

Family Life

AAP Schedule of Well-Child Care Visits

Parents know who they should go to when their child is sick. But pediatrician visits are just as important for healthy children.
The Bright Futures /American Academy of Pediatrics (AAP) developed a set of comprehensive health guidelines for well-child care, known as the " periodicity schedule ." It is a schedule of screenings and assessments recommended at each well-child visit from infancy through adolescence.
Schedule of well-child visits
- The first week visit (3 to 5 days old)
- 1 month old
- 2 months old
- 4 months old
- 6 months old
- 9 months old
- 12 months old
- 15 months old
- 18 months old
- 2 years old (24 months)
- 2 ½ years old (30 months)
- 3 years old
- 4 years old
- 5 years old
- 6 years old
- 7 years old
- 8 years old
- 9 years old
- 10 years old
- 11 years old
- 12 years old
- 13 years old
- 14 years old
- 15 years old
- 16 years old
- 17 years old
- 18 years old
- 19 years old
- 20 years old
- 21 years old
The benefits of well-child visits
Prevention . Your child gets scheduled immunizations to prevent illness. You also can ask your pediatrician about nutrition and safety in the home and at school.
Tracking growth & development . See how much your child has grown in the time since your last visit, and talk with your doctor about your child's development. You can discuss your child's milestones, social behaviors and learning.
Raising any concerns . Make a list of topics you want to talk about with your child's pediatrician such as development, behavior, sleep, eating or getting along with other family members. Bring your top three to five questions or concerns with you to talk with your pediatrician at the start of the visit.
Team approach . Regular visits create strong, trustworthy relationships among pediatrician, parent and child. The AAP recommends well-child visits as a way for pediatricians and parents to serve the needs of children. This team approach helps develop optimal physical, mental and social health of a child.
More information
Back to School, Back to Doctor
Recommended Immunization Schedules
Milestones Matter: 10 to Watch for by Age 5
Your Child's Checkups
- Bright Futures/AAP Recommendations for Preventive Pediatric Health Care (periodicity schedule)
Catch Up on Well-Child Visits and Recommended Vaccinations

Many children missed check-ups and recommended childhood vaccinations over the past few years. CDC and the American Academy of Pediatrics (AAP) recommend children catch up on routine childhood vaccinations and get back on track for school, childcare, and beyond.

Making sure that your child sees their doctor for well-child visits and recommended vaccines is one of the best things you can do to protect your child and community from serious diseases that are easily spread.
Well-Child Visits and Recommended Vaccinations Are Essential

Well-child visits and recommended vaccinations are essential and help make sure children stay healthy. Children who are not protected by vaccines are more likely to get diseases like measles and whooping cough . These diseases are extremely contagious and can be very serious, especially for babies and young children. In recent years, there have been outbreaks of these diseases, especially in communities with low vaccination rates.
Well-child visits are essential for many reasons , including:
- Tracking growth and developmental milestones
- Discussing any concerns about your child’s health
- Getting scheduled vaccinations to prevent illnesses like measles and whooping cough (pertussis) and other serious diseases

It’s particularly important for parents to work with their child’s doctor or nurse to make sure they get caught up on missed well-child visits and recommended vaccines.
Routinely Recommended Vaccines for Children and Adolescents
Getting children and adolescents caught up with recommended vaccinations is the best way to protect them from a variety of vaccine-preventable diseases . The schedules below outline the vaccines recommended for each age group.
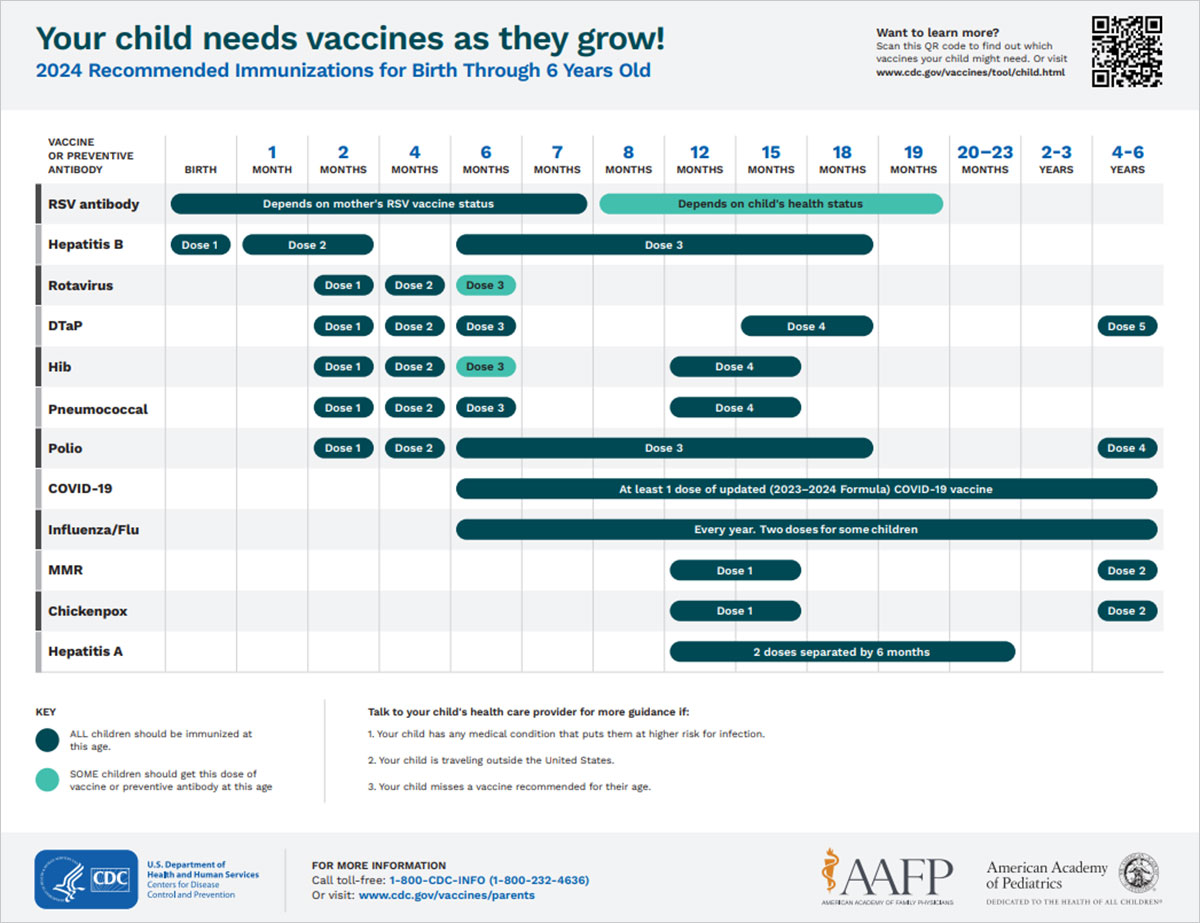
See which vaccines your child needs from birth through age 6 in this easy-to-read immunization schedule.
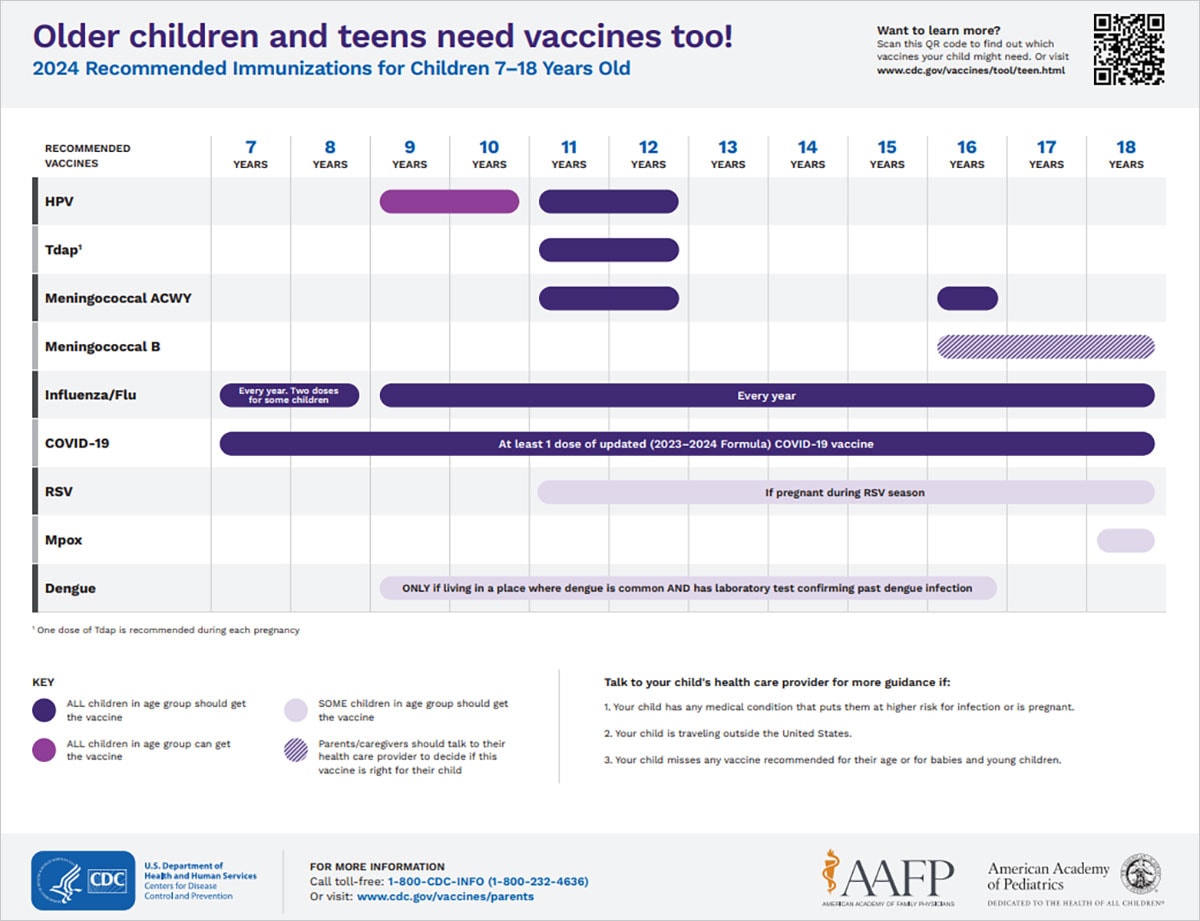
See which vaccines your child needs from ages 7 through 18 in this easy-to-read immunization schedule.
The Vaccines for Children (VFC) program provides vaccines to eligible children at no cost. This program provides free vaccines to children who are Medicaid-eligible, uninsured, underinsured, or American Indian/Alaska Native. Check out the program’s requirements and talk to your child’s doctor or nurse to see if they are a VFC provider. You can also find a VFC provider by calling your state or local health department or seeing if your state has a VFC website.

