You are using an outdated browser. Please upgrade your browser to improve your experience.
Skip to Site Navigation Skip to Page Content
- Physician Referrals
- Patient Resources
- Why UT Southwestern
Refine your search: Find a Doctor Search Conditions & Treatments Find a Location

Appointment New Patient Appointment or Call 214-645-8300
Kidney Transplant

Patient Journey
Appointment New Patient Appointment or 214-645-8300
Explore Kidney Transplant
We understand the road to transplant can seem overwhelming for patients. So we’ve created a series of videos to help explain the transplant journey from evaluation to waitlisting, and from pre- to post-transplant. Our dedicated team is here for you every step of the way. Hear from our experts on what to expect.
Kidney Transplant Overview
Learn how UT Southwestern approaches kidney transplantation in a multidisciplinary way. Discover how we make your path from evaluation to surgery as smooth as possible.
Hospital Course
Our Surgical Director, Dr. Parsia Vagefi , explains what to expect before, during, and after your kidney transplantation surgery.
Deceased-Donor Options
Our Medical Director, Dr. David Wojciechowski , explains the different types of deceased-donor options available once you are listed for transplant. Our team is dedicated to providing you with the best possible outcomes by finding innovative options to decrease your wait time.
The Benefit of Living Donors
Learn about the advantages of a living-donor kidney transplant, the different types of living-donor options, and how to talk to potential donors.
Nutrition and Transplant
Hear from our transplant dietitian about the importance of nutrition before and after your transplant in order to ensure the best recovery and long-term health maintenance. We talk about the support UT Southwestern offers you every step of the way.
Post-Transplant Medications
After your transplant, you will be on several medications. Our transplant pharmacist discusses the different types of medications and our team’s role after your transplant.
Basics of Transplant Finance
Learn about the basics of transplant finance and the role of our dedicated financial coordinator, who will help you navigate the financial aspects of transplantation and all phases of care.

Transforming Outcomes
Insights on skin, infection and patient care
Taking a Holistic View of the Patient Journey: a Transplant Coordinator’s Perspective

Patient experience and patient journey are two terms used in healthcare, often interchangeably, to describe how we thoughtfully interact with patients. However, these two terms refer to very different aspects of patient care. While most clinicians enter the patient’s journey for a moment in time, adding to the experiences that become their overall journey to wellness, there are few roles that allow the nurse to experience the full journey with the patient.
I learned, in one of those roles, that having a holistic view of the patient journey can make all the difference.
As a renal and pancreas transplant coordinator, I was the core touchpoint for all my patients. It was common to care for over 1,000 patients simultaneously, as when you receive an organ transplant the coordinator becomes like a member of your family, often for life. From the point of transplant, I constantly worked to ensure the patient could get labs drawn, reviewing those labs for trends or abnormalities and ensuring they were able to receive their medications without pause and took them correctly. In our complex health care system, doing all this could sometimes mean moving mountains to ensure patients have what they need. This close relationship helps ensure care is done holistically, with the patient at the core of the decision-making process. Eventually, recipients become less dependent on their coordinator, yet will reach out for every medical ailment or question, no matter how unrelated to their transplant it may be.
By closely following the patient journey, the coordinator can pick up on nuances that, ultimately, can be lifesaving. And, for Ron* that was literally the case. Ron was a new renal transplant recipient challenged with a lack of healthcare knowledge and support system as well as extreme comorbidities. Like many patients, I worked with him very closely following his transplant, and I learned that he loved coming into the clinic to learn about his health and how he could continue to improve to become more independent in his care. He enjoyed talking with all the coordinators, nephrologists, and surgeons and looked forward to his appointments. One day, he didn’t show up and when I called, he didn’t answer. Sixty minutes went by and still nothing. Most would leave it at that, with a voicemail to reschedule the appointment. But I knew that while Ron had many challenges, he was dedicated to his health care. When there was no answer from his emergency contact as well, I called 911 for a welfare check.
Ron was found unconscious. He had fallen in the middle of the night and couldn’t get up. He was transported to the hospital where he spent several days and, while he had a serious wound from his fall, he ultimately recovered.
While not all stories will involve literally saving someone’s life, Ron’s story is just one example of the difference a health care advocate following along the patient journey can have on the patient’s experience and outcomes.
Just a few additional ways this style of care can save both resources and money for the facility and patient may include:
- Ensuring the patient does not undergo unnecessary procedures. When we know a patient already had a procedure done, even if in another health system, we can navigate the system to receive the results and reduce extra work.
- Reducing the number of physician visits. The patient can talk to their transplant coordinator about any medical concerns and we can provide them direct access to the correct specialty clinic rather than numerous physician visits to address an issue.
- Faster therapeutic care. When a patient is prescribed a medication they previously reacted poorly to, we can call their physician to have them try something else.
Navigating the complex health care system is never easy, and I often consider how many patients could be helped and how many lives could be saved if they had a health care advocate such as a transplant coordinator. Understanding the full patient journey is key to improving the patience experience and ultimately improving outcomes. Most clinicians enter the patient’s journey for a moment in time, yet when we can put those experiences together, we can support the patient on their journey and provide holistic care that is empowering and effective.
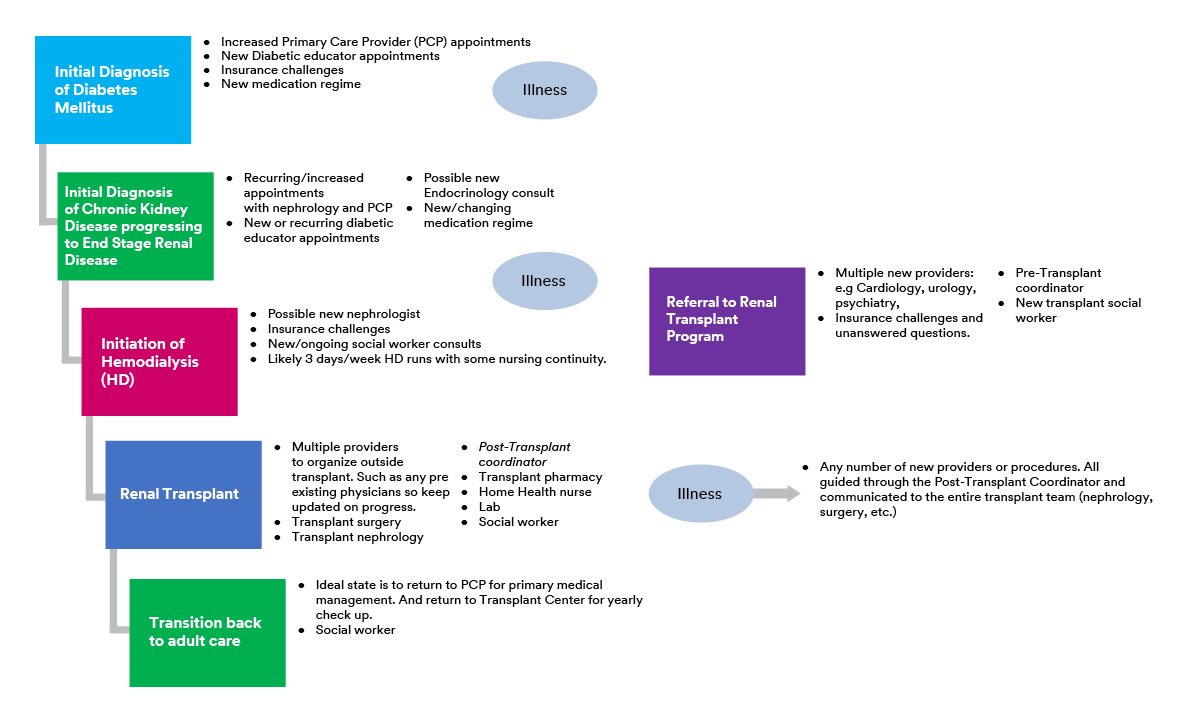
This example of a transplant patient’s experience through the health care system shows how complex and challenging the patient journey can be, with many touchpoints involving various different care providers.
*Name has been changed.

About Post Author
Whitney ficocello, bsn, rn, phn.
- Business of Healthcare
- Innovation and Science
- Patient Experience
- Reducing Preventable Infections
- Think Skin Deeper
- Skin and Wound Management
- Anna A. Kuang
- Caroline Johnson
- Debra M. Thayer
- Dr. Matthew Regulski
- Janet Prust
- Jessica Pehrson
- Kiley Black
- Kimberly Schommer
- Matthew M. Cooper
- Nikki Kluck
- Sarah Isakson
- Whitney Ficocello
- William Leiva
- Share Your Story
Related Post
New study shows 3m™ v.a.c.® therapy is more cost effective compared to competitors, being proactive in the wake of a positive brca2 result: susan’s story, the call for better diabetes care: why i had to amputate my father’s foot, no colon, still rollin’: amber doesn’t let an ostomy slow her down, patient becomes her own advocate for her central line, avoiding bsis for 12 years, meet marla: skin trauma and the patient experience.
- Find a Patient Campaign
- Start an Application

Second Chances Begin Here
If you are in need of an organ transplant or a living donor, you have come to the right place. We provide guidance through the process and grant opportunities to help cover out-of-pocket transplant-related expenses. Visit our “Start an Application” at the top of the page to get started.
If you’re a friend of family member of a transplant patient, we are glad you are here. We would love to talk to you about our fundraising tools and how you can help raise funds to help the Mission of National Foundation for Transplants. Click Fundraise and enter your email to create an account. We will reach out with ideas and best practices for fundraising.
If you are a referring medical professional, we can help. Contact Us to find out how.
To make a gift to National Foundation for Transplants, click the “Donate Now” button to find out how to help today!

Adopt-A-Patient
The Adopt-a-Patient site offers donors information to help them relate, connect, and give to individuals in need. This practical tool answers the questions of how their financial donation will be used and whose life can be saved or healed.

Second Chance Saturday
Meet NFT newest transplant patients. We look forward to serving them, their transplant center, medical professionals, family and friends.

Whose Life Can You Save?
Whose life can you save? They may be closer than you think. View the I Am BoLD video and learn the benefits of Living Donation
104,079 patients on the waiting list
42,888 January – December 2022
1:8 1 donor can save 8 lives
We’re here to help ensure nothing stands in the way of you and a second chance.
We support patients in all 50 states and u.s. territories..
Get informed >
Help is what we do

Fundraising Guidance
A fundraising consultant is assigned to every patient to assist their fundraising campaign. Consultants are full-time staff members, available M-F, 8:30 to 4:30 CST.

Payments & Reimbursement
Patients financial needs are immediate. NFT provides prompt processing of submitted payment requests via direct payment to providers or direct deposit to the patient.

Peace of Mind
NFT relies on public trust to do our work and strive to continuously maintain that trust through our commitment to ethical principles, transparency, and accountability. Our operation is one of the most efficient of its kind.

New CEO: Jared Wall
Jan 11, 2023
On Tuesday National Foundation for Transplants announced that Jared Wall is the organization’s new president and chief executive officer. Wall, coming from a senior leadership position with Children’s Miracle Network Hospitals, has joined the organization full time at...
How’s Your State Doing on Donor Protection Measures?
Oct 4, 2022
While awaiting passage of a federal Living Donor Protection Act (LDPA), more than half of states now have their own version (28 at last count). In fact, like North Carolina, some actually are more generous than the federal version (by including paid leave for state...
For all of our success, there are more patients every year who need our help. Help us fulfill our mission.

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.

Trusted Health Information from the National Institutes of Health
A patient's kidney transplant journey
Lupus patient shares organ donation experience with mother.

