
- Health & Wellness

What to Expect at Your Postpartum Checkups

During pregnancy, you likely got used to seeing your OB or midwife fairly often, especially as you neared your due date. Consistent visits are a standard part of prenatal care to ensure everything is progressing smoothly and that you and baby are healthy. So what happens now that baby is born? In the past, prenatal care has been far more thorough than postpartum care, but in recent years experts have called for a change. Giving birth is no small feat—it takes both a physical and emotional toll, and new moms need medical care and support, starting with their first postpartum checkup. Here, we talked to two experts to lay out everything you need to know about postpartum checkups, from when to expect them to how to prepare.
What Is a Postpartum Checkup?
Postpartum checkups are the visits to your OB or midwife that you’ll have after giving birth—and they’re just as important as your prenatal visits, as the first few weeks after delivery are a time of major transition for both you and baby.
During these checkups, your doctor will want to make sure you’re adapting well emotionally and recovering well physically. “Issues with blood pressure, infections, breastfeeding issues and hormonal imbalances can all happen postpartum,” says Rebekah Mustaleski , a certified professional midwife and compression director with Motif Medical . “It’s often hard to recognize the subtle differences that signal some of these issues because a new parent is consumed with caring for their newborn. It’s essential to be seen by your doctor or midwife so that they can do an assessment and make sure that your postpartum recovery is going smoothly.”
When Do Postpartum Checkups Happen?
It used to be that you’d have one postpartum checkup, typically six weeks after giving birth or sooner if you delivered via c-section. However, in recent years, experts have called for postpartum checkups to happen sooner and more frequently. The American College of Obstetricians and Gynecologists (ACOG) now recommends that postpartum care start no later than within the first three weeks after birth and should be followed by ongoing care as needed. “To optimize the health of women and infants, postpartum care should become an ongoing process, rather than a single encounter, with services and support tailored to each woman’s individual needs,” the guidance reads. Plus, the ACOG states women should receive a comprehensive postpartum checkup that includes “a full assessment of physical, social and psychological well-being” no later than 12 weeks postpartum.
According to Mustaleski, most providers schedule postpartum checkups the day after birth (where they’ll come see you bedside as you recover), two to three weeks postpartum and then again at six to eight weeks postpartum.
What Happens During Postpartum Checkups?
The postpartum checkups are a time to discuss how you’re healing and adapting to motherhood. During the visit, your doctor will check on several aspects of your physical and emotional recovery. According to the ACOG, it will also cover infant care and feeding, family planning, sleep and fatigue, chronic disease management and health maintenance.
“I usually talk to my patients about how the pregnancy and delivery went," says Laura Riley , MD, department chair of obstetrics and gynecology at Weill Cornell Medicine. She also asks how infant feeding is going, whether Mom has any questions about returning to work and when is a good time to resume exercise…
Postpartum checkups: Physical recovery
During the physical checkup, your doctor or midwife will check your vitals, assess your weight and take your blood pressure. According to Mustaleski and Riley, they’ll also:
- Check your breasts for lumps and abnormal discharge
- If you’re breastfeeding, make sure your ducts aren’t clogged and you don’t have an infection
- Look at your abdomen for returning muscle tone
- Do a pelvic exam to see if your uterus is returning to its normal pre-pregnancy size and that the cervix is closed
- For c-section deliveries, make sure the incision is healing well and has no signs of infection
- Check how well any episiotomy or laceration has healed
- Administer any lab tests they think are necessary (such as a blood count if you lost a lot of blood during birth)
- Ask about your postpartum bleeding
- Ask about your pelvic floor recovery and refer you to a pelvic floor physical therapist, if needed If you’re having excessive pain, bleeding or problems with an incision, definitely tell your doctor, Riley says.
Postpartum checkups: Family planning
Another big item to cover during your postpartum checkups is birth control options . According to Riley, risk of complications in any subsequent pregnancy goes down if you wait at least 12 months after giving birth to conceive again. (The ACOG recommends ideally waiting at least 18 months.) Just because you’re breastfeeding and not menstruating yet doesn’t mean you can’t get pregnant . (After all, you ovulate before your first postpartum period arrives!) Your provider should discuss when you can safely start having sex again and talk you through your family planning options.
“It may seem like it’s too soon for that discussion, but some people do show up to their six-week postpartum appointment and find out they’re pregnant again!” Mustaleski explains, adding, “At your six- to eight-week postpartum appointment, many providers will do a Pap smear, if you’re due to have one done.”
Postpartum checkups: Emotional recovery
While physical recovery is certainly important, your doctor will also want to check in on how you’re coping with the transition to motherhood. During the visit, expect to answer questions about your mood, sleeping patterns and other aspects of your emotional well-being.
One big thing providers look for are signs of postpartum depression , which up to 15 percent of women experience, according to the American Pregnancy Association . The most common assessment is the Edinburgh Postnatal Depression Scale. “It’s a series of 10 questions that gives your doctor or midwife an overview of how you’re doing emotionally over the last seven days,” Mustaleski says. “If your score indicates that you’re experiencing postpartum depression, your doctor or midwife will discuss treatment options with you to help you start feeling your best as soon as possible.”
How to Prepare for a Postpartum Checkup
When you’re exhausted and sore, getting yourself out of the house for a postpartum checkup may seem daunting—but remember, these critical visits are set up to ensure your health and well-being.
Since this post-pregnancy stuff is completely new to you—the aches, the pains, the emotions—be sure to track and flag any symptoms you’re worried about, and write down all your questions beforehand. “Most new parents are functioning on minimal sleep, so attempting to recall your questions in the moment is difficult,” Mustaleski says. Her advice? Start a list on your phone that you can easily bring with you to the appointment. Your questions might touch on the topics mentioned above, plus:
- How your delivery went
- Baby’s safety
- Physical activity and exercise goals
- Breastfeeding or formula-feeding
- Returning to pre-pregnancy activities
- Body changes or new pains (pay attention to worsening pressure in your vagina, difficulty with bowel movement and inability to fully empty your bladder, Mustaleski says)
Make sure to also note any additional support you feel you need, such as a lactation consultant, pelvic floor therapist, mental health therapist or other professional.
As you prepare for a postpartum checkup, remember to also plan for childcare. Due to COVID-19, some offices may not be allowing baby to come with you. It’s always best to call ahead and ask about the office’s policies. “Many midwives will do a well-baby check up at the same time as your postpartum visit, so you can also ask if that is an option with your provider,” Mustaleski says. If you do end up bringing baby to the appointment, remember to pack a change of clothes, diapers, wipes, burp cloths, pacifiers (if baby is using them) and an extra bottle if baby’s not breastfeeding.
Postpartum checkups can be a lot to take in, but they’re ultimately designed to support you. Come prepared with any and all questions! “The postpartum is a time of in-between—you aren’t pregnant anymore, but you aren’t back to your everyday life,” Mustaleski says. “If you have questions about what is okay or safe for you to do during that transition, ask your provider to give you guidance on how to safely help your body recover.”
About the experts:
Laura Riley , MD, is a board-certified obstetrician who specializes in high risk pregnancies. She serves as the department chair of obstetrics and gynecology at Weill Cornell Medicine , as well as the obstetrician and gynecologist-in-chief at NewYork-Presbyterian/Weill Cornell Medical Center, based in New York City. She received her medical degree and completed her residency at the University of Pittsburgh School of Medicine.
Rebekah Mustaleski , CPM-TN, IBCLC, is a certified professional midwife specializing in evidence-based maternity care. She cofounded Roots & Wings Midwifery in Knoxville, Tennessee. Mustaleski received her bachelor’s degree in psychology from Centre College and worked as a doula and birth photographer prior to establishing Roots & Wings.
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Navigate forward to interact with the calendar and select a date. Press the question mark key to get the keyboard shortcuts for changing dates.
Next on Your Reading List

- Trying to Conceive
- Signs & Symptoms
- Pregnancy Tests
- Fertility Testing
- Fertility Treatment
- Weeks & Trimesters
- Staying Healthy
- Preparing for Baby
- Complications & Concerns
- Pregnancy Loss
- Breastfeeding
- School-Aged Kids
- Raising Kids
- Personal Stories
- Everyday Wellness
- Safety & First Aid
- Immunizations
- Food & Nutrition
- Active Play
- Pregnancy Products
- Nursery & Sleep Products
- Nursing & Feeding Products
- Clothing & Accessories
- Toys & Gifts
- Ovulation Calculator
- Pregnancy Due Date Calculator
- How to Talk About Postpartum Depression
- Editorial Process
- Meet Our Review Board
Your Postpartum Doctor Appointment
Should You Wait Six Weeks? When to See the Doctor and Why
Verywell / Bailey Mariner
The Postpartum Period
When to see the doctor, why you need to go, what to expect.
- Bring Your Questions
Symptoms to Bring Up
When to call the doctor.
- Skipping It
Your body goes through many changes during pregnancy and childbirth . So, after your baby is born, your body needs time to heal. As you recover, it’s important to make an appointment to see your OB-GYN for postpartum care. Here’s what you need to know about the postpartum visit, including when to see your doctor and what you can expect.
The time of your life after you have a baby is called the postpartum or postnatal period . It is broken down into three phases.
- Phase one is the initial recovery during the first six to twelve hours after giving birth.
- The second stage lasts two to six weeks while your body is physically healing, and you are adjusting to life with your newborn.
- The third part is the gradual return of your body to the way it was before your pregnancy. Of course, some things may not entirely go back to the way they were. This time of healing can take up to six months.
Watch Now: The Three Stages of Postpartum Depression
In the past, a postpartum check-up was a one-time visit scheduled between four and six weeks after delivery. However, thoughts on postnatal care have changed in recent years. Health experts now consider postpartum care an ongoing process based on each individual’s needs.
The World Health Organization (WHO) guidelines published in 2013 recommend at least four postnatal interactions after delivery: in the first 24 hours, on the third day, between 7-14 days, and at six weeks.
In 2018, the American College of Obstetricians and Gynecologists (ACOG) updated its guidelines to reflect an ongoing process.
After the initial care at birth, the first postpartum contact or visit should be within three weeks. You should stay in contact with your healthcare provider during the first three months, and a complete and thorough postpartum exam should occur no later than twelve weeks.
After you have a baby, you experience physical and emotional changes . A visit with your doctor during this time can help prevent complications. If something isn't right, the doctor can catch it and treat it early before it becomes a problem.
This appointment is also time set aside to talk to your doctor about sensitive issues and get answers to questions you may have about bleeding, your sex drive, birth control , the baby blues, postpartum depression , and more.
All pregnant women should receive postpartum care even if the pregnancy ends with a devastating loss . Physical and emotional care and support are even more critical during a very difficult time.
You should see your doctor or talk to your doctor on the phone within three weeks of giving birth. If you have a c-section , complications, or other health issues such as gestational diabetes or high blood pressure , you may see your doctor sooner and keep in touch with the doctor more often as you heal.
At your first contact, you will spend some time talking to your doctor. The doctor may also check your blood pressure or follow up with any other concerns. As your care continues, the health care team can keep in touch with you in a variety of ways. You may go to the office, see a health care provider at home, or talk to the doctor on the phone or by text message.
As postpartum care nears its end, you should have a thorough health and wellness examination before you transition to well-care. Your comprehensive exam can take place as early as four weeks after birth, but no later than 12 weeks, depending on your situation. This visit is a complete check-up of your physical, social, and psychological health.
During this appointment, you will have a full physical exam. The doctor may:
- Check your weight
- Take your blood pressure
- Check your perineum to see how you’re healing
- Check an episiotomy , tear, or c-section wound if you have one
- Check to see if your uterus is shrinking as expected
- Check your breasts and talk about breastfeeding
- Discuss any health issues you have
- Talk to you about the postpartum blues and depression
- Answer questions about your labor and delivery if you have them
You may also have your general gynecological screening if you are due for it. It may include a Pap smear, bloodwork to check for anemia or high blood sugar, and a urine test if you have urinary problems or symptoms of a urinary tract infection.
The doctor will also talk to you about:
- How your body is recovering from childbirth
- Your emotions and how you feel about motherhood
- Any anxiety or depression that you may be feeling
- Your social support system
- How you are sleeping
- Nutrition and your eating habits
- How caring for your baby is going
- How bottle-feeding or breastfeeding is going
- If you are considering having more children
- Any concerns about sex
- Birth control
- Managing any health concerns such as high blood pressure, diabetes, or other conditions
- Following up with other health practitioners for any issues you may have
- Continuing to tend to your health through routine care
Bring Your Questions
You are bound to have questions, especially if you just had your first baby. But, since pregnancy and birth can be very different with each child, experienced moms can have questions, too.
As questions come up, write them down so you can bring them to your appointment. If you don't write them down, you may not remember everything you want to ask once you're sitting in the office. And remember, there are no silly questions. You shouldn't feel uncomfortable or embarrassed about asking your doctor anything. That's one of the reasons they're there, and they want to help. Some of the things you may want to ask about are:
- Your delivery
- The healing process
- Preventing problems now and in the future
- Breast issues such as pain or lumps
- Caring for your newborn
- Returning to work
Those pesky pregnancy symptoms may finally be gone, but the postpartum period has its own set of discomforts. Most of the time, postpartum symptoms are common and expected. However, sometimes they can be a sign of a complication. So, you should discuss all your symptoms with your doctor. The doctor can reassure you of what's normal and help you find relief, but also look into any concerning symptoms. You should talk to your doctor about:
- The amount and color of any bleeding you are experiencing
- Hemorrhoids
- Constipation
- Leaking urine
- How you're feeling
- If you are sad or under a lot of stress
You do not have to wait for your scheduled postpartum appointment to talk to or see the doctor if you have urgent concerns . You should call the doctor or go to the hospital if you have:
- A fever over 100.4 F
- Bleeding that is getting heavier
- Severe pain
- Swelling in your body, especially your hands or face
- Nausea and vomiting
- A headache that is not going away or getting worse
- Foul-smelling vaginal bleeding or discharge
- Difficulty caring for yourself and your baby
- Feelings of depression
- Painful, burning urination or urinary frequency
Skipping It
Not all women get postpartum care. Up to 40% of women do not follow up with a doctor after giving birth. There are many reasons for this, such as:
- Not knowing about it
- Not knowing who to call
- Being too busy
- Having too many other things to do
- Thinking it isn't necessary
- Feeling good
- Not having anyone to watch the baby
- Having been through it before many times
- Concerns about the cost
- The insurance will not cover it
While there are things that make can make it difficult or inconvenient to get there, you should make every effort to see the doctor. If you have to bring your baby with you, you can. If you’re concerned about the cost or your insurance, talk to the hospital staff or your health care provider for helpful resources.
Skipping out on postpartum care can have some unintended consequences.
- You may not realize you have an infection or a postpartum complication.
- You may not heal well.
- You could get pregnant again quickly.
- You could have undiagnosed postpartum depression.
A Word From Verywell
During pregnancy, prenatal visits are plentiful. But, the attention to an expecting mom's health and wellness seems to fade once the baby is born. Care during the postpartum period can be overlooked at a time when many women need it most.
The body changes so much during pregnancy, birth, and the postpartum period. It is incredible what the body goes through in less than one year. And, it's true that some women feel wonderful after childbirth. But, for others, the physical and emotional challenges of the fourth trimester can be a struggle.
The continuation of care after pregnancy is so important. Just as you need ongoing care during pregnancy, labor, and delivery, you need it while you're healing in the days, weeks, and months after your baby is born. Postpartum care should be part of your overall pregnancy care. You and doctor should work together to make sure your health is monitored and managed throughout the entire process. So, talk about it with your doctor while you're pregnant, be sure to make your appointments, and don't skip out on them even if you're feeling good.
Romano M, Cacciatore A, Giordano R, La Rosa B. Postpartum period: three distinct but continuous phases . Journal of prenatal medicine. 2010 Apr;4(2):22.
World Health Organization. WHO recommendations on postnatal care of the mother and newborn. World Health Organization; 2014.
Care OP. ACOG Committee Opinion No. 736 Optimizing Postpartum Care . American College of Obstetricians and Gynecologists. Obstetrics & Gynecology. 2018;131(5):e140-50.
Fahey JO, Shenassa E. Understanding and meeting the needs of women in the postpartum period: the perinatal maternal health promotion model . Journal of midwifery & women's health. 2013 Nov;58(6):613-21. doi:10.1111/jmwh.12139
Al-Safi Z, Imudia AN, Filetti LC, Hobson DT, Bahado-Singh RO, Awonuga AO. Delayed postpartum preeclampsia and eclampsia: demographics, clinical course, and complications . Obstetrics & Gynecology. 2011 Nov 1;118(5):1102-7. doi: 10.1097/AOG.0b013e318231934c
Jordan RG, Farley CL, Grace KT. Prenatal and postnatal care: a woman-centered approach. John Wiley & Sons; 2018 Apr 23.
DiBari JN, Yu SM, Chao SM, Lu MC. Use of postpartum care: predictors and barriers . Journal of pregnancy. 2014;2014. doi:10.1155/2014/530769
Nazik E, Eryilmaz G. The prevention and reduction of postpartum complications: Orem’s Model . Nursing science quarterly. 2013 Oct;26(4):360-4.
Martin A, Horowitz C, Balbierz A, Howell EA. Views of women and clinicians on postpartum preparation and recovery . Maternal and child health journal. 2014 Apr 1;18(3):707-13. doi:10.1007/s10995-013-1297-7
By Donna Murray, RN, BSN Donna Murray, RN, BSN has a Bachelor of Science in Nursing from Rutgers University and is a current member of Sigma Theta Tau, the Honor Society of Nursing.

