Registered Nurse RN
Registered Nurse, Free Care Plans, Free NCLEX Review, Nurse Salary, and much more. Join the nursing revolution.

Protrusion, Retrusion, and Excursion Anatomy
In this anatomy lesson, I’m going to demonstrate protrusion, retrusion, and excursion , which are special body movement terms in anatomy that refer to forward (anterior), backward (posterior), or side to side movements.
Protrusion in Anatomy
Protrusion refers to the movement of a structure in an anterior (forward) direction. In fact, the word protrude means “projecting something forward.”
I call protrusion the kissing movement because it occurs when you pucker your lips like you’re going to give someone a kiss or stick out your tongue. Moving the mandible (lower jaw) forward is also an example of protrusion.

Retrusion in Anatomy
Retrusion is the opposite of protrusion. It refers to the movement of a structure in a posterior, or backward, direction. Putting your tongue back in your mouth, moving the lips back, or moving the mandible back are all examples of retrusion in anatomy.

Excursion in Anatomy
Finally, we have excursion , which refers to the side-to-side movement of the lower jaw (mandible). If you’ve ever heard of a character named Ernest P. Worrell, then you’ve definitely seen the excursion movement. He’s the character in those movies such as Ernest Goes to Camp, Ernest Goes to Jail, etc. When Ernest saw something nasty, he’d move his jaw back and forth and say, “Ewwww.”

Excursion can occur in either direction, and anatomists use directional terms to specify the type of excursion. When the mandible moves to either the left or right, it’s moving away from the body’s midline, so it’s called lateral excursion . When the mandible moves closer to the midline of the body, it’s called medial excursion .

Protrusion and Retrusion vs Protraction and Retraction
What about protraction and retraction ? Some anatomy textbooks will refer to the forward movement of the mandible, lips, or tongue as protraction (instead of protrusion), and the backward (posterior) movement will be called retraction (instead of retrusion). The terms are sometimes used interchangeably, so use whatever method your anatomy professor suggests (they give you the grade, not me!).
However, some anatomists today use protraction and retraction to refer almost exclusively to the scapulae, as it is a combined movement (protraction is anterolateral, and retraction is posteromedial). In contrast, protrusion and retrusion are more of an anterior/posterior movement. Then again, some anatomists prefer not to use protraction and retraction at all, even when describing shoulder blade movement.
Protrusion, Retrusion, and Excursion in Healthcare
Healthcare professionals use protrusion, retrusion, and excursion when documenting, performing assessments on patients, or treating disorders. For example, in her head-to-toe assessment , Nurse Sarah asked me to stick out my tongue (an example of protrusion), to assess cranial nerve twelve .
In addition, something called a mandibular protrusion test (MPT) is sometimes used by anesthesiologists to predict difficult airways in patients.
Free Quiz and More Anatomy Videos
Take a free protrusion vs retrusion quiz to test your knowledge, or review our protrusion vs retrusion video . In addition, you might want to watch our anatomy and physiology lectures on YouTube, or check our anatomy and physiology notes .
Please Share:
- Click to print (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to share on Pocket (Opens in new window)
- Click to share on Telegram (Opens in new window)
Disclosure and Privacy Policy
Important links, follow us on social media.
- Facebook Nursing
- Instagram Nursing
- TikTok Nurse
- Twitter Nursing
- YouTube Nursing
Copyright Notice

- Introduction
- Palp/Percus
- Auscultation
Palpation/Percussion
Thoracic expansion:.
- Is used to evaluate the symmetry and extent of thoracic movement during inspiration.
- Is usually symmetrical and is at least 2.5 centimeters between full expiration and full inspiration.
- Can be symmetrically diminished in ankylosing spondylitis .
- Can be unilaterally diminished in chronic fibrotic lung disease , extensive lobar pneumonia, large pleural effusions, bronchial obstruction and other disease states.
Percussion:
Percussion is the act of tapping on a surface, thereby setting the underlying structures in motion, creating a sound and palpable vibration. Percussion is used to determine whether underlying structures are fluid-filled, gas-filled, or solid. Percussion:
- Penetrates 5 - 6 centimeters into the chest cavity.
- May be impeded by a very thick chest wall.
- Produces a low-pitched, resonant note of high amplitude over normal gas-filled lungs.
- Produces a dull, short note whenever fluid or solid tissue replaces air filled lung (for example lobar pneumonia or mass) or when there is fluid in the pleural space (for example serous fluid, blood or pus).
- Produces a hyperresonant note over hyperinflated lungs (e.g. COPD ).
- Produces a tympanitic note over no lung tissue (e.g. pneumothorax ).
Diaphragmatic excursion:
- Can be evaluated via percussion.
- Is 4-6 centimeters between full inspiration and full expiration.
- May be abnormal with hyperinflation , atelectasis , the presence of a pleural effusion , diaphragmatic paralysis, or at times with intra-abdominal pathology.
Type your tag names separated by a space and hit enter
There's more to see -- the rest of this topic is available only to subscribers.
1. Download the Nursing Central app by Unbound Medicine
2. Select Try/Buy and follow instructions to begin your free 30-day trial

Want to regain access to Nursing Central?
Renew my subscription
Not now - I'd like more time to decide
Log in to Nursing Central
Forgot your password, forgot your username, contact support.
- unboundmedicine.com/support
- [email protected]
- 610-627-9090 (Monday - Friday, 9 AM - 5 PM EST.)

1. Download the Taber's Online app by Unbound Medicine
2. Log in using your existing username and password to start your free, 30-day trial of the app
3. After 30 days, you will automatically be upgraded to a 1-year subscription at a discounted rate of $29.95

Type your tag names separated by a space and hit enter

There's more to see -- the rest of this topic is available only to subscribers.
2. Select Try/Buy and follow instructions to begin your free 30-day trial
We're glad you have enjoyed Taber's Online! As a thank-you for using our site, here's a discounted rate for renewal or upgrade.
Mobile + Web Renewal
1 Year Subscription
Consult Taber’s anywhere you go with web access + our easy-to-use mobile app.
Nursing Central
Nursing Central combines Taber’s with a medical dictionary, disease manual, lab guide, and useful tools.
Not now - I'd like more time to decide
Want to regain access to Taber's Online?
Renew my subscription
Log in to Taber's Online
Forgot your password, forgot your username, contact support.
- unboundmedicine.com/support
- [email protected]
- 610-627-9090 (Monday - Friday, 9 AM - 5 PM EST.)
Medical Dictionary
Search medical terms and abbreviations with the most up-to-date and comprehensive medical dictionary from the reference experts at Merriam-Webster. Master today's medical vocabulary. Become an informed health-care consumer!
Browse the Medical Dictionary
Featured game.

Find the Best Synonym
Test your vocabulary with our 10-question quiz!
Deniz Burnham & 'Astronaut'
Peyton Manning & 'Omaha'
Issa Rae & 'Insecure'
Word of the day, tendentious.
See Definitions and Examples »
Get Word of the Day daily email!
Games & Quizzes

