- Português Br
- Journalist Pass

Alzheimer’s and dementia: Understand wandering and how to address it
Dana Sparks
Share this:

Wandering and becoming lost is common among people with Alzheimer's disease or other disorders causing dementia. This behavior can happen in the early stages of dementia — even if the person has never wandered in the past.
Understand wandering
If a person with dementia is returning from regular walks or drives later than usual or is forgetting how to get to familiar places, he or she may be wandering.
There are many reasons why a person who has dementia might wander, including:
- Stress or fear. The person with dementia might wander as a reaction to feeling nervous in a crowded area, such as a restaurant.
- Searching. He or she might get lost while searching for something or someone, such as past friends.
- Basic needs. He or she might be looking for a bathroom or food or want to go outdoors.
- Following past routines. He or she might try to go to work or buy groceries.
- Visual-spatial problems. He or she can get lost even in familiar places because dementia affects the parts of the brain important for visual guidance and navigation.
Also, the risk of wandering might be higher for men than women.
Prevent wandering
Wandering isn't necessarily harmful if it occurs in a safe and controlled environment. However, wandering can pose safety issues — especially in very hot and cold temperatures or if the person with dementia ends up in a secluded area.
To prevent unsafe wandering, identify the times of day that wandering might occur. Plan meaningful activities to keep the person with dementia better engaged. If the person is searching for a spouse or wants to "go home," avoid correcting him or her. Instead, consider ways to validate and explore the person's feelings. If the person feels abandoned or disoriented, provide reassurance that he or she is safe.
Also, make sure the person's basic needs are regularly met and consider avoiding busy or crowded places.
Take precautions
To keep your loved one safe:
- Provide supervision. Continuous supervision is ideal. Be sure that someone is home with the person at all times. Stay with the person when in a new or changed environment. Don't leave the person alone in a car.
- Install alarms and locks. Various devices can alert you that the person with dementia is on the move. You might place pressure-sensitive alarm mats at the door or at the person's bedside, put warning bells on doors, use childproof covers on doorknobs or install an alarm system that chimes when a door is opened. If the person tends to unlock doors, install sliding bolt locks out of his or her line of sight.
- Camouflage doors. Place removable curtains over doors. Cover doors with paint or wallpaper that matches the surrounding walls. Or place a scenic poster on the door or a sign that says "Stop" or "Do not enter."
- Keep keys out of sight. If the person with dementia is no longer driving, hide the car keys. Also, keep out of sight shoes, coats, hats and other items that might be associated with leaving home.
Ensure a safe return
Wanderers who get lost can be difficult to find because they often react unpredictably. For example, they might not call for help or respond to searchers' calls. Once found, wanderers might not remember their names or where they live.
If you are caring for someone who might wander, inform the local police, your neighbors and other close contacts. Compile a list of emergency phone numbers in case you can't find the person with dementia. Keep on hand a recent photo or video of the person, his or her medical information, and a list of places that he or she might wander to, such as previous homes or places of work.
Have the person carry an identification card or wear a medical bracelet, and place labels in the person's garments. Also, consider enrolling in the MedicAlert and Alzheimer's Association safe-return program. For a fee, participants receive an identification bracelet, necklace or clothing tags and access to 24-hour support in case of emergency. You also might have your loved one wear a GPS or other tracking device.
If the person with dementia wanders, search the immediate area for no more than 15 minutes and then contact local authorities and the safe-return program — if you've enrolled. The sooner you seek help, the sooner the person is likely to be found.
This article is written by Mayo Clinic Staff . Find more health and medical information on mayoclinic.org .
- Answers to common questions about whether vaccines are safe, effective and necessary Consumer Health: Treating and living with HIV and AIDS
Related Articles

Diseases & Diagnoses
Issue Index
- Case Reports
Cover Focus | June 2022
Wandering & Sundowning in Dementia
Preventive and acute management of some of the most challenging aspects of dementia is possible..
Taylor Thomas, BA; and Aaron Ritter, MD
Alzheimer disease (AD) and related dementias are complex disorders that affect multiple brain systems, resulting in a wide range of cognitive and behavioral manifestations. The behavioral symptoms often have clinical analogs in idiopathic psychiatric disorders and are frequently referred to as neuropsychiatric symptoms (NPS) of dementia. Many therapeutic strategies for NPS are borrowed from treatment of idiopathic psychiatric disorders. For example, selective serotonin reuptake inhibitors (SSRIs) commonly used to treat major depressive disorder may also be prescribed for depressive symptoms in AD. This strategy has been deemed the “therapeutic metaphor” and has shown varying degrees of success in clinical trials. 1
Clinicians face significant challenges, however, when there is no suitable metaphor to guide treatment for behaviors that emerge solely in dementia. This is particularly problematic for 2 of the most burdensome behavioral manifestations of dementia—sundowning (the worsening of symptoms in the late afternoon and early evening) and wandering. Despite being among the most impactful behaviors in dementia, there is very little research evidence to guide therapeutic approaches. This review provides a brief update of the current literature regarding wandering and sundowning in dementia. Using evidence-based approaches from the research literature, where available, and best practices adopted from our own clinical practice when little evidence exists, we outline a practical treatment algorithm that can be used in the clinic when facing either of these common and problematic behaviors.
Wandering Frequency, Consequences & Causes
Wandering is a complex behavioral phenomenon that is frequent in dementia. Approximately 20% of community-dwelling individuals with dementia and 60% of those living in institutionalized settings are reported to wander .2 Most definitions of wandering incorporate a variety of dementia-related locomotion activities, including elopement (ie, attempts to escape), repetitive pacing, and becoming lost. 3 More recently, the term “critical wandering” or “missing incidents” have been used to draw distinctions between elopement and pacing vs wandering and becoming lost. 4 Critical wandering episodes have a high mortality rate of 20%, placing this symptom among the most dangerous behavioral manifestations of dementia. 5
The risk of wandering increases with severity of cognitive impairment, with the highest rate in those with Mini-Mental State Exam (MMSE) scores of 13 or less. 6 Individuals who frequently wander (ie, multiple times per week) almost always have at least moderate dementia. Few studies have compared wandering rates among people with different types of dementia. 7 Experience from our clinical practice suggests that wandering is most common in AD—where spatial disorientation and amnesia are common clinical features—but can also occur in moderate to advanced stages of behavioral variant frontotemporal dementia (FTD) and Lewy body dementia (LBD). The presence of comorbid NPS (eg, severe depression, sleep disorders, and psychosis) may increase the likelihood of wandering. 8
Causes of wandering are not well understood. Some hypothesize wandering emerges from disconnection among brain regions responsible for visuospatial, motor, and memory functions. A positron-emission tomography (PET) study of 342 individuals with AD, 80 of whom were considered wanderers, found a distinct pattern of hypometabolism in the cingulum and supplementary motor areas among wanderers. Correlations between specific brain regions and the type of wandering (eg, pacing, lapping, or random) were also seen. 9
A relatively larger body of research informs psychosocial perspectives on wandering with 3 scenarios identified in which wandering behaviors commonly emerge, including 1) escape from an unfamiliar setting; 2) desire for social interaction; and 3) exercise behavior triggered by restlessness or lack of activity. Other factors that increase wandering behavior include lifelong low ability to tolerate stress, an individual’s belief that they are still employed at a job, and a repeated desire to search for people (eg, dead family members) or places (eg, a home where they no longer reside). 10
Managing Wandering
There is little empiric evidence to inform treatment approaches to wandering in dementia. Nonpharmaceutical interventions that promote “safe walking” instead of aimless wandering are preferred initial approaches. Several “low tech” options with low associated costs and negligible side effects have some evidence for use, including exercise programs, aromatherapy, placing murals and other paintings in front of exit doors, or hiding door handles. 11 More recently, the explosion of discrete and affordable wearable devices that have global positioning system (GPS) tracking ability have significantly expanded the number of “high-tech” options available to address elopement. These include GPS tagging, bed and door alarms, and surveillance systems. Few have been tested in prospective, placebo-controlled studies, however, making it hard to make firm conclusions regarding efficacy. 12 The ethical implications of using these technologies—including potential infringements on privacy, dignity, and autonomy of individuals—are seldom considered in clinical trials or clinical practice. 13
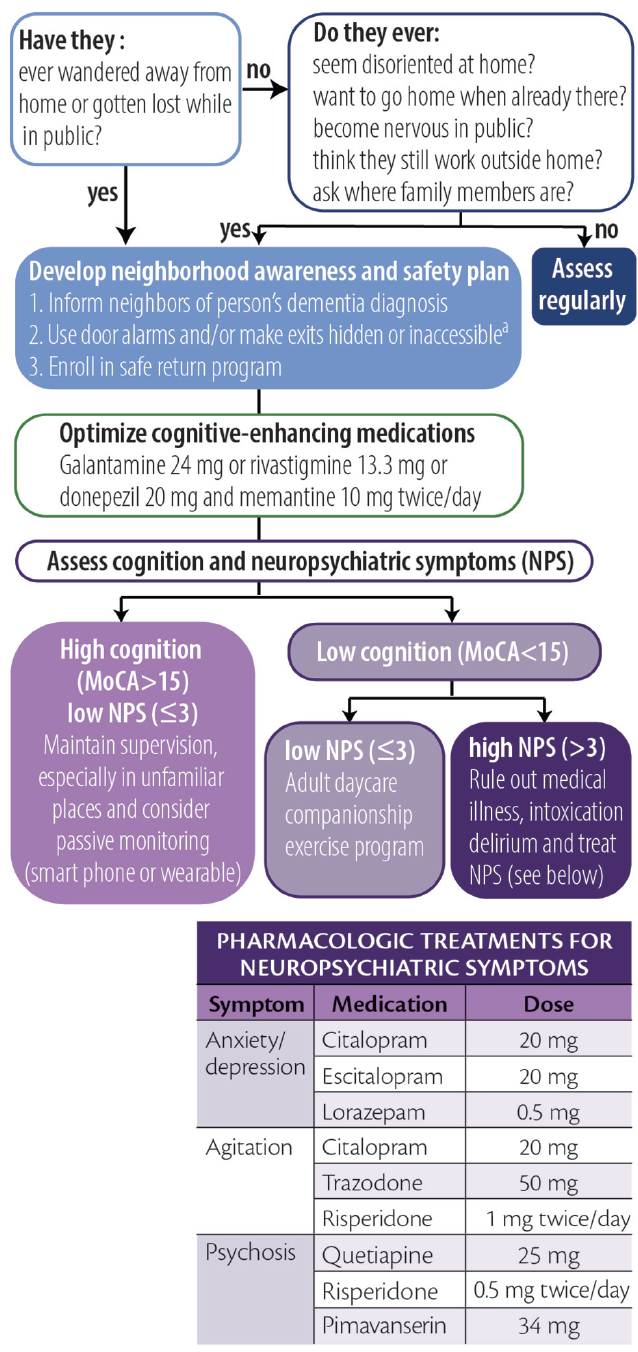
Considering the high prevalence and often deadly consequences associated with wandering, we offer a practical, algorithmic approach to wandering in dementia (Figure 1).
Figure 1. Algorithmic approach to wandering. Abbreviation: MoCA, Montreal Cognitive Assessment. a Persons with dementia should never be left alone behind locked doors.
Click to view larger
Screening for Wandering
To screen for wandering behavior, we ask the following 2 questions of or about all persons with dementia:
1. Have they ever wandered away from their home?
2. Have they ever gotten lost while in public?
If either of these are responded to affirmatively, we make recommendations and stratify risk as described below. If both questions are responded to with “no,” we ask if they:
1. ever seem disoriented at home or in familiar places?
2. ever report a desire to go home even while at home?
3. become excessively nervous while in public?
4. talk about needing to fulfill prior work obligations?
5. ask about the whereabouts of past family or friends?
An affirmative answer to any of these 5 questions may indicate an increased risk for wandering. For those who wander or are at high risk for wandering we provide basic education, recommend increased diligence, and maximize behavioral strategies to improve orientation (eg, display a written calendar and/or a large digital clock with time and date and optimize use of cognitive-enhancing agents when appropriate).
Creating a Wandering Safety Plan
Once a wandering event has occurred, we recommend families develop a neighborhood awareness and safety plan. The Alzheimer’s Association’s website has excellent resources devoted toward developing this plan ( https://www.alz.org/help-support/caregiving/stages-behaviors/wandering ). At a minimum, the safety plan should include notifying neighbors that the person has dementia, keeping a list of places they are likely to wander to, and having a recent photo readily available for emergency medical and other services. We also educate families about the initial steps to take if wandering occurs, including immediately searching areas favoring the direction of the dominant hand, focusing the search within 1.5 miles of the home, and calling 9-1-1 no more than 15 minutes after a person with dementia has been determined to be missing. Additional recommendations include obtaining medical identification jewelry, installing door alarms, and making locks inaccessible (ie, hiding them or placing them out of reach). Families should be encouraged to enroll in a safe return program (eg, MedicAlert, Project Lifesaver, or Silver Alert) if one is available in their area. It is important to note that people with dementia should never be locked by themselves inside a home.
Managing Risk by Stratified Wandering Type
Cluster analyses show people who wander can largely be grouped into 1 of 3 different types based on cognitive and behavioral characteristics. 14 These groupings are useful for tailoring interventions and can be identified for an individual with combined cognitive test scores and behavioral symptom profiles. We use the Montreal Cognitive Assessment (MoCA) 15 and the Neuropsychiatric Inventory–Questionnaire (NPI-Q) 16 because they are relatively quick to administer while providing important information and can be simultaneously administered to caregivers (NPI-Q) and patients (MoCA). These assessments can be used to stratify patients as follows.
Group 1: High Cognitive Function, Low Behavioral Disturbances. Individuals who score greater than 15 on the MoCA and have 3 or fewer behavioral symptoms wander infrequently (<1 time/month) and often only in unfamiliar settings. Because wandering is usually triggered by unexpected stressors, the main goal for these individuals is to provide adequate supervision in unfamiliar settings. Those in this group may also still carry a mobile phone with several high-tech options (eg, GPS systems or “find my phone” apps) that may be beneficial.
Group 2: Low Cognitive Function, Low Behavioral Disturbances. Persons with lower cognitive test scores (eg, ≤10 on the MoCA) and fewer than 3 NPS may wander because of boredom or a lack of physical or cognitive stimulation. For this group, we recommend a companion caregiver or adult daycare program to engage the patient in enjoyable activities and incorporate supervised walks or exercise programs during the day. Individuals in this group may benefit from the creation of an outdoor area that may be explored safely.
Group 3: Low Cognitive Function, High Behavioral Disturbances. People in this group require the most proactive approaches because they are likely to be the most frequent wanderers and may be at highest risk for dangerous outcomes. Wandering in this group may be driven by delusions, particularly the persecutory type. 8 We recommend, as a first step, determining whether other factors such as pain, delirium, or intoxication may be contributing to the person’s NPS. If no additional etiologies can be clearly identified, comorbid NPS should be addressed with best clinical practices, borrowing heavily from psychiatry with the “therapeutic metaphor” (See Neuropsychiatric Symptoms in Dementia in this issue). Many in this group may require institutionalization or constant supervision from hired caregivers to prevent harm. Nonpharmacologic strategies recommended for this group include taping a 2-foot black threshold in front of each door to serve as a visual barrier, installing cameras and warning alarms for outward facing doors, and installing safety gates around the house.
Sundowning Frequency, Consequences & Causes
Sundowning is the term used to describe the emergence or intensification of NPS occurring in the early evening. This phenomenon, thought to be unique to people with dementia, has long been recognized by researchers and caregivers as being among the most challenging elements of dementia care. 17 Although most frequently seen in AD, sundowning has also frequently been observed in other forms of dementia. Sundowning is among the most common behavioral manifestations of dementia, with rates in institutionalized settings exceeding 80%. 18 The risk of sundowning increases in moderate and severe dementia and because of its close association with sunlight, is more common in the autumn and winter seasons. 19
The impact of sundowning on persons with dementia is immense. Sundowning is among the most common reasons for institutionalization and is associated with faster rates of cognitive decline and increased risk for wandering. 17 Sundowning also increases care partner stress, which, in turn, may increase risk for agitation in patients. 18
The causes of sundowning are likely multifactorial. Sundowning is commonly linked to alterations in circadian rhythms. 19 Autopsy studies of people who had AD show a disproportionate loss of neurons in the suprachiasmatic nucleus (SCN), which regulates the release of melatonin in response to light. 20 Other research links sundowning to reductions in cholinergic neurotransmission, 21 and at least 1 study showed increased levels of cortisol, which may suggest alterations of the entire hypothalamic-pituitary axis. 21 Sleep disruption, inadequate sunlight exposure, and disrupted routines increase the likelihood of sundowning. 17 Medications with anticholinergic properties and sedatives may also exacerbate sundowning.
Management of Sundowning
The Progressively Lowered Stress Threshold (PLST) model provides a framework for understanding and managing sundowning. 22 In this model, sundowning occurs because diurnal alterations in circadian rhythms temporally correlate with increases in pain, hunger, or fatigue that occur later in the day. Disruptions in emotional regulation emerge when a person’s ability to tolerate such stressors is exceeded.
As with wandering, there is little empiric evidence to guide pharmacologic management of sundowning. Melatonin has been studied in several open-label studies and case series with varying levels of success. 23 Cholinesterase inhibitors and memantine reduce agitated behaviors, but have not been studied for management of sundowning. 24 Nonpharmacologic interventions (eg, eliminating daytime naps, increasing sunlight exposure, aerobic exercise, and playing music) can reduce sundowning, 17 but it is difficult to make firm conclusions about the efficacy of these measures because most have not been evaluated in prospective, placebo-controlled studies.
Analogous to headache management, approaches to sundowning can be broadly categorized as acute or preventive (Figure 2). Although preventive approaches may be more effective, caregivers may be able to reduce NPS associated with sundowning when it occurs.
Figure 2. Acute and preventative approaches to sundowning. Abbreviation: TSH, thyroid-stimulating hormone.
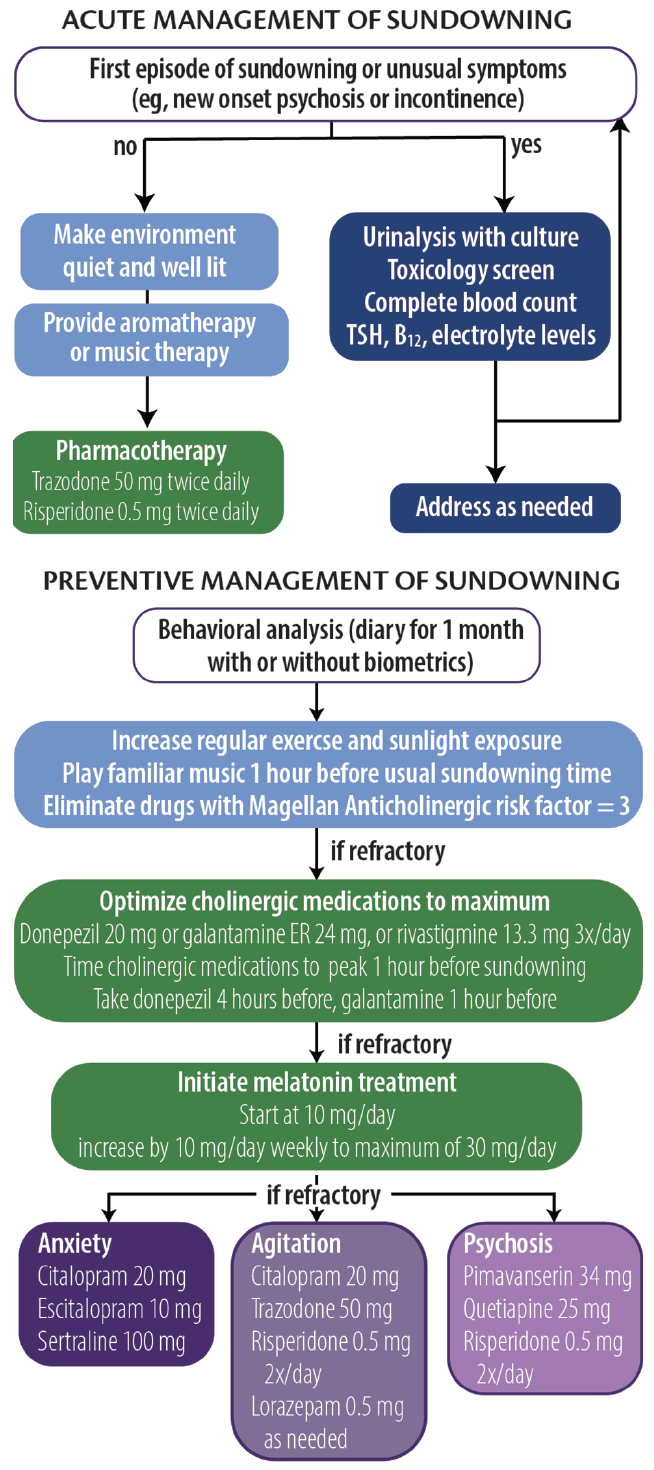
Acute Management
The PLST model can be used to identify any and all triggers that may contribute to sundowning episodes. For a first or unusual episode, it is recommended that a targeted medical and laboratory evaluation including urine culture, complete blood count, drug toxicology, and levels of electrolytes, thyroid-stimulating hormone (TSH), and vitamin B 12 be obtained. During an episode, whenever possible, a quiet, well-lit environment should be provided. Aromatherapy and familiar music at a medium volume may also help reduce anxiety and agitation. For persons at risk of hurting themselves or others, a low-dose psychotropic medication (eg, trazodone 50 mg repeated 1 hour later followed by risperidone 0.5 mg) may be necessary.
Preventive Management
In our clinical experience, prevention strategies may reduce the severity and frequency of sundowning. The first step is to conduct a behavioral analysis of the sundowning behavior. We recommend a daily journal be maintained for at least 1 month to document the types of behavior (eg, agitation, anxiety, psychosis, and disorientation) that occur, time of onset, and any extenuating circumstances that may have contributed to episodes of sundowning. Care partners can also provide information regarding medication administration and sleeping behavior to inform the analysis. The health care professional should analyze the journal, looking for patterns and correlations with other factors (eg, shift changes at care homes or changes to daily routines). The journal can be supported by biometric data from wearable technologies that provide objective measures of physical activity and sleep, which can be helpful in tailoring both pharmacologic and nonpharmacologic approaches.
We also recommend increasing the amount of regular exercise and sunlight exposure, preferably in the early afternoon. Caregivers are advised to start playing soothing or familiar music approximately 1 hour before sundowning behavior typically starts. Any medication with Magellan Anticholinergic Risk Scale scores of 3 should be eliminated, which requires scrutiny of medication lists. 25 Optimization of cognitive-enhancing medication doses and timing administration such that mean peak plasma concentrations are reached 1 hour before a person’s typical time of sundowning behavior may be beneficial.
If problematic sundowning behavior still persists, we recommend melatonin supplementation at an initial dose of 10 mg taken at nighttime, followed by a weekly increase by 10 mg to a maximum dose of 30 mg. This regimen is instituted regardless of reported sleep quality. If symptoms persist, the next step is to target NPS based on the individual’s most recent NPI-Q profile. The mantra of “start low and go slow” should guide therapeutic interventions, waiting at least 2 weeks before altering doses. In general, antidepressants are preferred first steps unless safety concerns necessitate more proactive approaches.
1. Cummings J, Ritter A, Rothenberg K. Advances in management of neuropsychiatric syndromes in neurodegenerative diseases. Curr Psychiatry Rep . 2019;21(8):79.
2. Cipriani G, Lucetti C, Nuti A, Danti S. Wandering and dementia. Psychogeriatrics . 2014;14(2):135-142.
3. Algase DL, Moore DH, Vandeweerd C, Gavin-Dreschnack DJ. Mapping the maze of terms and definitions in dementia-related wandering. Aging Ment Health . 2007;11(6):686-698.
4. Petonito G, Muschert GW, Carr DC, Kinney JM, Robbins EJ, Brown JS. Programs to locate missing and critically wandering elders: a critical review and a call for multiphasic evaluation. Gerontologist. 2013;53(1):17-25.
5. Rowe MA, Vandeveer SS, Greenblum CA, et al. Persons with dementia missing in the community: is it wandering or something unique? BMC Geriatr. 2011;11:28.
6. Hope T, Keene J, McShane RH, Fairburn CG, Gedling K, Jacoby R. Wandering in dementia: a longitudinal study. Int Psychogeriatr . 2001;13(2):137-147.
7. Ballard CG, Mohan RNC, Bannister C, Handy S, Patel A. Wandering in dementia sufferers. Int J Geriat Psychiatry . 1991;6:611-614.
8. Klein DA, Steinberg M, Galik E, et al. Wandering behaviour in community-residing persons with dementia. Int J Geriatr Psychiatry . 1999;14(4):272-279.
9. Yang Y, Kwak YT. FDG PET findings according to wandering patterns of patients with drug-naïve Alzheimer’s disease. Dement Neurocogn Disord . 2018;17(3):90-99.
10. Hope RA, Fairburn CG. The nature of wandering in dementia: a community-based study. Int J Geriat Psychiatry . 1990;5(4):239-245.
11. Neubauer NA, Azad-Khaneghah P, Miguel-Cruz A, Liu L. What do we know about strategies to manage dementia-related wandering? A scoping review. Alzheimers Dement (Amst). 2018;10:615-628.
12. Neubauer NA, Lapierre N, Ríos-Rincón A, Miguel-Cruz A, Rousseau J, Liu L. What do we know about technologies for dementia-related wandering? A scoping review: Examen de la portée: Que savons-nous à propos des technologies de gestion de l’errance liée à la démence? Can J Occup Ther. 2018;85(3):196-208.
13. O’Neill D. Should patients with dementia who wander be electronically tagged? No. BMJ. 2013;346:f3606.
14. Logsdon RG, Teri L, McCurry SM, Gibbons LE, Kukull WA, Larson EB. Wandering: a significant problem among community-residing individuals with Alzheimer’s disease. J Gerontol B Psychol Sci Soc Sci. 1998;53(5):P294-P299.
15. Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment [published correction appears in J Am Geriatr Soc. 2019;67(9):1991]. J Am Geriatr Soc. 2005;53(4):695-699. doi:10.1111/j.1532-5415.2005.53221.x
16. Kaufer DI, Cummings JL, Ketchel P, et al. Validation of the NPI-Q, a brief clinical form of the Neuropsychiatric Inventory. J Neuropsychiatry Clin Neurosci . 2000;12(2):233-239.
17. Canevelli M, Valletta M, Trebbastoni A, et al. Sundowning in dementia: clinical relevance, pathophysiological determinants, and therapeutic approaches. Front Med (Lausanne) . 2016;3:73.
18. Gallagher-Thompson D, Brooks JO 3rd, Bliwise D, Leader J, Yesavage JA. The relations among caregiver stress, “sundowning” symptoms, and cognitive decline in Alzheimer’s disease. J Am Geriatr Soc. 1992;40(8):807-810.
19. Madden KM, Feldman B. Weekly, seasonal, and geographic patterns in health contemplations about sundown syndrome: an ecological correlational study. JMIR Aging 2019;2(1):e13302. doi:10.2196/13302
20. Wang JL, Lim AS, Chiang WY, et al. Suprachiasmatic neuron numbers and rest-activity circadian rhythms in older humans. Ann Neurol. 2015;78(2):317-322.
21. Weinshenker D. Functional consequences of locus coeruleus degeneration in Alzheimer’s disease. Curr Alzheimer Res . 2008;5(3):342-345.
22. Smith M, Gerdner LA, Hall GR, Buckwalter KC. History, development, and future of the progressively lowered stress threshold: a conceptual model for dementia care. J Am Geriatr Soc . 2004;52(10):1755-1760.
23. Cohen-Mansfield J, Garfinkel D, Lipson S. Melatonin for treatment of sundowning in elderly persons with dementia - a preliminary study. Arch Gerontol Geriatr . 2000;31(1):65-76.
24. Gauthier S, Feldman H, Hecker J, et al. Efficacy of donepezil on behavioral symptoms in patients with moderate to severe Alzheimer’s disease. Int Psychogeriatr. 2002;14(4):389-404.
25. Rudolph JL, Salow MJ, Angelini MC, McGlinchey RE. The anticholinergic risk scale and anticholinergic adverse effects in older persons. Arch Intern Med . 2008;168(5):508-513.
TT reports no disclosures AR's work on this paper was supported by NIGMS P20GM109025

