Wandering Spleen Volvulus: A Case Report and Literature Review of This Diagnostic Challenge
Affiliations.
- 1 Department of Thoracic Surgery, University Hospital of Lausanne (CHUV), Lausanne, Switzerland.
- 2 Department of General Surgery, Hospital of Valais (CHVR), Sion, Switzerland.
- PMID: 32868755
- PMCID: PMC7483514
- DOI: 10.12659/AJCR.925301
BACKGROUND Wandering spleen is a rare condition in which the spleen lacks the usual peritoneal attachments, resulting in increased intra-abdominal mobility. Complications can occur due to the torsion of the splenic vascular pedicle, resulting in symptoms ranging from an incidental finding to an acute abdomen as a result of an ischemic necrosis of the spleen. CASE REPORT We present the case of a 25-year-old female patient who presented with a recurring abdominal pain associated with serum lipase and C-reactive protein elevation. The computed tomography scan revealed torsion of the splenic pedicle and hypoperfusion of the spleen. A surgical exploration was performed and a wandering spleen was diagnosed perioperatively. It was characterized by the lack of peritoneal ligaments, thus resulting in a splenic volvulus. A splenectomy was carried out due to the definite ischemic necrosis of the spleen. CONCLUSIONS The diagnosis of this rare condition can be very challenging since it can be presented with a vast variety of symptoms, mimicking other abdominal pathologies. The intermittent nature of an ultimate splenic torsion can add to the diagnostic challenge. Medical literature concerning the wandering spleen and knowledge about this pathology originates mainly from individual case reports. Despite the evolving diagnostic modalities available, this rare and ambiguous disorder remains misdiagnosed, and a high index of suspicion is needed for the appropriate diagnosis to be established.

Publication types
- Case Reports
- Abdomen, Acute*
- Intestinal Volvulus* / diagnostic imaging
- Intestinal Volvulus* / surgery
- Splenic Diseases*
- Torsion Abnormality / diagnostic imaging
- Torsion Abnormality / surgery
- Wandering Spleen* / diagnostic imaging
- Wandering Spleen* / surgery
- Case Report
- Open access
- Published: 26 November 2022
The wandering spleen: case report of laparoscopic splenectomy in a pregnant woman
- Lorenzo Crepaz ORCID: orcid.org/0000-0002-7918-7212 1 ,
- Alberto Di Leo 1 ,
- Giuseppe Borzellino 2 ,
- Paola Pomini 3 &
- Michele Genna 2
Bulletin of the National Research Centre volume 46 , Article number: 273 ( 2022 ) Cite this article
1330 Accesses
Metrics details
Wandering spleen is a rare condition, which is characterized by augmented mobility of the spleen, due to congenital or acquired causes. It is more frequent in multiparous women, but only a few cases are reported during pregnancy. Wandering spleen is usually asymptomatic until the onset of its possible complications, and this can mislead clinicians in reaching the correct diagnosis.
Case presentation
We report the case of a wandering spleen with acute splenic infarction in a pregnant woman and its minimally invasive surgical treatment, focusing on the clinical and radiological findings that could mislead or drive clinicians to the right diagnosis, or a potential disaster.
Conclusions
Splenic preservation in the wandering spleen where it is safe and possible is the main goal of the treatment. Clinical and radiological findings are the most relevant elements to drive surgical treatment. To reach the best and opportune treatment for the patient, the wandering spleen is an insidious condition and must be included in the differential diagnosis in the acute abdomen diagnostic process.
Wandering spleen (WS) is a rare and still relatively unknown condition. It is characterized by augmented mobility of the spleen, due to a congenital lack of splenic ligaments or an acquired increased laxity of these structures.
This relaxation of the tissues may lead to spontaneous torsions of the splenic hilum, with possible subsequent acute or chronic ischemic infarctions of the spleen, making WS a deceptive and misleading condition.
Until 2012 WS cases reported in the medical literature were about 500 worldwide, almost a 0.5% of splenectomies performed (Puranik et al. 2017 ). Since 2012, there have been reported in the literature almost 150 new cases.
The real incidence of this pathology is surely underestimated because of the healthy carriers, making WS a silent condition until the appearance of its complications, which could also be life-threatening.
Most of the cases are reported in childbearing-age women, in particular multiparous ones. It is probably related lo the augmented laxity of the tissue due to hormonal values acquired during pregnancies.
This hypothesis is confirmed by the observation of an asymmetrical distribution of WS in the adult population between females and males, with a proportion of approximately 7:1 (Wang et al. 2020 ).
The second peak incidence is in the pediatric population, with equal distribution between males and females, and a medium age of fewer than 10 years old (Wang et al. 2020 ; Antona et al. 2022 ). In these cases, the WS is probably related to a congenital lack of splenic ligaments, giving the organ augmented mobility and subsequent possible acute and/or chronic torsion on its longitudinal axis.
WS rests usually unknown until the appearance of a complication, such as chronic or acute ischemic damage, resulting from the torsion of the vascular axis, leading to potentially life-threatening conditions (Sentürk et al. 2022 ).
For this reason, there are no clear clinical features related to WS, because it depends on the phases of the splenic wandering and could remain undiagnosed all lifelong.
In the medical literature, there are only a few cases of WS during pregnancy (Parvaiz et al. 2004 ; Yücel et al. 2012 ), getting to complex and dangerous clinical pictures, complicated by the coexistence of the fetus.
A similar diagnosis later than our case report in pregnancy (e.g., last trimester) has not occurred yet as far as we know; it could potentially become delicate and dangerous to manage and must hold into consideration the WS vascular state, and the feasibility of an urgent surgical approach. Limitations of this paper are strongly linked to the case report essence, describing a single pathological situation, that is not necessarily applicable to different clinical circumstances.
This study is a case report regarding WS and a case report of the most advanced gestational age WS during pregnancy, as far as we know in the medical literature.
This case report has been reported in line with the SCARE criteria (Agha et al. 2020 ).
LZ, is a 31-year-old Caucasian white woman, normal weight (BMI 20 kg/m 2 ), primigravida, with no pathological history, pharmacologic chronic therapy, or allergies reported.
Mild thrombocytopenia was found in previous blood examinations, with a minimum value of 959 platelets/L in 2016, never examined with second-level examinations.
During the first obstetrical ultrasound check, a vascularized and capsulated mobile mass in the abdomen was detected, with a major axis of 12.5 cm, characterized by a hypertrophic and elongated hilar vascular axis. In parallel, there was no spleen in the left hypochondrium, confirming the WS diagnosis.
The WS had some parenchymal calcific strias, per previous parcellar ischemic infarctions.
This condition was asymptomatic, and the physical examination was negative for any pathological finding, with no palpable masses, and no abdominal evocable pain.
The result of the multidisciplinary consult executed was an indication of the close monitoring of WS through frequent ultrasound examinations and blood examinations, with conservative treatment because of the initial weeks of the pregnancy.
During week 17th of the pregnancy, the patient had blood examinations, demonstrating a reduction of platelets (PLTs) count to 879/L, with the stability of the WS in ultrasound check.
MRI has been planned to have more precise information and set the best treatment for the patient. During the waiting days for the scheduled MRI, on October 30, 2019, in course of the 22nd week of pregnancy, the patient got to the ER because of the onset of intense and diffuse abdominal pain during the night, without fever or any other clinical manifestation. Clinical examination confirmed the relevant widespread abdominal pain, Blumberg sign absent.
Blood examinations performed in the ER were in the range of normality, except for further thrombocytopenia, with a PLTs count of 749/L.
An urgent ultrasound examination was performed, observing the augmented volume of the WS (diameter 18 × 8 cm) and parenchymal ischemic injury; no vascular signal was detected at the splenic hilum with color Doppler technique, without free fluid in the belly (Fig. 1 ).

