- Log In Username Enter your ACP Online username. Password Enter the password that accompanies your username. Remember me Forget your username or password ?
- Privacy Policy
- Career Connection
- Member Forums
© Copyright 2024 American College of Physicians, Inc. All Rights Reserved. 190 North Independence Mall West, Philadelphia, PA 19106-1572 800-ACP-1915 (800-227-1915) or 215-351-2600
If you are unable to login, please try clearing your cookies . We apologize for the inconvenience.

Video Visits Billing, Coding and Regulations Information
Many patients have utilized telemedicine for medical care during the COVID pandemic and will continue to seek this option going forward. These resources will help refine and improve your delivery of virtual care, and practical implementation tips are offered below.
E/M and Other Medicare Allowed Services
This is a list of eligible CPT/HCPCS codes .
- Use POS code 10 for telehealth services provided in the patient's home - The location where health services and health related services are provided or received, through telecommunication technology. Patient is located in their home (which is a location other than a hospital or other facility where the patient receives care in a private residence) when receiving health services or health related services through telecommunication technology. (This code is effective January 1, 2022, and available to Medicare April 1, 2022.)
- Use POS 02 for telehealth services provided other than in patient's home - The location where health services and health related services are provided or received, through telecommunication technology. Patient is not located in their home when receiving health services or health related services through telecommunication technology. (Description change effective January 1, 2022, and applicable for Medicare April 1, 2022.)
- Modifier -95 should not be used with virtual check-ins (G2012) or the digital evaluations (99421-99423). It is for use with all other telehealth codes that use synchronous telemedicine service rendered via a real-time interactive audio and video telecommunications system.
- During the current PHE, telehealth E/M levels can be based on Medical Decision Making (MDM) OR time (total time associated with the E/M on the day of the encounter). Likewise, CMS has also removed any requirements regarding documentation of history and/or physical exam in the medical record for Telehealth visits.
- -GQ: Clinicians participating in the federal telemedicine demonstration programs in Alaska or Hawaii must submit the appropriate CPT or HCPCS code for the professional service along with the modifier GQ, “via asynchronous telecommunications system.”
- -GO: Use of telehealth for purposes of diagnosing stroke.
- Note: Medicare stopped the use of modifier -GT in 2017 when the place of service code 02 (telehealth) was introduced. However, private payer may still be using the modifier -GT.
Virtual Check-In
This is a set of telehealth-specific codes for the following use-cases:
- Any chronic patient who needs to be assessed as to whether an office visit is needed.
- Patients being treated for opioid and other substance-use disorders.
- Can be any real-time audio (telephone), or "2-way audio interactions that are enhanced with video or other kinds of data transmission."
- Nurse or other staff member cannot provide this service. It must be a clinician who can bill E&M services.
- If an E&M service is provided within the defined time frames, then the virtual check-in is bundled in that E&M service. It would be considered pre- or post-visit time of the associated E&M service and thus not separately billable.
- Should be initiated by the patient since a copay is required. Verbal consent to bill and documentation is required.
- No modifier needed as these are technology based codes.
Online Digital Evaluation and Management (E/M)
Telehealth-specific codes for the following use-cases:
- Given the temporary approval of E/M visits via telehealth, these online codes would primarily be used for patient interactions via a portal.
- Can be done synchronously and asynchronously and audio/video phone can be used (but not a traditional telephone).
- The patient can initiate a virtual check-in, the practice can let the patient know about their options. If the patient calls back within 7 days, then the time from the virtual check-in can be added to the digital E/M code and only the digital E/M code is billed.
- If the patient initiates a call to the physician office this would qualify for the remote check-in code (G2012), the time for the remote (virtual) check-in can be counted toward 99421-3 only if and when the patient calls back, so it is important to document the time. (See CPT book for further details regarding when the 7 days begins, how to count time, which “qualified non-physician health professionals” it applies to, and other documentation requirements.)
- Must be patient initiated.
- Cost sharing applies.
- Use only once per 7-day period. If the patient presents a new, unrelated problem during the 7-day period of an online digital E/M service, then the time is added to the cumulative service time for that 7-day period.
- Clinical staff time is not calculated as part of cumulative time.
- Service time must be more than 5 minutes.
- Do not count time otherwise reported with other services.
- Do not report on a day when the physician or other qualified health care professional reports other E/M services.
- Do not report when billing remote monitoring, CCM, TCM, care plan oversight, and codes for supervision of patient in home, domiciliary or rest home etc. for the same communication[s]).
- Do not report for home and outpatient INR monitoring when reporting 93792, 93793.
Private Payer and State Policies
Many states have issued their own public health emergencies, and some have ended theirs, which results in changes to Medicaid, private payer, and licensure for telehealth.
- The Center for Connected Health Policy (CCHP) is an excellent resource to keep up with state regulations and has two toolkits that track COVID-19 Telehealth Coverage Policies and COVID-19 Related State Actions , which include Medicaid clarification, waivers, and telehealth guidance, prescription and consent waivers, private payer requirements, and cross-state licensing.
- The Alliance for Connected Care also has a chart showing state changes to licensure, coverage, and other changes during COVID-19.
- Full listing of all blanket waivers and flexibilities related to provider enrollment, telehealth, 1135 waivers, and other changes resulting from the COVID-19 public health emergency.
Other Resources
Many Medicare restrictions related to virtual visits have been lifted during the COVID public health emergency. ACP will update this information when the federal PHE ends. Some states have already ended their PHE.
Medicare policies during the emergency:
- Patients can be at home and non-HIPAA compliant communication technology is allowed.
- Practices are allowed to waive cost sharing (copays and deductibles) for all telehealth services All E/M and other services that are currently eligible under the Medicare telehealth reimbursement policies are included in this waiver. This is a list of eligible CPT/HCPCS codes , including which codes are allowed to use audio-only telephone.
- New or established patients.
- Rural and site limitations are removed.
- CMS has issued additional guidance regarding flexibilities specific to FQHCs and RHCs.
- Informed Consent for Telehealth: Although it is not always required, it is important that patients understand the risks and benefits of using telehealth. AHRQ has a simple, customizable consent form and how-to guidance for clinicians on how to explain telehealth. Document verbal consent prior to each telehealth visit until you can receive a signed consent (either digitally or on paper) from the patient.
Coding Q&A: Coding telehealth services and virtual visits
by Stephanie Dybul, MBA, RT, FSIR
July 12, 2020
What are the CPT codes for a virtual video telehealth visit?
A virtual video visit is reported with the same CPT codes that you would use for in-person visits ( 99201 – 99205 new patient visit ; 99211 – 99215 established patient visit ; or 99241 – 99245 consultation visit [not recognized by CMS, see G-codes]). The service should be reported with a - 95 modifier (confirm your local payer rules). There must be a synchronous two-way audio and visual component to the visit in order to report using these standard codes. Additionally, it should be noted that the place of service (POS) listed on the claim should match wherever the intended POS would have been in normal circumstances. For example, if you typically perform your clinic visit in an on-campus, OP hospital setting, report POS 22 for facility or POS 11 for nonfacility/office setting . Currently, telehealth services are reimbursed under the CMS Physician Fee Schedule at the same amount as in-person services.
Are there any special documentation requirements for virtual video visit?
You should document all of the same elements that you would normally, with consideration of what is possible for you to achieve via the video connection. Typical elements of past medical history can be taken, limited examinations can be performed and documentation of your medical decision making (MDM) or time spent counseling should be clearly stated. However, CMS is removing requirements regarding documentation of history and/or physical exam in the medical record. Additionally, it should be noted that, on an interim basis, CMS is revising their policy to specify that the outpatient E&M level selection for these services when furnished via telehealth can be based on MDM or time, with time defined as all of the time associated with the E&M on the day of the encounter. It remains CMS’ expectation that providers will document E&M visits as necessary to ensure quality and continuity of care. These policy changes only apply to office/outpatient visits furnished via Medicare telehealth, and only during the Public Health Emergency (PHE) for the COVID-19 pandemic. It is strongly recommended to work with your coding/compliance team to ensure that language required by all payers is included in the documentation to ensure timely payment.
Can I bill an E&M service for telephone calls to patients?
Yes, there are CPT codes to support telephone E&M service, with the understanding that two-way audio-visual technology may not be available. Briefly, they are described as follows (see CPT® for full descriptors):
99441 : Telephone E&M, for an established patient, 5–10 minutes
99442 : Telephone E&M, for an established patient, 11–20 minutes
99443 : Telephone E&M, for an established patient, over 21 minutes
These codes are only reportable when providing E&M services to an established patient and cannot be reported within 7 days of a previously provided E&M service or within 24 hours of a procedure. During the PHE, CMS has established that these codes can be used for new patients.
Is responding to a patient’s electronic message billable?
Yes, CPT codes 99421 – 99423 can be used when a provider responds to a patient generated electronic inquiry. These E&M services do not use interactive audio or visual. As with other non-face-to-face E&M services, the codes are time based and are cumulative over a 7-day period; which begins when the provider reviews the initial patient generated inquiry. The time includes review of patient’s medical records, the time to perform medical decision-making, develop a plan and place orders, as well as the time for communication back to the patient. Permanent documentation should support the time and effort taken, including documentation of the time in minutes spent performing these activities. The codes may not be used for work done by clinical staff and should not be billed if/when other E&M services are provided within the past 7 days. During the PHE, these codes can be used for new patients or established patients.
99421 : Online digital E&M service, for an established patient, for up to 7 days cumulative time during the 7 days; 5 – 10 minutes
99422 : Online digital E&M service, for an established patient, for up to 7 days cumulative time during the 7 days; 11 – 20 minutes
99423 : Online digital E&M service, for an established patient, for up to 7 days cumulative time during the 7 days; 21 or more minutes
Disclaimer: SIR is providing this billing and coding guide for educational and information purposes only. It is not intended to provide legal, medical or any other kind of advice. The guide is meant to be an adjunct to the American Medical Association’s (AMA’s) Current Procedural Terminology (2020/CPT ® ). It is not comprehensive and does not replace CPT. Our intent is to assist physicians, business managers and coders. Therefore, a precise knowledge of the definitions of the CPT descriptors and the appropriate services associated with each code is mandatory for proper coding of physician service.
Every reasonable effort has been made to ensure the accuracy of this guide; but SIR and its employees, agents, officers and directors make no representation, warranty or guarantee that the information provided is error-free or that the use of this guide will prevent differences of opinion or disputes with payers. The publication is provided “as is” without warranty of any kind, either expressed or implied, including, but not limited to, implied warranties or merchantability and fitness for a particular purpose. The company will bear no responsibility or liability for the results or consequences of the use of this manual. The ultimate responsibility for correct use of the Medicare and AMA CPT billing coding system lies with the user. SIR assumes no liability, legal, financial or otherwise for physicians or other entities who utilize the information in this guide in a manner inconsistent with the coverage and payment policies of any payers, including but not limited to Medicare or any Medicare contractors, to which the physician or other entity has submitted claims for the reimbursement of services performed by the physician.
*The content and guidance described in this article was current at the time it was written. Due to the nature of the recent PHE, payment policy is likely to change rapidly and may vary geographically. Members should continue to follow and consult local/national payer guidelines for most up-to-date guidance. Also refer to SIR’s telehealth information within the COVID-19 Toolkit: bit.ly/2YcQz4u .
- Privacy policy
2024 The Society of Interventional Radiology. All rights reserved.