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Neurol
Thoracic Excursion Is a Biomarker for Evaluating Respiratory Function in Amyotrophic Lateral Sclerosis
Naohiko iguchi.
1 Department of Neurology, Nara Medical University, Kashihara, Japan
2 Department of Rehabilitation Medicine, Nara Medical University, Kashihara, Japan
Naoki Iwasa
Nanami yamada, naoya kikutsuji, kazuma sugie, associated data.
The original contributions presented in the study are included in the article/ Supplementary Material , further inquiries can be directed to the corresponding author/s.
To evaluate the usefulness of thoracic excursion as a biomarker in patients with amyotrophic lateral sclerosis (ALS).
We measured the forced the vital capacity (FVC), thoracic excursion, baseline-to-peak diaphragmatic compound muscle action potential (DCMAP) amplitude, diaphragm thickness at full inspiration (DTfi), Medical Research Council (MRC) sum score for muscle strength, and arterial partial pressures of oxygen and carbon dioxide and administered the Amyotrophic Lateral Sclerosis Functional Rating Scale-Revised (ALSFRS-R) and modified Medical Research Council (mMRC) Dyspnea Scale. The test–retest reliability of thoracic excursion was determined.
Results and Conclusions
Thirty-four patients with ALS and 26 age- and sex-matched healthy participants were enrolled. Thoracic excursion measurement had excellent test–retest reliability (intraclass coefficient: 0.974). Thoracic excursion was more strongly correlated with FVC ( r = 0.678, p < 0.001) than DCMAP amplitude ( r = 0.501, p = 0.003) and DTfi ( r = 0.597, p < 0.001). It was also correlated with ALSFRS-R score ( r = 0.610, p < 0.001), MRC sum score ( r = 0.470, p = 0.005), and mMRC Dyspnea Scale score ( r = −0.446, p = 0.008) and was the most sensitive parameter for assessing dyspnea and FVC. Thoracic excursion decreased as FVC declined in the early and late stages, there were no differences in DCMAP amplitude and DTfi between the early and late stages, and ALSFRS-R score and MRC sum score decreased only in the late stage. Thoracic excursion was well correlated with respiratory function and is useful for predicting respiratory and general dysfunction in patients with ALS regardless of stage.
Introduction
Amyotrophic lateral sclerosis (ALS) is a neurodegenerative disorder in which respiratory dysfunction occurs with disease progression. Eventually, the diaphragm and other muscles of respiration are involved, resulting in respiratory muscle paralysis, which is the primary cause of death. Respiratory function is most frequently assessed using the pulmonary function test (PFT). PFT parameters, such as forced vital capacity (FVC) and forced expiratory volume in 1 s, have been found to predict hypoventilation ( 1 , 2 ) and survival ( 3 – 5 ) in patients with ALS. However, PFT has been associated with a risk of viral infection, and PFT results may be inaccurate due to air leakage from around the breathing tube and through the glottis because of facial muscle weakness, especially in patients with bulbar onset ALS ( 6 – 8 ). Alternative methods for measuring respiratory function and predicting FVC based on neurophysiological principles have recently been reported. FVC has been found to be correlated with diaphragmatic compound muscle action potential (DCMAP) elicited through phrenic nerve stimulation ( 9 – 11 ) and diaphragm thickness (DT) measured using ultrasonography ( 12 , 13 ). However, these methods require a high level of skill. Thoracic excursion is estimated by measuring chest expansion. It is known to correlate with maximal inspiratory volume and is used as an outcome in respiratory rehabilitation. We aimed to determine the usefulness of thoracic excursion as an alternative to PFT in patients with ALS.
Materials and Methods
Ethical considerations.
This study was approved by the Ethics Committee of Nara Medical University (approval #2688). All study procedures were performed in accordance with the ethical standards of the ethics committee, Declaration of Helsinki, and Ethical Guidelines for Medical and Health Research Involving Human Subjects in Japan (UMIN: 000042222). All participants provided written and verbal informed consent after receiving information about the study.
Study Population
We included all patients diagnosed with definite, probable, or possible ALS based on the modified El Escorial criteria ( 14 ) who visited Nara Medical University Hospital between June 2020 and October 2021. The inclusion criteria were as follows: (1) patients aged between 20 and 90 years; (2) patients without tracheostomy; and (3) patients not on non-invasive positive pressure ventilation. The exclusion criteria were as follows: (1) patients who received drugs for ALS that had not been approved in Japan or had undergone surgery in the previous 12 months (48 weeks); (2) patients with dementia (Mini-mental State Exam score <10); (3) patients with severe psychiatric disorders; (4) patients who were unable to answer questionnaires; (5) patients with suicidal ideation; (6) patients undergoing treatment for respiratory disease; (7) patients with severe heart failure; (8) patients who were pregnant; and (9) patients judged to be inappropriate for this study by the investigator or coordinator.
We selected control participants from the in- and out-patients of the Departments of Neurology at Nara Medical University Hospital, Nara and Minami Nara General Medical Center, Nara. We excluded control participants with subjective breathlessness and those who could not walk.
General Assessment
The participants were administered the Amyotrophic Lateral Sclerosis Functional Rating Scale-Revised (ALSFRS-R). Total ALSFRS-R scores range from 0 to 48, and low scores strongly predict a poor outcome. In addition, ALSFRS-R consists of three subscales, which were scored separately: bulbar function (three items: speech, salivation, and swallowing), extremities function (six items: handwriting, cutting food and handling utensils, dressing and hygiene, turning in bed and adjusting bed clothing, walking, and climbing stairs), and respiratory function (three items: dyspnoea, orthopnoea and respiratory insufficiency). We used a cutoff score of 38 because patients with an ALSFRS-score <38 have a high 1-year mortality rate ( 15 ). Additionally, we graded the muscle strength of the limbs using the Medical Research Council (MRC) sum score, an established multifactorial scoring system with a total score between 0 and 60 ( 16 ). The MRC sum score evaluates global muscle strength by combining the scores of six muscles (shoulder abductors, elbow flexors, wrist extensors, hip flexors, knee extensors, and ankle dorsiflexors) that are evaluated bilaterally. We used an MRC sum score cutoff of 51, as an MRC sum score <51 has been reported to be associated with a poor outcome and high risk of mechanical ventilation in patients with neuromuscular disease ( 17 ). For assessment of dyspnea, the participants were administered the Modified Medical Research Council (mMRC) Dyspnea Scale. Patients who were unable to walk and those with dyspnea during activities of daily living and caregiving in bed were given a score of 4 and those with no dyspnea were given a score of 0.
Thoracic Excursion Measurement
Thoracic excursion from maximal inspiration to maximal expiration was measured using a measurement system (Takeikikikougyo, Niigata, Japan) that continuously measured chest expansion and automatically recorded the data. The measurement of thoracic excursion had high intra- and inter-rater reliability and validity ( 18 ). A wire was placed over the xiphoid process and horizontally wrapped around the trunk ( Figures 1A,B ). Thoracic excursion was measured during five timed maximal inspirations and expirations, and the average of the five measurements was used for analysis ( Figure 1C ).

Thoracic excursion measurement. (A) The scenery of thoracic excursion measurement. (B) The wire of the measurement device. (C) The display of the application.
Phrenic Nerve Conduction Study
We performed electrical phrenic nerve stimulation at the neck to elicit a DCMAP, which was recorded using surface electrodes. The active electrode was placed over the xiphoid process, and the reference electrode was placed at the costal margin 16 cm away from the active electrode ( 9 ). The phrenic nerve was supra-maximally stimulated three times on each side in all participants. The response with the highest baseline-to-peak amplitude was selected on each side, and the average amplitude of both sides was used for analysis.
Ultrasonography
DT was measured between the anterior and mid-axillary lines with the participant in the supine position using a Logiq S8 ultrasonography machine (GE Healthcare, Chicago, IL, USA) with a high-resolution 3–12 MHz linear probe in the B mode ( 19 , 20 ). The diaphragm was identified as a relatively non-echogenic muscle layer surrounded by two echogenic layers that represented the diaphragmatic pleural and peritoneal membranes ( 21 , 22 ). DT was measured at three points bilaterally at the end of inspiration, and the average diaphragmatic thickness at full inspiration (DTfi) of both sides was used for analysis.
PFT was performed with the participants seated upright. Spirometry was used to test pulmonary mechanics through the measurement of the percent-predicted FVC, forced expiratory volume in 1 s, forced expiratory and inspiratory flow rates, and maximal voluntary ventilation. These values are used to assess the ability of the lungs to quickly move large volumes of air through the airways and to identify airway obstruction. To identify the parameter that is most involved in the decline in FVC, we divided the participants into the severe (<50% FVC; late stage of FVC decline), mild (50– <80%; early stage of FVC decline), and no restriction (≥80%) groups. The two patients who were not able to perform PFT because of difficulty in breathing were included in the severe group.
Statistical Analysis
Based on the assumption that the difference in thoracic excursion between the groups would be 0.8 cm with a standard deviation of 1.0 cm, we set a target sample size of 26 participants in each group (ALS group and control group) to ensure that the power is at least 80% with a two-sided significance level of 0.05. Intraclass coefficients were calculated to determine the test-retest reliability of the measurement of thoracic excursion; both “test” and “re-test” were performed by the same examiner. The Shapiro–Wilk test was used to assess the distribution of the data, and Pearson's correlation coefficients ( r ) were calculated to evaluate the associations between thoracic excursion and respiratory function. Based on the r values, the correlation was categorized as weak ( r = 0.30–0.39), moderate ( r = 0.40–0.59), or strong ( r = 0.60–1.00). We used the t -test to compare the two groups and the Tukey–Kramer post-hoc test for multiple comparisons. Statistical significance was set at p < 0.05. Statistical analyses were performed using SPSS version 22.0 (SPSS Japan, Tokyo, Japan).
Clinical Characteristics and Thoracic Excursion of Patients With ALS and Control Participants
We enrolled 34 consecutive patients with sporadic ALS and 26 control participants. Their clinical characteristics are presented in Table 1 . In patients with ALS, the mean age was 70.1 ± 11.5 years (range: 39–88) and the mean disease duration was 22.4 ± 22.0 months. Twenty-six patients had spinal-onset ALS, and the remaining eight patients had bulbar-onset ALS. Between the two groups, there was no difference in FVC and neurophysiological parameters. ALSFRS-R bulbar function score and age at examination were lower in bulbar-onset ALS patients than spinal-onset ALS patients ( Table 2 ). In addition, there was no difference between the patients with ALS and control participants in sex, age at examination, body mass index, and smoking history, although thoracic excursion was significantly worse in the patients with ALS ( Figure 2A ).
Demographic characteristics of patients with ALS and control participants.
Data are shown as mean ± SD (range) and number (percentage). ALS, amyotrophic lateral sclerosis; N.A., not applicable; BMI, body mass index; mMRC, modified Medical Research Council; DCMAP, diaphragmatic compound motor-action potential; DTfl, diaphragm thickness at full inspiration; FVC, forced vital capacity; PaCO 2 , arterial partial pressures of carbon dioxide; PaO 2 , arterial partial pressures of oxygen; ALSFRS-R, amyotrophic lateral sclerosis functional rating scale-revised; MRC, medical research council .
Demographic characteristics of patients with spinal-onset and bulbar-onset ALS.
Data are shown as mean ± SD (range) and number (percentage). ALS, amyotrophic lateral sclerosis; BMI, body mass index; mMRC, modified Medical Research Council; DCMAP, diaphragmatic compound motor-action potential; DTfl, diaphragm thickness at full inspiration; FVC, forced vital capacity; PaCO 2 , arterial partial pressures of carbon dioxide; PaO 2 , arterial partial pressures of oxygen; ALSFRS-R, amyotrophic lateral sclerosis functional rating scale-revised; MRC, medical research council .

