South Africa Travellers' Diarrhea
Travel health information: south africa, country intro.
Country Overview

Immunizations
Required vaccinations.
Yellow Fever
Recommended Vaccinations
Hepatitis A
Routine Immunizations
Typhoid Fever
Selective Vaccinations
Hepatitis B
Health Risks
General health risks.
African Tick-Bite Fever
Air Pollution
Chikungunya
Coronavirus COVID-19
Hepatitis C
Schistosomiasis
Sexually Transmitted Infections
Travellers' Diarrhea
West Nile Virus
For Specific Travellers
Sleeping Sickness
Tuberculosis
Medical Directory
Doctors & Clinics in South Africa
Climate Information
View Climate Information by City
Resources, Guides & Charts
General Resources
South Africa: General Health Risks
Description.
The term Travellers' Diarrhea is used to describe gastrointestinal infections affecting travellers caused by ingesting bacteria, viruses, and protozoa. These microorganisms are found worldwide and are typically transmitted from person to person via the fecal-oral route – an infected person who does not practice proper hand or body hygiene passes on the infection to another person when handling food and water. Travellers' Diarrhea is one of the most common illness among travellers.
Travellers' Diarrhea can happen when:
- Eating raw, under cooked, unwashed, or improperly handled meat, poultry products, dairy products, fruits, vegetables, shellfish, and seafood.
- Drinking contaminated water or beverages.
- Inadvertently ingesting fecal matter, protozoa eggs, or viruses by touching the mouth with dirty or improperly washed hands.
- Eating in restaurants, from buffets, or from street vendors where food handling and hygienic practices are not followed properly.
The golden rule to prevent gastrointestinal infections is: Boil it, Cook it, Peel it, or Forget it! However, it’s not just about what you eat, it’s also important to consider where you eat. It’s not always easy to know if a restaurant or food vendor follows proper food handling and hygienic practices (such as separating raw from cooked ingredients, properly cleaning cutting boards and utensils, washing their hands, and correctly refrigerating food). Avoid restaurants and food vendors that appear unclean or that don’t have many customers. Be cautious of food that has been stored uncovered, has been improperly refrigerated, or has been standing out for a long time such as buffets.
If you are unsure about the tap water quality, bring the water to a rolling boil. Boiling water destroys pathogens that can cause Travellers’ Diarrhea and other gastrointestinal infections. If you cannot boil your water, opt for treated or bottled water instead.
The risk of Travellers’ Diarrhea can also be minimized by following good hygiene practices. Make sure to wash your hands for at least 20 seconds with warm water and soap, especially before preparing or eating food and after using the bathroom. If water and soap are unavailable, use an alcohol-based hand sanitizer that contains at least 60% alcohol.
Managing Travellers’ Diarrhea
At the first sign of diarrhea, drink an oral rehydration solution (ORS), a mixture of salt and sugar designed to replenish electrolytes and treat dehydration. Antimotility agents like loperamide can also be used to reduce symptoms, but they do not treat the gastrointestinal infection. Traveller’s diarrhea is usually a self-limiting infection (it resolves itself), but if it persists and becomes worse after 2 or 3 days, you may want to consider taking an antibiotic for treatment.
If you are on high blood pressure medication watch for signs of dehydration since it can become an emergency very quickly.
Before you go, consult your doctor for the best diarrhea treatment options. Travellers who have pre-existing health conditions and are more susceptible to gastrointestinal infections may consider taking preventive medication.
For more information on preventing Travellers' Diarrhea, check out these resources from IAMAT:
- Food and water safety
- How to prevent Travellers' Diarrhea
- How to prevent illness by washing your hands
Information last updated: February 23, 2021.
- Velarde JJ, Levine MM, Nataro JP,Escherichia coli Diarrhea. In: McGill, A; Ryan, E; Hill, D; Solomon, T, eds. Hunter's Tropical Medicine and Emerging Infectious Diseases. 9 th ed. New York: Saunders Elsevier; 2013: 442-447.
- Wolfe MS. Traveler’s Diarrhea. In: Jong, E; Stevens, D, eds. Netter’s Infectious Diseases. New York: Saunders Elsevier; 2012: 390-393.
- Virk A. Amebiasis, Giardiasis, and Other Intestinal Protozoan Infections. In: Jong, E; Sanford, C. eds. The Travel and Tropical Medicine Manual, 4 th ed. Waltham, Elsevier; 2008: 448-466.
- Centers for Disease Control and Prevention: Yellow Book, Traveler’s Diarrhea
- Committee to Advice on Tropical Medicine and Travel, PHAC: Statement on Travellers' Diarrhea
Previous for South Africa
Next for south africa.
- Patient Care & Health Information
- Diseases & Conditions
- Traveler's diarrhea
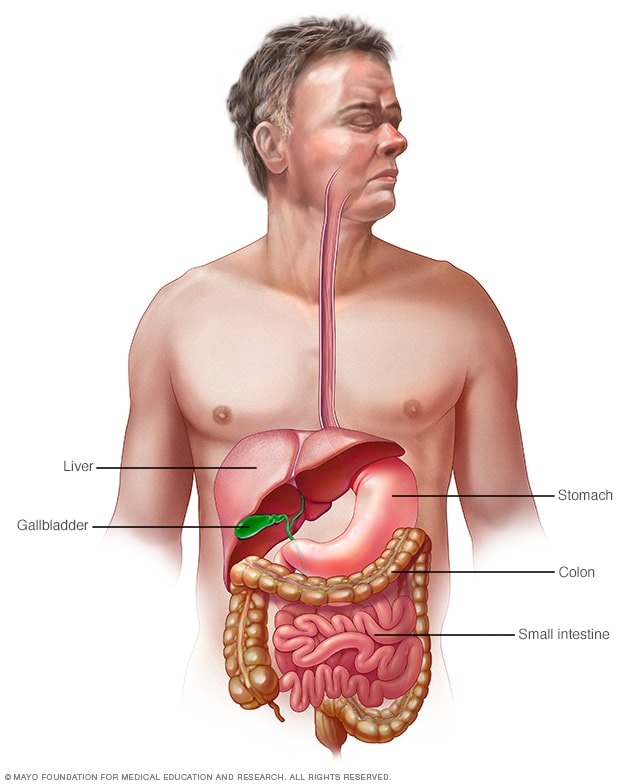
Gastrointestinal tract
Your digestive tract stretches from your mouth to your anus. It includes the organs necessary to digest food, absorb nutrients and process waste.
Traveler's diarrhea is a digestive tract disorder that commonly causes loose stools and stomach cramps. It's caused by eating contaminated food or drinking contaminated water. Fortunately, traveler's diarrhea usually isn't serious in most people — it's just unpleasant.
When you visit a place where the climate or sanitary practices are different from yours at home, you have an increased risk of developing traveler's diarrhea.
To reduce your risk of traveler's diarrhea, be careful about what you eat and drink while traveling. If you do develop traveler's diarrhea, chances are it will go away without treatment. However, it's a good idea to have doctor-approved medicines with you when you travel to high-risk areas. This way, you'll be prepared in case diarrhea gets severe or won't go away.
Products & Services
- A Book: Mayo Clinic Book of Home Remedies
- A Book: Mayo Clinic on Digestive Health
Traveler's diarrhea may begin suddenly during your trip or shortly after you return home. Most people improve within 1 to 2 days without treatment and recover completely within a week. However, you can have multiple episodes of traveler's diarrhea during one trip.
The most common symptoms of traveler's diarrhea are:
- Suddenly passing three or more looser watery stools a day.
- An urgent need to pass stool.
- Stomach cramps.
Sometimes, people experience moderate to severe dehydration, ongoing vomiting, a high fever, bloody stools, or severe pain in the belly or rectum. If you or your child experiences any of these symptoms or if the diarrhea lasts longer than a few days, it's time to see a health care professional.
When to see a doctor
Traveler's diarrhea usually goes away on its own within several days. Symptoms may last longer and be more severe if it's caused by certain bacteria or parasites. In such cases, you may need prescription medicines to help you get better.
If you're an adult, see your doctor if:
- Your diarrhea lasts beyond two days.
- You become dehydrated.
- You have severe stomach or rectal pain.
- You have bloody or black stools.
- You have a fever above 102 F (39 C).
While traveling internationally, a local embassy or consulate may be able to help you find a well-regarded medical professional who speaks your language.
Be especially cautious with children because traveler's diarrhea can cause severe dehydration in a short time. Call a doctor if your child is sick and has any of the following symptoms:
- Ongoing vomiting.
- A fever of 102 F (39 C) or more.
- Bloody stools or severe diarrhea.
- Dry mouth or crying without tears.
- Signs of being unusually sleepy, drowsy or unresponsive.
- Decreased volume of urine, including fewer wet diapers in infants.
It's possible that traveler's diarrhea may stem from the stress of traveling or a change in diet. But usually infectious agents — such as bacteria, viruses or parasites — are to blame. You typically develop traveler's diarrhea after ingesting food or water contaminated with organisms from feces.
So why aren't natives of high-risk countries affected in the same way? Often their bodies have become used to the bacteria and have developed immunity to them.
Risk factors
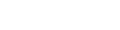
Each year millions of international travelers experience traveler's diarrhea. High-risk destinations for traveler's diarrhea include areas of:
- Central America.
- South America.
- South Asia and Southeast Asia.
Traveling to Eastern Europe, South Africa, Central and East Asia, the Middle East, and a few Caribbean islands also poses some risk. However, your risk of traveler's diarrhea is generally low in Northern and Western Europe, Japan, Canada, Singapore, Australia, New Zealand, and the United States.
Your chances of getting traveler's diarrhea are mostly determined by your destination. But certain groups of people have a greater risk of developing the condition. These include:
- Young adults. The condition is slightly more common in young adult tourists. Though the reasons why aren't clear, it's possible that young adults lack acquired immunity. They may also be more adventurous than older people in their travels and dietary choices, or they may be less careful about avoiding contaminated foods.
- People with weakened immune systems. A weakened immune system due to an underlying illness or immune-suppressing medicines such as corticosteroids increases risk of infections.
- People with diabetes, inflammatory bowel disease, or severe kidney, liver or heart disease. These conditions can leave you more prone to infection or increase your risk of a more-severe infection.
- People who take acid blockers or antacids. Acid in the stomach tends to destroy organisms, so a reduction in stomach acid may leave more opportunity for bacterial survival.
- People who travel during certain seasons. The risk of traveler's diarrhea varies by season in certain parts of the world. For example, risk is highest in South Asia during the hot months just before the monsoons.
Complications
Because you lose vital fluids, salts and minerals during a bout with traveler's diarrhea, you may become dehydrated, especially during the summer months. Dehydration is especially dangerous for children, older adults and people with weakened immune systems.
Dehydration caused by diarrhea can cause serious complications, including organ damage, shock or coma. Symptoms of dehydration include a very dry mouth, intense thirst, little or no urination, dizziness, or extreme weakness.
Watch what you eat
The general rule of thumb when traveling to another country is this: Boil it, cook it, peel it or forget it. But it's still possible to get sick even if you follow these rules.
Other tips that may help decrease your risk of getting sick include:
- Don't consume food from street vendors.
- Don't consume unpasteurized milk and dairy products, including ice cream.
- Don't eat raw or undercooked meat, fish and shellfish.
- Don't eat moist food at room temperature, such as sauces and buffet offerings.
- Eat foods that are well cooked and served hot.
- Stick to fruits and vegetables that you can peel yourself, such as bananas, oranges and avocados. Stay away from salads and from fruits you can't peel, such as grapes and berries.
- Be aware that alcohol in a drink won't keep you safe from contaminated water or ice.
Don't drink the water
When visiting high-risk areas, keep the following tips in mind:
- Don't drink unsterilized water — from tap, well or stream. If you need to consume local water, boil it for three minutes. Let the water cool naturally and store it in a clean covered container.
- Don't use locally made ice cubes or drink mixed fruit juices made with tap water.
- Beware of sliced fruit that may have been washed in contaminated water.
- Use bottled or boiled water to mix baby formula.
- Order hot beverages, such as coffee or tea, and make sure they're steaming hot.
- Feel free to drink canned or bottled drinks in their original containers — including water, carbonated beverages, beer or wine — as long as you break the seals on the containers yourself. Wipe off any can or bottle before drinking or pouring.
- Use bottled water to brush your teeth.
- Don't swim in water that may be contaminated.
- Keep your mouth closed while showering.
If it's not possible to buy bottled water or boil your water, bring some means to purify water. Consider a water-filter pump with a microstrainer filter that can filter out small microorganisms.
You also can chemically disinfect water with iodine or chlorine. Iodine tends to be more effective, but is best reserved for short trips, as too much iodine can be harmful to your system. You can purchase water-disinfecting tablets containing chlorine, iodine tablets or crystals, or other disinfecting agents at camping stores and pharmacies. Be sure to follow the directions on the package.
Follow additional tips
Here are other ways to reduce your risk of traveler's diarrhea:
- Make sure dishes and utensils are clean and dry before using them.
- Wash your hands often and always before eating. If washing isn't possible, use an alcohol-based hand sanitizer with at least 60% alcohol to clean your hands before eating.
- Seek out food items that require little handling in preparation.
- Keep children from putting things — including their dirty hands — in their mouths. If possible, keep infants from crawling on dirty floors.
- Tie a colored ribbon around the bathroom faucet to remind you not to drink — or brush your teeth with — tap water.
Other preventive measures
Public health experts generally don't recommend taking antibiotics to prevent traveler's diarrhea, because doing so can contribute to the development of antibiotic-resistant bacteria.
Antibiotics provide no protection against viruses and parasites, but they can give travelers a false sense of security about the risks of consuming local foods and beverages. They also can cause unpleasant side effects, such as skin rashes, skin reactions to the sun and vaginal yeast infections.
As a preventive measure, some doctors suggest taking bismuth subsalicylate, which has been shown to decrease the likelihood of diarrhea. However, don't take this medicine for longer than three weeks, and don't take it at all if you're pregnant or allergic to aspirin. Talk to your doctor before taking bismuth subsalicylate if you're taking certain medicines, such as anticoagulants.
Common harmless side effects of bismuth subsalicylate include a black-colored tongue and dark stools. In some cases, it can cause constipation, nausea and, rarely, ringing in your ears, called tinnitus.
- Feldman M, et al., eds. Infectious enteritis and proctocolitis. In: Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. 11th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 25, 2021.
- LaRocque R, et al. Travelers' diarrhea: Microbiology, epidemiology, and prevention. https://www.uptodate.com/contents/search. Accessed May 26, 2021.
- Ferri FF. Traveler diarrhea. In: Ferri's Clinical Advisor 2023. Elsevier; 2023. https://www.clinicalkey.com. Accessed April 28, 2023.
- Diarrhea. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/digestive-diseases/diarrhea. Accessed April 27, 2023.
- Travelers' diarrhea. Centers for Disease Control and Prevention. https://wwwnc.cdc.gov/travel/yellowbook/2020/preparing-international-travelers/travelers-diarrhea. Accessed April 28, 2023.
- LaRocque R, et al. Travelers' diarrhea: Clinical manifestations, diagnosis, and treatment. https://www.uptodate.com/contents/search. Accessed May 26, 2021.
- Khanna S (expert opinion). Mayo Clinic. May 29, 2021.
- Symptoms & causes
- Diagnosis & treatment
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
- GP practice services
- Health advice
- Health research
- Medical professionals
- Health topics
Advice and clinical information on a wide variety of healthcare topics.
All health topics
Latest features
Allergies, blood & immune system
Bones, joints and muscles
Brain and nerves
Chest and lungs
Children's health
Cosmetic surgery
Digestive health
Ear, nose and throat
General health & lifestyle
Heart health and blood vessels
Kidney & urinary tract
Men's health
Mental health
Oral and dental care
Senior health
Sexual health
Signs and symptoms
Skincare and conditions
- Travel and vaccinations
Treatment and medication
Women's health
Healthy living
Expert insight and opinion on nutrition, physical and mental health.
Exercise and physical activity
Healthy eating
Healthy relationships
Managing harmful habits
Mental wellbeing
Relaxation and sleep
Managing conditions
From ACE inhibitors for high blood pressure, to steroids for eczema, find out what options are available, how they work and the possible side effects.
Featured conditions
ADHD in children
Crohn's disease
Endometriosis
Fibromyalgia
Gastroenteritis
Irritable bowel syndrome
Polycystic ovary syndrome
Scarlet fever
Tonsillitis
Vaginal thrush
Health conditions A-Z
Medicine information
Information and fact sheets for patients and professionals. Find out side effects, medicine names, dosages and uses.
All medicines A-Z
Allergy medicines
Analgesics and pain medication
Anti-inflammatory medicines
Breathing treatment and respiratory care
Cancer treatment and drugs
Contraceptive medicines
Diabetes medicines
ENT and mouth care
Eye care medicine
Gastrointestinal treatment
Genitourinary medicine
Heart disease treatment and prevention
Hormonal imbalance treatment
Hormone deficiency treatment
Immunosuppressive drugs
Infection treatment medicine
Kidney conditions treatments
Muscle, bone and joint pain treatment
Nausea medicine and vomiting treatment
Nervous system drugs
Reproductive health
Skin conditions treatments
Substance abuse treatment
Vaccines and immunisation
Vitamin and mineral supplements
Tests & investigations
Information and guidance about tests and an easy, fast and accurate symptom checker.
About tests & investigations
Symptom checker
Blood tests
BMI calculator
Pregnancy due date calculator
General signs and symptoms
Patient health questionnaire
Generalised anxiety disorder assessment
Medical professional hub
Information and tools written by clinicians for medical professionals, and training resources provided by FourteenFish.
Content for medical professionals
FourteenFish training
Professional articles
Evidence-based professional reference pages authored by our clinical team for the use of medical professionals.
View all professional articles A-Z
Actinic keratosis
Bronchiolitis
Molluscum contagiosum
Obesity in adults
Osmolality, osmolarity, and fluid homeostasis
Recurrent abdominal pain in children
Medical tools and resources
Clinical tools for medical professional use.
All medical tools and resources
Traveller's diarrhoea
Peer reviewed by Dr Colin Tidy, MRCGP Last updated by Dr Toni Hazell Last updated 10 Feb 2023
Meets Patient’s editorial guidelines
In this series: Amoebiasis Giardia
Traveller's diarrhoea is diarrhoea that develops during, or shortly after, travel abroad. It is caused by consuming food and water, contaminated by germs (microbes) including bacteria, viruses and parasites. Other symptoms can include high temperature (fever), being sick (vomiting) and tummy (abdominal) pain. In most cases it causes a mild illness and symptoms clear within 3 to 4 days. Specific treatment is not usually needed but it is important to drink plenty of fluids to avoid lack of fluid in the body (dehydration). Always make sure that you get any advice that you need in plenty of time before your journey - some GPs offer travel advice but if yours doesn't then you may need to go to a private travel clinic.
In this article :
What is traveller's diarrhoea, what causes traveller's diarrhoea, are all travellers at risk, what are the symptoms of traveller's diarrhoea, how is traveller's diarrhoea diagnosed, when should i seek medical advice for traveller's diarrhoea, how is traveller's diarrhoea in adults treated, how is traveller's diarrhoea in children treated, side-effects of traveller's diarrhoea, how long does traveller's diarrhoea last, how can i avoid traveller's diarrhoea.
Continue reading below
Traveller's diarrhoea is diarrhoea that develops during, or shortly after, travel abroad. Diarrhoea is defined as: 'loose or watery stools (faeces), usually at least three times in 24 hours.'
Traveller's diarrhoea is caused by eating food, or drinking water, containing certain germs (microbes) or their poisons (toxins). The types of germs which may be the cause include:
Bacteria: these are the most common microbes that cause traveller's diarrhoea. Common types of bacteria involved are:
Escherichia coli
Campylobacter
Viruses: these are the next most common, particularly norovirus and rotavirus.
Parasites: these are less common causes. Giardia, cryptosporidium and Entamoeba histolytica are examples of parasites that may cause traveller's diarrhoea.
Often the exact cause of traveller's diarrhoea is not found and studies have shown that in many people no specific microbe is identified despite testing (for example, of a stool (faeces) specimen).
See the separate leaflets called E. Coli (VTEC O157) , Campylobacter, Salmonella, Cryptosporidium , Amoebiasis (dysentery information), Shigella and Giardia for more specific details on each of the microbes mentioned above.
Note : this leaflet is about traveller's diarrhoea in general and how to help prevent it.
Traveller's diarrhoea most commonly affects people who are travelling from a developed country, such as the UK, to a developing country where sanitation and hygiene measures may not meet the same standards. It can affect as many as 2 to 6 in 10 travellers.
There is a different risk depending on whether you travel to high-risk areas or not:
High-risk areas : South and Southeast Asia, Central America, West and North Africa, South America, East Africa.
Medium-risk areas : Russia, China, Caribbean, South Africa.
Low-risk areas : North America, Western Europe, Australia and New Zealand.
Sometimes outbreaks of diarrhoea can occur in travellers staying in one hotel or, for example, those staying on a cruise ship. People travelling in more remote areas (for example, trekkers and campers) may also have limited access to medical care if they do become unwell.
By definition, diarrhoea is the main symptom. This can be watery and can sometimes contain blood. Other symptoms may include:
Crampy tummy (abdominal) pains.
Feeling sick (nausea).
Being sick (vomiting).
A high temperature (fever).
Symptoms are usually mild in most people and last for 3 to 4 days but they may last longer. Symptoms may be more severe in the very young, the elderly, and those with other health problems. Those whose immune systems are not working as well as normal are particularly likely to be more unwell. For example, people with untreated HIV infection, those on chemotherapy, those on long-term steroid treatment or those who are taking drugs which suppress their immune system, for example after a transplant or to treat an autoimmune condition
Despite the fact that symptoms are usually fairly mild, they can often mean that your travel itinerary is interrupted or may need to be altered.
Traveller's diarrhoea is usually diagnosed by the typical symptoms. As mentioned above, most people have mild symptoms and do not need to seek medical advice. However, in some cases medical advice is needed (see below).
If you do see a doctor, they may suggest that a sample of your stool (faeces) be tested. This will be sent to the laboratory to look for any microbes that may be causing your symptoms. Sometimes blood tests or other tests may be needed if you have more severe symptoms or develop any complications.
As mentioned above, most people with traveller's diarrhoea have relatively mild symptoms and can manage these themselves by resting and making sure that they drink plenty of fluids. However, you should seek medical advice in any of the following cases, or if any other symptoms occur that you are concerned about:
If you have a high temperature (fever).
If you have blood in your stools (faeces).
If it is difficult to get enough fluid because of severe symptoms: frequent or very watery stools or repeatedly being sick (vomiting).
If the diarrhoea lasts for more than 5-7 days.
If you are elderly or have an underlying health problem such as diabetes, inflammatory bowel disease, or kidney disease.
If you have a weakened immune system because of, for example, chemotherapy treatment, long-term steroid treatment, or HIV infection.
If you are pregnant.
If an affected child is under the age of 6 months.
If you develop any of the symptoms listed below that suggest you might have lack of fluid in your body (dehydration). If it is your child who is affected, there is a separate list for children.
Symptoms of dehydration in adults
Dizziness or light-headedness.
Muscle cramps.
Sunken eyes.
Passing less urine.
A dry mouth and tongue.
Becoming irritable.
Symptoms of severe dehydration in adults
Profound loss of energy or enthusiasm (apathy).
A fast heart rate
Producing very little urine.
Coma, which may occur.
Note : severe dehydration is a medical emergency and immediate medical attention is needed.
Symptoms of dehydration in children
Passing little urine.
A dry mouth.
A dry tongue and lips.
Fewer tears when crying.
Being irritable.
Having a lack of energy (being lethargic).
Symptoms of severe dehydration in children
Drowsiness.
Pale or mottled skin.
Cold hands or feet.
Very few wet nappies.
Fast (but often shallow) breathing.
Dehydration is more likely to occur in:
Babies under the age of 1 year (and particularly those under 6 months old). This is because babies don't need to lose much fluid to lose a significant proportion of their total body fluid.
Babies under the age of 1 year who were a low birth weight and who have not caught up with their weight.
A breastfed baby who has stopped being breastfed during their illness.
Any baby or child who does not drink much when they have a gut infection (gastroenteritis).
Any baby or child with severe diarrhoea and vomiting. (For example, if they have passed five or more diarrhoeal stools and/or vomited two or more times in the previous 24 hours.)
In most cases, specific treatment of traveller's diarrhoea is not needed. The most important thing is to make sure that you drink plenty of fluids to avoid lack of fluid in your body (dehydration).