Alison Lee was diagnosed with lupus at 16 years old.
Alison Lee is a fighter. She has fought lupus, kidney failure, and cancer—all in just 35 short years.
Alison was diagnosed with lupus at 16 years old. Lupus is a disease in which your immune system attacks your healthy cells and tissue by mistake. Lupus may affect the kidneys and can lead to kidney failure.
However, Alison didn't experience serious lupus symptoms until she was in her mid-20s, when she started to have anemia (or lack of red blood cells), shortness of breath, and heart issues.
At that point, she was living in New York City and doing things many other 20-somethings do: working, hanging out with friends, and enjoying life.
Kidney failure
But things got worse in 2014 when her lupus started to damage her kidneys. She remembers feeling fatigued and very weak.
"When going to dinner with my friends a few blocks away, I would need to stop and take a break and sit on a bench because I couldn't walk three blocks," Alison said.
She also noticed decreased urine output. Her kidneys started to fail. She remembers feeling fatigued and going in and out of the hospital.
"I would go through an entire day at work without having to pee at all. I knew something was going on," Alison said.
Finally, in 2014, she decided to leave her job because she felt so sick. In 2015, she started kidney dialysis because her kidneys were unable to work well enough to keep her healthy.
"Because my heart had been struggling for so many years, my doctors said it wouldn't be able to handle a kidney transplant," Alison said.
"Dialysis was really difficult for me. At the beginning it was like a full-time job because you need to drain and refill the fluid every four to six hours. It was difficult to have a normal life," she added.
However, the dialysis improved Alison's health dramatically.
Preparing for a transplant
After six months on dialysis, she was healthy enough for a transplant. She had a transplant evaluation and asked family members to be tested to see if any of them would be good potential donors.
Alison was one of the lucky ones when it came to finding a donor. Her mom, sister, and brother all offered to donate.
"Of course, my mom being my mom said she would donate," Alison said.
Her mom wouldn't have it any other way. "My mom is so selfless, and she has helped me throughout all of my health issues in the past," Alison added.
Despite her fears, Alison said the excitement about the future outweighed her concerns about the surgery.
"The whole transplant experience was straightforward and easy. The hospital wanted to make sure I understood everything that was happening with the transplant and also post-transplant," Alison said. "I was more excited about the prospect of the future than scared about the procedure."
After surgery, Alison woke up and had to pee a lot, which was a good sign. It meant her kidney was working well. Her blood work was also positive.
Alison's mom, who was in her sixties at the time, also did well. She was back up and helping take care of Alison during her recovery just three days after surgery.
A difficult recovery
While the transplant surgery was straightforward, Alison's recovery wasn't easy.
About a month after surgery, she discovered a lump growing behind her ear. She ended up contracting lymphoma, a cancer of the lymph nodes. While very rare, a drug Alison needed to prevent rejection of her transplant allowed a slow-growing lymphoma she had before the transplant to transform into a more aggressive lymphoma.
"It's not common, but I had some history of a slow growing lymphoma in my past, so they knew this was a risk. Coupled with my recovery from transplant, I also had to go through the biopsy and the chemo treatment that I did for about four months," Alison said.
Despite the difficult battle of recovery coupled with chemotherapy, Alison's positive attitude and family helped her each step of the way. An unexpected benefit from her chemo was decreased rejection of her transplanted kidney. "The chemo was surprisingly beneficial for my transplant. I was given lots of fluid which helped to keep the new kidney hydrated. Also, the chemo itself essentially killed my immune system, preventing it from attacking the new kidney," Alison said.
The next chapter
Alison is in remission but still deals with related health issues. She works closely with the Lupus Research Alliance, focusing on patient advocacy and sharing her story and message of hope with others. She recommends other people struggling with health issues find a support group or organization.
"It's good for me to interact with other lupus patients. It helps me to feel more comfortable with my disease," Alison said.
Alison also works part time and carves out time to travel and enjoy the little things. She recently traveled to Mexico for a yoga retreat.
"I think a positive attitude is really important," said Alison. "Even through all of this, I've never felt like I was dying or wasn't going to survive. Each issue just becomes another bump that I have to get through until things will get better."
July 12, 2018
Explore More on MedlinePlus.gov
You may also like.

Getting a kidney transplant: What you need to know
In the U.S., an estimated 14 percent of the population has chronic kidney disease, and roughly 661,000 Americans have kidney failure....

Improving organ donation for all
Dorry Segev, M.D., Ph.D., is a leader in the field of organ transplantation. The Johns Hopkins University surgeon...
Trusted health information delivered to your inbox
Enter your email below
Click below to check your order status.
Note, order lookup is only supported in the following countries: United States, Canada. If you are outside one of those countries please reach out to One Lambda Customer Support to submit an order status inquiry.

The Transplant Journey and the Role of Clinical Diagnostics
Demystifying your journey to wellness.
While each person’s journey is unique, here is an overview of what you can expect to experience before, during, and after your transplant. One of the most important initial steps you can take is to empower yourself with information, so we have prepared this summary to help demystify your journey—specifically, to help you understand the role modern diagnostics play in supporting your care throughout the transplant process and your path toward an improved quality of life.
Share This Page

Assessment ❯

Eligibility and Preparation ❯

Pre-Transplant Screening ❯

Transplant Surgery ❯

Post-Surgery Recovery ❯

Post-Transplant Monitoring ❯
Understanding the Six Major Phases of the Transplant Process
The tests that labs use to help understand the genetic and physiological realities between a donor and recipient are vital to the transplant process, and will hopefully seem less mysterious to you. Ultimately, what all transplant diagnostics have in common is that, at every phase of your journey, they help your transplant team better understand your immune system. They also help make sure that you are ready to receive the new organ as quickly as possible, and that, after surgery, it will function harmoniously with your body. Even with the challenges of surgery and medication, transplantation is far less restrictive than other treatment options and holds the promise of a dramatic increase in both the quality and length of your life. (Click to expand this card)
Phase 1 – Assessment
The journey begins when your doctor identifies the need for a transplant. Depending on the nature of your case—the type of transplant needed and the urgency of your medical condition—your doctor may advise you to make lifestyle changes to increase the likelihood of a successful transplant or of your eligibility for placement on the organ transplant waiting list.
Your doctor will then refer you to a transplant program for further evaluation, or you may choose a program based on your location, resources, insurance, or other circumstances.
Phase 2 – Eligibility and Preparation
To begin preparing for your potential transplant, your transplant program team will learn more about you and help you understand the decisions that will determine your individual transplant journey. There are two types of donor organs for which you may be eligible: organs from either a deceased or living donor. Heart, and most lung and liver, donations are from deceased donors. For kidney, stem cell, and other transplant types, you may seek a living donor. Both types have a high success rate, but the scheduling can be more predictable with living donors. According to the Organ Procurement and Transplantation Network , in 2020, 85% of organ donations were from deceased donors. And while most living donations are from family members, one out of four are from donors who are not biologically related to the recipient ( American Transplant Foundation ). You will confer with your transplant team to determine the right type of donor for you.
Each transplant hospital team has its own criteria for determining your eligibility for receiving a transplant or being placed on the national waiting list. If you are found to be a good transplant candidate through the screening process, your team may schedule your transplant if you have been matched with a living donor, or they may add you to the waiting list, where your wait time will vary depending on your needs and the availability of a compatible donor. Transplant hospitals in the United States enter information from donors and candidates into a database operated by the United Network for Organ Sharing (UNOS ), which helps match candidates with donor organs.
Phase 3: Pre-Transplant Screening
As part of determining your transplant eligibility and needs, the pretransplant screening process involves three main types of clinical diagnostics (laboratory tests):
- Blood-type testing determines your “ABO” blood type. Everyone has one of the four inherited blood types: A, B, AB, or O, and within those types are many subtypes ; this test is important since ideally the transplant donor and recipient should have compatible blood types. Labs use real-time PCR technologies to identify ABO blood type quickly and accurately.
- HLA typing (tissue typing), along with blood type testing, helps your transplant team assess the compatibility of a donor. This test looks at gene types that encode human leukocyte antigens (HLAs), the molecular markers on your cells that help your body identify the difference between self (i.e., parts of your body) and non-self (i.e., things that are not part of your body). Recognizing this difference helps the body protect itself by attacking what isn’t a part of it, like a bacterial or viral infection. When your body recognizes antigens on a transplanted organ as different from its own, it directs white blood cells to attack. This is what is meant by rejection of a transplanted organ. In other words, HLA typing gives your transplant team information about how your body recognizes what is you and what is new. Modern HLA typing uses next-generation sequencing (NGS) technology to indicate whether the donor’s and recipient’s HLA genes are closely matched. In some transplants, such as for the kidney, a close match results in better graft function, longer graft and patient survival, and reduced risk of rejection. A graft is any tissue that is transplanted from one body to another. To further help prevent rejection, when you receive a new organ, you will be prescribed immunosuppressants—medicines that help control your immune system’s response to the organ. In kidney transplant patients, the level of donor and recipient HLA compatibility also helps determine how much immunosuppressant is needed to enable acceptance of the new organ.
- HLA antibody testing determines whether your body already has antibodies formed against HLA. While most patients won’t have HLA antibodies, if you do, it will be important to find a compatible donor that doesn’t display that antigenic target, so your immune system won’t recognize the transplant, and your body won’t trigger a rejection event. Under what conditions would you already have antibodies against a donor? The formation of HLA antibodies usually occurs via one of three different routes: previous transplantation, previous transfusion of blood products, or pregnancy. If you have received a previous transplant where there was not an optimal match, you may have formed antibodies against that transplant. Some patients who have had multiple transplants may have formed many different HLA antibodies. These patients may find that identifying a match for a further transplant is significantly more challenging. In the case of blood transfusions, cells with HLA genes that don’t match those of the person receiving the blood can be passed on to the recipient from the blood donor. This can result in an immune response in the patient, which may in turn lead to antibody production. Because a pregnant woman is exposed to the genetic material of the fetus, and the fetus contains HLA-coded genes from not only the mother but also the father, there is a high probability that HLA antibody formation will follow. Thus, clinicians have observed that there is a significant number of women on transplant waiting lists worldwide who have antibodies to HLA formed in this way. Even if your pretransplant test does not identify the presence of HLA antibodies, your antibody profile can change. That’s why you will undergo regular blood tests for HLA antibody screening when you are placed on a waiting list. The most important thing to know about HLA antibodies and your transplant journey is that transplant teams have tools and strategies to identify and characterize these antibodies and to know exactly what they target. Your transplant team can leverage that knowledge to help find the right donor. In recent years, patients with HLA antibodies have begun to receive priority status from organ allocation systems worldwide since their cases present a greater challenge. Additionally, laboratories now have at their disposal an advanced suite of antibody detection products like our LABScreen™ Single Antigen assays . Together, advancements in policy and innovation have led to significant increases in the successful transplant rates of even the most immunologically challenging patients. Thus, while HLA antibodies can complicate the transplant journey, the majority of patients will still be matched with a suitable donor.
Phase 4: Transplant Surgery
Immediately prior to surgery, an additional test, called a crossmatch test, is performed to verify that your donor organ is compatible. Think of it as a miniature test run on the transplanted organ, undertaken in the laboratory. Donor and recipient blood samples are mixed. If antibodies in the recipient's blood attack and kill the donor cells, the crossmatch is considered positive. This means the recipient has previously developed antibodies against the donor’s cells and the transplant cannot move forward. If the crossmatch is negative, the recipient does not have antibodies against the donor HLA and the transplant can be performed.
For heart and lung transplant patients, the crossmatch test is typically performed immediately after surgery, though there are exceptions where the transplant clinical team may choose to perform it beforehand.
Some transplant centers may perform a “virtual” crossmatch test, in which data on the patient’s HLA typing and antibody status are compared with the donor’s typing via analytical software, such as our HLA Fusion™ Software . This allows the transplant center to assess how a patient’s antibodies would interact with the donor cells in a regular crossmatch test. This virtual test is particularly helpful in cases when the transplant clinical team is trying to determine whether a donor organ from outside the regional area would be a good match for their patient.
Phase 5: Post-Surgery Recovery
The typical recovery time after transplant surgery can vary depending on the type of transplant. Kidney patients may require 3 to 4 weeks for recovery; heart and lung patients may take around 6 to 8 weeks. Regardless of the type of transplant, this is when you will begin your regimen of immunosuppression medication, which you’ll need to maintain for the life of your transplant. Transplant doctors emphasize the critical importance of complying with this medication regimen since there is a high rate of correlation between lack of adherence and transplant rejection. Simply put: after your transplant, taking your medicine becomes as vital a part of your life as breathing, eating, and sleeping.
Phase 6: Post-transplant Monitoring
Your journey doesn’t end with the transplant—even if you’ve received a donor organ from an excellent match, it’s not an exact duplicate of your organ. Therefore, an organ transplant is a lifelong treatment rather than a cure. Your life after transplant will include continued adherence to your medical regimen as well as regular monitoring for donor-specific antibodies (DSAs), usually every few months in the first year and less frequently in subsequent years, depending on your health, the circumstances of your transplant, and the protocols of your transplant center. You may require additional tests such as biopsies during the monitoring phase, and your immunosuppressive regimen may be adjusted based on the results.
In cases where your medical team may need a closer view of the state of your transplanted organ, a biopsy of the transplant organ may be required. By taking a biopsy sample, your transplant clinician can determine whether your organ is normal or may be experiencing rejection or injury. A test such as our Molecular Microscope ® Diagnostic System for Heart and Kidney (MMDx ® Heart and MMDx ® Kidney) allows your clinical team to assess the health of the organ on a molecular level and make a more accurate diagnosis.
Testing Enables Life!
The tests that labs use to help understand the genetic and physiological realities between a donor and recipient are vital to the transplant process, and hopefully, they now seem less mysterious to you. Ultimately, what all transplant diagnostics have in common is that, at every phase of your journey, they help your transplant team better understand your immune system. They also help make sure that you are ready to receive the new organ as quickly as possible, and that, after surgery, it will function harmoniously with your body. Even with the challenges of surgery and medication, transplantation is far less restrictive than other treatment options and holds the promise of a dramatic increase in both the quality and length of your life.