Abdominal ultrasound executed in ER and evidence of ischemic areas in the splenic parenchyma
For this reason, the patient underwent an urgent surgical procedure.
A laparoscopic approach was decided, noticing a hypertrophic mobile spleen in subhepatic space, surrounded by a multitude of ectasic and congested vessels. The principal vascular axis of the WS was also hypertrophic, with a diameter of around 4 cm (Fig. 2 ).
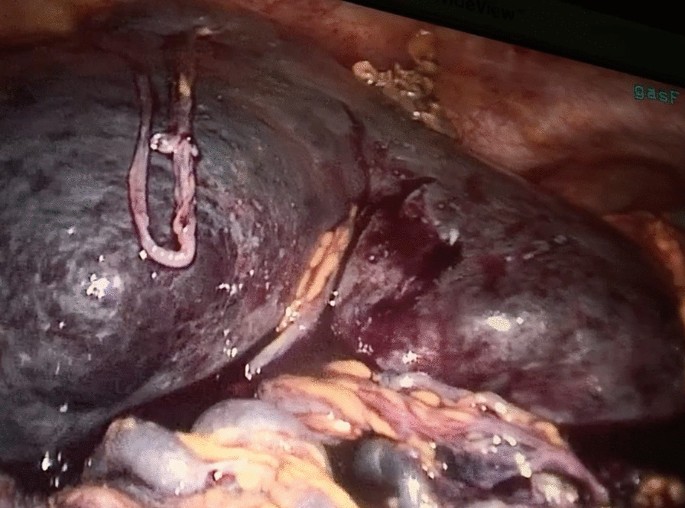
Splenic infarction with hypertrophic hilar vessels
After initial mobilization of the WS, partial dissection of the perisplenic vessels, and isolation of the principal vascular axis, a median mini-laparotomy was performed to dissect and tie the hypertrophic splenic vessels with non-resorbable suture (Fig. 3 ).
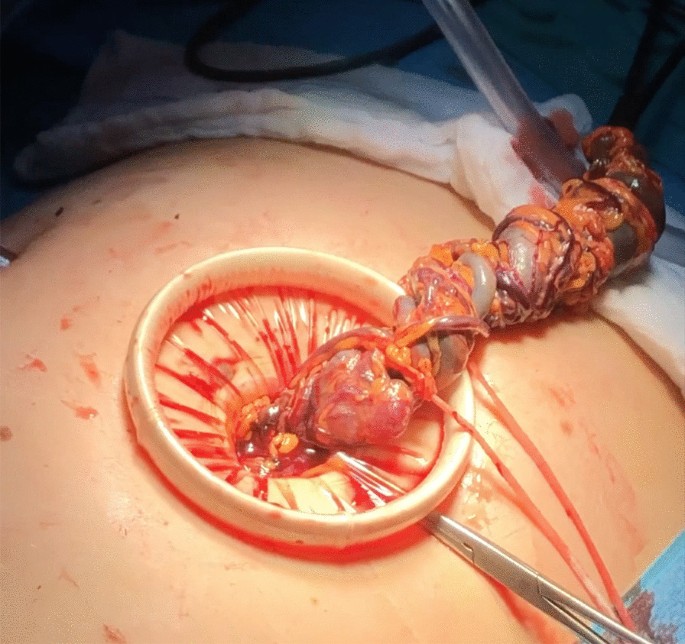
Interrupted hilar vessels through mini-laparotomy
Using laparoscopy, a complete mobilization of the WS was performed from its remaining ligaments.
Subsequent extraction of the spleen from the laparotomy was executed from the service laparotomy. Fetal parameters resulted in physiological and unaltered after surgery.
The postoperative course was regular and the PLTs count normalized in a few weeks, with a median of 300 9 /L. Subsequent blood examinations confirmed the normalization of PLTs values (Fig. 4 ).
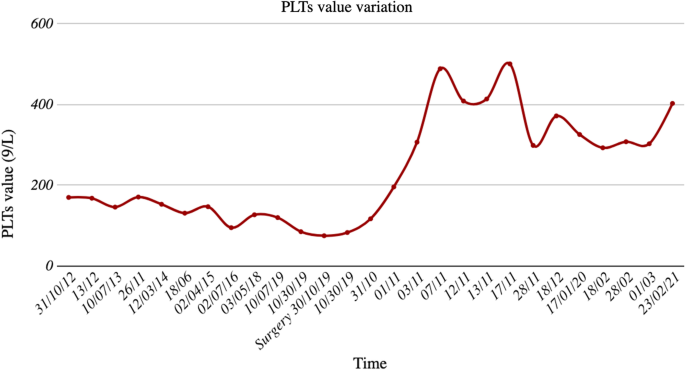
Variation of platelets value in time, in relation to urgent surgical intervention
The patient had natural childbirth at week 39th with no complications.
The patient, two weeks after delivery, received Streptococcus Pneumoniae , Haemophilus Influenzae , and Neisseria Meningitidis vaccinations, as standard prevention for most frequent severe infections after splenectomy.
WS is a rare and insidious condition, with many different possible manifestations, from asymptomatic patients to urgent and emergencies, requiring prompt and opportune diagnosis and treatment, making this condition very challenging for clinicians.
This case report describes a borderline case within a rare pathological entity, with pregnancy as an element of high risk.
WS is a diagnosis that must be included in the differential diagnosis in particular cases, such as multiparous women with an abdominal palpable mass or recurrent and vague abdominal pain.
The increase in WS diagnosis is supported by a constant and rapid improvement in radiological technique, getting more easily and accurately diagnosed in elective and acute examinations, making WS a less misdiagnosed life-threatening pathological entity, not only in multiparous women.
WS knowledge is principally based on an increasing number of single case reports, such as this one, driving clinicians to manage this rare and complex diagnosis, both in emergency and elective surgery.
A better understanding of WS etiopathogenesis is important to reach a complete comprehension of its pathological mechanisms, to get a better diagnostic and therapeutic ability, and to prevent a possible life-threatening condition.
Further studies are necessary to obtain a full understanding of WS’s genesis, to get a unique and standard diagnostic and therapeutic guidelines, making WS the best-known and less dangerous condition.
Availability of data and materials
All the data and images are originals and disposable upon request to the corresponding author.
Abbreviations
- Wandering spleen
Body mass index
Emergency room
Agha RA, Franchi T, Sohrabi C, Mathew G, Kerwan A, SCARE Group (2020) The SCARE 2020 Guideline: updating consensus surgical CAse report (SCARE) guidelines. Int J Surg 84:226–230. https://doi.org/10.1016/j.ijsu.2020.10.034
Article PubMed Google Scholar
Antona G, Arredondo Montero J, Ros Briones R, Bronte Anaut M, Moreno Ibérico MA, Bardají Pascual C (2022) Pediatric splenic torsion in an orthotopic spleen without fixation elements. J Pediatr S0022–3476(22):00730–00732. https://doi.org/10.1016/j.jpeds.2022.08.021
Article Google Scholar
Parvaiz A, Chandran S, Karim A, Kumar K, Jeffrey P, Lagattolla NR (2004) Torted and ruptured wandering spleen presenting as a surgical emergency in pregnancy. Sci World J 4:1035–1037. https://doi.org/10.1100/tsw.2004.208
Article CAS Google Scholar
Puranik AK, Mehra R, Chauhan S, Pandey R (2017) Wandering spleen: a surgical enigma. Gastroenterol Report 5(3):241–243. https://doi.org/10.1093/gastro/gov034
Sentürk M, Kasikci YS (2022) Wandering spleen, which is torsioned with the distal pancreas. Distal pankreas ile birlikte torsiyone olan gezici dalak. Turk J Trauma Emerg Surg 28(9):1363–1365. https://doi.org/10.14744/tjtes.2021.34288
Wang Z, Zhao Q, Huang Y, Mo Z, Tian Z, Yang F, Wang Y, Yao L (2020) Wandering spleen with splenic torsion in a toddler: a case report and literature review. Medicine 99(37):e22063. https://doi.org/10.1097/MD.0000000000022063
Article PubMed PubMed Central Google Scholar
Yücel E, Kurt Y, Ozdemir Y, Gun I, Yildiz M (2012) Laparoscopic splenectomy for the treatment of wandering spleen in a pregnant woman: a case report. Surg Laparosc Endosc Percutaneous Tech 22(2):e102–e104. https://doi.org/10.1097/SLE.0b013e318246beb5
Download references
Acknowledgements
Not applicable.
The authors received no financial support for this article's research, authorship, and/or publication.
Author information
Authors and affiliations.
Unit of General and Mini-Invasive Surgery, San Camillo Hospital, Trento, Italy
Lorenzo Crepaz & Alberto Di Leo
Department of Surgery, University Hospital of Verona, Verona, Italy
Giuseppe Borzellino & Michele Genna
Department of Obstetrics and Gynecology, University Hospital of Verona, Verona, Italy
Paola Pomini
You can also search for this author in PubMed Google Scholar
Contributions
LC and ADL wrote the manuscript. LC, GB, and PP took part in the surgical procedure described in the present paper. LC and MG managed preoperative and postoperative indications. All authors have read and approved the manuscript.
Corresponding author
Correspondence to Lorenzo Crepaz .
Ethics declarations
Ethics approval and consent to participate.
No ethical approval statement was required for this study. Fully informed written consent was obtained for surgery.
Consent for publication
Informed consent was obtained for publication.
Competing interests
The authors certify that they have no affiliations with or involvement in any organization with any financial interest in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Crepaz, L., Di Leo, A., Borzellino, G. et al. The wandering spleen: case report of laparoscopic splenectomy in a pregnant woman. Bull Natl Res Cent 46 , 273 (2022). https://doi.org/10.1186/s42269-022-00960-4
Download citation
Received : 07 October 2022
Accepted : 16 November 2022
Published : 26 November 2022
DOI : https://doi.org/10.1186/s42269-022-00960-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Acute abdomen
- Case report
- Case report
- Open access
- Published: 01 May 2014
A torted wandering spleen: a case report
- Aman Sharma 1 &
- Gisella Salerno 2
Journal of Medical Case Reports volume 8 , Article number: 133 ( 2014 ) Cite this article
3193 Accesses
17 Citations
Metrics details
Introduction
A torted wandering spleen is a rare clinical occurrence with fewer than 500 cases reported and an incidence of less than 0.2%. It is brought about through laxity of the gastrosplenic and splenorenal ligaments; however, the precise aetiology remains unknown. It can prove to be a diagnostic challenge with high mortality if misdiagnosed.
Case presentation
We present the case of a 27-year-old woman of Arabic ethnicity, who complained of a short history of severe abdominal pain with the background of recurrent abdominal pain and vomiting. An abdominal computerized tomography scan revealed a torted wandering spleen. This required a splenectomy due to splenic infarction.
This report highlights the investigations and management necessary for a patient who presents with an ischaemic torted wandering spleen.
Peer Review reports
A wandering spleen is a rare clinical occurrence with fewer than 500 cases reported and an incidence of less than 0.2% [ 1 , 2 ]. The spleen is an important component of the reticuloendothelial system, which is involved in immunological defence and can serve as a storage site for red blood cells [ 3 ].
The spleen is normally supported by the gastrosplenic, splenorenal and splenocolic ligaments, whereby failure of attachment of these ligaments to the spleen’s overlying peritoneum results in a hypermobile spleen [ 3 , 4 ]. All cases of a wandering spleen have been found associated with a long splenic pedicle which consists of the splenic vessels and the tail of the pancreas [ 2 – 4 ].
A wandering spleen can be either congenital or acquired. In the congenital condition the ligaments fail to develop properly, whereas in the acquired form the hormonal effects of pregnancy and abdominal wall laxity are proposed as determining factors [ 5 – 7 ]. In addition, failure of fusion of the dorsal mesogastrium during foetal development resulting in the characteristic long vascular pedicle has been attributed [ 8 ]. However, the precise aetiology of the wandering spleen is not known [ 2 ].
A 27-year-old woman of Arabic ethnicity, presented to the emergency department with a 24-hour history of central abdominal pain which she described as a tight band spanning from her right lumbar region to her left lumbar flank. The pain was of sudden onset, scored 10/10 and exacerbated by movement and eating. There was associated vomiting; clear vomitus and no haematemesis. Her bowels were opening regularly and there was no reported blood in her stools.
Prior to this, she presented to the emergency department four times within the last year, for a milder pain in her left iliac fossa radiating to her back, described as stabbing in nature. She did not have any lower urinary tract or any gynaecological symptoms. During these admissions she was treated for renal colic.
Her past medical history entailed oesophageal gastric reflux with no history of any connective tissue disorders.
On examination, she appeared in discomfort, was apyrexial but had a tachycardia of 117 beats per minute, with otherwise normal cardiorespiratory function.
Her abdomen was soft, with generalised tenderness, but specifically more in her right iliac fossa and left upper quadrant. Rovsing’s sign was negative and bowel sounds were sluggish.
On admission her haemoglobin was 11.7g/dL, white cell count 16.6×10 9 /L, neutrophils 14.8×10 9 /L, her renal, liver function, amylase and lactate were within normal limits.
An abdominal radiograph showed distended small and large bowel loops in the left upper quadrant and paucity of bowel gas in the rest of the image. A chest radiograph was normal.
She was resuscitated with intravenous fluids, given analgesia, antiemetics and started on antibiotics on the basis of an initial diagnosis of appendicitis, because the most tender point in her abdomen was in the right iliac fossa. However, further imaging was requested as the distribution of large bowel gas on the abdominal radiograph seemed abnormal.
An ultrasound (US) of her abdomen showed free fluid throughout her abdomen and pelvis. In the midline of her abdomen was a homogenous mass which resembled the spleen; no blood flow could be elicited on Doppler. The left upper quadrant contained no splenic tissue.
An urgent computed tomography (CT) was done (Figures 1 and 2 ) which showed a grossly enlarged spleen at 17cm, with a long mesentery, located in her mid-abdomen. It was torted with resultant splenic infarction. In addition there was swirling of the splenic vessels as they passed inferiorly into her abdomen towards the spleen, which lay above her pelvis. The left upper quadrant showed no splenic tissue but multiple loops of thickened small bowel and free fluid throughout her abdomen and pelvis. Liver, gallbladder, kidneys and adrenals were reported as normal. Her appendix was identifiable and normal, with pelvic organs being unremarkable.

