Disclaimer » Advertising
- HealthyChildren.org
- Facebook Icon
- Twitter Icon
- LinkedIn Icon

State, federal laws govern whether doctor visits can be recorded :
At a clinic visit for a child with developmental concerns, the patient’s father takes out his smartphone and begins videotaping your discussion of next steps for behavioral management of his child. He states that this will help him remember how to care for his child. You have had prior conflicts with this family and are uncomfortable with the conversation being recorded. What can you do?
Audio and video recordings of doctors’ visits can be used to improve patients’ and families’ understanding of medical conditions and care instructions. In some situations, however, providers may be concerned that recordings could be harmful or illegal or may cause liability down the line.
What legal protections apply to recordings of doctors’ visits, and what rights do doctors have to limit recordings when they are uncomfortable?
The federal wiretapping law (18 U.S. Code § 2511) requires that only one party consent to recording a conversation. States also have laws governing recording. In most cases, state laws that are more restrictive than federal law would supersede the federal statute ( Privacy: An Overview of Federal Statutes Governing Wiretapping and Electronic Eavesdropping. Report for Congress . January 2003, https://www.epic.org/privacy/wiretap/98-326.pdf ).
In states requiring only one party’s consent, a patient may claim to have a right to record the conversation regardless of whether the provider agrees. Twelve states (California, Connecticut, Florida, Illinois, Maryland, Massachusetts, Michigan, Montana, New Hampshire, Oregon, Pennsylvania and Washington) require all parties to a conversation to consent to recording. In these states, recording an encounter with a physician would not be allowed without the physician’s consent (Elwyn G, et al. JAMA. 2017;318:513-514).
Even if only one party’s consent is needed to record a conversation under state law, other policies and protections may limit recording of physician visits. Some health care practices have policies restricting patients’ and families’ abilities to use photography or recording devices in the facilities; others may call for approval to record clinical care or require that recordings are discontinued if the physician, nurse or another staff member deems this necessary. State laws and a practice’s location may govern the types of restrictions and policies that can be implemented. A practice on private property may have more options to limit recording of physician encounters.
If a patient or family member records an interaction with a provider, Health Insurance Portability and Accountability Act (HIPAA) privacy restrictions would not apply since the recording party is not a covered entity under HIPAA. Recording other patients, however, would be prohibited.
Practices can take steps to prevent prohibited recordings, such as posting signs restricting recording in the waiting room or other common areas or including such guidelines in privacy policies.
If someone makes an unauthorized recording in a state that requires all parties to consent, he or she may face legal consequences, including possible felony charges. There may be additional legal consequences for disseminating the recording.
While patients would not be prevented from disseminating a recording made in states in which only one party’s consent is required, other legal ramifications may apply, particularly if a physician’s reputation is damaged.
Risk management pointers
- Be familiar with laws regarding audio and video recording in your state of practice.
- Develop practice policies on recording or consult your institution about existing policies.
- Confer with a local malpractice carrier regarding recording policies and responsibilities under HIPAA in your state of practice.
- Consult an attorney or compliance officer if you are concerned about HIPAA violations or reputation damage resulting from recordings.
- Avoid responding to dissemination of information on social media or in public forums.
Dr. Sigman is a member of the AAP Committee on Medical Liability and Risk Management.
- AAP News article “Should pediatricians allow parents to videotape office visits?”
- Additional Pediatricians and the Law columns
Advertising Disclaimer »
Email alerts
1. New resources available as measles cases continue to rise
2. FDA approves new antibiotic for children, adults with community-acquired bacterial pneumonia
3. Pediatrics fill rate dips during 2024 Match
April issue digital edition

