment will involve taking drugs that stimulate your body so we can collect a number of eggs for fertilisation.
If you’re not sure which options are best for you, you can attend one of our FREE information events or contact your local clinic to understand your options.
1. Referrals
Your referral may come from your GP or hospital doctor, or you can self-refer. Learn more about the referrals process .
2. Pre-treatment
Preliminary fertility assessment tests and screening
To make the best decision about your treatment in the consultation, your doctor needs the results of some tests. There may be a combination of blood tests and a vaginal ultrasound scan to assess your ovaries, and a semen assessment where appropriate. Learn more about TFP fertility assessment packages .
Initial consultation
At your first consultation with a TFP fertility specialist, they will cover your medical history and explain your test results. You and your doctor will then discuss their recommended programme of treatment based on your personal results and circumstances.
3. Counselling
Counselling is available at any stage of your treatment pathway. Fertility treatment is a significant emotional journey for all patients, and counselling provides extra emotional support.
It is completely confidential. If you are going to be using donated eggs or sperm for your treatment, then you’ll be recommended to see the counsellor before starting treatment to discuss the implications for both you and any children that may be born. Learn more about fertility counselling .
4.Treatment planning appointment
At your treatment planning appointment one of our specialist fertility nurses will explain your treatment in full. You will be taken through your regime of drugs and shown how to use them.
You will have the opportunity to ask questions regarding your forthcoming treatment. It’s also the time when you officially consent to undergo fertility treatment , and we go over the legal side of things.
This is an important part of the process which ensures that your parenthood will be recognised legally after treatment. We require that everyone involved in the treatment comes to the treatment planning appointment. It generally takes 60 minutes. We use an online consent platform where you will be able to watch videos prior to electronically signing your consent. If you are funding your own treatment, you will need to pay for your treatment programme at this point. Once all the tests, consent forms and payment are completed, you are ready to start your IVF cycle. Learn more about the treatment planning appointment .
5. Starting treatment
Your treatment will start on the first day of your period. You will need to call the clinic to let us know and to receive the instruction to start the treatment plan, as explained by your fertility specialist in your consultation and nurse in your planning appointment. As you’re not undergoing ovarian stimulation, you may or may not have drugs to take in this cycle; this will be agreed upon with your doctor at your consultation. If you have a regular menstrual cycle, we will monitor you so that we can transfer the embryo(s) at the best point in your ‘natural cycle’.
6. Ovarian stimulation and monitoring
In general, treatment starts with drugs that stimulate your ovaries. This enables us to collect a number of eggs for insemination, rather than the usual single egg. The drugs are injections that can be taken at home – you’ll be shown how to do this.
Over a period of around two weeks of stimulation, you’re likely to have one to three scans and possibly blood tests, to monitor the development of the egg-producing follicles.
These are short appointments that last around 20 minutes, and the results are available later the same day. The timings are different for everyone, because treatment is tailored to suit each patient individually.
7. Trigger injection
Once your follicles are ready, the stimulation period ends with an injection that matures the eggs in the follicles to get them ready for egg collection.
8. Egg collection
The appointment to collect the eggs will take place 36-40 hours after the trigger injection. The procedure takes about half an hour, and you will be given drugs to make you sleepy during the procedure.
With the help of a scanning probe, a very fine needle is passed through the vaginal wall and into the ovary to collect the eggs. Usually, around 80% of follicles contain an egg. As you will have had sedation you cannot drive or operate machinery for 24 hours and you will need someone to stay with you.
9. Providing sperm
If your treatment uses a fresh sperm sample, it will be provided on the same day as the eggs. You provide the sample at the clinic, in one of our andrology (men’s) rooms. If you’re providing the sample via a surgical procedure, this will take place before the egg collection day, and the sample will be be frozen.
If you already have sperm in storage, or have been matched to a sperm donor, the sample will be thawed on the same day that the eggs are collected.
10. Insemination of the eggs
The sperm sample provided is prepared to ensure that the very best sperm are being used for insemination.
IVF – Prepared sperm will be added to the eggs in a culture dish.
ICSI – A single sperm will be selected and injected into each egg then put into a culture dish.
The culture dishes are placed in the incubator to allow fertilisation to take place.
11. Embryo development
The embryos are carefully monitored in the period after insemination, first to check for fertilisation, then for signs for development which indicate the embryo is growing. Time-lapse monitoring allows us to carefully monitor embryo development. Click here to learn more about time-lapse monitoring . The clinic will be able to update you on embryo development.
Shortly after egg collection, you may also start taking drugs to help prepare your uterus lining to receive an embryo (this is known as Luteal Phase Support).
If your treatment plan includes genetic testing, then this will happen during this phase.
12. Embryo transfer
The frozen embryo transfer takes place 5 days after egg collection. The embryos are monitored carefully in the Embryoscope by our Embryologists. The procedure can feel like a smear test, but it takes longer: around 15 minutes. A tiny drop of culture medium containing one or two embryos is carefully deposited in the uterus using a thin catheter.
If you decided before treatment to store any further good quality embryos for further cycles, you’ll be consulted again, and it will happen at this stage.
13. The wait
At TFP fertility clinic we appreciate how difficult this two-week wait can be. Please call us at any time if you are concerned; no worry is too small. It’s a good idea to make plans for after embryo transfer to help you feel more in control. Try to live life as normally as possible.
14. The outcome
Positive test.
If you’re pregnant, we schedule a scan in the clinic at around six to eight weeks. If everything looks good, then you’re discharged to your GP.
Negative test
If your period arrives before the test is due or if the test is negative, rest assured you are not alone.
We can meet to talk, review your treatment, and consider what the next step will be on your IVF journey. IVF conception often takes place over a number of cycles. You could be ready for a new cycle within a short time, even a couple of months if you have frozen embryos, but this is completely up to you.
Watch these 2 videos about:
What happens when a patient first starts their fertility journey with TFP?
What are the most challenging parts of the IVF journey for patients?
This service is offered in the following clinics:
&w=384&q=75)
TFP Belfast Fertility
BT3 9JQ Belfast
028 9009 7315
&w=384&q=75)
TFP 92 Harley Street
W1G 7HU London
0207 160 6379
&w=384&q=75)
TFP Boston Place Fertility
NW1 6ER London
0203 131 2152
&w=384&q=75)
TFP Wessex Fertility
SO15 5QS Southampton
0203 1318630
&w=384&q=75)
TFP Thames Valley Fertility
SL6 4BY Maidenhead
01628 702632
&w=384&q=75)
TFP Simply Fertility
CM2 8HN Chelmsford
01245 371849
&w=384&q=75)
TFP Oxford Fertility
OX4 2HW Oxford
01865 224819
&w=384&q=75)
TFP Nurture Fertility
NG10 5QG Nottingham
+44 0115 828 0246
&w=384&q=75)
TFP GCRM Fertility
G51 4FD Glasgow
0141 413 0715
&w=3840&q=75)
Ready to start your fertility journey? We're here for you
Schedule an appointment to start your fertility journey with us.
- Patient Care & Health Information
- Tests & Procedures
- In vitro fertilization (IVF)
- In vitro fertilization
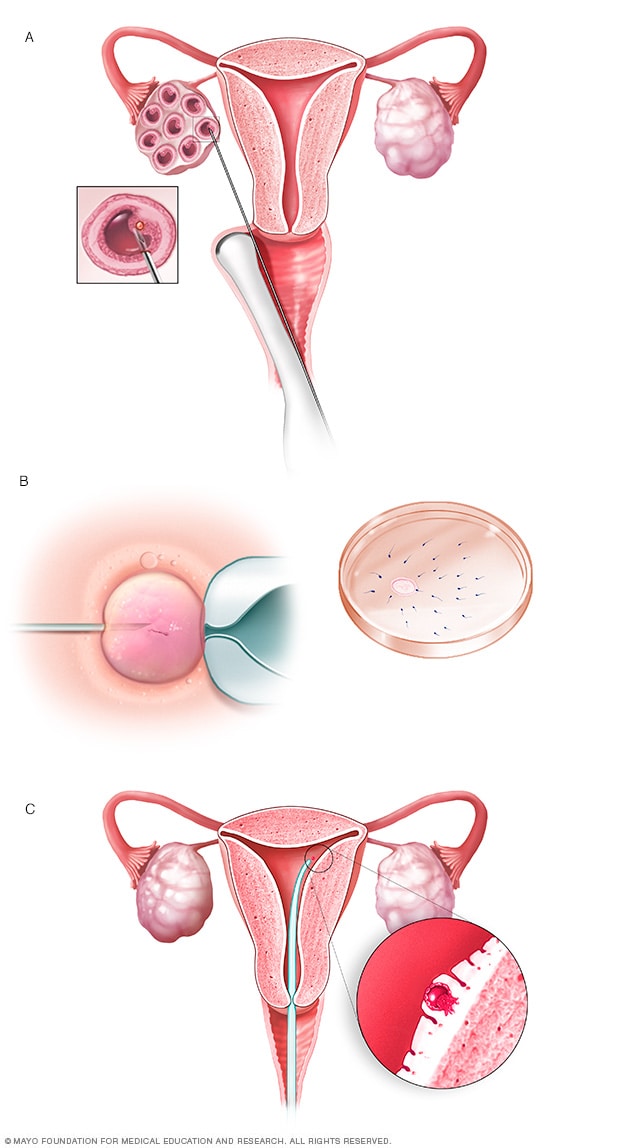
During in vitro fertilization, eggs are removed from sacs called follicles within an ovary (A). An egg is fertilized by injecting a single sperm into the egg or mixing the egg with sperm in a petri dish (B). The fertilized egg, called an embryo, is transferred into the uterus (C).
In vitro fertilization, also called IVF, is a complex series of procedures that can lead to a pregnancy. It's a treatment for infertility, a condition in which you can't get pregnant after at least a year of trying for most couples. IVF also can be used to prevent passing on genetic problems to a child.
During in vitro fertilization, mature eggs are collected from ovaries and fertilized by sperm in a lab. Then a procedure is done to place one or more of the fertilized eggs, called embryos, in a uterus, which is where babies develop. One full cycle of IVF takes about 2 to 3 weeks. Sometimes these steps are split into different parts and the process can take longer.
In vitro fertilization is the most effective type of fertility treatment that involves the handling of eggs or embryos and sperm. Together, this group of treatments is called assisted reproductive technology.
IVF can be done using a couple's own eggs and sperm. Or it may involve eggs, sperm or embryos from a known or unknown donor. In some cases, a gestational carrier — someone who has an embryo implanted in the uterus — might be used.
Your chances of having a healthy baby using IVF depend on many factors, such as your age and the cause of infertility. What's more, IVF involves getting procedures that can be time-consuming, expensive and invasive. If more than one embryo is placed in the uterus, it can result in a pregnancy with more than one baby. This is called a multiple pregnancy.
Your health care team can help you understand how IVF works, what the risks are and whether it's right for you.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- A Book: Mayo Clinic Guide to Fertility and Conception
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
In vitro fertilization is a treatment for infertility or genetic problems. Before you have IVF to treat infertility, you and your partner might be able to try other treatment options that involve fewer or no procedures that enter the body. For example, fertility drugs can help the ovaries make more eggs. And a procedure called intrauterine insemination places sperm directly in the uterus near the time when an ovary releases an egg, called ovulation.
Sometimes, IVF is offered as a main treatment for infertility in people over the age of 40. It also can be done if you have certain health conditions. For example, IVF may be an option if you or your partner has:
- Fallopian tube damage or blockage. Eggs move from the ovaries to the uterus through the fallopian tubes. If both tubes get damaged or blocked, that makes it hard for an egg to be fertilized or for an embryo to travel to the uterus.
- Ovulation disorders. If ovulation doesn't happen or doesn't occur often, fewer eggs are available to be fertilized by sperm.
- Endometriosis. This condition happens when tissue that's like the lining of the uterus grows outside of the uterus. Endometriosis often affects the ovaries, uterus and fallopian tubes.
- Uterine fibroids. Fibroids are tumors in the uterus. Most often, they're not cancer. They're common in people in their 30s and 40s. Fibroids can cause a fertilized egg to have trouble attaching to the lining of the uterus.
- Previous surgery to prevent pregnancy. An operation called tubal ligation involves having the fallopian tubes cut or blocked to prevent pregnancy for good. If you wish to conceive after tubal ligation, IVF may help. It might be an option if you don't want or can't get surgery to reverse tubal ligation.
- Issues with sperm. A low number of sperm or unusual changes in their movement, size or shape can make it hard for sperm to fertilize an egg. If medical tests find issues with sperm, a visit to an infertility specialist might be needed to see if there are treatable problems or other health concerns.
- Unexplained infertility. This is when tests can't find the reason for someone's infertility.
- A genetic disorder. If you or your partner is at risk of passing on a genetic disorder to your child, your health care team might recommend getting a procedure that involves IVF . It's called preimplantation genetic testing. After the eggs are harvested and fertilized, they're checked for certain genetic problems. Still, not all of these disorders can be found. Embryos that don't appear to contain a genetic problem can be placed in the uterus.
A desire to preserve fertility due to cancer or other health conditions. Cancer treatments such as radiation or chemotherapy can harm fertility. If you're about to start treatment for cancer, IVF could be a way to still have a baby in the future. Eggs can be harvested from their ovaries and frozen for later use. Or the eggs can be fertilized and frozen as embryos for future use.
People who don't have a working uterus or for whom pregnancy poses a serious health risk might choose IVF using another person to carry the pregnancy. The person is called a gestational carrier. In this case, your eggs are fertilized with sperm, but the embryos that result are placed in the gestational carrier's uterus.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
IVF raises the chances of certain health problems. From short term to longer term, these risks include:
- Stress. IVF can be draining for the body, mind and finances. Support from counselors, family and friends can help you and your partner through the ups and downs of infertility treatment.
- Complications from the procedure to retrieve eggs. After you take medicines to spur the growth of sacs in the ovaries that each contain an egg, a procedure is done to collect the eggs. This is called egg retrieval. Ultrasound images are used to guide a long, thin needle through the vagina and into the sacs, also called follicles, to harvest the eggs. The needle could cause bleeding, infection or damage to the bowel, bladder or a blood vessel. Risks are also linked with medicines that can help you sleep and prevent pain during the procedure, called anesthesia.
Ovarian hyperstimulation syndrome. This is a condition in which the ovaries become swollen and painful. It can be caused by receiving shots of fertility medicines, such as human chorionic gonadotropin (HCG), to trigger ovulation.
Symptoms often last up to a week. They include mild belly pain, bloating, upset stomach, vomiting and diarrhea. If you become pregnant, your symptoms might last a few weeks. Rarely, some people get a worse form of ovarian hyperstimulation syndrome that also can cause rapid weight gain and shortness of breath.
- Miscarriage. The rate of miscarriage for people who conceive using IVF with fresh embryos is similar to that of people who conceive naturally — about 15% for pregnant people in their 20s to over 50% for those in their 40s. The rate rises with the pregnant person's age.
- Ectopic pregnancy. This is a condition in which a fertilized egg attaches to tissue outside the uterus, often in a fallopian tube. The embryo can't survive outside the uterus, and there's no way to continue the pregnancy. A small percentage of people who use IVF will have an ectopic pregnancy.
- Multiple pregnancy. IVF raises the risk of having more than one baby. Becoming pregnant with multiple babies carries higher risks of pregnancy-related high blood pressure and diabetes, early labor and delivery, low birth weight, and birth defects than does pregnancy with a single baby.
- Birth defects. The age of the mother is the main risk factor for birth defects, no matter how the child is conceived. But assisted reproductive technologies such as IVF are linked with a slightly higher risk of a baby being born with heart issues, digestive problems or other conditions. More research is needed to find out if it's IVF that causes this raised risk or something else.
- Premature delivery and low birth weight. Research suggests that IVF slightly raises the risk that the baby will be born early or with a low birth weight.