Thoracic excursion in patients with ALS. (A) The values of thoracic excursion in patients with ALS are significantly smaller than those in control patients. (B) Thoracic excursion measurement shows excellent test-retest reliability. ALS, amyotrophic lateral sclerosis.
Test–Retest Reliability of Measurement of Thoracic Excursion
The intraclass coefficient of thoracic excursion was 0.974 ( Figure 2B ), which indicates excellent test–retest reliability.
Relationships Among Thoracic Excursion, Other Neurophysiological Parameters, and Clinical Characteristics
Thoracic excursion was moderately correlated with DCMAP amplitude ( r = 0.569, p < 0.001) and DTfi ( r = 0.494, p = 0.003; Figures 3A,B ). DCMAP amplitude was strongly correlated with DTfi ( r = 0.621, p < 0.001). Thoracic excursion was strongly correlated with FVC ( r = 0.678, p < 0.001; Figure 3C ), whereas DCMAP amplitude ( r = 0.501, p = 0.003) and DTfi ( r = 0.597, p < 0.001) were only moderately correlated with FVC. Conversely, there were no correlations between thoracic excursion and the patients' clinical characteristics, such as age at examination ( r = −0.163, p = 0.358), age at onset ( r = −0.113, p = 0.524), disease duration ( r = −0.258, p = 0.141), and body mass index ( r = −0.228, p = 0.195). Likewise, thoracic excursion was not correlated with age at examination ( r = −0.143, p = 0.487) and body mass index ( r = −0.055, p = 0.788) in control participants.

Relationships between thoracic excursion and other neurophysiological parameters, FVC, and mMRC Dyspnea Scale score. (A–C) Relationships between thoracic excursion and DCMAP amplitude, DTfi, and FVC. Thoracic excursion shows a strong correlation with FVC (C) and moderate correlation with DCMAP amplitude (A) and DTfi (B) . (D) Relationships between thoracic excursion and subjective dyspnea severity assessed using the mMRC Dyspnea Scale. Thoracic excursion is the most sensitive parameter for assessing subjective dyspnea. FVC, forced vital capacity; mMRC, modified Medical Research Council; DCMAP, diaphragmatic compound muscle action potential; DTfi, diaphragm thickness at full inspiration.
In addition, we investigated the relationship between mMRC Dyspnea Scale score, neurophysiological parameters, and FVC. mMRC Dyspnea Scale score was moderately correlated with thoracic excursion ( r = −0.446, p = 0.008) and FVC ( r = −0.428, p = 0.015) and weakly correlated with DCMAP amplitude ( r = −0.318, p = 0.067) and DTfi ( r = −0.392, p = 0.022). Patients with an mMRC Dyspnea Scale score of 1–4 had a significantly lower thoracic excursion than those with a score of 0 ( Figure 3D ). There were no differences in other parameters, such as FVC, DCMAP amplitude, and DTfi, between the mild and severe respiratory dysfunction groups ( Supplementary Figures 1A–C ).
Relationships Between Neurophysiological Parameters and ALSFRS-R Score
ALSFRS-R score was strongly correlated with thoracic excursion ( r = 0.610, p < 0.001; Figure 4A ) and FVC ( r = 0.622, p < 0.001). In contrast, DTfi was weakly correlated with ALSFRS-R score ( r = 0.308, p = 0.076), and DCMAP amplitude was not correlated with the ALSFRS-R score ( r = 0.239, p = 0.173; Supplementary Figures 2A–C ). Furthermore, patients with an ALSFRS-R score < 38 had a significantly lower thoracic excursion and FVC than those with an ALSFRS-R score of 38 or more ( Figure 4B ). In contrast, there were no differences in DCMAP amplitude and DTfi between the mild and severe respiratory dysfunction groups ( Supplementary Figures 2D–F ). In ALSFRS-R sub-scores analysis, FVC correlated with both ALSFRS-R extremities ( r = 0.500, p = 0.004) and bulbar function score ( r = 0.370, p = 0.037). Contrary to this, thoracic excursion correlated only with ALSFRS-R extremities function score ( r = 0.584, p < 0.001), not with bulbar function score ( r = 0.227, p = 0.197). Additionally, in bulbar-onset ALS patients, FVC correlated strongly with ALSFRS-R bulbar function score ( r = 0.709, p = 0.075) and moderately with extremities function score ( r = 0.506, p = 0.247). In contrast, FVC correlated strongly with ALSFRS-R extremities function score ( r = 0.678, p < 0.001) and weakly with bulbar function score ( r = 0.367, p = 0.072) in spinal-onset ALS patients. Similarly, thoracic excursion was strongly correlated with ALSFRS-R extremities function score in both spinal-onset ( r = 0.676, p < 0.001) and bulbar-onset ALS ( r = 0.696, p = 0.055).

Relationships between respiratory function parameters and general condition. (A) Relationship between thoracic excursion and ALSFRS-R score. Thoracic excursion is strongly correlated with ALSFRS-R score. (B) Thoracic excursion is significantly lower in the patients in the mild respiratory dysfunction group whose ALSFRS-R score is <38 than those whose ALSFRS-R score is not <38. (C) Relationship between thoracic excursion and MRC sum score. Thoracic excursion is strongly correlated with MRC sum score. (D) Thoracic excursion is significantly lower in patients in the mild respiratory dysfunction group whose MRC sum score is <51 than in those whose MRC sum score is not <51. ALSFRS-R, amyotrophic lateral sclerosis functional rating scale-revised; MRC, medical research council.
Relationships Between Neurophysiological Parameters and Limb Muscle Weakness
We examined the relationship between neurophysiological parameters, FVC, and MRC sum score. MRC sum score was moderately correlated with thoracic excursion ( r = 0.506, p = 0.006; Figure 4C ) and FVC ( r = 0.564, p = 0.003; Supplementary Figure 3A ). In contrast, it was not correlated with DCMAP amplitude and DTfi ( Supplementary Figures 3B,C ). Patients with a low (<51) MRC sum score had a significantly lower thoracic excursion and FVC than those with a high MRC sum score ( Figure 4D ). In contrast, there were no differences in DCMAP amplitude and DTfi between the high and low MRC sum score groups ( Supplementary Figures 3D–F ). Therefore, limb muscle weakness was associated with a decline of thoracic excursion and FVC but not with diaphragmatic function.
Relationships Between FVC and Neurophysiological Parameters
Thoracic excursion decreased in both the early and late stages of FVC decline ( Figure 5 ), but DCMAP amplitude and DTfi did not decrease in the late stage of FVC decline ( Figures 6A,B ). In contrast, ALSFRS-R score and MRC sum score did not decrease in the early stage of FVC decline, but they decreased in the late stage of FVC decline ( Figures 6C,D ).