Taylor Thomas, BA
University of Nevada-Las Vegas School of Medicine Las Vegas, NV

Aaron Ritter, MD
Clinical Assistant Professor of Neurology Cleveland Clinic Lou Ruvo Center for Brain Health Las Vegas, NV
Treating Dementias With Care Partners in Mind
Dylan Wint, MD
Neuropsychiatric Symptoms in Dementia
Jeffrey L. Cummings, MD, ScD
This Month's Issue
Jill R. Baron, MD; and Jennifer Villwock, MD
Swati Pradeep, DO; and Jaime M. Hatcher-Martin, MD, PhD
Matthew C. Varon, MD; and Mazen M. Dimachkie, MD

Related Articles
Abdalmalik Bin Khunayfir, MD; and Brian Appleby, MD
Simon Ducharme, MD, MSc, FRCPC
Sign up to receive new issue alerts and news updates from Practical Neurology®.
Related News
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Alzheimers Dement (Amst)

What do we know about strategies to manage dementia-related wandering? A scoping review
Noelannah a. neubauer.
a Department of Occupational Therapy, Faculty of Rehabilitation Medicine, University of Alberta, Edmonton, Alberta, Canada
Peyman Azad-Khaneghah
Antonio miguel-cruz.
b School of Medicine and Health Sciences, Universidad del Rosario, Bogotá, Colombia
Associated Data
Three of five persons with dementia will wander, raising concern as to how it can be managed effectively. Wander-management strategies comprise a range of interventions for different environments. Although technological interventions may help in the management of wandering, no review has exhaustively searched what types of high- and low-technological solutions are being used to reduce the risks of wandering. In this article, we perform a review of gray and scholarly literature that examines the range and extent of high- and low-tech strategies used to manage wandering behavior in persons with dementia. We conclude that although effectiveness of 49 interventions and usability of 13 interventions were clinically tested, most were evaluated in institutional or laboratory settings, few addressed ethical issues, and the overall level of scientific evidence from these outcomes was low. Based on this review, we provide guidelines and recommendations for future research in this field.
- • Twenty categories of high and low-tech wander-management strategies were identified.
- • Most strategies were only evaluated in institutional or laboratory settings.
- • Overall level of scientific evidence from the outcomes of these strategies was low.
- • Research is required to demonstrate the efficacy of high- and low-tech strategies.
1. Introduction
The rates of cognitive impairment are on the rise worldwide as our world population ages. In 2016, 46.6 million people globally were living with dementia, and this number is projected to increase to 75 million by 2030 [1] . As a result, the already high economic burden of $818 billion in 2015 has been estimated to have increased to $1 trillion by 2018. These staggering numbers have led to the establishment of more than 30 national dementia strategies worldwide as nations begin to work together to transform dementia care and support [2] .
One significant concern for persons with dementia and their family caregivers is becoming lost when alone or in unfamiliar environments [3] , [4] . This behavior is often indicative of wandering. Wandering has been defined as “a syndrome of dementia-related locomotion behavior having repetitive, frequent, temporally disoriented nature that is manifested in lapping, random, and/or pacing patterns some of which are associated with eloping, eloping attempts, or getting lost unless accompanied” [5] . It can be either an aimless or purposeful behavior [5] , and its severity can be affected by rhythm disturbances [6] , spatial disorientation and visual-perceptual deficits [7] , physical [8] and social [9] environments, or changes in personality and behavior patterns [10] . A more recent definition of wandering also includes critical wandering, the type of wandering that results in older adults to elope with no orientation to time and place. Indeed, critical wandering is what exposes persons with dementia to the potential dangers that is of concern to caregivers [11] .
More than 60% of persons with dementia will wander. The consequences of wandering vary from minor injuries [12] , to high search and rescue costs and death [13] . If not found within 24 hours, up to half of those who wander and get lost will suffer serious injury or death [14] . Wandering behavior also significantly impacts the care and economic burden of family caregivers. For example, caregivers have been found to experience increases in emotional distress and potential civil tort claims and regulatory penalties [15] . The severity of these outcomes has gained attention from caregivers and first responders alike [16] and raises questions about how the adverse outcomes associated with wandering can be managed, and whether managing this behavior can have an influence on improving the stressors that result from caring for a person with dementia [17] .
Early interventions to manage wandering included physical restraints and medications [18] ; however, use of such strategies have been in decline due to unwanted side effects [19] and negative consequences such as poor physical and social functioning [20] . High tech strategies, such as wearable global positioning system (GPS)–enabled devices [21] , and low-tech strategies, such as visual barriers [22] , offer options for mitigating risks while allowing a person with dementia with a degree of autonomy. These strategies may therefore be a preferred approach over restraints and medications [23] . Wander-management technologies may extend the time a person with dementia can live in a community and provide peace of mind to caregivers [21] , [22] , [24] . Although such strategies are more available to consumers, only one review [25] has been conducted to examine what existing interventions for wandering are being used, and whether their effectiveness has been tested in laboratory or community settings. This review, however, only included high-tech solutions, excluding several key strategies, such as door murals and distractions, which may also help with managing this behavior. Although that review presents state of the evidence to support these interventions, it excluded potential vital reviews and studies that fall outside of this focus, limiting the scope of all available solutions within the scholarly and gray literature.
The current review serves as an extension from Neubauer et al. [25] where only high-tech solutions used to manage dementia-related wandering behavior, and only studies evaluating their usability or effectiveness were included. Therefore, the purpose of this review was to identify the range and extent of all wander-management strategies, their product readiness level, and all associated outcomes. This information provides evidence for caregivers and clinicians when they select strategies to manage wandering in persons living with dementia.
2. Methodology
2.1. design.
This is a scoping literature review based on Daudt, van Mossel, and Scott's (2013) [26] modification of Arksey and O'Malley's (2005) [27] methodology. The original Arksey and O'Malley's methodology [27] includes six steps: (1) determine the research question; (2) identify the applicable studies; (3) study selection; (4) chart data; (5) collect, summarize, and report the results; and (6) consultation exercise (optional). Daudt, van Mossel, and Scott's (2013) [26] modification of this methodology involves an interprofessional team in step (2), and in step (3) uses a three-tiered approach to cross-check and select the articles.
2.2. Data sources and search strategy
We examined peer-reviewed and gray literature published between January 1990 and November 2017. Peer-reviewed literature studies were searched in six databases: EMBASE, CINAHL, Ovid Medline, PsycINFO, Web of Science, and Scopus. These databases were searched using the following terms identified in the title, abstract, or key words: (physical barrier* OR barrier* OR lock* OR low tech* OR nonpharmacological OR therap* OR exercise OR distraction OR pet therap* OR home modification* OR door mural* or signage OR identification information OR ID card* OR bracelet* OR jewelry OR technolog* OR gerontechnology OR telemonitoring OR telesurveillance OR telehealth OR assistive technology OR GPS OR sensor* OR mobile device OR application OR apps OR radio frequency telemetry OR radio frequency identification OR tracking OR surveillance OR alarms OR tagging OR electronic OR restraints) AND (wander* OR walk* OR sundowning OR escape OR restlessness OR pacing OR exit* OR missing OR stay OR benevolent wandering OR critical wandering OR non-critical wandering) AND (dementia OR Alzheimer's Disease OR cognitive disorders). Gray literature was searched in eight databases: Google, CADTH grey matters, Institute of Health Economics, Clinicaltrials.gov , The University of Alberta Grey Literature Collection, ProQuest Dissertations & Theses Global, National Guidelines Clearinghouse, and Health on the NET Foundation were searched for strategies developed to address wandering in persons with dementia—(dementia) AND (wander* OR elope OR sundowning OR critical wandering OR benevolent wandering OR non-critical wandering) (nonpharmacological OR therap* OR exercise OR distraction OR low tech* OR home modification OR technology OR tech* OR GPS OR RFID OR mobile applications OR iOS OR android OR wifi) ( Appendix A ).
2.3. Studies selection process
Articles were exported to a reference manager where duplicate articles were excluded. Two authors (N.A.N. and P.A.-K.) first screened the titles and abstracts, reviewed the full text of all potential articles, and extracted the data ( Fig. 1 ). Disagreements were resolved by consensus. Where disagreements were unresolved, the third reviewer (A.M.C.) provided input. To determine agreement between raters, 20% of the selected articles were extracted and compared. The level of agreement between the raters was high, that is, average agreement for abstracts 96% (298/310) (average κ score of 0.87, P < .000), and 97% (198/204) average agreement for full papers (overall κ score of 0.91, P < .000). For included articles, reviewers first extracted author initials, citation, and whether the study was eligible for review. If a study was considered ineligible for data extraction, the reason for exclusion was reported ( Fig. 1 ).