Fluid replacement
As a rough guide, drink at least 200 mls after each watery stool (bout of diarrhoea).
This extra fluid is in addition to what you would normally drink. For example, an adult will normally drink about two litres a day but more in hot countries. The above '200 mls after each watery stool' is in addition to this usual amount that you would drink.
If you are sick (vomit), wait 5-10 minutes and then start drinking again but more slowly. For example, a sip every 2-3 minutes but making sure that your total intake is as described above.
You will need to drink even more if you are dehydrated. A doctor will advise on how much to drink if you are dehydrated.
Note : if you suspect that you are becoming dehydrated, you should seek medical advice.
For most adults, fluids drunk to keep hydrated should mainly be water. However, this needs to be safe drinking water - for example, bottled, or boiled and treated water. It is best not to have drinks that contain a lot of sugar, such as fizzy drinks, as they can sometimes make diarrhoea worse. Alcohol should also be avoided.
Rehydration drinks
Rehydration drinks may also be used. They are made from sachets that you can buy from pharmacies and may be a sensible thing to pack in your first aid kit when you travel. You add the contents of the sachet to water.
Home-made salt/sugar mixtures are used in developing countries if rehydration drinks are not available; however, they have to be made carefully, as too much salt can be dangerous. Rehydration drinks are cheap and readily available in the UK, and are the best treatment. Note that safe drinking water should be used to reconstitute oral rehydration salt sachets.
Antidiarrhoeal medication
Antidiarrhoeal medicines are not usually necessary or wise to take when you have traveller's diarrhoea. However you may want to use them if absolutely necessary - for example, if you will be unable to make regular trips to the toilet due to travelling.You can buy antidiarrhoeal medicines from pharmacies before you travel. The safest and most effective is loperamide.
The adult dose of this is two capsules at first. This is followed by one capsule after each time you pass some diarrhoea up to a maximum of eight capsules in 24 hours. It works by slowing down your gut's activity.
You should not take loperamide for longer than two days. You should also not use antidiarrhoeal medicines if you have a high temperature (fever) or bloody diarrhoea.
Eat as normally as possible
It used to be advised to 'starve' for a while if you had diarrhoea. However, now it is advised to eat small, light meals if you can. Be guided by your appetite. You may not feel like food and most adults can do without food for a few days. Eat as soon as you are able but don't stop drinking. If you do feel like eating, avoid fatty, spicy or heavy food. Plain foods such as bread and rice are good foods to try eating.
Antibiotic medicines
Most people with traveller's diarrhoea do not need treatment with antibiotic medicines. However, sometimes antibiotic treatment is advised. This may be because a specific germ (microbe) has been identified after testing of your stool (faeces) sample.
Fluids to prevent dehydration
You should encourage your child to drink plenty of fluids. The aim is to prevent lack of fluid in the body (dehydration). The fluid lost in their sick (vomit) and/or diarrhoea needs to be replaced. Your child should continue with their normal diet and usual drinks. In addition, they should also be encouraged to drink extra fluids. However, avoid fruit juices or fizzy drinks, as these can make diarrhoea worse.
Babies under 6 months old are at increased risk of dehydration. You should seek medical advice if they develop acute diarrhoea. Breast feeds or bottle feeds should be encouraged as normal. You may find that your baby's demand for feeds increases. You may also be advised to give extra fluids (either water or rehydration drinks) in between feeds.
If you are travelling to a destination at high risk for traveller's diarrhoea, you might want to consider buying oral rehydration sachets for children before you travel. These can provide a perfect balance of water, salts and sugar for them and can be used for fluid replacement. Remember that, as mentioned above, safe water is needed to reconstitute the sachets.
If your child vomits, wait 5-10 minutes and then start giving drinks again but more slowly (for example, a spoonful every 2-3 minutes). Use of a syringe can help in younger children who may not be able to take sips.
Note : if you suspect that your child is dehydrated, or is becoming dehydrated, you should seek medical advice urgently.
Fluids to treat dehydration
If your child is mildly dehydrated, this may be treated by giving them rehydration drinks. A doctor will advise about how much to give. This can depend on the age and the weight of your child. If you are breastfeeding, you should continue with this during this time. It is important that your child be rehydrated before they have any solid food.
Sometimes a child may need to be admitted to hospital for treatment if they are dehydrated. Treatment in hospital usually involves giving rehydration solution via a special tube called a 'nasogastric tube'. This tube passes through your child's nose, down their throat and directly into their stomach. An alternative treatment is with fluids given directly into a vein (intravenous fluids).
Eat as normally as possible once any dehydration has been treated
Correcting any dehydration is the first priority. However, if your child is not dehydrated (most cases), or once any dehydration has been corrected, then encourage your child to have their normal diet. Do not 'starve' a child with infectious diarrhoea. This used to be advised but is now known to be wrong. So:
Breastfed babies should continue to be breastfed if they will take it. This will usually be in addition to extra rehydration drinks (described above).
Bottle-fed babies should be fed with their normal full-strength feeds if they will take it. Again, this will usually be in addition to extra rehydration drinks (described above). Do not water down the formula, or make it up with less water than usual. This can make a baby very ill.
Older children - offer them some food every now and then. However, if he or she does not want to eat, that is fine. Drinks are the most important consideration and food can wait until the appetite returns.
Loperamide is not recommended for children with diarrhoea. There are concerns that it may cause a blockage of the gut (intestinal obstruction) in children with diarrhoea.
Most children with traveller's diarrhoea do not need treatment with antibiotics. However, for the same reasons as discussed for adults above, antibiotic treatment may sometimes be advised in certain cases.
Most people have mild illness and complications of traveller's diarrhoea are rare. However, if complications do occur, they can include the following:
Salt (electrolyte) imbalance and dehydration .
This is the most common complication. It occurs if the salts and water that are lost in your stools (faeces), or when you are sick (vomit), are not replaced by you drinking adequate fluids. If you can manage to drink plenty of fluids then dehydration is unlikely to occur, or is only likely to be mild and will soon recover as you drink.
Severe dehydration can lead to a drop in your blood pressure. This can cause reduced blood flow to your vital organs. If dehydration is not treated, your kidneys may be damaged . Some people who become severely dehydrated need a 'drip' of fluid directly into a vein. This requires admission to hospital. People who are elderly or pregnant are more at risk of dehydration.
Reactive complications
Rarely, other parts of your body can 'react' to an infection that occurs in your gut. This can cause symptoms such as joint inflammation (arthritis), skin inflammation and eye inflammation (either conjunctivitis or uveitis). Reactive complications are uncommon if you have a virus causing traveller's diarrhoea.
Spread of infection
The infection can spread to other parts of your body such as your bones, joints, or the meninges that surround your brain and spinal cord. This is rare. If it does occur, it is more likely if diarrhoea is caused by salmonella infection.
Irritable bowel syndrome is sometimes triggered by a bout of traveller's diarrhoea.
Lactose intolerance
Lactose intolerance can sometimes occur for a period of time after traveller's diarrhoea. It is known as 'secondary' or 'acquired' lactose intolerance. Your gut (intestinal) lining can be damaged by the episode of diarrhoea. This leads to lack of a substance (enzyme) called lactase that is needed to help your body digest the milk sugar lactose.
Lactose intolerance leads to bloating, tummy (abdominal) pain, wind and watery stools after drinking milk. The condition gets better when the infection is over and the intestinal lining heals. It is more common in children.
Haemolytic uraemic syndrome
Usually associated with traveller's diarrhoea caused by a certain type of E. coli infection, haemolytic uraemic syndrome is a serious condition where there is anaemia, a low platelet count in the blood and kidney damage. It is more common in children. If recognised and treated, most people recover well.
Guillain-Barré syndrome
This condition may rarely be triggered by campylobacter infection, one of the causes of traveller's diarrhoea. It affects the nerves throughout your body and limbs, causing weakness and sensory problems. See the separate leaflet called Guillain-Barré syndrome for more details.
Reduced effectiveness of some medicines
During an episode of traveller's diarrhoea, certain medicines that you may be taking for other conditions or reasons may not be as effective. This is because the diarrhoea and/or being sick (vomiting) mean that reduced amounts of the medicines are taken up (absorbed) into your body.
Examples of such medicines are those for epilepsy, diabetes and contraception . Speak with your doctor or practice nurse before you travel if you are unsure of what to do if you are taking other medicines and develop diarrhoea.
As mentioned above, symptoms are usually short-lived and the illness is usually mild with most people making a full recovery within in few days. However, a few people with traveller's diarrhoea develop persistent (chronic) diarrhoea that can last for one month or more. It is also possible to have a second 'bout' of traveller's diarrhoea during the same trip. Having it once does not seem to protect you against future infection.
Avoid uncooked meat, shellfish or eggs. Avoid peeled fruit and vegetables (including salads).
Be careful about what you drink. Don't drink tap water, even as ice cubes.
Wash your hands regularly, especially before preparing food or eating.
Be careful where you swim. Contaminated water can cause traveller's diarrhoea.
Regular hand washing
You should ensure that you always wash your hands and dry them thoroughly; teach children to wash and dry theirs:
After going to the toilet (and after changing nappies or helping an older child to go to the toilet).
Before preparing or touching food or drinks.
Before eating.
Some antibacterial hand gel may be a good thing to take with you when you travel in case soap and hot water are not available.
Be careful about what you eat and drink
When travelling to areas with poor sanitation, you should avoid food or drinking water that may contain germs (microbes) or their poisons (toxins). Avoid:
Fruit juices sold by street vendors.
Ice cream (unless it has been made from safe water).
Shellfish (for example, mussels, oysters, clams) and uncooked seafood.
Raw or undercooked meat.
Fruit that has already been peeled or has a damaged skin.
Food that contains raw or uncooked eggs, such as mayonnaise or sauces.
Unpasteurised milk.
Drinking bottled water and fizzy drinks that are in sealed bottles or cans, tea, coffee and alcohol is thought to be safe. However, avoid ice cubes and non-bottled water in alcoholic drinks. Food should be cooked through thoroughly and be piping hot when served.
You should also be careful when eating food from markets, street vendors or buffets if you are uncertain about whether it has been kept hot or kept refrigerated. Fresh bread is usually safe, as is canned food or food in sealed packs.
Be careful where you swim
Swimming in contaminated water can also lead to traveller's diarrhoea. Try to avoid swallowing any water as you swim; teach children to do the same.
Obtain travel health advice before you travel
Always make sure that you visit your GP surgery or private travel clinic for health advice in plenty of time before your journey. Alternatively, the Fit for Travel website (see under Further Reading and References, below) provides travel health information for the public and gives specific information for different countries and high-risk destinations. This includes information about any vaccinations required, advice about food, water and personal hygiene precautions, etc.
There are no vaccines that prevent traveller's diarrhoea as a whole. However, there are some other vaccines that you may need for your travel, such as hepatitis A, typhoid, etc. You may also need to take malaria tablets depending on where you are travelling.
Antibiotics
Taking antibiotic medicines to prevent traveller's diarrhoea (antibiotic prophylaxis) is not generally recommended. This is because for most people, traveller's diarrhoea is mild and self-limiting. Also, antibiotics do not protect against nonbacterial causes of traveller's diarrhoea, such as viruses and parasites. Antibiotics may have side-effects and their unnecessary use may lead to problems with resistance to medicines.
Probiotics have some effect on traveller's diarrhoea and can shorten an attack by about one day. It is not known yet which type of probiotic or which dose, so there are no recommendations about using probiotics to prevent traveller's diarrhoea.
Further reading and references
- Bourgeois AL, Wierzba TF, Walker RI ; Status of vaccine research and development for enterotoxigenic Escherichia coli. Vaccine. 2016 Mar 15. pii: S0264-410X(16)00287-5. doi: 10.1016/j.vaccine.2016.02.076.
- Travellers' diarrhoea ; Fitfortravel
- Riddle MS, Connor BA, Beeching NJ, et al ; Guidelines for the prevention and treatment of travelers' diarrhea: a graded expert panel report. J Travel Med. 2017 Apr 1;24(suppl_1):S57-S74. doi: 10.1093/jtm/tax026.
- Giddings SL, Stevens AM, Leung DT ; Traveler's Diarrhea. Med Clin North Am. 2016 Mar;100(2):317-30. doi: 10.1016/j.mcna.2015.08.017.
- Diarrhoea - prevention and advice for travellers ; NICE CKS, February 2019 (UK access only)
Article History
The information on this page is written and peer reviewed by qualified clinicians.
Next review due: 9 Feb 2028
10 feb 2023 | latest version.
Last updated by
Peer reviewed by

Feeling unwell?
Assess your symptoms online for free
- Skip to content
- Accessibility help
Diarrhoea - prevention and advice for travellers
Last revised in September 2023
Travellers' diarrhoea is a clinical syndrome associated with contaminated food or water, that occurs during or shortly after travel
- Scenario: Diarrhoea - prevention and advice for travellers
Background information
- Risk factors
- Complications
Diarrhoea - prevention and advice for travellers: Summary
- Travellers' diarrhoea is defined as passing three or more unformed stools in a 24-hour period with at least one additional symptom, such as abdominal pain or cramps, nausea, vomiting, fever, or blood in the stools.
- Enteric bacteria are the most commonly documented (for example, Escherichia coli, Campylobacter spp., Salmonella spp., and Shigella spp .).
- Viruses and parasites can also cause travellers' diarrhoea.
- Low for people travelling to western European countries, the USA and Canada, Japan, Australia, and New Zealand.
- Intermediate for people travelling to southern European countries, Israel, South Africa, and some Caribbean and Pacific Islands.
- High for people travelling to Africa, Latin America, the Middle East, and most parts of Asia.
- Food hygiene and safe drinking water.
- Self-management and when to seek medical advice if diarrhoea develops during travel.
- The importance of personal hygiene, food hygiene, and safe drinking water should be emphasized.
- Advice regarding the risk of waterborne infection and avoiding contaminated recreational water should be offered.
- Antibiotic prophylaxis or 'stand-by' antibiotic treatment can be considered for certain high-risk travellers. Specialist advice should be sought.
- Most episodes are short-lived and self-limiting, lasting a few days.
- The person could consider purchasing sachets of oral rehydration salt before travelling.
- During an episode of diarrhoea, it is important to prevent dehydration — particularly for young children, pregnant women, elderly people, and those with pre-existing illnesses.
- Both loperamide and bismuth subsalicylate (for example, Pepto-Bismol ® ) may be considered in adults for the relief of mild-to-moderate diarrhoea. They should be used for a maximum of 2 days.
- When to seek medical assistance.
The content on the NICE Clinical Knowledge Summaries site (CKS) is the copyright of Clarity Informatics Limited (trading as Agilio Software Primary Care) . By using CKS, you agree to the licence set out in the CKS End User Licence Agreement .
Issues by year
Advertising
Volume 44, Issue 1, January-February 2015
Advising travellers about management of travellers’ diarrhoea
How is td defined.
Classic, severe TD is usually defined as at least three unformed bowel movements occurring within a 24-hour period, often accompanied by cramps, nausea, vomiting, fever and/or blood in the stools. 5–7 Moderate TD is defined as one or two unformed bowel movements and other symptoms occurring every 24 hours or as three or more unformed bowel movements without additional symptoms. Mild TD is defined as one or two unformed bowel movements without any additional symptoms and without interference with daily activities. 8,9 TD generally resolves spontaneously, usually after 3–4 days, 8 but, in the interim, frequently leads to disruption of planned activities.
What are the causes of TD?
Approximately 50–80% of TD is caused by bacterial infections; enterotoxigenic Escherichia coli (ETEC) is the most common cause overall. Other bacterial causes include enteroinvasive E. coli (EIEC), enteroaggregative E. coli (EAEC), Shigella , Campylobacter and Salmonella species. The exact breakdown of organisms varies according to destination, season and other factors. Noroviruses cause 10–20% of TD cases. Protozoal parasites should be considered particularly in those with persistent diarrhoea (illness lasting ≥14 days) or when antibacterial therapy fails to shorten illness. 10
How can TD be prevented?
Methods for preventing TD include avoidance, immunisation, non-antibiotic interventions or antibiotic prophylaxis. 11
What avoidance measures are generally recommended and do they work?
Avoidance of TD has traditionally relied on recommendations regarding careful food and drink choices (avoiding untreated/unboiled tap water, including ice and water used for brushing teeth, and raw foods such as salads, uncooked vegetables or fruits that cannot be peeled). This underpins the saying ‘Boil it, cook it, peel it or forget it…. easy to remember, impossible to do’. Additional standard advice is that undercooked or raw meat, fish and shellfish are high-risk foods. However, whether deliberately or inadvertently, most people find it very difficult to adhere to dietary restrictions 12 and over 95% of people disobey the rules of ‘safe’ eating and drinking within a few days of leaving home. Additionally, there is minimal evidence for a correlation between adherence to dietary precautions and a reduced risk of TD, 13 although common sense nevertheless supports care with food selection. 4
Where people eat may be more important than what people eat. Risks are associated, in descending order, with street vendors, restaurants and private homes. Use of antibacterial handwash before eating is also recommended. 14
Which vaccines can be considered?
Immunisation has little practical role in the prevention of TD and the only potentially relevant vaccines are those against rotavirus (infants only) and the oral cholera vaccine.
The cholera vaccine has >90% efficacy for prevention of Vibrio cholera but travellers are rarely at risk of infection with this pathogen. 1 The vaccine contains a recombinant B subunit of the cholera toxin that is antigenically similar to the heat-labile toxin of ETEC; therefore, the cholera vaccine may also reduce ETEC TD. However, it is not licensed for TD prevention in Australia and, although initially thought to offer a 15–20% short-term (3 months) reduction in TD, a recent Cochrane review showed no statistically significant effects on ETEC diarrhoea or all-cause diarrhoea. 15 Overall, there is, therefore, insufficient evidence to support general use of the cholera vaccine for TD protection, but it may still be considered for individuals with increased risk of severe or complicated TD (eg immunosuppressed or underlying inflammatory bowel disease).
Other vaccines directed against organisms spread by the faecal–oral route are the vaccines for typhoid, hepatitis A and polio, but infection with these organisms rarely causes TD. 15
Do non-antibiotic interventions work?
Several probiotic agents have been studied for treatment and prevention of TD, including Lactobacillus and Saccharomyces preparations. However, their effectiveness for TD prevention has been limited, 11,16,17 and a consensus group has recommended against their use. 4 Other over-the-counter agents are also available (eg travelan, which contains bovine colostrum harvested from cows immunised with an ETEC vaccine) but data regarding overall efficacy of reducing all-cause TD are currently lacking.
Should antibiotic prophylaxis against TD be given?
Quinolone antibiotics are highly effective (80–95%) in preventing TD, but antibiotic prophylaxis is rarely indicated. 4 It may result in a false sense of security and hence less caution in dietary choices, it poses risks of side effects, diarrhoea associated with Clostridium difficile , and, more importantly, would lead to a vast amount of antibiotic use, thus predisposing to more rapid development of antibiotic resistance globally. 11 Therefore non-antibiotic options for prevention and a focus instead on empirical self-treatment if needed according to symptoms are the mainstay of management, aligning with the antimicrobial stewardship perspective of minimisation of antimicrobial overuse and reducing promotion of antimicrobial resistance.
In rare circumstances, it may be reasonable to consider short courses of antibiotic prophylaxis in individuals at very high risk of infection (eg severely immunocompromised). 11 Globally, one of the most commonly used agents in this regard is rifaximin, a non-absorbed semisynthetic rifamycin derivative, which has been shown to be effective and is approved for use for TD prevention in some countries, but it is not approved for this indication in Australia. Other options include the antibiotics discussed below for TD self-treatment.
How should self-treatment of TD be managed?
Because of the limitations of TD prevention measures, the pre-travel consultation should be viewed as an opportunity to ‘arm’ travellers with the knowledge and medication needed to appropriately self-treat, should TD occur during their trip.
The first goal of therapy is the prevention and treatment of dehydration, which is of particular concern for young children, pregnant women and the elderly. Commercial packets of oral rehydration salts are readily available in pharmacies and should be purchased before travel. The other element of TD self-treatment is to recommend travellers bring an antimotility agent plus an antibiotic with them. Loperamide is preferred over the diphenoxylate/atropine combination, as the latter agent is generally less effective and associated with a greater potential for adverse effects.
When should loperamide alone versus loperamide plus an antibiotic be taken?
For mild symptoms of watery diarrhoea, self-treatment with oral rehydration plus loperamide is recommended. Loperamide therapy alone has no untoward effects in mild TD 18 but if symptoms worsen, or do not improve after 24 hours, antibiotics should be added. If TD is moderate or severe at onset, then combination therapy with loperamide plus antibiotics should be started immediately, as this optimises the clinical benefit of self-treatment by providing more rapid relief and shortening the symptom duration. 10,19
The recommended dose of loperamide is two tablets (4 mg) stat, then one tablet after each bowel motion to a maximum of eight per 24-hour period until the TD has resolved. Despite warnings regarding the safety of antidiarrhoeal agents with bloody diarrhoea or diarrhoea accompanied by fever, the combination with antibiotics is likely to be safe in the setting of mild febrile dysentery, 18 and a number of studies have shown the combination to be more efficacious than use of either agent alone. 7,18–20 Rapid institution of effective treatment shortens symptoms to 30 hours or less in most people. 12 For example, the duration of diarrhoea was significantly ( P = 0.0002) shorter following treatment with azithromycin plus loperamide (11 h) than with azithromycin alone (34 h). 19
Which antibiotic should be recommended for empirical elf-treatment of TD?
The most commonly used antibiotics for empirical TD therapy are fluoroquinolones (either norfloxacin or ciprofloxacin) or azithromycin ( Table 1 ). Cotrimoxazole has been used but is no longer recommended because of widespread resistance. For TD caused by ETEC, the fluoroquinolones and azithromycin have similar efficacy; however, in Asia (particularly South and South-East Asia), Campylobacter is a common cause of TD and strains occurring in this part of the world show a high degree of resistance to fluoroquinolones. 10,21 Therefore, azithromycin is preferred for travellers to this region. Azithromycin remains generally efficacious despite emerging resistance, and is also the preferred treatment for diarrhoea with complications of dysentery or high fever, and for use in pregnant women or children under the age of 8 years, in whom avoidance of quinolones is preferred. Moreover, the 24-hour dosing of azithromycin may be preferable to the 12-hourly dosing schedule required with fluoroquinolones.
What is the optimal dosing schedule?
The fluoroquinolones and azithromycin have been administered as a single dose or for 3 days ( Table 1 ). Usually a single dose is adequate and there is no apparent clinically important difference in efficacy with either dosing schedule for TD. 10 However, for bacteria such as Campylobacter and Shigella dysenteriae , single-dose therapy may be inadequate. 11 It is reasonable, therefore, to give travellers a 3-day supply of antibiotics and tell them to continue taking the therapy (either 12- or 24-hourly, depending on which antibiotic is prescribed) only if their TD symptoms persist. If the TD has resolved, no further antibiotics need to be taken and any remaining antibiotic doses can be kept in case of a second bout of TD. It is prudent to specifically highlight that this advice differs from the usual instructions to take all tablets even if symptoms have resolved.
What is the optimal empirical TD management in children?
There are few data on empirical treatment of TD in children and limited options for therapy. The mainstay of therapy is oral rehydration solution, particularly for children <6 years of age. Antimotility agents are contraindicated for children because of the increased risk of adverse effects, especially paralytic ileus, toxic megacolon and drowsiness (narcotic effect) with loperamide. 1 The lower age limit recommended for avoiding loperamide varies by location; US guidelines state that loperamide should not be given to infants <2 years of age, the UK <4 years and Australian guidelines state <12 years. 14 However, most Australian practitioners are prepared to use loperamide in children aged 6 years or older, if needed to control symptoms.
A paediatric (powder) formulation of azithromycin is available and is the most commonly recommended agent for children. The usual dose is 10–25 mg/kg for up to 3 days. A practical tip is to ensure that the pharmacy does not reconstitute the powder into a solution, as once dissolved, the solution lasts only for 10 days. Instead, sterile water should be provided along with instructions on how to reconstitute the powder if needed. Fluoroquinolones (ciprofloxacin or norfloxacin 10mg/kg bd) are an alternative option if there are reasons for avoiding azithromycin, with previous concerns regarding potential effects on cartilage not substantiated in recent studies. 14,22
Does starting antibiotics early prevent the chances of developing prolonged symptoms?