Subscribe to AAP News
Column collections
Topic collections
Affiliations
Advertising.
- Submit a story
- American Academy of Pediatrics
- Online ISSN 1556-3332
- Print ISSN 1073-0397
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- COVID-19 Vaccines
- Occupational Therapy
- Healthy Aging
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Secretly Recording Your Doctor’s Appointments
Secret recording is increasingly common and many times legal
According to the Pew Research Center, in 2016, a whopping 77% of Americans owned a smartphone. This number is more than double what it was when the Pew Research Center first started tracking smartphone ownership in 2011. Back then, 35% of Americans owned smartphones. Furthermore, in 2016, there was a sharp rise in ownership among both older people and lower-income people. Smartphones are everywhere, and their coverage is growing.
In addition to making phone calls, smartphones can do lots of other things. They can take photos, shoot video, play music, and access the Internet. They can also be used to record healthcare provider appointments without the knowledge of the practitioner.
Secretly recording clinical encounters may sound sneaky, but in 39 of 50 states, it’s legal. Furthermore, research shows that recorded clinical encounters can be empowering and educational for patients. However, many healthcare provider are understandably skittish about having a recording of their advice floating around somewhere out there.
How Common Is It?
There isn't a lot of data concerning how prevalent secret recording is; the issue has only recently risen to some prominence.
In one small UK study, Elwyn and co-authors found that 15% of respondents indicated that they had recorded a clinician encounter without consent, and 35% of participants said that they had considered doing it. Moreover, in the same survey, 11% of clinicians responded that they were aware of being secretly recorded by a patient in the past. According to the authors of the study, “69% of respondents indicated their desire to record clinical encounters, split equally between wanting to do so covertly or with permission.”
How Legal Is It?
Each state has its own wiretapping and eavesdropping statutes. The statutes vary from state to state based on whether one or two parties must consent to recording a conversation, thus referred to as single-party jurisdictions or all-party jurisdictions, respectively. In total, 39 of 50 states as well as the District of Columbia are single-party jurisdictions—where only one party needs to consent. In other words, in these jurisdictions, if somebody wants to record another person—including a clinical encounter—it’s legal.
There are 11 all-party-jurisdiction states in which both the clinician and patient must both consent to recording a conversation: California, Florida, Illinois, Maryland, Massachusetts, Michigan, Montana, New Hampshire, Oregon, Pennsylvania, and Washington. In these states, it’s a felony for a patient to record a healthcare provider without permission.
In single-party jurisdictions—or most of the United States—if a patient asks to record a clinical encounter and the clinician refuses, the patient can proceed to record the encounter anyway. The clinician must then choose to continue or terminate the encounter.
In all-party jurisdictions, the clinician must be asked by the patient to record the clinical encounter. Any illegal recording can then be reported by the clinician to the authorities. Possible repercussions include compensation for harm, attorney’s fees, and other costs, with disseminating the recording via the Internet being considered an additional violation.
What About HIPAA?
As with any formal medical record, the HIPAA Privacy Rule covers any audio or video recordings made by the healthcare provider, health plan, or health clearinghouse. However, HIPAA doesn’t extend to recordings made by the patient. In other words, in single-party jurisdictions, the patient can distribute the recording as pleased.
The Benefit of Recording