Scholarly reviewed literature article search results.
2.3.1. Inclusion criteria
- a. address wander-management strategies in the home or supportive care environments for persons with dementia or cognitive decline regardless of whether it was embedded in an environment, was worn, or was implemented as a form of therapy.
- b. address critical or noncritical wandering in older adults with dementia.
- c. include strategies that support independence and address outcomes associated with wandering, regardless of level of development.
- 2. Clinically oriented studies that included only persons with dementia over age 50 years.
- 3. Studies published in any language and available in full text in peer-reviewed journals or conference proceedings from electronic abstract systems.
- 4. Studies that used any type of study design or methodology, with positive or negative results.
- 5. Studies that used lower and higher complexity technologies for wander management such as GPS and door murals.
- 6. Studies published in books or book chapters and conference proceedings.
- 7. For gray literature: were websites suggesting or selling strategies to address dementia-related wandering.
2.3.2. Exclusion criteria
- 1. Abstracts or studies that were not available.
- 2. Publications that did not provide adequate information for categorizing the study (e.g., participant characteristics).
2.4. Bias control
The procedure of Neubauer et al. [25] was followed to address bias. By including any language, multiple databases, and data types, we conducted a thorough search, to achieve a high level of sensitivity [28] . Inclusion of studies with positive and negative results addressed publication bias [29] . Inclusion of studies registered in electronic abstract systems served as the first “ quality filter ” and ensured a degree of scientific level of conceptual methodological rigor [30] . Studies published before 1990 were not included because most development of wander-management strategies occurred later [17] , [31] . The use of two pairs of raters during the selection for relevant articles, and a third and fourth rater when there was disagreement, minimized rater-bias that may have arisen from the subjective nature of applying the inclusion and exclusion criteria.
2.5. Publications review and data abstraction
Peer-reviewed articles were examined for the following attributes: features of wander-management strategies (i.e., strategy type, specifications, cost, product readiness level) and characteristics of research (i.e., clinical implications, sample size, participant characteristics, level of clinical evidence of outcomes). Gray literature was reviewed for features of wander-management strategies (i.e., strategy type, specifications, cost, device features). Two raters individually extracted data from articles.
2.5.1. Features of wander-management strategies
- (a) Strategy type. Refers to the name and strategy used to manage wandering. Primary categories identified include high tech [32] (e.g., locating, alarms/surveillance, wandering detection, wayfinding belt, distraction/redirection, and locks/barriers) and low tech [32] (e.g., exercise, distraction/redirection, locks/barriers, physical restraints, community, signage, wayfinding, supervision, education, and other).
- (b) Product readiness level (PRL). Assesses the maturity of evolving products during their development. We used the PRL [33] in which nine levels are used and ranged from PRL1 (basic principles observed) to PRL9 (actual system proven in operational environment).
2.5.2. Characteristics of research conducted in wander-management strategies
- (a) Type of study, design of the study, level of clinical evidence, and outcomes in the studies regarding wander-management strategies. Studies were classified into four types, including strategy- and clinical-oriented studies, usability, program-oriented, review, or a combination of them. Study design was categorized using the McMaster assessment of study appraisal [34] , [35] . An adaptation of the modified Sackett criteria proposed by Teasell et al., (2013) [36] was used to determine the level of evidence provided by the clinical-oriented studies. Using this criterion, raters assigned a level of evidence for a given technological intervention based on a seven-level scale. Quality of the randomized controlled trials (RCTs) was measured by the Physiotherapy Evidence Database ( PEDro ) scale [37] . The PEDro scale has 11 criteria, 10 being the maximum score that a trial can achieve. Scores of 9–10 are considered “excellent” quality; 6–8 indicates “good” quality; 4–5 are “fair” quality; and below 4 is “poor” quality [38] . As the field of wander-management technologies is diverse, we assessed the levels of evidence across three device categories: mobile locator, sensor and alarm, and wayfinding. Data on sample size, experiment length, study strategy (i.e., clinical, usability, combined), study design (i.e., qualitative or quantitative research method), main outcomes of the study, and data collection location (i.e., home, community, facility) were collected.
- (b) Ethical concern associated with the implementation of the wander-management strategy. Refers to the ethical concerns that were addressed regarding the implementation or use of the wander-management strategy. Examples of concerns include but not limited to protecting privacy, dignity, and autonomy of the person with dementia.
2.6. Data analysis
Data analysis was conducted by one person (N.A.N.). Due to the diversity of the included articles, a qualitative approach was used, where content analysis was performed on the extracted data highlighted (in bold) previously. Descriptive statistics (i.e., averages and standard deviations [SDs]) were calculated for diversity of the technology specifications, strategy cost, and PRL across the included wander-management strategies, in addition to participant age, number of participants from the included studies, and study length.
The initial search identified 4096 peer-reviewed studies; 118 studies were included in the data-abstraction phase and final analysis (2.9%, 118/4096) ( Fig. 1 ). Most studies (68.6%, 59/86) were excluded because they did not meet inclusion criteria 1a, 1b, 1c, or all three. Other reasons for exclusion from the final data-abstraction phase were that studies were not available (31.4%, 27/86).
For the gray literature, 130 strategies from 44 commercial websites, 1 dissertation website, 5 self-help websites, 8 Alzheimer's-specific websites, and 1 online magazine were included in the data-abstraction phase and final analysis. All met inclusion criteria (7), that is, were websites suggesting or selling strategies to address dementia-related wandering.
Studies containing high-tech–only strategies were characterized by low journal impact factor (i.e., Source Normalized Impact per Paper mean 0.94, SD 0.59; 95% confidence interval [0.79, 1.08]) and were published in journals located in Q1 (13 studies), Q2 (16 studies), Q3 (5 studies), and Q4 (6 studies) journal quartile per SCImago Journal Rank classification [39] . Studies containing low-tech–only strategies were characterized by low journal impact factor (i.e., Source Normalized Impact per Paper mean 0.99, SD 0.51; 95% confidence interval [0.84, 1.14]) and were published in journals located in Q1 (19 studies), Q2 (16 studies), Q3 (6 studies), and Q4 (2 studies) journal quartile per SCImago Journal Rank classification [39] . Studies containing both high- and low-tech strategies were characterized by low journal impact factor (i.e., Source Normalized Impact per Paper mean 0.99, SD 0.82; 95% confidence interval [0.58, 1.40]) and were published in journals located in Q1 (4 studies), Q2 (7 studies), and Q3 (1 studies) journal quartile per SCImago Journal Rank classification [39] .
Regarding design [34] , [35] , seven high-tech studies were of qualitative design [phenomenology (4) and grounded theory (3)], 21 were of quantitative design [cross-sectional design (10), single-case design (4), case study (3), before-after design (1), randomized controlled trial (1), randomized pre-post (1), and descriptive (1)], and 9 were reviews [systematic review (4) and other review (5)]. Low-tech strategies included two studies that were of qualitative design [grounded theory (2)], 14 were of quantitative design [cross-sectional design (4), case study (4), single-case design (2), retrospective (1), pretest-posttest (1), ABA descriptive design (1), and randomized controlled trail (1)], and 17 were reviews [systematic review (10), Cochrane review (1), and other review (6)]. Publications containing both high- and low-tech strategies included two studies that were of qualitative design [phenomenology (2)], 4 were of quantitative design [cross-sectional design (1), single-case design (1), randomized controlled trail (1), and case study (1)], and 4 were reviews [systematic review (2), Cochrane review (1), and other review (1)] ( Table 1 ).
Table 1
Positive and negative outcomes per type of strategy (high tech vs. low tech) (n = 118) of scholarly literature
NOTE. Three of 61 high-tech, 8/42 low-tech, and 2/15 articles that contained both high- and low-tech strategies did not evaluate the effectiveness of wander-management strategies and only proposed potential strategies. Therefore, outcomes of these included articles could not be provided. Level of evidence according to Sackett criteria proposed by Teasell et al. [36] .
Included peer-reviewed literature came from 20 countries, with over half of the studies being conducted in the USA (58%, 47/118) and the UK (16%, 19/118). Similarly, for the gray literature, strategies were found to originate from 7 countries, with almost 80% of the technologies being from the USA and UK (75% USA, 12% Canada, and 7% UK). Publication year of the included peer-reviewed literature varied, with wander-management strategy publications appearing in the early 1990s, and the total number of publications increasing over the last 27 years. A trend was evident pertaining to the type of strategy being published, where there has been a predominant focus on high- versus low-tech strategies over the last decade.
3.1. Features of wander-management technologies
3.1.1. wander-management strategy—type used and strategy specifications.
A total of 183 high-tech strategies (109 from peer-reviewed and 74 from gray literature) and 143 low-tech strategies (85 from peer-reviewed and 58 from gray literature) were included in this scoping review and included 6 subcategories of high-tech strategies and 14 subcategories of low-tech strategies. The most commonly used high-tech subcategories from the scholarly literature were locating strategies (i.e., GPS, radio frequency, Bluetooth, and Wi-Fi; 71.6%, 78/109) and alarm and sensors (i.e., motion and occupancy sensors, monitors, and optical systems; 19.3%, 21/109). The most commonly used high-tech subcategories from the gray literature were also locating technologies (i.e., GPS and radio frequency; 63.5%, 47/74) and alarm and sensors (i.e., motion sensors; 35.1%, 26/74) ( Fig. 2 ). The most commonly used low-tech subcategories from the scholarly literature were distraction/redirection strategies (i.e., doll therapy, music therapy, mirrors in front of exit doors, visual barriers such as cloth on exit doors or door murals, and the integration of purposeful activities such as chores and crafts; 35.3%, 30/85), exercise groups (i.e., walking; 12.9%, 11/85), and identification strategies (i.e., ID cards, labels, and the Safe Return Program; 8.2%, 7/85) ( Fig. 2 ). The most commonly used low-tech subcategories from the gray literature were distraction/redirection strategies (i.e., visual barriers, planning meaningful activities, animal therapy; 25.9%, 15/58), locks/barriers (i.e., door locks; 15.5%, 9/58), and identification strategies (i.e., Safe Return and Medic Alert; 12.1%, 7/58) ( Fig. 2 ).

