
TRAVELING WITH MS:
The Ultimate Guide
ActiveMSers has prepared an exhaustive guide for traveling with a disability, with a focus on multiple sclerosis. This practical advice has been collected from fellow MSers, travel agents, airline staff, cruise lines, disability specialists, and personal experience. There are many aspects to consider when traveling with a disability, from the earliest of planning stages to packing advice to medication tips and tricks. Whether you are jetting off to explore the Himalayan Kingdom of Bhutan or driving out of town for a quick overnight at a nearby bed and breakfast, here’s how to manage all of it.

As one of the most seasoned MS travelers on the planet —having explored over 50 countries on six continents—I have learned the ins and outs of touring the globe while coping with myriad challenges. Walking difficulties. Fatigue. Bathroom challenges. Wheelchair impediments (sooo many impediments). Even full-on relapses. Alas, the days when I could just touch a spot on the map and then go vanished after my 2006 diagnosis of multiple sclerosis. Navigating the globe when you are juggling a disease, chronic illness, or permanent disability is the very definition of touch and go. But damn, if I don’t still go. I seriously get around. You can, too. This guide will show you how
As an Amazon Associate I earn from qualifying purchases. These funds help maintain this website. Details .
EXPLORE THIS GUIDE:
Best Advice for Disabled Explorers
MS-Specific Considerations When Traveling
General Medication Advice
Favorite Accessible Destinations
Planning Your Accessible Trip
Disability Hotel Room Recommendations
Before You Go
What to Pack
Flying with a Disability
At Your Destination
BEST ADVICE FOR DISABLED EXPLORERS
If you read only one section of this guide, read this one.
Ditch the checklists. See what you can see and do not fret for a moment if you can't see it all. I know, the guidebook says you CAN’T MISS something or other. Whatever. Prioritize a few special things and let the rest unfold as it unfolds. Over planning only sets you up for disappointment later.
Pace yourself. You know your body better than anyone. If you know going all-out is going to put the hurt on your body, save that climb of Kilimanjaro for the end of your holiday and recover on that plane ride. And remember, you don't have to do everything in the guidebooks for your holiday to be called a success. Choose activities wisely and build in recovery time.
Check the ego. You have lots of tools at your disposal to make traveling easier—use them. Wheelchairs, canes, trekking poles, scooters, rollaters, disposable undergarments, you name it. Is someone staring? Who bloody cares. And please, ask for help if you need it. People are amazingly accommodating if asked nicely with a smile.
Don’t panic. There will always be hiccups when you travel some little, some bigger. It happens. And I’ve been through so many messes: missed connections, lost baggage, shuttered hotels, no-show guides, entire legs of vacations cancelled due to unrest, unexpected MS relapses, the works. Catch your breath, count your lucky stars you are in one piece, and set about to fix the situation. Don’t let it fester! Yeah, it sucks. But it won’t ruin your trip unless you let it.
Seek a travel partner. Do not underestimate the importance of a reliable travel companion or caregiver. When you need a little extra assistance, an extra pair of able-bodied hands (and legs) can be a godsend. Treat them well. After all, this is supposed to be their vacation as well!
Eye restrooms. Mentally note all bathrooms and, when traveling internationally, avoid passing up a good one. There are cell phone apps that help you find public potties, but watch data fees overseas. And if you do, remember where it is so you can hustle back to it when nature calls. She always tends to ring at the most inopportune times!
Don't wait. Don't save that dream trip until you retire. Or until the kids are grown. Or until you feel better. MS is unpredictable; go now.
Carpe diem. Seize the day, savor moments, and make your vacation unforgettable for all the right reasons. Focus on the instances that make travel enjoyable, not on your disease.

MS-SPECIFIC CONSIDERATIONS WHEN TRAVELING
Becoming an MS globetrotter requires a few extra steps in order to successfully navigate planet earth with a disease. This advice may apply to other chronic illnesses, but since I don’t have an ostomy bag or wear a blood glucose monitor, I can’t speak to those.
A doctor’s note. A letter from your doctor stating you have multiple sclerosis is a good idea. I read about a woman denied an extra drink on a flight because she looked drunk. She claimed she had MS. Now a doctor’s letter might not have helped in that particular situation because you can still be drunk and have MS, but I digress.
Contact info. Keep with you your MS specialist’s phone number, e-mail, and off-hours emergency number. If you are traveling out of the country, don’t forget to add on the country code when you dial.
Original bottles. It's probably wise that you don’t take your medication out of their original labeled containers when it comes to cryptic pills (disease-modifying injectable MS meds are okay since they are labeled). The dudes, especially in customs, don’t really like to guess what pills are what.
Infusions. Taking an infused MS treatment, like Tysabri, Lemtrada or Ocrevus? Be sure to plan around your infusion dates. Katmandu likely does not have an infusion center you can use. Same goes for Mavenclad, the oral medication that is given in infrequent cycles.
Pills. On an oral drug like Gilenya, Mayzent, Aubagio, or Tecfidera? Avoid extreme temps. In other words, don't leave them roasting in the glovebox of a hot car or exposed when you are camping overnight in Siberia in January. And if you are camping in Siberia in January, I recommend you see a therapist.
Injections. Taking an injectable like Copaxone, Rebif, Betaseron, Extavia or Avonex? A small, soft-sided cooler (with an ice park or two, but watch that you don't accidentally freeze your meds) works great to tote your medication and can be stored in a carry-on backpack. Taking a cooler is always a good idea when traveling with your injectables even if they don’t require refrigeration because you never know when your drugs will be sitting in a hot car while you are out on a hike.
Xray scanners. The Xray machines used at airports should not harm your medications. And TSA generally does not care about your sharp needles. I personally have never been stopped at security for having a boatload of potentially subcutaneous weapons, but I’ve been pulled aside for an eyeglass screwdriver that was immediately confiscated with appropriate scolding.
Prednisone. Before I transitioned to secondary progressive MS, I traveled with a 3-day oral course of high-dose steroids to treat surprise relapses. You may want to ask your neurologist for an advance prescription as a stop-gap measure to save a vacation, particularly if you are traveling outside your country to remote areas. That way, if you have an exacerbation on a long trekking trip, say in Nepal, a dose of oral steroids could trim your attack symptoms big time and save your vacation. NOTE: Only do this if you have previously taken oral steroids and are aware of how the drug affects you.
Pseudoexacerbations. Remember that there is a difference between an exacerbation and a pseudoexacerbation. According to the NMSS website, a true exacerbation “is a worsening of old symptoms or the appearance of new ones that last at least 24 hours. This is important because stress, heat, and/or fatigue (all of which easily happen while traveling) could cause a temporary symptom flare, which should clear by the next day.”
Exercise. Don’t forget to stretch regularly and exercise. I know it’s your holiday, but your health doesn’t take a holiday. MS researchers have found that regular exercise reduces fatigue, so even on vacation I try to squeeze in workouts, especially if I feel that icky fatigue fog start to roll in.

GENERAL MEDICATION ADVICE
There are some notable steps to take when traveling with medications, steps that tend to be overlooked by novice travelers.
Carry on only. Always keep your medications with you as part of your carry on luggage. That’s one piece of luggage you can’t afford to lose.
Refrigeration. Meds require refrigeration? Call ahead to your hotel and ask that a portable refrigerator be put in your room if it does not have a mini bar. Most hotels will be able to honor that request. Note: when removing items from your minibar to make room for meds, be sure to later check your bill. Some minibars have the ability to automatically charge your bill for items removed from the fridge, even if you put them back.
Temperature check. If you need to keep meds chilled, consider bringing a digital thermometer that records the ambient air temperature. Do NOT store your medication in the fridge unless you are certain they won’t freeze, 36 degrees or above. One trick if you don’t have a thermometer: a bottle with just a touch of water (a tablespoon) will do nicely. Put it in the coldest part of the fridge BEFORE you add your meds. Wait at least a few hours. If it freezes, even on the warmest setting, find a new fridge.
Needles. Instead of lugging around a big sharps container for your needles, you might consider a needle clipper / storage device like the BD Safe Clip , allowing you to store the syringe safely. A word of caution, medical waste usually can't be tossed in the trash, so you'll need to find a place to store the empties. At least you won't get poked.
Extras. Bring a few extra doses just in case you do something stupid and pooch one of your injections or drop a pill down a gutter. And if the weather causes delays or cancellations, you won’t be stuck without your medication.
Cannabis. Medical marijuana in any form can get you into deep do-do, especially if jetting about internationally. Even driving across state lines can be cause for concern. That said, domestic travel in America with cannabis, even flying, is unlikely to land you in serious hot water unless you do something stupid. So don’t be stupid.
A final warning. A friend had her baggage confiscated twice--coming and going--because her drugs were packed with her checked luggage. Of course, it didn't help matters that we had a transfer in Singapore, noted for hanging folks with too much Tylenol (actually kilos of heroin, but you get the picture). Her bags were delayed for a couple of days, but fortunately her stash of pills was preventative in nature and not critical.

FAVORITE ACCESSIBLE DESTINATIONS
Having been to thousands of cities and towns around the globe, I can say from personal experience that virtually every place I’ve ever visited can be experienced—at least to some extent—with a disability, including if you use a wheelchair. And even if there are major accessibility issues, there are almost always workarounds if you have assistance and patience. That said, “doable” doesn’t necessarily mean “enjoyable.” Here are a few destination ideas that are more reliable than most.
National parks. In the U.S., the National Park Service generally does an adequate job in accessibility. Each park’s website details ease of disability access and many have full and extremely detailed guides. Yellowstone is a standout with detailed trail guides (hills to steep for wheelchairs, steps on the trail, etc.) and their guide even identifies every wheelchair-accessible bathroom and vault toilet.
Major amusement parks and tourist attractions. While many of the rides may be off limits, they cater to so many people from so many walks of life and generations, that accessibility is standard. Scooters and wheelchairs are almost always available to borrow or rent at major tourist attractions.
Olympic cities. Cities that host the Olympic games also host the Paralympics, and that means accessibility. Cities are required to meet certain benchmarks to aid handicapped travelers, from wheelchair users to the visually impaired. Host cities like Barcelona, London, Tokyo, Vancouver, and Athens have all been improved—from sidewalks to public transportation—to accommodate disabled visitors and are noted for their accessibility.
A cruise. Consider a cruise, even if you are not a "cruiser." I've traveled by ship extensively pre and post MS, and it has a host of advantages. You unpack once (great for fatigue), disability access is good (especially if you need mobility aids), a doctor is always onboard (helpful if you have a relapse), and your travel time is often at night when you are sleeping (no exhausting car rides). See my detailed cruise guide here .
African safari. Want a far-flung adventure? An African safari is a good option for those with limited mobility because you travel by vehicle, which means access to A/C and that you are seated. The lodges can be spectacular (in Kenya I actually slept in a bed that was 11x9, the size of a bedroom!) and the staff will cater to your special needs. Wheelchair-accessible safaris are an option in some countries.
Ziplining, Water Skiing, Ballooning, Sailing, Riding Camels. For virtually every passion out there, there is an accessible solution. There are many outfitters, far too many to list here, who are specially geared to aid wheelchair adventurers and those with other disabilities. In the Grand Tetons I managed to tack on an afternoon of unbelievable handcycling with Teton Adaptive Sports .

PLANNING YOUR ACCESSIBLE TRIP
So you are going on vacation!? Woohoo! There are so many things to consider before traveling that you might need a vacation from planning your vacation. Here are some things to think about as you gear up to go on your next adventure.
Budget. I’ve got all sorts of rules when it comes to spending money on travel, and then inevitably I break them. In general, I prefer to spend money on experiences rather than things, so I give myself flexibility to splurge on trips. Over the years I’ve rarely regretted spending the extra cash for something special, even though at the time I’ll often think to myself WHAT THE HELL AM I DOING. But I’ll never forget watching Ronaldo score a hat trick from a sky box in Madrid instead of watching a tired touristy flamenco show that was the original (and far more affordable) plan.
Length. Listen to your body, it’s the ultimate arbiter. If three weeks sounds exhausting, don’t suck it up—shoot for a shorter trip. I’ve discovered that these days my sweet spot with MS is 10-14 days. Long enough to get into vacation mode, but not so long that I’m ready to go home. Plus it doesn’t exhaust my caregiver. And of course I love short weekend adventures.
When to go. The time of year you travel absolutely makes a difference. I prefer to travel in the off season (less standing in line, easier to get into restaurants, better seats at special events) and when temperatures are cooler (heat and MS go together like cereal and gravy). If heat wears you out, traveling when it's toasty could turn a vacation into little more than a quest for A/C.
Travel agents. Consider using a travel agent who specializes in making arrangements for those with disabilities, especially for those big trips. This is particularly useful if you require a wheelchair and often doesn’t cost extra—you may even save. Be sure to inform your agent about your special needs: your current mobility, equipment you will be bringing (or need at your destination), seating preferences, etc. Here is a detailed list of travel agents around the US and around the world who are experienced in working with handicapped folks. For Europe, Sage Traveling has gobs of trips in dozens of cities that are wheelchair accessible. Travel agents specializing in MS include Tarita Davenock with Travel for All and Sylvia Longmire from Spin the Globe .
Insurance. If the trip is $$$ and the loss of those funds would be detrimental, consider purchasing travel insurance when you book your trip (we like Travel Guard ). Most travel insurance companies WILL recognize pre-existing conditions like MS, but only if you purchase the insurance within 10-15 days of putting down a deposit on the trip. If you miss that window, any MS event will void out your travel insurance and you are on your own.
Doh, insurance! Now if you meant to buy travel insurance and spaced it (I can be such a dolt!), there are plans from Travel Insured International that you can purchase up 30 days after your initial deposit. Remember, "initial deposit" includes any funds to the trip down to the penny. And a word of warning: if you buy your insurance from the same company you are traveling with and they go belly up, you are SOL. So I always recommend buying your insurance from a third party and NOT through your travel agent/company or cruise ship.

DISABILITY HOTEL ROOM RECOMMENDATIONS
Extra care needs to be taken when booking a hotel room if you have a disability, particularly if you have a disability that impairs walking or if you use a wheelchair. Expect issues, even with major hotel chains. When I have the time, I plan to have a heart-to-heart with all the major players. And maybe some public spats if that’s what it takes for them to be more cognizant of disability issues.
Trust and verify. View your accommodations online before you make reservations. Note stairs, pool access, restrooms, exercise room, etc. Have questions? E-mail or call. You don't want to be stuck going up stairs at a B&B when you thought it was a single level. Also, don't trust "handicap accessible" declarations. What some folks think is accessible is downright laughable. The best solution if you have severe mobility issues: ask for pics and even video.
Trust only so much. Even then you can't trust areas to be accessible. In Peru, I cannot count the number of bathrooms that were "wheelchair accessible" that, despite appearances—oversized with grab bars galore—required getting out of the chair before you were anywhere near the toilet. Stall doors often would not close if you brought in the wheelchair. On another occasion, the bathroom door when open blocked the toilet! If I was 100% restricted to my wheelchair, the only way to access the “accessible” bathroom would be to remove the door.
Accessibility if you need it. A room with an accessible bathroom isn't just for folks who use wheelchairs. As one fellow member of ActiveMSers discovered, having a bathroom with grab bars was essential after an exhausting day. But if you don’t need the extra assistance, save the room for someone who needs it more.
Shower chairs. Some hotels will have shower chairs available if the shower is not already equipped with one, but again its smart to ask in advance or bring your own . And even that might not always help. Our lodge in the Grand Tetons only had a tub/shower combo for wheelchair users. That combo can only work if you have a transfer shower bench . They said they had one. No, they just had a standard shower chair. That wobbled. If the chair is too unstable, request another one. And if one isn’t available? Sponge bath it is!
Get creative. If you travel it is bound to happen: something won’t go right, and that includes your base lodging. The bed might be too high… so ask staff to remove the box spring or request a rollaway. The room might be next to the ice maker that makes ice only between the hours of 2-4 a.m…. so ask to switch rooms or use those earplugs.
Measure. Sinks may or may not allow you to roll under them, so if you are wheeling it, ask. And doorways and/or bathrooms (heck, even bedrooms) may not be wide enough for your chair, especially if you are traveling overseas, so have a tape measurement of your minimum requirements needed.
A forewarning. If you get an accessible room, a forewarning: it’s likely going to be bigger… and subpar. Oh, it’ll have much of the same amenities as the other rooms in the hotel, but almost certainly the view will be worse, the location will be worse, the noise disturbances will be greater, and there is nothing much you can do. Except complain. Remind management about the ADA. And demand an upgrade or a discount.

BEFORE YOU GO
As your departure date approaches, you’ll want to start doing your due diligence in the trip-planning department. The earlier the better to keep stress levels at a low burble.
Create a packing checklist. I have my own that I’ve used for decades, updating it for every trip. I’m constantly tweaking it depending on the type of adventure (so I don’t forget a bike helmet if I plan to bike) and the level of disability (I no longer list a cane because I use a wheelchair). There are plenty of list templates online that you can build off. Remember to add your meds and disability aids.
Generate a prior-to-departure checklist. I tack this on to my packing list, and it reminds me about all the little things that tend to get overlooked. Reminders to make a plan to water plants, stop the mail and newspaper, inform the neighbors, set the DVR for that show I don’t want to miss, take down the hummingbird feeder so they don’t get pissed off drinking air, stuff like that.
Research online guidebooks. Sure, you can use Tripadvisor. But before you do, research your own city on that website. Not helpful. Instead I steer to the recommendation of expert travel guides. Frommer’s , Fodor’s , Moon , and Lonely Planet . For short adventures, I’ll cut and paste advice. For longer ones, the $15 is a pittance compared to what my trip costs.
Dig deeper. I’ll often turn to newspaper and magazine articles about the destination I am visiting for even more guidance. My favorites include Conde Nast Traveler , Travel + Leisure , and The New York Times 36 Hours travel series.
Get specific. For a trip to Yellowstone, I researched specifically for wheelchair advice in the national park. I skimmed a handful of blogs and cherry picked their best recommendations. I might have skipped an out-of-the-way accessible trail that wasn’t trumped in any of the mainstream guides, but one wheelchair reviewer said it was a must see. He was right.
Download maps. If you are traveling internationally or to areas with sketchy cell service (hello Death Valley!), this is especially helpful. Maps are useless if your phone can’t access them, and overseas they can chew up gobs of data if you try to load them. While Google Maps is the standard, I especially like HERE WeGo (apps for Apple and Google Play ). Their maps show stairs in the pedestrian mode, so if you use a wheelchair you can avoid sidewalks with stairs, which I discovered are surprisingly common in Chicago.
Download apps. Can you say multiple sclerosis in 35 languages? If you are traveling to a country where you don't speak the language, then download onto your phone the free Accessible Travel Phrase Book PDF by Lonely Planet . Asking for an accessible bathroom, an elevator, and countless other essentials when you have a disability just got way easier. There are many other accessibility apps, including those that help you find bathrooms, that could be a boon in your travels.