Counting on You: 5 Milestones Reached Since Amelia Received a Heart Transplant
At just one-week old, Amelia needed a heart transplant. Discover how she's thriving, reaching baby milestones, and looking forward to many more.

Counting on You: Two New Organs and a New Outlook on Life
Marcus Roberts went from pursuing a career of service to struggling to stay alive. Discover how a dual transplant has helped him live a healthier, fuller life.

Counting on You: 16 Years, 3 Kidney Transplants, and 20 Music Artists Discovered
Kadin Hoven is a 16-year-old music enthusiast and 3-time kidney transplant recipient. See his story and learn how you can help transplant patients like him.

Counting on You: 13 Years Post-Transplant and Over 60 Patients Supported with Transplant Housing
After she received a heart transplant, Ava Kaufman made a promise to give back. Today, she saves lives by providing transplant housing to patients in need.

A Marvelous Gift: The Kidney Transplant Story of Two Friends
When Dayna and David met as college students, they never thought that 40 years later, Dayna would give David her kidney. Read the story of their kidney transplant journey and lifelong friendship.

Kidneys Quest Foundation
This organization helps renal patients in diverse communities who have limited financial resources get access to transplant and donor information, assistance getting on the waitlist, help raise funds for medical expenses, and provide dietary and emotional support.

Meeting the Need for Transplantation: UT Health San Antonio Lab Director Donates a Kidney to Save Lives
Dr. Kelley Hitchman shares her experience as a living kidney donor and an expert in transplant histocompatibility and immunogenetics at UT Health.

Ava's Heart
This Los Angeles-based organization provides critically needed assistance that insurance does not cover to transplant patients including the mandated pre- and post-transplant local housing, assisting donor families with burial expenses, and promoting organ donation.

Receiving a Diagnosis | Letters of Hope - Episode 1
In this video, our patient advocate, Valen Keefer, shares the emotions she felt when receiving a kidney transplant diagnosis and discusses ways to cope while processing the news.

The Painted Turtle
Many children with life-threatening and chronic illnesses would not have the opportunity to have a camping experience. This summer camp provides these children the opportunity to meet other children sharing a similar experience and enjoy being a kid.

In the News | Valen Keefer received new kidney 20 years ago, transplant still going strong
Keefer and Dr. Lawrence were in Boston to attend the 2022 ATC. Keefer hopes to encourage more Americans to become organ donors, and to serve as a resource for those facing future transplantation.

While each person’s journey is unique, here is an overview of what you can expect to experience before, during, and after your transplant.
Join Our Community
Never miss an update from ThermoFisher. Subscribe for news and information.
Please leave your feedback for the current page
Does this page meet your expectations?
Please sign in to access your account. Customers must log in to access some content, recorded webinars, training materials, documents, and software.
Please provide the following to setup your user account. If you do not know your center ID, please leave the center ID field blank.
Passwords do not match
How satisfied are you with your One Lambda experience?

Stages of the Transplant Process

Each transplant journey is different. Some people wait for a long period of time hoping for the day when they get the call that an organ is available. Others arrive at the transplant stage with an eligible living donor and move quickly to surgery and life with their new organ. No matter how it happens there are certain things that happen to nearly all transplant recipients. To best assist you at the stage you are in right now, we have broken down the transplant process into three stages: pre-transplant, during transplant and post-transplant. Please click on each stage to learn more.
Stage of Transplant

Pre - Transplant
The pre-transplant process for children undergoing organ transplantation involves several important steps. First, a thorough evaluation is conducted to assess the child's overall health and suitability for a transplant. This includes medical tests, imaging studies, and consultations with various specialists. The child's medical history, current condition, and any existing complications are carefully considered. Additionally, the transplant team will discuss the potential risks, benefits, and alternatives with the child and their family. Financial aspects and insurance coverage are also addressed to ensure adequate support during the transplant process. If the child is deemed eligible for a transplant, they are placed on the transplant waiting list. Throughout this pre-transplant phase, close communication and coordination between the medical team, child, and their family are critical for ensuring the child's physical and emotional well-being as they prepare for the transplantation journey.

Helpful Resources:
This is not an exhaustive list. Please email us at: [email protected] if you would like to add a resource to this list.
Hospital Packing List for your stay by Pressing On
Pressing On - Hospital Packing Checklists
What Every Parent Needs to Know: A guide when your child needs a transplant
https://optn.transplant.hrsa.gov/media/2464/weparentntk_optn.pdf
Organ Transplants: What Every Kid Needs to Know by United Network of Organ Sharing
https://unos.org/wp-content/uploads/Brochure-113k-What-every-kid-needs-to-know.pdf
What Every Patient Needs to Know by United Network of Organ Sharing
https://unos.org/wp-content/uploads/Brochure-113-What-every-patient-needs-to-know.pdf
How to Find a Living Donor: Make Your Transplant Happen by United Network of Organ Sharing
https://optn.transplant.hrsa.gov/media/2267/find_a_living_donor.pdf
Living Donation: Information You Need to Know by United Network of Organ Sharing
https://unos.org/wp-content/uploads/Brochure-107-Living-donation.pdf
Living Donation by United Network of Organ Sharing
https://unos.org/transplant/living-donation/?gclid=Cj0KCQjwmZejBhC_ARIsAGhCqnd_xoPHK-NosFggsMJSvfibJqYSXrSOwxapslbBjV2uPHEfAZR6bBUaAiqVEALw_wcB
Frequently Asked Questions about Multiple Listing and Waiting Time Transfer by United Network of Organ Sharing
https://unos.org/transplant/?gclid=Cj0KCQjwmZejBhC_ARIsAGhCqndmAuHZ9EQ6qP1zAM9ORHg1MMwnBBky_m2hLbmu5JauF1N_hJogmfkaArCYEALw_wcB
What I Wish I Had Known: Transplant Families Share What They Wish They Had Known Before Their Child Underwent Transplant Surgery by Starzl Network
https://starzlnetwork.org/resource/what-i-wish-d-known/
During Transplant

Staying in the hospital during a pediatric transplant can present various challenges for both the child and their family. Firstly, the extended hospitalization period can be emotionally and physically demanding. Children may experience homesickness, anxiety, and fear due to being away from their familiar surroundings and routines. They might miss out on school, social activities, and time with friends. Family members may face significant stress, juggling responsibilities, and adjusting to the demands of the hospital environment. Secondly, the child may undergo numerous medical procedures, including frequent blood tests, medication adjustments, and monitoring. These procedures can be uncomfortable and tiring for the child, and lead to feelings of frustration or sadness. Thirdly, the risk of infections is high
during a hospital stay, requiring strict infection control measures and limited contact with others. This isolation can impact a child's social and emotional well-being. Lastly, the financial burden of prolonged hospitalization, medical expenses, and potential loss of income can add to the family's challenges. However, with the support of healthcare professionals, social workers, and loved ones, families can navigate these challenges and provide the best possible care for the child during their hospital stay.
The patients and families at Transplant Families have been there and are here to help! During a hospital stay after a pediatric transplant, patients and families may benefit from various resources to support them during this challenging time. Please take a look at the following resources we have gathered that can help make an extended hospital stay following a transplant just a little bit better. We encourage you to lean on all of these resources to try to make the time spent in the hospital as tolerable as possible:
Transplant Team
The transplant team consisting of doctors, nurses, social workers, and other medical professionals involved in the child’s care is a valuable resource. They can provide information, answer questions, and offer support during the hospital stay.
Post - Transplant
After a pediatric transplant, children may face various challenges during their post-transplant life. First, they must follow a strict medication regimen to prevent organ rejection and manage potential side effects. This can be challenging, as medications may have unpleasant side effects and require strict timing and dosage. Additionally, regular medical check-ups, lab tests, and follow-up appointments become routine to monitor the transplanted organ's function and overall health. Secondly, the child may experience physical limitations and fatigue as they recover from the transplant surgery. They may need to engage in rehabilitation programs to regain strength, mobility, and stamina. Adjusting to the new organ and its requirements can

take time. Thirdly, maintaining a healthy lifestyle becomes crucial. Children must adopt a nutritious diet, engage in appropriate physical activity, and avoid activities or substances that can harm the transplanted organ. Finally, emotional and psychological adjustments are necessary. Children may face anxiety, fear of rejection, or concerns about their future health. Regular support from healthcare professionals, mental health providers, and their support system is vital in helping children overcome these challenges and lead fulfilling lives post-transplant.
Immunosuppression FAQ by the Starzl Network
https://starzlnetwork.org/wp-content/uploads/2020/12/Immunosuppression-FAQ.pdf
Medication Adherence Information for Teens by the Starzl Network
https://starzlnetwork.org/wp-content/uploads/2020/12/Medication-Adherence-for-Teens.pdf
Immunosuppression Medication Interactions by the Starzl Network
https://starzlnetwork.org/wp-content/uploads/2020/12/Medication-Interactions.pdf
Psychosocial Care: Emotional and Behavioral Needs by Developmental Age by Starzl Network
https://starzlnetwork.org/wp-content/uploads/2020/12/Psychosocial-Care.pdf
Rejection FAQ: Frequently Asked Questions About Rejection by Starzl Network
https://starzlnetwork.org/wp-content/uploads/2020/12/Rejection-FAQ.pdf
School Resource Packet for Transplant Families: A Comprehensive Guide for Educational Resources by Starzl Network
https://starzlnetwork.org/wp-content/uploads/2020/12/School-Resource-Packet.pdf
It’s important to remember that pediatric transplant is a treatment and not a cure. There are a number of excellent organizations who focus on making each pediatric transplant successful. We encourage you to take a look at the websites of the following organizations.
Helpful Organizations
American Society of Transplantation / Power2Save : https://www.myast.org/
Power2Save is on a mission to prove that everyone has the power to save a life by supporting transplant research, advocating for public health, and promoting organ donation. Anyone has the power—whether you are an organ donor, family or friend of someone who needs an organ or has donated one, a medical professional, or an individual or organization who simply believes in making a difference—we all play a part. The Power2Save initiative reaches thousands of recipient families, the medical community, individual advocates and registered donors. Companies who support Power2Save programming allow AST to continue to educate the public on the importance of funding transplant research, donating organs and advocating for recipient health.
Children's Organ Transplant Association (COTA) : https://cota.org/
Children’s Organ Transplant Association helps children and young adults who need a life-saving transplant by providing fundraising assistance and family support.
Organ Procurement Transplant Network (OPTN) : https://optn.transplant.hrsa.gov/
The Organ Procurement and Transplantation Network (OPTN) is a unique public-private partnership that links all professionals involved in the U.S. donation and transplantation system. Also crucial to the system are individuals who sign organ donor cards, people who comment on policy proposals and countless volunteers who support donation and transplantation, among many others. A driving force of the OPTN is to improve the U.S. system so that more life-saving organs are available for transplant. Patient safety is at the forefront of activities at transplant hospitals, organ procurement organizations (OPOs) and labs.
Scientific Registry of Transplant Recipients (SRTR) : https://www.srtr.org/
SRTR reports on transplant programs and on organ procurement organizations. The OPO reports include detailed information about the donation process at each OPO in the country.
Transplant Life Foundation : www.transplantlifefoundation.org
Serve transplant recipients, donor families, living donors, future recipients, and others in the Donation and Transplant community with programs and educational materials to enhance and improve their lives.
Transplant Living Today : https://transplantliving.org/
Transplant Living Today provides information, resources and support about Transplant Living in our world today.
United Network of Organ Sharing : www.unos.org
Our mission is to unite and strengthen the donation and transplant community to save lives.