Number of strategies that were high (n = 183) and low (n = 142) tech.
3.1.2. Product readiness level
For the peer-reviewed articles, two were in the analytical and experimental critical functions phase (PRL3), and 21 were either in development and testing phases in laboratory, or validated in relevant environments (PRL 4 and 5), or the technologies were in demonstration or pilot phase (PRL6). The remaining 31 articles contained strategies either prototypes near or planned in an operational system or were mature strategies in which actual systems operated over the full range of expected conditions (PRL9) ( Table 1 ). A total of 19 high-tech articles, 34 low-tech articles, and 11 articles containing both high- and low-tech strategies could not be classified using the PRL scale. Primary reasons were due to the high number of review articles included in this study, in addition to many strategies that were proposed but not evaluated. Articles containing both high- and low-tech solutions were found to have the highest technology readiness level (PRL9), in comparison with high-tech–only articles with an average PRL7 and low-tech–only strategies with an average PRL7.
3.2. Descriptive analysis of studies
3.2.1. characteristics of the research conducted in wander-management technologies.
- (a) Participant characteristics, sample size, length, and location of included studies. Participants of the included studies had a mean age of 75 years (SD 9.7). The age ranged from 23 to 90 years for caregivers and 60 to 103 years for persons with dementia, with a high dispersion in the number of participants (i.e., mean of n = 217 and SD = 77.2). Although all peer-reviewed articles included persons with dementia, only 19 articles (16%, 19/118) specified their underlying degree of dementia and level of cognitive decline. Almost 43% (38/88) of the included clinically oriented studies were small trials with a total number of participants less than 50 (i.e., mean of n = 10.8; SD 10.0), whereas the remaining trials can be described as medium-large (i.e., >50) with a mean of n = 200.5 (SD 338.0). No mean differences were found across low- and high-tech strategy studies for small and medium-large trials ( P > .05). Of the 88 included clinical studies, 29 did not report sample size and therefore were not included in the aforementioned calculations. Fourteen studies involved caregivers; however, only seven reported the relationship between the individual with dementia and caregiver. The most common type of family caregiver was a combination of children and spouse (18.6%), followed by spouse only (17.7%), and children (16.7%). Professional caregivers, search and rescue workers, and nurses were also included, making up nearly half of the reported involved stakeholders (40.3%). Forty-three of the studies reported the ratio of male-to-female dementia clients and caregivers. The average total number of females included in this review was 60 (SD 27), whereas the average total number of males included in this review was 39 (SD 36). Only 11 of the 118 studies reported ethnicity of participants. Of these, two were 100% Caucasian, five were more than 70% Caucasian, four were 100% Asian, and five contained <25% for Latino, African American, and African Caribbean decent. The lengths of the included studies varied (mean 4.8 months; SD 11.5). Only 57 of the 118 studies (48%) reported the location of the study. The setting of tests for the included studies ranged from long-term care (43.9%), community (26.3%), laboratory (10.5%), home (7.0%), hospital (5.3%), assisted living (3.5%), and outdoor environments (3.5%).
Table 2
High-tech main outcomes of scholarly literature
Abbreviations: RFID, radio-frequency identification; GPS, global positioning system; RF, radio frequency.
The outcome variables for low-tech strategies included wandering prevalence/frequency, attempted door testing/exiting/entries, total time seated, number of aggressive events, restlessness, and success facilitating return of the missing person ( Table 3 ). For the measures used to assess the proposed outcome variables, 17 measures were reported, and of these, 76% (13/17) were different. The most commonly used approaches were time between door testing/exiting (4/17) and observations (3/17). Finally, the outcome variables for studies that included low- and high-tech strategies included effectiveness of the intervention, experience and advise using the different strategies, acceptability related to the intervention, distance of wandering, and agitation and irritability ( Tables 2 and and3). 3 ). For the measures used to assess the proposed outcome variables, 16 measures were reported, and of these, 88% (14/16) were different. The most commonly used approaches were interviews (2/16) and observations (2/16).
Table 3
Low-tech main outcomes of scholarly literature
For the overall outcomes, 48.3% (57/118) of the included peer-reviewed literature showed advantages of wander-management strategies in terms of managing wandering in persons with dementia. Forty-eight of the 118 studies reported negative or nonsignificant differences, but positive versus negative outcomes were not significantly different ( P > .05). When separating the number of positive and negative or mixed outcomes by technology complexity, 52% (32/61) of the high-tech strategies, 50% (21/42) of the low-tech strategies, and 27% (4/15) of the studies that included both low- and high-tech strategies demonstrated positive results. Thirteen studies did not include results that evaluated wander-management strategies; therefore, they were not included in calculations. The above indicates that although the implementation of strategies to manage the adverse outcomes associated with wandering is promising, there is significant room for improvement and requires further investigation. Table 1 shows the number of studies classifying the positive and negative outcomes per device type, in addition to details on the total number of participants and study design types.
- (c) Evidence of the clinical outcomes. The level of scientific evidence of the clinical-oriented studies that evaluated wander-management strategies using quantitative methods was low. Regarding the level of scientific evidence for the studies that evaluated high-tech strategies, only one article incorporated an RCT design [13] ; however, details were not explained. Ten papers used a cross-sectional design. All studies were at a level of evidence 5, and results indicated that high-tech strategies have great potential for locating the wanderer quickly; however, many devices do not follow to their claims, which could in part be due to the low quality of effectiveness testing. GPS locating devices consistently demonstrated superior accuracy to radio frequency devices. Family caregivers were perceived significantly more important in the decision-making process than figures outside of the family. Four studies used a single-case study design without a baseline phase, also at a level of evidence 5, indicating that individuals with mild dementia are capable of following vibrotactile signals, that wandering detection devices can contribute toward improved safety by identifying attempts to elope by setting up alarms and sensors, and that locating devices demonstrate promise as a novel and competent healthcare approach in the case of dementia scenarios. Seven studies used qualitative approaches, which cannot be assessed using Sackett's criteria [36] .
Regarding low-tech strategies, only one study incorporated an RCT design. This RCT [40] achieved a PEDro score of 5, with a level of evidence 2, where adapted exercise games (i.e., active activities with a softball) significantly decreased agitated behaviors, such as searching or wandering behaviors (54%, P < .05), whereas escaping restraints had no significant change (40%, P = .07). Four articles used a cross-sectional design with a level of evidence 5, and results indicated that lighting conditions had no effect on disruptive behaviors such as door testing/exiting, and few persons with dementia who exercises in ways other than walking may influence sundown syndrome and sleep quality. Four studies used a single-case study design with a baseline phase and had a level of evidence 4, indicating that cloth barriers reduced entry into restricted areas with a high treatment acceptability, music therapy can increase the amount of time seated by the persons with dementia, and highlighted the need to educate caregivers that all persons with dementia are at risk of getting lost, regardless of whether they have exhibited the risky behavior in the past. Early education would allow caregivers to adopt preventative measures to reduce these impending risks. One study used a pretest-posttest design, with a level of evidence of 4. Results demonstrated the effectiveness of integrating a wall mural painted on the entrance of doorways, through the reduction of door testing behaviors exhibited by the participants. Two articles used qualitative methods, which cannot be assessed using Sackett's criteria [36] .
Regarding studies that included high- and low-tech solutions, one study included an RCT design [41] ; however, the details were not explained. Results from this study highlighted that most devices presently used by family caregivers do not comprise new technology but rather use established items, such as baby monitors, and home modifications that are recommended by an occupational or physical therapist. There was level 5 evidence from two case study [42] , [43] designs indicating that no evidence of benefit from exercise or walking therapies were found, that tracking devices and home alarms and sensors both effectively detected wandering and locating lost patients in uncontrolled, nonrandomized studies, and that IC tag monitoring system needed further improvement for clinical use.
- (d) Usability and strategy acceptance. Of the peer-reviewed studies, 12% (13 studies) aimed to study the usability and acceptance of wander-management strategies. Of these, nine (69%, 9/13) examined acceptance of high-tech solutions and 4 (31%, 4/13) examined acceptance of low-tech solutions. Overall acceptability and usability of these strategies were high among participants. For example, one study found that most respondents agreed that the use of locator devices was superior to existing search methods and would improve quality of life of caregivers and persons with dementia, that they were appropriate devices, and that they could operate the device successfully [24] . Those who were more inclined to use wander-management technologies were older adults who had been lost once or more (89%) or who had been diagnosed with mild dementia and had a history of being lost (73%) [44] . For low-tech solutions, cloth barriers, for example, were found to have high treatment acceptability [22] . Low-tech solutions were also seen as strategies that have already been implemented within a person's home, in part due to their affordable nature, and as established strategies that result from professional recommendations from occupational and physical therapists [41] .
- (e) Although the acceptability of certain strategies was high, others did not have the same result. Locator devices used by Yung-Ching & Leung (2012) [44] , for example, were met with resistance. Barriers toward the implementation of wander-management strategies are suggested to be partly related to caregivers' acceptance of the suggestions, which they often perceive as not necessary or that they would not work in their situation. In addition to acceptance of wander-management strategies, barriers on the use of high-tech strategies include concerns about damaging the device, cost of equipment, difficulties in using the strategy, false alarms caused by the device, uncomfortable wear of the device, inaccuracy of the coordinates for locator devices, forgetting to wear the device, and concerns about privacy and stigmatization. Device esthetics was also considered important in purchase consideration [44] . Barriers on the use of low-tech strategies include participants not being aware of the strategy (e.g., mirrors and grids on doors), not enough staff to implement the strategy (e.g., exercise programs), poor product design, unavailability or lack of cooperation, issues with building codes (i.e., locked door strategies), and the implementation of the strategy being challenging due to raised ethical concerns (i.e., doll therapy being seen as demeaning and patronizing).
Table 4
Ethical concerns associated with wander-management strategies
4. Discussion
This review examined the range and extent of all possible strategies used to manage wandering behavior in persons with dementia. We included 118 studies (of 4096) and 130 strategies from the gray literature. Overall, 183 high- and 143 low-tech strategies were included, with the majority (59.5%) of the strategies being derived from the scholarly literature. The percentage of strategies derived from scholarly and gray literature differs from that of Neubauer et al. [25] where most strategies were from the gray literature. This is in part due to the addition of low-tech solutions and studies that do not evaluate the usability or effectiveness of the wander-management strategies to the current review. Of the 296 strategies, there were 183 high- and 143 low-tech solutions. Of these, there were six different subcategories of high- and 14 different subcategories of low-tech strategies, with locating strategies, alarms and sensors, and distraction/redirection strategies were the most common. Of the 118 included studies, less than half (48.3%) evaluated the usability or effectiveness of the strategies.
Only 16% were clinically tested in home or community settings, and 25% were tested in formal care settings. In addition, all testing locations took place in urban settings. The lack of real-world evaluation raises question about the degree of effectiveness of the proposed wander-management strategies, and whether users are able and willing to adopt these solutions. In addition, rural regions were significantly underrepresented, leaving out a significant cohort, which may have presented different and necessary views by caregivers on the use and integration of these interventions in their communities [46] . An increased focus on usability testing in home-based rural and urban settings and the use of user-centered and participatory design approaches would enable real users to identify problems with existing strategy designs, which could enhance adoption and acceptance of wander-management strategies [47] .
Aside from a lack of usability testing and user-centered approaches of wander-management strategies, available solutions were difficult to find and were vastly scattered across the gray literature. Most high-tech solutions were available through an array of commercial websites selling the technology. Two websites, tech.findingyourwayontario.ca and alzstore.com , were the only websites containing strategies from multiple companies. Low-tech solutions were primarily suggested in Alzheimer's-specific websites such as through the Alzheimer Association; however, little information was provided on where or how to access these strategies. In addition, no website provided an in-depth description of all available low- and high-tech wander-management strategies. These findings help to support difficulties caregivers and persons with dementia may face when trying to choose a strategy that works best for their individual needs. A guideline available through different mediums and locations is therefore necessary to simplify this information for a population that is often time constrained due to their caregiving responsibilities [48] .
Although the mass diversity of wander-management strategies may be promising in terms of having multiple options to help serve the unique needs of persons with dementia and their caregivers, only 13% of studies (15/118) in this review included high- and low-tech strategies together. Even fewer (2%; 2/118) compared their effectiveness. This raises the question whether certain high- and low-tech strategies are more effective than others, and if various combinations of wander-management strategies are necessary to meet the unique needs of persons with dementia and their family caregivers. Some persons with dementia, for example, wander inside and outside of their homes [49] , whereas some may only wander in one of these settings. In terms of living arrangements, there are a growing number of persons with dementia who are living at home alone in the community, changing the scope of how one might care for these individuals [50] . When looking at the diverse context of those affected by dementia, income levels, perceptions of risk associated with wandering behavior, culture, and beliefs may all play key roles in the successful adoption of wander-management strategies [46] . These factors, however, have yet to be evaluated within the present literature.
In addition to examining the range and scope of high- and low-tech wander-management strategies in this review, we wanted to identify their level of product readiness, and to characterize the present evidence on the implementation of such interventions. Overall, most peer-reviewed articles described strategies in which they were prototypes that were planned in an operational setting. This signifies the positive state of wander-management strategies in that most have been tested in a relevant environment and are in the process of being deployed in operational environments. Despite the potential advantages of using high- and low-tech strategies to manage wandering, only 52% (61/118) of the studies could be evaluated using the PRL scale because many studies were only proposing the strategy. With 194 different high- and low-tech strategies being included in the scholarly literature alone, this highlights the sheer infancy of present strategies that are being used to manage wandering. Further research in this area is therefore required because of the low percentage of strategies that could be evaluated using the PRL scale.
Mixed outcomes were found for both high- and low-tech strategies, where positive outcomes were found for 52% of the included high-tech strategies and 50% for the low-tech strategies. Overall, the use of nonconstraining strategies provided promise to facilitate persons with dementia to support independence and enable them to engage in meaningful activities, such as walking and remaining engaged within their community [51] . For high-tech strategies, locating technologies, such as GPS and RFID devices, were suggested to have great potential for locating wandering persons with dementia quickly, provides increased confidence and peace of mind of caregivers, and was found to be a preferred option by users. The implementation of alarms and surveillance strategies were also promising. Issues, however, such as cost, over sensitivity, appearance, privacy, stigma, and the need to combine multiple products to meet the variable needs of users, are to be considered. For low-tech interventions, strategies such as door murals, methods of distraction, visual barriers, exercise programs, and therapies (i.e., doll and music therapy) all demonstrated reductions in wandering and exit seeking behaviors. Conflicting evidence, however, was found across all strategies, and scientific rigor was repeatedly mentioned as being poor quality [52] . This raises questions on the feasibility and effectiveness of the adoption of these strategies in formal and community-based settings. Aside from the outcomes that measured caregivers' perceptions on strategies to manage wandering, like the findings of Neubauer et al. [25] , none of the included studies addressed the needs and opinions of persons with dementia, more specifically those with mild dementia. Although addressing the concerns of family caregivers is important, the end outcome of these strategies is to ensure the safety of persons with dementia at risk of getting lost. The involvement of both caregivers and persons with dementia in the design and implementation of wander-management strategies is therefore critical to enable enhanced user satisfaction, adherence, and inevitably improved safety and quality of life of persons with dementia.
The significant variation of included outcomes, participant type, assessment tools, study duration, testing settings, and study design may have influenced the mixed outcomes of the high- and low-tech wander-management strategies. Intervention implementation, for example, ranged from 25 minutes to 1 year, with most (78%) being only applied for 3 months or less. The high variation and short study length indicates a need to determine a duration that is best suited for strategy development and evaluation. Longitudinal field studies are also required to identify the long-term impact of each wander-management strategy, and there remains a critical need for standardized outcomes to compare the effectiveness of strategies to manage wandering. Other measures based on models such as the Technology Acceptance Model [53] and the Unified Theory of Acceptance and Use of Technology [54] are necessary to ensure strategies are designed in a way that take into consideration factors that are essential to user adoption. The level of scientific evidence provided by clinical-oriented studies that used quantitative methods is low as the highest level per Sackett criteria [36] was 2, with most studies containing at level of evidence of 4 or less for both high and low tech included studies. Thus, there is a need for more RCT studies to increase the level of evidence of wander-management strategies for persons with dementia.
Finally, there is a gap in the literature with respect to privacy and ethics of persons affected using wander-management strategies. There has been no approach or recommendations published to address ethical issues. Future studies on privacy versus safety, the influence of stigma, and conflicts of interest between caregivers and persons with dementia need to be further explored.
4.1. Limitations of this review
We could only quantitatively assess the strength of studies that used RCTs (using PEDro scale); as far as we know there is no standardized scale that determines the quality of either quantitative or qualitative non-RCT studies. Although there are tools and guidelines available for performing a critical appraisal of research literature, the result was a proxy measure of quality. Without a scale, comparison of the relative quality of the included studies was not possible.
5. Future research and conclusions
From this review, we can conclude that many high- and low-tech strategies exist to manage the negative outcomes associated with wandering in persons with dementia. There is a general agreement that wander-management strategies can reduce risks associated with wandering, while enabling persons with dementia with a sense of freedom and independence. Further research could determine the factors that may influence intervention adoption and demonstrate the efficacy of high- and low-tech wander-management strategies.
Research in Context
- 1. Systematic review: We conducted an extensive search on gray and scholarly literature databases. Three levels of screening were employed, that is, title screening, abstract screening, and full-text screening.
- 2. Interpretation: We identified six categories of high-tech and 14 subcategories of low-tech strategies that can be used by caregivers and persons with dementia. Although wander-management strategies were believed to mitigate the risks associated with wandering, few addressed ethical issues, few were evaluated in community settings, and the overall scientific evidence from these outcomes was low. Available solutions were scattered across the gray literature and difficult to find.
- 3. Future directions: Rigorous research is required to demonstrate the efficacy of high- and low-tech wander-management strategies and their feasibility in urban and rural community-dwelling environments. A guideline is also necessary to simplify all possible strategy types and to allow stakeholders to choose wander-management strategies based on their individual needs.
Acknowledgments
The first author received support from the Glenrose Rehabilitation Hospital through the Dr. Peter N. McCracken Legacy Scholarship, Thelma R. Scambler Scholarship, Gyro Club of Edmonton Graduate Scholarship, and the Alberta Association on Gerontology Edmonton Chapter Student Award.
The authors have no conflicts of interest to declare.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.dadm.2018.08.001 .
Supplementary data
- Best of Senior Living
- Most Friendly
- Best Meals and Dining
- Best Activities
- How Our Service Works
- Testimonials
- Leadership Team
- News & PR
Dementia and Wandering: Causes, Prevention, and Tips You Should Know

What caregivers can do about wandering
The Joint Commission International considers wandering a sentinel event , which is an event that can result in temporary, severe, or permanent harm or death. [14] The Joint Commission. Sentinel Event. Viewed Aug. 20, 2023. Found on the internet at https://www.jointcommission.org/resources/sentinel-event Maintaining a safe environment can help prevent wandering and injury.
According to the Alzheimer’s Association, as the disease progresses, you can make your home safer with tactics that include making doors the same color as walls to camouflage them, installing monitoring devices above doors to detect when they’re opened, installing or planting fences or hedges around patios and yards, and creating indoor areas that are safe to explore. [4] Alzheimer’s Association. Wandering. Found on the internet at https://www.alz.org/help-support/caregiving/stages-behaviors/wandering
Conduct a wandering risk assessment
A wandering risk assessment evaluates a person’s condition and likelihood of wandering. Several tools can help determine an older adult’s risk of wandering, including the Rating Scale for Aggressive Behavior in the Elderly (RAGE) and the Neuropsychiatric Inventory (NPI), which measures dementia-related behavioral symptoms . [15] American Psychological Association. Neuropsychiatric Inventory. 2011. Foud on the internet at https://www.apa.org/pi/about/publications/caregivers/practice-settings/assessment/tools/neuropsychiatric-inventory
Consider having a risk assessment done by a health provider, so you can be fully prepared for a wandering incident while someone is in your care.
If you’re unsure if a professional assessment is needed, conducting a basic at-home assessment of your care recipient’s habits can help determine if they may be at risk for wandering behavior. Ask yourself questions, like: [6] MeetCaregivers. Elopement and Wandering in Seniors. June 27, 2022. Found on the internet at https://meetcaregivers.com/dementia-wandering-prevention-management [16] Agency for Healthcare Research and Quality (AHRQ). Elopement. Dec. 1, 2007. Found on the internet at https://psnet.ahrq.gov/web-mm/elopement
- How frequently has your care recipient wandered?
- When was the first time your care recipient wandered?
- Do they tend to wander more during the day or night?
- Are common triggers noise or discomfort?
- When your care recipient wanders, is it random, or does it happen at regular intervals?
- Can you identify a motivation for when your care recipient wanders?
- Does your care recipient have a court-appointed legal guardian?
- Is your care recipient dangerous to you or others?
- Has cognitive decline impacted your care recipient’s ability to make decisions?
These questions are excellent for caregivers to be familiar with, so they’re not caught (completely) off-guard if an incident occurs. Answering these questions may provide a reliable assessment of wandering risk. Once you complete this assessment, it should assist in determining if further assessment is needed.
Check out our Wandering Risk Assessment
Unable to display PDF file.
Understand triggers
Recognizing the behaviors or events that may lead to wandering is one of the most critical factors caregivers need to prevent this from occurring. Examples of potential triggers for missing incidents include: [9] ECRI Institute. Continuing Care Risk Management: Wandering and Elopement. April 2014. Found on the internet at https://alnursing.org/wp-content/uploads/2020/03/WanderingandElopementPacket.pdf [6] MeetCaregivers. Elopement and Wandering in Seniors. June 27, 2022. Found on the internet at https://meetcaregivers.com/dementia-wandering-prevention-management
- Disorientation from the current location, going off in the wrong direction, and the inability to reorient due to dementia. People may not be able to self-correct, particularly in the later stages of the disease, but someone else with the right approach can often reorient them
- Experiencing feelings of hunger, pain, boredom, anxiety, or urge to use the bathroom
- Exposure to high-traffic areas
- Being near stairwells and elevators, which may prompt them to try to exit the area
- Easily locating suitcases, outdoor clothing, or other items associated with leaving their current location or taking a trip
- Exposure to noise, discomfort, or other distress
Understanding their habits and usual activity time frames can help you be more aware of when their triggers may occur. Watch your care recipient for signs of hunger, boredom, and anxiety, and act quickly when triggered. Be sure to keep your care recipient in an area with easy access to the bathroom and other frequently visited rooms to reduce their risk of wandering. Store suitcases, outdoor clothing, or other travel items, like keys, wallets, and handbags, in an area not usually accessible to your care recipient.
Take preventive steps
Avoiding wandering is crucial to prevent serious injury or death. Some suggestions for prevention include: [9] ECRI Institute. Continuing Care Risk Management: Wandering and Elopement. April 2014. Found on the internet at https://alnursing.org/wp-content/uploads/2020/03/WanderingandElopementPacket.pdf [6] MeetCaregivers. Elopement and Wandering in Seniors. June 27, 2022. Found on the internet at https://meetcaregivers.com/dementia-wandering-prevention-management [17] Sparks, Dana. Mayo Clinic. Alzheimer’s and Dementia: Understand Wandering and How to Address it. Nov. 30, 2020. Found on the internet at https://newsnetwork.mayoclinic.org/discussion/alzheimers-and-dementia-understand-wandering-and-how-to-address-it [4] Alzheimer’s Association. Wandering. Found on the internet at https://www.alz.org/help-support/caregiving/stages-behaviors/wandering
- Use a medical alert system that includes GPS tracking . Many new systems available on the market today have wearable GPS devices for older adults in the form of necklaces or smartwatches .
- If there is a risk of wandering by using a car, storing the keys in a location unknown to your care recipient may be beneficial. You can also track someone if wandering occurs in a vehicle using a GPS locator system, like OnStar’s Guardian or Safepoint.
- Provide a stimulating environment. Instances of wandering can begin with the person feeling bored. Keep an eye on your care recipient to prevent overstimulation, which can also trigger wandering.
- Create a safe space where your care recipient may wander without the risk of leaving. Gardens, walking paths, or outdoor lounge areas may serve this purpose.
- Create a schedule of daily activities for your care recipient. Participating in these activities may help them feel a sense of purpose and can prevent boredom.
- Use alarm systems and locks to prevent wandering away from the home.
Make a plan ahead of time
Readying a plan of action can help you find your care recipient sooner. Making sure recent photographs are available can assist authorities in searching for your care recipient, and ensuring they are wearing a medical ID bracelet can help with identification while providing crucial medical information in an emergency. These can be obtained through the Alzheimer’s Association or are available through stores, like Amazon. Additional considerations include: [4] Alzheimer’s Association. Wandering. Found on the internet at https://www.alz.org/help-support/caregiving/stages-behaviors/wandering [18] Alzheimer’s Society. Supporting a Person With Dementia Who Walks About. Found on the internet at https://www.alzheimers.org.uk/about-dementia/symptoms-and-diagnosis/supporting-person-dementia-who-walks-about [9] ECRI Institute. Continuing Care Risk Management: Wandering and Elopement. April 2014. Found on the internet at https://alnursing.org/wp-content/uploads/2020/03/WanderingandElopementPacket.pdf
- Secure a case number from the police if your care recipient goes missing. Be sure to specify they are diagnosed with dementia or other cognitive deficits.
- Talk to anyone in the surrounding area where your care recipient was last seen to get information regarding their direction of travel.
- Request the police issue a Silver Alert (a public notification system broadcasting missing older adults with Alzheimer’s disease, dementia, or other cognitive decline) to media outlets and other police departments in the area.
- If your care recipient has a cellphone, contact the service provider and see if they can assist you in finding the phone’s location. Apps, like Find My iPhone or Life360 , can help you track your care recipient as long as they have their phone on them.
- Contact nearby hospitals and describe your missing care recipient, including any medical issues they have.
- Check locations your care recipient frequently visits. These locations may include their favorite restaurant or shopping center. Leave missing person signs in these locations if available.
- Maintain a list of up-to-date phone numbers for friends and family, so you can alert them if your care recipient is missing or inquire when they last saw them and where they were headed next.
Coping with wandering
When a care recipient wanders, friends and family may experience many emotional challenges, commonly including anxiety, pain, and grief. [19] Cake End-of-Life Planning. How to Cope When a Loved One is Missing: 11 Tips. May 2, 2022. Found on the internet at https://www.joincake.com/blog/grief-for-missing-persons
Here are five steps to cope with a missing care recipient: [19] Cake End-of-Life Planning. How to Cope When a Loved One is Missing: 11 Tips. May 2, 2022. Found on the internet at https://www.joincake.com/blog/grief-for-missing-persons
- Seek support from friends and family. Ask them to assist with the search or other tasks to help you.
- Take care of yourself physically and emotionally. Avoid isolation.
- Find ways to express your feelings. Denying yourself the expression of grief can cause damage to your physical and emotional health.
- Limit your exposure to news coverage. Ask a friend or family member to share the responsibility of monitoring the news to prevent you from becoming overwhelmed.
- Keep hope alive. Seek out grief or missing person support groups online.
Bottom line
People with dementia benefit from exercise and activity, but caregivers should also be aware of the risk their care recipient will wander.
About six in 10 people with dementia will wander at least once. [4] Alzheimer’s Association. Wandering. Found on the internet at https://www.alz.org/help-support/caregiving/stages-behaviors/wandering Wandering is common among people with dementia, including Alzheimer’s. Serious injury or death can occur when wandering leads to leaving a safe place.
Preventive measures may include monitoring for triggers, like looking for car keys or stating they need to leave for work or home. [6] MeetCaregivers. Elopement and Wandering in Seniors. June 27, 2022. Found on the internet at https://meetcaregivers.com/dementia-wandering-prevention-management Prior planning is essential for quick response and recovery if a care recipient leaves home.
Many options are available to help find your care recipient should they go missing. Modern technology has brought us medical alert systems with wearable GPS locators. Additional location assistance may be available through vehicle GPS services, like OnStar , which can help find people quickly and safely. Consequently, when wandering occurs, anxiety, pain, and grief are common for caregivers and clinicians, so emotional support is critical to helping you cope with these emotions. [19] Cake End-of-Life Planning. How to Cope When a Loved One is Missing: 11 Tips. May 2, 2022. Found on the internet at https://www.joincake.com/blog/grief-for-missing-persons
Have questions about this review? Email us at [email protected] .
- Gavin, Kara. University of Michigan News. Most Older Adults Want to ‘Age in Place’ But Many Haven’t Taken Steps to Help Them Do So. April 13, 2022. Found on the internet at https://news.umich.edu/most-older-adults-want-to-age-in-place-but-many-havent-taken-steps-to-help-them-do-s
- National Institutes of Health (NIH). Aging in Place: Growing Older at Home. May 1, 2017. Found on the internet at https://www.nia.nih.gov/health/aging-place-growing-older-home
- Centers for Disease Control and Prevention (CDC). Disability and Safety: Information on Wandering (Elopement). Sept. 18, 2019. Found on the internet at https://www.cdc.gov/ncbddd/disabilityandsafety/wandering.html
- Alzheimer’s Association. Wandering. Found on the internet at https://www.alz.org/help-support/caregiving/stages-behaviors/wandering
- Alzheimer’s Association. Causes and Risk Factors for Alzheimer’s Disease. Found on the internet at https://www.alz.org/alzheimers-dementia/what-is-alzheimers/causes-and-risk-factors
- MeetCaregivers. Elopement and Wandering in Seniors. June 27, 2022. Found on the internet at https://meetcaregivers.com/dementia-wandering-prevention-management
- The Helper Bees. Wandering and Elopement: A Brief Guide. Viewed Aug. 19, 2023. Found on the internet at https://www.thehelperbees.com/families/healthy-hive/wandering-and-elopement-a-brief-guide
- BMC Geriatrics. Persons With Dementia Missing in the Community: Is It Wandering or Something Unique? June 5, 2011. Found on the internet at https://bmcgeriatr.biomedcentral.com/articles/10.1186/1471-2318-11-28
- ECRI Institute. Continuing Care Risk Management: Wandering and Elopement. April 2014. Found on the internet at https://alnursing.org/wp-content/uploads/2020/03/WanderingandElopementPacket.pdf
- University of Michigan News. Risk of Death for People With Dementia Increases After a Hurricane Exposure. March 13, 2023. Found on the internet at https://news.umich.edu/risk-of-death-for-people-with-dementia-increases-after-a-hurricane-exposure
- Sundara Living. Elopement in Dementia. What Do I Do? July 26, 2021. Found on the internet at https://sundaraliving.com/living-with-dementia/elopement-in-dementia-what-do-i-do
- Centers for Disease Control and Prevention (CDC). Facts About Falls. May 12, 2023. Found on the internet at https://www.cdc.gov/falls/facts.html
- Dementia & Neuropsychologia. Cognitive Impairment and Driving: A Review of the Literature. October 2009. Found on the internet at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5619413
- The Joint Commission. Sentinel Event. Viewed Aug. 20, 2023. Found on the internet at https://www.jointcommission.org/resources/sentinel-event
- American Psychological Association. Neuropsychiatric Inventory. 2011. Foud on the internet at https://www.apa.org/pi/about/publications/caregivers/practice-settings/assessment/tools/neuropsychiatric-inventory
- Agency for Healthcare Research and Quality (AHRQ). Elopement. Dec. 1, 2007. Found on the internet at https://psnet.ahrq.gov/web-mm/elopement
- Sparks, Dana. Mayo Clinic. Alzheimer’s and Dementia: Understand Wandering and How to Address it. Nov. 30, 2020. Found on the internet at https://newsnetwork.mayoclinic.org/discussion/alzheimers-and-dementia-understand-wandering-and-how-to-address-it
- Alzheimer’s Society. Supporting a Person With Dementia Who Walks About. Found on the internet at https://www.alzheimers.org.uk/about-dementia/symptoms-and-diagnosis/supporting-person-dementia-who-walks-about
- Cake End-of-Life Planning. How to Cope When a Loved One is Missing: 11 Tips. May 2, 2022. Found on the internet at https://www.joincake.com/blog/grief-for-missing-persons