WHAT TO PACK
I have a detailed “trek checklist” that I have used for decades, expanding (and deleting) items as my level of disability has progressed. Before each trip, I print it out and cross off items after I round them up. I recommend you create one for yourself.
Handicap placard. Have a handicap placard? Bring it! Even if you never plan to drive. With proof of a disability, many entrance fees are waived for you and your caregiver, especially outside the US. If your country offers a disability identification card, don’t leave it at home.
Walking aids. Ideally, bring multiple forms of walking aids. Why? If you lose your cane, you still have your trekking poles and vice versa. Also, if you primarily use a rollator/walker, bring a cane or forearm crutches! I heard from one MSer who had so much trouble with cobblestone streets in Italy that her rollator was essentially useless. The cane, although it meant slower going, saved her vacation. A pair of forearm crutches offers three times the support of a single cane and can make getting around on uneven surfaces a cakewalk. Incidentally, I don't like the cane/seat combo (oh, but it sounds so convenient): it's a crummy cane and a crummy seat. Get your pants a little dirty and sit on a curb if you must.
Gait belt. I travel with one now (I own this one ), and it should have been in my arsenal a long time ago. Basically, a gait belt secures around your waist and makes for a great handhold for a caregiver or crew member to grab and assist you. It can be used for transfers (say bed to wheelchair), help you stand after a fall, or save your bacon in a dicey situation, like getting off a tender on a cruise. I don’t wear it around, but it’s nice to know it’s available if needed.
Cooling vests and wraps. Since usable freezers while on the go can be hard to find, my preferred all-around travel vests are those phase change vests that recharge in ice or at room temperature. The easiest cooling vest to pack is one that is evaporative, since it is lightweight uncharged, but they perform poorly in humid conditions. Refer to ActiveMSers’ cooling vest guide for more. Another convenient cooling companion is a lightweight wrap that you dampen, like those from WrapMeCool .
Carry-on luggage. Smart packing advice taken from veteran travelers: when flying, make whatever you bring fit into a single carry-on bag, especially if you are going to be traveling to multiple destinations. Yes, this includes if you are going overseas for three weeks. You'll never lose a bag, it's far easier to handle than larger luggage, substantially lighter, and you can pawn it off on a travel companion if need be! This one from Briggs & Riley checks all the boxes and comes with a lifetime warranty.
Or a large wheelie bag. I know, I just recommended small. But as my disability has progressed, I’ve gravitated to one large shared bag (we use this one , it is pricey but dynamite). The larger bag is always checked, easily hold all of my aids, and is convenient on driving trips. Laura rolls this while I roll my wheelchair. If need be, she puts it on my lap, and I become the luggage cart. If we add on luggage, it is usually a carry-on and a backpack, which can also carry loose wheelchair parts when flying.
Sun protection. This sounds like a no brainer, but with heat being an issue for MSers, every cooling trick helps. I like a wide-brimmed floppy sun hat. I’ve tried sun-protective clothing ( Solumbra is highly recommended, but it’s still warmer than I’d like, so I tend to use sunscreen liberally. Finally, a UV umbrella makes a difference, and our testing confirms they really do keep temps cooler under their canopy. Amazon has many options, and this lightweight version would be ideal for travel. Umbrellas also have an added benefit. You know, for keeping you dry in a rainstorm.
Lighten up. I like a tiny, lightweight digital camera or cell phone (keep a smartphone in airplane mode if abroad to avoid outrageous bills; FaceTime and WiFi can still be used) to record my travel memories: photographs, audio and video. The weight savings and convenience of just slipping it in your pocket is invaluable. Of course an SLR is great, but not so great to lug.
Portable grab bars. In the past when stability aids weren’t mandatory but merely helpful, I’ve used portable suction cup grab bars (I recommend this one ) . These are a boon when staying in a standard room or bed and breakfasts when you need a little extra help getting in and out of the shower.
Rolling considerations. If you need a wheelchair when traveling, a foldable manual chair, especially one with removable wheels, offers the most flexibility. Rigid chairs usually work fine, but not in all situations. Scooters and electric wheelchairs may limit you in ground transportation options, but if you use these devices you already know that drill. Renting a wheelchair is an option in some countries (e.g., most pharmacies in France rent them), but I’d only rely on that in a pinch. Renting scooters is also an option. You can have them delivered directly to your hotel. I’ve tested and reviewed the best travel mobility scooters .
Bedside commode. For road trips, this can be an unexpected boon. Bathroom out of service? Lines too long? Rest stop closed? Restroom not wheelchair accessible? If you *need* a bathroom and can’t do the squat pot, having one of these in the car for emergencies is a nice security blanket. Plus you could use it as a shower chair. Ideally find a spot out of the way (duh) and for bonus privacy, you could always drape a sheet or pop an umbrella.

FLYING WITH A DISABILITY
One of the most stressful aspects of traveling with a handicap can be the simple act of flying. For many of us, taking to the air used to be so carefree, but now hazards are everywhere. Here’s some advice to help you breathe easier.
Preboard. Take advantage of early boarding and ask a flight attendant for help if you need it. If you are unable to walk, you’ll want to request an aisle chair. Note: airlines have various rules. Southwest lets you board early and gives you extra time, while other airlines may have you go on after first class and business. And then others might actually have you board dead last, because, you know, they are assholes.
Walking aids. Canes are allowed aboard airplanes, trekking poles are as well (tell anyone who asks that they are mobility aids), ski poles are almost always frowned upon. Forearm crutches are no problem, but a flight attendant may have to store them in another area on the plane if they don’t fit in your overhead bin. If that happens, you’ll need to ask for them back for restroom visits or be relegated to seat surfing. Note: Picked up a cool sword-cane in Kenya? If you can't fit it into your checked luggage, I guarantee you it will be confiscated, walking aid or not. And then all you'll have is a cool sword-cane story of woe.
TSA advice. “One thing you have to watch is that the TSA loves to search bags that are carrying cooling vests/hats/scarves that have hydration beads. Avoid someone pawing through your luggage. Take them in your carry on and inform the screener.” — Mary, Washington
More TSA advice. A United Airlines security rep wants me to remind all of you with cooling vests NOT to actually wear it when going through security. You know what those gel packs look like when they scan your body? Like a bomb strapped to your chest! Take it off or tell your friends to break out their cameras to film the chaos.
Final TSA advice. Review the rules for disabilities and medical conditions here .
Wheelchair assistance. “Request wheelchair assistance when booking your flight if you are not bringing your own. When you check in, tell the ticket agent that you had requested assistance and they will call someone for you. This person will take you and whoever is traveling with you thru security—without having to stand in the long lines and right to the gate. If you have to switch planes because you’re not flying direct, they will have someone waiting for you to take you to the next gate. If there isn’t anyone there, let the gate agent know and they will call for someone for you. When you arrive at your destination, someone will be there and take you to baggage claim. Remember to take some dollar bills to tip with. The wheelchair assistance will help you conserve your energy.” — Mary, Oklahoma
Personal wheelchairs. If you are traveling with a personal wheelchair, be sure to gate-check your wheels, so that you can take it all the way up to actually boarding the plane. When you leave your chair at the plane's entry, detach all easily removable items and take them aboard the plane personally as a carry-on item. That includes seat cushions, footplates, and armrests. I like to bring a small stuff sack to, well, stuff everything into so that my wheelchair knickknacks stay in one place, limiting the risk of something falling out of the bin and clunking an innocent stranger on the head. And by taking gear with you, it will minimize the risk of losing an important piece of equipment. It will seriously suck if they lose a left footplate and you've got to enjoy your entire vacation with your legs crossed... even when you don't have to tinkle.
TSA Precheck. Is TSA Precheck worth it ($85 for 5 years, Global Entry is $100)? If you fly more than once or twice a year, probably. You get to speed through the security check, waits are usually less than 5 minutes, and you get to keep your shoes on, belt on (I you are brave enough to wear such things with an unpredictable bladder), and your liquids can stay in your bag. If you use a wheelchair, there is usually no pat-down and they just test your hands and chair for explosive residue. Super quick and easy.
Batteries. If you are traveling with a scooter or electric wheelchair, it's best if you have a "gel cell" or "dry cell" battery. If you have a wet cell battery (a rarity these days), the airline will have to remove it from your chair for special storage, a hassle. Again, don't forget to remove seat cushions, etc., to prevent them from getting lost in the belly of the plane as your scooter will either be gate checked or go through checked luggage. Don't forget to secure the key (or power pin) with something a bit stronger than a rubber band. Some suggest fishing line. And setting the throttle on the slowest setting and taping over it will help prevent speedy joyrides.
Weight considerations. How much does your scooter or wheelchair weigh? If it is too heavy, it may not be allowed on some flights. We recommend calling ahead to check for any restrictions.
Power chair tip. On your power chair, if you can remove the joystick, that is recommended. Or at least point it downward. Those little buggers, sticking up at attention, have an uncanny ability to attract errant luggage.
Curbside check-in. Consider using curbside check-in and the luggage porters when you arrive at the airport. Saving your energy for a few bucks is usually worth it.
Recommended seating. Request an isle or forward seat on the airplane. The closer you are to the front of the airplane, the less walking you have to do. Another reason: hey, sometimes when we MSers have to go to the lavatory, well, we really gotta go. If the front of the plane is not available, head to the rear. On international flights, I always check www.seatguru.com to find seats close to the toilet, since there are a number of them located in various areas of large planes. Also note that in the last row the seats may not recline fully, but if you have walking aids, you often can store them behind the seat, which makes retrieving them cake.
Change of clothes. Speaking of bathrooms, it wouldn’t hurt to have a change of clothes in your carry on. In fact, I’d consider this mandatory. Sometimes our bodies don’t do what they are supposed to do, and wearing clean clothes is a lot better than wearing wet clothes washed in the airplane lavatory.
Bathroom advice. And I’d suggest hitting the restrooms just before boarding. Now, of course, don’t dehydrate because of the above advice. Drink plenty of H20.
Jetlag. Jetlag may be mitigated with a sleep aid and it can make even an 18-hour plane trip a relative breeze. BUT a few important words of caution. 1) Never drink alcohol and take a sleep aid. 2) Don't try it for the first time on an airplane. 3) Only take it if you have a companion. A United Airlines security rep warned me that altitude, alcohol and Ambien can be a dangerous mix.

AT YOUR DESTINATION
Pat yourself on the back, you’ve arrived! Here are some tips to make your holiday enjoyable and stress free. Okay, there will always be a little stress. Sorry.
Time your adventures. You know your body. If you have morning energy and splat in the afternoons, maximize mornings. Personally, my bladder gives me fits until 10 or 11, so we rarely are on the road before then. It is what is!
Don't rush. You don't have to cram everything in. Be selective and enjoy what you do. When you get home you'll have far better memories than racing the clock to hit all of the Smithsonian Museums in one D.C. afternoon.
Daypack. I always have one and it has all the essentials. A touch of extra medication, a water bottle, hand sanitizer, a lightweight raincoat or poncho (I’ve got this for my wheelchair ), and an emergency clothing pack (replacement adult undergarment, sanitizing wipes, and a pair of pants).
Skip to the front. If you are using a wheelchair, especially internationally, museums and sights are often free and you go straight to the front of the line, no questions asked. Eiffel Tower with a 2-hour wait? Bam, next elevator. Hordes of people surrounding the Mona Lisa? Bam, front-row access, even closer than any able-bodied person. Sistine Chapel access? Bam, through back corridors and hidden passages of the Vatican.
Toilet scouting. When you get to a cafe or hotel that you will be hanging out at for a bit, ask where the toilets are located before you need them. Some are so well hidden, you would never find them. Ever. At one hotel after dinner I was befuddled as to where the bathrooms were. It was around a screen, in a closet, behind a closed door. Also, some are downstairs, requiring a new plan if stairs are off limits. In one case, a waiter took me to a different building altogether to get me to any easy-access toilet. If you don't see an accessible bathroom, ask. One cafe had it hidden behind brooms and boxes.
Wheelchair assistance. If you need help getting around the airport or a massive hotel or a museum, ask. Don’t be shy. This is your vacation and you don’t want to spend two days recovering from what amounts to stubborn pride. Most facilities have wheelchairs you can borrow, although be forewarned: you'll often get a beater. On a trip to Boston, I got overconfident and failed to bring my wheelchair. And none were available to rent. So we switched hotels to one that provided a chair to guests and used it all weekend. It saved our trip from being a series of short cab rides.
Take advantage of breaks. Seek shade, drink some icy beverages, and sit down when you can. The energy you save will come in handy later, trust me.
Splurge. Sometimes convenience costs a little extra. It's often money well spent. Remember that.
Sidewalks. If you are rolling, your travel companion may need to scout ahead and alter your route to find curb cuts, since some will be blocked or nonexistent.
Folks are accommodating... if you ask. A table by the wall (perfect for stashing my forearm crutches), a spot near the bathroom (for those uncertain times), a seat upfront (to avoid the maze of diners).
Souvenirs. Okay, so you found some incredible (and easily breakable) souvenir on the last days of your trip that will not fit into your luggage with all your clothes ... because you listened to me imploring you not to take a large suitcase. And if you ship it home, odds are high it will break. What to do? Ship home your clothes and toss your new treasure into your bag.
Keepsakes. Laura and I have collected a souvenir from virtually every place we’ve ever traveled. Now before you think our house is nothing more than a pile of cheap trinkets and commemorative shot glasses littering every available shelf, I’ve got to let you in on a secret. Christmas ornaments. They are small, easy to pack, and affordable. Every holiday we decorate the tree together and relive our adventures and experiences for a good month before tucking them away to get discovered anew the following year. Um, yeah, we’re gonna need a bigger tree.
That’s a wrap, our best recommendations and advice for traveling with multiple sclerosis or other disabilities. For more specific tips on how to cruise with multiple sclerosis, don’t miss our exhaustive guide on cruising with a disability .
Happy and safe, stress-free travels!

Featured Links : >
- Newly Diagnosed
- Ask an MS Expert
- MS Navigator
- Ways to Give
Join a Local Support Group
If you are a marketing representative or researcher.
- Smaller Text
- Larger Text
Many groups are meeting virtually. Please reach out to individual group leaders for more information. You can also participate in our online MS communities .
Visit our COVID-19 page for the latest information about COVID-19 and MS – including guidance on vaccines. Check out the Ask an MS Expert webinar series to learn more about topics related to the MS community or reach out to an MS Navigator for additional support.
Self-help groups bring people together who share common life experiences for support, education and mutual aid. Benefits of participating in a self-help group include:
- Learning new information and strategies for confronting problems.
- Finding support from others.
- The opportunity to help others.
- Feeling empowered and more self-confident in coping with challenges.
National MS Society self-help groups focus on support, advocacy, education, wellness or may be more social in nature. Some groups also serve specific populations, such as young adults, parents with MS or carepartners. Other groups may have a specific focus, such as physical activity, wellness or healthy living. People come together at self-help groups to lift each other up through personal struggles and encourage each other to try new things and live each day to its full potential. Learn more about the sense of community and the power of connection offered at National MS Society groups. Find a group in your area here, or to talk to someone about establishing a group, contact an MS Navigator at 1-800-344-4867 or online .
Find Local Groups
Denver west ms self help group, southeast denver ms support group, denver men's self-help group - meets virtually and in-person, ms caregivers of colorado support group, highlands ranch self-help group, arvada ms self-help group, aurora positive support group - now meeting hybrid, north area ms social group, aurora 70/four70 ms men's group, boulder self-help group - now meeting virtually, loveland breakfast social, fort collins men with ms self-help group, ms thriving together, programs calendar.
Explore the variety of programs and events offered by the National MS Society and partners to live your best life.
View Calendar
Discover More
Here are a few related topics that may interest you
Online MS Communities
Ask an ms navigator, msfriends®: one-on-one connections, multiple sclerosis and your emotions (.pdf).
Download Brochure
Someone You Know Has MS: A Book for Families (.pdf)
Depression and ms (.pdf), intimacy and sexuality (.pdf), the national ms society is here to help, we are here.
Contact an MS Navigator

Connect with others who understand.

- Resources Living with MS Work, School, and Leisure
Travel Tips for Those With Multiple Sclerosis

