You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.

Pregnant Travelers

Pregnant travelers can generally travel safely with appropriate preparation. But they should avoid some destinations, including those with risk of Zika and malaria. Learn more about traveling during pregnancy and steps you can take to keep you and your baby healthy.
Before Travel
Before you book a cruise or air travel, check the airlines or cruise operator policies for pregnant women. Some airlines will let you fly until 36 weeks, but others may have an earlier cutoff. Cruises may not allow you to travel after 24–28 weeks of pregnancy, and you may need to have a note from your doctor stating you are fit to travel.
Zika and Malaria
Zika can cause severe birth defects. The Zika virus is spread through mosquito bites and sex. If you are pregnant, do not travel to areas with risk of Zika . If you must travel to an area with Zika, use insect repellent and take other steps to avoid bug bites. If you have a sex partner who lives in or has traveled to an area with Zika, you should use condoms for the rest of your pregnancy.
Pregnant travelers should avoid travel to areas with malaria, as it can be more severe in pregnant women. Malaria increases the risk for serious pregnancy problems, including premature birth, miscarriage, and stillbirth. If you must travel to an area with malaria, talk to your doctor about taking malaria prevention medicine. Malaria is spread by mosquitoes, so use insect repellent and take other steps to avoid bug bites.
Make an appointment with your healthcare provider or a travel health specialist that takes place at least one month before you leave. They can help you get destination-specific vaccines, medicines, and information. Discussing your health concerns, itinerary, and planned activities with your provider allows them to give more specific advice and recommendations.
Plan for the unexpected. It is important to plan for unexpected events as much as possible. Doing so can help you get quality health care or avoid being stranded at a destination. A few steps you can take to plan for unexpected events are to get travel insurance , learn where to get health care during travel , pack a travel health kit , and enroll in the Department of State’s STEP .
Be sure your healthcare policy covers pregnancy and neonatal complications while overseas. If it doesn’t get travel health insurance that covers those items. Consider getting medical evacuation insurance too.
Recognize signs and symptoms that require immediate medical attention, including pelvic or abdominal pain, bleeding, contractions, symptoms of preeclampsia (unusual swelling, severe headaches, nausea and vomiting, and vision changes), and dehydration.
Prepare a travel health kit . Pregnant travelers may want to include in your kit prescription medications, hemorrhoid cream, antiemetic drugs, antacids, prenatal vitamins, medication for vaginitis or yeast infection, and support hose, in addition to the items recommended for all travelers.
During Travel
Your feet may become swollen on a long flight, so wear comfortable shoes and loose clothing and try to walk around every hour or so. Sitting for a long time, like on long flight, increases your chances of getting blood clots, or deep vein thrombosis. Pregnant women are also more likely to get blood clots. To reduce your risk of a blood clot, your doctor may recommend compression stockings or leg exercises you can do in your seat. Also, see CDC’s Blood Clots During Travel page for more tips on how to avoid blood clots during travel.
Choose safe food and drink. Contaminated food or drinks can cause travelers’ diarrhea and other diseases and disrupt your travel. Travelers to low or middle income destinations are especially at risk. Generally, foods served hot are usually safe to eat as well as dry and packaged foods. Bottled, canned, and hot drinks are usually safe to drink. Learn more about how to choose safer food and drinks to prevent getting sick.
Pregnant women should not use bismuth subsalicylate, which is in Pepto-Bismol and Kaopectate. Travelers to low or middle income destinations are more likely to get sick from food or drinks. Iodine tablets for water purification should not be used since they can harm thyroid development of the fetus.
After Travel

If you traveled and feel sick, particularly if you have a fever, talk to a healthcare provider immediately, and tell them about your travel. Avoid contact with other people while you are sick.
More Information
CDC Yellow Book: Pregnant Travelers
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Flying While Pregnant? Check Out the Policies on 25 Global Airlines
In the absence of obstetric or medical complications, occasional air travel during pregnancy is generally safe, according to the American College of Obstetrics and Gynecology (ACOG). Like other travelers, pregnant women should use seat belts while seated.
Most commercial airlines allow pregnant women to fly up to 36 weeks of gestation, with some restrictions on international flights.
ACOG does not recommend air travel for pregnant women with medical or obstetric conditions that may be exacerbated by flight or that could require emergency care. It advises checking flight durations when planning travel and that the most common obstetric emergencies occur in the first and third trimesters.
Once aboard a flight, conditions including changes in cabin pressure and low humidity, coupled with the physiologic changes of pregnancy, do result in adaptations, including increased heart rate and blood pressure, reports ACOG. And those traveling on long-haul flights face the risks associated with immobilization and low cabin humidity. This can cause issues such as lower extremity edema and venous thrombotic events.
ACOG recommends preventive measures to minimize these risks, including the use of support stockings, regular movement of the lower extremities, avoid wearing restrictive clothing and encourage regular hydration. It also advises against consuming gas-producing foods or drinks before a flight.
Other ways for pregnant women to be comfortable on their flights include: booking a bulkhead seat for more legroom; reserving an aisle seat for easy access to lavatories and to walk; elevating your legs on a carry-on bag to avoid swelling and cramps; and wearing a layered, comfortable outfit for changing cabin temperatures.
Airlines around the world have different rules and regulations on when and how long pregnant women can fly. Below are the policies from 25 airlines around the world.
The French flag carrier does not require pregnant women to carry a medical certificate for travel during pregnancy. It recommends avoiding travel in the final month of pregnancy, as well as during the first seven days after delivery. The airline also recommends expecting mothers seek their doctor's opinion before traveling.
India’s flag carrier allows expectant mothers in good health to fly up to and including their 27th week of pregnancy. After 27 weeks, if the pregnancy is anticipated to be a normal delivery, an expectant mother will be accepted for travel up to the 35th week, but a medical certificate confirming the mother is fit to travel is required by an attending obstetrician and dated within three days of travel.
Air New Zealand
For single, uncomplicated pregnancies and clearance from a doctor or midwife women can take flights more than four hours up to the end of their 36th week. For flights under four hours, it's up to the end of the 40th week. Women pregnant with twins can fly more than four hours up to their 32nd week and less than four hours until the 36th week.
The airline recommends that women past their 28th week carry a letter from a doctor or midwife that says you are fit for travel, confirming your pregnancy dates and that there are no complications.
The airline's medical team must offer clearance for women experiencing the following: a complicated pregnancy, such as placenta previa or bleeding; a multiple pregnancy; a history of premature labor; or have begun the early stages of labor.
Italy's flag carrier has no travel restrictions for expectant mothers during the first eight months of pregnancy. But if traveling within the last four weeks of pregnancy, expecting multiple births, or having a complicated pregnancy, medical clearance is required. Completion of a Medical Information Form, MEDIF , prior to travel and signed by both the passenger and doctor is required.
Alitalia advises pregnant not to fly seven days prior to and seven days after giving birth, or if there is a risk of a premature birth or other complications. It will make staff available to escort pregnant women from the airport check-in counter to the boarding gate. Staff onboard the flight will help stow carry-on luggage. Seats can be pre-assigned and women cannot sit in an exit row.
All Nippon Airways
The Japanese carrier requires women within 15 to 28 days of their due date to fill out and carry a medical information form . Women within 14 days of their due date are required to have a medical form and travel with a doctor. The form must indicate there are no complications of pregnancy, that the passenger has no health problems preventing them from flying and the due date. It must be completed by a doctor and submitted no more than seven days prior to departure.
American Airlines
The Fort Worth-based carrier has different rules for international and domestic flights. If a due date is within four weeks of a flight, you must provide a doctor’s certificate stating that you’ve been recently examined and you’re fit to fly. For domestic flights under five hours, pregnant women won’t be permitted to travel within seven days (before and after) their delivery date. Those who need travel within this timeframe will need approval from a physician and help from a special assistance coordinator . The pregnant woman's physician will be required to fill out a passenger medical form before a flight. A special assistance coordinator will send the form directly to your physician.
Clearance from a special assistance coordinator is required for international travel or travel over water. Within four weeks of a due date also requires a physician's note stating that you’ve been examined within the past 48 hours and you’re fit to fly. And seven days before or after delivery also requires a passenger medical form to be completed by your physician.
British Airways
The U.K. carrier does not allow pregnant women to fly after the end of the 36th week if you are pregnant with one baby or the end of the 32nd week if you are pregnant with more than one baby. While it isn't mandated, British Airways recommends all expecting mothers carry a confirmation from a doctor or midwife, such as a letter or certificate, in addition to your pregnancy record. It should be written within seven days prior to travel and confirm your approximate due date, that you're fit to travel and that there are no complications with your pregnancy.
Cathay Pacific
Hong Kong's flag carrier requires that women with pregnancies after 28 weeks carry a medical certificate, dated within 10 days of travel that states the following:
- single or multiple pregnancy
- estimated week of pregnancy
- expected due date
- certifying you are in good health and the pregnancy is progressing normally, without complications
- that you are fit to travel
The airline accepts pregnant women with uncomplicated single pregnancies to travel up to 36 weeks and uncomplicated multiple pregnancies up to 32 weeks.
Delta Air Lines
The Atlanta-based carrier does not impose restrictions on flying for pregnant women, so a medical certificate is not required to travel. But the airline will not waive ticket change fees and penalties for pregnancy. The airline recommends that those flying after their eight month should check with their doctor to be sure travel is not restricted.
The U.K.-based airline has no restrictions for pregnant passengers traveling up to the end of the 35th week of single pregnancies and the end of the 32nd week for multiple pregnancies.
Pregnant women can travel up to their 29th week without a medical certificate. After that, they require a certificate or letter signed by a qualified doctor or midwife that states whether the pregnancy is single or multiple, is progressing without complications, includes an estimated due date, that you are in good health and there's no known reason to prevent you from flying. Pregnant passengers are not allowed to fly after the 32nd week of a multiple pregnancy, and after the 36th week of a single pregnancy.
This Abu Dhabi-based carrier allows women with single or multiple pregnancies to travel during the first 28 weeks without a medical certificate. For single pregnancies between 29 and 36 weeks, a medical certificate is required. After 37 weeks, pregnant women will not be allowed to travel. For multiple pregnancies, a certificate is required between the 29th and 32nd week; after that, women will not be allowed to travel.
The medical certificate must include the following:
- Be issued and signed by a doctor or midwife
- Written on a clinic/hospital letterhead and/or stamped by the doctor or midwife
- State that the guest is fit to fly
- State if the pregnancy is single or multiple
- State the number of weeks of pregnancy and the Expected Date of Delivery
- Easily understood and written in Arabic or English. Other languages are accepted but must be verified by Etihad Airways' check-in staff
The original medical certificate shall be accepted for the whole journey (originating, return and stopover flights), provided the above validity criteria is met for each sector. And it is valid for three weeks from the date of issue.
The New York-based carrier does not allow pregnant customers expecting to deliver within seven days to travel unless they provide a doctor's certificate dated no more than 72 hours prior to departure stating that the woman is physically fit for air travel to and from the destinations requested on the date of the flight and that the estimated date of delivery is after the date of the last flight.
The Dutch flag carrier recommends pregnant mothers not fly after the 36th week, along with the first week following delivery. For those expecting more than one baby, the carrier recommends consulting with a physician prior to flying. If you have had complications, you always need to have permission to fly from your physician.
Expectant mothers with complication-free pregnancies can fly on the German flag carrier until the end of the 36th week of pregnancy or up to four weeks before their expected due date without a medical certificate from a gynecologist. But the airline recommends that pregnant women beyond the 28th week have a current letter from a gynecologist that includes confirmation that the pregnancy is progressing without complications and the expected due date. The doctor should expressly state that the patient’s pregnancy does not prevent her from flying.
Because of the increased risk of thrombosis during pregnancy, the airline does recommend that expectant mothers wear compression stockings while flying.
Malaysia Airlines
The Malaysian flag carrier requires medical clearance for expectant mothers approaching 35 weeks for international travel or 36 weeks for domestic travel. If medical clearance is required, the MEDIF application form should be completed by a doctor and submitted to the airline through its ticketing offices or travel agents at least five working days before traveling.
Philippine Airlines
An expectant mother who is in normal health and with no pregnancy complications will be allowed to fly after filling out an EMIS form . Pregnant women may be accepted for travel if they are not beyond 35 weeks when they fill out Part One of the EMIS form. Those between 24 and 32 weeks of pregnancy will have to fill out EMIS Form Part 2. And if the expectant mother is below 21 years of age, the consent in writing of the husband, parent or guardian must be secured. For expectant mothers beyond 32 weeks of pregnancy, EMIS Part 3 must be accomplished by the Flight Surgeon or Company Physician, who shall issue the clearance for travel
After the 28th week, women are required to have a certificate or letter from a registered medical practitioner or registered midwife confirming the delivery date, whether it's a single or multiple pregnancy and that the pregnancy is routine.
For flights longer than four hours, women can fly up to the end of the 36th week for single pregnancies and the end of the 32nd week for multiple pregnancies. For flights under four hours, women can travel up to the end of the 40th week for single pregnancies and the end of the 36th week for multiple pregnancies. The carrier requires medical clearance if there are pregnancy complications or it's not a routine pregnancy.
Qatar Airways
No doctor's note is required for women traveling through their 28th week of pregnancy. Expectant mothers can fly between week 29 and week 32 with a doctor's note and a pregnancy with no complications. Those with a multiple pregnancy will need a doctor's note and a Medical Information Form (MEDIF) . Between weeks 33 and 35, women will need a doctor's note and a MEDIF. The airline does not accept women in their 36th week and beyond.
The low-cost Irish carrier allows expectant mothers to fly up to their 28th week of pregnancy. After that, the airline requires women to have a ‘fit to fly’ letter from their midwife or doctor. For an uncomplicated single pregnancy, travel is not permitted beyond the end of the 36th week of pregnancy, while the cut-off for an uncomplicated multiple pregnancy is 32 weeks.
Singapore Airlines
For uncomplicated single pregnancies, the carrier restricts expectant mothers from travelling beyond the 36th week of pregnancy; for uncomplicated multiple pregnancies, the restriction is the 32nd week.
For uncomplicated single pregnancies between 29 weeks and 36 weeks, expectant mothers must provide a medical certificate stating the following: (1) fitness to travel, (2) number of weeks of pregnancy and (3) estimated date of delivery. The certificate should be dated within ten days of the date of the first flight exceeding 28 weeks of pregnancy. This certificate will have to be presented at check-in when requested.
Southwest Airlines
The Dallas-based carrier advises expectant mothers at any stage of pregnancy to consult with their physicians prior to air travel. The airline recommends against air travel beginning at the 38th week of pregnancy. It warns that in some cases, traveling by air has been known to cause complications or premature labor. Depending on their physical condition, strength, and agility, pregnant women may, in some cases, be asked not to sit in the emergency exit row.
Turkish Airlines
Turkey's flag carrier allows mothers pregnant with one child to travel between the 28th and 35th week if they have a doctor's report that includes the phrase, “There is no particular reason for the patient not to fly.” For women pregnant with more then one baby, the travel cut-off is the end of the 31st week with a doctor's report. The report has to be no more than seven days from the travel date.
United Airlines
Any woman in the first 36 weeks of pregnancy will be allowed to travel on the Chicago-based carrier without medical documentation. An expectant mother traveling after the 36 weeks of pregnancy must have the original and two copies of an obstetrician’s certificate, which must be dated within 72 hours of a flight’s departure. The original certificate should be submitted to a United representative at check-in.
Virgin Atlantic
The London-based airline allows travel without restrictions until the 28th week of pregnancy provided that you're free from complications to that point. The carrier asks pregnant mothers to inform its Special Assistance department so they can offer appropriate inflight health advice. Between the 28th and 36th weeks of pregnancy, a doctor's or midwife's certificate is required, stating that the passenger is safe for travel and the expected due date (32 weeks if carrying multiples in an uncomplicated pregnancy). Beyond the 36th week of pregnancy, travel is only permitted for medical/compassionate reasons and the pregnant passenger is required to be accompanied by a medical escort. This travel is subject to the approval of a Virgin Atlantic doctor.
The 10 Best Compression Socks for Travel of 2024
North American Airlines on Rules for Overweight Passengers
The 7 Best Travel Car Seats of 2024
Booking a Baby Bassinet for Your Flight
The 11 Best Carry-on Backpacks of 2024, Tested and Reviewed
Car Seat Policies for the Top 15 North American Airlines
Pet Birds and Air Travel
How to Travel Internationally With Your Pet
Budget Airline Baggage Fees
Everything International Travelers Need to Know About Planning a Trip to the US
Guide to Planning a Trip to Israel
How to Travel to Cuba If You Are an American
Morocco Reopens Its Borders to Citizens of 67 Countries, Including the U.S.
8 Air Travel Rights You Didn’t Know You Have
What to Know About French Customs Regulations
The 14 Cheapest Airlines in North and South America
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
Traveling while pregnant: Your complete guide
Unless you're nearing your due date or have certain complications, your healthcare provider will generally give you the green light for pregnancy travel. Here's how to safely explore – plus what to consider before making plans.

