- Operated by Occupational & Physical Therapists

- All Categories
- New! Products
Customer Service:

1-800-827-8283
How to choose the best wandering alarm for dementia patients [updated for 2022].

It's common for a person living with dementia to wander or be confused about their location. As scary as that is for a caregiver who can’t find a patient, it’s even more frightening for the patient, who might truly not have any idea where they are as things slowly become less and less familiar to them. Some common reasons patients wander , and can benefit from anti-wandering alarms, are confusion about where they are, delusions about what responsibility they have in their lives, escape from a real or imagined threat, and agitation, boredom, or restlessness. Whatever sets the patient off on an escape route, Alzheimer’s and dementia wander safety products can help keep the patient where they need to be to remain safe and comfortable.
What is a patient safety alarm?
Patient safety alarms come in many forms. All are designed to alert a caregiver when a dementia patient moves unsupervised, which can lead to the patient getting into an unsafe situation via a fall or wandering or both.
Who needs a patient safety alarm?
If there is any risk of someone wandering away from safety, or into spaces that could pose a threat of injury because of a fall or some other safety issue, a patient safety alarm will mitigate the risk and minimize the probability of an injury or worse.
What are the types of patient safety alarms?
Some alarms are attached to a piece of equipment or furniture, and some are attached to the patient. The best patient safety alarm for your situation will transmit the appropriate signal for a caregiver to intervene or remind the patient to stay put. It will also be something the patient cannot disable.
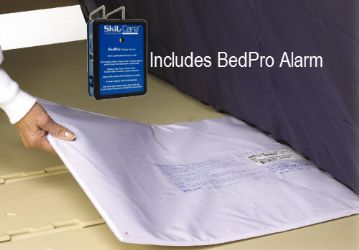
A bed alarm - some of which go under the mattress and some of which go over the mattress - is sometimes appropriate for use with chairs too. This anti-wandering alarm allows a caregiver to monitor the activity and position of a patient. With sensors that detect a reduction of pressure when patients get up, bed alarms will go off when someone is no longer sitting or laying on the bed.
- Protects patients prone to bed falls
- Alerts caregivers as soon as someone gets out of bed
- Simple to set up and use
- This style of alarm can go off if someone simply changes position, sending a false warning if someone rolls off the alarm sensor but not the bed
Best: Smart Caregiver Bed Alarm - CordLess® Alert Systems
Toilet alarm.
Toilet alarms reduce the risk of injuries due to an unassisted exit from the toilet. Pressure activated, as soon as someone rises from the toilet, the alarm will sound.
- Let caregivers know when assistance is needed
- Does not require any work or effort on the part of the patient
- Reduces risk of bathroom falls
- Alarm might not work properly if the sensor has lime and calcium scales
- Some people don’t sit on the seat when toileting so the sensor is not activated
Best: Skil-Care Gel-Foam Toilet Seat Cushion Alarm System
Best: posey toilet seat sensor, wheelchair/chair alarm.
A wheelchair alarm has a sensor that is pressure activated. When there is a reduction in pressure on the sensor from someone leaving the wheelchair’s seat, the alarm sounds. This alarm will alert to someone falling out of or getting up from the wheelchair. One design has the chair sensor or pad on top of the seat, while another kind (better for incontinent users) has the sensor placed under the seat.
- Informs caregivers when a patient rises from a wheelchair, potentially wandering into a dangerous situation
- Reminds patients who are confused to stay seated for safety
- Difficult for users to disable the alarm
- People who self-propel often shift positions in their wheelchairs, potentially setting off a false alarm
Best Wireless Alarm: Smart Caregiver Wireless Patient Chair Alarm with Pager
Best under seat alarm: skil-care underseat alarm system, fall detection device.
Not all falls can be prevented. When they happen, assistance arriving sooner rather than later can make a big difference in outcomes. A fall detection device acts as a personal alert safety system, determining when a fall has occurred, and connecting the user with help. A patient can summon help with the push of a button on a pendant, while this helpful device can make the call for assistance on the user’s behalf if they are unable to do so. For anyone at risk of a fall, this equipment provides peace of mind while helping maintain independence, knowing help will be on the way if it’s needed.
- Allows a user to be alone while still being able to summon help if necessary
- Lightweight pendant that is inconspicuous to wear and easy to use
- Acts on the user’s behalf if the patient is injured and unable to utilize the call button
- Must be worn all the time, and dementia patients might forget to keep it within reach
Best: Personal Alert Safety System - TEQ Secure for Fall Detection by SOFIHUB
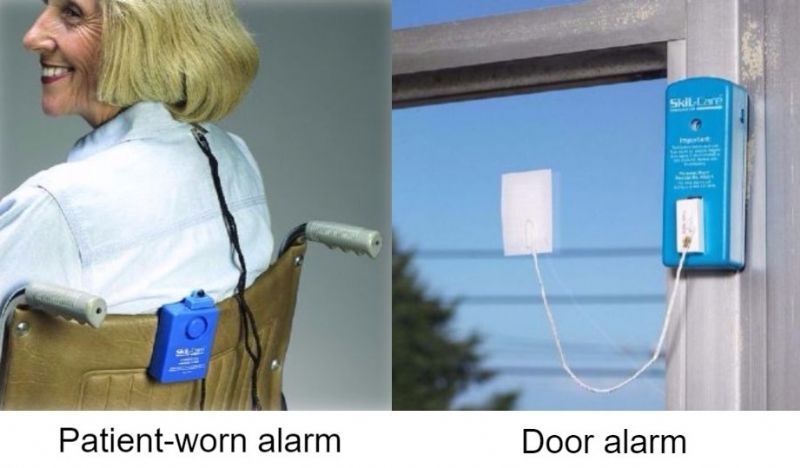
A wandering alarm for dementia patients on a door significantly reduces the risk of a patient leaving a building and becoming endangered when disoriented or lost. With one part of a magnetic door alarm attached to the door frame and the other attached to the door. When the connection between the two parts is broken, an alarm will sound indicating the door has been opened. Alarms can also be attached to cupboard or closet doors to deter access to areas that are off limits because of safety concerns.
- Easy to install
- Need no electricity
- Can be used on almost any door or window without any special specifications
- Can be very loud and scary for patients
Best: Smart Caregiver Door Alarm Exit Alert System
Best: stop strip magnetic door alarm system, window alarm.
The best window alarms have the versatility to allow the window to open a bit for ventilation and fresh air without setting off the alarm. These work with sensors that are attached via a short wire. The window can be opened or closed, as long as the distance the window raises and lowers is less than the length of the wire.
- Allows for opening the window enough for ventilation
- No electricity needed
- Batteries run out and have to be monitored and changed regularly
Best: Skil-Care Door and Window Alarm with Magnetic Strip Skil-Care Door and Window Alarm with Magnetic Strip
Wheelchair alarm belt.
A wheelchair alarm belt resembles a car seatbelt, and alerts a caregiver when a patient is about to leave the wheelchair. It goes off when the belt is unfastened, providing some advance warning before the patient actually gets out of the chair. It can be the difference between preventing a fall and arriving after it’s just happened.
- Secures to all standard wheelchairs
- Eliminates sensor strips and clothing clips
- Nylon belt has an easy-release buckle for restraint-free care
- Can feel restrictive and reduce patient independence
Best: Skil-Care Seat Belt Alarm System
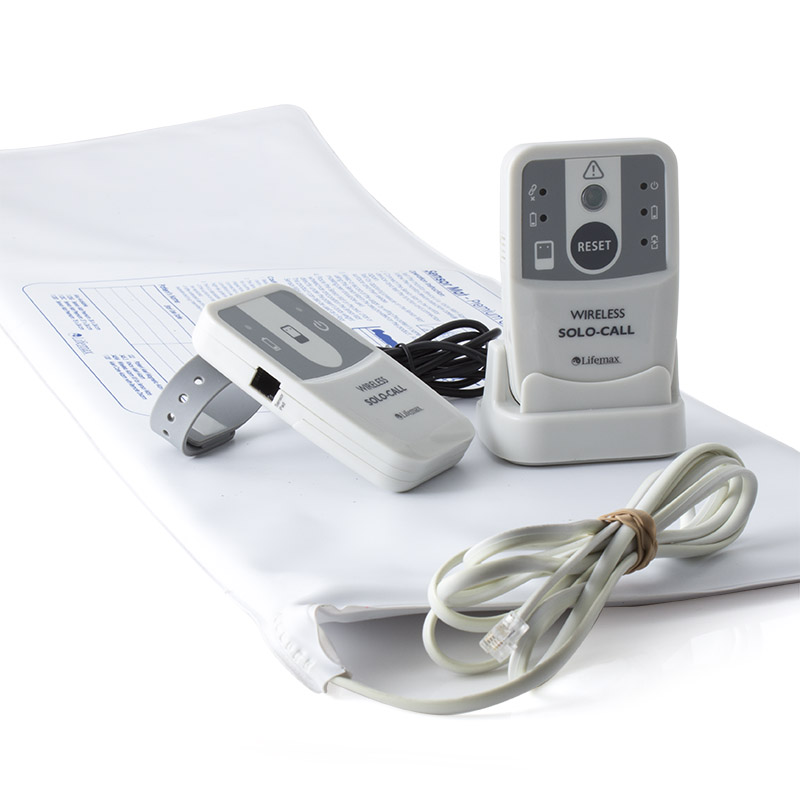
Pressure sensitive floor mat alarm.
An alarmed floor mat next to a chair or bed will alert a caregiver when a patient gets up from a chair or gets out of bed unexpectedly and steps onto the mat. The weight on the mat triggers the pressure sensors to set off the alarm so a caregiver knows to come help a patient attempting to move unassisted.
- Non-restrictive device to help keep patients from wandering away from safety
- Can be used next to the bed or a chair
- Large size available to cover large bedside area of the floor
- Might not be activated by patients who don’t weigh very much
Best: Smart Caregiver Floor Alarm Mat with Pager
Patient-worn alarm.
Wearable patient alarms come in a variety of styles with one part of the alarm attached to a bed, chair, or wheelchair and the other part attached to the patient. If the patient goes on the move, the pull switch engages the alarm to signal a caregiver that the patient has moved away from the alarmed chair, bed, or wheelchair. These alarms might be a clip to the patient’s clothing, they could be magnet, or they could have a pull string.
- Can be used at home or while out and about
- Simple design
- Easy for a caregiver to switch off after activation
- Can sometimes be removed by patients without triggering the alarm
Best Magnetic Alarm: Advantage Magnetic Safety Alarm by Medline
Best pull cord alarm: drive medical magnetic pull cord alarm, lap cushion alarm.
Providing a useful lap cushion for a patient seated in a wheelchair, this alarm will sound if the patient tries to make an unplanned exit from the chair. This non-restrictive patient safety alarm system is ideal for use where restraint reduction is the goal. It is secured by hook-and-loop fasteners. When they are unfastened, the alarm sounds. No sensor or sensor strips are required.
- Lap pad is a comfortable positioning aid
- Does not require sensors
- Lap cushion pad is easy to wipe clean
- Bulky and can make some patients feel too hot
Best: Skil-Care Lift-Off Lap Cushion Alarm System
Features to consider.
Factors to consider when choosing an alarm to address wandering in patients with dementia include physical and mental condition of the patient, who they share their living space with, the sound level needed to alert a caretaker while not disturbing others or scaring a patient, and how adept the patient is at disabling or getting around an alarm device. Whether in a home care or clinical setting, dementia patients and their caregivers can benefit from the extra level of protection provided by these devices.
Patient Risk Level
If a patient with dementia is at risk of wandering or falling, an alarm can alert a caregiver when action is needed. An alarm that sounds when a person opens a door or window can help prevent them from leaving a safe area and exposing themselves to danger. An alarm notifying a caregiver that a patient has gotten up from a toilet or a wheelchair or sat up in bed can summon assistance to mitigate the risk of a fall.
Environment
The care setting can impact which alarm is most appropriate. Some alarms sound at nursing stations so the noise doesn’t disturb other patients who are trying to sleep.
Alert Sound
Many alarm tones can be loud and jarring, which can be very upsetting for dementia patients who can startle easily. There are alarms that allow for recording soothing voice prompts that direct the patient back to bed.
Patient-Worn or Mounted
Some anti-wandering alarms have one end attached to a bed or chair and the other end clipped to a patient’s clothing. They are activated when their movement disconnects the two elements. Others are mounted on door frames or windows or are placed on seats or on the ground. Whether they go with the patient or are in a fixed location, most are easy to install.
Cognitive Ability
Even if their memory is fading and they are sometimes confused, dementia patients often have the cognitive ability to figure out how to outsmart an alarm. If a patient has figured out how to unclip an alarm from their clothing and leave it behind or step over a floor pad sensor, alarms that are out of reach or that they can’t disable are the best option.
Urinary Incontinence
If a user struggles with incontinence, alarms that don’t have a pressure sensor they sit on or something that goes across their lap will work the best and be the most comfortable.
Frequently Asked Questions
Q: are bed alarms effective.
A: Yes, and they are a big help to home caregivers because you do not have to sit by the patient's bed or stand outside their bedroom on high alert. It frees up caregivers to take care of other tasks while the patient is asleep, alerting if assistance is needed because the patient exited the bed.
Q: Do bed alarms prevent falls?
A: Bed alarm systems can reduce falls by alerting personnel when at-risk patients attempt to leave a bed without assistance. They can also get the attention of the patient to stop them from trying to get out of bed unassisted or remind them they need to be extra careful when getting out of bed.
Q: What is a Posey alarm?
A: Posey Alarms provide notification when a fall-risk patient attempts to rise without caregiver assistance. They have prerecorded messages so patients might hear family members speaking to them advising them not to get out of bed, or they can translate a soothing message in the patient’s native language.
Q: How does a bed exit alarm work?
A: Bed exit alarms warn caregivers , and in some cases patients themselves, when a patient leaves or attempts to leave the bed. They can be patient-worn or they can be pressure sensitive pads that go off when a patient moves. They warn the caregiver that the patient has changed position and is about to leave the bed, alert the caregiver that the patient has already left the bed, and remind the patient they are doing something they shouldn’t be doing.
Q: Do chair alarms work for the elderly?
A: Yes. If wandering is an issue, a chair alarm will notify a caregiver a patient is on the move. If falling is a consideration, chair alarms work best if a caregiver is close by, even if their attention is on something else. This type of alarm will give someone close enough to the patient time to be at their side to prevent a possible fall should they choose to get up from a chair.
Q:What is a wheelchair alarm?
A: A wheelchair alarm helps to monitor the activity of someone seated in a wheelchair. Typically, these alarms are either magnetic (safety belt or clothing clip alarms) or they combine with a sensor or pad (seat alarm) that detects a reduction in pressure and alerts when a patient tries to leave the chair.
Q: How do fall detection devices work?
A: Fall detection devices use accelerometers, a type of radio wave technology sensor, to monitor movement. The fall alert detectors can measure when the user has suddenly fallen by detecting the abrupt changes of body movements. The technology can evaluate an individual’s body position, physical activity, and the smoothness of acceleration of movements. If it’s determined these variables are within the danger zone, a fall alert will be sounded.
Final Thoughts
Six in 10 people with dementia will wander at least once, and many do it repeatedly, as they lose their ability to recognize familiar places and people. Wandering can be extremely dangerous, so the risk cannot be ignored. Patient Safety Alarms are a valuable tool to ensure dementia patients remain in a comfortable and safe environment.
If leaving a building is the greatest concern, a door frame model will suit your situation well. If getting up unassisted from a bed or a toilet presents an additional fall risk, a pressure sensitive alarm is a good choice. If a patient is transferred multiple times a day, an alarm that clips to their clothing and attaches to the seat or bed they’re in means they can take this safety precaution with them no matter where they are. Whether being cared for at home or in a hospital or care home setting, there is an alarm that can help keep them safe.
Thank you for reading about choosing the best Alzheimer's and dementia wander safety products. Visit Caregiver University for more helpful articles with information on providing the best care for aging loved ones and patients.

Elderly Monitoring System | Non-Invasive Remote Monitoring Plug with No Monthly Fee

Smart Sensor Senior Medical Alert System with Fall Detection | Elderly Monitoring with No Monthly Fee

Fall Prevention Monitor

Skil-Care Door and Window Alarm with Magnetic Strip

Smart Caregiver CordLess® Bed Alarm and Chair Alarm Packages

Pressure Sensitive Floor Mat with Alarm

Smart Caregiver Bed Alarm - CordLess® Alert Systems

Skil-Care Door and Window Alarm
Skil-Care BedPro UnderMattress Alarm System

Drive Medical Pressure Sensitive Chair or Bed Patient Alarm
Subscribe for caregiver university updates, shipping information, standard ground shipping, freight shipping (truck freight).

Guide to Choosing the Right Wandering Alarms and Sensors for Dementia Patients
If you have a loved one who has Alzheimer’s or dementia, or if you are a caregiver for someone with these conditions, you are probably aware that they have the tendency to wander away. It’s because wandering is a common behavior in patients with Alzheimer’s disease or other forms of dementia. When they start to show signs of wandering behaviors, they are at a high risk of wandering away and becoming lost, which is very distressing for family members and caregivers and dangerous for the individual.
The exact causes of wandering behavior are not fully understood. It may happen to people who are searching for something or trying to get back to a certain place that they remember, such as a job or a favorite place. However, there are also some who just wander or walk away because they feel restless or agitated. [ 1 ]
If your loved ones or patients with dementia often wander and you’re worried about them being lost, there are different ways that you can do to keep them safe and reduce the risk of wandering. One example is giving them meaningful activities to do throughout the day, particularly during the time that they usually wander. Reassuring them whenever they feel lost, abandoned, or disoriented may also help. [ 2 ] Aside from that, you may also use wandering alarms and sensors, which can notify you whenever they move around.
There are many safety alarms available for patients with dementia, and they come in various forms. But all of them are designed to alert a caregiver when a dementia patient moves unsupervised, which can lead them to get into an unsafe situation. If you are interested in getting one but unsure of what to buy, we are here to help you. In this post, we are giving you a guide to choosing the right wandering alarms and sensors.
What are Wandering Alarms and Sensors?