See All Patient & Visitor Information
- All Specialties & Services
- Gastroenterology (GI)
- Heart & Vascular
- LGBTQ+ Care & Services
- Neurology & Neurosurgery
- Orthopaedics
- Patient Information
- Billing & Financial Assistance
- Classes & Events
- Insurance Information
- International Patients
- Visiting Us From Out of State?
- Online Second Opinions
- Price Transparency
- Request Medical Records
- Video Visits
- Visitor Information
- Dining Options
- Locations & Directions
- Our Neighborhood & City
- Visitor's Guide
- Magnet Site Visit: Public Notice
Schedule an Appointment
We offer online appointment scheduling for adult and pediatric primary care and many specialties.
Patient Portal
Communicate with your doctor, view test results, schedule appointments and more.

See All Healthcare Professionals Information
- Referring Physicians
- About our Physicians
- Physician Relations Team
- Refer a Patient
- Molecular and Genomic Diagnostic Laboratories
- Nurse Residency Program
- Nursing Careers at UChicago Medicine
- Nursing Careers at Ingalls Memorial
- Nursing Programs
- Nursing Research
- Nursing Student Opportunities
- Employee Resources
- Continuing Medical Education
- Continuing Nursing Education
- Employee Login
- Graduate Medical Education
- Password Reset Self-Service
UChicago Medicine and Ingalls Memorial offer a broad range of challenging clinical and non-clinical career opportunities doing work that really matters.
Research & Clinical Trials
- Clinical Trials
Find a Clinical Trial
- Clinical Trial FAQs
- Clinical Trial Resources
- Office of Clinical Research
- Clinical Trials at Ingalls
- Our Research
- Firsts at the Forefront
- Research & Innovation
- Our Nobel Laureates
- The Forefront: Health & Science News
- Research & Discoveries News
- Biological Science News
Learn more about clinical trials and find a trial that might be right for you.
- Conditions & Services
Pre- & Post-Transplant Care
Transplant care at uchicago medicine.
- Find Transplant Experts
- Find a Location
- Contact Us 1-773-702-4500
Gift of Hope is a non-profit organization that coordinates organ and tissue donation and services to families of donors in Illinois.
Making Your Transplant Process as Easy as Possible
When you come to the University of Chicago Medicine, you can be confident that you will receive the highest level of care. Our experienced team of specialty physicians, nurses and other health care professionals is dedicated to your well-being.
Our mission is to provide superior health care in a compassionate manner, ever mindful of each patients' dignity and individuality. We encourage you to discuss your schedule with your caregivers and to ask questions about your treatment plan. Your team will keep you up to date on scheduled tests, procedures, medications and other aspects of your care.
What to Expect Before Your Transplant
Patients in need of transplantation come to us in a variety of ways. Your first visit with us may be with a transplant coordinator, in a transplant education session or an appointment with one of our medical physicians who specializes in transplant. No matter which of our transplant team members you see first, your transplant evaluation will include a few key steps:
- A pre-transplant coordinator will help set up all of your tests and meetings. How quickly the evaluation is completed depends on your availability as well as your medical condition. You may need to take some time off work to complete the tests, but we will try to make appointments as convenient as possible.
- A review of your insurance coverage will be done to calculate what out-of-pocket expenses you may have for a transplant and for the medications you will need to take after the transplant.
- In preparation for finding a donor for your transplant, your blood will be tested for blood type, genetic markers and antibodies. The testing you have as part of your transplant evaluation will depend on your medical history.
After you have completed the evaluation testing and appointments, your case is reviewed by our team of specialty physicians to determine the best course of treatment.
- Kidney transplant evaluation locations
- Liver transplant evaluation locations
What to Expect After Your Transplant
In most cases, you should be able to resume your daily activities — such as driving, household chores, work, school and some sport activities — in three to six months after the procedure.
You will receive advice about your recovery period, including wound care and/or line care, showering, driving, physical activity and what to expect when you are able to return to you usual routine.
We will advise you about diet, medication, emotional issues and the important task of preventing infections, as well as what happens if your body rejects the organ or transplanted cells.
Your team will be available for post-operative clinic visits, checkups and advice on a variety of life issues. After your transplant, you will have frequent appointments with the transplant team to make sure you are recovering well. These visits will be less frequent over time. We are available 24 hours a day, seven days a week to answer questions and help you enjoy this new phase of your life.
Transplant Support Team
Besides the doctors, University of Chicago Medicine offers transplant patients a team of support staff. Here's a rundown of each member of the support team.
Transplant Social Worker
The problem solver who directs issues to the appropriate team member. Provides emotional support and helps the patient navigate the health care system and pay for needed post-surgery services.
Pre-Transplant Coordinator
A nurse or nurse practitioner who educates patients about their upcoming evaluation and potential surgery. Monitors their pre-surgery tests, lab work, appointments and instructions.
Post-Transplant Coordinator
A nurse practitioner who stays connected to patients for life, or until they move out of the area and to another hospital. Adjusts medication as needed, sees patients in clinic, monitors labs and tests, schedules appointments and orders or interprets diagnostic tests. Prepares patients for post-hospital life. Works with insurance companies to get tests approved and handles disability paperwork.
Insurance/ Financial Coordinator
Deals with insurance approval for evaluation and potential transplant surgery.
Designs a customized dietary regimen to help prevent nutrition-related illnesses or problems.
Manages and dispenses medications. Watches for dangerous medication interactions, and adjusts medications based on test results. Works to keep patients’ drug costs low by finding medicines covered by insurance or helping patients enroll in special prescription programs.
Help When Traveling from Outside the Chicago Area for Medical Care
For Logan Andrews and his family, traveling from North Carolina to Chicago for Logan's heart and liver transplant care required special assistance beyond medical expertise. The family turned to the Destination UChicago Medicine team to help scheduling appointments, arranging travel and finding accommodations.

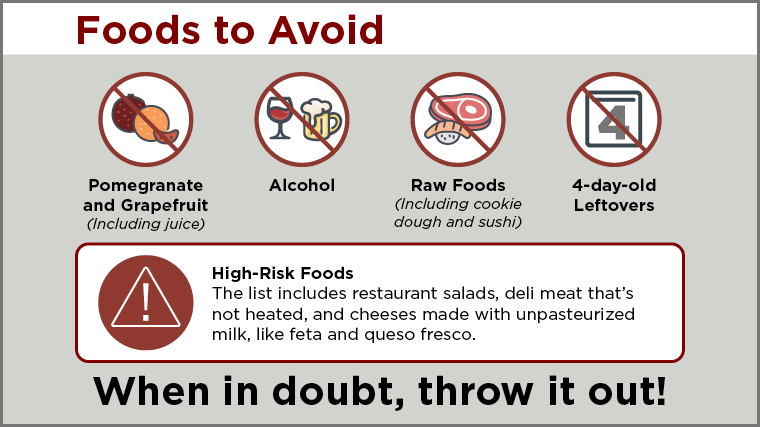
Healthy Diet and Food Safety Tips for Transplant Recipients
Transplant recipients must follow a strict diet after their surgery to prevent getting a foodborne illness. Due to their immunosuppressive medications that keep their bodies from rejecting a new organ, transplant recipients are more susceptible to developing infections, and a foodborne illness can make a patient seriously ill. Here are some of the main takeaways from our experts.
Explore the Process for Each Type of Transplant Surgery
Transplant articles.

I'd Like to
- Make an Appointment
- Find Classes & Events
- Make a Donation
- Apply for a Job
- Patients & Visitors
- Healthcare Professionals
- Comer Children's Hospital
The spiritual journey of an organ transplant patient
Affiliation.
- 1 Our Lady of the Resurrection Medical Center, 5645 W. Addison Street, Chicago, IL 60634, USA.
- PMID: 12875126
- DOI: 10.1177/154230500305700209
In this article, a hospital chaplain presents a detailed narrative of the psychological, emotional, and spiritual dynamics of an organ transplant patient. The chaplain explicates the many complex factors that may characterize an organ transplant patient's recovery and the many persons--family members and hospital personnel--who can be impacted by such a journey.
- Chaplaincy Service, Hospital
- Family / psychology
- Interpersonal Relations
- Organ Transplantation / psychology*
- Pastoral Care
- Professional-Patient Relations
- Spirituality*
- United States
Jump to content

OptumHealth Education
- Create account
Bookmark/Search this post

You are here
Transplant patient perspective: navigating the transplant journey and enhancing patient care.

- Faculty and planners
- Accreditation
- Register/Continue
ACTIVITY DESCRIPTION
Patients who have received an organ transplant can provide valuable insights into the entire transplant journey, bringing new awareness to the physical, emotional, and psychological aspects of the transplant journey. In this session, Melissa Roberts, MSN, RN, who is the director of organ donation and transplant services at her institution as well as a double-organ transplant recipient, will share her personal experiences, including pre-transplant preparations, the peri-transplant period, and post-transplant challenges. She will candidly discuss her concerns, issues, and the unique aspects of patient care that can impact outcomes, drawing from both her transplant journey and her professional experiences with other transplant patients. This session will provide healthcare professionals with a deeper understanding of the transplant process and enable them to improve the care they provide to transplant recipients.
Provided by This activity is provided by Optum Health Education.
Commercial support There was no commercial support received for this activity.
Target Audience
This activity has been designed to meet the educational needs of dentists/allied dental staff, dietitians, dietetic technicians, nurses, nurse practitioners, pharmacists, pharmacy technicians, PAs, physicians, psychologists, social workers and other health care professionals.
Learning Objectives
At the end of this educational activity, participants should be able to:
- Describe the transplant experiences of organ recipients, including the challenges and concerns they face throughout the journey.
- Identify the unique aspects of patient care that the medical community should be educated about to improve the overall care and support provided to transplant patients.
- Discuss the physical, emotional, and psychological impact of organ transplantation on patients and how this knowledge can help enhance providers’ empathy, communication skills and clinical care.
- 1.00 ACPE - Pharmacists
- 1.00 ACPE - Pharmacy Technicians
- 1.00 ADA - CERP (Dentists/Allied Dental Staff)
- 1.00 AMA - Physicians
- 1.00 ANCC - Nurses
- 1.00 APA - Psychologists
- 1.00 Attendance - General Attendance
- 1.00 CDR - Dietitians
- 1.00 ASWB - Social Workers
Presenter Melissa Roberts, MSN, RN Kidney and Pancreas Transplant Recipient Senior Director UW Health Transplant Center Madison, WI
Planners Elizabeth Albert, MD Clinical Activity Manager Optum Health Education
Rebecca Gleason, RN, CCM Activity Manager Optum Health Education
Lisa Latts, MD, MSPH, MBA, FACP Senior Medical Director, Value-Based Care Optum
Jennifer Malin, MD, PhD Senior Vice President, Clinical Value Optum Health Chief Medical Officer Optum Health Solutions
Tina Rydland, PharmD Executive Pharmacy Consultant
Crystal Wong, MD President Propoint Medical Writing
Disclosures of relevant financial relationships In accordance with the Accreditation Council for Continuing Medical Education's (ACCME) Standards for Integrity and Independence in Accredited Continuing Education, OptumHealth Education (OHE) requires all those in control of educational content to disclose their financial relationships with ineligible companies within the prior 24 months. Ineligible companies are defined by the ACCME as companies whose primary business is producing, marketing, selling, re-selling, or distributing health care products used by or on patients. Individuals must disclose all financial relationships, regardless of the amount, with ineligible companies and regardless of their view of the relevance of the relationship to the education. OHE ensures that the content is independent of commercial bias.
The presenters and planners have no financial relationships to disclose.
Method for calculating CE credit CE credit was calculated by the complexity of content.
Credit designation statements