Contact | Patient Info | Foundation | AASM Engage JOIN Today Login with CSICloud
- AASM Scoring Manual
- Artificial Intelligence
- COVID-19 Resources
- EHR Integration
- Emerging Technology
- Patient Information
- Practice Promotion Resources
- Provider Fact Sheets
- #SleepTechnology
- Telemedicine

- Annual Meeting
- Career Center
- Case Study of the Month
- Change Agents Submission Winners
- Compensation Survey
- Conference Support
- Continuing Medical Education (CME)
- Maintenance of Certification (MOC)
- State Sleep Societies
- Talking Sleep Podcast
- Young Investigators Research Forum (YIRF)

- Leadership Election
- Board Nomination Process
- Membership Directory
- Volunteer Opportunities
- International Assembly

- Accreditation News
- Accreditation Verification
- Program Changes

AASM accreditation demonstrates a sleep medicine provider’s commitment to high quality, patient-centered care through adherence to these standards.
- AASM Social Media Ambassador
- Advertising
- Affiliated Sites
- Autoscoring Certification
- Diversity, Equity and Inclusion
- Event Code of Conduct Policy
- Guiding Principles for Industry Support
- CMSS Financial Disclosure
- IEP Sponsors
- Industry Programs
- Newsletters
- Patient Advocacy Roundtable
- President’s Report
- Social Media
- Strategic Plan
- Working at AASM
- Practice Standards
- Coding and Reimbursement
- Choose Sleep
- Advanced Practice Registered Nurses and Physician Assistants (APRN PA)
- Accredited Sleep Technologist Education Program (A-STEP)
- Inter-scorer Reliability (ISR)
- Coding Education Program (A-CEP)
- Individual Member – Benefits
- Individual Member – Categories
- Members-Only Resources
- Apply for AASM Fellow
- Individual Member – FAQs
- Facility Member – Benefits
- Facility Member – FAQs
- Sleep Team Assemblies
- Types of Accreditation
- Choose AASM Accreditation
- Special Application Types
- Apply or Renew
Telemedicine Codes
Telemedicine and telehealth are used interchangeably throughout the United States healthcare system, in reference to the exchange of medical information from one site to another through electronic communication. Reporting of telemedicine/telehealth services varies by payer and state regulations.
AASM Telemedicine/Telehealth Resources
- AASM Coding FAQs
- AASM Telemedicine Video Library
CMS Telemedicine/Telehealth Codes
The codes below are commonly reported for Medicare patients:
CMS finalized the creation of two additional G codes that can be billed by practitioners who cannot independently bill for E/M services. G2250 and G2251 are billable by certain non-physician practitioners, consistent with the scope of these practitioners’ benefit categories.
CPT Telemedicine Codes
Modifier 95 indicates a synchronous telemedicine service rendered via a real-time interactive audio and video telecommunications system. The 2020 CPT® manual includes Appendix P, which lists a summary of CPT codes that may be used for reporting synchronous (real-time) telemedicine services when appended by modifier 95. Procedures on this list involve electronic communication using interactive telecommunications equipment that includes, at a minimum, audio and video.
HCPCS LEVEL II CODES
There are also HCPCS Level II codes that describe telemedicine services.
Place of Service (POS) Code for Telemedicine
On January 1, 2017 the Center for Medicare and Medicaid Services (CMS) introduced place of service (POS) code 02 to identify telemedicine services. The descriptor for POS code 02 is “The location where health services and health related services are provided or received, through telecommunication technology.” Use of the telehealth POS code certifies that the service meets all of the telehealth requirements. Many private payers have also begun requiring use of POS code 02 for telemedicine services.
GT/GQ Modifiers
Medicare previously required providers to submit claims for telehealth services using the appropriate procedure code along with the telehealth GT modifier (“via interactive audio and video telecommunications systems”) or GQ modifier (“via an asynchronous (delayed communications) telecommunications system”). As of January 1, 2018, the GT modifier is only allowed on institutional claims billed under Critical Access Hospital (CAH) Method II since institutional claims do not use a POS code. If the GT modifier is billed by other provider types, the claim line will be rejected. The GQ modifier is still required when applicable (e.g., for those providers participating in the Alaska or Hawaii federal telemedicine demonstration programs).
Additional CMS Telemedicine/Telehealth Resources
- Complete list of CMS Telehealth Services
- General Provider Telehealth and Telemedicine Toolkit
- Medicare Telehealth Frequently Asked Questions (FAQs)
- Medicare Telehealth Services
Note: CPT Copyright 2021 American Medical Association. All rights reserved. CPT® is a registered trademark of the American Medical Association.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Springer Nature - PMC COVID-19 Collection