Personalize Your Experience
Log in or create an account for a personalized experience based on your selected interests.
Already have an account? Log In
Free standard shipping is valid on orders of $45 or more (after promotions and discounts are applied, regular shipping rates do not qualify as part of the $45 or more) shipped to US addresses only. Not valid on previous purchases or when combined with any other promotional offers.
Register for an enhanced, personalized experience.
Receive free access to exclusive content, a personalized homepage based on your interests, and a weekly newsletter with topics of your choice.
Home / Pregnancy / Post-partum: What to expect in the 6 weeks after delivery
Post-partum: What to expect in the 6 weeks after delivery
Please login to bookmark.
Everything’s new. Everything’s exciting. And everything’s hard. The first six weeks after birth probably aren’t talked about enough. Myra J. Wick, M.D., Ph.D., Mayo Clinic obstetrician, gynecologist and medical geneticist, joins Co-hosts Angela Mattke, M.D., and Nipunie Rajapakse M.D., for candid convo of what comes after birth, including:
* Diapers, pads, witch hazel, laxatives and other essentials
* Post-partum depression and anxiety
* Getting baby to sleep — mom, too!
* Building a village to help child and parents
* Fatigue and exhaustion
* Healing the birth canal
* Keeping up with the parent treadmill — and regularly stepping off
Listen: Post-partum: What to expect in the 6 weeks after delivery
Read the transcript:
Dr. Angela Mattke:
Welcome to the Mayo Clinic Moms podcast. We’re having candid conversations and answering difficult questions about pregnancy, raising kids, and everything mom-related. I’m Dr. Angela Mattke, and I’m a mom of two and a pediatrician at Mayo Clinic Children’s Center in Rochester, Minnesota. My co-host is Dr. Nipunie Rajapakse, who’s a pediatric infectious disease doctor, also at Mayo Clinic, and is also pregnant.
On today’s episode, we’re talking about what to expect in the postpartum period, which is the first six weeks after delivery. You might be asking yourself if it’s normal to feel this way. This isn’t what Instagram told me that postpartum was going to be like. Why don’t I look great? Why am I so exhausted? Why isn’t my baby sleeping? We’re also going to talk about postpartum depression, the baby blues, and anxiety. We’ll also talk about surviving exhaustion and feeling alone with the baby. How do you deal with the changes that have happened in your body?
Nipunie, I know that you’ve had some things in your pregnancy — you talked about having morning sickness, and your prenatal vitamin makes you sick. And now you’re probably pretty uncomfortable. You’re not sleeping well, and you’re tired; but I’m telling you, you’re probably in a pretty good place right now as far as the pregnancy journey goes, and I don’t want to scare you, but what happens in the postpartum period, I feel I wasn’t really prepared for, and nobody really told me about it. And so, I think we really want to prepare you for this today, and all of our listeners as well.
Dr. Nipunie Rajapakse:
Yeah. I thought this was going to be a bundle of joy, but the more I learn, the more I hear about this postpartum period getting home, [I’m learning] what that entails with some of the struggles that come along with it. I’m really interested to learn from your experience and Dr. Wick’s experience as well.
Yeah, absolutely. A baby is a bundle of joy, and it’s such a blessing, and it’s a wonderful experience, but we need to talk about what happens after you have pushed a baby through your vagina — and what happens to that vagina afterwards, and the carnage that it has experienced, especially after a vaginal delivery.
Yeah. What would you say, Angie, surprised you most when you brought your kids home for the first time?
It wasn’t the changes or the pain or the bleeding or things like that. I think it was the exhaustion. I thought I could handle exhaustion because we were used to not sleeping every fourth day, and working for 30 hours straight or more; but there’s no post-call day with a baby. You don’t get to go take a five-hour nap. It’s continuous, and especially if you’re trying to breastfeed, and you spend 40 minutes breastfeeding and then 20 minutes cleaning up and trying to get the baby to sleep. And then you’ve got one hour left to try and fall asleep, get a nap, and wake up again in order to get the baby up to breastfeed. It’s this never-ending treadmill that you’re on, where you feel like you just don’t catch up.
Yeah. I have felt the same way. I thought I knew lack of sleep and exhaustion from going through medical training, but everyone tells me this is on a whole other level than what we experienced then for sure. When it comes to things that you needed at home, was there anything that you would recommend having ready to go at home in terms of helping with the recovery from delivery? Maybe things you didn’t think of, or that you missed?
Dr. Wick, I want to hear your thoughts on this, but I think having appropriate pads at home and even bringing home some of the stuff from the hospital was really helpful. Some of the ice, the special little plastic or paper container that is waterproof is helpful for icing. Bringing home some of that mesh underwear that’s super sexy that you’re really excited to wear. But that can be helpful because you won’t ruin some of your own underwear. And then someone had told me to have some witch hazel on hand, and I found that helpful as well. Dr. Wick, what do you think?
Dr. Myra Wick:
Yeah, yeah. I think all those things are good tips. I think things that surprised me were how fast you went through diapers. Oh my gosh.
That’s so true. You go through 15 a day in the first couple weeks.
Yeah. If you’re having a term delivery, don’t buy a ton of newborn diapers because the baby is going to grow out of them so fast. And you won’t be able to use ’em; the baby will be too big. And then just feeling like I was wet all the time. You know, my breasts were leaking, and I needed a pad and the engorgement with the first baby, it’s crazy, and now we’re dismissing patients from the hospital early. A lot of times that engorgement happens when you’re at home, and it’s uncomfortable. Sometimes you can even get a little low-grade fever. I think those are the things.
Yeah, it’s pretty miserable.
I love the tip about the newborn diapers because we have a friend who has generously donated their 800 extra newborn diapers that they bought to us.
800?! Oh my goodness.
800 extras. I think we’re set there with our supply.
Maybe your baby will be small and will fit in those for a while. Good luck with that.
Yeah, for sure. In terms of other unexpected things I’ve heard — we talked a bit about pooping during the delivery itself, but I’ve heard first stool after delivery can sometimes be an adventure, and issues with constipation can certainly make that part of recovery more difficult. Any tips or tricks there that you have to offer?
I have a story there. After our last child, I was so constipated, and my in-laws were coming to visit, and it was a different time, of course. My mom came over, and I was sobbing in the shower, and she came in the bathroom and she’s like, “What can I do?”. She ran to the drugstore and got everything she could– Dulcolax, MiraLAX. And finally, I just decided I needed that cocktail, and then things were fine! But yeah, I was miserable. They’ll give you stool softeners with senna in the hospital. If you do have to use a little bit of laxative in your breastfeeding, that’s okay. It’s okay to do that.
Yeah. Absolutely.
And make sure you’re drinking a lot of water. Breastfeeding takes a lot of liquid, and your bowels need water to function normally. Just really push the water.
I like how you said they’ll give you that in the hospital. I would say don’t not take it because sometimes you can say, “Oh I don’t need it. I’m stooling fine.” You’re stooling fine now, but you don’t know what you’re going to be stooling like tomorrow or the next day. Keep it going so you’re not having to strain, because it’s pretty miserable. You’ll be in a lot of pain if that happens. It’s a great question, by the way, Nipunie; it’s a really good question.
And nobody wants to talk about it.
Yeah, exactly. There’s very little discussion about it. I thought it was a good one to bring up. I know we’ve spent a lot of time talking about some of the physical health effects, what your body goes through during the pregnancy, during the delivery. Obviously, pregnancy postpartum period, there are a lot of different types of mood disturbances that can happen as well. And so, in wanting to be proactive about that, what would be some of the factors that might put someone at higher risk for having postpartum depression or postpartum anxiety, for example, or other postpartum mood disorders?
Well, I think having a mood disorder before delivery or even before you’re pregnant puts patients at risk. Sometimes having a really difficult pregnancy or difficult labor experience might contribute as well. Those are some of the things that we look at. We do a lot of screening during pregnancy. We have a couple of different screening tools, and I know sometimes patients get tired of filling out those same questionnaires over and over, but it’s our way of assessing how people are doing and making sure that we’re catching things early. The other thing that we’ve started doing is offering a two-week postpartum mood check. We’re doing that virtually so that moms don’t have to come dragging in and find a parking spot and all that when they have a two-week-old baby.
We do that over the phone, but if moms want to come in or feel like they need to come in, we can certainly do that in person, too. We are also extremely fortunate to have some psychiatrists that are specially trained in prenatal and perinatal psychiatry. We actually have them in our outpatient unit one day a week or half a day a week. They are just an awesome resource for our whole practice. And I know we’re very blessed to have that, but we have all those tools that help us as providers take care of our patients.
I would add in, Dr. Wick, that because you guys see them usually at six weeks or eight weeks, depending on what type of delivery, at least at Mayo Clinic, we screen all moms for postpartum depression at their well-child visits with their infants. I think that this has been an initiative across the United States because postpartum depression can happen anytime, up to about a year after birth. You might not be under the care of your obstetrician or midwife or family medicine provider at that time, but you’re coming into our office. So we are doing screening at 2, 4, 6, 9, and 12 months for postpartum depression symptoms. And I can say in my own personal experience, we have been able to help a lot of women identify that they were struggling with depression, because sometimes it’s hard to realize where you’re at by yourself, but looking from the outside, it’s a lot more obvious to other people, and we can get them the help they need. Because we know that babies do better when their mom’s mental health is in a better place. We can help address that for them when they’re struggling.
INTERMISSION
Are you thinking about getting pregnant, or maybe you’re a current mom-to-be, or you’re like myself and you’re in the midst of raising kids, and you’re looking for practical evidence-based advice from Mayo Clinic experts? Mayo Clinic Press has got you covered. We have a series of four books, starting from Fertility and Conception to Guide to a Healthy Pregnancy , Guide to Your Baby’s First Years, and the last book in this series, the one I was the medical editor of, Guide to Raising a Healthy Child . You can find these amazing books from Mayo Clinic Press wherever books are sold, or on the Mayo Clinic Press website.
BACK TO THE SHOW
I know that many of these things exist on a spectrum, from more severe to more moderate symptoms. What would be some of the things to keep an eye out for and to know to seek help if you’re experiencing them?
It’s really common to have postpartum baby blues the first two to three weeks where you feel up and down; you’re so excited and overwhelmed and sleep-deprived and you may just cry spontaneously for no reason. And those are all normal responses. I think things to watch out for, after that period of two to three weeks – very, very down, very anxious, not able to function; maybe you’re not able to take care of the baby or you’re not taking care of yourself. Care for yourself is a little different postpartum—but specifically when you’re really just not keeping up. Maybe you’re not getting out of bed. You’re not doing the things that would be normally done by a new mom. Those are things your partner can help watch for as well. Obviously, if things are very severe, if you’re feeling suicidal, then we’re going to refer you to an emergency department. But more often, it’s feeling really down and unable to function the way you’d like to.
I think that’s a great point about the role that partners can play, Dr. Wick, and recognizing some of these things as well. I think we’re also starting to recognize postpartum mood disorders occurring in partners as well, more and more commonly. I think it’s important to make sure you’re looking out for each other during this phase as well.
Right. We’re seeing a lot of anxiety and I don’t know if it’s probably related to the pandemic. I feel like we are really seeing a lot of anxiety in the last couple of years. We can help with that too. And the psychiatrists we work with are very aware and happy to see those patients as well.
By myself, I anticipate that I’ll be anxious about the baby — is the baby okay? Are they eating enough, are they gaining enough weight, and all that. How do you know when it is above and beyond the usual anxiety that a new mom would experience with a new baby?
I think if it’s interfering with how you’re functioning daily. I had a patient recently that said I can’t even go to the grocery store and leave the baby with my mother-in-law because I’m afraid that something’s going to happen, or she’s not going to do something right. That’s probably a little bit beyond what a normal reaction would be. It’s normal to go to Target and think, “Oh, I wonder what my baby’s doing. And I hope my husband’s okay with the baby.” And you know they are; in your heart, you know they are. But to not be able to leave because of that is probably beyond what would be considered typical.
I noticed in the first couple weeks after — even in the first couple days, I just couldn’t sleep because every little sound the baby would make would wake me up. And now we have recommendations that all babies co-room, so meaning they sleep in their parents’ room for at least the first six months of life, if not the first 12 months of life. We know that that’s good for reducing sudden infant death syndrome, but it also has been shown to decrease sleep quality for everyone else in their room. I know I definitely experienced that, and I think it was just driving me crazy because I couldn’t sleep, and I’d worry I’d missed something. I think it just was the cycle. The less sleep you get, the more anxious you get, and then you get less sleep again because you’re worried you’re going to miss something. That was a hard thing for me. Getting some white noise in the room so I could sleep and I wouldn’t hear everything was really, really helpful. Then your anxiety gets better because you finally get some sleep. It’s this vicious cycle. Something to think about.
For sure. Yeah. I think the sleep deprivation and tips on how and when to sleep are going to be really helpful for us for that period after the baby comes home, for sure. And hopefully, being able to trade off a bit and things like that will be helpful also.
Yeah. Having a partner is helpful. But for those people that don’t have partners, try and get their community, get their village — friends and their parents and other people that can help out. Don’t be afraid to ask for help and ask them to come watch the baby for a little bit. Your baby’s going to be okay; you’ll be sleeping in the room down the hall. Everything will be fine. Nipunie, you mentioned that you’ve been getting a lot of hits on Instagram about baby stuff and pregnancy. Have you seen some of those snapback photos or the postpartum pictures?
Yeah. It’s a lot of people posting and they’re looking back to their usual self within a couple weeks of having this child. And I think realistic expectations are what I want to know. Is that realistic or what can you actually expect to happen to your body afterwards? I’m sure it’s not as fast as what they show on social media.
No. And they’ve got lighting and glam teams and everything like that too. Keep in mind that there’s a lot of editing that goes into those photos, but Dr. Wick, I think you can weigh in on this a little bit more, but I think that’s completely unrealistic. You just spent nine months being pregnant. I think, in my mind, it should take at least nine months, if not more, for your body to go back to a similar way it looked and felt at that time. Also keep in mind that your body’s never going to be the same. It’s going to be different. You just grew a child in your body and then gave birth to it. That’s a beautiful thing. Things shouldn’t probably be like they were before because you want to show that you did something pretty powerful. What do you think, Dr. Wick?
Yeah, I agree. Everything’s saggier.
Even though you might be exercising and working on things, it’s never really quite the same.
Exactly. I feel like those ab muscles, they never really go back together as much as you want. So yeah, quit looking at Instagram. I think everyone needs to stop the snapback photos and just be more supportive. I really love this trend of people posting realistic photos of what your body actually looks like after birth. I’ve really enjoyed a lot of the celebrities who’ve shed some reality on what life is really like.
Yeah, definitely nice to see what the reality is. When it comes to getting back into exercise, Dr. Wick, are there restrictions or guidance on when it’s safe to start exercising after you’ve had a baby?
Yeah. You know, for the first couple of weeks, especially if you’ve had a C-section, we want you to be careful, and we don’t want you lifting more than 25 pounds after C-section for the first six weeks. We want all those layers, the fascia, the tough layer that holds everything in, to be well-healed. But it’s okay to start walking a little bit, especially if it’s nice outside — get out and take the baby in a stroller and listen to your body. If you’re starting to feel tired or something’s pulling or tugging, then maybe it’s time to turn around and rest. But gradually work your way back. Don’t expect that you’re going to go out and run a 10-mile run after six weeks. Most people have to gradually work their way back into things. I think the most important thing is just listening to what your body’s telling you about fatigue.
I want to thank you both for this great discussion today, and I want to thank our audience for listening. I hope you can join us on more episodes of our pregnancy podcast. The next episode will be all about feeding your baby — questions about breastmilk versus formula, or — how do I know if my baby’s getting enough? Can what I eat affect my breast milk? Can I have a glass of wine once in a while? And what about antibodies from vaccines? COVID vaccines, influenza vaccines — will those transfer to my baby? And more. Make sure you catch that episode. Thanks everyone for joining today. Make sure you don’t miss any of our upcoming episodes by subscribing and following along on either Apple Podcasts or Spotify. If you enjoyed this episode, and you want other moms out there to hear this valuable information, make sure that you leave a review wherever you listen. Thanks for joining us. We’ll see you next time.