Physicians Optum Health Education designates this enduing activity for a maximum of 1.00 AMA PRA Category 1 Credits ™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
PAs The American Academy of PAs (AAPA) accepts credit from organizations accredited by the ACCME.
Pharmacists/Pharmacy technicians This activity is approved for 1.00 contact hours (0.10 CEUs) in states that recognize ACPE. Attending the full program will earn 1.00 contact hours (0.10 CEUs). Unique activity number: JA0007123-0000-23-006-H01-P/T
Nurses The participant will be awarded up to 1.00 contact hours of credit for attendance and completion of supplemental materials.
Nurse practitioners The American Academy of Nurse Practitioners Certification Program (AANPCP) accepts credit from organizations accredited by the ACCME and ANCC.
Dentists/Allied Dental Staff

Optum Health Education is an ADA CERP Recognized Provider. ADA CERP is a service of the American Dental Association to assist dental professionals in identifying quality providers of continuing dental education. ADA CERP does not approve or endorse individual courses or instructors, nor does it imply acceptance of credit hours by boards of dentistry.
Optum Health Education designates this activity for 1.00 continuing education credits.
Concerns or complaints about a CE provider may be directed to the provider, or to the Commission for Continuing Education Provider Recognition at ADA.org/CERP.
Dietitians Completion of this RD/DTR profession-specific or IPCE activity awards CPEUs (One IPCE credit=One CPEU).
RD's and DTRs are to select activity type 102 in their Activity Log. Performance indicator selection is at the learner's discretion.
Psychologists Optum Health Education is approved by the American Psychological Association (APA) to offer continuing education for psychologists. Optum Health Education maintains responsibility for this program. 1.00 CE hours.

Attendance A certificate of attendance will be provided to learners upon completion of activity requirements, enabling participants to register with licensing boards or associations that have not been preapproved for credits. To apply for credit types not listed above, participants should use the procedure established by the specific organization with which they wish to obtain credit.
Available Credit
You must be logged into your account to participate in this activity. Get started by clicking “Register” and following the instructions. At the end of the activity, you will be able to view, save or print your certificate of participation. A complete listing of all of your activities can be found under “My Account,” “My Activities.”
- Bureaus and Offices
- Contact HRSA
- Learn About Donation
- How Donation Works
The Organ Transplant Process
A surgeon moves a donated organ to someone whose organ failed. This is an organ transplant. Certain diseases can lead to organ failure. So can injury or birth defects.
How do I get on the organ transplant waiting list?
Your doctor must refer you. A transplant center or program then checks if a transplant makes sense for you.
Learn about transplant lists, costs, and recovery. The United Network for Organ Sharing (UNOS) created, What Every Parent Needs to Know (PDF - 5 MB) . It gives you an overview of the process.
Make sure the transplant center meets your needs.
Consider its location, if your insurance will pay, how you pay, and if they have support groups. The Organ Procurement and Transplantation Network (OPTN) has a list of member transplant centers .
Contact the transplant hospital. Set an appointment for them to evaluate you. They will decide if you qualify for a transplant.
During the evaluation, ask questions. Learn about that hospital and its transplant team.
If you qualify, the transplant team will add you to the OPTN waiting list . The transplant team will contact you in writing about 10 days after they list you.
Direct any questions about your waiting list status to your transplant team.
How much will it cost me?
Transplants cost money before, during, and after the surgery. You pay these costs, not the donor.
Your health insurance may cover some costs. Call your insurance company or your employer's benefits office. Ask what costs your insurance will pay and how.
What do costs include?
- Lab tests, organ removal, transplant surgeons, and other operating room staff
- In-hospital stays, getting to and from the transplant hospital for surgery and checkups
- Recovery, including physical or occupational therapy
- Medicine (e.g., anti-rejection drugs)
Review questions you should ask your insurance provider and financial coordinator .
Why should I make a financial plan?
You must pay for any costs that insurance doesn’t cover. Think about how you’ll pay these costs. This may include savings, sale of property, etc.
Who can help me with the plan?
Members of the transplant team, such as the social worker and financial coordinator, can help you develop a plan. They may put you in touch with groups that help pay transplant costs.
How else can the financial coordinator help?
Speak with the financial coordinator before you make financial decisions about your transplant.
They can help you:
- understand how your insurance company's benefits apply to transplant surgery;
- make a plan to pay for your transplant;
- make a plan for nonmedical costs, such as living expenses;
- locate sources of funding; and
- understand bills from hospitals, doctors, pharmacies, and other providers.
Can Medicare or Medicaid help me?
Medicare is a federal program. States operate Medicaid. Both are health insurance programs that may help with your transplant costs.
What is Medicare?
Medicare is for people age 65 or older, people with disabilities, or people who have end-stage renal disease (ESRD).
What will Medicare cover for my transplant?
- Medicare Part A is free to those who qualify. It covers inpatient hospital care and some nursing home care.
- outpatient care;
- doctor bills;
- some home health care; and
- prescription medicines including, in some cases, anti-rejection drugs.
Medicare certifies transplant programs throughout the country. You must use a Medicare-approved transplant facility to receive full Medicare benefits.
Find out more about Medicare and organ transplants .
What is Medicaid?
Medicaid is an insurance program for people with low incomes. The federal government and states fund it. States decide who can get it and what benefits and services they’ll cover.
What does Medicaid cover for organ transplants?
Some states' Medicaid plans cover only transplants done in the state. That is, unless there’s no transplant center for that organ in the state.
Some states' Medicaid programs don’t cover transplants. Check what your state Medicaid program covers.
How can Social Security help? Contact your local Social Security office online or call them at 800-772-1213. They can answer questions you have about Medicare or Medicaid. You may qualify for benefits after an organ transplant.
How does the system match organs?
The OPTN has rules for how donor organs match to patients on the waiting list.
This might include how sick a patient is. Their blood type may also be a factor. It depends on the organ.
What happens after my transplant?
Doctors will watch your health years after your transplant. Lab tests will be a regular part of your life.
Talk to your transplant team. Ask:
- what monitoring you’ll need;
- what you can have done at home; and
- what will require visits to the transplant center or other locations.
How will my body react?
Your body may reject a transplanted organ or tissue. It sees it as an invader and tries to destroy it.
Anti-rejection medicine can help. A weak immune system can be slower in defending against germs.
You may get infections more easily. You may find it harder to recover from infections and illnesses.
Protect your health. Follow good prevention practices to avoid illness and injury. Get treatment early when you do get sick.
What medicines can I expect to take?
You’ll probably need to take several kinds of medicine. You may take some medicines several times a day and others only on certain days. Your medicines or dosages may change.
Why should I get to know my pharmacist?
Get to know your pharmacist. They can help you:
- understand your medicines;
- manage your medication schedule;
- explain the effects and side effects of medicines; and
- recommend tools like timers and organizers. These help you keep track of medications.
What should I eat, drink, and avoid?
- High-fiber foods, such as raw vegetables and fruits;
- Calcium-rich foods, like low-fat dairy products and green, leafy vegetables. You could also take calcium supplements.
- Foods high in protein, such as meat, poultry, fish, eggs, unsalted nuts, and beans. Protein helps you build muscles and tissue. This helps you heal.
- Plenty of water, unless your doctor tells you to limit fluids.
- A lot of salt, processed foods, and snacks. Use herbs and spices to add flavor.
- Eating too much.
What kind of exercise can I do?
Limit exercise and muscle strain when you first return home. Talk with your doctor. They’ll tell you what to expect. And they’ll tell you what activity to limit.
Most people feel weak after surgery. You’ll have to recover from the operation. You’ll also have to recover from the illness or injury that made you need a transplant.
When you feel better, exercise will help you regain your strength. You may feel tired at first. Take rest breaks during exercise. Gradually, increase the amount and type of physical activity you enjoy.
Can I contact my donor’s family?
You may want to thank your donor’s family. Sometimes donor families want to check on you. Federal law requires transplant centers and Organ Procurement Organizations (OPOs) to protect donors and receiving patients’ privacy. They can arrange for contact between the families when both sides agree. The process may begin with a letter from you to the donor family. Read the guidelines for the first letter in, Contacting My Donor Family .

Blake was just 16 days old when he received the gift of life. Today, at 14, Blake is a normal, active teenager ... who loves sports, loves his team, and whose favorite subject in school is algebra.
See Blake's Story
You have the potential to help save lives as a donor. You can start by signing up through your state’s registry.
Sign Up Now
- Share full article
Advertisement
Supported by
Patient With Transplanted Pig Kidney Leaves Hospital for Home
Richard Slayman, 62, is the first patient to receive a kidney from a genetically modified pig. Two weeks after the procedure, he was well enough to be discharged, doctors said.