Coding Telemedicine Visits for Proper Reimbursement
Gary n. gross.
Internal Medicine, Southwestern Medical Center, University of Texas, Dallas, TX USA
Purpose of Review
Coding for patient visits and monitoring via telehealth have expanded over the past years with a wide acceptance of telemedicine as a consequence of the coronavirus pandemic. Coding topics of interest to the allergist/immunologist in regard to services provided via telemedicine will be of increasing importance in the coming years.
Recent Findings
CPT coding for telephone as well as synchronous face-to-face telehealth visits has changed over the past few years. With the need for distancing and patient protection during the coronavirus pandemic, telehealth services have increased dramatically. The introduction of newer devices to remotely monitor patients will increase and be incorporated into patient care.
This review will summarize current codes available for designating what services have been provided. The area of telemedicine is changing and will continue to evolve as other platforms for visits are designed and other methods of monitoring patients become available. Coding for these services will be an ongoing need for the provider.
Introduction
Current procedural terminology (CPT) has recognized the need for designations of procedures done using technology. Although initial codes focused primarily on telephone visits, in 2017, CPT recognized a new place-of-service (POS) code designating “The location where health services and health related services are provided or received, through a telecommunication system.” This POS “02” was a step forward in awareness of the need for distant patient encounters and procedures. Further codes for both monitoring and evaluating via telehealth will be discussed. Table Table1 1 lists current CPT codes available for designating services provided.
Current CPT codes [ 1 ]
Telehealth Coding
Two words must be remembered whenever coding is discussed. The two words, “it depends,” define the lack of consistency in coding throughout the industry. Coding is generally driven by The Centers for Medicare & Medicaid Services (CMS) and CPT (although they do not always align). CPT codes exist for procedures, but some carriers may not recognize or reimburse for the codes [ 2 ]. Some carriers may create their own limits on reimbursing for codes, arbitrarily considering procedures bundled with evaluation and maintenance (E&M) visits. Codes may be paid for certain disease states but not for others. Insurers vary with regard to expectations of what place-of-service to use or how to bill for some procedures. New modifiers for telehealth visits further complicate billing. The modifiers –GT and -95 are used by some carriers for telehealth visits and vary depending on the insurer. Similarly, place of service may be either “02,” the telecommunication POS mentioned above, or remain “11” which designates the office location. Therefore, one must be flexible and informed. Keeping track of each carrier’s latest provider information and appealing denials with alternative codes may be necessary.
As with conventional patient encounters, documentation is key. For telehealth visits, there is also the need to document the patient’s consent for the encounter via telehealth. Most of the telehealth codes are for providers who could bill for evaluation and management (E/M) services such as physicians, physician assistants (PAs), and nurse practitioners (NPs). These providers are considered qualified healthcare providers (QHP).
Non-face-to-face Telehealth Patient Visits
Telephone services (99441–99443).
These codes are non-face-to-face E/M services used by QHP. They are designed for telephone calls initiated by an established patient and have certain restrictions. If the call includes the decision to see the patient in the next 24 h or next available urgent appointment, it cannot be billed. Similarly, if the call refers to an E/M service reported by the QHP within the past 7 days, the telephone codes cannot be used. Thus, these calls are initiated by the patient or guardian of the patient and stand apart from other E/M visits as described.
- 99441 - 5–10 min of medical discussion
- 99442 - 11–20 min of medical discussion
- 99442 - 11–30 min of medical discussion
An established patient, who has not been seen in the past month, calls the office because of a recent ant bite. The patient wants to speak to the physician since the physician also treats the son for anaphylaxis to wasps and the patient is concerned. The physician talks to the patient about the kinds of reactions that might occur and notifies him of what symptoms he should be aware of. Out of an abundance of caution, the physician reminds the patient about using an epinephrine autoinjector. The conversation takes 25 min. The staff calls in the autoinjector to the pharmacy and is on the phone for 15 min waiting for the pharmacist.
The patient is billed 99443 for the physician time. The staff time would not enter into the total time. The note in the chart would document that the visit was via telephone and that the patient called the clinic about the problem. The discussion would be documented and the note would indicate the patient had not been seen and no E/M visit was anticipated. The note would also indicate that 25 min was spent in discussion.
Online Digital Evaluation and Management Services (99421–99423)
These codes are electronic communication codes. The problem may be new to the physician or QHP but the patient must be established. These services are patient-initiated through HIPAA-compliant secure platforms or portals.
These services include evaluation, assessment, and management of the patient.
These services are reported once during a 7-day period and therefore time is cumulative.
The time includes (1) review of the initial inquiry, (2) review of patient records or data pertinent to assessment of the patient’s problem, (3) interaction with clinical staff focused on the patient’s problem and development of management plans, (4) physician or other QHP generation of prescriptions or ordering of tests, and (5) subsequent communication with the patient through online, telephone, email, or other digitally supported communication, which does not otherwise represent a separately reported E/M service.
These services require permanent documentation storage (electronic or hard copy) of the encounter.
If within 7 days of the initial patient-initiated contact a separate E/M visit (in person or synchronous telemedicine) occurs, then the Online Digital visit is not billed but the time is incorporated into the subsequent E/M visit. If the Online Digital visit is initiated within 7 days of a previous E/M visit for the same or related problem, the Online Digital visit is not reported. If a new or different problem is being addressed in the Online Digital visit, then the visit is billable and should be reported.
- 99421-5–10 min (over a 7-day period)
- 99422-11–20 min (over a 7-day period)
- 99423-21 or more minutes (over a 7-day period)
Remember that only physician or other QHP time is used in the calculation. Staff time is not included.
An established patient who was seen 3 days ago for allergic rhinitis wakes up with hives. She uses the practice’s HIPAA compliant portal to message her doctor about the hives. The PA responds to the message and gathers information about the hives, the patient’s activities, and ultimately prescribes an antihistamine. The encounter takes 10 min. Two days later, the patient messages again saying the hives are better but not gone. She wants stronger medicine. The PA responds to the message and offers to prescribe a short course of corticosteroids. The PA describes the possible side effects of the steroids and also tells the patient what should be done if the hives do not clear. The PA spends 12 min with the encounter. The patient does not call back and does not come to the office for the hives. The PA bills the patient 99423 since the sum of the two encounters was 22 min within a 7-day period and the hives were not related to the allergic rhinitis the patient had been seen for 3 days before the hives.
The chart would document that the patient contacted the clinic for a new problem. All time spent by the PA would be documented to support the total time billed. It would be documented that no E/M visit was anticipated for this new problem.
Healthcare Common Procedure Coding System (HCPCS) have 2 levels of commonly used codes. Level 1 codes are CPT codes and level 2 codes are alphanumeric codes. One group of HCPCS codes are “G codes.” The G codes are used to identify professional healthcare procedures and services that would otherwise be coded in CPT but for which there are no CPT codes. Two “G codes” are relevant to telehealth and do not yet have matching CPT codes [ 3 ].
was in the 2019 physician fee schedule and is used for remote evaluation of established patient’s submitted videos or still images. The purpose of the evaluation is to determine whether or not an E/M visit is necessary. It may be billed if the evaluation does not lead to an E/M visit and does not occur within 7 days of a previous E/M visit. To bill for the evaluation, the physician or other QHP must evaluate the image within 24 business hours and follow-up with the patient in the form of a 5–10 min discussion with the patient.
An established patient develops a rash and is uncertain about its cause. The patient sends the physician a picture of the rash. The physician evaluates the photo and determines it is a hive. The physician calls the patient and tells him that these are common and if they last more than 6 weeks or get worse he can check back, but that he does not need to have an E/M visit.
Documentation of this remote evaluation would include the picture in the chart and the provider’s note that the picture was viewed and that no visit would be necessary unless the hives lasted more than 6 weeks. The presumed diagnosis of acute urticaria would also be included.
was also included in the 2019 physician fee schedule. It has been referred to as a “virtual check-in.” It is considered to be a call or video check in to see if an E/M visit is needed. Similar to some other e-codes, it cannot be billed if there was a related E/M service within the previous 7 days or it leads to an E/M visit within the next 24 h or soonest available appointment. The code is used for established patients having direct interaction with the billing practitioner (not the staff). The service must be medically reasonable and necessary but there is no limitation on frequency. The code assumes 5–10 min of medical discussion.
An established patient calls the nurse practitioner and describes a large, local reaction they have from a mosquito bite. The patient wants to know if they need to come in or go to the ER. The nurse practitioner informs the patient about the type of reaction and tells the patient they only need to come in if they have trouble breathing or if the reaction spreads. The patient is reassured and watches the reaction as it gradually goes away. The practitioner can bill G2012.
The documentation for this virtual check in would include the main points of discussion including the bite and the likely diagnosis as well as the 5+ min the provider is on the platform talking with the patient.
Face-to-face Telehealth Patient Visits
The Centers for Medicare & Medicaid Services (CMS) defines telehealth services to include those services that require a face-to-face meeting with the patient. These are visits commonly considered “office visits” but delivered via synchronous audio and video contact with the patient. The usual E/M visit codes (99201–99215) would apply.
Prior to 2021, these E/M visits level of service was determined by history, physical exam, and medical decision-making as documented in the CPT book each year. If more than 50% of the face-to-face time with the patient and/or family was used in counseling and/or coordination of care, time becomes the key factor in determining level of service.
Beginning with CPT 2021, time alone may be used to select the appropriate level for the office or other outpatient E/M services codes (99202, 99203, 99204, 99205, 99212, 99213, 99214, 99215). This “time” requires a face-to-face encounter with the physician or other QHP. Time spent with staff such as registering in the office or making future appointments is not used in the calculation of time. Also, note that the new patient level one code (99201) has been deleted.
Medical decision-making (MDM) includes establishing diagnoses, assessing the status of a condition, and/or selecting a management option. Beginning in 2021, MDM may be used independently in establishing a level of service (without consideration of history or physical exam as was required previously). These changes were designed to reduce duplication and unnecessary, repetitious documentation, and should also make coding for telehealth E/M visits easier.
The telemedicine E/M visits are coded just as an in-office E/M visit would be but possibly with the addition of a modifier or a different place of service code depending on the insurance company. Some provisions for telemedicine have been waived during the pandemic to allow more patients access to medical care and to avoid exposure to others in waiting rooms and offices. The telemedicine waivers include evaluation of new patients via telehealth, beneficiaries living in any geographic area and accessing telemedicine from their homes, and use of smartphones and audio only connections for some services. Whether all these waivers will remain in place following the pandemic is unknown.
An established patient calls the office to set up an appointment and is offered a telemedicine option. The patient finds this attractive since it will save him time in traffic and reduce his time away from work. It is for a follow-up to see how he is doing after starting immunotherapy a month ago. The patient signs into the doctor’s telehealth platform and gives verbal consent for the visit. They discuss symptoms, reactions to injections, medications, and concerns of the patient regarding future injections if he goes on vacation. The face-to-face time with the physician is 22 min and the code billed is 99213 (less than the minutes currently typical for 99214 and within the 20–29 min designated for 2021).
These telemedicine visits will require documentation similar to in-person visits. They will include the notation that the patient consents to the telehealth visit. Since the visits for new patients require physical examinations, the best way to document and bill these visits will be based on time. Until 2021, the notation that over 50% of the time with the patient was related to counseling and/or coordination of care is also needed. For follow-up visits before 2021, only two major components of the E/M visit are necessary, so history and medical decision-making with documentation could be used. It may be easier since most telemedicine visits are largely counseling and coordination of care, to base these encounters on total time also and indicate that greater than 50% was devoted to counseling/coordination of care. Typical documentation will include the consent for the visit, the discussion with the patient, the differential diagnosis, the plan of care, and the total “face-to-face” time spent on the visit. The further notation that > 50% of the time was related to counseling and coordination of care (assuming it was) should also be documented.
Remote Monitoring
In addition to patient encounters whether non-face-to-face or face-to-face, the allergist/immunologist may also do remote monitoring of the patient. The 2020 CPT book lists the following codes for remote patient monitoring (RPM). Although some requirements for telehealth services have been modified during the pandemic, RPM services have never been limited by geography to rural or medically underserved areas, nor is there any “originating site” restriction for RPM services. In fact, RPM services can be provided anywhere the patient is located, including at the patient’s home.
- 99453 Remote monitoring of physiologic parameter(s) (e.g., weight, blood pressure, pulse oximetry, respiratory flow rate), initial; set-up and patient education on use of equipment
- 99454 Device(s) supply with daily recording(s) or programmed alert(s) transmission, each 30 days (provided monitoring occurs at least 16 days during the 30-day period)
- 99457 Remote physiologic monitoring treatment management services, clinical staff/physician/other qualified healthcare professional time in a calendar month requiring interactive communication with the patient/caregiver during the month; first 20 min.
- 99458 Each additional 20 min
As more devices become available to monitor asthma and other diseases treated by the allergist/immunologist, these codes will become more widely used just as blood pressure monitoring and diabetes monitoring are today.
An established patient is in the office and has poorly controlled, moderately severe persistent asthma. You provide the patient with a home spirometer that will transmit the FEV1 and FVC to your office. The patient is instructed on how to set up and use the device. He provides data via the portal for 20 days of the next month and you and your staff retrieve the data and analyze it. The time involved in retrieving and analyzing the information is 18 min. You modify the patient’s treatment program and describe the new treatment program during a telemedicine visit.
Billing would be 99453, 99454, and 99457 (each one unit). The E/M visit would be billed based on the time spent with the patient in describing the new treatment plan.
The documentation for these services might include a statement such as “we have provided this patient a remote spirometer and taught the patient its proper use. The patient has used it and transmitted information to us 20 days this month and the staff and I have spent 18 min total in the monitoring and responding to this patient in regard to asthma management based on results of the information transmitted.”
An older CPT code used for remote patient monitoring is 99091. This older code requires 30 min to bill based on a 30-day period. It is also limited to physicians and QHPs. There must be a face-to-face visit within 1 year and consent must be given and documented. The platform used must both collect and transmit data in real time or near real time to be eligible.
Another set of spirometry codes (94014, 94015, 94016) relate to patient-initiated remote spirometry, transmission of tracings, and review and interpretation by a physician or QHP. The second code (94015) does not include review and interpretation by a physician or other QHP whereas the third code (94016) is the review and interpretation by the provider. 94014 is an inclusive code of the latter two.
Interprofessional Telephone/Internet/Electronic Health Record Consultations
Codes 99446, 99447, 99448, 99449, and 99451/99452 are used to report a consultation when there is an interprofessional electronic consultation regarding assessment and management of a patient who is not seen face-to-face by the consulting provider. The patient may be a new patient to the consultant or an established patient with a new problem. The patient should not have been seen by the consultant for a face-to-face encounter in the past 14 days. Similarly, there should not be a transfer of care or a face-to-face encounter within the following 14 days of the consultation. Greater than 50% of the time for service must be devoted to the verbal or internet discussion. These codes should not be reported more than once within a 7-day interval. The consulting provider delivers a written or verbal report to the patient’s treating provider. The patient or family must give verbal consent (documented in the record) for the consult.
- 99446 reported by the consulting provider for 5–10 min of consultative discussion/review
- 99447 11–20 min
- 99448 21–30 min
- 99449 31 min or more
Code 99451 is reported by the consultant for 5 min or more time but does not require that more than 50% of the time be consultative time as opposed to data review. Furthermore, 99451 requires a written report.
Code 99452 is billed by the treating/requesting provider. This code is for time spent in preparing the consult and/or time communicating with the consultant for 16 min or more time.
Conclusions
Telemedicine will continue to be a significant part of the allergy/immunology practice even after the pandemic. Both Medicare and commercial insurance companies have made special provisions for telehealth during the pandemic in order to make medical care more readily available for patients who are concerned about their symptoms and also concerned about possible exposure to illness in a healthcare facility. Such provisions as allowing telephone calls (without video) to be sufficient for a “face-to-face” telemedicine visit for patients who do not have access to computers or other means of communicating via video connections will probably not continue after the pandemic [ 3 , 4 ]. The leniency on what platforms can be used by practices for telehealth visits will also likely change after the pandemic. These possible changes will likely be rolled out at different times for different carriers so it will be critical to review EOBs and look at insurers’ websites and newsletters.
It will be important to learn the codes and understand what codes different insurers require in order to be properly reimbursed for your work. Remembering to get consent for visits, to document what was done, to adhere to procedures that are medically necessary, and to code correctly will help practices receive payment for these services. It would be helpful to medicine in general if the commercial insurance companies and CMS provided a uniform approach and guideline for telemedicine coding. Until such time that these stakeholders provide a consistent and uniform coding guide to telemedicine, remember that “it depends” as you select the appropriate code, modifier, and place of service for telemedicine encounters.
Compliance with Ethics Guidelines
The authors declare no conflicts of interest relevant to this manuscript.
This article does not contain any studies with human or animal subjects performed by any of the authors.
This article is part of the Topical Collection on Telemedicine and Technology
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
2024 Telehealth CPT Codes: Cheat Sheet
Charika Wilcox-Lee, VP, Revenue Cycle Management
Keeping track of telehealth reimbursements accurately directly impacts your healthcare organization’s bottom line. We’ve compiled a list of telehealth CPT codes to help you better navigate telehealth billing for your care program.
Source: American Academy of Sleep Medicine (AASM)