COVID-19 Vaccines for Children and Teens
Everyone aged 6 months and older can get an updated COVID-19 vaccine to help protect against severe illness, hospitalization and death. Learn more about making sure your child stays up to date with their COVID-19 vaccines .
- Vaccines & Immunizations
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.

KATHERINE TURNER, MD
Am Fam Physician. 2018;98(6):347-353
Related letter: Well-Child Visits Provide Physicians Opportunity to Deliver Interconception Care to Mothers
Author disclosure: No relevant financial affiliations.
The well-child visit allows for comprehensive assessment of a child and the opportunity for further evaluation if abnormalities are detected. A complete history during the well-child visit includes information about birth history; prior screenings; diet; sleep; dental care; and medical, surgical, family, and social histories. A head-to-toe examination should be performed, including a review of growth. Immunizations should be reviewed and updated as appropriate. Screening for postpartum depression in mothers of infants up to six months of age is recommended. Based on expert opinion, the American Academy of Pediatrics recommends developmental surveillance at each visit, with formal developmental screening at nine, 18, and 30 months and autism-specific screening at 18 and 24 months; the U.S. Preventive Services Task Force found insufficient evidence to make a recommendation. Well-child visits provide the opportunity to answer parents' or caregivers' questions and to provide age-appropriate guidance. Car seats should remain rear facing until two years of age or until the height or weight limit for the seat is reached. Fluoride use, limiting or avoiding juice, and weaning to a cup by 12 months of age may improve dental health. A one-time vision screening between three and five years of age is recommended by the U.S. Preventive Services Task Force to detect amblyopia. The American Academy of Pediatrics guideline based on expert opinion recommends that screen time be avoided, with the exception of video chatting, in children younger than 18 months and limited to one hour per day for children two to five years of age. Cessation of breastfeeding before six months and transition to solid foods before six months are associated with childhood obesity. Juice and sugar-sweetened beverages should be avoided before one year of age and provided only in limited quantities for children older than one year.
Well-child visits for infants and young children (up to five years) provide opportunities for physicians to screen for medical problems (including psychosocial concerns), to provide anticipatory guidance, and to promote good health. The visits also allow the family physician to establish a relationship with the parents or caregivers. This article reviews the U.S. Preventive Services Task Force (USPSTF) and the American Academy of Pediatrics (AAP) guidelines for screenings and recommendations for infants and young children. Family physicians should prioritize interventions with the strongest evidence for patient-oriented outcomes, such as immunizations, postpartum depression screening, and vision screening.
Clinical Examination
The history should include a brief review of birth history; prematurity can be associated with complex medical conditions. 1 Evaluate breastfed infants for any feeding problems, 2 and assess formula-fed infants for type and quantity of iron-fortified formula being given. 3 For children eating solid foods, feeding history should include everything the child eats and drinks. Sleep, urination, defecation, nutrition, dental care, and child safety should be reviewed. Medical, surgical, family, and social histories should be reviewed and updated. For newborns, review the results of all newborn screening tests ( Table 1 4 – 7 ) and schedule follow-up visits as necessary. 2
PHYSICAL EXAMINATION
A comprehensive head-to-toe examination should be completed at each well-child visit. Interval growth should be reviewed by using appropriate age, sex, and gestational age growth charts for height, weight, head circumference, and body mass index if 24 months or older. The Centers for Disease Control and Prevention (CDC)-recommended growth charts can be found at https://www.cdc.gov/growthcharts/who_charts.htm#The%20WHO%20Growth%20Charts . Percentiles and observations of changes along the chart's curve should be assessed at every visit. Include assessment of parent/caregiver-child interactions and potential signs of abuse such as bruises on uncommonly injured areas, burns, human bite marks, bruises on nonmobile infants, or multiple injuries at different healing stages. 8
The USPSTF and AAP screening recommendations are outlined in Table 2 . 3 , 9 – 27 A summary of AAP recommendations can be found at https://www.aap.org/en-us/Documents/periodicity_schedule.pdf . The American Academy of Family Physicians (AAFP) generally adheres to USPSTF recommendations. 28
MATERNAL DEPRESSION
Prevalence of postpartum depression is around 12%, 22 and its presence can impair infant development. The USPSTF and AAP recommend using the Edinburgh Postnatal Depression Scale (available at https://www.aafp.org/afp/2010/1015/p926.html#afp20101015p926-f1 ) or the Patient Health Questionnaire-2 (available at https://www.aafp.org/afp/2012/0115/p139.html#afp20120115p139-t3 ) to screen for maternal depression. The USPSTF does not specify a screening schedule; however, based on expert opinion, the AAP recommends screening mothers at the one-, two-, four-, and six-month well-child visits, with further evaluation for positive results. 23 There are no recommendations to screen other caregivers if the mother is not present at the well-child visit.
PSYCHOSOCIAL
With nearly one-half of children in the United States living at or near the poverty level, assessing home safety, food security, and access to safe drinking water can improve awareness of psychosocial problems, with referrals to appropriate agencies for those with positive results. 29 The prevalence of mental health disorders (i.e., primarily anxiety, depression, behavioral disorders, attention-deficit/hyperactivity disorder) in preschool-aged children is around 6%. 30 Risk factors for these disorders include having a lower socioeconomic status, being a member of an ethnic minority, and having a non–English-speaking parent or primary caregiver. 25 The USPSTF found insufficient evidence regarding screening for depression in children up to 11 years of age. 24 Based on expert opinion, the AAP recommends that physicians consider screening, although screening in young children has not been validated or standardized. 25
DEVELOPMENT AND SURVEILLANCE
Based on expert opinion, the AAP recommends early identification of developmental delays 14 and autism 10 ; however, the USPSTF found insufficient evidence to recommend formal developmental screening 13 or autism-specific screening 9 if the parents/caregivers or physician have no concerns. If physicians choose to screen, developmental surveillance of language, communication, gross and fine movements, social/emotional development, and cognitive/problem-solving skills should occur at each visit by eliciting parental or caregiver concerns, obtaining interval developmental history, and observing the child. Any area of concern should be evaluated with a formal developmental screening tool, such as Ages and Stages Questionnaire, Parents' Evaluation of Developmental Status, Parents' Evaluation of Developmental Status-Developmental Milestones, or Survey of Well-Being of Young Children. These tools can be found at https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/Screening/Pages/Screening-Tools.aspx . If results are abnormal, consider intervention or referral to early intervention services. The AAP recommends completing the previously mentioned formal screening tools at nine-, 18-, and 30-month well-child visits. 14
The AAP also recommends autism-specific screening at 18 and 24 months. 10 The USPSTF recommends using the two-step Modified Checklist for Autism in Toddlers (M-CHAT) screening tool (available at https://m-chat.org/ ) if a physician chooses to screen a patient for autism. 10 The M-CHAT can be incorporated into the electronic medical record, with the possibility of the parent or caregiver completing the questionnaire through the patient portal before the office visit.
IRON DEFICIENCY
Multiple reports have associated iron deficiency with impaired neurodevelopment. Therefore, it is essential to ensure adequate iron intake. Based on expert opinion, the AAP recommends supplements for preterm infants beginning at one month of age and exclusively breastfed term infants at six months of age. 3 The USPSTF found insufficient evidence to recommend screening for iron deficiency in infants. 19 Based on expert opinion, the AAP recommends measuring a child's hemoglobin level at 12 months of age. 3
Lead poisoning and elevated lead blood levels are prevalent in young children. The AAP and CDC recommend a targeted screening approach. The AAP recommends screening for serum lead levels between six months and six years in high-risk children; high-risk children are identified by location-specific risk recommendations, enrollment in Medicaid, being foreign born, or personal screening. 21 The USPSTF does not recommend screening for lead poisoning in children at average risk who are asymptomatic. 20
The USPSTF recommends at least one vision screening to detect amblyopia between three and five years of age. Testing options include visual acuity, ocular alignment test, stereoacuity test, photoscreening, and autorefractors. The USPSTF found insufficient evidence to recommend screening before three years of age. 26 The AAP, American Academy of Ophthalmology, and the American Academy of Pediatric Ophthalmology and Strabismus recommend the use of an instrument-based screening (photoscreening or autorefractors) between 12 months and three years of age and annual visual acuity screening beginning at four years of age. 31
IMMUNIZATIONS
The AAFP recommends that all children be immunized. 32 Recommended vaccination schedules, endorsed by the AAP, the AAFP, and the Advisory Committee on Immunization Practices, are found at https://www.cdc.gov/vaccines/schedules/hcp/child-adolescent.html . Immunizations are usually administered at the two-, four-, six-, 12-, and 15- to 18-month well-child visits; the four- to six-year well-child visit; and annually during influenza season. Additional vaccinations may be necessary based on medical history. 33 Immunization history should be reviewed at each wellness visit.
Anticipatory Guidance
Injuries remain the leading cause of death among children, 34 and the AAP has made several recommendations to decrease the risk of injuries. 35 – 42 Appropriate use of child restraints minimizes morbidity and mortality associated with motor vehicle collisions. Infants need a rear-facing car safety seat until two years of age or until they reach the height or weight limit for the specific car seat. Children should then switch to a forward-facing car seat for as long as the seat allows, usually 65 to 80 lb (30 to 36 kg). 35 Children should never be unsupervised around cars, driveways, and streets. Young children should wear bicycle helmets while riding tricycles or bicycles. 37
Having functioning smoke detectors and an escape plan decreases the risk of fire- and smoke-related deaths. 36 Water heaters should be set to a maximum of 120°F (49°C) to prevent scald burns. 37 Infants and young children should be watched closely around any body of water, including water in bathtubs and toilets, to prevent drowning. Swimming pools and spas should be completely fenced with a self-closing, self-latching gate. 38
Infants should not be left alone on any high surface, and stairs should be secured by gates. 43 Infant walkers should be discouraged because they provide no benefit and they increase falls down stairs, even if stair gates are installed. 39 Window locks, screens, or limited-opening windows decrease injury and death from falling. 40 Parents or caregivers should also anchor furniture to a wall to prevent heavy pieces from toppling over. Firearms should be kept unloaded and locked. 41
Young children should be closely supervised at all times. Small objects are a choking hazard, especially for children younger than three years. Latex balloons, round objects, and food can cause life-threatening airway obstruction. 42 Long strings and cords can strangle children. 37
DENTAL CARE
Infants should never have a bottle in bed, and babies should be weaned to a cup by 12 months of age. 44 Juices should be avoided in infants younger than 12 months. 45 Fluoride use inhibits tooth demineralization and bacterial enzymes and also enhances remineralization. 11 The AAP and USPSTF recommend fluoride supplementation and the application of fluoride varnish for teeth if the water supply is insufficient. 11 , 12 Begin brushing teeth at tooth eruption with parents or caregivers supervising brushing until mastery. Children should visit a dentist regularly, and an assessment of dental health should occur at well-child visits. 44
SCREEN TIME
Hands-on exploration of their environment is essential to development in children younger than two years. Video chatting is acceptable for children younger than 18 months; otherwise digital media should be avoided. Parents and caregivers may use educational programs and applications with children 18 to 24 months of age. If screen time is used for children two to five years of age, the AAP recommends a maximum of one hour per day that occurs at least one hour before bedtime. Longer usage can cause sleep problems and increases the risk of obesity and social-emotional delays. 46
To decrease the risk of sudden infant death syndrome (SIDS), the AAP recommends that infants sleep on their backs on a firm mattress for the first year of life with no blankets or other soft objects in the crib. 45 Breastfeeding, pacifier use, and room sharing without bed sharing protect against SIDS; infant exposure to tobacco, alcohol, drugs, and sleeping in bed with parents or caregivers increases the risk of SIDS. 47