Relevant reading
Bedtime Book for Bump
This gorgeously presented keepsake is the perfect gift for expectant parents, allowing them to start bonding with their unborn baby.

Discover more Pregnancy content from articles, podcasts, to videos.
You May Also Enjoy

Privacy Policy
We've made some updates to our Privacy Policy. Please take a moment to review.
- Getting Pregnant
- Registry Builder
- Baby Products
- Birth Clubs
- See all in Community
- Ovulation Calculator
- How To Get Pregnant
- How To Get Pregnant Fast
- Ovulation Discharge
- Implantation Bleeding
- Ovulation Symptoms
- Pregnancy Symptoms
- Am I Pregnant?
- Pregnancy Tests
- See all in Getting Pregnant
- Due Date Calculator
- Pregnancy Week by Week
- Pregnant Sex
- Weight Gain Tracker
- Signs of Labor
- Morning Sickness
- COVID Vaccine and Pregnancy
- Fetal Weight Chart
- Fetal Development
- Pregnancy Discharge
- Find Out Baby Gender
- Chinese Gender Predictor
- See all in Pregnancy
- Baby Name Generator
- Top Baby Names 2023
- Top Baby Names 2024
- How to Pick a Baby Name
- Most Popular Baby Names
- Baby Names by Letter
- Gender Neutral Names
- Unique Boy Names
- Unique Girl Names
- Top baby names by year
- See all in Baby Names
- Baby Development
- Baby Feeding Guide
- Newborn Sleep
- When Babies Roll Over
- First-Year Baby Costs Calculator
- Postpartum Health
- Baby Poop Chart
- See all in Baby
- Average Weight & Height
- Autism Signs
- Child Growth Chart
- Night Terrors
- Moving from Crib to Bed
- Toddler Feeding Guide
- Potty Training
- Bathing and Grooming
- See all in Toddler
- Height Predictor
- Potty Training: Boys
- Potty training: Girls
- How Much Sleep? (Ages 3+)
- Ready for Preschool?
- Thumb-Sucking
- Gross Motor Skills
- Napping (Ages 2 to 3)
- See all in Child
- Photos: Rashes & Skin Conditions
- Symptom Checker
- Vaccine Scheduler
- Reducing a Fever
- Acetaminophen Dosage Chart
- Constipation in Babies
- Ear Infection Symptoms
- Head Lice 101
- See all in Health
- Second Pregnancy
- Daycare Costs
- Family Finance
- Stay-At-Home Parents
- Breastfeeding Positions
- See all in Family
- Baby Sleep Training
- Preparing For Baby
- My Custom Checklist
- My Registries
- Take the Quiz
- Best Baby Products
- Best Breast Pump
- Best Convertible Car Seat
- Best Infant Car Seat
- Best Baby Bottle
- Best Baby Monitor
- Best Stroller
- Best Diapers
- Best Baby Carrier
- Best Diaper Bag
- Best Highchair
- See all in Baby Products
- Why Pregnant Belly Feels Tight
- Early Signs of Twins
- Teas During Pregnancy
- Baby Head Circumference Chart
- How Many Months Pregnant Am I
- What is a Rainbow Baby
- Braxton Hicks Contractions
- HCG Levels By Week
- When to Take a Pregnancy Test
- Am I Pregnant
- Why is Poop Green
- Can Pregnant Women Eat Shrimp
- Insemination
- UTI During Pregnancy
- Vitamin D Drops
- Best Baby Forumla
- Postpartum Depression
- Low Progesterone During Pregnancy
- Baby Shower
- Baby Shower Games
Postpartum recovery timeline
Your postpartum body will recover on its own schedule following childbirth, but there's a general postpartum recovery timeline that applies to most women. Afterpains will stop in the first week, for example, and bleeding will subside during the first month. You may have breast tenderness, night sweats, and exhaustion, and if you've had a C-section, you'll need additional recovery time. From one week to one year postpartum, here's what to expect.