Left upper quadrant filled with small bowel.

Lower abdomen/pelvis showing spleen.
She was prepared for urgent laparotomy with findings of an infarcted wandering spleen in her mid-abdomen. Her spleen was enlarged to 20cm at its maximum diameter due to venous congestion and resultant infarction. There were no ligamentous attachments to her spleen and the tail of her pancreas was attached to the hilar vessels of her spleen which were on a long mesentery. The infarct was due to 360° twisting of the splenic hilum around the tail of her pancreas. Of note her caecum, right and transverse colon were dilated but there was no obstruction, and her small bowel and appendix were normal (Figures 3 , 4 , 5 and 6 ).

Image of torted spleen.

Image of resected spleen.

Postsplenectomy.
Her spleen was unrotated, her hilar vessels were divided close to her spleen with LigaSure™, taking care to preserve the tail of her pancreas, and a splenectomy was performed. The ends of her hilar vessels and pancreatic tail were closed with 1.0 Vicryl sutures. A saline washout was done, and a left Robinson drain was left at the pancreatic tail site, and a right Robinson drain left in her pelvis.
The histology report concluded that within her spleen there was extensive haemorrhagic tissue with a few small residual lymphoid aggregates. A few blood vessels with neutrophilic infiltration were present and the hilum showed blood vessels with minimal intraluminal neutrophilic exudate and neutrophilic infiltration of the vessel wall. In addition there was a surrounding small abscess formation within the hilar tissue. The features were consistent with splenic infarction of ischaemic origin. However, there was no evidence of granuloma or malignancy.
Her postoperative recovery was good; she was started on long-term penicillin V and was given Haemophilius influenza type B, meningococcal and pneumococcus vaccinations 2 weeks after her splenectomy. She was also commenced on long-term aspirin for postsplenectomy thrombocythaemia. The drains were removed after her amylase level was checked and found to be within normal serum levels.
A literature review conducted by Buehner and Baker [ 3 ] concluded that patients most commonly presented with: an asymptomatic mass, in the subacute setting with nonspecific gastrointestinal complaints and could also present with an acute abdomen [ 3 ]. The use of biochemical blood tests has been found to be nonspecific in terms of helping with diagnosis. [ 3 ].
Symptoms may remain quiescent over long periods, but complications are related to torsion or compression of abdominal organs [ 3 ]. These can include pancreatitis, bowel obstruction, gastric volvulus, gastric and duodenal compression and most commonly splenic infarction [ 7 ]. Splenomegaly is usually a result of torsion of the pedicle and splenic sequestration.
A wandering spleen usually presents between the ages of 20 and 40 years, being more common in women [ 9 , 10 ]. Children make up one-third of cases, with an equal preponderance in boys and girls under 10 years [ 9 ].
US imaging with duplex scanning can be used as an initial mode of imaging which can show the position of the wandering spleen with concomitant replacement of bowel in the left upper quadrant [ 7 ]. CT contrast imaging is the preferred mode of investigation, with the contrast helping to elucidate the viability of the spleen [ 6 , 7 ]. The most characteristic finding is the absence of the spleen in its normal position and an ectopic mass found somewhere else in the abdomen or pelvis [ 6 ]. The whirl sign of the splenic pedicle and surrounding fat is specific for splenic torsion as was the case with our patient [ 5 , 6 ].
Splenopexy is the choice of treatment if the spleen is not infarcted but a splenectomy proceeding detorsion is necessary if there is any sign of infarction [ 3 , 11 – 13 ]. This should be appropriately followed up by the prophylactic vaccines against postsplenectomy sepsis syndrome. Ideally they should be administered before surgery; however, in emergencies this is not always possible.
Conclusions
The wandering spleen is a rare differential diagnosis of an acute abdomen but must be considered if a patient presents with abdominal pain associated with a palpable mass and displacement of bowel loops to the left upper quadrant. The best method of confirming the diagnosis seems to be a CT scan, however, US imaging is an equally helpful modality.
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Abbreviations
Computed tomography
Ultrasound.
Raissaki M, Prassopoulos P, Daskalogiannaki M, Magkanas E, Gourtsoyiannis N: Acute abdomen due to torsion of wandering spleen: CT diagnosis. Eur Radiol. 1998, 8: 1409-1412. 10.1007/s003300050562.
Article CAS PubMed Google Scholar
Satydas T, Nasir N, Bradpiece HA: Wandering spleen: case report and literature review. J R Coll of Surg Edin. 2002, 47: 512-514.
Google Scholar
Buehner M, Baker MS: The wandering spleen. Surg Gynecol Obstet. 1992, 175: 373-
CAS PubMed Google Scholar
Desai DC, Hebra A, Davidoff AM, Schnaufer L: Wandering spleen: a challenging diagnosis. South Med J. 1997, 90: 439-10.1097/00007611-199704000-00017.
Gomez D, Patel R, Rahman SH, Guthrie JA, Menon KV: Torsion of a wandering spleen associated with congenital malrotation of the gastrointestinal tract. Int J Radiol. 2006, 5: 1-
Ben Elya A, Zissinb R, Copela L, Vassermana M, Hertzc M, Gottlieba P, Gayera G: The wandering spleen: CT findings and possible pitfalls in diagnosis. Clin Radiol. 2006, 61: 954-958. 10.1016/j.crad.2006.06.007.
Article Google Scholar
Karmazyn B, Steinberg R, Gayer G, Grozovski S, Freud E, Kornreich L: Wandering spleen-the challenge of ultrasound diagnosis: report of 7 cases. J Clin Ultrasound. 2005, 33: 9-
Allen KB, Gay BB, Skandalakis JE: Wandering spleen: anatomic and radiologic considerations. South Med J. 1992, 85: 976-984. 10.1097/00007611-199210000-00011.
Dawson JH, Roberts NG: Management of the wandering spleen. Aust N Z J Surg. 1994, 64: 441-444. 10.1111/j.1445-2197.1994.tb02249.x.
Steinberg R, Karmazyn B, Dlugy E, Gelber E, Freud E, Horev G, Zer M: Clinical presentation of wandering spleen. J Pediatr Surg. 2002, 37: 30-
Steele RD: A torted pelvic spleen. Aust N Z J Surg. 1988, 58: 157-159. 10.1111/j.1445-2197.1988.tb01027.x.
Rodkey ML, Macknin ML: Pediatric wandering spleen: case report and review of the literature. Clin Pediatr (Phila). 1992, 31: 289-294. 10.1177/000992289203100505.
Article CAS Google Scholar
Gunning KA, Rosenberg IL: Symptomatic wandering spleen. Br J Surg. 1993, 80: 93-10.1002/bjs.1800800130.
Download references
Acknowledgements
We would like to acknowledge the Radiology department at Wexham Park Hospital for providing their assistance in reporting the imaging.
Author information
Authors and affiliations.
FY2 in Paediatric Surgery at John Radcliffe, Headley Way, Oxford, OX3 9DU, UK
Aman Sharma
Wexham Park General Surgery Hospital, Slough, UK
Gisella Salerno
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Aman Sharma .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contributions
AS made substantial contributions to: conception, design, acquisition of data, analysis and interpretation of data and was involved in drafting the manuscript. GS was involved in revising the manuscript critically for important intellectual content. Both authors read and approved the final manuscript.

Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Authors’ original file for figure 2, authors’ original file for figure 3, authors’ original file for figure 4, authors’ original file for figure 5, authors’ original file for figure 6, rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Sharma, A., Salerno, G. A torted wandering spleen: a case report. J Med Case Reports 8 , 133 (2014). https://doi.org/10.1186/1752-1947-8-133
Download citation
Received : 25 November 2013
Accepted : 18 March 2014
Published : 01 May 2014
DOI : https://doi.org/10.1186/1752-1947-8-133
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Gastrosplenic
- Hypermobile
- Splenectomy
- Splenorenal
Journal of Medical Case Reports
ISSN: 1752-1947
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Search Menu
- Volume 2024, Issue 4, April 2024 (In Progress)
- Volume 2024, Issue 3, March 2024
- Bariatric Surgery
- Breast Surgery
- Cardiothoracic Surgery
- Colorectal Surgery
- Colorectal Surgery, Upper GI Surgery
- Gynaecology
- Hepatobiliary Surgery
- Interventional Radiology
- Neurosurgery
- Ophthalmology
- Oral and Maxillofacial Surgery
- Otorhinolaryngology - Head & Neck Surgery
- Paediatric Surgery
- Plastic Surgery
- Transplant Surgery
- Trauma & Orthopaedic Surgery
- Upper GI Surgery
- Vascular Surgery
- Author Guidelines
- Submission Site
- Open Access
- Reasons to Submit
- About Journal of Surgical Case Reports
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, case presentation.
- < Previous
Infarcted wandering spleen: A case report from Saudi Arabia
- Article contents
- Figures & tables
- Supplementary Data
Raid Alghamdi, Amer Alzahrnai, Abdulaziz Alosaimi, Ibrahim Albabtain, Infarcted wandering spleen: A case report from Saudi Arabia, Journal of Surgical Case Reports , Volume 2021, Issue 6, June 2021, rjab277, https://doi.org/10.1093/jscr/rjab277
- Permissions Icon Permissions
Spleen is normally positioned in the left upper quadrant. Abnormal location where it is not found in its normal anatomical position is called wandering spleen (WS). Wandering spleen is a rare medical condition that occurs due to developmental abnormality or acquired laxity of the ligaments that hold the spleen in its normal anatomical position. It affects children and young adults, especially childbearing age women. Patients affected with this condition may present with nonspecific symptoms requiring a high index of suspicion. Here, we are presenting a 20-year-old female known to have WS ended up with infarcted WS requiring emergency splenectomy.
Spleen is normally positioned in the left upper quadrant. Abnormal location where it is not found in its normal location is called Wandering spleen (WS). WS is a rare medical condition that occurs due to developmental abnormality or acquired laxity of the ligaments that hold the spleen in its normal anatomical position. It affects children and young adults, especially childbearing age women. Patients affected with this condition may present with nonspecific symptoms requiring a high index of suspicion. Here, we are presenting a 20-year-old female known to have WS ended up with infarcted WS.
A 20-year-old female, not married, presented to the emergency department with severe left lower quadrant abdominal pain for one day. The pain is continuous described as dull in nature none radiating with history of previous similar milder attacks. The patient denies any lower urinary tract symptoms, nausea, vomiting, chills, rigors, diarrhea and trauma. She reports regular periods and her last menstrual period was three weeks ago.
The patient is known to have William syndrome with a past surgical history of atrial septal defect repair when she was 8 years of age. She is following with cardiac surgery as she was recently diagnosed to have mitral valve prolapse with severe mitral regurgitation planned for surgery.
On examination, she looked well but in pain. Heart rate 107 beats per minute and a blood pressure of 141/69 mmHg. Her temperature was 36.8°C and saturating well on RA 100%. Her abdominal examination positive only for moderate left lower quadrant tenderness and palpable tender mass in the left lower quadrant, soft abdomen with no signs of peritoneal irritation nor abdominal distention.
Her laboratory investigations were unremarkable aside from mild leukocytosis with a white cell count of 16 d/L. Computed tomography (CT) abdomen with intravenous contrast revealed twisted wandering dysmorphic spleen in the left mid abdomen with subsequent infarction ( Fig. 1 ).
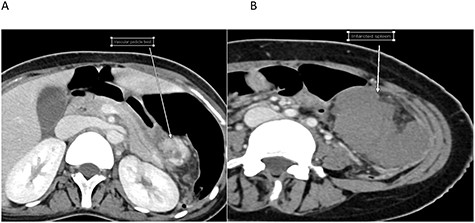
Cross-sectional images of the same patient at the time of infarction. A. Twisted pedicle. B. Infarcted WS.
Upon reviewing her file, she had a CT scan done two years prior to this presentation for an abdominal pain and it confirmed the diagnosis of WS; however, no treatment options were offered to her with no follow-ups ( Fig. 2 ).