DIET AND ACTIVITY
The USPSTF, AAFP, and AAP all recommend breastfeeding until at least six months of age and ideally for the first 12 months. 48 Vitamin D 400 IU supplementation for the first year of life in exclusively breastfed infants is recommended to prevent vitamin D deficiency and rickets. 49 Based on expert opinion, the AAP recommends the introduction of certain foods at specific ages. Early transition to solid foods before six months is associated with higher consumption of fatty and sugary foods 50 and an increased risk of atopic disease. 51 Delayed transition to cow's milk until 12 months of age decreases the incidence of iron deficiency. 52 Introduction of highly allergenic foods, such as peanut-based foods and eggs, before one year decreases the likelihood that a child will develop food allergies. 53
With approximately 17% of children being obese, many strategies for obesity prevention have been proposed. 54 The USPSTF does not have a recommendation for screening or interventions to prevent obesity in children younger than six years. 54 The AAP has made several recommendations based on expert opinion to prevent obesity. Cessation of breastfeeding before six months and introduction of solid foods before six months are associated with childhood obesity and are not recommended. 55 Drinking juice should be avoided before one year of age, and, if given to older children, only 100% fruit juice should be provided in limited quantities: 4 ounces per day from one to three years of age and 4 to 6 ounces per day from four to six years of age. Intake of other sugar-sweetened beverages should be discouraged to help prevent obesity. 45 The AAFP and AAP recommend that children participate in at least 60 minutes of active free play per day. 55 , 56
Data Sources: Literature search was performed using the USPSTF published recommendations ( https://www.uspreventiveservicestaskforce.org/BrowseRec/Index/browse-recommendations ) and the AAP Periodicity table ( https://www.aap.org/en-us/Documents/periodicity_schedule.pdf ). PubMed searches were completed using the key terms pediatric, obesity prevention, and allergy prevention with search limits of infant less than 23 months or pediatric less than 18 years. The searches included systematic reviews, randomized controlled trials, clinical trials, and position statements. Essential Evidence Plus was also reviewed. Search dates: May through October 2017.
Gauer RL, Burket J, Horowitz E. Common questions about outpatient care of premature infants. Am Fam Physician. 2014;90(4):244-251.
American Academy of Pediatrics; Committee on Fetus and Newborn. Hospital stay for healthy term newborns. Pediatrics. 2010;125(2):405-409.
Baker RD, Greer FR Committee on Nutrition, American Academy of Pediatrics. Diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0–3 years of age). Pediatrics. 2010;126(5):1040-1050.
Mahle WT, Martin GR, Beekman RH, Morrow WR Section on Cardiology and Cardiac Surgery Executive Committee. Endorsement of Health and Human Services recommendation for pulse oximetry screening for critical congenital heart disease. Pediatrics. 2012;129(1):190-192.
American Academy of Pediatrics Newborn Screening Authoring Committee. Newborn screening expands: recommendations for pediatricians and medical homes—implications for the system. Pediatrics. 2008;121(1):192-217.
American Academy of Pediatrics, Joint Committee on Infant Hearing. Year 2007 position statement: principles and guidelines for early hearing detection and intervention programs. Pediatrics. 2007;120(4):898-921.
Maisels MJ, Bhutani VK, Bogen D, Newman TB, Stark AR, Watchko JF. Hyperbilirubinemia in the newborn infant > or = 35 weeks' gestation: an update with clarifications. Pediatrics. 2009;124(4):1193-1198.
Christian CW Committee on Child Abuse and Neglect, American Academy of Pediatrics. The evaluation of suspected child physical abuse [published correction appears in Pediatrics . 2015;136(3):583]. Pediatrics. 2015;135(5):e1337-e1354.
Siu AL, Bibbins-Domingo K, Grossman DC, et al. Screening for autism spectrum disorder in young children: U.S. Preventive Services Task Force recommendation statement. JAMA. 2016;315(7):691-696.
Johnson CP, Myers SM American Academy of Pediatrics Council on Children with Disabilities. Identification and evaluation of children with autism spectrum disorders. Pediatrics. 2007;120(5):1183-1215.
Moyer VA. Prevention of dental caries in children from birth through age 5 years: U.S. Preventive Services Task Force recommendation statement. Pediatrics. 2014;133(6):1102-1111.
Clark MB, Slayton RL American Academy of Pediatrics Section on Oral Health. Fluoride use in caries prevention in the primary care setting. Pediatrics. 2014;134(3):626-633.
Siu AL. Screening for speech and language delay and disorders in children aged 5 years and younger: U.S. Preventive Services Task Force recommendation statement. Pediatrics. 2015;136(2):e474-e481.
Council on Children with Disabilities, Section on Developmental Behavioral Pediatrics, Bright Futures Steering Committee, Medical Home Initiatives for Children with Special Needs Project Advisory Committee. Identifying infants and young children with developmental disorders in the medical home: an algorithm for developmental surveillance and screening [published correction appears in Pediatrics . 2006;118(4):1808–1809]. Pediatrics. 2006;118(1):405-420.
Bibbins-Domingo K, Grossman DC, Curry SJ, et al. Screening for lipid disorders in children and adolescents: U.S. Preventive Services Task Force recommendation statement. JAMA. 2016;316(6):625-633.
National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents. October 2012. https://www.nhlbi.nih.gov/sites/default/files/media/docs/peds_guidelines_full.pdf . Accessed May 9, 2018.
Moyer VA. Screening for primary hypertension in children and adolescents: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;159(9):613-619.
Flynn JT, Kaelber DC, Baker-Smith CM, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents [published correction appears in Pediatrics . 2017;140(6):e20173035]. Pediatrics. 2017;140(3):e20171904.
Siu AL. Screening for iron deficiency anemia in young children: USPSTF recommendation statement. Pediatrics. 2015;136(4):746-752.
U.S. Preventive Services Task Force. Screening for elevated blood lead levels in children and pregnant women. Pediatrics. 2006;118(6):2514-2518.
Screening Young Children for Lead Poisoning: Guidance for State and Local Public Health Officials . Atlanta, Ga.: U.S. Public Health Service; Centers for Disease Control and Prevention; National Center for Environmental Health; 1997.
O'Connor E, Rossom RC, Henninger M, Groom HC, Burda BU. Primary care screening for and treatment of depression in pregnant and post-partum women: evidence report and systematic review for the U.S. Preventive Services Task Force. JAMA. 2016;315(4):388-406.
Earls MF Committee on Psychosocial Aspects of Child and Family Health, American Academy of Pediatrics. Incorporating recognition and management of perinatal and postpartum depression into pediatric practice. Pediatrics. 2010;126(5):1032-1039.
Siu AL. Screening for depression in children and adolescents: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2016;164(5):360-366.
Weitzman C, Wegner L American Academy of Pediatrics Section on Developmental and Behavioral Pediatrics; Committee on Psychosocial Aspects of Child and Family Health; Council on Early Childhood; Society for Developmental and Behavioral Pediatrics; American Academy of Pediatrics. Promoting optimal development: screening for behavioral and emotional problems [published correction appears in Pediatrics . 2015;135(5):946]. Pediatrics. 2015;135(2):384-395.
Grossman DC, Curry SJ, Owens DK, et al. Vision screening in children aged 6 months to 5 years: U.S. Preventive Services Task Force recommendation statement. JAMA. 2017;318(9):836-844.
Donahue SP, Nixon CN Committee on Practice and Ambulatory Medicine, Section on Ophthalmology, American Academy of Pediatrics; American Association of Certified Orthoptists, American Association for Pediatric Ophthalmology and Strabismus, American Academy of Ophthalmology. Visual system assessment in infants, children, and young adults by pediatricians. Pediatrics. 2016;137(1):28-30.
Lin KW. What to do at well-child visits: the AAFP's perspective. Am Fam Physician. 2015;91(6):362-364.
American Academy of Pediatrics Council on Community Pediatrics. Poverty and child health in the United States. Pediatrics. 2016;137(4):e20160339.
Lavigne JV, Lebailly SA, Hopkins J, Gouze KR, Binns HJ. The prevalence of ADHD, ODD, depression, and anxiety in a community sample of 4-year-olds. J Clin Child Adolesc Psychol. 2009;38(3):315-328.
American Academy of Pediatrics Committee on Practice and Ambulatory Medicine, Section on Ophthalmology, American Association of Certified Orthoptists, American Association for Pediatric Ophthalmology and Strabismus, American Academy of Ophthalmology. Visual system assessment of infants, children, and young adults by pediatricians. Pediatrics. 2016;137(1):28-30.
American Academy of Family Physicians. Clinical preventive service recommendation. Immunizations. http://www.aafp.org/patient-care/clinical-recommendations/all/immunizations.html . Accessed October 5, 2017.
Centers for Disease Control and Prevention. Recommended immunization schedule for children and adolescents aged 18 years or younger, United States, 2018. https://www.cdc.gov/vaccines/schedules/hcp/child-adolescent.html . Accessed May 9, 2018.
National Center for Injury Prevention and Control. 10 leading causes of death by age group, United States—2015. https://www.cdc.gov/injury/images/lc-charts/leading_causes_of_death_age_group_2015_1050w740h.gif . Accessed April 24, 2017.
Durbin DR American Academy of Pediatrics Committee on Injury, Violence, and Poison Prevention. Child passenger safety. Pediatrics. 2011;127(4):788-793.
American Academy of Pediatrics Committee on Injury and Poison Prevention. Reducing the number of deaths and injuries from residential fires. Pediatrics. 2000;105(6):1355-1357.
Gardner HG American Academy of Pediatrics Committee on Injury, Violence, and Poison Prevention. Office-based counseling for unintentional injury prevention. Pediatrics. 2007;119(1):202-206.
American Academy of Pediatrics Committee on Injury, Violence, and Poison Prevention. Prevention of drowning in infants, children, and adolescents. Pediatrics. 2003;112(2):437-439.
American Academy of Pediatrics Committee on Injury and Poison Prevention. Injuries associated with infant walkers. Pediatrics. 2001;108(3):790-792.
American Academy of Pediatrics Committee on Injury and Poison Prevention. Falls from heights: windows, roofs, and balconies. Pediatrics. 2001;107(5):1188-1191.
Dowd MD, Sege RD Council on Injury, Violence, and Poison Prevention Executive Committee; American Academy of Pediatrics. Firearm-related injuries affecting the pediatric population. Pediatrics. 2012;130(5):e1416-e1423.
American Academy of Pediatrics Committee on Injury, Violence, and Poison Prevention. Prevention of choking among children. Pediatrics. 2010;125(3):601-607.
Kendrick D, Young B, Mason-Jones AJ, et al. Home safety education and provision of safety equipment for injury prevention (review). Evid Based Child Health. 2013;8(3):761-939.
American Academy of Pediatrics Section on Oral Health. Maintaining and improving the oral health of young children. Pediatrics. 2014;134(6):1224-1229.
Heyman MB, Abrams SA American Academy of Pediatrics Section on Gastroenterology, Hepatology, and Nutrition Committee on Nutrition. Fruit juice in infants, children, and adolescents: current recommendations. Pediatrics. 2017;139(6):e20170967.
Council on Communications and Media. Media and young minds. Pediatrics. 2016;138(5):e20162591.
Moon RY Task Force on Sudden Infant Death Syndrome. SIDS and other sleep-related infant deaths: evidence base for 2016 updated recommendations for a safe infant sleeping environment. Pediatrics. 2016;138(5):e20162940.
American Academy of Pediatrics Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics. 2012;129(3):e827-e841.
Wagner CL, Greer FR American Academy of Pediatrics Section on Breastfeeding; Committee on Nutrition. Prevention of rickets and vitamin D deficiency in infants, children, and adolescents [published correction appears in Pediatrics . 2009;123(1):197]. Pediatrics. 2008;122(5):1142-1152.
Huh SY, Rifas-Shiman SL, Taveras EM, Oken E, Gillman MW. Timing of solid food introduction and risk of obesity in preschool-aged children. Pediatrics. 2011;127(3):e544-e551.
Greer FR, Sicherer SH, Burks AW American Academy of Pediatrics Committee on Nutrition; Section on Allergy and Immunology. Effects of early nutritional interventions on the development of atopic disease in infants and children: the role of maternal dietary restriction, breastfeeding, timing of introduction of complementary foods, and hydrolyzed formulas. Pediatrics. 2008;121(1):183-191.
American Academy of Pediatrics Committee on Nutrition. The use of whole cow's milk in infancy. Pediatrics. 1992;89(6 pt 1):1105-1109.
Fleischer DM, Spergel JM, Assa'ad AH, Pongracic JA. Primary prevention of allergic disease through nutritional interventions. J Allergy Clin Immunol Pract. 2013;1(1):29-36.
Grossman DC, Bibbins-Domingo K, Curry SJ, et al. Screening for obesity in children and adolescents: U.S. Preventive Services Task Force recommendation statement. JAMA. 2017;317(23):2417-2426.
Daniels SR, Hassink SG Committee on Nutrition. The role of the pediatrician in primary prevention of obesity. Pediatrics. 2015;136(1):e275-e292.
American Academy of Family Physicians. Physical activity in children. https://www.aafp.org/about/policies/all/physical-activity.html . Accessed January 1, 2018.
Continue Reading