Research shows that patients put a high value on audio recordings made of clinical encounters. For instance, in a 2014 review, Tsulukidze and colleagues found that, on average, 72% of patients listened to recorded consultations. Furthermore, 60% of patients shared these audio recordings with loved ones and others. For the most part, these recordings have been shown to improve patient recall and understanding of their conditions.
Other research findings suggest that patients and their family members often have difficulty comprehending what’s presented during a healthcare provider's appointment because they are overcome with grief and complex emotions. Recordings can be played back later when the patient and family members are better prepared to understand the message, guidance, and advice. Oncologists have known about this phenomenon for some time, which is why recordings of encounters are commonly offered to patients who are being treated for cancer .
In the previously mentioned UK survey, Elwyn and co-authors found that the prime motivation to record clinician encounters is to enhance the healthcare experience and to share the experience with others. However, some patients reported wanting to use the recordings as evidence of poor care.
How Do Healthcare Providers Feel?
Especially at work, few people like to be recorded without their permission; healthcare providers are no different.
In a Viewpoint from JAMA , Rodriguez and Morrow write the following:
"Not all possible uses of these recorded conversations are beneficial to patients and healthcare provider. Patient or family members who disagree with the advice of their practitioners or who are upset with their healthcare provider for whatever reason can easily take comments from these recordings out of context and, with a few keystrokes, disseminate them via social media. Patients can conceivably record conversations with the specific intent of establishing the grounds for a lawsuit or gathering material with which to manipulate a physician."
Moreover, if a healthcare provider suspects or later finds out that an encounter has been recorded without consent, the healthcare provider-patient relationship can suffer. First, these practitioners may believe that they were denied the right to consent to recording. Second, healthcare providers may feel vulnerable to scrutiny and distrustful of the patient.
A Word From Verywell
Ultimately, healthcare providers, policy makers, and patient advocacy organizations must come together to work out guidelines and regulatory guidance regarding patient recording.
In the meantime, however, it may be a good idea for healthcare providers in single-party jurisdictions to embrace the possibility that they’re being secretly taped during every clinical encounter. The healthcare provider could then proceed without letting any concerns about being recorded affect patient care, medical decision-making , or attitudes toward the patient.
Alternatively, a healthcare provider could ask whether the encounter is being recorded, express assent, and educate the patient about the utility and best use of these recordings.
Finally, even if there’s no legal obligation, it may behoove a patient to inform the clinician that they plan to record the encounter. Doing so may obviate any hard feelings, trepidation, or indignation on the part of the healthcare provider.
Smith A. Record shares of Americans now own smartphones, have home broadband . Pew Research Center.
Elwyn G, Barr PJ, Grande SW. Patients recording clinical encounters: a path to empowerment? Assessment by mixed methods . BMJ Open . 2015;5:e008566.
Tsulukidze M, et al. Providing recording of clinical consultation to patients – A highly valued but underutilized intervention: A scoping review . Patient Educ Couns . 2014;95:297–304. doi:10.1016/j.pec.2014.02.007
Rodriguez M, Morrow J. Ethical implications of patients and families secretly recording conversations with physicians . JAMA . 2015;313(16):1615-1616. doi:10.1001/jama.2015.2424
Elwyn G, Barr PJ, Castaldo M. Can patients make recordings of medical encounters? JAMA . 2017;318(6):513-514. doi:10.1001/jama.2017.7511
By Naveed Saleh, MD, MS Naveed Saleh, MD, MS, is a medical writer and editor covering new treatments and trending health news.
Can Doctors Record Patients Without Consent?