Although TD symptoms are short-lived in most cases, 8–15% of affected travellers are symptomatic for more than a week and 2% develop chronic diarrhoea lasting a month or more. 11 Episodes of TD have been shown to be associated with a quintuple risk of developing irritable bowel syndrome (IBS), and post-travel IBS occurs in 3–10% of travellers. However, it is unknown whether IBS can be prevented by starting antimicrobial therapy earlier in the course of enteric infection. 4,18,23
Should tinidazole also be prescribed and, if so, for whom?
Tinidazole can be prescribed as a second antibiotic for empirical self‑treatment as it is effective against the protozoan parasitic enteric pathogen Giardia intestinalis . A dose of 2 g (4 x 500 mg tablets) stat is recommended. However, for most short-term travellers, tinidazole may be unnecessary and the complexity of the additional instructions required may be unwarranted. It is optimally recommended, therefore, for travellers departing on trips of significant duration (>2–3 weeks). If prescribed, the instructions should be to take tinidazole if the TD persists following the 3-day course of antibiotic therapy (fluoroquinolone or azithromycin). This will mean that the TD has lasted for at least 72 hours, thus increasing the likelihood of a parasitic cause.
When should medical care for acute symptoms be recommended?
While most episodes of TD are amenable to self-treatment, if there is a risk of dehydration due to intolerance of oral fluids or comorbidities, as well as in the setting of frank blood in the stool or unremitting fevers (>38.5°C for 48 hours), medical therapy should be sought. 18
How should TD be managed after return?
While a full description of TD management is beyond the scope of this article, for returning travellers with diarrhoea, at least one (preferably three) stool sample(s) should be taken, including specific requests for evaluation of parasites. For patients who are unwell, particularly those with fevers or dysentery, initiation of empirical antibiotic treatment with azithromycin or a quinolone may be needed while awaiting results. For those with prolonged symptoms, tinidazole as empirical therapy for protozoan parasites may be considered. Endoscopic evaluation may also be advisable if no infectious cause is found and symptoms do not resolve.
- Travellers’ diarrhoea continues to affect 20–50% of people undertaking trips to areas with under-developed sanitation and there is minimal evidence for beneficial effects of dietary precautions.
- Evidence for the benefit of cholera vaccine in reducing TD is limited, but it can be considered in people at high risk of infection.
- In 50–80% of TD cases, TD is caused by bacterial infection. Mild diarrhoea can be managed with an antimotility agent (loperamide) alone, but for moderate or severe diarrhoea, early self-treatment with loperamide in conjunction with antibiotics is advised.
- Recommended empirical antibiotics are fluoroquinolones (norfloxacin / ciprofloxacin) or azithromycin for up to 3 days, although in the setting of increasing resistance, the latter is preferred for travellers to South and South-East Asia.
Competing interests: Karin Leader received a consultancy fee from Imuron in relation to the C. difficile vaccine. She is also an ISTM board member and received a consultancy from ISTM to join the GeoSentinel leadership team. She received grants from Sanofi to develop a mobile phone app for splenectomised patients and from GSK to research the use of the HBV vaccine. GSK also paid her to lecture on travel risks at the Asia Pacific Travel Health Conference. She has received support from both GSK and Sanofi to attend travel medicine conferences.
Provenance and peer review: Commissioned, externally peer reviewed
- Diemert DJ. Prevention and self-treatment of travelers’ diarrhea. Prim Care 2002;29:843–55. Search PubMed
- Department of Health and Human Services. Centers for Disease Control and Prevention. Travelers’ Diarrhea. Available at www.cdc.gov/ncidod/dbmd/diseaseinfo/travelersdiarrhea_g.htm [Accessed 25 November 2014]. Search PubMed
- Paredes-Paredes M, Flores-Figueroa J, Dupont HL. Advances in the treatment of travelers’ diarrhea. Curr Gastroenterol Rep 2011;13:402–07. Search PubMed
- DuPont HL, Ericsson CD, Farthing MJ, et al. Expert review of the evidence base for prevention of travelers’ diarrhea. J Travel Med 2009;16:149–60. Search PubMed
- Nair D. Travelers’ diarrhea: prevention, treatment, and post-trip evaluation. J Fam Pract 2013;62:356–61. Search PubMed
- De Bruyn G, Hahn S, Borwick A. Antibiotic treatment for travellers’ diarrhoea. The Cochrane Database Syst Rev 2000:CD002242. Search PubMed
- Riddle MS, Arnold S, Tribble DR. Effect of adjunctive loperamide in combination with antibiotics on treatment outcomes in traveler’s diarrhea: a systematic review and meta-analysis. Clin Infect Dis 2008;47:1007–14. Search PubMed
- Steffen R. Epidemiology of traveler’s diarrhea. Clin Infect Dis 2005;41(Suppl 8):S536–40. Search PubMed
- Steffen R, Collard F, Tornieporth N, et al. Epidemiology, etiology, and impact of traveler’s diarrhea in Jamaica. JAMA 1999;281:811–17. Search PubMed
- DuPont HL, Ericsson CD, Farthing MJ, et al. Expert review of the evidence base for self-therapy of travelers’ diarrhea. J Travel Med 2009;16:161–71. Search PubMed
- Diemert DJ. Prevention and self-treatment of traveler’s diarrhea. Clin Microbiol Rev 2006;19:583–94. Search PubMed
- Travelers’ diarrhea. NIH Consensus Development Conference. JAMA 1985;253:2700–04. Search PubMed
- Shlim DR. Looking for evidence that personal hygiene precautions prevent traveler’s diarrhea. Clin Infect Dis 2005;41(Suppl 8):S531–35. Search PubMed
- Plourde PJ. Travellers’ diarrhea in children. Paediatr Child Health 2003;8:99–103. Search PubMed
- Ahmed T, Bhuiyan TR, Zaman K, Sinclair D, Qadri F. Vaccines for preventing enterotoxigenic Escherichia coli (ETEC) diarrhoea. Cochrane Database Syst Rev 2013;7:CD009029. Search PubMed
- Ritchie ML, Romanuk TN. A meta-analysis of probiotic efficacy for gastrointestinal diseases. PloS One 2012;7:e34938. Search PubMed
- Centers for Disease Control Prevention. Yellow Book. Chapter 2. Travelers’ Diarrhea. Available at wwwnc.cdc.gov/travel/yellowbook/2014/chapter-2-the-pre-travel-consultation/travelers-diarrhea [Accessed 25 November 2014]. Search PubMed
- Wingate D, Phillips SF, Lewis SJ, et al. Guidelines for adults on self-medication for the treatment of acute diarrhoea. Aliment Pharmacol Ther 2001;15:773–82. Search PubMed
- Ericsson CD, DuPont HL, Okhuysen PC, Jiang ZD, DuPont MW. Loperamide plus azithromycin more effectively treats travelers’ diarrhea in Mexico than azithromycin alone. J Travel Med 2007;14:312–19. Search PubMed
- Murphy GS, Bodhidatta L, Echeverria P, et al. Ciprofloxacin and loperamide in the treatment of bacillary dysentery. Ann Intern Med 1993;118:582–86. Search PubMed
- Tribble DR, Sanders JW, Pang LW, et al. Traveler’s diarrhea in Thailand: randomized, double-blind trial comparing single-dose and 3-day azithromycin-based regimens with a 3-day levofloxacin regimen. Clin Infect Dis 2007;44:338–46. Search PubMed
- Yung A, Leder K, Torresi J, et al. Manual of Travel Medicine. 3rd edn. Melbourne: IP Communciations, 2011. Search PubMed
- Stermer E, Lubezky A, Potasman I, Paster E, Lavy A. Is traveler’s diarrhea a significant risk factor for the development of irritable bowel syndrome? A prospective study. Clin Infect Dis 2006;43:898–901. Search PubMed
- Expert Group for Antibiotic. Antiobiotic: gastrointestinal tract infections: acute gastroenteritis: acute diarrhoea in special groups: travellers’ diarrhoea. In: eTG Complete [Internet] Melbourne. Therapeutic Guidelines Ltd, 2014. Search PubMed
Also in this issue: Environmental
Professional
Printed from Australian Family Physician - https://www.racgp.org.au/afp/2015/january-february/advising-travellers-about-management-of-travellers © The Australian College of General Practitioners www.racgp.org.au
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
Travellers’ diarrhoea
Chinese translation.
- Related content
- Peer review
- Jessica Barrett , infectious diseases registrar 1 ,
- Mike Brown , consultant in infectious diseases and tropical medicine 1 2
- 1 Hospital for Tropical Diseases, University College London Hospitals NHS Trust, London WC1E 6AU, UK
- 2 Clinical Research Department, London School of Hygiene & Tropical Medicine, London, UK
- Correspondence to: J Barrett jessica.barrett{at}gstt.nhs.uk
What you need to know
Enterotoxic Escherichia coli (ETEC) is the most common cause of acute travellers’ diarrhoea globally
Chronic (>14 days) diarrhoea is less likely to be caused by bacterial pathogens
Prophylactic antibiotic use is only recommended for patients vulnerable to severe sequelae after a short period of diarrhoea, such as those with ileostomies or immune suppression
A short course (1-3 days) of antibiotics taken at the onset of travellers’ diarrhoea reduces the duration of the illness from 3 days to 1.5 days
Refer patients with chronic diarrhoea and associated symptoms such as weight loss for assessment by either an infectious diseases specialist or gastroenterologist
Diarrhoea is a common problem affecting between 20% and 60% of travellers, 1 particularly those visiting low and middle income countries. Travellers’ diarrhoea is defined as an increase in frequency of bowel movements to three or more loose stools per day during a trip abroad, usually to a less economically developed region. This is usually an acute, self limiting condition and is rarely life threatening. In mild cases it can affect the enjoyment of a holiday, and in severe cases it can cause dehydration and sepsis. We review the current epidemiology of travellers’ diarrhoea, evidence for different management strategies, and the investigation and treatment of persistent diarrhoea after travel.
We searched PubMed and Cochrane Library databases for “travellers’ diarrhoea,” and “travel-associated diarrhoea,” to identify relevant articles, which were added to personal reference collections and clinical experience. Where available, systematic reviews and randomised controlled trials were preferentially selected.
Who is at risk?
Variation in incidence 1 2 may reflect the degree of risk for different travel destinations and dietary habits while abroad. Destinations can be divided into low, medium, and high risk (see box 1). Rates of diarrhoea are likely to correlate closely with the quality of local sanitation.
Box 1: Risk of travellers’ diarrhoea according to destination 1 3
High risk destinations.
South and South East Asia*
Central America*
West and North Africa*
South America
East Africa
Medium risk
South Africa
North America
Western Europe
Australia and New Zealand
*Regions with particularly high risk of travellers’ diarrhoea
Backpackers have roughly double the incidence of diarrhoea compared with business travellers. 4 Travel in cruise ships is associated with large outbreaks of viral and bacterial gastroenteritis. 5 General advice is to avoid eating salads, shellfish, and uncooked meats. There is no strong evidence that specific dietary measures reduce incidence of diarrhoea, but studies examining this are likely to be biased by imperfect recall of what was eaten. 6 Risk factors for travellers’ diarrhoea are listed in box 2.
Box 2: Factors increasing risk of travellers’ diarrhoea 4 7 8 9
By increased dietary exposure.
Backpacking
Visiting friends and family
All-inclusive holidays (such as in cruise ships)
By increased susceptibility to an infectious load
Age <6 years
Use of H 2 receptor antagonists and proton pump inhibitors
Altered upper gastrointestinal anatomy
Genetic factors (blood group O predisposes to shigellosis and severe cholera infection)
What are the most important causes of travellers’ diarrhoea?
Most studies report a failure to identify the causative pathogen in between 40% and 70% of cases. 10 This includes multicentre studies based in high prevalence settings (that is, during travel). 3 10 11 12 This low diagnostic yield is partly due to delay in obtaining samples and partly due to the insensitivity of laboratory investigations. Older studies did not consistently attempt to identify enteroaggregative Escherichia coli (EAEC), and surveillance studies vary in reporting of other E coli species. 3 Where a pathogen is identified, bacteria are the commonest cause of acute travellers’ diarrhoea, with the remainder being caused by norovirus, rotavirus, or similar viruses (see table 1 ⇓ ). Protozoa such as Giardia lamblia can also cause acute diarrhoea, but they are more often associated with persistent diarrhoea, lasting more than two weeks. Cyclospora catayensis , another protozoan cause of diarrhoea, was identified in an increased number of symptomatic travellers returning from Mexico to the UK and Canada in 2015. 13
Frequency of pathogens causing travellers’ diarrhoea 2 3 10 11 12
- View inline
Table 1 ⇑ illustrates overall prevalence of causative agents in returning travellers with diarrhoea. However relative importance varies with country of exposure. Rates of enterotoxigenic E coli (ETEC) are lower in travellers returning from South East Asia than in those returning from South Asia, sub-Saharan Africa, and Latin America, whereas rates of Campylobacter jejuni are higher. Norovirus is a more common cause in travellers to Latin America and sub-Saharan Africa, and Giardia lamblia and Entamoeba histolytica are more common in travellers to South and South East Asia. 10
The importance of enterotoxigenic E coli as a cause for diarrhoea in travellers returning from Latin America has been decreasing over the past four decades. 10 A large scale analysis of EuroTravNet surveillance data shows increasing incidence of Campylobacter jejuni infection in travellers returning from India, Thailand, and Pakistan. 2
How does travellers’ diarrhoea present?
Most episodes of travellers’ diarrhoea start during the first week of travel, with the peak incidence on the second or third day after arrival. 8 14
Typically diarrhoea caused by enterotoxigenic E coli (“turista”) is watery and profuse, and preceded by abdominal cramps, nausea, and malaise. Symptoms are not a reliable guide to aetiology, but upper gastrointestinal manifestations such as bloating and belching tend to predominate with Giardia lamblia , while colitic symptoms such as urgency, bloody diarrhoea, and cramps are seen more often with Campylobacter jejuni and Shigella spp.
Most episodes will last between one and seven days, with approximately 10% lasting for longer than one week, 5% lasting more than two weeks, and 1% lasting more than 30 days. 8 During the illness, few patients will be severely incapacitated (in one large prospective cohort about 10% of 2800 participants were confined to bed or consulted a physician), but planned activities are often cancelled or postponed. 8
How can travellers’ diarrhoea be prevented?
Several controlled trials have failed to demonstrate an impact of food and drink hygiene advice on rates of diarrhoea. 15 However, the clear food-related source of most diarrhoeal pathogens means that general consensus among travel physicians is to continue to recommend boiling water, cooking food thoroughly, and peeling fruit and vegetables. 6 Other basic advice includes avoiding ice, shellfish, and condiments on restaurant tables, using a straw to drink from bottles, and avoiding salads and buffets where food may have been unrefrigerated for several hours. Travellers should be advised to drink bottled water where available, including in alcoholic drinks, as alcohol does not sterilise non-bottled water. If bottled water is not available, water can be purified by boiling, filtering, or use of chlorine based tablets. 16 There is some weak evidence that use of alcohol hand gel may reduce diarrhoea rates in travellers, 17 but, based on studies in non-travellers, it is reasonable to strongly encourage travellers to adhere to good hand hygiene measures. Two recent systematic reviews estimated hand washing with soap reduces the risk of diarrhoeal illness by 30-40%. 18 19

When is antibiotic prophylaxis recommended?
For most travellers antibiotic chemoprophylaxis (that is, daily antibiotics for the duration of the trip) is not recommended. While diarrhoea is annoying and distressing, severe or long term consequences from a short period of diarrhoea are rare, and routine use of chemoprophylaxis would create a large tablet burden and expose users to possible adverse effects of antibiotic therapy such as candidiasis and diarrhoea associated with Clostridium difficile .
Chemoprophylaxis should be offered to those with severe immune suppression (such as from chemotherapy for malignancy or after a tissue transplant, or advanced HIV infection), underlying intestinal pathology (inflammatory bowel disease, ileostomies, short bowel syndrome), and other conditions such as sickle cell disease or diabetes where reduced oral intake may be particularly dangerous (table 2 ⇓ ). 22 These patient groups may be unable to tolerate the clinical effects and dehydration associated with even mild diarrhoea, or the consequences of more invasive complications such as bacteraemia. For such patients, it is important to discuss the benefits of treatment aimed at preventing diarrhoea and its complications against the risks of antibiotic associated diarrhoea and other side effects. If antibiotics are prescribed then consideration should be given to any possible interactions with other medications that the patient is taking.
Antibiotic chemoprophylaxis options for immunosuppressed or other high risk travellers
A small comparative study in US soldiers showed that malaria prophylaxis with daily doxycycline has the added benefit of reducing rates of travellers’ diarrhoea caused by enterotoxigenic E coli and Campylobacter jejuni . 23
Do vaccines have a role in prevention of travellers’ diarrhoea?
Vaccines have been developed and licensed against Salmonella typhi , Vibrio cholerae , and rotavirus—all with reasonable efficacy. However, unlike enterotoxigenic E coli , none of these is a major cause of travellers’ diarrhoea, and only vaccines against S typhi are recommended for most travellers to endemic settings. Phase 3 trials of enterotoxigenic E coli toxin vaccines have been undertaken but have failed to demonstrate efficacy. 24 Studies suggest vaccines against enterotoxigenic E coli would have a major public health impact in high burden countries, and further candidate vaccines are in development. 25
What are the options for self administered treatment?
Table 3 ⇓ summarises the options for self treatment.
Summary of self treatment choices
Anti-motility agents and oral rehydration therapy
For most cases of travellers’ diarrhoea, oral rehydration is the mainstay of treatment. This can be achieved with clear fluids such as diluted fruit juice or soups. Young children, elderly people, and those at greater risk from dehydration (that is, those with medical comorbidities) are recommended to use oral rehydration salts (or a mixture of six level teaspoons of sugar and half a teaspoon of salt in a litre of clean water if rehydration salts are unavailable) (see http://rehydrate.org/rehydration/index.html ).
Anti-motility agents such as loperamide may be appropriate for mild symptoms, or where rapid cessation of diarrhoea is essential. Case reports of adverse outcomes such as intestinal perforation suggest anti-motility agents should be avoided in the presence of severe abdominal pain or bloody diarrhoea, which can signify invasive colitis. 26 Systematic review of several randomised controlled trials have demonstrated a small benefit from taking bismuth subsalicylate, but this has less efficacy in reducing diarrhoea frequency and severity than loperamide. 27
Antibiotics
Symptomatic treatment is usually adequate and reduces antibiotic use. However, some travellers will benefit from rapid cessation of diarrhoea, particularly if they are in a remote area with limited access to sanitation facilities or healthcare. Several systematic reviews of studies comparing antibiotics (including quinolones, azithromycin, and rifaximin) against placebo have shown consistent shortening of the duration of diarrhoea to about one and a half days from around three days. 28 29 30 Short courses (one to three days) of antibiotics are usually sufficient to effect a cure. 30
For some people travelling to high and moderate risk areas (see box 1) it will be appropriate to provide a short course of a suitable antibiotic, with advice to start treatment as soon as they develop diarrhoea and to keep well hydrated. Choice of antibiotic will depend on allergy history, comorbidities, concomitant medications, and destination. Avoid quinolones for both prophylaxis and treatment of travellers to South East and South Asia as levels of quinolone resistance are high. 31 Azithromycin remains effective in these areas, but resistance rates are likely to increase.
A meta-analysis of nine randomised trials showed that the addition of loperamide to antibiotic treatment (including azithromycin, ciprofloxacin, and rifamixin) resulted in statistically significantly higher rates of cure at 24 and 48 hours compared with antibiotic alone. 32 Travellers can be advised to add loperamide to their antibiotic treatment to reduce the time to symptomatic improvement as long as there are no features of invasive colitis such as severe pain, high fever, or blood visible in the diarrhoea. 30 If any of these symptoms develop, travellers are advised to seek medical advice immediately.
Returned travellers with persistent diarrhoea
Most bacterial causes mentioned do not cause persistent diarrhoea in immune competent adults. Travellers with diarrhoea persisting beyond 14 days may present in primary or secondary care on their return and require assessment for other underlying causes of persistent diarrhoea.
Table 4 ⇓ lists the important clinical history and symptoms that can point to the underlying cause.
Assessment of chronic diarrhoea
What investigations should be sent?
For diarrhoeal symptoms that persist beyond 14 days following travel (or sooner if there are other concerning features such as fever or dysentery), offer patients blood tests for full blood count, liver and renal function, and inflammatory markers; stool samples for microscopy and culture; and examination for ova, cysts, and parasites. Historically, advice has been to send three stool samples for bacterial culture, but this is unlikely to increase the diagnostic yield. Instead, stool microscopy can be used to distinguish inflammatory from non-inflammatory causes: a small observational study found presence of faecal leucocytes was predictive of a positive bacterial stool culture. 33 Yield from stool culture may be increased by dilution of the faecal sample, and the introduction of molecular tests such as polymerase chain reaction (PCR) for common gastrointestinal pathogens such as Campylobacter spp may decrease turnaround times and increase yield. 34
Additional tests should be offered according to symptoms and risk (table 4 ⇑ ). If the patient has eosinophilia and an appropriate travel history, the possibility of schistosomiasis, strongyloides, and other helminthic infections should be considered. While schistosomiasis can rarely cause diarrhoea in the context of acute infection, serology may be negative in the first few months of the illness.
Imaging is required only if the patient has signs of severe colitis or local tenderness, in which instances toxic megacolon, inflammatory phlegmon, and hepatic collections should be excluded. Patients with severe colitis or proctitis may need joint assessment with gastroenterology and consideration of endoscopy, or laparotomy if perforation has occurred.
Where infectious and non-infectious causes have been appropriately excluded, the most likely diagnosis is post-infectious irritable bowel syndrome, although diarrhoea can also herald underlying bowel pathology and anyone with red flags for malignancy should be referred by the appropriate pathway for assessment. Post-infectious irritable bowel syndrome has an incidence of around 30% after an acute episode of travel associated gastroenteritis. 35 36 It is more commonly a sequela of prolonged episodes of diarrhoea or diarrhoea associated with fever and bloody stools. 36 There is weak evidence from small randomised trials suggesting that exclusion of foods high in fermentable carbohydrates (FODMAP) may be helpful. 37 Exclusion of dietary lactose and use of loperamide, bile acid sequestrants, and probiotics can also be tried, but there is limited evidence for long term benefit. 35 37 38
How should giardiasis be managed?
The most common pathogen identified in returning travellers with chronic diarrhoea is Giardia lamblia, particularly among people returning from South Asia. 39 Use of G lamblia PCR testing has increased detection, 40 which potentially will identify infection in some patients previously labelled as having post-infectious irritable bowel syndrome and in those whose diarrhoea may have been attributed to non-pathogenic protozoa. Most patients respond to 5-nitroimidazoles (a systematic review of a large number of trials has shown similar cure rates with tinidazole 2 g once only or metronidazole 400 mg three times daily for five days 41 ), but refractory cases are increasingly common and require investigation, identification of underlying risk factors, and repeated treatment (various antimicrobials have been shown to be effective but may have challenging risk profiles). .
Questions for future research
What is the justification for using antibiotics to treat a usually self limiting illness, in the wider context of rising levels of global antimicrobial resistance rates? What is the clinical impact of resistant enterobacteriaciae found in stool samples from returning travellers? 42 43
To what extent do host genetic factors increase susceptibility to gastrointestinal pathogens, and can this help to identify at risk populations and tailor treatments to individual patients?
What is the long term efficacy of new pharmacological treatments such as selective serotonin reuptake inhibitors and rifaximin in post-infectious irritable bowel syndrome?
Tips for non-specialists
Include consideration of chemoprophylaxis for high risk individuals in pre-travel assessment
Advise all travellers on hygiene measures (such as hand washing and food consumption) and symptom management of diarrhoea
Avoid quinolones for prophylaxis or treatment in travellers to South East and South Asia
Where diarrhoea persists beyond 14 days, consider investigations to rule out parasitic and non-infectious causes. The presence of white blood cells on stool microscopy indicates an inflammatory cause
Additional educational resources
Resources for patients.
National Travel Health Network and Centre (NaTHNaC): http://travelhealthpro.org.uk/travellers-diarrhoea/
Provides pre-travel advice, as well as links to country-specific advice
Fit for Travel: www.fitfortravel.nhs.uk/advice/disease-prevention-advice/travellers-diarrhoea.aspx
Provides similar pre-travel advice on hygiene and disease prevention
Patient.co.uk: http://patient.info/doctor/travellers-diarrhoea-pro
Has patient leaflets and more detailed information about investigation and management of travellers’ diarrhoea
Resources for healthcare professionals
Centers for Disease Control and Prevention yellow book: http://wwwnc.cdc.gov/travel/yellowbook/2016/the-pre-travel-consultation/travelers-diarrhea
Provides a guide to pre-travel couselling
Rehydration Project website: http://rehydrate.org/rehydration/index.html
Has additional information about non-pharmacological management of diarrhoea
How patients were involved in the creation of the article
No patients were involved in the creation of this review.