More in AFP
More in pubmed.
Copyright © 2018 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Internet Explorer Alert
It appears you are using Internet Explorer as your web browser. Please note, Internet Explorer is no longer up-to-date and can cause problems in how this website functions This site functions best using the latest versions of any of the following browsers: Edge, Firefox, Chrome, Opera, or Safari . You can find the latest versions of these browsers at https://browsehappy.com
- Publications
- HealthyChildren.org
Shopping cart
Order Subtotal
Your cart is empty.
Looks like you haven't added anything to your cart.
- Career Resources
- Philanthropy
- About the AAP
- The Role of the Pediatrician in the Promotion of Healthy, Active Living
- How Can You Support Patients in Healthy, Active Living? Check Out Updated Report
- Helping Kids Build Healthy Active Lives: AAP Policy Explained
- Climate Change & Children’s Health: AAP Policy Explained
- News Releases
- Policy Collections
- The State of Children in 2020
- Healthy Children
- Secure Families
- Strong Communities
- A Leading Nation for Youth
- Transition Plan: Advancing Child Health in the Biden-Harris Administration
- Health Care Access & Coverage
- Immigrant Child Health
- Gun Violence Prevention
- Tobacco & E-Cigarettes
- Child Nutrition
- Assault Weapons Bans
- Childhood Immunizations
- E-Cigarette and Tobacco Products
- Children’s Health Care Coverage Fact Sheets
- Opioid Fact Sheets
- Advocacy Training Modules
- Subspecialty Advocacy Report
- AAP Washington Office Internship
- Online Courses
- Live and Virtual Activities
- National Conference and Exhibition
- Prep®- Pediatric Review and Education Programs
- Journals and Publications
- NRP LMS Login
- Patient Care
- Practice Management
- AAP Committees
- AAP Councils
- AAP Sections
- Volunteer Network
- Join a Chapter
- Chapter Websites
- Chapter Executive Directors
- District Map
- Create Account

- Materials & Tools
- Clinical Practice
- States & Communities
- Quality Improvement
- Implementation Stories
Well-Child Visits: Parent and Patient Education
The Bright Futures Parent and Patient Educational Handouts help guide anticipatory guidance and reinforce key messages (organized around the 5 priorities in each visit) for the family. Each educational handout is written in plain language to ensure the information is clear, concise, relevant, and easy to understand. Each educational handout is available in English and Spanish (in HTML and PDF format). Beginning at the 7 year visit , there is both a Parent and Patient education handout (in English and Spanish).
For the Bright Futures Parent Handouts for well-child visits up to 2 years of age , translations of 12 additional languages (PDF format) are made possible thanks to the generous support of members, staff, and businesses who donate to the AAP Friends of Children Fund . The 12 additional languages are Arabic, Bengali, Chinese, French, Haitian Creole, Hmong, Korean, Polish, Portuguese, Russian, Somali, and Vietnamese.
Reminder for Health Care Professionals: The Bright Futures Tool and Resource Kit, 2nd Edition is available as an online access product. For more detailed information about the Toolkit, visit shop.aap.org . To license the Toolkit to use the forms in practice and/or incorporate them into an Electronic Medical Record System, please contact AAP Sales .
Parent Educational Handouts
Infancy visits.

3 to 5 Day Visit
1 Month Visit
2 Month Visit
4 Month Visit
6 Month Visit
9 Month Visit
Early childhood visits.
12 Month Visit
15 Month Visit
18 Month Visit
2 Year Visit
2.5 Year Visit
3 Year Visit
4 Year Visit
Parent and patient educational handouts, middle childhood visits.
5-6 Year Visit
7-8 Year Visit
7-8 Year Visit - For Patients
9-10 Year Visit
9-10 Year Visit - For Patients
Adolescent visits.
11-14 Year Visit
11-14 Year Visit - For Patients
15-17 Year Visit

15-17 Year Visit - For Patients

18-21 Year Visit - For Patients
Last updated.
American Academy of Pediatrics
- Second Opinion
Well-Care Visits

What is a well-care visit?
It's important to take your child to the healthcare provider when your child is ill. Or when you child needs an exam to take part in a sport. But routine well-care visits are also recommended.
Well-care, well-baby, or well-child visits are routine visits to your child's healthcare provider for the following:
Physical exam
Immunization updates
Tracking growth and development
Finding any problems before they become serious
Providing information on health and safety issues
Providing information on nutrition and physical fitness
Providing information on how to manage emergencies and illnesses
Your child's healthcare provider can also provide guidance on other issues, such as the following:
Behavioral problems
Learning problems
Emotional problems
Family problems
Socialization problems
Puberty and concerns about teenage years
When should well-care visits be scheduled?
Your child's healthcare provider will give you a schedule of ages when a well-care visit is suggested. The American Academy of Pediatrics recommends well-care visits at the following ages:
Before a newborn is discharged from the hospital, or at 48 to 72 hours of age
3 to 5 days
2 to 4 weeks
Annually, between ages 6 and 21
- Pediatric Cardiology
- Our Services
- Chiari Malformation Center at Stanford Medicine Children's Health
Related Topics
When to Call Your Child's Healthcare Provider
Home Page - Pediatrics
Pediatrician
Connect with us:
Download our App:
- Leadership Team
- Vision, Mission & Values
- The Stanford Advantage
- Government and Community Relations
- Get Involved
- Volunteer Services
- Auxiliaries & Affiliates
© 123 Stanford Medicine Children’s Health
Preventive Health Care Visits in Children
Scheduled visits to the doctor (also called well-child visits) provide parents with information about their child's growth and development. Such visits also give parents an opportunity to ask questions and seek advice, for example, about toilet training .
The American Academy of Pediatrics recommends that after the first year of life children should see their doctor for preventive health care visits at 12, 15, 18, 24, and 30 months of age and then yearly until age 10. Visits can be made more often based on the advice of the doctor or the needs of the family.
Examination
At each visit, several measurements are taken, screening procedures are done, and vaccinations are given depending on the schedule.
Height and weight are checked, and head circumference is measured until the child is 36 months old. Good growth is one indicator that the child is generally healthy. The child's actual size is not nearly as important as whether the child stays at or near the same percentile on the height and weight charts at each visit. A child who is always in the 10th percentile is likely fine (although smaller than most children of the same age), whereas a child who drops from the 35th percentile to the 10th may have a medical problem.
Beginning at age 3, blood pressure is measured at each visit.
The doctor also monitors how the child has progressed developmentally (see Childhood Development ) since the last visit. For example, the doctor may want to know whether an 18-month-old child has begun speaking or whether a 6-year-old child has begun reading a few words (see table Developmental Milestones From Ages 18 Months to 6 Years ). In the same way, doctors often ask age-appropriate questions about the child's behavior. Does the 18-month-old child have tantrums ? Does the 2-year-old child sleep through the night ? Does the 6-year-old child wet the bed at night ? Parents and doctors can discuss these types of behavioral and developmental issues during the preventive health care visits and together design approaches to address any issues.
Finally, the doctor does a complete physical examination. In addition to examining the child from head to toe, including the heart, lungs, abdomen, genitals, spine, arms, legs, head, neck, eyes, ears, nose, mouth, and teeth, the doctor may ask the child to perform some age-appropriate tasks. To check gross motor skills (such as walking and running), the doctor may ask a 4-year-old child to hop on one foot. To check fine motor skills (manipulating small objects with the hands), the child may be asked to draw a picture or copy some shapes.
Preventive visits should include a check of vision and hearing. Vision screening may begin at 3 years of age, if children are cooperative, but is recommended at 4 and 5 years of age. Parents should let the doctor know before then if they have any concerns about their child's vision. At this age, vision tests include the use of charts and testing machines.
Hearing tests, after the newborn testing, typically begin at 4 years of age, but parents should let the doctor know before then if they have any concerns about their child's hearing.
Some children may need to have their blood checked for anemia or an increased level of lead .
Children who are at risk of having high cholesterol should have a blood test between the ages of 2 years and 10 years. Children at risk include those who have a family history of high cholesterol levels, heart attack, or stroke or have risk factors for heart disease (for example, diabetes, obesity, or high blood pressure). All children should have a cholesterol test at age 9 to 11 years and again at age 17 to 21 years.
Children are screened for tuberculosis (TB) risk factors with a questionnaire at all well-child visits. Risk factors include exposure to TB, being born in or having traveled to areas of the world where TB is common (countries other than the United States, Canada, Australia, and New Zealand and Western and North European countries), having a family member with TB, and having parents or close contacts who are recent immigrants from an area where TB is common or who have recently been in jail. Those with risk factors then usually have tuberculosis screening tests done.
The age of the child and various other factors determine whether other tests are done.
Child safety is discussed during preventive visits. Specific safety concerns are based on the age of the child. For example, the discussion might be focused on bicycle safety for a 6-year-old child. The following examples of injury prevention apply to children aged 12 months to 4 years:
Use an age-appropriate and weight-appropriate car seat. (Infants and toddlers should ride rear-facing until they outgrow the rear-facing weight or height limits of a convertible car seat. Convertible car seats have limits that will allow most children to ride rear-facing up to age 2 years. Once they are 2 years old or, regardless of age, have outgrown their rear-facing car seat, toddlers should sit in a forward-facing car seat with harness straps for as long as possible based on weight and height limits.)
Place car seats in the back seat of the vehicle.
Review automobile safety both as passenger and pedestrian.
Tie up window cords to avoid strangulation.
Use safety caps and latches.
Prevent falls.
Remove handguns from the home.
Closely supervise children while in or near any body of water (for example, bathtubs, pools, spas, wading pools, ponds, irrigation ditches, or any other standing water). Children 1 year of age and older should have swim lessons and should wear a life jacket while swimming and always while boating.