- Cancer. Some early studies suggested that certain medicines used to stimulate egg growth might be linked with getting a specific type of ovarian tumor. But more-recent studies do not support these findings. There doesn't seem to be a significantly higher risk of breast, endometrial, cervical or ovarian cancer after IVF .
How you prepare
To get started, you'll want to find a reputable fertility clinic. If you live in the United States, the Centers for Disease Control and Prevention and the Society for Assisted Reproductive Technology provide information online about clinics' individual pregnancy and live birth rates.
A fertility clinic's success rate depends on many things. These include the ages and medical issues of people they treat, as well as the clinic's treatment approaches. When you talk with a representative at a clinic, also ask for detailed information about the costs of each step of the procedure.
Before you start a cycle of IVF using your own eggs and sperm, you and your partner will likely need various screening tests. These include:
- Ovarian reserve testing. This involves getting blood tests to find out how many eggs are available in the body. This is also called egg supply. The results of the blood tests, often used together with an ultrasound of the ovaries, can help predict how your ovaries will respond to fertility medicines.
- Semen analysis. Semen is the fluid that contains sperm. An analysis of it can check the amount of sperm, their shape and how they move. This testing may be part of an initial fertility evaluation. Or it might be done shortly before the start of an IVF treatment cycle.
- Infectious disease screening. You and your partner will both be screened for diseases such as HIV .
- Practice embryo transfer. This test doesn't place a real embryo in the uterus. It may be done to figure out the depth of your uterus. It also helps determine the technique that's most likely to work well when one or more actual embryos are inserted.
- Uterine exam. The inside lining of the uterus is checked before you start IVF . This might involve getting a test called sonohysterography. Fluid is sent through the cervix into the uterus using a thin plastic tube. The fluid helps make more-detailed ultrasound images of the uterine lining. Or the uterine exam might include a test called hysteroscopy. A thin, flexible, lighted telescope is inserted through the vagina and cervix into the uterus to see inside it.
Before you begin a cycle of IVF , think about some key questions, including:
How many embryos will be transferred? The number of embryos placed in the uterus often is based on age and the number of eggs collected. Since the rate of fertilized eggs attaching to the lining of uterus is lower for older people, usually more embryos are transferred — except for people who use donor eggs from a young person, genetically tested embryos or in certain other cases.
Most health care professionals follow specific guidelines to prevent a multiple pregnancy with triplets or more. In some countries, legislation limits the number of embryos that can be transferred. Make sure you and your care team agree on the number of embryos that will be placed in the uterus before the transfer procedure.
What will you do with any extra embryos? Extra embryos can be frozen and stored for future use for many years. Not all embryos will survive the freezing and thawing process, but most will.
Having frozen embryos can make future cycles of IVF less expensive and less invasive. Or you might be able to donate unused frozen embryos to another couple or a research facility. You also might choose to discard unused embryos. Make sure you feel comfortable making decisions about extra embryos before they are created.
- How will you handle a multiple pregnancy? If more than one embryo is placed in your uterus, IVF can cause you to have a multiple pregnancy. This poses health risks for you and your babies. In some cases, a surgery called fetal reduction can be used to help a person deliver fewer babies with lower health risks. Getting fetal reduction is a major decision with ethical, emotional and mental risks.
- Have you thought through the risks linked with using donor eggs, sperm or embryos, or a gestational carrier? A trained counselor with expertise in donor issues can help you understand the concerns, such as the legal rights of the donor. You also may need an attorney to file court papers to help you become legal parents of an embryo that's developing in the uterus.
What you can expect
After the preparations are completed, one cycle of IVF can take about 2 to 3 weeks. More than one cycle may be needed. The steps in a cycle go as follows:
Treatment to make mature eggs
The start of an IVF cycle begins by using lab-made hormones to help the ovaries to make eggs — rather than the single egg that usually develops each month. Multiple eggs are needed because some eggs won't fertilize or develop correctly after they're combined with sperm.
Certain medicines may be used to:
- Stimulate the ovaries. You might receive shots of hormones that help more than one egg develop at a time. The shot may contain a follicle-stimulating hormone (FSH), a luteinizing hormone (LH) or both.
- Help eggs mature. A hormone called human chorionic gonadotropin (HCG), or other medicines, can help the eggs ripen and get ready to be released from their sacs, called follicles, in the ovaries.
- Delay ovulation. These medicines prevent the body from releasing the developing eggs too soon.
- Prepare the lining of the uterus. You might start to take supplements of the hormone progesterone on the day of the procedure to collect your eggs. Or you might take these supplements around the time an embryo is placed in the uterus. They improve the odds that a fertilized egg attaches to the lining of your uterus.
Your doctor decides which medicines to use and when to use them.
Most often, you'll need 1 to 2 weeks of ovarian stimulation before your eggs are ready to be collected with the egg retrieval procedure. To figure out when the eggs are ready, you may need:
- Vaginal ultrasound, an imaging exam of the ovaries to track the developing follicles. Those are the fluid-filled sacs in the ovaries where eggs mature.
- Blood tests, to check on how you respond to ovarian stimulation medicines. Estrogen levels often rise as follicles develop. Progesterone levels remain low until after ovulation.
Sometimes, IVF cycles need to be canceled before the eggs are collected. Reasons for this include:
- Not enough follicles develop.
- Ovulation happens too soon.
- Too many follicles develop, raising the risk of ovarian hyperstimulation syndrome.
- Other medical issues happen.
If your cycle is canceled, your care team might recommend changing medicines or the amounts you take, called doses. This might lead to a better response during future IVF cycles. Or you may be advised that you need an egg donor.
Egg retrieval
This is the procedure to collect the eggs from one or both ovaries. It takes place in your doctor's office or a clinic. The procedure is done 34 to 36 hours after the final shot of fertility medicine and before ovulation.
- Before egg retrieval, you'll be given medicine to help you relax and keep you from feeling pain.
- An ultrasound device is placed into the vagina to find follicles. Those are the sacs in the ovaries that each contain an egg. Then a thin needle is inserted into an ultrasound guide to go through the vagina and into the follicles to collect the eggs. This process is called transvaginal ultrasound aspiration.
- If your ovaries can't be reached through the vagina this way, an ultrasound of the stomach area may be used to guide the needle through the stomach and into the ovaries.
- The eggs are removed from the follicles through a needle connected to a suction device. Multiple eggs can be removed in about 20 minutes.
- After the procedure, you may have cramping and feelings of fullness or pressure.
- Mature eggs are placed in a liquid that helps them develop. Eggs that appear healthy and mature will be mixed with sperm to attempt to create embryos. But not all eggs are able to be fertilized with success.
Sperm retrieval
If you're using your partner's sperm, a semen sample needs to be collected at your doctor's office or clinic the morning of egg retrieval. Or sperm can be collected ahead of time and frozen.
Most often, the semen sample is collected through masturbation. Other methods can be used if a person can't ejaculate or has no sperm in the semen. For example, a procedure called testicular aspiration uses a needle or surgery to collect sperm directly from the testicle. Sperm from a donor also can be used. Sperm are separated from the semen fluid in the lab.
Fertilization
Two common methods can be used to try to fertilize eggs with sperm:
- Conventional insemination. Healthy sperm and mature eggs are mixed and kept in a controlled environment called an incubator.
- Intracytoplasmic sperm injection (ICSI). A single healthy sperm is injected right into each mature egg. Often, ICSI is used when semen quality or number is an issue. Or it might be used if fertilization attempts during prior IVF cycles didn't work.
In certain situations, other procedures may be recommended before embryos are placed in the uterus. These include:
Assisted hatching. About 5 to 6 days after fertilization, an embryo "hatches" from the thin layer that surrounds it, called a membrane. This lets the embryo attach to the lining of the uterus.
If you're older and you want to get pregnant, or if you have had past IVF attempts that didn't work, a technique called assisted hatching might be recommended. With this procedure, a hole is made in the embryo's membrane just before the embryo is placed in the uterus. This helps the embryo hatch and attach to the lining of the uterus. Assisted hatching is also useful for eggs or embryos that were frozen, as that process can harden the membrane.
Preimplantation genetic testing. Embryos are allowed to develop in the incubator until they reach a stage where a small sample can be removed. The sample is tested for certain genetic diseases or the correct number of threadlike structures of DNA, called chromosomes. There are usually 46 chromosomes in each cell. Embryos that don't contain affected genes or chromosomes can be transferred to the uterus.
Preimplantation genetic testing can lower the chances that a parent will pass on a genetic problem. It can't get rid of the risk completely. Prenatal testing may still be recommended during pregnancy.
Embryo transfer
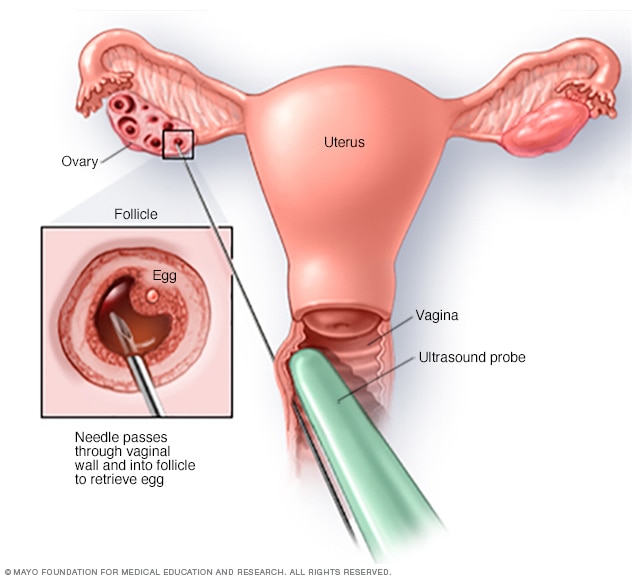
Egg-retrieval technique
Typically, transvaginal ultrasound aspiration is used to retrieve eggs. During this procedure, an ultrasound probe is inserted into the vagina to identify follicles. A needle is guided through the vagina and into the follicles. The eggs are removed from the follicles through the needle, which is connected to a suction device.
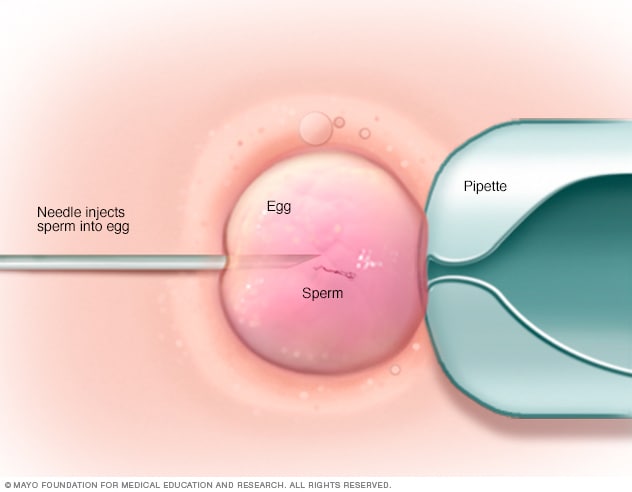
In intracytoplasmic sperm injection (ICSI), a single healthy sperm is injected directly into each mature egg. ICSI often is used when semen quality or number is a problem or if fertilization attempts during prior in vitro fertilization cycles failed.
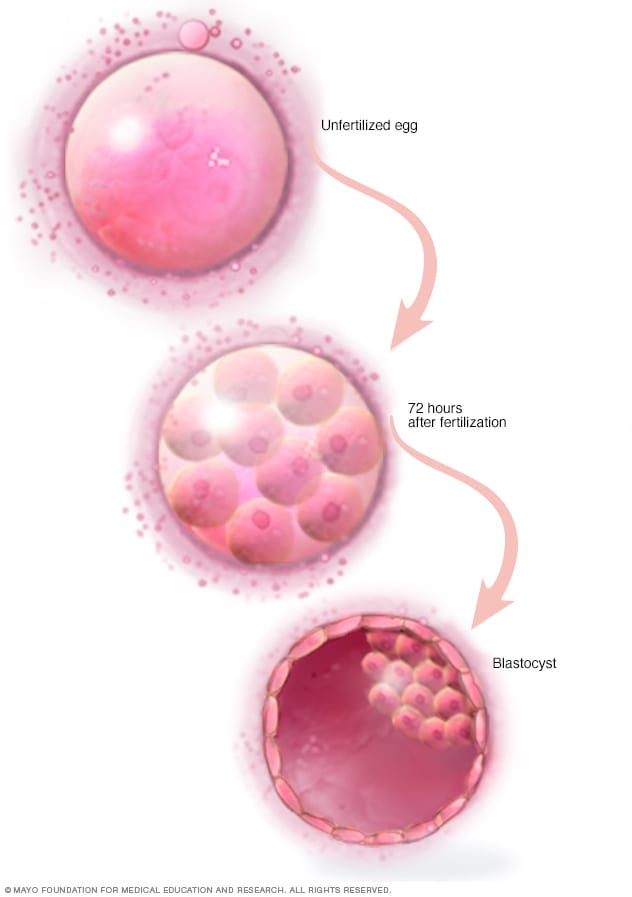
Three days after fertilization, a healthy embryo will contain about 6 to 10 cells. By the fifth or sixth day, the fertilized egg is known as a blastocyst — a rapidly dividing ball of cells. The inner group of cells will become the embryo. The outer group will become the cells that nourish and protect it.
The procedure to place one or more embryos in the uterus is done at your doctor's office or a clinic. It often takes place 2 to 6 days after eggs are collected.
- You might be given a mild sedative to help you relax. The procedure is often painless, but you might have mild cramping.
- A long, thin, flexible tube called a catheter is placed into the vagina, through the cervix and into the uterus.
- A syringe that contains one or more embryos in a small amount of fluid is attached to the end of the catheter.
- Using the syringe, the embryo or embryos are placed into the uterus.
If the procedure works, an embryo will attach to the lining of your uterus about 6 to 10 days after egg retrieval.
After the procedure
After the embryo transfer, you can get back to your usual daily routine. Your ovaries may still be enlarged, so vigorous activities or sex might cause discomfort. Ask your care team how long you should stay away from these.
Typical side effects include:
- Passing a small amount of clear or bloody fluid shortly after the procedure. This is due to the swabbing of the cervix before the embryo transfer.
- Breast tenderness due to high estrogen levels.
- Mild bloating.
- Mild cramping.
- Constipation.
Call your care team if you have moderate or severe pain, or heavy bleeding from the vagina after the embryo transfer. You'll likely to need to get checked for complications such as infection, twisting of an ovary and ovarian hyperstimulation syndrome.
At least 12 days after egg retrieval, you get a blood test to find out whether you're pregnant.
- If you're pregnant, you'll likely be referred to an obstetrician or other pregnancy specialist for prenatal care.
- If you're not pregnant, you'll stop taking progesterone and likely get your period within a week. Call your care team if you don't get your period or if you have unusual bleeding. If you'd like to try another cycle of IVF , your care team might suggest steps you can take to improve your chances of getting pregnant next time.
The chances of giving birth to a healthy baby after using IVF depend on various factors, including:
- Maternal age. The younger you are, the more likely you are to get pregnant and give birth to a healthy baby using your own eggs during IVF . Often, people 40 and older are counseled to think about using donor eggs during IVF to boost the chances of success.
- Embryo status. Transfer of embryos that are more developed is linked with higher pregnancy rates compared with less-developed embryos. But not all embryos survive the development process. Talk with your care team about your specific situation.
- Reproductive history. People who've given birth before are more likely to be able to get pregnant using IVF than are people who've never given birth. Success rates are lower for people who've already tried IVF multiple times but didn't get pregnant.
- Cause of infertility. Having an average supply of eggs raises your chances of being able to get pregnant using IVF . People who have severe endometriosis are less likely to be able to get pregnant using IVF than are those who have infertility without a clear cause.
- Lifestyle factors. Smoking can lower the chance of success with IVF . Often, people who smoke have fewer eggs retrieved during IVF and may miscarry more often. Obesity also can lower the chances of getting pregnant and having a baby. Use of alcohol, drugs, too much caffeine and certain medicines also can be harmful.
Talk with your care team about any factors that apply to you and how they may affect your chances of a successful pregnancy.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
- FAQs: Treating infertility. American College of Obstetricians and Gynecologists. http://www.acog.org/Patients/FAQs/Treating-Infertility. Accessed Feb. 23, 2023.
- In vitro fertilization. AskMayoExpert. Mayo Clinic; 2022.
- ART: Step-by-step guide. American Society for Reproductive Medicine. https://www.sart.org/patients/a-patients-guide-to-assisted-reproductive-technology/general-information/art-step-by-step-guide/. Accessed Feb. 27, 2023.
- Anchan RM, et al. Gestational carrier pregnancy. https://www.uptodate.com/contents/search. Accessed Feb. 23, 2023.
- Infertility fact sheet. Office on Women's Health. http://www.womenshealth.gov/publications/our-publications/fact-sheet/infertility.html. Accessed Feb. 23, 2023.
- Ho J. In vitro fertilization. https://www.uptodate.com/contents/search. Accessed Feb. 23, 2023.
- FAQs: IVF. Society for Assisted Reproductive Technology. https://www.sart.org/patients/frequently-asked-questions/. Accessed Feb. 23, 2023.
- FAQs: Infertility. Centers for Disease Control and Prevention. http://www.cdc.gov/reproductivehealth/Infertility/. Accessed Feb. 23, 2023.
- FAQs: Evaluating infertility. American College of Obstetricians and Gynecologists. https://www.acog.org/Patients/FAQs/Evaluating-Infertility. Accessed Feb. 23, 2023.
- Ovarian hyperstimulation. Society for Assisted Reproductive Technology. https://www.sart.org/patients/a-patients-guide-to-assisted-reproductive-technology/stimulation/ovarian-hyperstimulation-syndrome/. Accessed Feb. 23, 2023.