If your patient or loved one who has Alzheimer’s disease or a different type of dementia wanders and tries to leave your home or facility, one way to keep them safe is to place door alarms, as well as bed and chair exit alarms. [ 3 ] In addition to patients with dementia, these alarms and sensors are also used for those who struggle to get around and have an increased risk of falling. It’s because a lot of falls can occur when the elderly are moving from one chair to another or getting in and out of bed. [ 4 ]
Some might think that they can simply place other locking mechanisms like a latch high up the door. However, the downside of that strategy is when an emergency occurs, such as a fire, the person inside may not be able to escape safely out of the room or house. [ 3 ] Using wandering alarms and sensors allow the person to attempt exiting through the door, but they will also alert you to his or her need for assistance.
Wandering alarms and sensors are used to protect individuals from elopement and wandering. Whether the patients intentionally attempt elopement or simply wander around to find a door, those who are at risk of going out without the needed supervision may benefit from these technologies.
In addition to that, wandering alarms and sensors can also be used to alert others for assistance. For example, they can be placed on bathroom doors as they will sound when the door is opened, letting you or the caregiver know that your loved one or patient needs assistance in the bathroom. [ 3 ]
Benefits of Using Wandering Alarms and Sensors

Using wandering alarms and sensors come with many benefits, both for caregivers and patients. Below are some of them:
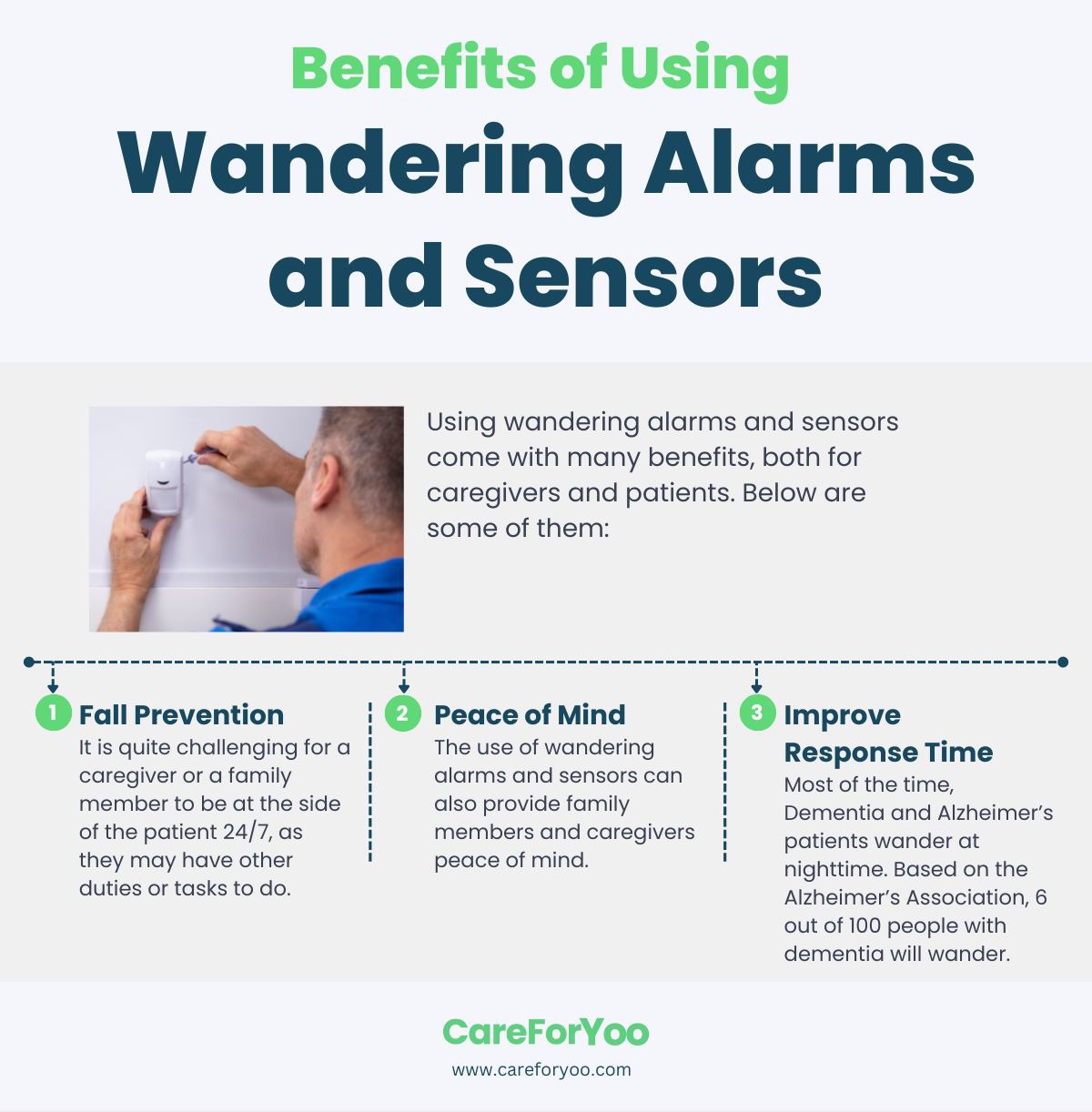
Fall Prevention
It is quite challenging for a caregiver or a family member to be at the side of the patient 24/7, as they may have other duties or tasks to do. If the caregiver is unaware that the patient is trying to leave the bed, chair, or room, it can lead to a dangerous situation. Therefore, investing in an exit alarm or sensor can help in reducing falls and accidents as you can always be aware whenever the patient moves around and might need help. [ 4 ]
Peace of Mind
The use of wandering alarms and sensors can also provide family members and caregivers peace of mind. With these technologies, you will be alerted when the patient has left their chair or bed or when they pass through a door. They will also let you know when the patient may need assistance but does not want to ask for help.
Improve Response Time
Most of the time, Dementia and Alzheimer’s patients wander at nighttime. Based on the Alzheimer’s Association, 6 out of 100 people with dementia will wander. Without any advanced security technologies, there can be a higher risk for wandering patients to become lost or leave the house or building without the caregiver knowing immediately. But with the use of wandering alarms and sensors, family members or caregivers will be alerted immediately, which improves the response time. [ 5 ]
What are the Different Types of Wandering Alarms and Sensors?
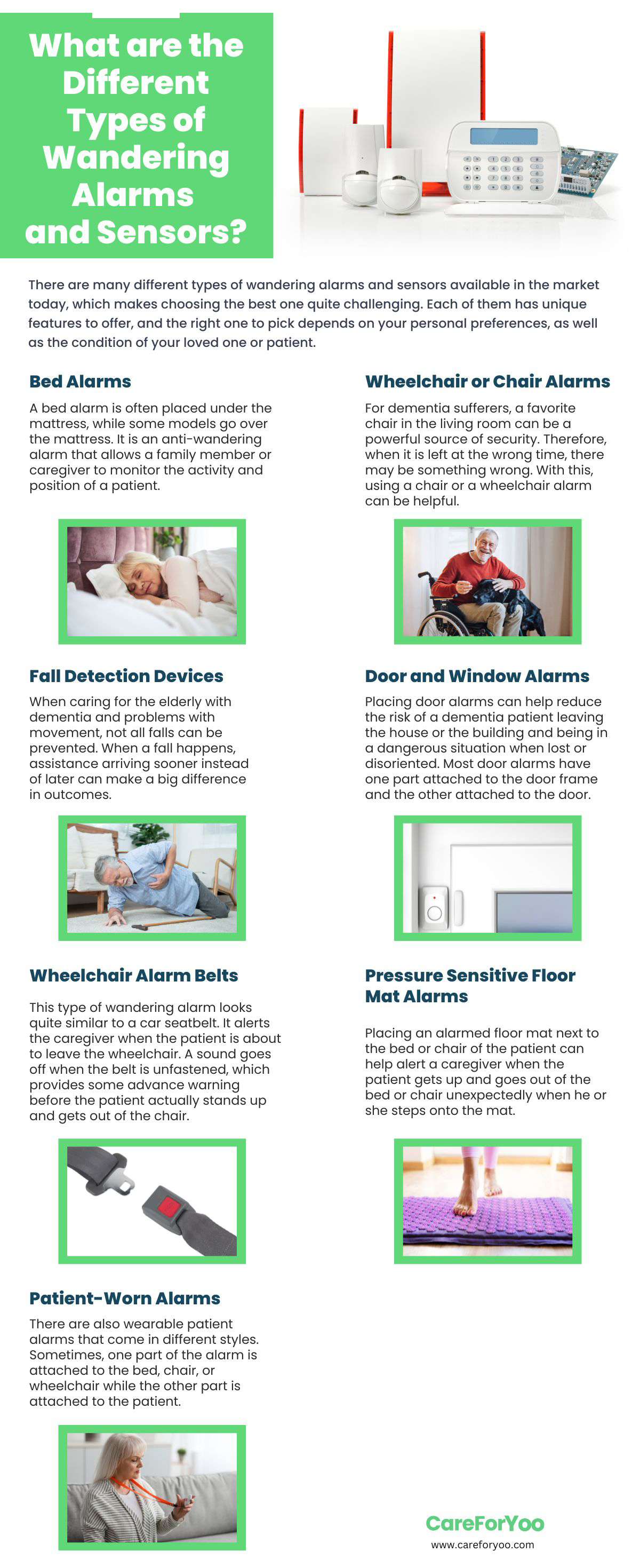
There are many different types of wandering alarms and sensors available in the market today, which makes choosing the best one quite challenging. Each of them has unique features to offer, and the right one to pick depends on your personal preferences, as well as the condition of your loved one or patient. There are some alarms and sensors that are attached to a piece of equipment or furniture, while some are attached to the patient.
The best patient safety alarm for your situation will send the right signal for a caregiver to intervene or remind the patient to stay put. These alarms and sensors can’t also be disabled by patients. To help you choose the right type of wandering alarms and sensors, below are the different types and what each of them offers:

A bed alarm is often placed under the mattress, while some models go over the mattress. It is an anti-wandering alarm that allows a family member or caregiver to monitor the activity and position of a patient. The sensors detect a reduction of pressure when patients get up and leave the bed. The bed alarm will go off when someone is no longer sitting or lying on the bed. [ 6 ]
The best thing about bed alarms is that they protect patients who are prone to bed falls, as they alert caregivers as soon as someone gets out of bed. It is also very simple to set up and use. However, the downside is that some bed alarms can easily go off if someone simply changes position, which sends a false warning. But choosing a good quality bed alarm can be helpful. Below are some examples that might help you in choosing the right one:
- Smart Caregiver Wireless Bed Alarm System : This is a bed alarm system that alerts caregivers when the patient gets off the bed. It is simply placed under the patient’s back or the buttock area underneath the fitted sheet. When the patient takes their weight off the sensor pad, the remote alert monitor will notify the caregiver with a sound. It works up to 300 feet. The pad is made of soft, latex-free vinyl with a foam interior, making it comfortable. It also does not make any noise inside the patient’s room.
- Val-U-Care Safety Monitor with Bed Exit Pad : This system comes with a safety monitor and a bed sensor pad made of soft vinyl, which is easy to clean. The safety monitor features an adjustable volume and low battery light. It uses 3 AA batteries to operate.
Wheelchair or Chair Alarms
For dementia sufferers, a favorite chair in the living room can be a powerful source of security. Therefore, when it is left at the wrong time, there may be something wrong. With this, using a chair or a wheelchair alarm can be helpful. These alarms feature a sensor that is pressure activated. When there is a decrease in pressure on the sensor from someone leaving the seat, the alarm will sound and alert to someone falling out or getting up from the chair. There are chair sensors or pads that are placed on top of the seat, while others are under the seat. [ 6 ]
The best thing about wheelchair or chair alarms is that they inform caregivers when a patient rises from the chair and possibly wanders into a dangerous situation. In addition, it also reminds patients who are confused to stay seated for safety. However, people who self-propel usually shift positions often in their wheelchairs, which may set off a false alarm.
Below are some examples of wheelchair or chair alarms to help you choose:
- Lunderg Chair Alarm System : This chair alarm system has a chair sensor pad that connects wirelessly using a handheld monitor. When the patient stands up, the alarm will sound or vibrate continuously. The pressure pad is easy to wipe clean and incontinence resistant. It also includes a portable pager with an adjustable volume. It also has an improved sensor to reduce false alarms.
- Secure Safety Solutions 14CSET-1Y Chair Alarm : This chair alarm system has an 80 dB alarm sound, a flashing alert light, and a tamper-resistant reset button. The alarm also reset when the patient returns to the sensor pad. The chair sensor pad is durable and comfortable to sit on. It is best for fall-risk patients who often attempt to exit a chair or a wheelchair.
Fall Detection Devices

When caring for the elderly with dementia and problems with movement, not all falls can be prevented. When a fall happens, assistance arriving sooner instead of later can make a big difference in outcomes. Fall detection devices act as personal alert safety systems which determine when a fall has occurred, connecting the user with help.
These devices also provide patients a button that they can push to summon help. But the device can also call for assistance on the user’s behalf if they are unable to do so. This type of equipment gives peace of mind to anyone with a loved one who is at risk of a fall. It also allows the patient to be independent while still being able to ask for help if needed. The only downside is that it needs to be worn at all times by the patients. [ 6 ] Below are some examples of fall detection devices to help you choose:
- SkyAngle911FD Automatic Fall Detection Device : This fall detection device can be placed on a keychain. It is waterproof, and even when it is dropped in the water, you can still talk through it. It only has one button to press to speak with 911. If it detects a fall, it will automatically call for help. It is always in 2-way speakerphone mode.
- Mini Guardian Medical Alert System : This is a mini alarm system that can be attached to a lanyard and worn as a medical alert necklace for elderly people. It is used by simply pushing a button. It connects patients to a live USA-based and trained operator at any time of the day.
Door and Window Alarms

Placing door alarms can help reduce the risk of a dementia patient leaving the house or the building and being in a dangerous situation when lost or disoriented. Most door alarms have one part attached to the door frame and the other attached to the door. When the connection between them is broken, an alarm will sound, indicating that the door has been opened. The alarms can also be attached to closet doors or cupboards to deter access areas that are off-limits for safety concerns. [ 6 ]
Most door alarms are easy to install and do not require electricity to work. They can also be used on almost any type of door without any special specifications. However, there are some door alarms that are too loud and scary for patients. That’s why carefully choosing the best one for dementia patients is important.
Aside from door alarms, having a window alarm installed is also a good idea. The best ones have the versatility to allow the window to open a bit for ventilation and the fresh air without setting off the alarm. Window alarms work with sensors attached to a short wire. The window can be opened and closed as long as the distance between the window raises and lowers less than the length of the wire. [ 6 ] When the window is opened big, as if someone is escaping from it, the alarm will sound.
Below are some examples that might help you pick:
- Flyoukki Door Alarm Sensor : This is a battery-operated door alarm sensor that features a 120dB alarm. It does not include any wiring, allowing you to install it on any door. It has a slim design, making it discreet and simple to install.
- YisTech Wireless Caregiver Door Sensor Alarm : This is a door sensor chime that sounds to notify you when the door opens. It has adjustable volume levels from 0 dB to 110 dB, which is perfect to not startle the patient. It also has an LED indicator, and it is very easy to use.
Wheelchair Alarm Belts
This type of wandering alarm looks quite similar to a car seatbelt. It alerts the caregiver when the patient is about to leave the wheelchair. A sound goes off when the belt is unfastened, which provides some advance warning before the patient actually stands up and gets out of the chair. It can help in preventing a fall and from keeping the patient from wandering.
Most wheelchair alarm belts are secure to all standard wheelchairs. However, they can sometimes feel restrictive and may reduce the independence of the patient. But it eliminates the use of sensor strips and clothing clips. Below are some examples for more ideas:
- Secure Safety Solutions Wheelchair Seat Belt Alarm System : This is an adjustable belt that has a quick-release and non-restraint alarm activation. It has 85 dB of sound with an auto-reset feature. It is also tamper resistant and always on for safety. It can be attached to a wheelchair easily by using screws. It also does not have any breakable parts.
- ChairPro Seatbelt Alarm System : This is a nylon belt that has an easy-release buckle. An alarm sounds when the buckle is released, and it automatically resets when the buckle is secured. It is compatible with all standard wheelchairs.
Pressure Sensitive Floor Mat Alarms
Placing an alarmed floor mat next to the bed or chair of the patient can help alert a caregiver when the patient gets up and goes out of the bed or chair unexpectedly when he or she steps onto the mat. The weight triggers the pressure sensors on the mat to set off the alarm. It is a non-restrictive device that can help in keeping patients from wandering away from safety. However, some mat alarms might not be activated by patients who do not weigh that much. [ 6 ] Below are a few examples to help you choose:
- Smart Caregiver Cordless Floor Mat Pressure Pad : This is a cord-free floor alarm mat that does not have any alarming noise in the patient’s room. When it is stepped on, a signal will be sent to the alarm monitor, which has a radius of 150 to 300. The alarm has three volume levels and an on-and-off switch.
- Wander Prevention Alarm Monitor and Pressure Sensing Floor Mat : This is a wander prevention system that comes with a sensor pad monitor and a pull-string monitor. When the magnetic pull-string is pulled free of the monitor or when pressure is added to the floor mat, an alarm noise will sound to alert the caregiver.
Patient-Worn Alarms

There are also wearable patient alarms that come in different styles. Sometimes, one part of the alarm is attached to the bed, chair, or wheelchair while the other part is attached to the patient. When the patient wanders, the pull switch engages the alarm to signal to the caregiver that the patient has moved away from the chair, bed, or wheelchair. Patient-worn alarms can be clipped to the patient’s clothes or could be attached by a magnet. There are also some that feature a pull string. [ 6 ]
What’s great about patient-worn alarms is that they can be used at home or while outdoors. They also have simple designs. However, these alarms are sometimes removed by patients without triggering the alarm. That’s why choosing a high-quality one is essential. Below is an example to give you more idea of what they are:
- Safe-T Mate Magnetic Personal Alarm : This alarm is attached to the patient with a string that is clipped to the clothing. An alarm sounds when the cord is removed from the unit that is attached to the chair or bed.
Things to Consider When Buying Wandering Alarms and Sensors