One week postpartum
Two weeks postpartum, six weeks postpartum, six months postpartum, one year postpartum.
You've entered your "fourth trimester" now and are on your way to recovering from pregnancy and childbirth. How that recovery progresses is very individual, depending on everything from your age and overall fitness to what kind of pregnancy, labor, and delivery you experienced. Here are some general guidelines, though, so you know what to expect when it comes to recovering – both mentally and physically – during the postpartum period.
Your physical recovery: vaginal birth
Bleeding: You may still have some spurts of vaginal bleeding on and off through the day. But, overall, the lochia – the combination of blood, tissue and mucus that your body sheds after birth – has decreased and may even already be just a watery, pinkish discharge. Many women continue to have a small gush of light bleeding a few times a day, especially while breastfeeding .
Your lochia will change into a white or yellow-white discharge and then keep tapering off until it stops in another two to four weeks. It's very important that you call your provider immediately if you have extensive bleeding, which is a sign of postpartum hemorrhage .
Perineum soreness: If you had a vaginal birth without tearing, your perineum (which may have been swollen and sore at first) is probably fine by now. Depending on how your labor went and if you tore or had an episiotomy , though, you may still be sore and even have vaginal and perineal pain .
Cramping: Postpartum cramping happens as your uterus contracts and is usually most intense on days two and three after delivery. These afterpains should be gone by now.
Pelvic floor discomfort: You may have symptoms resulting from the stretching and/or injuring of your pelvic floor muscles during delivery. These symptoms – such as incontinence , difficulty walking, and pelvic pain – usually get better within weeks, but they don't always return to pre-pregnancy strength without assistance. If you continue to have symptoms, ask your provider at your postpartum checkup if pelvic floor therapy might help.
Breast changes: Your breasts may have been tender, full, and/or engorged as your milk came in this past week. If you're not breastfeeding, your breasts probably have stopped making milk by now, which means you're more comfortable. If you're breastfeeding, your breasts have likely adapted by now, although some women take a little bit longer to get the supply and demand equation just right. Talk with your provider, your baby's pediatrician, or a lactation consultant for advice. You may feel nipple soreness as your baby latches onto your breast in the first week or so. (The pain shouldn't last through the feeding, though.)
Swelling: Postpartum edema (swelling) should be going away now by now, though it may last a few days more, especially if you had excess swelling due to preeclampsia or pregnancy-related high blood pressure . If you had swollen labia during pregnancy, it should also be getting better now.
Your uterus is now half the size it was after you gave birth. You lost about 13 pounds after delivery, and you probably lost about 4 to 6 pounds of water weight this week.
Fatigue: Tiredness is common. You're recovering from childbirth, experiencing a major life change, learning to take care of your baby, and likely not getting much sleep. It's no surprise that you're tired. Ask for help and talk with your healthcare provider about your level of fatigue .
Hot flashes and night sweats : These may be intense at times, and you may wake up to feed your baby and find your night clothes soaked. Your hormones have changed drastically in the past week, and just as your milk was coming in, the sweating started. This is normal and will pass within the next few days.
Your physical recovery: C-section
In addition to most of the recovery mentioned above for vaginal birth, you're also recovering from major abdominal surgery. That means more healing and a slower recovery.
You might be finding it difficult to move around very much, but it's important that you do. Mild activity speeds healing, plus it prevents blood clots. Just take it slowly.
Your incision should be healing nicely, and your provider may schedule a post-op visit to make sure. It may still feel tender, but it should be a lot less painful now. (Most women are off painkillers by this point.) You may feel numbness and some twinges of pain around the incision for several months.
You're able to lift your baby now (usually within two to four days), but nothing heavier.
Your mental health and postpartum hormones
Your hormone levels are changing - estrogen and progesterone levels are dropping, and prolactin and oxytocin levels rise and fall as baby nurses. Add sleep deprivation to the mix, and it's no wonder you're feeling a little unsteady.
It's normal to feel exhausted and overwhelmed. In fact, many moms experience the baby blues – feelings of sadness, emotional sensitivity, and weepiness – in the days after giving birth. (Think of it like the worst PMS you've ever had.) These feelings can last up to two weeks.
Things to do if you're feeling blue after delivery .
If you're not feeling better in a couple of weeks, or if your feelings are intense, talk with your healthcare provider. You may be experiencing postpartum depression . It's a treatable condition, and the sooner you get help the better.
Take our postpartum depression quiz if you're wondering about the feelings you're having.
Your lochia (vaginal bleeding and discharge) is continuing to taper off and may be very light by now. You may still have occasional, small bursts of bleeding, though.
If you had a second-degree tear (involving skin and muscle), it's probably healing this week and next. Any stitches for a tear may be feeling itchy now. This is a good sign that they're healing.
Depending on how breastfeeding is going, you may have sore nipples for a number of reasons. If your baby's latch is shallow, for example, or if they have thrush or are tongue-tied , your nipples may hurt. Talk with a lactation consultant about possible causes and remedies.
Your uterus has now returned to your pelvis, and you're continuing to lose water weight.
If you had bloodshot eyes from the pushing and straining of labor, these have resolved by now.
While you're still probably a little sore, you can probably move around a bit better now.
Your scar may be a little itchy as the incision heals.
If you had steri-strips (small, white, sticky bandages) on the incision, they should fall off now (if they don't, you can gently remove them). If you have glue over your incision, you can probably remove it now, too. Both the steri strips and glue tend to get a little gross after three weeks, so make sure you remove them at that point. If you have trouble seeing your incision, you can ask your partner (or doctor) for help.
You may be able to drive now, if you're no longer taking narcotic pain killers and if you can react quickly enough to drive safely. You can test to make sure you can move comfortably to check your blind spot, press the brake pedal, etc., by practicing the movements in the passenger seat. If you hesitate or wince prior to pretend braking or merging, it's not quite time yet.
If you had the baby blues, they may be fading now. If you're having extreme feelings of sadness or are crying often, or have other signs of postpartum depression, talk with your healthcare provider to get help as soon as possible.
You may or may not feel 100 percent back to "normal," but six weeks is generally considered a postpartum milestone for recovery. Here's why:
- Though it can start up again once in a while, for most women postpartum bleeding has stopped.
- Your uterus is back to its pre-pregnancy size, having shrunk from about 2.5 pounds after childbirth to only 2 ounces now. That doesn't mean your abdomen looks the same, though. Your abdominal muscles have stretched, and it takes time and exercise to get them back in shape.
- Most moms have lost about half their pregnancy weight at this point.
- Your healthcare provider may give you the go-ahead for exercise and sex at your six-week postpartum checkup.
- If you had an uncomplicated vaginal delivery, you may have regained pelvic floor strength by now. (If you had a multiple birth or a birth injury during delivery, it can take longer.) Ask your provider about pelvic floor physical therapy if you note leaking of urine or signs of prolapse.
- If you're exclusively formula feeding your baby, you may get your first postpartum period in the next couple of weeks.
- Even if you had a third- or fourth-degree laceration during childbirth, the pain should have subsided by now.
- If, during pregnancy, you had diastasis recti (a vertical bulge where the long, flat muscles running vertically down each side of your abdomen have separated), it should have resolved by now. If it hasn't, a physical therapist can work with you to strengthen your muscles and reduce that gap between them.
By your six-week mark, you should be feeling well recovered from surgery. You shouldn't have pain, and your incision scar should be healed, though it may still occasionally feel itchy or burn. You can now lift most things (ask your provider for guidelines).
Hopefully you're adjusting well to your new role and feeling settled in by now. Still, it's normal to feel tired and upset now and then. But it shouldn't be all the time. You still need to be on the lookout for signs of postpartum depression and contact your healthcare provider right away if you're concerned.
Your physical recover: vaginal birth
Most women have lost one-half of their pregnancy weight gain by now (but remember, all women are different, so it may take more or less time for you).
Any melasma (dark spots) or stretch marks on your belly or breasts are beginning to fade. If you have linea nigra (a dark line down your abdomen), it will fade, too, though it may not completely go away.
On the negative side, you may have started noticing some hair loss in recent months, as your estrogen level dropped and your hair follicles entered their resting/shedding phase. (During pregnancy, when your estrogen climbed, the growing stage was prolonged. That's why you may have had such luxurious locks during pregnancy.) You'll notice the new hair growth as short, wispy bits.
Don't be alarmed if you're still feeling tired. Many of your physical symptoms are vastly improved, and you should feel overall pretty recovered from surgery, but it's not unusual to still be tired. In one study Opens a new window of over 1500 women, those who had a C-section were more likely to report extreme tiredness at 6 months postpartum and 12 months postpartum than those who had a spontaneous vaginal birth.
May be feeling pretty upbeat now, especially if your baby is sleeping more and you're adjusting well. If you have any signs of postpartum depression, talk with your healthcare provider right away.
Though they may not completely disappear, any stretch marks and linea nigra have continued to lighten.
You may have a period by now too, even if you're breastfeeding.
Your numbness around the scar will likely have resolved by now. The scar has healed, and while it's appearance will continue to fade over time, it will do so much more gradually now.
Your baby is a toddler now! Your new life comes with new stresses, whether it's balancing work and family , helping siblings get along, weaning your baby from breastfeeding, or deciding whether or not to have another baby . While you're technically outside the definition of "postpartum" depression now, moms carry a lot for their families, and you deserve support. Reach out to your doctor if you're experiencing symptoms of depression.
Learn more:
- Postpartum warning signs
- C-section recovery
Can you take a bath after giving birth – and when?
- When can I go back to work after having a baby?
- How to deal with a difficult birth experience
Was this article helpful?
Warning signs of postpartum complications

Postpartum cramping

Postpartum swelling (edema)

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
March of Dimes. 2018. Your body after baby: The first 6 weeks. https://www.marchofdimes.org/pregnancy/your-body-after-baby-the-first-6-weeks.aspx Opens a new window [Accessed March 2022]
Mayo Clinic. 2020. Postpartum care: What to expect after a vaginal birth. https://www.mayoclinic.org/healthy-lifestyle/labor-and-delivery/in-depth/postpartum-care/art-20047233 Opens a new window [Accessed March 2022]
Thurston RC et al 2013. Prospective evaluation of hot flashes during pregnancy and postpartum. Fertility and Sterility 100(6): 1667-1672. https://www.fertstert.org/article/S0015-0282(13)02967-1/fulltext [Accessed March 2022]
Woolhouse H et al. 2012. Physical health and recovery in the first 18 months postpartum: Does cesarean section reduce long-term morbidity? Birth 39(3): 221-9. https://pubmed.ncbi.nlm.nih.gov/23281904/ Opens a new window [Accessed April 2022]

Where to go next

- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Postpartum Care: A Guide to Taking Care of a Body That Just Delivered
- First 24-Hours Instructions
- Days and Weeks After Birth
- Coping Through Changes
- Postpartum Follow-Up
- Resources and Support
The postpartum period, the time after giving birth, is a crucial time for recovery and the long-term health of the parent and baby. It's also a time of intense physical and emotional changes.
It is normal and expected to experience several physical symptoms like swelling, cramping, breast tenderness , constipation , and leaking milk. It is also common to experience emotional changes like feeling sad and overwhelmed.
This article discusses postpartum care, what to expect, and how to care for yourself.
Yoss Sabalet / Getty Images
Postpartum Care: Instructions for the First 24 Hours
The first 24 hours after birth can feel like a whirlwind. Your focus is both on healing physically and caring for your newborn.
Physical symptoms you may experience in the first 24 hours include:
- Perineum soreness : If you had a vaginal birth , the area between the vagina and the rectum may feel sore or painful. This is because of stretching or tearing during labor and delivery.
- C-section pain : If you had a surgical deliver known as a cesarean section (C-section), you may feel exhausted and pain around your incision. Rest is crucial.
- Afterbirth pains : After giving birth, your uterus will begin to shrink back to its original size, which may cause abdominal cramping.
- Vaginal discharge : Vaginal bleeding after delivery is expected. However, call your provider if you have heavy, bright red bleeding or are passing golf ball–sized blood clots.
- Breast engorgement : This occurs when the breasts fill with milk a few days after delivery.
- Swelling : Pregnancy causes water retention in the body, especially the hands, feet, and face. It may also be a sign of preeclampsia and should be discussed with a medical provider.
- Constipation : It may feel difficult to have a bowel movement after giving birth.
- Pain with urination : If you had vaginal tearing with birth, you may experience pain or burning with urination, leaking, and incontinence .
- Fatigue : Your body will feel tired from the exertion of childbirth, blood loss, and a lack of sleep.
It's common to feel overwhelmed and exhausted or down and sad. The "baby blues" are typical feelings that come after having a baby and are typical for up to two weeks.
Postpartum Care in Days and Weeks After Birth
The days and weeks after giving birth can be emotional. You will likely not feel like yourself because of your physical recovery, changing hormone levels, and caring for a newborn.
It is important to see your healthcare provider during the postpartum period. Your provider can help keep you and your newborn healthy.
Healing From Birth
Giving birth is physically exhausting and requires time to heal. There are many symptoms you might feel during the postpartum period. Fortunately, there are ways to help relieve them.
Postpartum sleep can be challenging. You will likely feel tired in the weeks and months after giving birth. To help your body heal, focus on resting as much as possible. Sleep when your baby sleeps. Consider limiting visitors to help you catch up on rest. If some of your loved ones have offered to help you, ask them to take over household chores so you can use that time to rest.
Mental Health
It's common to feel sad, anxious , or irritable for up to two weeks after giving birth. When frequent feelings of sadness, anxiety, hopelessness, or anger last longer than two weeks, you may have postpartum depression .
Postpartum depression affects about 1 in 8 people in the postpartum period. Symptoms may include:
- Feeling angry, sad, hopeless, guilty, or worthless much of the time
- Eating more or less than usual
- Sleeping more or less than usual
- Crying frequently
- Losing interest in favorite activities
- Withdrawing from friends and family
- Having thoughts of hurting yourself or your baby
If you are concerned about your mood, talk with your healthcare provider right away. Fortunately, postpartum depression is treatable with therapy support groups, medication, and support. Other measures that may help include:
- Rest as much as possible.
- Ask for help.
- Make time to see friends and family.
- Share your experience with fellow parents or a support group.
- Avoid making significant life changes.
Contraception
It may seem too soon to start thinking about future pregnancies, but it is important to have a contraception plan when you are postpartum. Most healthcare providers recommend abstaining from sex for about four to six weeks after giving birth. This is how long it usually takes to heal.
Once you are ready to have sex again, talk with your provider about a contraception plan. You may consider barrier methods like condoms and diaphragms or hormonal methods like pills , patches, intrauterine devices (IUDs), or shots.
Coping Through Postpartum Changes
The postpartum period brings countless changes. It may be helpful to make a plan for changes in this new chapter of life.
Physical and Self-Esteem
The physical exertion of childbirth, lack of sleep, and other factors may make you uncomfortable. Focus on rest and recovery. Caring for a newborn requires a lot of time, but aim to eat, sleep, and shower daily.
Plan to wear a sanitary pad in the days and weeks after birth due to vaginal bleeding. Drink plenty of water, and add healthy, fresh foods to your meals when possible.
Talk with your healthcare provider about an exercise plan. There are several benefits to working out in the postpartum period, including increased energy, better sleep, stress relief, and stronger muscles. Start slow, taking 10-minute walks, and work up from there.
Adjusting to Parenthood
Adjusting to life as a new parent (or a parent with another child) takes time. Try to focus on small things that help you feel like yourself. Sleep whenever you can, and spend time resting throughout the day. Talk to your partner, friends, or loved ones about how they can support you.
It's normal to not feel like yourself at first or to feel sad and overwhelmed in the postpartum period. If you find yourself feeling this way for more than two weeks, speak to your healthcare provider because you could be experiencing postpartum depression.
Learning how to feed your newborn takes time and may be challenging. If you are using formula to feed your baby, discuss recommendations with your child’s pediatrician.
If breastfeeding , seek support from a lactation consultant, midwife, or healthcare provider. They can help with any breastfeeding challenges or questions. It's important for people who breastfeed to drink water throughout the day and consume an extra 500 calories daily.
When your milk first comes in, it may cause engorgement when the breasts fill with milk and feel full and tender. Frequent feedings, breast massage, and warm showers can help. See your healthcare provider if you develop a fever or chills while breastfeeding. Mastitis is a common infection in breastfeeding people and can be treated with antibiotics.
Going Back to Work
Going back to work is an emotional experience after having a baby. If possible, start planning your return to work while pregnant. Talk with your employer about any accommodations you may need, like a flexible schedule or breaks to pump breast milk.
It is also important to develop a childcare plan ahead of time. Decide if you will need to hire a babysitter or nanny or take your baby to a daycare in a home or facility.
As your return to work gets closer, practice for the big day. It may help to have a morning in which you get ready as if for work and think through any possible issues that could come up. If you are planning to continue breastfeeding after going back to work, practice with the breast pump ahead of time.
When you return to work, remember it’s normal to feel different. You have undergone changes. Try to be patient with yourself and those around you. This is a big transition, and it will take time.
Postpartum Follow-Up
It is important to continue seeing your healthcare provider after giving birth. Healthcare providers recommend checking in within three weeks of giving birth and seeing them for a visit within 12 weeks. Most people see their providers about six weeks after giving birth. About 40% of people do not attend their postpartum visit.
During your follow-up visit, your provider will ask about your physical and emotional health. They will talk with you about your mood and any symptoms you are experiencing. Your provider will likely examine your incisions if you have them and will perform a pelvic exam to determine if you have healed from birth. Talk with your provider about any concerns you have.
Resources and Support
Everyone needs support during the postpartum period. If you have friends and family members offering to help, take them up on it. If you do not have people in your life to help you, there are still resources available. These resources include:
- Postpartum: The Birth Injury Center , Centering Pregnancy/Parenting
- Breastfeeding: La Leche League , American Academy of Family Physicians
- Mental health: 988 Suicide & Crisis Lifeline (phone or text 988), National Domestic Violence Hotline , Live Another Day
- Healthy food: Women Infant Children , Cooking Matters
- Affordable housing: Volunteers of America , Catholic Charities
If a loved one recently gave birth, you may wonder how best to support them. Ways to show support include:
- Listening to their concerns
- Learning the signs of postpartum depression
- Providing rides to medical appointments
- Offering to help care for the baby
- Assisting with daily chores
The postpartum period is an intense time of life. You will likely experience several changes, both physical and emotional. It is important to focus on your health and well-being in addition to your newborn.
It is normal and expected to experience several physical symptoms like swelling, cramping, breast tenderness, constipation, and leaking milk. Emotional changes like feeling sad and overwhelmed are common, too. There are resources available to help you during the postpartum period.
MedlinePlus. Postpartum care .
American College of Obstetricians and Gynecologists. Optimizing postpartum care .
Adams YJ, Miller ML, Agbenyo JS, Ehla EE, Clinton GA. Postpartum care needs assessment: women's understanding of postpartum care, practices, barriers, and educational needs . BMC Pregnancy Childbirth . 2023;23(1):502. doi:10.1186/s12884-023-05813-0
Centers for Disease Control and Prevention. Pregnant and postpartum women .
Paladine HL, Blenning CE, Strangas Y. Postpartum care: an approach to the fourth trimester . Am Fam Physician . 2019;100(8):485-491.
Nemours Kids Health. Recovering from delivery .
Reichner CA. Insomnia and sleep deficiency in pregnancy . Obstet Med . 2015 Dec;8(4):168-71. doi:10.1177/1753495X15600572
Office on Women’s Health. Postpartum depression .
American College of Obstetricians and Gynecologists. Postpartum birth control .
Office on Women’s Health. Recovering from birth .
American College of Obstetricians and Gynecologists. Exercise after pregnancy .
Centers for Disease Control and Prevention. Partners, friends, and family of pregnant or postpartum women .
By Carrie Madormo, RN, MPH Madormo is a health writer with over a decade of experience as a registered nurse. She has worked in pediatrics, oncology, chronic pain, and public health.
- Profile & Preferences
- My Documents
Our other sites
There's a chat in progress.
The experience of giving birth