Preparing to travel is often a time-consuming task. When you have a medical condition like multiple sclerosis (MS), it can be even more so. One MyMSTeam member said they had stopped traveling because of all of the complications. “We gave up traveling years ago, especially airplanes. I really don’t trust them and I have too many things I need.” But your diagnosis doesn’t have to mean the end of your travels.
Whether it’s making sure medications can get through security checkpoints or checking to see if your destination is accessible for people with disabilities, many things can add frustration to travel. However, planning ahead can make travel a lot less frustrating. Here are some things you can do to make travel as stress-free as possible with MS.
What To Do Before the Trip
Packing for a trip can take a lot out of anyone, even someone without MS, but some tips can help make travel planning a bit easier.
It can be helpful to pack a little bit at a time over a week or two. It reduces the stress of finding everything at once and makes dealing with fatigue easier. If you use a wheelchair, be sure to bring a backpack and bungee cords that can allow you to attach things to the chair while leaving your hands free. If you are renting a car and usually use disabled parking, bring a disabled placard.
Arranging Accommodations
If possible, get a map of the hotel and any destinations you plan to visit so you can figure out how to access them most easily. Call ahead to ask the hotel about their experience in accommodating people with disabilities and their accessibility options. One member explained, “In the U.S., hotels are required to have handicapped-accessible rooms. You just need to tell them that as part of your booking.” Also, if your medication requires refrigeration, make sure you will have a mini-fridge in your room or suite .
Medical Appointments
Get a note from your doctor or neurologist for any injectables and medications you need to carry, if needed. One MyMSTeam member mentioned that even with a note, some medications still pose a problem. “When it comes to meds, it can be an issue in countries that do not accept certain pain medications or narcotics, even if you have a doctor’s note,” they said.
If you need vaccinations for wherever you are traveling, make sure your medications won’t interfere with their effects .
Communicating
Make sure you and your travel companions are on the same page . Talk about any concerns and make it clear who is responsible for what to prevent headaches on travel day. As one member shared, “I would suggest cutting down the traveling time especially — for your own health.” Discuss your travel expectations — for example, how long you’re willing to be in a plane or car.
Travel Insurance
Travel insurance can be valuable if there is a chance you may not make the trip. Travel agents can help you find insurance.
Traveling by Plane
The Air Carrier Access Act prohibits discrimination based on disability in all forms of air travel. Although airlines generally do not need advance notice of a passenger with disabilities on a flight, certain items (like an electric wheelchair on a flight when the plane has 60 seats or fewer) might need 48 hours of advance notice. Check what kind of plane you will be flying on in advance if you have a wheelchair you need to use. If an airplane has 100 seats or more, the crew is required to store a folding wheelchair in a priority space in the cabin. Most planes are required to have accessible bathrooms. If you have disabilities, you can usually request early boarding to have extra time to get settled on the aircraft.
Additional tips to make flying easier include asking for a seat near the aisle or bathroom. “Request an aisle seat close to the bathrooms while in flight,” one member advised. Another agreed: “Sit in an aisle seat so you can get up and move around whenever you need to.”
Also, take steps to make your time in the airport as easy as possible. Make sure all carry-on medications are in bottles that clearly label the type and who it is prescribed for so there will be fewer delays at security check-in. Although the TSA doesn’t have a specific labeling requirement , there are different laws for prescriptions in different states, so it’s best to be prepared. “If you keep the medication in the original labeled container and have a doctor's note, that should help you overcome any questions,” one member said. See if you can enroll in the TSA PreCheck program beforehand, too. If you are accepted, you don’t need to follow the rules for removing liquids and can wear a jacket, shoes, and a belt through security.
It can be helpful to tell an airport worker about any special needs you have. One member suggested, “Ask for wheelchair assistance at the airport.” Another shared, “I called the airport ahead of time to set up assistance and they picked me up at the entrance and took me everywhere I needed to go.”
Injectable Medications and Air Travel
Some injectable medications can be stored at room temperature and others need to be kept cold. The National Library of Medicine can help you determine which one you have. If you do need to keep medication refrigerated, a travel cooler with an ice pack can help. You must declare all injectables and anything that is used to cool them at airport security checks. To make it simpler for you and the security officials, put them in a plastic bag inside the cooler so they can be taken in and out more easily. “Make sure it’s in original packaging with the prescription on the box,” one member advised. Another said, “I also advise keeping your medicine with you, rather than risk it getting lost in your luggage.”
What To Do During the Trip
Once you finally get to your destination, there are a few things you can do to make your stay more comfortable.
You might want to tell workers you’ll have regular contact with (for example, at a restaurant or hotel) about any noticeable symptoms. Explaining to them that these symptoms are not things to worry about can help ease their minds.
Find out where the nearest emergency services are and the quickest way to them, in case you experience any exacerbations, flare-ups, or worsening of your MS symptoms.
Take rest days . It can be easier to see all the sights if you come back to your hotel room and rest for a while between them. If you usually don’t use mobility aids, consider renting a scooter or a walker. That way, you can still do what you want while reducing fatigue from mobility issues.
Get Support From People Who Understand
MyMSTeam is the social network for people with multiple sclerosis and their loved ones. Members come together to ask questions, give advice, and share their stories with others who understand life with MS.
Looking for advice on how to best travel with MS, or have some tips of your own? Comment below or start a new conversation on MyMSTeam .
- Accessible Travel Basics: From Planning to Execution — National Multiple Sclerosis Society
- Passengers With Disabilities — US Department of Transportation
- Can You Pack Your Meds in a Pill Case and More Questions Answered — Transportation Security Administration
- TSA PreCheck ® — Transportation Security Administration
- DailyMed — National Library of Medicine
- Disabilities and Medical Conditions — Transportation Security Administration
- How to Take Insulin and Needles on a Plane — USA Today
- Globe Trotting — Momentum
- Travel — National Multiple Sclerosis Society
Get medically reviewed MS resources delivered to your inbox
Don’t miss the latest news, tips, and treatment options.
Thank you for subscribing!
Become a member to get even more:.

sign up for free
Attach a gif
Click on a gif to attach it
Become a Subscriber
Get the latest articles about multiple sclerosis sent to your inbox.

Is It Safe To Get Tattoos When You Have Multiple Sclerosis?

When To Quit Working With MS vs. Taking a Medical Leave
Related articles, 6 ways to manage ms fatigue.

MS Fatigue: How Is It Measured?

MS and Sleep: Strategies for Battling Sleep Disturbances

Can Stimulants Help With MS Fatigue?

What Causes Heavy Arms in MS?

How To Conserve Energy With MS

Recent Articles
Relapsing ms playbook.

Managing Relapsing MS: Frequently Asked Questions About Symptoms and Treatments (VIDEO)

What Are the Most Effective Treatments for MS? Know Your DMTs

MyMSTeam Stories: Real Stories From Real Members

My Advocacy Tips: Taking Care of Future Me With MS

Music and Community: How I Fight MS


Travel with MS Jess
The Multiple Sclerosis Travel Guide
Don't let Mulitple Sclerosis stop you from your next GREAT ADVENTURE! Living with MS can present a number of challenges in your life, but that does not mean you can't see the world! With some flexibility, smart planning, and tips from MS Jess, your next adventure awaits!

Traveling with multiple sclerosis (MS) can be challenging, but it is certainly not impossible. It requires careful planning and preparation, including consulting with a healthcare provider and arranging for necessary accommodations. MS can cause a range of symptoms, including fatigue, mobility issues, and cognitive difficulties, which can make traveling more difficult. However, with the right planning and mindset, individuals with MS can still enjoy the joys of travel. This may include selecting destinations that are accessible and accommodating, such as those with good public transportation or mobility aids. Bringing necessary medications and medical supplies is also important. Additionally, taking breaks, staying hydrated, and practicing self-care can help manage symptoms while traveling. With patience, flexibility, and a sense of adventure, traveling with MS can be a rewarding and fulfilling experience that allows individuals to continue exploring the world and making unforgettable memories.

- Sep 15, 2022
GREECE IS A DOOR TO PARADISE

ITALY...COMING SOON

America's National Parks...Coming Soon

Hear from Kathy, Jessica, and Molly as they share their own experiences in response to questions from the MS community .
Watch videos

Home & Travel
Getting around with MS
Tips for making the most of your transportation.

This has been added to your Favorites
For many people living with multiple sclerosis (MS), maintaining an independent lifestyle is very important. Traveling to where you need to go can be a concern, especially if you don’t drive. But the good news is that there are plenty of ways to get around. In the age of the internet and modern transportation, more information and services are available than ever before.
Here are some tips to help you navigate the world of independent travel for everyday life with MS:
Today, there are more ways than ever to plan a trip, whether by bus, train, taxi, or car. Consider using internet trip-planning services and GPS apps to help make your trips more efficient. No matter how you get around, planning ahead can help save time and energy. You can get directions, find different route options, compare modes of transportation (for example, buses versus trains), and keep up with traffic reports. Watch Jessica T. share her routine for planning ahead before running errands.
Make the most of public transportation
Depending on where you live, buses and trains can be great ways to get around for people with MS. If your schedule allows, you can avoid the crowds by traveling during off-peak hours to help make your ride more comfortable. If you use a mobility assistive device, be sure to research special services in your area, such as wheelchair accessible stations and buses. Also, look to see if your city has a public transportation app to help you plan your trip Find more information about public transportation in your area.
Consider taxis and car services
From traditional taxis to car services, there are more options available now than ever. So take a look into which services and apps are in your area. Taxis and car services may help make traveling more efficient. Using mobile apps for these services could make pickups and payment even easier. These services can get a bit pricey if used on a regular basis, so try to plan your trips carefully and make sure they fit into your budget. If you have any issues with mobility or special needs, be sure to look into any special services that may be available.
Ask a friend or family member for a ride
If you have somewhere to go, try asking a loved one to take you. It’s okay to ask for help if you need it. Try to see these rides as a great opportunity for you to spend some quality time with a care partner. Enjoy the bonding experience while still being productive!
Look into getting a handicap plate or placard for your car
If you are cleared to drive by your healthcare team and are legally eligible, a handicap plate or placard can help make your driving experience more convenient. A plate or placard may help you find a parking spot closer to your location, possibly helping you use less energy. Remember to regularly check in with your healthcare team about your ability to drive.
Read more about your state’s laws.
Choose your state below to see which local laws affect you.
Select your state
EXPLORE OTHER TOPICS
You may also like.

10 tips for traveling with MS
From Paul P.

Bathroom modifications for people living with MS
From Dr. Kalina

Bedroom modifications for people living with MS

Commuting to work
From Jessica T.

Entertaining guests in your home
From Gina F.

Kitchen modifications for people living with MS

Getting ready for your next event
From Biogen

Running errands with MS

Tips for traveling by air

Tips for the kitchen
.jpg/_jcr_content/renditions/cq5dam.web.1280.1280.jpeg)
Tools that may help with your mobility
This website uses cookies to ensure you get the best experience on our website. Learn more

Information on how to stay safe and healthy abroad. About us.
- General Travel Health Advice
Multiple Sclerosis and Travel
Multiple Sclerosis (MS) is an autoimmune disorder that affects the brain and spinal cord. The exact cause of MS is unknown but there may be a genetic and environmental element to the development of the illness. At present there is no cure although there are many treatment therapies available to manage the condition. In the UK around 100,000 people are affected.
Prior to travel the following should be considered.
Pre travel Medical Check Up
Travellers should ensure they have had a recent specialist review and have discussed their intention to travel.
Travelling with Medication
All medication should be requested from the GP well in advance of the trip.
- Twice as much medication required for the trip should be taken to cover unexpected delays, damages or losses.
- Medication should be kept in its original packaging and carried in hand luggage to avoid loss or damage in the hold.
- Many medications must be stored within a particular temperature range, this will be detailed in the product information leaflet.
- Gabapentin, used for neuropathic pain, is classed as a Class C controlled drug since April 2019 – see additional advice for travelling with controlled drugs under ‘Home Office Requirements’.
- For those using injectable treatment, a doctors’ letter is necessary for passing through security or customs and can facilitate seeking medical attention abroad.
Travel Health Insurance
MS is considered a pre-existing medical condition and must be declared to the insurer before travel.
- Purchasing comprehensive travel insurance is strongly recommended to pay for any medical expenses whilst abroad.
- Check the FCDO website to see if there is any reciprocal health arrangements with the UK and the country you are visiting to cover the costs of emergency medical treatment whilst you are abroad.
Accessing Healthcare Abroad
Find out about the location of local health facilities prior to travel – this information can be found in travel guides and online resources.
Reducing Risk of Travel Related Illness
Serious infection may impact on the course of MS. The majority of travel-related infections are not vaccine preventable but can be avoided through taking other precautions.
Gastrointestinal Infections and Travellers Diarrhoea
- Taking food and water precautions will reduce the risk of infections that cause travellers’ diarrhoea .
Respiratory/Airborne Infections
- The risk of respiratory infections can be reduced by practising good respiratory hygiene.
- Most MS patients will have been offered the annual inactivated influenza vaccine under UK immunisation guidelines.
Insect-borne Infections
- Vaccines do not exist against the majority of insect-borne infections. Practical measures should be taken on insect bite avoidance .
Travellers with MS are not at a higher risk of acquiring malaria but severe infections may worsen MS symptoms.
- Be aware of malaria risk .
- Take good mosquito bite prevention measures.
- Take antimalarial medications when indicated.
- Seek prompt medical attention if you become unwell of develop a fever after being in a malaria area.
Sun Exposure
- Travellers should be advised to take appropriate steps to minimise sun exposure .
- Some immunosupressive medication may make sunburn more likely as a side effect.
Accidents and Injury
- Accidental injury is more common during travel than infectious disease. Accidental injury may be even more likely if symptoms of MS affect mobility.
Vaccination
- MS itself does not result in increased risk of infection, except in advanced disease.
- Having an infection may provoke a relapse of MS, therefore preventing infection through vaccination is protective.
- There is no evidence of an increased risk of side effects from vaccination in those with MS.
Inactivated Vaccines
- Vaccination should be avoided during serious relapse and until 4 to 6 weeks after full recovery.
- Vaccination may be less effective in those on immunosuppressive medication.
Live Vaccines
- Live vaccines (including yellow fever) are contraindicated in travellers with MS taking immunosuppressive medication.
Yellow Fever Vaccine
In travellers with MS, who are not on immunosuppressive medication, the possible risk of relapse versus the actual risk of yellow fever infection during travel must be discussed.
back to top
- Disease Prevention Advice

America’s first and only
Ultra relay run.
MS Run the US is dedicated to raising awareness and funds to support multiple sclerosis (MS) research, while also aiding those living with disability due to MS.
Apply To Run The Relay
Our Ultra Relay is an epic cross-country relay run from CA to NY for multiple sclerosis, with a limited 19 spots each year! Want to a spot on the team? Become an Ambassador to partner with our mission! Join and be part of the first group considered for the next team!
JOIN OUR COMMUNITY
Become an ambassador.
Each year we run across America, but that’s not all we do! Sign up to join our community of amazing individuals that support our mission all year long through our exciting and inclusive nationwide programs and events!
RUN FOR A REASON
Every year we run across America and rally thousands in support to help STOP multiple sclerosis (MS)! This is our story and why we run for a reason. Join us!
As seen in:


Hepatitis A Vaccine
Because response to HepA vaccine might be reduced in people with HIV infection, perform postvaccination serologic testing on all people with HIV infection ≥1 month after they complete the HepA vaccine series. Consider repeating the vaccine series for patients with poor immune response (i.e., hepatitis A virus [HAV] IgG titer <10 mIU/mL), particularly those who later demonstrate improved immune status (e.g., increased CD4+ T-lymphocyte counts, decreased HIV viral load). If HAV IgG titers are still <10 mIU/mL ≥1 month after the revaccination series, additional vaccination is not recommended; instead, counsel the person on the need to receive HepA immune globulin after an exposure or for higher-risk travel.
Hepatitis B Vaccine
In a study of people infected with HIV who had no immune response to 1 or 2 courses of recombinant HepB vaccine, 2 doses of adjuvanted vaccine (Heplisav-B) were 87% effective in achieving seroprotection.
Intravenous Immunoglobulin
People with HIV might receive periodic doses of intravenous immunoglobulin (IVIG), which can interfere with the immune response to MMR and varicella vaccine. If considering vaccination with MMR or varicella vaccine, administer the vaccines ≈14 days before the next scheduled IVIG dose.
Measles-Mumps-Rubella Vaccine
Two doses of measles-mumps-rubella (MMR) vaccine are recommended for all HIV-infected individuals aged ≥12 months who do not have evidence of current severe immunosuppression (i.e., individuals aged ≤5 years must have CD4+ T-lymphocyte percentages ≥15% for ≥6 months; individuals aged >5 years must have CD4+ T-lymphocyte percentages ≥15% and CD4+ T-lymphocyte counts ≥200 lymphocytes/mL for ≥6 months). Specific recommendations are available for MMR vaccine in people living with HIV .
Chronic Diseases
Factors to consider when assessing the level of immune competence of patients with chronic diseases include clinical stability, comorbidities, complications, duration, severity, and any potentially immunosuppressing treatment (see Sec. 3, Ch. 3, Travelers with Chronic Illnesses ). The pretravel health consultation is an opportunity to ensure that these individuals are vaccinated with recommended routine vaccinations (e.g., HepB and pneumococcal vaccines).
Complement Deficiencies
Patients with complement deficiencies can receive any live or inactivated vaccine.
Dysgammaglobulinemias
Many people with hypogammaglobulinemia or dysgammaglobulinemia receive periodic doses of IVIG, which can interfere with the immune response to MMR and varicella vaccine. If considering vaccination MMR or varicella vaccine, administer the vaccines ≈14 days before the next scheduled IVIG dose.
Multiple Sclerosis
Modern multiple sclerosis (MS) therapy often includes aggressive and early immunomodulatory therapy, even for patients with stable disease. Inactivated vaccines, including HepB, human papillomavirus, influenza, tetanus, and recombinant zoster vaccines generally are considered safe for people with MS. In the event of a clinical relapse, however, delay vaccination until patients have stabilized or begun to improve, typically 4–6 weeks after the relapse began. Although safety and efficacy data are lacking, inactivated vaccines are theoretically safe for people with MS being treated with interferon medication, glatiramer acetate, mitoxantrone, fingolimod, or monoclonal antibody class drugs (e.g., natalizumab, ocrelizumab, rituximab). Published studies are lacking on the safety and efficacy of other vaccines (e.g., HepA, meningococcal, pertussis, pneumococcal, polio, typhoid).
Live Vaccines
Do not administer live vaccines to people with MS during therapy with immunosuppressant drugs (e.g., azathioprine, cladribine, cyclophosphamide, methotrexate, mitoxantrone, ponesimod, teriflunomide); during chronic corticosteroid therapy; or during therapy with any immunosuppressive biologic agents, including alemtuzumab, nataluzimab, ocrelixumab, ocrelizumab, ofatumumab, ozanimod, rituximab, and siponimod. Although definitive studies of glatiramer acetate and interferon therapy are lacking, MS experts generally do not classify them as immunosuppressive medications, and their use does not preclude live vaccine administration. Published studies suggest that live viral MMR and varicella vaccines are safe for people with stable MS if administered 1 month before starting, or at the appropriate interval after discontinuing, immunosuppressive therapy (see Vaccine Considerations for Travelers with Severe Immune Compromise, later in this chapter).
Yellow Fever Vaccine
A small case series published in 2011 reported worsening of MS symptoms and plaques in 5 of 7 patients with relapsing-remitting MS who received yellow fever (YF) vaccine. In contrast, two other studies (published in 2020 and 2021) identified no exacerbations among 55 people with MS who received YF vaccine at different stages of their disease and who were taking a wide variety of medications. Before administering YF vaccine to people with MS who are receiving disease-modifying therapy or nataluzimab, consider the risk of YF virus infection at the destination, as well as potential vaccine-associated risks. Because the effects of YF vaccination in patients receiving disease-modifying therapy or nataluzimab have not been fully studied, decisions about YF vaccination should be made in consultation with the patient’s neurologist. For brief exposures (e.g., only a few days in a YF endemic area) vaccinating travelers with MS against YF likely should be avoided. Weigh the risks and benefits of vaccination for travelers anticipating more prolonged exposures.
Preparing Travelers with Severe Immune Compromise
Severely immunocompromising conditions.
Severely immunocompromised people include those with aplastic anemia, graft-versus-host disease, symptomatic HIV/AIDS, some congenital immunodeficiencies, active leukemia or lymphoma, or generalized malignancy. Others with severe immune compromise include people who recently received radiation therapy or checkpoint inhibitor treatment (therapy of autoimmune complications of treatment is immunosuppressive); people receiving active immunosuppression for solid organ transplants; and both chimeric antigen receptor (CAR)-T cell and hematopoietic stem cell transplant (HSCT) recipients (≤2 years of transplantation or still taking immunosuppressive drugs).
In most cases, severely immunocompromised people should not receive live vaccines, and inactivated vaccines will likely be less effective. These patients should consider postponing travel until their immune function improves. For people likely to travel in the future, usual travel-related vaccines can be initiated before beginning immunosuppressive therapies, if feasible. Whenever possible, administer inactivated vaccines ≥2 weeks and live vaccines ≥4 weeks before immunosuppression.
Symptomatic HIV/AIDS
Clinicians need to know an HIV-infected traveler’s current CD4+ T-lymphocyte count for the pretravel consultation. People with HIV and CD4+ T-lymphocyte counts <200/mL, a history of an AIDS-defining illness without immune reconstitution, or clinical manifestations of symptomatic HIV are considered to have severe immunosuppression (see Sec. 5, Part 2, Ch. 11, Human Immunodeficiency Virus / HIV ), and they should not receive live viral or live bacterial vaccines because of the risk that the vaccine could cause serious systemic disease. For MMR vaccine, severe immunosuppression is defined as CD4+ T-lymphocyte percentages <15% in any age group or CD4+ T-lymphocyte counts <200/mL in people >5 years old.
Recommend that newly diagnosed, treatment-naïve patients with CD4+ T-lymphocyte counts <200/mL delay travel pending reconstitution of CD4+ T-lymphocyte counts with antiretroviral therapy and, ideally, complete suppression of detectable viral replication. Delaying travel helps minimize the risk for infection and avoid immune reconstitution illness while away.
Chronic Lymphocytic Leukemia & Hematopoietic Stem Cell Transplant
People with chronic lymphocytic leukemia have poor humoral immunity, even early in the disease course, and rarely respond to vaccines. Hematopoietic stem cell transplant (HSCT) recipients who received vaccines before their transplant should be revaccinated routinely afterward, regardless of the source of the transplanted stem cells. Begin complete revaccination with standard childhood vaccines 6 months after HSCT, with the caveat that MMR and varicella vaccines should be administered 24 months after transplant and only if the recipient is immunocompetent. Thus, HSCT recipients ideally should delay travel ≥2 years after transplant to allow for full revaccination.
Administer inactivated influenza vaccine beginning ≥6 months after HSCT and annually thereafter. A dose of inactivated influenza vaccine can be given ≥4 months after transplant if there is a community outbreak.
Solid Organ Transplant Recipients
For solid organ transplant recipients, the risk for infection is greatest in the first year after transplant; recommend to travelers that they should postpone trips to high-risk destinations until after that time.
Medications that Compromise the Immune System
A variety of medications and biologic agents compromise the immune system. Regard anyone taking these medications as severely immunocompromised. Doses of inactivated vaccines received while receiving immunosuppressive medications or during the 2 weeks before starting such medications should not be counted toward a primary vaccination series or relied upon to induce adequate immune responses. Patients should be revaccinated with all indicated inactivated vaccines at least 3 months after potent immunosuppressive therapy is discontinued.
Alkylating Agents
Regard anyone taking alkylating agents (e.g., cyclophosphamide) as severely immunocompromised.
Antimetabolites
Regard anyone taking antimetabolites (e.g., 6-mercaptopurine, azathioprine, methotrexate) as severely immunocompromised.
Biologic Agents
Immunosuppressive or immunomodulatory biologic agents can produce immunocompromise by the mechanisms outlined in Table 3-04 . B cell–depleting agents (cladribine, ocrelizumab, ofatumumab, ozanimod, rituximab, siponimod) and lymphocyte-depleting agents (alemtuzumab, thymoglobulin) induce major immunosuppression. Consideration of the clinical context in which these were given is important, especially in hematologic malignancies.
Table 3-04 Immunosuppressive & immunomodulatory biologic agents that preclude use of live vaccines 1
Abbreviations: CD, cluster of differentiation; CTLA, cytotoxic T-lymphocyte antigen; EGFR, epidermal growth factor receptor; IL, interleukin; PD, programmed cell death protein; TGF, transforming growth factor; TNF, tumor necrosis factor; VEGF, vascular endothelial growth factor.
1 This table is based primarily on conservative expert opinion, given the lack of clinical data. Numerous agents often are given in combination with other agents (especially chemotherapy) and are immunosuppressive when given together. The list provides examples but is not inclusive of all biologic agents that suppress or modulate the immune system. Not all therapeutic monoclonal antibodies or other biologic agents result in immunosuppression; details of individual agents not listed here must be reviewed before determining whether live viral vaccines can be given. Interferon and glatiramer acetate given to patients with multiple sclerosis (MS) are immunomodulators and are generally not classified by MS experts as immunosuppressive so do not preclude live vaccine administration (except perhaps yellow fever vaccine), but clinical data to support safety with live vaccines are lacking.
Cancer Chemotherapeutic Agents
Cancer chemotherapeutic agents are classified as severely immunosuppressive, as demonstrated by increased rates of opportunistic infections and blunting of responses to certain vaccines among patient groups. Some of these agents are less immunosuppressive than others (e.g., tamoxifen and trastuzumab, given to breast cancer patients, are less immunosuppressive than alkylating agents or antimetabolites), but clinical data to support safety with live vaccines are lacking. Vaccination following immunotherapies (e.g., checkpoint inhibitors, CAR-T cell treatments) has not been well studied, and until additional data are available, avoid vaccinating patients receiving these treatments with live attenuated vaccines for 3–6 months after treatment or until they have had immune reconstitution.
High-Dose Corticosteroids
Most clinicians consider a dose of >2 mg/kg of body weight or ≥20 mg per day of prednisone (or its equivalent) in people who weigh >10 kg, when administered for ≥2 weeks, as sufficiently immunosuppressive to raise concern about the safety of vaccination with live vaccines. Furthermore, the immune response to vaccines could be impaired. Clinicians should wait ≥1 month after discontinuation of high-dose systemic corticosteroid therapy before administering a live-virus vaccine.
Transplant-Related Immunosuppressive Drugs
Regard anyone receiving transplant-related immunosuppressive drugs as severely immunocompromised. Examples of transplant-related immunosuppressive drugs include azathioprine, belatacept, cyclosporine, everolimus, mycophenolate mofetil, prednisone, sirolimus, and tacrolimus.
Tumor Necrosis Factor Blockers
Tumor necrosis factor (TNF) blockers (e.g., adalimumab, certolizumab pegol, etanercept, golimumab, infliximab) blunt the immune response to certain chronic infections and certain vaccines. When used alone or in combination regimens with other disease-modifying agents to treat rheumatoid disease, TNF blockers are associated with an impaired response to HepA, influenza, and pneumococcal vaccines, suggesting that for better protection, all doses in the HepA and pneumococcal series should be given before travel. The use of live vaccines is contraindicated for most people receiving these therapies.
Vaccine Considerations for Travelers with Severe Immune Compromise
Inform severely immunocompromised people that their response to vaccination might be muted. The immunosuppressive regimen does not predict the decrease in response to vaccination. No basis exists for interpreting laboratory studies of general immune parameters to predict vaccine safety or efficacy. Recent data in solid organ transplant recipients vaccinated before transplant suggest that a prolonged phase of protective antibody titers can exist after transplant. In general, serologic testing for response to most travel-related vaccines is not clinically recommended.
The length of time clinicians should wait after discontinuation of immunosuppressive therapies before administering a live vaccine is not uniform and depends on the therapy. For cancer chemotherapy, radiation therapy, and highly immunosuppressive medications (exclusive of lymphocyte-depleting agents and organ transplant immunosuppression), the waiting period is 3 months. For lymphocyte-depleting agents (alemtuzumab, rituximab), the waiting period is ≥6 months, although IDSA guidelines suggest that the waiting period should be ≥1 year. For immunosuppressive corticosteroid regimens, the waiting period is 1 month. Restarting immunosuppression after live vaccination has not been studied, but some experts would recommend waiting ≥1 month. Special considerations for travelers with severe immune compromise apply for several travel-related vaccines.
The safety and effectiveness of the oral live attenuated bacterial cholera vaccine, Vaxchora, has not been established in immunocompromised people. An older formulation of CVD 103-HgR vaccine was not associated with serious or systemic adverse events in patients with HIV, although the data are limited.
Safety and efficacy of Ebola Zaire live recombinant vaccine (ERVEBO, rVSV-ZEBOV vaccine [Merck Sharp & Dohme Corp.]) has not been adequately assessed in immunocompromised adults. A small number of adults living with HIV have been vaccinated with ERVEBO, and additional studies are ongoing to investigate its use in people living with HIV without severe immune compromise. The risk from vaccination with ERVEBO in immunocompromised people should be weighed against the risk for Ebola virus disease.
Hepatitis A
Data indicate that immunocompromised people, notably those being treated with immunosuppressive drugs, can have inadequate or slow seroconversion after a single dose of HepA vaccine. Limited data also suggest that modified dosing regimens, including a doubling of the standard antigen dose or administration of additional doses prior to travel, might increase response rates.
Solid organ transplant candidates who are unvaccinated, undervaccinated, or seronegative for HepA should receive a 2-dose HepA vaccine series. People with immunocompromising conditions should start a 2-dose HepA vaccine series as soon as travel is considered. Immunocompromised people traveling in <2 weeks should simultaneously receive the initial dose of HepA vaccine and HepA immune globulin (IG); administer the vaccine and the IG in separate limbs. Testing for the presence of HAV antibody after vaccination is recommended for immunocompromised people whose subsequent clinical management depends on knowledge of their immune status and people for whom revaccination might be indicated. Because response to HepA vaccine might be reduced in people with HIV infection, perform postvaccination serologic testing on all people with HIV infection ≥1 month after they complete the HepA vaccine series.
Hepatitis B
The humoral immune response to HepB vaccine is reduced in immunocompromised children and adults. Limited data indicate that modified dosing regimens could increase response rates. As with dialysis patients, use a 3-dose series of 40 µg Recombivax HB at 0, 1, and 6 months, or a 4-dose series of 40 µg Engerix-B at 0, 1, 2, and 6 months. Heplisav-B (HepB-CpG) is an adjuvanted vaccine and is administered as 2 doses, 1 month apart, in people ≥18 years old. Postvaccination serologic testing after any HepB vaccination series is recommended to confirm response and guide the need for revaccination in immunocompromised people.
Japanese Encephalitis
Although recommended for numerous destinations (see Sec. 5, Part 2, Ch. 13, Japanese Encephalitis ), no data are available on the safety or efficacy of Japanese encephalitis (JE) vaccines in immunocompromised patients. JE vaccine should be given to at-risk travelers. As with other vaccines, immunocompromised patients likely will have decreased intensity and durability of protection, and more frequent booster doses might be indicated.
Immunocompromised people deemed at risk for vaccine-preventable rabies should receive a 3-dose series of vaccine on days 0, 7, and 21 or 28, but not the 2-dose series (day 0 and day 7) recommended in 2021 for immunocompetent people. Furthermore, administer the vaccine as an intramuscular injection, not as an intradermal injection as recommended by some authorities outside the United States. Serologic postvaccination testing might be indicated. For postexposure rabies prophylaxis, all severely immunocompromised people should generally receive rabies vaccine at days 0, 3, 7, 14, and 28, plus human rabies immune globulin, regardless of previous vaccination history.
Smallpox / Monkeypox
JYNNEOS (Imvamune, Imvanex) is an approved by the US Food and Drug Administration (FDA) vaccine for prevention of smallpox and monkeypox, but it is not commercially available. JYNNEOS is a live, attenuated, nonreplicating, virus-derived vaccine that is indicated for first responders participating in smallpox or monkeypox outbreaks. Unlike the live, replication-competent smallpox vaccine (ACAM2000), JYNNEOS is not contraindicated for use in immunocompromised people and should be safe. Immunocompromised people might, however, have a diminished immune response to the vaccine.
Tick-Borne Encephalitis
Immunocompromised people might have a diminished immune response to killed tick-borne encephalitis vaccine, which is FDA-approved and safe for this population.
Typhoid Fever
CDC recommends administering injectable Vi capsular polysaccharide vaccine (Typhim Vi, ViCPS) rather than live, oral Salmonella typhi vaccine Ty21A (Vivotif) for at-risk, immunocompromised patients. Data on the safety and efficacy of typhoid vaccines in immunocompromised patients are lacking.
Yellow Fever
Contraindications.
In general, strongly discourage unvaccinated travelers with severe immune compromise from traveling to destinations where infection with YF virus is a risk. Severe immunosuppression is a contraindication to YF vaccination because these patients are at increased risk of developing a serious adverse event (e.g., life-threatening YF vaccine–associated viscerotropic disease, YF vaccine–associated neurologic disease). Additionally, YF vaccination is contraindicated in people with a history of a thymus disorder associated with abnormal immune cell function (e.g., myasthenia gravis or thymoma); this contraindication applies regardless of whether the person has undergone therapeutic thymectomy (see Sec. 5, Part 2, Ch. 26, Yellow Fever ). No data are available to support IgA deficiency as a contraindication to YF vaccination.
If patients are unable to avoid travel to areas where YF vaccination is recommended (see Maps 5-10 and 5-11 ) and the immunocompromised traveler is previously unvaccinated, inform them of YF risk, carefully instruct them in methods to avoid mosquito bites, and provide them with a vaccination medical waiver in their International Certificate of Vaccination or Prophylaxis (see
International Certificate of Vaccination or Prophylaxis , and Sec. 5, Part 2, Ch. 26, Yellow Fever ). Travelers falling into this category might choose to travel during periods of lower disease activity. Warn travelers that some countries with YF vaccine entry requirements might not honor YF vaccination waiver documents and that the traveler might be refused entry or quarantined.
Precautions (Relative Contraindications)
ACIP considers certain conditions with limited immune deficits (e.g., asymptomatic HIV infection) to be precautions (as opposed to contraindications) to administration of YF vaccine. For these patients, offer YF vaccine if travel to YF-endemic areas is unavoidable, and monitor vaccine recipients closely for possible adverse effects. If country entry requirements, and not true exposure risk, are the only reasons to vaccinate a traveler with asymptomatic HIV infection or a limited immune deficit, the physician should provide a waiver (see /travel/page/icvp, and Sec. 5, Part 2, Ch. 26, Yellow Fever ). Studies show that higher CD4+ T-lymphocyte counts and suppressed HIV viral loads seem to be the key determinants for developing protective neutralizing antibodies after YF vaccination. Patients with undetectable viral loads respond well to YF vaccination regardless of CD4+ T-lymphocyte counts, although data are limited in those with CD4+ T-lymphocyte counts <200/mL. Because vaccine response might be suboptimal, such vaccinees are candidates for serologic testing 1 month after vaccination. For information about serologic testing, contact the state health department or CDC’s Division of Vector-Borne Diseases at 970-221-6400. Current data from clinical and epidemiologic studies are insufficient to evaluate the actual risk for severe adverse effects associated with YF vaccine among recipients with limited immune deficits.
Booster Doses
Because a single dose of YF vaccine provides long-lasting protection, ACIP no longer recommends booster doses for most travelers. Additional doses of YF vaccine are recommended, however, for some people who might not have as robust or sustained immune response to YF vaccine.
People who received HSCT after receiving a dose of YF vaccine and who are sufficiently immunocompetent to be safely vaccinated should be revaccinated if travel puts them at risk for YF. People infected with HIV when they received their last dose of YF vaccine should receive a dose every 10 years if they continue to be at risk for YF and if their current CD4+ T-lymphocyte counts do not indicate precautions or contradictions. Recent data suggest that YF vaccination before solid organ transplant, even long before transplant, generally provides protective antibody levels after transplant.
Although no extra pretravel indication exists, many travel clinics administer zoster vaccines. In 2021, the FDA approved the use of recombinant zoster vaccine (RZV), now the only available preparation in the United States, for all immunocompromised people ≥18 years of age.