Is traveling while pregnant safe?
When to avoid pregnancy travel, when is the best time to travel while you're pregnant , can pregnant women travel during covid, when should you stop traveling while pregnant, your pregnancy travel checklist, when to call your doctor while traveling.
Yes, it's generally safe to travel during pregnancy as long as you're not too close to your due date and you're not experiencing any serious pregnancy complications. There are special precautions to take, of course, and you may find yourself stopping to use the bathroom more than you're used to, but that babymoon can be within reach.
Before you pack your suitcase, talk with your healthcare provider to make sure it’s safe for you to travel and that your destination is a good choice. You'll want to avoid places where infectious diseases are prevalent (or there are high outbreaks of Zika or malaria, for example). The COVID-19 pandemic has made people reconsider where they feel safe traveling as well; if you're fully vaccinated, the CDC says you can travel Opens a new window , but it's always best to check with your doctor first.
And bear in mind that the activities you take part in might be different than normal – you'll want to skip the Scuba diving lessons, for example (though snorkeling is okay!).
It's safe to fly when you're pregnant as well, and most airlines will allow you to fly domestically until about 36 weeks of pregnancy. International routes may have different rules, so be sure to check with your airline before booking anything. Your doctor will tell you to avoid flying, however, if you have a health concern that might require emergency care or any other health conditions that aren’t well controlled.
It's best to avoid traveling while pregnant if you have any health conditions that can be life-threatening to both you or your baby. If you have any of the following conditions, your doctor will almost certainly advise you against travel:
- Placental abruption
- Preeclampsia
- You're in preterm or active labor
- Cervical insufficiency (incompetent cervix)
- Premature rupture of membranes (PROM)
- A suspected ectopic pregnancy
- Vaginal bleeding
You might also need to be extra-cautious or skip travel if you're experiencing intrauterine growth restriction , you have placenta previa , or you have other conditions that may place your pregnancy at a higher risk. It’s always a good idea to discuss your concerns with your healthcare provider before travel regarding any medical conditions you have, and they'll be able to advise you on what's best, depending on the trip.
The sweet spot for pregnancy travel is during your second trimester , between 14 weeks and 27 weeks. By the second trimester, any struggles you’ve had with morning sickness and fatigue during the earlier weeks of pregnancy should have hopefully subsided – and after 12 weeks, your risk of miscarriage decreases significantly as well. And you're not too far along to worry about third trimester exhaustion or going into preterm labor yet, either.
Your energy levels are likely to be good during your second trimester too (bring on the sightseeing!), and it will still be relatively easy and comfortable for you to travel and move around at this time. Keep in mind that once you hit that third trimester, pregnancy travel might be more difficult as you find it harder to move around and stay still for long periods of time.
It's complicated (and often a personal decision based on your own risk factors), but the CDC says that if you're fully vaccinated against COVID-19, you can travel. Of course, it's important you still do everything you can to keep yourself and others around you safe, including following all mask-wearing and social distancing guidelines in the destination you visit.
Women are at an increased risk for severe illness if they contract COVID-19 while pregnant , and they're more likely to experience preterm birth and other poor pregnancy outcomes. (This is why the CDC, the American College of Obstetricians and Gynecologists, and the Society for Maternal-Fetal Medicine all recommend that women who are pregnant, breastfeeding, or are planning on becoming pregnant get the COVID vaccine .)
If you're vaccinated and decide to travel, the CDC advises avoiding international destinations that are designated Level 4, due to high rates of local COVID-19 transmission.
Take all this information into account and talk to your doctor before you decide on where and when to travel while you're pregnant. And if you experience any symptoms of COVID-19, whether while traveling or at home, call your healthcare provider as soon as possible.
The guidelines for when to stop traveling while you're pregnant vary based on your mode of travel, but more or less, you should wrap up travel before you're 36 weeks pregnant.
Most airlines will let pregnant women fly domestically until they're 36 weeks pregnant – and many cut that off earlier for international travel. This rule is often enforced on an honor system policy, but some airlines may ask for a doctor’s note – so make sure you have that from your healthcare provider if you're traveling in the third trimester, just in case.
Most cruise ships don't allow travel after 24 weeks of pregnancy. Some cruise lines' cutoff dates vary, so verify policies before booking a cruise.
As for road trips, there's no official deadline for when you need to stop traveling, but your personal comfort level (physically and emotionally) – and your doctor's advice – might help you decide. You can drive while pregnant all the way up until your due date, but things may get considerably less comfortable on longer trips as you approach full term.
Travel of any kind requires advance preparation, but when you're pregnant and traveling, that pre-trip checklist gets a little longer. Give yourself a little more time than usual to plan for a trip – and use the tips below to stay safe and comfortable on your next adventure.
Before you travel
- Talk to your healthcare provider to determine if your trip is safe for you and if there are any medical concerns to consider. It's a good idea to discuss any activities you plan to do while you're away too. If you're planning an international trip, make sure to ask about any vaccines you may need for the areas you're visiting.
- Make sure you know your prenatal test schedule. Plan travels around any prenatal tests you need to schedule, including ultrasounds and other important screening tests.
- Book an aisle seat. You'll likely be more comfortable being able to get up to stretch or go to the bathroom on longer flights.
- Buy travel insurance. You don't need special travel insurance when you're pregnant, but it's never a bad idea to secure a policy. You may want to consider one with a “cancel for any reason” clause that reimburses you for money lost on cancelled trips for reasons (read: any reason) beyond what’s listed on the base policy. Check with your personal health insurance, too, to make sure it covers potential pregnancy complications while traveling internationally (some don’t). Consider adding evacuation insurance as part of a travel insurance plan, too.
- Gather your medical records and health information . If you’re in your second or third trimester, ask your ob-gyn or midwife for a digital copy of your prenatal chart, and have that easily accessible during your trip. Typically, this chart includes your age, your blood type, the name and contact information for your healthcare provider, the date of your last menstrual period, your due date, information about any prior pregnancies, your risk factors for disease, results of pregnancy-related lab tests (including ultrasounds or other imaging tests), your medical and surgical history, and a record of vital signs taken at each visit.
- Keep a list of key names and numbers you may need in the event of an emergency saved on your phone and written on a piece of paper (in case your battery dies).
- Have a contingency plan for doctors and hospitals that will take your insurance where you're going in case you go into labor early or experience pregnancy complications that require urgent care while you're away from home.
- Pack medicines and prenatal vitamins. That might include an extended supply of prescriptions and over-the-counter remedies , too. Bring enough to cover your entire trip and a written prescription that you can fill if you lose anything. It's a good idea to keep prescription medicine in its original container, so if your bags are searched it will be clear that you're not using medication without a prescription.
- Prepare for the unexpected. On a road trip, that might mean an unexpected breakdown, so join an auto club that provides roadside assistance. Download any apps you use for renting cars and accessing boarding passes before you leave so you can easily reschedule things in the event of a last-minute cancellation.
- If you're flying during your third trimester, be sure to call the airline to check about the cutoff week for pregnancy travel. A note from your doctor that says you’re cleared to travel is always good to have when traveling during your third trimester.
During your trip
- Drink plenty of water and continue to eat healthy foods . Keep in mind that many restaurants abroad commonly serve unpasteurized foods (like soft cheeses and milk), which can be dangerous for pregnant women due to the presence of listeria.
- Avoid eating raw or undercooked meat or fish , drinks with ice (which may be contaminated), non-bottled water, and other foods that can cause traveler's diarrhea, which can be more of a problem for pregnant women than other people.
- On long flights and drives, take time to stretch by pulling over for a walk or strolling up and down the airplane aisle. And when seated, always wear your seat belt .
- Maternity compression socks are handy to have along – both in transit and worn under your clothes while you’re out and about exploring – because they can ease the symptoms of swollen feet and legs. These are a few of our favorite pregnancy compression socks .
- Take advantage of help. Many countries have dedicated lines in shops and airports for pregnant travelers, so don't feel any shame taking a shorter wait if you see one.
- Go easy on yourself. Remember, you're growing a baby. You might not have quite the stamina for sightseeing and late nights like you used to pre-pregnancy. Make the most of your vacation but don't fret you miss out on things because you need more downtime from exploring than you usually would.
- Don’t forget to get photos of your bump. When your baby is older, you'll have fun showing them all the places you traveled with them before they were born.
- Go for the comfy shoes. Travel during pregnancy is the best reason ever to forgo those strappy stilettos for your favorite sneakers .
- Pack snacks so you always have something to curb your appetite if there’s a long wait for a restaurant or you get stuck in transit or someplace remote with no food offerings.
- Try to be in the moment with your travel partners as much as possible. Once your baby is born, your attention will be pulled in a whole new direction.
If you have any medical concerns traveling while pregnant, don’t hesitate to pick up the phone and call your doctor for advice. The below are a few symptoms that definitely warrant calling your ob-gyn or health care provider or seeking emergency care while traveling or at home:
- Signs of pre-term labor (including a constant, low dull backache, bleeding, etc.)
- Ruptured membranes (your water breaks)
- Severe cramping
- Spiking blood pressure
- Severe nausea or vomiting
- COVID-19 symptoms
Was this article helpful?
Best compression socks for pregnancy

Is it safe to fly while I'm pregnant?

Is it safe to travel to high altitudes while pregnant?

Placenta previa: Symptoms, complications, and treatment

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
AAFP. 2020. Ultrasound during pregnancy. American Academy of Family Physicians. https://familydoctor.org/ultrasound-during-pregnancy/ Opens a new window [Accessed April 2023]
ACOG. 2020. FAQ055: Travel during pregnancy. American College of Obstetricians and Gynecologists. https://www.acog.org/womens-health/faqs/travel-during-pregnancy Opens a new window [Accessed April 2023]
CDC. 2019. Pregnant Travelers. https://wwwnc.cdc.gov/travel/yellowbook/2020/family-travel/pregnant-travelers Opens a new window [Accessed April 2023]
CDC. 2022. Domestic Travel During Covid-19. https://www.cdc.gov/coronavirus/2019-ncov/travelers/travel-during-covid19.html Opens a new window [Accessed April 2023]
CDC 2023. International Travel During Covid-19. https://www.cdc.gov/coronavirus/2019-ncov/travelers/international-travel-during-covid19.html Opens a new window [Accessed April 2023]
CDC. 2022. Covid-19: Pregnant and Recently Pregnant People. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/pregnant-people.html Opens a new window [Accessed April 2023]

Terry Ward is a freelance travel, health, and parenting writer who has covered everything from flying with toddlers to why you should travel with your kids even when they're too young to remember it. She lives in Tampa, Florida, with her husband and their young son and daughter, and enjoys camping, sailing, scuba diving, skiing, and almost anything else done in the great outdoors.
Where to go next