- Guidance on the limits to the number of embryos to transfer: A committee opinion. Practice Committee of the American Society for Reproductive Medicine and the Practice Committee for the Society for Assisted Reproductive Technologies. https://www.asrm.org/news-and-publications/practice-committee-documents/. Accessed March 1, 2023.
- In vitro fertilization (IVF): What are the risks? American Society for Reproductive Medicine. https://www.sart.org/patients/risks-of-ivf/ Accessed Feb. 2, 2024.
- Preparing for IVF: Emotional considerations. Society for Assisted Reproductive Technology. https://www.sart.org/patients/a-patients-guide-to-assisted-reproductive-technology/general-information/preparing-for-ivf-emotional-considerations/. Accessed March 1, 2023.
- Micromanipulation. Society for Assisted Reproductive Technology. https://www.sart.org/patients/a-patients-guide-to-assisted-reproductive-technology/general-information/micromanipulation/. Accessed March 1, 2023.
- Preparing for in vitro fertilization (IVF): Lifestyle factors. Society for Assisted Reproductive Technology. https://www.sart.org/patients/fyi-videos/preparing-for-in-vitro-fertilization-ivf-lifestyle-factors/. Accessed March 1, 2023.
- Ubaldi FM, et al. Advanced maternal age in IVF: Still a challenge? The present and the future of its treatment. Frontiers in Endocrinology. 2019;10:94.
- Can I freeze my eggs to use later if I'm not sick? American Society for Reproductive Medicine. https://www.reproductivefacts.org/news-and-publications/patient-fact-sheets-and-booklets/documents/fact-sheets-and-info-booklets/can-i-freeze-my-eggs-to-use-later-if-im-not-sick/. Accessed Feb. 24, 2023.
- Medications for inducing ovulation: A guide for patients. American Society for Reproductive Medicine. https://www.reproductivefacts.org/news-and-publications/patient-fact-sheets-and-booklets/documents/fact-sheets-and-info-booklets/medications-for-inducing-ovulation-booklet/. Accessed Feb. 24, 2023.
- In vitro fertilization (IVF): What are the risks? American Society for Reproductive Medicine. https://www.reproductivefacts.org/news-and-publications/patient-fact-sheets-and-booklets/documents/fact-sheets-and-info-booklets/in-vitro-fertilization-ivf-what-are-the-risks/. Accessed Feb. 24, 2023.
- Commonly asked questions about the US national ART surveillance system. Centers for Disease Control and Prevention. https://www.cdc.gov/art/reports/2019/commonly-asked-questions.html. Accessed Feb. 27, 2023.
- Evaluation before IVF. Society for Assisted Reproductive Technology. https://www.sart.org/patients/sart-patient-evaluation/. Accessed Feb. 27, 2023.
- Multifetal pregnancy reduction. The American College of Obstetricians and Gynecologists. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2017/09/multifetal-pregnancy-reduction. Accessed Feb. 27, 2023.
- Third party reproduction. Society for Assisted Reproductive Technology. https://www.sart.org/patients/third-party-reproduction/. Accessed Feb. 27, 2023.
- Ho J. In vitro fertilization: Overview of clinical issues and questions. https://www.uptodate.com/contents/search. Accessed Feb. 27, 2023.
- American Society for Reproductive Medicine. Fertility drugs and cancer: A guideline. Fertility and Sterility. 2016; doi:10.1016/j.fertnstert.2016.08.035.
- Bart CJM. Overview of ovulation induction. https://www.uptodate.com/contents/search. Accessed March 2, 2023.
- Gershenson DM, et al. In vitro fertilization. In: Comprehensive Gynecology. 8th ed. Elsevier; 2022. https://www.clinicalkey.com. Accessed March 2, 2023.
- Barcroft JF, et al. Fertility treatment and cancers-the eternal conundrum: A systematic review and meta-analysis. Human Reproduction. 2021; doi:10.1093/humrep/deaa293.
- Hornstein MD, et al. Endometriosis: Treatment of infertility in females. https://www.uptodate.com/contents/search. Accessed March 2, 2023.
- Egg retrieval technique
- Female fertility tips
- Female infertility
- High-risk pregnancy
- Infertility
- Low sperm count
- Male infertility
- Male masturbation: Does frequency affect male fertility?
- Ovarian cysts and infertility: A connection?
News from Mayo Clinic
- Mayo Clinic in Rochester team ranked among 'America's Best Fertility Clinics' by Newsweek April 23, 2024, 05:30 p.m. CDT
- Mayo Clinic in Rochester top ranked on 'America's Best Fertility Clinics' in Newsweek rankings March 15, 2023, 01:33 p.m. CDT
- Doctors & Departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
- Trying to Conceive
- Signs & Symptoms
- Pregnancy Tests
- Fertility Testing
- Fertility Treatment
- Weeks & Trimesters
- Staying Healthy
- Preparing for Baby
- Complications & Concerns
- Pregnancy Loss
- Breastfeeding
- School-Aged Kids
- Raising Kids
- Personal Stories
- Everyday Wellness
- Safety & First Aid
- Immunizations
- Food & Nutrition
- Active Play
- Pregnancy Products
- Nursery & Sleep Products
- Nursing & Feeding Products
- Clothing & Accessories
- Toys & Gifts
- Ovulation Calculator
- Pregnancy Due Date Calculator
- How to Talk About Postpartum Depression
- Editorial Process
- Meet Our Review Board
In Vitro Fertilization (IVF): What to Expect
Where to Start With the IVF Process
IVF Process Basics
- Success Rates
- IVF Safety and Risks
- Step 1: Before Treatment
- Step 2: Treatment Cycle Begins
- Step 3: Ovarian Stimulation
- Step 4: Oocyte Maturation
- Step 5: Egg Retrieval
- Step 6: Fertilization
- Step 7: Embryo Transfer
- Step 9: Pregnancy Test
When IVF Treatment Fails
Frequently asked questions.
Starting the in vitro fertilization (IVF) process can be an exciting and nerve-wracking experience. Most people pursue IVF only after other fertility treatments have failed. You may have been trying to conceive for months. or, more likely, for years. But this is not always the case. Sometimes, doctors recommend starting with IVF treatment.
For example, IVF may be the first option if a person's fallopian tubes are blocked or if you will be using a gestational carrier and/or an egg donor . IVF also may be used in severe cases of male infertility or when previously cryopreserved eggs are being used. Still, even in these cases, IVF may come after trying to get pregnant and several fertility tests .
The more you understand about what's coming next, the more in control you'll feel. While every clinic's protocol, and every person's treatment needs, will be slightly different, this step-by-step breakdown takes you through the IVF process and helps you learn where to start with IVF.
In vitro means “in the lab” and fertilization refers to conception. Usually, IVF involves taking eggs (retrieved via a transvaginal ultrasound-guided needle) and placing them in a petri dish with specially washed sperm cells (retrieved via masturbation). The entire cycle from start to finish can take four to six weeks.
These eggs are retrieved after the ovaries have been stimulated. For conventional IVF, you need lots of eggs. Injectable fertility drugs stimulate the ovaries to mature a dozen or more eggs for retrieval. There also is minimal stimulation IVF (aka mini IVF) , where oral fertility drugs or very low dose injectable drugs help mature just a few eggs.
If all goes well, some of the retrieved eggs will be fertilized by the sperm cells and become embryos. One or two of those healthy embryos will be transferred to your uterus.
IVF Success Rates
IVF is pretty successful. According to a study of approximately 156,000 women, the average live-birth rate for the first cycle was 29.5%. This is comparable to the success rates for a natural cycle in couples with healthy fertility.
The best odds for success may come from repeated treatment cycles. This same study found that after six IVF cycles, the cumulative live-birth rate was 65.3%. These six cycles usually took place over 2 years.
Age does play an important role in your success, as does the reason for your infertility. Using an egg donor will also affect your success.
Be sure to discuss your personal odds for success with your healthcare provider before starting treatment.
While your provider can’t tell you for certain whether treatment will work for you, they should have an idea of your odds in relation to the average and in relation to other patients like yourself.
IVF is expensive. It’s also frequently not covered by insurance, putting the treatment out of reach for many people who need it. Studies have found that only one in four couples who need IVF to conceive can actually get the treatment they need.
The average cost of IVF often quoted is between $12,000 and 15,000 per cycle. Some say this estimate is really below the reality, and the out-of-pocket average costs are higher.
One study found that the average couple paid $19,234 for their initial IVF cycle, with an additional $6,955 for each additional cycle. Why such a difference between the first and subsequent? Partially because some of those second and third cycles are frozen embryo transfers.
This is all for conventional, no-frills IVF. If you need any additional technologies—like ICSI, PGT, assisted hatching , an egg donor, or a gestational carrier—costs will be higher (sometimes much higher).
There are ways to pay less or get financial assistance for IVF treatment . Look into all your options before making a decision on whether or not you can afford treatment.
Safety and Risks of IVF
IVF is generally safe, but as with any medical procedure, there are risks. Your provider should explain all the possible side effects and risks of each procedure before you begin.
Ovarian Hyperstimulation Syndrome
For instance, ovarian hyperstimulation syndrome (OHSS) occurs in 10% of people whose ovaries are stimulated for IVF treatment. For most people, symptoms are mild, and they recover easily. For a small percentage, OHSS can be more serious and may require hospitalization. Less than 1% of people going through egg retrieval will experience blood clots or kidney failure due to OHSS.
Cramping, Discomfort, or Infection
Egg retrieval may cause cramping and discomfort during or after the procedure. Rare complications include accidental puncture of the bladder, bowel, or blood vessels; pelvic infection; or bleeding from the ovary or pelvic vessels.
If pelvic infection does occur, you'll be treated with intravenous antibiotics. In rare cases of severe infection, the uterus, ovaries or fallopian tubes may need to be surgically removed.
The embryo transfer also may cause mild cramping during the procedure. Rarely, people will experience cramping, bleeding, or spotting after the transfer. In very rare cases, infection can occur. Infection is typically treated with antibiotics.
There is a risk of multiples, which includes twins, triplets, or more. Multiple pregnancies can be risky for both the babies and the parent. It's important to discuss with your healthcare provider how many embryos to transfer, as transferring more than necessary will increase your risk of conceiving twins or more. When embryos have been tested with PGT, typically only a single embryo is transferred.
Birth Defects
Some research has found that IVF may raise the risk of some very rare birth defects, but the risk is still relatively low. Research has also found that the use of ICSI with IVF, in certain cases of male infertility, may increase the risk of infertility and some sexual birth defects for male children. This risk, however, is very low (less than 1%).
IVF Step 1: Before Treatment
The cycle before your IVF treatment is scheduled, you may be put on birth control pills. This may seem backward, but using birth control pills before a treatment cycle may improve your odds of success. Also, it may decrease the risk of ovarian hyperstimulation syndrome and ovarian cysts.
Not every healthcare provider uses birth control pills the cycle before. Another possibility is that your provider will ask you to track ovulation the cycle before. Most likely, they will recommend using an ovulation predictor kit . However, they may also suggest basal body temperature charting , especially if you have experience charting your cycles.
Then, you will need to let your healthcare provider know as soon as you detect ovulation. Sometime after ovulation, the fertility clinic may then have you start taking a GnRH antagonist (like Ganirelix ) or a GnRH agonist (like Lupron) . These are injectable drugs, but some are available as a nasal spray or implant.
These medications allow your provider to have complete control over ovulation once your treatment cycle begins. If you don't get your cycles on your own, your provider may take yet another approach. In this case, they may prescribe progesterone in the form of Provera. This would bring on your period.
In this case, your healthcare provider will probably ask that you start taking the GnRH agonist or antagonist about 6 days or more after your first Provera pill. Again, though, this may vary. Always follow your provider's instructions.
IVF Step 2: Treatment Cycle Begins
The first official day of your treatment cycle is the day you get your period. On the second day of your period, your healthcare provider will likely order bloodwork and a transvaginal ultrasound .
These first-day tests are referred to as your baseline bloodwork and your baseline ultrasound. In your bloodwork, your healthcare provider will be looking at your estrogen levels, specifically your E2 or estradiol. This is to make sure your ovaries are “sleeping." That's the intended effect of the Lupron shots or GnRH antagonist.
The ultrasound is to check the size of your ovaries. Your provider will also look for ovarian cysts. If there are cysts, they will decide how to deal with them. Sometimes your provider will just delay treatment for a week. Most cysts resolve on their own with time. In other cases, your provider may aspirate the cyst (suck out the fluid) with a needle.
Usually, these tests will be fine. If everything looks OK, treatment moves on.
IVF Step 3: Ovarian Stimulation and Monitoring
Ovarian stimulation with fertility drugs is the next step. Depending on your treatment protocol, this may mean anywhere from one to four shots every day for about a week to 10 days. Your clinic should teach you how to give yourself the injections before treatment begins.
During ovarian stimulation, your doctor will monitor the growth and development of the follicles . At first, this may include bloodwork and ultrasounds every few days. Your provider will be monitoring your estradiol levels. During the ultrasounds, they will monitor the oocyte growth. (Oocytes are the eggs in your ovaries.)
Monitoring the cycle is very important. This is how your provider will decide how to adjust your medications. You may need to increase or decrease dosages. Once your largest follicle is 16 to 18 mm in size, your clinic will probably want to see you daily.
IVF Step 4: Final Oocyte Maturation
The next step in your IVF treatment is triggering the oocytes to go through the last stage of maturation. The eggs must complete their growth and development before they can be retrieved.
This last growth is triggered with human chorionic gonadotropin (hCG). Brand names for this include Ovidrel , Novarel, and Pregnyl. Timing this shot is vital. If it's given too early, the eggs will not have matured enough. If given too late, the eggs may be “too old” and won't fertilize properly.
Daily ultrasounds help time this trigger shot just right. Usually, the hCG injection is given when four or more follicles have grown to be 18 to 20 mm in size and estradiol levels are greater than 2,000 pg/ML.
This shot is typically a one-time injection. Your healthcare provider will likely give you an exact hour to do this shot. Be sure to follow these instructions!
IVM vs. IVF
During conventional IVF, eggs must complete their development and growth before being retrieved. IVM treatment is slightly different. IVM stands for in vitro maturation . It is similar to IVF but significantly differs at this point in the process.
During IVM, the eggs are retrieved before they go through all stages of maturity. You will not have a "trigger shot" during IVM. The eggs retrieved will be matured in the lab environment. Once the eggs are matured, the rest of the steps follow the IVF process.
If the Follicles Don't Grow
We've assumed to this point that the ovarian stimulation drugs have worked properly. But that isn't always how it goes. Sometimes the follicles don't grow. If this happens, your healthcare provider may increase the medications, but if your ovaries still don't respond, the cycle will likely be canceled .
This doesn't mean another cycle won't work. You may just need different medications. However, if this occurs repeatedly, your provider may suggest using an egg or embryo donor. You may want to get a second opinion before moving forward at this point.
If You're at Risk for OHSS