CMS Telehealth & RPM Billing Guidelines [PDF]
In recent years, the Centers for Medicare & Medicaid Services (CMS) have released the physician fee schedule with expanded reimbursement for remote patient monitoring (RPM). The guidelines notably increase reimbursement for other services like remote therapeutic care and chronic care management, while making slight adjustments to allowances for RPM.
Top 4 Common Telehealth Billing Mistakes—And How to Avoid Them
The surge of telehealth adoption in recent years has led to regulatory changes and telemedicine coverage expansion that greatly benefits healthcare providers—if reimbursement is done correctly. Here are the top four common mistakes when billing for telehealth, and how you can avoid them.
Mistake #1: Not keeping up with the correct billing codes
As Medicare regulations change in response to public healthcare needs, the billing codes that you’re already familiar with could change as well. Submitting claims with the wrong code could result in delayed reimbursement and in some worst cases, be flagged for abuse.
Avoid by : Staying up to date with additions or deletions to the list of Medicare telehealth services .
Mistake #2: Not maintaining post-visit documentation
Ensuring that you document the right information during telehealth visits is key to getting prompt payment. For a start, touch base with your administrative team to understand the type of information you should be keeping a record of.
Avoid by : Creating a checklist that you can go over before the telehealth visit for cross-checking purposes.
Mistake #3: Not training your team on telehealth billing processes
Your team already has to keep track of thousands of CPT codes on a daily basis. With the new batch of telehealth CPT codes added to the mix, things can easily get very complicated for your team.
Avoid by : Training your team on the types of codes, processes, and all things reimbursement.
Mistake #4: Not checking with the patient’s insurance beforehand
While most major private payers provide coverage for telemedicine, it’s prudent to call up the payer and confirm if the services offered are covered. The good news is, that you’ll only need to verify this once for that particular policy.
Avoid by : Being more diligent about checking insurance coverage before the patient’s first telehealth visit. Use an insurance verification form to log the call and make sure you’re asking the right questions.
8 Key Updates to Telehealth Reimbursement in 2024
CMS has released its final rule for Medicare payments under the Physician Fee Schedule (PFS), introducing significant changes that will impact healthcare providers across the country. To help you stay informed and prepared, we've compiled the eight key updates you need to know.
Telehealth Reimbursement Resources & Expert Support
At Health Recovery Solutions, we provide a host of resources on reimbursement and telehealth billing modeled after best practices that we established from working with our healthcare partners—and we’re ready to help. Whether you're in the early stages of researching the benefits of telehealth and remote patient monitoring for your patients or you have an existing program in place and you're considering options to maximize the value of RPM, our team of experts is here to support you.