Cross-sectional image at the time initial diagnosis shows normal enhancement.
Patient was then pushed to the operating theater for diagnostic laparotomy and possible splenectomy. Abdomen was explored an 8-cm midline incision revealing a wondering spleen in the mid abdomen connected only with colonosplenic ligament with twisted splenic pedicle. Splenectomy performed and patient was shifted to postanesthesia care unit in stable condition ( Fig. 3 ). Hospital course was unremarkable and patient was kept in the hospital for three days for observation then discharged home.
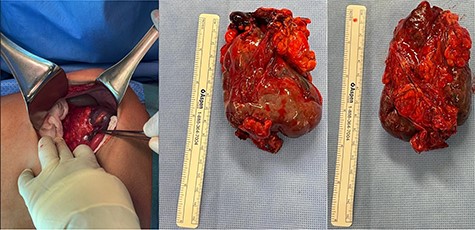
Intraoperative clinical photographs showing infarcted malformed WS.
WS is a rare condition that is characterized by laxity or sometimes absence of the ligaments that hold the spleen in its normal anatomical position [ 1 ]. The incidence of WS is estimated to be 0.2% [ 2 ]. It has a female predominance and the most common age of presentation is childhood, and in adults, if affects female of childbearing age [ 1 , 3 ]. It has been hypothesized that laxity of the ligaments that hold the spleen is due to effects of estrogen [ 4 ]. Moreover, maldevelopment or absence of the suspensory ligaments is another proposed caused of this rare condition [ 5 ].
Statistically, it is 2.5 times more common in males under the age of 1 year. However, it is seven times more common in females after age 10. The most common age of clinical presentation is variable. It can be asymptomatic and discovered only on imaging or during clinical examination as a palpable mass and may never be symptomatic [ 6 ]. While another set of patients might present with recurrent attacks of abdominal pain due to torsion and spontaneous detorsion of the splenic pedicle. Acute surgical abdomen is more serious presentation secondary to splenic torsion and subsequently acute splenic infarction, a life-threatening condition [ 7 ].
Our patient has a previous presentations for a milder abdominal pain attacks; this is could be related to her malformed spleen being subjected to torsion and detorsion. Her first attack was two years prior to this presentation for which she had a CT scan confirming the presence of WS. One case report of a young married woman was published in the year 2020 with a history of recurrent abdominal pain with an US showed no spleen in the LUQ, that was suggestive of WS; however, family ignored to complete full investigations. This case presented five months later with an acute abdomen ended up with emergency laparotomy and splenectomy due to infarcted WS. This highlights the importance of family and patient education as well as planned follow-ups [ 2 ].
Diagnostic modalities include CT, magnetic resonance imaging or doppler ultrasound can help to confirm the diagnosis; however, CT scan remains the investigation of choice not only to confirm the diagnosis of WS but more importantly to rule out other causes of acute abdomen as this condition can mimic other pathologies especially in women of childbearing age where it can present as ovarian torsion or rupture ectopic pregnancy [ 8 ].
Findings on CT scan include absence of spleen in its normal position, lower pelvic mass representing the malpositioned spleen, homogenous or heterogeneous splenic parenchyma with loss of attenuation [ 9 ].
The case presented came with acute abdominal pain and CT scan out of its normal anatomical position was already evident on her previous scans and twisted pedicle with infarcted spleen warranting exploratory laparotomy and eventually splenectomy. WS can be complicated with hypersplenism, splenic infarction, portal hypertension and/or mesenteric varices. Portal hypertension and mesenteric varices is a rare complication and was already reported in the literature, which was hypothesized to be due to mechanical effect of the malpositioned spleen on the extrahepatic portal vasculature [ 10 ].
Up to date, the only recommended treatment is operative even in asymptomatic patient due to high rate of complications without removing the spleen. Surgical options can be formal splenectomy laparoscopic or open in case of infarcted spleen or splenopexy as a viable option and as a splenic preservation modality for young patients and those with high risk for overwhelming postsplenectomy sepsis [ 11 ].
WS remains a rare cause of acute abdominal pain. I acknowledge changes, diagnosis is difficult sometimes; however, when torsion and infarction happens patient will present with acute surgical abdomen requiring emergency splenectomy or splenopexy in a salvageable spleen. We recommend regular follow-ups for patient whom the diagnosis of WS is established and possible splenopexy as viable option to prevent future complications. Future studies are needed for this rare disease in order to improve identifying, monitoring and following up those patient before complication occurs.
Varga I , Galfiova P , Adamkov M , Danisovic L , Polak S , Kubikova E , et al. Congenital anomalies of the spleen from an embryological point of view . Med Sci Monit 2009 ; 15 : RA269 – 76 .
Google Scholar
Assaf R , Shebli B , Alzahran A , Rahmeh AR , Mansour A , Hamza R , et al. Acute abdomen due to an infarction of wandering spleen: case report . J Surg Case Reports 2020 ; 2020 :rjz378.
Magowska A . Wandering spleen: a medical enigma, its natural history and rationalization . World J Surg 2013 ; 37 : 545 – 50 .
Gilman RS , Thomas RL . Wandering spleen presenting as acute pancreatitis in pregnancy . Obstet Gynecol 2003 ; 101 : 1100 – 2 .
Allen KB , Andrews G . Pediatric wandering spleen–the case for splenopexy: review of 35 reported cases in the literature . J Pediatr Surg 1989 ; 24 : 432 – 5 .
Padilla D , Ramia JM , Martin J , Pardo R , Cubo T , Hernandez-Calvo J , et al. Acute abdomen due to spontaneous torsion of an accessory spleen . Am J Emerg Med 1999 ; 17 : 429 – 30 .
Viana C , Cristino H , Veiga C , Leão P . Splenic torsion, a challenging diagnosis: case report and review of literature . Int J Surg Case Rep 2018 ; 44 : 212 – 6 .
Lahiri S , Dasgupta N , Mondal AU . A case of splenic torsion and rupture presenting as ruptured ectopic pregnancy . J Surg Case Rep 2010 ; 2010 : 4 .
Gayer G , Zissin R , Apter S , Atar E , Portnoy O , Itzchak Y . CT findings in congenital anomalies of the spleen . Br J Radiol 2001 ; 74 : 767 – 72 .
Rafie BA , AbuHamdan OJ , Trengganu NS , Althebyani BH , Almatrafi BS . Torsion of a wandering spleen as a cause of portal hypertension and mesenteric varices: a rare aetiology . J Surg Case Reports 2018 ; 2018 :rjy107.
Faridi MS , Kumar A , Inam L , Shahid R . Wandering spleen- a diagnostic challenge: case report and review of literature . Malaysian J Med Sci 2014 ; 21 : 57 – 60 .
- congenital abnormality
- saudi arabia
- splenectomy
- splenic infarction
- wandering spleen
- young adult
- ligament laxity
- left upper quadrant of abdomen
Email alerts
Citing articles via, affiliations.
- Online ISSN 2042-8812
- Copyright © 2024 Oxford University Press and JSCR Publishing Ltd
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