The question of whether "can doctors record patients without consent?" is one that dives into many legal and ethical concerns. This issue becomes more intricate when considering the reverse scenario of patients and healthcare workers being secretly recorded by patients. To fully understand the situation, let us examine perspectives from various sources and cover the legal, ethical, and practical implications of these actions.
Doctors Recording Patients
Recording patients without consent is regarded by many as a breach of trust and an infringement on privacy. The law varies depending on the jurisdiction and nature of the recording. That being said, it's legal in 39 out of 50 states.
In certain states, only one party's consent is enough to legally record a conversation, meaning a patient or a doctor can record the conversation regardless of whether the other party agrees. There are 11 states - California, Florida, Illinois, Maryland, Massachusetts, Michigan, Montana, New Hampshire, Oregon, Pennsylvania, and Washington - in which both the clinician and patient must consent to record a conversation.
It’s important to note that state laws, ethical guidelines, and federal laws, such as the Health Insurance Portability and Accountability Act (HIPAA), often require medical professionals to maintain the confidentiality of patients' medical records unless granted permission by the patient.
In summary, although doctors may have legal permission to record conversations without patient consent in certain states, they must exercise extra caution in adhering to ethical guidelines and federal laws like HIPAA. These guidelines and laws prioritize protecting patient privacy and confidentiality. It is always recommended for healthcare professionals to attain consent before recording conversations to mitigate any risk of violating legal and ethical standards.
Patients Recording Doctors and Nurses
Can patients record doctors, nurses, and other healthcare professionals without their consent? This question explores the rights and limitations of patients. In many jurisdictions, patients can record their interactions with healthcare professionals for personal use or to understand their treatment better. However, such actions may be subject to state or country laws.
Patient-recorded videos might expose inadequate care or a lack of professionalism, potentially leading to legal action or public shaming. On the other hand, such recordings can also hold healthcare professionals accountable and ensure high-quality care.
While audio and video recordings can enhance patients' and families' understanding of medical conditions and treatments, doctors can have reservations about recordings due to potential harm, legalities, or future liabilities. Federal wiretapping law requires only one party to consent to the recording, but some states demand all parties' agreement (those states are listed above).
In healthcare settings, other policies may further restrict recordings, and such policies vary based on practice locations and state laws. Unauthorized recordings can lead to legal consequences, so patients should familiarize themselves with state laws before recording or distributing that recording.
Hospital Policy on Video Recording and Legal Considerations
Questions like "Can you record in a hospital?" or "Can patients video record nurses without consent?" touch upon hospital policy and legal considerations. Policies and guidelines implemented by hospitals regarding recording in medical settings are vital to maintaining a respectful and secure environment for both patients and providers. These policies often balance patient rights with the need for privacy and confidentiality.
Both patients and healthcare professionals should understand and respect these policies. Failing to adhere to these guidelines can lead to legal challenges, negative publicity, or a breakdown in trust.
Can a Doctor Refuse to Be Recorded?
Yes. Although laws governing this matter range from locale to locale, most healthcare professionals can assert their right not to be recorded during medical procedures or appointments. However, if the recording is necessary for transparency or accountability purposes, both parties must engage in an open discussion leading to an agreement rooted in mutual consent.
Emergency Room Videos
The prevalence of smartphones and cameras has increased the frequency of emergency room videos recorded by both patients and healthcare providers. These recordings, while capturing precise details of the event, can also unintentionally expose patients' personal information.
Audiovisual recordings in the ED can be used to document clinical information, assist with diagnosis and treatment, or monitor the quality of medical procedures and security measures. However, with the ubiquity of smartphones, concerns arise about unauthorized recordings made by patients and visitors.
Covert recordings can undermine patient-doctor trust and violate the privacy rights of caregivers, staff, or patients. Laws and hospital policies regarding recording permissions vary greatly. As of 2019, at least 11 states have laws that make audiovisual recording without prior two-party consent illegal, usually as part of their wiretapping laws. The American College of Emergency Physicians (ACEP) considers unauthorized recording in areas of patient care to be unethical and recommends regulating and restricting such recordings where privacy and confidentiality are expected.
Clear protocols regarding using cameras and video recording in emergency rooms must be established. This not only preserves patient confidentiality but also prevents potentially harmful situations resulting from unauthorized recordings.
To conclude, determining if doctors can record patients without consent or if patients can secretly record healthcare providers is a complex issue, requiring consideration of legal, ethical, and practical elements. Ensuring clear policies are in place and that both doctors and patients fully understand their rights is crucial to avoiding untoward consequences.
Fostering an environment of trust, communication, and transparency when it comes to recording sessions benefits all involved in the healthcare process, from doctors and nurses to patients and their families.
In the ever-evolving field of health care, assuring the well-being and trust of patients is paramount. To excel in safeguarding health information requires a thorough understanding of HIPAA's latest standards and regulations.
That's why we designed the HIPAA Training for Healthcare Workers and Office Staff . These comprehensive 90-minute courses will boost your knowledge of HIPAA Privacy, HIPAA Security, Enforcement of HIPAA violations, and even the latest 2022 updates!
Upon successful completion, you will be rewarded with a Certificate of Completion that can enhance your credentials and, most importantly, help you guarantee the privacy and security of your patients' information.
Whether you're a seasoned professional or just starting your journey, our 100% online HIPAA training will adapt to your pace. Empower yourself with the necessary skills to navigate HIPAA rules and requirements and be a beacon of trust and assurance in your healthcare workspace.
Take the first step towards HIPAA mastery. Enroll in our HIPAA Training for Healthcare Workers or Office Staff course today.

- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
November 2, 2020
Want to record your doctor's appointment? Great idea, but first, check it's legal
by Amelia Hyatt, Carolyn Johnston, Megan Prictor, The Conversation

As you fire up your computer for a telehealth appointment, or prepare to walk in to see your doctor, you may be wondering whether to record your appointment. You might even think about doing it without asking permission first.
But recording without permission might be illegal depending on where you live, according to our latest research, published today .
And there may be repercussions for you and your health-care professional.
Why record a consultation?
When feeling unwell, or overwhelmed with a new diagnosis, it can be hard to take in and remember important health information your health-care practitioner provides.
Recording your appointments can help. It can help you recall and understand what you discussed. You can also share information about your diagnosis or ongoing care with family and friends.
Many health professionals support the idea of their patients recording their appointments.
Can technology help?
In the past few years there has been increasing interest in using digital technology to help people record their health-care consultations.
In Australia, we developed the SecondEars smartphone app at Peter MacCallum Cancer Center to allow people diagnosed with cancer to record on their phone, with back-up copies sent directly to their health service for storage.
In the United States and Europe , health services and clinics are developing in-house recording software and technology.
Most smartphones also have basic recording software that lets you record with or without asking your health professional. And amid the boom in telehealth due to COVID-19, it's worth remembering videoconferencing software (such as Zoom) also has built-in recording functions.
What happens if I record?
Imagine you are going to record without telling your doctor, nurse or other health-care professional, or plan on sharing the recording later with other people. What does the law say?
We found this differs in each part of Australia, depending on where you are when you create or share the recording. The law doesn't differ by the type of recording; audio and video are treated the same.
In some jurisdictions ( Victoria , Queensland , NT , NSW , ACT and Tasmania ) patients don't need permission to record their appointment with a doctor, nurse or other health professional if the recording is just for their own use. So, if you want to record to remember what the doctor told you about upcoming surgery or how to take your medicines, you can, even without asking first.
In SA and WA , you usually need the health professional's consent before recording.
In these states, a person who makes a covert recording for their own use can even face a fine or prison term (for example, in SA , there are fines of up to A$15,000 or prison for up to three years).
Can I share the recording?
Sharing a recording with others—whether this is in person or online—is subject to other rules. The health professional's consent is sometimes needed for this even if it wasn't needed for the recording in the first place.
However, in Queensland , Tasmania , NSW , SA and the ACT , as long as the original recording was done within the rules, you don't need to ask for consent to share it just with family or close friends.
Sharing it more widely is another matter. Only in NSW and SA can you do this without the health professional's consent (as long as the original recording was lawful).
While the law is messy, we think the overall answer is clear. Even if you don't need your health professional's permission to record your consultation, it is best to tell them you want to.
What if I ask and the doctor says 'no'?
Some health-care professionals and organizations might be concerned you might share recordings on social media, or use them as a basis for a complaint.
The indemnity insurer MIPS tells its doctors that if the idea of recording makes them uncomfortable, they have the option to decline it. But we argue saying "no" to a patient's reasonable request to record the consultation might harm the doctor-patient relationship, by eroding patient trust and confidence.
If you want to record your medical appointment, it could be worth talking with your doctor about how the recording could help you take better care of your health, and telling them what you intend to do with it.
You could also point out that advice in the United Kingdom suggests recordings can actually support doctors where there are legal disputes.
In one US institution , doctors who let their consultations be recorded get a discount for their indemnity insurance, because of the reduced risk of being sued for malpractice. It makes sense, because when there's a recording, there is less chance of a disagreement arising over who said what.
Iron out any concerns early
Even if making or sharing a recording doesn't break the law, doing so without everyone's knowledge risks harming your relationship with your health-care professional, especially if they find out about it later.
Ultimately, a constructive dialog between you and your health -care professional should iron out concerns on both sides. While it might feel challenging—and depending on where you are, the law might not require you to—it is usually best to ask for consent, so there are no surprises.
Explore further
Feedback to editors

Two key brain systems are central to psychosis, study finds
8 hours ago

COVID-19 vaccine effectiveness: Results from Norway demonstrate the reproducibility of federated analytics
11 hours ago

Elucidating the link between Guillain–Barré syndrome and Takotsubo cardiomyopathy
12 hours ago

Artificial intelligence can help people feel heard, study finds
13 hours ago

A new diagnostic model offers hope for Alzheimer's

New study validates prediction rules for pediatric intra-abdominal and traumatic brain injuries
14 hours ago

Chemicals stored in home garages linked to amyotrophic lateral sclerosis risk

In the drive to deprescribe, heartburn drug study teaches key lessons

Researchers identify new genetic risk factors for persistent HPV infections

New AI method captures uncertainty in medical images
Related stories.

Missed something the doctor said? Recording your appointments gives you a chance to go back
Mar 25, 2019

Can patients record doctor's visits? What does the law say?
Jul 10, 2017

The digital doctor's visit: Enormous potential benefits with equally big risk
May 14, 2018

First-of-kind study reveals public and physician attitudes toward recording clinical visits
Sep 12, 2018

Uber to let users record audio of rides in Brazil, Mexico
Nov 20, 2019

Using a smartphone and audio software to pick a physical lock
Aug 24, 2020
Recommended for you

Study shows air pollution is associated with increased risk of developing Alzheimer's disease
15 hours ago

High rate of death soon after release from jail is avoidable: Researchers call for coordinated whole government response
18 hours ago

Analysis finds mixed diets balance nutrition and reduce carbon footprints
Apr 10, 2024

Research shows pregnancy accelerates biological aging in a healthy, young adult population
Apr 8, 2024

Research finds pretzel size affects intake by governing how quickly a person eats and how big their bites are
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter

What To Do When Patients Want To Record Their Doctor Visits
By richard cahill, jd | published 3/1/2017 9, “doctor, can i record our conversation today” have you ever heard that question from a patient or a patient’s family member what are the pros & cons of allowing those recordings in clinic or the operating room.
“ Doctor, can I record our conversation today? ”
Have you ever heard that question from a patient or a patient’s family member? Or have you ever been worried a patient might record the visit without asking permission? As smartphones have become ubiquitous, giving patients a video and audio recorder that’s always at hand, the question of whether or not these devices should be allowed in the clinic or hospital setting is becoming increasingly more common.
A high-profile case involved a patient who accidentally recorded his colonoscopy, capturing derogatory remarks from the anesthesiologist while he was under anesthesia. The patient sued for malpractice and was awarded $500,000. While this case is extreme, it has raised the importance of addressing the issue in each practice and hospital.
Patients: To record or not to record?
The issue of allowing patients to record their appointments requires balancing potential privacy and liability risks with the potential benefits of improved patient recollection of instructions and treatment adherence. Patient pamphlets and other educational materials handed out at office visits are often lost or forgotten, and patients forget or remember inaccurately a significant portion of information shared at doctor visits. Patients who have a better and more complete understanding of their condition and the treatment plan are more likely to be actively engaged and involved in their healthcare.
Despite these potential benefits, it’s typically not the best course to allow patients to record the appointment. The recording devices could be disruptive and could be potentially intimidating to physicians and staff. In addition, these recordings—unlike the electronic health record—can be altered or manipulated to create an inaccurate portrayal of what actually occurred. These recordings can also easily be streamed or posted online, raising the issue of patient and staff privacy and HIPAA compliance. In addition, recording the visit may inhibit the flow of information between the doctor and patient. Patients may be less likely to be open about sensitive health issues because of the fear that the recording might be listened to by an outside party.
If a patient records a visit without the doctor’s permission, that can result in a loss of trust, which is the basis of a strong physician-patient relationship. Only about a dozen states nationwide prohibit electronic recordings done without the explicit consent of all participants in the encounter. It is important to know the specific laws concerning recordings in the jurisdiction where you practice. Regardless, it is recommended that patients be advised unequivocally that digital recordings by handheld devices, such as smartphones, are prohibited on the premises in order to protect the privacy of other patients and staff in compliance with federal and state privacy laws.
Post this notice clearly on your practice website, in the conditions of treatment signed by the patient at the outset of the relationship, and as office signage near the reception window. Suspected violations should be handled immediately. If this policy is violated, meet with the patient in a confidential setting to discuss the issue and reiterate the office policy. Depending on the circumstances and the status of the patient’s current episode of care, advise the patient that further violations may result in termination of the physician-patient relationship.
If patients ask to record the visit, encourage them instead to take notes or to have a trusted family member or friend join them for the office visit to help take notes, remember information, and ask questions. Doctors can also encourage patients to be engaged in the conversation with “ Ask Me 3 ,” a program that promotes clear communication through these three main questions:
- What is my main problem?
- What do I need to do?
- Why is it important for me to do this?
Doctors should also ask patients to repeat back the information shared, and then correct any misunderstandings.
Important policies for recording surgical procedures
Practices and surgical centers also must decide whether they should video-record clinic visits or operative procedures. Office practices may want to record patient encounters to document when the informed consent occurred. Surgical centers may want to record surgeries for educational purposes.
It is important to note that this additional documentation will become a part of the record and can be subsequently accessed by government agencies responsible for healthcare oversight, such as state medical boards, the Centers for Medicare and Medicaid Services, and the Office of the Inspector General for the United States Department of Health & Human Services, among others. Law enforcement will also be able to secure a copy with a search warrant or other court order. A patient may also obtain the recording with a valid HIPAA-compliant authorization.
If a medical group or healthcare facility is considering doing audio or video recordings, it is recommended that several factors be considered and implemented:
- The practice or facility should create a written protocol detailing under what circumstances a digital recording—whether audio, video, or both—may be done.
- The policy should also indicate how the digital recording will be stored, where it will be retained and by whom, and for how long it will be kept.
- Any such protocol should reference the manner in which the digital document will be destroyed, consistent with federal and state privacy laws.
- Patients should be advised in advance that a digital recording is being considered. The patient should sign a written release that explains the reasons for the recording. As with all consent forms, the signed authorization should be placed in the chart as part of the permanent record.
- The practice or facility should put a procedure in place to ensure that the policies are being followed and that a responsible administrator conducts a periodic review to ensure the effectiveness of the protocols. Adopting and following these procedures helps to protect the practice or facility in the event of a subsequent inquiry as to the validity and completeness of the patient’s chart.
This post was sponsored by The Doctors Company , the nation’s largest physician-owned medical malpractice insurer.
- medicolegal
- patient safety
Richard Cahill, JD
Website: http://www.thedoctors.com.
Richard Cahill is Vice President and Associate General Counsel for The Doctors Company. Mr. Cahill provides legal support to the Claims and Patient Safety Departments. He has specialized in various facets of healthcare litigation for more than 25 years, including the defense of hospital and physician professional liability claims, managed care contract disputes, and related business torts. His principal clients have included Cigna, Kaiser Permanente, and Tenet Health Systems. Mr. Cahill has completed in excess of 175 trials and binding arbitrations during his career and has been appointed as an arbitrator in more than 350 cases involving healthcare issues.
Mr. Cahill received his undergraduate degree summa cum laude from UCLA in 1975 and his juris doctor from Notre Dame Law School in 1978. He lectures frequently around the country on topics related to the healthcare industry. He has an AV Preeminent Rating from Martindale-Hubbell.