Another possible problem is your ovaries respond too well. If your healthcare provider thinks you're at risk of developing severe ovarian hyperstimulation syndrome (OHSS), your trigger shot will be canceled and the cycle will be stopped at this point.
Another possibility is your provider will retrieve the eggs, fertilize them, but delay the embryo transfer. This is because pregnancy can worsen and extend recovery from OHSS. Once your body recovers, you can try a frozen embryo transfer.
During your next cycle, your provider may suggest lower doses of medications, try different medications before your cycle starts, or even suggest IVM instead of IVF.
If You Ovulate Prematurely
While not common, a cycle may also be canceled if ovulation occurs before retrieval can take place. Once the eggs ovulate on their own, they can't be retrieved. Your healthcare provider will likely tell you to refrain from sexual intercourse.
It's important you follow these instructions! It's possible you've ovulated up to a dozen eggs, maybe even more. There is danger to both you and the children if you got pregnant naturally with even half of those eggs.
Cancellation happens in 10% to 20% of IVF treatment cycles. The chance of cancellation rises with age. Those older than age 35 are more likely to experience treatment cancellation.
IVF Step 5: Egg Retrieval
About 34 to 36 hours after you receive the trigger shot, the egg retrieval will take place. It's normal to be nervous about the procedure, but most people go through it without much trouble or pain.
Before the retrieval, an anesthesiologist will give you some medication intravenously to help you feel relaxed and pain-free. Usually, a light sedative is used. This isn't the same as general anesthesia, which is used during surgery. Side effects and complications are less common.
Once the medications take effect, your doctor will use a transvaginal ultrasound to guide a needle through the back wall of your vagina, up to your ovaries. They will then use the needle to aspirate the follicle, or gently suck the fluid and oocyte from the follicle into the needle. There is one oocyte per follicle. These oocytes will be transferred to the embryology lab for fertilization.
The number of oocytes retrieved varies, but can usually be estimated before retrieval via ultrasound. The average number of oocytes is 8 to 15, with more than 95% of patients having at least one oocyte retrieved.
After the retrieval procedure, you'll stay in a recovery area for a few hours to make sure all is well. Light spotting is common, as well as lower abdominal cramping, but most people feel better in a day or so after the procedure. You'll also be told to watch for signs of ovarian hyperstimulation syndrome.
IVF Step 6: Egg Fertilization
While you're recovering from the retrieval, the follicles that were aspirated will be searched for oocytes, or eggs. Not every follicle will contain an oocyte.
Once the oocytes are found, they'll be evaluated by the embryologist. If the eggs are overly mature, fertilization may not be successful. If they are not mature enough, the embryology lab may be able to stimulate them to maturity in the lab.
Fertilization of the oocytes must happen within 12 to 24 hours. Your partner will likely provide a semen sample the same morning you have the retrieval. The stress of the day can make it difficult for some, and so just in case, your partner may provide a semen sample for backup earlier in the cycle, which can be frozen until the day of the retrieval.
Once the semen sample is ready, it will be put through a special washing process, which separates the sperm from the seminal fluid. The embryologist will choose the best-looking sperm, placing about 10,000 sperm in each culture dish with an oocyte. The culture dishes are kept in a special incubator, and after 12 to 24 hours, they are inspected for signs of fertilization.
With the exception of severe male infertility, 70% of the oocytes will become fertilized. In the case of severe male infertility, ICSI, or intracytoplasmic sperm injection , may be used to fertilize the eggs, instead of simply placing them in a culture dish. With ICSI, the embryologist will choose a healthy-looking sperm and inseminate the oocyte with the sperm using a needle.
IVF Step 7: Embryo Transfer
About three to five days after the retrieval, an embryologist will identify the healthiest looking embryos. This is typically done visually (with a microscope), but in some cases, genetic screening is performed. This is known as preimplantation genetic diagnosis (PGD) or preimplantation genetic screening (PGS).
Sometimes, with PGD/PGS, the embryos are cryopreserved and transfer is delayed until the next cycle. Otherwise, a "fresh" transfer takes place. The procedure for embryo transfer is just like intrauterine insemination ( IUI) treatment . You won't need anesthesia.
During the embryo transfer, a thin tube, or catheter, will be passed through your cervix. You may experience very light cramping but nothing more than that. The doctor will transfer the embryos through the catheter, along with a small amount of fluid.
The number of embryos transferred will depend on the quality of the embryos and discussion with your healthcare provider. Depending on your age, anywhere from one to five embryos may be transferred.
After the transfer, you will remain lying down for a couple hours and then go home. If there are high-quality embryos left, you may be able to freeze them. This is called embryo cryopreservation. They can be used later if this cycle isn't successful in a frozen embryo transfer , or they can be donated.
Currently, many providers suggest transferring just one embryo and freezing the rest. This is known as elective single embryo transfer (eSET), and it can reduce your risk of a multiple pregnancy. When you get pregnant with just one healthy baby, you reduce your risks for pregnancy complications. Speak to your provider to find out if elective single embryo transfer is best for you.
IVF Step 8: The Two-Week Wait
On or after the day of your retrieval, and before the embryo transfer, you'll start giving yourself progesterone supplements. Usually, the progesterone during IVF treatment is given as a self-injection. Sometimes, though, a progesterone supplement is a pill, vaginal gel, or vaginal suppository.
Besides the progesterone, there really isn't much going on for the next two weeks. In some ways, the two weeks after the transfer may be more difficult emotionally than the two weeks of treatment. During the previous steps, you will have visited your provider perhaps every other day. Now, after transfer, there will be a sudden lull in activity.
All you can do is wait the two weeks and see if pregnancy takes place. It can help to keep busy with your life during this wait time and avoid sitting and thinking about whether or not treatment will be successful.
IVF Step 9: Pregnancy Test and Follow-Up
About 9 to 12 days after the embryo transfer, a pregnancy test is ordered. This is usually a blood test and also will include a test to check the level of progesterone. The test may be repeated every few days.
If the test is positive , you may need to keep taking progesterone for another several weeks. Your provider will also follow up with occasional bloodwork and ultrasounds to monitor the pregnancy.
Possible IVF Pregnancy Risks
Your healthcare provider will also monitor whether or not the treatment led to a multiple pregnancy. IVF has a higher risk of conceiving multiples, and a multiple pregnancy carries risks for both the parent and the babies , including premature labor and delivery , maternal hemorrhage, C-section delivery , pregnancy induced high blood pressure, and gestational diabetes .
People who conceive with IVF are more likely to experience spotting in early pregnancy , though it's more likely for their spotting to resolve without harm to the pregnancy.
The risk of miscarriage is about the same for people who conceive naturally, with the risk going up with age. For those in their 20s, the rate of miscarriage is as low as 15%, while for people over 40, the rate of miscarriage may be over 50%.
There is a 2% to 4% risk of ectopic pregnancy with IVF conception. If you developed OHSS from the fertility drugs, and you get pregnant, recovery may take longer.
If the pregnancy test is still negative 12 to 14 days post-transfer, your healthcare provider will ask you to stop taking the progesterone. Then, you'll wait for your period to start.
It will be up to you, your partner, and your provider to determine next steps. If this was your first cycle, another cycle may be recommended. Remember that your best chances for success are after doing several cycles.
Having a treatment cycle fail is never easy. It's heartbreaking. It's important, however, to keep in mind that having one cycle fail doesn't mean you won't be successful if you try again. There are many steps you can take after a treatment cycle fail.
Even though IVF has relatively high success rates, there are times that it fails. Sometimes IVF fails due to chromosomal abnormalities. Age also can play a factor in the success rate of IVF. Other times, a failure just can't be explained.
If you are considering IVF, there are lifestyle changes you can make that will improve your chances of success. These include eating a balanced diet, exercising on a consistent basis, getting plenty of water, and practicing good sleep hygiene.
You also want to be sure you are reducing your stress levels and taking care of yourself. Going through IVF can be a challenging experience and you want to ensure you are in the best shape you can be.
When it comes to IVF, it is important to make the lifestyle changes that your healthcare provider recommends. For instance, many providers recommend avoiding alcohol, caffeine, and smoking. They also may suggest certain dietary changes like limiting red meat, dairy products, refined sugars, and processed foods. Before you make any drastic changes to eating patterns, you should discuss your goals with your provider. They can let you know what is the best meal plan for you.
American College of Obstetricians and Gynecologists. Treating Infertility .
Cleveland Clinic. In vitro fertilization .
Santos MA, Kuijk EW, Macklon NS. The impact of ovarian stimulation for IVF on the developing embryo . Reproduction . 2010;139(1):23-34. doi:10.1530/REP-09-0187
Smith ADAC, Tilling K, Nelson SM, Lawlor DA. Live-birth rate associated with repeat in vitro fertilization treatment cycles . JAMA . 2015;314(24):2654-2662. doi:10.1001/jama.2015.17296
Klitzman R. How much is a child worth? Providers' and patients' views and responses concerning ethical and policy challenges in paying for ART . PLoS One . 2017;12(2):e0171939. doi:10.1371/journal.pone.0171939
Wu AK, Odisho AY, Washington SL, Katz PP, Smith JF. Out-of-pocket fertility patient expense: Data from a multicenter prospective infertility cohort . J Urol. 2014;191(2):427-432. doi:10.1016/j.juro.2013.08.083
Zivi E, Simon A, Laufer N. Ovarian hyperstimulation syndrome: Definition, incidence, and classification . Semin Reprod Med. 2010;28(6):441-447. doi:10.1055/s-0030-1265669
Levi-Setti PE, Cirillo F, Scolaro V, et al. Appraisal of clinical complications after 23,827 oocyte retrievals in a large assisted reproductive technology program . Fertil Steril. 2018;109(6):1038-1043.e1. doi:10.1016/j.fertnstert.2018.02.002
Boulet SL, Kirby RS, Reefhuis J, et al. Assisted reproductive technology and birth defects among liveborn infants in Florida, Massachusetts, and Michigan, 2000-2010 . JAMA Pediatr. 2016;170(6):e154934. doi:10.1001/jamapediatrics.2015.4934
Lacamara C, Ortega C, Villa S, Pommer R, Schwarze JE. Are children born from singleton pregnancies conceived by ICSI at increased risk for congenital malformations when compared to children conceived naturally? A systematic review and meta-analysis . JBRA Assist Reprod . 2017;21(3):251-259. doi:10.5935/1518-0557.20170047
Wang L, Zhao Y, Dong X, et al. Could pretreatment with oral contraceptives before pituitary down regulation reduce the incidence of ovarian hyperstimulation syndrome in the IVF/ICSI procedure? . Int J Clin Exp Med . 2015;8(2):2711-2718.
Jungheim ES, Meyer MF, Broughton DE. Best practices for controlled ovarian stimulation in in vitro fertilization . Semin Reprod Med . 2015;33(2):77-82. doi:10.1055/s-0035-1546424
Abbara A, Vuong LN, Ho VNA, et al. Follicle size on day of trigger most likely to yield a mature oocyte . Front Endocrinol (Lausanne) . 2018;9:193. doi:10.3389/fendo.2018.00193
Lu X, Khor S, Zhu Q et al. Decrease in preovulatory serum estradiol is a valuable marker for predicting premature ovulation in natural/unstimulated in vitro fertilization cycle . J Ovarian Res. 2018;11(1):96. doi:10.1186/s13048-018-0469-x
Shalom-Paz E, Holzer H, Son WY, Levin I, Tan SL, Almog B. PCOS patients can benefit from in vitro maturation (IVM) of oocytes . Eur J Obstet Gynecol Reprod Biol. 2012;165(1):53-56. doi:10.1016/j.ejogrb.2012.07.001
Lainas GT, Kolibianakis EM, Sfontouris IA, et al. Outpatient management of severe early OHSS by administration of GnRH antagonist in the luteal phase: an observational cohort study . Reprod Biol Endocrinol. 2012;10:69. doi:10.1186/1477-7827-10-69
Avraham S, Seidman DS. The multiple birth epidemic: Revisited . J Obstet Gynaecol India . 2012;62(4):386-390. doi:10.1007/s13224-012-0309-7
Shaulov T, Vélez MP, Buzaglo K, Phillips SJ, Kadoch IJ. Outcomes of 1503 cycles of modified natural cycle in vitro fertilization: a single-institution experience . J Assist Reprod Genet . 2015;32(7):1043-1048. doi:10.1007/s10815-015-0502-6
Society for Assisted Reproductive Technology. ART: Step-by-Step Guide .
Nagarajan S, Lew E. Anesthetic choices in IVF practice . In: Cheong Y, Tulandi T, Li TC, eds. Practical Problems in Assisted Conception . Cambridge University Press, 2018;97-101. doi:10.1017/9781108149891.021
Magnusson Å, Källen K, Thurin-Kjellberg A, Bergh C. The number of oocytes retrieved during IVF: a balance between efficacy and safety . Hum Reprod. 2018;33(1):58-64. doi:10.1093/humrep/dex334
Patrat C, Kaffel A, Delaroche L, et al. Optimal timing for oocyte denudation and intracytoplasmic sperm injection . Obstet Gynecol Int. 2012;403531. doi:10.1155/2012/403531
Eftekhar M, Mohammadian F, Yousefnejad F, Molaei B, Aflatoonian A. Comparison of conventional IVF versus ICSI in non-male factor, normoresponder patients . Iran J Reprod Med . 2012;10(2):131-136.
American Society for Reproductive Medicine. What is intracytoplasmic sperm injection (ICSI)? .
Simpson JL. Preimplantation genetic diagnosis at 20 years . Prenat Diagn. 2010;30(7):682-695. doi:10.1002/pd.2552
Schoolcraft WB. Importance of embryo transfer technique in maximizing assisted reproductive outcomes . Fertil Steril. 2016;105(4):855-860. doi:10.1016/j.fertnstert.2016.02.022
McLernon DJ, Harrild K, Bergh C, et al. Clinical effectiveness of elective single versus double embryo transfer: meta-analysis of individual patient data from randomised trials . BMJ . 2010;341:c6945. doi:10.1136/bmj.c6945
Montagnana M, Trenti T, Aloe R, Cervellin G, Lippi G. Human chorionic gonadotropin in pregnancy diagnostics . Clinica Chimica Acta . 2011;412(17-18):1515-1520. doi:10.1016/j.cca.2011.05.025
Lazarov S, Lazarov L, Lazarov N. Multiple pregnancy and birth: Twins, triplets and high-order multiples . Trakia J Sci . 2016;14(1):103-107. doi:10.15547/tjs.2016.01.015
Qazi G. Obstetric and perinatal outcome of multiple pregnancy . J Coll Physicians Surg Pak. 2011;21(3):142-145.
Jabara S, Barnhart K, Schertz JC, Patrizio P. Luteal phase bleeding after IVF cycles: comparison between progesterone vaginal gel and intramuscular progesterone and correlation with pregnancy outcomes . J Exp Clin Assist Reprod . 2009;6:6.
Magnus MC, Wilcox AJ, Morken NH, Weinberg CR, Håberg SE. Role of maternal age and pregnancy history in risk of miscarriage: prospective register based study . BMJ . 2019;364:l869. doi:10.1136/bmj.l869
Perkins KM, Boulet SL, Kissin DM, Jamieson DJ. Risk of ectopic pregnancy associated with assisted reproductive technology in the United States, 2001–2011 . Obstet Gynecol. 2015;125(1):70-78. doi:10.1097/AOG.0000000000000584
Bhattacharya S, Maheshwari A, Mollison J. Factors associated with failed treatment: an analysis of 121,744 women embarking on their first IVF cycles . PLoS One . 2013 Dec 5;8(12):e82249. doi:10.1371/journal.pone.0082249
By Rachel Gurevich, RN Rachel Gurevich is a fertility advocate, author, and recipient of The Hope Award for Achievement, from Resolve: The National Infertility Association. She is a professional member of the Association of Health Care Journalists and has been writing about women’s health since 2001. Rachel uses her own experiences with infertility to write compassionate, practical, and supportive articles.