An official website of the United States government
The .gov means it’s official. A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Billing and coding Medicare Fee-for-Service claims
Read the latest guidance on billing and coding Medicare Fee-for-Service (FFS) telehealth claims.
On this page:
Telehealth codes covered by medicare, coding claims, common telehealth billing mistakes, more information about ffs billing.
Medicare added over one hundred CPT and HCPCS codes to the list of telehealth services .
Telephone visits and audio-only telehealth
Medicare is temporarily waiving the audio-video requirement for many telehealth services. Codes that have audio-only waivers are noted in the list of telehealth services .
Place of Service codes
When billing telehealth claims, it is important to understand the place of service (POS) codes as it affects reimbursement.
The POS code (PDF) explains where the provider and patient are located during the telehealth encounter. There are currently two POS codes:
- POS 02: Telehealth provided other than in patient's home. Patient is not located in their home when receiving health services or health related services through telecommunication technology.
- POS 10: Telehealth provided in patient's home. Patient is located in their home (which is a location other than a hospital or other facility where the patient receives care in a private residence) when receiving health services or health related services through telecommunication technology.
Avoiding mistakes in the reimbursement process can help implementing telehealth into your practice a smoother experience.
Incorrect billing codes
More than 100 telehealth services are covered under Medicare. However, some CPT and HCPCS codes are only covered temporarily.
Using the wrong code can delay your reimbursement. This can happen for a variety of reasons, such as a misunderstanding of what code applies to what service or input error.
Stay up to date on the latest Medicare billing codes for telehealth to keep your practice running smoothly.
Documentation
Post-visit documentation must be as thorough as possible to ensure prompt reimbursement.
While there are many similarities between documenting in-person visits and telehealth visits, there are some key factors to keep in mind.
Patient consent
Make a note of whether the patient gave you verbal or written consent to conduct a virtual appointment.
Code categories
Telephone codes are required for audio-only appointments, while office codes are for audio and video visits.