Pregnancy Travel Tips
Medical review policy, latest update:, can you travel while pregnant , read this next, when should you stop traveling while pregnant, how should you prepare for a trip during pregnancy, what do pregnant women need to know about travel and the zika virus, travel tips for pregnant people, when should you seek medical care while traveling during pregnancy.
While traveling during pregnancy is generally considered safe for most moms-to-be, you’ll need to take some precautions before making any plans — and get the green light from your practitioner first.
What to Expect When You’re Expecting , 5th edition, Heidi Murkoff. WhatToExpect.com, Zika Virus and Pregnancy , October 2020. WhatToExpect.com, What to Know About COVID-19 if You’re Pregnant , February 2021. American College of Obstetricians and Gynecologists, Travel During Pregnancy , August 2020. Johns Hopkins Medicine, Traveling While Pregnant or Breastfeeding , 2021. Centers for Disease Control and Prevention, COVID-19 Travel Recommendations by Destination , May 2021. Centers for Disease Control and Prevention, Pregnant and Recently Pregnant People , May 2021. Centers for Disease Control and Prevention, Pregnant Travelers , December 2020. Centers for Disease Control and Prevention, Travel: Frequently Asked Questions and Answers , April 2021. Centers for Disease Control and Prevention, COVID-19 and Cruise Ship Travel , March 2020.
Jump to Your Week of Pregnancy
Trending on what to expect, signs of labor, pregnancy calculator, ⚠️ you can't see this cool content because you have ad block enabled., top 1,000 baby girl names in the u.s., top 1,000 baby boy names in the u.s., braxton hicks contractions and false labor.
Appointments at Mayo Clinic
- Pregnancy week by week
Is it safe to fly during pregnancy?
Generally, air travel before 36 weeks of pregnancy is considered safe for people who aren't dealing with any pregnancy problems. Still, if you're pregnant, it's a good idea to talk with your health care provider before you fly.
Your provider might suggest that you not fly if you have certain pregnancy complications that could get worse because of air travel or that could require emergency care. Examples include a history of miscarriage or vaginal bleeding, severe anemia, and high blood pressure or diabetes that's not well controlled. If you had preeclampsia during a previous pregnancy — a condition that causes high blood pressure and extra protein in urine — flying may not be advised. The same is true if you're pregnant with twins or other multiples.
Tell your provider how far you are flying, as the length of the flight might make a difference. Also, be aware that some airlines may not allow pregnant people on international flights. Check with your airline before you make travel arrangements.
After 36 weeks of pregnancy, your health care provider may advise against flying. And some airlines don't allow pregnant people to fly after 36 weeks. The airline also may require a letter from your health care provider that states how far along in your pregnancy you are and whether flying is advised.
If your health care provider says it's okay for you to fly, and your plans are flexible, the best time to travel by air might be during the second trimester. The risks of common pregnancy emergencies are lowest during that time.
When you fly:
- Buckle up. During the trip, keep your seatbelt fastened when you are seated, and secure it under your belly.
- Drink plenty of fluids. Low humidity in the airplane could cause you to become dehydrated.
- Avoid gassy foods and drinks before you fly. Gases expand during flight, and that could make you uncomfortable. Examples of foods and drinks to avoid include broccoli and carbonated soda.
- Think about medical care. Plan for how you'll get obstetric care during your trip if you need it. Bring copies of your medical information in case you need care while you're away.
Blood clots
Air travel can raise the risk for blood clots in the legs, a condition called venous thrombosis. The risk is higher for pregnant people. Moving your legs may help prevent this problem. Take a walk up and down the aisle every hour during the flight. If you must remain seated, flex and extend your ankles from time to time. In general, it's best to avoid tightfitting clothing, as that can hinder blood flow. Wearing compression stockings can help with blood circulation during a long flight.
Radiation exposure linked to air travel at high altitudes isn't thought to be a problem for most people who fly during pregnancy. But pilots, flight attendants and others who fly often might be exposed to a level of radiation that raises concerns during pregnancy. If you must fly frequently during your pregnancy, talk about it with your health care provider.
Mary Marnach, M.D.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Allergy medications during pregnancy
- AskMayoExpert. Health considerations for air travelers: Pregnancy considerations. Mayo Clinic; 2022.
- Air Travel During Pregnancy: ACOG Practice Bulletin No. 746. American College of Obstetricians and Gynecologists. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/08/air-travel-during-pregnancy. Accessed Dec. 1, 2022.
- Ram S, et al. Air travel during pregnancy and the risk of venous thrombosis. American Journal of Obstetrics and Gynecology. 2022; doi:10.1016/j.ajogmf.2022.100751.
Products and Services
- A Book: Obstetricks
- Available Solutions for Prenatal Nutrition from Mayo Clinic Store
- A Book: Taking Care of You
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- Ankle swelling during pregnancy
- Antibiotics and pregnancy
- Aspirin during pregnancy
- Pregnancy back pain
- Falling during pregnancy: Reason to worry?
- Fetal ultrasound
- Flu shot in pregnancy
- Headaches during pregnancy: What's the best treatment?
- Iron deficiency anemia during pregnancy: Prevention tips
- Leg cramps during pregnancy
- Pregnancy acne
- Pregnancy and fish
- Pregnancy constipation
- Pregnancy diet: Essential nutrients
- Pregnancy due date calculator
- Pregnancy exercises
- Pregnancy nutrition don'ts
- Pregnancy stretches
- Pregnancy weight gain
- Pregnant. Now What Happens?
- Prenatal testing
- Prenatal vitamins and pregnancy
- Sex during pregnancy
- Twin pregnancy
- Vaccines during pregnancy
- Vaping during pregnancy
- Working during pregnancy
- X-ray during pregnancy
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Expert Answers
- Air travel during pregnancy Is it safe
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
- Credit cards
- View all credit cards
- Banking guide
- Loans guide
- Insurance guide
- Personal finance
- View all personal finance
- Small business
- Small business guide
- View all taxes
You’re our first priority. Every time.
We believe everyone should be able to make financial decisions with confidence. And while our site doesn’t feature every company or financial product available on the market, we’re proud that the guidance we offer, the information we provide and the tools we create are objective, independent, straightforward — and free.
So how do we make money? Our partners compensate us. This may influence which products we review and write about (and where those products appear on the site), but it in no way affects our recommendations or advice, which are grounded in thousands of hours of research. Our partners cannot pay us to guarantee favorable reviews of their products or services. Here is a list of our partners .
Can You Fly While Pregnant? Not Always
Many or all of the products featured here are from our partners who compensate us. This influences which products we write about and where and how the product appears on a page. However, this does not influence our evaluations. Our opinions are our own. Here is a list of our partners and here's how we make money .
Table of Contents
Is it safe to fly while pregnant?
Airline restrictions for pregnant passengers, when not to fly while pregnant, can you fly internationally while pregnant, tips for flying while pregnant, flying while pregnant, recapped.
Do you want to plan a trip but aren’t sure if you should hop on a plane when you’re expecting? Is it okay to fly while pregnant? How late can you fly pregnant internationally? What are the important considerations to factor in when booking?
The short answer: Flying while pregnant is possible, so long as you and your doctor align on what is safe for you and your baby.
That said, flying when pregnant may be a bit more complicated, especially if you’re planning a trip close to your due date. Here’s what to keep in mind when plotting your next air-based excursion and traveling while pregnant.
According to the American College of Obstetricians and Gynecologists, most people experiencing healthy pregnancies can travel by air until quite close to their due date.
How close depends on several factors, including recommendations from your healthcare provider and airline rules, which vary between carriers.
So if you’re planning a trip, start by talking with your doctor before you book a ticket, as those experiencing high-risk pregnancies may be advised not to travel.
Your provider can perform an exam, check medical records and advise when, where and how far you should travel. Every pregnancy is different, and your doctor will consider your specific needs and concerns.
Keep in mind, you can travel during nearly any point in your pregnancy, though airline restrictions may prevent you from flying too close to your due date.
If you’ve been cleared to travel, ACOG recommends to do so is in the second trimester, between 14 and 28 weeks. That’s because any morning sickness may have lessened by then, and there’s a lower risk of miscarriage. Moving around or sitting for long periods in your last trimester can also become uncomfortable.
» Learn more : How to fly with your baby
Airline policies regarding pregnant travelers vary, but most don’t require any special documentation until late into pregnancy.
United Airlines allows pregnant travelers to board without medical documentation before their 36th week of pregnancy.
American Airlines allows pregnant passengers to fly without documentation up to four weeks before their due date.
Southwest Airlines doesn’t require any special documentation, but it doesn’t recommend travel after 38 weeks.
As you get closer to your due date, you’ll need to check with your airline, as many require special permissions to fly.
For example, on American Airlines you’ll need a doctor’s note to travel domestically within four weeks of your due date. For international travel, you’ll also need approval from a special assistance coordinator.
Airlines may provide specific guidance about what documentation is required, but typically this is a certificate from an obstetrician stating that you're fit for air travel for the dates of your trip.
Depending on the airline, the certificate might need to be dated within 48 or 72 hours of your scheduled departure, so you’ll need to plan ahead.
No matter which airline you’re flying with, check the restrictions and requirements if you’ll be booking close to the end of your third trimester.
While many pregnant travelers are fine to hop on a plane, there are others who should avoid air travel or be cautious about it.
This is especially true for those with the following conditions:
A history of blood clots or heart disease.
A history of miscarriage, premature labor or ectopic pregnancy.
Those carrying twins or other multiples.
First-time mothers who are over 35 years old.
This list is not exhaustive, which is why it’s always a good idea to talk with your doctor to find out if air travel is safe for you.
Pregnant travelers should also choose their destinations carefully. The U.S. Centers for Disease Control and Prevention recommends expectant mothers stay away from any regions with a high risk of contracting Zika or malaria or any locales where live vaccines are required or recommended for travel.
How long should your flight be if you’re flying while pregnant? The United Kingdom’s National Health Service states that flying for longer than four hours carries a small risk of blood clots.
So not only will a shorter flight be more comfortable, it’s also safer for you and your baby.
According to the CDC, some airlines will let you fly internationally until 36 weeks, but others may have an earlier cutoff. Generally, it’s wise to check the individual airline’s policies related to flying internationally while pregnant.
For example, British Airways allows passengers with one baby to fly until the end of the 36th week (or the end of the 32nd week if you’re pregnant with more than one baby). Meanwhile, Delta Air Lines has no requirements for pregnant passengers and only recommends checking with your doctor before flying.
In short: How late you can fly pregnant internationally varies from airline to airline.
Consider purchasing a separate travel insurance policy or booking your trip with a credit card that offers coverage as a perk if you want more flexibility to adjust travel plans. Cancel For Any Reason coverage is an add-on option that can refund you anywhere from 50% to 75% of any upfront deposits, depending on your specific policy.
» Learn more: The best travel insurance providers
Flying while pregnant may look and feel different, so to make travel as enjoyable as possible, consider taking a few extra precautions before heading to the airport.
Talk to your doctor about vaccines and immunizations : Depending on where you’re headed, it’s important to make sure you’re up to date on important vaccines.
Reduce your risk of poor circulation : Stay hydrated, wear loose clothing, get up to stretch or walk the aisle often and talk to your doctor about whether you should wear compression socks.
Book an aisle seat : This will offer you the option to get up, move around and use the bathroom as often as you need without disturbing seatmates. Alternatively, use this time as an excuse to book a first class ticket .
Bring a well-stocked first aid kit : While every traveler could benefit from packing a first aid kit, pregnant travelers may want to add items like nausea medication, hemorrhoid cream, treatment for yeast infections, personal medicines and prenatal vitamins.
Know where the nearest hospital is at your destination : Hopefully, you won’t need to visit during your trip, but knowing where it is can help ensure you can get to medical treatment quickly if needed.
Consider buying travel insurance : Should complications happen when you’re far from home, including premature labor, travel insurance can bring peace of mind. It may also save you money if you need to return home quickly for medical reasons. Just make sure to get a travel insurance policy that suits your needs.
» Learn more : Does travel insurance cover medical expenses?
Flying while pregnant is acceptable for most people during most pregnancies.
That said, before you book your ticket, check with your doctor to make sure you’re cleared to travel. Additionally, look into airline restrictions and requirements and make plans to help you be more comfortable while flying.
Following these steps will help you have a safe and enjoyable experience, whether you’re flying across the country or around the world.
How to maximize your rewards
You want a travel credit card that prioritizes what’s important to you. Here are our picks for the best travel credit cards of 2024 , including those best for:
Flexibility, point transfers and a large bonus: Chase Sapphire Preferred® Card
No annual fee: Bank of America® Travel Rewards credit card
Flat-rate travel rewards: Capital One Venture Rewards Credit Card
Bonus travel rewards and high-end perks: Chase Sapphire Reserve®
Luxury perks: The Platinum Card® from American Express
Business travelers: Ink Business Preferred® Credit Card

on Chase's website
1x-5x 5x on travel purchased through Chase Travel℠, 3x on dining, select streaming services and online groceries, 2x on all other travel purchases, 1x on all other purchases.
75,000 Earn 75,000 bonus points after you spend $4,000 on purchases in the first 3 months from account opening. That's over $900 when you redeem through Chase Travel℠.

1.5%-5% Enjoy 5% cash back on travel purchased through Chase Travel, 3% cash back on drugstore purchases and dining at restaurants, including takeout and eligible delivery service, and unlimited 1.5% cash back on all other purchases.
Up to $300 Earn an additional 1.5% cash back on everything you buy (on up to $20,000 spent in the first year) - worth up to $300 cash back!

on Capital One's website
2x-5x Earn unlimited 2X miles on every purchase, every day. Earn 5X miles on hotels and rental cars booked through Capital One Travel, where you'll get Capital One's best prices on thousands of trip options.
75,000 Enjoy a one-time bonus of 75,000 miles once you spend $4,000 on purchases within 3 months from account opening, equal to $750 in travel.