Appointments at Mayo Clinic
Alzheimer's: managing sleep problems.
If you're caring for a loved one who has Alzheimer's, sleep disturbances can take a toll on both of you. Here's help promoting a good night's sleep.
Sleep problems and Alzheimer's disease often go hand in hand. Understand what contributes to sleep problems in people with Alzheimer's or other dementia — and what you can do to help.
Common sleep problems related to dementia
Many older adults have problems sleeping, but people with dementia often have an even harder time. Sleep disturbance may affect up to 25% of people with mild to moderate dementia and 50% of people with severe dementia. Sleep disturbances tend to get worse as dementia progresses in severity.
Possible sleep problems include excessive sleepiness during the day and insomnia with difficulty falling asleep and staying asleep. Frequent awakenings during the night and premature morning awakenings are also common.
People with dementia might also experience a phenomenon in the evening or during the night called sundowning. They might feel confused, agitated, anxious and aggressive. Night wandering in this state of mind can be unsafe.
Obstructive sleep apnea is also more common in people with Alzheimer's disease. This potentially serious sleep disorder causes breathing to repeatedly stop and start during sleep.
Factors that might contribute to sleep disturbances and sundowning include:
- Mental and physical exhaustion at the end of the day
- Changes in the body clock
- A need for less sleep, which is common among older adults
- Disorientation
- Reduced lighting and increased shadows, which can cause people with dementia to become confused and afraid
Supporting a good night's sleep
Sleep disturbances can take a toll on both you and the person with dementia. To promote better sleep:
- Treat underlying conditions. Sometimes conditions such as depression, sleep apnea or restless legs syndrome cause sleep problems.
- Establish a routine. Maintain regular times for eating, waking up and going to bed.
- Avoid stimulants. Alcohol, caffeine and nicotine can interfere with sleep. Limit use of these substances, especially at night. Also, avoid TV during periods of wakefulness at night.
- Encourage physical activity. Walks and other physical activities can help promote better sleep at night.
- Limit daytime sleep. Discourage afternoon napping.
- Set a peaceful mood in the evening. Help the person relax by reading out loud or playing soothing music. A comfortable bedroom temperature can help the person with dementia sleep well.
- Manage medications. Some antidepressant medications, such as bupropion and venlafaxine, can lead to insomnia. Cholinesterase inhibitors, such as donepezil, can improve cognitive and behavioral symptoms in people with Alzheimer's but also can cause insomnia. If the person with dementia is taking these kinds of medications, talk to the doctor. Administering the medication no later than the evening meal often helps.
- Consider melatonin. Melatonin might help improve sleep and reduce sundowning in people with dementia.
- Provide proper light. Bright light therapy in the evening can lessen sleep-wake cycle disturbances in people with dementia. Adequate lighting at night also can reduce agitation that can happen when surroundings are dark. Regular daylight exposure might address day and night reversal problems.
When a loved one wakes during the night
If the person with dementia wakes during the night, stay calm — even though you might be exhausted yourself. Don't argue. Instead, ask what the person needs. Nighttime agitation might be caused by discomfort or pain. See if you can determine the source of the problem, such as constipation, a full bladder, or a room that's too hot or cold.
Gently remind him or her that it's night and time for sleep. If the person needs to pace, don't restrain him or her. Instead, allow it under your supervision.
Using sleep medications
If nondrug approaches aren't working, the doctor might recommend sleep-inducing medications.
But sleep-inducing medications increase the risk of falls and confusion in older people who are cognitively impaired. As a result, sedating sleep medications generally aren't recommended for this group.
If these medications are prescribed, the doctor will likely recommend attempting to discontinue use once a regular sleep pattern is established.

Remember that you need sleep, too
If you're not getting enough sleep, you might not have the patience and energy needed to take care of someone with dementia. The person might also sense your stress and become agitated.
If possible, have family members or friends alternate nights with you. Or talk with the doctor, a social worker or a representative from a local Alzheimer's association to find out what help is available in your area.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Sleeplessness and sundowning. Alzheimer's Association. https://www.alz.org/care/alzheimers-dementia-sleep-issues-sundowning.asp. Accessed Dec. 2, 2019.
- Treatments for sleep changes. Alzheimer's Association. https://www.alz.org/alzheimers-dementia/treatments/for-sleep-changes. Accessed Dec. 2, 2019.
- 6 tips for managing sleep problems. National Institute on Aging. https://www.nia.nih.gov/health/6-tips-managing-sleep-problems-alzheimers. Accessed Dec. 2, 2019.
- Kryger MH, et al., eds. Alzheimer disease and other dementias. In: Principles and Practice of Sleep Medicine. 6th ed. Elsevier Saunders; 2017. https://www.clinicalkey.com. Accessed Dec. 2, 2019.
Products and Services
- A Book: Mayo Clinic on Alzheimer's Disease
- A Book: Day to Day: Living With Dementia
- Alzheimer's: New treatments
- Caregiver stress
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Alzheimer s Managing sleep problems
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Alzheimer's Dementia
- Early Stage
- Middle Stage
- Cognitive Testing
- Laboratory Tests
- MRI (Magnetic Resonance Imaging)
- Doctor Diagnosis
- Alzheimer’s Disease
- Vascular Dementia
- Lewy Body Dementia
- Frontotemporal Dementia
- Huntington’s Disease
- Creutzfeldt-Jakob Disease
- Posterior Cortical Atrophy (PCA)
- Parkinson’s Disease Dementia
- Normal Pressure Hydrocephalus
- Wernicke-Korsakoff Syndrome
- HIV Associated Dementia
- Mixed Dementia
- Alzheimer’s Disease Facts
- Dementia vs Alzheimer’s
- Early-Onset Alzheimer’s
- Alzheimer’s Gum Disease Link
- Risk Factors
- Dementia Diet
- Pain Management
- Eating Difficulties
- Psychological Therapies
- Hospice Care
- Respite Care
- Adult Day Care Centers
- July 20, 2022
Share This Post
Alzheimer’s disease and other forms of dementia are associated with a greater propensity for wandering, frequently placing people in dangerous situations. In addition, there are an increasing number of possible risks associated with the prolonged period of intense cold in winter.
According to the Alzheimer’s Association, people with Alzheimer’s and other forms of dementia experience wandering as a common symptom, impacting six out of every 10 of those diagnosed. Although it is one of the most disturbing behavioral changes typical of someone with the disease, family caregivers are frequently taken aback by it.
Most people who wander because of dementia do so with intent and are trying to reach a certain destination. However, people with Alzheimer’s disease often exhibit impairments in their judgment and direction, which can cause them to wander during any stage of the disease, including the early, middle, and late stages .
Wandering can take place if the individual is still driving or if they have access to the keys to the vehicle. For example, they might get in their car and drive away, but then they would be lost and unable to find their way back.
Any person with memory problems who is physically capable of walking is in danger of wandering, regardless of whether or not they have left the facility. Wandering is a common symptom of dementia that can strike at any stage of the disease and any hour of the day. From my experience, I have found that this mostly occurs in the middle stages of dementia .
Even though they can maintain a comfortable lifestyle in their own homes, some people who are adults and have dementia nonetheless express a desire to “go home.” It’s possible that you’re wandering because you’re under a lot of pressure, in a lot of pain, feeling lost and confused, not getting enough sleep, or because you have unmet needs like being lonely, bored, or hungry, or seeking comfort and want to feel safe.
A loved one who wanders is among the most important concerns for caretakers, but it is possible to avoid wandering by putting the appropriate protections and training into place.
Continue reading as I explain what leads someone with dementia to move away from familiar settings mistakenly. I also discuss techniques to decrease wandering behavior and keep elders safe even when they do wander.
Reasons For Wandering
It might be challenging to determine why a person with dementia goes off when they are alone. Every person who lives with dementia is different; nevertheless, some reasons are universal to all cases of dementia:
1. Confusion And a Lack of Orientation
The confusion and disorientation that people with dementia, such as Alzheimer’s disease , are prone to encounter can help to explain a significant portion of the wandering behavior. For example, they could become disoriented and believe they should be somewhere else or even forget where they are.
They can become unaware of the passage of time or their location altogether. This may result in the individual continuing to walk or drive in an attempt to reorient themselves, which might lead to additional confusion rather than answers. Confusion and disorientation can also be made worse by being in an overly stimulating or unpleasant atmosphere.
2. They Have The Misconception That They Have to “Go Home”
It is not uncommon for people who have dementia to assume that they are not at home, although they may, in reality, be there. Because of this idea, they can become disoriented and wander off in pursuit of the location they consider their home.
It’s possible that the desire to remain at home or find “comfort” has a part in this behavior.
3. Behavior That is Either Repetitive or Agitated
People with dementia may have an overwhelming need to move around or engage in activities requiring them to repeat themselves frequently. Because of this, they could get the impression that they have to be somewhere else or that they have to keep walking or moving for no purpose at all.
Sometimes a person’s inability to verbally communicate a requirement or discomfort, such as pain, side effects of medicine, hunger, or the urgent need to use the restroom, might be the root cause of an urge to move. The need might be so difficult to resist that it almost compels them to go in search of it.
4. Need For Routine And Other Internal Drives
If your loved one has dementia, it may be difficult for them to remember changes in their environment or their daily routine, such as the fact that their old job is no longer available. They may also be unable to recall whether or not they’ve done routine everyday activities like eating, napping, or going to the bathroom.
However, the need to carry out routines, especially those that have been practiced for a long time, such as going to work, eating, or going to a specific location, persists. As a result, people with dementia who have had this experience may feel compelled to depart at a specific time of day or to move around more frequently.
A good example of this is if you see your loved one attempting to leave the house around the time they used to go to work in the morning. To get food or the bathroom, to look for something they’ve been thinking about, and find something they’ve seen or heard may also cause them to roam. They may also roam as a result of being bored.
5. Delusions
A delusion is known as a false belief. It is common for individuals to get disoriented and confused about what is happening around them.
Delusions is more common in those with dementia. In dementia care, the person living with dementia will believe this false belief is real. For example, the person living with dementia thinking that someone they know is trying to poison them. Those living with dementia who have never wandered before should be checked out by a medical professional if they suddenly begin exhibiting uncertainty, disorientation, and wandering symptoms.
Ways to Prevent Wandering
For those who can’t always watch their loved one, there are ways to identify the causes of wandering and create environmental changes that will help decrease the episodes of wandering.
1. Behavior Management Approach
Behavior management techniques, like the DICE approach, enable loved ones to take on the role of a “scientist” in order to better understand the causes of wandering.
As an example, might the conduct be a result of variables such as pain and suffering that they are unable to verbally express? Does their wandering coincide with when they used to go to work or go out? Are they putting up any kind of effort to keep themselves busy and productive when they’re on the job? As part of the DICE model, you’d
- D: Describe what takes place.
- I: Investigate possible reasons.
- C: Create a plan.
- E: Evaluate it.
In this and other approaches to behavior management, the focus is less on altering the person who has limited insight into their behaviors (assuming that they have dementia) and more on modifying any physiological, environmental, or medical variables.
For instance, if you see that roaming typically takes place shortly after getting up in the morning, you can speculate that the want to eat or the desire to participate in daily rituals has a role in the behavior. You may next devise a plan to involve the person with dementia in the preparation of meals, to engage in reminiscence about previous work responsibilities, or to have them participate in one or two activities that would remind them of their previous responsibilities.
After putting the strategy to the test, you would next determine whether or not there has been a reduction in wandering.
2. Establish a Routine
Routine and structure are provided by creating a daily schedule. Keeping a checklist of tasks that must be completed at a specific time and location can assist keep people from becoming lost. Making a list even more meaningful should contain items that the person personally appreciates or has previously found meaningful.
There are a variety of different sensory reminders that may be beneficial in reminding the person that this timetable does exist. Some examples of these include alarms, lighting, or writing a timetable on a whiteboard or a daily planner in large font.
3. Plan Your Activities to Coincide With Periods of Restlessness or Agitation
People with dementia who are agitated, restless, or bored are more prone to get lost. The likelihood of wandering can be lessened if you can identify these periods and plan activities around them, perhaps using the behaviour management or DICE strategy mentioned above. It is also possible to use items such as music or art as a sensory distraction or to soothe to help you relax.
4. Locks And Alarms on Windows And Doors
Whenever the person with dementia wanders, we need to think about home safety recommendations to put into place. An Occupational Therapist can help with this! Ask your doctor about a referral.
The external door should have a deadbolt lock installed. Install it higher or lower than usual so that it isn’t in your line of vision. This is to ensure that a person with dementia is not left alone in their home in the event of a crisis. Also, install alarms on all windows and doors of their room and the living room (alarms that will notify you, but not the person with dementia).
Everybody in the house should be made aware of the importance of fire safety. To ensure the safety of people with cognitive disabilities, ensure that all locks are easily reachable. When there is an emergency, the doors should be able to be opened in a matter of seconds. Check out my post here on 5 door locks .
5. Avoid Crowded Places
Even for those with Alzheimer’s, navigating crowded places like shopping malls can be difficult for those with dementia. Excessively stimulating environments can result in wandering and other behavioral problems. Visiting these spots at off-peak times will help to keep the crowds at bay.
6. Make Use of Visual Cues or Distractions
You may have noticed that your loved one has trouble remembering environmental and life events shifts due to dementia. Dementia affects the ability to recall details about these changes, but it has less of an impact on the ability to recall previously practiced visual or procedural concepts.
Put a stop sign at your front entrance, for example, to let your loved one know that they need to stop or leave the doorway. A door can also be painted to fit the room’s colour scheme or represent something special to the person, like a flower, sport, or place.
7. GPS Devices
If your loved one is always wearing a GPS tracking device, you may feel more secure. Most of these wearable GPS devices like a a bracelet or watch have a build in GPS locator incase they wander out of the house.
Investing in a GPS or similar wearable monitoring equipment that allows you to keep track of a person’s whereabouts and locate the person living with dementia. If your elderly loved one won’t wear a wearable tracker, you can buy shoes, bracelets, necklaces, and anklets from vendor websites that contain these devices. Here is a post I wrote on 5 best GPS trackers to check out!
Decisions on electronic tracking devices should be made with the permission of those with dementia wherever possible.
8. Register With a Safe Return Program
For peace of mind in case they do wander away from home, enrol them in a service such as the Alzheimer’s Association’s Medic Alert Safe Return. This option does not provide GPS tracking, but provides the personal ID number and other relevant information.
When your elderly loved one is enrolled, they will receive a wearable ID that can be used to recognize your loved one and call you. Calling a toll-free hotline is another option if you need to report your elderly loved one missing.
Silver Alert or similar programs to help families identify missing elderly individuals may also be available through local law enforcement authorities.
9. Involve The Neighborhood
Have a neighbour call you if they spot your aging loved one wandering around the neighbourhood and introduce them to your loved one. Wear an ID bracelet or pendant or sew identity tags onto clothing to ensure your loved one is always identified.
10. Camouflage The Doors
Another way to keep your elderly loved one from opening outside doors is to disguise them.
People with dementia often have difficulty finding or opening doors that have been covered up or marked with prominent signs.
For example, if you want a curtain hanging above the entrance, you may attach a curtain rod. Make sure your senior does not notice your opening and closing the curtain.
Large placards reading “Stop” or “No Entry” could also be placed on the door to deter people from entering. It’s not uncommon for someone with dementia who exhibits such symptoms to refuse to open a door at all.
11. Exercise
Anxiety and depression appear to be reduced by physical activity, as do agitation and disorientation. Additionally, it may help you sleep better and longer. Behavioural and psychological symptoms of dementia may be reduced by exercising for at least half an hour, many times a week, although the exact type, duration, and frequency of the exercise remain unknown (including wandering).
People with dementia, including Alzheimer’s, may begin to wander at some point, but this may not endure indefinitely. I typically see wandering in the middle stages of dementia. Managing this behavior can be difficult because there is no one-size-fits-all pattern. The most important objective is to keep the person who is at risk of wandering safe.
A safe and monitored area in the home or yard should be provided for seniors to walk or pace rather than keeping them from roaming. Walking together throughout the day may also help prevent dementia patients from attempting to elope in the evening when many suffer from symptoms of sundowner’s syndrome.
In addition to aiding in mobility, this will also assist seniors in burning off surplus energy and feeling more in control of their motions.
Alzheimer’s patients often show no signs of wandering before they actually start. What course of action would you take if someone you cared about wandered away from home despite your best efforts to keep them safe? You should also consider using the anti-wandering goods and tactics mentioned above, including a recent photo and a comprehensive physical profile of your care recipient in their emergency medical file, as well as any relevant information regarding their vehicle.
- https://dailycaring.com/8-ways-to-prevent-alzheimers-wandering/
- https://www.verywellhealth.com/prevent-wandering-dementia-causes-97639
- https://www.hebrewseniorlife.org/blog/why-do-people-dementia-wander
- https://www.rightathome.net/blog/alzheimers-understanding-preventing-wandering-behavior
- https://www.seniorliving.org/health/wandering/
- https://www.brightfocus.org/alzheimers/article/how-prevent-wandering-alzheimers-patients
Mary Osborne
Subscribe to our newsletter, get updates and learn from the best, more to explore, how does validation therapy help in dementia.
Witnessing the gradual decline of a loved one diagnosed with dementia, can be emotionally devastating.
5 Ways to Deal With False Accusations by a Person With Dementia
Dealing with false accusations from a loved one affected by dementia can be emotionally challenging
A holistic approach to dementia care providing digital education to dementia caregivers
Useful Links
- Privacy Policy
- Terms and Conditions
Subscribe to YDT's Newsletter & Live a Better Life
COPYRIGHT © 2023. YOUR DEMENTIA THERAPIST.
- Do your parents need more help?
- Care definitions
- Navigating care services
- Care assessments
- Local NHS services
- Plan for an emergency
- Hospital discharge process
- Live-in care
- Tech solutions
- Tips to prevent falls
- Hiring a carer
- Finding the right care home
- Moving to a care home
- Complaints about care
- Care for the carer
- Emotional help
- Practical help
- A carers assessment
- Working and caring
- Respite care
- Death and grief
- Visit Care Section
- What is Dementia?
- Early signs of Dementia
- Diagnosing Dementia
- Alzheimer's or Dementia?
- Dementia treatments
- Dementia care options
- Caring for someone with Dementia
- Dementia sleep disturbance
- Dementia eating issues
- Dementia support
- Managing legal affairs
- Living well with Dementia
- Types of Dementia
- Guide to Alzheimer's disease
- Guide to Vascular Dementia
- Guide to Lewy Body Dementia
- Guide to Frontotemporal Dementia
- Visit Dementia Section
- Funding later life/care
- Getting a care assessment
- Local Authority funding guide
- State benefits funding guide
- State benefits - Attendance allowance
- State benefits - Carer's allowance
- NHS funded care guide
- Self-funding care guide
- Immediate care needs annuities
- Equity release
- Lifetime mortgages
- Deferred payment agreements
- Inheritance tax planning
- Visit Finance Section
- Introduction to legal matters
- Guide to writing a Will
- Will writing services
- Dying without a Will
- Guide to probate
- Applying for probate
- Inheritance tax guide
- Guide to Power of Attorney
- Setting up a Power of Attorney
- Guide to the Court of Protection
- Power of Attorney for someone with Dementia
- Guide to Living Wills
- Guide to Do not rescuscitate orders (DNRs)
- Visit Legal Section
- Staying healthy in old age
- Good bone health
- Healthy eating
- Elderly mental health
- Avoiding dehydration
- Preventing falls
- Mobility aids
- Tech products at home
- Fall alarms
- Renew a driving licence
- Alzheimer's disease
- Eyesight - macular degeneration
- Hearing loss
- Heart disease
- Incontinence
- Urinary Tract Infections
- Activities for elderley parents
- Holidays with care
- Holiday planning
- Travel insurance for over 70s
- Virtual travel
- Best Personal Alarms
- Taking Care
- Best Video Calling Devices
- CallGenie Video Calling
- Komp Video Calling
- Best Home Monitoring Services
- SECOM CareTech Care Alert
- Best GPS Trackers
- Best Mobile Phones
- Best Live-in Care Companies
- Elder live-in care
- Best Mobility Scooters & Mobility Aids
- Wheelfreedom
- Tenura Non-Slip Living Aids
- SureSafeGO 24/7 Alarm
- SureSafe 24/7 Connect Alarm
- Telecare24 Pendant Plan
- Taking Care Anywhere Alarm
- Lifeline24 GO GPS Alarm
- Lifeline24 GSM Alarm
- Komp Video Calling Device
- End of life care
- Prepare for emergencies
- Advance Decisions/Living Wills
- Do not rescusitate orders
- What you need to do when someone dies
- Planning a funeral
- Dealing with grief
- Bereavement support services
- Visit At The End Section
- Buckinghamshire
- Cambridgeshire
- Hertfordshire
- Hampshire & IoW
- Find Home Care
How to prevent people with dementia wandering
Medical conditions such as dementia can make the prospect of an elderly parent wandering from home and going missing a serious worry, with both health and safety concerns. Keeping safe does need to be balanced with enabling them to retain their dignity and independence as much as possible. We have created a useful checklist, 15 ways to help prevent elderly people going missing:
Outside the home
- Secure the garden or outside space as well as gates/other access points.
- Make the garden an interesting place to spend time – flowers, an outdoor bench or a bird feeder;
- When it looks like your parent is getting ready to go out, help them get ready with appropriate clothing and walk with them until you are ready to return home; you may need to distract them to head home, perhaps for a cup of tea and a biscuit.
- If your parent or relative goes walking alone encourage them to take ID; perhaps sew their name and phone number on a label into a jacket they usually wear or a bag they take with them;
- Ensure that all useful contact numbers are stored in their mobile phone. If your parent goes missing and they have their phone which is switched on, it may be possible to trace them. If your parent allows, you could put a GPS tracker on the phone;
- Consider a safe return programme such as Medic Alert which will provide an identification bracelet; making contact with the number on the bracelet will provide medical information as well as next of kin details.
- Provide neighbours and local shopkeepers with your contact telephone numbers.
- Consider placing coats and keys out of view to stop any impulsive walks.
- If your parent has recently house, show them around the area to help them feel more settled in their new surroundings
- If your parent is prone to getting agitated late afternoon or evening, they may be suffering from ‘sundowning’ . Before they usually start to get restless, suggest going for a walk with them to help bring a sense of calm.
Inside the home
11. Look into assistive technology , such as door alarms, pressure mats and GPS tracking devices which could make a huge difference to alerting you should your parent go missing. These devices identify movement, such as the time they left the house, to help finding them quickly.
12. If your parent has a carer or lives in a care home inform the carers about any walking habits which could include favourite haunts, houses they may have lived in etc;
13. Try and encourage parents and relatives to take up hobbies or other activities to keep them busy to reduce likelihood of taking a walk;
14. If your parent suffers from loneliness and you are unable to check in on them as often as you would like to, you may find the services of local befriending organisations useful, where someone can make a visit or call. Neighbours and local friends could also pop in on a regular basis;
15. If your parent gets disorientated at home consider putting signs and labels on doors to indicate where they are in the house. Black writing on yellow signs has been identified as the easiest to read and understand.
And last but not least, complete the information required for The Herbert Protocol – the system managed by the police to facilitate the speedy and safe return of elderly people who wander.