By Roni Caryn Rabin
The first patient to receive a kidney transplanted from a genetically modified pig has fared so well that he was discharged from the hospital on Wednesday, just two weeks after the groundbreaking surgery.
The transplant and its encouraging outcome represent a remarkable moment in medicine, scientists say, possibly heralding an era of cross-species organ transplantation.
Two previous organ transplants from genetically modified pigs failed. Both patients received hearts, and both died a few weeks later. In one patient, there were signs that the immune system had rejected the organ, a constant risk.
But the kidney transplanted into Richard Slayman, 62, is producing urine, removing waste products from the blood, balancing the body’s fluids and carrying out other key functions, according to his doctors at Massachusetts General Hospital.
“This moment — leaving the hospital today with one of the cleanest bills of health I’ve had in a long time — is one I wished would come for many years,” he said in a statement issued by the hospital. “Now it’s a reality.”
He said he had received “exceptional care” and thanked his physicians and nurses, as well as the well-wishers who reached out to him, including kidney patients who were waiting for an organ.
“Today marks a new beginning not just for me, but for them as well,” Mr. Slayman said.
The procedure brings the prospect of xenotransplantation, or animal-to-human organ transplants, significantly closer to reality, said Dr. David Klassen, the chief medical officer for the United Network for Organ Sharing, which manages the nation’s organ transplant system.
“Though much work remains to be done, I think the potential of this to benefit a large number of patients will be realized, and that was a question mark hovering over the field,” Dr. Klassen said.
Whether Mr. Slayman’s body will eventually reject the transplanted organ is still unknown, Dr. Klassen noted. And there are other hurdles: A successful operation would have to be replicated in numerous patients and studied in clinical trials before xenotransplants become widely available.
If these transplants are to be scaled up and integrated into the health care system, there are “daunting” logistical challenges, he said, starting with ensuring an adequate supply of organs from genetically engineered animals.
The cost, of course, may become a substantial obstacle. “Is this something we can really realistically attempt as a health care system?” Dr. Klassen said. “We need to think about that.”
The treatment of kidney disease is already a huge expense. End-stage kidney disease, the point at which the organs are failing, affects 1 percent of Medicare beneficiaries but accounts for 7 percent of Medicare spending, according to the National Kidney Foundation.
Yet the medical potential for pig-to-human transplantation is tremendous.
Mr. Slayman opted for the experimental procedure because he had few options left. He was having difficulty with dialysis because of problems with his blood vessels, and he faced a long wait for a donated kidney.
The kidney transplanted into Mr. Slayman came from a pig genetically engineered by the biotech company eGenesis. Company scientists removed three genes that might trigger rejection of the organ, inserted seven human genes to enhance compatibility and took steps to inactivate retroviruses carried by pigs that may infect humans.
More than 550,000 Americans have kidney failure and require dialysis, and over 100,000 are on a waiting list to receive a transplanted kidney from a human donor.
In addition, tens of millions of Americans have chronic kidney disease, which can lead to organ failure. Black Americans, Hispanic Americans and Native Americans have the highest rates of end-stage kidney disease. Black patients generally fare worse than white patients and have less access to a donated kidney.
While dialysis keeps people alive, the treatment of choice for many patients is a kidney transplant, which dramatically improves quality of life. But just 25,000 kidney transplants are performed each year, and thousands of patients die annually while waiting for a human organ because there is a lack of donors.
Xenotransplantation has for decades been discussed as a potential solution.
The challenge in any organ transplantation is that the human immune system is primed to attack foreign tissue, causing life-threatening complications for recipients. Patients receiving transplanted organs generally must take drugs intended to suppress the immune system’s response and preserve the organ.
Mr. Slayman exhibited signs of rejection on the eighth day after surgery, according to Dr. Leonardo V. Riella, medical director for kidney transplantation at Mass General. (The hospital’s parent organization, Mass General Brigham, developed the transplant program.)
The rejection was a type called cellular rejection, which is the most common form of acute graft rejection . It can happen at any time but especially within the first year of an organ transplant. Up to 25 percent of organ recipients experience cellular rejection within the first three months.
The rejection was not unexpected, though Mr. Slayman experienced it more quickly than usual, Dr. Riella said. Doctors managed to reverse the rejection with steroids and other medications used to tamp down the immune reaction.
“It was a roller coaster the first week,” Dr. Riella said. Reassuringly, he added, Mr. Slayman responded to treatment like patients who receive organs from human donors.
Mr. Slayman is taking several immunosuppressive drugs, and he will continue to be closely monitored with blood and urine tests three times a week, as well as with doctor visits twice a week.
His physicians do not want Mr. Slayman to go back to work, at the state transportation department, for at least six weeks, and he must take precautions to avoid infections because of the medications that suppress his immune system.
“Ultimately, we want patients to go back to the things they enjoy doing, to improve their quality of life,” Dr. Riella said. “We want to avoid restrictions.”
By Wednesday, Mr. Slayman was clearly ready to go home, Dr. Riella said.
“When we first came in, he had a lot of apprehension and anxiety about what would happen,” Dr. Riella said. “But when we rounded on him at 7 a.m. this morning, you could see a big smile on his face and he was making plans.”
Roni Caryn Rabin is a Times health reporter focused on maternal and child health, racial and economic disparities in health care, and the influence of money on medicine. More about Roni Caryn Rabin
The Spiritual Journey of an Organ Transplant Patient
- Related Documents
Lack of immune response after mRNA vaccination to SARS‐CoV‐2 in a solid organ transplant patient
T-cell posttransplant lymphoproliferative disorder occurring in a pediatric solid-organ transplant patient, the organ transplant patient in the obstetric critical care setting, skin cancer in the organ transplant patient, gastrointestinal mucormycosis in a renal transplant patient.
The clinical course and management of a rare case of gastrointestinal mucormycosis occurring in a renal transplant patient are presented. The diagnosis was made on pathological examination of surgically resected tissue from the colon, spleen and stomach. The patient did not survive the infection. To the best of our knowledge, this is the 11th reported case of gastrointestinal mucormycosis in a solid organ transplant patient. The pathophysiology, incidence and prognosis of this disease are discussed.
Catastrophic cutaneous carcinomatosis in the non-organ transplant patient
Penile prosthesis placement in the organ transplant patient, infection in the organ transplant patient: a modern hegelian dialectic (joint symposium with the international immunocompromised host society), chronic hepatitis e infection in an immunosuppressed, solid organ transplant patient, cryptogenic ascites from biopsy proven coccidiomycosis in a seronegative immunosuppressed solid organ transplant patient, export citation format, share document.

Massachusetts General Hospital Discharges First Patient with Genetically Modified Pig Kidney Transplant
A landmark medical accomplishment has been realized as the recipient of the first pig kidney transplant is discharged.
The groundbreaking procedure took place at the esteemed Massachusetts General Hospital (MGH) in Boston where Richard “Rick” Slayman received the organ in March.
Suffering from the life-threatening condition of end-stage renal failure, 62-year-old Slayman can now envision a future without the constraints of this chronic disease.
“This release from the hospital is a defining moment – a significant marker of progress in my health journey,” expressed Slayman joyfully.
“Finally, the hope I’ve nurtured for so long has blossomed into this jubilant reality.”
Overcome with gratitude, Slayman thanked the entire hospital staff for their dedication throughout this unprecedented transplant process.”
“Anticipating a life emancipated from the rigorous schedule of dialysis brings me great joy. I am indebted to all those sending their support, affirming hope for myself and fellow kidney transplant hopefuls,” he continued.
“A wonderful day filled with elation,” described Dr. Leonardo Riella from MGH regarding Slayman’s hospital departure.
The success of this surgery ignites hope that xenotransplantation could be the solution to the acute global donor organ shortage.
“The unmet need for transplant organs is glaring, and this breakthrough could signify a glimmer of hope for the numerous patients awaiting a lifesaving transplant,” commented Dr. Riella.
Remarkably, the kidney implanted in Mr. Slayman was engineered by eGenesis, a company in Massachusetts.
The transplant utilized a cutting-edge genetically-altered pig kidney, modified to enhance compatibility with the human body and diminish rejection risks.
In the quest to conquer transplant rejections, researchers have strived for decades to genetically modify pigs in a manner suited for human transplantation.
For additional insights: Zeroing in on the disarmament debate in Israel & the diminishing use of death row in the US.
In the landscape of organ transplantation, statistics from UNOS reveal that over 100,000 Americans are in need of an organ, with daily fatalities averaging 17 as they wait for a transplant. Kidneys are the most frequently requested organ. In the UK, the waiting list surpasses 5,200 patients, while annual transplants hover around 3,300 operations, Kidney Research UK reports.
FAQ About Genetically Modified Pig Kidney Transplant
This pioneering transplant from a genetically modified pig to a human marks a monumental stride in medical innovation. As Rick Slayman embarks on a new chapter of his life, the broader implications for countless patients worldwide set a precedent for future organ transplant procedures. With continued success, xenotransplantation may soon revolutionize the field of organ donation, bringing hope and life to those who wait.


- Request an Appointment
- Get a Second Opinion
- Share Your Story
- Patient Stories
- Clinical Care
- Our Community

An act of kindness — Raul and Larry’s journey to a non-directed transplant donation

Acts of kindness can come in many forms, like volunteering or donating to a charity of choice. At 52, Larry loves giving back to his local community in Vermont, which is why he works in law enforcement. However, he has taken these thoughtful acts of kindness to another level — he’s donated one of his kidneys and a part of his liver to two different people he had never met. His motivation? Larry says he just wanted to help others.
“The first was a directed donation — meaning I knew what was needed and who would get my kidney — but I didn’t know them personally,” he explains. “For my liver, I decided to do a non-directed donation — so instead of knowing the name of who would receive the piece of my liver, I only knew that I was a match for a child in need.”
For Larry, the reason was simple. “I knew I was healthy and thought that if I could make someone else almost as healthy as I am, why not?”
The road to donating
Larry underwent five months of testing in 2021 before he was approved to donate his kidney. “The call came two days after my birthday and I thought, ‘Wow — now that is a birthday gift,” Larry remembers.
The recovery process was intense, but Larry says it was nothing in comparison to what his recipient must have experienced before the donation. “I knew that the recipient was an adult who had kidney disease for almost eight years, and now he’s able live without that pain,” So, when he heard that he had the chance to help a child with his second donation, he was thrilled.
A year after his kidney donation, Larry was medically cleared to donate again and began testing for his next donation. During this time, he learned that the anatomy of his liver would not be safe to donate to an adult but would be a great fit for a child in need.
When Raul enters the story
While Larry was preparing for his liver donation, a little boy in Connecticut was battling a rare disease and needed a life-saving operation. Raul was born with a urea cycle disorder , a rare disease caused by a faulty enzyme within the urea cycle — the way the body converts excess ammonia into a type of molecule, called urea, in liver cells. Without aggressive treatment including special nutrition formulas, very low protein foods, and multiple medications, high levels of ammonia build up in the blood and brain leading to brain injury. Although this faulty enzyme is in all parts of the body, it can be cured with a liver transplant.
Raul’s mom, Marie, worked with doctors in their home state to have a gastrostomy tube (G-tube) connected to his stomach so they could give him all the medications and special formulas he needed.
Raul was stable until he turned 3 years old, when his bloodwork showed that he was no longer responding to his aggressive treatment plan — a red flag that his body was not clearing ammonia properly and his brain was being affected. The only option left was to receive a liver transplant to fully treat and recover from this disease.
Raul and his family came to the Boston Children’s Pediatric Transplant Center and he was placed on the liver transplant list. Three months later, the piece of Larry’s liver was donated to Boston Children’s and Marie got the call that there was a match for Raul. They drove to Boston Children’s and Raul underwent successful transplant surgery with Dr. Heung Bae Kim and his team of surgeons. Raul has been closely monitored by Dr. Scott Elisofon and his team of pediatric liver specialists.

Finding Larry
A few months after Raul’s transplant, Marie mailed a handwritten donor letter to try and thank his organ donor. As a result, Larry was given her contact information and was told by the transplant team that he could reach out to the family if or when he was ready — which he eventually chose to do online.
Raul’s family and Larry recently met this past Valentine’s Day in Connecticut — providing closure to such an emotional journey for both. With Larry’s donation, he has helped Raul thrive in ways that Marie didn’t think possible. Now age 4, he’s able to eat foods that he couldn’t previously, he’s making friends in kindergarten, and “he’s finally able to just be a kid,” Marie says.
For Larry, being a non-directed organ donor has meant helping others that he never met and allowing them a chance at a healthier life. “I’d do it again if I could, especially seeing how much it has helped Raul,” he says.
Learn more about the Pediatric Transplant Center and register to be an organ donor .
Related Posts :

From Florida to Boston and back again: Reagan's liver transplant journey
Reagan, 18, is gearing up for her freshman year of college this fall, and she has a solid idea about her ...

One day on the field, admitted to the ICU the next: Rob's liver transplant journey
When you’re a teen, it’s not very common to worry about what’s going on inside your body — ...

Running the Boston Marathon with a purpose: Ben's liver transplant journey
Ben is no stranger to sports — in fact he’s probably the most excited when he’s able to get ...

From Virginia to Boston for a kidney transplant: Joshy’s story
Joshy Buchheit is a lot like most 4-year-old boys. He loves playing in the mud, riding his scooter, and keeping ...
Idaho Falls news, Rexburg news, Pocatello news, East Idaho news, Idaho news, education news, crime news, good news, business news, entertainment news, Feel Good Friday and more.