Travelling in pregnancy
With the proper precautions such as travel insurance, most women can travel safely well into their pregnancy.
Wherever you go, find out what healthcare facilities are at your destination in case you need urgent medical attention. It's a good idea to take your maternity medical records (sometimes called handheld notes) with you so you can give doctors the relevant information if necessary.
Find out more about getting healthcare abroad .
Make sure your travel insurance covers you for any eventuality, such as pregnancy-related medical care during labour, premature birth and the cost of changing the date of your return trip if you go into labour .
When to travel in pregnancy
Some women prefer not to travel in the first 12 weeks of pregnancy because of nausea and vomiting and feeling very tired during these early stages. The risk of miscarriage is also higher in the first 3 months, whether you're travelling or not.
Travelling in the final months of pregnancy can be tiring and uncomfortable. So, many women find the best time to travel or take a holiday is in mid-pregnancy, between 4 and 6 months.
Flying in pregnancy
Flying isn't harmful to you or your baby, but discuss any health issues or pregnancy complications with your midwife or doctor before you fly.
The chance of going into labour is naturally higher after 37 weeks (around 32 weeks if you're carrying twins), and some airlines won't let you fly towards the end of your pregnancy. Check with the airline for their policy on this.
After week 28 of pregnancy, the airline may ask for a letter from your doctor or midwife confirming your due date, and that you are not at risk of complications. You may have to pay for the letter and wait several weeks before you get it.
Long-distance travel (longer than 4 hours) carries a small risk of blood clots (deep vein thrombosis (DVT)) . If you fly, drink plenty of water and move about regularly – every 30 minutes or so. You can buy a pair of graduated compression or support stockings from the pharmacy, which will help reduce leg swelling.
Travel vaccinations when you're pregnant
Most vaccines that use live bacteria or viruses aren't recommended during pregnancy because of concerns that they could harm the baby in the womb.
However, some live travel vaccines may be considered during pregnancy if the risk of infection outweighs the risk of live vaccination. Ask your GP or midwife for advice about specific travel vaccinations. Non-live (inactivated) vaccines are safe to use in pregnancy.
Malaria tablets
Some anti-malaria tablets aren't safe to take in pregnancy so ask your GP for advice.
Zika virus is mainly spread by mosquitoes found in some parts of the world. For most people it's mild and not harmful, but can cause problems if you're pregnant.
If you are pregnant, it is not recommended to travel to parts of the world where the Zika virus is present, such as parts of:
- South and Central America
- the Caribbean
- the Pacific islands
Check before you travel
It's important to check the risk for the country you're going to before you travel.
Find out more about the Zika virus risk in specific countries on the Travel Health Pro website
Car travel in pregnancy
It's best to avoid long car journeys if you're pregnant. However, if it can't be avoided, make sure you stop regularly and get out of the car to stretch and move around.
You can also do some exercises in the car (when you're not driving), such as flexing and rotating your feet and wiggling your toes. This will keep the blood flowing through your legs and reduce any stiffness and discomfort. Wearing compression stockings while on long car journeys (more than 4 hours) can also increase the blood flow in your legs and help prevent blood clots.
Tiredness and dizziness are common during pregnancy so it's important on car journeys to drink regularly and eat natural, energy-giving foods, such as fruit and nuts.
Keep the air circulating in the car and wear your seatbelt with the cross strap between your breasts and the lap strap across your pelvis under your bump, not across your bump.
Road accidents are among the most common causes of injury in pregnant women. If you have to make a long trip, don't travel on your own. You could also share the driving with your companion.
Sailing in pregnancy
Ferry companies have their own restrictions and may refuse to carry heavily pregnant women (often beyond 32 weeks on standard crossings and 28 weeks on high-speed crossings ). Check the ferry company's policy before you book.
For longer boat trips, such as cruises, find out if there are onboard facilities to deal with pregnancy and medical services at the docking ports.
Food and drink abroad in pregnancy
Take care to avoid food- and water-borne conditions, such as stomach upsets and travellers' diarrhoea . Some medicines for treating stomach upsets and travellers' diarrhoea aren't suitable during pregnancy.
Always check if tap water is safe to drink. If in doubt, drink bottled water. If you get ill, keep hydrated and continue eating for the health of your baby, even if you're not hungry.
Find out about a healthy diet in pregnancy , and foods to avoid in pregnancy .
Page last reviewed: 17 August 2022 Next review due: 17 August 2025
Coronavirus (COVID-19): Latest Updates | Visitation Policies Visitation Policies Visitation Policies Visitation Policies Visitation Policies | COVID-19 Testing | Vaccine Information Vaccine Information Vaccine Information
Health Encyclopedia
International travel while pregnant or breastfeeding, special considerations for traveling while pregnant.
Traveling during pregnancy is normal, and a lot of women do it. But it's important to think about potential problems that could come up during international travel. Also think about how you would get quality healthcare in the countries you are visiting. Get all of the vaccines you need before becoming pregnant instead of waiting to get them during pregnancy.
The American College of Obstetricians and Gynecologists says the safest time for a woman to travel is in the second trimester of her pregnancy, from 14 to 28 weeks. This is the time when you will feel your best. You are also at the lowest risk for spontaneous abortion (miscarriage) or premature labor. During the third trimester (28 to 40 weeks), many healthcare providers and midwives advise staying within a 300-mile radius of home because of potential problems, such as high blood pressure, phlebitis, and false or preterm labor. Generally, women are not allowed to travel by air after 36 weeks for domestic travel, and after 28 to 35 weeks for international travel. The decision on whether to travel and how far to travel at any time during pregnancy should be a joint decision between you and your healthcare provider.
For most pregnant women, flying does not pose a risk to the fetus from cosmic radiation. But aircrew and women who often fly may exceed radiation limits.
According to the CDC, pregnant women with the following conditions may be advised against traveling to countries that need pretravel vaccines. This list may be incomplete. So discuss your health history with your provider or midwife before planning travel:
History of miscarriage
Incompetent cervix
History of ectopic pregnancy
History of premature labor or premature rupture of membranes
History of or current placental abnormalities
Threatened miscarriage or vaginal bleeding during current pregnancy
Multiple fetuses in current pregnancy
History of pre-eclampsia, high blood pressure, or diabetes with any pregnancy
History of infertility or trouble getting pregnant
Pregnancy for the first time over the age of 35 years
Heart valve disease or congestive heart failure
History of blood clots
Severe anemia
Chronic organ system problems that need to be treated
You may also be advised against traveling to places that may have hazards. The list below may be incomplete. Talk about your travel plans with your healthcare provider or midwife before planning a trip.
Places with high altitudes
Places that have outbreaks of life-threatening food- or insect-borne infections
Places where malaria is common
Places where live-virus vaccines are needed or recommended
Healthy tips for traveling while pregnant
Here are tips for traveling while pregnant:
Try to plan ahead for any problems or emergencies that could come up before you travel. Check that your health insurance is valid while you are abroad. Also check to see whether the plan will cover a newborn, should you deliver while away. You may want to think about getting a supplemental travel and medical evacuation insurance.
Research medical facilities in your destination. Women in the last trimester of pregnancy should look for places that can manage complications of pregnancy, pre-eclampsia, and cesarean sections.
If you will need prenatal care while you are abroad, arrange for this before you leave. Talk with your healthcare provider or midwife to figure out the best way to handle this.
Know your blood type and check that blood is screened for HIV and hepatitis B in the areas you will be visiting.
Check that safe food and beverages, such as bottled water and pasteurized milk, are available at your destinations.
If flying, ask for an aisle seat at the bulkhead. This gives you the most space and comfort. If morning sickness is a problem, try to arrange travel during a time of day when you generally feel well. Seats over the wing in the midplane region will give you the smoothest ride.
Try to walk every half-hour during a smooth flight. Flex and extend your ankles often to prevent blood clots in the veins (thrombophlebitis).
Fasten your seat belt at the pelvis level, below your hips.
Drink plenty of fluids to stay hydrated. Aircraft cabins have low humidity.
Try to rest as much as possible while away. Exercise and activity during pregnancy are important but try not to overdo it.
Special considerations for traveling while breastfeeding
Breastfeeding gives babies the most nutritional start in life. It also gives them vital protection against certain infections. But traveling internationally while nursing can be challenging.
If you are breastfeeding only, you don't have to worry about sterilizing bottles or having clean water. You may get vaccines to protect against disease, depending on where you are traveling. But diseases such as yellow fever, measles, and meningococcal meningitis may be a threat to infants who can't be vaccinated at birth. Discuss this with both your healthcare provider and your infant's caregiver before you travel.
If you are feeding your baby formula, it's best to use powdered formula made with boiled water. You may also want to carry a supply of prepared infant formula in cans or ready-to-feed bottles for emergencies.
Breastfeeding helps lower the chance of your baby getting traveler's diarrhea. If you get traveler's diarrhea, drink more fluids and continue to nurse your baby.
Watch your eating and sleeping patterns, as well as your stress levels. This will affect your milk output. Drink more fluids. Stay away from alcohol and caffeine, as well as exposure to smoke.
If you are traveling without your infant, you will need to pump to maintain your milk supply. Check with TSA about transporting your milk on flights.
Medical Reviewers:
- Donna Freeborn PhD CNM FNP
- Heather M Trevino BSN RNC
- Michele Burtner CNM
- Ask a Medical Librarian Make an Appointment Patient Education Medline Plus: Pregnancy

- Pregnancy Classes

Travel During Pregnancy
As long as there are no identified complications or concerns with your pregnancy, it is generally safe to travel during your pregnancy. The ideal time to travel during pregnancy is the second trimester . In most cases, you are past the morning sickness of the first trimester and several weeks from the third stage of pregnancy when you are more easily fatigued .
Is it safe to travel during pregnancy?
Traveling by air is considered safe for women while they are pregnant; however, the following ideas might make your trip safer and more comfortable.
- Most airlines allow pregnant women to travel through their eighth month. Traveling during the ninth month is usually allowed if there is permission from your health care provider.
- Most airlines have narrow aisles and smaller bathrooms, which makes it more challenging to walk and more uncomfortable when using the restroom. Because of potential turbulence that could shake the plane, make sure you are holding on to the seatbacks while navigating the aisle.
- You may want to choose an aisle seat which will allow you to get up more easily to reach the restroom or just to stretch your legs and back.
- Travel on major airlines with pressurized cabins and avoid smaller private planes. If you must ride in smaller planes, avoid altitudes above 7,000 feet.
- Although doubtful, the risk of DVT can be further reduced by wearing compression stockings.
The Royal College of Obstetricians and Gynaecologists and the International Air Travel Association recommend that expecting mothers in an uncomplicated pregnancy avoid travel from the 37th week of pregnancy through birth. Avoiding travel from 32 weeks through birth is recommended for women who have complicated pregnancies with risk factors for premature labor, such as mothers carrying multiples.
Risk factors that warrant travel considerations include the following:
- Severe anemia
- Cardiac disease
- Respiratory disease
- Recent hemorrhage
- Current or recent bone fractures
Traveling by Sea During Pregnancy
Traveling by sea is generally safe for women while they are pregnant; the motion of the boat may accentuate any morning sickness or make you feel nauseous all over again. There are a few considerations to make your trip safer and more comfortable:
- Check with the cruise line to ensure that there is a health care provider on board in case there are any pregnancy complications .
- Review the route and port-of-calls to identify if there is access to any medical facilities if needed.
- Make sure any medications for seasickness are approved for women who are pregnant and that there is no risk to the developing baby.
- Seasickness bands use acupressure points to help prevent upset stomach and maybe a good alternative to medication.
International Travel During Pregnancy
Traveling overseas has the same considerations that local or domestic travel has, but it also has additional concerns that you need to know about before making an international trip. The information below is provided to help you assess whether an international trip is good for you at this time:
- It is important to talk with your health care provider before you take a trip internationally to discuss safety factors for you and your baby.
- Discuss immunizations with your health care provider and carry a copy of your health records with you.
- With international travel, you may be exposed to a disease that is rare here in the United States but is common in the country you visit.
- Contact the Centers for Disease Control and Prevention at (800) 311-3435 or visit their website at www.cdc.gov to receive safety information along with immunization facts related to your travels.
- Diarrhea is a common concern when traveling overseas because you may not be used to the germs and organisms found in the food and water of other countries. This can lead to a problem of dehydration .
Here are some tips to avoid diarrhea and help keep you safe:
- Drink plenty of bottled water
- Used canned juices or soft drinks as alternatives
- Make sure the milk is pasteurized
- Avoid fresh fruits and vegetables unless they have been cooked or can be peeled (such as an orange or a banana)
- Make certain that all meat and fish has been cooked completely; if you are unsure, do not eat it
Travel Tips During Pregnancy
Whether you are going by car, bus, or train, it is generally safe to travel while you are pregnant; however, there are some things to consider that could make your trip safer and more comfortable.
- It is essential to buckle-up every time you ride in a car. Make sure that you use both the lap and shoulder belts for the best protection of you and your baby.
- Keep the airbags turned on. The safety benefits of the airbag outweigh any potential risk to you and your baby.
- Buses tend to have narrow aisles and small restrooms. This mode of transportation can be more challenging. The safest thing is to remain seated while the bus is moving. If you must use the restroom, make sure to hold on to the rail or seats to keep your balance.
- Trains usually have more room to navigate and walk. The restrooms are usually small. It is essential to hold on to rails or seat backs while the train is moving.
- Try to limit the amount of time you are cooped up in the car, bus, or train. Keep travel time around five to six hours.
- Use rest stops to take short walks and to do stretches to keep the blood circulating.
- Dress comfortably in loose cotton clothing and wear comfortable shoes.
- Take your favorite pillow.
- Plan for plenty of rest stops, restroom breaks and stretches.
- Carry snack foods with you.
- If you are traveling any distance, make sure to carry a copy of your prenatal records.
- Enjoy the trip.
Want to Know More?
- How to Treat Jet Lag Naturally During Pregnancy
Compiled using information from the following sources:
1. Planning Your Pregnancy and Birth Third Ed. The American College of Obstetricians and Gynecologists, Ch. 5. William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 8.
2. Royal College of Obstetricians and Gynaecologists, Air Travel and Pregnancy (Scientific Impact Paper No. 1), https://www.rcog.org/uk, May 22, 2013.
BLOG CATEGORIES
- Can I get pregnant if… ? 3
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Breastfeeding 29
- Changes In Your Body 5
- Cord Blood 4
- Genetic Disorders & Birth Defects 17
- Health & Nutrition 2
- Is it Safe While Pregnant 54
- Labor and Birth 65
- Multiple Births 10
- Planning and Preparing 24
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Pregnancy Health and Wellness 149
- Pregnancy Products & Tests 8
- Pregnancy Supplements & Medications 14
- The First Year 41
- Week by Week Newsletter 40
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Paternity Tests 2
- Pregnancy Symptoms 5
- Prenatal Testing 16
- The Bumpy Truth Blog 7
- Uncategorized 4
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Women's Health 34
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
Share this post:
Similar post.

Preconception Wellness - Prepare for the Unexpected

Leg Cramps During Pregnancy

Prenatal Vitamin Limits
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
Traveling Abroad while Pregnant: Firsthand Advice from a Pregnant Travel Addict
When I told people that I was planning to travel to a foreign country while 7 months pregnant, I got looked at like I was crazy. The look turned into shock when they heard I was going to a developing country: Egypt.
“Is it safe to travel while pregnant?”
“Can you fly while pregnant?”
“What if something happens???”
There are some legit concerns about traveling abroad while pregnant – but those can easily be addressed by making some smart travel choices and precautions.
This is NOT Your Last Chance to Travel
Apparently, most people believe that their lives come to a screeching halt once they have a baby. They have to travel “while they still can.” There is even a name for these pregnancy holidays – a “ babymoon .”
Fear that this is your “last chance to travel” is a terrible reason to plan a trip!!!
It is perfectly possible to travel with a baby . In some ways, traveling with a baby is even more fun (such as how you get priority treatment and meet locals easier). So don’t feel pressured to rush out and take a trip “while you still can.” There will be plenty of opportunities to travel later on.

Get the Timing Right
I am one of those unlucky women who gets hyperemesis gravidarum during pregnancy. Don’t confuse HG with morning sickness. I’m talking about puking blood because the vomit has eroded your throat. I’m talking about getting IV transfusions because I couldn’t keep water down…
So it was a bad mistake to go backpacking while 4 weeks pregnant . I ended up having to cut the trip short. It’s no fun puking all over the trail!!!
But, because this was my second pregnancy, I knew that I would probably stop puking at 6 months. So that’s when I planned my Egypt trip for.

You don’t know how you’ll feel as pregnancy progresses, so here’s what I’d recommend about planning a trip abroad:
- Go during months 6 or 7: In general, these are the best months for most pregnant women. The hormones and morning sickness have leveled off, but you aren’t so huge that you tire easily.
- Wait until the last minute to plan your trip: If possible, hold off on planning your trip until you know how you feel.
- Check refund policies: Most travel insurance policies don’t allow pregnancy as a reason for cancellation . So, be sure you understand cancellation/refund policies. Otherwise you’ll be out a lot of money if you decide to cancel the trip because you feel too crappy.
You Probably Can’t Get Travel Health Insurance while Pregnant
One of the biggest issues with traveling abroad while pregnant is that almost no travel insurance company will give coverage to pregnant women.
If something happens while on your trip, you’ll be stuck with the bill!
Consider the case of Jennifer Huculak-Kimmel and her “ million dollar baby .” The Canadian couple were on vacation in the USA when Jennifer went into premature labor. Two months in the ICU ran up a hospital bill of $950,000 – none of which was covered under her insurance policy!
I admit that the idea of being saddled with a huge hospital bill terrified me. Before going to Egypt, I intensely researched the cost of giving birth there, as well as how much a night in ICU would cost. Egypt is a poor country, so the costs weren’t too high – so I was willing to take the risk.
Know Airline Policies for Pregnant Women

Flying while pregnant is perfectly safe . The real reason that airlines put restrictions on flying while pregnant is because they are afraid you will give birth in the air.
Thus, a lot of airlines won’t let pregnant women fly after 36 weeks (or 32 weeks if you are having multiples). You may need a doctor’s note before being allowed to fly. This was the case with Air Cairo. The note had to be no more than 7 days old, so I actually had to visit a gynecologist while in Egypt – which was actually a cool part of the trip.
You can find a good breakdown on airline pregnancy restrictions here .
Choose the Right Climate
Since you are already going abroad, you might as well choose an agreeable climate! The entire reason we chose Egypt for our trip was because it was January.
While everyone else was battling snow, we were swimming in the Red Sea!
However, there is no way in hell that I’d go to Egypt in summer while pregnant. For a summer trip, I would have chosen a cooler country like Norway or gone into the mountains.