Time of visit
A common mistake made by health care providers is billing time a patient spent with clinical staff. Providers should only bill for the time that they spent with the patient.
Store-and-forward
Many states require telehealth services to be delivered in “real-time”, which means that store-and-forward activities are unlikely to be reimbursed. You can find information about store-and-forward rules in your state here .
Originating sites and distant sites
Learn about eligible sites as well as telehealth policies specific to Federally Qualified Health Centers and Rural Health Clinics.
If you are looking for detailed guidance on what is covered and how to bill Medicare FFS claims, see:
- Billing for Telehealth Encounters: An Introductory Guide on Fee-for-Service (PDF) – from the National Policy Center - Center for Connected Health Policy
Medicaid and Medicare billing for asynchronous telehealth
Learn how to bill for asynchronous telehealth, often called “store and forward".
Billing Medicare as a safety-net provider
Medicare billing and coding guidelines on telehealth for Rural Health Clinics (RHCs) and Federally Qualified Health Centers (FQHCs).

New series ‘The Tattooist of Auschwitz’ tells the story of Holocaust survivors finding love

Jenna Bush Hager reveals her daughter Mila calls her ‘Jenner’

Weekend watchlist: ‘Abigail,’ ‘Our Living World’ and more

Michelle Collins talks comedy tour, singing 'Les Mis' parodies
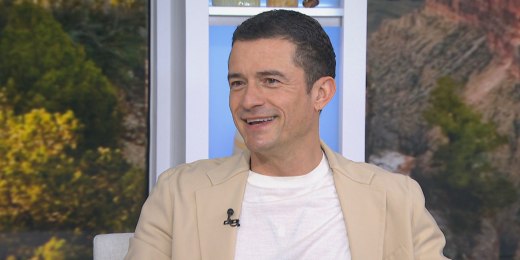
Orlando Bloom urges Hoda Kotb to skydive for her birthday: 'Do it'

Two weddings on the same day: How to decide which one to go to

'George to the Rescue' renovates jazz lover's 1800s home

Taylor Swift and Beyoncé lead the charge for ‘Pop Girl Spring’

Cowboys cheerleaders are the focus of new Netflix doc

See Glen Powell in trailer for ‘Hit Man’ rom-com
See behind the scenes of viral 'Beavis' sketch on 'SNL'
Taylor Swift reveals 'Tortured Poets' is a secret double album!

Jurnee Smollett talks narrative behind the film ‘We Grown Now’
Tony Danza on teaching acting to kids, 'Who’s The Boss' reboot
Am I 'crazy' that my boyfriend texting his ex doesn't bother me?

'The Sympathizer' stars on 'different perspective' of Vietnam War

Orlando Bloom talks new adventure show, support from Katy Perry

Watch John Stamos surprise Chris Stapleton as he sang about him
Jennifer Garner dances in oven mitts on her feet for 52nd birthday

Mariska Hargitay mistaken for real cop by lost child on ‘SVU’ set
Nbc news now.
It’s been nearly 80 years since the end of the Holocaust, but the harrowing experiences of survivors are still coming to light. One of those stories is the focus of a new Peacock series, “The Tattooist of Auschwitz,” inspired by the true story of two survivors who met and fell in love in the Auschwitz-Birkenau concentration camps. NBC News’ Savannah Sellers spoke with actor Jonah Hauer-King about his role in the series. April 19, 2024
Best of NBC News

Apparent conspiracy theorist sets himself on fire outside of Trump trial

Special report: Man sets himself on fire outside court as a jury is seated in Trump hush money trial

Jury seated in Trump hush money trial

Gazan civilians bombed while sheltering in U.N. school

Man sets himself on fire outside Trump trial, witness says

Mobile Menu Overlay
The White House 1600 Pennsylvania Ave NW Washington, DC 20500
Statement from President Joe Biden on Iran’s Attacks against the State of Israel
Earlier today, Iran—and its proxies operating out of Yemen, Syria and Iraq—launched an unprecedented air attack against military facilities in Israel. I condemn these attacks in the strongest possible terms.
At my direction, to support the defense of Israel, the U.S. military moved aircraft and ballistic missile defense destroyers to the region over the course of the past week. Thanks to these deployments and the extraordinary skill of our servicemembers, we helped Israel take down nearly all of the incoming drones and missiles.
I’ve just spoken with Prime Minister Netanyahu to reaffirm America’s ironclad commitment to the security of Israel. I told him that Israel demonstrated a remarkable capacity to defend against and defeat even unprecedented attacks – sending a clear message to its foes that they cannot effectively threaten the security of Israel.
Tomorrow, I will convene my fellow G7 leaders to coordinate a united diplomatic response to Iran’s brazen attack. My team will engage with their counterparts across the region. And we will stay in close touch with Israel’s leaders. And while we have not seen attacks on our forces or facilities today, we will remain vigilant to all threats and will not hesitate to take all necessary action to protect our people.
Stay Connected
We'll be in touch with the latest information on how President Biden and his administration are working for the American people, as well as ways you can get involved and help our country build back better.
Opt in to send and receive text messages from President Biden.
Telehealth Billing and Coding Basics
Get familiar with common coding and billing terms and practices that you need to know to be able to sustain your telehealth program.
What are the different telehealth places of service (POS)?
There are two telehealth-specific places of service (POS):
- POS 02 is used for telehealth services provided in a location other than the patient’s home.
- POS 10 is used for telehealth services provided to a patient located in their home.
A home is considered a location other than a hospital or other facility where the patient receives care in a private residence.
Payers are gradually transitioning from their temporary COVID-19 policies to permanent telehealth policies. Review the AAFP’s telehealth coding scenarios and check with your local provider relations representatives for information regarding which POS they require.
What are the different telehealth modifiers?
There are several modifiers that may be appended to telehealth services. The modifier may depend on the type of service.
-95: Synchronous telemedicine service rendered via a real-time interactive audio and video communications system.
-93: Synchronous telemedicine service rendered via telephone or other real-time interactive audio-only telecommunications system.
-GQ: Telehealth service rendered via asynchronous telecommunications system.
-GT: Telehealth service rendered via interactive audio and video telecommunications systems
-FQ: A telehealth service was furnished using real-time audio-only communication technology.
Medicare no longer uses the GT modifier for professional services. However, many private payers still accept it.
Review the AAFP’s telehealth coding scenarios and check with your local provider relations representatives for information regarding which modifiers they require.