LIVE UPDATES
Day 3 of jury selection underway in chad daybell case, “now we’re family.” neighbors describe life-saving organ transplant after 34-year-old’s tragic death almost 15 years ago.
Kaitlyn Hart, EastIdahoNews.com

IDAHO FALLS – ‘GTBA’ is a four-letter acronym that Robert Parkinson lives by since his neighbors saved his life in 2010.
“My license plate on my truck says ‘GTBA,'” says Parkinson. “Good To Be Alive.”
During a flag-raising event held Tuesday at Eastern Idaho Regional Medical Center to celebrate Organ Donation Awareness Month, Parkinson shared his experience receiving a liver donation from his neighbor, Jeremy Rose.
Rose was involved in a tragic construction accident in Hawaii in 2010 that caused him to become brain-dead at the age of 34.

Jeremy L Rose | 1975 – 2010 | Obituary
Emily Bowcutt, Rose’s sister and a medical and surgical director at EIRMC, described her family’s harrowing and selfless journey with organ donation after the loss.
“(Jeremy) was very quiet. He was very kind, he would do anything for anybody,” said Bowcutt.
When it came time do decide what to do with Jeremy’s organs, at first the family was hesitant.
According to the family, Jeremy’s wife Kristine Howell was initially opposed to the organ donation process for her husband, hoping that he would recover.
Shortly after, the family learned that their neighbor, Parkinson, was desperately in need of a liver and was not expected to survive the week.
After understanding that Rose was not going to recover, his liver was donated on the condition it went to Parkinson, saving his life.
The organs were quickly harvested in Hawaii and sent to Salt Lake City as Parkinson and his family began the journey toward the rest of his life.
“It’s very humbling to me to have been in that position where I was going to pass away,” said Parkinson. “We’d had discussions with our family and said dad is reaching the end, and what it was going to be like to not have a dad. To think that someone in their time of tragedy would think outside of themselves at a time like that is truly, truly humbling.”
Bowcutt says Jeremy would’ve “100%” wanted to help as much as he could in donating his organs to save not one, but three total lives. Parkinson received a liver, and two Hawaiian residents received Rose’s kidneys.
“I 100% know this is what he would’ve wanted,” says Bowcutt. “Not a doubt in my mind he would want this.”
Because of her experience working in the hospital, Bowcutt says she knew no matter what they did, she was going to lose her brother. Because of the organ donation, they found meaning in their loss.
“Whether we donated Jeremy’s organs or not, our outcome would have been the same. Jeremy was still dead,” said Bowcutt. “His kids still didn’t have their dad. We were still grieving. But through donation, Jeremy’s death gained meaning.”

The experience has caused the two families to grow closer, Parkinson describing his neighbors now as family.
“We were more acquaintances before, and now we’re family,” says Parkinson. “I just want to express appreciation for the gift of life. There’s a lot of people involved, a lot of medical people involved, there’s the donor family involved, and they’re the real heroes of these stories. I’m just grateful.”
Parkinson now has 24 grandchildren that he gets to watch grow up because of the love and sacrifice of Rose and his family.
“I asked a transplant coordinator once, I said, ‘How do you repay a gift like that? It seems impossible. I can’t do it,'” says Parkinson. “She said you basically pay it forward for the rest of your life. I’m not very good at it, but I’m making attempts to pay it forward for the beautiful gift these people have given me.”
According to the Health Resources & Services Administration, 17 people die nationally every day as they wait for an organ transplant.
In 2023, 27 EIRMC patients and their families donated their organs to someone in need.
The hospital is working with Donor Connect to dispel misconceptions about organ donation and make sure more patients can access live-saving organs.
“We’re a non-profit government regulated agency,” says Rob Stoback with Donor Connect. “We work with the local hospitals to have them identify perspective donors for us, and then we start to get into medical records to understand the overall potential of those organs.”
Kristi Caldera, director of Critical Care at EIRMC says it’s important to talk to your loved ones and tell them your wishes for if you were to experience an untimely death.
“It’s important to let your loved ones know your wishes related to organ donation as well,” says Caldera. “In the event that you become an organ donor, it will bring them peace to know that this is what you wanted.”
The easiest way to choose organ donation in Idaho is to indicate your preference on your driver’s license or state ID card or through yesidaho.org.
SUBMIT A CORRECTION
Watch CBS News
How a biased test kept thousands of Black patients from getting a new kidney
Updated on: April 1, 2024 / 10:48 AM EDT / AP
Jazmin Evans had been waiting for a new kidney for four years when her hospital revealed shocking news: She should have been put on the transplant list in 2015 instead of 2019 — and a racially biased organ test was to blame.
As upsetting as that notification was, it also was part of an unprecedented move to mitigate the racial inequity. Evans is among more than 14,000 Black kidney transplant candidates so far given credit for lost waiting time, moving them up the priority list for their transplant.
"I remember just reading that letter over and over again," said Evans, 29, of Philadelphia, who shared the notice in a TikTok video to educate other patients. "How could this happen?"
At issue is a once widely used test that overestimated how well Black people's kidneys were functioning, making them look healthier than they really were — all because of an automated formula that calculated results for Black and non-Black patients differently. That race-based equation could delay diagnosis of organ failure and evaluation for a transplant, exacerbating other disparities that already make Black patients more at risk of needing a new kidney but less likely to get one.
A few years ago, the National Kidney Foundation and American Society of Nephrology prodded laboratories to switch to race-free equations in calculating kidney function. Then the U.S. organ transplant network ordered hospitals to use only race-neutral test results in adding new patients to the kidney waiting list.

"The immediate question came up: What about the people on the list right now? You can't just leave them behind," said Dr. Martha Pavlakis of Boston's Beth Israel Deaconess Medical Center and former chair of the network's kidney committee.
Pavlakis calls what happened next an attempt at restorative justice: The transplant network gave hospitals a year to uncover which Black kidney candidates could have qualified for a new kidney sooner if not for the race-based test — and adjust their waiting time to make up for it. That lookback continues for each newly listed Black patient to see if they, too, should have been referred sooner.
Between January 2023 and mid-March, more than 14,300 Black kidney transplant candidates have had their wait times modified, by an average of two years, according to the United Network for Organ Sharing, which runs the transplant system. So far more than 2,800 of them, including Evans, have received a transplant.
But it's just one example of a larger problem permeating health care. Numerous formulas or "algorithms" used in medical decisions — treatment guidelines, diagnostic tests, risk calculators — adjust the answers according to race or ethnicity in a way that puts people of color at disadvantage.
Given how embedded these equations are in medical software and electronic records, even doctors may not realize how widely they impact care decisions.
"Health equity scholars have been raising alarm bells about the way race has been misused in clinical algorithms for decades," said Dr. Michelle Morse, New York City's chief medical officer.
- Study finds racial disparities in online patient portal responses
- Black cardiologists are rare, but vital for Black patients
Change is beginning, slowly. No longer are obstetricians supposed to include race in determining the risk of a pregnant woman attempting vaginal birth after a prior C-section. The American Heart Association just removed race from a commonly used calculator of people's heart disease risk. The American Thoracic Society has urged replacing race-based lung function evaluation.
The kidney saga is unique because of the effort to remedy a past wrong.
"Lots of time when we see health inequities, we just assume there's nothing we can do about it," Morse said. "We can make changes to restore faith in the health system and to actually address the unfair and avoidable outcomes that Black people and other people of color face."
Black Americans are over three times more likely than white people to experience kidney failure. Of the roughly 89,000 people currently on the waiting list for a new kidney, about 30% are Black.
Race isn't a biological factor like age, sex or weight — it's a social construct. So how did it make its way into calculations of kidney function?
The eGFR, or estimated glomerular filtration rate, evaluates kidney health based on how quickly a waste compound called creatinine gets filtered from blood. Because of a long-ago false theory about differences in creatinine levels, many lab reports until recently often would list two results - one calculated for non-Black patients and another for Black patients that could overestimate kidney function by as much as 16%.
- First Black patient to receive face transplant advocates for more donors, raise awareness
Not every Black kidney candidate was affected. Some may have had kidney failure diagnosed without that test. For others to have a chance at benefitting from UNOS' mandated lookback, transplant center staff-turned-detectives often worked after hours and weekends, hunting years-old records for a test that, recalculated without the race adjustment, might make the difference.
"You're reaching out to the nephrologist, their primary care doctors, the dialysis units to get those records," said Dr. Pooja Singh of Jefferson Health's transplant institute in Philadelphia, where Evans received her new kidney. "That first patient getting transplanted for us was such a great moment for our program that the work didn't feel like work after that."
A high school sports physical first spotted Evans' kidney disease at age 17. While finishing her master's degree and beginning to earn her Ph.D. at Temple University, she started dialysis — for nine hours a night while she slept — and was placed on the transplant list.
How long it takes to get a kidney transplant depends on patients' blood type, medical urgency and a mix of other factors — including how long they've spent on the waiting list. Evans was first listed in April 2019. When the Jefferson transplant center unearthed her old lab tests, they found she should have qualified in September 2015.
"Just for context, when I was still an undergrad I should have been on the list," she said, recalling the anger she felt as she read the letter. What she called "a mind-blowing" credit of 3½ more years waiting also provided "a glimmer of hope" that she'd be offered a matching kidney soon.
Evans got a new kidney on July 4 and is healthy again, and grateful the policy change came in time for her.
"You don't know if people would be alive today" if it had been enacted earlier, she said. Still, that extra step of "making amends to fix the situation for those that we can — I feel like it's very important and it's very necessary if you're truly wanting to bring more equity and equality into the medical field."
- Organ Transplant
- kidney donation
More from CBS News