When choosing the type of wandering alarms and sensors to buy, the first and most important thing that you need to consider is the physical and mental condition of the patient. Aside from that, you also need to look into who they are sharing their living space with, the sound level needed to alert a caregiver without disturbing other people or scaring the patient, and how adept the patient is when it comes to disabling or getting around the alarms and sensors.
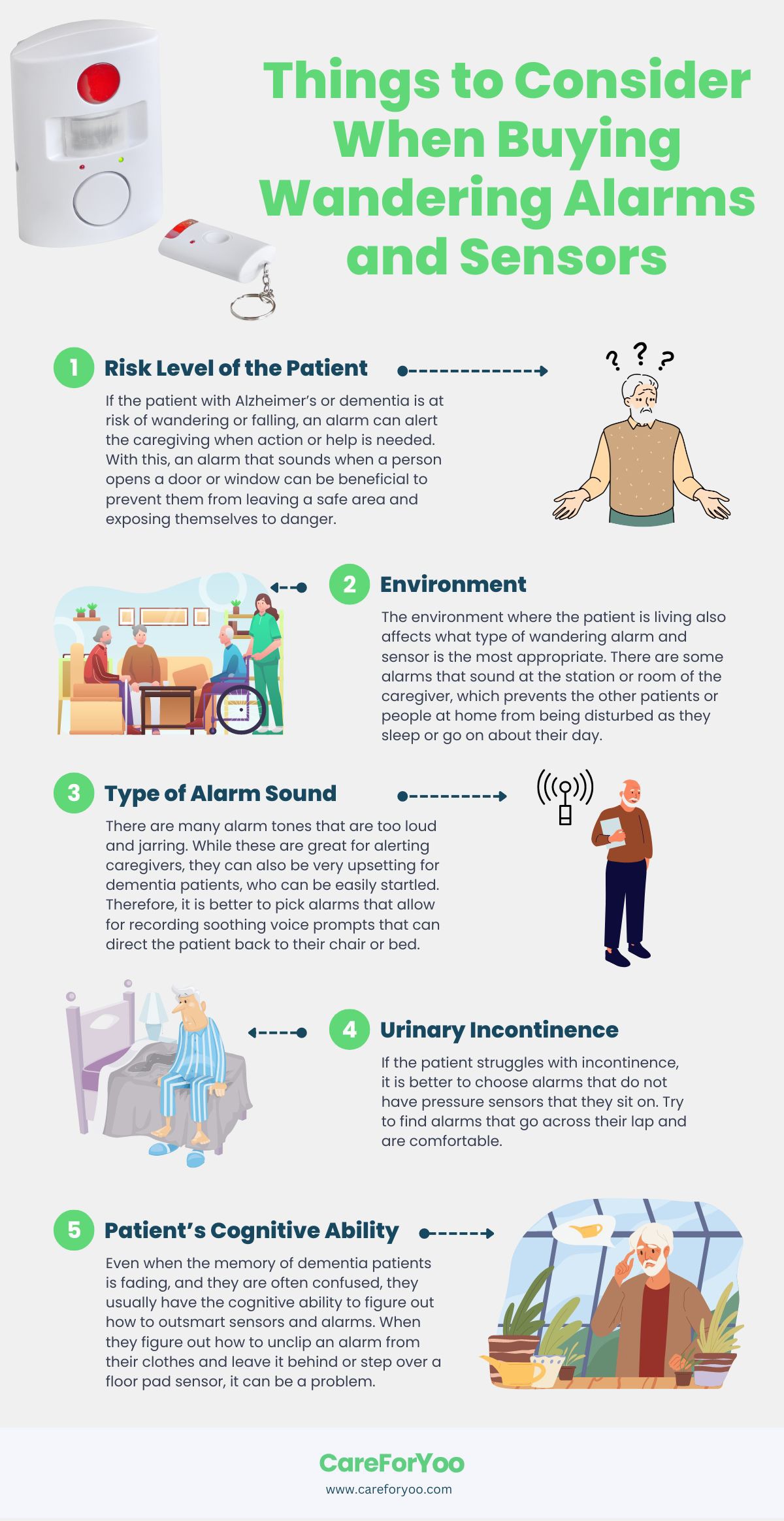
The following are the important things that you need to consider before you buy wandering alarms and sensors:
Risk Level of the Patient
If the patient with Alzheimer’s or dementia is at risk of wandering or falling, an alarm can alert the caregiving when action or help is needed. With this, an alarm that sounds when a person opens a door or window can be beneficial to prevent them from leaving a safe area and exposing themselves to danger. [ 6 ]
Environment
The environment where the patient is living also affects what type of wandering alarm and sensor is the most appropriate. There are some alarms that sound at the station or room of the caregiver, which prevents the other patients or people at home from being disturbed as they sleep or go on about their day.
Type of Alarm Sound
There are many alarm tones that are too loud and jarring. While these are great for alerting caregivers, they can also be very upsetting for dementia patients, who can be easily startled. Therefore, it is better to pick alarms that allow for recording soothing voice prompts that can direct the patient back to their chair or bed. [ 6 ]
Urinary Incontinence
If the patient struggles with incontinence, it is better to choose alarms that do not have pressure sensors that they sit on. Try to find alarms that go across their lap and are comfortable.
Patient’s Cognitive Ability
Even when the memory of dementia patients is fading, and they are often confused, they usually have the cognitive ability to figure out how to outsmart sensors and alarms. When they figure out how to unclip an alarm from their clothes and leave it behind or step over a floor pad sensor, it can be a problem. Therefore, it is also great to choose alarms and sensors that are out of reach or those that they can’t disable or turn off easily. [ 6 ]
Wandering alarms and sensors are beneficial to monitor patients with dementia, as well as those who are at risk of falling. It is also great that there are various options available in the market today so you can choose the right one that will match the condition of your loved one or patient.
In addition to using wandering alarms and sensors, other things that might help you in keeping your loved ones safe include using night lights throughout the home, camouflaging doors by painting them the same color as the walls, and not leaving the person alone for too long. We hope that this post helped you learn more about choosing the right wandering alarms and sensors.
[1] UPMC, E. (2022). Wandering tendencies in patients with Alzheimer’s disease and dementia . UPMC. Retrieved October 11, 2022, from https://www.upmc.com/services/seniors/resources-for-caregivers/wandering-tendencies-patients-alzheimers-dementia
[2] Alzheimer’s Association, E. (2022). Wandering . Alzheimer’s Disease and Dementia. Retrieved October 11, 2022, from https://www.alz.org/help-support/caregiving/stages-behaviors/wandering
[3] Heerema, E. (2022, April 23). Types of door alarms to improve safety for wandering in dementia . Verywell Health. Retrieved October 11, 2022, from https://www.verywellhealth.com/safety-in-dementia-door-alarms-98172
[4] Val-U-Care, E. (2021, September 6). The top 3 benefits of bed and chair exit alarm systems – val-U-care . Val. Retrieved October 11, 2022, from https://val-u-care.com/the-top-3-benefits-of-bed-and-chair-exit-alarm-systems/
[5] Technology Install Partners, E. (2022). 4 benefits of wandering management systems . Technology Install Partners. Retrieved October 11, 2022, from https://technologyinstallpartners.com/4-benefits-of-wandering-management-systems
[6] Price, OT, M. (2022). How to choose the best wandering alarm for dementia patients [updated for 2022] . Rehabmart.com. Retrieved October 11, 2022, from https://www.rehabmart.com/post/how-to-choose-the-best-patient-safety-alarm
Normal 0 false false false EN-US JA X-NONE /* Style Definitions */ table.MsoNormalTable {mso-style-name:"Table Normal"; mso-tstyle-rowband-size:0; mso-tstyle-colband-size:0; mso-style-noshow:yes; mso-style-priority:99; mso-style-parent:""; mso-padding-alt:0in 5.4pt 0in 5.4pt; mso-para-margin:0in; mso-para-margin-bottom:.0001pt; mso-pagination:widow-orphan; font-size:12.0pt; font-family:Cambria; mso-ascii-font-family:Cambria; mso-ascii-theme-font:minor-latin; mso-hansi-font-family:Cambria; mso-hansi-theme-font:minor-latin;} Normal 0 false false false EN-US JA X-NONE /* Style Definitions */ table.MsoNormalTable {mso-style-name:"Table Normal"; mso-tstyle-rowband-size:0; mso-tstyle-colband-size:0; mso-style-noshow:yes; mso-style-priority:99; mso-style-parent:""; mso-padding-alt:0in 5.4pt 0in 5.4pt; mso-para-margin:0in; mso-para-margin-bottom:.0001pt; mso-pagination:widow-orphan; font-size:12.0pt; font-family:Cambria; mso-ascii-font-family:Cambria; mso-ascii-theme-font:minor-latin; mso-hansi-font-family:Cambria; mso-hansi-theme-font:minor-latin;} SafeWander™ Monitors Those Who May Wander or Fall
You are not alone. More than 60% of the 47.5 million dementia patients wander. Wandering is also a concern for people with autism and other conditions. If not detected quickly, wandering can result in tragic incidents.
On the other hand, one in every three adults age 65 or older have risks of falling. Falls often happen when these individuals get up from their beds or chairs. A simple fall can have devastating consequences.
The world's first wearable sensor that alerts wandering on your mobile device, SafeWander™ gives you peace of mind.
Consisting of a tiny Button Sensor worn by your patient, a Gateway plugged near his/her bed, and a mobile device App, the SafeWander™ system sends a beeping alert to your mobile device as soon as the sensor detects your patient getting up.
The SafeWander™ System requires that you have an an Apple mobile device with iOS 8.0 or newer (iPhone, iPad, iPod Touch) or Android mobile device (Google Nexus 4/5/6, Samsung Galaxy S 4/5/6, Samsung Note 3, or Android 4.3 BLE devices) and strong WiFi in your home/facility.
- Português Br
- Journalist Pass
Alzheimer’s and dementia: Understand wandering and how to address it
Dana Sparks
Share this:

Wandering and becoming lost is common among people with Alzheimer's disease or other disorders causing dementia. This behavior can happen in the early stages of dementia — even if the person has never wandered in the past.
Understand wandering
If a person with dementia is returning from regular walks or drives later than usual or is forgetting how to get to familiar places, he or she may be wandering.
There are many reasons why a person who has dementia might wander, including:
- Stress or fear. The person with dementia might wander as a reaction to feeling nervous in a crowded area, such as a restaurant.
- Searching. He or she might get lost while searching for something or someone, such as past friends.
- Basic needs. He or she might be looking for a bathroom or food or want to go outdoors.
- Following past routines. He or she might try to go to work or buy groceries.
- Visual-spatial problems. He or she can get lost even in familiar places because dementia affects the parts of the brain important for visual guidance and navigation.
Also, the risk of wandering might be higher for men than women.

Prevent wandering
Wandering isn't necessarily harmful if it occurs in a safe and controlled environment. However, wandering can pose safety issues — especially in very hot and cold temperatures or if the person with dementia ends up in a secluded area.
To prevent unsafe wandering, identify the times of day that wandering might occur. Plan meaningful activities to keep the person with dementia better engaged. If the person is searching for a spouse or wants to "go home," avoid correcting him or her. Instead, consider ways to validate and explore the person's feelings. If the person feels abandoned or disoriented, provide reassurance that he or she is safe.
Also, make sure the person's basic needs are regularly met and consider avoiding busy or crowded places.
Take precautions
To keep your loved one safe:
- Provide supervision. Continuous supervision is ideal. Be sure that someone is home with the person at all times. Stay with the person when in a new or changed environment. Don't leave the person alone in a car.
- Install alarms and locks. Various devices can alert you that the person with dementia is on the move. You might place pressure-sensitive alarm mats at the door or at the person's bedside, put warning bells on doors, use childproof covers on doorknobs or install an alarm system that chimes when a door is opened. If the person tends to unlock doors, install sliding bolt locks out of his or her line of sight.
- Camouflage doors. Place removable curtains over doors. Cover doors with paint or wallpaper that matches the surrounding walls. Or place a scenic poster on the door or a sign that says "Stop" or "Do not enter."
- Keep keys out of sight. If the person with dementia is no longer driving, hide the car keys. Also, keep out of sight shoes, coats, hats and other items that might be associated with leaving home.
Ensure a safe return
Wanderers who get lost can be difficult to find because they often react unpredictably. For example, they might not call for help or respond to searchers' calls. Once found, wanderers might not remember their names or where they live.
If you are caring for someone who might wander, inform the local police, your neighbors and other close contacts. Compile a list of emergency phone numbers in case you can't find the person with dementia. Keep on hand a recent photo or video of the person, his or her medical information, and a list of places that he or she might wander to, such as previous homes or places of work.
Have the person carry an identification card or wear a medical bracelet, and place labels in the person's garments. Also, consider enrolling in the MedicAlert and Alzheimer's Association safe-return program. For a fee, participants receive an identification bracelet, necklace or clothing tags and access to 24-hour support in case of emergency. You also might have your loved one wear a GPS or other tracking device.
If the person with dementia wanders, search the immediate area for no more than 15 minutes and then contact local authorities and the safe-return program — if you've enrolled. The sooner you seek help, the sooner the person is likely to be found.
This article is written by Mayo Clinic Staff . Find more health and medical information on mayoclinic.org .
- Answers to common questions about whether vaccines are safe, effective and necessary Consumer Health: Treating and living with HIV and AIDS
Related Articles

- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Door Alarms for Wandering in Alzheimer's and Dementia
SilviaJansen / Getty Images
If your loved one with Alzheimer's disease or a different type of dementia wanders and attempts to leave your home or facility, one option to increase their safety is to place alarms on the doors. You can also try different locking mechanisms such as a latch up high, but the concern with that strategy is that in case of a fire, the person may not be able to escape safely out of the house.
An alarm can allow the person to attempt exiting through the door but will also alert you to her need for assistance. Alarms can offer you a little support and reassurance in your efforts to ensure your loved one's safety so that, rather than feel that you have to constantly check on her, you know that the alarm will sound if she suddenly wakes and needs assistance.
Protect individuals from elopement and wandering: Whether people with dementia intentionally attempt lopement or are simply wandering around to locate a door, those at risk for exiting without the needed supervision may benefit from a door alarm on the exterior doors.
Alerts others for assistance: Door alarms can also be used on the bathroom door. They can be placed in such a way that they'll sound when the door is opened, letting you know that your loved one requires assistance in the bathroom.
String alarm: A string alarm can be placed high up on the door frame with the string placed across the door opening. If the door opens, it will cause the string, which is held in place by a magnet, to detach from the alarm, causing it to sound. The alarm will stop sounding once the magnet is reattached.
Passive InfraRed (PIR) alarms: A PIR alarm can be utilized across a door opening so that if the plane across the door is broken, the alarm will sound and alert you to your loved one's need for assistance.
Magnetic door alarms: Magnetic door alarms have two parts that are connected magnetically. One part is attached to the door frame right at the edge next to the door and the other part is attached to the door right next to the frame. The alarm sounds when the two parts are no longer connected by the magnet.
Floor sensor alarms: Floor sensor alarms have a sensor pad on the floor and a magnetic lock on the door. They can be preset to different settings, some of which will alarm immediately and other settings that allow a person to exit out the door and return just a short time later before sounding.
Remote sounding alarms: Some alarms are designed so that they sound away from the person who is trying to get out the door. You might place the sounding device of the alarm near you so that it doesn't startle the person with dementia but will alert you to their need for assistance.
Keypad locks: Another option if you have doors in your house that you don't want your loved one to open, you can simply lock them or have a keypad lock installed on those doors. The keypad locks will unlock once you enter the correct number code in the keypad. Keypad locks can connected be to the smoke or fire alarm system so that they will unlock in case of a fire.
GPS alert systems: There are several GPS devices that can assist with keeping your loved one safe. GPS trackers can be used in a variety of ways, such as in shoes. watches and bracelets. You can set up perimeters for when you want to be alerted (such as a doorway) or you can continuously track the person on an app on your phone. These types of systems allow you to have a flexible level of monitoring, depending on your loved one's needs.
A Word From Verywell
As caregivers , one of our worst fears may be that our loved one with dementia will accidentally get lost or purposely leave a house or facility, not be able to find her way back home and then become endangered. Utilizing strategies to prevent wandering, such as understanding the common causes and using door alarms, can hopefully reduce this risk significantly and provide a little more peace of mind.
National Institute on Aging. Home Safety Checklist for Alzheimer's Disease.
Agrawal AK, Gowda M, Achary U, Gowda GS, Harbishettar V. Approach to management of wandering in dementia: ethical and legal issue. Indian Journal of Psychological Medicine . 2021;43(5_suppl):S53-S59. doi: 10.1177/02537176211030979
Au-Yeung WT, Miller L, Beattie Z, Kaye J. Passive infrared motion sensors improved the detection accuracy of nocturnal agitation. Innovation in Aging . 2021;5(Supplement_1):955-955. doi: 10.1093/geroni/igab046.3417
Hall A, Wilson CB, Stanmore E, Todd C. Implementing monitoring technologies in care homes for people with dementia: A qualitative exploration using Normalization Process Theory. International Journal of Nursing Studies . 2017;72:60-70. doi: 10.1016/j.ijnurstu.2017.04.008
Megges H, Freiesleben SD, Rösch C, Knoll N, Wessel L, Peters O. User experience and clinical effectiveness with two wearable global positioning system devices in home dementia care. Alzheimer’s & Dementia: Translational Research & Clinical Interventions . 2018;4(1):636-644. doi: 10.1016/j.trci.2018.10.002
By Esther Heerema, MSW Esther Heerema, MSW, shares practical tips gained from working with hundreds of people whose lives are touched by Alzheimer's disease and other kinds of dementia.
- Sign In