Wandering Spleen Presents as an Acute Surgical Emergency: A Case Report
Annie Reiss 1 , Safi Khuri 1,2* , Kenan Hallon 1 , Ahmad Assalia 1,3 , Sa'd Sayida 1,3
1 Department of General Surgery, Rambam Health Care Campus, Haifa, Israel
2 HPB and Surgical Oncology Unit, Rambam Health Care Campus, Haifa, Israel
3 Advanced Laparoscopic and Bariatric Surgery Unit, Rambam Health Care Campus, Haifa, Israel
*Corresponding author : Safi Khuri, Department of General Surgery, Rambam Health Campus, Haifa, Israel. Email: [email protected]
Received Date: 27 June, 2019; Accepted Date: 01 July, 2019; Published Date: 05 July, 2019
Citation: Reiss H, Khuri S, Hallon K, Assalya A, Sayida S (2019) Wandering Spleen Presents as an Acute Surgical Emergency: A Case Report. J Surg 13: 1236. DOI: 10.29011/2575-9760.001236
Introduction : The wandering spleen is a very rare cause of acute abdominal pain, occurring mostly in children and females of reproductive age. It is characterized by weakness or absence of one or more of the ligaments that hold the spleen in its normal location at the left upper quadrent of the abdomen. Herein, we present a rare case of wandering spleen in a patient with intestinal malrotation and history of an unknown abdominal surgery in the left upper quadrant.
Case Presentation : A 37-year-old female patient, presented to our Emergency Medicine department with acute abdominal pain. She was diagnosed with a wandering spleen and intestinal malrotation. Prompt laparotomy was performed, and the patient underwent splenectomy, appendectomy and intestinal fixation.
Discussion : We discuss the potential association between the patient’s wandering spleen, intestinal malrotation and prior surgery. Congenital malformation of peritoneal ligaments may account for the patient’s wandering spleen as well as her intestinal malrotation. The possibility of a repaired congenital diaphragmatic hernia at infancy would support a congenital cause. An acquired laxity of ligaments, more common among women who have experienced pregnancy, provides an alternative though incomplete explanation.
Conclusion : We hope this unusual case would raise awareness of the rare diagnosis of the wandering spleen and its potentially associated anomalies.
Introduction
Wandering spleen, also known as hypermobile spleen, is a very rare clinical entity with an estimated reported incidence of
Case Presentation
A 37-year-old healthy female patient, presented to our Emergency Medicine department with a three-day history of diffuse abdominal pain, which increased on the day of admission, associated with the sudden appearance of a palpable mass in the right lower quadrent of the abdomen. The patient had no recent history of fever and no gastrointestinal, urinary or gynecological complaints. The patient’s history included three normal vaginal deliveries, years before. She also underwent an abdominal surgery for unknown reason at one year of age. Neither the patient nor family members had any recollection or records that would help ascertain the type of surgery.
Upon her admission, the patient’s vital signs were within normal limits. Physical examination revealed a slightly distended abdomen, with a palpable sensitive mass at the right lower quadrent and no signs of peritonitis ( REF _Ref7801741 \h \* MERGEFORMAT Figure 1 08D0C9EA79F9BACE118C8200AA004BA90B02000000080000000C0000005F0052006500660037003800300031003700340031000000 ). Digital rectal exam was normal without palpable masses. Complete blood count, liver and kidney function tests were within normal limits. Urine analysis revealed slightly increased urine amylase. Gynecological exam, including Trans-Vaginal Ultrasound (US), was normal. A urine test was negative for pregnancy.
Abdominal US revealed a homogenous elongated mass in the patient’s right lower abdomen, separated from adjacent pelvic organs.
A contrast-enhanced Computer Tomography (CT) scan of the abdomen and pelvis revealed an enlarged spleen, measuring 15 cm, located at the abdominopelvic junction rather than the left upper quadrant ( REF _Ref7801771 \h \* MERGEFORMAT Figure 2 08D0C9EA79F9BACE118C8200AA004BA90B02000000080000000C0000005F0052006500660037003800300031003700370031000000 ). Torsion of the splenic vessels were suspected due to positive whirl sign, along with the presence of several splenic hypodense lesions that appeared to be infarcts. The tail of the pancreas was pulled in the right anterior direction. The duodenum, normally crossing the midline from right to left, was found on the right side of the abdomen along with the jejunum, while the ileum, cecum and colon were found on the left. A normal appearing appendix was seen on the left side of the abdomen. The aformentioned CT scan finding were highly suggestive for the diagnosis of a wandering spleen and intestinal malrotation.
Due to suspected splenic infarction and a concern of torsion of the small bowel mesentery, the patient underwent an emergent exploratory laparotomy. On exploration of the abdomin, a large and mobile spleen was found in the right lower abdomin ( REF _Ref7802485 \h \* MERGEFORMAT Figure 3 08D0C9EA79F9BACE118C8200AA004BA90B02000000080000000C0000005F0052006500660037003800300032003400380035000000 ). The spleen appeared congested with patches of infarction, and torsion of its vascular pedicle was evident. The small intestine was viable, but abnormally located: the duodenum and jejunum were found in the right upper quadrant, while the cecum was entirely mobile and in the left abdomen, with a normal appearing appendix. Despite partial recovery after detorsion, patches of ischemic splenic tissue were still grossly evident, and splenopexy was unfortunately inappropriate ( REF _Ref7802505 \h \* MERGEFORMAT Figure 4 08D0C9EA79F9BACE118C8200AA004BA90B02000000080000000C0000005F0052006500660037003800300032003500300035000000 ). Total splenectomy and appendectomy (due to cecal malposition) were performed. The cecum was fixated in the right lower abdomen. Her post-operative period was uneventfull, and she discharged home on post-operative day 5. Histopathological report revealed spleen with extensive areas of infarction. 2 months following discharge, patient is in good general condition, without any complaint.
This is an unusual case of a young woman diagnosed with a wandering spleen and previously unknown intestinal malrotation. We discuss the potential association between these conditions, as well as their connection to the patient’s unknown prior abdominal surgery. A wandering spleen is a mobile spleen, abnormally located or oriented due to the hyperlaxity of its ligamentous attachments [2]. It may be displaced from its normal location in the left upper quadrant, raising the risk of torsion around its elongated vascular pedicle and consequent splenic infarction. Clinical presentation may be asymptomatic, chronic intermittent abdominal pain due to recurring torsion and detorsion, or acute abdominal pain due to vessel obstruction and infarct as was the case of our patient. Physical examination may reveal a palpable, solid, oval abdominal mass. Imaging studies are generally required for definitive diagnosis, and CT scan is the imaging modality of choice. Treatment options include operative vs non-operative management. Non-operative management is usually not recommended, as the risk for vascular torsion and splenic infarction is more than 60%. Surgical intervention includes detorsion and splenopexy or splenectomy, and depends on the vacularity of the spleen. Detorsion and splenopexy can be done when there is no vacular compromise, to reduce post-splenectomy risks, such as overwhelming postsplenectomy sepsis, while splenectomy is recommended in case of splenic infarction.
As wandering spleen is a very rare clinical entity, other more common differential diagnosis, such as incarcerated ventral hernia, ovarian torsion or periapendicular abscess, are usually highly suspected. The wandering spleen is a rare condition, and not easily diagnosed. Reviewing the English literature revealed approximately five hundred cases that were reported REF _Ref7808842 \r \h \* MERGEFORMAT [3] 08D0C9EA79F9BACE118C8200AA004BA90B02000000080000000C0000005F0052006500660037003800300038003800340032000000 . One third of cases affects children, present equally in both sexes, and presumably stem from congenital malformation of the splenic ligaments. Over the age of ten, the incidence among females is approximately tenfold, with an average age of 20-40 years at presentation. Laxity of the splenic ligaments may be congenital, for instance due to an underlying connective tissue disorder, or acquired; it may be exacerbated by trauma or splenomegaly, and may stem from the hormonal effects of pregnancy, explaining the female predominance [2]. An unusual finding in our patient’s CT scan and abdominal exploration was the abnormally located intestine. Intestinal malrotation is mostly discussed regarding the pediatric population, as 90% of cases are discovered by one year of age. However, there are patients who enter adulthood undiagnosed. Kapfer and Rappold discuss adult cases, among them a previously undiagnosed 80-year-old man [4]. Apart from fetal ultrasound during her pregnancies, our patient had no previous abdominal imaging. We cannot therefore determine with certainty whether this was a case of asymptomatic congenital malrotation, or a laxity of peritoneal attachments combined with the sudden decent of the patient’s spleen toward the pelvis that displaced the bowel. A review of the literature revealed a case of acquired wandering spleen with intestinal malrotation in a 20-year-old female, described by Dalpe and Cunningham [5]. The authors suggested that both the malrotated bowel and the wandering spleen could be attributable to malformed peritoneal attachments, implying a congenital cause of ligamentous laxity. That patient, however, had additional developmental anomalies that supported this claim. Ooka et al. presented a case of a 22-year-old male with wandering spleen, gastric volvulus and intestinal malrotation [6]. They also suggest a common etiology for the malfixation of the bowel, mesentery and spleen.
History and physical examination indicated our patient underwent an unknown abdominal surgery in her left upper quadrant before the age of one year. Possibilities include prior splenopexy, supporting a congenital issue with spleen fixation; other splenic procedures such as splenic cystectomy; and surgery on adjacent structures, for instance the diaphragm. Had the patient been born with a left-sided Congenital Diaphragmatic Hernia (CDH), and underwent surgery to repair the defect, this may have reduced the strength of the splenic ligaments. We could not confirm nor refute our suspicion with the available history, and our intraoperative exploration revealed neither mesh nor signs of prior splenopexy or primary repair of the diaphragm. Our literature review revealed a case of an 11-year-old female with splenic torsion and a history of left-sided CDH repaired shortly after birth, reported by Mehta, et al. [3]. Four other cases of wandering spleen following CDH repair have been reported. In such cases, a wandering spleen may result from the primarily abnormal splenic attachments due to splenic herniation into the left hemithorax during pregnancy, or from a loss of retroperitoneal fixation following the diaphragmatic repair. An association between CDH and intestinal malrotation has been established. The herniation of abdominal viscera in the thorax is presumed to promote nonfixation of the mesentery and malrotation of the intestinal tract.
In our literature review, we have found one case of a wandering spleen with intestinal malrotation and a history of CDH repair. Hosgor et al. reviewed 20 children with a late presentation of congenital diaphragmatic hernia, 12 of whom had intestinal malrotation. Among them was a 10-year-old female, diagnosed with malrotation and a wandering spleen. This patient presented with abdominal pain, anorexia, fatigue, severe failure to thrive and a palpable abdominal mass. She had been initially misdiagnosed with malignancy and treated accordingly; when correctly diagnosed with congenital diaphragmatic hernia, the patient underwent primary diaphragm repair, a Ladd procedure and splenopexy [7]. The coexistence of a wandering spleen, intestinal malrotation and a suspected congenital diaphragmatic hernia in a single patient is extremely rare. The suggested mechanisms of congenital vs. acquired tissue laxity may help further the discussion of this uncommon condition. We encourage health professionals to consider the diagnosis of wandering spleen in patients presenting with acute abdominal pain, especially in those with intestinal malrotation and/or a history of surgery in the left upper quadrant.
In conclusion, we present a rare case of wandering spleen and intestinal malrotation in an otherwise healthy female with history of an unknown abdominal procedure at infancy. The wandering spleen is a rare, yet noteworthy cause of acute abdominal pain. We hope to raise awareness of this rare entity and suggest future directions of study regarding its etiology and associated anomalies.
Figure SEQ Figure \* ARABIC 1 : Inspection of the patient’s abdomen. A protruding mass can be seen in the right lower quadrant. A surgical scar can be seen in the left upper quadrant.
Figure 2: Computed tomography scan of the patient’s abdomen and pelvis. (A): Coronal view. The wandering or prolapsed spleen (S) is seen in the abdominopelvic junction, compressing the urinary bladder. Torsion of the vascular pedicle is also seen (arrow). (B): Axial view, showing the whirl sign, representing torsion of the splenic vessels. (C): Axial view of the torsed splenic pedicle (arrow) entering the splenic hilum. Hypodense areas, likely infarcts, are visible in the splenic parenchyma.
Figure SEQ Figure \* ARABIC 3 : Intraoperative image, showing the prolapsed spleen at the right lower abdomen. The torsed vascular pedicle is visible at the center of the image (arrow). The large intestine is seen on the left side of the abdomen.
Figure SEQ Figure \* ARABIC 4 : The enlarged prolapsed spleen with its torsed splenic pedicle, lifted from the right lower quadrant and detorsed. Areas of infarct are grossly apparent in the splenic parenchyma. Insufficient improvement following detorsion indicated the need for splenectomy.
1. FARIDI MS, KUMAR A, INAM L, SHAHID R (2014) Wandering Spleen- A Diagnostic Challenge: Case Report and Review of Literature. Malays J Med Sci 21: 57-60.
2. Reisner DC, Burgan CM (2018) Wandering Spleen: An Overview. Current Problems in Diagnostic Radiology 47: 68-70.
3. Mehta A, Vana PG, Glynn L (2013) Splenic torsion after congenital diaphragmatic hernia repair: Case report and review of the literature. Journal of Pediatric Surgery 48: 29-31.
4. Kapfer SA, Rappold JF (2004) Intestinal malrotation-not just the pediatric surgeon’s problem. Journal of the American College of Surgeons 199: 628-635.
5. Dalpe C, Cunningham M (2003) Wandering spleen as an asymptomatic pelvic mass. Obstetrics & Gynecology 101: 1102-1104.
6. Ooka M, Kohda E, Iizuka Y, Nagamoto M, Ishii T, et al. (2013) Wandering spleen with gastric volvulus and intestinal non-rotation in an adult male patient. Acta Radiologica Short Reports 2.
7. Hosgor M, Karaca I, Karkıner A, Ucan B, Temir G, et al. (2004) Associated malformations in delayed presentation of congenital diaphragmatic hernia. Journal of Pediatric Surgery 39: 1073-1076.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA : Creative Commons Attribution-Share Alike 4.0 International License. With this license, readers can share, distribute, download, even commercially, as long as the original source is properly cited. Read More .
Journal of Surgery
- About Journal
- Aims and Scope
- Board Members
- Article in Press
- Recent Articles
- Articles Search
- Current Issue
We use cookies for a better experience. Read privacy policy . Manage your consent settings:
Manage Your Consent:
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Radiol Case Rep
- v.17(9); 2022 Sep
Wandering spleen with torsion and infarction: A case report
Wandering spleen, also known as ectopic spleen, is a rare condition in which the spleen's anatomical location is other than its fixed position in the abdomen's left upper quadrant. The cause of such an abnormality could be due to congenital or acquired factors, which could ultimately lead to torsion and splenic infarct. Given the nonspecific clinical symptoms and the potential complications associated with wandering spleen, computed tomography scans provide a crucial means for proper diagnosis. In this article, we report the case of a 16-year-old female with a diagnosis of wandering spleen with torsion and splenic infarct.
Introduction
The spleen is an intraperitoneal organ usually situated in the left upper quadrant of the abdomen; however, in the instance that it is not found in its typical location or orientation, it is referred to as a wandering or ectopic spleen [1] . The cause of this condition is associated with ligamentous hyperlaxity or absence, which can often be acquired through pregnancy, splenomegaly, or through congenital factors [2] . Due to the ligament's laxity, the vascular pedicle is elongated, often leading to splenic torsion and infarction, which can ultimately lead to necrosis, ischemia, and even splenic rupture [3] . Given the nonspecific clinical symptoms related to wandering spleen, computed tomography (CT) imaging is critical for an accurate diagnosis [4] .
Case report
A 16-year-old female presented to her local hospital with severe periumbilical abdominal pain. A CT scan revealed that the spleen was located in an inverted position in the right lower quadrant, with swirling of the mesenteric vessels leading to the splenic pedicle, as well as the splenic artery towards the splenic hilum in the right lower quadrant before a sudden cut-off ( Fig. 1 ). Subsequently, a diagnostic laparoscopy confirmed the diagnosis of a torsed wandering spleen. As a result, the patient was brought into the operating room where the spleen was found to be torsed upon itself 720 degrees around an abnormal vascular pedicle. Following complete detorsion, there were no sign of perfusion; therefore, a splenectomy was performed. Postoperatively, the patient was well with no reports of abdominal pain, and with her incisions healing adequately.