Why there might be wandering
If you are concerned that your parent is of high risk of going missing try to identify what they are trying to achieve when they go walking, perhaps keep a diary of where they go. While it is great for physical and mental well-being, the worry that that they could become disorientated and lost whilst out is very real. Try to accompany your parent on their walks and establish the purpose. Possible reasons for leaving the house could include:
- A long established routine of going for a walk is something they wish to continue
- Going for a walk gives a sense of purpose
- It’s a great way to use up some energy, particularly if they feel sleep is an issue
- It may bring pain relief or certainly some distraction or relief from anxiety
- Perhaps they have recently moved and feel uncertain about their new surroundings
- They might be searching for something or someone from the past
- Perhaps doing something useful they used to do such as collecting the children from school gives a sense of fulfilment
- Confusion about the time of day
- Confusion in the home which has meant they accidentally leave the house without meaning to whilst looking for eg the loo or the kitchen
It is a frightening prospect to imagine your parent wandering lost away from home, but there are plenty of things you can do to minimise the risk; and also practical things such as tech solutions and The Herbert Protocol that can help should it happen.
Tips & advice from our founder Annabel + discounts on useful products!
- Name First Last
- 1 Prepare To Care
- 2 Smart Home Monitoring Services
- 3 Personal Alarms
- 4 Live-in Care Companies
- 5 Best GPS Trackers for Elderly
- 6 Will Writing Services
- 7 Video Calling Devices for the Elderly
- 8 Dementia Sleeping Tips
- 9 Useful Dementia Products
- 10 Equity Release Calculator

Useful products and services
Personal Alarms
Live-in Care

- Agespace in the News
- Advertising
- Terms & Privacy
This website uses cookies to improve your experience. We'll assume you're ok with this, but you can opt-out if you wish.
Cookie Settings

10 Triggers for Wandering in Dementia
Dementia is a debilitating disease that affects millions of people worldwide. It not only affects the memory but also causes changes in mood, behavior, and communication skills. Wandering is one of the most dangerous and common behaviors associated with dementia. It can lead to injury, death, and a lot of stress for caregivers. In this blog post, I talk about the triggers for wandering in dementia and how to prevent it.
Jump Directly To
What is Wandering in Dementia?
Wandering is a behavior characterized by aimless or repetitive movements, without a clear purpose or destination. It can take many forms, such as pacing, walking in circles, leaving home without a plan, or getting lost in unfamiliar surroundings.
Wandering is particularly dangerous for people with dementia, as they may not remember where they are or how to get back home. They may also become disoriented, confused, and agitated, leading to a higher risk of falls, accidents, and injury.
Triggers for Wandering in Dementia
1. feeling lost or disoriented.
One common trigger for wandering in dementia is feeling lost or disoriented. For example, imagine an elderly woman with dementia who gets up in the middle of the night to use the bathroom. She may become confused or disoriented and wander around the house, looking for the bathroom or trying to find her way back to bed.
2. Boredom or Lack of Stimulation
Another trigger for wandering in dementia is boredom or lack of stimulation. For instance, a man with dementia who used to be an avid gardener may become restless and agitated if he no longer has access to his garden. Without stimulating activities or hobbies, he may wander in search of something to do.
3. Unmet Needs
Unmet needs can also trigger wandering in dementia. For example, an elderly man with dementia who is hungry or thirsty may wander around the house, looking for food or water. Similarly, a woman with dementia who is in pain or discomfort may wander around in search of relief.
4. Confusion or Memory Loss
Confusion and memory loss are hallmark symptoms of dementia and can trigger wandering in some individuals. For instance, a man with dementia who forgets where he is or what he is supposed to be doing may wander in search of familiar surroundings or routine activities.
5. Changes in Routine or Environment
Changes in routine or environment can also trigger wandering in dementia. For example, a woman with dementia who is moved to a new care facility or taken on vacation may become disoriented and wander around in search of familiar surroundings.
6. Side Effects of Medications
Some medications used to treat dementia or other health conditions can have side effects that trigger wandering. For instance, a woman with dementia who is taking a medication that causes drowsiness or confusion may wander around in a disoriented state.
7. Sleep Disturbances
Sleep disturbances are common in people with dementia and can trigger wandering behavior. For example, a man with dementia who experiences frequent nighttime awakenings may become disoriented and wander around in the dark.
8. Fear or Anxiety
Fear or anxiety can also trigger wandering in some individuals with dementia. For instance, a woman with dementia who is afraid of a thunderstorm or unfamiliar noise may wander around in search of safety or reassurance.
9. Unfamiliar Surroundings
Unfamiliar surroundings can also trigger wandering behavior. For example, an elderly man with dementia who is taken to a new doctor’s office or hospital may become disoriented and wander around in search of familiar surroundings.
10. Desire for Independence
Finally, some individuals with dementia may wander to assert their independence or control over their surroundings. For example, a woman with dementia who is used to being in charge of her own life may wander in an attempt to take back control and feel more independent.
These are just a few real-life examples of triggers for wandering in dementia. By understanding these triggers and taking steps to prevent wandering, caregivers can help ensure the safety and well-being of their loved ones with dementia.
10 Real-Life Examples To Help You Understand the Situation Better
1. Mary is an 80-year-old woman with early-stage dementia. She lives alone in her home and enjoys walking in her neighborhood. However, lately, Mary has been wandering more frequently and getting lost. Her daughter, who lives out of town, visited and noticed that Mary’s home was cluttered and disorganized, which may be causing her stress and confusion.
2. Tom is a 75-year-old man with mid-stage dementia. He lives in a care facility and enjoys participating in group activities. However, Tom has been wandering more frequently and leaving the facility without permission. Staff members discovered that Tom’s medication dosage was incorrect, causing him to feel restless and disoriented.
3. Emma is a 90-year-old woman with advanced-stage dementia. She lives in a nursing home and enjoys spending time with her family. However, Emma has been wandering more frequently and getting agitated. Her family discovered that Emma’s hearing aid was not working properly, causing her to feel frustrated and confused.
4. Jack is an 85-year-old man with mid-stage dementia. He lives with his wife in their home and enjoys reading and watching TV. However, Jack has been wandering more frequently and becoming lost. His wife noticed that Jack’s sleep schedule was irregular, causing him to feel tired and disoriented during the day.
5. Alice is an 85-year-old woman with early-stage dementia. She lives in a retirement community and enjoys playing cards with her friends. However, Alice has been wandering more frequently and forgetting where she is. Her friends noticed that Alice’s glasses were missing, causing her to have difficulty seeing and feeling disoriented.
6. Peter is a 70-year-old man with mid-stage dementia. He lives in a care facility and enjoys taking walks outside. However, Peter has been wandering more frequently and becoming agitated. Staff members discovered that Peter’s room was too hot, causing him to feel uncomfortable and restless.
7. Karen is a 78-year-old woman with early-stage dementia. She lives with her daughter and enjoys cooking and baking. However, Karen has been wandering more frequently and forgetting important tasks. Her daughter noticed that Karen’s kitchen was cluttered, causing her to feel overwhelmed and confused.
8. David is an 80-year-old man with mid-stage dementia. He lives in a care facility and enjoys listening to music. However, David has been wandering more frequently and becoming anxious. Staff members discovered that David’s favorite music was not available, causing him to feel frustrated and disoriented.
9. Rose is an 85-year-old woman with advanced-stage dementia. She lives in a nursing home and enjoys looking at family photos. However, Rose has been wandering more frequently and becoming agitated. Her family discovered that Rose’s hearing aid batteries were dead, causing her to feel frustrated and confused.
10. James is a 75-year-old man with early-stage dementia. He lives with his wife and enjoys working in his garden. However, James has been wandering more frequently and getting lost. His wife noticed that James was not eating enough, causing him to feel weak and disoriented.
What does the research say?
In this study , the researchers were trying to understand something called “wandering” in people with dementia. You see, wandering is when someone with dementia starts walking around aimlessly without any clear reason. It’s like they’re on a journey, but they don’t know where they’re going.
To figure out more about this wandering behavior, the researchers searched for information in places like Medline and Google Scholar. They were looking for articles, chapters, and books that had been published since way back in 1975. They used words like ‘wandering,’ ‘behavioral and psychological symptoms,’ ‘dementia,’ ‘nursing,’ and ‘elopements’ to find this information.
After finding these sources, they looked through them to see if they could find more references that would help them learn even more. So, they were kind of like detectives searching for clues about why people with dementia wander.
Now, let’s talk about why wandering is important to understand. Wandering can be a big problem for people with dementia and those who take care of them, like family members or nursing home staff. Imagine if your grandma or grandpa with dementia suddenly started walking around the neighborhood without knowing where they were. That would be really scary, right? Wandering can lead to bad things happening, and it’s a major reason why some people with dementia end up in nursing homes.
The tricky part is that we don’t really know why people with dementia wander. It’s like a mystery that hasn’t been solved yet. But the researchers think that maybe if we can treat other problems that people with dementia might have, like feeling sad or anxious, it could help reduce wandering.
So, in simple words, this study was all about trying to understand why people with dementia wander and how we can help them and their caregivers deal with this challenging behavior. It’s like trying to solve a puzzle to make life better for people with dementia and their families.
Preventing Wandering in Dementia
Maintain a structured routine.
Maintaining a structured routine can help reduce disorientation and boredom in people with dementia. A consistent routine can provide a sense of familiarity and predictability, making it easier for them to understand their surroundings and stay engaged in daily activities. A structured routine can include regular meal times, exercise, social activities, and a consistent bedtime.
Provide Adequate Stimulation
Providing adequate stimulation can help reduce boredom and restlessness in people with dementia. Activities that are mentally, physically, or socially stimulating can include things like puzzles, music, art, exercise, and conversation. It’s important to find activities that are appropriate for the person’s cognitive and physical abilities, as well as their interests.
Ensure Basic Needs are Met
Ensuring basic needs are met can help reduce the risk of wandering in people with dementia. Make sure they have access to food, water, and a bathroom at all times. Check to see if they are feeling hot, cold, or uncomfortable, and adjust the environment accordingly. If they are experiencing pain or discomfort, speak with their doctor to determine if medication or other interventions are necessary.
Create a Safe Environment
Creating a safe environment can help reduce the risk of injury or accidents in people with dementia. Install locks on doors and windows, remove tripping hazards, and install handrails or grab bars in areas where they may need assistance. Use a monitoring system or alarm to alert you if they wander out of the house or into unsafe areas.
Communicate Clearly and Effectively
Communicating clearly and effectively can help reduce the risk of unmet needs in people with dementia. Use simple, direct language and avoid talking down to them or using complicated sentences. Give them plenty of time to process information and ask clarifying questions if necessary. Use visual cues, such as pictures or signs, to help them understand their surroundings and locate important items.
Wandering in dementia can be frightening and dangerous behavior for both the person with dementia and their caregivers. By understanding the triggers for wandering and taking steps to prevent it, we can help reduce the risk of injury, accidents, and stress.
Maintaining a structured routine, providing adequate stimulation, ensuring basic needs are met, creating a safe environment, and communicating clearly and effectively are all important strategies for preventing wandering in dementia.
Have you ever cared for someone with dementia who wandered? What strategies have you used to prevent wandering and keep them safe? Let’s start a discussion in the comments section below.
I have lived-experience taking care of my parent with dementia. My goal is to help you overcome challenges involved in family caregiving.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Door Alarms for Wandering in Alzheimer's and Dementia
SilviaJansen / Getty Images
If your loved one with Alzheimer's disease or a different type of dementia wanders and attempts to leave your home or facility, one option to increase their safety is to place alarms on the doors. You can also try different locking mechanisms such as a latch up high, but the concern with that strategy is that in case of a fire, the person may not be able to escape safely out of the house.
An alarm can allow the person to attempt exiting through the door but will also alert you to her need for assistance. Alarms can offer you a little support and reassurance in your efforts to ensure your loved one's safety so that, rather than feel that you have to constantly check on her, you know that the alarm will sound if she suddenly wakes and needs assistance.
Protect individuals from elopement and wandering: Whether people with dementia intentionally attempt lopement or are simply wandering around to locate a door, those at risk for exiting without the needed supervision may benefit from a door alarm on the exterior doors.
Alerts others for assistance: Door alarms can also be used on the bathroom door. They can be placed in such a way that they'll sound when the door is opened, letting you know that your loved one requires assistance in the bathroom.
String alarm: A string alarm can be placed high up on the door frame with the string placed across the door opening. If the door opens, it will cause the string, which is held in place by a magnet, to detach from the alarm, causing it to sound. The alarm will stop sounding once the magnet is reattached.
Passive InfraRed (PIR) alarms: A PIR alarm can be utilized across a door opening so that if the plane across the door is broken, the alarm will sound and alert you to your loved one's need for assistance.
Magnetic door alarms: Magnetic door alarms have two parts that are connected magnetically. One part is attached to the door frame right at the edge next to the door and the other part is attached to the door right next to the frame. The alarm sounds when the two parts are no longer connected by the magnet.
Floor sensor alarms: Floor sensor alarms have a sensor pad on the floor and a magnetic lock on the door. They can be preset to different settings, some of which will alarm immediately and other settings that allow a person to exit out the door and return just a short time later before sounding.
Remote sounding alarms: Some alarms are designed so that they sound away from the person who is trying to get out the door. You might place the sounding device of the alarm near you so that it doesn't startle the person with dementia but will alert you to their need for assistance.
Keypad locks: Another option if you have doors in your house that you don't want your loved one to open, you can simply lock them or have a keypad lock installed on those doors. The keypad locks will unlock once you enter the correct number code in the keypad. Keypad locks can connected be to the smoke or fire alarm system so that they will unlock in case of a fire.
GPS alert systems: There are several GPS devices that can assist with keeping your loved one safe. GPS trackers can be used in a variety of ways, such as in shoes. watches and bracelets. You can set up perimeters for when you want to be alerted (such as a doorway) or you can continuously track the person on an app on your phone. These types of systems allow you to have a flexible level of monitoring, depending on your loved one's needs.
A Word From Verywell
As caregivers , one of our worst fears may be that our loved one with dementia will accidentally get lost or purposely leave a house or facility, not be able to find her way back home and then become endangered. Utilizing strategies to prevent wandering, such as understanding the common causes and using door alarms, can hopefully reduce this risk significantly and provide a little more peace of mind.
National Institute on Aging. Home Safety Checklist for Alzheimer's Disease.
Agrawal AK, Gowda M, Achary U, Gowda GS, Harbishettar V. Approach to management of wandering in dementia: ethical and legal issue. Indian Journal of Psychological Medicine . 2021;43(5_suppl):S53-S59. doi: 10.1177/02537176211030979
Au-Yeung WT, Miller L, Beattie Z, Kaye J. Passive infrared motion sensors improved the detection accuracy of nocturnal agitation. Innovation in Aging . 2021;5(Supplement_1):955-955. doi: 10.1093/geroni/igab046.3417
Hall A, Wilson CB, Stanmore E, Todd C. Implementing monitoring technologies in care homes for people with dementia: A qualitative exploration using Normalization Process Theory. International Journal of Nursing Studies . 2017;72:60-70. doi: 10.1016/j.ijnurstu.2017.04.008
Megges H, Freiesleben SD, Rösch C, Knoll N, Wessel L, Peters O. User experience and clinical effectiveness with two wearable global positioning system devices in home dementia care. Alzheimer’s & Dementia: Translational Research & Clinical Interventions . 2018;4(1):636-644. doi: 10.1016/j.trci.2018.10.002
By Esther Heerema, MSW Esther Heerema, MSW, shares practical tips gained from working with hundreds of people whose lives are touched by Alzheimer's disease and other kinds of dementia.
Call our 24 hours, seven days a week helpline at 800.272.3900