Best Dementia Wandering Products
Caring for people with dementia can be a challenge, especially if that person is prone to wandering. Whether they end up out in the world, or are simply roaming around the house, they're at serious risk of falls or other accidents. In both professional and home care environments, preventative measures are essential, and help avoid stressful and frightening situations.
In this Best Dementia Wandering Products guide, we go over some brilliant dementia care items that our customers love. Each product is designed to help avoid specific wandering scenarios, so you can find the most appropriate items for you.
What Does This Guide Cover?
- Best Dementia Chair Pressure Mat
- Best Dementia Bed Pressure Mat
- Best Dementia Floor Pressure Mat
Best Dementia GPS Tracker
Best dementia alarm for doors and windows, best dementia motion sensor, best dementia crash mat, best dementia hip protector, looking for a full fall and wandering system, what else can you do to help prevent wandering, best dementia chair pressure mat.
Winner: Wireless Care Alarm Kit with Chair Leaving Sensor Mat
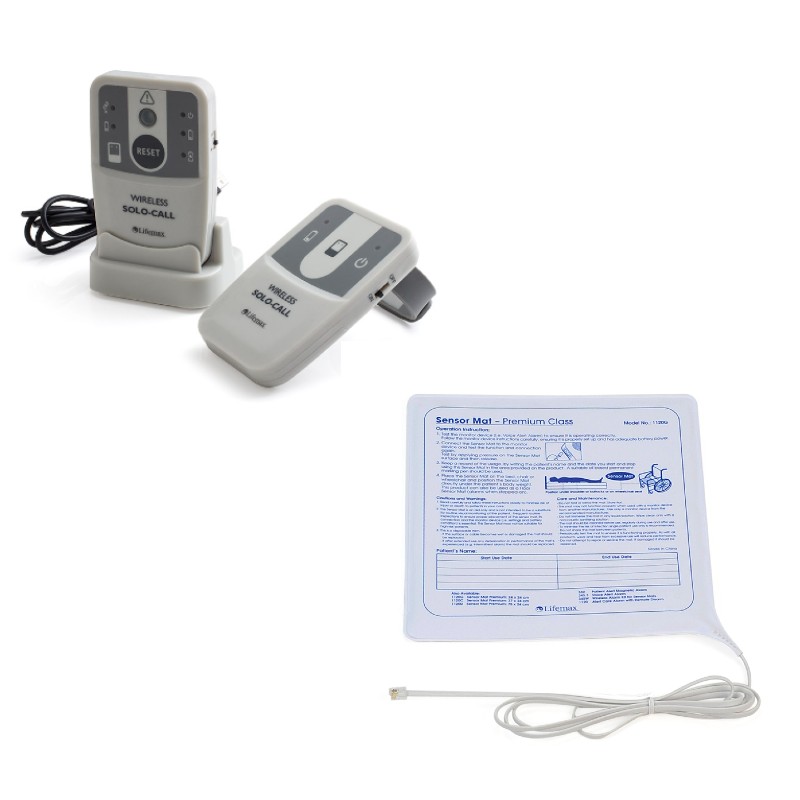
Why We Love It...
✔ Lets carers know immediately if a patient leaves or falls out of chair ✔ Small sensor pad fits comfortably and seamlessly on most chairs ✔ Receiver is wireless so a carer can always carry it with them
Not The Best For...
✘ Monitoring a larger surface area like a bed ( See our solution )
Customer Verdict: "A fantastic product. Very quick and easy to set up and it has been a great help in keeping my 95 year old father safe. His carer can now leave him sitting in his chair while she does jobs and know instantly if he has stood up. It has saved him from falling many times already and we have only had it a couple of weeks." Stephanie ★★★★★
Best Dementia Bed Pressure Mat
Winner: Nutrix Wireless Care Alarm Kit with Large Bed Leaving Sensor Mat
✔ Lets carers know immediately if a patient leaves or falls out of bed ✔ Design fits under patients back and can be used in nearly any bed ✔ Receiver is wireless with wristband so a carer can always carry it with them
✘ Protecting a patient from harm if they do fall ( See our solution )
Customer Verdict: "This sensor mat is really Brilliant. My mother gets out of bed during the night and this alarm let's me get to her before the possible of her having a fall." David ★★★★★
Best Dementia Floor Pressure Mat
Winner: Floor Pressure Mat Wander Alarm With Pager and Transmitter

✔ Huge 120m range so can be placed in most beneficial position in home ✔ Can be hidden under a rug or carpet for more discrete home care ✔ Wireless receiver is fantastic for busy, professional home care settings
✘ Keeping track of patients if they don't trip the alarm ( See our solution )
Customer Verdict: "Purchased this for my husband who has dementia and wonders a lot in the night. It alerts me when he is out if bed so I can reassure him and tuck him in again. Simple to set up and can hear it just on vibration or vibration and low level alarm bearing in mind I am quite deaf." Patricia ★★★★★
Winner: Medpage GPS Location Tracker Watch Phone with Fall Detection
✔ SOS fall alarm has precise mapping location so patient for safety ✔ Blood pressure and heart rate monitoring, plus medication reminders ✔ Battery lasts for 7 - 10 days to so it won't lose charge in an emergency
✘ Physical protection in event of fall ( See our solution )
Editor's Verdict: As well as being a tracker and SOS fall alarm, this Medpage watch is also a phone. This allows carers or loved ones to call the wearer in the event of wandering, to talk to them or someone that has found them. It's also a versatile care device with blood pressure and heart rate monitoring, along medication reminders
Winner: Wireless Door and Window Security Alarm with Radio Pager Kit

✔ Fixed next to doors or windows to notify when they've been opened ✔ Three notification settings: high volume, low volume and vibration ✔ 100m transmission range and a massive 6 months of battery life
✘ Preventing accidents within a room ( See our solution )
Customer Verdict: "Peace of Mind - This product is exactly what I needed. My father has dementia and can become confused at night. I now know instantly if he leaves his bedroom...so I can get a good nights sleep". Lorraine ★★★★★
Winner: Alerta Detect Motion Sensor and Wall Point Wireless Receiver
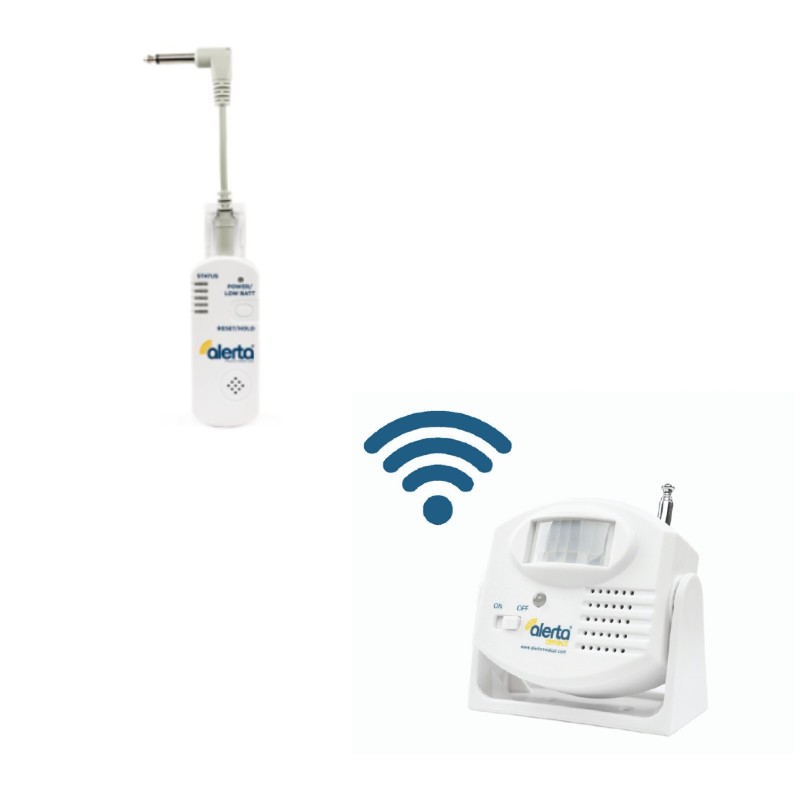
✔ Infrared PIR sensor detects body movement without physical contact ✔ Allows for greater patient freedom than floor pressure mats ✔ Powered by either mains or battery and connects to nurse call system
✘ A higher level of precaution ( See our solution )
Editor's Verdict: Offering an alternative to pressure mats, this infrared sensor detects patient movement without them having to physically trigger it. It offers greater freedom than a mat as it allows patients to get out of bed or move around the room without triggering an alarm, as long as they don't cross the sensor beam threshold.
Reducing Injury In Case of a Fall
Winner: Harvest High Density Foam Crash Mat

✔ High density foam ensures a cushioned landing in case of bed falls ✔ Waterproof and vapour-permeable cover ideal for incontinent patients ✔ Gives both patients and carers greater peace of mind when unsupervised
✘ Alerting carers before a patient falls ( See our solution )
Editor's Verdict: Ideally, if you use a bed pressure mat, a patient won't fall out of bed. However, in the time it takes for a carer to reach a patient, accidents can happen and it's important to be prepared. This high density foam mat offers fantastic cushioning to help avoid falls, which can be extremely dangerous for elderly patients.
Winner: Safehip AirX Hip Pad Hip Protector Underwear

✔ Wearable fall protection, not limited by location like a crash mat ✔ Breathable and elastane build offers long-lasting comfort ✔ Designed to be discreet and fit easily under regular clothes
✘ Protecting other parts of the body in case of falls ( See our solution )
Editor's Verdict: Hip injuries can be particularly debilitating for elderly people, especially those with dementia who might find rehab tricky. These underwear offer wearable hip protection that dementia sufferers can take with them wherever they go.
The mats, sensors and protective equipment above are great, especially for smaller scale, or home care environments. But if you're looking after multiple patients with dementia or other memory issues, you might want to consider a more comprehensive system like the Alerta Wireless Full Fall and Wander Alarm System .

✔ Incredibly comprehensive system for maximum patient safety ✔ Wireless receiver links to all five transmitters at the same time ✔ Includes 3 pressure sensors, a electric crash mat and a call button
✘ Smaller rooms or spaces ( See our solution )
Editor's Verdict: Perfect for professional care environments, or for extra-safe home care, this six-item bundle hugely reduces the chances of dementia wandering accidents. The receiver monitors all five sensors at the same time and can differentiate which one has been activated, so a carer knows exactly where they are needed.
To help prevent the worst case scenario, here are some simple steps you can take:
- Create a Routine - Having a concrete daily plan can help to prevent the restlessness that often leads to wandering. If your loved one is occupied with getting through their day, the risk of distraction can be greatly reduced.
- Ensure Needs are Met - Wandering is often triggered by a need to find water, food or go to the bathroom. If you make it safe and easy for your loved one to achieve these simple goals, it can go a long way to keeping them happy and relaxed.
- Have an Action Plan - If wandering does occur, make sure you're prepared. Ensure your loved one has an ID on them at all times, keep a recent photo and updated medical information on hand, and contact emergency services as soon as possible.
Need More Help Selecting A Dementia Wandering Product?
The alarms and other products we've talked about are some of our favourites, tried and trusted by our customers, but we understand everyone's care situation can be different. If you still haven't found what you're looking for, why not have a look at the rest of our Anti-Wander Alarm range.
Whether you're looking to make a professional care home safer, or just give a loved one a bit of peace mind, we're sure we have something for you!
Do you have any questions about our products to prevent dementia wandering, or something to add? Share your thoughts below or contact us on Facebook and Twitter .
Tags: Alarms and Alerts , Care Support , Dementia , Wandering
My mother has dementia and we need to get a floor mat as she is falling. Do you supply to ireland
Hi Marie, I'm sorry to hear about your mother, hopefully something like the Fall Alarm with Voice Alert mentioned above will be able to help. To answer your question, we do deliver to Ireland. This will usually incur an extra £10 delivery fee. If there's anything else you need, don't hesitate to ask and we'll get back to you as soon as we can. Kind regards, Eugene at Health and Care

- Managing Wandering Behavior in Dementia Seniors
Managing Wandering Behavior in Dementia Seniors: Memory Care Community Solutions
By Publisher | Published April 12, 2023 | Last updated April 12, 2023
Wandering behavior in seniors with dementia can be both perplexing and concerning for their loved ones and caregivers. With a lack of understanding of their environment and a diminished ability to express their needs, seniors with dementia may wander aimlessly, attempting to fulfill a basic need or to escape perceived dangers.
Memory care communities are specifically designed to provide safe and supportive living spaces that address wandering behavior while preserving the dignity and individuality of their residents. This article will explain the reasons behind wandering behavior in seniors with dementia . We will also explore the various strategies memory care communities implement to create secure, nurturing environments.
Understanding Wandering Behavior in Seniors with Dementia
Causes of wandering behavior.
Wandering can stem from multiple factors — physical, emotional, and environmental — which may include:
- Unmet needs : Hunger, thirst, or the need to use the bathroom may trigger wandering as the individual searches for a way to satisfy these basic requirements.
- Disorientation : Memory loss and confusion can cause seniors to feel lost, prompting them to wander in search of familiar surroundings.
- Boredom or excess energy : Idleness or restlessness may lead to wandering as a means to expend energy or find cognitive stimulation.
- Past routines : The ingrained desire to follow previously established routines or habits may spur wandering behavior.
The Risks of Wandering
Unmonitored wandering can lead to various hazards, including:
- Falls or injuries
- Accidents or getting lost outdoors
- Exposure to harsh weather conditions
- Fear, anxiety, and emotional distress for the individual and their family
Memory Care Communities: Creating Safe Living Spaces for Seniors with Dementia
Memory care communities strive to provide a comprehensive support system that addresses the unique needs and challenges of individuals with dementia. By incorporating specialized staff training, state-of-the-art security measures, and evidence-based design elements, these communities create safe and engaging living spaces that minimize wandering behavior and its associated risks.
Staff Education and Training
Expertly trained staff is crucial in managing wandering behavior in seniors with dementia. Memory care communities prioritize ongoing education and skill development, ensuring staff members:
- Understand the possible triggers for wandering.
- Recognize signs of agitation or anxiety that may precede wandering behavior.
- Employ effective communication techniques to guide residents calmly and compassionately.
- Respond quickly and effectively in case of emergencies.
Security and Monitoring Systems
Preventing incidents associated with wandering requires comprehensive security measures. Implementing these measures in memory care communities can include:
- Secure, monitored entrances and exits to prevent unauthorized departures and wandering outdoors
- Location tracking technologies to monitor resident movement within the community
- Video surveillance systems to maintain a visual record of resident activity
- Alarmed doors and windows to signal potential wandering attempts
Therapeutic Design Elements
Architectural and design features can significantly minimize wandering behavior, creating safe and easily navigable environments for seniors with dementia. Key design elements in memory care communities can comprise:
- Circular or looped walking paths that allow residents to wander with a purpose and prevent agitation from dead-end corridors
- Visual cues and signage to assist residents in locating restrooms, dining areas, and other common spaces
- Private and secure outdoor spaces where residents can explore safely and interact with nature
- Contrasting colors and patterns to help residents distinguish between various surfaces and objects, reducing potential confusion
Individualized Care Plans and Engaging Activities
Focusing on personalized care and tailored activities is crucial in addressing the root causes of wandering behavior. Memory care communities strive to:
- Develop comprehensive care plans that address individual needs, preferences, and personal histories
- Offer a variety of engaging activities and programs that meet residents' cognitive and physical abilities
- Monitor residents' daily routines and adapt care plans as needed , ensuring continued satisfaction of basic needs and desires
What is wandering behavior in seniors with dementia?
Wandering behavior refers to aimless movement or walking with no apparent goal, often indicative of confusion and disorientation resulting from dementia.
How do memory care communities address wandering behavior?
Memory care communities utilize specialized staff training, comprehensive security measures, therapeutic design elements, and personalized care plans to minimize wandering behavior and ensure the safety and well-being of their residents.
What are some possible causes of wandering behavior in seniors with dementia?
Wandering behavior can stem from unmet needs, disorientation, boredom, excess energy, or a desire to follow past routines.
How can I help prevent wandering behavior in a loved one with dementia?
Providing a safe and structured environment, addressing basic needs, offering engaging activities that match their cognitive abilities, and maintaining familiar routines can help prevent wandering behavior in seniors with dementia.
Addressing wandering behavior in seniors with dementia is an essential aspect of providing comprehensive and compassionate care. Memory care communities focus on creating safe living spaces that foster autonomy, self-esteem, and dignity. Through uniquely tailored strategies, memory care communities continue to enhance their residents' safety and overall quality of life, offering peace of mind to families, caregivers, and their loved ones living with dementia.
Related Articles
- Aging in Place
- Assisted Living vs. Nursing Home Care
- Depression: What Does it Look Like and When to Seek Help
- Memory Care: How to Find the Right One
- Memory Help — How to Boost Your Brain
- Senior Home Care
- Sundowners Syndrome: Facts and Care Tips
- What is Assisted Living?
- What is Dementia?
- What to Expect From the Aging Process
- When You Need to Place Your Parent in a Nursing Home
GreatSeniorLiving.com is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for sites to earn advertising fees by advertising and linking to Amazon.com and its partner websites.
© 2017 - 2024 GreatSeniorLiving.com
We may earn money when you buy through our links.
Home | Senior Safety | Best Door Chimes for Seniors with Dementia
Best Door Chimes for Seniors with Dementia