It’s a big day, 9 months in the making — your little one is ready to make their entrance. No 2 people experience labor and delivery in quite the same way, but the more you know about what to expect, the more you can focus on what really matters — the joy of meeting your new baby for the very first time.
How much will your hospital stay cost?
Get a personalized estimate based on your plan benefits. Only Kaiser Permanente members can use this secure feature, and you’ll need to be registered on kp.org.
Members: Get an estimate of how much you’ll pay to have your baby with us
*Cost calculator may not apply to members with a Medi-Cal plan.
Your labor and delivery care team
When you give birth to your baby at Kaiser Permanente, you may be surprised at how many people are there to support you — before, during, and after your delivery. They’ll all work together to help give you the happiest, healthiest birth possible.
Find out who’s in the delivery room
Planning an out-of-hospital birth?
If you’re a Kaiser Permanente member and choose not to have your baby in the hospital, let your care team know what your birth plan is. We’ll care for you during your pregnancy, help you prepare for your out-of-hospital birth, and talk about care for you and your baby after they’re born. If delivery day arrives and you need to come to the hospital after all, we’ll be here to support you through labor and delivery.
Stages of labor
It’s hard to predict exactly what your baby’s birth will be like — it’s different from pregnancy to pregnancy. But knowing what to expect can help you feel more relaxed and in control as labor progresses.
Learn what happens during labor and delivery
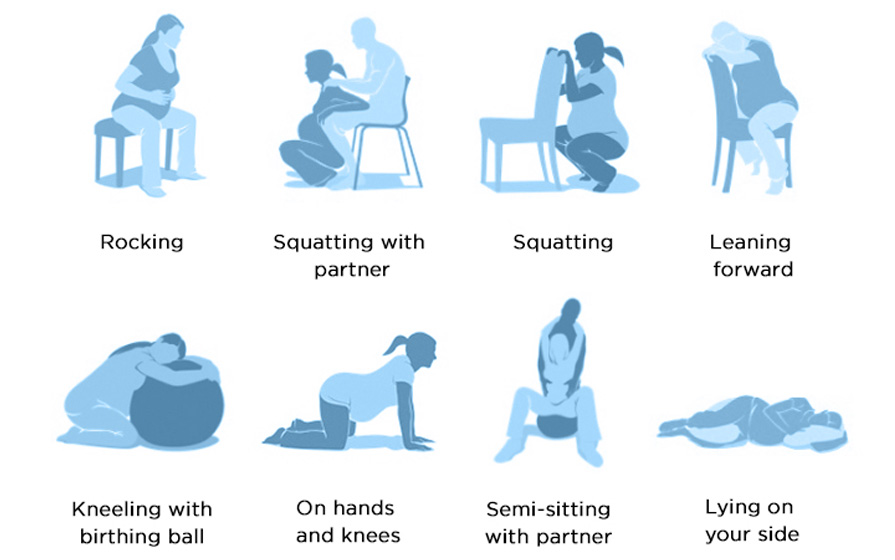
Labor and birth positions
Despite what you see on TV, most people don’t lie in bed throughout labor and delivery. Unless you have an epidural , you’re free to walk around and choose whichever position feels most comfortable to you. These common positions can help ease pressure and might even help labor progress more quickly.
Managing pain during childbirth
Pain is a normal part of labor and delivery. How you cope with it is up to you. We can help you with medication, or you can choose to manage it naturally. One of the most important reasons to make a birth plan is so everyone on your labor and delivery team knows how you want to manage pain. If you’re a Kaiser Permanente member, your care team can view all your birth plan information through your Health/Medical Record number.
But remember, you can change your mind at any time — a lot of parents do.
Learn your options for managing pain
Medical help during delivery
Most babies come into the world with very little help from us. Your labor and delivery team is primarily there to monitor you and your baby, and make sure everything progresses normally. But sometimes we do need to step in — and that’s what we’re trained to do. We even do simulation training to practice reacting to specific emergency situations. If you need extra help during delivery, knowing what to expect — and knowing that your care team is highly skilled and ready for anything — can help ease your mind.
Learn about common medical procedures during childbirth
Right after your baby is born
Right after your baby is born, we’ll check your little one’s heart rate, breathing, muscle tone, reflex response, and color. Once we make sure that you and your baby are doing well (as most new families are!), you’ll spend the first moments after delivery together. Your labor and delivery care team will be right there if you need them, but this special time is about you, your partner, and your new baby.
Skin-to-skin contact
During the first hour after birth, most babies are alert and curious. Holding your baby against your chest, skin-to-skin with no blankets or clothing in between, is a wonderful way to help your baby transition from life inside the womb to life in the outside world. Skin-to-skin contact after birth triggers healthy baby behaviors, helping your little one stay warm on their own, breathe on their own, and learn to nurse. It also helps your baby stay calm and cry less as they adjust to so many new sights, sounds, feelings, and experiences.
You’ll benefit from skin-to-skin contact, too. It helps your body produce breast milk, speeds up recovery time, and increases your level of maternal oxytocin — a hormone that promotes nurturing and bonding.
Breastfeeding for the first time
All babies are born with a natural instinct to search for the nipple. Many want to nurse right after birth, but others wait a little longer. We encourage you to try to breastfeed right away, because it helps the uterus contract and reduces bleeding.
Your labor and delivery nurse can help you get into the right position to breastfeed your baby, and let you know when your little one is latched on properly. After the first hour or 2 of bonding, nursing, holding, and gazing at your beautiful baby, you’ll probably both be ready to rest and sleep.

Did you know?
We’re big believers in the benefits of breastfeeding. That’s why we offer classes , 1 lactation consultants, and breastfeeding support for members during pregnancy, at the hospital, and after you and your baby go home.
74.5% of babies born at Kaiser Permanente are exclusively breastfed. For babies born at other hospitals, the national average is 51.5%. 2
Care for you after delivery
We’ll give you and your baby as much bonding time as possible, but we’ll be in to check on you both from time to time. We’ll also need to come into your room to:
- Cover you with a warm blanket. Shaking and chills are common after delivery.
- Rub your lower abdomen to help tighten your uterus and stop bleeding.
- Help you empty your bladder.
- Repair any tears or incisions if you tore or had an episiotomy.
- Remove the tube from your back if you had an epidural.
Ready to get maternity care? Find a hospital or care provider near you.
YOU MIGHT ALSO LIKE

1 Some classes may require a fee.
2 The Joint Commission, October 2018–September 2019.
When to call us
Symptoms you shouldn't ignore and how to get in touch with us
Switching to {{aocRegion}}
Want to stay signed on?
We are unable to switch you to this area of care
We’re getting your information
Appointments at Mayo Clinic
- Labor and delivery, postpartum care
Postpartum complications: What you need to know
After you give birth, you're likely focused on the care that your baby needs. But health problems can happen to you in the weeks and months after childbirth. They are called postpartum complications.
Some of these problems can be life-threatening. A pregnancy-related death is the death of a person while pregnant or within one year of the end of a pregnancy. More than half of pregnancy-related deaths happen after a baby is born.
In recent decades in the U.S., there has been a large rise in pregnancy-related deaths. Black, American Indian and Alaska Native people are 2 to 3 times more likely to die of pregnancy-related causes than are white people. More than 60% of pregnancy-related deaths are thought to be preventable.
Why some problems may be overlooked
After childbirth, it's common to feel tired and have some pain. It also is common to deal with lack of sleep, changing hormones and breastfeeding concerns.
You might not know what's typical for recovery after childbirth or what symptoms may signal a problem. And you may not know when to seek medical care.
If you give birth in a hospital, your healthcare team might not find risk factors for postpartum complications before you leave the hospital.
People often don't see a healthcare professional until 4 to 6 weeks after childbirth. As many as 40% of people don't have an appointment with their healthcare team at all for a checkup after giving birth. Not being able to visit a healthcare professional and not having insurance to cover the cost are two reasons why that visit might not happen. As a result, many people get little or no guidance on recovery after giving birth.
Common postpartum complications
According to the Centers for Disease Control and Prevention (CDC), common causes of pregnancy-related deaths are:
- Diseases that affect the heart and blood vessels, called cardiovascular diseases.
- Other medical conditions often present before childbirth.
- A serious infection such as sepsis.
- Heavy bleeding after giving birth, called hemorrhage.
- A disease of the heart muscle called cardiomyopathy. This condition makes it hard for the heart to pump blood to the rest of the body.
- A blockage in one of the blood vessels in the lungs that carry blood from the heart to the lungs. Blood clots that travel to the lungs from the legs, called thrombotic pulmonary embolism, often are the cause of the blockage.
- High blood pressure, called hypertension, or high blood pressure linked with protein spilled into the urine during pregnancy, called preeclampsia.
- A rare condition that happens when the fluid that surrounds the baby during pregnancy, called amniotic fluid, or fetal material such as fetal cells enters a pregnant person's bloodstream. This is called amniotic fluid embolism.
- Problems with the medicines used to prevent pain during delivery or surgery, called anesthetic.
Sometimes the cause of a pregnancy-related death is not known.
Risk factors
The overall risk of dying of a pregnancy-related complication is low. But people with chronic conditions such as heart disease, obesity or high blood pressure are at greater risk of dying of pregnancy-related complications. If you have these risk factors, take extra care of your health after giving birth.
Warning signs
Many postpartum complications can be treated if found early.
Seek emergency medical care if you have:
- Chest pain.
- Trouble breathing or shortness of breath.
- Extreme tiredness that doesn't get better with rest.
- Thoughts of hurting yourself or your baby.
Call your healthcare professional if you have:
- Bleeding that soaks through more than one pad an hour or passing blood clots the size of an egg or bigger.
- A cut from surgery, also called an incision, that isn't healing.
- A leg that has changed color or swells and is painful or warm to the touch.
- A temperature of 100.4 degrees Fahrenheit (38 degrees Celsius) or higher.
- A headache that doesn't get better even after taking medicine, or a bad headache with vision changes.
- More than one blood pressure reading of 150/100 or greater if you're measuring your blood pressure at home after giving birth.
How to prevent postpartum problems
Your health should be one of your main concerns after childbirth. Start thinking about your postpartum care plan before you give birth. Talk with your healthcare professional about that plan.
After childbirth, talk to your healthcare professional about your risk of a pregnancy-related complication. Your risk might be higher if you had a problem during pregnancy such as gestational diabetes or high blood pressure. Your risk also may be higher if you had a cesarean birth. Ask about special care you may need. Learn the symptoms of problems that you could have.
The American College of Obstetricians and Gynecologists says to make postpartum care an ongoing process rather than a single visit after you give birth. Have contact with your healthcare professional by phone or in person within three weeks of delivery. Within 12 weeks of delivery, see your healthcare professional for a complete checkup.
If you have trouble making time for an appointment, contact your care team and ask about your options. If possible, ask a family member or friend for help with child care while you go to your appointment.
During the appointment, your healthcare professional checks your mood and emotional well-being. You can talk about birth control and how long to wait before getting pregnant again. You can review information about your baby's care and feeding. Tell your healthcare professional about your sleep habits and talk about any concerns you may have about being too tired.
The physical exam might include a check of your breasts, belly, vagina, cervix and uterus to make sure you're healing well. This is a good time to talk about any concerns you have. That may include when you can start having sex again and getting used to life with a new baby.
Also, when you see anyone on your healthcare team in the year after childbirth, tell them when you gave birth. This can help your care team know whether any symptoms you have might be linked to pregnancy.
- Postpartum care for women up to one year after pregnancy. Agency for Healthcare Research and Quality Effective Health Care Program. https://effectivehealthcare.ahrq.gov/products/postpartum-care-one-year/protocol. Accessed Dec. 11, 2023.
- American College of Obstetricians and Gynecologists. Committee Opinion No. 736: Optimizing postpartum care. Obstetrics & Gynecology. 2018; doi:10.1097/AOG.0000000000002628.
- Pregnancy-related deaths in the United States: Most pregnancy-related deaths are preventable. Centers for Disease Control and Prevention. https://www.cdc.gov/hearher/pregnancy-related-deaths/. Accessed Dec. 11, 2023.
- You know your body best. Centers for Disease Control and Prevention. https://www.cdc.gov/hearher/pregnant-postpartum-women/index.html.Accessed Dec. 11, 2023.
- Pregnancy mortality surveillance system. Centers for Disease Control and Prevention. https://www.cdc.gov/reproductivehealth/maternal-mortality/pregnancy-mortality-surveillance-system.htm. Accessed Dec. 12, 2023.
- Expert view: 5 reasons why you need a postpartum support network. American College of Obstetricians and Gynecologists. https://www.acog.org/womens-health/experts-and-stories/the-latest/5-reasons-why-you-need-a-postpartum-support-network. Accessed Dec. 11, 2023.
Products and Services
- Available Solutions for Postpartum from Mayo Clinic Store
- A Book: Obstetricks
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- Breastfeeding and medications
- Breastfeeding nutrition: Tips for moms
- C-section recovery
- Eating the placenta
- Exercise after pregnancy
- Kegel exercises
- Postpartum care: After a vaginal delivery
- Postpartum depression
- Pregnancy and breastfeeding when you have psoriasis
- Sex after pregnancy: Set your own timeline
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Postpartum complications What you need to know
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Search Please fill out this field.
- Newsletters
- Sweepstakes
- Postpartum & New Parenthood
Postpartum Timeline: What You Can Do When After Giving Birth
Wondering what you'll be able to do after the baby makes their grand arrival? Consider this your ultimate postpartum timeline.
Why Do Activities Need to Be Limited Postpartum?
- Immediately After Delivery
- Hours After Delivery
- One Day After Delivery
- One Week After Delivery
- Two Weeks After Delivery
- Three Weeks After Delivery
- Six Weeks After Delivery
While everyone's postpartum experience is unique, the post-delivery recovery timeline is usually fairly predictable. For example, it's always advised to avoid housework, heavy lifting, and other strenuous physical activity immediately after giving birth and during those first days and weeks postpartum. However, some new parents will need a bit more or less time to be ready for various activities like having sex, driving, or starting to take on regular household work after delivery.
You'll be sore, tired, and recovering right after the birth, so aim to ease into your new routine with help from family and friends. Prepare to limit trips up and down the stairs, hold off on doing extensive household chores, and wait to exercise until you've gotten the go-ahead from your doctor. Learn more about what you can do when after giving birth.
GETTY IMAGEs
The postpartum period is sometimes referred to as the " fourth trimester ." This is because it is a time of recovery and adjustment to parenthood. "You need sufficient rest for the muscles and ligaments that hold your uterus in place to regain their strength," says Coralie Macqueen, a certified nurse-midwife in private practice in New York City. And in the case of a C-section, a longer period of rest is required for your body to heal from major abdominal surgery.
Most importantly, be gentle and flexible with yourself. Your body is unlikely to snap right back to its pre-pregnancy state. And the emotional whirlwind of new parenthood needs to be processed as well. So, honor when you feel like you need rest and/or to postpone certain things until you're feeling ready. In other words, focus on caring for yourself and your baby and err on the side of slowly easing back into regular life—you don't need to do it all!
As for the specifics? After your baby's born, here's when you can expect to get the green light for nursing, showering, driving, doing household work, and more during your postpartum recovery.
What Can You Do Immediately After Delivery?
If you're feeling up for it, you can likely do the following activities right after giving birth.
Hold your baby
As long as you've had an uncomplicated birth and you're feeling up to it, you'll be able to hold your baby immediately after giving birth. If you've had a C-section birth , your partner might actually be the one holding baby, but you'll still get a chance to steal some snuggles while you get stitched up and prepped for the recovery room.
Breastfeed your baby
While you're enjoying those first sweet snuggles with your baby, if you plan to breastfeed , it's time to try breastfeeding for the first time. Your first milk will be colostrum, also known as first milk ; this nutrient-dense milk is packed with antioxidants and antibodies designed to support your newborn and build up their immune system. The first hours after birth is a critical time for establishing a breastfeeding bond . If you choose to use formula, you can feed your baby with a bottle.
Are you wondering how soon you can walk after giving birth? If so, know that the answer varies greatly depending on the type of pain medication you opted for. If you deliver without the use of an epidural , you'll likely be able to walk immediately. If you've used an epidural , it generally takes an hour or so before you'll be able to fully feel your legs, says Dr. Martine Tesone, a Certified Nurse Midwife specialist in Loveland, Colorado.
If you've had a C-section , however, you will need to stay in bed a few hours longer or even wait until the day following your surgery. Walking—at least to the bathroom and back, and possibly farther—shortly after a C-section is encouraged as it helps circulation, improves bowel function, and will speed recovery .
What Can You Do Hours After Delivery?
While you'll want to focus on resting and bonding with your newborn, after a few hours, you'll be able to start doing some additional self-care activities.
Take a shower
Once your epidural wears off and the baby's been checked over thoroughly, you'll likely be transported together from the delivery room to the postpartum recovery room. This is often on a different floor of the maternity ward, and the nursery is typically on this floor as well. Here, you'll be able to enjoy your first postpartum shower. (Just gently pat yourself dry down there!)
Nandini Raghuraman , M.D., MSCI, an OB-GYN at The Women & Infants Center, Washington University School of Medicine in St. Louis, says, "This can even be done the day of your delivery if you feel okay standing independently without dizziness or lightheadedness." If you had a C-section, you can typically shower within a day of your surgery; doing so helps reduce the risk of infection. Don't scrub your incision; just let the water run over it.
Use the bathroom on your own
Your first trip to the restroom after giving birth may be a bit more awkward (and uncomfortable) than you expected. That's because you'll be accompanied by your attending nurse, who will ensure you're steady on your feet, help navigate cords, wires, and your hospital gown, and help you get set up with your first postpartum pad and ice pack. This typically happens as soon as your epidural wears off if you had one, or about one to two hours after giving birth.
Following a C-section, however, your first bathroom trip will generally be the morning after your surgery when doctors remove your catheter.
Note that constipation is common after childbirth . Drinking a lot of liquids, moving your body as much as possible (try walking the hospital hallways!), and constipation medication can all help.
Drink alcohol (yes, really)
Hoping to toast your new arrival with a sip of bubbly at the hospital? Go for it, but it's a good idea to wait until after you and your baby have been checked over, and you've tried breastfeeding for the first time. Even then, it's recommended you keep the celebration to one small glass . Dr. Heather Bartos , M.D., an OB-GYN and the founder of Badass Women, Badass Health reminds us that if you're taking narcotics for pain relief, you shouldn't use alcohol at all.
What Can You Do One Day After Delivery?
You will likely be feeling mighty sore and tired but you can still start doing a few more things one day postpartum.