Contributors: Both authors contributed equally to the preparation of this manuscript. MB is guarantor. We thank Dr Ron Behrens for sharing his extensive expertise on this subject.
Competing interests: We have read and understood BMJ policy on declaration of interests and have no relevant interests to declare.
Provenance and peer review: Commissioned; externally peer reviewed.
- ↵ Greenwood Z, Black J, Weld L, et al. GeoSentinel Surveillance Network. Gastrointestinal infection among international travelers globally. J Travel Med 2008 ; 15 : 221 - 8 . doi:10.1111/j.1708-8305.2008.00203.x pmid:18666921 . OpenUrl Abstract / FREE Full Text
- ↵ Schlagenhauf P, Weld L, Goorhuis A, et al. EuroTravNet. Travel-associated infection presenting in Europe (2008-12): an analysis of EuroTravNet longitudinal, surveillance data, and evaluation of the effect of the pre-travel consultation. Lancet Infect Dis 2015 ; 15 : 55 - 64 . doi:10.1016/S1473-3099(14)71000-X pmid:25477022 . OpenUrl CrossRef PubMed
- ↵ Health Protection Agency. Foreign travel-associated illness: a focus on travellers’ diarrhoea. HPA, 2010. http://webarchive.nationalarchives.gov.uk/20140714084352/http:/www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1287146380314 .
- ↵ Schindler VM, Jaeger VK, Held L, Hatz C, Bühler S. Travel style is a major risk factor for diarrhoea in India: a prospective cohort study. Clin Microbiol Infect 2015 ; 21 : 676.e1 - 4 . doi:10.1016/j.cmi.2015.03.005 pmid:25882361 . OpenUrl CrossRef
- ↵ Freeland AL, Vaughan GH Jr, , Banerjee SN. Acute gastroenteritis on cruise ships - United States, 2008-2014. MMWR Morb Mortal Wkly Rep 2016 ; 65 : 1 - 5 . doi:10.15585/mmwr.mm6501a1 pmid:26766396 . OpenUrl PubMed
- ↵ DuPont HL, Ericsson CD, Farthing MJ, et al. Expert review of the evidence base for prevention of travelers’ diarrhea. J Travel Med 2009 ; 16 : 149 - 60 . doi:10.1111/j.1708-8305.2008.00299.x pmid:19538575 . OpenUrl Abstract / FREE Full Text
- ↵ Bavishi C, Dupont HL. Systematic review: the use of proton pump inhibitors and increased susceptibility to enteric infection. Aliment Pharmacol Ther 2011 ; 34 : 1269 - 81 . doi:10.1111/j.1365-2036.2011.04874.x pmid:21999643 . OpenUrl CrossRef PubMed
- ↵ Pitzurra R, Steffen R, Tschopp A, Mutsch M. Diarrhoea in a large prospective cohort of European travellers to resource-limited destinations. BMC Infect Dis 2010 ; 10 : 231 . doi:10.1186/1471-2334-10-231 pmid:20684768 . OpenUrl CrossRef PubMed
- ↵ Flores J, Okhuysen PC. Genetics of susceptibility to infection with enteric pathogens. Curr Opin Infect Dis 2009 ; 22 : 471 - 6 . doi:10.1097/QCO.0b013e3283304eb6 pmid:19633551 . OpenUrl CrossRef PubMed
- ↵ Shah N, DuPont HL, Ramsey DJ. Global etiology of travelers’ diarrhea: systematic review from 1973 to the present. Am J Trop Med Hyg 2009 ; 80 : 609 - 14 . pmid:19346386 . OpenUrl Abstract / FREE Full Text
- ↵ von Sonnenburg F, Tornieporth N, Waiyaki P, et al. Risk and aetiology of diarrhoea at various tourist destinations. Lancet 2000 ; 356 : 133 - 4 . doi:10.1016/S0140-6736(00)02451-X pmid:10963251 . OpenUrl CrossRef PubMed Web of Science
- ↵ Steffen R, Collard F, Tornieporth N, et al. Epidemiology, etiology, and impact of traveler’s diarrhea in Jamaica. JAMA 1999 ; 281 : 811 - 7 . doi:10.1001/jama.281.9.811 pmid:10071002 . OpenUrl CrossRef PubMed Web of Science
- ↵ Nichols GL, Freedman J, Pollock KG, et al. Cyclospora infection linked to travel to Mexico, June to September 2015. Euro Surveill 2015 ; 20 . doi:10.2807/1560-7917.ES.2015.20.43.30048 pmid:26536814 .
- ↵ Steffen R, Collard F, Tornieporth N, et al. Epidemiology, etiology, and impact of traveler’s diarrhea in Jamaica. JAMA. 1999 ; 281 : 811 - 7 . doi:10.1001/jama.281.9.811 pmid:10071002 . OpenUrl CrossRef PubMed Web of Science
- ↵ DuPont HL. Systematic review: prevention of travellers’ diarrhoea. Aliment Pharmacol Ther 2008 ; 27 : 741 - 51 . doi:10.1111/j.1365-2036.2008.03647.x pmid:18284650 . OpenUrl CrossRef PubMed Web of Science
- ↵ Clasen TF, Alexander KT, Sinclair D, et al. Interventions to improve water quality for preventing diarrhoea. Cochrane Database Syst Rev 2015 ; 10 : CD004794 . pmid:26488938 . OpenUrl PubMed
- ↵ Henriey D, Delmont J, Gautret P. Does the use of alcohol-based hand gel sanitizer reduce travellers’ diarrhea and gastrointestinal upset?: A preliminary survey. Travel Med Infect Dis 2014 ; 12 : 494 - 8 . doi:10.1016/j.tmaid.2014.07.002 pmid:25065273 . OpenUrl CrossRef PubMed
- ↵ Ejemot-Nwadiaro RI, Ehiri JE, Arikpo D, Meremikwu MM, Critchley JA. Hand washing promotion for preventing diarrhoea. Cochrane Database Syst Rev 2015 ; 9 : CD004265 . pmid:26346329 . OpenUrl PubMed
- ↵ Freeman MC, Stocks ME, Cumming O, et al. Hygiene and health: systematic review of handwashing practices worldwide and update of health effects. Trop Med Int Health 2014 ; 19 : 906 - 16 . doi:10.1111/tmi.12339 pmid:24889816 . OpenUrl CrossRef PubMed
- Hu Y, Ren J, Zhan M, Li W, Dai H. Efficacy of rifaximin in prevention of travelers’ diarrhea: a meta-analysis of randomized, double-blind, placebo-controlled trials. J Travel Med 2012 ; 19 : 352 - 6 . doi:10.1111/j.1708-8305.2012.00650.x pmid:23379704 . OpenUrl Abstract / FREE Full Text
- Alajbegovic S, Sanders JW, Atherly DE, Riddle MS. Effectiveness of rifaximin and fluoroquinolones in preventing travelers’ diarrhea (TD): a systematic review and meta-analysis. Syst Rev 2012 ; 1 : 39 . doi:10.1186/2046-4053-1-39 pmid:22929178 . OpenUrl CrossRef PubMed
- ↵ Sommet J, Missud F, Holvoet L, et al. Morbidity among child travellers with sickle-cell disease visiting tropical areas: an observational study in a French tertiary care centre. Arch Dis Child 2013 ; 98 : 533 - 6 . doi:10.1136/archdischild-2012-302500 pmid:23661574 . OpenUrl Abstract / FREE Full Text
- ↵ Arthur JD, Echeverria P, Shanks GD, Karwacki J, Bodhidatta L, Brown JE. A comparative study of gastrointestinal infections in United States soldiers receiving doxycycline or mefloquine for malaria prophylaxis. Am J Trop Med Hyg 1990 ; 43 : 608 - 13 . pmid:2267964 . OpenUrl Abstract / FREE Full Text
- ↵ Behrens RH, Cramer JP, Jelinek T, et al. Efficacy and safety of a patch vaccine containing heat-labile toxin from Escherichia coli against travellers’ diarrhoea: a phase 3, randomised, double-blind, placebo-controlled field trial in travellers from Europe to Mexico and Guatemala. Lancet Infect Dis 2014 ; 14 : 197 - 204 . doi:10.1016/S1473-3099(13)70297-4 pmid:24291168 . OpenUrl CrossRef PubMed
- ↵ Bourgeois AL, Wierzba TF, Walker RI. Status of vaccine research and development for enterotoxigenic Escherichia coli. Vaccine 2016 ; S0264-410X(16)00287-5 . pmid:26988259 .
- ↵ McGregor A, Brown M, Thway K, Wright SG. Fulminant amoebic colitis following loperamide use. J Travel Med 2007 ; 14 : 61 - 2 . doi:10.1111/j.1708-8305.2006.00096.x pmid:17241255 . OpenUrl Abstract / FREE Full Text
- ↵ Heather CS. Travellers’ diarrhoea. Systematic review 901. BMJ Clin Evid 2015 www.clinicalevidence.com/x/systematic-review/0901/overview.html .
- ↵ De Bruyn G, Hahn S, Borwick A. Antibiotic treatment for travellers’ diarrhoea. Cochrane Database Syst Rev 2000 ;( 3 ): CD002242 . pmid:10908534 .
- ↵ Ternhag A, Asikainen T, Giesecke J, Ekdahl K. A meta-analysis on the effects of antibiotic treatment on duration of symptoms caused by infection with Campylobacter species. Clin Infect Dis 2007 ; 44 : 696 - 700 . doi:10.1086/509924 pmid:17278062 . OpenUrl Abstract / FREE Full Text
- ↵ Steffen R, Hill DR, DuPont HL. Traveler’s diarrhea: a clinical review. JAMA 2015 ; 313 : 71 - 80 . doi:10.1001/jama.2014.17006 pmid:25562268 . OpenUrl CrossRef PubMed
- ↵ Dalhoff A. Global fluoroquinolone resistance epidemiology and implictions for clinical use. Interdiscip Perspect Infect Dis 2012 ; 2012 : 976273 . pmid:23097666 . OpenUrl CrossRef PubMed
- ↵ Riddle MS, Arnold S, Tribble DR. Effect of adjunctive loperamide in combination with antibiotics on treatment outcomes in traveler’s diarrhea: a systematic review and meta-analysis. Clin Infect Dis 2008 ; 47 : 1007 - 14 . doi:10.1086/591703 pmid:18781873 . OpenUrl Abstract / FREE Full Text
- ↵ McGregor AC, Whitty CJ, Wright SG. Geographic, symptomatic and laboratory predictors of parasitic and bacterial causes of diarrhoea in travellers. Trans R Soc Trop Med Hyg 2012 ; 106 : 549 - 53 . doi:10.1016/j.trstmh.2012.04.008 pmid:22818743 . OpenUrl Abstract / FREE Full Text
- ↵ Public Health England. Investigations of faecal specimens for enteric pathogens. UK Standards for Microbiology Investigations. B 30 Issue 8.1. 2014. www.hpa.org.uk/SMI/pdf .
- ↵ DuPont AW. Postinfectious irritable bowel syndrome. Clin Infect Dis 2008 ; 46 : 594 - 9 . doi:10.1086/526774 pmid:18205536 . OpenUrl Abstract / FREE Full Text
- ↵ Schwille-Kiuntke J, Mazurak N, Enck P. Systematic review with meta-analysis: post-infectious irritable bowel syndrome after travellers’ diarrhoea. Aliment Pharmacol Ther 2015 ; 41 : 1029 - 37 . doi:10.1111/apt.13199 pmid:25871571 . OpenUrl CrossRef PubMed
- ↵ Halland M, Saito YA. Irritable bowel syndrome: new and emerging treatments. BMJ 2015 ; 350 : h1622 . doi:10.1136/bmj.h1622 pmid:26088265 . OpenUrl Abstract / FREE Full Text
- ↵ Orekoya O, McLaughlin J, Leitao E, Johns W, Lal S, Paine P. Quantifying bile acid malabsorption helps predict response and tailor sequestrant therapy. Clin Med (Lond) 2015 ; 15 : 252 - 7 . doi:10.7861/clinmedicine.15-3-252 pmid:26031975 . OpenUrl CrossRef PubMed
- ↵ Swaminathan A, Torresi J, Schlagenhauf P, et al. GeoSentinel Network. A global study of pathogens and host risk factors associated with infectious gastrointestinal disease in returned international travellers. J Infect 2009 ; 59 : 19 - 27 . doi:10.1016/j.jinf.2009.05.008 pmid:19552961 . OpenUrl CrossRef PubMed Web of Science
- ↵ Nabarro LE, Lever RA, Armstrong M, Chiodini PL. Increased incidence of nitroimidazole-refractory giardiasis at the Hospital for Tropical Diseases, London: 2008-2013. Clin Microbiol Infect 2015 ; 21 : 791 - 6 . doi:10.1016/j.cmi.2015.04.019 pmid:25975511 . OpenUrl CrossRef PubMed
- ↵ Pasupuleti V, Escobedo AA, Deshpande A, Thota P, Roman Y, Hernandez AV. Efficacy of 5-nitroimidazoles for the treatment of giardiasis: a systematic review of randomized controlled trials. PLoS Negl Trop Dis 2014 ; 8 : e2733 . doi:10.1371/journal.pntd.0002733 pmid:24625554 . OpenUrl CrossRef PubMed
- ↵ Tham J, Odenholt I, Walder M, Brolund A, Ahl J, Melander E. Extended-spectrum beta-lactamase-producing Escherichia coli in patients with travellers’ diarrhoea. Scand J Infect Dis 2010 ; 42 : 275 - 80 . doi:10.3109/00365540903493715 pmid:20121649 . OpenUrl CrossRef PubMed
- ↵ Kantele A. A call to restrict prescribing antibiotics for travellers’ diarrhea--Travel medicine practitioners can play an active role in preventing the spread of antimicrobial resistance. Travel Med Infect Dis 2015 ; 13 : 213 - 4 . doi:10.1016/j.tmaid.2015.05.005 pmid:26005160 . OpenUrl CrossRef PubMed
- Destinations
- Traveler Library
Travelers' Diarrhea
On this page, introduction, transmission, risk factors, consequences of infection, need for medical assistance, self-diagnosis and self-treatment, traveler summary.
- Travelers' diarrhea (TD), the most common health problem for travelers, is an intestinal infection affecting up to 70% of travelers going to developing countries.
- Risk is higher for young adults, persons with underlying illnesses, and those taking medicines that decrease gastric acidity.
- Symptoms can vary from mild to severe and can include uncomfortable, crampy diarrhea with nausea or vomiting; fever sometimes occurs. Significant dehydration is uncommon in adults.
- Consequences of infection may include persistent diarrhea, recurrent diarrhea, and other chronic gastrointestinal discomfort.
- Prevention includes observing food and beverage precautions and hand hygiene (frequent, thorough handwashing) and treating water.
No vaccine is available in the US, and preventive antibiotics are not recommended. A vaccine with limited effectiveness is available in some countries but is not recommended.
- Self-treatment includes fluid rehydration and antimotility or antisecretory agents. Travelers should reserve the use of antibiotics for severe diarrhea.
TD is the most common health problem for travelers, affecting up to 70% of travelers going to some developing countries. TD is caused primarily by bacteria (uncommonly by parasites or viruses) acquired through consumption of contaminated food or beverages. TD is characterized by the sudden onset of abnormally loose or liquid stools, such that the illness is either tolerable, interferes with many planned activities, or is incapacitating and prevents all planned activities. TD is usually a self-limiting disease that resolves in 3 to 4 days, but strategies are available to self-treat and shorten the duration of symptoms.
The traveler’s destination is the most important determinant of risk. TD can be acquired whenever people from countries with a high level of hygiene travel to countries with a low level of hygiene. Developing countries in Africa, Asia, Latin America, and the Middle East are considered high risk. Most countries in southern Europe and a few Caribbean islands are deemed intermediate risk. Low-risk areas include Australia, Canada, northern Europe, Japan, New Zealand, the US, and several of the Caribbean islands.
Poor sanitation, the presence of stool in the environment, and the absence of safe restaurant practices lead to risk of diarrhea from eating a variety of foods contaminated by fecal organisms, especially bacteria. Because travelers are usually careful to avoid drinking untreated water, many acquire TD from eating contaminated food. In long-stay travelers and expatriates who tend to eat adventurously for longer periods of time, parasites can account for 10% to 20% of diarrhea. Persons with a vomiting predominant illness, with or without diarrhea, may have a norovirus infection (especially if other close individuals have a similar illness) and are highly infectious for others sharing living quarters or bathroom facilities.
Individuals at high risk for TD or adverse consequences include young adults (prone to risk-taking behavior and often on limited budgets); persons with compromised immunity, inflammatory bowel disease, or diabetes; and those taking medicines (e.g., omeprazole) that decrease gastric acidity.
TD caused by bacteria typically presents with abrupt onset of uncomfortable, crampy diarrhea and may be accompanied by nausea or vomiting and, less commonly, fever. TD caused by parasites is usually mild and begins gradually with loose stools occurring in distinct episodes during the day, slowly becoming more bothersome and associated with fatigue. Significant dehydration is uncommon in adults. Persons with protozoal infections often do not seek medical care for several weeks due to the generally mild nature of the symptoms.
Persistent diarrhea, recurrent diarrhea, and other chronic gastrointestinal discomfort (e.g., bloating, gas, constipation) may occur as a result of TD. When diagnostic testing yields no other diagnoses, these chronic gastrointestinal symptoms may be attributed to "postinfectious irritable bowel syndrome."
Persons who develop bloody stools or severe symptoms such as intense cramps, fever and chills, or severe thirst (with inability to keep liquids down) that do not rapidly improve with self-treatment should seek medical attention. Illnesses unresponsive to self-treatment will require specific investigation for possible protozoal causes.
Immediate medical care is imperative if an infant or child shows signs of severe dehydration, bloody diarrhea, fever higher than 38.5°C (101.5°F), or persistent vomiting.
Food and Beverage Precautions
Guaranteeing the safety of food and beverages is difficult if not impossible when traveling, especially in developing countries. Nevertheless, travelers can continue to enjoy local foods, which is part of the pleasure of international travel; however, completely avoiding diarrhea in certain high-risk destinations may not be possible, even with the strictest adherence to preventive measures. Although some evidence exists to suggest that where food is eaten is more important than what food is eaten, observing food and beverage precautions helps minimize risk and decreases the number of organisms ingested and the severity of TD if contracted. These precautions also help reduce the risk of other infections, such as dysentery, hepatitis A and E, giardiasis, typhoid, and paratyphoid.
Developing countries don't always have the resources needed to ensure a pure water supply; consequently, tap water is not safe to drink because bacteria or parasites in food or water may go undetected. Even if the local population can drink the water, travelers should not assume that they can. Residents have built up some immunity to organisms in the water, but visitors have not.
See the following articles: Food and Beverage Precautions and Treating Water .
The decision to self-treat depends on the severity of the functional disability caused by TD. Increased fluid intake is necessary to correct dehydration. Most cases will resolve with hydration and symptomatic treatment with antimotility or antisecretory agents (see Nonantibiotic Agents , under Drug Treatment). Adding antibiotics for moderate TD may shorten the duration or severity of illness. All severe TD cases should receive antibiotics.
Discuss self-treatment options with a health care provider to obtain appropriate medications for a personal medical kit for travel. A strategy for self-treatment of TD under different circumstances is shown in Table 1.
Fluid and Dietary Management
TD in adults is not typically associated with clinically significant dehydration, but replacement of fluids that are lost remains a cornerstone of self-treatment. Mild dehydration can be corrected with any fluid, and a patient should drink any available appropriate fluid until oral rehydration solution (ORS) is obtained. ORS is designed to be rapidly absorbed from the intestine, thus it can be useful even in the presence of vomiting. If an ORS is thought to be indicated, many stores and pharmacies in developing countries carry ORS packets. Travelers going to remote areas should carry their own ORS packets. If not hungry, the ill traveler should drink fluids and not force food. If hungry, eating is encouraged, but avoid alcohol, coffee, strong tea, spicy food, greasy food, and dairy products.
For treating dehydration in children, the following recommendations for use of ORS should be followed:
- Severe dehydration, bloody diarrhea, fever higher than 38.5°C (101.5°F), or persistent vomiting: Immediate medical care is imperative for infants and children.
- Mild to moderate dehydration: Give 60 to 120 mL (2-4 oz) of ORS for every loose stool or vomiting episode to an infant weighing less than 10 kg (22 lb), and give 120 to 240 mL (4-8 oz) to children weighing more than 10 kg.
- Recovery period: Introduce a normal diet as quickly as the child will accept it. Use of specific, restrictive, or liquid diets or withholding food is not necessary.
Drug Treatment
Nonantibiotic agents.
Loperamide (an antimotility drug), which is available over-the-counter, appears to be safer than diphenoxylate (Lomotil), a prescription medicine. Take 4 mg initially; if mild diarrhea continues, take an additional 2 mg every 6 hours, not to exceed 8 mg/day for over-the-counter use and 16 mg/day by prescription; the latter accounts for physician screening for patient contraindications. For children aged ≥ 2 years, loperamide may dosed at 0.25 mg/kg/day when the modest benefit of a 1-day reduction in the duration of diarrhea is worth the slight risk of an adverse event. Taking higher than the recommended dose of loperamide can cause cardiac adverse events that may result in death in significant overdoses.
Antimotility agents sometimes induce prolonged constipation, even at low doses, and can lead to a bloated, uncomfortable feeling if taken for moderately severe infections without taking an antibiotic as well. Use of these agents should be discontinued if symptoms last more than 48 hours. Loperamide should not be taken by travelers with fever or with bloody stool. Antisecretory agents, such as bismuth subsalicylate (BSS; i.e., Pepto-Bismol and the US formulation of Kaopectate), can also improve some symptoms of TD.
Antibiotics
Travelers are often in areas where prompt, effective medical care is unavailable. Therefore, self-treatment of bacterial diarrhea with antibiotics prescribed and purchased prior to leaving for the trip may be more practical. The use of antibiotics can turn a 3- or 4-day illness into a 1-day illness. However, antibiotic use for TD increases the intestinal carriage of antibiotic-resistant bacteria in returning travelers, especially in South Asia where 80% of travelers treated with antibiotics acquired resistant bacteria. Antibiotic choice for the treatment of moderate (antibiotics discouraged) and severe TD in adults is shown in Table 2.
Antiparasitic Drugs
In general, patients should not carry these medicines for self-treatment. See a health care provider because a proper diagnosis for parasitic infection is necessary, and these medicines are administered under supervision. Travelers going to extremely remote locations or on long trips may be given tinidazole to carry on a case-by-case basis.

JOHNNIE YATES, M.D.
Am Fam Physician. 2005;71(11):2095-2100
Patient Information: Seen related handout on traveler’s diarrhea , written by the author of this article.
Acute diarrhea affects millions of persons who travel to developing countries each year. Food and water contaminated with fecal matter are the main sources of infection. Bacteria such as enterotoxigenic Escherichia coli , enteroaggregative E. coli , Campylobacter, Salmonella, and Shigella are common causes of traveler’s diarrhea. Parasites and viruses are less common etiologies. Travel destination is the most significant risk factor for traveler’s diarrhea. The efficacy of pretravel counseling and dietary precautions in reducing the incidence of diarrhea is unproven. Empiric treatment of traveler’s diarrhea with antibiotics and loperamide is effective and often limits symptoms to one day. Rifaximin, a recently approved antibiotic, can be used for the treatment of traveler’s diarrhea in regions where noninvasive E. coli is the predominant pathogen. In areas where invasive organisms such as Campylobacter and Shigella are common, fluoroquinolones remain the drug of choice. Azithromycin is recommended in areas with quinolone-resistant Campylobacter and for the treatment of children and pregnant women.