Only Plan ONE Activity Per Day
In general, I’m not the type of traveler who tries to see/do a zillion things. But I knew to take it even easier while pregnant.
I made a list of the things I absolutely wanted to do in each destination. Then planned to do just one per day. Some days we managed to do more than one thing, but only if I still felt up to it. This kept the pace relaxed so I didn't inadvertently overexert myself.
Consider the Bathroom Situation
One piece of travel advice for pregnant women which commonly gets overlooked is the bathroom situation. Since pregnancy makes you pee like crazy, this is not something which should not be overlooked.
Going to the bathroom actually ended up being the hardest part of traveling abroad while pregnant. After this ordeal, here’s what I’d recommend to other pregnant travelers:
- Make sure you can squat: Public bathrooms aren’t exactly known for their cleanliness – do you really want to sit on them? If you can’t squat over them, you are going to be in for some trouble. Squats are great exercises for preparing for childbirth anyway. 😉
- Consider a pee funnel: If you can’t squat, then get a pee funnel . This makes it possible to pee standing up.
- Map out some nicer restaurants: As is the case in many developing countries, it was very hard to find a bathroom in Egypt. The local restaurants didn’t have bathrooms (seriously!) and cafes usually only had a bathroom for men (which might just be a bucket in a corner!!!). The tourist restaurants consistently had nice bathrooms, so I mapped these out so I knew where to go to pee.
- Carry TONS of wet wipes and antiseptic gel: Once you have a baby, you’ll be carrying tons of these anyway. 🙂 For traveling abroad, these come in handy for wiping down disgusting surfaces and sanitizing your hands – don’t expect soap in every bathroom!


Budget for Luxury Transportation
Normally I’m fine taking cramped minibuses and crowded trains. But, at 7 months pregnant, I wasn’t keen about shoving into Egypt’s crowded local transportation.
It probably would have ended with me puking or passing out. Or, worse, someone banging into my stomach.
Luckily we were able to afford taxis everywhere (we used Uber to avoid haggling with the crooked taxi drivers). We took things a step further and even hired a private driver to take us between cities.
Since it was Egypt (and not, for example, Norway), it wasn’t too expensive. In developed countries, this sort of luxury travel will definitely cost more.
Even a short taxi ride each day in somewhere like Europe can add a huge amount to your travel budget. But in developed countries the public transportation won’t be as crazy. So really think about the cost vs. hassle of public transport and budget your trip accordingly.

Some Activities Will Be Off-Limits While Traveling Pregnant
In the weeks before my Egypt trip, I was Googling things like “Can you ride a camel while pregnant?”
It turns out that riding a camel is a relatively safe activity while pregnant (riding a horse, however, is not). But, to play it safe, I still decided not to ride a camel while at the pyramids.
I also had to pass on sandboarding, quad biking, and going into certain tombs (because of low oxygen levels inside). Unfortunately, it was only after I got into a jeep on our excursion into the desert that I realized that off-roading might be off-limits too! Luckily, the ride wasn't too bumpy — but I still held on tightly to prevent my stomach from getting bounced too much.

Playing It Safe with Food while Pregnant
Another major concern I had about traveling to Egypt (or any developing country) while pregnant was getting a stomach bug from tainted water or food.
Most of the time, food poisoning while pregnant isn’t particularly danger. The biggest risk is that you’ll get dehydrated.
The best thing to do is avoid food poisoning in the first place:
- Only drink safe water. I stuck to bottled water. I also have a Sawyer Mini water filter in case bottled water isn’t available.
- Remember to avoid ice cubes and juices too! Unless you know these were made with safe water, don’t drink them.
- Be cautious about street food. My doctor told me to not eat any street food. But that’s half the fun of traveling abroad! So I instead was careful about the street food I ate. I stuck with thing that were deep fried since this would have killed most bacteria. I’m vegetarian, but would have avoided all street meat regardless.
- Take probiotics the first few days. This will help your body adjust to and combat any “bad” bacteria it comes in contact with.
In case you do develop a stomach bug, the CDC says it is best to wait for it to go away on its own (if it’s severe, that’s when you’ll want to contact a doctor). You’ll need to stay hydrated while waiting for the diarrhea and vomiting to subside.
My traveler’s first aid kit is always stockpiled with electrolytes. It also has activated charcoal and other remedies for food poisoning.

Enjoy the Memories
Taking a trip while I was 7 months pregnant was by far the best decision I made – for both me and my family.
It was a much-needed break from all the pregnancy woes. For the first time in months, I stopped frantically Googling everything pregnancy related. I was able to RELAX and enjoy myself!
Even more importantly, I was able to spend some quality time with my husband and older daughter.
If I had a high-risk pregnancy, then I wouldn’t have done the trip. But for any other pregnant travel addicts who need a break from focusing on their growing baby, a trip is great for your mental health.
My only regret is that I didn’t take more photos using my bump. It would have been great to have a funny picture of my belly with a pyramid coming out of it. 🙂
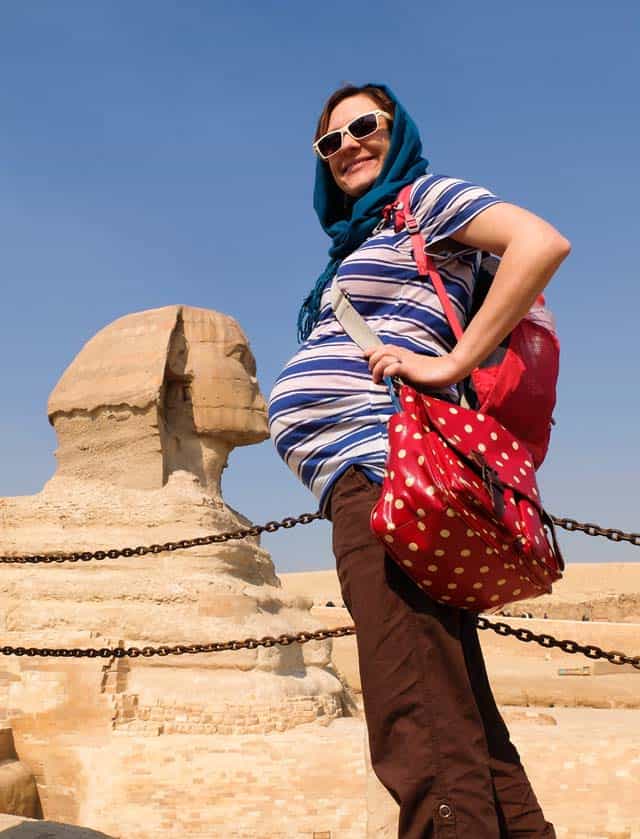
Have you traveled abroad while pregnant? What tips would you add?
Image credit: squat toilet , by Maksym Kozlenko , Creative Commons Attribution-Share Alike 4.0 International license
Sharing is caring!
1 thought on “Traveling Abroad while Pregnant: Firsthand Advice from a Pregnant Travel Addict”
Pingback: Traveling Abroad while Pregnant: Firsthand Advice from a Pregnant Travel Addict – Cuddle Baby
Comments are closed.
What to expect when traveling in each trimester of pregnancy

So you're pregnant? Congrats! It's an exciting time but also one in which many aspects of your life will begin to change, including travel. While you'll quickly need to understand the airline industry's rules for flying while pregnant , there are some more personal tips I'd like to share with you based on my experience traveling throughout the first, second and third trimesters of both of my pregnancies.
A few truths about pregnancy
Picky, starving moms need to travel with snacks.
I didn't know I was pregnant when I took the first flight of my second pregnancy. I was on a mileage run from Houston to Los Angeles, and by the time we landed, I was super tired, kinda grumpy and oh-my-so-hungry.
Then began a mad search for food. Luckily, Counter Burger was open and serving up sweet potato fries and burgers. Out of habit, I went for the veggie burger but I quickly regretted my decision, which left me far from satisfied with ground-up veggie mush.
In the early stages of pregnancy, your normal travel habits of going a little hungry for a while, or making due with what's around, may not work well.
Throughout your pregnancy, travel with water to stay hydrated and snacks to stave off hunger pangs and keep you going through travel delays. If you're feeling particularly food sensitive, research the food options at your destination ahead of time. I virtually lived on chicken noodle soup for a whole week early in my pregnancy and then, for a couple of days, all I wanted were hush puppies. I know how to get those items at home but when you are on the road, you either need to do more research or be more flexible -- which is sometimes easier said than done.
Related: 4 tips for planning travel while planning a pregnancy
Research and make choices about inflight radiation and other risks
I'm not an expert, but because I fly often, I have given some thought to inflight radiation exposure , especially during the early stages of pregnancy.
For pregnant flight attendants and pilots, the Federal Aviation Administration recommends a limit of 1 mSv during pregnancy, with no more than 0.5 mSv per month. I don't fly as much as an airline employee, but it doesn't take much research to learn that the amount of radiation you (and your gestating baby) are exposed to in the air varies dramatically from route to route. The highest-level routes are typically longer, higher-altitude polar routes. Here's some information from NASA about polar flights and radiation .
Every expectant mother should discuss the risks of flying during pregnancy with her doctor before getting on a plane. For me, nine months was a tiny moment in my traveling life, so I was OK adjusting my behavior a bit out of an abundance of caution. However, I didn't adjust to the point of never leaving my house. We still flew when I was pregnant, but I was judicious about when and where I would fly.
Check your health insurance policy
If you aren't familiar with your medical insurance coverage for when you travel, brush up on those facts now. Look at in-network and out-of-network benefits, as well as coverage for procedures for medical emergencies in other countries, if relevant. Most likely, if you do have coverage for treatment in other countries, you will still be on the hook to pay for your care up front and then submit for reimbursement from your health insurer. Plan accordingly and plan for the unexpected. If your baby decides to arrive early, for instance, check to make sure your insurance would cover possible extended and expensive care in an intensive care unit in a hospital away from your home.
Be sure to check what your health insurance coverage provides if you deliver at another facility later in your pregnancy. I once had an insurance plan that specifically did not cover out-of-network deliveries after 36 weeks, so that is something you would want to know before venturing away from home late in pregnancy.
Consider travel insurance
Trip insurance can be helpful if you are traveling while pregnant. Read the plan's fine print to determine what might be covered and whether you are covered if you already knew you were pregnant when you purchased the plan. Typically, a normal pregnancy or normal delivery would not be covered but if there are unexpected complications with the pregnancy, then related trip-cancellation or trip-interruption coverage may kick in on certain plans in certain situations.
Here are some travel insurance providers to check out: Allianz Travel Insurance, Travel Guard and Travelex Insurance . You can also compare a variety of plans at a portal like SquareMouth .
Here are some articles that will help you brush up on your travel insurance knowledge:
- The best travel insurance policies and providers
- What is independent travel insurance and when is it worth it?
- When to buy travel insurance versus when to rely on credit card protections
- Is credit card travel insurance sufficient on its own?
- Why I buy travel insurance
Traveling in the first trimester
Traveling in the first trimester can range from "no big deal" to "I think I'm going to die from misery right this very instant." Symptoms in early pregnancy can vary widely and can change by the day. A flight in your first trimester may be no different from any other flight you've ever taken or it may feel like you are flying with the worst hangover of your life.
Unless you are very high risk or have other extenuating medical issues, your doctor will probably give you the green light to travel in early pregnancy. Feeling extra tired, nauseous and queasy doesn't make for the perfect travel experience, so here are some tips to make travel easier:
Pick an aisle seat and move about the cabin
When you do hit the skies early on, choose a seat where you will be the most comfortable, likely an aisle seat so you can get to the restroom easily. I also recommend getting up to walk around and stretch your legs. (Here are tips for credit cards that will defeat basic economy and let you get a seat assignment in advance.)
Room service come to the rescue
In my first trimester of my second pregnancy, I went on a trip with my daughter and parents to New York City to see the Macy's Thanksgiving Day Parade and I was met with another challenge. I was at the point in my pregnancy when I needed food immediately upon waking or I was going to get queasy. Since I was staying in a hotel room with my young daughter, this meant room service. I also had granola bars and fruit on hand, but that was not enough to really do the trick some mornings. Had my husband been there, he could have gone in search of a warm bagel and juice, but since he wasn't on this trip, we had to improvise. Thanks goodness Marriott elite status helped defray the cost of most of the breakfast!

Take it easy when you need to
Once you are further along in your pregnancy and you actually look pregnant, you will sometimes get a little sympathy or, at least, empathy while traveling. Strangers may offer to help with your bag and people may have more patience with you if you're moving slowly. However, in the first trimester nobody can tell you are pregnant, and no one is going to feel sorry for you. If you act queasy on the plane, you will pretty much be treated like you have Ebola, and any other issue or ailment will pretty much not interest anyone. I once told the flight attendant I was pregnant when she was giving me the eye about looking queasy.
Take care of yourself, don't overdo it and know when to say enough is enough. You may be used to very busy travel days, but now find yourself needing a nap during your first trimester, and that's OK. Listen to your body and adjust accordingly.
Traveling in the second trimester
You have probably heard that the second trimester is generally the easiest of the three trimesters for most expecting moms. You usually aren't as sick and or as tired as in the first trimester, and you aren't as large, uncomfortable and exhausted as in the third trimester. From roughly weeks 13 to 27 of a pregnancy, your activity and comfort levels are often good, and this means that it can be a great time to travel. Couples that like to take "babymoons" (one last couples trip before the baby arrives) often try to schedule them in the second trimester.
Related: The best babymoon destinations for every month of the year
The beginning and end of the second trimester are quite different
You will probably enter the second trimester not really looking pregnant, and end it looking quite different. This means that you may feel very different at the beginning and end of the second trimester. The second trimester is when lots of belly growing happens and this can mean that some types of travel will be more uncomfortable toward the end of these few months of pregnancy than at the beginning.