Take a bath (with the doctor's okay)
If you've had an uncomplicated vaginal delivery, there's a good chance you'll get the all-clear to take a warm bath just one day postpartum. But if you're a c-section parent, this luxury will, unfortunately, be off-limits for several weeks to come. "After a cesarean section, you may be advised to wait until after your six-week postpartum visit before taking a full bath," says Dr. Tesone. However, showering is still an option.
Leave the hospital
Unless you've had a C-section, you should be able to leave the hospital approximately 24 hours after giving birth, assuming both you and your baby have been cleared by your doctors. The C-section recovery timeline has you staying for approximately two to four days.
What Can You Do One Week After Delivery?
After a week, you'll be feeling much more like yourself, but you've still got a lot of healing to go. However, there are new things you can resume doing.
Drive a car
Wait a week to drive a car after a vaginal birth, says Robert Atlas , M.D., an OB-GYN at Mercy Medical Center in Baltimore. "You use your abs to move your foot from the gas to the brake." If you've had a C-section, expect to wait two to three weeks before getting behind the wheel.
"After a C-section, you won't be able to lift anything more than your baby's weight, so lifting a car seat is not feasible," says Dr. Tesone. "In addition, you won't have the abdominal muscles to press down on the brake pedal in an emergency."
Care for other children
If you can swing it, it's best to wait until at least one week postpartum before resuming full-time childcare duties for your other kids. This allows you time to heal, establish a feeding routine, and promote bonding time with your new baby.
What Can You Do Two Weeks After Delivery?
After 2 weeks, you'll be feeling a lot better but your body is still healing. Be sure to stay well-fed and get as much rest and support as you can. Accept help when offered and ask for assistance when needed!
Resume light exercise
If you haven't already and you're feeling up for it, you should be able to resume a light workout schedule —think walks and stretches—about two weeks postpartum. Just remember to take it slow and avoid trying new or intense workouts right now.
Take on light household chores
Similarly, you should be able to resume day-to-day tasks around the house without much trouble around two weeks after delivery. "But always listen to your body," notes Dr. Raghuraman. "If there is any discomfort, immediately stop and rest."
However, if you've had a C-section , the 2-week mark will be the time you'll go back to the doctor for a wound check to make sure your incision is healing well. Only after this will your doctor clear you for any increased activity. So, hold off on doing the dishes or laundry if you can!
What Can You Do Three Weeks After Delivery?
After three weeks postpartum, you can start resuming many of your normal activities. However, it's still important to take it easy.
Expect less bleeding
Wondering if you'll ever stop bleeding? Dr. Bartos says most people start to see a much lighter flow by the end of the third week. However, it's not abnormal to go a few weeks longer than that or even for the flow to trickle off and start up again a few times.
Take on more household work
By three weeks, you can start doing more household work. However, don't overdo it. Instead, lean on your support system as much as possible. Listen to your body and if you need a break, take one!
What Can You Do Six Weeks After Delivery?
While you're likely still adjusting to the 24-hour demands of parenting, by six weeks postpartum your body's physical recovery from pregnancy and delivery is typically in good shape. So, you'll likely get the go-ahead from your doctor to resume most activities.
Enjoy sexual activity
At your 6-week postpartum doctor's visit, you'll likely be cleared for sexual activity . But don't sweat it if you're not in the mood yet. You're in control here, and just because you've reached this milestone doesn't mean you need to be intimate again right away. However, if you feel ready, go for it! Everyone's situation is different, so you get to you decide when you feel truly ready. And remember, you can start slow, and "sex" doesn't have to include penetration!
Start taking birth control again
You're potentially fertile even with a newborn in your arms, even if you're breastfeeding, so be sure to use birth control. Talk to your healthcare provider about the best pill to take if you're breastfeeding . Since your breastfeeding routine is likely well established by now, it's safe to start taking a mini-pill at six weeks postpartum, which is a progesterone-only form of birth control. The mini pill is effective at preventing pregnancy without causing your milk supply to suffer.
Do Kegel exercises
We know there are surely many other priorities on your to-do list as a new parent, but there's no time like the present to start working on those pelvic floor muscles . But it's advisable to wait until the 6-week mark to ensure that any vaginal tears/repairs have fully healed, says Dr. Raghuraman.
Going to the gym
Whether you delivered vaginally or by C-section, skip intense gym workouts for six weeks to give your body time to finish most of its healing. While it may not seem like it right now, you will get back to your pre-baby and pre-pregnancy exercise routines (if that's your goal), so there is no need to rush things. Take it slow.
Key Takeaways
While there are general guidelines on what you can do when postpartum, remember that each new parent recovers from childbirth on their own timeline. So, listen to your doctor and your body—and go at whatever pace feels right to you.
Listen to Parents' "That New Mom Life" podcast for expert advice on breastfeeding, the emotional highs and lows of parenthood, sleepless nights, and more!
Related Articles
Help Me, Heidi! How Do I Tell My Mother-in-Law She Can't Be the First to Come Visit Our New Baby?
Latest update:, “i’m currently fighting with my mother-in-law about when the best time to visit our new baby will be — and did i mention baby j hasn’t even made his appearance yet she finally admitted she was upset about not being invited to his birth, but i don't feel like being a host to my mother, grandmother, and mil after having a baby, and nobody wants to get a hotel room. any suggestion for this first-time mama before i cave and let everyone just do what they want” ~ mikala h, get to know your newborn baby.
Help Me, Heidi! is a weekly advice column in which What to Expect creator Heidi Murkoff answers your most pressing pregnancy and parenting questions. She’s tackling the stuff you are desperate to know right now — so if you have a question, ask Heidi here or on Facebook and she might answer in an upcoming column. (Not sure if Heidi's answered one of your questions? Check out the rest of the columns here .)
Trending On What to Expect
How to keep your house clean and healthy for your baby and your family, spacing your kids: the pros & cons of every age gap, ⚠️ you can't see this cool content because you have ad block enabled., how to make — and keep — a family budget, different types of parenting styles, how to earn money as a stay-at-home mom.
- EXPLORE Random Article
How to Deal with Visitors After Giving Birth
Last Updated: September 13, 2022 References
This article was co-authored by Jami Yaeger . Jami Yaeger is a Parenting Specialist, Doula, and the Owner of AustinBorn, an online community offering comprehensive and modern education to growing families. With 10 years of experience, Jami specializes in whole family support for pregnancy, birth, postpartum, and parenting. Jami earned her BA in Theatre Performance from San Diego State University and earned her Certification as a Lactation Education Counselor from the University of California, San Diego. She is a Certified Infant and Child CPR Instructor, Birth and Postpartum Doula, and Childbirth Educator. There are 8 references cited in this article, which can be found at the bottom of the page. This article has been viewed 17,162 times.
Congratulations! You may have or soon expect a new baby. You’re probably pretty excited about the new member of your family. Chances are that other family members and friends are just as happy. [1] X Trustworthy Source HealthyChildren.org Health information from the American Academy of Pediatrics. Go to source It’s not uncommon for people to want to meet your baby as soon as possible. In some cases, they may want to visit you shortly after birth. But childbirth and getting used to a new baby can overwhelm you and visitors may add to this feeling. You can deal with visitors after giving birth by planning your wishes in advance and accommodating your needs both in the hospital and at home.
Planning Your Wishes with Visitors in Advance

- Make a list of people whom you’d like as visitors and those who can wait a bit. For example, you may only want your parents or siblings to visit in the first few weeks. You may also feel comfortable inviting other friends or even colleagues to visit you in the hospital or at home.
- Develop a couple of different contingencies for visitors that don’t put stress on you or them. Ask yourself questions such as, “What do I do if there are complications?,” “What if I don’t feel like visitors after giving birth?,” or, “Is this person going to cause me stress?”

- Spread out your guests as much as possible. The key is to make visits as stress-free as possible and it’s generally easier to handle 1-2 people than a group. [3] X Research source
- Make a schedule of potential visits. You probably want the people closest to you to see you and your new baby first. Put them on your schedule either on your delivery day or a day or two afterward. Then spread out visits every couple of days to let yourself rest and deal with potential complications.