SafeWise experts have years of firsthand experience testing the products we recommend. Learn how we test and review .
Door chimes alert in-home caregivers when seniors leave the house—which could be dangerous for people with Alzheimer’s and dementia.
These door chimes for seniors differ from traditional home security door sensors because they don’t send alerts to a monitoring center or app, nor do they set off a loud siren meant to scare people. Instead, the in-home caregiver keeps the chime box in their pocket or a central location for instant alerts.
Our favorite door chime for seniors is the SMPL Alerts 4-in-1 kit because the caregiver can carry around its alarm pager, and there’s a motion sensor and wearable call button to round out the package.
Best door chimes for seniors
- SMPL Alerts : Best overall
- YoLink : Best for multiple doors
- Stechro : Best for budgets
- EverNary : Best motion sensor
- Alerta Patch : Best wearable
- How we reviewed
Compare the best door chimes for seniors with dementia
*Amazon.com price as of post date. Read full disclaimer .
Best senior door chimes reviews
1. smpl alerts: best overall.
*Amazon.com price as of post date. Read full disclaimer .
The SMPL Alert 4-in-1 Kit covers all the bases for ensuring your loved one doesn’t wander out the door. The motion sensor can be placed near the door for an early warning alarm, while the door sensor lets you know when the door opens. This kit includes a portable pager and a wearable help button.
You can also use the motion sensor from this kit in another area of the home, such as near the senior’s bed for a fall alert.
The pager includes a belt clip and works within 250 feet of the sensors. And the pager sounds an alarm while also vibrating and flashing.
We love that this system also includes a help button seniors can use to call for help. It only works if they’re still in range of the pager, though, so it won’t work if they’ve already wandered too far.
2. YoLink: Best for multiple doors
The YoLink Smart Home Starter Kit includes four door sensors and a base station. Its station announces which door opened, which is especially useful in a larger home since caregivers will know which exit to check.
The base station works within 1000 feet of each sensor and uses a special technology called LoRa to improve its range over multiple floors. YoLink can also tell you when a door is ajar.
3. Stechro Wireless Door Chime: Best for budgets
The Stechro Wireless Door Chime is a budget-friendly option with one flaw: the chime must stay plugged in. But with five volume levels, it should be loud enough for caregivers to hear, especially when placed in a central location.
You can get kits with up to three Stechro Door chimes to cover all exits in the home. Up to 62 ringtones are available, which helps prevent the chime sound from scaring seniors who may already feel confused.
The Stechro Wireless Door Chime has the second-longest range on our list at 600 feet, making it ideal for larger homes.
4. EverNary: Best motion sensor
The EverNary Wireless Caregiver Pager connects to a motion sensor instead of a door chime. This connection makes it ideal for an open floor-plan space to alert the caregiver when the senior wanders close to the door.
We especially like the adjustability of the EverNary motion sensor, allowing you to set it up just right for fewer false alarms.
Be sure to select the Portable Pager option for a chime caregivers can take with them. It has a limited range of just 260 feet in an open area. We recommend testing how far the pager works in your home since walls and other obstructions can lower the range.
5. Alerta Patch: Best proximity wearable
The Alerta Patch offers a unique solution for Alzheimer’s and dementia wandering prevention. A wearable sensor applies to the skin on the person’s upper back for one month. The sensor pairs to a “Wedge,” which looks like a remote control. An alarm goes off if the sensor travels farther than 65 to 95 feet away from the Wedge.
This option is excellent for seniors who have tried to remove other wearable devices or may be a flight risk when attending appointments or other activities away from home.
Unfortunately, there’s no tracking technology in the patch. If your loved one disappears, the Alerta Patch can’t help you find them. Check out our recommended GPS trackers for Alzheimer’s and dementia instead if you need tracking.
We think the best door chime for seniors is the SMPL Alert . It’s a basic bundle of senior monitoring products for in-home caregivers. It also has a portable pager that offers three alerts. You can stick with the starter kit or buy additional SMPL sensors to cover every exit.
Are there other types of wandering alerts for seniors?
Yes, there are other types of wandering alerts for seniors. For instance, you can use pressure-sensitive floor mats as a door alert instead of motion or door sensors.
Can I use a video doorbell as a wandering sensor?
Yes, video doorbells can be positioned inside the door and used as a more sophisticated motion sensor. Be sure to get one with a motion-activated chime so that the in-home caregiver can hear when it goes off. However, we like portable pagers made especially for seniors who wander because the chime goes off continuously.
How we reviewed door chimes for seniors
We looked for door chimes offering a connection to a portable pager or had another unique alert system for in-home caregivers. We also based our top recommendations on the signal range and the ability to add more sensors if needed. Learn more on our methodology page.
Related articles
- Best Medical Alert Systems
- Room-by-Room Guide to Senior Safety
- Best Safety Devices for Seniors
*Product prices and availability are accurate as of post date and are subject to change. Any price and availability information displayed on Amazon at the time of purchase will apply to the purchase of this product. Safewise.com utilizes paid Amazon links.
Certain content that appears on this site comes from Amazon. This content is provided “as is” and is subject to change or removal at any time.
Recent Articles

About Contact Press News Deals
Home Security Internet Security Home Safety Family Safety Senior Safety
Car Safety Smart Home Emergency Prep Pet Safety Personal Safety
Subscribe to SafeWise for updates on safety news, product releases, and deals!
Terms of Service | Privacy Policy | How We Rank and Review |
*SafeWise has conducted impartial research to recommend products. This is not a guarantee. Each individual’s unique needs should be considered when deciding on chosen products.
©2024 SafeWise. All rights reserved.

Sweet Moment Senior Dog With Dementia Forgets He's Already Greeted Owner
S eeing our four-legged best friends age and deteriorate is one of the hardest experiences to go through, because after so many years of love, they need us more than ever.
That's exactly what Dennis Gerard, 60, is facing with his rescue dog Piper, who turned 17 years old last year. The senior dog is now blind, deaf, and suffers from dementia. Gerard told Newsweek that he's "slowly getting worse," which is devastating to witness.
However, age isn't going to stop Piper from adhering to his usual routine, so he still loves to greet his owner with a kiss and a happy dance when he returns home. But Gerard, from Jacksonville, Florida, recently captured the moment Piper evidently forgot that his owner had already come back home, and he continued to wait in the hallway for him and got stuck as he couldn't see where he was going.
"I came home from work and Piper was waiting in the foyer by the back door for me. Once I entered and he smelled me, then he performed his usual ritual of kissing me and dancing and welcoming me home," Gerard said.
"A half-hour later, I was making a sandwich and watched him wander into the foyer and position himself for me to come through the door again. He was having a bad day and he forgot that I'd just come home. He was waiting for me again, it was so sad."
Gerard rescued Piper when he was 2 years old, and they've shared countless happy memories in the 15 years since. But it's been heart-breaking for the owner to watch the pooch's health slowly decline, especially this moment, which was the first time Piper had forgotten that his owner was already home.
Dog dementia is not uncommon in senior pooches, and it can also be referred to as canine dysfunction syndrome (CDS). One study revealed that signs of dog dementia increased to 68 percent in dogs aged over 15 years.
The American Kennel Club states that symptoms usually include disorientation, house soiling, a change in sleep patterns, and a change in activity levels. Owners may also see a change in their relationships, as a once independent dog may become clingier for example. Senior dogs may also develop new fears or vocalize more, which can be attributed to increased nervousness.
Sundowner syndrome is another sign of cognitive deterioration, causing a dog to sleep more during the day and then become restless at night, or they may pace or bark for no apparent reason during the night instead of sleeping.
Sadly, there is no cure for dog dementia or CDS, but the AKC recommends that owners help manage the symptoms, provide the dog with a schedule they can follow, and give them plenty of mental enrichment.
How Did Social Media React?
Living with a senior dog isn't easy, but Gerard documents his life with Piper on social media (@dennis.gerard on TikTok and @pipersdad3 on Instagram ), to show that an old dog is no less important or loving. The sweet clip of Piper getting "stuck while sundowning" has been viewed over 2.4 million times and gained more than 186,900 likes on TikTok in just a matter of days.
"People can really connect emotionally with posts like this," Gerard told Newsweek after the video went viral. "I've had thousands of comments, and every one of them is positive and uplifting, people are sharing their similar experiences with their dogs both past and present.
"We live in a time of great division, but senior dogs like Piper can unite us around a common platform of love, empathy, and compassion. This is one of those things that's sad and cute at the same time, I love it and I hate it. I am his whole world, and it does bring me great joy seeing how much he loves me."
Despite his age, it's not just Gerard who loves Piper so much as the senior dog has earned plenty of fans through social media. And one thing is for certain, they can all agree that "Piper is a good boy" no matter how old he gets.
Many TikTok users were deeply moved by the video, and it's already gained over 5,300 comments. One person wrote: "Why does any of this have to happen to our babies."
Another TikTok user responded: "We are the keepers of their souls until it's time to cross the rainbow bridge."
A third comment reads: "So beautiful and sad at the same time."
Do you have any heartwarming videos or pictures of your pet you want to share? We want to see the best ones! Send them in to [email protected] and they could appear on our site.
Start your unlimited Newsweek trial

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Sensors (Basel)

Intelligent Sensing Technologies for the Diagnosis, Monitoring and Therapy of Alzheimer’s Disease: A Systematic Review
Associated data.
Not applicable.
Alzheimer’s disease is a lifelong progressive neurological disorder. It is associated with high disease management and caregiver costs. Intelligent sensing systems have the capability to provide context-aware adaptive feedback. These can assist Alzheimer’s patients with, continuous monitoring, functional support and timely therapeutic interventions for whom these are of paramount importance. This review aims to present a summary of such systems reported in the extant literature for the management of Alzheimer’s disease. Four databases were searched, and 253 English language articles were identified published between the years 2015 to 2020. Through a series of filtering mechanisms, 20 articles were found suitable to be included in this review. This study gives an overview of the depth and breadth of the efficacy as well as the limitations of these intelligent systems proposed for Alzheimer’s. Results indicate two broad categories of intelligent technologies, distributed systems and self-contained devices. Distributed systems base their outcomes mostly on long-term monitoring activity patterns of individuals whereas handheld devices give quick assessments through touch, vision and voice. The review concludes by discussing the potential of these intelligent technologies for clinical practice while highlighting future considerations for improvements in the design of these solutions for Alzheimer’s disease.
1. Introduction
Globally, neurological diseases (ND) are the primary cause of disability-adjusted life years (DALYs) [ 1 ]. Of these, stroke and Alzheimer’s along with other types of dementia are the two leading causes of DALYs [ 2 ]. Moreover, neurological diseases are the second leading cause of death all over the world [ 1 ]. People suffering from neurodegeneration undergo neuronal structure and functional losses. These abnormal structural changes in the brain provide a hindrance to normal brain function. As in the case of Alzheimer’s, the typical neuropathological hallmarks are the accumulation of beta-amyloid plaques and the formation of protein tau-tangles beside others [ 3 ]. These lesions provide interruptions in the synaptic transmissions from one neuron to another. The neurons start to lose their connections with the other neurons in the brain [ 4 ]. This results in the deterioration of the normal brain and human body functions [ 5 ]. Thus, the people that suffer from neurodegenerative diseases such as Alzheimer’s slowly start to lose their cognitive abilities and motor functions. This eventually renders them to be dependent on others for carrying out their activities of daily life (ADLs). To date, no standard cure has been put into practice for these conditions, although there have been extensive attempts in this regard [ 6 ].
Besides genetics and inheritance, age is one of the greatest risk factors for Alzheimer’s disease (AD). According to the 2020 annual report by the Alzheimer’s Association, 3% of people between the age of 65 and 74 years are currently suffering from Alzheimer’s disease. This number drastically increases with the increasing age window. This is evident from the statistics that show 17% of the people aged from 75 to 84 years, and 32% of the total people aged 85 and above are currently suffering from Alzheimer’s disease [ 7 ]. Neurodegeneration is relatively a slow process. However, once started, it cannot be reverted.
At present, the diagnosis of Alzheimer’s disease heavily depends on neuroimaging techniques. These tests include brain scans such as Magnetic Resonance Imaging (MRI), Positron Emission Tomography (PET) and Computed Tomography (CT). These scans although being effective, prove to be a challenge for people with neurological conditions. These methods are bulky, expensive and even invasive as in the case of PET scan. Dedicated lab requirements result in random episodic monitoring of the Alzheimer’s patient. This increases the chance for late detection of further neuronal damage. Moreover, the majority of the existing therapeutic solutions for Alzheimer’s include physical exercises to retain the physical functionality of the body and cognitive exercises for strengthening the existing brain cells. However, for these type of solutions, dedicated time and frequent or continuous help of either a clinician, nurse, formal or informal caregiver are required. This all amounts to the social, emotional, economical and physical burden on the caregivers. Given the progressive nature of the disease, the individuals suffering from it must be monitored regularly or continuously.
With the advancements in ubiquitous and pervasive computing, cloud and wireless technology, topping it all up with Artificial Intelligence (AI), the literature is rich with their application in dementia [ 8 , 9 , 10 ]. The proliferation of miniature sensors in smart devices such as smartphones and tablets, and ambient sensors that are designed for smart homes are playing a substantial part in the remote and continuous monitoring of Alzheimer’s disease [ 11 ]. Sensors form the backbone of these intelligent systems which enable these to sense various signals of interest from the environment. These sensors monitor signals from the humans and as well as the surroundings thus providing contextual information. These signals are then monitored and processed by embedded processors which provide an automatic response through actuators. This feature of the provision of apt feedback and response distinguishes these smart and intelligent technologies from the conventional ones [ 12 , 13 , 14 ]. This particular strength can be used for the management of diseases where continuous monitoring and adaptive responses are required, such as in Alzheimer’s disease. These technologies have the potential to provide autonomous care along with continuous yet remote monitoring of the patient improving their quality of life [ 15 ].
A handful of review studies exist that focus on the complex and specific needs of Alzheimer patients using assistive technology. Costanzo et al. [ 16 ] talk about the treatment and diagnostics of Alzheimer’s disease and mild cognitive impairment (MCI) with the help of telemedicine. They emphasize the fact that the use of technological services such as emails and video conferencing can prove effective sources for the detection and follow-up between the patient and the doctors. The work in [ 17 ] presents a scoping review of the general technological solutions for AD patients. Pillai and Bonner-Jackson [ 18 ] provide an overview in their study on the randomized clinical trials for AD patients using general information and communication systems. The systems mentioned in their study are used for monitoring cognitive and functional decline. The study outlines the strengths and weaknesses of these systems focusing on randomized clinical trials; however, it includes published articles until 1 September 2014. Hence, it is not an up-to-date overview of these solutions anymore. Elfaki and Alotaibi [ 19 ] present an overview of only the mobile health applications used for the assistance of AD. Studies [ 20 , 21 ] deal with the role of Virtual Reality Technology used for the diagnostics and cognition training of Alzheimer patients.
Based on the existing reviews, the following research gaps are identified:
- The existing reviews focus on the role of telemedicine or the general information and communication technologies for Alzheimer’s disease [ 16 , 17 ]. No recent review exists that focuses on the management of Alzheimer’s disease alone, using intelligent systems and devices.
- The existing review studies focus on a sub-class of intelligent or smart assistive technologies such as mobile phones or virtual reality for AD [ 19 , 20 , 21 ] and do not cover a broader spectrum of intelligent feedback systems.
- Some of the review studies are general in nature, covering intelligent technological solutions for all types of dementia, including Parkinson’s disease, etc., such as in [ 14 ]. This hampers the understanding of how these intelligent solutions can effectively be used for the complex and intricate needs of Alzheimer’s patients.
- The existing reviews either focus on part of the disease progression such as the early detection of AD [ 9 , 20 , 22 ] or therapy [ 21 ] or only on the monitoring of the functional decline of AD patients [ 18 ]. No review study exists that categorizes the intelligent solutions for the complete progression of Alzheimer’s disease, hence, providing a comprehensive picture of the role of these sensing technologies for Alzheimer’s disease.
Thus, there is a need for a recent up to date review that highlights the existing intelligent and smart technologies that are capable of assisting and managing Alzheimer’s disease. This review study aims to provide an up-to-date state of the knowledge for the intelligent assistive technological solutions for Alzheimer’s disease by searching the literature in the last five years. Moreover, according to [ 14 ], the number of intelligent assistive technologies is doubling every five years. Hence, the current systematic review intends to address the above-mentioned research gaps and contributes to the literature in the following ways:
- It provides a detailed overview of the recently researched intelligent technologies mentioned in the literature, focusing only on Alzheimer’s disease. Thus, the findings of the review will help in translating the researched solution into clinical practice as well as remote diagnosis and monitoring of the disease. The review tends to raise awareness of the potential of these automated intelligent solutions among the stakeholders (clinicians, caregivers and Alzheimer’s patients). Moreover, emphasizing only on Alzheimer’s disease will facilitate future research focus on the complex needs and particular symptoms of Alzheimer’s patients.
- The review covers a broad spectrum of intelligent solutions designed and researched for the complete progression (diagnosis, monitoring and therapy) of Alzheimer’s disease. This will aid in provision of a broader picture and a comprehensive understanding of the role of these sensing technologies throughout the Alzheimer’s progression.
- The review study also aims to evaluate the efficacy and usability of these proposed solutions. For this purpose, the review focuses on the studies, identified in the searched databases, which implemented the solution and involved Alzheimer patients for the validity of their proposed intelligent solution.
- The review study discusses the practical implications of these intelligent solutions. Moreover, it also highlights the limitations of the current researched studies and the areas that need consideration for better and improved solutions, thus indicating new directions for researchers in this field.
The remaining review article is organized as follows: Section 2 describes the materials and research methodology undertaken for the systematic review. It states the research questions for the current study, followed by the detailed description of the database search and the articles’ screening methodology. Section 3 gives a comprehensive analysis of the results identified in the literature search. This is followed by Section 4 , which discusses the results, the social and economic impact of these technologies and how they can play a vital role in improving the quality of life of Alzheimer patients and of those who are responsible for caring for and treating them. This section also highlights the current limitations identified in the searched studies and provides suggestions for future improvements. Finally, Section 5 provides the conclusion of the review study.
2. Materials and Research Methodology
To provide an oriented and impactful outcome, the research questions addressed in our review article are explicitly stated in Table 1 . The first two questions highlight the overall motivation behind the study. They focus on the kind of intelligent sensing technologies that exist in the literature for the care of Alzheimer’s disease and the purpose served by these technologies, in its management. Keeping in view the scope of the current article, we tend to focus on intelligent sensing technologies that can provide low-cost solutions and do not require dedicated labs or expensive equipment for the diagnosis, treatment and monitoring of Alzheimer’s disease patients. The third research question is a focused research question (FRQ). It tends to focus on how the different stakeholders are involved in the design of these systems and devices and what are the challenges faced and limitations in the existing solutions. Emphasis is given on how the proposed designs or prototypes have used the user-centric design approach.
Research questions.
RQ: Research Question; FRQ: Focused Research Question.
Systematic Search Methodology
A systematic search was carried out using the PRISMA guidelines [ 23 ]. Four databases were explored. The database search engines accessed were: Scopus, PubMed (Medline), Web of Science and IEEE Xplore. The articles searched were from 2015 until the 6 January 2021, the date on which the databases were searched. Only English language articles indexed in the above search engines were considered for inclusion in this review. The document type selected for the current review included only ‘Articles’ that were published in the journals whereas all remaining document type categories, such as books, book chapters, conference proceedings, etc., were excluded.
Significant consideration was given while choosing the keywords for searching the required studies. Various combinations were tried. As an example, the very first combination that was used by the authors was “Alzheimer” AND “smart OR intelligent” AND “sensor OR device”. After seeing the results, a modification was made by adding the keywords ‘assist, assistive or robot’ with ‘device OR sensor’, to widen the spectrum of the required results. Hence, the final combination of the keywords used was the combination of: (Alzheimer) AND (smart OR intelligent) AND (device OR sensor OR assist OR assistive OR robot). These keywords were searched in the data fields of the ‘Article title, Abstract and keywords’ in the advanced search option. For example, the search strategy in the IEEE Xplore database performed on the 6 January, 2021 was: (“All Metadata”: Alzheimer) AND (“All Metadata”: smart OR “All Metadata”: intelligent) AND (“All Metadata”: device OR “All Metadata”: sensor OR “All Metadata”: assist OR “All Metadata”: assistive OR “All Metadata”: robot). The same was repeated for Scopus, Web of Science and PubMed databases.
This search methodology resulted in a total of 253 journal articles (Scopus: 63, Web of Science: 60, PubMed: 23 and IEEE Xplore: 107). Next, 57 duplicates were removed, first by using the EndNote software and then by screening the articles for the title, abstract and author names. Based on the scope and inclusion criteria, 121 articles were removed after screening the title and abstracts. Finally, reading of the full text of the remaining articles was carried out by the first author and thorough discussions between both the authors led to the inclusion of 20 articles. The inclusion and exclusion criteria used by the authors is described in detail below.
To be included in the current review study the articles needed to
- Have included an intelligent or smart solution for the diagnosis, monitoring, assistance or therapy of Alzheimer’s disease.
- Include Alzheimer’s or MCI patients along with sufficient information about the methodology of the design and study. However, those studies were also included whose participants were older adults aged 55 years and above. The studies including young healthy controls were also included if they were used as a control group, acting as comparators to the AD patients.
- Have sufficient information about the evaluation metric and result validation.
- Be written in the English language.
- Be a published journal article.
- Be published between the years 2015 to 2020.
However, the articles were not included if
- They had AI algorithms implemented on neuroimaging scans, EEG signals or similar data from existing Electronic Medical Records.
- Used specialized or dedicated lab equipment for the detection of metal ions, chemical structures or drug delivery inside the body.
- Were theoretical such as interviews or perspectives from caregivers.
- Implemented activity recognition or systems to mimic human behaviour for smart future agents.
Figure 1 , below, describes the PRISMA flow diagram for the searching, screening, eligibility and inclusion of the identified articles for the current review.