208-342-5900

The IVF Process from Start to Finish: Creating a Reliable IVF Calendar & IVF Timeline
Planning for an infertility treatment like in vitro fertilization (IVF) is a significant step toward realizing your dream of becoming a parent—and it takes time, energy, and considerate planning. An IVF cycle calendar is one tool that can help.
Whether you’re considering IVF as an option, have just started your IVF journey, or are well into the process, creating an IVF calendar can help you know what to expect of your treatment so that you can better plan for and manage your treatment—and ultimately achieve a successful pregnancy.
How do you determine an IVF calendar?
Like many infertility treatments, IVF often involves a complex of hormone therapies, medications, and coordinating fertility treatments. With so many moving parts and diverging timelines, creating an IVF timeline calendar isn’t quite as simple as mapping out the IVF cycle itself.
The IVF process from start to finish depends on your specific goals and infertility diagnoses. Some intended parents, for example, might be using an egg donor , sperm donor, or gestational carrier to build their family with IVF. This involves coordinating with a surrogacy agency, egg donor program, or sperm bank; choosing your donor or surrogate, and legally securing the third party.
The timeline for this process varies widely, ranging anywhere from two weeks to secure a sperm donor to several months to secure a gestational carrier —depending on factors like your family’s personal third-party requirements, the availability of donors or gestational carriers, and whether you’re working with an external or in-house donor program .
Another preliminary process is pre-genetic carrier screening . Some parents choose to test their carrier status for genetic health conditions, either informing their donor selection or their selection of a healthy embryo later in the process. Depending on your IVF centre, it typically takes 1–2 weeks to receive these test results.
When it comes to the IVF cycle itself, there is still plenty of timeline variability from one family to the next—depending on personal health factors, third-party factors, and whether your treatment involves a fresh or frozen embryo transfer .
Your fertility specialist will help you create a more precise timeline, but to begin creating an IVF calendar or to get a general sense, you can work from the time ranges involved in a typical IVF cycle, which begins in coordination with your menstrual cycle.
What does a realistic IVF calendar look like?
A full round of IVF spans one menstrual cycle (1 month) for a fresh embryo transfer and at least two menstrual cycles (2 months) for a fresh cycle followed by a frozen embryo transfer cycle.
Frozen embryo transfer (FET) is the more common option for several reasons, including lower cost, reduced strain on the parent’s body, the option for preimplantation testing of embryos (PGT) , and the potential for multiple embryos which can be cryopreserved .
After retrieving and freezing embryos, intended parents can choose to wait any amount of time before beginning the FET cycle, but for the sake of presenting one continuous IVF calendar and timeline range, we’ll walk through the stages of the IVF cycle assuming no additional waiting times.
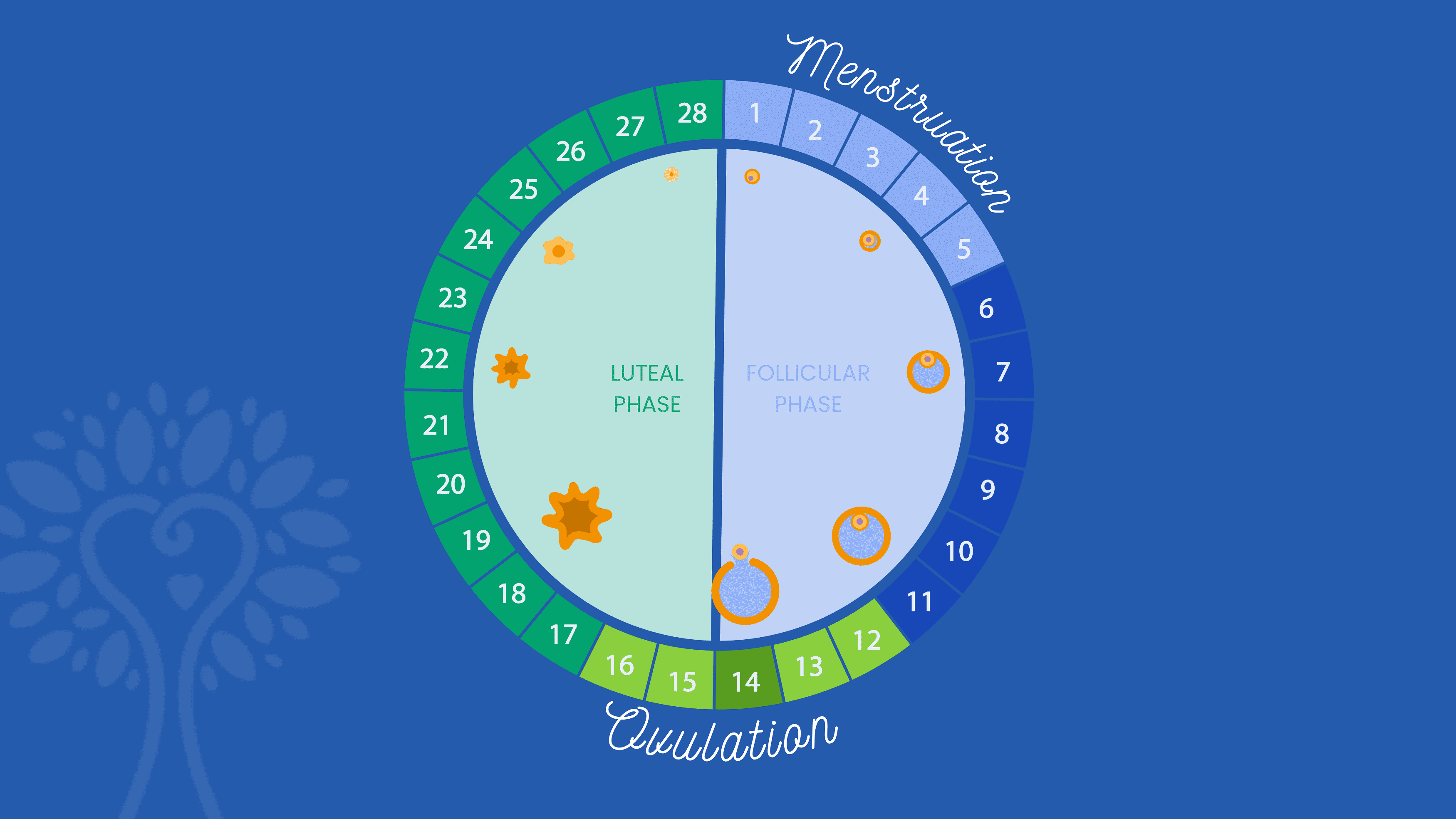
Assuming Day 1 is the first day of your menstrual cycle, here’s what a typical IVF calendar will include:
Ovarian Stimulation : The IVF cycle starts with a 9–15 day period of ovarian stimulation, using hormone injections called gonadotropins or follicle stimulating hormones, to produce multiple follicles and allow as many eggs as possible to mature for retrieval from the ovaries. Sometimes birth control pills or estrace are prescribed for you to take prior to starting the follicle stimulating hormones.
Monitoring : Throughout the ovarian stimulation phase, regular monitoring through ultrasounds and blood tests is conducted to track follicle growth and hormone levels and to inform any adjustments to medication dosages or changes in your IVF calendar.
Trigger Injection : Once a sufficient number of follicles have reached maturity, a different gonadotropin injection is administered to induce final egg maturation.
Egg Retrieval : The egg retrieval procedure is performed as an outpatient procedure under sedation or anesthesia. A needle is used to extract the mature eggs from the ovaries.
Sperm Collection and Fertilization : Sperm is either collected on the same day as the egg retrieval or cryopreserved earlier for later use. Once the eggs are retrieved and the sperm collected, both are transferred to an embryology lab where they are fertilized and closely monitored by embryologists.
Beginning of Embryo Culturing : Once fertilized, the embryos are cultured in the lab for 5–7 days, until they reach the blastocyst stage, at which point embryologists evaluate the embryos’ quality to determine which can be used. At this point, viable embryos can either be transferred back into the uterus directly or frozen for FET and/or PGT.
Day 20–27 (Optional – FET only)
Preimplantation Genetic Testing (PGT) : Often informed by a genetic risk found during the earlier carrier screening, PGT allows parents to test the carrier status and chromosomal health of each embryo . The embryos are biopsied and sent into a lab for testing, which typically takes 1–2 weeks.
Beginning of Uterine Preparation : In the case of an FET, the parent or gestational carrier undergoes 3–4 weeks of hormone treatments to enhance the uterine receptivity and support the early stages of pregnancy. This involves 2–3 weeks of estrogen treatments, followed by progesterone.
The embryo transfer is commonly done on the 6th day of progesterone. For a fresh embryo transfer, progesterone treatment is typically started within 24 hours of the egg retrieval and continues throughout the first trimester.
Embryo Transfer : On the 6th day of progesterone treatment, the fresh or thawed embryo is transferred to the uterus.
Pregnancy Test : Approximately 10–14 days after the embryo transfer, a blood test is performed to determine if pregnancy has been achieved.
How long do you have to wait after a failed round of IVF?
Experiencing a failed round of IVF—whether at the egg retrieval or embryo transfer stage—can be very discouraging and emotionally painful. Fortunately, there are often several treatment adjustments and therapeutic additions that can be made to increase odds of success in the next round. Before beginning the next IVF cycle attempt, it’s important to wait at least one menstrual cycle.
This waiting period, which typically amounts to about 4 weeks, allows the body to recover from the hormonal stimulation and any procedures associated with the previous cycle, ensuring a more stable and receptive uterine environment for the next attempt.
Like most aspects of your IVF calendar, it’s important to note that the specific waiting time may be different for each person, and your fertility specialist may recommend more based on your medical history and the reasons for the previous IVF failure.
Creating an IVF Calendar with ICRM
No matter where you find yourself on your fertility journey, the Idaho Center for Reproductive Medicine is here to provide support, guidance, and tailored treatment for your unique family.
During an IVF treatment with ICRM, our dedicated coordinators work closely with you to create and maintain an IVF calendar, schedule appointments, and navigate the intricacies of your treatment to help you achieve a successful pregnancy.
The Idaho Center for Reproductive Medicine
Quick Links
Request a Consultation
Patient Portal
Pay your Bill
Patient Resources
Refer a Patient
Freedom Injection Training
Privacy Policy
Share your Story
Patient Survey
Our Partner
1000 E. Park Blvd., Suite 110 Boise, Idaho 83712
3875 E. Overland Rd., Suite 103 Meridian, Idaho 83642
Office: 208-342-5900
Fax: 208-342-2088
Toll Free: 866-865-BABY
Email – Domestic Patients: [email protected]
Email – International Patients: [email protected]
Regular Hours of Operation: M-F 8:00am – 5:00pm. Meridian Appointment Availability: M-F 7:00am – 12:00pm