- Professionals

- Younger/Early-Onset Alzheimer's
- Is Alzheimer's Genetic?
- Women and Alzheimer's
- Creutzfeldt-Jakob Disease
- Dementia with Lewy Bodies
- Down Syndrome & Alzheimer's
- Frontotemporal Dementia
- Huntington's Disease
- Mixed Dementia
- Normal Pressure Hydrocephalus
- Posterior Cortical Atrophy
- Parkinson's Disease Dementia
- Vascular Dementia
- Korsakoff Syndrome
- Traumatic Brain Injury (TBI)
- Know the 10 Signs
- Difference Between Alzheimer's & Dementia
- 10 Steps to Approach Memory Concerns in Others
- Medical Tests for Diagnosing Alzheimer's
- Why Get Checked?
- Visiting Your Doctor
- Life After Diagnosis
- Stages of Alzheimer's
- Earlier Diagnosis
- Part the Cloud
- Research Momentum
- Our Commitment to Research
- TrialMatch: Find a Clinical Trial
- What Are Clinical Trials?
- How Clinical Trials Work
- When Clinical Trials End
- Why Participate?
- Talk to Your Doctor
- Clinical Trials: Myths vs. Facts
- Can Alzheimer's Disease Be Prevented?
- Brain Donation
- Navigating Treatment Options
- Lecanemab Approved for Treatment of Early Alzheimer's Disease
- Aducanumab Discontinued as Alzheimer's Treatment
- Medicare Treatment Coverage
- Donanemab for Treatment of Early Alzheimer's Disease — News Pending FDA Review
- Questions for Your Doctor
- Medications for Memory, Cognition and Dementia-Related Behaviors
- Treatments for Behavior
- Treatments for Sleep Changes
- Alternative Treatments
- Facts and Figures
- Assessing Symptoms and Seeking Help
- Now is the Best Time to Talk about Alzheimer's Together
- Get Educated
- Just Diagnosed
- Sharing Your Diagnosis
- Changes in Relationships
- If You Live Alone
- Treatments and Research
- Legal Planning
- Financial Planning
- Building a Care Team
- End-of-Life Planning
- Programs and Support
- Overcoming Stigma
- Younger-Onset Alzheimer's
- Taking Care of Yourself
- Reducing Stress
- Tips for Daily Life
- Helping Family and Friends
- Leaving Your Legacy
- Live Well Online Resources
- Make a Difference
- Daily Care Plan
- Communication and Alzheimer's
- Food and Eating
- Art and Music
- Incontinence
- Dressing and Grooming
- Dental Care
- Working With the Doctor
- Medication Safety
- Accepting the Diagnosis
- Early-Stage Caregiving
- Middle-Stage Caregiving
- Late-Stage Caregiving
- Aggression and Anger
- Anxiety and Agitation
- Hallucinations
- Memory Loss and Confusion
- Sleep Issues and Sundowning
- Suspicions and Delusions
- In-Home Care
- Adult Day Centers
- Long-Term Care
- Respite Care
- Hospice Care
- Choosing Care Providers
- Finding a Memory Care-Certified Nursing Home or Assisted Living Community
- Changing Care Providers
- Working with Care Providers
- Creating Your Care Team
- Long-Distance Caregiving
- Community Resource Finder
- Be a Healthy Caregiver
- Caregiver Stress
- Caregiver Stress Check
- Caregiver Depression
- Changes to Your Relationship
- Grief and Loss as Alzheimer's Progresses
- Home Safety
- Dementia and Driving
- Technology 101
- Preparing for Emergencies
- Managing Money Online Program
- Planning for Care Costs
- Paying for Care
- Health Care Appeals for People with Alzheimer's and Other Dementias
- Social Security Disability
- Medicare Part D Benefits
- Tax Deductions and Credits
- Planning Ahead for Legal Matters
- Legal Documents
- ALZ Talks Virtual Events
- ALZNavigator™
- Veterans and Dementia
- The Knight Family Dementia Care Coordination Initiative
- Online Tools
- Asian Americans and Pacific Islanders and Alzheimer's
- Native Americans and Alzheimer's
- Black Americans and Alzheimer's
- Hispanic Americans and Alzheimer's
- LGBTQ+ Community Resources for Dementia
- Educational Programs and Dementia Care Resources
- Brain Facts
- 50 Activities
- For Parents and Teachers
- Resolving Family Conflicts
- Holiday Gift Guide for Caregivers and People Living with Dementia
- Trajectory Report
- Resource Lists
- Search Databases
- Publications
- Favorite Links
- 10 Healthy Habits for Your Brain
- Stay Physically Active
- Adopt a Healthy Diet
- Stay Mentally and Socially Active
- Online Community
- Support Groups
- Find Your Local Chapter
- Any Given Moment
- New IDEAS Study
- RFI Amyloid PET Depletion Following Treatment
- Bruce T. Lamb, Ph.D., Chair
- Christopher van Dyck, M.D.
- Cynthia Lemere, Ph.D.
- David Knopman, M.D.
- Lee A. Jennings, M.D. MSHS
- Karen Bell, M.D.
- Lea Grinberg, M.D., Ph.D.
- Malú Tansey, Ph.D.
- Mary Sano, Ph.D.
- Oscar Lopez, M.D.
- Suzanne Craft, Ph.D.
- About Our Grants
- Andrew Kiselica, Ph.D., ABPP-CN
- Arjun Masurkar, M.D., Ph.D.
- Benjamin Combs, Ph.D.
- Charles DeCarli, M.D.
- Damian Holsinger, Ph.D.
- David Soleimani-Meigooni, Ph.D.
- Donna M. Wilcock, Ph.D.
- Elizabeth Head, M.A, Ph.D.
- Fan Fan, M.D.
- Fayron Epps, Ph.D., R.N.
- Ganesh Babulal, Ph.D., OTD
- Hui Zheng, Ph.D.
- Jason D. Flatt, Ph.D., MPH
- Jennifer Manly, Ph.D.
- Joanna Jankowsky, Ph.D.
- Luis Medina, Ph.D.
- Marcello D’Amelio, Ph.D.
- Marcia N. Gordon, Ph.D.
- Margaret Pericak-Vance, Ph.D.
- María Llorens-Martín, Ph.D.
- Nancy Hodgson, Ph.D.
- Shana D. Stites, Psy.D., M.A., M.S.
- Walter Swardfager, Ph.D.
- ALZ WW-FNFP Grant
- Capacity Building in International Dementia Research Program
- ISTAART IGPCC
- Alzheimer’s Disease Strategic Fund: Endolysosomal Activity in Alzheimer’s (E2A) Grant Program
- Imaging Research in Alzheimer’s and Other Neurodegenerative Diseases
- Zenith Fellow Awards
- National Academy of Neuropsychology & Alzheimer’s Association Funding Opportunity
- Part the Cloud-Gates Partnership Grant Program: Bioenergetics and Inflammation
- Pilot Awards for Global Brain Health Leaders (Invitation Only)
- Robert W. Katzman, M.D., Clinical Research Training Scholarship
- Funded Studies
- How to Apply
- Portfolio Summaries
- Supporting Research in Health Disparities, Policy and Ethics in Alzheimer’s Disease and Dementia Research (HPE-ADRD)
- Diagnostic Criteria & Guidelines
- Annual Conference: AAIC
- Professional Society: ISTAART
- Alzheimer's & Dementia
- Alzheimer's & Dementia: DADM
- Alzheimer's & Dementia: TRCI
- International Network to Study SARS-CoV-2 Impact on Behavior and Cognition
- Alzheimer’s Association Business Consortium (AABC)
- Global Biomarker Standardization Consortium (GBSC)
- Global Alzheimer’s Association Interactive Network
- International Alzheimer's Disease Research Portfolio
- Alzheimer’s Disease Neuroimaging Initiative Private Partner Scientific Board (ADNI-PPSB)
- Research Roundtable
- About WW-ADNI
- North American ADNI
- European ADNI
- Australia ADNI
- Taiwan ADNI
- Argentina ADNI
- WW-ADNI Meetings
- Submit Study
- RFI Inclusive Language Guide
- Scientific Conferences
- AUC for Amyloid and Tau PET Imaging
- Make a Donation
- Walk to End Alzheimer's
- The Longest Day
- RivALZ to End ALZ
- Ride to End ALZ
- Tribute Pages
- Gift Options to Meet Your Goals
- Founders Society
- Fred Bernhardt
- Anjanette Kichline
- Lori A. Jacobson
- Pam and Bill Russell
- Gina Adelman
- Franz and Christa Boetsch
- Adrienne Edelstein
- For Professional Advisors
- Free Planning Guides
- Contact the Planned Giving Staff
- Workplace Giving
- Do Good to End ALZ
- Donate a Vehicle
- Donate Stock
- Donate Cryptocurrency
- Donate Gold & Sterling Silver
- Donor-Advised Funds
- Use of Funds
- Giving Societies
- Why We Advocate
- Ambassador Program
- About the Alzheimer’s Impact Movement
- Research Funding
- Improving Care
- Support for People Living With Dementia
- Public Policy Victories
- Planned Giving
- Community Educator
- Community Representative
- Support Group Facilitator or Mentor
- Faith Outreach Representative
- Early Stage Social Engagement Leaders
- Data Entry Volunteer
- Tech Support Volunteer
- Other Local Opportunities
- Visit the Program Volunteer Community to Learn More
- Become a Corporate Partner
- A Family Affair
- A Message from Elizabeth
- The Belin Family
- The Eliashar Family
- The Fremont Family
- The Freund Family
- Jeff and Randi Gillman
- Harold Matzner
- The Mendelson Family
- Patty and Arthur Newman
- The Ozer Family
- Salon Series
- No Shave November
- Other Philanthropic Activities
- Still Alice
- The Judy Fund E-blast Archive
- The Judy Fund in the News
- The Judy Fund Newsletter Archives
- Sigma Kappa Foundation
- Alpha Delta Kappa
- Parrot Heads in Paradise
- Tau Kappa Epsilon (TKE)
- Sigma Alpha Mu
- Alois Society Member Levels and Benefits
- Alois Society Member Resources
- Zenith Society
- Founder's Society
- Joel Berman
- JR and Emily Paterakis
- Legal Industry Leadership Council
- Accounting Industry Leadership Council
Find Local Resources
Let us connect you to professionals and support options near you. Please select an option below:
Use Current Location Use Map Selector
Search Alzheimer’s Association

Join Our END ALZ One-Week Match Challenge!
The alzheimer’s association and rippl partner to improve quality dementia care and caregiver support.
— Creating unprecedented access and value that addresses the gap in dementia care for individuals and caregivers —
- Nearly 7 million Americans are living with Alzheimer’s. By 2050, that number will approach 13 million.
- 60% of health care workers believe that the U.S. health care system is not effectively helping patients and their families navigate dementia care.
- A majority of caregivers (70%) report that coordination of care is stressful and 2 in 3 (66%) have difficulty finding resources and support for their needs.
About the Alzheimer's Association
The Alzheimer’s Association is a worldwide voluntary health organization dedicated to Alzheimer’s care, support and research. Our mission is to lead the way to end Alzheimer's and all other dementia — by accelerating global research, driving risk reduction and early detection, and maximizing quality care and support. Our vision is a world without Alzheimer's and all other dementia®. Visit alz.org or call 800.272.3900.
About Rippl
Rippl provides specialty dementia care for patients and caregivers, on demand. Leveraging a value-based approach, disruptive technology, and a relentless focus on empowering and enabling its clinicians, Rippl is pioneering a new care model to dramatically expand access to high quality, wraparound dementia care for seniors, their families and caregivers. ripplcare.com .
Keep Up With Alzheimer’s News and Events
The first survivor of alzheimer's is out there, but we won't get there without you., learn how alzheimer’s disease affects the brain..
Take the Brain Tour
Don't just hope for a cure. Help us find one. Volunteer for a clinical trial.