PRISMA flow diagram for search methodology.
Following the research methodology detailed in Section 2 , a total of 20 articles were included in the analysis and classification for the current review paper. Two broad categorizations of the intelligent technologies used in the article studies were observed. These include self-contained handheld devices and the distributed systems. Out of the studies selected, 11 fell under the category of distributed systems. These distributed systems included the installation of various sensors in a residential setting or a care home. These sensing nodes collected various signals from the patients and environment, sending them to the cloud or other processing units. After computations, suitable actuators in the homes were activated providing intelligent feedback to Alzheimer’s patients. The remaining nine studies dealt with the implementation of solutions involving technologies such as smart devices, the development of software applications that run on these smart devices, and virtual assistants such as robots.
The following subsections describe in detail the kind of sensing technologies and their supporting systems used in the proposed solutions. This addresses Research Question 1 which states that ‘What intelligent technological solutions exist in the literature that may help in the assistance and management (diagnosis, monitoring and therapy) of Alzheimer’s disease?’ The different study outcomes, that is, the various stages of disease profiling (diagnosis, monitoring and therapy), require different methodology and require the monitoring of different signals. Hence, the initial part of the results provides a description of the methodology, participants involved and the intervention used, describing the effectiveness and acceptability of the proposed solutions. This addresses Research Question 2 which states that ‘How do the proposed intelligent technological solutions help in the assistance and management (diagnosis, monitoring and therapy) of Alzheimer’s disease?’
To evaluate the effectiveness of the researched intelligent solutions, the comparator used in the study for result validation is also clearly reported. Some studies compared their results to a standard clinical test while others used a control group to explain their evidence-based outcomes. These descriptions then are followed by tables that further classify the studies implementing the distributed and self-contained solutions for Alzheimer’s disease. The tables summarize the duration, participants, technology used, study design and the particular measurements monitored by the sensors and devices for the study outcomes (diagnosis, monitoring and therapy). The tables also highlight the key findings, limitations and report whether the design or study included the user-centred design approach or not. These thus address the last Focused Research Question which states that ‘How are these intelligent systems and devices incorporating the user-centric design and what are the limitations in the existing designs implementations?’ The limitations and challenges are also further discussed in detail in Section 4 of the review article.
3.1. Distributed Systems
Distributed systems are systems that have multiple sensing nodes, data processing sub-systems and actuators that are activated according to the requirement and context as sensed by the sensors. These multiple components interact with each other through computer networks via network protocols. According to [ 6 ], the subsystems “host processes and use a set of protocols to aid in the coherent execution of the distributed activities”. The studies that realized these distributed systems were conducted longitudinally in either the care homes, nursing homes, labs or residential homes where the Alzheimer’s patients resided. The following subsections provide a classification of the studies based on their outcomes.
3.1.1. Diagnosis of Alzheimer’s Disease
In the clinic, there are standard tests used for the diagnosis of Alzheimer’s disease. Besides the neuroimaging scans which indicate structural changes in the brain, there are other questionnaire-based tests as well. These tests evaluate the cognition of an individual through questionnaires or similar screening tools. Common examples include Clinical Dementia Rating (CDR) [ 24 ], Mini-Mental State Exam (MMSE) [ 25 ] and Montreal Cognitive Assessment (MoCA) [ 26 ]. However, these tests provide a sporadic and subjective assessment. The continuous monitoring of the vulnerable population can result in an early diagnosis as well as objective measurement for the detection of Alzheimer’s disease progression.
Autonomous detection of early-stage Alzheimer’s, MCI, was carried out in a study by Akl et al. in 2015 [ 27 ]. The study included 97 participants all aged 70 years or above with CDR score < 0.5 and MMSE > 24 at the start of the study. Each participant was living independently in a home equipped with smart sensors. They were continuously monitored for a period of 3 years. CDR and MMSE assessment was repeated by the end of each year, for the three years. For comparison, at the start of the study, participants were categorized as cognitively intact or baseline MCI. The data collected was that of walking speed and activity throughout the day. Passive infrared sensors, installed in the homes, were used to collect the walking speed data. Signal processing and machine learning algorithms (Support Vector Machine (SVM) and Random Forest (RF)) were applied to the data. The authors concluded that the most important measurements in detecting MCI were weekly trajectories, the variation coefficient of walking speed, coefficient of variation of the subject’s morning and evening walking speed along with their age and gender. In their study, they successfully distinguished MCI individuals from the cognitively healthy elderly.
In another study by Akl et al. in 2017 [ 28 ], the authors used the data from smart homes of 68 elderly patients having the same characteristics and in the same environment as mentioned in their earlier study [ 27 ]. However, in [ 28 ], they built generalized linear models (GLMs) of the everyday activities of the individuals and did not use any predefined measures for the detection of cognition. They concluded that by using normalized Kullback-Leibler divergence on the GLMs with 12-week window size, their technique resulted in a successful generalized solution for the detection of MCI. They also noticed that while the participants transitioned to the MCI stage there was no significant slowing in the gait speed.
A detection system based on Alzheimer disease ontology using agent-based technology, smart IoT devices including mobile phones and RFIDs was implemented by Kaur et al. [ 29 ]. Data collected from 374 patients with ages 60 to 96 years was used in the study. A cloud platform for the storage of the data and their processing was used. The detailed information of the patients including all the demographic, health (including symptoms) and MMSE data was fed to the smart system for the detection of Alzheimer’s disease. The study was qualitatively validated based on accuracy, usability, readability and convenience as compared to the similar four existing ontologies in the literature. Quantitatively, it was verified by using 100 patients out of the 374 for testing. Various classifiers were used such as Naïve Bayesian, J48 and the ontology Bayesian Network, with the latter performing the best. The measure used for assessing the accuracy of the system was the area under the curve (AUC) [ 30 ] with a value of 0.76. This was the greatest as compared to other classifiers used in the study. In addition to this Bayesian Network decision model, the system also monitored the physical location of the 100 patients using RFIDs that continuously updated the clinician through an android application developed for the purpose. The application also gave reminders to the patients for medicine and had memory recall exercises. Thus, assisting the patients as well as diagnosis.
In the study done by Alberdi et al. [ 31 ], the authors attempt to predict various symptoms that are an indication of Alzheimer’s disease. Smart-home sensor data were used to detect decline of cognition, changes in mobility and mood decline. The duration of the study was more than 2 years, and a total of 29 older adults were involved in the study. Various standard tests for mobility, cognition and mood were carried out at the beginning of the study and repeated after a period of every six months. For mobility, the tests included Arm Curl [ 32 ], Timed Up and Go Test (TUG) [ 33 ]. For cognitive decline, the standard test used was Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) [ 34 ] and Prospective and Retrospective Memory Slips (PMRQ) while the mood was assessed using Geriatric Depression Scale (GDS) [ 35 ]. Based on the tests scores, the 29 participants aged 73–97 years old were classified as cognitively healthy (N = 13), at-risk (N = 10) and participants with cognitive difficulties (N = 6). Regression analysis was performed, and the study concluded that mobility, depression and cognition can reliably be predicted using smart home sensors. The results also indicated that mobility scores were correlated most with behaviour followed by cognition. The daily routine and socializing patterns of the participants were important indicators for the various symptoms’ detection. Moreover, the overnight activities such as visits to the toilet and sleep patterns and mobility routines were correlated with cognition. Finally, in-home and outing activity was considered to be related to a diagnosis of depression although it lacked statistical evidence.
3.1.2. Continuous Monitoring of Alzheimer’s Patients
Alzheimer patients suffer a range of functional deterioration along with a decline in cognition. The continuous context-aware monitoring can help in timely detection of this descent in daily capabilities providing opportunities for timely interventions. The sensors used in the distributed systems can measure certain signals that may reveal information about the individual’s changing health and personal behaviour. Algorithms and models then can make a viable assessment to predict the declining functionality of the individual. The continuous monitoring of the individuals also enables them to assist either automatically using intelligent voice assistants, pre-recorded messages or can alert the caregiver for a timely intervention. The studies included in the review provide with assistance as described below:
- (a) Detection of Abnormal Behaviour
Abnormal behaviour is one of the main challenges when it comes to Alzheimer’s patients. Alzheimer patients often suffer from agitation and decline in mood. Alvarez et al. [ 36 ] used a range of sensors including wearable bracelet, zenith camera, Microsoft Kinect v2, magnetic binary sensors and wireless sensor network beacons to detect abnormal behaviour. These were used in an indoor multi-patient setting. The signals measured from the sensors included physiological data such as heart rate and skin temperature along with motion and location tracking data. The study included 18 patients in a hospital setting, aged 55–94 years, however, not suffering from cognitive issues. These patients were classified as very ill, moderate ill and mildly ill by their doctors. The duration of the study was 10 weeks. A weighted probabilistic model was used depending on the fusion scheme of the collected data from the multiple sensors used. The system was able to detect abnormal behaviour with an accuracy of 98.4%. This decision was based on the correlation calculation of the activities performed by the individuals and where those particular activities were performed.
- (b) Detection of Autonomy in Activity Performance
Automatic and objective detection of autonomy in the everyday tasks of Alzheimer patients was carried out by Karakostas et al. [ 37 ]. In total 109 participants were part of the lab-based study across two different geographical regions (France and Greece). From France, there was a total of 11 participants which included both, MCI patients and Healthy Controls (HC). Similarly, the remaining 98 participants were categorized as 27 AD, 38 MCI and 33 Healthy Controls (HC). These were assessed on MMSE scores (both sites), Functional Rating Scale for Dementia (FRSSD) and Functional Cognitive Assessment. The labs were instrumented with the necessary information computed technologies; video cameras, tags on house objects and mobile phones to run applications were used. The data collected from these sensors were used for the automatic detection of the (i) participants and (ii) tasks performed, and (iii) autonomy level was done using AI and signal processing algorithms on video signals. The instrumental Activities of Daily Living (iADLs) used for assessment were making an online payment, preparing a drink, medicine box preparation and talking on the phone. Results indicated a statistical correlation between the findings from both geographical regions. Moreover, using statistical analysis using the ANOVA (analysis of variance) test, the results confirmed that the autonomy level of HC is much better than MCI patients, and similarly, the autonomy level of MCI patients is better than that of AD patients.
- (c) Provision of Assistance
Barley et al. [ 38 ] used a smart auto-prompting system to assist people with cognitive problems. The system developed was used for guiding the patients with cognitive problems or memory problems while they perform their iADLs. The eight activities performed included common household chores such as cleaning the kitchen, using the telephone, doing laundry, and cooking. The participants in the study included 15 elderly aged 59–91 years old. All of them met the criteria for mental disorders defined by the Diagnostic and Statistical Manual of Mental Disorders-IV-TR. A university furnished apartment fitted with smart sensors, actuators, speakers, cameras and TV screens was used as a testbed. The prompting system consisted of pre-recorded automated messages. If the user could not follow the instructions given by the auto-prompt system, they were told to go to the nearest TV screen. There a video with all the required steps for the particular task was shown on how to complete the activity they were having difficulty performing. Two experimenters observed the reactions of the elderly patients to how they responded to the automatic prompting systems. Qualitative assessment was carried out with a team of 4 experts from gerontology, nursing neuropsychology and assistive technology. It was concluded that context and the level of cognition level affects the acceptability of auto-prompting systems, as the people suffering from cognition problems showed levels of stress while responding to non-human prompts.
Similarly, in a study by Cavallo et al. [ 39 ], a system using smart domiciliary sensors was developed to assist Alzheimer patients and their caregivers. The design phase of the system involved a team of physicians, patients, caregivers and psychologists. Initially, they tried to assess specific user needs through interviews, hence, giving a good example of user-centric design. Based on the results, they identified four key concerns, including functional monitoring, alerting of an emergency, social behaviour and support for cognition. Based on these results, they designed solutions for the four domains mentioned. A total of 14 Alzheimer disease patients were recruited for the study, aged 80 years and above. According to MMSE, they were classified as AD-phase 1 and 2 patients. To address the concerns the researchers developed an in-home bed-chair monitoring system, patient location indicator and a home enter exit system. The sensors used for the bed-chair system were two metallic plates that acted as a closed switch when someone sat on them. The door open-close was monitored by a magnetic switch while to indicate the location the patients had to wear a device integrated with Global Positioning System (GPS) and Global System for Mobile Communication (GSM). All the sensors communicate with a remote computer monitored either by a caregiver or spouse of the patient through Zigbee. To support cognition, the system included the use of music and videos related to the past of the users for therapy purposes acting as stimuli. The duration of the study was not fixed, and only those systems were implemented in the home of the patients as per need or specified by the users themselves. The authors concluded that the acceptability and usefulness value of the implemented systems was 50% and 30%, respectively, as reported by the users after the study. Another important conclusion was that the wearable device was not suitable for AD patients with adverse symptoms.
Night-time wanderings are another common characteristic of Alzheimer’s patients. Radziszewski et al. [ 40 ] devised a system that tries to detect a night-time wandering of patients and tries to return them to their bed. The study included a single participant, a female aged 78 years old. According to her score on the MoCA test, she was an MCI patient. The system consists of 30 ambient smart-home sensors that were installed in her home where she lived alone. Moreover, a smart wristband was used as a wearable and smart home objects such as LED bulbs and lamps were also installed in the home. The first week of the study was used to test the sensors and understand the participant’s routine. The next two weeks were used for the testing phase of the study. In this phase, only the data were collected, but no assistance was provided. However, the caregiver was also involved at this stage for collaboration. K-means algorithm and clustering techniques were used to classify the patients’ day and night activities. Then actuators, speakers for voice messages and calming music apparatus were installed in the home for assistance, and after testing the system for a week, a 15-day validation study period was carried out. At the end of this, MoCA and Dementia Rating Scale (DRS) were performed again. The results indicated that the data collected in the 42-day study were insufficient for determining nocturnal patterns; however, the small clustering of activities gave an overall view to the caregiver for better assistance.
The system developed by Kaur et al. [ 29 ] also assists by generating automatic alarms and message reminders to help Alzheimer patients in memory. It also has cognitive support exercises, and through a GPS, it can guide an AD patient back to a rehabilitation centre.
- (d) Monitoring Functional and Cognitive decline
In an 8-year longitudinal study carried out by Lyon and co-authors. [ 41 ], smart sensors were strategically placed in 480 homes of an elderly population. All the participants were 70 years or older in age and had scores MMSE > 24 and CDR ≤ 0.5 at the beginning of the study. The sensors include passive and wrist-worn sensors such as actigraph acting as ground truth. The sensors were used to monitor the gait, activities performed, mobility patterns, leisure time (computer usage and socializing) and medicine adherence of the residents of the homes. Statistical analysis, logistic regression along other predictive analysis were applied to the multi-domain data. Results showed that using multimodal data collected from sensors, they could identify decline in cognition, loneliness and mood anomaly within a short period. These were identified using the changes in mobility, socializing and activity patterns as observed by the sensors. Some of the symptoms of decline and Alzheimer disease progression were detected within six months. It is also noted that various behaviours such as speed of computer usage and sleep patterns are different for MCI patients as compared to people in the later stage of Alzheimer’s.
3.1.3. Therapy and Rehabilitation
The effective use of assistive technology on the cognition, behaviour and functional challenges experienced by Alzheimer patients was evaluated by Lazarou et al. [ 42 ]. In their study, they recruited 18 patients (12 MCI, 6 AD patients) and divided them into 3 control groups. Each group had 4 MCI patients and 2 AD. The MCI patients were selected on Peterson criteria [ 43 ], and the AD participants were selected according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-V) criteria [ 44 ]. The duration of the study ranged from 4 to 12 months. The interventions used were off-the-shelf IoT devices including wireless tags for in-home objects, Infrared (IR) motion sensors, sleep monitoring sensors, wearable band and ambient depth cameras. Sleep, motion and activity patterns were monitored for the first and second control group. Based on the information generated by these sensors, the first group received automatic, clinical updates, recommendations and alerts for their care and other non-pharmacological purposes. The second group received these automated prompts based on self-reported methods. The third group did not have the system installed in their homes neither did they receive any proposed interventions. All the participants underwent MMSE and various neuropsychological tests before and after the study. The study concluded that the group that was continuously monitored and received all the appropriate automatic, system-generated interventions, and hence, the timely treatment showed significant improvement in cognition by the end of the study. The cognitive and memory abilities of the patients in group 1 remained better intact, even better, as compared to group 2, which was receiving partial on-demand interventions. Moreover, the results of group 2 were better than that of the third group that received no treatment and no automatic monitoring system. Hence, the functional and cognitive decline of the third group progressed as expected in Alzheimer’s disease.
Table 2 provides a summary of all the studies implementing the distributed systems for the diagnosis, assistance and therapy of Alzheimer’s disease.
Distributed systems based solutions for Alzheimer’s disease.
Table Acronyms: AD: Alzheimer’s Disease; MCI: Mild Cognitive Decline; MMSE: Mini-Mental State Exam; CDR: Clinical Dementia Rating; MoCA: Montreal Cognitive Assessment; RBANS: Repeatable Battery for the Assessment of Neuropsychological Status (RBANS); PMRQ: Prospective and Retrospective Memory Slips; GDS: Geriatric Depression Scale; AUROC: Area Under Receiver Operating Characteristic Curve; HC: Healthy Controls; ADL: Activities of Daily Life; IADL: Instrumental Activities of Daily Life.
3.2. Handheld Devices
This section deals with the intelligent sensing technologies that are not spread throughout the care homes, nursing homes or individual’s smart home. These instead are based on interactive devices such as a smartphone or a tablet which takes the user input through touch, video or voice. Robotic interfaces, socially assistive robots and virtual assistants are also part of this category of intelligent sensing technologies. Mobile phones and tablets have software applications running on them that provide adaptive feedback to the user using the touch screens. Out of the 20 studies, 9 were categorized as those whose solutions involved self-contained devices. These devices were further classified into the following groups: smartphones/tablets, interactive robots, applications implemented on smartphones/tablets and smart furniture.
These devices are being used for the diagnosis, therapy and assistance of Alzheimer’s disease. These sensing technologies are playing their part in the diagnosis and detection of various Alzheimer related symptoms such as cognitive and memory decline, tremors and visio-motor coordination skills. For therapy purposes, there exist devices that are working to aid for medicine adherence of the Alzheimer’s patient. Moreover, devices and applications are implemented for cognition and memory exercises. Music therapy for mood-boosting purposes and for strengthening episodic memory is also being carried out. The following subsections provide a classification of the studies based on their outcomes.
3.2.1. Diagnosis of Alzheimer’s Disease
Gonzalez et al. [ 45 ] designed a system that evaluates the memory of an individual. Their system includes a three-door cupboard installed with magnetic switch sensors for each door of the cupboard, a Raspberry Pi and an external battery. The 23 participants involved in the study include adults in the range of 18–60 years old. The young adults were included as a control group for comparison purposes. The attributes assessed in the study were memory and the reaction time of an individual. To validate the memory assessment, a shorter version of the standard test ‘face-name pairs’ [ 46 ] along with a self-reported memory test [ 47 ] were used as an evaluation and validation metric. The algorithm on the Raspberry Pi recorded information of the number of attempts of finding an object in the cupboard versus actually finding the object. An experimenter also independently observed the individuals during the task. The memory measurements from the study were compared with that of the standard tests. Pearson correlation test was performed. A high correlation between the results from the designed system and the memory tests were observed. Moreover, the study results indicate that no correlation exists between the reaction time of older adults versus younger adults.
The study carried out by Suzumura et al. [ 48 ] also tends to diagnose the decline in cognitive function using finger dexterity. They were able to do so using a smart terminal device ‘JustTouch’ which was used to assess the various finger tapping patterns. These tests included rhythmic (left or right hand and then both simultaneously) and sounded rhythmic (using either hand) patterns. The response time was also calculated with precision. The participants in the study consisted of 31 AD patients (mean age 74.2 years) and 15 people diagnosed with MCI (mean age 74.3 years). Healthy controls (HC) (mean age 74.6 years) also participated in the study. MMSE test was carried out for all participants at the start of the study. The statistical analysis using Spearman’s correlation coefficient shows that significant differences exist between the three groups (AD, MCI and HC) in the contact duration, rhythm and response time (lag time). A negative correlation was also indicated between the MMSE and contact duration of the touch screen.
Lee et al. [ 49 ] built a small play apparatus consisting of four different colours Light Emitting Diodes (LEDs), an Arduino board and a small speaker. This system is connected to a smartphone using Bluetooth. The system is capable of diagnosing cognition problems as well as providing treatment for them. The diagnosis is carried out by calculating the reaction rate as a response to the game. The cognition therapy is carried out by providing repeated cognition stimulations and taking care of the hand, vision and hearing coordination. The participants included in the study were healthy control adults in their 20 s and 70 s, and 10 measurements from each patient were taken while the other group consisted of 14 people suffering from cognition problems and MCI patients, and they were tested twice as much as those of the first group. It was noticed that the response rate for cognition of the elderly in their 70 s was 300 ms slower than that of those in their 20 s. However, the response time of the patients with cognitive issues was 9.64 s slower as compared to healthy controls in their 20 s while 5.53 times slower than those in their 70 s. Hence, the device was successful in differentiating the age-related as well as detecting impairment in cognition of the individuals.
Low-cost haptic feedback robotic interface was developed by Bartoli et al. [ 50 ]. The apparatus consists of a computer screen on which a visual target appears and a haptic interface. The apparatus was developed to detect the Visio-motor deficits of Alzheimer patients. The commercially available haptic device, Omni SensAble, was integrated with the Windows XP monitor using customized software. The device helps to draw the hand trajectory while the user tries to follow the visual target on the screen. The study consisted of controlled randomized trials. The control group involved 20 healthy, cognitively sound adults aged between 53–90 years, while the experimental group consisted of 20 AD patients aged 57–82 years of age. The reaction times, position tracking of the object and stability of the position tracking were observed for trials that lasted less than an hour. In addition, MMSE and standard vision tests such as Rey’s Figure copy-REY-Clock Drawing test were performed. Results of the study indicate that there was a marked correlation between cognitive abilities and memory to that of visio-motor performance. The experimental group was significantly slower in response time. Moreover, the Attentive Matrices test and MMSE were negatively correlated with reaction time. The tracking error also increased for the AD patients, and hence, the performance of position tracking was better with the cognitively well group.
3.2.2. Assistance in Everyday Activities
Fardoun et al. [ 51 ] built a prototype system consisting of a smartwatch and mobile that helps Alzheimer patients in recognizing people. They made use of a smartwatch that had a built-in camera and cloud technology. The Alzheimer patient takes the picture of the person in front of him/her using the smartwatch. The picture is then sent to the mobile which is then compared to a pre-existing customized database on the cloud data. A face recognition algorithm recognizes the face and displays the information of the person on the screen of the smartwatch. This aids the Alzheimer’s patient to recognize the person, thus helping in memory rehabilitation. The prototype was tested on 41 people aged 55 to 72 years old that experienced no visual difficulties. Results show that although the system works well in face recognition, the vision of the information displayed on the small smartwatch screen proved to be challenging for the elderly especially those with Alzheimer’s.