Acute diarrhea is the most common illness among travelers. Up to 55 percent of persons who travel from developed countries to developing countries are affected. 1 , 2 A study 3 of Americans visiting developing countries found that 46 percent acquired diarrhea. The classic definition of traveler’s diarrhea is three or more unformed stools in 24 hours with at least one of the following symptoms: fever, nausea, vomiting, abdominal cramps, tenesmus, or bloody stools. Milder forms can present with fewer than three stools (e.g., an abrupt bout of watery diarrhea with abdominal cramps). Most cases occur within the first two weeks of travel and last about four days without treatment. 1 , 3 Although traveler’s diarrhea rarely is life threatening, it can result in significant morbidity; one in five travelers with diarrhea is bedridden for a day and more than one third have to alter their activities. 1 , 3
Destination is the most significant risk factor for developing traveler’s diarrhea. 1 – 4 Regions with the highest risk are Africa, South Asia, Latin America, and the Middle East. Travelers who are immunocompromised and those with lowered gastric acidity (e.g., patients taking histamineH 2 blockers or proton pump inhibitors) are more susceptible to traveler’s diarrhea. Recently, a genetic susceptibility has been demonstrated. 5 Younger age and adventurous travel increase the risk of developing traveler’s diarrhea, 3 , 6 but persons staying at luxury resorts or on cruise ships also are at risk. 7 , 8
Food and water contaminated with fecal matter are the main reservoirs for the pathogens that cause traveler’s diarrhea. Unsafe foods and beverages include salads, unpeeled fruits, raw or poorly cooked meats and seafood, unpasteurized dairy products, and tap water. Eating in restaurants increases the probability of contracting traveler’s diarrhea 6 and food from street vendors is particularly risky. 9 , 10 Cold sauces, salsas, and foods that are cooked and then reheated also are risky. 6 , 11
In contrast to the largely viral etiology of gastroenteritis in the United States, diarrhea acquired in developing countries is caused mainly by bacteria 1 , 4 , 6 , 12 ( Table 1 ) . Enterotoxigenic Escherichia coli is the pathogen most frequently isolated, but other types of E. coli such as enteroaggregative E. coli have been recognized as common causes of traveler’s diarrhea. 13 Invasive pathogens such as Campylobacter, Shigella, and non-typhoid Salmonella are relatively common depending on the region, while Aeromonas and non-cholera Vibrio species are encountered less frequently.
Protozoal parasites such as Giardia lamblia , Entamoeba histolytica , and Cyclospora cayetanensis are uncommon causes of traveler’s diarrhea, but increase in importance when diarrhea lasts for more than two weeks. 14 Parasites are diagnosed more frequently in returning travelers because of longer incubation periods (often one to two weeks) and because bacterial pathogens may have been treated with antibiotics. Rotavirus and noroviruses are infrequent causes of traveler’s diarrhea, although noroviruses have been responsible for outbreaks on cruise ships.
The prevalence of specific organisms varies with travel destination. 1 , 4 , 12 , 13 , 15 Available data suggest that E. coli is the predominant cause of traveler’s diarrhea in Latin America, the Caribbean, and Africa, while invasive pathogens are relatively uncommon. Enterotoxigenic E. coli and enteroaggregative E. coli may be responsible for up to 71 percent of cases of traveler’s diarrhea in Mexico. 13 In contrast, Campylobacter is a leading cause of traveler’s diarrhea in Thailand 15 – 17 and also is common in Nepal. 6 Regional variation also exists with parasitic causes of traveler’s diarrhea ( Table 2 ) . 12 , 13 For example, Cyclospora is endemic in Nepal, Peru, and Haiti.
Food poisoning is part of the differential diagnosis of traveler’s diarrhea. Gastroenteritis from preformed toxins (e.g., Staphylococcus aureus , Bacillus cereus ) is characterized by a short incubation period (one to six hours), and symptoms typically resolve within 24 hours. 18 Seafood ingestion syndromes such as diarrhetic shellfish poisoning, ciguatera poisoning, and scombroid poisoning also can cause diarrhea in travelers. These syndromes can be distinguished from traveler’s diarrhea by symptoms such as perioral numbness and reversal of temperature sensation (ciguatera poisoning) or flushing and warmth (scombroid poisoning). 19
Although travelers often are advised to “Boil it, cook it, peel it, or forget it,” data on the effectiveness of dietary precautions in preventing traveler’s diarrhea are inconclusive. 3 , 6 , 20 Many travelers find it difficult to adhere to dietary recommendations. 21 In a study 3 of American travelers, nearly one half developed diarrhea despite pretravel advice on avoidance measures; even persons who strictly followed dietary recommendations developed diarrhea. Avoiding high-risk foods and adventuresome eating behaviors may reduce the inoculum of ingested pathogens or prevent the development of other enteric diseases such as typhoid and hepatitis A and E.
Boiling is the best way to purify water. Iodination or chlorination is acceptable but does not kill Cryptosporidium or Cyclospora, and increased contact time is required to kill Giardia in cold or turbid water. 22 Filters with iodine resins generally are effective in purifying water, although it is uncertain whether the contact time with the resin is sufficient to kill viruses. Bottled water generally is safe if the cap and seal are intact.
DRUG PROPHYLAXIS
Antibiotic prophylaxis is not recommended by the Centers for Disease Control and Prevention (CDC) even for high-risk travelers because it can lead to drug-resistant organisms and may give travelers a false sense of security. Although antibiotic prophylaxis does not prevent viral or parasitic infection, some health care professionals believe that it may be an option for travelers who are at high risk of developing traveler’s diarrhea and related complications (e.g., immunocompromised persons). Prophylaxis with fluoroquinolones is up to 90 percent effective. 23 Rifaximin (Xifaxan) may prove to be the preferred antibiotic because it is not absorbed and is well tolerated, although data on its effectiveness for prophylaxis have not yet been published.
Bismuth subsalicylate (Pepto-Bismol) provides a rate of protection of about 60 percent against traveler’s diarrhea. 24 However, it is not recommended for persons taking anticoagulants or other salicylates. Because bismuth subsalicylate interferes with the absorption of doxycycline (Vibramycin), it should not be taken by travelers using doxycycline for malaria prophylaxis. Travelers should be warned about possible reversible side effects of bismuth subsalicylate, such as a black tongue, dark stools, and tinnitus.
Probiotics are a more natural approach to prophylaxis of traveler’s diarrhea. Probiotics colonize the gastrointestinal tract and theoretically prevent pathogenic organisms from infecting the gut. Studies 25 , 26 of Lactobacillus GG (Culturelle) have suggested protection rates of up to 47 percent. More studies are needed to confirm the efficacy of probiotic prophylaxis. Agents for the prophylaxis of traveler’s diarrhea are summarized in Table 3 .
Empiric Treatment
Counseling travelers about food precautions does not eliminate the risk of traveler’s diarrhea, and nonantibiotic prophylaxis requires frequent dosing to achieve only a modest reduction in risk. In addition, the traveler with diarrhea may have difficulty accessing medical care, the quality of care may be poor, and the quality of medications purchased abroad may be substandard. 27 However, because antibiotics reduce the duration and severity of traveler’s diarrhea and generally are well tolerated, 28 providing the traveler with the means for empiric self-treatment can effectively reduce morbidity from traveler’s diarrhea.
Waiting 24 hours to confirm the diagnosis of traveler’s diarrhea results in unnecessary discomfort and time away from activities. Therapy can be initiated after the first episode of “distressing” diarrhea (i.e., diarrhea that is uncomfortable or interferes with activities). 29 , 30 If symptoms resolve within 24 hours, no further treatment is necessary. 31 , 32 If diarrhea persists after one day, treatment should be continued for one or two more days. An algorithm for the treatment of traveler’s diarrhea is presented in Figure 1 . 33 , 34
Antibiotic selection is based on the likelihood that an invasive organism is present and on antibiotic resistance patterns. These factors are determined largely by travel destination. Although blood in the stool suggests invasive disease, fever is not a sensitive indicator of dysentery. Fluoroquinolones have been the drug of choice for traveler’s diarrhea in most parts of the world because of their efficacy against most enteropathogens. Rifaximin recently became available for the treatment of noninvasive diarrhea caused by E. coli . For persons traveling to destinations where noninvasive E. coli is the predominant pathogen (e.g., Mexico), rifaximin is a good choice. 35 , 36
In regions where invasive pathogens are responsible for a significant proportion of traveler’s diarrhea, quinolones should be used. Azithromycin (Zithromax) is recommended in places where quinoloneresistant Campylobacter is prevalent (e.g., Thailand). 15 , 16 Antibiotics used for the treatment of traveler’s diarrhea are listed in Table 4 . 16 , 32 , 37 Trimethoprim-sulfamethoxazole (Bactrim, Septra) and doxycycline are no longer recommended because of the development of widespread resistance. 12
Therapy that involves an antibiotic with loperamide (Imodium) often limits symptoms to one day. 38 , 39 Loperamide has antimotility and antisecretory effects and is taken as two 2–mg tablets after the first loose stool, followed by one tablet after each subsequent loose stool (maximum of 8 mg in 24 hours for two days). The use of loperamide in dysentery has been controversial because of concerns about prolonging illness, but it is now considered safe when combined with an antibiotic. 29 , 34 , 38 A conservative approach would be to use loperamide for dysentery only if combined with an antibiotic and if the traveler has a long trip or will have no toilet access.
Oral rehydration solutions generally are unnecessary in adults younger than 65 years. 40 However, all travelers with diarrhea should be encouraged to drink plenty of fluids and to replace lost electrolytes using foods such as salt crackers or broth.
Traveler’s Diarrhea in Infants, Children, and Pregnant Women
Traveler’s diarrhea is more common in young children than in adults, and they have a higher risk of dehydration and severe illness. 41 Parents should seek immediate medical attention if their child shows signs of moderate to severe dehydration, bloody diarrhea, a temperature higher than 39°C (102°F), or persistent vomiting. Few data exist on the treatment of diarrhea in children. The use of oral rehydration solutions is essential, and parents should include prepackaged packets (to be mixed with safe water) in their travel kits. These packets are available in camping stores in the United States or in pharmacies in other countries.
Because infants and toddlers normally can have three or more loose stools, an alternate definition of diarrhea in this age group is a twofold increase in the frequency of unformed stool. 37 Nursing infants should continue to breastfeed on demand, and infants and older children should be offered their usual food.
Fluoroquinolones are not approved by the U.S. Food and Drug Administration (FDA) for use in children, and rifaximin is approved only for children 12 years and older. Therefore, azithromycin is the drug of choice for most children with traveler’s diarrhea. 37 Another option is nalidixic acid (Neggram) in a dosage of 55 mg per kg per day divided into four doses, not to exceed 1 g in 24 hours. 37 Loperamide is approved for children older than two years, but should not be used in children with dysentery. Bismuth subsalicylate should be avoided for prophylaxis in children because of the possible risk of Reye’s syndrome.
Pregnant women may be at higher risk of traveler’s diarrhea than nonpregnant women because of lowered gastric acidity and increased gastrointestinal transit time. 42 Quinolones (FDA pregnancy category C) generally are not advised during pregnancy, but azithromycin (FDA pregnancy category B) is safe. Oral rehydration should be emphasized. Although rifaximin is not absorbed, the safety of this medication in pregnant women has not been established. Loperamide (FDA pregnancy category B) may be used, but bismuth subsalicylate (FDA pregnancy category D) should be avoided. Being careful with food and water is particularly important during pregnancy because infections such as listeriosis can cause miscarriage, and hepatitis E can result in maternal mortality.
Complications
Dehydration is the main complication of traveler’s diarrhea, especially in children and older adults. Because E. coli O157:H7 is a rare cause of traveler’s diarrhea, there is little risk of hemolyticuremic syndrome. Other complications include Guillain-Barré syndrome after Campylobacter enteritis, Reiter’s syndrome (especially in persons who are HLA-B27 positive), Clostridium difficile colitis after antibiotic use, and postinfectious irritable bowel. These conditions may appear after the traveler has returned home.
If diarrhea persists despite antibiotic treatment, medical attention should be sought. Parasitic causes should be suspected in travelers who return with prolonged diarrhea or who do not respond to antibiotics. For those traveling to remote areas for extended periods, it is reasonable to discuss empiric treatment of protozoal infections (e.g., metronidazole [Flagyl] 250 mg three times a day for five days or tinidazole [Fasigyn] in a single 2–g dose for Giardia). 43
Resources such as the Travelers’ Health section of the CDC Web site ( http://www.cdc.gov/travel/diarrhea.htm ) or commercial sites such as Travel Health Online ( http://www.tripprep.com ) can keep physicians up to date on the epidemiology and resistance patterns of traveler’s diarrhea. Better preventive and prophylactic strategies will be needed until newer antibiotics become available and the sanitation and hygiene in developing countries improve.
von Sonnenburg F, Tornieporth N, Waiyaki P, Lowe B, Peruski LF , DuPont HL, et al. Risk and aetiology of diarrhoea at various tourist destinations.. Lancet. 2000;356:133-4.
Castelli F, Pezzoli C, Tomasoni L. Epidemiology of travelers’ diarrhea.. J Travel Med. 2001;8(suppl 2):S26-S30.
Hill DR. Occurrence and self-treatment of diarrhea in a large cohort of Americans traveling to developing countries.. Am J Trop Med Hyg. 2000;62:585-9.
Steffen R, Sack RB. Epidemiology. In: Ericsson CD, DuPont HL, Steffen R, eds. Travelers’ diarrhea. Hamilton, Ont.: BC Decker, 2003:112–23.
Jiang ZD, Okhuysen PC, Guo DC, He R, King TM, DuPont HL, et al. Genetic susceptibility to enteroaggregative Escherichia coli diarrhea: polymorphism in the interleukin–8 promotor region.. J Infect Dis. 2003;188:506-11.
Hoge CW, Shlim DR, Echeverria P, Rajah R, Herrmann JE, Cross JH. Epidemiology of diarrhea among expatriate residents living in a highly endemic environment. JAMA. 1996;275:533-8.
Hardie RM, Wall PG, Gott P, Bardhan M, Bartlett LR. Infectious diarrhea in tourists staying in a resort hotel.. Emerg Infect Dis. 1999;5:168-71.
Daniels NA, Neimann J, Karpati A, Parashar UD, Greene KD, Wells JG, et al. Traveler’s diarrhea at sea: three outbreaks of waterborne enterotoxigenic Escherichia coli on cruise ships.. J Infect Dis. 2000;181:1491-5.
Ansdell VE, Ericsson CD. Prevention and empiric treatment of traveler’s diarrhea.. Med Clin North Am. 1999;83:945-73
Mensah P, Yeboah-Manu D, Owusu-Darko K, Ablordey A. Street foods in Accra, Ghana: how safe are they?. Bull World Health Organ. 2002;80:546-54.
Adachi JA, Mathewson JJ, Jiang ZD, Ericsson CD, DuPont HL. Enteric pathogens in Mexican sauces of popular restaurants in Guadalajara, Mexico, and Houston, Texas.. Ann Intern Med. 2002;136:884-7.
Jiang ZD, Lowe B, Verenkar MP, Ashley D, Steffen R, Tornieporth N, et al. Prevalence of enteric pathogens among international travelers with diarrhea acquired in Kenya (Mombasa), India (Goa), or Jamaica (Montego Bay).. J Infect Dis. 2002;185:497-502.
Adachi JA, Jiang ZD, Mathewson JJ, Verenkar MP, Thompson S, Martinez-Sandoval F, et al. Enteroaggregative Escherichia coli as a major etiologic agent in traveler’s diarrhea in 3 regions of the world.. Clin Infect Dis. 2001;32:1706-9.
Taylor DN, Houston R, Shlim DR, Bhaibulaya M, Ungar BL, Echeverria P. Etiology of diarrhea among travelers and foreign residents in Nepal.. JAMA. 1988;260:1245-8.
Kuschner RA, Trofa AF, Thomas RJ, Hoge CW, Pitarangsi C, Amato S, et al. Use of azithromycin for the treatment of Campylobacter enteritis in travelers to Thailand, an area where ciprofloxacin resistance is prevalent.. Clin Infect Dis. 1995;21:536-41.
Hoge CW, Gambel JM, Srijan A, Pitarangsi C, Echeverria P. Trends in antibiotic resistance among diarrheal pathogens isolated in Thailand over 15 years.. Clin Infect Dis. 1998;26:341-5.
Sanders JW, Isenbarger DW, Walz SE, Pang LW, Scott DA, Tamminga C, et al. An observational clinic-based study of diarrheal illness in deployed United States military personnel in Thailand: presentation and outcome of Campylobacter infection.. Am J Trop Med Hyg. 2002;67:533-8.
Tauxe RV, Swerdlow DL, Hughes JM. Foodborne disease. In: Mandell GL, Douglas RG, Bennett JE, Dolin R, eds. Mandell, Douglas, and Bennett’s Principles and practice of infectious diseases. 5th ed. Philadelphia: Churchill Livingstone, 2000:1150–65.
Barbier HM, Diaz JH. Prevention and treatment of toxic seafoodborne diseases in travelers.. J Travel Med. 2003;10:29-37.
Kozicki M, Steffen R, Schar M. ‘Boil it, cook it, peel it or forget it’: does this rule prevent travellers’ diarrhoea?. Int J Epidemiol. 1985;14:169-72.
Mattila L, Siitonen A, Kyronseppa H, Simula II, Peltola H. Risk behavior for travelers’ diarrhea among Finnish travelers.. J Travel Med. 1995;2:77-84.
Backer H. Water disinfection for international and wilderness travelers.. Clin Infect Dis. 2002;34:355-64.
RendiWagner P, Kollaritsch H. Drug prophylaxis for travelers’ diarrhea.. Clin Infect Dis. 2002;34:628-33.
Steffen R, Heusser R, DuPont HL. Prevention of travelers’ diarrhea by nonantibiotic drugs.. Rev Infect Dis. 1986;8(suppl 2):S151-9.
Oksanen PJ, Salminen S, Saxelin M, Hamalainen P, Ihantola-Vormisto A, Muurasniemi-Isoviita L, et al. Prevention of travellers’ diarrhoea by Lactobacillus GG.. Ann Med. 1990;22:53-6.
Hilton E, Kolakowski P, Singer C, Smith M. Efficacy of Lactobacillus GG as a diarrheal preventive in travelers.. J Travel Med. 1997;4:41-3.
World Health Organization. Substandard and counterfeit medicines. Fact sheet no. 275, November 2003. Accessed online April 6, 2005, at: http://www.who.int/mediacentre/factsheets/2003/fs275 .
De Bruyn G, Hahn S, Borwick A. Antibiotic treatment for travellers’ diarrhoea.. Cochrane Database Syst Rev. 2005;;1:CD002242.
Shlim DR. Self diagnosis and treatment of traveler’s diarrhea. In: Keystone JS, Kozarsky PE, Freedman DO, Nothdurft HD, Connor BA, eds. Travel medicine. St. Louis: Mosby, 2003:201–4.
Ericsson CD. Travelers’ diarrhea: epidemiology, prevention, and self-treatment.. Infect Dis Clin North Am. 1998;12:285-303.
Salam I, Katelaris P, Leigh-Smith S, Farthing MJ. Randomised trial of singledose ciprofloxacin for travellers’ diarrhoea.. Lancet. 1994;344:1537-9.
Adachi JA, Ericsson CD, Jiang ZD, DuPont MW, Martinez-Sandoval F, Knirsch C, et al. Azithromycin found to be comparable to levofloxacin for the treatment of US travelers with acute diarrhea acquired in Mexico.. Clin Infect Dis. 2003;37:1165-71.
DuPont HL, Mattila L. Antimicrobial treatment: an algorithmic approach. In: Ericsson CD, DuPont HL, Steffen R, eds. Travelers’ diarrhea. Hamilton, Ont.: BC Decker, 2003:227–37.
Adachi JA, OstroskyZeichner L, DuPont HL, Ericsson CD. Empirical antimicrobial therapy for traveler’s diarrhea.. Clin Infect Dis. 2000;31:1079-83.
DuPont HL, Jiang ZD, Ericsson CD, Adachi JA, Mathewson JJ, DuPont MW, et al. Rifaximin versus ciprofloxacin for the treatment of traveler’s diarrhea: a randomized, double-blind clinical trial.. Clin Infect Dis. 2001;33:1807-15.
Steffen R, Sack DA, Riopel L, Jiang ZD, Sturchler M, Ericsson CD, et al. Therapy of travelers’ diarrhea with rifaximin on various continents.. Am J Gastroenterol. 2003;98:1073-8.
Stauffer WM, Konop RJ, Kamat D. Traveling with infants and young children. Part III: travelers’ diarrhea.. J Travel Med. 2002;9:141-50.
Murphy GS, Bodhidatta L, Echeverria P, Tansuphaswadikul S, Hoge CW, Imlarp S, et al. Ciprofloxacin and loperamide in the treatment of bacillary dysentery.. Ann Intern Med. 1993;118:582-6.
Taylor DN, Sanchez JL, Candler W, Thornton S, McQueen C, Echeverria P. Treatment of travelers’ diarrhea: ciprofloxacin plus loperamide compared with ciprofloxacin alone. A placebo-controlled randomized trial.. Ann Intern Med. 1991;114:731-4.
Caeiro JP, DuPont HL, Albrecht H, Ericsson CD. Oral rehydration therapy plus loperamide versus loperamide alone in the treatment of traveler’s diarrhea.. Clin Infect Dis. 1999;28:1286-9.
Pitzinger B, Steffen R, Tschopp A. Incidence and clinical features of traveler’s diarrhea in infants and children.. Pediatr Infect Dis J. 1991;10:719-23.
Samuel BU, Barry M. The pregnant traveler.. Infect Dis Clin North Am. 1998;12:325-54.
Drugs for parasitic infections. Med Lett Drugs Ther. 2004;46:1-12.
Continue Reading
More in afp.
Copyright © 2005 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Clin Microbiol Rev
- v.19(3); 2006 Jul

Prevention and Self-Treatment of Traveler's Diarrhea
David j. diemert.
Human Hookworm Vaccine Initiative, Sabin Vaccine Institute, 1889 F St. NW, Suite 200S, Washington, D.C.
Of the millions who travel from the industrialized world to developing countries every year, between 20% and 50% will develop at least one episode of diarrhea, making it the most common medical ailment afflicting travelers. Although usually a mild illness, traveler's diarrhea can result in significant morbidity and hardship overseas. Precautions can be taken to minimize the risk of developing traveler's diarrhea, either through avoidance of potentially contaminated food or drink or through various prophylactic measures, including both nonpharmacological and antimicrobial strategies. If diarrhea does develop despite the precautions taken, effective treatment—usually a combination of an antibiotic and an antimotility agent—can be brought by the traveler and initiated as soon as symptoms develop. In the future, vaccines—several of which are in the advanced stages of clinical testing—may be added to the list of prophylactic measures.
INTRODUCTION
In 2004, the United Nations World Tourism Organization estimated that 170 million international travelers visited countries in developing and tropical areas such as Latin America, the Caribbean, the Middle East, South and Southeast Asia, and Africa and that at least 20%, or 34 million, of these travelers arrived from their homes in the industrialized world ( 168 ). Between 20% and 50% of such individuals will experience diarrhea as a result of ingesting fecally contaminated water or food ( 67 , 108 , 152 ). In 5% to 10%, symptoms typical of dysentery (fever, chills, and bloody stools) occur ( 20 , 141 ).
Traveler's diarrhea usually begins within the first week of travel, and without treatment, it usually resolves without sequelae within 3 to 5 days ( 155 ). However, symptoms can be severe enough to force a change in travel plans and to result in confinement to bed or, rarely, hospitalization ( 100 , 126 ). Traveler's diarrhea carries significant economic costs both to the traveling public and to developing countries through loss of tourism income and loss of business investment opportunities caused by the threat of disease. Traveler's diarrhea among military personnel also results in reduced combat readiness, a factor of serious concern to the U.S. military as thousands of personnel are increasingly being deployed in areas of elevated risk of infection ( 149 ). However, the impact of traveler's diarrhea can be reduced by education about ways to prevent the illness. Similarly, the severity of this disease can be minimized by prompt and well-informed self-treatment. Health care providers can help considerably in ensuring that travelers have safe and enjoyable trips overseas.
EPIDEMIOLOGY
Destination represents the single most important risk factor for developing traveler's diarrhea. High-risk regions include the developing countries of Latin America, Africa, Asia, and parts of the Middle East, which have reported attack rates for traveler's diarrhea ranging between 20 and 75% ( 20 , 126 ). Areas of intermediate risk include China, southern Europe, Israel, South Africa, Russia, and several Caribbean islands (especially Haiti and the Dominican Republic); attack rates of 8% to 20% have been recorded among travelers to these regions. Low-risk (<5%) destinations include Canada, the United States, Australia, New Zealand, Japan, northern European countries, and a few Caribbean islands ( 10 ).
Season of travel also affects the level of risk. Numerous studies have demonstrated that attack rates of traveler's diarrhea are highest during the summer months and in rainy seasons ( 20 , 80 ). Since ingestion of contaminated food or drink is the means of acquiring traveler's diarrhea, risk varies according to the attention paid to diet. High-risk foods include uncooked vegetables and unpeeled fresh fruit, raw or undercooked meat or seafood (particularly shellfish), and salads. Safe drinks include bottled carbonated beverages, beer or wine, and boiled or treated water (see “PREVENTION”), while ice, tap water, and unpasteurized milk carry increased risks of infection.