Consider where you are comfortable traveling
A very personal and important decision to make during the second trimester is to determine if there are certain restrictions you will place on yourself in terms of where you're comfortable traveling. Some types of travel will ban women from traveling during the second trimester. For example, many cruise lines will not allow a woman to book a cruise if she will enter her 24th week of pregnancy (or later) while on the voyage.
Royal Caribbean's policy bars pregnant women from sailing at and after the 24th week. It was developed in concert with the Cruise Lines International Association endorsement of the American College of Emergency Physicians Health Care Guidelines for Cruise Ship Medical Facilities .
Many consider unborn fetuses to be viable if born beginning around 24 weeks (though that age threshold is getting earlier and earlier). This means that a baby born at 24 weeks gestation would have anywhere from a 50% to 70% chance of survival outside the womb if (and only if) there is immediate access to advanced medical care. A cruise ship clearly doesn't have an advanced neonatal care unit on board, so presumably the policy is related to why cruise lines draw the line for pregnant passengers.
I personally draw the line for travel at 23 or 24 weeks when talking about destinations that don't have the same level of advanced medical care as the United States -- or long flights or a flight path that could hinder prompt access to advanced medical care if I happened to unexpectedly go into labor. The Maldives is an example of somewhere I would not want to travel in this instance because there would be significant delays in obtaining medical care on these remote islands.
Plan big, but not too big
The second trimester is a great time to squeeze in a pre-baby trip or two since you will probably feel relatively like to your pre-pregnant self much of the time. We went to Aruba when I was 14 weeks pregnant and it was a fantastic trip. I had lots of energy and a normal appetite. Flying was not uncomfortable because my belly was still pretty small and the only real adjustment was to make sure I had a somewhat larger bathing suit before the trip.
At 23 weeks, I traveled to Spain and still felt pretty energetic and "normal." I will admit that the flight in economy wasn't super comfortable since I did have a belly that was hindering curling up in positions that usually help me sleep on the plane, but our time on the ground in Spain wasn't really impacted at all by the pregnancy other than missing out on the Spanish wine.
The great thing about both of those trips was that they were at my own pace. This meant that if I didn't feel like doing much one afternoon, I could take it easy. Even though you may feel great in the second trimester, you can still tire more quickly than normal, so be sure to limit your vacation activities to those you can manage. There are also activities that some doctors might advise against by the second trimester like thrill rides, scuba diving or horseback riding, so double-check any restrictions before planning more adventurous outings.

Traveling in the third trimester
Pregnancy isn't an illness or disease. For many families, it's just a normal phase in a woman's life before a new baby joins the family. Assuming things are going well, it's not a time when you have to cancel all travel. However, once the third trimester rolls around, travel can get a more complicated and does eventually have to stop.
The beginning and end of the third trimester are quite different
Changes come even more quickly in the third trimester. You enter the third trimester about 28 weeks pregnant and end it with a newborn. This means that types of travel that are possible at 27 and 28 weeks pregnant may be inadvisable, or even prohibited, at 37 and 38 weeks pregnant.
Select destinations and activities carefully
In the final months of pregnancy, some activities are probably going to be more comfortable and enjoyable than others. For example, swimming and spa time may be exactly what you need.
I give strong preference to visiting beach and resort destinations in the final trimester. Trust me when I say that few activities are as comfortable in the third trimester as floating in the water! We went to The Phoenician (a Marriott property) in Scottsdale, Arizona, when I was about 31 weeks pregnant and even with my big belly, it was the perfect mix of spa, swimming and fun activities for our 5 year old before both our lives changed.

You are going to get uncomfortable
Maybe this isn't universal and there are some magical creatures out there who never feel uncomfortable during pregnancy, but every mom I know eventually hit a point in her pregnancy when she wasn't comfortable. For many, this means that sitting for an extended time in a small airline seat, standing in long lines or trekking around in the heat to explore a city all day eventually become pretty miserable activities.
No one can tell you when you will hit that point, but it will likely happen in the third trimester. For me, my back started giving me a bunch of trouble at around week 30 or 31. I was incredibly grateful there were no more flights scheduled during that pregnancy beyond that point.
If you are going to fly during the later weeks of your third trimester and have the ability to secure a more comfortable seat up front, or at least one with extra legroom so you can stretch out, it may well be a good investment in your comfort. I brought a tennis ball with me when I flew so I could give myself a bit of a "back massage" against the airplane seat.

Bring your own pillows
Sleep becomes a challenge in the third trimester for many women and a pillow fort of sorts becomes a necessity to get some good shut-eye. Many pregnant moms find that using some sort of body pillow or pillow arrangement helps to keep their bellies supported and comfortable at night. You can't assume that the hotel will have similar pillows, so bring your own if they become essential to good rest in your third trimester. I had no shame in hauling my pillow fort with me on our last road trip at eight months pregnant.
See if you are allowed to fly
Even if your doctor OKs it, many airlines have rules about women flying in the third trimester. Check out airline rules for traveling while pregnant for complete details, but generally speaking, most U.S. airlines don't have many flight restrictions until the last month of pregnancy. However, many international airlines do have restrictions and documentation requirements beginning at 28 weeks. If you are pregnant with more than one baby, the restrictions kick in even earlier.
Decide when to stop traveling
I'm all for traveling while pregnant but, realistically, most women will want to stop traveling at some point in the third trimester. I would imagine by about 36 or 37 weeks, most women will probably decide to stay closer to home. I went on a road trip about three hours from home at 35 weeks and then called it quits for the rest of the pregnancy. There's still a whole new world of travel waiting once a new baby joins the family .

Bottom line
There is usually no reason to stop traveling when you're expecting. During my last pregnancy, I went on 12 trips, 28 flights, visited four countries and I'm very glad I had the opportunity to stay that active. I'm also glad that I grounded myself from flight after 31 weeks and from road trips at 35 weeks because those were the right decisions for my comfort level.
Ticket for Two – International travel during pregnancy

By Stacie Dunkle
“We don’t recommend international travel during pregnancy for first-time mothers,” said my nurse midwife. Those words stopped me in my tracks. As an officer in the Epidemic Intelligence Service with three years of experience working overseas, I couldn’t believe what this nurse was telling me. Rarely a month went by that I wasn’t waiting in a security line at the airport. “Why?” I asked. I was up-to-date on all of my vaccines, even yellow fever, which I knew shouldn’t be given during pregnancy, and I was well-practiced in methods for staying healthy in developing countries (wearing seatbelts and avoiding untreated drinking water, food from street vendors, raw vegetables, etc.). I began to wonder how I was going to break the news to my supervisor that I wouldn’t be able to conduct the investigation we were planning in Nepal in two weeks. We had been preparing for over a month. Our colleagues on the ground were ready to go, and my plane tickets were already booked.
Reality Check
When my partner and I decided to have a baby, I knew that once our little one arrived, my life would change dramatically. There would be no more hopping on planes to far-off places during public health emergencies—I’d have to think about who would watch my baby and how I’d cope with potentially missing all those precious moments with him. Still, the decision was easy since I had always wanted to have children and I was finally at a point in life when the timing felt right. Pregnancy can be a difficult thing to plan, of course, so when it did happen, somehow it still felt unexpected. Even more unexpected was how much my life was suddenly changing before the baby had even arrived.

“You’ll be taking a big risk,” the nurse said. “You can’t take any of the drugs we usually prescribe to prevent malaria.” Although most pregnant women can take a drug called mefloquine to prevent malaria, I couldn’t take it because of my personal health history. I wasn’t just thinking about myself anymore; I also had to consider my baby. Because of the serious risk associated with getting malaria during pregnancy, I decided it was best to cancel my trip.
Of course, my supervisor was very understanding. He had been planning to travel to Nepal as well, and with his guidance, our partners were able to carry out the investigation on their own. Although I was disappointed to not participate fully, I changed my focus to health issues that were closer to home and still traveled quite a bit. During my second trimester, I flew to Mexico, Ohio, Michigan, Canada, Arizona, and Florida. It’s too bad I couldn’t get double the frequent flyer miles while traveling for two! During these flights, I avoided lifting heavy baggage, always requested an aisle seat, and was careful to drink plenty of fluids and walk around every 30 minutes or so. Of course, the latter was no problem since I had to use the restroom that often anyway! I enjoyed traveling while pregnant and laughed thinking that my baby would be born already familiar with the sound of jet engines and having memorized the safety features aboard aircrafts.
The Home Stretch
When my third trimester arrived, I was offered an opportunity to travel to Lima, Peru to attend a training summit. It would be a valuable trip for me professionally because it would provide background for a project I was working on. I would be able to network with colleagues and focus my work to make it more useful to them. When I looked at the dates for the trip, I realized I would be 33 weeks pregnant upon departure and staying for a little over a week. I hesitated because many physicians don’t recommend traveling after 32 weeks, and most airlines restrict travel after 36 weeks for single, uncomplicated pregnancies. I was fortunate to have been very healthy during pregnancy and decided the trip was worth the risk, but swore I would cancel if any concerns came up before departure.
I still took a number of precautions before I committed to traveling. These included getting approval from my certified nurse midwife and reviewing CDC’s website of “ Health Information for Travelers to Peru .” My biggest concern was premature delivery in an unfamiliar country where Spanish is the primary language. My experience with Spanish is limited to high school classes and a few weeks traveling in Spain and Mexico. If I had to ask anything more than, “Dónde están los baños?” I would be out of luck; that included trying to describe symptoms I might be experiencing to a doctor. Fortunately, I have a friend who had just recently moved back to the US after living in Lima for a year. She was able to provide local English-speaking contacts and recommended an obstetrician and hospital where I could receive care. I also checked to make sure my health insurance would cover any medical expenses I might have had while travelling.

To everyone’s surprise, I went into labor six days later. My mind raced with questions. Will my baby be healthy arriving at 35 weeks? What would have happened if I had gone into labor in Peru without the support of my loved ones? After reviewing my medical records, my midwife predicted that my due date was off by at least a week and I was closer to full term than we had originally thought. My son was born the following night, completely healthy, into the loving arms of his mother, father, and grandparents. The question I kept asking myself was: if I had it to do again, would I have travelled so far knowing I was so close to delivery?

What do you think?
We want to hear from you. Have you traveled during pregnancy or had to pass on a trip because you were expecting? How has being a parent changed your career?
If you would like more information on traveling during pregnancy please visit http://wwwnc.cdc.gov/travel/yellowbook/2012/chapter-8-advising-travelers-with-specific-needs/pregnant-travelers.htm
15 comments on “Ticket for Two – International travel during pregnancy”
Comments listed below are posted by individuals not associated with CDC, unless otherwise stated. These comments do not represent the official views of CDC, and CDC does not guarantee that any information posted by individuals on this site is correct, and disclaims any liability for any loss or damage resulting from reliance on any such information. Read more about our comment policy » .
I was a little over 20 weeks pregnant with our first. We lived in Seoul, South Korea at the time. We were coming back to the states to visit for Christmas vacation. I was less then enthused about enduring a long 20 hour travel time haul to Boston. I have to say, we flew on Korean Air and it was a wonderfu! From my experience the flight crew on international airlines take great care of their passengers, especially the pregnant women!
Do you regret missing overseas opportunities and wish you had gotten pregnant after EIS?
(From Author Stacie Dunkle) Not at all. EIS is about developing skills to respond to disease outbreaks that occur both here in the US as well as internationally. It’s very important to me to have a balance of career and family. Thank you for your question!
We are currently a year into a journey the length of the Andes from Ushuaia to the the north of Colombia, and my wife became pregnant in Peru. We are frustrated by the lack of coherent advice available. Apart from the not at all helpful ‘Don’t go if you are pregnant’ which you encountered, we have read widely differing reports of risk levels in Colombia. Advice as to the safe altitudes varies from ‘anything above 800m to >1700m. The British seem to have Colombia as low risk for chloroquine resistant malaria anywhere outside the Amazon. The WHO have high risk areas in the Amazon AND along the pacific coast with particular pockets of danger near Panama and Venezuela. As we are travelling by vehicle the oft trotted out advice that you are safe in all cities is of no comfort to us as we have to drive between them through rural areas.
Another dilemma is what anti-malarials are safe in pregnancy. Mixed reports on Mefloquine although the CDC have just come out saying it’s safe (reflecting new FDA guidelines) despite reports of teratogenicity in rats. We tried the top three hospitals in Quito and none had anything but chloroquine despite Ecuador also having choloroquine resistant malaria. The official line from all of them is denial…that there is no malaria in Ecuador. We’re finding the same thing in Colombia…”As long as you don’t go to the jungle there’s no malaria here. Just use DEET (also contraindicated in pregnancy) and wear long sleeves and don’t go out after dusk”. My experience of the tropics is that determined mosquitoes are rarely put off by repellents for long.
If we can find mefloquine we’ll take it but we have major concerns. Data may show that there is little chance of teratogenicity or increased risk of still birth but it is well known for serious neurological side effects such as anxiety and depression and it does cross the placenta. So what affect does it have on a developing brain? No one knows. We have also read that chloroquine along with proguanil might be a safe alternative although proguanil suppresses folic acid so the advice is to take 5mg Folic acid a day which is basically an entire packet at the dosage strengths available here! It may be a blind alley anyway as we haven’t seen proguanil on sale here yet.
We are also facing up to the fact that we may also have to alter our plans due to lack of clear guidance and safeguards.
On the plus side Echo scans are very easy to get here and in these days of internet getting hold of literature on pregnancy has been no problem. Nutrition has been an problematic issue. Fruit is plentiful here which is great but salads are hard to find and even when they are they might have been washed in unsafe water. Concerns about picking up food poisoning are ramped up considerably since we knew about the pregnancy. Any further advice you can send our way would be greatly appreciated.
Sincerely Glyn Griffiths
I felt I had to be exra careful because I was an older mom. Absolutely no risk taking for me because this might have been my last chance to be a mother.
I was also lucky to be married to a man who felt I should be an at-home mom. We gave up a lot of economic advantages but we have felt it was well worth it over the years. I have worked at home on Fetal Alcohol Syndrome information retrieval for the past 15 years.
Please do not drink before, during or after your pregnancy if you are nursing. The behavioral problems caused by prenatal alcohol exposure are not worth the risk.
I think you made a good decision by cancelling your trip due to risks in the destination country.
After reading your experience I’m more in a dilema than I was before. I have a planned trip since last year to the US. It will be the end of this March and my pregnancy will come to week 11. Everything is set, ticket bought, accomodation paid and seminar fee also paid (I will attend a week seminar). My concerns are related to long travel (22hours from my country, Indonesia) and how expensive it would be in the US if anything happens. This is my first pregnancy aswell and I’m 36-year old mother to be. I don’t want to risk it…but I’m still torn in two..go or not.
@Peggy Oba: Thanks a lot for your comments and wise words.
This is a helpful story. I will be three months pregnant and am planning to travel to Galapagos and Peru with my partner and two year old. These are work trips and I really want to go, but still trying to weigh the risks. I had a normal pregnancy with my son but am considered high-risk because I am 38.
I was pregnant once and once was enough. In labor for 50 hours. I could not even imagine flying when pregnant, but “to each his own.” I asked doctor (I had already decided on a tubal after that pregnancy) if a “second would be as bad.” He said: “It could be worse.” Thus, the tubal and I have never, ever regretted it. Only wanted one child.
As an international business executive …extensive travel comes with the territory. I am an “older mom” in that my two year old son was born when I was 37. Presently, at the age of 39, my second son is due in the late Summer. I traveled fairly extensively with my now two year old and have trips to Amsterdam/London/Puerto Rico/Miami during my final trimester. The OB is completely fine with my travel and the airlines say that up to 36 weeks is fine.
With my first pregnancy, I lived in northern India. I took precautions to avoid malaria, typhus, TB, HIV, and food poisoning. I spent time in Amritsar and Delhi. My daughter is now 12 and healthy. I’m pregnant with my second and currently in Delhi, India, waiting to fly to the States for a holiday. Women here have babies, and healthy ones at that. If one takes precautions, traveling while pregnant is safe. We’ve lived in India for four years and not contracted maleria or Dengue fever. I don’t expect to now that I’m pregnant again. My point is that you can choose to be afraid or careful. Being afraid keeps you at home. Being careful allows you to make solid decisions and take calculated risks that lead can present opportunities.
I have planned to travel to India in my 13th week and return on 24th week of my pregnancy. This is my first pregnancy and I will be travelling alone. I am worried if it is safe to take a 22 hours flight and I want to know if something happens what are the services available on board. I spoke to airline but didn’t get satisfactory reply.
I am a student admitted already to do my masters in Cyprus from Africa, I just realized I will be a month pregnant when I travel. Please its really hard on me but please what advice have you for me. Am just 20 years old.
My sister has to travel out of the country in the coming week as she is pregnant I don’t want her to go at this time. She is 4 months pregnant, she anyway wants to go that is why I have booked tickets online using CouponZeta site but I still have that fear whether it is safe for her to travel at this time or not. After reading the above article I have that question am I doing any wrong thing allowing her to travel so long?
After reading your experience I’m more in a dilema than I was before. I have a planned trip since last year to the US. It will be the end of this March and my pregnancy will come to week 11. Everything is set, ticket bought, accomodation paid and seminar fee also paid (I will attend a week seminar). My concerns are related to long travel (22hours from my country, Indonesia) and how expensive it would be in the US if anything happens. This is my first pregnancy aswell and I’m 36-year old mother to be. I don’t want to risk it…but I’m still torn in two..go or not.
Post a Comment
Your email address will not be published. Required fields are marked *
To receive email updates about this page, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.