Changes in thoracic excursion with FVC decline. Thoracic excursion decreases in both the early and late stage of FVC decline in patients with ALS. FVC, forced vital capacity; ALS, amyotrophic lateral sclerosis.

Changes in neurophysiological parameters and general condition with FVC decline. (A,B) DCMAP amplitude and DTfi decrease only in the early stage of FVC decline. (C,D) ALSFRS-R score and MRC sum score decrease only in the late stage of FVC decline. FVC, forced vital capacity; DCMAP, diaphragmatic compound motor-action potential; DTfl, diaphragm thickness at full inspiration; ALSFRS-R, amyotrophic lateral sclerosis functional rating scale-revised; MRC, medical research council.
This is the first study that used thoracic excursion measurement to evaluate respiratory dysfunction in patients with ALS. We found that thoracic excursion is a reliable and valid biomarker of respiratory function in patients with ALS. We observed that thoracic excursion was strongly correlated with FVC and can be used as a surrogate marker of FVC. Since FVC decline predicts hypoventilation ( 1 , 2 ) and survival ( 3 – 5 ), a decline in thoracic excursion might also be able to predict hypoventilation and survival in patients with ALS. Furthermore, thoracic excursion is easier to measure than DCMAP amplitude and DT; it can be measured at home or in a clinic.
Thoracic excursion was a better predictor of respiratory dysfunction and general condition than DCMAP amplitude and DTfi. Phrenic nerve conduction study is a technique used for measuring respiratory function ( 9 , 10 ). A previous study reported that the DCMAP amplitude of healthy individuals is 1.0 mV ( 10 ). DCMAP amplitude has been reported to be correlated with FVC and other respiratory parameters, such as maximum inspiratory pressure and sniff nasal inspiratory pressure ( 11 ), and it may be an indicator of prognosis in ALS ( 23 – 25 ). Low DCMAP amplitude has been found to predict a poor outcome in patients with ALS ( 11 , 26 ). Diaphragm ultrasonography is another useful tool for measuring respiratory function ( 27 , 28 ). DT at full expiration and full inspiration is correlated with FVC ( 12 , 13 , 21 ), as is DT ratio ( 21 , 29 ). In patients with ALS, a low DT at expiration indicates atrophy of the diaphragm and hypoventilation, and a low DT at inspiration or low DT ratio indicates respiratory muscle weakness.
Thoracic excursion has been reported to correlate with inspiratory capacity ( 18 ). Previous studies have used chest expansion to assess the severity of rheumatologic diseases ( 30 , 31 ) and the effects of inspiratory muscle training in patients with chronic obstructive pulmonary disease ( 32 ), ankylosing spondylitis ( 33 ), and myasthenia gravis ( 34 ). In patients with ALS, thoracic and abdominal excursion recorded using respiratory magnetometry were used to assess the response to diaphragm training ( 35 ). However, measurement of chest expansion had never been used for assessing pulmonary function in patients with ALS.
Thoracic excursion was strongly correlated with MRC sum score and ALSFRS-R score, and especially with ALSFRS-R extremities function score. The measurement of thoracic excursion involves the evaluation of ribcage movement and the function of all the muscles of respiration. Hence, respiratory function is affected by the strength of the muscles of the extremities, general condition, and movement of the diaphragm. In this report, we confirmed that the general condition and the strength of the muscles of the extremities strongly affect respiratory function in patients with ALS.
We found that decline in thoracic excursion was strongly correlated with the severity of respiratory function. There were no differences in DCMAP amplitude and DTfi between the mild and severe respiratory dysfunction groups, and ALSFRS-R score and MRC sum score decreased only in the severe group. These results suggest that the factors affecting respiratory function differ between the early- and late-stages of ALS. Diaphragm weakness may affect thoracic excursion and FVC in the early stage, and weakness of the limb muscles and accessory muscles of respiration may affect thoracic excursion and FVC in the late stage. During inspiration, contraction of the diaphragm expands the abdominal ribcage, and contraction of the intercostal muscles and accessory muscles of respiration simultaneously expands the pulmonary ribcage ( 36 ). In patients with diaphragmatic dysfunction, the intercostal muscles and accessory muscles of respiration expand the pulmonary ribcage to compensate for diaphragm failure during inspiration ( 37 ). As their condition progresses, patients with ALS with diaphragmatic dysfunction show paradoxical abdominal motion as inspiration primarily relies on the action of the intercostal muscles and accessory muscles of respiration and the diaphragm is drawn into the chest wall during inspiration because of its dysfunction ( 38 ). Additionally, increased compound muscle action potential amplitudes have been observed in the external intercostal muscles in an end-stage SOD1 transgenic rat model of ALS, which reflects compensation for decreased trans-diaphragmatic pressure due to diaphragm dysfunction ( 39 ). Therefore, when paradoxical abdominal motion is observed, DCMAP amplitude and DT findings suggestive of severe diaphragmatic dysfunction and decreased FVC and thoracic excursion can be expected. The intercostal muscles and other accessory muscles of respiration elevate and expand the thoracic rib cage and compensate for diaphragmatic dysfunction to limit the decrease in FVC and thoracic excursion. With the progression of ALS, weakness of these muscles appears with worsening general condition, leading to decreases in thoracic excursion and FVC. Therefore, evaluation of diaphragmatic dysfunction is adequate for assessing pulmonary function in the early stage of ALS. Notably, thoracic excursion is useful for the evaluation of pulmonary function and general condition in ALS regardless of stage. Among all the neurophysiological parameters and FVC, we found thoracic excursion to be the most sensitive for assessing dyspnea. Thoracic excursion predicts the appearance of subjective dyspnea and decline in objective respiratory dysfunction.
The results of clinical trials of disease-modifying therapies for neurodegenerative disorders underscore the need for testing before the onset of neurological symptoms and evaluating disease severity and progression regardless of stage ( 40 – 42 ). Although clinical trials of potential therapies have been done in ALS, definite efficacy has not been demonstrated in RCTs ( 43 ). These results appear to be partly attributable to the absence of established outcome measures as well as the limited number of patients, which may diminish statistical power. Our findings suggest that thoracic excursion could be used as a surrogate marker in clinical trials. In recent ALS clinical trials, the following are often used as endpoints: the change in the ALSFRS-R, the decrease of muscle strength and FVC, and time from the allocation day to the onset of an event (24-h use of non-invasive respiratory support, use of invasive respiratory support, or death) ( 42 – 45 ). ALSFRS-R is highly reproducible and objective, although there is a slight variation by therapy in short-term clinical trial. The time from the allocation day to an event needs to take into account the effects of other factors such as the patient's stage of inclusion and living environment ( 45 ). FVC is used to determine whether to provide respiratory support rather than the prediction of the prognosis, as it is difficult to reliably measure respiratory function even at an early stage in bulbar-onset ALS ( 46 , 47 ). In this study, FVC had a weak correlation with bulbar function score in total ALS patients. Additionally, FVC correlated more strongly with bulbar function score than extremities function score in bulbar-onset ALS patients, but not in spinal-onset ALS patients. Bulbar palsy symptoms may affect the measurement of FVC, especially in bulbar-onset ALS patients. By contrast, thoracic excursion had no correlation with bulbar function score. Taken together, measurement of thoracic excursion is a useful evaluation method of respiratory function and may take the place of FVC as an endpoint of respiratory function in clinical trials, which is not affected by bulbar palsy symptoms.
The measurement of thoracic excursion is simple and non-invasive, does not involve a special technique and requires only chest binding, and can be performed even at the bedside. However, our procedure involves a few additional steps. Thoracic excursion must be measured in an upright sitting or standing position to avoid friction between the wire wound around the thorax and the backrest of the chair (in reclined sitting) or bed (in supine). The other limitation in this study is that thoracic excursion in excessively obese patients may not be measured accurately. The wire of the measurement system does not shrink easily because of subcutaneous fat. Additionally, in this study, we have attempted to tackle the major challenges associated with identifying a surrogate biomarker for evaluating respiratory function and prognosis in patients with ALS. However, floor and ceiling effects could not be adequately analyzed. A large-scale longitudinal study is necessary to confirm the results of this study.
Data Availability Statement
Ethics statement.
The studies involving human participants were reviewed and approved by Nara Medical University Hospital. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
NIg and TM: conceptualization and writing—original draft preparation. NIg, NIw, and NY: performed data acquisition and interpretation. MO: performed formal analysis. AK and KS: supervision. All authors have read and agreed to the published version of the manuscript.
This work was supported by the Ministry of Education, Culture, Sports, Science, and Technology of Japan under grant KAKENHI No. 20K19453.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The author thanks the participants and their families for their commitment and dedication to research on pulmonary function measurement in patients with amyotrophic lateral sclerosis. Also, thank staff at the Department of Neurology at Nara Medical University Hospital for their contributions.