Your health in one app

Listen To Dr. Slater’s Most Recent Podcast!
In the latest episode of the SART Fertility Experts podcast, Dr. Slater and Betsy Campbell from RESOLVE discuss current barriers to reproductive medicine and how advocacy efforts are expanding access to care.

- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
What is IVF, and how does it work?
In vitro fertilization (IVF) is when sperm and eggs are combined outside the body – and it can help you get pregnant in a number of circumstances.

What is IVF?
Why choose ivf, what happens before in vitro fertilization, how does in vitro fertilization work, how long will ivf take, what is natural cycle ivf, what's the success rate for ivf, what are the pros of ivf, what are the cons of ivf, what does ivf cost.
In vitro fertilization (IVF) is a procedure that may be able to help you get pregnant. It's the main type of assisted reproductive technology (ART), and has been in use since the 1970s.
When you do IVF, your eggs are extracted and combined with sperm in a petri dish ("in vitro" means "in glass" in Latin). IVF can be done using an egg and sperm from you and your partner, or you can use donor eggs and/or donor sperm.
After IVF, the embryo or embryos that result are transferred to your uterus through the cervix. If all goes well, an embryo will implant in your uterine lining and continue to develop.
The use of ART has more than doubled over the past decade, according to the Centers for Disease Control and Prevention Opens a new window (CDC). About 2 percent of all infants born in the United States each year are conceived using ART.
"Assisted reproductive technology has helped so many individuals and couples on their path to parenthood who otherwise may have never had that chance," says Sasha Hakman, M.D., a double board-certified ob-gyn and reproductive endocrinologist with HRC Fertility Opens a new window in Los Angeles.
"We're so lucky to live in a time where we have this option at our disposal," says Dr. Hakman, who specializes in treating infertility and is a member of the BabyCenter Medical Advisory Board .
IVF can help you get pregnant if you or your partner have problems with:
- Egg quality
- Blocked fallopian tubes
- Endometriosis
- Sperm count or motility
- Unexplained infertility (when all fertility tests come back normal and the problem can't be identified)
IVF is also part of the journey to parenthood for some LGBTQ+ families , people using a gestational carrier (surrogate ), and single parents by choice.
Before undergoing any IVF procedures, you'll have preconception testing and fertility testing.
Preconception testing includes:
- An antibody screen to test for immunity to rubella and chicken pox
- An option for genetic carrier screening to help identify your risk of having children with genetic diseases
- Infectious disease testing for hepatitis B and C , HIV , syphilis , gonorrhea , and chlamydia
- Blood type testing, including Rh status
- A pap smear
Fertility testing includes:
- Ovarian reserve testing, called Anti Mullerian Hormone (AMH), to determine the number of eggs you have available
- Hormone testing (TSH and anything else that might be applicable, based on your history)
- Uterine evaluation, to make sure your uterus is healthy enough to carry a pregnancy
- Reviewing your partner's semen quality
Your doctor may recommend a trial (or mock) transfer. This is a practice run of the procedure, without the transfer of any embryos. During the trial, the doctor uses an empty embryo transfer catheter to determine the best path through your cervix to your uterus.

Once all the preliminaries are taken care of, IVF treatment usually goes something like this:
1. Ovarian stimulation. For eight to 14 days near the beginning of your menstrual cycle , you take a gonadotropin, a type of fertility drug that stimulates your ovaries to develop multiple mature eggs for fertilization (instead of just one). You'll also need to take a synthetic hormone like leuprolide or cetrorelix to keep your body from releasing the eggs too early.
2. Follicle development. While taking these medications, you'll visit your doctor's office or clinic every two to three days to have your blood hormone levels checked and ultrasound measurements of your follicles done. (Follicles are the fluid-filled sacs in your ovaries that each contain an egg.)
3. The trigger shot. When the follicles are ready, you get a "trigger shot," an injection that causes the eggs to mature fully and become capable of being fertilized. About 36 hours after your trigger shot, your eggs are ready to be retrieved.
4. Gathering the eggs. Your doctor gives you an anesthetic and inserts an ultrasound probe through your vagina to look at your ovaries and identify the follicles. A thin needle is then inserted through the vaginal wall to remove the eggs from the follicles. Eight to 15 eggs are usually retrieved. You may have some cramping and spotting for a few days afterward, but most women feel better in a day or two. Unless you're using donor sperm, sperm will be collected from your partner at this same appointment.
5. Fertilization. An embryologist (a scientist who specializes in eggs, sperm, and embryos) will examine your eggs before combining them with the sperm and incubating them overnight. Fertilization usually happens during this time.
If sperm quality is poor, or if fertilization was unsuccessful during previous IVF cycles, your doctor may recommend using a technique called intracytoplasmic sperm injection (ICSI). With ICSI, a single sperm is injected directly into each mature egg.
6. Developing embryos. Three days after the egg retrieval, some of the eggs that were successfully fertilized become six- to 10-celled embryos. By the fifth day, some of these embryos will become blastocysts with a fluid-filled cavity and cells that are beginning to separate into the placenta and baby.
7. Embryo selection. The embryologist selects the most viable embryo or embryos to place in your uterus three to seven days after the egg retrieval. Extra embryos, if there are any, may be frozen and used for future IVF cycles.
8. Placing the embryos. Depending on your age and diagnosis, your doctor places between one and five embryos in your uterus by inserting a thin tube (a catheter) through your cervix. You might feel some mild cramping, but you won't need anesthesia. In most cases only one embryo is transferred at a time. If more than one embryo is transferred, your chance of pregnancy is higher, but so are the odds of having twins or multiples .
9. Successful implantation. If the treatment works, an embryo implants in your uterine wall and continues to grow into a baby. If at any time during the IVF cycle your doctor feels that conditions aren't promising (your hormone levels are lower than necessary, fertilization failed, or no eggs are retrieved, for example), they will cancel the cycle.
You can take a pregnancy test about 9 to 12 days after the embryos are placed in your uterus. If it's positive, you'll be advised to repeat it in a couple of days. If it's negative, your physician will advise you to stop taking the medication you were given to support the pregnancy.
It takes about four to six weeks to complete one cycle of IVF.
- After taking drugs to stimulate your ovaries, you'll wait – usually a few weeks – for your eggs to mature. Then you'll spend a few hours at your doctor's office or clinic having your eggs retrieved and fertilized.
- You may go back again three to seven days later to have the embryos inserted into your uterus. You'll be able to go home that same day.
Then it's a matter of waiting to see if the embryo successfully implants in your uterus.
If you're using already-frozen embryos, the embryo transfer process is quicker, since IVF has already been completed. You'll take medications to prepare the uterine lining, and be monitored until your lining is ready for the embryo transfer. This typically takes about 19 to 21 days, but it might be longer or shorter, depending on your response to the medications. Following the transfer, you'll wait for successful implantation.
The long waiting period, along with the procedures, can be stressful. According to the Society for Assisted Reproductive Technology (SART), "patients have rated the stress of undergoing IVF as more stressful than or almost as stressful as any other major life event, such as the death of a family member or separation or divorce."
Being well informed about the process and asking for support can help. Learn more about how to cope with the emotional toll of infertility and prepare for and cope with the emotional considerations of IVF Opens a new window .
Natural cycle IVF is performed without the use (or with limited use) of medications – the injectable fertility drugs that are routinely given. Sometimes just one medication, the hCG trigger shot, is used.
The medications are expensive, and using them means more office visits and more testing. To make the process more affordable and attractive to some patients, some clinics offer IVF without injectable drugs. While this approach reduces the cost of the procedure, it also reduces the success rate, because fewer eggs are available.
Natural cycle IVF might appeal to patients who:
- Are at risk of ovarian hyperstimulation syndrome (which can be triggered by medications)
- Aren't interested in embryo cryopreservation (freezing), and so don't need to produce a number of eggs for fertilization
- Want to limit the number of eggs to be fertilized (for ethical or religious reasons)
- Don't have many follicles that develop mature eggs, despite receiving injectable medications
There are also variations of natural cycle IVF. A "mini IVF" procedure, for example, uses a lower dose of medication to create a smaller number of eggs than traditional IVF.
Here are the success rates for IVF procedures, based on national data collected for 2020 and preliminary data for 2021.
Using a patient's own eggs, the success rate for women undergoing IVF in 2021:
- 45% for women age 34 and under
- 32% for women age 35 to 37
- 20% for women age 38 to 40
- 10% for women age 41 to 42
- 3% for women age 43 and over
But to achieve the numbers above may take more than one transfer. On the first embryo transfer, the success rates for women using their own eggs are:
- 37% for women age 34 and under
- 28% for women age 35 to 37
- 18% for women age 38 to 40
- 9% for women age 41 to 42
IVF success rates are higher when using donor eggs, because donor eggs are only retrieved from women who are young and healthy. For all ages, IVF using fresh donor eggs has an overall success rate of 41%, and using frozen donor eggs has a success rate of 40%.
Thawed embryos have an overall success rate of 46%, and donated embryos have an overall success rate of 42%.
SART provides tools for estimating your individual chances of IVF success Opens a new window , and the CDC has a similar IVF success estimator Opens a new window .
- Successful track record. IVF is the oldest assisted reproductive technology (ART) procedure – it's been around since 1978. IVF has been used long enough for researchers to have done extended health studies on the children conceived using this method. So far, no medical problems have been directly linked to the procedure.
- Improved techniques. Researchers continue to refine and improve IVF procedures. For example, advances in embryo freezing have resulted in IVF pregnancy rates that are about the same for frozen and fresh embryos.
We now know, too, that there's no link between IVF and cancer. Early studies suggested that exposure to fertility drugs might lead to a higher risk of ovarian cancer or other cancers of the female reproductive system. But recent studies have shown no connection.
A recent analysis Opens a new window of 29 studies published in Human Reproduction concluded that "Overall, fertility treatment does not significantly increase the incidence of ovarian, breast, or endometrial cancer and may even reduce the incidence of cervical cancer."
- Cost and time. Fertilizing your eggs outside of your body requires costly lab work and medications. Monitoring your response to fertility drugs also requires a lot of time, with frequent trips to the doctor's office for blood tests and ultrasounds.
- Odds of multiples . Because more than one embryo may be placed in your uterus, your chance of having twins or more is increased with IVF. Though many couples consider this a blessing, multiple fetuses increase your risk of miscarriage and other complications , such as preterm delivery .
- Risk of ectopic pregnancy. Women who have difficulty getting pregnant and older women have an increased risk for ectopic pregnancy , and this can happen to those who conceive via IVF. An ectopic pregnancy occurs when an embryo implants in a fallopian tube or the abdominal cavity rather than in the uterus. Unfortunately, there's no way to save an ectopic pregnancy. Treatment involves medication or surgery to end the pregnancy.
- Risk of ovarian hyperstimulation syndrome (OHSS). OHSS can happen when women respond too well to fertility drugs and produce too many eggs. About 10 to 20% of women who take gonadotropins develop a mild form of OHSS, a condition marked by weight gain and a full, bloated feeling. Some also have shortness of breath, dizziness, pelvic pain, nausea, and vomiting. If you have OHSS, your ovaries swell to several times the normal size and produce fluid that accumulates in your abdominal cavity. Normally this resolves itself with careful monitoring by a physician and bed rest . But in rare cases, OHSS is severe and may be life-threatening. If this happens, you may have to be hospitalized for more intensive monitoring or treatment.
- Potential complications for the baby. Babies conceived via IVF may be more likely to be born prematurely or have a low birth weight (even if they're singletons). They may also have a slightly higher risk of birth defects . But experts aren't sure whether that's due to the factors that cause infertility (such as age) or infertility treatments.
- It may not work. Up to 20% of IVF cycles may be cancelled before eggs are retrieved, usually because not enough follicles developed. Even if the cycle isn't cancelled, the embryo may not successfully implant and develop.
In the United States, expect to spend an average of about $20,000 to $25,000 for one cycle of IVF, once you include evaluation, medication, bloodwork, egg retrieval, the transfer procedure, and follow-up care. (One cycle means one egg retrieval procedure and all the embryo transfers that result from that retrieval.)
IVF costs vary a great deal, though, depending on how much medicine you need, where you live, whether you have insurance coverage for fertility treatments, and whether you add specialized procedures. Many insurers don't cover assisted reproduction technology, which would mean you'd need to pay the entire cost up front.
Some insurers will cover part of the cost – say consultations and blood work, for example. Others may pay for everything but have a cap on the total expenditure.
Make sure you iron out your coverage with your insurer before you start the process. And keep in mind that you'll have to account for any unpaid time off, as well as travel and accommodation expenses if you travel to a clinic that's not close to home.
Learn more:
- Does sex selection work?
- Early signs of pregnancy
- What is an egg shower?
- Egg freezing
Was this article helpful?
What is a hysterosalpingogram (HSG) test?