ACIP recommends 2 doses of recombinant zoster vaccine for all adults ≥19 years old who are or who will be immunodeficient or immunosuppressed due to disease or therapy, regardless of travel plans. Qualifying underlying conditions include, but are not limited to, HSCT or solid organ transplant recipients, hematologic and or generalized cancer, HIV, and people receiving immunosuppressive therapy.
Routine Vaccines
Three live vaccines (MMR, rotavirus, and varicella) should be administered to susceptible household contacts and other close contacts of immunocompromised patients when indicated. If a varicella vaccine recipient has a rash after vaccination, direct contact with susceptible household contacts with altered immunocompetence should be avoided until the rash resolves. Educate immunocompromised patients about the risk for fecal–oral transmission of poliovirus in countries where the oral polio vaccine is used, since there have been reports of reversion to wild type virus with associated clinical disease.
For influenza vaccination, choose inactive influenza vaccine (IIV); household and other close contacts of mildly or moderately immunocompromised patients can safely receive LAIV if they are unable to receive IIV. LAIV is contraindicated in close contacts and caregivers of severely immunocompromised people who require a protected environment.
Smallpox / Monkeypox Vaccine
ACAM2000 is a live, replicating smallpox vaccine, indicated for use in military personnel and laboratory workers with potential exposure to the virus. Recipients of the vaccine can transmit the virus to household and intimate contacts; therefore, vaccinated family or household members should implement infection control measures, particularly those with immunocompromise. JYNNEOS is an FDA-approved but not commercially available live nonreplicating smallpox/monkeypox vaccine that would not be contraindicated in immunocompromised individuals or their contacts.
Yellow fever vaccine can be administered to household contacts when indicated.
Malaria infection and the drugs used to treat it can exacerbate an immunocompromised traveler’s underlying condition. Moreover, asplenia, HIV, and some immunosuppressive regimens can predispose travelers to more serious malaria infection. For these reasons, stress the need for malaria prophylaxis and strict adherence to mosquito bite avoidance to immunocompromised travelers to malaria-endemic areas (see Sec. 2, Ch. 5, Yellow Fever Vaccine & Malaria Prevention Information, by Country ; Sec. 4, Ch. 6, Mosquitoes, Ticks & Other Arthropods ; and Sec. 5, Part 3, Ch. 16, Malaria ).
People Infected with HIV
Malaria is more severe in people infected with HIV; malaria infection increases HIV viral load and could exacerbate disease progression. In addition, take extra care when researching potential drug interactions in people with HIV who are receiving antiretroviral therapy. The University of Liverpool offers an interactive web-based resource for assessing possible drug interactions ( mobile application also is available).
Chemoprophylaxis
Some older maintenance regimens for HIV have been noted to interact with drugs used for malaria chemoprophylaxis. Notably, chloroquine, mefloquine, and primaquine can interact with older maintenance regimens for HIV, particularly those containing protease inhibitors (PIs). Efavirenz lowers serum levels of both atovaquone and proguanil, but no evidence suggests clinical failure of these agents when used concurrently. Efavirenz also potentially can increase the production of hemotoxic primaquine metabolites.
Most current first-line regimens for HIV (integrase and entry inhibitors) have few drug interactions. Commonly used integrase inhibitors (bicetegravir, cabotegravir, dolutegravir, elvitegravir, raltegravir), and nucleoside/nucleotide reverse transcriptase inhibitor (NRTI) combinations (brand names include Descovy-Tivicay, Truvada-Tivicay) have no known interactions with CDC-recommended malaria chemoprophylactic drugs; the cobicistat booster co-formulated with elvitegravir (Stribild, Genvoya) theoretically could increase mefloquine levels. The emtricitabine, rilpivirine, tenofovir alafenamide (TAF)/tenofovir disoproxil fumarate (TDF) combinations (Odefsey and Complera) similarly have no interactions with antimalarial drugs.
Malaria treatment regimens, including artemisinin derivatives, quinine/quinidine, lumefantrine (part of the artemether/lumefantrine combination, Coartem), and atovaquone and proguanil potentially could have interactions with many non-nucleoside reverse transcriptase inhibitors (NNRTIs), PIs, and the CCR5 receptor antagonist, maraviroc. Seek advice from CDC or other malaria experts when treating patients for malaria who are also on antiretrovirals.
Organ Transplant Recipients
In organ transplant recipients, atovaquone-proguanil might be the most appropriate malaria prophylactic agent because other antimalarials can interact with calcineurin inhibitors and mTor inhibitors (cyclosporine, everolimus, sirolimus, tacrolimus). Chloroquine, doxycycline mefloquine, and primaquine can elevate calcineurin inhibitor levels. Chloroquine and mefloquine can interact with calcineurin inhibitors to prolong the QT interval. Some travel-related medications need to be dose-adjusted according to altered hepatic or renal function.
Many foodborne and waterborne infections (e.g., those caused by Campylobacter , Cryptosporidium , Giardia , Listeria , Salmonella , or Shigella ) can be severe or become chronic in immunocompromised people. Provide all travelers with instruction on safe food and beverage precautions; travelers’ diarrhea can occur despite strict adherence. Meticulous hand hygiene, including frequent and thorough handwashing with soap and water, is the best prevention against gastroenteritis. Travelers should wash hands after contact with public surfaces, after any contact with animals or their living areas, and before preparing or eating food.
Travelers’ Diarrhea
Selecting antimicrobial drugs for appropriate self-treatment of travelers’ diarrhea (see Sec. 2, Ch. 6, Travelers’ Diarrhea ) requires special consideration of potential drug interactions in patients already taking medications for chronic medical conditions. Fluoroquinolones, rifaximin, and rifamycin SV are active against several enteric bacterial pathogens and are not known to have major interactions with highly active antiretroviral therapy (HAART) drugs. Macrolide antibiotics can, however, interact with HAART drugs. Fluoroquinolones and azithromycin are generally well tolerated in combination with calcineurin inhibitors and mTor inhibitors, but in rare instances increase a prolonged QT interval (caution in those >500 ms).
Waterborne Diseases
To reduce the risk for cryptosporidiosis, giardiasis, and other waterborne infections, immunocompromised travelers should avoid swallowing water during swimming and other water-based recreational activities and should not swim in water that might be contaminated with sewage or animal waste. Travelers with liver disease should consider avoiding direct exposure to salt water because of the risk for Vibrio spp. exposure, and all immunocompromised people should avoid raw seafood. Patients and clinicians should be aware of the risk for infection or colonization with multidrug-resistant organisms during travel; remind immunosuppressed travelers who become ill to report recent travel to their doctors.
Geographically focal infections that pose an increased risk for severe outcomes for immunocompromised people include visceral leishmaniasis (see Sec. 5, Part 3, Ch. 15, Visceral Leishmaniasis ) and inhaled fungal infections such as Talaromyces marneffei (formerly Penicillium marneffei ) in Southeast Asia, and coccidioidomycosis (see Sec. 5. Part 4, Ch. 1, Coccidioidomycosis / Valley Fever ) and histoplasmosis (see Sec. 5, Part 4, Ch. 2, Histoplasmosis ) in the Americas.
Coronavirus Disease 2019
People with immunocompromising conditions or who are on immunosuppressive therapy are at increased risk for severe illness, hospitalization, and death if infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes coronavirus disease 2019 (COVID-19). Moreover, moderately or severely immunocompromised people might routinely shed infectious virus for ≤20 days (see Sec. 5, Part 2, Ch. 3, COVID-19 ).
Counsel moderately and severely immunocompromised people to be up to date with their COVID-19 vaccinations before travel. Because people who are immunocompromised might have a less robust immune response to COVID-19 vaccines, even those whose vaccinations are up to date should maintain awareness of the COVID-19 situation at their destination. In the pretravel consultation, discuss the possible options of reconsidering travel or delaying travel to destinations where COVID-19 transmission is currently high and risk for infection is greater.
CDC also provides COVID-19 cruise ship information . SARS-CoV-2 spreads easily on cruise ships; outbreaks can overwhelm onboard medical capacity, and ship-to-shore medical evacuations can be challenging (see Sec. 8, Ch. 6, Cruise Ship Travel ).
In addition to helping ensure that moderately and severely immunocompromised travelers are up to date with their COVID-19 vaccinations, provide information on the importance of taking protective measures (e.g., wearing a well-fitting mask or respirator while in public indoor spaces, avoiding spending time in poorly ventilated indoor locations). Suggest to immunocompromised travelers that they also consider wearing a well-fitting mask or respirator when outdoors during sustained close contact with others. Advise close contacts (e.g., household members, caregivers) of immunocompromised people to adhere to the same precautions. See the latest guidance and recommendations regarding COVID-19 vaccinations, boosters, and therapeutic options .
Tuberculosis
Establishing the tuberculosis status of immunocompromised travelers going to regions endemic for tuberculosis can be helpful in the evaluation of subsequent illness (see Sec. 5, Part 1, Ch. 23, . . . perspectives: Testing Travelers for Mycobacterium tuberculosis Infection ). Depending on the traveler’s degree of immune suppression, the baseline tuberculosis status might be assessed by a tuberculin skin test, Mycobacterium tuberculosis antigen–specific interferon-γ assay (i.e., QuantiFERON-TB Gold or T-SPOT TB, both generally more sensitive in immunocompromised patients than skin testing), or chest radiograph. The need for posttravel testing (often 3 months after travel) depends on exposure risk during the trip, medical conditions, and other factors.
People with HIV and transplant recipients might require primary or secondary prophylaxis for opportunistic infections (e.g., Mycobacterium , Pneumocystis , and Toxoplasma spp.). Adherence to all indicated prophylactic regimens should be confirmed before travel.
The following authors contributed to the previous version of this chapter: Camille Nelson Kotton, Andrew T. Kroger, David O. Freedman
Bibliography
Agarwal N, Ollington K, Kaneshiro M, Frenck R, Melmed GY. Are immunosuppressive medications associated with decreased responses to routine immunizations? A systematic review. Vaccine. 2012;30(8):1413–24.
Barte H, Horvath TH, Rutherford GW. Yellow fever vaccine for patients with HIV infection. Cochrane Database Syst Rev. 2014;(1):CD010929.
Buchan CA, Kotton CN; AST Infectious Diseases Community of Practice. Travel medicine, transplant tourism, and the solid organ transplant recipient—Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice. Clin Transplant. 2019;33(9):e13529.
Dekkiche S, de Valliere S, D’Acremont V, Genton B. Travel-related health risks in moderately and severely immunocompromised patients: a case-control study. J Travel Med. 2016;23(3):taw001.
Farez MF, Correale J. Yellow fever vaccination and increased relapse rate in travelers with multiple sclerosis. Arch Neurol. 2011;68(10):1267–71.
Garcia Garrido HM, Wieten RW, Grobusch MP, Goorhuis A. Response to hepatitis A vaccination in immunocompromised travelers. J Infect Dis. 2015;212(3):378–85.
Huttner A, Eperon G, Lascano AM, Roth S, et al. Risk of MS relapse after yellow fever vaccination: A self-controlled case series. Neurol Neuroimmunol Neuroinflamm. 2020;7(4):e726. Infectious Disease Society of America. Guidelines for the prevention and treatment of opportunistic infections in adults and adolescents with HIV. Available from: www.idsociety.org/practice-guideline/prevention-and-treatment-of-opportunistic-infections-among-adults-and-adolescents.
Kroger A, Bahta L, Hunter P. General best practice guidelines for immunization. Best practices guidance of the Advisory Committee on Immunization Practices (ACIP) [updated May 4, 2021]. Available from: www.cdc.gov/vaccines/hcp/acip-recs/general-recs/downloads/general-recs.pdf.
Loebermann M, Winkelmann A, Hartung HP, Hengel H, Reisinger EC, Zettl UK. Vaccination against infection in patients with multiple sclerosis. Nat Rev Neurol. 2011;8(3):143–51. Luks AM, Swenson ER. Evaluating the risks of high altitude travel in chronic liver disease patients. High Alt Med Biol. 2015;16(2):80–8.
Pacanowski J, Lacombe K, Campa P, Dabrowska M, Poveda JD, Meynard JL, et al. Plasma HIV-RNA is the key determinant of long-term antibody persistence after yellow fever immunization in a cohort of 364 HIV-infected patients. J Acquir Immune Defic Syndr. 2012;59(4):360–7.
Papeix C, Mazoyer J, Maillart E, Bensa C, et al. Multiple sclerosis: Is there a risk of worsening after yellow fever vaccination? Multiple Sclerosis J. 2021;27(14):2280–3.
Perry RT, Plowe CV, Koumare B, Bougoudogo F, Kotloff KL, Losonsky GA, et al. A single dose of live oral cholera vaccine CVD 103-HgR is safe and immunogenic in HIV-infected and HIV-noninfected adults in Mali. Bull World Health Organ. 1998;76(1):63–71.
Rubin LG, Levin MJ, Ljungman P, Davies EG, Avery R, Tomblyn M, et al. 2013 IDSA clinical practice guideline for vaccination of the immunocompromised host. Clin Infect Dis. 2014;58(3):309–18.
Schwartz BS, Rosen J, Han PV, Hynes NA, Hagmann SH, Rao SR, et al. Immunocompromised travelers: demographic characteristics, travel destinations, and pretravel health care from the U.S. Global TravEpiNet Consortium. Am J Trop Med Hyg. 2015;93(5):1110–6.
Visser LG. TNF-α antagonists and immunization. Curr Infect Dis Rep. 2011;13(3):243–7.
Wieten RW, Goorhuis A, Jonker EF, de Bree GJ, de Visser AW, van Genderen PJ, et al. 17D yellow fever vaccine elicits comparable long-term immune responses in healthy individuals and immune-compromised patients. J Infect. 2016;72(6):713–22.
Wyplosz B, Burdet C, Francois H, Durrbach A, Duclos-Vallee JC, Mamzer-Bruneel MF, et al. Persistence of yellow fever vaccine-induced antibodies after solid organ transplantation. Am J Transplant. 2013;13(9):2458–61.
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Multiple Sclerosis (MS) Support Groups
Find the right community that fits your needs
Multiple sclerosis (MS) is a disease of impaired nerve signaling within a person’s brain and spinal cord. The variable symptoms of MS—fatigue, pain, walking difficulties, vision problems, and more—can be socially isolating and interfere with daily functioning.
Support groups are a valuable resource for those living with MS because they connect people with similar experiences, so they do not feel so alone.
Besides providing social companionship, comfort, and a shared bond, support groups can provide coping strategies for managing the day-to-day struggles of living with MS. They can also help strengthen your overall emotional well-being.
Below we have chosen some MS support groups. These communities will hopefully give you the comfort, information, social interaction, and emotional support you deserve as you navigate your unique MS journey.
National Multiple Sclerosis Society
The National Multiple Sclerosis Society (NMSS) is a prominent organization in MS research, education, and awareness.
NMSS offers a vast network of free, in-person and virtual support groups located throughout the country. Some of these communities target certain populations, like young adults, veterans, or African Americans living with MS, with focuses on learning about the condition, coping with challenges, being an advocate, and connecting socially with others.
NMSS also offers a free, confidential telephone program called MSFriends . This program connects you with trained volunteers who are also living with MS. The organization also offers MS Navigators , which are highly skilled, devoted professionals who work directly with people with MS. MS Navigators can also work with loved ones, family members, and/or caregivers of those living with MS.
MS World is a patient-run organization that has served more than 225,000 members. Its mission is to end the isolation of living with MS, and it promotes the idea of “wellness being a state of the mind,” which emphasizes the healing power of the mind-body connection.
This organization has a very large and active MS forum and chat room where you can connect with others living with MS, as well as loved ones of those with MS, or people who think they may have MS.
MS World has dozens of well-organized subforums that allow members to share their stories or discuss specific MS topics like symptoms, treatments, and assistive devices. There is also a subforum for general MS questions and answers.
Additionally, the forum has perks, acting as a wellness center where members can share recipes, books, and movies, and discuss healthy eating habits. Volunteer moderators on the site also review all member posts beforehand, deleting any that are potentially harmful or misleading.
Can Do Multiple Sclerosis
Can Do Multiple Sclerosis is a nonprofit organization that addresses not only the disease, but also its widespread physical, emotional, and spiritual implications.
There are two free support and educational workshops offered by this organization. JUMPSTART is a free, two-hour virtual workshop, with a different topic every month. This program gives people with MS and their support partners the education, tips, and tools for managing their disease and overall health and well-being. The workshops focus on topics like mood and cognition, exercise, navigating the activities of daily life, and healthy eating.
Another option is TAKE CHARGE , which is a free, two-day interactive weekend workshop for people aging with MS and their support partners. The virtual retreat is offered a few times per year, and pre-program courses have people with MS and their partners develop personal goals with a team of coaches and other participants to find solutions on how to live better with MS. Participants will also receive individual coaching from financial planners, dietitians, physical therapists, and medical professionals. Courses cover topics such as aging and MS, cognition, managing mobility challenges, sleep, and intimacy.
MyMSTeam is part of MyHealthTeam , an independent startup based in San Francisco.
This free social network of over 158,000 members is easy to navigate and is a good place to start if you are recently diagnosed or looking to foster new friendships.
On the website, you can find people like you by searching through a directory, which sorts members using various filters, such as the type of MS they have or their symptoms.
Their network also provides a friendly, guided question and answer section. Another cool feature is the activity page, where members can post and share pictures, stories, thoughts, jokes, and inspirational quotes.
An added note—the organization does report that it may partner with a pharmaceutical company or university on occasion. MyMSTeam states that it occasionally shares information about members, which is kept anonymous and does not reveal any specifics. MyMSTeam will always let individuals know ahead of time if it is doing so, and does not give these companies access to the actual network.
Multiple Sclerosis Association of America
The Multiple Sclerosis Association of America (MSSA) is a nonprofit organization that aims to improve the lives of those with MS through service and support.
The My MSAA Community is a free online support forum (powered by HeathUnlocked.com) for people living with MS and their loved ones. The forum has more than 8,000 members.
The forum layout is well-organized and easy to navigate. Registration is fast and straightforward. Members write a post, and then others can respond with a reply or a "like." You can also search on the forum for members who live near you for a better connection.
Another one of MSSA’s services is its toll-free Helpline, which allows people with MS and their family members, friends, and caregivers to speak with a trained social services specialist or counselor.
The Multiple Sclerosis Foundation (MSF) created a supportive community called the MS Focus Independent Support Group Network. Within this program, individuals living with MS or healthcare professionals can receive various materials and resources through MSF to launch and lead their own support groups.
People can share their MS journey and struggles and the support group leader can share tips on living well with MS, encourage positive thinking, and provide up-to-date MS research findings.
To find a support group (not necessarily start one), you can search the online directory for meetings near you. MS Focus also has a Facebook group for folks who prefer online support, which includes discussions about alternative medicine, therapy, medications, and pain management. There are moderators for the community, but conversations are free-flowing.
PatientsLikeMe
PatientsLikeMe is a MS community where members can share personal data (i.e. log their MS symptoms or treatments they tried). This data is then collected, combined, and revealed through a series of illustrated, colorful, and easy-to-read graphs and charts, which is available for members.
The data provided by members is voluntary, so HIPAA privacy rules do not apply to the site's user health profiles. Nevertheless, the numbers are robust, and even examined and used by clinicians and researchers as a tool for better understanding the disease.
When registering for this support group, you will first fill out a profile. To make your experience more personal, you can choose to include a picture and share your MS story in a blurb that is visible to others.
Frequently Asked Questions
MS support groups are communities of people who come together, either virtually or in-person, to connect and share their experiences and struggles with living with MS. The mission of these communities may vary slightly, but it generally entails sharing resources and coping strategies and providing emotional support and encouragement.
Living with a chronic, unpredictable disease like MS can be isolating. Participating in a support group is one way to see that you are not alone in your experiences and the challenges you face. Besides a social connection, a support group can be a pathway for you to learn more about MS. In addition, support groups can be a source of inspiration. Many people find comfort in helping others and sharing their unique MS struggles. Deciding whether or not to join a support group is a personal choice—and keep in mind, it is not something that is permanent by any means. You can join, leave, and rejoin as you like.
MS support groups are generally structured around one or more common goals—for example, to combat isolation, help form friendships, or provide MS education.
Online and in-person support groups usually have a leader or moderator to help guide the community and keep them on track with the goal or topic in mind (if applicable). With online groups, the moderator may read messages beforehand to ensure they are appropriate and safe.
The vast majority of MS support groups are free, as are their provided educational resources. Some of the organizations do engage in various fundraising activities to support their cause. Therefore, by joining a support group or subscribing to its website, you may receive emails about participating in a fundraising activity or making a monetary donation to the site, so that they can continue to provide resources for free to those with MS.
Ghasemi N, Razavi S, Nikzad E. Multiple sclerosis: Pathogenesis, symptoms, diagnoses and cell-based therapy . Cell J . 2017;19(1):1-10. doi:10.22074/cellj.2016.4867
Steadman J, Pretorius C. The impact of an online Facebook support group for people with multiple sclerosis on non-active users . Afr J Disabil .2014;3(1):132. doi:10.4102/ajod.v3i1.132
Agency for Healthcare Research and Quality. PatientsLikeMe .
By Colleen Doherty, MD Dr. Doherty is a board-certified internist and writer living with multiple sclerosis. She is based in Chicago.