I love this post but just a tip… you should really write longer articles. I hear it helps a lot with getting new visitors. And I think your writing style would keep people really interested in what you had to say about all of this
Clearly written by an attorney whose clients are doctors and not a reflection of patient centered care. What do you have to hide? Doctors now often have scribes in the room so it is only fair for the patient to be able to record the visit as well.
Is it possible, just possible, maybe even a little *tiny* bit, that preventing recordings also prevents evidence that could be useful in a malpractice claim?
Useful to whom?
I wish my patients would record our sessions. How often do they even remember the simple things I tell them, much less the more complex ideas I may share. If they could record my advice and listen to it over and over, maybe they would understand and actually follow some of my suggestions. This article is what you get when you ask a lawyer to comment on medical practice. Bad advice.
This position is anachronistic and headed in the wrong direction on many levels. Healthcare Advocacy Coaching considers recording doctor visits as a basic tenet of advocating for one’s self. During most visits doctors are invariably rushed, do not focus on patient needs /questions/ concerns but moreso on what the doctor wants to discuss. The majority of doctors speak in couched language, using sophisticated language and medical terminology that eludes all but the most medically sophisticated patients. Patients need to record the session so that they can review it repeatedly at home, slowly dissecting each chunk / topic that was discussed. Anxiety levels surrounding doctor visits are very high for most people and their anxiety (assiduously documented and reported) clouds their ability to ask questions, make comments, and advocate for their own needs. They are vulnerable, fearful, unsure and sometimes a bit confused about what the doctor is saying. Recording the session is currently the only option they have to eventually understand what happened during the interaction. All Healthcare Advocacy coaches are advising patients to: 1. Record their sessions 2. Change doctors if the doctor won’t allow them to record. Good luck with your plan.
Thank you for sharing your thoughts—I think we all agree that patient engagement and understanding is very important, as is trust between doctor and patient. We offer many resources on our site (thedoctors.com) to help doctors address issues with communication, including how to share information with patients who have varying levels of health literacy, using the repeat-back method, and how to involve family members or trusted friends to assist the patient during and after appointments. With all patient engagement methods, we try to examine the benefits and risks for both doctor and patient as we did here.
This commentary is wrong on so many scores at once – including advising doctors to tell patients things about the law in the relevant jurisdiction which may be simply untrue. There is no good reason to try to prevent a patient taking an audio-recording of their consultation home. Hostility to this well-established patient initiative is in my view both unethical and counter-productive. It will simply ensure that the practice continues to be carried out predominantly covertly. Happy with that docs?
We encourage doctors to know the specific laws concerning recordings in the jurisdiction where they practice and to use that to guide the policies in their practice. A strong physician-patient relationship with mutual trust is key, and we highly encourage doctors to use programs such as Ask Me 3 (www.thedoctors.com/AskMe3) that teach both patient and doctor how to help build that relationship and have effective conversations during office visits.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
This site uses Akismet to reduce spam. Learn how your comment data is processed .
Comment will held for moderation
- RELATED ARTICLES
- MORE FROM AUTHOR