Location also modifies the level of risk: meals eaten in a private home carry lower risk than those eaten in a restaurant ( 50 , 80 , 166 ). The type of travel also influences the likelihood of developing diarrhea: those who participate in “adventure” travel or who go on hiking or camping trips are at increased risk, likely because of hygiene practices and choice of food ( 100 ). However, dining in expensive restaurants or luxury hotels does not reduce the risk of traveler's diarrhea to zero; several outbreaks in such establishments have been reported ( 73 , 128 ). Purchasing food from street vendors is especially risky ( 47 ).
Although gender has no influence on the incidence of diarrhea in travelers ( 54 ), age plays a significant role. Those with the highest incidence include small children and young adults aged 21 to 29 years ( 10 , 29 , 135 ), the latter likely due to a lack of vigilance in avoiding contaminated food combined with a more adventurous lifestyle ( 80 ). Diarrhea in the former group is probably secondary to a relative lack of immunity and increased fecal-oral contamination. Individuals with achlorhydria have been shown to be at increased risk of traveler's diarrhea ( 61 , 83 ), and therefore those on proton pump inhibitors or long-acting H 2 blockers, or those who have had gastrectomies, may be similarly affected: in one study, the use of omeprazole, a proton pump inhibitor, was associated with a 10-fold-increased risk of infection due to Campylobacter ( 121 ). Although conclusive evidence is lacking, travelers with specific medical conditions may also be at higher risk, especially persons with human immunodeficiency virus and reduced CD4 cell counts, patients receiving cytotoxic chemotherapy, and persons with secretory immunoglobulin A (IgA) deficiency.
Certain host genetic factors have been shown to affect susceptibility to traveler's diarrhea. For example, persons with blood group O are at increased risk of developing severe symptoms when infected with Vibrio cholerae O1 ( 8 , 63 , 105 ), although a recent study has suggested that people with this blood group are less likely to be infected with this organism ( 74 ). Similarly, individuals with the blood group O phenotype are at increased risk of developing disease due to norovirus, as demonstrated in two independent challenge studies ( 87 , 107 ). Genetic factors also play a role in susceptibility to traveler's diarrhea due to enteroaggregative Escherichia coli (EAEC). In a study of American students staying in Mexico, the likelihood of developing EAEC-associated diarrhea was significantly increased among those with the AA or AT genotype at the −251 position in the promoter region of the interleukin-8 (IL-8) gene, compared to those with the TT genotype ( 93 ). This IL-8 polymorphism is also likely to impact the course of infection due to other pathogens that cause traveler's diarrhea, such as enterotoxigenic E. coli (ETEC), Campylobacter jejuni , and Salmonella , Shigella , and Cryptosporidium species, all of which have been shown to result in increased levels of fecal IL-8 ( 4 , 69 , 76 , 85 ).
By far the most important etiologic agents of traveler's diarrhea are bacterial pathogens (Table (Table1), 1 ), which have been implicated in more than 80% of cases in several studies ( 5 , 15 , 126 ), including a large survey of more than 30,000 short-term visitors to Jamaica ( 154 ). Of the bacteria implicated, ETEC accounts for the majority of infections, although Shigella species, Campylobacter species, Salmonella species, Aeromonas species ( 173 ), Plesiomonas shigelloides , and noncholera vibrios have also been isolated from travelers ( 10 ). Enteroinvasive E. coli (EIEC) and EAEC are increasingly recognized as possible causes of traveler's diarrhea ( 3 , 92 , 147 , 172 ), although in the case of EAEC, not all strains may be pathogenic, and virulence factors are still unidentified ( 69 ). Both the destination and the season of travel have been shown to affect the identity of the predominant causative organism: ETEC is the most common cause of diarrhea in travelers to Latin America ( 10 ), whereas Campylobacter jejuni is relatively more common in Southeast Asia, particularly Thailand ( 9 ). Vibrio parahaemolyticus has been isolated particularly in travelers to Southeast Asia ( 151 ), whereas Vibrio cholerae is a rare causative agent, limited mostly to relief workers visiting areas afflicted by cholera epidemics. Aeromonas spp. and P. shigelloides have also been associated with travel to Asia ( 148 , 170 ). Seasonal variation in the incidence of ETEC infection has been documented in semitropical countries such as Morocco ( 112 ) and Mexico ( 47 ); ETEC is isolated more commonly in the wet summer and fall months and uncommonly during the dry winters, when Campylobacter acquires greater importance.
Common enteric pathogens isolated in cases of traveler's diarrhea
Viruses—most notably norovirus, rotavirus, and enteric adenoviruses—have been isolated from 2 to 27% of returning travelers with diarrhea ( 20 , 122 , 135 ), although their etiologic importance is tempered by the fact that bacterial pathogens, especially in the case of rotavirus, are often concomitantly isolated. Some serologic evidence implicating norovirus as an agent of traveler's diarrhea has been reported: studies of Peace Corps volunteers in both Thailand ( 44 ) and Honduras ( 142 ) have demonstrated seroconversion following diarrheal episodes. Norovirus has particularly been implicated in outbreaks of traveler's diarrhea in certain situations, especially on cruise ships ( 16 ).
Among parasites, Giardia intestinalis is an important cause of diarrhea in travelers to the mountainous regions of North America ( 57 ) and to St. Petersburg, Russia ( 13 , 95 ), but has also been isolated in an outbreak of illness among British tourists in a Greek hotel ( 73 ) and from 7% of Austrian tourists returning from all parts of the globe ( 135 ). Entamoeba histolytica , Cryptosporidium parvum , and Cyclospora cayetanensis are less common causes of diarrhea in travelers ( 10 , 89 ), although cyclosporiasis should be considered in the case of travelers returning from Peru and Nepal ( 81 ) whereas cryptosporidiosis has been reported with relatively increased frequency in travelers to Russia. Diarrhea caused by parasites is more commonly chronic and is more likely to affect travelers who visit developing countries for prolonged periods: in the study by Reinthaler et al. of returning Austrian tourists, 42% of those with parasitic causes of diarrhea had been abroad for more than 2 months, compared to only 18% of those with bacterial etiologies ( 135 ).
Overall, no pathogens are isolated in 10 to 50% of all cases of traveler's diarrhea despite the usual investigations. However, most of these cases either are self-limited or respond to empirical antibiotic treatment.
PATHOPHYSIOLOGY
Virulence factors associated with ETEC include heat-labile toxin (LT), heat-stable toxin (STa), and various colonization factors (CFs) ( 130 ). Strains producing only LT, only STa, or both toxins have been isolated from travelers with diarrhea, depending on the country visited, and thus likely represent circulating strains ( 91 , 146 ). In general, ETEC strains producing STa alone or both STa and LT are associated with more severe symptoms than those producing only LT ( 131 ), although this may be related to the low prevalence of CFs in LT-producing ETEC strains ( 60 , 114 ). The LT is a heterohexamer consisting of one A subunit (A1 and A2 linked by a disulfide bond) and five B subunits, bearing 75% sequence homology with cholera toxin ( 19 , 150 ). LT binds to the GM1 glycophospholipid receptor on the enterocyte microvillous membrane, which induces configurational changes in the membrane that facilitate entry of the enzymatically active A1 subunit. The A1 subunit functions as an ADP-ribosyltransferase that covalently links ADP ribose to adenylate cyclase, resulting in irreversible enzyme activation and increased intracellular concentrations of cyclic AMP (cAMP) ( 15 ). Increased levels of cAMP result in activation of a secretory cascade involving protein kinase C, protein phosphorylation, and the opening of chloride channels in the apical membrane of the enterocyte, predominantly in the crypts, resulting in extrusion of these ions and H 2 O into the intestine.
The STa toxin binds to an apical receptor linked to membrane-bound guanylate cyclase G ( 58 ), activating guanylate cyclase and thereby increasing intracellular concentrations of cyclic GMP (cGMP). Like cAMP, cGMP results in opening of membrane chloride channels. In addition to affecting enterocyte chloride ion secretion, both LT and STa enterotoxins inhibit sodium and chloride absorption. Furthermore, evidence suggests that in addition to the direct effects that ETEC enterotoxins have on enterocyte electrolyte secretion, interactions with the enteric nervous system (stimulation of sensory afferents in the intestinal wall) also occur, further enhancing the intestinal secretory cascade ( 56 ).
The pathogenesis of diarrhea caused by EAEC, on the other hand, is not as clear, although it has been demonstrated that these strains do not secrete heat-stable or heat-labile enterotoxins ( 117 ). EAEC colonizes the mucosal surface of the small and large bowel abundantly, mediated by structures referred to as aggregative adherence fimbriae ( 25 , 116 , 118 ). Colonization is followed by mild but significant mucosal damage which is most severe in the large bowel and is likely mediated by enterotoxins ( 77 ). Most EAEC strains express the Shigella enterotoxin 1 (ShET1) ( 26 , 75 ), which may contribute to secretory diarrhea. Additionally, many EAEC strains secrete an autotransporter toxin called Pet, which has been shown to induce a rounding of epithelial cells in culture that is dependent on the presence of functional protease activity ( 52 , 119 , 120 ). Pet induces disruption of the actin cytoskeleton in affected cells, possibly through cleavage of spectrin ( 171 ).
The microbial pathogens that cause dysentery express virulence factors that either allow direct invasion of enterocytes or liberate cytotoxins which produce cell death. Salmonella spp., Shigella spp., and EIEC all express invasion plasmid antigens on their surfaces which disrupt the epithelial cell cytoskeleton, thus allowing formation of endocytotic vesicles which transport the organism into the enterocyte cytoplasm. Subsequent intracellular bacterial multiplication eventually leads to cell lysis, with liberation of cytotoxin extracellularly. The invasion and cytotoxin virulence factors are only part of a cascade of events that produces inflammation in the distal ileum and colon ( 15 ).
Viral pathogens such as norovirus and rotavirus produce cytopathic changes in epithelial cells lining the small intestine, resulting in acute villous atrophy. The associated loss of enterocytes has been implicated in the transient decrease in disaccharidase activity and temporary lactose intolerance that has been ascribed to these infections. In contrast to viral causes of traveler's diarrhea, the protozoan pathogen Entamoeba histolytica induces enterocyte loss in the colon without directly invading cells; after adhering to the epithelial cell wall via surface lectins, E. histolytica releases several cytotoxic molecules such as proteinases and a pore-forming protein which creates high-conductance ion channels in the cell membrane, allowing the rapid influx of calcium and other ions, leading to cell death ( 15 ). E. histolytica then phagocytoses the dead enterocytes, enabling it to penetrate further into the mucosa, forming the classic “flask-shaped” ulcers.
CLINICAL SYNDROMES
Traveler's diarrhea is usually defined in studies as the passage of at least three unformed stools within a 24-h period, in association with at least one symptom of gastrointestinal disease such as nausea, vomiting, fever, abdominal pain or cramps, tenesmus, fecal urgency, or the passage of bloody or mucoid stools. By convention, it usually refers to disease that develops in a resident of the industrialized world who travels to a developing tropical or semitropical country. Typically, symptoms develop within the first week of travel, and more than 90% of cases occur within the first 2 weeks ( 155 ). Between four and five loose or watery stools a day with little to no fever is the norm; without treatment, the diarrhea usually lasts for only 3 to 4 days before resolving spontaneously in most cases ( 9 ). Approximately 80% of travelers with diarrhea complain of abdominal cramping, 10% to 25% have fever, 20% have vomiting, and between 5% and 10% report having blood or mucus in their stool ( 20 , 141 ). Traveler's diarrhea can result in significant disruption to an individual's trip: as many as 40% must modify their activities in some way, approximately 20% of persons are bed bound for 1 or 2 days, and hospitalization is required for 1%, although mortality is rare ( 5 , 9 , 100 , 126 ). Although symptoms are short-lived in the majority of cases, between 8% and 15% of affected travelers are symptomatic for longer than a week, and 2% develop chronic diarrhea that lasts for 1 month or more; such long-lived disease is particularly associated with protozoan causes of infection ( 32 , 152 ).
Severe diarrhea can result in water and electrolyte losses, leading to significant dehydration, electrolyte imbalances, and even impairment of renal function. Traveler's diarrhea, especially when caused by invasive bacteria such as Salmonella , Shigella , or Campylobacter , may exacerbate inflammatory bowel disease, whereas irritable bowel syndrome has been reported to be a chronic complication in as many as 10% of North Americans who develop diarrhea while traveling in Mexico ( 123 ).
Prevention of traveler's diarrhea falls into four broad categories: immunization, avoidance, nonpharmacological therapy, and antibiotic prophylaxis. For U.S. residents, immunization plays an almost insignificant role in the prevention of diarrhea, since vaccines are not yet commercially available in this country for the vast majority of causative agents, although several are currently under development or in the process of licensure (see “Future Developments”). A live-attenuated oral cholera vaccine (Mutacol, Orochol) has been shown to have protective efficacy as high as 90% when recipients were challenged with Vibrio cholerae within 3 months of vaccination ( 161 ), whereas an oral combination vaccine consisting of both recombinantly produced cholera toxin B (CTB) subunit and inactivated whole-cell V. cholerae O1 (Dukoral) has shown protection against diarrhea due to both V. cholerae and ETEC, the latter presumably because of the significant homology between LT and CTB. In a large, placebo-controlled trial of Dukoral administered to Finnish travelers to Morocco, protection against diarrhea caused by ETEC was 52%, whereas protective efficacy against ETEC and any other pathogen was 71% ( 127 ); this finding was confirmed in another trial with travelers to Mexico, in which the vaccine conferred 50% protective efficacy against all ETEC strains ( 139 , 159 ).
Both the live-attenuated and CTB/whole-cell cholera vaccines have received regulatory approval in Canada and in Europe; however, neither has been approved for marketing in the United States. Furthermore, cholera is a very uncommon cause of traveler's diarrhea, and vaccination should be considered only for high-risk individuals such as those involved in relief efforts during cholera epidemics. Similarly, Salmonella enterica serovar Typhi is an uncommon cause of traveler's diarrhea, although infection with this organism can cause serious illness. Since effective oral (Ty21a) and injectable (Vi) vaccines targeting this pathogen are available, they should be offered to those who will be at high risk of ingesting contaminated food or drink, such as those traveling in rural areas of developing countries for extended periods.
Dietary Counseling
Avoidance of high-risk foods and drink is an oft-cited means of reducing the risk of traveler's diarrhea, although there is little direct evidence that such behavior modification actually reduces disease incidence ( 17 , 80 , 103 , 111 , 129 , 155 ). Studies assessing the relationship between the level of care taken in what is eaten and the risk of traveler's diarrhea have yielded conflicting results; furthermore, it is often difficult to assess the effect of dietary counseling, since most studies are retrospective and are thus influenced by recall bias ( 144 ).
Nevertheless, because of the simplicity of this risk modification, those seeking pretravel advice should be counseled to drink only “safe” beverages, such as those that have been boiled, bottled, or carbonated. Water should be boiled vigorously for at least 1 min before consuming, which will kill most pathogens. Care should be taken when one is traveling at altitudes higher than 6,562 feet (2,000 m) to boil water for at least 3 min due to the lower atmospheric pressure. Adding either tincture of iodine (5 drops/qt) or tetraglycine hydroperiodide tablets, or using iodinizing filters, is also an effective means of purifying water, although protozoan cysts are often halide resistant; any of these items can be purchased in travel stores or pharmacies and should be used as directed by the manufacturer. While many people take pains to avoid drinking unsafe water while in developing countries, ice cubes are often overlooked, despite the fact that freezing does not kill most microorganisms. Carbonation of water kills enteropathogenic bacteria by reducing the pH; noncarbonated bottled water has been implicated in outbreaks of diarrhea in both Mexico and Portugal ( 11 , 64 ). Travelers should take care to verify the seals of bottles, since filling discarded bottles with tap water and reselling them is a frequent occurrence in developing countries ( 53 ).
Fruit, including tomatoes, should be peeled, unless it has been washed thoroughly in “safe” water. Although the rind is not eaten, watermelons still carry some risk, since they may be injected with water to increase their weight and therefore their price. Salads and raw vegetables should be avoided, and only thoroughly and recently cooked meats or fish should be eaten. Leftovers and condiments in open bottles, as well as food from street vendors, have consistently been shown to carry an increased risk of contamination with organisms that cause traveler's diarrhea ( 2 ).
Nonantibiotic Options
Several nonantibiotic agents have been studied for the prevention of traveler's diarrhea (Table (Table2). 2 ). The most effective of these is bismuth subsalicylate (BSS; Pepto-Bismol), which has been shown to have mild antimicrobial activity as well as antisecretory and anti-inflammatory properties ( 23 , 46 , 55 , 59 , 65 , 110 , 115 ). After ingestion, BSS undergoes acid hydrolysis in the gastrointestinal tract, resulting in the generation of numerous bismuth moieties in addition to free salicylate ( 30 ). Whereas the antimicrobial effects of BSS derive from the bismuth moieties ( 23 , 110 ), the antisecretory and anti-inflammatory properties are likely due to the antiprostaglandin and ion channel-inhibitory effects of free salicylate ( 46 , 55 , 59 , 115 ). When taken in the form of two 262-mg tablets four times a day with food, BSS decreased attack rates of traveler's diarrhea from 40% to 14% compared to the placebo; twice-daily dosing was less effective ( 36 , 156 ).
Drugs used for chemoprophylaxis of traveler's diarrhea
BSS should be avoided by children under the age of 3 years and by persons allergic to salicylates, and caution is advised for patients taking other salicylate-containing medications or anticoagulants, as well as for individuals with gout or chronic renal insufficiency. Side effects are minimal at recommended doses if BSS is taken for short periods (i.e., less than 3 weeks), although BSS may produce tinnitus as well as a blackening of the stool (thus creating diagnostic confusion with melena should diarrhea develop) and tongue, although rinsing the mouth after ingestion can minimize this particular side effect. Lastly, BSS may interfere with the absorption of doxycycline—commonly prescribed for antimalarial prophylaxis—and certain other medications ( 49 ).
Lactobacillus preparations have also been used for the prevention of traveler's diarrhea, in the hope of interfering with the colonization of the gastrointestinal tract by pathogenic organisms. However, their effectiveness has been limited, with reported protective efficacy ranging from zero to 47% ( 78 , 124 , 143 ).
Antibiotics
Several antibiotics have been shown to be highly effective in the prevention of traveler's diarrhea, with protection levels between 80% and 90% reported. Despite this, most experts agree that antibiotic prophylaxis should be given only for short courses and only under special circumstances ( 67 , 158 ). Individuals for whom antibiotic prophylaxis might be considered include those who are at increased risk of developing severe or complicated disease, such as the immunocompromised, those with inflammatory bowel disease, insulin-dependent diabetics, and those taking diuretics (who are therefore more susceptible to dehydration). Prophylaxis may also be offered to those with increased susceptibility to traveler's diarrhea because of achlorhydria, having had a gastrectomy, or taking a proton pump inhibitor. Arguments have been advanced to offer antibiotic prophylaxis to those who undertake “critical travel,” such as diplomats or business travelers, for whom even a short-lived illness may not be acceptable.
When used as prophylaxis, antibiotics should be taken daily as a single dose while in an area of risk and continued for 1 to 2 days after leaving. Early studies using either doxycycline ( 138 , 142 ) or trimethoprim-sulfamethoxazole (TMP-SMX) ( 37 ) showed that they were effective in preventing traveler's diarrhea in many parts of the world; however, widespread resistance to both of these agents has subsequently developed ( 79 ), thus limiting their usefulness.
The fluoroquinolones, such as ciprofloxacin, ofloxacin, norfloxacin, and levofloxacin, have been shown to be highly effective in the prevention of diarrhea in travelers (Table (Table2). 2 ). Daily ciprofloxacin given at a dose of 500 mg has been shown to be up to 95% effective in preventing traveler's diarrhea ( 134 ). However, as with doxycycline and TMP-SMX, microbial resistance to this agent—particularly with Campylobacter species—has been reported with increasing frequency, especially in Southeast Asia: ciprofloxacin resistance among Campylobacter species isolated from both native Thais and travelers to Thailand increased from zero in 1991 to 84% in 1995 ( 79 ). Although azithromycin has been shown to be an effective treatment for traveler's diarrhea ( 1 , 104 ) and likely would be effective as a chemoprophylactic drug, this has not been studied and dosing recommendations cannot be made at this time. Use of azithromycin as a treatment for persons developing acute diarrhea while on fluoroquinolone prophylaxis should be considered, especially for travelers to Thailand, where quinolone-resistant Campylobacter is common.
Recently, the drug rifaximin has been shown to be effective for the prevention of diarrhea in travelers to Mexico ( 42 ). This semisynthetic rifamycin derivative, although only recently approved in the United States for the treatment of uncomplicated traveler's diarrhea, has been licensed for this indication in several European countries since the 1980s. When administered orally, rifaximin remains active in the gastrointestinal tract and less than 0.4% is systemically absorbed ( 28 , 62 ). In vitro antibacterial activity has been shown against most of the gram-negative enteric pathogens, in addition to gram-positive rods and anaerobic bacteria ( 84 ). In the prophylaxis study reported recently, adult travelers to Guadalajara, Mexico, who took rifaximin daily for 2 weeks reported 72% and 77% protection against traveler's diarrhea and antibiotic-treated traveler's diarrhea, respectively, with minimal side effects ( 42 ). Previous studies, as well as the current study, have demonstrated that ETEC is the predominant etiology of traveler's diarrhea in this region. Therefore, further trials must be conducted in areas where etiologic agents other than ETEC predominate before this antibiotic can be generally recommended to travelers. Poorly absorbed antibiotics such as rifaximin have potential advantages over absorbed drugs such as the fluoroquinolones in terms of fewer systemic side effects, improved safety for children and pregnant women (although these have not yet been studied and therefore cannot be recommended), and “sparing” of systemically absorbed antibiotics used for other infections in terms of development of antimicrobial resistance.
Given the existence of a relatively unabsorbed antibiotic with few side effects, the option of offering universal prophylaxis to all travelers has been raised. However, several arguments can be made against universal prophylaxis—whether it be with an absorbed or an unabsorbed antibiotic—including the cost of providing prophylaxis to tens of millions of travelers annually to prevent what in most cases is a relatively mild disease, the risk that development of antimicrobial resistance will be accelerated, and the fact that effective self-treatment can be provided that generally limits the duration of symptoms to a few hours ( 31 , 66 ).
Furthermore, if chemoprophylaxis is taken, it should remain short-term (generally defined as less than 3 weeks), for a number of reasons. First, antibiotic prophylaxis engenders a false sense of security in the traveler who might otherwise use more caution in what is eaten. The development of antibiotic-resistant pathogens, severe reactions such as Stevens-Johnson syndrome or anaphylaxis ( 136 ), candida vaginitis ( 37 ), Clostridium difficile -associated diarrhea, and photosensitivity reactions are all potential disadvantages of the use of chemoprophylaxis.
SELF-TREATMENT
For individuals seen in the pretravel period, counseling should focus on safe beverage and food selection. Chemoprophylaxis with either bismuth subsalicylate or antibiotics should be contemplated only in special situations such as those outlined above and is generally discouraged ( 67 , 158 ). In most cases, prompt self-treatment using a combination of an antimotility agent (usually loperamide) and an antibiotic (usually either a fluoroquinolone or rifaximin)—both of which can be obtained prior to departure and carried unrefrigerated while traveling—is the preferred alternative (Table (Table3). 3 ). Travelers should be advised of the dangers of purchasing drugs to treat diarrhea while traveling abroad, especially in developing countries. Such drugs may contain agents such as the antibiotic chloramphenicol, which may induce aplastic anemia, or iodochlorhydroxyquin (EnteroVioform), which can cause serious neurologic damage and optic atrophy ( 137 ); both of these medications have been banned in the United States.
Drugs used for treatment of traveler's diarrhea
Fluid and Electrolytes
In most cases, traveler's diarrhea is neither life threatening nor severe. Treatment, therefore, is directed at minimizing the symptoms and duration of illness. The first goal of therapy is the prevention and treatment of dehydration, which can be of special concern for children, pregnant women, and the elderly. Travelers with mild diarrhea that does not interfere with activity can readily replace fluid and electrolyte losses with a combination of salted crackers, carbonated noncaffeinated beverages, canned fruit juices, purified water, and clear salty soups. Dairy products may worsen symptoms, and caffeine may increase gastrointestinal fluid secretion, thereby intensifying fluid losses.