Fertility drugs for men

What the first trimester feels like


Fertility treatment: Intrauterine insemination (IUI)

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
ACOG. 2020. Perinatal risks associated with assisted reproductive technology. Committee Opinion Number 671. The American College of Obstetricians and Gynecologists. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2016/09/perinatal-risks-associated-with-assisted-reproductive-technology Opens a new window [Accessed November 2023]
ASRM. 2021. Guidance on the limits to the number of embryos to transfer: A committee opinion. The Practice Committee of the American Society for Reproductive Medicine and the Practice Committee for the Society for Assisted Reproductive Technologies. Fertility and Sterility 116(3): 651-654. https://www.sciencedirect.com/science/article/pii/S001502822100563X Opens a new window [Accessed November 2023]
ASRM. 2016. Fertility drugs and cancer: A guideline. Fertility and Sterility 106(7): 1617-1626. https://pubmed.ncbi.nlm.nih.gov/27573989/ Opens a new window [Accessed November 2023]
ASRM. Undated. In vitro fertilization (IVF): What are the risks? ReproductiveFacts.org Opens a new window . American Society for Reproductive Medicine. https://www.sart.org/globalassets/_rf/news-and-publications/bookletsfact-sheets/english-pdf/in_vitro_fertilization_ivf_what_are_the_risks_factsheet.pdf Opens a new window [Accessed November 2023]
Barcroft JF et al. 2021. Fertility treatment and cancers – the eternal conundrum: A systematic review and meta-analysis. Human Reproduction 36(4): 1093-1107. https://pubmed.ncbi.nlm.nih.gov/33586777/ Opens a new window [Accessed November 2023]
CDC. 2023. ART success rates. U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/art/artdata/index.html Opens a new window [Accessed November 2023]
CDC. 2023. IVF success estimator. U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/art/ivf-success-estimator/index.html Opens a new window [Accessed November 2023]
Diakosavvas M et al. 2021. A potential pathogenic link between cancer of female reproductive system and infertile women treated with assisted reproduction Techniques. In Vivo 35: 1393-1399. https://iv.iiarjournals.org/content/invivo/35/3/1393.full.pdf Opens a new window [Accessed November 2023]
Reimundo P et al. 2021. Single-embryo transfer: A key strategy to reduce the risk for multiple pregnancy in assisted human reproduction. Advances in Laboratory Medicine 2(2): 179-188. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10197809/ Opens a new window [Accessed November 2023]
SART. Undated. ART: Step-by-step guide. Society for Assisted Reproductive Technology. https://www.sart.org/patients/a-patients-guide-to-assisted-reproductive-technology/general-information/art-step-by-step-guide/ Opens a new window [Accessed November 2023]
SART. 2020. Fertility data table. Final National Summary Report for 2020. Society for Reproductive Medicine. https://www.sartcorsonline.com/rptCSR_PublicMultYear.aspx Opens a new window [Accessed November 2023]
SART. 2020. Fertility data table. Preliminary National Summary Report for 2021. Society for Reproductive Medicine. https://www.sartcorsonline.com/rptCSR_PublicMultYear.aspx?reportingYear=2021 Opens a new window [Accessed November 2023]
SART. Undated. Frequently asked questions. Society for Assisted Reproductive Technology. https://www.sart.org/ivf-info/frequently-asked-questions/ Opens a new window [Accessed November 2023]
SART. Undated. Ovarian hyperstimulation syndrome. Society for Assisted Reproductive Technology. https://www.sart.org/patients/a-patients-guide-to-assisted-reproductive-technology/stimulation/ovarian-hyperstimulation-syndrome/ Opens a new window [Accessed November 2023]
UptoDate. 2023. In vitro fertilization: Overview of clinical issues and questions. https://www.uptodate.com/contents/in-vitro-fertilization-overview-of-clinical-issues-and-questions Opens a new window [Accessed November 2023]

Where to go next

What Is IVF? Here's Why People Choose It and How It Works
It's under the spotlight now, but in vitro fertilization is a health technology that's been around for decades.

- Added coconut oil to cheap coffee before keto made it cool.

The Alabama Supreme Court ruled (PDF) in February that embryos created through in vitro fertilization have the same legal rights as children , moving the national spotlight on a medical procedure many people use to become pregnant and grow their families.
Some fertility clinics in Alabama paused their services , out of new legal concern for the handling of embryos, though the state legislature has quickly moved to protect IVF providers . The wider effect on infertility services following the overturning of Roe v. Wade in 2022 remains to be seen.
IVF is the most common form of assisted reproductive technology , which describes the handling of eggs and embryos for fertility treatment. In a nutshell, IVF is the process of fertilizing an egg and sperm in a medical lab and then implanting the resulting embryo into someone's uterus, with the hope it will continue to develop into a successful pregnancy and baby.
A little more than 2% of all babies born in the US each year are conceived through IVF or a similar treatment, according to the US Centers for Disease Control and Prevention, and use of it has "more than doubled" in the last decade. But despite its growing popularity, IVF remains a complicated procedure, full of financial and sometimes emotional burden for hopeful parents. It also highlights the nuances of human reproduction, whether it be natural conception or conception assisted by a little bit of science.
"I think it's important for people to understand that we, as humans, are not that efficient with reproduction," Dr. Asima Ahmad, chief medical officer of Carrot Fertility , wrote in an email. Many embryos created in IVF will not make it to a live birth because they won't continue to grow, or they'll fail to implant into the uterus and continue as a pregnancy, for example.
"There are many things that have to align the right way for a live birth to occur," Ahmad said.
Read more: For These Personal Finance Influencers, Infertility Wasn't Part of the Plan
Why would someone need IVF?
People use IVF for many different reasons. These include instances of medical problems that make it difficult for someone to get pregnant naturally, saving childbearing for an age when pregnancy becomes more difficult, and the need for donor eggs or sperm to have a child.
In other cases, people may use IVF or freeze embryos to preserve their fertility if they have a medical procedure that can affect it, like cancer treatment, or if they're undergoing gender affirmation surgery.
How does IVF work?
Many steps go into IVF treatment -- one of the reasons why it's so expensive -- but it's basically taking a process that has traditionally occurred in the fallopian tube out into the world, with additional reproductive assistance from doctors and embryologists when required by the patient or doctor running the IVF procedure.
Here's how the process breaks down, according to information from NYU Langone , Johns Hopkins Medicine and Penn Medicine .
Step 1: Collect the eggs
In the month leading up to a natural conception, only one egg is released (sometimes two) during ovulation for potential fertilization and pregnancy. But when conception takes place outside the body, you need more eggs to work with, so you'll go through an egg retrieval.
Egg retrieval requires whoever is using their eggs for the pregnancy to be given a hormone injection that causes multiple eggs to mature instead of just one. (Many people who are using IVF will use their own eggs to become pregnant, but some patients may find an egg donor or even a surrogate to carry the pregnancy.)
To get the mature eggs from the ovary, you'll go through a process called follicular aspiration, where a very thin needle is guided through the vagina during an ultrasound. The device will suction out the eggs. You'll be given medication for this part. (Fun fact: Human egg cells are gigantic compared to the other cells in our body.)
How many times someone will need to go through egg retrieval depends on a few factors, including their reasons for infertility and their age. The number of healthy eggs your body releases declines with age, so an IVF patient in their 40s, for example, may need more eggs and cycles to have a chance at a successful pregnancy. But some people have higher or lower egg quality and quantity due to medical history or individual biology, as is true for sperm, or step No. 2.
Step 2: Collect the sperm
Because much of the sperm-production part of conception takes part outside the body, getting sperm for IVF is less medically involved than retrieving the eggs. Whoever is using their sperm in the pregnancy will probably be asked to abstain from ejaculating for a few days before the collection to ensure a higher sperm count, and most clinics prefer your sample be given in-office.
For those who don't produce sperm in their ejaculation, contributing to a case of infertility, sperm can sometimes be retrieved in a minor surgical procedure, similar in theory to egg retrieval. Whether you donate sperm before or after the egg donation will be up to your case and your doctor.
Step 3: Lab fertilizes the egg
Once you have eggs and sperm, the next step in IVF (and how the procedure gets its name) is the fertilization of the egg in a lab.
Quickly after the eggs have been retrieved, an embryologist will fertilize the eggs, either by letting a sperm find its own way to the egg, or by injecting a sperm cell directly into the egg (a process called intracytoplasmic sperm injection ). Whichever method is used for you will depend on your reasons for IVF or your lab.
Then, everyone waits. It takes about 18 hours to determine whether an egg has been successfully fertilized, and then a couple more days to see if the embryo is developing properly. In many cases, genetic testing of the embryos is done to determine its health or its likelihood of resulting in a baby.
Regardless of fertility status, not every fertilized egg will make it to a healthy embryo. Estimates on how many are lost during a natural conception seem to vary , but as many as one half of fertilized eggs are lost quickly after conception . During IVF, these early losses and failed conceptions are under a microscope, literally.
According to Ahmad, the chance of getting pregnant even in "the most fertile age range" is about 25% to 30% per cycle.
Step 4: Healthy embryo implanted into uterus
Once an embryo is selected and starts to develop, it will be transferred into a uterus for pregnancy to continue normally during a time in the menstrual cycle when the uterine lining can successfully receive it. This is a relatively short procedure where the embryo is released directly into the uterus, passing the cervix.
After some time , patients will know whether the embryo was able to successfully go through the " hatching " process of embed itself into the uterine lining, which then triggers someone's body to go into pregnancy mode , hopefully resulting in a baby nine months later.
Step 5: Remaining embryos stored if requested
The Alabama court case centered on embryos that were stored by patients at a fertility clinic.
People often have "extra" embryos if they went through the first parts of the IVF procedure and were able to become pregnant. If someone wants additional children in the future, they may keep those embryos frozen in a protective fluid with the use of liquid nitrogen for whenever they're ready to try to become pregnant again. The price of embryo storage varies based on the clinic, but may cost at least a few hundred dollars per year, according to an estimate by ReproTech.

Embryos are preserved and frozen using flash-freezing with liquid nitrogen to protect the embryos from forming ice crystals that could damage their cells, according to Johns Hopkins Medicine.
What happens when someone doesn't use their remaining embryos, or they're frozen for a while?
People may be left with stored or additional embryos they don't know what to do with, have more embryos left than they initially planned for, they're unable to go through pregnancy again for medical reasons, or they decide not to implant embryos that testing deemed genetically abnormal or those who don't have a good chance of resulting in a healthy pregnancy.
If embryos are not used or frozen, embryos are discarded as medical waste , or they're transferred into someone's womb during a time in the menstrual cycle when pregnancy wouldn't be possible . They can also be donated to science for research, and even to another person.
Whatever the choice, deciding the fate of remaining embryos created during IVF can be difficult for patients for a variety of reasons. The American Society for Reproductive Medicine, an organization in the field of reproductive science and medical practice, acknowledges the "ethical concerns" unused embryos pose for patients and the clinics that store them. The ASRM calls patient choice a "core value" of reproductive medicine and that patient wishes about their embryos should be "respected if practical and within legal limits." The legal limits of what you're able to do as a patient depend on state laws, as well as individual protocols at fertility clinics.
In general, patients have the wheel in deciding how to proceed in their IVF journey, according to Ahmad, which includes whether to only transfer "fresh" embryos and not store any (transferring frozen embryos may be recommended by physicians for different reasons, including a higher chance of pregnancy), and whether or not to do genetic testing. She notes that some fertility clinics may have individual protocols for freezing all embryos for testing or another reason, but choices in IVF should involve a risk-benefit discussion between patients and their doctors.
"Ultimately," Ahmad said, "the goal is for the best possible outcome for the patient."
Other Wellness Guides
- Best Places to Buy Glasses Online
- Best Places to Buy Contacts Online
- Best Prescription Sunglasses
- Best Place to Buy Replacement Prescription Lenses
- Best Blue Light Blocking Glasses
- Best Electric Toothbrush
- Best Invisible Braces
- Best Sunscreen
- Best Mattress
- Best Mattress for Back Pain
- Best Adjustable Mattress
- Purple Mattress
- Saatva Mattress
- Best Headphones for Sleeping
- Best Pillow
- Best Sheets
- Best Elliptical
- Best Treadmill
- Best Rowing Machine
- Best Peloton Alternative
- Best Adjustable Dumbbells
- Best Weightlifting Shoes
- Best Massage Gun
- Theragun Review
- Best Meal Kit Delivery Service
- Best Healthy Meal Delivery Service
- Best Cheap Meal Delivery Service
- Best Plant-Based Meal Delivery Service
- Best Keto Meal Delivery
- Best DNA Test
- Ancestry vs 23 and Me
- Best Continuous Glucose Monitors
- Best Blood Pressure Monitor
- Best Prescription Delivery Services
- Best Portable Humidifiers
- Best Mental Health Apps
- Best Teas for Stress and Anxiety
- Best Fidget Toys for Anxiety
- Best Online Therapy
- Amazon Promo Codes
- Air Up Coupons
About IVF Journey
Hello, I’m Lisa. A thirty-something year old on an IVF journey. Passionate about removing the stigma of infertility and supporting others who find themselves in a similar position.
1 in 6 people globally struggle to concieve, a whopping 17.5% of the adult population!…yet solutions for preventions, diagnosis and treatment remain underfunded and inaccessible.
Four years into the journey, I have learned many things that I believe will be valuable to others. The hope is that the words, tips, and research in this blog help you navigate the path to motherhood. Most importantly, I hope it helps you feel less alone xx
Recommended
11 insanely helpful ivf injection tips that every ivf warrior should know.
IVF injections…one of the necessary evils of the IVF process! Here’s the truth, …
5 Most Effective Ways to Manage IVF Weight Gain
Going through IVF is taxing on the body. If you’re …
The Most Important Things You Need To Know About IVF Egg Retrieval
Egg retrieval: a major step in your IVF journey! …
IVF Essentials
I have rounded up my tried and true IVF …
5 Things I Wish I Knew Before Starting IVF
There is a lot of clarity in hindsight. When …
Our Response to the Alabama IVF Ruling
« View All Posts
How Long Does the IVF Process Take? The Timeline From Start to Finish
August 22nd, 2023 | 12 min. read
By Christina Dias, RN, BSN