Search Smartraveller
Advice for pregnant travellers.

If you're pregnant and planning to travel overseas, research your destination before you go. Consult your doctor and understand potential risks to you and your unborn child.
Being informed about the risks will help you manage them. It will increase your chance of having a great time overseas. Explore this page to learn about:
- planning for travel during pregnancy
- medications and pregnancy
- terminating a pregnancy overseas
- going overseas to give birth
- how the Australian Government can help overseas
This page is for Australians who are pregnant, or planning to get pregnant overseas. If you're looking for information about adopting a child or engaging in surrogacy, refer to surrogacy and adoption .
Planning for travel during pregnancy
Travelling when pregnant can be challenging, but there are things you can do to stay safe and comfortable and reduce your risks.
Timing your travel
Visit your doctor or obstetrician at least 8 weeks before you go. Discuss the timing and location of your trip. Check if you're allowed to travel and if they recommend travel.
If they advise against travel, don't go. Find time to travel later, when the risk has passed.
Airlines and cruise lines have specific rules on when you can travel while pregnant. If you're having more than one baby, the rules may differ again. Most airlines won't let you fly beyond 28 weeks of pregnancy.
Ask your airline or cruise line about any rules or restrictions that could affect you while in transit.
Read more about pregnancy and travel (Victorian Government Department of Health and Human Services).
Choosing where to travel when you're pregnant
Consider the risks of going overseas, including the risks to your unborn child.
You and your baby will be more at risk in some countries. Avoid countries with poor sanitation, hygiene and medical facilities. Read the travel advisory for each country you're visiting. Note the health risks.
If the travel advisory says do not travel to that country, then do not travel at this time. You're putting yourself and your unborn child at serious risk.
Things can go wrong quickly when you're pregnant. Check how close you'll be to good medical facilities. Stay within reach of hospitals and doctors.
See a doctor before you go
See a doctor at least once before you travel. Your doctor will advise what vaccines and medications you can take when you're pregnant.
If you have a high-risk pregnancy, your doctor may advise against travel. If they advise against travel, then don't go. You're putting yourself and your unborn child at serious risk.
Most airlines will ask you to show a letter from your doctor.
Buy travel insurance to cover pregnancy
You need travel insurance.
Ask your travel insurer if your policy covers:
- pregnancy, and until what stage
- IVF pregnancy, if applicable
- pregnancy complications or premature birth while you're away
- cancellation of your trip due to pregnancy or birth issues
For cover during pregnancy, you may need to pay extra. You may need medical evidence.
You may face limitations to your cover, depending on where you're going. For example, in Saudi Arabia, medical insurance won't cover pregnancy unless you're married.
Read more about travel ins urance .
Medications and pregnancy
Not all medication available over the counter or by prescription in Australia is available in other countries. Some may even be considered illegal or a controlled substance, even if prescribed by an Australian doctor.
Get the facts, before you go.
- See if your medication is legal in your destination .
- Ensure you have enough medication for your trip.
- Check with a doctor that your medication is suitable for travel.
Refer to the 'Look after your health' section on Advice for women travellers for more information. Also see our advice on travelling with medications .
Terminating pregnancy overseas (abortion)
Abortion and the law.
Abortion may be illegal in the country you're visiting.
You're subject to all local laws and penalties, including those that may appear harsh by Australian standards. Research local laws before considering an abortion.
If you're arrested or jailed for having an abortion, the Australian Government will do what it can to help you. However, we can't get you out of trouble or out of jail.
- Understand our limits. Read the Consular Services Charter .
Health care standards overseas can vary. If you choose to end your pregnancy, find a proper medical facility to help you.
Choose the safest option, not the cheapest option.
Read more about medical assistance overseas .
Medical treatment for ending a pregnancy can be costly. As with other medical procedures overseas, get a quote from the hospital first.
Find out if this procedure is covered by your travel insurance . If not, consider the cost of having this procedure overseas versus back in Australia. You may be eligible for subsidised care in Australia through Medicare.
Read more about travel insurance .
Going overseas to give birth
If you choose to give birth overseas, you'll need to check:
- healthcare costs and travel insurance
- safety and quality of care
- your budget to pay for a private hospital, if you aren't covered by the public health system via a partner or a reciprocal agreement
- any changes to your legal status, marriage and parent rights
- if you need a special visa as a medical tourist
Citizenship and passports
Giving birth overseas doesn't automatically grant your child citizenship of that country. Research local immigration and citizenship laws before you travel.
If authorities think you're planning to give birth there for visa reasons, they may refuse you entry.
In Australia
To register your child's birth with Australian authorities, you'll need to contact your state or territory registry of births, deaths and marriages (Australian Government).
Consular officials can assist with your child's passport .
There may be higher costs for processing a passport for your baby while you're overseas.
- Learn more about Australian citizenship by descent (Department of Home Affairs).
Becoming a new parent can feel overwhelming. Consider how you'll find support overseas, both practically and emotionally.
Supplies and services
Prepare ahead for how you'll travel with your new baby. Make sure you have all the medications and supplies you need.
The Australian Government can't help with medical costs or services overseas.
Learn more about medical assistance overseas .
If our travel advisory for the country in which you plan to give birth says ' do not travel ', then don't travel there. You're putting yourself and your unborn child at serious risk.
Learn more about staying safe and avoiding danger .
Consular services and pregnancy
The Australian Government is limited in how and when it can help Australians overseas.
In most cases, when you need help overseas you, or your travel insurer, must organise and pay for it.
What we can do
- We can give you a list of local medical facilities with doctors who speak English.
- We can give you a list of local lawyers who speak English.
- We can help you contact your family in Australia in an emergency.
- We can notify you when we update our travel advice for your destination . Learn more about subscriptions .
What we can't do
- We can't guarantee your safety when you travel.
- We can't pay for your bills if you need medical assistance overseas .
- We can't get you out of jail if you're arrested because you've broken a local law. Be aware laws vary greatly on abortions, medications and sex outside of marriage.
- We can't give you medical or legal advice.
Final tips before you go
Prepare before you travel:
- get medical advice, vaccinations and a health check
- know the laws about pregnancy, adoption, surrogacy and abortion overseas
- arrange adequate travel insurance and check coverage
- arrange emotional and practical support
- Read our general advice for people travelling with children .
- See information about international surrogacy .
- See information about going overseas to adopt .
- Before you go, get travel insurance that covers your pregnancy.
- See more advice on pregnancy and travel (Victorian Department of Health and Human Services).
- Read more about travelling while pregnant (CHOICE).
Related content
Information for Australians going overseas for surrogacy. Learn about types of arrangements, laws, citizenship and visas.
All travellers face risks overseas. In certain countries or cultures, women face greater risks than men and may be more vulnerable.
In many countries age, gender and sexual preferences can pose challenges. Understanding the culture and laws in your destination will help things go smoothly.
- Skip to main content
- Skip to site information
Language selection
Help us to improve our website. Take our survey !
Travelling while pregnant
Find useful information and considerations to help you prepare for safe and healthy travels outside Canada while pregnant.
With careful preparation, travelling while pregnant can be safe. The decision to travel should be made in consultation with your health care professional, based on your personal health circumstances.
On this page
Before you go, while you're away, if you need help.
Medical practices, health standards and infection control measures vary from country to country. You may not have access to the same level of care, procedures, treatments and medications as you would in Canada.
You could also be at increased risk of getting an infection and/or developing severe complications from certain infections, which could also affect the fetus.
Before leaving Canada:
- consult a health care professional or visit a travel health clinic at least 6 weeks before travelling to get personalized health advice and recommendations
- check our Travel Advice and Advisories for country-specific information, including about possible health risks
- know how to seek medical assistance outside of Canada
- review the policy and the coverage it provides
- most policies do not automatically cover pregnancy-related conditions or hospital care for premature infants
- ask your insurance provider about coverage for medical care during pregnancy, giving birth and intensive care for you and your fetus or newborn
- carry a copy of your prenatal records
- talk to your health care professional about any additional items you may want to bring that are specific to your health needs
Local laws and medical services relating to pregnancy can differ from Canada. Learn the local laws, and how these may apply to you before you travel.
Pre-travel vaccines and medications
Many vaccines can be safely given during pregnancy. Due to a higher risk of more severe outcomes for you and your fetus, some vaccines are recommended specifically during pregnancy, such as tetanus-diphtheria-pertussis (DTaP) and influenza.
Don’t take medications you may still have from prior trips. Tell the health care professional about your pregnancy, or intended pregnancy, before filling any prescriptions. The decision to get any pre-travel vaccinations or medications should be discussed with your health care professional.
The decision can depend on:
- your purpose of travel (e.g., tourism, visiting friends and relatives)
- your planned destination(s)
- the length of your trip
- your risk of getting a disease
- how severe the effect of a disease would be to you and/or your fetus
- your planned activities
- any underlying medical issues and/or pregnancy-related complications
Malaria could cause major health problems for a mother and her unborn baby. A pregnant woman may want to consider avoiding travel to areas where malaria transmission occurs.
Description of malaria risk by country and preventative measures.
If you can’t avoid travelling to an area where malaria is present:
- some medications to prevent or treat malaria may not be safe during pregnancy
- take extra care to protect yourself from mosquito bites
Zika virus infection during pregnancy can pose significant risks to your fetus even if you don’t develop symptoms. While pregnant, you may want to consider avoiding travelling to a country or areas with risk of Zika virus.
Latest travel health advice on Zika virus.
If you choose to travel, take precautions to avoid infection with Zika virus:
- prevent mosquito bites at all times
- protect yourself from contact with semen, vaginal fluid and blood
- always use condoms correctly or avoid sexual contact while in countries or areas with risk of Zika virus
Learn more about Zika virus and pregnancy:
- Zika virus: Pregnant or planning a pregnancy
- Zika virus: Advice for travellers
- Pregnancy and travel (tropical medicine and travel)
Monitor your health and be prepared
Emergencies can happen at any time. Know where the nearest hospital or medical centre is while you are travelling and confirm they will accept your medical insurance.
Seek medical attention immediately if you develop any of the following symptoms while travelling:
- persistent vomiting and/or diarrhea
- dehydration
- vaginal bleeding
- passing tissue or clots
- abdominal pain, cramps or contractions
- your water breaks
- excessive swelling of face, hands or legs
- excessive leg pain
- severe headaches
- visual problems
If you develop these symptoms after your return to Canada, you should see a health care professional immediately and tell them about your recent trip.
Transportation
Always wear a seatbelt when travelling by plane or car. When using a diagonal shoulder strap with a lap belt, the straps should be placed carefully above and below your abdomen. If only a lap belt is available, fasten it at the pelvic area, below your abdomen.
If you have any medical or pregnancy-related complications, discuss with your health care professional whether air travel is safe for you.
Most airlines restrict travel in late pregnancy or may require a written confirmation from a physician. Check this with the airline before booking your flight.
During long flights, you may be at higher risk of developing blood clots, known as deep vein thrombosis (DVT). The risk of deep vein thrombosis can be reduced by:
- getting up and walking around occasionally
- exercising and stretching your legs while seated
- selecting an aisle seat when possible
- wearing comfortable shoes and loose clothing
Your health care professional may recommend additional ways to reduce your risk such as wearing compression stockings.
Always stay well hydrated while travelling.
Land travel
The risk of deep vein thrombosis can be reduced by:
- stopping the vehicle to walk around every couple of hours
Motion sickness
Certain medications used to treat nausea and vomiting during pregnancy may also be effective in relieving motion sickness.
If you think you might experience motion sickness during your trip, speak to your health care professional about the use of these medications.
Environmental and recreational risks
Some activities may not be recommended or may require additional precautions. Discuss your travel plans, including any planned or potential recreational activities with a health care professional.
High altitude
You should avoid travelling to an altitude above 3,658 metres (12,000 feet).
However, if you have a high-risk pregnancy and/or are in the late stages of pregnancy, the highest altitude should be 2,500 metres (8,200 feet).
If you have pregnancy-related complications, you should avoid unnecessary high-altitude exposure.
Keep in mind that most high-altitude destinations are far from medical care services.
Personal protective measures
Food-borne and water-borne diseases.
Eat and drink safely while travelling while travelling. Many food-borne and water-borne illnesses can be more severe during pregnancy and pose a risk to the fetus.
This can include:
- toxoplasmosis
- listeriosis
- hepatitis A and E
To help avoid food-borne and water-borne diseases:
- before eating or preparing food
- after using the bathroom or changing diapers
- after contact with animals or sick people
- before and after touching raw meat, poultry, fish and seafood
- if you’re at a destination that lacks proper sanitation and/or access to clean drinking water, only drink water if it has been boiled or disinfected or if it’s in a commercially sealed bottle
- use ice made only from purified or disinfected water
- this could cause the fetus or newborn to develop thyroid problems
- unpasteurized dairy products, such as raw milk and raw milk soft cheeses
- unpasteurized juice and cider
- raw or undercooked eggs, meat or fish, including shellfish
- raw sprouts
- non-dried deli meats, including bologna, roast beef and turkey breast
- don’t use bismuth subsalicylate (Pepto-Bismol®)
- Information on travellers’ diarrhea
Illnesses acquired from insect and other animals
Protect yourself from insect bites:
- wear light-coloured, loose clothes made of tightly woven materials such as nylon or polyester
- prevent mosquitoes from entering your living area with screening and/or closed, well-sealed doors and windows
- use insecticide-treated bed nets if mosquitoes can’t be prevented from entering your living area
- information on insect bite and pest prevention
Some infections, such as rabies and influenza, can be shared between humans and animals. You should avoid contact with animals including dogs, livestock (pigs, cows), monkeys, snakes, rodents, birds, and bats.
Information for if you become sick or injured while travelling outside Canada.
For help with emergencies outside Canada, contact the:
- nearest Canadian office abroad
- Emergency Watch and Response Centre in Ottawa
More information on services available at consular offices outside Canada.
Related links
- Immunization in pregnancy and breastfeeding: Canadian Immunization Guide
- Advice for Canadians travelling to Zika-affected countries
- Advice for women travellers
- If you get sick before or after returning to Canada
- Receiving medical care in other countries
- Travel vaccinations
- What you can bring on a plane
Help and Support
Requirements for flying whilst pregnant, 27/06/2023 • knowledge, information.
What are the requirements for flying whilst pregnant?
Flights 4 hours duration or greater You can travel up to the end of the 36th week for single pregnancies and the end of the 32nd week for multiple pregnancies (e.g. twins). Flights less than 4 hours duration You can travel up to the end of the 40th week for single pregnancies and the end of the 36th week for multiple pregnancies. Medical clearance is required if you are having complications with your pregnancy. Read more about medical requirements for travelling while pregnant on Qantas flights or see the relevant consulate or embassy.
Was this article helpful?
Other useful articles.
- Infant and child age requirements
- Qantas Club access for Qantas Club members flying with Jetstar
- Identification requirements for Adults, Children and Infants
- Ways to earn Qantas Points without flying
- Information about the ‘Thank you for flying with us’ offer