Image courtesy of the Centers for Disease Control and Prevention (CDC), National Center for Injury Prevention and Control ( Transportation Safety Resources ). This guidance from the CDC is for the United States, and regulations may differ in other countries.

In addition to those in the list above, the following examples of injury prevention apply to children age 5 years and older:
Use a forward-facing car seat with a harness for as long as possible (until children outgrow the weight or height limits for the car seat) and then use a belt-positioning booster seat until the vehicle seat belt fits properly (typically when children have reached 4 feet 9 inches in height and are between 8 years and 12 years of age).
Have children under 13 years of age restrained with a seat belt in the back seat of the vehicle.
If the vehicle does not have a back seat, disable the air bag in the front passenger seat.
Have children wear a bicycle helmet and protective sports gear.
Instruct children about safe street crossing.
Closely supervise swimming and sometimes have children wear a life jacket while swimming and always while boating.
The doctor may also emphasize other safety topics, such as the importance of installing and maintaining smoke alarms and of keeping potential toxins (such as cleaners and drugs) and firearms (guns) out of the reach of children. Parents should take the opportunity to bring up topics that are most relevant to their unique family situation. As children get older, they can be active participants in these discussions.
Nutrition and exercise
Parents can help prevent obesity and type 2 diabetes by establishing healthy eating patterns and promoting regular exercise. Parents should provide children with a variety of healthy foods, including fruits and vegetables along with sources of protein. Regular meals and small nutritious snacks encourage healthy eating in even a picky preschooler. Although children may avoid some healthy foods, such as broccoli or beans, for a period of time, it is important to continue to offer healthy foods. In addition, parents should limit the child's intake of fruit juices, which, despite their seemingly healthy origin, are mainly sugar water. Some children lose their appetite for food at mealtime if they drink too much fruit juice. Parents should guide children away from frequent snacking and foods that are high in calories, salt, and sugar.
Exercising and maintaining good physical and emotional health are very beneficial for children. Playing outdoors with the family or participating on an athletic team is a good way to encourage children to exercise and prevent obesity.
Screen time (for example, television, video games, cell phones and other handheld devices, and noneducational computer time) may result in inactivity and obesity. Limits on the time a child spends using devices with screens should start at birth and be maintained throughout adolescence.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
All About Your Child’s Well-Baby Visits

From the first few days of life all the way through to age 21, your child will have regular appointments with her healthcare provider. These are often referred to as well-baby visits or well-child checkups. Initially, they will happen every few months or so, but later on they will happen annually. Learn why well-child checkups are important, what the typical schedule is, and how to get the most out of each visit.
Well-Child Checkup Schedule
Well-child checkups are crucial for keeping your little one healthy and safe as she grows and develops. Below you will find the standard schedule of well-child checkups for the first three years, along with a few examples of what may come up during each checkup. Beginning at age 3, most children will have annual well-child visits. Keep in mind that your child’s healthcare provider may recommend additional visits, and you can always schedule an extra visit between appointments if your little one needs medical care.
The First Week
This visit usually happens within 72 hours of your newborn being home—usually when your baby is about 3 to 5 days old. As part of this checkup your child’s skin color may be checked for signs of jaundice . Your child’s provider may also take a peek inside your newborn’s mouth for signs of tongue-tie . If you are breastfeeding, your little one’s provider can answer any questions you have about latch or sore nipples , for example. The provider may also be able to recommend a lactation consultant for additional help and support.
1 Month Old Checkup
During this visit, your child’s healthcare provider may check things like your baby’s reflexes and muscle tone, as well examining the soft spots on your baby’s head called the fontanelles. If there’s something specific you’d like your child’s provider to check, go ahead and mention it. Your baby’s provider may ask you about how feeding is going. For example, you may be asked how much formula you’re offering, or how often you breastfeed your baby. If you’re planning to return to work soon while continuing to breastfeed, your newborn’s provider may give you advice on pumping and storing breast milk. You might also like to use this opportunity to ask how to go about finding good childcare. Use this appointment to ask any questions you have about adjusting to life as a parent. For example, if you suspect you may have postpartum depression or are not recovering as you had hoped after childbirth , bring this up as well. If you’re the dad, you might like to ask about what you can do to bond with your baby.
2 Months Old Checkup
At this visit your baby may receive some vaccines, including the DTaP, Hib, and IPV vaccines. Vaccinations will be given at a number of different well-child checkups, so it’s worth taking a look at the immunization schedule or asking your child’s provider for guidance on which vaccines to expect when. Your baby’s heart and lung health may be checked. Your child’s provider will use a stethoscope to listen to your baby’s heartbeats for signs of irregularity, and to listen to your baby’s lungs for signs of breathing difficulties. If your baby has diaper rash , your child’s healthcare provider can recommend ointments or barrier creams for treatment and prevention. Your child’s provider can also let you know about other common baby rashes to keep an eye out for.