Rudzicz et al. [ 52 ] made use of a human interactive robot named ED that could have a conversation and direct patients with cognition problems in their daily tasks. They assessed the feasibility of using such a robot in a nursing home-like setting, interacting with 10 AD patients simultaneously. The robot assisted the AD patients with verbal prompts after visually monitoring. The robot was movable and had a video display screen, speakers and cameras installed on it. Speech recognition was an integral part of the robot used in the study. A total of 10 AD patients along with their caregivers were recruited for the study. Throughout the study, the robot was teleoperated, and when a caregiver was required or intervened, the robot was no longer used for assistance in that particular task or time. It was used while guiding the patients to perform simple tasks that had a specific number of steps involved such as making tea. It also guided them or followed them to the washroom. It was noted that the patients seldom interacted with the robot in two way-conversations. It was better used when engaging in familiar tasks; however, human-human (patient-caregiver) interactions were more used by the patients in interview type conversations. The AD patients ignored the robot prompts over 40% of the behaviours that indicated confusion. However, the automatic speech recognition capability of the robot was assessed to be 70% which was greater than the already existing in the literature.
McGoldrick et al. [ 53 ] evaluated an application ‘MindMate’ that was developed to help and support people with later stages of Alzheimer’s (dementia). It was developed to assist in memory tasks by using reminders. The study was carried out to assess the usability of the application to aid in memory management. Three participants diagnosed with Alzheimer’s (at MCI stage) according to ICD-10 criteria (International Statistical Classification of Diseases and Related Health Problems) and reported to experience memory problems were recruited for the study. Moreover, partners (responsible for taking care of the patients) also participated in the study. Baseline performance was recorded by the carers of the patients for the first phase without using the application for five to seven weeks. Then, a weekly assessment was made for 5 weeks after the intervention was introduced. One of the AD patients withdrew from the study in the first week of the intervention. The patient was irritated with the reminders and the difficulty of turning them off. In addition to observational data analysis, Tau-U (Unified Theory of Acceptance and Use of Technology) [ 54 ] was also carried out. Results showed significant improvement in the memory performance for the two remaining patients.
3.2.3. Therapy and Rehabilitation
Lyu et al. [ 55 ] developed a system consisting of a smart robotic dog along with an adaptive fuzzy logic inference module and cloud technology. A corresponding web application along with a few sensors such as pulse oximeter, electroencephalogram (EEG) and smartwatch was also part of the system. The overall system was used to detect symptoms of pneumonia in AD patients. The robotic dog was used to detect the emotions of the AD patient and respond to them accordingly. When simulated, it played music. For AD patients, music therapy is used to calm their mood and sometimes it is used for their memory rehabilitation. Furthermore, depending on the beat of the music, it can also encourage movements in AD patients [ 56 ]. The smart dog provided the patients with companionship as well as it was designed to lessen the caregiver burden. The system was tested on 18 AD patients diagnosed with middle to late-stage AD and their caregivers aged 25 to 78 years old. Before the usage of the system, various questions regarding time and stress burden were asked from the caregivers through the Caregiver Burden Inventory (CBI) system. The system was tested for 12 weeks day and night. After the test period, the caregivers were again asked questions in the form of a user satisfaction questionnaire and CBI. Results showed that the robotic dog was a great help in managing behaviour, sadness and agitations of the AD patients. This resulted in lessening the physical, emotional, time and social burden of the caregivers to a significant extent. The system also helped in reducing the frequency of night-time wanderings and agitated mood of AD patients. The system was rated in terms of usability (89%), readability (74%), convenience (78%) and accuracy (63%), according to the survey.
Stoekle and Freund [ 57 ] also developed a smart personalized music device for the therapy of AD patients. The prototype was developed using open-source code of Java script and Hypertext Markup Language (HTML) on an Apple iPad 4. It consisted of a simple user interface with few textual features and more visual features. The 40 songs in the music player consisted of classical (10 songs), North American folk (5 songs) and 25 popular songs. The cross-sectional study took place in a care setting for memory loss and the disabled population. The study included the presence of the researcher, caregiver and the 5 selected sample of elderly patients, aged 62–69 years. The patients although not diagnosed with AD were considered a close proxy with AD patients. The data were collected through videos and direct observation. Results from the observational study show that the device can independently be used by the patients, and they enjoyed listening to the songs, and their mood was alleviated. The device was also able to automatically detect user preferences of songs.
Table 3 below provides a summary of all the studies implementing the self-contained device solutions for the diagnosis, assistance and therapy of Alzheimer’s disease.
Self-contained device-based solutions for Alzheimer’s disease.
Table: Acronyms: AD: Alzheimer’s Disease; MCI: Mild Cognitive Decline; MMSE: Mini-Mental State Exam; HC: Healthy Controls.
4. Discussion
With the ever-increasing population of the elderly, the number of Alzheimer patients is also likely to increase. According to a 2019 report, ‘Projections of older people with dementia care in the United Kingdom, 2019–2040′, Wittenberg et al. state that currently 7.2% of people in the United Kingdom (UK) are suffering from dementia. This number is expected to increase exponentially in the years to come. Moreover, the increase in the prevalence rate of dementia is estimated to be 80% by the year 2040 [ 58 ]. This indicates a substantial increase within the next two decades, while in the United States of America (USA), it is estimated that the current number of people that are suffering from Alzheimer’s over the age of 65 years is 5.5 million [ 59 ]. According to the ‘Centre for Disease Control and Prevention, the problem of Alzheimer’s disease and related dementia is to double by the year 2060 in the USA [ 60 ]. These numbers tend to increase in other parts of the world as well. As the average life expectancy increases all over the globe, the prevalence of Alzheimer’s disease patients will tend to increase too. Global statistics state that in 2018, the total number of people with dementia was 50 million. This number is projected to rise to 152 million, which is a 204% percentage increase by the year 2050 [ 61 ].
The high incidence numbers of this vulnerable population are associated with a high cost of care. The complex physiological changes, functional assistance and neuropsychiatric needs of Alzheimer’s patients pose social and financial pressures on society, families and the overall healthcare systems. According to the research study of 2013, by Hurd et al. [ 62 ], Alzheimer’s and related dementia is the costliest disease in western countries. They state that out of all the types of dementia, the most expensive is Alzheimer’s disease. Almost 160 billion dollars were spent annually on these diseases [ 14 , 63 , 64 ]. According to the Alzheimer’s statistics report, these costs in 2018 have risen to 277 billion dollars [ 64 ]. These costs will keep on increasing with the ever-growing disease’s prevalence, as stated above. Such high costs indicate that automated, sustainable and low-cost technological solutions need to be put into practice. The intelligent solutions as identified by the review can help individuals with their everyday tasks yet provide remote up-to-date health status information to the clinicians and caregivers for timely interventions whenever required.
The main objective of this review paper was to see the advancements in recent literature and the proposed solutions that exist for the management of Alzheimer’s disease. These have the potential to assist the clinicians and Alzheimer’s patients, in the selection of appropriate solutions mapping them into their daily practice for Alzheimer’s disease management. The advantage of implementing such systems and devices in the daily life of Alzheimer patients is manifold. Moreover, the current study aimed to identify research gaps and challenges faced to orient the researchers for a better user-centric design for the intended purpose. The research studies reviewed and presented in the results section in this article have been classified according to the sensing technology (Research question 1). The details of how these technologies are playing their role in the care and management of Alzheimer’s disease have also been discussed in the results section (Research question 2). The discussion section presents an overview of these results presented in Section 3 and the associated challenges and limitations, in accordance with the focused research question of this review paper.
The breadth and depth of the reviewed research articles in the current study indicate prospective outcomes of these intelligent sensing technologies for viable solutions for Alzheimer’s disease. The range of solutions and the type of assistance they provide indicates that these intelligent sensing technologies, for the use of intricate diseases such as Alzheimer’s, are still a developing area. However, the widespread use of smart devices and miniature sensing technologies is paving the way for them to be integrated into daily living without being noticed by the users. Moreover, their ability to provide context-aware adaptive responses increases their prospects in being suitable for use in managing Alzheimer’s disease.
These solutions include both the distributed systems as well as the handheld devices and the robots. The distributed systems increase the possibilities of remote health monitoring of AD patients. These systems are suitable for in-home and care-home settings. The idea of intelligent assistive technology is to provide automated context-aware updates that can not only help in the early diagnosis but also monitor the progression of the disease. Moreover, it enables timely therapeutic interventions based on the progression speed of the disease. This helps in less damage as compared to no monitoring or even self-paced decision making as is evident by the study by Lazarou et al. [ 42 ].
4.1. Practical Implications of Using Intelligent Systems and Devices
The following subsection discusses the strengths of these systems with a focus on the sensors used, signals being monitored through the sensors, and how these can play a role in the early diagnosis, daily monitoring and therapy of Alzheimer’s disease patients in the comfort of their homes as well as in care home settings.
4.1.1. Diagnosis of Alzheimer’s Disease
It is observed that in the case of the distributed systems, the diagnosis of Alzheimer’s disease is being done by monitoring the activities and mobility patterns of the subjects of interest. The signals monitored in the studies include walking speed [ 27 , 28 ], changes in mobility, absence from home, visitors, sleep patterns and toilet visits at night-time [ 31 ]. Gait speed was measured using passive infrared sensors installed in the homes of the patients. While absence from home, the presence of visitors and night-time toilet visits were monitored by magnetic door binary switches. In [ 29 , 31 ], RFID tags on active IoT devices carried by the patients such as mobile phones were also used to track the location and motion sensors were used to assess the environment of the user. Making using of Machine Learning algorithms, Bayesian inference and regression models, the studies use these sensor data to correlate these signals with the prevalence of cognitive decline and depression. A decline in cognition and mood changes both are symptoms of Alzheimer’s disease.
In the case of handheld devices, the most common signal monitored is the pattern of finger tapping and measuring response time, reaction time and rhythm [ 45 , 48 , 49 ]. These have been monitored by smartphones and simple home furniture which was made intelligent using magnetic switches and programming an Arduino board. The smart cupboard assessed the decline in memory which is also a common symptom of early-stage Alzheimer’s. Whereas, smart devices such as mobile phones and tablets are equipped with built-in motion and magnetic sensors. According to the study results, the response and reaction time are relatively much slower for those who suffer cognitive problems as compared to healthy controls. Mobile applications that access these sensors and calculate the response time can be of use and easily put into practice in daily lives especially in care-home setting and personal homes. The major advantage of such devices is that the results are quick, and their ubiquitous nature nowadays makes it a lucrative prospect for the early detection of Alzheimer’s disease. Moreover, simple low-cost systems, as described in [ 45 , 50 ], that assess memory and visio-motor coordination of individuals can easily be implemented not only aiding in a quick diagnosis, but also these kinds of systems can help in therapy purposes as well. The repetition of such tasks strengthens their motor and cognitive abilities thus aiding in slowing down the progression of the neuronal and functional damage caused by Alzheimer’s disease.
4.1.2. Monitoring and Assistance of Alzheimer’s Disease Patients
The smart-home sensors, such as magnetic switches attached to doors and cupboards, pressure mats for monitoring the presence of a person in and out of the bed or chair and tags attached to the everyday household objects can give valuable activity and contextual information. This data collected by various ambient home sensors combined with some wearables that monitor the physiological parameters such as heart rate and temperature can be used to assess the erratic mood changes of Alzheimer’s patients [ 36 ]. The monitoring of the mobility and daily activities of the patients can help in assessing the autonomy, abnormal behaviours and functional decline [ 37 , 39 , 41 ] of Alzheimer’s patients. The monitoring of daily activities can also aid in assisting caregivers, alerting them during abnormal activities or risky situations such as falls and night-time wanderings [ 40 ]. The provision of assistance in daily tasks, such as cleaning, cooking etc., such as that in [ 38 ] through automated recorded messages can enhance the confidence of the elderly patients, ensuring autonomy and self-reliance. Moreover, the system introduced in [ 40 ] that assists the patient back to bed through the activation of actuators can help reduce the caregiver burden, allowing the caregiver and family members also take adequate rest.
In the case of self-contained devices, the assistance is provided by sending reminder alerts for tasks and medicine [ 53 ] or using robots that are equipped with various sensors such as cameras, temperature sensors, distance sensors, motion sensors, sensing the environment and using Natural Language Processing to interact with the patients [ 52 ]. There are commercial robots present for the aid of Alzheimer’s patients; one such example is PARO (a seal robot). The robot assesses the mood of the patient and provides her company by responding to the gestures of the patients [ 65 ]. These socially assistive robots prove to be successful mood boosters for Alzheimer’s patients.
4.1.3. Therapy of Alzheimer’s Patients
The system described in [ 42 ], makes use of ambient smart home sensors, such as motion sensors and tags attached to simple everyday household objects as well as wearables to monitor the sleep and mobility patterns of the subjects. The tags were also attached to drug boxes to monitor the subject’s adherence to medicine. The study results indicated that the group which received automated reminders for medicine and regular updates from the clinicians based on their daily activities showed marked improvement in cognition as compared to the groups receiving the self-assessed, on-demand intervention and no intervention at all. This study indicates that continuous monitoring at home and sharing of the sensor data with clinicians can result in timely interventions and avoid drastic neuronal damage. Hence, such systems can practically play a vital role in slowing the progression of Alzheimer’s disease.
In the case of handheld smart devices, [ 55 ] introduced a robotic dog that could monitor mood changes, temperature and heart rate using various sensors. The results of the study indicate that the mood of the patients improves due to the interactive robot, posing less burden on the caregivers. Similar results were evident from a simple music application [ 57 ], intended to boost the mood of Alzheimer’s patients.
4.2. Future Research Directions for Intelligent Systems
The literature indicates the potential of intelligent systems; however, the translation of these systems to clinical practice is hampered by a few limitations. Below are listed a few shortcomings and suggestions for future research to make intelligent systems more effective for the diagnosis, monitoring and therapy for Alzheimer’s disease.
- (a) Maintaining long-term Patient Databases for Distributed Systems
A positive aspect of the distributed systems is that they can continuously or regularly share updates with the clinician. However, to make such solutions effective, database management systems are required as an integral part of the system. These systems should maintain the patient’s history to easily identify any irregular changes in the times to come. The studies that focused on the diagnosis of cognitive decline either have used datasets from the patient databases or have resulted as part of larger projects such as the dem@care and Oregon Center for Aging and Technology (ORCATECH) [ 27 , 28 ]. Moreover, Alberdi et al. [ 31 ] have studied 29 patients over a period of 2 years while the study in [ 41 ] resulted from the patient data of 480 homes collected over a period of 8 years. Hence, these studies indicate that the diagnosis and indication of cognitive decline is a slow process that requires time, and it may vary from patient to patient.
- (b) Multi-person settings in Distributed System Designs
Most of the studies just mentioned for database management and implementing distributed systems have taken place in societies that had smart homes built for individual patients. Although this may be a lucrative solution for people living independently, it is not suitable for homes where more than one person resides. Such examples include the family of the patient living with her or multi-person settings such as care homes. As for those homes with more than one person, the first challenge comes from recognizing the person (person identification). As the simple motion sensors used in most of the studies can only detect motions and not identify by whom the motion was made. Hence, the motion sensors placed in common areas may detect motion through anyone present, thus making the activity profiling of the individual challenging unless indoor tracking is also done.
- (c) Maintaining Privacy of the Individuals
The prospect of continuous monitoring of Alzheimer patients by using simple smart home sensors that are commercially and readily available in the market seems much advantageous. These sensors are being used for the continuous monitoring of the individuals, recognizing the daily activity patterns and then separating these from the changing or risky profiles such as less socializing, less movement and increased visits to the toilets. Moreover, these systems can monitor behavioural changes which is also an important neuropsychiatric symptom of Alzheimer’s disease. This symptom cannot be judged or indicated in short clinical visits. However, these distributed systems use cameras such as in [ 36 , 37 , 38 ] along with other sensors for the intended purpose. The drawback of the usage of cameras is the infringement of privacy.
The solutions need to be designed such that the privacy and citizenship of the patients are guarded. Although cameras can provide a more direct context-aware sensing system these also cause severe privacy infringements. Privacy is not only an issue in the sensing technology; in the case of data storage systems, there is also a potential threat of misuse of the patient data. Huge data storage systems and well maintained electronic medical records, on one hand, are lucrative aspects for the researchers but, on the other, are vulnerable to privacy risks. Hence, there is a need for clear policies for maintaining the data privacy rights of these storage systems. Policymakers and concerned organizations should come together to look into this issue.
- (d) Need of Increase in Systems for Detection of Anomaly in Behaviour
A study in [ 66 ] was conducted by Gary and Mary West Health Institute in collaboration with the Centre to Advance Palliative Care (CAPC) to understand the most challenging behaviours of Alzheimer’ patients. They surveyed over 500 caregivers by forming four in-person focus groups. According to their study, the most challenging behaviours of Alzheimer’s patients is agitation, aggression and changing moods of the patients. This problem amounted to the maximum, contributing 25% among other challenges. This challenge of abnormal behaviour was followed by other problems such as speech decline or repeated speech (12%), wanderings of the patients (10%), inconsistence (10%), late-day confusion (8%), sleeplessness and adherence to medicine (6% and 4%, respectively). Given these statistics of the problems, only behavioural issues account for one-fourth of the remaining problems. Hence, feasible and practical solutions to mitigate this issue should be researched. According to the reviewed studies, only a couple of the studies are detecting mood issues [ 36 , 55 ] while only one study focuses on emotional encouragement through music [ 57 ]. Hence, further research should be carried out giving more attention to incorporate behavioural changes of Alzheimer’s patients.
- (e) Improving Provision of Everyday Assistance
Intelligent sensing technologies are also being used to assist Alzheimer patients by helping them in their everyday tasks. This assistance is being provided by first observing the patients in a context that is, understanding the surroundings of the patient and then guiding them through alerts and messages. Alzheimer’s disease patients have difficulty performing their daily tasks especially in adhering to medicine due to forgetfulness along with dressing difficulties because of disorientation and confusion. Moreover, a very typical symptom and challenge experienced by caregivers is the night-time wanderings of Alzheimer’s patients. Studies have developed systems to aid these problems through soothing music, automated voice messages and video assistants [ 37 , 39 , 40 , 52 ]. However, these solutions also have a few limitations.
- (i) Privacy Concern: The first is that some of the studies are using cameras which raise the privacy concerns of the stakeholders.
- (ii) Minimum User-Centric Approach: It has been observed in the studies themselves, that AD patients feel stressed while responding to automated voice commands. Moreover, in [ 39 ], although the system alerts the caregivers of the risky behaviour of the AD patient, the acceptability and usability rate were 50% and 30% which is quite low. The application used in [ 53 ] as a reminder of medicine also deals with only 3 AD patients of which one left the study due to agitation experienced by the reminders generated by the application.
- (iii) Low Accuracy: The study that assisted the AD patient back to bed during night-time wandering involves only one patient, and the duration of the study was not enough to reach viable conclusions. Hence, a limited number of AD patients in the studies and low accuracy rates are of concern. Moreover, Fardoun et al. [ 51 ] developed the device to aid in-person recognition for the AD patient; however, the screen size of the watch made it difficult for them to read or see the information. Hence, efforts should be made to take these considerations into account to improve the design solutions for assistance.
- (f) Increase in Therapeutic Solutions
As observed in the reviewed literature, the distributed systems and devices are also being implemented for non-pharmacological therapeutic purposes. The handheld devices either use a simple apparatus, mobile applications or virtual assistants that guide the patients in various ways through their therapies. Studies such as [ 50 , 53 ] aid the patient through automatic exercises for visio-motor coordination therapy, cognitive exercises or alerts aiding in memory. The smart robotic dog and the music player [ 55 , 57 ] also provide emotional support through music therapy. However, in the case of distributed systems [ 42 ], the only therapy that is being provided is medication alerts and timely interventions by the clinician or caregiver. This limitation indicates an inadequate number of solutions for the therapy of Alzheimer’s patients.
- (g) Robust Diagnostic using Handheld Devices
In the case of handheld devices, the studies [ 48 , 49 ] try to assess the cognition decline through finger tapings using a mobile screen and a simple play apparatus attached to the mobile. The diagnosis of other symptoms of functional decline related to the disease progression has been done only using self-contained devices. These diagnostic symptoms include the decline of memory [ 45 ], and visio-motor coordination [ 50 ]. These methods are quick, and the results confirm their accuracy. Although these devices have their strengths in a quick decision, a limitation mentioned by [ 50 ] is that the user can learn the patterns of visio-motor games if played again and again. This limitation can be addressed if the cognitive exercises are designed based on randomized patterns. This will make the exercise a little challenging yet useful.
- (h) Involvement of Clinicians in Solution Designs
Another important observation that was seen is that clinicians were minimally involved in the development and design of the solutions for Alzheimer’s disease. Most of the studies involve caregivers as stakeholders for their perspectives while designing the distributed systems, applications and handheld devices. Progression is a slow process, and to truly translate the technological solutions into long-term healthcare practice, the clinicians also need to be involved in the design and development phase of these technological solutions. Such a limitation implies that the proposed solutions cannot be confidently implemented by caregivers or clinicians for the management of Alzheimer’s disease. However, this constraint also indicates the challenge faced by the researchers proposing solutions for such an intricate disease. The direct involvement of the vulnerable population requires great care and precautions for many reasons. The prime reasons being the old age, easily agitated moods and frailty of such individuals. Furthermore, the widely varying symptoms between various individuals and the range of age of the patients also pose further challenges for user-centred designs. Hence, there is a need for the combined efforts where the researchers, clinicians, formal and informal caregivers can collaborate to come up with solutions that are effective and safe resulting in the user-centric design in true spirit.
5. Conclusions
The current study presents an overview of the intelligent technologies designed and developed for Alzheimer’s disease management, mentioned in the recent literature from 2015 to 2020. Alzheimer’s is an incurable, progressive neurodegenerative disease, which with time results in serious dysfunction of the individual suffering from it. Intelligent sensing technologies have the potential to provide low cost, sustainable clinical and home-based solutions as compared to the existing expensive and dedicated lab-oriented solutions. These can help in prolonging the stay of the patients at home and reducing hospitalizations. The continuous monitoring of the patients and regular updates being sent to the clinicians can result in timely therapeutic interventions. This can potentially aid in reducing the extensive healthcare costs spent every year on the management and care of Alzheimer’s disease. Moreover, with the existing challenge of the pandemic, these intelligent solutions become all the more necessary. Now that Alzheimer’s patients are forced to stay at home for their safety, interventions of smart technology can provide a viable solution. These technologies can help in avoiding visits to clinics and hospitals for regular check-ups and follow-ups, minimizing the risk of exposing the vulnerable elderly to other disease risks such as COVID-19. Automated solutions integrated into the daily lives of Alzheimer’s disease patients cannot only help in assisting the individuals but also reduce the stress and burden of the formal and informal caregivers. These solutions if effectively implemented can help improve the quality of life of the patients and their caregivers. Hence, awareness is to be increased among the societies and people who are directly involved in the care of Alzheimer’s patients. They need to be made aware that how these intelligent, context-aware, ubiquitous and low-cost technological solutions can help in prolonging the life of their loved one by making it easy, safe and independent. However, the practical implementation of these intelligent technological solutions is hampered by a few limitations and challenges as discussed in the discussion section above. Hence, this review article not only highlights the practical role of intelligent sensing technologies for Alzheimer’s patients but also suggests future improvements for further research in this area.
Author Contributions
Conceptualization: N.G.; Methodology: N.G. and T.A.; Formal Analysis: N.G.; Investigation: N.G. and T.A.; Resources: N.G.; Writing and Original Draft: N.G.; Review and Editing: N.G.; Supervision: T.A. All authors have read and agreed to the published version of the manuscript.
This research received no external funding.
Institutional Review Board Statement
Informed consent statement, data availability statement, conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