Abbreviations
Supplementary material.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2022.853469/full#supplementary-material
- Daily Crossword
- Word Puzzle
- Word Finder
- Word of the Day
- Synonym of the Day
- Word of the Year
- Language stories
- All featured
- Gender and sexuality
- All pop culture
- Grammar Coach ™
- Writing hub
- Grammar essentials
- Commonly confused
- All writing tips
- Pop culture
- Writing tips
Advertisement
[ ik- skur -zh uh n , -sh uh n ]
a pleasure excursion; a scientific excursion.
weekend excursions to mountain resorts.
an excursion of tourists.
excursions into futile philosophizing.
- Physics. the displacement of a body or a point from a mean position or neutral value, as in an oscillation.
- an accidental increase in the power level of a reactor, usually forcing its emergency shutdown.
- the range of stroke of any moving part.
- the stroke itself.
- Obsolete. a sally or raid.
verb (used without object)
- to go on or take an excursion.
an excursion fare; an excursion bus.
/ -ʒən; ɪkˈskɜːʃən /
- a short outward and return journey, esp for relaxation, sightseeing, etc; outing
- a group of people going on such a journey
an excursion ticket
an excursion into politics
- (formerly) a raid or attack
- a movement from an equilibrium position, as in an oscillation
- the magnitude of this displacement
- the normal movement of a movable bodily organ or part from its resting position, such as the lateral movement of the lower jaw
- machinery the locus of a point on a moving part, esp the deflection of a whirling shaft
Discover More
Other words from.
- ex·cursion·al ex·cursion·ary adjective
- preex·cursion noun
Word History and Origins
Origin of excursion 1
Example Sentences
It’s important that your significant other or family is supportive, since your new obsession will likely become all-consuming, and most of your outdoor excursions will now revolve around searching for animal poop in the woods.
Insulated, waterproof footwear like the Paninaro Omni-Heat Tall Boot will go a long way in making your snow bike or snowshoe excursion a treat rather than a trial.
More time outdoors has been great for dialing in our kit for weekend excursions.
The thought of being able to knock out a three-day excursion with just a single carry-on is tantalizing.
I’ve spent the past two months testing the pack on a handful of short camp-outs and a seven-day family surf excursion, and the SEG42 delivered the organization I desperately needed.
It is disappointing and, frankly, frightening that Thompson walked away from his repugnant Sea World excursion scot-free.
Several events specifically cater to kids, making this a fun excursion for the whole family.
I learned a lot about myself on that excursion, and from the trip as a whole.
There was, instead, a nauseating excursion into base and sad fantasies.
While a two-day feeding frenzy makes for a fun excursion, the human body is only capable of so much consumption.
Out gets Uncle David, looking brown and healthy after his northern excursion.
The other day an excursion was arranged to Sondershausen, a town about three hours' ride from Weimar in the cars.
We got back to Weimar about eight in the evening, and this delicious excursion, like all others, had to end.
To my friends ever since I have not failed to recommend the passage of the Butterley tunnel as a desirable pleasure excursion.
From childhood I had longed to see something of the world, and this excursion to Paris was the first gratification of that wish.
Related Words
- Dictionaries home
- American English
- Collocations
- German-English
- Grammar home
- Practical English Usage
- Learn & Practise Grammar (Beta)
- Word Lists home
- My Word Lists
- Recent additions
- Resources home
- Text Checker
Definition of excursion noun from the Oxford Advanced Learner's Dictionary
- on an excursion They've gone on an excursion to York.
- There are regular weekend excursions throughout the summer.
- a business trip
- a five-minute trip by taxi
- a long and difficult journey across the mountains
- a tour of Bavaria
- the first expedition to the South Pole
- We went on an all-day excursion to the island.
- The children were on a day’s outing from school.
- We had a day out at the beach.
- a(n) foreign/overseas trip/journey/tour/expedition
- a bus/coach/train/rail trip/journey/tour
- to go on a(n) trip/journey/tour/expedition/excursion/outing/day out
- to set out/off on a(n) trip/journey/tour/expedition/excursion
- to make a(n) trip/journey/tour/expedition/excursion
- destination
- Our ship offers 13 different excursions.
- Princess Tours runs independent excursions from selected hotels.
- We decided to make an all-day excursion to the island.
- We signed up for a shore excursion to New Orleans.
- Optional excursions include a tour of the ancient city and a day's horse-riding.
- take (somebody on)
- excursion into
- excursion to
Questions about grammar and vocabulary?
Find the answers with Practical English Usage online, your indispensable guide to problems in English.
- After a brief excursion into drama, he concentrated on his main interest, which was poetry.
- her first excursion into business
Other results
- Advance Purchase Excursion
Nearby words
- Search Menu
- Animal Research
- Cardiovascular/Pulmonary
- Health Services
- Health Policy
- Health Promotion
- History of Physical Therapy
- Implementation Science
- Integumentary
- Musculoskeletal
- Orthopedics
- Pain Management
- Pelvic Health
- Pharmacology
- Population Health
- Professional Issues
- Psychosocial
- Advance Articles
- COVID-19 Collection
- Featured Collections
- Special Issues
- PTJ Peer Review Academies
- Author Guidelines
- Submission Site
- Why Publish With PTJ?
- Open Access
- Call for Papers
- Self-Archiving Policy
- Promote your Article
- About Physical Therapy
- Editorial Board
- Advertising & Corporate Services
- Permissions
- Journals on Oxford Academic
- Books on Oxford Academic
Article Contents
- < Previous
Normal Chest Excursion
- Article contents
- Figures & tables
- Supplementary Data
Betty Carlson, Normal Chest Excursion, Physical Therapy , Volume 53, Issue 1, January 1973, Pages 10–14, https://doi.org/10.1093/ptj/53.1.10
- Permissions Icon Permissions
Nineteen normal adults were studied to establish a chest excursion norm based on a clinically practical standardized method of measurement. The factors influencing accurate measurement such as type of tape measure used, patient position, room temperature, and underclothing are discussed. A normal circumferential measurement of three and one-fourth inches (8.48 cm) is explained. The importance of this chest excursion measurement in the respiratory portion of the patient's evaluation is related to his treatment program and activity goal. The mean and standard deviations of age, vital capacity, and excursion according to the groups of men and women, active and sedentary, are included.
Email alerts
Citing articles via.
- Recommend to Your Librarian
- Advertising and Corporate Services
- Journals Career Network
Affiliations
- Online ISSN 1538-6724
- Copyright © 2024 American Physical Therapy Association
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Cambridge Dictionary +Plus
Meaning of excursion in English
Your browser doesn't support HTML5 audio
- break-journey
- circumnavigation
excursion | American Dictionary
Examples of excursion, translations of excursion.
Get a quick, free translation!