Learn how telemedicine can help simplify your practice.
What services can I provide via telehealth?
The Medicare list of approved telehealth services is available as a zipped file, which also includes the list of services that Medicare will allow via audio-only communications technology.
Contact your local provider relations representatives for their lists of approved telehealth services.
Can I provide the annual wellness visit via telehealth?
The annual wellness visit (AWV) is on Medicare’s list of approved telehealth services. Medicare will also allow the AWV to be completed using audio-only communications technology.
Medicare states that self-reported vitals may be used when a beneficiary is at home and has access to the types of equipment they would need to self-report vitals. The visit must also meet all other requirements.
Note : the Initial Preventive Physical Exam (IPPE) is not on Medicare’s list of approved telehealth services.

Telehealth Collection: Resources on the basics, workflow, billing, and more
How is an office visit conducted via audio-video billed?
Office visit evaluation and management services (CPT codes 99202-99205, 99211-99215) furnished using audio-video telecommunications technology are reported using the same CPT codes as you would have had the visit been conducted in-person. However, telehealth services are reported using a different place of service and/or require a modifier. The specific POS and modifier vary by payer. Review the AAFP’s telehealth coding scenarios for additional information.
FREE Toolkit
Getting Started with Telehealth
Equip your practice to offer sustainable telemedicine offerings that will help you provide the care your patients need, when and where they need it.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
China foreign ministry welcomes Blinken's visit to China as tensions simmer
- Medium Text

The Reuters Daily Briefing newsletter provides all the news you need to start your day. Sign up here.
Reporting by Eduardo Baptista; Writing by Bernard Orr; Editing by Muralikumar Anantharaman and Tom Hogue
Our Standards: The Thomson Reuters Trust Principles. New Tab , opens new tab

World Chevron
Russian missiles hit the port of Pivdennyi in Ukraine's southern Odesa region on Friday, destroying grain storage facilities and foodstuffs they contained, President Volodymyr Zelenskiy and other officials said.

- FanNation FanNation FanNation
- Swimsuit SI Swimsuit SI Swimsuit
- Sportsbook SI Sportsbook SI Sportsbook
- Tickets SI Tickets SI Tickets
- Shop SI Shop SI Shop
- What's on TV
- NFL NFL NFL
- Home Home Home
- Free Agency Free Agency Free Agency
- Scores Scores Scores
- Schedule Schedule Schedule
- Standings Standings Standings

- Stats Stats Statistics
- Odds Odds Odds
- Futures Futures Futures
- Injuries Injuries Injuries
- Transactions Transactions Transactions
- Teams Teams Teams

Adam Schefter Sheds Light on Commanders' Unusual Quarterback Evaluation Strategy
Washington decided to bring in multiple quarterback prospects on the same visit earlier this week.
- Author: Liam McKeone
In this story:
The Washington Commanders have made headlines this week thanks to the way they're going about the NFL draft. Holding the No. 2 pick, first-year general manager Adam Peters happily told assembled media on Thursday that the team had no plans to trade down — a decision usually kept under wraps until draft day. The most notable item, however, came in the form of how the Commanders are evaluating quarterbacks. On Friday, ESPN NFL insider Adam Schefter shed some light on that aspect of their draft process.
Usually, interested teams hold visits with each individual quarterback prospect. Washington (for some reason) held one big visit for four potential picks . Jayden Daniels, Drake Maye, J.J. McCarthy, and Michael Penix Jr. all came to the team facilities earlier this week. Schefter appeared on Get Up to discuss the unusual method and said it didn't sit well with Daniels because he was under the impression it was a solo visit.
Schefter on Jayden Daniels visit with WAS "It didn't seem to go over too well with his agent who sounded off on social media that he didn't seem particularly pleased with the process. Daniels thought it would be a visit for just him, but WAS essentially opened up the process." pic.twitter.com/Y69c7pFcUN — Billy M (@BillyM_91) April 19, 2024
In regards to the other aspect of the above report, Ron Butler is the agent for Daniels and he did express discontent with the process on his X (formerly known as Twitter) account.
🤔 https://t.co/GG2nOEwmtM — Ron Butler (@Agentbutler1) April 18, 2024
All of this only highlights how strange it was that the Commanders went this route. There are certainly benefits to evaluating a prospect in a group environment; playing well with others is a key component of succeeding as an NFL quarterback. Minnesota Vikings head coach Kevin Stefanski even likes to see how potential draft picks order their food . But there are plenty of people Washington can ask about that and get an accurate read on it. That's what old teammates and coaches are there for.
There are few opportunities during the pre-draft process to get in a room with a prospect one-on-one for a substantial period of time. That time is pretty important! The Commanders will be paying whoever they select tens of millions of dollars right off the bat, and if things go according to plan, they'll end up paying hundreds of millions. Passing up the chance to get more individual time with the prospect they hope will be the face of their franchise doesn't look good.
And that's what this is all about. The perception is poor. Washington is surely doing all the homework necessary and met with individual quarterbacks at the NFL Combine. But putting those four together into one visit comes across like they were trying to check several boxes at once because it is more convenient for the team. It's the absolute last thing long-suffering fans of the franchise wants to see.
A strange decision-making process, and one that Daniels (a very likely selection at No. 2) is reportedly not happy about.
Latest NFL News

Chargers Named Best Team Fit For Star WR Free Agent

BREAKING: Eagles Sign Giants Ex Parris Campbell

Former Buccaneers Quarterback Tom Brady's Raiders Bid Will Have To Wait A Little Longer