- Use conversations about the baby as a way to inform people of your wishes. For example, “Aw, Christopher and I really excited to have you meet the baby, too. Since this is our first, we’re going to wait a few days to see people so we can settle into our new life. I’ll text you as soon as we’re ready to see you.” You might also say, “We decided to do a home birth and are excited to have people see us and meet the baby. I’ll let you know when Sara goes into labor and feel free to stop by whenever you like.”
- Be honest with people, knowing that most will understand and respect your wishes. For example, “Mom, this has been a really difficult pregnancy and I’m really worried about this baby’s health. I think it’s easiest if I let you know when it’s born and then figure out the best time to visit from there.”

- Use a website such as Take Them a Meal or Meal Train to set up your meal train. This gives you a chance to organize when people come over and visit with your baby. [5] X Research source It can also ensure you get food you like and prevent unexpected knocks at the door.
Accommodating Visitors When They’re With You

- Inform scheduled or other potential visitors that you’re not ready to see them. You don’t have to provide extensive details. A simple, “Hey Sam, I am really looking forward to seeing you and introducing Ellie, but we’re really exhausted today after the C-section. I’ll let you know when we’re ready for a visit. I’m so sorry to break our plans.”
- Bringing food, coffee, or beverages for your family
- Helping with laundry
- Doing dishes
- Taking the dog out

- Set aside on comfortable, clean outfit for guests you don’t want to visit with in pajamas. You can also throw on a cardigan over pajamas or dirty clothes.
- Keep a stash of cosmetics or other beauty products within reach if you want to freshen up.
- Host people in one room and close the doors to others you don’t want them to see. Stash dirty laundry under the bed or in closets if you like.
- Avoid feeling the need to apologize for not cleaning, showering, or offering guests something to eat or drink. Visitors are often there because they love you and want to meet the baby.

- Let friends and family with children know you would like them to visit without their children because your baby doesn’t have their vaccinations. Set up an alternative time after your baby has had their first round of shots.
- Recognize that small children have a lot of energy and may be loud. They can also be curious and get into things in your home you don’t want others to see.

- ”Hey there, Peg, thanks for stopping by! Come on in and see the baby. Unfortunately, I’m going to have to cut out to feed Felix at 2:30, but we’d love to see you until then.”
- ”It’s been really wonderful to see you, Bob. It’s time for Charlotte’s feeding and I want to help out Sara with it. Let’s try and get together sometime soon.”
- ”Alexander just put down Eloise. I usually take a nap with her, so I’m going to sneak away now.”
Dealing with Unwanted Visitors

- Empathize with people’s excitement and remember they’re trying to share in your joy. Stay as positive as you can, even if you’re surprised. An, “Oh, Teresa, how lovely to see you, I wasn’t expecting anyone,” is much better than, “Teresa, please leave.”
- Gently cue people to leave if you are tired or not ready to see anyone. You can simply say, “Thank you so much for coming over, Mrs. Newman, but I was just about to feed Jack and put him down for a nap. Maybe you could stop by later this week?”
- Avoid apologizing for yourself if you want to see people but may not feel presentable. Instead, try saying, “Hey Molly, it’s so great to see you! Anna and I weren’t expecting guests but would love to introduce you to Max—and the tornado of laundry he creates!”

- Say, “Oh, jeez, where did the time go? I’m unfortunately going to have to leave because it’s Annie’s feeding and naptime. I really like to keep it a consistent routine at home.”

- Have a diplomatic conversation with a person if you are on relatively good terms. For example, “Peg, it would be better if you visited in a few weeks or months. We’re still getting used to having a baby and want to limit visitors as much as we can so we can establish a routine.”
- Enlist the help of your partner, a relative, or close friend if you don’t have a good relationship to the visitor. Ask them to explain to the person your feelings. For example, “Sam, my mom is at the door and I’m sure she wants to see the baby. I just don’t want her to meet our baby after how she’s treated me,” or, “Allie, can you please tell Cat to just stay away? We’re not friends any longer and the baby doesn’t change my feelings.”
Expert Q&A

You Might Also Like

- ↑ https://www.healthychildren.org/English/ages-stages/prenatal/delivery-beyond/Pages/Bringing-Baby-Home.aspx
- ↑ http://www.whattoexpect.com/pregnancy/visitors-hospital-birthing-center/
- ↑ http://www.parents.com/baby/care/newborn/managing-baby-visitors/
- ↑ https://www.mealtrain.com/
- ↑ Jami Yaeger. Parenting Specialist. Expert Interview. 29 September 2020.
- ↑ http://www.parkslopeparents.com/Nesting-and-Preparation/tips-for-maging-the-family-before-during-after-giving-birth.html
About this article

Did this article help you?

- About wikiHow
- Terms of Use
- Privacy Policy
- Do Not Sell or Share My Info
- Not Selling Info

New mom refuses to visit MIL after she body-shames her, 'I didn't think she would be so mean.' AITA?
"aita for refusing to visit my mil after she body-shamed me following the birth of my baby".
I (26f) and my husband (26m) just welcomed our first baby a few months ago. Him and I are overjoyed and I am so in love with our tiny bundle. My family has been super supportive, bringing us dinners and making sure we had time for napping while we adjusted to parent life.
My husband’s family is different from mine in a lot of ways. They didn’t want to visit us and only wanted us to come to them (they live about 20 minutes away) and didn’t really care to offer much for support following the birth. We were fine with it and brought our baby over when we were able to - around 3 times a month.
After the first month, my MIL began commenting about how much she prioritized “losing the baby weight” after she had her first baby. At first I didn’t think anything of it, I thought she was just voicing her experience as many people do when they are around babies. She then started commenting on my baby's chubby cheeks, and how similar they are to mine.
I felt a bit hurt but let it slide once again. The final straw was when my husband was talking to her casually about my wanting to start going on runs again and how we were planning on making it work since our baby is very attached to me.
She very loudly said “you’re thinking about trying to run? Shouldn’t you start with walking?” His whole family was in the room and looked at me waiting for my answer. I am an avid runner who only stopped due to my pregnancy, and her comment really hurt. When I was a teenager I had really bad body issues, one that I am still struggling with. Comments on my body or physical abilities are hurtful to hear, and she is someone who I knew talked about peoples bodies behind their backs, but I didn’t think she would be so mean to my face. I am not skinny by any means, but live a healthy and active lifestyle so weight should not be my concern.
This is where I feel like the ahole. I don’t want to see her anymore. She makes me feel like crap about myself and my husband is backing me up 100%. His mom is angry because she thinks we are just keeping her grandchild away from her and believes it is unfair. He goes there without me but it is difficult to take our baby because she is exclusively breastfed and refuses bottles of any kind. AITA?
EDIT: After reading the first few comments I realize that I left out some info. I am currently 5 months postpartum and have been fully cleared by my doctor to begin my running regiment.
Here's what top commenters had to say about this one:
tessherelurkingnow said:
NTA. Commenting on the weight of someone who just had a baby is an incredible ahole move, no one asked her.
Charlie_Parkers_Mood said:
NTA. There's nothing wrong with not wanting to waste your time around people who only want to tear you down.
mochafiend said:
NTA at all. Glad your husband is backing you. That seems to so rarely happen in these cases.
esmerelofchaos said:
NTA. Your in laws definitely suck. I’d be all “nah, I’d rather run my body. It’s so much better for everyone than just running my mouth about what other people are doing.” And then just smile.
cayjay00 said:
NTA. Protect your peace. Your husband can visit MIL without the kid, and MIL can feel the weight of FAFO consequences (sorry boutcha). Assuming “a few months ago” is in the 2-4 month range, you’re still healing, your hormones are not even close to “back to normal,” your kid is breastfed.
But irrespective of time range, you have enough on your plate without dealing with some ahole who can’t hold her tongue (or just, you know, be a decent human). MIL is husband’s problem to manage. Call it dad duty…one he’ll have to take on for a good while. Unless y’all go no contact, that is.
gezeitenspinne said:
NTA. But honestly, I think your husband shouldn't visit her either. Let her make an actual effort before she gets any contact. Especially as there will be a time when he'll be able to bring the kid. And she'll sure as hell do the same thing to your child.
Everyone was on OP's side for this one. What's your advice for this situation?
- WEATHER ALERT Coastal Flood Advisory Full Story
- ABC7 New York 24/7 Eyewitness News Stream Watch Now
- THE LOOP | NYC Weather and Traffic Cams Watch Now
Rutgers doctoral student gives birth on same day she defends dissertation

NEW JERSEY (WABC) -- This Mother's Day will be especially poignant for a New Jersey woman who will not only celebrate being a mom, but also becoming a doctor.
Tamiah Brevard-Rodriguez was working on her doctoral dissertation presentation from Rutgers when she went into labor on March 25.
She was only eight months pregnant and was scheduled to deliver her dissertation defense that day.
"I was physically prepared for a pregnancy, mentally my brain was not on a baby," she said. "So I was having a very emotional response to knowing I was in labor, knowing I had this defense. I was literally shaking."
She had everything planned out with staff and faculty at Rutgers to examine standards Black women face on historically white college campuses.
But things went off schedule when her water broke. Brevard-Rodriguez's wife rushed to their car after their doula told them to get moving as contractions increased.
The drive on the Garden State Parkway to the hospital was a race against time.
"The doula is trying to tell me don't grunt him out, just breathe and I'm like 'this baby is coming,'" Brevard-Rodriguez said.
At that point, her wife, Alyza Brevard-Rodriguez, said she was probably driving 120 mph on the highway.
"I had three pushes, so the first one was baby's head was crowning, second push he was out, third one we were just there," Brevard-Rodriguez said.
Once at the hospital, baby Enzo was checked out and all was well.
But since Tamiah was well-rehearsed for the dissertation, she delivered her defense about seven hours after Enzo came into the world.
"I was like, I think I could do it, I was prepared for it, what did I do, some final touches on it and I did the study," she said.
She said all she needed was a nap, a shower and to regroup.
No one knew about the delivery until after the successful defense was complete.
So she delivered a baby and became a doctor on the same very special day.
Sunday is not only Mother's Day, it is also her graduation ceremony.
ALSO READ | Comedian Tracy Morgan pays special visit to cancer patient and lifelong fan

* Get Eyewitness News Delivered
* More New Jersey news
* Send us a news tip
* Download the abc7NY app for breaking news alerts
* Follow us on YouTube
Submit a tip or story idea to Eyewitness News
Have a breaking news tip or an idea for a story we should cover? Send it to Eyewitness News using the form below. If attaching a video or photo, terms of use apply.
Related Topics
- FAMILY & PARENTING
- RUTGERS UNIVERSITY
- BABY DELIVERY

Mother gives birth, defends PhD dissertation on same day

Woman wins half marathon while 23 weeks pregnant

Carli Lloyd announces she and her husband are expecting a baby

Ashanti and Nelly are engaged and expecting a baby
Top stories.

New NYC pay-by-plate parking meters bid farewell to paper receipts

16-year-old shot, killed in SoHo; suspect takes off on Citi Bike

Streamer Kai Cenat won't be prosecuted for role in Union Square riot

Truck driver speaks out after surviving I-95 tanker fire in Norwalk

Man accused of stealing $300K worth of jewelry caught on camera
AccuWeather: Showers to warm sun
Rangers beat the Hurricanes 4-3 in double overtime
Trump trial updates: Judge denies mistrial over Daniels' testimony
Family delivers baby at Lowe’s with help of law enforcement
GALAX, Va. (WDBJ) - Daisy Musser was on the way to a hospital with her husband Kris Musser to give birth to their baby boy Thursday night after having contractions. While they were expecting the baby to come that day, they were not expecting to deliver the baby anywhere but a hospital.
“The labor did not feel intense until we got to Walmart, which is just a block away from Lowe’s. Then, I told Kris that the baby was coming,” said Daisy.
Kris then pulled the car over in the Lowe’s parking lot, ran to the passenger seat to help his wife, and immediately dialed 911 for help.
“It was less than less than a minute after I hung up with 911. Our son was born I caught him there in the parking lot,” said Kris.
Kris said helping deliver the baby in the car was the easy part.
“Our son came into this world pretty naturally, like no real big complicating factors, but once he was born, that’s when I realized like, okay, this is where I really need some help,” said Kris.
Shortly after the delivery, their baby boy started losing his color, turning a little blue in some areas. That’s when Galax Police Officer Michael Tozollo showed up to save the day.
“He sprinted back to his car, got a blanket out, and he said, I can’t think of a better time for this. He put it on our son. Then from there, things started to take a little bit more of a positive turn,” said Kris.
When Officer Tozollo cleared the baby’s airways and more officers, along with Piper’s Gap rescue members, arrived at the parking lot, Kris had no doubts his son was going to be okay.
Kris and Daisy say they will never forget the caring officers who helped keep their baby safe.
“One thing that I would like to just take away from all this, I guess you could say is these first responders are everyday people. Like I said, they could have gone back to sleep. It was in the middle of the night. But they really are local heroes,” said Kris.
They look forward to telling their son about the story of his birth when he’s all grown up.
“It’ll be obviously something that we’ll remember for the rest of our lives and something that he will obviously be able to just tell all his friends and everybody growing up too,” said Kris.
Their baby boy has been healthy since the delivery.
Copyright 2024 WDBJ. All rights reserved.

Boy Scouts of America changing name to be more inclusive after years of woes

Man killed in Greenbrier County in officer-involved shooting

Missing Virginia 10-month-old boy found safe

Tazewell County teen opens her own bakery in Richlands

School board votes to hire armed security personnel
Latest news.