Word of the Day
of or relating to birds

Dead ringers and peas in pods (Talking about similarities, Part 2)

Learn more with +Plus
- Recent and Recommended {{#preferredDictionaries}} {{name}} {{/preferredDictionaries}}
- Definitions Clear explanations of natural written and spoken English English Learner’s Dictionary Essential British English Essential American English
- Grammar and thesaurus Usage explanations of natural written and spoken English Grammar Thesaurus
- Pronunciation British and American pronunciations with audio English Pronunciation
- English–Chinese (Simplified) Chinese (Simplified)–English
- English–Chinese (Traditional) Chinese (Traditional)–English
- English–Dutch Dutch–English
- English–French French–English
- English–German German–English
- English–Indonesian Indonesian–English
- English–Italian Italian–English
- English–Japanese Japanese–English
- English–Norwegian Norwegian–English
- English–Polish Polish–English
- English–Portuguese Portuguese–English
- English–Spanish Spanish–English
- English–Swedish Swedish–English
- Dictionary +Plus Word Lists
- excursion into something
- American Noun
- Translations
- All translations
Add excursion to one of your lists below, or create a new one.
{{message}}
Something went wrong.
There was a problem sending your report.
An Initiative of the Program for Bedside Medicine
- See us on youtube
- See us on facebook
- See us on twitter
Pulmonary Exam: Percussion & Inspection
The pulmonary exam is one of the most important and often practiced exam by clinicians. While auscultation is most commonly practiced, both percussion and inspection are equally valuable techniques that can diagnose a number of lung abnormalities such as pleural effusions, emphysema, pneumonia and many others.
Introduction to the Pulmonary Exam
Though taught extensively in early medical training the pulmonary exam is often neglected apart from auscultation.
Percussion During the Pulmonary Exam
The "5-7-9 rule".
- The upper border of liver dullness is defined by:
- 5th intercostal space in the midclavicular line
- 7th intercostal space in the midaxillary line
- 9th intercostal space in the scapular line
- Note: 9th intercostal space is located approximately at the inferior border of the scapula
- Hyperresonance that continues below these boundaries can be suggestive of hyperinflation (e.g. emphysema)
Cardiac dullness
Be able to outline the area of "absolute" cardiac dullness— a fist sized area just to the left of the sternum. If it is not there it suggests emphysema.
Traube's space
- Superiorly: Left 6th rib
- Inferiorly: Left costal margin
- Laterally: Anterior axillary line
- Left pleural effusion (however NOT in left lower lobe pneumonia without effusion as it is the effusion that falls into the costophrenic recess that is above the gastric bubble)
- Splenomegally (less reliable compared to Castell’s Sign)
- Very full colon
- Recently eaten (i.e. stomach is full)
Click here to read an article on the Ludwig Traube.
Tidal Percussion
- Percuss down the back until the normal hyperresonance of the lungs becomes dull over the diaphragm. Then simply have the patient breath in and out deeply while continuing to percuss. The sound should wax and wane.
- Pleural effusion
- Hyperinflation such as emphysema from a maximally contracted diaphragm
Major and Minor Fissures of the Lung
- The major fissure can be located by drawing a line from the T2 spinous process to where the 6th rib meets the sternum. The minor fissure can be approximated by drawing a horizontal line from the 4th rib attachment of the sternum to the major fissure.
- Easier method: Simply ask the patient to put their hands over their head. The scapula will rotate externally and its medial border will outline the major fissure (see figure below).
Historical Perspective of the Pulmonary Exam
Percussion was first described by Dr. Josef Leopold Auenbrugger , an Austrian physician who first observed his father tapping on wine barrels in the cellar of his hotel to determine how much wine was left. The son applied this technique to patients when he became a physician. He is credited with bringing the technique of percussion to the field of medicine. Much of his work occurred around 1760 where he described that by percussing the thorax he could accurately predict the contents of what was inside, as confirmed with post-mortum studies he conducted.
Inspection During the Pulmonary Exam
Signs of copd.
- Inspiratory descent of trachea.
- Use of accessory muscles.
- Pursed lips on exhalation (provides a small amount of PEEP).
- Normal in infancy and increased with aging.
- Prominent angle of Louis (or sternal angle).
- Flaring of the lower costal margins.
- Dahl Sign: Above the knee, patches of hyperpigmentation or bruising caused by constant 'tenting' position of hands or elbows.
- The "subcostal angle" is the angle between the xiphoid process and the right or let costal margin. Normally, during inhalation the chest expands laterally, increasing this angle. When the diaphragms are flattened (as in COPD), inhalation paradoxically causes the angle to decrease.
- Harrison's sulcus: a horizontal grove where the diaphragm attaches to the ribs; associated with chronic asthma, COPD, & Rickets.
REMEMBER : "The side that moves less, is the side of disease!"
Look for signs of volume loss (or gain) on the side that moves less (hollow supraclavicular fossae, intercostal spaces prominent, shoulder droopy, scapula outline more prominent).
Consult the Expert