How Black Mats Can Keep Dementia Patients Safe and Happy
D ementia is a condition that affects millions of people around the world, causing changes in their memory, thinking and behavior. One of the challenges that people with dementia and their caregivers face is wandering, which can lead to accidents, injuries or even death.
Wandering is often triggered by confusion, boredom, anxiety or curiosity. People with dementia may wander because they are looking for something familiar, trying to escape from a stressful situation, or following a habit or routine. Sometimes, they may not even realize that they are wandering.
One of the ways to prevent wandering is to use black mats in front of unsafe areas, such as outside exits. This technique is based on the observation that people with dementia may have visual perception problems, meaning that they may see things differently than they really are.
For example, they may see a dark space on the floor as a hole, and avoid stepping on it due to a fear of falling. This can create a natural barrier that discourages them from leaving the safe zone. This technique is considered an alternative to antipsychotic drugs and lockdown units, which may have negative effects on the person’s dignity, health and well-being.
However, this technique may also raise ethical concerns, as it uses fear and deception to control the person’s behavior. Some people may argue that this is disrespectful and manipulative, and that it may not work for everyone or in every situation.
Chuck Klosterman, a columnist for The New York Times Magazine, addressed this dilemma in his The Ethicist column. He wrote: “When dealing with ethical dilemmas involving those who have lost the ability to reasonably lobby on their own behalf, one must consider what they would most likely prefer if they were still in a position to do so.”
He added: “If a dementia patient were in a position to describe how she would want to be treated, I’d assume she would want the maximum level of independence, the highest degree of protection and the greatest potential for mental clarity. This concept comes closest to achieving those goals.”
The Alzheimer’s Society, a leading charity for people with dementia and their carers, also offers some advice on how to support a person experiencing changes in perception. They suggest: “By responding in a supportive way, you can keep up their confidence and help them to cope with the misunderstanding.”
They also recommend some ways to make the home environment safer and more comfortable for people with dementia, such as using bright colors, clear labels, familiar pictures and avoiding patterns or clutter.
The use of black mats is not the only solution for wandering, but it may be a helpful option for some people with dementia and their caregivers. As Psychiatric Times noted: “The third, a verbal interpretation of the visual deception created by a black mat, is a threat rather than a distraction. Demented patients’ avoidance of dark mats, tiles, or even lines on the floor has long been observed-and sometimes exploited clinically-although we could not locate any studies of the effectiveness and safety of this maneuver.”
Relevant articles:
– How to safeguard against visual pitfalls – Alzheimer’s and Dementia, Alzlive.com, December 12, 2012
– How can dementia change a person’s perception?, Alzheimer’s Society, no date
– A Dark Side of Dementia Care, Psychiatric Times, April 15, 2014
![Dementia is a condition that affects millions of people around the world, causing changes in their memory, thinking and behavior. One of the challenges that people with dementia and their caregivers face is wandering, which can lead to accidents, injuries or even death. Wandering is often triggered by confusion, boredom, anxiety or curiosity. People with […] Dementia is a condition that affects millions of people around the world, causing changes in their memory, thinking and behavior. One of the challenges that people with dementia and their caregivers face is wandering, which can lead to accidents, injuries or even death. Wandering is often triggered by confusion, boredom, anxiety or curiosity. People with […]](https://img-s-msn-com.akamaized.net/tenant/amp/entityid/AA1jvbgL.img?w=768&h=490&m=6&x=762&y=249&s=396&d=396)
Missing in Mexico: Charleston family searching for loved one with dementia
CHARLESTON, S.C. (WCSC) - The family of a Charleston man who suffers from dementia says he has been missing since last Wednesday in Cozumel and they want others in the Lowcountry to be proactive so no one else has to go through this.
Charleston native Edmond Bradley Solomon III just celebrated his 66 birthday at the beginning of the seven-day cruise to Mexico.
“My sister knew it would probably be the last vacation that she was able to take with Brad based on his deterioration over the last couple months,” Ashley Hyer, Solomon’s sister-in-law, said.
Solomon’s family says he has frontotemporal dementia, which is an earlier onset dementia that causes personal, behavioral and emotional changes in one’s personality. The group was shopping along the terminal area docked in Cozumel when Solomon wandered off. Hyer says there’s only been a few sightings since then.
“In a grocery store,” Hyer said. “And the grocery store owner try to approach him and he ran.”
Medical University of South Carolina Neuroscience professor Dr. Heather Boger says wandering is very common for those with dementia. She advises how to best approach the situation if one recognizes a missing person who may have some sort of mental diagnosis.

“Obviously don’t broach the person, but instead follow them,” Boger said. “Contact law enforcement — again, number one response. And try to follow that individual and keep law enforcement on the phone until you have the connection made between the three parties.”
Boger says if someone’s loved one has dementia, to get a tracker. “Baby-proof” or “dementia-proof” the house so they don’t have easy access to things that may harm them. And most importantly, be proactive.
“Be patient with the individual because you don’t understand what they’re going through,” Boger said. “They don’t ultimately understand what they’re going through. And you want to be as patient with them as possible, but make sure you also realize the warning signs so that they’re getting the proper care and attention.”
Trident Area Agency on Aging dementia consultant Don Bagwell agrees that wandering is common and it can even occur with the most attentive caregivers. He says it’s easy to get overwhelmed as a caregiver, but to remember the top priority for the patient is safety.
Bagwell says GPS and technology devices are helpful too, but they have limitations and can offer a false sense of security.
Hyer says Solomon did have a tracker, but only one that works with Bluetooth and Wi-Fi, which stopped pinging about two hours into the search. She says everyone should have some sort of GPS tracker instead.
“That could’ve made all the difference in the world if we had just known,” Hyer said.
When talking about Solomon’s impact on their family, Hyer speaks through tears.
“He adores, Mimi, my sister,” Hyer said. “All he wants to do is be with her. So, he’s a good man.”
As the search continues, the family wants those in the Lowcountry to think about them.
“Pray,” Hyer said. “Pray about this. That Brad is found safe.”
Click here for more information on MUSC’s Memory Disorders Clinic.
Bagwell provided additional documents for a more comprehensive breakdown on keeping your loved ones with dementia safe:
TridentAAA Scans (1) by Live 5 News on Scribd
TridentAAA Scans by Live 5 News on Scribd
FBI Columbia spokesman Kevin Wheeler says they are aware of the missing person report and have been in contact with Mexican authorities, but are unable to comment further.
Royal Caribbean has also not responded for a comment.
A spokesperson for the U.S. State Department released the following statement on Tuesday:
The Department of State has no higher priority than the welfare and safety of U.S. citizens abroad. We are aware of reports of a missing U.S. citizen in Merida, Mexico. When a U.S. citizen is missing, we work closely with local authorities as they carry out their search efforts, and we share information with families however we can. We are monitoring the situation and seeking additional information, and we stand ready to provide consular assistance. We have no further comment at this time.
Copyright 2024 WCSC. All rights reserved.

Walterboro Police confirm body found in suitcase is woman reported missing

Wanted 18-year-old remains at large after Beaufort Co. deputies suspend search

Isle of Palms Police arrest 11, including 4 juveniles during ‘Senior Skip Day’

SLED confirms investigation into SC State Rep. Pendarvis

Mt. Pleasant woman charged with assaulting officer in domestic incident
Latest news.

Group addresses 'disproportionate' SC preschool suspensions for Black children

New report shows 300+ use of force incidents by Charleston police in 2023

VIDEO: Isle of Palms Police arrest 11, including 4 juveniles during ‘Senior Skip Day’

VIDEO: New report shows 300+ use of force incidents by Charleston police in 2023

Personal Perspectives
How to ask for and receive help, personal perspective: asking for help is hard, but it's already helping me heal..
Posted April 10, 2024 | Reviewed by Lybi Ma
It’s hard to ask for help, it may be even harder to need the help. But I do. I need it because tomorrow I'm having a big surgery, spinal fusion at eight levels. This surgery is both known and unknown to me. It’s my third fusion surgery, but my memories of the first two are vague. I remember they hurt a lot. The first was an emergency, so that was a terrorizing and traumatic blur. After the second, I couldn’t swallow solid foods for nearly six months; I remember that part more than anything else. Not being able to eat was awful—I really, really love to eat, especially fried foods.
Anyway, today I am striving to stay in a cautiously optimistic space. It is a wonder and a gift that this surgery is available to me. I have insurance that will pay for (most of) it and I have access to very talented doctors I come from a family of doctors to help me navigate those other doctors. If all goes well, I’ll regain the strength in my right hand and keep the strength in my left. I might even be able to hold my head up without the special backrest that I bring with me everywhere I go. I might be in less overall pain, possibly.
(I have to stop the happy thoughts there because if I think more about what my life would be like with less pain I get too excited. I’d have so much freaking energy. I could go grocery shopping without planning for recovery time. I could stand up to chit-chat at a party or wait in line at the bank. I could go dancing, maybe in high heels. I could sit in the horrible chairs to watch my kid get an award at the school assembly. Maybe, maybe, maybe)
I have thought about all of this before my previous spine surgeries, but because of my condition ( hypermobility-type Ehlers-Danlos Syndrome ), it has been my experience that fusion surgery, while keeping my spine stable, does not make my life much better. But maybe this time.
I am also trying to stay out of the dark place, where I think about pain and dependency and further disability and infection and death. But I wrote this at three o’clock in the morning; you can guess how well that’s going.
I have had so much to do but had a hard time concentrating—finish my taxes, update my advanced healthcare directive, wind down all my open work contracts, and figure out kid-care. But my mind kept wandering, and fighting the fear takes energy. In reality, I spent a lot of time staring into space.
Last week, my sister-in-law sat down with me to create a meal train website for people in my community to deliver food. So many people have offered to help. The minute they hear about the surgery they ask: What can I do? How can I help? I tend to thank them, nod and smile, then go about my business. But here I am, newly divorced , a consultant dependent on being able to work for my income, co- parenting two fabulous children. And I really, really, need the help.
These past few days I’ve been watching the sign-ups roll in on that site, and it makes my heart do funny things. At first, I was uncomfortable, and a little embarrassed. I had to walk away from my computer and stare into space. But then I reminded myself, this is love. This is my people showing up for me. I’m getting a little worried about where we will store all the food that’s coming in my tiny apartment refrigerator (note: this is a much more enjoyable worry than any of the ones listed above). I have help for driving my kid to soccer and frisbee, help to pay someone to come in and clean for a few months, and help with Jen-sitting to keep my spirits up. So much help. And love. And support.

It makes me feel held. Even now, in the darkest hour of the night, when I look at that website I don’t feel so alone. Instead of feeling ashamed, I’m deciding to feel insanely proud that I have built this community that is so willing and ready to surround me. I’m grateful and humbled, and deeply, deeply touched. Those are the emotions I’ll take with me into the operating room, and they are what will help me heal best, whatever that looks like. I know I’ve got this because so many of you have me and that makes me the luckiest person alive.

Jen Sarché is a writer and public health officer who has worked with the Kaiser Family Foundation, the San Francisco Department of Public Health, among others.
- Find a Therapist
- Find a Treatment Center
- Find a Support Group
- International
- New Zealand
- South Africa
- Switzerland
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience
Get the best experience and stay connected to your community with our Spectrum News app. Learn More
Continue in Browser
Get hyperlocal forecasts, radar and weather alerts.
Please enter a valid zipcode.

New Florida law to establish dementia training for law enforcement
TAMPA, Fla. — Gov. Ron DeSantis signed a bill last week that will give law enforcement access to dementia training.
What You Need To Know
Gov. ron desantis signed hb801, which provides training for law enforcement the available training can address possible encounters with those who have dementia the training will be available in october.
The bill, HB801 , provides training for law enforcement and corrections officers, so that they can better recognize and communicate during encounters with people who have dementia.
“The Alzheimer’s Association Florida chapters join caregivers across our state in applauding the Governor and Florida legislature for taking a step to protect our most vulnerable citizens,” said Alex Anderson, vice president of Public Policy at the Alzheimer’s Association Florida chapters . “We encourage all law enforcement agencies to work with the Department of Elder Affairs to roll out dementia training for their staff.”
Kip Corriveau helps care for his father-in-law, who has Alzheimer’s disease. Corriveau said the 89-year-old frequently wanders.
“I literally used to sit in my house with my shoes on at 6, 7 o’clock in the morning,” Corriveau said. “Shoes on, keys in my hand, phone next to me in case he ran out the front door.”
According to the Alzheimer’s Association , 6 in 10 people with dementia will wander. Which is why Corriveau said he joined members of the organization in Tallahassee to lobby for the bill’s passage. Now, with it signed into law, he said families will have some peace of mind.
“Having law enforcement have a better understanding of the disease and how to interact with our loved ones is priceless,” Corriveau said.
The dementia training will be online and available starting in October.

IMAGES
COMMENTS
The Alzheimer's Association suggests 60% of people with dementia will experience wandering at least once. Some may do it repeatedly. It notes that wandering can occur at any stage of dementia ...
Wandering and becoming lost is common among people with Alzheimer's disease or other disorders causing dementia. This behavior can happen in the early stages of dementia — even if the person has never wandered in the past. Understand wandering If a person with dementia is returning from regular walks or drives later than usual or […]
Wandering is a complex behavioral phenomenon that is frequent in dementia. Approximately 20% of community-dwelling individuals with dementia and 60% of those living in institutionalized settings are reported to wander .2 Most definitions of wandering incorporate a variety of dementia-related locomotion activities, including elopement (ie ...
Wandering. Alzheimer's disease causes people to lose their ability to recognize familiar places and faces. It's common for a person living with dementia to wander or become lost or confused about their location, and it can happen at any stage of the disease. Six in 10 people living with dementia will wander at least once; many do so repeatedly.
Reduce the risk of wandering The following tips may help reduce the risk of wandering and can bring peace of mind to caregivers and family members; however, these actions cannot guarantee that a person living with dementia won't wander. Provide opportunities for the person to engage in structured, meaningful activities throughout the day.
Abstract. Wandering behavior is one of the most important and challenging management aspects in persons with dementia. Wandering behavior in people with dementia (PwD) is associated with an increased risk of falls, injuries, and fractures, as well as going missing or being lost from a facility. This causes increased distress in caregivers at ...
According to the Alzheimer's Association, 60% of people living with the disease will wander at least once. Most individuals who wander, wander repeatedly. As you can imagine, wandering is ...
Consider enrolling the person in the MedicAlert® + Alzheimer's Association 24/7 Wandering Support for a Safe Return Program. (link is external) (call 1-800-432-5378 to find the program in your area). Let neighbors and the local police know that the person with Alzheimer's tends to wander. Ask them to alert you immediately if the person is ...
a. address wander-management strategies in the home or supportive care environments for persons with dementia or cognitive decline regardless of whether it was embedded in an environment, was worn, or was implemented as a form of therapy. b. address critical or noncritical wandering in older adults with dementia. c.
Wandering is a common behavior in patients with Alzheimer's disease or other forms of dementia. And once the individual begins to show signs of wandering behaviors, they are at a high-risk of wandering away or becoming lost. This behavior can be very distressing for caregivers, and dangerous for the individual.
Enroll your relative in a dementia wandering response service. MedicAlert's Safe Return program has a 24/7 caregiver hotline in case of dementia wandering at night. Tell the local police or sheriff's department your loved one has dementia and may wander, says Denny.
Wandering (dementia) Wandering occurs when a person with dementia roams around and becomes lost or confused about their location. It is a common behavior that can cause great risk for the person, and is often the major priority (and concern) for caregivers. It is estimated to be the most common form of disruption from people with dementia ...
The Alzheimer Society of B.C. can assist people with dementia and their families to explore a variety of practical strategies to minimize the risk of wandering and to be prepared if wandering does occur. Contact your local Alzheimer Resource Centre or the First Link ® Dementia Helpline at 1-800-936-6033.
Approximately 36% of people with dementia will wander. The top dangers for people who wander include injuries, dehydration, harsh weather exposure, medical complications, drowning, or being hit by a car. Understanding and planning for wandering is vital in caring for someone with dementia.
People with dementia might also experience a phenomenon in the evening or during the night called sundowning. They might feel confused, agitated, anxious and aggressive. Night wandering in this state of mind can be unsafe. Obstructive sleep apnea is also more common in people with Alzheimer's disease. This potentially serious sleep disorder ...
The Alzheimer's and Dementia Care Program provides ongoing care for patients with a dementia diagnosis. Call 310-319-3222 to learn more about dementia care at UCLA Health. Jane's father has been living with her for two years. He often exhibits wandering behaviors such as trying to go leave the house through the front door while saying he ...
Behavioural and psychological symptoms of dementia may be reduced by exercising for at least half an hour, many times a week, although the exact type, duration, and frequency of the exercise remain unknown (including wandering). Summary. People with dementia, including Alzheimer's, may begin to wander at some point, but this may not endure ...
Responding to wandering and exit-seeking behaviors effectively could help people with dementia remain as independent as possible in their homes and communities and help relieve caregiver stress. 1 Hebert, L. E., Weuve, J., Scherr, P. A., & Evans, D. A. (2013). Alzheimer disease in the United States (2010-2050) estimated using the 2010 census.
Inside the home. 11. Look into assistive technology, such as door alarms, pressure mats and GPS tracking devices which could make a huge difference to alerting you should your parent go missing. These devices identify movement, such as the time they left the house, to help finding them quickly. 12.
Sleep disturbances are common in people with dementia and can trigger wandering behavior. For example, a man with dementia who experiences frequent nighttime awakenings may become disoriented and wander around in the dark. 8. Fear or Anxiety. Fear or anxiety can also trigger wandering in some individuals with dementia.
Protect individuals from elopement and wandering: Whether people with dementia intentionally attempt lopement or are simply wandering around to locate a door, those at risk for exiting without the needed supervision may benefit from a door alarm on the exterior doors. Alerts others for assistance: Door alarms can also be used on the bathroom door.
Like most people, a person with dementia may want to spend time walking. Walking is good exercise and can help relieve stress and boredom. However, a person with dementia may walk repeatedly around at home or leave the house during the day or night. When a person with dementia walks about, it is often referred to as 'dementia wandering'.
Alzheimer's & Dementia Wander Safety Products Wandering is the single most critical worry for a caregiver. Those living with Alzheimer's, other forms of Dementia and Memory Loss have a tendency to wander whether they are at home or in unfamiliar surroundings. They are trying to make sense of the world they find themselves in at that moment.
— Creating unprecedented access and value that addresses the gap in dementia care for individuals and caregivers — CHICAGO, April 5, 2024 — Today, the Alzheimer's Association and Rippl announced a partnership designed to revolutionize access to high-quality dementia care across the country. The Dementia Care Navigation Service (DCNS), powered by Rippl and the Alzheimer's Association ...
Wandering is often triggered by confusion, boredom, anxiety or curiosity. People with dementia may wander because they are looking for something familiar, trying to escape from a stressful ...
Midlife, not your 70s or 80s, is when brain changes start to occur that can pave the way toward dementia, Alzheimer's disease and cognitive decline later, according to a growing body of research ...
Trident Area Agency on Aging dementia consultant Don Bagwell agrees that wandering is common and it can even occur with the most attentive caregivers. He says it's easy to get overwhelmed as a caregiver, but to remember the top priority for the patient is safety.
But my mind kept wandering, and fighting the fear takes energy. In reality, I spent a lot of time staring into space. In reality, I spent a lot of time staring into space.
The single most important determinant of quality dementia care across all settings is direct care staff (Alzheimer's Association 2017) • Staffing levels should be adequate to allow for proper care at all times—day and night. • Staff should be sufficiently trained in all aspects of care, including dementia care. • Staff should be adequately compensated for their valuable work.
According to the Alzheimer's Association, 6 in 10 people with dementia will wander. Which is why Corriveau said he joined members of the organization in Tallahassee to lobby for the bill's ...