4 Months Old Checkup
At this visit, your baby’s provider may examine your child's eyes and track her eye movements. Your child’s provider may also move your baby’s legs to check that the joints are developing well, and press gently on your baby’s tummy to check whether the organs are forming well. At this point your doctor will ask you about your baby’s sleep, including nap times. To help you keep track of this, and to help make sure your baby’s sleeping well, we suggest downloading the Smart Sleep Coach by Pampers™. Co-developed with pediatricians and backed by science, this easy-to-use app is like having a personal sleep coach, in your pocket! Get started today by taking their free sleep assessment .
6 Months Old Checkup
This month, your child’s healthcare provider may offer pointers on introducing solids and tell you about signs of an allergic reaction to watch for as you introduce new foods one at a time. Your child’s provider can also give you personalized advice on which foods to start with, how to set up healthy eating habits, and how to actually feed your baby solids.
9 Months Old Checkup
As your baby’s teeth start erupting , your child’s healthcare provider may check on their growth and recommend a good pediatric dentist in your area. Your baby’s provider can also show you how to care for those first tiny teeth. Other topics that may come up at this checkup include how to wean your baby off the bottle when the time comes, when to start giving cow’s milk, and when to introduce utensils and a sippy cup.
1 Year Old Checkup
During this visit your child’s healthcare provider may ask about certain fine and gross motor skills , such whether your child can pull up to a standing position, or walk on his own or with his hand held, or use his finger to point at objects he wants. You might like to ask your child’s healthcare provider about when your little one might start walking , if he isn’t already; what baby proofing measures you should take at home now that your child is getting more mobile; and where to go to get shoes fitted for your child.
15 Months Old Checkup
Your child’s healthcare provider may ask about how your toddler’s interpersonal, language, and cognitive skills are coming along. For example, she might ask whether your child is starting to explore more independently, whether he points to common objects when you say their names, and whether he can follow simple instructions like “give the spoon to Daddy.” If you are planning to have another baby soon, you might like to ask the healthcare provider about how to introduce your toddler to the concept of him getting a little brother or sister.
18 Months Old Checkup
As your child gets more active and independent you may like to ask your child’s provider about strategies for keeping your child safe in your home environment. This is also a good time to discuss ways to manage your child's behavior and set up age-appropriate rules and boundaries. If your toddler has certain risk factors, the relevant screening tests may be offered at this checkup. For example, screening tests may be recommended for things like hearing, vision, development delays, or autism. Your provider may also bring up the topic of potty training, and go over some of the signs of readiness for potty training .
2 Years Old Checkup
Before this visit you may have been wondering about the upcoming “terrible twos” and how you should handle temper tantrums and the inevitable meltdowns at the grocery store. This visit is a great chance to bring up your questions and concerns around how your child’s behavior and personality may be evolving. Your child’s provider will explain what is normal during this stage of development and how to support your child’s growing independence. Preschool could be coming up in the next year or two, and your provider can help you find a preschool that's a good fit for your child.
2 ½ Years Old Checkup
Besides the usual checks, one topic that may come up during this visit is potty training. If potty training has begun and isn't going well, or if you're unsure how to get the process started , your provider can offer suggestions. This checkup may also be a great time to talk to your child’s provider about your little one’s temperament and personality. For example, if you have any concerns about how your toddler is interacting with other children, or if your child seems particularly shy, you might like to bring it up to see what advice or reassurance your toddler’s provider can give you.
3 Years Old Checkup
During this session your toddler’s healthcare provider may ask you about anything that’s disturbing your child’s sleep, like nightmares, for example, and how to handle other sleep issues. Screen time may also come up. You may talk about how much screen time a 3-year-old should be getting, and what type of programming is good for a child of this age.
Baby Growth Chart Calculator
Keep an eye on your baby’s average growth by tracking height, weight, and head circumference with our simple tool.
This is a mandatory field.
*Input details of your baby’s last measurements. **Source: World Health Organization
What Happens at a Well-Child Visit?
Each visit may be a little different based on your child’s age and stage of development, any specific needs your child has, and the way your child’s healthcare provider does things. However, here are some of the things that typically happen at a well-child visit in the early years:
Tracking your child’s growth by measuring her length, weight, and head circumference
A physical exam that could include checking your baby’s ears, eyes, mouth, skin, limbs, tummy, and other body parts
An assessment of your child's physical development, including her movement and motor skills
An evaluation of her emotional and cognitive development; for example, checking that your child is reacting and interacting normally for her age, and is learning appropriately for her age
Immunizations may be given
Screening tests or other tests may be recommended if needed
Your child’s provider may give you advice on feeding and nutrition or recommend extra vitamins or supplements, like vitamin D or iron, if they are needed
Your provider may share insights into the next phase of your child’s development. If your child is not developing as expected, the provider will also be able to offer recommendations on treatment or therapies to help your child get back on track.
Your child’s healthcare provider will answer any questions you have about parenting or about your child’s health and well-being. No question is too big or too small. You can ask anything from how much your child should be sleeping during the day to when to switch your car seat from rear facing to front facing.
Your child’s healthcare provider can give your information about resources in your area, and about how to go about certain things like choosing a good babysitter, finding an affordable pediatric dentist, or selecting the right preschool.
Benefits of the Well-Child Visit
Well-child checkups are invaluable for both you and your child. Here are just some of the benefits of the well-child checks:
Spotting issues early. Your child’s healthcare provider will use these visits to keep an eye out for any possible problems so that steps can be taken to get your child back on the right track. As an example, if your little one is gaining too much weight, your provider can give you advice on nutrition so that your child gets back to a healthy weight.
Preventing problems. As an example, ensuring your child is immunized against certain childhood diseases helps prevent your child from getting sick with a preventable disease.
Getting answers. You might have some questions that aren’t pressing enough to warrant a separate doctor’s visit. Knowing that you have a well-child visit coming up gives you a chance to collect all of your questions and have them answered by a medical professional you trust. Remember, there are no “silly questions” when it comes to your child’s health and well-being.
Learning about what’s to come. Your child’s healthcare provider can give you insights and information about the next stage of your child’s development. That means that certain things might be less of surprise when they happen. As an example, your child’s provider might tell you what kind of behavioral changes to expect with the “terrible twos” and how to manage the tantrums that follow.
Creating a strong relationship with your child’s healthcare provider. Seeing your child’s provider regularly gives you the chance to build up a rapport. You’ll get to know her during these well-child visits, and she’ll get to know you and your little one. Having a relationship built on trust ensures that you can work as a team for the best outcomes for your child.
How to Make the Most of the Well-Child Visit
There are a few things you can do to ensure you get the most out of your child’s well-child checkups:
If it’s workable, schedule the visit for a time when you think your child will be well-rested and well-fed, and try to pick a time when you yourself aren’t rushed. Also, consider how busy your child’s healthcare provider will be. It may be easiest if you can get the first appointment of the day, or one that’s not during “rush hour.”
If it’s possible, both parents should be at the first few visits to ensure that you both get to know your child’s healthcare provider and get the same basic information about newborn baby care
Pack everything you’ll need like your insurance information, your child’s medical history, and your diaper bag (filled with extra diapers, snacks, and toys)
Consider keeping a physical or digital record of what was discussed at each well-child visit. Keep copies of your child’s lab results and evidence of immunizations in the same spot or format as well. Having all this information in one place from the start will make it easier to look back and find the information when you need it. When your child enters preschool or school, you may need to provide documentation of certain medical details.
Dress your child in clothes that are easy to remove and put back on. Your little one may be undressed for part of the visit and your child’s healthcare provider may need easy access to give immunizations.
Write down any questions you have and take the list with you so you don’t forget anything important. Having a list of questions also allows you to focus on the answers instead of thinking ahead about what to ask next.
Using the Smart Sleep Coach by Pampers™ to track your baby’s night sleeps and naps can be a huge help when discussing your baby’s health and development with your doctor. By taking a broad view of your baby’s sleep, you can understand and shape your baby’s sleep and give them the rest they need to keep growing and developing well. In fact, if you're experiencing sleep challenges, you can take this free sleep assessment to get helpful guidance and support on how to get sleep back on track!
The bottom line
Well-child checkups are important for your child. They allow the healthcare provider to to track your child’s growth and development, give vaccinations or screening tests that are needed, and identify any problems nice and early. By working together, you and your child’s provider can give your child the best possible start in life.
Plus, each well-child visit is a great opportunity for you to ask any questions you have about your child’s health and parenting in general.
Try not to miss your scheduled well-baby checkups; they can be a wealth of information and an important way to help ensure your child’s happy and healthy development. By taking advantage of these one-on-one sessions with your child’s provider, you may find he becomes less of a “provider” and more of a partner in your parenting journey.
How We Wrote This Article The information in this article is based on the expert advice found in trusted medical and government sources, such as the American Academy of Pediatrics and the American College of Obstetricians and Gynecologists. You can find a full list of sources used for this article below. The content on this page should not replace professional medical advice. Always consult medical professionals for full diagnosis and treatment.
- healthychildren.org. “AAP Schedule of Well-Child Care Visits.”
- Kids Health. “Your Child's Checkup: 3 Years.”
- CDC. “Developmental Monitoring and Screening.”
- Kids Health. “Your Child's Checkup: 1.5 Years (18 Months).”
- Kids Health. “Your Child's Checkups.”
Review this article:
Read more about baby.
- Explore Baby Sleep
- Parenting Life
- Development
Join a World of Support
through Pregnancy and Parenthood.

TRACK WITH TOOLS

LEARN WITH EXPERTS

GET REWARDED

Where You Already Belong
Health Library 15 Month Well-Child Visit
Find another condition or treatment, healthy child development and behavior.
Below are milestones most children will reach between now and 18 months of age. Talk with your doctor at your child’s next well-visit if your child is not yet reaching these milestones or there are skills your child no longer shows each day.
Social and Emotional Milestones
- Moves away from you, but looks to make sure you are close by
- Points to show you something interesting
- Puts their hands out for you to wash them
- Looks at a few pages in a book with you
- Helps you dress them by pushing their arm through the sleeve or lifting up their foot
Language and Communication Milestones
- Tries to say three or more words (besides “mama” or “dada”)
- Follows one-step directions without any gestures, like giving you the toy when you say, “give it to me”
Thinking and Learning Milestones
- Copies you doing chores, like sweeping with a broom
- Plays with toys in a simple way, like pushing a toy car
Physical Development Milestones
- Walks without holding on to anyone or anything
- Scribbles with a crayon
- Drinks from a cup without a lid (may spill sometimes)
- Feeds themselves with their fingers
- Tries to use a spoon
- Climbs on and off a couch or chair without help
Healthy Ways to Help Your Child Learn and Grow
Development.
- Teach your child to talk by using simple words and phrases. Repeat and add to what your child says. Describe feelings and emotions. Read books together and use simple words to talk about the pictures.
- Encourage empathy for others by teaching your child to comfort someone who is sad with a hug or pat on the back.
- Play with puzzles and blocks to encourage problem-solving. Practice throwing, rolling and kicking a ball. Use pretend play toys that require imagination, like dolls or play telephones.
- Nurture independence by letting your child dress and feed themselves.
- Teach your child “wanted behaviors.” Give your child attention and praise when behaving well.
- Tantrums are common at this age. Below are tips to help you manage tantrums:
- Use distraction to stop tantrums when you can.
- Set limits to teach and protect your child, not to punish them. Always tell or show your child what they should do instead.
- Limit the need to say “no” by making your home and yard safe for play.
- Let your child choose between two good options when possible.
- It is normal for your child to be anxious or shy around new people. Be sure to comfort your child.
- Give water and 16–24 ounces of whole milk each day. Avoid sugary drinks like juice.
- Cut food into small pieces to help prevent choking.
- Offer your child three meals and two–three healthy snacks each day. Encourage drinking from a cup and using a spoon or fork. Wean your child from the bottle.
- Toddlers need less food because they don’t grow as fast as babies. Don’t worry if your child is picky or eats inconsistently. Let your child choose between healthy options.
- Your child may sleep up to 12–14 hours in a 24-hour period, including one–two naps during the day.
- Have a consistent routine for bed (bathing, brushing teeth, books, bedtime). The hour before bedtime should be calm. Avoid giving your child a bottle or cup in bed.
- If your child wakes during the night, avoid giving enjoyable attention. Use words to reassure them and give a blanket or toy to hold for comfort.
Digital Media Use
- Limit screen time. Smart phones, tablets and TVs are not recommended for children younger than 2 years of age. Children learn best by talking and playing with others.
Water Safety
- Drowning is silent and can happen quickly. Do NOT leave your child alone near any water (including buckets, bathtubs, toilets, pools, ponds, whirlpools). Install a four-foot-tall fence with a self-closing and self-latching gate around home pools. Learn more about water safety .
Vehicle Safety
- Your child’s car seat should stay rear facing in the backseat until they reach the highest weight or height allowed by the car safety seat manufacturer. Learn more about car seat safety and installation.
Home Safety
- Lock up medicines and cleaning supplies. Save the Poison Help Line number (1-800-222-1222) in all phones.
- Keep small electronics that use button batteries out of reach (for example, remote controls, key fobs, calculators, musical greeting cards, flashing holiday jewelry). Learn more about swallowing hazards.
- Store any guns unloaded and locked in a safe. Keep the ammunition locked separately.
This information is to support your visit with your child’s doctor. It should not take the place of the advice of your pediatrician.
Sources: Centers for Disease Control and Prevention, Bright Futures (4th Edition) by the American Academy of Pediatrics
Last Updated 06/2023
Cincinnati Children’s has primary care services at locations throughout Greater Cincinnati.
Translations
- Japanese Translation
- Spanish Translation

Connect With Us
3333 Burnet Avenue, Cincinnati, Ohio 45229-3026
© 1999-2024 Cincinnati Children's Hospital Medical Center. All rights reserved.