Bluefield University partners with local school system for teacher apprenticeship program

WVU Med. PCH brings pet therapy to hospital for National Nurses Week

WVU Med. PCH brings therapy dogs to hospital for National Nurses Week

More than just flowers: Fayette County greenhouse works hard to make all moms feel appreciated on Mother’s Day

Local mother and baby visit UMC to thank heroes ahead of first Mother's Day together
by News 3 Staff

LAS VEGAS (KSNV) — A local woman will be able to celebrate her first Mother's Day after a heroic action from a Las Vegas Fire and Rescue crew and UMC nurses.
Jessica Spellacy was at work when she realized her daughter was not only coming early but in an upside-down, breech position.
LVFR immediately took her to UMC. During transport, the crew found a way to ensure oxygen continued getting to the baby by holding pressure away from the umbilical cord.
READ MORE NEWS 3 | Clark County School District teachers recognized for 40 years of service
Spellacy gave birth to baby Johanna nearly one minute after she arrived at UMC.
Doctors say the heroic actions of the LVFR crew and the nurses involved in the delivery ensured both Spellacy and Johanna not only survived, but continue to thrive.
Johanna, now a healthy 3-month-old, joined UMC leadership on Tuesday to honor the heroes who saved their lives.
Grandmother arrested after 10-month-old baby tests positive for fentanyl
TIGARD, Ore. ( KPTV /Gray News) - Oregon authorities say a grandmother is facing several charges for exposing her granddaughter to drugs.
A Tigard Police Department officer reports they were patrolling a shopping plaza last Friday night when they saw an unlicensed Jeep parked and running in the parking lot.
According to the officer, the driver, later identified as 53-year-old Julia Apostello, was passed out behind the wheel with drug paraphernalia out in plain view.
A 10-month-old was also in the back seat sitting in a car seat.
The department said officers later learned that the baby was the woman’s granddaughter.
Tigard police said they spoke with the 10-month-old’s mother when she was walking back to the car.
The baby’s mother told police that she was inside a nearby business with her 4-year-old child for about 30 minutes before returning to the Jeep.
Officers said they woke Apostello up, removed the substance from the Jeep that was identified as fentanyl, and arrested her.
The 10-month-old was taken to the hospital due to concern for her safety and potential exposure to drugs. Medical personnel confirmed the child tested positive for fentanyl and she was treated at the hospital.
Tigard police said the child was released from officer supervision over the weekend, and they believe she is doing OK.
Apostello was booked into Washington County Jail on charges of criminal mistreatment, two counts of child neglect, endangering the welfare of a minor, two counts of criminal mistreatment and recklessly endangering.
“To believe a 10-month-old is around a drug like that is outrageous,” said Nick Haywood, who works in the plaza. “It’s one of the deadliest drugs out there and it doesn’t take a lot to kill someone.”
Copyright 2024 KPTV via Gray Media Group, Inc. All rights reserved.

Boy Scouts of America changing name to be more inclusive after years of woes

‘Grease’ actress who played Sandy’s cheerleading friend dies

Robeson County Sheriff’s Office rules pastor’s wife’s death as suicide

Lexington woman pleads guilty to homicide by child abuse after giving birth, leaving child in trash bag

Family of former Summerton mayor files wrongful death lawsuit following deadly crash
Latest news.

TikTok sues to block potential US ban

Police: 2 dead in downtown Charleston shooting

US soldier detained in Russia on theft charges

Officer run over by trailer during traffic stop suffers serious back injuries

Officer run over by trailer says he's thankful his injuries weren't worse
- TODAY Plaza
- Share this —

- Watch Full Episodes
- Read With Jenna
- Inspirational
- Relationships
- TODAY Table
- Newsletters
- Start TODAY
- Shop TODAY Awards
- Citi Concert Series
- Listen All Day
Follow today
More Brands
- On The Show
Mom gives birth in a restaurant and names her baby after the seafood spot
Alyse Sparkman used to read stories about babies born in unusual places and think, “That will never be me.”
Then she gave birth at a seafood restaurant.
“It was right out of a movie,” Alyse’s husband, Sean Sparkman, 35, tells TODAY.com .
On April 27, Alyse, who was 37 weeks along in her pregnancy, began experiencing consistent contractions. The Sparkmans were certain it was go time and headed to the hospital, but doctors concluded that Alyse wasn’t in active labor and sent her home.

At that point, the Sparkmans decided they would grab a light bite to eat at Lily’s Seafood Grill and Brewery in Royal Oak, Michigan. It was 75 degrees outside and they were excited to enjoy a meal on the patio.
Apparently, the couple’s unborn daughter was very eager to join them.
Alyse was still chewing her first bite of trout Caesar salad when she felt her water break. She alerted Sean to what was happening and he took off sprinting to get their car. He would have had to teleport to get back in time.
Two minutes after her water broke, Alyse had a newborn baby girl on her chest.
“I’m sitting at a light and she calls me and says, ‘I had the baby,’” Sean recalls. When Sean realized she wasn't kidding, he felt his heart sink.
"I was like, ‘Oh no, I can’t believe I missed it. I feel so bad,'" Sean recalls. "She goes, ‘Don’t feel bad — just get here!’”

In a stroke of luck, the Sparkmans were seated next to two retired nurses, who were able to untangle the baby’s umbilical cord, which was wrapped around her neck.
"She came out purple," Alyse says.
After the baby let out her first cry, fellow diners erupted into cheers and applause.
“God is good,” the Sparkmans say in unison.
The Sparkmans gave their daughter Penelope the middle name Lily in honor of where she made her entrance into the world.
“It really worked out because we had originally chosen Danielle, but we weren’t crazy about it,” Sean says. “We both love Lily.”
Penelope, who weighed 4 pounds, 8 ounces, at birth, was discharged from the hospital two days later alongside her mom. Penelope joined brothers Logan, 5, and Quill, 3.
The restaurant will be placing a plaque dedicated to Penelope Lily at the table where she was born — a gesture that Sean calls "pretty cool."
Rachel Paula Abrahamson is a lifestyle reporter who writes for the parenting, health and shop verticals. Her bylines have appeared in The New York Times, Good Housekeeping, Redbook, and elsewhere. Rachel lives in the Boston area with her husband and their two daughters. Follow her on Instagram .
No charges for woman after bodies of 4 babies are found in Boston freezer

No charges will be filed against a 69-year-old woman after the bodies of four frozen infants were found in a Boston apartment freezer in 2022, the Suffolk County district attorney announced this week.
District Attorney Kevin Hayden called the investigation into the circumstances of the grim discovery on Nov. 17, 2022, “one of the most complex, unusual and perplexing that this office has ever encountered.”
Investigators don’t know whether the four babies were born alive, which in part led to the decision not to bring criminal charges, Hayden said in a statement Tuesday.
The babies were found in a freezer in an apartment in South Boston after a man called police and said his wife found them while she was cleaning out the apartment of the man’s sister, the district attorney’s office said.
The babies, two male and two female, were frozen solid in shoe boxes wrapped in foil, the prosecutor’s office said. DNA tests showed they were all siblings.
The medical examiner could not determine the cause of death or whether the babies were born alive — and there was no obvious trauma visible, the district attorney’s office said. The babies’ father, confirmed by DNA tests, died in 2011.
The mother is in a health-care facility and when investigators questioned her she “appeared confused and demonstrated a lack of understanding about where she was and who she was speaking to,” Hayden said in the statement.
“We will never know if the four babies were born alive, and we will never know exactly what happened to them,” he said, or why the woman concealed the pregnancies.
Investigators determined the woman had five children with the babies’ father, one of which was put up for adoption, Hayden said. The only birth record found was for the birth of one child, he said.
Phil Helsel is a reporter for NBC News.

IMAGES
VIDEO
COMMENTS
Vaginal discharge. After delivery, a mix of blood, mucus and tissue from the uterus comes out of the vagina. This is called discharge. The discharge changes color and lessens over 4 to 6 weeks after a baby is born. It starts bright red, then turns darker red. After that, it usually turns yellow or white.
Your postpartum checkup. Your six-week postpartum checkup is a comprehensive visit with your OB or midwife to check on your recovery after childbirth. You'll have a complete examination, including a mental health screening and any tests or immunizations you need. If all is well, you'll get the okay to start exercising and having sex again.
During your postpartum checkup, your ob-gyn should explain the kind of ongoing care you may need for any medical problems and help you connect with health care professionals who can provide it. Ideally, you can have several postpartum checkups. Postpartum checkups used to always be limited to one visit, 4 to 6 weeks after birth.
The postpartum checkups are a time to discuss how you're healing and adapting to motherhood. During the visit, your doctor will check on several aspects of your physical and emotional recovery. According to the ACOG, it will also cover infant care and feeding, family planning, sleep and fatigue, chronic disease management and health maintenance.
What is a postpartum checkup? A postpartum checkup is a post-birth appointment with your doctor or midwife to check how you're doing physically, mentally and emotionally after having a baby. [1] Your practitioner will examine you to make sure you're recovering as expected physically and also ask you questions about how you're handling your life ...
The time of your life after you have a baby is called the postpartum or postnatal period. It is broken down into three phases. Phase one is the initial recovery during the first six to twelve hours after giving birth. The second stage lasts two to six weeks while your body is physically healing, and you are adjusting to life with your newborn.
There are several things you will need to remember to do after delivery to take care of your own health. Some physical tips to remember include: Resting: Delivering a baby is hard work and you probably weren't able to sleep much in the hospital. The first few weeks after delivery are an important time for you to rest whenever you can.
A postpartum checkup is an important part of your medical care after you have a baby. Postpartum care is important because new moms are at risk of serious and sometimes life-threatening health complications. Get a complete postpartum checkup no later than 12 weeks after giving birth. During your visit, your provider will check to make sure you ...
Yeah, absolutely. A baby is a bundle of joy, and it's such a blessing, and it's a wonderful experience, but we need to talk about what happens after you have pushed a baby through your vagina — and what happens to that vagina afterwards, and the carnage that it has experienced, especially after a vaginal delivery. Dr. Nipunie Rajapakse: Yeah.
You will likely have a complete postpartum visit in the first 3 months after delivery. At that time, your doctor or midwife will check on your recovery from childbirth. ... In the first few days after birth, your baby may sleep a lot and only be awake to eat or have a diaper change. Your baby will become gradually more alert throughout the month.
Afterpains will stop in the first week, for example, and bleeding will subside during the first month. You may have breast tenderness, night sweats, and exhaustion, and if you've had a C-section, you'll need additional recovery time. From one week to one year postpartum, here's what to expect. Medically reviewed by Cheryl Axelrod, M.D., ob-gyn.
Postpartum (or postnatal) refers to the period after childbirth. Most often, the postpartum period is the first six to eight weeks after delivery, or until your body returns to its pre-pregnancy state. But the symptoms and changes that occur during the postpartum period can last far beyond eight weeks. Major body and life changes are happening ...
The postpartum period, the time after giving birth, is a crucial time for recovery and the long-term health of the parent and baby. It's also a time of intense physical and emotional changes. It is normal and expected to experience several physical symptoms like swelling, cramping, breast tenderness, constipation, and leaking milk.
Unless you choose to have a home birth, your first couple of days of healing after birth will be in the hospital. Most people stay between 24 and 48 hours after a vaginal delivery. "Once you ...
Once you give birth, though, you're often so wrapped up with caring for your baby and adjusting to life with a newborn that you may not give much thought to your own health. But that first post-birth visit with your OB/GYN is an important one. Typically, many doctors want to schedule the first postpartum visit six weeks after you deliver.
Postpartum care refers to the care of a mother after giving birth to her baby. In the United States, the standard "postpartum visit" is typically about four to six weeks after giving birth. However, you can expect to be seen sooner if you have/had a: high-risk medical condition in pregnancy such as preeclampsia (high blood pressure)
That's why we offer classes ,1 lactation consultants, and breastfeeding support for members during pregnancy, at the hospital, and after you and your baby go home. 74.5% of babies born at Kaiser Permanente are exclusively breastfed. For babies born at other hospitals, the national average is 51.5%.2. Care for you after delivery.
The American College of Obstetricians and Gynecologists says to make postpartum care an ongoing process rather than a single visit after you give birth. Have contact with your healthcare professional by phone or in person within three weeks of delivery. Within 12 weeks of delivery, see your healthcare professional for a complete checkup.
Unless you've had a C-section, you should be able to leave the hospital approximately 24 hours after giving birth, assuming both you and your baby have been cleared by your doctors. The C-section ...
The days and weeks following childbirth—the postnatal period—are a critical phase in the lives of mothers and newborn babies. Most maternal and infant deaths occur in the first month after birth: almost half of postnatal maternal deaths occur within the first 24 hours,1 and 66% occur during the first week.2 In 2013, 2.8 million newborns ...
But the bottom line is that there are three people who should be guaranteed bonding time at and after delivery: you, your partner, and Baby J. It's that threesome that needs to meet, greet, and get to know each other first and foremost. To snuggle skin to skin, eye-to-eye, face-to-face, breathing in his sweet new baby smell while he breathes ...
You probably want the people closest to you to see you and your new baby first. Put them on your schedule either on your delivery day or a day or two afterward. Then spread out visits every couple of days to let yourself rest and deal with potential complications. 3. Talk to potential visitors about your wishes.
3- to 5-day well-baby checkup. Just a few days after birth, your baby's first checkup appointment will take place with the doctor you've chosen for them. In some cases, babies may need to be seen sooner than the recommended 3-5 days after birth. For example, if a newborn has jaundice, or weight or feeding issues, they may need to be seen ...
My husband's family is different from mine in a lot of ways. They didn't want to visit us and only wanted us to come to them (they live about 20 minutes away) and didn't really care to offer much for support following the birth. We were fine with it and brought our baby over when we were able to - around 3 times a month.
No one knew about the delivery until after the successful defense was complete. So she delivered a baby and became a doctor on the same very special day. Sunday is not only Mother's Day, it is ...
Shortly after the delivery, their baby boy started losing his color, turning a little blue in some areas. That's when Galax Police Officer Michael Tozollo showed up to save the day.
Local mother and baby visit UMC to thank heroes ahead of first Mother's Day together. by News 3 Staff. ... Spellacy gave birth to baby Johanna nearly one minute after she arrived at UMC.
The department said officers later learned that the baby was the woman's granddaughter. Tigard police said they spoke with the 10-month-old's mother when she was walking back to the car.
Alyse Sparkman used to read stories about babies born in unusual places and think, "That will never be me." Then she gave birth at a seafood restaurant. "It was right out of a movie ...
No charges will be filed against a 69-year-old woman after the bodies of four frozen infants were found in a Boston apartment freezer in 2022, the Suffolk County district attorney announced this week.