Multiple Sclerosis
What is multiple sclerosis.
Multiple sclerosis (MS) is the most common disabling neurological disease of young adults with symptom onset generally occurring between the ages of 20 to 40 years.
In MS, the immune system cells that normally protect us from viruses, bacteria, and unhealthy cells mistakenly attack myelin in the central nervous system (brain, optic nerves, and spinal cord). Myelin is a substance that makes up the protective sheath (myelin sheath) that coats nerve fibers (axons).
MS is a chronic disease that affects people differently. A small number of people with MS will have a mild course with little to no disability, whereas others will have a steadily worsening disease that leads to increased disability over time. Most people with MS, however, will have short periods of symptoms followed by long stretches of relative quiescence (inactivity or dormancy), with partial or full recovery. The disease is rarely fatal and most people with MS have a normal life expectancy.
Myelin and the immune system
MS attacks axons in the central nervous system protected by myelin, which are commonly called white matter. MS also damages the nerve cell bodies, which are found in the brain's gray matter, as well as the axons themselves in the brain, spinal cord, and optic nerves that transmit visual information from the eye to the brain. As the disease progresses, the outermost layer of the brain, called the cerebral cortex, shrinks in a process known as cortical atrophy.
The term multiple sclerosis refers to the distinctive areas of scar tissue (sclerosis—also called plaques or lesions) that result from the attack on myelin by the immune system. These plaques are visible using magnetic resonance imaging (MRI). Plaques can be as small as a pinhead or as large as a golf ball.
The symptoms of MS depend on the severity of the inflammatory reaction as well as the location and extent of the plaques, which primarily appear in the brain stem, cerebellum (involved with balance and coordination of movement, among other functions), spinal cord, optic nerves, and the white matter around the brain ventricles (fluid-filled cavaties).
Signs and symptoms of MS
The natural course of MS is different for each person, which makes it difficult to predict. The onset and duration of MS symptoms usually depend on the specific type but may begin over a few days and go away quickly or develop more slowly and gradually over many years.
There are four main types of MS, named according to the progression of symptoms over time:
- Relapsing-remitting MS—Symptoms in this type come in the form of attacks. In between attacks, people recover or return to their usual level of disability. When symptoms occur in this form of MS, it is called an attack, a relapse, or exacerbation. The periods of disease inactivity between MS attacks are referred to as remission. Weeks, months, or even years may pass before another attack occurs, followed again by a period of inactivity. Most people with MS are initially diagnosed with this form of the disease.
- Secondary-progressive MS—People with this form of MS usually have had a previous history of MS attacks but then start to develop gradual and steady symptoms and deterioration in their function over time. Most individuals with severe relapsing-remitting MS may go on to develop secondary progressive MS if they are untreated.
- Primary-progressive MS—This type of MS is less common and is characterized by progressively worsening symptoms from the beginning with no noticeable relapses or exacerbations of the disease, although there may be temporary or minor relief from symptoms.
- Progressive-relapsing MS—The rarest form of MS is characterized by a steady worsening of symptoms from the beginning with acute relapses that can occur over time during the disease course.
There are some rare and unusual variants of MS, such as:
- Marburg variant MS (also known as malignant MS) causes swift and relentless symptoms and decline in function, and may result in significant disability or even death shortly after disease onset.
- Balo's concentric sclerosis causes concentric rings of myelin destruction that can be seen on an MRI and is another variant type of MS that can progress rapidly.
Early MS symptoms often include:
- Vision problems such as blurred or double vision, or optic neuritis, which causes pain with eye movement and rapid vision loss
- Muscle weakness, often in the hands and legs, and muscle stiffness accompanied by painful muscle spasms
- Tingling, numbness, or pain in the arms, legs, trunk, or face
- Clumsiness, especially difficulty staying balanced when walking
- Bladder control problems
- Intermittent or constant dizziness
MS may also cause later symptoms, such as:
- Mental or physical fatigue which accompanies the early symptoms during an attack
- Mood changes such as depression or difficulty with emotional expression or control
- Cognitive dysfunction—problems concentrating, multitasking, thinking, learning, or difficulties with memory or judgment
Muscle weakness, stiffness, and spasms may be severe enough to affect walking or standing. In some cases, MS leads to partial or complete paralysis and the use of a wheelchair is not uncommon, particularly in individuals who are untreated or have advanced disease. Many people with MS find that weakness and fatigue are worse when they have a fever or when they are exposed to heat. MS exacerbations may occur following common infections.
Pain is rarely the first sign of MS but pain often occurs with optic neuritis and trigeminal neuralgia, a disorder that affects one of the nerves that provides sensation to different parts of the face. Painful limb spasms and sharp pain shooting down the legs or around the abdomen can also be symptoms of MS.
Conditions associated with MS
- Transverse myelitis (an inflammation of the spinal cord) may develop in those with MS. Transverse myelitis can affect spinal cord function over several hours to several weeks before partial or complete recovery. It usually begins as a sudden onset of lower back pain, muscle weakness, abnormal sensations in the toes and feet, or difficulties with bladder control or bowel movements. This can rapidly progress to more severe symptoms, including arm and/or leg paralysis. In most cases, people recover at least some function within the first 12 weeks after an attack begins.
- Neuromyelitis optica is a disorder associated with transverse myelitis as well as optic nerve inflammation (also known as optic neuritis). People with this disorder usually have abnormal antibodies (proteins that normally target viruses and bacteria) against a specific channel in optic nerves, the brain stem or spinal cord, called the aquaporin-4 channel. These individuals respond to certain treatments, which are different than those commonly used to treat MS.
- Trigeminal neuralgia is a chronic pain condition that causes sporadic, sudden burning or shock-like facial pain. The condition is more common in young adults with MS and is caused by lesions in the brain stem, the part of the brain that controls facial sensation.
Who is more likely to get multiple sclerosis?
Females are more frequently affected than males. Researchers are looking at several possible explanations for why the immune system attacks central nervous system myelin, including:
- Fighting an infectious agent (e.g., a virus) that has components that mimic components of the brain (molecular mimicry)
- Destroying brain cells because they are unhealthy
- Mistakenly identifying normal brain cells as foreign
There is also something known as the blood-brain barrier, which separates the brain and spinal cord from the immune system. If there is a break in this barrier, it exposes the brain to the immune system. When this happens, the immune system may misinterpret structures in the brain, such as myelin, as “foreign.”
Research shows that genetic vulnerabilities combined with environmental factors may cause MS.
Genetic susceptibility
MS itself is not inherited, but susceptibility to MS may be inherited. Studies show that some individuals with MS have one or more family member or relative who also have MS.
Current research suggests that dozens of genes and possibly hundreds of variations in the genetic code (gene variants) combine to create vulnerability to MS. Some of these genes have been identified, and most are associated with functions of the immune system. Many of the known genes are similar to those that have been identified in people with other autoimmune diseases as type 1 diabetes, rheumatoid arthritis, or lupus.
Infectious factors and viruses
Several viruses have been found in people with MS, but the virus most consistently linked to the development of MS is the Epstein-Barr virus (EBV) which causes infectious mononucleosis.
Only about five percent of the population has not been infected by EBV. These individuals are at a lower risk for developing MS than those who have been infected. People who were infected with EBV in adolescence or adulthood, and who therefore develop an exaggerated immune response to EBV, are at a significantly higher risk for developing MS than those who were infected in early childhood. This suggests that it may be the type of immune response to EBV that may lead to MS, rather than EBV infection itself. However, there is still no proof that EBV causes MS and the mechanisms that underlie this process are poorly understood.
Environmental factors
Several studies indicate that people who spend more time in the sun and those with relatively higher levels of vitamin D are less likely to develop MS or have a less severe course of disease and fewer relapses. Bright sunlight helps human skin produce vitamin D. Researchers believe that vitamin D may help regulate the immune system in ways that reduce the risk of MS or autoimmunity in general. People from regions near the equator, where there is a great deal of bright sunlight, generally have a much lower risk of MS than people from temperate areas such as the U.S. and Canada.
Studies have found that people who smoke are more likely to develop MS and have a more aggressive disease course. Indeed, people who smoke tend to have more brain lesions and brain shrinkage than non-smokers.
How is multiple sclerosis diagnosed and treated?
Diagnosing MS
There is no single test used to diagnose MS. The disease is confirmed when symptoms and signs develop and are related to different parts of the nervous system at more than one interval and after other alternative diagnoses have been excluded.
Doctors use different tests to rule out or confirm the diagnosis. In addition to a complete medical history, physical examination, and a detailed neurological examination, a doctor may recommend:
- MRI scans of the brain and spinal cord to look for the characteristic lesions of MS. A special dye or contrast agent may be injected into a vein to enhance brain images of the active MS lesions.
- Lumbar puncture (sometimes called a spinal tap) to obtain a sample of cerebrospinal fluid and examine it for proteins and inflammatory cells associated with the disease. Spinal tap analysis also can rule out diseases that may look like MS.
- Evoked potential tests, which use electrodes placed on the skin and painless electric signals to measure how quickly and accurately the nervous system responds to stimulation.
Treating MS
There is no cure for MS, but there are treatments that can reduce the number and severity of relapses and delay the long-term disability progression of the disease.
- Corticosteroids, such as intravenous (infused into a vein) methylprednisolone, are prescribed over the course of three to five days. Intravenous steroids quickly and potently suppress the immune system and reduce inflammation. They may be followed by a tapered dose of oral corticosteroids. Clinical trials have shown that these drugs hasten recovery from MS attacks, but do not alter the long-term outcome of the disease.
- Plasma exchange (plasmapheresis) can treat severe flare-ups in people with relapsing forms of MS who do not have a good response to methylprednisolone. Plasma exchange involves taking blood out of the body and removing components in the blood's plasma that are thought to be harmful. The rest of the blood, plus replacement plasma, is then transfused back into the body. This treatment has not been shown to be effective for secondary progressive or chronic progressive MS.
Disease-modifying treatments
Current therapies approved by the U.S. Food and Drug Administration (FDA) for MS are designed to modulate or suppress the inflammatory reactions of the disease. They are most effective for relapsing-remitting MS at early stages of the disease.
Injectable medications include:
- Beta interferon drugs are among the most common medications used to treat MS. Interferons are signaling molecules that regulate immune cells. Potential side effects of these drugs include flu-like symptoms (which usually fade with continued therapy), depression, or elevation of liver enzymes. Some individuals will notice a decrease in the effectiveness of the drugs after 18 to 24 months of treatment. If flare-ups occur or symptoms worsen, doctors may switch treatment to alternative drugs.
- Glatiramer acetate changes the balance of immune cells in the body, but how it works is not entirely clear. Side effects are usually mild and consist of local injection site reactions or swelling.
Infusion treatments include:
- Natalizumab is administered intravenously once a month. It works by preventing cells of the immune system from entering the brain and spinal cord. It is very effective but is associated with an increased risk of a serious and potentially fatal viral infection of the brain called progressive multifocal leukoencephalopathy (PML). Natalizumab is generally recommended only for individuals who have not responded well to or who are unable to tolerate other first-line therapies.
- Ocrelizumab is administered intravenously every six months and treats adults with relapsing or primary progressive forms of MS. It is the only FDA-approved disease-modifying therapy for primary-progressive MS. The drug targets the circulating immune cells that produce antibodies, which also play a role in the formation of MS lesions. Side effects include infusion-related reactions and increased risk of infections. Ocrelizumab may increase the risk of cancer as well.
- Alemtuzumab is administered for five consecutive days followed by three days of infusions one year later. It targets proteins on the surface of immune cells. Because this drug increases the risk of autoimmune disorders it is recommended for those who have had inadequate responses to two or more MS therapies.
- Mitoxantrone, which is administered intravenously four times a year, has been approved for especially severe forms of relapsing-remitting and secondary progressive MS. Side effects include the development of certain types of blood cancers in up to one percent of those with MS, as well as with heart damage. This drug should be considered as a last resort to treat people with a form of MS that leads to rapid loss of function and for whom other treatments did not work.
Oral treatments include:
- Fingolimod is a once-daily medication that reduces the MS relapse rate in adults and children. It is the first FDA-approved drug to treat MS in adolescents and children ages 10 years and older. The drug prevents white blood cells called lymphocytes from leaving the lymph nodes and entering the blood, brain, and spinal cord. Fingolimod may result in a slow heart rate and eye problems when first taken. Fingolimod can also increase the risk of infections, such as herpes virus infections, or in rare cases be associated with PML.
- Dimethyl fumarate is a twice-daily medication used to treat relapsing forms of MS. Its exact mechanism of action is not currently known. Side effects of dimethyl fumarate are flushing, diarrhea, nausea, and lowered white blood cell count.
- Teriflunomide is a once-daily medication that reduces the rate of proliferation of activated immune cells. Teriflunomide side effects can include nausea, diarrhea, liver damage, and hair loss.
- Cladribine is administered as two courses of tablets about one year apart. Cladribine targets certain types of white blood cells that drive immune attacks in MS. The drug may increase the risk of developing cancer and should be considered for individuals who have not responded well to other MS treatments.
- Diroximel fumarate is a twice-daily drug similar to dimethyl fumarate (brand name Tecfidera) but with fewer gastrointestinal side effects. Scientists suspect these drugs, which have been approved to treat secondary progressive MS, reduce damage to the brain and spinal cord by making the immune response less inflammatory, although their exact mechanism of action is poorly understood.
- Siponimod tablets (Mayzent) is taken orally and has a similar mechanism of action to fingolimod. Siponimod has been approved by the FDA to treat secondary-progressive MS.
Clinical trials have shown that cladribine, diroximel fumarate, and dimethyl fumarate decrease the number of relapses, delay the progress of physical disability, and slow the development of brain lesions.
Managing MS symptoms
MS causes a variety of symptoms that can interfere with daily activities but can usually be treated or managed. Many of these issues are best treated by neurologists who have advanced training in the treatment of MS and who can prescribe specific medications to treat these problems.
Eye and vision problems are common in people with MS but rarely result in permanent blindness. Inflammation of the optic nerve (optic neuritis) or damage to the myelin that covers the nerve fibers in the visual system can cause blurred or grayed vision, temporary blindness in one eye, loss of normal color vision, depth perception, or loss of vision in parts of the visual field. Uncontrolled horizontal or vertical eye movements (nystagmus), “jumping vision" (opsoclonus), and double vision (diplopia) are common in people with MS. Intravenous steroid medications, special eyeglasses, and periodically resting the eyes may be helpful.
Muscle weakness and spasticity is common in MS. Mild spasticity can be managed by stretching and exercising muscles using water therapy, yoga, or physical therapy. Medications such as gabapentin or baclofen can reduce spasticity. It is very important that people with MS stay physically active because physical inactivity can contribute to worsening stiffness, weakness, pain, fatigue, and other symptoms.
Tremor, or uncontrollable shaking, develops in some people with MS. Assistive devices and weights attached to utensils or even limbs are sometimes helpful for people with tremor. Deep brain stimulation and drugs, such as clonazepam, may also be useful.
Problems with walking and balance occur in many people with MS. The most common walking problem is ataxia—unsteady, uncoordinated movements—due to damage to the areas of the brain that coordinate muscle balance. People with severe ataxia generally benefit from the use of a cane, walker, or other assistive device. Physical therapy also can reduce walking problems. The FDA has approved the drug dalfampridine to improve walking speed in people with MS.
Fatigue is a common symptom of MS and may be both physical (tiredness in the arms or legs) and cognitive (slowed processing speed or mental exhaustion). Daily physical activity programs of mild to moderate intensity can significantly reduce fatigue, although people should avoid excessive physical activity and minimize exposure to hot weather conditions or ambient temperature. Other drugs that may reduce fatigue include amantadine, methylphenidate, and modafinil. Occupational therapy can help people learn how to walk using an assistive device or in a way that saves physical energy. Stress management programs, relaxation training, membership in an MS support group, or individual psychotherapy may help some people.
Pain from MS can be felt in different parts of the body. Trigeminal neuralgia (facial pain) is treated with anticonvulsant or antispasmodic drugs, or less commonly, painkillers. Central pain, a syndrome caused by damage to the brain and/or spinal cord, can be treated with gabapentin and nortriptyline. Treatments for chronic back or other musculoskeletal pain may include heat, massage, ultrasound, and physical therapy.
Problems with bladder control and constipation may include urinary frequency, urgency, or the loss of bladder control. A small number of individuals retain large amounts of urine. Medical treatments are available for bladder-related problems. Constipation is also common and can be treated with a high-fiber diet, laxatives, and stool softeners.
Sexual dysfunction can result from damage to nerves running through the spinal cord. Sexual problems may also stem from MS symptoms such as fatigue, cramped or spastic muscles, and psychological factors. Some of these problems can be corrected with medications. Psychological counseling may be helpful.
Clinical depression is frequent among people with MS. MS may cause depression as part of the disease process and chemical imbalance in the brain. Depression can intensify symptoms of fatigue, pain, and sexual dysfunction. It is most often treated with cognitive behavioral therapy, and selective serotonin reuptake inhibitor (SSRI) antidepressant medications, which are less likely than other antidepressant medications to cause fatigue.
Inappropriate and involuntary expressions of laughter, crying, or anger—symptoms of a condition called pseudobulbar affect—sometimes are associated with MS. These expressions are often incongruent with mood; for example, people with MS may cry when they are actually happy or laugh when they are not especially happy. The combination treatment of the drugs dextromethorphan and quinidine can treat pseudobulbar affect, as can other drugs such as amitriptyline or citalopram.
Cognitive impairment—a decline in the ability to think quickly and clearly and to remember easily—affects up to 75 percent of people with MS. These cognitive changes may appear at the same time as the physical symptoms or they may develop gradually over time. Drugs such as donepezil may be helpful in some cases.
Complementary and alternative therapies
Many people with MS benefit from complementary or alternative approaches such as acupuncture, aromatherapy, ayurvedic medicine, touch and energy therapies, physical movement disciplines such as yoga and tai chi, herbal supplements, and biofeedback.
Because of the risk of interactions between alternative and conventional therapies, people with MS should discuss all the therapies they are using with their doctor, especially herbal supplements. Herbal supplements have biologically active ingredients that could have harmful effects on their own or interact harmfully with other medications.
What are the latest updates on multiple sclerosis?
The National Institute of Neurological Disorders and Stroke ( NINDS ), a component of the National Institutes of Health ( NIH ), is the leading federal funder of research on the brain and nervous system, including research on MS.
In addition to NINDS , other NIH Institutes—including the National Institute of Allergy and Infectious Diseases ( NIAID )—fund research on multiple sclerosis. Find more information on NIH research efforts through NIH RePORTER , a searchable database of current and past research projects supported by NIH and other federal agencies. RePORTER also includes links to publications and patents citing support from these projects.
Although researchers have not been able to identify the cause of MS with any certainty, there has been excellent progress in other areas of MS research—especially in the development of new treatments to prevent exacerbations of the disease. New discoveries are constantly changing MS treatment options and helping to reduce MS-related disability.
Research projects conducted by NINDS scientists or through NIH grants to universities and other sites across the U.S. cover a wide range of topics such as comorbidities, mechanisms of cognitive impairment, blood-brain barrier breakdown in MS, the role of sleep and circadian rhythms, rehabilitation strategies, and telehealth. Other topics include:
- Biomarkers to accurately diagnose MS and monitor disease progression, including blood and imaging tests (e.g., MRI)
- Genetic and environmental risk factors for MS, such as low Vitamin D or the Epstein-Barr virus
- The role of the gut microbiome and diet in MS
- Mechanisms that underlie gender differences in the incidence and presentation of MS
- MS risk factors and disease course in African American and Hispanic populations, and disparities in care
- The role of the immune system in MS, including its function in the central nervous system (CNS)
- The role and crosstalk of various cell types in the CNS with relation to MS
- Basic functions of myelination, demyelilnation, and axonal degeneration, and strategies to overcome axonal and myelin loss
Scientists sponsored by NIAID are testing an experimental stem cell treatment titled, autologous hematopoietic stem cell transplantation (AHSCT), against the best available biologic therapies for severe forms of relapsing MS.
Investigators in the clinical trial BEAT-MS (BEst Available Therapy versus autologous hematopoietic stem cell transplant for Multiple Sclerosis) are removing some immune cells and then infusing some of the person's own blood-forming stem cells to reset the immune system so it no longer attacks the CNS.
Genetic research funded by NINDS is exploring the roles of "susceptibility genes"—genes that are associated with an increased risk for MS. Several candidate genes have been identified and researchers are studying their function in the nervous system to discover how they may lead to the development of MS.
Other studies aim to develop better neuroimaging tools, such as more powerful MRI methods, to diagnose MS, track disease progression, and assess treatments. NINDS scientists are collecting MRIs of the brain and spinal cord and scans of the retina, along with other clinical and biological data, from more than 100 individuals with MS and 50 individuals without the disease over a period of years to observe changes in the course of MS. Investigators are using MRI to study the natural history of MS and to help define the mechanism of action and cause of side effects of disease modifying therapies.
Intramural research programs on MS
NINDS and other NIH Institutes have a very active MS intramural research program among scientists working at NIH. Together, they have:
- Established and continue to develop MRI as a critical tool for examining the natural course of the disease in humans, monitoring disease progression, assessing effects of treatments in clinical trials, and understanding MS biology
- Played an important role in understanding why some patients develop a rare and potentially fatal brain infection (progressive multifocal leukoencephalopathy) when taking potent MS drugs, and they are developing new treatments for this infection
- Unraveled mechanisms by which viruses, especially the Epstein-Barr virus, contribute to the development of MS
- Conducted next-generation treatment trials targeting specific mechanisms of disease progression, using advanced MRI and fluid biomarkers as outcome measures
- Developed the first MRI method to visualize the lymph vessels surrounding the brain, which play a critical role in neuro-immune communication
Translational research
NIH supports translational studies to develop therapies that will stop or reverse the course of the disease, focusing on pathways that modify immune system function, repair damaged myelin, or protect neurons from damage. Researchers are also developing animal models of MS to more accurately predict drug response in human disease. However, current animal models share some of the disease mechanisms and symptoms of MS but do not fully mimic the disease, especially in its clinically progressive phase.
Focus on progressive MS therapies
Scientists continue to study the biology and mechanisms of relapsing-remitting MS while increasing efforts to stop or prevent the steady decline in function that occurs in progressive MS. In the MS-SPRINT trial, the NINDS NeuroNEXT clinical trials network tested the drug ibudilast as a potential neuroprotective drug for progressive MS and showed that the drug slowed the rate of brain shrinkage as compared to a placebo. NINDS Intramural scientists are conducting proof-of-concept clinical trials to address a key driver of clinical progression called the “slowly expanding lesion.”
Focus on biomarkers
As part of a larger effort to develop and validate effective biomarkers (signs that may indicate risk of a disease or be used to monitor its progression) for neurological disease, NINDS is supporting two definitive multicenter MS studies:
- The Central Vein Sign in MS (CAVS-MS) study, which is testing whether a rapid MRI approach designed by NINDS Intramural scientists can use the detection of a central vein passing through brain plaques to differentiate MS from other common neurological disorders that can mimic MS. The goal is to develop a reliable imaging test for MS in order to achieve rapid yet accurate diagnosis and reduce misdiagnosis, which may affect up to 20 percent of people currently diagnosed with MS.
- A study to test whether a simple new blood test that measures small amounts of neuron-derived proteins (neurofilaments) can be used to predict the severity of disease and help determine whether MS drugs are working to protect brain tissues.