(A-E) A 16-year-old female presented to her local hospital with severe periumbilical abdominal pain and a CT was done to better define the cause of the patient's symptoms. The CT scan demonstrated a torsed spleen situated in the pelvis with swirling of the mesenteric vessels leading to infarction of the wandering spleen. (A) CT scan through the upper abdomen shows a normal liver and a distended stomach with no evidence of the spleen. (B) CT scans through the mid-abdomen demonstrate the swirling of the mesenteric vessels (arrow) consistent with low flow to the spleen. (C) CT scans through the pelvis demonstrate a low-density mass in the pelvis (S) which was an infarcted ectopic spleen. (D, E) CT scans in coronal plane nicely define the infarcted wandering spleen in the pelvis (S) with haziness by splenic hilum due to twisting of the mesenteric arcade (arrow).
This article reviews a case of wandering spleen, an extremely rare condition in which the spleen, normally found in the left upper quadrant, is found in an abnormal anatomical position. The spleen is fixed into position by the splenorenal, splenocolic, and gastrosplenic ligaments; however, the hyperlaxity or absence of the peritoneal ligaments, due to either acquired or congenital factors, can cause the spleen to shift to a more caudal location [1 , 5] . As a result of the ligament's hyperlaxity, the vascular pedicle is abnormally elongated leading to torsion, which can range from mild (90°) to severe (2160°) [6] , and splenic infarction. Correlated with a strong female predominance, especially in women of reproductive age [7] , the diagnosis of ectopic spleen presents a challenge due to its nonspecific symptoms.
We report a 16-year-old female who presented with severe abdominal pain and an abdomen that was firm and tender to palpation, especially in the right lower quadrant, as well as reflexive or voluntary guarding. A subsequent CT scan and diagnostic laparoscopy showed a 720° torsed, ischemic, and completely necrotic spleen. Consequently, the patient underwent a laparoscopic splenectomy, the treatment of choice in cases with splenic infarction, necrosis, or unreducible torsion [5] .
Due to the broad symptoms and potential complications associated with wandering spleen, including sepsis, splenic rupture, and acute pancreatitis [3] , CT is considered the preferred diagnostic tool for this condition. Typically, the combination of the absence of the spleen in the left upper quadrant and a mass in the abdomen indicates an ectopic spleen [2 , 8] .
Patient consent
The patient reported in the manuscript signed the informed consent/authorization for participation in research which includes the permission to use data collected in future research projects including presented case details and images used in this manuscript.
Acknowledgments
The authors thank senior science writer Edmund Weisberg, MS, MBE, who helped us to review and edit this article.
Competing Interests: All authors declare no conflict of interest.
Funding: There was no funding associated with this work.

- Wandering spleen
Citation, DOI, disclosures and case data
At the time the case was submitted for publication Oscar Gutierrez had no financial relationships to ineligible companies to disclose.
Presentation
Severe abdominal pain in the left hypochondriac region after physical assault.
Patient Data
The spleen is not seen in the anatomical location.
In the left iliac fossa, there is a well-defined homogeneously enhancing oval-shaped soft tissue density mass of about 9 cm in its craniocaudal axis, which is vascularized by an elongated splenic artery that originated from the celiac trunk and venous drainage is mainly within the left renal vein.
Dorsolumbar scoliosis.
Bone remodeling in both hips probably related to bilateral congenital dysplasia.
Case Discussion
This case demonstrates a wandering spleen , a rare finding that is usually asymptomatic. It may be congenital (as in this case) or acquired and can often be an incidental finding when performing abdominal imaging tests for other reasons.
Patients with this condition are at increased risk of developing splenic torsion and splenic infarction, so in some cases, splenopexy may be considered as a treatment.
1 article features images from this case
1 public playlist includes this case.
- Superheros by Dalia Ibrahim ◉
Related Radiopaedia articles
- Splenunculus
Promoted articles (advertising)
How to use cases.
You can use Radiopaedia cases in a variety of ways to help you learn and teach.
- Add cases to playlists
- Share cases with the diagnosis hidden
- Use images in presentations
- Use them in multiple choice question
Creating your own cases is easy.
- Case creation learning pathway
ADVERTISEMENT: Supporters see fewer/no ads
By Section:
- Artificial Intelligence
- Classifications
- Imaging Technology
- Interventional Radiology
- Radiography
- Central Nervous System
- Gastrointestinal
- Gynaecology
- Haematology
- Head & Neck
- Hepatobiliary
- Interventional
- Musculoskeletal
- Paediatrics
- Not Applicable
Radiopaedia.org
- Feature Sponsor
- Expert advisers