New parking rates at Stanley Marketplace are free for first 3 hours

Increase in mail theft and fraud tied to missing USPS carrier keys

New program coming to Aurora to help with nursing shortage

Colorado launches nation's first e-bike tax credit, could strain bike shops
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Anaesthesiol Clin Pharmacol
- v.32(3); Jul-Sep 2016
The journey of liver transplantation: Milestones covered and the road ahead
Tvsp murthy.
Department of Anaesthesiology and Critical Care, Command Hospital, AFMC, Pune, Maharashtra, India
Liver transplantation has now become an established approach for managing end-stage liver diseases, and the journey in the complex procedure of liver transplantation has come a long way, witnessing many ups and downs. Better understanding of the physiological and pathological changes in the context of end-stage liver disease has made anesthesia, an important denominator for the successful outcome of this complex surgical procedure.
As the prevalence of the liver disease is rising, especially with hepatitis C infection, alcoholic/nonalcoholic-related liver disease, and hepatocellular carcinoma in an aging population, there is a significant impact on the perioperative and intensive care services. Perioperative mortality during liver transplantation is of concern, and it increases in proportion to disease severity but is affected by functional status, nutritional impairment, other comorbidities, and requirement for organ support. Model for End-stage Liver Disease (MELD) score is now commonly used to allocate and prioritize patients for transplant and has gained more importance than the conventional Child-Pugh scoring.[ 1 ] MELD score uses patient's serum bilirubin, prothrombin time, and creatinine to predict survival based on a calculation. Serum sodium concentration has been incorporated in the UK model of MELD to make it more meaningful.[ 2 , 3 ]
Long standing liver disease results in high flow state and shunting between pulmonary, peripheral, and splanchnic beds, resulting in increase of cardiac output. This causes imbalance in splanchnic and peripheral compartments, causing several significant effects which need to be addressed.[ 4 ] Among the various issues of concern for the anesthesiologist, the most significant are portal hypertension, contracted central blood volume, and cardiac changes which are specific to liver disease.
Portal hypertension a result of increased splanchnic flow rather than of intrahepatic resistance contributes to ascites, bacterial translocation, and aggravated bleeding during surgical dissection. The contracted central blood volume stimulates a powerful neuroendocrine response mimicking volume depletion, causing prerenal failure, or hepatorenal syndrome making these patients more susceptible to perioperative renal injury.[ 5 ]
The issue of fluid balance in patients of advanced liver disease undergoing liver transplantation or any other surgery is a tight rope walk and caution is to be exercised while administering fluids as it can increase portal hypertension. This especially makes bleeding, more worse, in procedures involving division of portosystemic collaterals.[ 6 ]
The anesthesiologist should be aware of the cardiac changes due to high flow state in this condition, resulting in cirrhotic cardiomyopathy. This causes impaired responsiveness to preload, afterload, QT prolongation, and increased chamber dimensions.[ 7 ] The diastolic dysfunction associated with raised cardiac output can precipitate secondary pulmonary hypertension or portopulmonary hypertension.[ 8 ]
Evidence suggests that these liver-related changes have important therapeutic implications in use of vasopressors, especially in the setting of hepatorenal syndrome. Vasopressin usage during the peritoneal dissection phase of liver transplantation has shown to reduce portal flow and pressure,[ 9 ] and phenylephrine helps to maintain the reduction in portal pressure while increasing central venous and mean arterial pressures. These measures aid in renal function maintenance and minimize surgical bleeding. This helps in maintaining renal function and reduces operative bleeding due to volume shift from splanchnic to central venous compartment.[ 10 ] Vasopressor therapy in low dose, especially in an underlying liver disease undergoing general anesthesia, maintains adequate cardiac output, with relatively less input of volume. It also ensures adequacy of renal and splanchnic blood flow. This prevents disruption of vascular intimal glycocalyx, which is the causative factor for fluid translocation and edema at capillary level.[ 11 ] This issue is to be borne in mind while dealing with any patient of liver disease subjected for surgery.
Pulmonary hypertension associated with advanced liver disease has to be evaluated with transthoracic echocardiography as it is a treatable entity. The possible predisposition to renal function compromise and sepsis should be borne in mind and fluid administration adjusted. Hypotension with general anesthesia requires management with a low vasopressor and be guarded fluid administration dose.
Advances in the understanding of the coagulation system in liver disease in the form of reduced Vitamin K-dependent factors, protein C, and antithrombin III have also had a significant clinical impact. Routine tests of prothrombin time and activated partial thromboplastin time are often misleading in predicting bleeding in liver transplantation.[ 12 ] Similarly, although platelet numbers and in vitro function may be reduced, more than adequate levels of factor VIII and Willebrand factor, typically seen in cirrhosis, may compensate.[ 13 ] The flbrinolytic system is also affected causing fibrinolysis on a lower grade. This can be aggravated especially during transplantation and can be managed with prophylactic tranexamic administration.[ 14 ] The routine clinical practice of administering fresh frozen plasma is questionable and now stands disputed. The management is best based on clinical findings such as leaky surgical field or failure of blood to clot. Clinical coagulopathy if present due to low fibrinogen can be effectively managed with prompt replacement.[ 13 , 14 ] Thromboelastography (TEG) has been an important tool helping to identify multifactorial coagulation impairment and aids in institution of proper blood component before loss of valuable time. This aid has now been accepted as a point of care requirement in transplantation procedures.[ 15 ]
Another challenging situation is the issue of significant hyponatremia, common in severe liver disease and liver transplantation. This has also given us insight into the risks associated with rapid correction of hyponatremia. Myelinolysis is a major concern and a hazard if serum sodium concentration rises abruptly, especially when citrated blood products are administered in large quantity. A safe and manageable threshold value for elective surgery is probably 125 mmol/l.[ 16 ] A postoperative fall in serum sodium concentration is associated with a significant increase in hospital morbidity and mortality. Vigilance is essential in monitoring of serum sodium and potassium concentration in the postoperative period, especially for hyperkalemia when large quantity of bank blood is used.
Routine use of preoperative echocardiography and TEG is beneficial especially for major elective liver surgeries. Early use of alpha-agonists for anesthesia-induced hypotension, avoiding overzealous administration of fluids, will preserve coagulation and renal function and minimize portal hypertension. Tranexamic acid is safe when bleeding is anticipated or uncontrolled. The use of factor concentrates is to be considered whenever significant coagulopathy so dictates. Postoperatively, it is mandatory that all patients with high MELD scores be managed in intensive care with special attention to mental alertness, sodium balance, and urine output.
The issue of meeting the imbalance between demand and supply in the field of liver transplantation still needs to be addressed. The gulf between both is only increasing in spite of institution of best practices and policies in tackling this rather complicated issue. There has been a significant improvement in the techniques making the availability of donor liver more in the form of utilizing marginal liver, reduced size liver transplantation, liver reduction, split liver transplantation, living-related transplantation – especially in the Asian continent and usage of nonheart-beating donors, auxiliary liver transplantation – for fulminant failures and metabolic disease. The idea of xenotransplantation though found to be very optimistic initially is unlikely to be a good substitute for human liver in clinical transplantation at least without major genetic engineering.
The road ahead: Liver transplantation has become a victim of its own success, with the inexorable rise in patients waiting for surgery and a donor pool who remain static. The future must involve improved utilization of potential organ donors and their optimization. Living donor transplantation has become today a viable option to redress the shortage of donors. Improvements in immunosuppression have had a major effect on the survival of liver transplant patients, a phenomenon that is promising. The journey of liver transplantation initially had been rough and bumpy, but with the experience gained, better understanding of the physiopathological changes, improved surgical techniques, better postoperative care, and better immunosuppression, the road ahead now seems to be smooth and clear.

IMAGES
VIDEO
COMMENTS
Patient Journey. We understand the road to transplant can seem overwhelming for patients. So we've created a series of videos to help explain the transplant journey from evaluation to waitlisting, and from pre- to post-transplant. Our dedicated team is here for you every step of the way. Hear from our experts on what to expect.
The Transplant Journey. Our goal is to ensure referring health care professionals are aware of the help we can provide immediately after a specialist's initial diagnosis - to help the patient navigate through this process earlier, leverage our resources sooner and make the process for the patient and their family much smoother. The diagram ...
It was common to care for over 1,000 patients simultaneously, as when you receive an organ transplant the coordinator becomes like a member of your family, often for life. From the point of transplant, I constantly worked to ensure the patient could get labs drawn, reviewing those labs for trends or abnormalities and ensuring they were able to ...
Meet NFT newest transplant patients. We look forward to serving them, their transplant center, medical professionals, family and friends. Say hello! ... There are three key areas that highlight the many ways we help patients and their families navigate the organ transplant journey. Fundraising Guidance.
Patients, family members, and friends needing additional information about living donation and organ transplant, contact the OPTN Patient Services Line at 1-888-894-6361 or [email protected].
A patient's kidney transplant journey. Lupus patient shares organ donation experience with mother. Alison Lee was diagnosed with lupus at 16 years old. Alison Lee is a fighter. She has fought lupus, kidney failure, and cancer—all in just 35 short years.
The journey begins when your doctor identifies the need for a transplant. Depending on the nature of your case—the type of transplant needed and the urgency of your medical condition—your doctor may advise you to make lifestyle changes to increase the likelihood of a successful transplant or of your eligibility for placement on the organ transplant waiting list.
Patient journey — A step-by step description of the stem cell transplant process. Your providers at the UC Davis Comprehensive Cancer Center understand that undergoing a stem cell or cord blood transplant is a significant and complex process that can affect every aspect of your life and your loved ones. It's also a procedure that offers ...
The pre-transplant process for children undergoing organ transplantation involves several important steps. ... and their family are critical for ensuring the child's physical and emotional well-being as they prepare for the transplantation journey. ... During a hospital stay after a pediatric transplant, patients and families may benefit from ...
Transplant recipients must follow a strict diet after their surgery to prevent getting a foodborne illness. Due to their immunosuppressive medications that keep their bodies from rejecting a new organ, transplant recipients are more susceptible to developing infections, and a foodborne illness can make a patient seriously ill.
People often think that the process of organ or stem cell transplantation ends once the patient receives the transplant. But this, in fact, is only half of the patient journey. Olivier Charmeil is ...
Abstract. In this article, a hospital chaplain presents a detailed narrative of the psychological, emotional, and spiritual dynamics of an organ transplant patient. The chaplain explicates the many complex factors that may characterize an organ transplant patient's recovery and the many persons—family members and hospital personnel—who can ...
The spiritual journey of an organ transplant patient. 2003 Summer;57 (2):191-6. doi: 10.1177/154230500305700209. Our Lady of the Resurrection Medical Center, 5645 W. Addison Street, Chicago, IL 60634, USA. In this article, a hospital chaplain presents a detailed narrative of the psychological, emotional, and spiritual dynamics of an organ ...
Describe the transplant experiences of organ recipients, including the challenges and concerns they face throughout the journey. Identify the unique aspects of patient care that the medical community should be educated about to improve the overall care and support provided to transplant patients.
A Patient's Journey Becoming a live kidney donor. Annabel Ferriman, ... Most transplant units have established clinical pathways for live related organ donation, which focus on ensuring that the donor completely understands the risks and benefits for informed consent, and confirming the donor's suitability as well as the recipient's health. ...
Introduction. Solid-organ transplantation is a cost-effective medical treatment for patients with end-stage organ failure (World Health Organization, 2019).Around 135,000 transplantations are carried out annually worldwide, offering life-saving or significant health-enhancing treatment for patients with kidney, liver, heart, lungs, pancreas, or small bowel diseases (Global Observatory on ...
They now see organ transplantation very differently. My friends from the swimming club now give blood. ... (including patients and caregivers). While defining the patient journey, three main dynamics were taken into consideration. Firstly, referral from multiple centers implies an administrative burden. Secondly, there is a high number of ...
To undergo a heart transplant is to undertake a journey to a new life. Since 1984, the Temple Heart & Vascular Institute has guided more than 1,300 survivors through the heart transplant process, including patients considered to be too high risk at other transplant centers.. One of the most important factors for the success of a heart transplant is the preparation of our patients — medically ...
Your doctor must refer you. A transplant center or program then checks if a transplant makes sense for you. Gather Information. Learn about transplant lists, costs, and recovery. The United Network for Organ Sharing (UNOS) created, What Every Parent Needs to Know (PDF - 5 MB). It gives you an overview of the process. Select a Transplant Center
Published March 21, 2024 Updated March 25, 2024. Surgeons in Boston have transplanted a kidney from a genetically engineered pig into an ailing 62-year-old man, the first procedure of its kind. If ...
The organ owed its vitality to this machine, which was preserving it for transplantation into a needy patient. "It's a little bit science fiction," said Dr. Daniel Borja-Cacho, a transplant ...
Pre-transplant mortality: A program's pre-transplant mortality rate relative to the mortality rate experienced by similar patients across the nation. If implemented in July 2024, the MPSC will consider program performance on mortality for candidates appearing on the waiting list at any time during the period of January 2022 through December 2023.
Richard Slayman, 62, is the first patient to receive a kidney from a genetically modified pig. Two weeks after the procedure, he was well enough to be discharged, doctors said. A pig kidney before ...
The American Liver Foundation (ALF) is rolling out new patient resources, programs and support to mark Donate Life Month, an annual event focused on the importance of organ, eye and tissue ...
Organ Transplant Patient. The clinical course and management of a rare case of gastrointestinal mucormycosis occurring in a renal transplant patient are presented. The diagnosis was made on pathological examination of surgically resected tissue from the colon, spleen and stomach. The patient did not survive the infection.
In the landscape of organ transplantation, statistics from UNOS reveal that over 100,000 Americans are in need of an organ, with daily fatalities averaging 17 as they wait for a transplant ...
An act of kindness — Raul and Larry's journey to a non-directed transplant donation. Thanks to Larry's non-directed donation of a piece of his liver, Raul is able to be a kid again. Acts of kindness can come in many forms, like volunteering or donating to a charity of choice. At 52, Larry loves giving back to his local community in Vermont ...
According to the Health Resources & Services Administration, 17 people die nationally every day as they wait for an organ transplant. In 2023, 27 EIRMC patients and their families donated their ...
Between January 2023 and mid-March, more than 14,300 Black kidney transplant candidates have had their wait times modified, by an average of two years, according to the United Network for Organ ...
The future must involve improved utilization of potential organ donors and their optimization. Living donor transplantation has become today a viable option to redress the shortage of donors. Improvements in immunosuppression have had a major effect on the survival of liver transplant patients, a phenomenon that is promising.