Severe diarrhea, especially in infants and pregnant women, requires careful fluid replacement. Commercial packets of oral rehydration salts containing both glucose (or complex sugars) and sodium chloride are readily available in pharmacies and can be purchased prior to travel. It is important to reconstitute them with purified water in the quantities indicated by the packet's manufacturer and to adjust administered volumes according to weight (CDC website, http://www2.ncid.cdc.gov/travel/yb/utils/ybGet.asp?section =children&obj=children_gen_info.htm&cssNav=browseoyb). Oral rehydration solution promotes the absorption of both sodium and water in the small intestine by the active transport of glucose, to which the absorption of sodium is coupled. Rehydration packets containing complex sugars (“rice based”) may have a greater effect on reducing fluid losses than those that are glucose based, since glucose itself may paradoxically increase the output of diarrhea fluid ( 18 ). If oral rehydration salts are unavailable, a less ideal substitute can be prepared by adding one teaspoon of table salt and eight teaspoons of sugar to one liter of purified water.
During the acute phase of the illness, a diet consisting of complex carbohydrates such as rice, bread, potatoes, bananas, and crackers is prudent, although a recent study reported that restriction of diet during concomitant treatment with an antibiotic did not impact either the duration or the severity of symptoms ( 86 ). As soon as the diarrhea begins to resolve, the diet can be quickly advanced as tolerated.
Symptomatic Therapy
Although replacement of fluid losses forms the cornerstone of treatment of traveler's diarrhea, it does not by itself completely relieve the symptoms of this illness. Self-treatment of traveler's diarrhea with antimotility agents and antibiotics has become the standard advice given in most travel clinics in North America. Individuals can take both of these agents with them when they travel, so as to begin treatment as soon as symptoms occur.
Loperamide (Imodium) remains the antimotility agent of choice for traveler's diarrhea. In addition to its antiperistaltic effect, it has also been shown to increase the intestinal absorption of fluid and electrolytes ( 70 ). When used as sole therapy, loperamide provides relief for mild to moderate diarrhea (up to five loose stools per day with or without mild cramping pain), in comparison to either a placebo or bismuth subsalicylate ( 94 , 169 ). Diphenoxylate plus atropine (Lomotil) is another readily available antimotility agent but is less effective than loperamide and may even prolong symptoms, as has been reported with infection secondary to Shigella ( 33 ). In addition, atropine has a higher incidence of side effects, including urinary retention (especially in elderly men) and central nervous system toxicity, and may be addictive.
Antimotility agents are contraindicated for children under the age of 2 years because of the increased risk of adverse effects, especially narcotic intoxication with loperamide ( 12 ). In addition, they should be avoided if there is evidence of dysentery as manifested by symptoms such as high fever or bloody diarrhea, because of the possibility that they may delay clearance of invasive enteropathogens and hence prolong the course of disease.
As previously mentioned, BSS is another nonantibiotic antidiarrheal agent that has antisecretory, anti-inflammatory, and antimicrobial properties and that reduces the number of unformed stools passed and the duration of diarrhea by approximately 50% ( 23 , 46 , 55 , 59 , 65 , 110 , 115 ). However, it is less effective than loperamide and has several negative properties that preclude its use as treatment, including large required doses (1 oz or one tablet every 30 min for up to eight doses), delayed onset of action (up to 4 h), possible interference with the absorption of other medications such as doxycycline that may be used as malaria chemoprophylaxis, and potential adverse effects such as tinnitus ( 38 , 39 ).
It should be noted that although both antimotility agents and BSS alleviate symptoms, they do not effectively treat the underlying infectious causes of the diarrhea, and that relapse of symptoms following cessation of use has been reported ( 94 ).
Antimicrobial Therapy
Antibiotic therapy is recommended either with or without loperamide for travelers with moderate to severe symptoms (three or more unformed stools during an 8-h period, particularly if associated with nausea, vomiting, abdominal cramping, fever, or bloody stools). Antimicrobials reduce the duration of diarrhea from 50 to 95 h if untreated to 16 to 30 h, as well as reducing related symptoms such as abdominal cramping and time spent incapacitated ( 27 , 34 , 40 ).
The choice of which antibiotic to carry when traveling has changed since the subject of traveler's diarrhea was first studied. Until recently, TMP-SMX was the drug of choice for the treatment of traveler's diarrhea; however, ubiquitous drug resistance of ETEC and salmonellae to this drug now renders it less effective ( 79 ). Moreover, it is inactive against C. jejuni , which, as already mentioned, is an important etiologic agent of traveler's diarrhea in Southeast Asia. The only instance in which TMP-SMX might be useful would be in areas where Cyclospora is a significant cause of diarrhea, such as Nepal during the summer months. Even then, it should be used only in cases where treatment with a fluoroquinolone and an antimicrobial active against Giardia (such as metronidazole or tinidazole) has failed.
Fluoroquinolones such as ciprofloxacin, norfloxacin, ofloxacin, and levofloxacin have until recently been the drugs of choice for the empirical treatment of traveler's diarrhea in adults ( 31 , 45 ). Either alone or in combination with loperamide, they have been shown to reduce the duration of diarrhea by more than 50% compared to placebo ( 48 , 51 , 113 , 157 , 165 ). Not only are they safe and well tolerated fluoroquinolones maintain high concentrations in the stool, which may theoretically limit invasive disease. Disadvantages of their use include drug interactions, such as those with warfarin and anticonvulsants, and the recent emergence of drug resistance, especially among Campylobacter isolates from Thailand ( 79 ).
In instances where the use of a fluoroquinolone is appropriate, a 3-day course is usually effective ( 34 ). Single-dose therapy has been studied and been shown to be adequate in most cases ( 68 , 140 ); however, for bacteria such as Campylobacter and Shigella dysenteriae , concerns have been raised that single-dose therapy may be inadequate ( 5 , 98 ). As a rule of thumb, if evidence of invasive disease exists, such as high fever, chills, or bloody diarrhea, a 3-day course of treatment should be taken.
In areas where fluoroquinolone-resistant C. jejuni has been found, azithromycin may be an effective option: in a study comparing azithromycin (500 mg) with ciprofloxacin (500 mg) daily for 3 days for treatment of acute diarrhea in U.S. military personnel in Thailand, azithromycin was shown to be superior in decreasing the duration of excretion of Campylobacter and was as effective as ciprofloxacin in decreasing the duration of symptoms ( 104 ). Single-dose azithromycin (1,000 mg) has also been shown to be equivalent to single-dose ciprofloxacin (500 mg) for the treatment of traveler's diarrhea in adults visiting Mexico, although microbial eradication rates were nonsignificantly lower with azithromycin than with ciprofloxacin ( 1 ). Azithromycin may also be the treatment of choice for children between the ages of 2 and 8 years and for pregnant women, in which cases the use of fluoroquinolones is contraindicated. The treatment of traveler's diarrhea in children under the age of 2 years is usually recommended to be oral rehydration alone.
The drug rifaximin has recently been shown to be an effective chemotherapeutic agent for traveler's diarrhea. Four major studies assessing the efficacy of rifaximin in the treatment of traveler's diarrhea have been conducted in Mexico, Guatemala, Kenya, and Jamaica ( 35 , 41 , 88 , 153 ). Compared to placebo, administration of either 200 mg or 400 mg three times daily was associated with improvement in the duration of diarrhea ( 88 , 153 ), whereas equivalency with ciprofloxacin and superiority to TMP-SMX have also been shown. However, these studies have been conducted primarily with individuals without dysentery, so treatment with rifaximin should be limited to those without fever, bloody stool, or systemic toxicity.
APPROACH TO SELF-TREATMENT
In most cases, travelers to developing countries should bring loperamide and an antibiotic to use for empirical self-treatment should they develop diarrhea. Mild diarrhea (up to three loose bowel movements a day) can be self-treated with oral rehydration and loperamide. If symptoms worsen or do not improve after 24 h, treatment with an antibiotic should be initiated. Traveler's diarrhea that is associated with more severe symptoms warrants immediate treatment with both loperamide and an antibiotic. Loperamide, however, should be avoided in cases of dysentery as evidenced by symptoms such as high fever, chills, and/or bloody diarrhea.
Until recently, the preferred antibiotic class for self-treatment of traveler's diarrhea has been the fluoroquinolones, although the exact choice should be decided by a host of factors, such as the traveler's itinerary, age, pregnancy status, and drug allergies; potential drug interactions; and whether or not chemoprophylaxis against traveler's diarrhea or malaria will also be taken. However, the unabsorbed antibiotic rifaximin should now also be considered a potential agent for self-treatment, especially for travelers going to areas where ETEC is the predominant etiologic organism, such as Mexico. The addition of rifaximin to the armamentarium of chemoprophylactic agents for traveler's diarrhea carries several advantages, namely, the low rate of side effects and the public health benefit of sparing systemically absorbed antibiotics such as the fluoroquinolones for treatment of other, life-threatening bacterial infections, thereby delaying the development of antimicrobial resistance to these agents. Furthermore, recent evidence that irritable bowel syndrome may be a sequela of traveler's diarrhea ( 123 ) has prompted some experts to suggest this agent as a potential universal chemoprophylactic agent to prevent this outcome, although further studies to confirm this finding are needed ( 29 , 43 ).
If possible, medical advice should be sought if symptoms do not diminish after initial treatment, especially in cases of persistently high fever with chills, blood and mucus in the stool, and frequent vomiting that prevents adequate fluid replacement. However, in certain cases, provision of second- or third-line antibiotics to travelers, for self-treatment of persistent diarrhea after initial treatment, may be considered in lieu of advice to automatically seek medical evaluation. This may be of special concern for travelers to Thailand, where initial treatment with a fluoroquinolone may fail secondary to infection with drug-resistant Campylobacter ; in these cases, azithromycin would be the second-line agent of choice. Also, for those travelers departing on trips of significant duration, provision of metronidazole (or tinidazole) as a third-line agent may be appropriate, to treat infections secondary to G. intestinalis or E. histolytica infection.
Almost 3% of travelers to developing countries will develop diarrhea that persists for longer than 2 weeks despite standard antimicrobial treatment. Infection with antibiotic-resistant bacteria may account for this, although illness due to parasites such as G. intestinalis , C. parvum , and C. cayetanensis is also a possibility. Possible noninfectious etiologies include inflammatory bowel disease, disaccharidase deficiency, irritable bowel syndrome, and bowel carcinoma. Wherever possible, chronic symptoms should be investigated by a health care professional; if still traveling, individuals can often obtain the names of competent English-speaking physicians from the embassies of the United States, Canada, Australia, New Zealand, or the United Kingdom.
FUTURE DEVELOPMENTS
Given the large health and economic costs related to traveler's diarrhea, more effective prevention strategies are clearly warranted. Development of a broadly protective vaccine against this syndrome would be beneficial; unfortunately, the wide range of organisms that cause traveler's diarrhea greatly complicates development of such a vaccine and makes it unlikely that a single candidate will effectively prevent most cases. Despite this, considerable effort is being undertaken to develop novel vaccines against the more important agents of traveler's diarrhea, including ETEC, Shigella spp., Salmonella enterica serovar Typhi, and C. jejuni .
Given ETEC's place as the most common cause of traveler's diarrhea, development of a vaccine against this pathogen has been the priority, and several candidate vaccines are currently undergoing clinical testing. The most studied ETEC vaccine currently in development is an oral whole-cell vaccine consisting of five ETEC strains that express the CF CFA/I and the different subcomponents of CFA/II and CFA/IV combined with recombinant CTB. In adult Swedish volunteers, the vaccine induced high levels of IgA against both CTB and the individual CF components ( 90 ). Subsequent studies with Egyptian children and adults ( 72 ), and with Bangladeshi children ( 132 , 133 ), have confirmed the vaccine's safety and immunogenicity in these settings where the disease is endemic, although the results of larger efficacy studies are pending.
Other ETEC vaccines under development include recombinant ETEC CF CS6 in combination with LT, delivered transcutaneously by means of a topical patch ( 71 ); an oral live-attenuated vaccine ( 167 ); and a candidate vaccine consisting of CS6 encapsulated in biodegradable microspheres ( 96 ). All three of these candidates have been evaluated in phase 1 studies and have demonstrated promising safety and immunogenicity profiles.
Although less advanced in clinical development, vaccines are also being developed against shigellosis, including Shigella sonnei strain WRSS1, consisting of a live, oral candidate vaccine attenuated by a deletion in the virG plasmid virulence gene, which has shown good immunogenicity in phase 1 trials in both the United States and Israel ( 102 , 125 ). A vaccine consisting of a live, attenuated Shigella flexneri type 2a strain carrying mutations in the virG and aerobactin ( iuc ) virulence genes ( 97 ) has shown 50% efficacy in a challenge study conducted with adults in the United States, although this encouraging result was tempered by safety concerns due to fever and diarrhea that was observed at the higher doses ( 24 ). Parenteral conjugate vaccines of purified S. flexneri type 2a and S. sonnei lipopolysaccharide conjugated to recombinant Pseudomonas aeruginosa exotoxin A are also being developed ( 21 , 164 ); in particular, the S. sonnei conjugate vaccine has been shown to be 74% efficacious against disease due to this organism when tested in a field trial on Israeli military recruits ( 22 ).
Several new attenuated Salmonella enterica serovar Typhi strains are under development for use as live oral vaccines; three of these are currently at an advanced stage of clinical testing. CVD908- htrA is an aroC / aroD / htrA deletion mutant that has been successfully tested in a phase 2 trial ( 162 ), whereas the CVD909 derivative of this strain, which constitutively expresses the Vi antigen, has shown improved mucosal immunity to this virulence factor in a phase 1 trial in the United States ( 163 ) without compromising safety. The Ty800 strain, a mutant of the wild-type strain Ty2 with deletion of the phoP / phoQ virulence regulatory genes, has been shown to stimulate vigorous IgA and serum antibody responses to the lipopolysaccharide O antigen in a phase 1 trial ( 82 ). A third live, oral attenuated, single-dose typhoid vaccine consists of the M01ZH09 strain, carrying the targeted mutation of a structural protein (SsaV) of Salmonella pathogenicity island-2, a virulence factor that allows Salmonella species to inject bacterial effector components into host cells, allowing them to escape being killed by oxidative burst. M01ZH09 has shown acceptable safety and excellent immunogenicity in preliminary human trials ( 99 ), although results from field trials are pending. Finally, the currently licensed polysaccharide Vi vaccine has been conjugated to a nontoxic recombinant P. aeruginosa exotoxin A carrier in an effort to improve its immunogenicity, particularly in young children ( 101 , 160 ). A randomized, controlled trial of 2 doses of the conjugate vaccine given to 12,000 Vietnamese children of 2 to 5 years of age resulted in 91.5% protective efficacy after 27 months of active surveillance, which remained at 89% protection after an additional 19 months of passive case detection ( 106 , 109 ).
A prototype oral whole-cell killed C. jejuni vaccine administered with ETEC LT as a mucosal adjuvant has been developed ( 7 ); however, immunity to Campylobacter appears to be strain specific and complex, and the antigens conferring immunity have not yet been adequately elucidated, which has hampered vaccine development ( 145 ). Furthermore, there is concern that whole-cell vaccines against this pathogen may induce the Guillain-Barre syndrome, as the exact mechanism of Camplyobacter -related Guillain-Barre syndrome remains uncertain.
In addition to vaccines, another area of research includes an effort to better assess the value of personal hygiene precautions in preventing traveler's diarrhea, in order to guide travelers in their choice of food and drink while abroad ( 144 ). Besides further research, improvements in the public health infrastructure in tropical and developing countries will likely lead to benefits not only to local populations but also to visitors ( 14 ). Hotels and restaurants can also play a role in reducing the risk of their guests' developing traveler's diarrhea by instituting educational programs that improve the culinary hygiene of their workers, which has been shown to reduce the incidence of traveler's diarrhea in Jamaica ( 6 ). Together, these efforts will hopefully reduce the enormous morbidity related to traveler's diarrhea, which would otherwise continue to increase as a global health problem due to ever-increasing international travel—for both leisure and business—that is the reality of today's world.
Travellers’ Diarrhoea
What is travellers’ diarhhoea?
Horrible bugs guilty of causing diarrhoea, vomiting and in some cases severe dehydration in people travelling to areas of high or intermediate risk, including Asia, the Middle East, Africa, Mexico, and South and Central America.
Risk areas for Travellers’ Diarrhoea
More than 20% of travellers visiting high risk areas get travellers’ diarrhoea, which can significantly disrupt their travel plans. 3,5
How do you get travellers’ diarrhoea?
Mostly from ingesting food or water that has been contaminated with the viruses, bacteria or protozoa which cause the disease. 2,3
Which countries are affected by travellers’ diarrhoea?
Travellers’ diarrhoea can occur in many areas of the world but is the most common in Asia, the Middle East, Africa, Mexico, and South and Central America. (see map). 1
What are the symptoms of travellers’ diarrhoea?
Travellers’ diarrhoea is defined as three or more unformed stools in a 24 hour period with at least one additional symptom. 4 Symptoms can start from as little as 6 hours and will depend on the type of bug that has caused the infection. They may include watery or bloody diarrhoea, abdominal pain, fever, and vomiting. 2
How serious is travellers’ diarrhoea?
Without treatment, travellers’ diarrhoea usually lasts three to seven days. 2 Medical care should be sought if symptoms do not clear up within three days or immediately in the case of fever, blood and/or mucus in stools, altered mental state, severe stomach pain, jaundice or rash. 5 Early medical care is also recommended for children, the elderly or vulnerable people cannot tolerate fluids or are dehydrated. 5
Can I prevent getting travellers’ diarrhoea?
You can take the following precautions to help reduce your risk of infection:
- Visit your nearest convenient pharmacy or specialist travel health clinic for a risk assessment before your trip
- Wash your hands frequently, especially before preparing or eating food, and after using the toilet 5
- Ensure good hygiene is practiced when swimming. Don’t swim if you have diarrhoea, and avoid ingesting any pool water 5
- Use boiled, bottled or disinfected water for drinking, preparing food and drinks, as well as brushing your teeth 6
- Avoid ice in drinks 6
- Avoid eating raw or undercooked meat, fruit and vegetables that you haven’t prepared yourself. It is also advised to avoid eating shellfish and seafood 6
Ready to get started? Check now for your nearest travel health clinic.
Get vaccinations and friendly advice from the UK's largest network of travel clinics*.
* This list is not exhaustive and other travel health providers are available.
Get started, for your free online assessment!
- Centers for Disease Control and Prevention. Yellow Book 2024. Chapter 4 Travel-Associated Infections & Diseases. Escherichia coli, Diarrheagenic. May 2023. Available online: https://wwwnc.cdc.gov/travel/yellowbook/2024/infections-diseases/escherichia-coli-diarrheagenic (Last accessed May 2023)
- Centers for Disease Control and Prevention. Yellow Book 2024. Section 2 Preparing International Travelers. Travelers’ Diarrhea. May 2023. Available online: https://wwwnc.cdc.gov/travel/yellowbook/2024/preparing/travelers-diarrhea (Last accessed May 2023)
- Ericsson CD. Travelers’ diarrhea. Epidemiology, prevention, and self treatment. Infect Dis Clin North Am 1998;12:285–303
- Steffen R. Epidemiology of travellers’ diarrhea. J Travel Med 2017;24:S2-S5.
- Factsheets. Travellers’ Diarhhoea. August 2019. Available online: https://travelhealthpro.org.uk/factsheet/53/travellers-diarrhoea (Last accessed May 2023)
- Centers for Disease Control and Prevention. Yellow Book 2024. Section 2 Preparing International Travelers. Food & Water Precautions. May 2023. Available online: https://wwwnc.cdc.gov/travel/yellowbook/2024/preparing/food-and-water-precautions (Last accessed May 2023)
UK-BOTB-2100034 (v2.0) May 2023
You are about to leave a Valneva UK Limited website and will be directed to a third party website.
Valneva are not responsible for the content provided by linked sites.
Privacy Overview
Functional cookies help to perform certain functionalities like sharing the content of the website on social media platforms, collect feedbacks, and other third-party features.
Performance cookies are used to understand and analyze the key performance indexes of the website which helps in delivering a better user experience for the visitors.
Other uncategorized cookies are those that are being analyzed and have not been classified into a category as yet.
- Travel Clinic
- Health Checks & Blood Tests
- Family Health
- Sexual Health
- Aesthetic Clinics
- Occupational Health
- Pricing List
- Login / Register
- Online Booking

Find a Clinic
Travellers’ Diarrhoea tablet
Travellers’ diarrhoea is a condition which commonly affects travellers to certain high risk countries in Africa, Asia, and South America. It can be caused by viruses, bacteria, and protozoa, and is usually transmitted via contaminated foods and water.
About the medication
- Dosage : The usual dose of Azithromycin to treat travellers’ diarrhoea is 500 mg per day.
- How to take: Take one 500mg tablet every day after symptoms start for 3 days.
- Side effects: As most medications, Azithromycin can cause side effects in some patients. Possible side effects include nausea, vomiting, abdominal discomfort, diarrhoea.
- Who can take it? Azithromycin is a prescription only medication, so a healthcare professional needs to assess whether you can use it. It may not suitable for women who are pregnant or breastfeeding, or for people taking medications that could interact with antibiotics.
- Additional precautions: Take Azithromycin exactly as you’ve been instructed. Even if you have taken tablets with you, you should also take precautions to avoid food and waterborne diseases.
How it Works
Book an appointment online, attend your consultation, get your treatment, frequently asked question, about travellers’ diarrhoea.
Travellers’ diarrhoea is a common complaint, which can be caused by bacteria, viruses and protozoa. Many travellers experience diarrhoea at some point during their travels when visiting high risk countries in South America, Africa, or Asia. Most diagnosed cases of travellers’ diarrhoea are caused by bacteria, and they are transmitted via contaminated food or drink.
Symptoms usually clear up without treatment. However, if you experience severe symptoms while travelling, or your symptoms don’t improve within three days, you need to see a doctor.
Travellers who are planning to visit high risk regions for travellers’ diarrhoea, and who will be unable to access medical help during their trip, may be advised to take medication with them in order to be able to treat the condition if they catch it.
Travellers’ diarrhoea treatment
Most patients with travellers’ diarrhoea find that they get better without treatment. During your travel health consultation, the nurse or pharmacist will assess whether it’s advisable to take treatment for travellers’ diarrhoea with you. This will depend on your medical history, as well as the countries you are travelling to and what you have planned during your trip.
While the majority of cases of travellers’ diarrhoea are caused by bacteria, it is important to note that bacteria is not the only cause of travellers’ diarrhoea, and these antibiotics will be ineffective against diarrhoea caused by viral infections or protozoa. There is no treatment that can guarantee successful treatment of travellers’ diarrhoea from every possible cause.
How is the treatment taken?
If you need to take it, treatment for travellers’ diarrhoea comes in the form of tablets that you take once a day for 3 days. Generally, treatment should be started when there is no medical help available and if bowel movements become very frequent and watery for more than 3 days. A Superdrug nurse or pharmacist can advise you more on this during a free consultation.
Even if you speak to a travel nurse or pharmacist, you should also see a doctor as soon as possible to get diagnosed. There are a range of conditions which can cause similar symptoms as travellers’ diarrhoea which may require treatment to prevent complications. Some other infections that can cause diarrhoea include cholera , typhoid , and hepatitis A .
Treating travellers’ diarrhoea without antibiotics
It is important that you drink plenty of fluids to prevent dehydration. Rehydration salts can be helpful to ensure you remain hydrated and maintain the correct balance of sugars and salts despite your symptoms.
You can try using over the counter diarrhoea remedies such as loperamide or Bismuth subsalicylate to reduce your symptoms where toilet facilities may be an issue.
If you experience traveller’s diarrhoea lasting beyond 3 days and you haven’t been prescribed an antibiotic treatment, or you have very severe symptoms, you should see a doctor without delay. If your symptoms are mild, they may resolve without treatment.
What symptoms does travellers’ diarrhoea cause?
The bacteria that cause travellers’ diarrhoea cause you to pass stools more frequently than normal, and your stool may be unusually watery.
You may find that you need to visit the toilet very urgently. If you notice any blood in your stools, have a high fever, or are getting dehydrated it’s really important you seek medical attention as soon as possible.
In addition, you may experience other digestive problems such as nausea, vomiting and stomach cramps.
In order to prevent travellers’ diarrhoea and other food and waterborne diseases, you need to practise food and water safety.
- The following will help prevent infection:
- Make sure any cooked food you buy has been cooked through and is piping hot.