Journals By Subject
- Proceedings
Information

Infarcted Wandering Spleen: Case Report from Tirunesh Beijing General Hospital, Addis Ababa, Ethiopia
Mengistu Solomon Sefu
Department of Surgery, Yekatit 12 Hospital Medical College, Addis Ababa, Ethiopia
YabsiraMichael Tsegaye
Michael Berega Sibhat
Department of Surgery, Tirunesh Beijing General Hospital, Addis Ababa, Ethiopia
Add to Mendeley
Wandering spleen or hypermobile spleen results from the elongation or maldevelopment of the spleen’s suspensory ligaments. It is rare clinical entity with fewer cases reports worldwide. It is found mostly in children and in adult it is said to be common in females of reproductive age group. Its clinical presentation is different from asymptomatic palpable abdominal mass, intermittent abdominal discomfort due to torsion and spontaneous detorsion to acute abdomen due to torsion with subsequent ischemia and infarction. Because of the rarity of the condition the patient might end with global spleen infarction with splenectomy unless the physician has high index of suspicion. Here we will present a case report of a 19 year old female patient who presented with abdominal pain, vomiting, nausea, anorexia and fever of 3 days duration. Has abdominal tenderness with leukocytosis and abdominal ultrasound finding of anechoic splenic lesions with peritoneal collection. Due to lack of other imaging modalities, exploratory laparotomy was done with an impression of ruptured splenic abscess. The spleen was frankly infarcted with 720 degrees of torsion with no ligaments attachment. Total splenectomy was done and the patient was vaccinated with pentavalent vaccine during her discharge. Even though wandering spleen is rare conditions, one has to consider as differential diagnosis in patient with acute presentation of left upper quadrant abdominal pain with later generalized. And if possible early high index of suspicion might salvage the spleen.
Wandering Spleen, Infarcted Spleen, Peritonitis, Exploratory Laparotomy
Mengistu Solomon Sefu, YabsiraMichael Tsegaye, Michael Berega Sibhat. (2023). Infarcted Wandering Spleen: Case Report from Tirunesh Beijing General Hospital, Addis Ababa, Ethiopia. Reports , 3 (1), 7-10. https://doi.org/10.11648/j.reports.20230301.12
Mengistu Solomon Sefu; YabsiraMichael Tsegaye; Michael Berega Sibhat. Infarcted Wandering Spleen: Case Report from Tirunesh Beijing General Hospital, Addis Ababa, Ethiopia. Reports . 2023 , 3 (1), 7-10. doi: 10.11648/j.reports.20230301.12
Mengistu Solomon Sefu, YabsiraMichael Tsegaye, Michael Berega Sibhat. Infarcted Wandering Spleen: Case Report from Tirunesh Beijing General Hospital, Addis Ababa, Ethiopia. Reports . 2023;3(1):7-10. doi: 10.11648/j.reports.20230301.12
Cite This Article
- Author Information
Verification Code/
The verification code is required.
Verification code is not valid.
Science Publishing Group (SciencePG) is an Open Access publisher, with more than 300 online, peer-reviewed journals covering a wide range of academic disciplines.
Learn More About SciencePG
- Special Issues
- AcademicEvents
- ScholarProfiles
- For Authors
- For Reviewers
- For Editors
- For Conference Organizers
- For Librarians
- Article Processing Charges
- Special Issues Guidelines
- Editorial Process
- Peer Review at SciencePG
- Open Access
- Ethical Guidelines
Important Link
- Manuscript Submission
- Propose a Special Issue
- Join the Editorial Board
- Become a Reviewer

IMAGES
VIDEO
COMMENTS
Wandering spleen or hypermobile spleen results from the elongation or maldevelopment of the spleen's suspensory ligaments. It is a rare clinical entity that mainly affects children. Among adults, it is most commonly found in females of active reproductive age. It may present as an asymptomatic mass in the abdomen, or it may present with ...
The intermittent nature of an ultimate splenic torsion can add to the diagnostic challenge. Medical literature concerning the wandering spleen and knowledge about this pathology originates mainly from individual case reports. Despite the evolving diagnostic modalities available, this rare and ambiguous disorder remains misdiagnosed, and a high ...
Wandering spleen, also known as ectopic spleen, is a rare condition in which the spleen's anatomical location is other than its fixed position in the abdomen's left upper quadrant. ... computed tomography scans provide a crucial means for proper diagnosis. In this article, we report the case of a 16-year-old female with a diagnosis of wandering ...
Wandering spleen is defined as the spleen being located in the lower part of the abdomen, even in the pelvic cavity, rather than the normal site (i.e., the left upper quadrant) because of the absence or loosening of the ligaments fixing the spleen ( ). It is a rare clinical condition with an incidence of <0.2% ( ).
We report the case of a wandering spleen with acute splenic infarction in a pregnant woman and its minimally invasive surgical treatment, focusing on the clinical and radiological findings that could mislead or drive clinicians to the right diagnosis, or a potential disaster. Splenic preservation in the wandering spleen where it is safe and ...
Gastric volvulus and wandering spleen with torsion both are life-threatening conditions unless managed urgently. Abdominal ultrasound has an important role in diagnosis. It shows the absence of the spleen in the normal position, or floating in the abdomen is a diagnostic of a wandering spleen as seen in our case.
Abstract. Wandering spleen refers to a spleen that is ectopic in its location contrary to a normal spleen which rests in the left hypochondrium. Although it is a rare clinical entity seen in children, it can also be rarely seen in females of reproductive age group. We present one such case of wandering spleen which was misdiagnosed earlier as a ...
A torted wandering spleen is a rare clinical occurrence with fewer than 500 cases reported and an incidence of less than 0.2%. It is brought about through laxity of the gastrosplenic and splenorenal ligaments; however, the precise aetiology remains unknown. It can prove to be a diagnostic challenge with high mortality if misdiagnosed. We present the case of a 27-year-old woman of Arabic ...
Raid Alghamdi, Amer Alzahrnai, Abdulaziz Alosaimi, Ibrahim Albabtain, Infarcted wandering spleen: A case report from Saudi Arabia, Journal of Surgical Case Reports, Volume 2021, Issue 6, June 2021, rjab277, ... Pediatric wandering spleen-the case for splenopexy: review of 35 reported cases in the literature ...
Torsion of a wandering spleen: a case report with emphasis onimage findings. Ligaments of the spleen. (a) CT at T12 shows splenomegaly and hypertrophied left kidney. (b) CT at L5 shows ...
BACKGROUND:Wandering spleen is a rare condition in which the spleen lacks the usual peritoneal attachments, resulting in increased intra-abdominal mobility. ... resulting in symptoms ranging from an incidental finding to an acute abdomen as a result of an ischemic necrosis of the spleen. CASE REPORT:We present the case of a 25-year-old female ...
Wandering spleen is a rare condition characterized by the absence or underdevelopment of one or all of the ligaments that hold the spleen in its normal position in the left upper quadrant of the abdomen.Wandering spleen and gastric volvulus share a common cause, the absence of an intraperitoneal visceral ligament. Herein we describe an unusual case of pediatric wandering spleen in association ...
Clinical presentation. A wandering spleen can be an elusive diagnosis as its presentation is greatly variable and intermittent torsion can cause non-specific signs and symptoms. It can present as an asymptomatic or painful abdominal mass, intermittent abdominal pain, or as an acute abdomen (e.g. bowel obstruction, acute pancreatitis) 3,4,6.
We discuss a case that presented to our clinic with acute abdominal findings after the torsion of wandering spleen. Case Report. A 26-year-old man presented to the emergency service of our hospital because of severe abdominal pain that began 3 days earlier. Other than abdominal pain, nausea and abdominal distention were present.
DOI: 10.29011/2575-9760.001236. Abstract. Introduction: The wandering spleen is a very rare cause of acute abdominal pain, occurring mostly in children and females of reproductive age. It is characterized by weakness or absence of one or more of the ligaments that hold the spleen in its normal location at the left upper quadrent of the abdomen.
Wandering spleen, also known as ectopic spleen, is a rare condition in which the spleen's anatomical location is other than its fixed position in the abdomen's left upper quadrant. ... In this article, we report the case of a 16-year-old female with a diagnosis of wandering spleen with torsion and splenic infarct. Keywords: Spleen, Wandering ...
Wandering accessory spleen is a rare finding, usually asymptomatic. It may be congenital (as in this case) or acquired and can often be an incidental finding when performing abdominal imaging tests for other reasons. Patients with this condition are at increased risk of developing splenic torsion and splenic infarction, so in some cases ...
The wandering spleen: case report of laparoscopic splenectomy in a pregnant woman. Bulletin of the National Research Centre (2022) 46: 273. [3] Jawad M, Yusuf M H, Al Doaibel K A, et al. Wandering Spleen: A Rare Case From the Emergency Department. Cureus 15 (1): 2023.