IMAGES
COMMENTS
Help prevent dangerous Alzheimer's wandering events with monitors, indoor motion sensors, door alarms, bed sensors & more. We carry a full line of dementia monitoring solutions that stop wandering at the source and also provide GPS Tracking Watches and Location Devices in case a loved-one leaves the house unexpectedly.
The Alzheimer's Association suggests 60% of people with dementia will experience wandering at least once. Some may do it repeatedly. It notes that wandering can occur at any stage of dementia ...
A wandering alarm for dementia patients on a door significantly reduces the risk of a patient leaving a building and becoming endangered when disoriented or lost. With one part of a magnetic door alarm attached to the door frame and the other attached to the door. When the connection between the two parts is broken, an alarm will sound ...
Contact the Alzheimer's Association 24/7 Helpline (800.272.3900) for more information. Ask neighbors, friends and family to call if they see the person wandering, lost or dressed inappropriately. Keep a recent, close-up photo of the person on hand to give to police, should the need arise. Know the person's neighborhood.
Wander Prevention Alarm Monitor and Pressure Sensing Floor Mat: This is a wander prevention system that comes with a sensor pad monitor and a pull-string monitor. When the magnetic pull-string is pulled free of the monitor or when pressure is added to the floor mat, an alarm noise will sound to alert the caregiver.
More than 60% of the 47.5 million dementia patients wander. Wandering is also a concern for people with autism and other conditions. If not detected quickly, wandering can result in tragic incidents. ... The world's first wearable sensor that alerts wandering on your mobile device, SafeWander™ gives you peace of mind.
Introduction to Dementia Wandering Devices. In the context of dementia, a progressive neurological disorder affecting millions worldwide, dementia wandering devices have become pivotal tools. This disorder impairs cognitive function, memory, and decision-making abilities, thus presenting considerable challenges for both those living with the condition and their caregivers.
Wandering and becoming lost is common among people with Alzheimer's disease or other disorders causing dementia. This behavior can happen in the early stages of dementia — even if the person has never wandered in the past. Understand wandering If a person with dementia is returning from regular walks or drives later than usual or […]
It tends to occur in moderate to advanced stages of Alzheimer's disease. According to the Alzheimer's Association, 60% of people living with the disease will wander at least once. Most ...
a. address wander-management strategies in the home or supportive care environments for persons with dementia or cognitive decline regardless of whether it was embedded in an environment, was worn, or was implemented as a form of therapy. b. address critical or noncritical wandering in older adults with dementia. c.
Keywords: dementia, wandering behavior, turning, cognitive impairment, body-worn inertial sensor Introduction People with Alzheimer's disease (AD) and AD-related dementias (ADRD) can experience impaired spatial awareness and navigation ability, which is thought to lead to wandering behavior ( 1 - 4 ).
Protect individuals from elopement and wandering: Whether people with dementia intentionally attempt lopement or are simply wandering around to locate a door, those at risk for exiting without the needed supervision may benefit from a door alarm on the exterior doors. Alerts others for assistance: Door alarms can also be used on the bathroom door.
Wandering and dementia: A guide for caregivers 3 Wandering Wandering refers to a variety of behaviours that may result in a person living with dementia becoming lost. Wandering is a direct result of physical changes in the brain and: • Is a common behaviour associated with dementia. • May occur at any time of the day or night.
Wandering is a common behavioral disorder that imposes hazards to older adults, particularly with dementia. Wandering means aimless ambulation in a living facility and is one of the most common symptoms of dementia. ... UWB-IR sensor in eNightLog was used for detecting small vibrations such as breathing, which was also exploited for supporting ...
The AlzStore offers remote alarms & other solutions for Alzheimer's wandering prevention. Use the motion detector in one room and wireless monitor in the other. ... Home > SHOP > Wandering with Dementia > Motion Detector With Remote ... This item has been replaced with our NEW motion sensor alarms found HERE. Price: $ 79.95. Availability ...
Best Dementia Bed Pressure Mat. Winner: Nutrix Wireless Care Alarm Kit with Large Bed Leaving Sensor Mat. Why We Love It... Lets carers know immediately if a patient leaves or falls out of bed. Design fits under patients back and can be used in nearly any bed. Receiver is wireless with wristband so a carer can always carry it with them.
Even people in the earliest stages of dementia can be prone to wandering. Someone with dementia is easily disoriented, and crowded or unfamiliar settings can cause confusion and a strong desire to get away. ... Consider motion-sensor lights. Wandering Zone Consider providing a safe location for your loved one to wander, like a fenced-in yard ...
Staff Education and Training. Expertly trained staff is crucial in managing wandering behavior in seniors with dementia. Memory care communities prioritize ongoing education and skill development, ensuring staff members: Understand the possible triggers for wandering. Recognize signs of agitation or anxiety that may precede wandering behavior.
It comprises a 3D time-of-flight near-infrared sensor and an ultra-wideband sensor for detecting human presence and to determine postures without a video camera. A threshold-based algorithm was developed to classify different activities, such as leaving the bed. ... especially elderly people with dementia and wandering behaviour. In care homes ...
The Alerta Patch offers a unique solution for Alzheimer's and dementia wandering prevention. A wearable sensor applies to the skin on the person's upper back for one month. The sensor pairs to a "Wedge," which looks like a remote control. An alarm goes off if the sensor travels farther than 65 to 95 feet away from the Wedge.
Dementia and the risk of taking antipsychotic drugs. The researchers reported that antipsychotic drug use was associated with increased risks for all outcomes, except ventricular arrhythmia ...
Keywords included MESH terms and phrases synonymous with "dementia", "sensor", "patient", "monitoring", "behavior", and "therapy". Studies applying both cross sectional and prospective designs, either as randomized controlled trials, cohort studies, and case-control studies were included. ... Nighttime wandering in ...
That's exactly what Dennis Gerard, 60, is facing with his rescue dog Piper, who turned 17 years old last year. The senior dog is now blind, deaf, and suffers from dementia. Gerard told Newsweek ...
1. Introduction. Globally, neurological diseases (ND) are the primary cause of disability-adjusted life years (DALYs) [].Of these, stroke and Alzheimer's along with other types of dementia are the two leading causes of DALYs [].Moreover, neurological diseases are the second leading cause of death all over the world [].People suffering from neurodegeneration undergo neuronal structure and ...