Dr. Peadar Noone
Dr. Peadar Noone trained in Galway, Dublin, Boston, the UK and Chapel Hill, where he is now Associate Professor of Medicine and Medical Director of the Lung Transplant Program at the University of North Carolina, Chapel Hill.
Clinical Pearl
Insert (in a normal individual) three fingers vertically in the space under the cricoid cartilage, and above the sternal notch. As the person breathes in, the space may reduce to two fingers at most (i.e. the fingers get "squeezed" as the sternum rises with inspiration). In a patient with severe hyperinflation, the crico-sternal distance is much shorter (because the sternum is elevated), maybe 1-2 fingers at most. With inspiration one's fingers get "squeezed" out as the already "high" sternum rises up to the level of the cricoid, thus, in many cases, obliterating the crico-sternal distance altogether. Some clinicians label this sign "tracheal shortening" but strictly speaking, the actual tracheal length does not get shorter. Classically this is seen with severe emphysema / hyperinflation, or severe air trapping. Often accompanied by reduced hepatic and cardiac dullness on percussion, a widened / flared costal angle, and Hoover's sign.
Other Findings in the Chest
- Pectus Excavatum (Funnel Chest) : depression of sternum; in severe cases may compress heart and great vessels.
- Pectus Carinatum (Pigeon chest) : anterior displacement of sternum, usually benign.
- Flail Chest: secondary to multiple rib fractures, depression of diaphragm causes injured area to cave inward producing a "paradoxical thoracic movement" in breathing.
Key Learning Points
- Percussion of the lung exam
- Inspection of the lung exam
Related to Pulmonary Exam: Percussion & Inspection
- Precordial Movements
- Cardiac Second Sounds
- Neck Veins & Wave Forms
- BP & Pulsus Paradoxus
The Stanford Medicine 25
- Aortic Regurgitation Exam
- Ankle Brachial Index
- Ankle and Foot Exam
- Ascites & Venous Patterns
- Bedside Ultrasound
- Breast Exam
- Carpal Tunnel Exam
- Cerebellar Exam
- Deep Tendon Reflexes
- Dermatology Exam: Acne vs. Rosacea
- Dermatology Exam: Learning the Language
- Dermatology Exam: Nevi (Mole) Exam
- Fundoscopic Exam (Ophthalmoscopy)
- Gait Abnormalities
- Hip Region Exam
- Internal Capsule Stroke
- Involuntary Movements and Tremor Diagnosis: Types, Causes, and Examples
- Low Back Exam
- Lymph Node Exam
- Neck Vein Exam
- Pelvic Exam
- Precordial Movements in the Cardiac Exam
- Pulmonary Exam: Percussion & Inspection
- Pupillary Responses
- Pulsus Paradoxus and Blood Pressure Measurement Techniques
- Rectal Exam
- Spleen Exam
- Tarsal Tunnel Exam
- Thyroid Exam
- Tongue Exam
- Liver Disease, Head to Foot
- Visit the 25
- Shoulder Exam Tutorial
- Parkinson's Disease Exam
- Diastolic Murmurs Exam
Annular excursion contributes to efficient cardiac output: a three-dimensional echocardiographic approach
Affiliation.
- 1 Department of Cardiovascular Surgery, Funabashi Municipal Medical Center, Chiba, Japan. [email protected]
- PMID: 20369511
Background and aim of the study: The heart produces an efficient cardiac output by repeating diastole and systole. With the evolution of three-dimensional (3D) echocardiography, it is possible to evaluate cardiac motion using detailed 3D morphologic echocardiography. The study aim was to evaluate mitral and aortic annulus excursions towards the apex of the left ventricle, using 3D echocardiography. Measurements of the angle variation between the mitral and aortic valve throughout the cardiac cycle were performed to determine the effects of annulus excursion on cardiac function.
Methods: Seven healthy adolescents (five males, two females; mean age 15.9 +/- 1.1 years; Group H) and seven patients with dilated cardiomyopathy (seven males; mean age 63.6 +/- 12.9 years; Group D) were selected. All subjects underwent 3D echocardiography between November 2007 and June 2008. Annulus excursion (AE) was defined as the annular motion towards the apex. The Ex-Ratio A (%) and Ex-Ratio M (%) were defined as the ratios of aortic or mitral excursion, respectively, to the maximal distance from the annulus to the left ventricular apex. The annulus was defined simply as a flat round disc, and the annular area calculated as the annular distance between the anterior and posterior annulus as a circle diameter. The annulus excursion volume (AEV) was calculated by multiplying the annular area by AE, and determined for each valve of each patient. The total AEV was the summation of the mitral and aortic AEVs. The ratio of AEV to left ventricular diastolic volume was expressed as AEV/EDV. Angular variation between the valves was measured during the cardiac cycle with the following values: maximal angle (Dmax), minimal angle (Dmin), and the difference between Dmax and Dmin (Dmax-min).
Results: In all cases, the apex was in a fixed position. The AE was significantly greater for group H than for group D. While AEV did not differ between groups, AEV/EDV(A) and AEV/EDV(M) were greater for group H than for group D. The angle between the mitral and aortic annulus changed throughout the cardiac cycle. The Dmax-min value was significantly greater for group H than for group D.
Conclusion: Annulus excursion contributes to an efficient cardiac output. The angle variation was measured during the cardiac cycle and found to be greater in healthy adolescents. 3D echocardiography represents a useful modality for clarifying 'motional cardiac morphology'.
- Aortic Valve / diagnostic imaging*
- Aortic Valve / physiology*
- Cardiac Output*
- Cardiomyopathy, Dilated / diagnostic imaging
- Cardiomyopathy, Dilated / physiopathology
- Echocardiography, Three-Dimensional*
- Middle Aged
- Mitral Valve / diagnostic imaging*
- Mitral Valve / physiology*
- Myocardial Contraction
- Patient Care & Health Information
- Diseases & Conditions
- Mitral valve disease
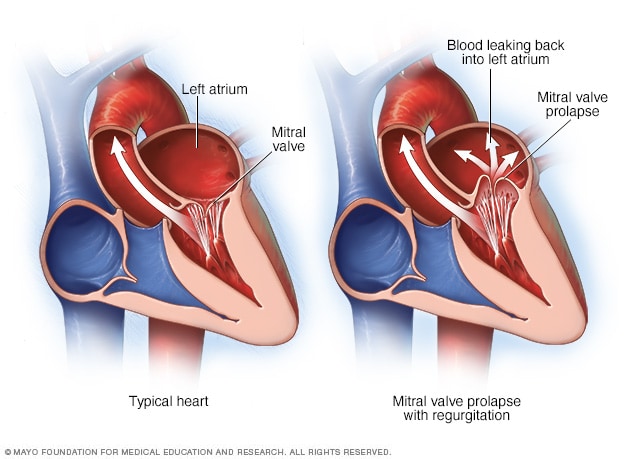
Mitral valve prolapse and regurgitation
The mitral valve separates the two chambers of the left side of the heart. In mitral valve prolapse, the valve flaps bulge into the upper left chamber during each heartbeat. Mitral valve prolapse can cause blood to leak backward, a condition called mitral valve regurgitation.
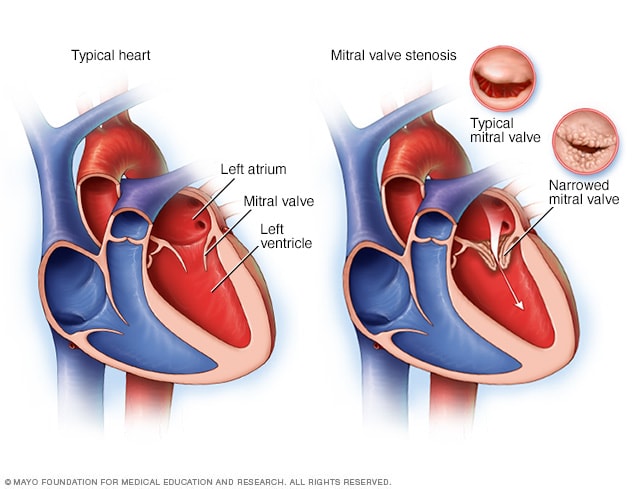
Typical heart and heart with mitral valve stenosis
Mitral valve stenosis, shown in the heart on the right, is a condition in which the heart's mitral valve is narrowed. The valve doesn't open properly, blocking blood flow coming into the left ventricle, the main pumping chamber of the heart. A typical heart is shown on the left.
Mitral valve disease is a problem with the valve located between the left heart chambers. The upper left heart chamber is called the left atrium. The bottom left heart chamber is called the left ventricle.
Mitral valve disease includes:
- Mitral valve regurgitation. The mitral valve flaps, also called leaflets, may not close tightly. This causes blood to leak backward.
- Mitral valve stenosis. The flaps of the mitral valve become thick or stiff, and they can fuse together. This narrows the valve opening, which reduces blood flow from the left atrium to the left ventricle.
Treatment for mitral valve disease depends on the severity of the condition and whether it is worsening. Sometimes, surgery is recommended to repair or replace the mitral valve.
- Mitral valve regurgitation
- Mitral valve stenosis
Some people with mitral valve disease might not have symptoms for many years, if at all.
Symptoms of mitral valve disease can include:
- Irregular heartbeat.
- Shortness of breath.
When to see a doctor
If you have symptoms of mitral valve disease, you may be referred to a doctor trained in heart diseases, called a cardiologist.
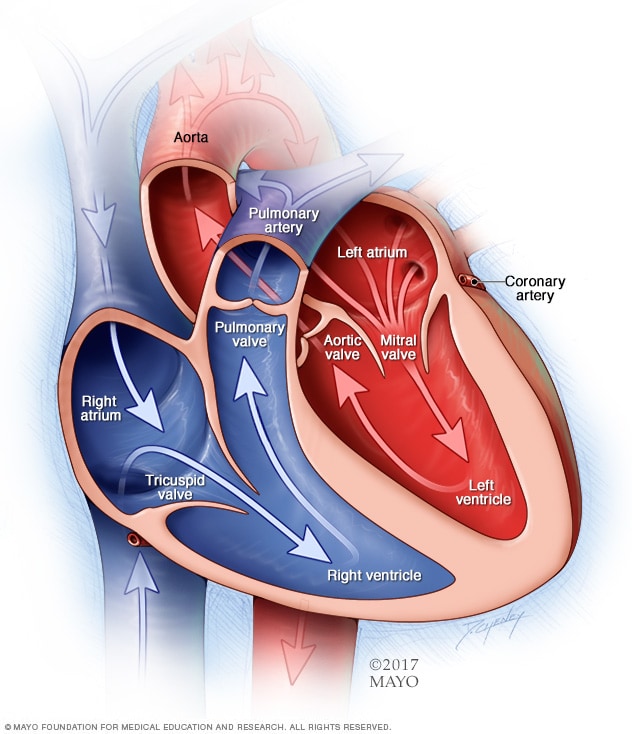
Chambers and valves of the heart
A typical heart has two upper and two lower chambers. The upper chambers, the right and left atria, receive incoming blood. The lower chambers, the more muscular right and left ventricles, pump blood out of the heart. The heart valves, which keep blood flowing in the right direction, are gates at the chamber openings.
To understand the causes of mitral valve disease, it may be helpful to know how the heart works.
The mitral valve is one of four valves in the heart that keep blood flowing in the right direction. Each valve has flaps, called leaflets, that open and close once during each heartbeat. If a valve doesn't open or close properly, blood flow through the heart to the body can be reduced.
- In mitral valve regurgitation, the flaps don't close tightly. Blood flows backward when the valve is closed, making it harder for the heart to work properly.
- In mitral valve stenosis, the valve opening narrows. The heart now must work harder to force blood through the smaller valve opening. If the opening in the valve becomes small enough, it can reduce blood flow between the left heart chambers.
Mitral valve disease has many causes. Some forms of mitral valve disease can be present at birth. A heart problem that you're born with is called a congenital heart defect.
Mitral valve disease also may develop later in life. This means it is acquired. For example, mitral valve stenosis is often caused by rheumatic fever. This fever is a complication of a strep infection that can affect the heart. When this happens, it's called rheumatic mitral valve disease.
Other causes of acquired mitral valve disease include:
- Other heart conditions.
- Age-related changes.
- Autoimmune disease, such as lupus.
Risk factors
Several things can increase the risk of mitral valve disease, including:
- Certain infections that affect the heart.
- Heart attack and some types of heart disease.
- Use of certain drugs.
- Heart condition present at birth, called a congenital heart defect.
- Radiation to the chest.
Complications
Mitral valve disease can cause many complications. Severe mitral valve regurgitation, for example, causes the heart to work harder, which can cause the left ventricle to enlarge and the heart muscle to weaken.
Other complications of mitral valve disease may include:
- Irregular and often rapid heartbeat, called atrial fibrillation.
- High blood pressure in the blood vessels in the lungs, called pulmonary hypertension.
- Blood clots.
- Congestive heart failure.
Mitral valve disease care at Mayo Clinic
Living with mitral valve disease?
Connect with others like you for support and answers to your questions in the Heart & Blood Health support group on Mayo Clinic Connect, a patient community.
Heart & Blood Health Discussions