WATCH: Steelers QB Russell Wilson Sends Message Through Hype Video

Next Steps for Chiefs After First Wave of Free Agency

IMAGES
VIDEO
COMMENTS
Medicare requires audio-video for most office visit evaluation and management (E/M) services (CPT codes 99202-99215) telehealth services. Audio-only encounters are allowed for certain services.
Code. Description. G2010. Remote evaluation of recorded video and/or images submitted by an established patient (e.g. store and forward), including interpretation with followup with the patient within 24 business hours, not originating from a related E&M service provided within the previous 7 days nor leading to an E&M service or procedure within the next 24 hours or soonest available appointment.
Medicare requires audio-video for office visit (CPT 99201-99215) telehealth services. Audio-only encounters can be provided using the telephone evaluation and management codes (CPT codes 99441-99443).
What are the CPT codes for a virtual video telehealth visit? A virtual video visit is reported with the same CPT codes that you would use for in-person visits (99201-99205 new patient visit; 99211-99215 established patient visit; or 99241-99245 consultation visit [not recognized by CMS, see G-codes]).The service should be reported with a -95 modifier (confirm your local payer rules).
CPT Telemedicine Codes Modifier 95 indicates a synchronous telemedicine service rendered via a real-time interactive audio and video telecommunications system. The 2020 CPT® manual includes Appendix P, which lists a summary of CPT codes that may be used for reporting synchronous (real-time) telemedicine services when appended by modifier 95.
Append this modifier to an appropriate CPT code (listed in Table 4 in this fact sheet or refer to the 2023 CPT manual) for an audio-only real-time interaction between a physician or other qualified healthcare professional and a patient who is located at a distant site from the reporting provider. The totality of the
Code. Description. Telehealth visits (face-to-face) Audio/visual visit between a patient and clinician for evaluation and management (E&M) New patient level one code (99201) has been deleted. CPT code 99202-99205. Office or other outpatient visit for the evaluation and management of a new patient. CPT code 99212-99215.
99423: Online digital evaluation and management service, for a patient, for up to 7 days, cumulative time during the 7 days; 21 or more minutes. E-visits should not be billed on the same day the ...
Telephone or audio-only evaluation and management services for new and established patients cannot originate from a related E/M service provided within the previous 7 days nor lead to an E/M service or procedure within the next 24 hours or soonest available appointment. Covered but not separately payable. 99441: 5-10 minutes. 99442: 11-20 minutes.
Page 1 of 6. MLN901705 February 2024. We pay for specific Medicare Part B services that a physician or practitioner provides via 2-way, interactive technology (or telehealth). Telehealth substitutes for an in-person visit, and generally involves 2-way, interactive technology that permits communication between the practitioner and patient.
Video Visit Established Patient E/M Telephone E/M Online Digital E/M Virtual Check-ins CPT 2021 Time Range 2021 Pmt wRVU CPT Time 2021 PHE Pmt 2021 PHE wRVU CPT Time 2021 Pmt wRVU CPT Time 2021 Pmt wRVU 99211 NA $23.03 0.18 G2010 NA $12.21 0.18 99212 10-19 min $56.88 0.70 99441 5-10 min $56.88 0.70 99421 5-10 min $15.00 0.25 G2012 5-10 min $14. ...
Example: line one- CPT code 99213-95, line two- CPT code 99442; or CPT code 99442. ... Hi, does the patient need to be present (in the video) in order to bill a telemed visit? For in-person visits, i.e. 99213, patient or family, is required to be present. Renee Dustman says: June 10, 2020 at 5:42 am.
The payment amount for HCPCS code Q3014 (Telehealth originating site facility fee) is 80% of the lesser of the actual charge ($28.64 for CY 2023 services). We base this on the percentage increase in the Medicare Economic Index (MEI) as defined in section 1842(i)(3) of the Social Security Act. The 2023 MEI increase is 3.8%.
We've compiled a list of telehealth CPT codes to help you better navigate telehealth billing for your care program. Remote Patient Monitoring CPT Codes. Telehealth Visits. 99202 - 99215. Office or other outpatient visits. New and established patients. G0425 - G0427. Consultations, emergency department, or initial inpatient.
Video Visit Documentation Requirement . Coding Corner. Example 3. A 38 yr old female presents with left hip pain and joint pain lasting > 4 weeks. Last seen on 3/4/20 for positive anti-nuclear anti-body and emphysema. Labs ordered from 3/4/20 were reviewed. New labs were ordered, and patient is
Telephone service codes exist for providers who cannot report E/M services (e.g., LCSW's, psychologists, RD/PT/OT/SLP) CPT 98966-98968. 98966 (5-10 minutes) 98967 (11-20 minutes) 98968 (21-30 minutes) Use normal Place of Service code (e.g., POS 11 for Office) No modifiers needed. SelectHealth is currently reimbursing these services.
CPT 9921 2 is an office or other outpatient visit for the evaluation and management (E&M) of an established patient. This ... interactive audio & video telecommunications system that permits real-time communication. ... CPT 9921 3 is an office or other outpatient visit for the evaluation and management (E&M) of an established patient. ...
Telephone codes are required for audio-only appointments, while office codes are for audio and video visits. Time of visit. A common mistake made by health care providers is billing time a patient spent with clinical staff. Providers should only bill for the time that they spent with the patient. Store-and-forward
Telehealth Video Visits Time-Based Coding New Patient CPT Code CPT Typical Time CMS Typical Time 99201 10 Min 17 Min 99202 20 Min 22 Min 99203 30 Min 29 Min 99204 45 Min 45 Min 99205 60 Min 67 Min ... • Use total time that the practitioner (not staff) spends on that day of the visit, independent of whether
video. CMS IS WAIVING THE REQUIREMENT FOR BOTH AUDIO AND VIDEO CONNECTIVITY DURING THE COVID-19 PUBLIC HEALTH EMERGENCY. These visits are considered the same as in-person visits and are billed and reimbursed by CMS the same rate as regular, in-person visits. Scenario 1: Telehealth Visit Action Patient evaluated via: E/M Telehealth, Telephone Visit
Telehealth visits (real-time audio and video), E-visits (online E/M visits), ... Virtual visit algorithm. Click for full-size version. Posted on Mar 23, 2020 by FPM Editors Advertisement chevron ...
ACCS COVID Note Critical Care via In-Person or Video COVID Video Visit Documentation Brief COVID Questionnaire via Video AAH COVID-19 Telephone ... For IP telehealth performed via video, the below CPT codes are appropriate for use. Clinicians must append modifier GT to flag that a visit was performed via telehealth. Note: For clinicians ...
Video/Hill.TV See all Hill.TV See all Video Rising Rising: April 19, 2024 by TheHill.com 04/19/24 1:20 PM ET Rising / 51 mins ago Rising Rising: April 18, 2024 by TheHill.com ...
A Brazilian woman brought a 68-year-old man in a wheelchair into a bank branch and tried to get him to sign for a loan, but police said he had been dead for hours.
Video/Hill.TV See all Hill.TV See all Video Rising Rising: April 19, 2024 by TheHill.com 04/19/24 1:20 PM ET Rising / 2 hours ago Rising Rising: April 18, 2024 by TheHill.com ...
It's been nearly 80 years since the end of the Holocaust, but the harrowing experiences of survivors are still coming to light. One of those stories is the focus of a new Peacock series, "The ...
We'll be in touch with the latest information on how President Biden and his administration are working for the American people, as well as ways you can get involved and help our country build ...
Office visit evaluation and management services (CPT codes 99202-99205, 99211-99215) furnished using audio-video telecommunications technology are reported using the same CPT codes as you would ...
China's foreign ministry on Thursday welcomed U.S. Secretary of State Antony Blinken's visit to China as tensions rise between the two countries over global trade, regional conflicts and the ...
Washington (for some reason) held one big visit for four potential picks. Jayden Daniels, Drake Maye, J.J. McCarthy, and Michael Penix Jr. all came to the team facilities earlier this week.