Privacy Preference Center
Your privacy, strictly necessary cookies, performance cookies, functional cookies, targeting cookies.
When you visit any website, it may store or retrieve information on your browser, mostly in the form of cookies. This information might be about you, your preferences or your device and is mostly used to make the site work as you expect it to. The information does not usually directly identify you, but it can give you a more personalized web experience. Because we respect your right to privacy, you can choose not to allow some types of cookies. Click on the different category headings to find out more and change our default settings. However, blocking some types of cookies may impact your experience of the site and the services we are able to offer.
These cookies are necessary for the website to function and cannot be switched off in our systems. They are usually only set in response to actions made by you which amount to a request for services, such as setting your privacy preferences, logging in or filling in forms. You can set your browser to block or alert you about these cookies, but some parts of the site will not then work. These cookies do not store any personally identifiable information.
These cookies allow us to count visits and traffic sources so we can measure and improve the performance of our site. They help us to know which pages are the most and least popular and see how visitors move around the site. All information these cookies collect is aggregated and therefore anonymous. If you do not allow these cookies we will not know when you have visited our site, and will not be able to monitor its performance.
These cookies enable the website to provide enhanced functionality and personalisation. They may be set by us or by third party providers whose services we have added to our pages. If you do not allow these cookies then some or all of these services may not function properly.
These cookies may be set through our site by our advertising partners. They may be used by those companies to build a profile of your interests and show you relevant adverts on other sites. They do not store directly personal information, but are based on uniquely identifying your browser and internet device. If you do not allow these cookies, you will experience less targeted advertising.
Cookie List
Ready Steady Baby
Travelling when pregnant.
Whether you’re doing short journeys in the car or getting on a plane for a holiday abroad, it’s important to take extra care of yourself when you’re pregnant. Making a few small changes and planning ahead will help to make sure you have a comfortable and safe journey.
Wherever you’re going, it’s a good idea to take your maternity notes with you in case you need medical help.

It’s fine to drive or be a passenger in a car while you’re pregnant.
It’s important to wear a seat belt as you normally would. Make sure the straps don’t go over your bump by:
- placing the lap strap across your hips so it fits comfortably under your bump
- placing the diagonal strap between your breasts and around your bump
Take regular breaks when driving and make sure you bring some water and snacks with you for the journey.
Going on holiday or abroad
If you’re planning a holiday, seek health advice as early as possible.
You should give some thought to where you want to go as:
- the things you may normally love, like hot sunny weather, may not be a great idea if you’re uncomfortable or finding it hard to sleep
- you shouldn’t travel to areas where there’s malaria or the Zika virus if you can avoid it
You should also consider the quality of medical care in the country you plan to visit.
Fitfortravel has more advice for pregnant travellers
Staying safe on holiday
Activities like walking and swimming are fine while you’re pregnant, but it’s not a good idea to do any activity where you might fall.
Take care to avoid coming into contact with water or food that could cause tummy upsets. Some medicines for treating diarrhoea may not be suitable in pregnancy.
Talk to your midwife if you have questions.
Travel vaccinations
You’ll need vaccinations before you travel to certain countries.
There are some vaccinations you shouldn’t have when you’re pregnant, especially in the first 3 months, so always check before you book anything.
Find out which travel vaccinations you might need
Travel insurance
Before you travel, you’ll need special travel insurance that:
- covers any medical costs
- allows you to cancel for any issues with your pregnancy
If you don’t tell your insurer you’re pregnant before you travel, your insurance may not be valid.
If you’re travelling in Europe, the European Health Insurance Card (EHIC) may allow you to use the health services in these countries.
Apply for a European Health Insurance Card
Flying while pregnant
Air travel is generally safe if you’re having an uncomplicated pregnancy.
If you have any pregnancy complications, check with your midwife or GP that there’s no medical reason to stop you flying, such as high blood pressure or a risk of deep vein thrombosis .
Most airlines won’t let you fly if you’re within about a month of your due date. Some will need a letter from your GP or midwife saying you’re fit to fly when you’re 7 months pregnant. Check with the airline before you book.
Having a comfortable flight
When travelling by plane:
- drink plenty of water as you’re much more likely to get dehydration while flying.
- take healthy snacks with you so you can follow your own eating plan
- take whatever makes you more comfortable, such as an extra pillow or warm socks
Be aware it may take you a bit longer than before to recover from jet lag.
Deep vein thrombosis
Deep vein thrombosis (DVT) is a blood clot in a deep vein in your leg, calf or pelvis.
You’re more likely to get DVT if:
- you sit for long periods of time
- do very little activity
If you’re travelling on a long-distance flight or sitting for 4 hours or more, talk to your midwife as you may need medication. F ollow your midwife or doctor’s advice.
More about deep vein thrombosis
Further information, other languages and alternative formats
Translations and alternative formats of this information are available from Public Health Scotland .
If you need a different language or format, please contact [email protected].
- Ready Steady Baby leaflet in Arabic, Polish, Simplified Chinese (Mandarin) and Ukrainian
- Ready Steady Baby leaflet in English (Easy Read)
Source: Public Health Scotland - Opens in new browser window
Last updated: 14 December 2023
Help us improve NHS inform
Your feedback has been received
Don’t include personal information e.g. name, location or any personal health conditions.
Also on NHS inform
- Travel health and vaccinations
Other health sites
- fitfortravel: Advice for pregnant women
- Institute for Health Visiting: Travelling with your baby
- Disabled Living Foundation (DLF)
- Rica: consumer research charity
- Health & Care Professions Council (HCPC)

Advertisement
Tracking Abortion Bans Across the Country
By The New York Times Updated May 1, 4:40 P.M. ET
- Share full article
Twenty-one states ban abortion or restrict the procedure earlier in pregnancy than the standard set by Roe v. Wade, which governed reproductive rights for nearly half a century until the Supreme Court overturned the decision in 2022.
In some states, the fight over abortion access is still taking place in courtrooms, where advocates have sued to block bans and restrictions. Other states have moved to expand access to abortion by adding legal protections.
Latest updates
- The Arizona state legislature voted to repeal an 1864 ban on nearly all abortions. Officials warned that the near-total ban may be briefly enforceable this summer until the repeal takes effect in the fall. A 15-week ban remains in effect.
- A ban on abortion after about six weeks of pregnancy took effect in Florida , following a ruling by the Florida Supreme Court that the privacy protections of the state’s Constitution do not extend to abortion.
The New York Times is tracking abortion laws in each state after the Supreme Court’s decision in Dobbs v. Jackson Women’s Health Organization , which ended the constitutional right to an abortion.
Where abortion is legal
In a few states that have enacted bans or restrictions, abortion remains legal for now as courts determine whether these laws can take effect. Abortion is legal in the rest of the country, and many states have added new protections since Dobbs.
Ban in effect
Note: TK note here.
Legal for now
State details.
More details on the current status of abortion in each state are below.
An earlier version of this article misstated the legal status of abortion in Utah. As of 4 p.m. on June 24, the state attorney general had issued a statement saying the state’s abortion ban had been triggered, but it had not yet been authorized by the legislature’s general counsel. By 8:30 p.m., the counsel authorized the ban and it went into effect.
A table in an earlier version of this article misstated which abortion ban is being challenged in Texas state court. Abortion rights supporters are challenging a pre-Roe ban, not the state’s trigger ban.
An earlier version of this article referred incorrectly to the legal status of abortion in Indiana. While Indiana abortion providers stopped offering abortion services in anticipation of an abortion ban taking effect on Aug. 1, the law did not take effect.

IMAGES
VIDEO
COMMENTS
Before you book a cruise or air travel, check the airlines or cruise operator policies for pregnant women. Some airlines will let you fly until 36 weeks, but others may have an earlier cutoff. Cruises may not allow you to travel after 24-28 weeks of pregnancy, and you may need to have a note from your doctor stating you are fit to travel.
Virgin Australia. No restrictions. Travel permitted; requires a medical certificate dated within 10 days of departure date once you reach 28 weeks. For flights longer than four hours, travel is not permitted after 36 weeks of pregnancy (32 weeks if pregnant with multiples), or within 48 hours of normal vaginal delivery.
After 37 weeks, pregnant women will not be allowed to travel. For multiple pregnancies, a certificate is required between the 29th and 32nd week; after that, women will not be allowed to travel. The medical certificate must include the following: Be issued and signed by a doctor or midwife.
Download any apps you use for renting cars and accessing boarding passes before you leave so you can easily reschedule things in the event of a last-minute cancellation. If you're flying during your third trimester, be sure to call the airline to check about the cutoff week for pregnancy travel. A note from your doctor that says you're ...
Stand up and stretch. Pregnant women are at higher risk for developing blood clots, so it's important to avoid sitting still for long periods of time. Wear loose clothes and keep the blood flowing in your legs: Whether you're flying or driving, take breaks to get up, walk around and stretch every half hour or so.
Answer From Mary Marnach, M.D. Generally, air travel before 36 weeks of pregnancy is considered safe for people who aren't dealing with any pregnancy problems. Still, if you're pregnant, it's a good idea to talk with your health care provider before you fly. Your provider might suggest that you not fly if you have certain pregnancy ...
In general, most airlines won't allow you to fly in your last month of pregnancy, though some limit travel as early as 28 or 29 weeks of pregnancy. And international flights often have an ...
United Airlines allows pregnant travelers to board without medical documentation before their 36th week of pregnancy. American Airlines allows pregnant passengers to fly without documentation up ...
Most airlines do allow pregnant women to fly until about a month before their due dates. Chervenak agrees: "As long as there are no known complications to pregnancy, traveling on an airplane is ...
When to travel in pregnancy. Some women prefer not to travel in the first 12 weeks of pregnancy because of nausea and vomiting and feeling very tired during these early stages. The risk of miscarriage is also higher in the first 3 months, whether you're travelling or not. Travelling in the final months of pregnancy can be tiring and uncomfortable.
Threatened miscarriage or vaginal bleeding during current pregnancy . Multiple fetuses in current pregnancy . History of pre-eclampsia, high blood pressure, or diabetes with any pregnancy . History of infertility or trouble getting pregnant . Pregnancy for the first time over the age of 35 years . Heart valve disease or congestive heart failure
During a healthy pregnancy, occasional air travel is almost always safe. Most airlines allow you to fly domestically until about 36 weeks of pregnancy. Your ob-gyn can provide proof of your due date if you need it. If you are planning an international flight, the cut-off for traveling may be earlier. Check with your airline.
Travel During Pregnancy. As long as there are no identified complications or concerns with your pregnancy, it is generally safe to travel during your pregnancy. The ideal time to travel during pregnancy is the second trimester. In most cases, you are past the morning sickness of the first trimester and several weeks from the third stage of ...
There are some legit concerns about traveling abroad while pregnant - but those can easily be addressed by making some smart travel choices and precautions. ... You don't know how you'll feel as pregnancy progresses, so here's what I'd recommend about planning a trip abroad: Go during months 6 or 7: In general, these are the best ...
Check out airline rules for traveling while pregnant for complete details, but generally speaking, most U.S. airlines don't have many flight restrictions until the last month of pregnancy. However, many international airlines do have restrictions and documentation requirements beginning at 28 weeks.
In general, most airlines allow for travel until 35 to 36 weeks. It is advisable to ask your doctor before you plan your travel, as complications in pregnancy may limit your ability to travel. It is useful to carry a doctor's letter of certification for fitness to travel to avoid being turned away at the airport.
Ticket for Two - International travel during pregnancy. By Stacie Dunkle. "We don't recommend international travel during pregnancy for first-time mothers," said my nurse midwife. Those words stopped me in my tracks. As an officer in the Epidemic Intelligence Service with three years of experience working overseas, I couldn't believe ...
See a doctor at least once before you travel. Your doctor will advise what vaccines and medications you can take when you're pregnant. If you have a high-risk pregnancy, your doctor may advise against travel. If they advise against travel, then don't go. You're putting yourself and your unborn child at serious risk.
You should avoid travelling to an altitude above 3,658 metres (12,000 feet). However, if you have a high-risk pregnancy and/or are in the late stages of pregnancy, the highest altitude should be 2,500 metres (8,200 feet). If you have pregnancy-related complications, you should avoid unnecessary high-altitude exposure.
What are the requirements for flying whilst pregnant? Flights 4 hours duration or greater. You can travel up to the end of the 36th week for single pregnancies and the end of the 32nd week for multiple pregnancies (e.g. twins). Flights less than 4 hours duration. You can travel up to the end of the 40th week for single pregnancies and the end ...
Some medicines for treating diarrhoea may not be suitable in pregnancy. Talk to your midwife if you have questions. Travel vaccinations. You'll need vaccinations before you travel to certain countries. There are some vaccinations you shouldn't have when you're pregnant, especially in the first 3 months, so always check before you book ...
High-risk pregnancies and travel. Pregnant women experiencing complications are advised not to travel. Some complications include: cervical problems, such as 'incompetent cervix'. vaginal bleeding. multiple pregnancy. gestational diabetes, past or present. high blood pressure, past or present. pre-eclampsia (a toxic condition sometimes ...
There is a slight chance you could have an ectopic pregnancy — when the pregnancy implants outside the womb. 6. Thyroid issues. Your thyroid gland makes hormones to help with growth and development. But an overactive (hyperthyroidism) or underactive (hypothyroidism) thyroid can cause menstrual irregularities, including amenorrhea.
A 15-week ban remains in effect. A ban on abortion after about six weeks of pregnancy took effect in Florida, following a ruling by the Florida Supreme Court that the privacy protections of the ...