100 Replies Wed, Apr 24, 2024

71 Replies Wed, Apr 24, 2024

24 Replies Mon, Apr 22, 2024
- Heart valve diseases. National Heart, Lung, and Blood Institute. http://www.nhlbi.nih.gov/health/health-topics/topics/hvd. Accessed May 17, 2023.
- Mitral regurgitation. Merck Manual Professional Version. https://www.merckmanuals.com/professional/cardiovascular-disorders/valvular-disorders/mitral-regurgitation. Accessed May 17, 2023.
- Mitral stenosis. Merck Manual Professional Version. http://www.merckmanuals.com/professional/cardiovascular-disorders/valvular-disorders/mitral-stenosis. Accessed May 17, 2023.
- Otto CM, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Journal of the American College of Cardiology. 2021; doi:10.1016/j.jacc.2020.11.018.
- Valvular heart disease. Centers for Disease Control and Prevention. https://www.cdc.gov/heartdisease/valvular_disease.htm. Accessed June 5, 2021.
- American Heart Association adds sleep to cardiovascular health checklist. American Heart Association. https://newsroom.heart.org/news/american-heart-association-adds-sleep-to-cardiovascular-health-checklist. Accessed May 17, 2023.
- Ami TR. Allscripts EPSi. Mayo Clinic. May 3, 2023.
- Phillips SD (expert opinion). Mayo Clinic. Sept. 30, 2021.
- Lloyd-Jones DM, et al. Life's essential 8: Updating and enhancing the American Heart Association's construct of cardiovascular health: A presidential advisory from the American Heart Association. Circulation. 2022; doi:10.1161/CIR.0000000000001078.
- Mitral valve disease in children
- Mitral valve repair
- Repair of previously replaced valve
Associated Procedures
- Cardiac catheterization
- Chest X-rays
- Echocardiogram
- Electrocardiogram (ECG or EKG)
- Heart valve surgery
- Minimally invasive heart surgery
- Mitral valve repair and mitral valve replacement
Mayo Clinic in Rochester, Minnesota, has been recognized as one of the top Cardiology & Heart Surgery hospitals in the nation for 2023-2024 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Make twice the impact
Your gift can go twice as far to advance cancer research and care!

IMAGES
VIDEO
COMMENTS
excursion. [ ek-skur´zhun] a range of movement regularly repeated in performance of a function, e.g., excursion of the jaws in mastication. adj., adj excur´sive. lateral excursion sideward movement of the mandible between the position of closure and the position in which cusps of opposing teeth are in vertical proximity.
excursion: [noun] a going out or forth : expedition. a usually brief pleasure trip. a trip at special reduced rates.
Protrusion, Retrusion, and Excursion in Healthcare. Healthcare professionals use protrusion, retrusion, and excursion when documenting, performing assessments on patients, or treating disorders. For example, in her head-to-toe assessment, Nurse Sarah asked me to stick out my tongue (an example of protrusion), to assess cranial nerve twelve.
Diaphragmatic excursion. Diaphragmatic excursion is the movement of the thoracic diaphragm during breathing. Normal diaphragmatic excursion should be 3-5 cm, but can be increased in well-conditioned persons to 7-8 cm. This measures the contraction of the diaphragm. It is performed by asking the patient to exhale and hold it.
Protrusion, retrusion, and excursion are terms used in anatomy to describe body movements going anteriorly (forward), posteriorly (backward), or side-to-side...
Percussion is the act of tapping on a surface, thereby setting the underlying structures in motion, creating a sound and palpable vibration. Percussion is used to determine whether underlying structures are fluid-filled, gas-filled, or solid. Percussion: Penetrates 5 - 6 centimeters into the chest cavity. May be impeded by a very thick chest wall.
excursion. 1. Wandering from the usual course. 2. The extent of movement of a part such as the extremities or eyes. 3. In diabetes, an increase in blood glucose levels above normal or typical values, esp. after a meal. There's more to see -- the rest of this topic is available only to subscribers.
excursion. (ek-skŭr′zhŏn) To hear audio pronunciation of this topic, purchase a subscription or log in. [L. excursio, a running out, attack] 1. Wandering from the usual course. 2. The extent of movement of a part such as the extremities or eyes. 3.
Introduction. The diaphragm is the main muscle of respiration [].Diaphragmatic excursion is 1-2 cm during tidal breathing and 7-11 cm during deep inspiration [].The assessment of diaphragmatic function is important for diagnosis and follow up of various physiologic and pathologic conditions [].Several methods exist for the evaluation of diaphragmatic function.
Ultrasound assessment of diaphragmatic excursion was done by experienced ultrasonologists. Diaphragmatic excursion for patients was measured on GE make, Voluson S8 series ultrasound machine. The assessment was done in supine position using M-mode and B-mode techniques in quiet and deep breathing scenarios.
Medical Dictionary. Search medical terms and abbreviations with the most up-to-date and comprehensive medical dictionary from the reference experts at Merriam-Webster. Master today's medical vocabulary. Become an informed health-care consumer!
Methods. We measured the forced the vital capacity (FVC), thoracic excursion, baseline-to-peak diaphragmatic compound muscle action potential (DCMAP) amplitude, diaphragm thickness at full inspiration (DTfi), Medical Research Council (MRC) sum score for muscle strength, and arterial partial pressures of oxygen and carbon dioxide and administered the Amyotrophic Lateral Sclerosis Functional ...
Excursion definition: a short trip or outing to some place, usually for a special purpose and with the intention of a prompt return. See examples of EXCURSION used in a sentence.
EXCURSION meaning: 1. a short journey usually made for pleasure, often by a group of people: 2. a short involvement…. Learn more.
diaphragmatic excursion: In respiration, the movement of the diaphragm from its level during full exhalation to its level during full inhalation. Normal diaphragmatic excursion is 5 to 7 cm bilaterally in adults. It may be seen during fluoroscopic or ultrasonographic examinations of the chest, or percussed during physical examination of the ...
Synonyms trip trip journey tour expedition excursion outing day out These are all words for an act of travelling to a place. trip an act of travelling from one place to another, and usually back again:. a business trip; a five-minute trip by taxi; journey an act of travelling from one place to another, especially when they are a long way apart:. a long and difficult journey across the mountains
A normal circumferential measurement of three and one-fourth inches (8.48 cm) is explained. The importance of this chest excursion measurement in the respiratory portion of the patient's evaluation is related to his treatment program and activity goal. The mean and standard deviations of age, vital capacity, and excursion according to the ...
EXCURSION definition: 1. a short journey usually made for pleasure, often by a group of people: 2. a short involvement…. Learn more.
Pulmonary Exam: Percussion & Inspection. The pulmonary exam is one of the most important and often practiced exam by clinicians. While auscultation is most commonly practiced, both percussion and inspection are equally valuable techniques that can diagnose a number of lung abnormalities such as pleural effusions, emphysema, pneumonia and many ...
Annulus excursion contributes to an efficient cardiac output. The angle variation was measured during the cardiac cycle and found to be greater in healthy adolescents. 3D echocardiography represents a useful modality for clarifying 'motional cardiac morphology'.
lateral excursion: [ ek-skur´zhun ] a range of movement regularly repeated in performance of a function, e.g., excursion of the jaws in mastication. adj., adj excur´sive. lateral excursion sideward movement of the mandible between the position of closure and the position in which cusps of opposing teeth are in vertical proximity.
Complications. Mitral valve disease can cause many complications. Severe mitral valve regurgitation, for example, causes the heart to work harder, which can cause the left ventricle to enlarge and the heart muscle to weaken. Other complications of mitral valve disease may include: Irregular and often rapid heartbeat, called atrial fibrillation.