Navigating the complexities of IVF isn't easy, and the abundance of information you need to absorb might leave you feeling overwhelmed. In this comprehensive guide, we will explore how long the IVF process takes and what you need to know - every step of the way.
In this article: How long does the IVF process really take? Preparing for IVF Treatment 5 Things to Do Before Starting IVF Why Preconception Health is Essential The 4 Stages of an IVF Cycle What might make my IVF cycle take longer? How long does it take an embryo to implant after transfer? How long after embryo transfer will I know if I’m pregnant?
How long does the IVF process really take?
You’ve made the decision to seek the help of a fertility specialist – which is a huge step towards achieving your family-building goals. At this point, you are likely eager to get the process started, and may be wondering: how long will IVF treatment take from start to finish?
As Illume Fertility's Director of Nursing , with many years of fertility nursing experience, I'm here to break it all down for you and - hopefully - make it a little less intimidating.
Before we dive in, let's talk about some actionable steps you can take right now to prepare for fertility treatment . As any fertility patient will tell you, this stage of the process takes time - lots of communication, consultations, phone calls, and decisions happen well before you do your first injection.
While the IVF cycle itself only takes around 4 weeks, the full process (including your preconception health regimen and fertility testing) can take up to 4 months , from your initial consultation to when you have your first beta hCG test to see if you’re pregnant.
Preparing for IVF Treatment
To give you the absolute best chance at a successful IVF cycle and healthy pregnancy, we begin by performing a variety of tests that offer a full picture of your current fertility and overall health. Fertility treatment can begin only after initial fertility testing is completed.
This will involve a medical evaluation that looks at everything from any potential genetic issues to elevated thyroid or blood sugar levels. Certain medical conditions may warrant lifestyle modifications that will make it easier for you to conceive, which can add to your timeline, but make all the difference.
Fertility testing typically includes:
- Comprehensive blood work
- Genetic carrier screening
- Transvaginal ultrasound to assess ovarian reserve
- Evaluations of the uterine cavity (SHG) and fallopian tubes (HSG)
- Semen analysis and blood work for male partner, if applicable
Did you know? Male fertility issues account for up to 40% of infertility cases! That's why evaluating the quantity and quality of sperm is essential. As sperm is produced every 64 days, focusing on preconception health is important for a male partner as well.
5 Things to Do Before Starting IVF
- Schedule your initial consultation and learn more from your doctor
- Meet with a nutritionist to give your body the very best chance at success
- Meet with a counselor who can help prepare you for the road ahead
- Connect with other fertility patients through our virtual support groups , led by Illume Fertility's Patient Advocate, Lisa Rosenthal (who also offers free, one-on-one support)
- Download our 90-Day Preconception Checklist to stay on track
Why Preconception Health is Essential
To put it simply: a healthy body has the best chance of success.
Even small changes to nutrition and lifestyle in the period leading up to IVF can increase your odds of a healthy pregnancy. For this reason, the ideal time to start focusing on your preconception wellness is around three months before the start of an IVF cycle. We have developed an easy-to-reference 90-Day Preconception Checklist for this very purpose!
During this time, you should begin your physician-approved preconception health regimen, which will likely include taking prenatal vitamins , increasing your water intake, improving your sleep hygiene, and eating a balanced and nutritious diet .
Limiting alcohol and caffeine, stopping smoking, and incorporating low-impact exercise will also prepare your body for the rigors of fertility treatment and pregnancy.
Don't forget: Now is also the perfect time to identify your emotional support network as well as inquire about your insurance benefits . Your fertility doctor will also begin testing you for various risk factors.
Trying to conceive?
Increase your chances of a healthy pregnancy by downloading our free 3-month preconception checklist and learning what steps you can take.

The 4 Stages of an IVF Cycle
Once diagnostic testing is complete, your IVF cycle can finally begin!
You're likely feeling a lot of conflicting emotions right now, which is completely normal. Acknowledge all the hard work you've done to get to this point, and communicate any concerns to your team as you enter your treatment cycle. Here's what to expect:
Stage 1: Oral Contraceptives
Although it may seem counterintuitive, IVF patients must take oral contraceptives (birth control) for 10-14 days prior to beginning their fertility medication protocol.
When taken before ovarian stimulation, studies have shown that oral contraceptives can increase the number of eggs available for retrieval, ensure follicles grow as a cohesive group, and support ovarian health throughout IVF.
Stage 2: Ovarian Stimulation
After completing a course of oral contraceptives, you will begin injections of fertility medication for approximately 9-11 days . These medications consist of naturally occurring hormones that help develop and mature your follicles (eggs are contained within the follicles).
The number of follicles and their size determine how many mature eggs will be available for retrieval. During this time, you should plan to be in your fertility clinic's office approximately every other day for a transvaginal ultrasound and monitoring via blood work.
Stage 3: Egg Retrieval
Egg retrieval refers to a one-day procedure where the eggs are extracted from the ovarian follicles and then handed over to the IVF lab, where they will fertilize and divide.
At Illume Fertility , we monitor the growth of your embryos in our own onsite lab. A specially-trained embryologist cares for each embryo, watching it divide and multiply for five days, at which point they transition from the "zygote" stage to the "blastocyst" stage.
Did you know? Research supports that transferring embryos into the uterus at the blastocyst stage yields better results than transferring them on Day 3 (when they're still in the less mature zygote stage).
Stage 4: Embryo Transfer
After being closely monitored in the IVF lab, an embryo will be transferred back to the uterus on Day 5. ( Egg retrieval day is considered Day 0.) This is referred to as a "fresh" transfer. If you want to wait for any reason, your embryos can be safely cryopreserved until you're ready for a "frozen" embryo transfer.
Embryo transfer is also a one-day procedure that should take approximately 20 to 30 minutes . You will be awake for this painless procedure, and will not require any anesthesia.
Following this is a waiting period to see if the embryo implants in the uterus, which typically takes 9-10 days, depending on the maturity of the embryo at the time of transfer.
What might make my IVF cycle take longer?
You've worked so hard to get to this point, and any delays in the process can feel incredibly frustrating. If your IVF cycle was delayed or cancelled (or is taking longer than expected), it's understandable to want to know why this could have happened.
Here are the three most common reasons:
#1 Poor Ovarian Response
Sometimes the body doesn’t respond as expected to IVF medications , which can delay or cancel your IVF cycle. For example, there might be a delay or cancellation if a lower number of follicles develop in the ovaries than expected, meaning fewer eggs were produced.
#2 Suboptimal Hormone Levels
Sometimes hormone levels are not ideal for continuing an IVF cycle , and delaying can actually lead to better odds of success in your next cycle.
Although this can be difficult news to receive, remember that every cycle is diagnostic, as well as therapeutic. Your fertility doctor will gain important knowledge about your body and how it responds to medication throughout each cycle, increasing your chances of success for the next one.
Remember: A poor hormonal response from this round of IVF does not mean you'll have the same fate should you decide to continue with IVF treatments . Sometimes, it just takes a little time to figure out the right protocol for your body.
Reason #3: Embryo Screening
Another reason your IVF cycle might take longer than expected is if you opt to have your embryos undergo genetic testing before transfer. This can add 4-5 weeks to the process.
Preimplantation genetic testing (PGT) can offer the highest degree of certainty for a genetically healthy child, particularly when partners are known carriers or at higher risk for passing on genetic diseases.
Whatever the reason, we understand that delays can be challenging and upsetting. Should there be a delay or cancellation, your doctor will carefully review your case and make necessary adjustments - providing support and information every step of the way.
Want our full IVF guide?
Grab our comprehensive guide to IVF to learn about how much it costs, where to find resources, and how it all works.

IVF Treatment FAQs
Have more questions about the IVF process? We've got answers!
Do I need preauthorization for IVF?
The cost of IVF is an unfortunate roadblock for the majority of people seeking treatment. The good news? An increasing number of companies offer fertility benefits, and some states even have mandated fertility coverage . (If you don't have insurance, read our guide to paying for IVF with the help of other resources, like grants, scholarships, and loans.)
Many insurance companies also provide benefits for fertility testing and procedures, though coverage varies by state and employer. Depending on the type of insurance plan you have, your policy may require that you obtain referrals or authorizations.
Beyond a simple phone call to your insurance company, we suggest requesting a written predetermination letter that outlines your fertility benefits and clarifies any specific requirements that must be met for you to be covered.
This step might be necessary for both you and your partner if you carry individual insurance. To avoid delays, seek out this information as soon as IVF becomes a consideration.
Knowing how stressful this process can be, Illume Fertility appoints you a designated Insurance & Billing Advocate to help communicate with your insurance company and understand your coverage. They will help determine your benefits, outline any out-of-pocket expenses, and review specific plan details to eliminate surprises along the way.
Why do I have to start IVF the month before my egg retrieval?
An IVF cycle corresponds with the length of a normal ovulation cycle, which is about a month long. Ovulation occurs when a mature egg is released from the ovary and "pushed" into the fallopian tube where it can be fertilized, or in the case of IVF - retrieved.
The goal of IVF is to prepare and stimulate the ovaries to produce many mature eggs for retrieval and ready your uterus for implantation. Ovarian preparation and stimulation occur at the start of and during the ovulation cycle.
How long does it take an embryo to implant after transfer?
Depending on the maturity of the embryo, it can take between 1-5 days after the transfer for the embryo to nestle into the uterine lining and successfully implant.
How long after embryo transfer will I know if I’m pregnant?
Waiting to learn if your IVF cycle was a success can be the hardest part of treatment, and it's tempting to take at-home pregnancy tests! However, it's important to know that at-home tests simply won’t be reliable if taken too early, so stay strong during that " two-week wait ."
To detect actual amounts of human chorionic gonadotropin (hCG), the hormone produced by the placenta after implantation, an in-office pregnancy blood test is performed around 9-10 days after embryo transfer .
We encourage you to practice good self care, connect with others in the same boat, and reach out for support during this often challenging waiting period!
Your IVF Experience
Remember that everyone's journey is unique.
Try not to compare your situation to anyone else's - even if they seem similar. What works for one IVF patient may not work for you. Be patient, stay connected to your team, reach out for support, and don't be afraid to ask questions. They're there to help!
We at Illume Fertility wish you all the luck on your path to parenthood, and hope this guide to the IVF process helps you feel as prepared as possible for the journey ahead.
Christina Dias, RN, BSN
Christina Dias, RN, BSN joined the team at Illume Fertility in 2004. She currently serves as our Director of Nursing, overseeing our clinical care teams. She received her Bachelor of Science in Nursing from Sacred Heart University.
No fertility coverage?
There are other ways to afford IVF treatment! Explore your options with our helpful guide.

More Fertility Resources
A twin pregnancy after years of loss & infertility | kate & mike's story.
April 26th, 2024 9 min read
Two Sets of Fraternal Twins in Three Years | Dionicio & Ruddy's Story
April 25th, 2024 8 min read
Finally Pregnant at 49: How IVF Made My Dream a Reality | Alicia's Story
April 22nd, 2024 10 min read
Trying to Conceive With a Unicornuate Uterus | Brittany's Story
April 20th, 2024 8 min read
Choosing Single Motherhood | Kaitlyn's Story
April 19th, 2024 8 min read
Our Journey to IVF Identical Twins | Christa & Aland's Story
March 27th, 2024 9 min read
23 IVF Questions to Ask a Fertility Doctor at Your First Appointment
March 20th, 2024 16 min read
Braving Recurrent Pregnancy Loss & Endometriosis | Katie's Story
March 14th, 2024 8 min read
Illume Fertility Joins the Fight to Protect IVF After Alabama Ruling
March 4th, 2024 17 min read
What Are My Chances of Success with Fertility Treatment?
February 27th, 2024 16 min read
We Don't Speak About Infertility | Shiraine's Story
February 22nd, 2024 11 min read
IVF Success After Endometriosis | Nicole's Story
February 21st, 2024 6 min read
$20,000 IVF Grants Offered to Local Families by Nest Egg Foundation
January 15th, 2024 9 min read
How Years of Infertility Led to Two Miracles | Deanna & Justin's Story
December 14th, 2023 11 min read
The Ultimate IVF Gift Guide for Fertility Warriors
December 5th, 2023 9 min read
How IVF and Genetic Testing Can Help Prevent Sickle Cell Anemia
November 29th, 2023 10 min read
From Injections to Self-Reflections: Your IVF Medication Breakdown
November 27th, 2023 13 min read
How to Pay for IVF Treatment Without Insurance
November 10th, 2023 12 min read
From Unexplained Fertility to IVF Success | Juliana & Ryan's Story
November 8th, 2023 9 min read
Becoming a Mother After Recurrent Pregnancy Loss | Alyson's IVF Story
October 25th, 2023 8 min read
Becoming a Mother After Surviving Breast Cancer | Erin's Story
October 18th, 2023 8 min read
IVF Success Stories: 44 Parents Share Their Family-Building Journeys
October 11th, 2023 14 min read
Overcoming Obstacles to Meet Our Miracle Baby | Kristen & Jeff's Story
September 15th, 2023 6 min read
In Vitro Fertilization (IVF) Step-By-Step Guide from a Fertility Nurse
August 16th, 2023 14 min read
- --> EN --> | --> AR -->