Sima Stein, MD
Pediatrician located in bay area, san jose, ca.
"The best pediatrician in the Bay Area!"
Olga P. Google
"Amazing and very knowledgeable. My whole family appreciates all of Dr. Stein's help."
Levon B. Google
"Dr. Stein is the nicest and most professional pediatrician I ever met."
Simona S. Google
"Thank you for the 8 years of service. I'm lucky to have found Dr. Stein."
Jeanine G. Google
"The best doctor I've ever had for my kids. Thank you Dr. Stein for your hard work!"
Vagif Z. Google
"We love Dr. Stein and her staff. It's refreshing to have such dedicated individuals."
Lawrence C. Google
"Dr. Stein has been my children's pediatrician for many years, and will continue to be."
Adele Z. Yelp
Give our office a call to schedule your office visit for travel vaccinations and consultation!
Sima Stein, MD, is a well-known and much-respected pediatrician who leads the team at Stein Pediatrics in San Jose, California. She provides high-quality, personalized medical care to infants, children, teenagers, and young adults.
Dr. Stein welcomes patients up to 21 years of age and offers a full range of skilled medical services in an inviting, patient-focused environment. One of her goals throughout her career has been creating long-term relationships with her young charges and their parents.
Her expertise includes evaluation and management of newborns, sick-child visits, as well as monitoring childhood development, which includes gross and fine motor skills, cognition, and speech. She’s a longtime advocate of helping prevent childhood illnesses through parental instruction, healthy nutrition, and preventive medicine.
Her outreach to the teens and young adults in her community includes education, screening, and treatment regarding sports injuries, acne, birth control counseling, STDs, and healthy lifestyle choices such as routine exercise.
Even her offices are designed with her patients and their parents in mind. Her waiting rooms include a separate area that helps limit contact between patients scheduled for well-child exams and routine monitoring and those who are feeling ill.
There’s a private room available for nursing mothers, should they wish to use it, and a pharmacy nearby for convenience. Patients and parents alike will appreciate the toys, books, and popular high-resolution videos available to help relieve boredom.
Stein Pediatrics is equipped to provide services in English, Chinese, Hindu, Russian, Spanish, Ukrainian, and Vietnamese. Dr. Stein is also certified to conduct immigration medical exams.
Dr. Stein is a board-certified pediatrician who received her medical degree from Second Moscow State Medical Institute. She completed residency programs in pediatrics at New York Methodist Hospital and Stanford University Medical Center.
Abbott has initiated a proactive, voluntary product recall of certain powder formulas (Similac, Alimentum, and EleCare) manufactured in Sturgis, Michigan, one of the company’s manufacturingfacilities.
The products under recall have a multidigit number on the bottom of the container starting with the first two digits 22 through 37, contains K8, SH, or Z2 and with an expiration date of April 1, 2022, or after.
If your baby has been consuming either of these formulas, and you are experiencing any symptoms such as, but not limited to,
- Baby off regular pattern
Please call or email us at your earliest convenience for a further discussion. The care and safety of our patients are our top priority, we are here to help!
(To find out if a product is included in this recall, visit similacrecall.com and type in the code on the bottom of the package, or call +1-800-986-8540 (U.S.) and follow the instructions provided. No action is needed for previously consumed products.)
School and sports physicals are available same day!
Call now: 408-292-0100.

Nasal Flu Vaccine (Flumist) is Now Available! Call the practice to schedule an appointment
Influenza A&B Screening Test Available

Drug Screen and Urine Analysis Available

At Stein Pediatrics, we accept most major insurance plans. Here is a short-list of some of the most popular plans we accept. Please contact our office if you do not see your insurance provider listed.

Network Insurances
- Blue Cross Blue Shield
- Blue Shield
- Harvard Pilgrim Health Care
- Nippon Life Benefits
- Oxford Health
- Santa Clara County IPA
- United Healthcare

Traveling Overseas This Summer? Now's the Time to Consider Travel Vaccines
Planning an international family adventure this summer? Learn what you need to do to keep you and your children healthy overseas.

Our Top Tips to Help Your Child Nip Springtime Allergies in the Bud
Are you and your child dreading the spring weather because of allergies? Dr. Stein shares her top tips for enjoying the season without troublesome allergy symptoms.

What to Expect from Your Child’s First Developmental Screening
Should your baby be walking? Talking? Your child’s first developmental screening can answer all your questions about your child’s development and more.
Words from our patients

"I would definitely recommend Dr. Sima Stein for anyone needing to collect their USCIS-related medical evidence and in a timely manner."
"Dr. Stein is highly knowledgeable and quick to identify a problem, which is why she has multiple recognitions for being an outstanding educator and Doctor."
"Dr. Stein has been my kids doctor since day one. She always has a way to make things easy for me and helping my kids feel better."
"Thank you Dr. Sima Stein, from our Family and friends that continue to go to your Office. You are greatly appreciated!"
"One of the best doctors in the area. A Good communication with kids and parents and deep medical knowledge and experience. Thank you doctor Stein!"
"I always recommend Doctor Stein to my friends and family and will continue to do so with all my pleasure."

"There is no better pediatrician than Dr. Stein. We love her and her staff and appreciate all that they do for us."
Office Hours
Monday 8:30 am - 4:00 pm 8:30 am to 4:00 pm Tuesday 8:30 am - 4:00 pm 8:30 am to 4:00 pm Wednesday 8:30 am - 4:00 pm 8:30 am to 4:00 pm Thursday 8:30 am - 4:00 pm 8:30 am to 4:00 pm Friday 8:30 am - 4:00 pm 8:30 am to 4:00 pm Saturday Closed Closed Sunday Closed Closed
Get in touch
408-214-1337 Book Online
Email Opt-out
Appointment confirmed.
Doctor Visits
Make the Most of Your Teen’s Visit to the Doctor (Ages 15 to 17 Years)

Take Action
Teens ages 15 to 17 years need to go to the doctor or nurse for a “well-child visit” once a year.
A well-child visit is when you take your teen to the doctor to make sure they’re healthy and developing normally. This is different from other visits for sickness or injury.
At a well-child visit, the doctor or nurse can help catch any problems early, when they may be easier to treat.
Learn what to expect so you can make the most of each visit.
Child Development
How do i know if my teen is growing and developing on schedule.
Your teen’s doctor or nurse can help you identify “developmental milestones,” or signs to look for that show your teen is developing normally. This is an important part of the well-child visit.
Some developmental milestones are related to your teen’s behavior and learning, and others are about physical changes in your teen’s body.
See a complete list of developmental milestones for your teen .
Behavior Changes
What are some changes i might see in my teen’s behavior.
Developmental milestones for teens ages 15 to 17 years include:
- Spending less time with family and more time with friends
- Worrying more about the future (like going to college or finding a job)
- Thinking more about romantic relationships and sex
- Trying new things like new sports or hobbies — or possibly experimenting with tobacco, alcohol, or drugs
This is also a time when some teens may start showing signs of depression, anxiety, or eating disorders. That’s why it’s important to:
- Make sure the doctor screens your teen for depression
- Have your teen screened for anxiety
Physical Changes
What are some physical changes my teen is going through.
Teens ages 15 to 17 years may be nearing the end of puberty. Puberty is when a child’s body develops into an adult’s body.
- Get more information about puberty to share with your daughter
- Get more information about puberty to share with your son
Teens might not ask you questions about sex, their bodies, or relationships. That’s why it’s a good idea for you to start the conversation. You can also encourage your teen to ask the doctor or nurse any questions they have about body changes or other health concerns.
Learn how to talk with your teen about sex .
Take these steps to help you and your teen get the most out of well-child visits.
Gather important information.
Take any medical records you have to the appointment, including a record of vaccines (shots) your teen has received.
Make a list of any important changes in your teen’s life since the last visit, like a:
- New brother or sister
- Separation or divorce — or a parent spending time in jail or prison
- New school or a move to a new neighborhood
- Serious illness or death of a friend or family member
Use this tool to keep track of your teen’s family health history .
Help your teen get more involved in visits to the doctor.
The doctor will probably ask you to leave the room during part of the visit, usually the physical exam. This lets your teen develop a relationship with the doctor or nurse and ask questions in private. It’s an important step in teaching your teen to take control of their health care.
Your teen can also:
- Call to schedule appointments
- Help you fill out medical forms
- Write down questions for the doctor or nurse
For more ideas, check out these tips to help teens take charge of their health care . You can also share this list of questions for the doctor with your teen .
What about cost?
Under the Affordable Care Act, insurance plans must cover well-child visits. Depending on your insurance plan, you may be able to get well-child visits at no cost to you. Check with your insurance company to find out more.
Your teen may also qualify for free or low-cost health insurance through Medicaid or the Children’s Health Insurance Program (CHIP). Learn about coverage options for your family.
If you don’t have insurance, you may still be able to get free or low-cost well-child visits. Find a health center near you and ask about well-child visits.
To learn more, check out these resources:
- Free preventive care for children covered by the Affordable Care Act
- How the Affordable Care Act protects you and your family
- Understanding your health insurance and how to use it [PDF - 698 KB]
Ask Questions
Make a list of questions you want to ask the doctor..
Before the well-child visit, write down 3 to 5 questions you have. This visit is a great time to ask the doctor or nurse any questions about:
- A health condition your teen has (like acne or asthma)
- Changes in your teen’s behavior or mood
- Loss of interest in favorite activities
- Tobacco, alcohol, or drug use
- Problems at school (like learning challenges or not wanting to go to school)
Here are some questions you may want to ask:
- Is my teen up to date on vaccines?
- How can I make sure my teen is getting enough physical activity?
- How can I help my family eat healthy?
- How can I help my teen succeed at school?
- How can our family set rules more effectively?
- How can I help my teen become a safe driver?
- How can I talk with my teen about tobacco, alcohol, and drugs?
Take a notepad, smartphone, or tablet and write down the answers so you can remember them later.
Ask what to do if your teen gets sick.
Make sure you know how to get in touch with a doctor or nurse when the office is closed. Ask how to get hold of the doctor on call, or if there's a nurse information service you can call at night or on the weekend.
What to Expect
Know what to expect..
During each well-child visit, the doctor or nurse will ask you questions, do a physical exam, and update your teen’s medical history. You and your teen will also be able to ask your questions and discuss any problems.
The doctor or nurse will ask your teen questions.
The doctor or nurse may ask about:
- Behavior — Do you have trouble following directions at home or at school?
- Health — Do you often get headaches or have other kinds of pain?
- Safety — Do you always wear a seatbelt in the car? Do you and your friends use tobacco, alcohol, or drugs?
- School and activities — Do you look forward to going to school? What do you like to do after school?
- Family and friends — Have there been any changes in your family recently? Do you have close friends?
- Emotions — Do you often feel sad or bored? Do you often feel scared or very worried? Is there someone you trust who you can talk to about problems?
- Sexuality — Do you have any questions about your body? Have you talked with your parents about dating and sex? Are you dating anyone now?
- The future — Have you started to think about what you want to do after high school?
The answers to questions like these will help the doctor or nurse make sure your teen is healthy, safe, and developing normally.
Physical Exam
The doctor or nurse will also check your teen’s body..
To check your teen’s body, the doctor or nurse will:
- Measure height and weight and figure out your teen's body mass index (BMI)
- Check your teen’s blood pressure
- Check your teen's vision and hearing
- Check your teen’s body parts (called a physical exam)
- Decide if your teen needs any lab tests, like a blood test
- Give your teen vaccines they need
Behavior and Emotions
The doctor or nurse will pay special attention to signs of certain issues. .
The doctor or nurse will offer additional help if your teen may:
- Be depressed
- Have anxiety
- Struggle with an eating disorder
- Use tobacco, alcohol, or other drugs
- Experience any kind of violence
And if your teen may be having sex, the doctor or nurse will talk about preventing STIs (sexually transmitted infections) — also called STDs (sexually transmitted diseases) — and pregnancy. Learn how to talk with your teen about preventing STIs .
The doctor or nurse will make sure you and your teen have the resources you need.
This may include telling you and your teen about:
- Websites or apps that have helpful health information
- Organizations in your community where you can go for help
If needed, the doctor or nurse may also refer your teen to a specialist.
Content last updated February 16, 2024
Reviewer Information
This information on well-child visits was adapted from materials from the Centers for Disease Control and Prevention and the National Institutes of Health.
Reviewed by: Sara B. Kinsman, M.D., Ph.D. Director, Division of Child, Adolescent and Family Health Maternal and Child Health Bureau Health Resources and Services Administration
You may also be interested in:

Talk to Your Kids About Tobacco, Alcohol, and Drugs

Talk to Your Kids About Sex and Healthy Relationships

Get Your Teen Screened for Depression
The office of disease prevention and health promotion (odphp) cannot attest to the accuracy of a non-federal website..
Linking to a non-federal website does not constitute an endorsement by ODPHP or any of its employees of the sponsors or the information and products presented on the website.
You will be subject to the destination website's privacy policy when you follow the link.
Lawyer fatally shoots former daughter-in-law, fellow attorney at Las Vegas law firm
A lawyer fatally shot his former daughter-in-law, as well as a fellow attorney, during a deposition at a Las Vegas law firm Monday morning, two sources familiar with the investigation said.
The shooter opened fire at the Prince Law Group office in Summerlin during a deposition of his son, whom he had been representing, the sources said Monday afternoon.
The other lawyer was representing his own wife, who was the former daughter-in-law of the shooter and opposing counsel, the sources said.
The alleged gunman died after he turned the gun on himself, according to the sources. His son survived.
The sources characterized the shooting as targeted and domestic-related.
The incident occurred about 10 a.m. at the fifth-floor law office on West Charleston Boulevard near Pavilion Center Drive, Clark County Sheriff Kevin McMahill said at a news conference. Responding officers found the three people with gunshot wounds, police said Tuesday. They were pronounced dead at the scene by medical personnel.
"The suspect was not killed by my police. We believe he took his own life," he said, adding that there was no further threat to the public.
The Clark County coroner's office on Tuesday identified the deceased people as Ashley Prince, 30; Dennis Prince, 57 and Joseph Houston, 77.
Ashley Prince and Dennis Prince died from multiple gunshot wounds, the coroner said, ruling each death was a homicide. Houston died by suicide, according to the coroner.
Robert Eglet told NBC News that the attorney who was slain was his former law partner and that they had known each other for 30 years. The pair “were close friends for a very, very long time," Eglet said.
“He was a very good guy. He was one of the finest trial lawyers in the state of Nevada. It’s tragic, and it’s senseless," he said.
Eglet said his friend specialized in medical malpractice cases.
There are businesses adjacent to the law office where the shooting occurred, McMahill said. First responders evacuated the building and followed an active-shooter protocol, officials said. Hundreds of people were evacuated, police said.
The suspect's vehicle was being investigated, McMahill said, adding that police were trying to shore up a motive.
"We have a theory at this point, but I cannot release any of that information until we've confirmed that information," he said.
A law office on the fifth floor did not answer a call seeking comment Monday afternoon. Police said they were using nearby Red Rock Casino as an assistance center.
If you or someone you know is in crisis, call or text 988 to reach the Suicide and Crisis Lifeline or chat live at 988lifeline.org . You can also visit SpeakingOfSuicide.com/resources for additional support.
Andrew Blankstein is an investigative reporter for NBC News. He covers the Western U.S., specializing in crime, courts and homeland security.
Antonio Planas is a breaking news reporter for NBC News Digital.

IMAGES
VIDEO
COMMENTS
The Bright Futures/American Academy of Pediatrics (AAP) developed a set of comprehensive health guidelines for well-child care, known as the "periodicity schedule." It is a schedule of screenings and assessments recommended at each well-child visit from infancy through adolescence. Schedule of well-child visits. The first week visit (3 to 5 ...
Well-child visits and recommended vaccinations are essential and help make sure children stay healthy. Children who are not protected by vaccines are more likely to get diseases like measles and whooping cough. These diseases are extremely contagious and can be very serious, especially for babies and young children.
A typical schedule includes well-child checks at ages: 3 to 5 days; 2-4 weeks; 2 months; 4 months; 6 months; 9 months; 12 months; ... Well-child visits are important for keeping good health and ...
A comprehensive head-to-toe examination should be completed at each well-child visit. Interval growth should be reviewed by using appropriate age, sex, and gestational age growth charts for height ...
flu. 4 years old. DTaP. IPV. MMR. varicella. flu. After age 4, a well-child visit should take place every year and should include a physical exam and a growth, developmental, behavioral, and ...
Beginning at the 7 year visit, there is both a Parent and Patient education handout (in English and Spanish). For the Bright Futures Parent Handouts for well-child visits up to 2 years of age, translations of 12 additional languages (PDF format) are made possible thanks to the generous support of members, staff, and businesses who donate to the ...
Young children need to go to the doctor or nurse for a "well-child visit" 7 times between ages 1 and 4. A well-child visit is when you take your child to the doctor to make sure they're healthy and developing normally. This is different from other visits for sickness or injury. At a well-child visit, the doctor or nurse can help catch any ...
Overview. Kids ages 11 to 14 years need to go to the doctor or nurse for a "well-child visit" once a year. A well-child visit is when you take your child to the doctor to make sure they're healthy and developing normally. This is different from other visits for sickness or injury. At a well-child visit, the doctor or nurse can help catch ...
When should well-care visits be scheduled? Your child's healthcare provider will give you a schedule of ages when a well-care visit is suggested. The American Academy of Pediatrics recommends well-care visits at the following ages: Before a newborn is discharged from the hospital, or at 48 to 72 hours of age. 3 to 5 days. 2 to 4 weeks. 2 months.
Child safety is discussed during preventive visits. Specific safety concerns are based on the age of the child. For example, the discussion might be focused on bicycle safety for a 6-year-old child. The following examples of injury prevention apply to children aged 12 months to 4 years: Use an age-appropriate and weight-appropriate car seat.
Your child's doctor will recommend a schedule for well-child visits. One example is for visits at ages: footnote 1. 3 to 5 days old. By 1 month. 2 months. 4 months. 6 months. 9 months. 1 year. 15 months. 18 months. 2 years. 30 months. 3 years. After age 3, well-child visits are usually scheduled yearly through the teen years.
Children ages 5 to 10 years need to go to the doctor or nurse for a "well-child visit" once a year. A well-child visit is when you take your child to the doctor to make sure they're healthy and developing normally. This is different from other visits for sickness or injury. At a well-child visit, the doctor or nurse can help catch any ...
Parents should take their babies for well-child visits at these ages: 2 to 4 days: 9 months: 1 month: 12 months. 2 months: 15 months: 4 months: 18 months: 6 months 24 months (2 years) After your child is 2 years old, schedule a well-child visit once a year. Children are sometimes scared of going to the doctor. But you can prepare your child for ...
Regular well-child visits can keep your kid and family healthy and prevent serious illness. It's normal to have questions as they quickly grow from birth to adulthood. Make sure you have plenty of time before and after their checkup to avoid any stress. Write down questions or concerns as soon as they come to mind before your kid's well ...
The Well-Child Visit: Why Go and What to Expect Depending on your child's age, you may have well-child visits every few weeks, months, or yearly (see the AAP Schedule of Well-Child Care Visits link below). To help you create a plan for when you get home, write a "to do" list during the visit. List tasks that you can easily fit into your
7-10 years: Annual well-child check. Vision/hearing and TB screenings; any immunizations previously missed. 11-12 years: Annual well-child check. Depression and TB screenings; DTaP, HPV and ...
Well-Child Checkup Schedule. Well-child checkups are crucial for keeping your little one healthy and safe as she grows and develops. Below you will find the standard schedule of well-child checkups for the first three years, along with a few examples of what may come up during each checkup. Beginning at age 3, most children will have annual ...
Give water and 16-24 ounces of whole milk each day. Avoid sugary drinks like juice. Cut food into small pieces to help prevent choking. Offer your child three meals and two-three healthy snacks each day. Encourage drinking from a cup and using a spoon or fork.
California Children's Services. CCS is a State program for children with certain diseases or health problems. Through this program, children up to 21 years old can get the health care and services they need. CCS will connect you with doctors and trained health care people who know how to care for your child with special health care needs.
Office Hours. Now providing Telehealth visits - Book a virtual appointment today! Trusted Pediatrician serving Bay Area San Jose, CA. Contact us at 408-214-1337 or visit us at 105 N Bascom Ave, Suite 102, San Jose, CA 95128.
Overview. Teens ages 15 to 17 years need to go to the doctor or nurse for a "well-child visit" once a year. A well-child visit is when you take your teen to the doctor to make sure they're healthy and developing normally. This is different from other visits for sickness or injury. At a well-child visit, the doctor or nurse can help catch ...
CDC Childhood Milestones Tracker: Track your child's milestones from age 2 months to 5 years with CDC's easy-to-use illustrated checklists; get tips from CDC for encouraging your child's development; and find out what to do if you are ever concerned about how your child is developing.; John Hopkins Developmental Milestones: provides parents and caregivers examples of how to support their ...
child's health care provider as soon as possible to obtain a record or make appointment for your child to receive these immunizations. Required within 30 days of your child's 1st day of school or Home Base Home Visit: Health Assessment (Physical Exam or Well-Baby Check): We need a copy of your child's
April 8, 2024, 12:36 PM PDT / Updated April 10, 2024, 12:04 PM PDT. By Andrew Blankstein and Antonio Planas. A lawyer fatally shot his former daughter-in-law, as well as a fellow attorney, during ...