How can I or my loved one help improve care for people with multiple sclerosis?
Consider participating in a clinical trial so clinicians and scientists can learn more about MS and related disorders. Clinical research uses human volunteers to help researchers learn more about a disorder and perhaps find better ways to safely detect, treat, or prevent disease.
All types of volunteers are needed— those who are healthy or may have an illness or disease— of all different ages, sexes, races, and ethnicities to ensure that study results apply to as many people as possible, and that treatments will be safe and effective for everyone who will use them.
For information about participating in clinical research visit NIH Clinical Research Trials and You . Learn about clinical trials currently looking for people with MS at Clinicaltrials.gov .
Where can I find more information about multiple sclerosis? Information may be available from the following organizations and resources: Accelerated Cure Project for Multiple Sclerosis Phone: 781-487-0008 Autoimmune Association Phone: 586-776-3900 Multiple Sclerosis Association of America (MSAA) Phone: 856-488-4500 or 800-532-7667 Multiple Sclerosis Foundation (MS Focus) Phone: 954-776-6805 or 888 673-6287 Myelin Repair Foundation (MRF) Phone: 408-871-2410 National Ataxia Foundation (NAF) Phone: 763-553-0020 National Multiple Sclerosis Society Phone: 800-344-4867 National Organization for Rare Disorders (NORD) Phone: 203-744-0100 National Rehabilitation Information Center (NARIC) Phone: 301-459-5900 or 800-346-2742; 301-459-5984 Paralyzed Veterans of America Phone: 202-872-1300 or 800-555-9140
- Patient Care & Health Information
- Diseases & Conditions
- Multiple sclerosis
- What is multiple sclerosis? An expert explains
Learn more from neurologist Oliver Tobin, M.B., B.Ch., B.A.O., Ph.D.
I'm Dr. Oliver Tobin, a neurologist specializing in multiple sclerosis at Mayo Clinic. In this video, we'll be covering the basics of multiple sclerosis. What is it? Who gets it? The symptoms, diagnosis, and treatment. Whether you're looking for answers about your own health or that of someone you love, we're here to provide you with the best information available. Multiple sclerosis is a disorder in which the body's immune system attacks the protective covering of the nerve cells in the brain, optic nerve and spinal cord, called the myelin sheath. And this sheath is often compared to the insulation on an electrical wire. When that covering is damaged, it exposes the actual nerve fiber, which can slow or block the signals being transmitted within it. The nerve fibers themselves might also be damaged. The body can repair damage to the myelin sheath, but it's not perfect. The resulting damage leaves lesions or scars, and this is where the name comes from: multiple sclerosis, multiple scars. Now everyone loses brain cells and spinal cord cells as they get older. But if part of the brain or spinal cord has been damaged by MS, the nerve cells in that area will die off faster than the areas around it that are normal. This happens very slowly, usually over decades and typically shows up as gradual walking difficulty happening over several years. When you read about multiple sclerosis, you may hear about different types -- the most frequent being relapsing-remitting multiple sclerosis. And this is characterized by attacks, or relapses.
We don't know what causes MS, but there are certain factors that may increase the risk or trigger its onset. So while MS can occur at any age, it mostly makes its first appearance in people between the ages of 20 and 40. Low levels of vitamin D and low exposure to sunlight, which enables our body to make vitamin D, are associated with an increased risk of developing MS. As people who have MS who have low vitamin D tend to have more severe disease. So people who are overweight are more likely to develop MS and people who have MS and are overweight tend to have more severe disease and a faster onset of progression. People who have MS and who smoke tend to have more relapses, worse progressive disease, and worse cognitive symptoms. Women are up to three times as likely as men to have relapsing-remitting MS. The risk for MS in the general population is about 0.5%. If a parent or sibling has MS, your risk is about twice that or about 1%. Certain infections are also important. A variety of viruses have been linked to MS, including Epstein-Barr virus, which causes mono. Northern and southern latitudes have a higher prevalence, including Canada, the northern US, New Zealand, southeastern Australia, and Europe. White people, especially of northern European descent, are at the highest risk. People of Asian, African, and Native American ancestry have the lowest risk. A slightly increased risk is seen if a patient already has autoimmune thyroid disease, pernicious anemia, psoriasis, type 1 diabetes, or inflammatory bowel disease.
Symptoms of a relapse usually come on over 24 to 48 hours, last for a few days to a few weeks and then improve in the region of 80 to a 100 percent. Those symptoms include loss of vision in an eye, loss of power in an arm or leg or a rising sense of numbness in the legs. Other common symptoms associated with MS include spasms, fatigue, depression, incontinence issues, sexual dysfunction, and walking difficulties.
There's currently no single test to make a diagnosis of MS. However, there are four key features which help to secure the diagnosis. Firstly, are there typical symptoms of multiple sclerosis? Again, those are loss of vision in an eye, loss of power in an arm or leg, or sensory disturbance in an arm or leg lasting for more than 24 hours. Secondly, do you have any physical examination findings consistent with MS? Next, is the MRI of your brain or spine consistent with MS? Now here it's important to note that 95 percent of people over the age of 40 have an abnormal brain MRI, just the same as many of us have wrinkles on our skin. Lastly, are the results of the spinal fluid analysis consistent with MS? Your doctor may recommend blood tests to check for other diseases that share the same symptoms. They may also recommend an OCT test or optical coherence tomography. This is a short scan of the thickness of the layers at the back of your eye.
So the best thing to do when living with MS is to find a trusted interdisciplinary medical team that can help you monitor and manage your health. Having a multidisciplinary team is essential for addressing the individual symptoms that you're experiencing. If you have an MS attack or relapse, your doctor may prescribe you corticosteroids to reduce or improve your symptoms. And if your attack symptoms do not respond to steroids, another option is plasmapheresis or plasma exchange, which is a treatment similar to dialysis. About 50 percent of people who do not respond to steroids have a significant improvement with a short course of plasma exchange. There are over 20 medications currently approved for prevention of MS attacks and prevention of new MRI lesions.
As learning to function with MS can be challenging, there are medical experts ready to work with you to help you manage it, so you can still live a full life. Consulting with a physiatrist, physical or occupational therapist can help you deal with physical difficulties. Physical activity is strongly recommended for all people with MS. Mental health is also an important consideration. So keeping up personal connections with friends and family and trying to stay involved with your hobbies is important. But also be kind to yourself and realistic about what you're up for. This can change from day to day, so it's okay to give yourself permission if something seems like too much or if you need to cancel plans. You may also find support groups helpful to connect with people who understand what you are going through and discuss your feelings and concerns with a doctor or a counselor. Meanwhile, scientists are hard at work, expanding our understanding of this disease and developing new treatments and medications which are ever more effective. If you want to learn more, watch more of our videos or visit mayoclinic.org. We wish you well.
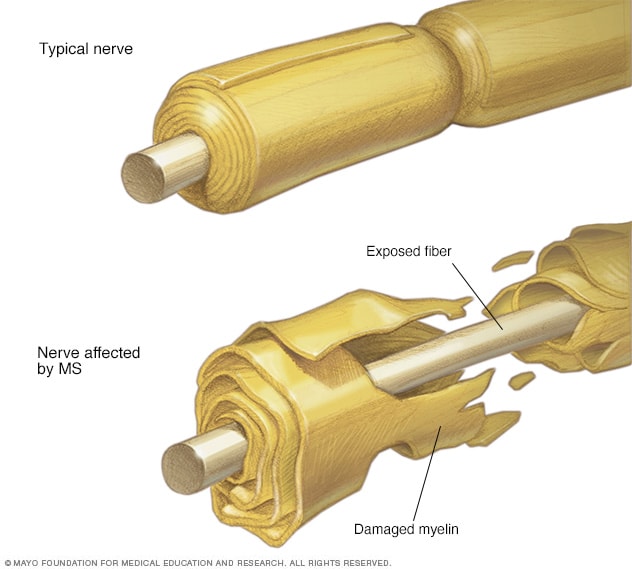
In multiple sclerosis, the protective coating on the nerve fibers (myelin) is damaged and may eventually be destroyed. Depending on where the nerve damage occurs, MS can affect vision, sensation, coordination, movement, and bladder or bowel control.
Multiple sclerosis (MS) is a potentially disabling disease of the brain and spinal cord (central nervous system).
In MS , the immune system attacks the protective sheath (myelin) that covers nerve fibers and causes communication problems between your brain and the rest of your body. Eventually, the disease can cause permanent damage or deterioration of the nerve fibers.
Signs and symptoms of MS vary widely between patients and depend on the location and severity of nerve fiber damage in the central nevous system. Some people with severe MS may lose the ability to walk independently or ambulate at all. Other individuals may experience long periods of remission without any new symptoms depending on the type of MS they have.
There's no cure for multiple sclerosis. However, there are treatments to help speed the recovery from attacks, modify the course of the disease and manage symptoms.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
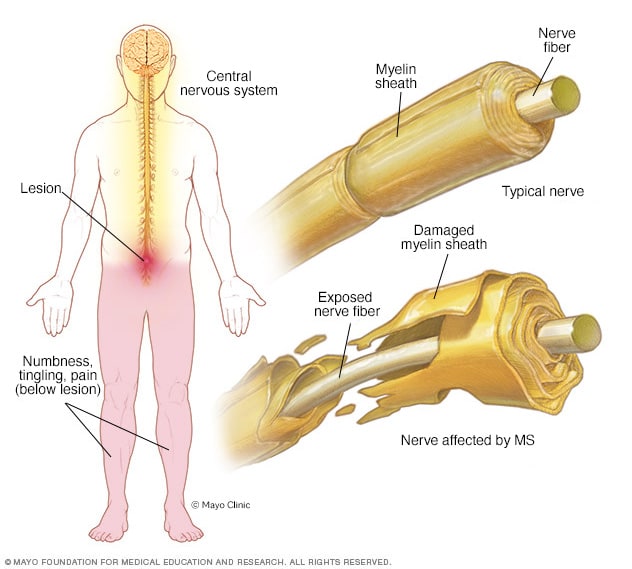
- Myelin damage and the nervous system
In multiple sclerosis, the protective coating on nerve fibers (myelin) in the central nervous system is damaged. This creates a lesion that, depending on the location in the central nervous system, may cause symptoms such as numbness, pain or tingling in parts of the body.
Multiple sclerosis signs and symptoms may differ greatly from person to person and over the course of the disease depending on the location of affected nerve fibers.
Common symptoms include:
- Numbness or weakness in one or more limbs that typically occurs on one side of your body at a time
- Electric-shock sensations that occur with certain neck movements, especially bending the neck forward (Lhermitte sign)
- Lack of coordination
- Unsteady gait or inability to walk
- Partial or complete loss of vision, usually in one eye at a time, often with pain during eye movement
- Prolonged double vision
- Blurry vision
- Problems with sexual, bowel and bladder function
- Slurred speech
- Cognitive problems
- Mood disturbances
When to see a doctor
See a doctor if you experience any of the above symptoms for unknown reasons.
Disease course
Most people with MS have a relapsing-remitting disease course. They experience periods of new symptoms or relapses that develop over days or weeks and usually improve partially or completely. These relapses are followed by quiet periods of disease remission that can last months or even years.
Small increases in body temperature can temporarily worsen signs and symptoms of MS . These aren't considered true disease relapses but pseudorelapses.
At least 20% to 40% of those with relapsing-remitting MS can eventually develop a steady progression of symptoms, with or without periods of remission, within 10 to 20 years from disease onset. This is known as secondary-progressive MS .
The worsening of symptoms usually includes problems with mobility and gait. The rate of disease progression varies greatly among people with secondary-progressive MS .
Some people with MS experience a gradual onset and steady progression of signs and symptoms without any relapses, known as primary-progressive MS .
More Information
Multiple sclerosis care at Mayo Clinic
- Multiple sclerosis: Can it cause seizures?
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
The cause of multiple sclerosis is unknown. It's considered an immune mediated disease in which the body's immune system attacks its own tissues. In the case of MS , this immune system malfunction destroys the fatty substance that coats and protects nerve fibers in the brain and spinal cord (myelin).
Myelin can be compared to the insulation coating on electrical wires. When the protective myelin is damaged and the nerve fiber is exposed, the messages that travel along that nerve fiber may be slowed or blocked.
It isn't clear why MS develops in some people and not others. A combination of genetics and environmental factors appears to be responsible.
Risk factors
These factors may increase your risk of developing multiple sclerosis:
- Age. MS can occur at any age, but onset usually occurs around 20 and 40 years of age. However, younger and older people can be affected.
- Sex. Women are more than 2 to 3 times as likely as men are to have relapsing-remitting MS .
- Family history. If one of your parents or siblings has had MS , you are at higher risk of developing the disease.
- Certain infections. A variety of viruses have been linked to MS , including Epstein-Barr, the virus that causes infectious mononucleosis.
- Race. White people, particularly those of Northern European descent, are at highest risk of developing MS . People of Asian, African or Native American descent have the lowest risk. A recent study suggests that the number of Black and Hispanic young adults with multiple sclerosis may be greater than previously thought.
- Climate. MS is far more common in countries with temperate climates, including Canada, the northern United States, New Zealand, southeastern Australia and Europe. Your birth month may also affect the chances of developing multiple sclerosis, since exposure to the sun when a mother is pregnant seems to decrease later development of multiple sclerosis in these children.
- Vitamin D. Having low levels of vitamin D and low exposure to sunlight is associated with a greater risk of MS .
- Your genes. A gene on chromosome 6p21 has been found to be associated with multiple sclerosis.
- Obesity. An association with obesity and multiple sclerosis has been found in females. This is especially true for female childhood and adolescent obesity.
- Certain autoimmune diseases. You have a slightly higher risk of developing MS if you have other autoimmune disorders such as thyroid disease, pernicious anemia, psoriasis, type 1 diabetes or inflammatory bowel disease.
- Smoking. Smokers who experience an initial symptom that may signal MS are more likely than nonsmokers to develop a second event that confirms relapsing-remitting MS .
Complications
People with multiple sclerosis may also develop:
- Muscle stiffness or spasms
- Severe weakness or paralysis, typically in the legs
- Problems with bladder, bowel or sexual function
- Cognitive problems, like forgetfulness or word finding difficulties
- Mood problems, such as depression, anxiety or mood swings
- Seizures, though very rare
- What is multiple sclerosis? National Multiple Sclerosis Society. https://www.nationalmssociety.org/What-is-MS. Accessed June 2, 2022.
- Daroff RB, et al. Multiple sclerosis and other inflammatory demyelinating diseases of the central nervous system. In: Bradley's Neurology in Clinical Practice. 7th ed. Philadelphia, Pa.: Elsevier Saunders; 2012. https://www.clinicalkey.com. Accessed June 2, 2022.
- Ferri FF. Multiple sclerosis. In: Ferri's Clinical Advisor 2019. Philadelphia, Pa.: Elsevier; 2019. https://www.clinicalkey.com. Accessed June 2, 2022.
- Olek MJ. Clinical presentation, course, and prognosis of multiple sclerosis in adults. https://www.uptodate.com/contents/search. Accessed June 2, 2022.
- Wingerchuk DM (expert opinion). Mayo Clinic, Phoenix/Scottsdale, Ariz. Jan. 21, 2019.
- Ciccarelli O. Multiple sclerosis in 2018: New therapies and biomarkers. The Lancet. 2019; doi: 10.1016/S14744422 (18)30455-1.
- Keegan BM. Therapeutic decision making in a new drug era in multiple sclerosis. Seminars in Neurology. 2013; doi:10.1055/s0033-1345709.
- Goldman L, et al., eds. Multiple sclerosis and demyelinating conditions of the central nervous system. In: Goldman-Cecil Medicine. 25th ed. Philadelphia, Pa.: Saunders Elsevier; 2016. https://www.clinicalkey.com. Accessed Jun. 2, 2022.
- Lotze TE. Pathogenesis, clinical features, and diagnosis of pediatric multiple sclerosis. https://www.uptodate.com/contents/search. Accessed June 2, 2022.
- Kantarci OH, et al. Novel immunomodulatory approaches for the management of multiple sclerosis. Clinical Pharmacology & Therapeutics. 2014; doi:10.1038/clpt.2013.196.
- Olek MJ. Disease-modifying treatment of relapsing-remitting multiple sclerosis in adults. https://www.uptodate.com/contents/search. Accessed June 2, 2022.
- Olek MJ, et al. Treatment of acute exacerbations of multiple sclerosis in adults. https://www.uptodate.com/contents/search. Accessed June 2, 2022.
- Wingerchuk DM. Multiple sclerosis: Current and emerging disease-modifying therapies and treatment strategies. Mayo Clinic Proceedings. 2014; doi:10.1016/j.mayocp.2013.11.002.
- Pizzorno JE, et al. Multiple sclerosis. In: Textbook of Natural Medicine. 4th ed. St. Louis, Mo.: Churchill Livingstone Elsevier; 2013. https://www.clinicalkey.com. Accessed June 2, 2022.
- Olek MJ, et al. Evaluation and diagnosis of multiple sclerosis in adults. https://www.uptodate.com/contents/search. Accessed June 2, 2022.
- Gaetani L, et al. 2017 revisions of McDonald criteria shorten the time to diagnosis of multiple sclerosis in clinically isolated syndromes. Journal of Neurology. 2018;265:2684.
- http://onlinelibrary.wiley.com/doi/10.1002/ana.22366.
- Olek MJ, et al. Pathogenesis and epidemiology of multiple sclerosis.
- Ingram G, et al. Cannabis and multiple sclerosis. Practical Neurology. 2019; doi:10.1136/practneurol-2018-002137.
- Olek MJ, et al. Symptom management of multiple sclerosis in adults. https://www.uptodate.com/contents/search. Accessed June 2, 2022.
- Yadav Y, et al. Summary of evidence-based guideline: Complementary and alternative medicine in multiple sclerosis. Neurology. 2014; doi: 10.1212/WNL.0000000000000250.
- Nimmagadda R. Allscripts EPSi. Mayo Clinic. April 22, 2022.
- National MS Society. Network of Pediatric MS Centers. https://www.nationalmssociety.org/What-is-MS/Who-Gets-MS/Pediatric-MS/Care-for-Pediatric-MS. Accessed June 2, 2022.
- Rodriguez M. Plasmapheresis in acute episodes of fulminant CNS inflammatory demyelination. Neurology. 1993; doi:10.1212/wnl.43.6.1100.
- Deb C. CD8+ T cells cause disability and axon loss in a mouse model of multiple sclerosis. PLoS One. 2010; doi:101371/journal.pone.0012478.
- FDA approves new drug to treat multiple sclerosis. U.S. Food & Drug Administration. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm549325.htm. Accessed June 1, 2022.
- Keegan BM (expert opinion). Mayo Clinic, Rochester, Minn. January 15, 2019.
- FDA approves new oral drug to treat multiple sclerosis. U.S. Food and Drug Administration. https://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm634469.htm. Accessed June 2, 2022.
- Kappos L, et al. Siponimod versus placebo in secondary progressive multiple sclerosis (EXPAND): A double-blind, randomized, phase 3 study. The Lancet. 2018; doi: 10.1016/S0140-6736(18)30475-6.
- Marin Collazo IV (expert opinion). Mayo Clinic, Rochester, Minn. April 2, 2019.
- AskMayoExpert. Multiple sclerosis. Mayo Clinic; 2020.
- AskMayoExpert. Medication monitoring guidelines. Mayo Clinic; 2020.
- Vumerity. National MS Society. https://www.nationalmssociety.org/Treating-MS/Medications/Vumerity. Accessed March 16, 2020.
- Gianfrancesco M, et al. Obesity during childhood and adolescence increases susceptibility to multiple sclerosis after accounting for established genetic and environmental risk factors. Obesity Research and Clinical Practice. 2014; doi.org/10.1016/j.orcp.2014.01.002.
- Pantavou KG, et al. Season of birth and multiple sclerosis: A systematic review and multivariate meta-analysis. Journal of Neurology. 2020; doi:10.1007/s00415019-09346-5.
- Cifu DX, et al., eds. Multiple sclerosis. In Braddom's Physical Medicine and Rehabilitation. 6th ed. Elsevier; 2021 https://www.clinicalkey.com. Accessed Jun. 2, 2022.
- Langer-Gould AM, et al. Racial and ethnic disparities in multiple sclerosis prevalence. Neurology. 2022; doi:10.1212/WNL.0000000000200151.
- Kasper LH, et al. Immunomodulatory activity of interferon-beta. Annals of Clinical and Translational Neurology. 2014; doi:10.1002/acn3.84.
- Goldschmidt CH, et al. Re-evaluating the use of IFN-B and relapsing multiple sclerosis: Safety, efficacy and place in therapy. Degenerative Neurological and Neuromuscular Disease. 2020; doi:10.2147/DNND.S224912.
- Kieseie BC. The mechanism of action of interferon-B in relapsing multiple sclerosis. Central Nervous System Drugs. 2011; doi:10.1007/s10067-008-0972-3.
- Betaseron. Bayer AG; 1993. www.bayer.com. Accessed Jun. 1, 2022.
- Hauser SL, et al. Ofatumumab versus teriflunomide in multiple sclerosis. The New England Journal of Medicine. 2020; doi:10.1056/NEJMoa1917246.
- Kesimpta. Novartis; 2020. www.novartis.com. Accessed Jun. 1, 2022.
- Marin Collazo V (expert opinion). Mayo Clinic. June 13, 2020.
- Olek MJ. Treatment of progressive multiple sclerosis in adults. https://www.uptodate.com/contents/search. Accessed Jun. 2, 2022.
- Wingerchuk DM, et al. Disease modifying therapies for relapsing multiple sclerosis. British Medical Journal. 2016; doi:10.1136/bmj.i3518.
- Saadeh RS, et al. CSF kappa free light chains: Cutoff validation for diagnosing multiple sclerosis. Mayo Clinic Proceedings. 2022; doi:10.1016/j.mayocp.2021.09.014.
- Goldschmidt C, et al. Advances in the treatment of multiple sclerosis. Neurologic Clinics. 2021; doi:10.1016/j.ncl.2020.09.002.
- Bafiertam. Banner Life Sciences LLC; 2013. www.bannerls.com. Accessed Jun. 1, 2022.
- Baliertam delayed release capsule. Banner Life Sciences LLC; 2013. www.bannerls.com. Accessed Jun. 1, 2022.
- Oral ponesimod versus teriflunomide in relapsing multiple sclerosis (OPTIMUM). ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT02425644. Accessed Jun. 2, 2022.
- Ponvory. Janssen Pharmaceuticals; 2021. www.janssen.com. Accessed Jun. 1, 2022.
- Torke S, et al. Inhibition of Bruton's tyrosine kinase as a novel therapeutic approach in multiple sclerosis. Expert Opinion on Investigational Drugs. 2020.
- Nash RA, et al. High-dose immunosuppressive therapy and autologous hematopoietic cell transplantation for relapsing-remitting multiple sclerosis (HALT-MS): A 3-year interim report. Journal of the American Medical Association Neurology. 2015; doi:10.1001/jamaneurol.2014.3780.
- Reston, et al. Autologous hematopoietic cell transplantation for multiple sclerosis: A systematic review. Multiple Sclerosis. 2011; doi:10,1177/1352458510383609.
- Petrou P, et al. Beneficial effects of autologous mesenchymal stem cell transplantation in active progressive multiple sclerosis. Brain. 2020; doi:10.1093/brain/awaa333.
- Liang J, et al. Allogenic mesenchymal stem cell transplantation in the treatment of multiple sclerosis. Multiple Sclerosis. 2009; doi:10.1177/1352458509104590.
- Wingerchuk DM, et al. Multiple sclerosis: Current and emerging disease-modifying therapies and treatment strategies. Mayo Clinic Proceedings. 2014; doi:101016/j.mayocp.2013.11.002.
- Multiple sclerosis information page. National institute of neurological disorders and stroke. https://www.ninds.nih.gov/Disorders/All-Disorders/Multiple-Sclerosis-Information-Page. Accessed Jun. 2, 2022.
- Sadovnick AD. Genetic background of multiple sclerosis. Autoimmunity Reviews. 2012; doi:10.1016/j.autrev.2011.05.007.
- Acetyl-L-carnitine: Can it relieve MS fatigue?
- Demyelinating disease: What can you do about it?
- Emerging treatments for multiple sclerosis
- Exercise and multiple sclerosis
- Explaining multiple sclerosis
- Infographic: Multiple Sclerosis
- MRI multiple sclerosis lesions
- Multiple sclerosis FAQs
- Physical therapy for multiple sclerosis
- Vitamin D and MS: Any connection?
- Vitamins for MS: Do supplements make a difference?
Associated Procedures
- Lumbar puncture (spinal tap)
News from Mayo Clinic
- Mayo Clinic Q&A podcast: Advances in managing MS July 12, 2022, 02:29 p.m. CDT
Mayo Clinic in Rochester, Minnesota, Mayo Clinic in Phoenix/Scottsdale, Arizona, and Mayo Clinic in Jacksonville, Florida, have been ranked among the best Neurology & Neurosurgery hospitals in the nation for 2023-2024 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Support Groups
Speaking with other people who have MS can be one of the most empowering and helpful things for someone with MS. Sharing stories, feelings, and experiences with people in similar situations is not only therapeutic, but also enlightening, and can often improve emotional health. Support groups frequently provide the best available opportunities to have these interactions, and MS Focus is here to help you find or start a support group in your community.
The MS Focus Independent Support Group Network
Find a support group.
We recognize that each support group is uniquely positioned to serve the needs of its specific members and community. Through the Independent Support Group Network, MS Focus provides guidance, resources, and structure while allowing affiliated support groups to maintain their independence.
The goals of our affiliated support groups are to:
- be educational and encouraging,
- connect you with the latest information about MS,
- give you an opportunity to share stories and experiences with other people who will understand,
- inspire you to discover new strengths and abilities you didn’t know you had,
- help you focus on what you can do,
- share tips and tricks to help you get through even the toughest days, and
- find ways to stay positive in the journey through life with MS.
Anyone with MS can start a support group and become a leader. Healthcare professionals can also start or affiliate their support groups with us. Through the MS Focus Independent Support Group Program, support group leaders receive personalized attention, ongoing support for their meetings, and many types of unique assistance -- including materials for meetings and resources for member recruitment.
If you would like to start or affiliate a support group, or if you have any questions, please contact our Support Groups Department by email at [email protected] or call 888-673-6287.
If you are looking for an existing support group to join, search our national independent support group directory on the upper left side of the page. Please call the leaders for the support group you are interested in to confirm the date, time, and location of their next meeting.
- Search Please fill out this field.
- Manage Your Subscription
- Give a Gift Subscription
- Newsletters
- Sweepstakes
Selma Blair Walks Red Carpet in Heels and Without Her Cane in Glam Fashion Event Appearance
The actress, who’s been in remission from multiple sclerosis, last attended the Vanity Fair Oscar Party with a cane in March
Selma Blair made a statement at the Fashion Trust U.S. Awards , making her first red carpet appearance without her cane since her remission from multiple sclerosis in 2021.
At the star-studded April 9 event in Beverly Hills, Calif., the Cruel Intentions star, 51, posed in a mini double-breasted blazer dress and high heels adorned with bauble details on the straps. She accessorized with a two-layered puka shell necklace, a statement ring and a gold clutch in one hand.
She wore her blonde bob in an edgy half-up hairstyle and a blush pink lipstick with her natural glam.
Monica Schipper/Getty
Blair recently attended Vanity Fair ’s Oscars afterparty on March 10, wearing a coral pink Sebastian Gunawan corset ball gown with a center cutout revealing the bow-like bustier. While walking with her cane, which supports her mobility , the actress made sure to give the camera a 360-degree view of the voluminous design.
In an interview with British Vogue last summer, Blair said that she had an “emotional and physical attachment to the cane,” adding that it had become an “extension” of her.
Axelle/Bauer-Griffin/FilmMagic
Multiple sclerosis is a “potentially disabling disease” that impacts the brain and spinal cord, according to the Mayo Clinic , and happens when the immune system attacks the protective sheath that covers nerves.
Symptoms vary depending on the severity of the disease, but the Mayo Clinic states “some people with severe MS may lose the ability to walk independently or ambulate at all. Other individuals may experience long periods of remission without any new symptoms.”
Daniele Venturelli/Getty
Never miss a story — sign up for PEOPLE's free daily newsletter to stay up-to-date on the best of what PEOPLE has to offer, from celebrity news to compelling human interest stories.
On Jan. 29, Blair posted a health update in a lengthy Instagram video, in which she shared that while she’s still in remission from multiple sclerosis, she’s in daily pain because she has Ehlers-Danlos Syndrome.
“I hurt all the time,” Blair said. “I say that only for you people that hurt also. Like, I get it. And for all of us, just aging, it hurts. You have to stretch,” which is “hard” for her to do. EDS is a group of inherited disorders that affects connective tissue, like skin and the joints, the Mayo Clinic explains . Those with EDS often have “overly flexible joints and stretchy, fragile skin” — and this can lead to injuries.
Yet, Blair is taking life in stride. “This is nothing that’s like horrible, scary stuff or anything. It’s just like one of those extra things that turns into a chronic thing, and you have to watch, because people think stretching’s so good for you, and I’m technically not allowed to stretch, because I’m always stretching.”
Related Articles