- Avoid raw foods or wash them well with clean, safe water.
- Peel fruits and vegetables or wash them with clean, safe water before use.
- Drink bottled water; If unsure whether water is safe to drink, boil it or purify it before use. When buying bottled water, ensure the security seal is intact.
- Wash your hands regularly, with water and soap.
For further advice read our guide on food and water safety .
Related services
£32 per dose, cholera vaccination, from £0.65 per tablet, malaria tablets, £55 per dose, meningitis acwy vaccination, what our customers think, find your nearest clinic.
Check which of our 60+ clinics is closest to you

View all clinics

How it works
1 book an appointment.
Book online or call our booking line. Our lines are open every day!
2 Attend Consultation
During your appointment, the nurse or pharmacist will assess which vaccines or medications you need.
3 Get your treatment
Once our health advisor has assessed your needs, you'll receive your vaccinations & treatments straight away.
Popular destinations
South africa.
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
South Africa Traveler View
Travel health notices, vaccines and medicines, non-vaccine-preventable diseases, stay healthy and safe.
- Packing List
After Your Trip

There are no notices currently in effect for South Africa.
⇧ Top
Check the vaccines and medicines list and visit your doctor at least a month before your trip to get vaccines or medicines you may need. If you or your doctor need help finding a location that provides certain vaccines or medicines, visit the Find a Clinic page.
Routine vaccines
Recommendations.
Make sure you are up-to-date on all routine vaccines before every trip. Some of these vaccines include
- Chickenpox (Varicella)
- Diphtheria-Tetanus-Pertussis
- Flu (influenza)
- Measles-Mumps-Rubella (MMR)
Immunization schedules
All eligible travelers should be up to date with their COVID-19 vaccines. Please see Your COVID-19 Vaccination for more information.
COVID-19 vaccine
Active cholera transmission is widespread in South Africa. Cholera is rare in travelers. Certain factors may increase the risk of getting cholera or having severe disease ( more information ). Avoiding unsafe food and water and washing your hands can also help prevent cholera.
Vaccination may be considered for children and adults who are traveling to areas of active cholera transmission. The following areas do not have active cholera transmission: Cape Town, Durban, Kruger National Park, and Port Elizabeth.
Cholera - CDC Yellow Book
Hepatitis A
Recommended for unvaccinated travelers one year old or older going to South Africa.
Infants 6 to 11 months old should also be vaccinated against Hepatitis A. The dose does not count toward the routine 2-dose series.
Travelers allergic to a vaccine component or who are younger than 6 months should receive a single dose of immune globulin, which provides effective protection for up to 2 months depending on dosage given.
Unvaccinated travelers who are over 40 years old, immunocompromised, or have chronic medical conditions planning to depart to a risk area in less than 2 weeks should get the initial dose of vaccine and at the same appointment receive immune globulin.
Hepatitis A - CDC Yellow Book
Dosing info - Hep A
Hepatitis B
Recommended for unvaccinated travelers younger than 60 years old traveling to South Africa. Unvaccinated travelers 60 years and older may get vaccinated before traveling to South Africa.
Hepatitis B - CDC Yellow Book
Dosing info - Hep B
CDC recommends that travelers going to certain areas of South Africa take prescription medicine to prevent malaria. Depending on the medicine you take, you will need to start taking this medicine multiple days before your trip, as well as during and after your trip. Talk to your doctor about which malaria medication you should take.
Find country-specific information about malaria.
Malaria - CDC Yellow Book
Considerations when choosing a drug for malaria prophylaxis (CDC Yellow Book)
Malaria information for South Africa.
Cases of measles are on the rise worldwide. Travelers are at risk of measles if they have not been fully vaccinated at least two weeks prior to departure, or have not had measles in the past, and travel internationally to areas where measles is spreading.
All international travelers should be fully vaccinated against measles with the measles-mumps-rubella (MMR) vaccine, including an early dose for infants 6–11 months, according to CDC’s measles vaccination recommendations for international travel .
Measles (Rubeola) - CDC Yellow Book
Rabid dogs are commonly found in South Africa. If you are bitten or scratched by a dog or other mammal while in South Africa, there may be limited or no rabies treatment available.
Consider rabies vaccination before your trip if your activities mean you will be around dogs or wildlife.
Travelers more likely to encounter rabid animals include
- Campers, adventure travelers, or cave explorers (spelunkers)
- Veterinarians, animal handlers, field biologists, or laboratory workers handling animal specimens
- Visitors to rural areas
Since children are more likely to be bitten or scratched by a dog or other animals, consider rabies vaccination for children traveling to South Africa.
Rabies - CDC Yellow Book
Recommended for most travelers, especially those staying with friends or relatives or visiting smaller cities or rural areas.
Typhoid - CDC Yellow Book
Dosing info - Typhoid
Yellow Fever
Required for travelers ≥1 year old arriving from countries with risk for YF virus transmission; this includes >12-hour airport transits or layovers in countries with risk for YF virus transmission. 1
Yellow Fever - CDC Yellow Book
- Avoid contaminated water
Leptospirosis
How most people get sick (most common modes of transmission)
- Touching urine or other body fluids from an animal infected with leptospirosis
- Swimming or wading in urine-contaminated fresh water, or contact with urine-contaminated mud
- Drinking water or eating food contaminated with animal urine
- Avoid contaminated water and soil
Clinical Guidance
Schistosomiasis
- Wading, swimming, bathing, or washing in contaminated freshwater streams, rivers, ponds, lakes, or untreated pools.
Avoid bug bites
African tick-bite fever.
- Avoid Bug Bites
African Tick-bite fever
Chikungunya
- Mosquito bite
Crimean-Congo Hemorrhagic fever
- Tick bite
- Touching the body fluids of a person or animal infected with CCHF
- Avoid animals
Rift Valley Fever
- Touching blood, body fluids, or tissue of infected livestock
- Mosquito bite
Rift Valley fever
Airborne & droplet
Avian/bird flu.
- Being around, touching, or working with infected poultry, such as visiting poultry farms or live-animal markets
- Avoid domestic and wild poultry
- Breathing in air or accidentally eating food contaminated with the urine, droppings, or saliva of infected rodents
- Bite from an infected rodent
- Less commonly, being around someone sick with hantavirus (only occurs with Andes virus)
- Avoid rodents and areas where they live
- Avoid sick people
Tuberculosis (TB)
- Breathe in TB bacteria that is in the air from an infected and contagious person coughing, speaking, or singing.
Learn actions you can take to stay healthy and safe on your trip. Vaccines cannot protect you from many diseases in South Africa, so your behaviors are important.
Eat and drink safely
Food and water standards around the world vary based on the destination. Standards may also differ within a country and risk may change depending on activity type (e.g., hiking versus business trip). You can learn more about safe food and drink choices when traveling by accessing the resources below.
- Choose Safe Food and Drinks When Traveling
- Water Treatment Options When Hiking, Camping or Traveling
- Global Water, Sanitation and Hygiene | Healthy Water
- Avoid Contaminated Water During Travel
You can also visit the Department of State Country Information Pages for additional information about food and water safety.
Prevent bug bites
Bugs (like mosquitoes, ticks, and fleas) can spread a number of diseases in South Africa. Many of these diseases cannot be prevented with a vaccine or medicine. You can reduce your risk by taking steps to prevent bug bites.
What can I do to prevent bug bites?
- Cover exposed skin by wearing long-sleeved shirts, long pants, and hats.
- Use an appropriate insect repellent (see below).
- Use permethrin-treated clothing and gear (such as boots, pants, socks, and tents). Do not use permethrin directly on skin.
- Stay and sleep in air-conditioned or screened rooms.
- Use a bed net if the area where you are sleeping is exposed to the outdoors.
What type of insect repellent should I use?
- FOR PROTECTION AGAINST TICKS AND MOSQUITOES: Use a repellent that contains 20% or more DEET for protection that lasts up to several hours.
- Picaridin (also known as KBR 3023, Bayrepel, and icaridin)
- Oil of lemon eucalyptus (OLE) or para-menthane-diol (PMD)
- 2-undecanone
- Always use insect repellent as directed.
What should I do if I am bitten by bugs?
- Avoid scratching bug bites, and apply hydrocortisone cream or calamine lotion to reduce the itching.
- Check your entire body for ticks after outdoor activity. Be sure to remove ticks properly.
What can I do to avoid bed bugs?
Although bed bugs do not carry disease, they are an annoyance. See our information page about avoiding bug bites for some easy tips to avoid them. For more information on bed bugs, see Bed Bugs .
For more detailed information on avoiding bug bites, see Avoid Bug Bites .
Stay safe outdoors
If your travel plans in South Africa include outdoor activities, take these steps to stay safe and healthy during your trip.
- Stay alert to changing weather conditions and adjust your plans if conditions become unsafe.
- Prepare for activities by wearing the right clothes and packing protective items, such as bug spray, sunscreen, and a basic first aid kit.
- Consider learning basic first aid and CPR before travel. Bring a travel health kit with items appropriate for your activities.
- If you are outside for many hours in heat, eat salty snacks and drink water to stay hydrated and replace salt lost through sweating.
- Protect yourself from UV radiation : use sunscreen with an SPF of at least 15, wear protective clothing, and seek shade during the hottest time of day (10 a.m.–4 p.m.).
- Be especially careful during summer months and at high elevation. Because sunlight reflects off snow, sand, and water, sun exposure may be increased during activities like skiing, swimming, and sailing.
- Very cold temperatures can be dangerous. Dress in layers and cover heads, hands, and feet properly if you are visiting a cold location.
Stay safe around water
- Swim only in designated swimming areas. Obey lifeguards and warning flags on beaches.
- Practice safe boating—follow all boating safety laws, do not drink alcohol if driving a boat, and always wear a life jacket.
- Do not dive into shallow water.
- Do not swim in freshwater in developing areas or where sanitation is poor.
- Avoid swallowing water when swimming. Untreated water can carry germs that make you sick.
- To prevent infections, wear shoes on beaches where there may be animal waste.
Schistosomiasis, a parasitic infection that can be spread in fresh water, is found in South Africa. Avoid swimming in fresh, unchlorinated water, such as lakes, ponds, or rivers.
Keep away from animals
Most animals avoid people, but they may attack if they feel threatened, are protecting their young or territory, or if they are injured or ill. Animal bites and scratches can lead to serious diseases such as rabies.
Follow these tips to protect yourself:
- Do not touch or feed any animals you do not know.
- Do not allow animals to lick open wounds, and do not get animal saliva in your eyes or mouth.
- Avoid rodents and their urine and feces.
- Traveling pets should be supervised closely and not allowed to come in contact with local animals.
- If you wake in a room with a bat, seek medical care immediately. Bat bites may be hard to see.
All animals can pose a threat, but be extra careful around dogs, bats, monkeys, sea animals such as jellyfish, and snakes. If you are bitten or scratched by an animal, immediately:
- Wash the wound with soap and clean water.
- Go to a doctor right away.
- Tell your doctor about your injury when you get back to the United States.
Consider buying medical evacuation insurance. Rabies is a deadly disease that must be treated quickly, and treatment may not be available in some countries.
Reduce your exposure to germs
Follow these tips to avoid getting sick or spreading illness to others while traveling:
- Wash your hands often, especially before eating.
- If soap and water aren’t available, clean hands with hand sanitizer (containing at least 60% alcohol).
- Don’t touch your eyes, nose, or mouth. If you need to touch your face, make sure your hands are clean.
- Cover your mouth and nose with a tissue or your sleeve (not your hands) when coughing or sneezing.
- Try to avoid contact with people who are sick.
- If you are sick, stay home or in your hotel room, unless you need medical care.
Avoid sharing body fluids
Diseases can be spread through body fluids, such as saliva, blood, vomit, and semen.
Protect yourself:
- Use latex condoms correctly.
- Do not inject drugs.
- Limit alcohol consumption. People take more risks when intoxicated.
- Do not share needles or any devices that can break the skin. That includes needles for tattoos, piercings, and acupuncture.
- If you receive medical or dental care, make sure the equipment is disinfected or sanitized.
Know how to get medical care while traveling
Plan for how you will get health care during your trip, should the need arise:
- Carry a list of local doctors and hospitals at your destination.
- Review your health insurance plan to determine what medical services it would cover during your trip. Consider purchasing travel health and medical evacuation insurance.
- Carry a card that identifies, in the local language, your blood type, chronic conditions or serious allergies, and the generic names of any medications you take.
- Some prescription drugs may be illegal in other countries. Call South Africa’s embassy to verify that all of your prescription(s) are legal to bring with you.
- Bring all the medicines (including over-the-counter medicines) you think you might need during your trip, including extra in case of travel delays. Ask your doctor to help you get prescriptions filled early if you need to.
Many foreign hospitals and clinics are accredited by the Joint Commission International. A list of accredited facilities is available at their website ( www.jointcommissioninternational.org ).
In some countries, medicine (prescription and over-the-counter) may be substandard or counterfeit. Bring the medicines you will need from the United States to avoid having to buy them at your destination.
Malaria is a risk in some parts of South Africa. If you are going to a risk area, fill your malaria prescription before you leave, and take enough with you for the entire length of your trip. Follow your doctor’s instructions for taking the pills; some need to be started before you leave.
Select safe transportation
Motor vehicle crashes are the #1 killer of healthy US citizens in foreign countries.
In many places cars, buses, large trucks, rickshaws, bikes, people on foot, and even animals share the same lanes of traffic, increasing the risk for crashes.
Be smart when you are traveling on foot.
- Use sidewalks and marked crosswalks.
- Pay attention to the traffic around you, especially in crowded areas.
- Remember, people on foot do not always have the right of way in other countries.
Riding/Driving
Choose a safe vehicle.
- Choose official taxis or public transportation, such as trains and buses.
- Ride only in cars that have seatbelts.
- Avoid overcrowded, overloaded, top-heavy buses and minivans.
- Avoid riding on motorcycles or motorbikes, especially motorbike taxis. (Many crashes are caused by inexperienced motorbike drivers.)
- Choose newer vehicles—they may have more safety features, such as airbags, and be more reliable.
- Choose larger vehicles, which may provide more protection in crashes.
Think about the driver.
- Do not drive after drinking alcohol or ride with someone who has been drinking.
- Consider hiring a licensed, trained driver familiar with the area.
- Arrange payment before departing.
Follow basic safety tips.
- Wear a seatbelt at all times.
- Sit in the back seat of cars and taxis.
- When on motorbikes or bicycles, always wear a helmet. (Bring a helmet from home, if needed.)
- Avoid driving at night; street lighting in certain parts of South Africa may be poor.
- Do not use a cell phone or text while driving (illegal in many countries).
- Travel during daylight hours only, especially in rural areas.
- If you choose to drive a vehicle in South Africa, learn the local traffic laws and have the proper paperwork.
- Get any driving permits and insurance you may need. Get an International Driving Permit (IDP). Carry the IDP and a US-issued driver's license at all times.
- Check with your auto insurance policy's international coverage, and get more coverage if needed. Make sure you have liability insurance.
- Avoid using local, unscheduled aircraft.
- If possible, fly on larger planes (more than 30 seats); larger airplanes are more likely to have regular safety inspections.
- Try to schedule flights during daylight hours and in good weather.
Medical Evacuation Insurance
If you are seriously injured, emergency care may not be available or may not meet US standards. Trauma care centers are uncommon outside urban areas. Having medical evacuation insurance can be helpful for these reasons.
Helpful Resources
Road Safety Overseas (Information from the US Department of State): Includes tips on driving in other countries, International Driving Permits, auto insurance, and other resources.
The Association for International Road Travel has country-specific Road Travel Reports available for most countries for a minimal fee.
For information traffic safety and road conditions in South Africa, see Travel and Transportation on US Department of State's country-specific information for South Africa .
Traffic flows on the left side of the road in South Africa.
- Always pay close attention to the flow of traffic, especially when crossing the street.
- LOOK RIGHT for approaching traffic.
Maintain personal security
Use the same common sense traveling overseas that you would at home, and always stay alert and aware of your surroundings.
Before you leave
- Research your destination(s), including local laws, customs, and culture.
- Monitor travel advisories and alerts and read travel tips from the US Department of State.
- Enroll in the Smart Traveler Enrollment Program (STEP) .
- Leave a copy of your itinerary, contact information, credit cards, and passport with someone at home.
- Pack as light as possible, and leave at home any item you could not replace.
While at your destination(s)
- Carry contact information for the nearest US embassy or consulate .
- Carry a photocopy of your passport and entry stamp; leave the actual passport securely in your hotel.
- Follow all local laws and social customs.
- Do not wear expensive clothing or jewelry.
- Always keep hotel doors locked, and store valuables in secure areas.
- If possible, choose hotel rooms between the 2nd and 6th floors.
Healthy Travel Packing List
Use the Healthy Travel Packing List for South Africa for a list of health-related items to consider packing for your trip. Talk to your doctor about which items are most important for you.
Why does CDC recommend packing these health-related items?
It’s best to be prepared to prevent and treat common illnesses and injuries. Some supplies and medicines may be difficult to find at your destination, may have different names, or may have different ingredients than what you normally use.
If you are not feeling well after your trip, you may need to see a doctor. If you need help finding a travel medicine specialist, see Find a Clinic . Be sure to tell your doctor about your travel, including where you went and what you did on your trip. Also tell your doctor if you were bitten or scratched by an animal while traveling.
If your doctor prescribed antimalarial medicine for your trip, keep taking the rest of your pills after you return home. If you stop taking your medicine too soon, you could still get sick.
Malaria is always a serious disease and may be a deadly illness. If you become ill with a fever either while traveling in a malaria-risk area or after you return home (for up to 1 year), you should seek immediate medical attention and should tell the doctor about your travel history.
For more information on what to do if you are sick after your trip, see Getting Sick after Travel .
Map Disclaimer - The boundaries and names shown and the designations used on maps do not imply the expression of any opinion whatsoever on the part of the Centers for Disease Control and Prevention concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Approximate border lines for which there may not yet be full agreement are generally marked.
Other Destinations
If you need help finding travel information:
Message & data rates may apply. CDC Privacy Policy
File Formats Help:
- Adobe PDF file
- Microsoft PowerPoint file
- Microsoft Word file
- Microsoft Excel file
- Audio/Video file
- Apple Quicktime file
- RealPlayer file
- Zip Archive file
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.

IMAGES
VIDEO
COMMENTS
Description. The term Travellers' Diarrhea is used to describe gastrointestinal infections affecting travellers caused by ingesting bacteria, viruses, and protozoa. These microorganisms are found worldwide and are typically transmitted from person to person via the fecal-oral route - an infected person who does not practice proper hand or ...
Each year millions of international travelers experience traveler's diarrhea. High-risk destinations for traveler's diarrhea include areas of: Central America. South America. Mexico. Africa. South Asia and Southeast Asia. Traveling to Eastern Europe, South Africa, Central and East Asia, the Middle East, and a few Caribbean islands also poses ...
Travelers' Diarrhea. Travelers' diarrhea is the most common travel-related illness. It can occur anywhere, but the highest-risk destinations are in Asia (except for Japan and South Korea) as well as the Middle East, Africa, Mexico, and Central and South America. In otherwise healthy adults, diarrhea is rarely serious or life-threatening, but it ...
Treatment. Travelers' diarrhea (TD) is the most predictable travel-related illness. Attack rates range from 30%-70% of travelers during a 2-week period, depending on the destination and season of travel. Traditionally, TD was thought to be prevented by following simple dietary recommendations (e.g., "boil it, cook it, peel it, or forget ...
Traveller's diarrhoea is diarrhoea that develops during, or shortly after, travel abroad. Diarrhoea is defined as: 'loose or watery stools (faeces), usually at least three times in 24 hours.' ... West and North Africa, South America, East Africa. Medium-risk areas: Russia, China, Caribbean, South Africa. Low-risk areas: North America, Western ...
Traveler's diarrhea is the most common travel-related illness. It affects between 30% and 70% of travelers, depending on the destination and the season. ... Africa, Mexico and Central and South America have this type of climate at least some of the time, so travelers there are more often affected. Advertisement. What does traveler's ...
Intermediate risk areas (8-20% of travellers experience travellers' diarrhoea) include southern Europe, Israel, South Africa, and some Caribbean and Pacific islands. ... High-risk areas (more than 20% of travellers experience travellers' diarrhoea) include Africa, Latin America, the Middle East, and most parts of Asia. ...
The risk of travellers' diarrhoea can be classed as follows: Low for people travelling to western European countries, the USA and Canada, Japan, Australia, and New Zealand. Intermediate for people travelling to southern European countries, Israel, South Africa, and some Caribbean and Pacific Islands. High for people travelling to Africa, Latin ...
Contrary to the widely held belief that travelers to South Africa are at low risk of acquiring traveler's diarrhea, 5, 6 our data show that South Africa travelers are just as likely to present with traveler's diarrhea as those from neighboring countries in the region. Acute, unspecified diarrhea was the most common category reported, which may ...
Although TD symptoms are short-lived in most cases, 8-15% of affected travellers are symptomatic for more than a week and 2% develop chronic diarrhoea lasting a month or more. 11 Episodes of TD have been shown to be associated with a quintuple risk of developing irritable bowel syndrome (IBS), and post-travel IBS occurs in 3-10% of travellers.
Table 1 ⇑ illustrates overall prevalence of causative agents in returning travellers with diarrhoea. However relative importance varies with country of exposure. Rates of enterotoxigenic E coli (ETEC) are lower in travellers returning from South East Asia than in those returning from South Asia, sub-Saharan Africa, and Latin America, whereas rates of Campylobacter jejuni are higher.
If you are experiencing traveler's diarrhea, you will need to drink at least three quarts (3 liters) a day, to replace lost fluids. A sports drink (Gatorade, Powerade, Lucozade, etc) often works well, and several glasses of this should be drunk each day you are experiencing symptoms. If you can't find a sports drink, you can make your own with ...
Diagnosed only rarely in travelers, its cause is unknown. Brainerd diarrhea is a syndrome of acute onset of watery diarrhea lasting ≥4 weeks. Symptoms include 10-20 episodes of explosive, watery diarrhea per day, fecal incontinence, abdominal cramping, gas, and fatigue. Nausea, vomiting, and fever are rare. Although the cause is believed to ...
Travelers' diarrhea (TD), the most common health problem for travelers, is an intestinal infection affecting up to 70% of travelers going to developing countries. Risk is higher for young adults, persons with underlying illnesses, and those taking medicines that decrease gastric acidity. Symptoms can vary from mild to severe and can include ...
Travellers to resource-poor countries in Africa, Asia, the Middle East, and South America are at higher risk than travellers to high-income countries. Travellers' diarrhoea is frequently self-limiting in otherwise-healthy adults and children and may require only supportive treatment unless symptoms are prolonged or severe.
Destination is the most significant risk factor for developing traveler's diarrhea. 1 - 4 Regions with the highest risk are Africa, South Asia, Latin America, and the Middle East. Travelers ...
EPIDEMIOLOGY. Destination represents the single most important risk factor for developing traveler's diarrhea. High-risk regions include the developing countries of Latin America, Africa, Asia, and parts of the Middle East, which have reported attack rates for traveler's diarrhea ranging between 20 and 75% (20, 126).Areas of intermediate risk include China, southern Europe, Israel, South ...
Traveller's diarrhoea affects over 50% of travellers to some destinations and can disrupt holidays and business trips. This review examines the main causes and epidemiology of the syndrome, which is associated with poor public health infrastructure and hygiene practices, particularly in warmer climates. Although travellers may be given common sense advice on avoidance of high-risk foods and ...
Travellers' diarrhoea can occur in many areas of the world but is the most common in Asia, the Middle East, Africa, Mexico, and South and Central America. (see map). 1 What are the symptoms of travellers' diarrhoea?
Travellers' diarrhoea is a condition which commonly affects travellers to certain high risk countries in Africa, Asia, and South America. It can be caused by viruses, bacteria, and protozoa, and is usually transmitted via contaminated foods and water.
Before the trip. For Canadian travelers, the risk of TD is highest in Asia, the Middle East, Africa, and Central and South America. 2 Canadians traveling to Eastern Europe, South Africa, Mexico, and the Caribbean Islands also have a higher risk of TD. 2 Patients planning trips to these locations should plan ahead by packing oral rehydration solution, loperamide, and an antibiotic such as ...
Recommended for unvaccinated travelers younger than 60 years old traveling to South Africa. Unvaccinated travelers 60 years and older may get vaccinated before traveling to South Africa. CDC recommends that travelers going to certain areas of South Africa take prescription medicine to prevent malaria.