IMAGES
VIDEO
COMMENTS
Our MS Navigators help identify solutions and provide access to the resources you are looking for. Call 1-800-344-4867 or contact us online. Multiple Sclerosis changes how you enjoy your home and leisure time. You can continue to live your life at home and engage in activities you love. Find out how.
Happy and safe, stress-free travels! be active - stay fit - keep exploring. ActiveMSers has prepared an exhaustive guide for traveling with a disability, with a focus on multiple sclerosis. This practical advice has been collected from fellow MSers, travel agents, airline staff, cruise lines, disability specialists, and personal experience.
Our MS Navigators help identify solutions and provide access to the resources you are looking for. Call 1-800-344-4867 or contact us online. If you or somone close to you has recently been diagnosed, access our MS information and resources. Self-help groups bring people together who share common life experiences for support, education and ...
Other areas to consider in general are the type of transportation you'll require, which may depend on personal devices, the need for a service dog, and any documentation if needed. As an example, airlines might ask for a U.S. DOT form defining the health, behavior, and training received for your service dog. Be sure to check with the airlines ...
Preparing to travel is often a time-consuming task. When you have a medical condition like multiple sclerosis (MS), it can be even more so. One MyMSTeam member said they had stopped traveling because of all of the complications. "We gave up traveling years ago, especially airplanes. I really don't trust them and I have too many things I ...
MS Cruisers are a part of Fun Cruise and Travel. At Fun Cruise and Travel our top priority is to serve the MS community through this unique venue with empathy, resourcefulness and responsibility. We do our best to listen and support those with multiple sclerosis, thier family members and caregivers to help them live proactively and manage their ...
Traveling with multiple sclerosis (MS) can be challenging, but it is certainly not impossible. It requires careful planning and preparation, including consulting with a healthcare provider and arranging for necessary accommodations. MS can cause a range of symptoms, including fatigue, mobility issues, and cognitive difficulties, which can make ...
Plan for: 2-3 days. Great for: Single, group, and family travelers. Cost: Hotels prices vary; see our accessibility resource guide. Tranquil Adventures base rates are $350/half day and $500/full ...
Summer travel season is in full force. Being diagnosed with multiple sclerosis does not mean that you have to give up on your hopes and dreams of traveling to far away destinations. Rather, you can use your diagnosis as a call to action to get out there and explore new places that you have always wanted to visit.
For many people living with multiple sclerosis (MS), maintaining an independent lifestyle is very important. Traveling to where you need to go can be a concern, especially if you don't drive. But the good news is that there are plenty of ways to get around. In the age of the internet and modern transportation, more information and services ...
The Transportation Security Administration has a special help line, called TSA Cares, for travelers with disabilities and medical conditions: 855-787-2227. Call 72 hours before check-in to find ...
General Travel Health Advice. Travellers with MS are a diverse group, ranging from those who are well with no disability to those with symptoms and significant disability. UK MS support websites offer advice for travellers with MS, for example the Multiple Sclerosis Trust or the MS Society. Prior to travel the following should be considered.
Multiple Sclerosis; Migraine; Pain Management; Psoriasis; ... Support Groups; Orthopedics; Subscribe . Log In . ... Multiple Sclerosis Blog; Travel Smart and Safe . See More on Multiple Sclerosis ...
MS Run the US is dedicated to raising awareness and funds to support multiple sclerosis (MS) research, while also aiding those living with disability due to MS. Partner With Us. Apply To Run The Relay. ... Join and be part of the first group considered for the next team! JOIN OUR COMMUNITY. BECOME AN AMBASSADOR. Each year we run across America ...
Reducing Risk for Other Diseases. Immunocompromised people make up 1%-2% of patients seen in US travel clinics, and they largely pursue itineraries like those of immunocompetent travelers. Pretravel preparation for people with a suppressed immune status, whether due to a health condition, medication, or other treatment, is complex.
I hope you continue to travel wherever you want to go, and that it gets a little easier for you.<br/><br/></p> reactions . reply . View 1 previous replies . Therry Neilsen Moderator & Contributor <p><inline-mention username="Jenny Angus" user-id="4203455"/> that settles it. Out of the union with them!
Multiple sclerosis (MS) is a disease of impaired nerve signaling within a person's brain and spinal cord. The variable symptoms of MS—fatigue, pain, walking difficulties, vision problems, and more—can be socially isolating and interfere with daily functioning. Support groups are a valuable resource for those living with MS because they ...
Multiple sclerosis (MS) is the most common disabling neurological disease of young adults with symptom onset generally occurring between the ages of 20 to 40 years. In MS, the immune system cells that normally protect us from viruses, bacteria, and unhealthy cells mistakenly attack myelin in the central nervous system (brain, optic nerves, and spinal cord).
People with multiple sclerosis may also develop: Muscle stiffness or spasms. Severe weakness or paralysis, typically in the legs. Problems with bladder, bowel or sexual function. Cognitive problems, like forgetfulness or word finding difficulties. Mood problems, such as depression, anxiety or mood swings.
If you would like to start or affiliate a support group, or if you have any questions, please contact our Support Groups Department by email at [email protected] or call 888-673-6287. If you are looking for an existing support group to join, search our national independent support group directory on the upper left side of the page.
00:00. 00:28. Selma Blair made a statement at the Fashion Trust U.S. Awards, making her first red carpet appearance without her cane since her remission from multiple sclerosis in 2021. At the ...