Featured Clinical Reviews
- Screening for Atrial Fibrillation: US Preventive Services Task Force Recommendation Statement JAMA Recommendation Statement January 25, 2022
- Evaluating the Patient With a Pulmonary Nodule: A Review JAMA Review January 18, 2022
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Can Patients Make Recordings of Medical Encounters? What Does the Law Say?
- 1 Dartmouth Institute for Health Policy and Clinical Practice, Lebanon, New Hampshire
For many clinicians, it is possible that some of their patients are recording their office visit, with or without permission. In a cross-sectional survey administered to the general public in the United Kingdom, 19 of 128 respondents (15%) indicated that they had secretly recorded a clinic visit, and 14 of 128 respondents (11%) were aware of someone covertly recording a clinic visit. 1 Because every smartphone can record conversations, this may become even more commonplace. The motivation is often reasonable: patients want a recording to listen to again, improve their recall and understanding of medical information, and share the information with family members. 2 A review identified 33 studies (including 18 randomized trials) of patient use of audio-recorded clinic-visit information. Audio recordings were highly valued; across the studies, 72% of patients listened to their recordings, 68% shared them with a caregiver, and individuals receiving recordings reported greater understanding and recall of medical information. 3
Read More About
Elwyn G , Barr PJ , Castaldo M. Can Patients Make Recordings of Medical Encounters? What Does the Law Say? JAMA. 2017;318(6):513–514. doi:10.1001/jama.2017.7511
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

Is it OK to record your doctor visit without permission?

Christine Martinello is no stranger to the doctor’s office.
“Currently, I go for myself and for injuries that I've had, or I went to the hospital a lot for my dad when he had cancer,” she explains.
She says she sometimes forgot the doctor’s instructions once she got home, so now, “Whenever I feel like I need to remember all the information, I'll record the visit.”
She does it right on her phone, using a recording app. A recent study shows 15-percent of patients now record visits, either with or without permission.
“Many patients actually are afraid to ask for permission to record and therefore they’re doing it by keeping the phone on in a pocket or whatever,” says Professor Glyn Elwyn of the Dartmouth Institute for Health Policy & Clinical Practice. Dr. Elwyn co-authored a study, which found a variety of reasons for why patients record and for what they do with those recordings.
Dr. Elwyn says, “They actually listen to them, often many times, and then they share them with their relatives, their sons, their daughters, their caregivers.”
Whether it is legal to record varies around the country, but legality aside, Dr. Elwyn says there is a question of ethics and common courtesy.
“If somebody finds out that I've recorded this encounter secretly, that leads to a breakdown of relationships between clinicians and patients,” he explains.
Some physicians are concerned with liability, however, some practices actually encourage the option, even offering to make recordings for you.
Both Christine and Dr. Elwyn see great benefits for patients and doctors in pressing record.
“If you're in the recording, as a clinician, you might take more care to spell out exactly what it is you want people to do,” Dr. Elwyn says.
And Christine adds, “The more information you have, the better you can make decisions. It's better for everyone.”
Sign up for the Morning Newsletter and receive up to date information.
Now signed up to receive the morning newsletter..

WXYZ named Station of the Year by MAB
Watch CBS News
More patients are recording their doctor visits
By Mary Elizabeth Dallas
July 10, 2017 / 3:48 PM EDT / HealthDay
Smartphones are capturing all of life's moments, and doctor visits are no exception.
At least 1 in 10 U.S. patients now records discussions at medical appointments , researchers said.
But do they have the right to do so?
The legality of these taped visits depends on where you live, said investigators from the Dartmouth Institute for Health Policy and Clinical Practice.
"In the U.S., the situation is complex," said professor and senior scientist Dr. Glyn Elwyn.
"Wiretapping or eavesdropping statutes provide the primary legal framework guiding recording practices and protecting privacy , so a patient who would like to record a doctor's visit should familiarize themselves with laws in their state," Elwyn said.
There are two main differences between state wiretapping laws, Elwyn and his colleagues said in a new report.
In "all-party" states, recordings made by doctors or patients are illegal unless everyone involved is aware and provides consent.
In "one-party" states, just one person involved in a conversation needs to be aware and consent to the recording. Only in these states can patients legally record an office visit without their doctor's consent and vice versa.
The authors said 39 states and Washington, D.C., follow the one-party consent rule; all others adhere to the all-party requirement.
How are patients using these increasingly common recordings?
After reviewing 33 studies involving audio-recorded clinical visits, the researchers found that about 7 out of 10 patients listened to their own recordings. A similar number shared them with a caregiver .
In many cases, patients used the tapes to remember important details about their office visits.
"Most people are sharing their recordings with a family member or caregiver, or they are listening to recording themselves, so they can better recall the information they received during the encounter," Elwyn said in an institute news release.
- Are you skipping that doctor visit or pill you need?
Patients said the recordings left them feeling more satisfied with their care.
"Health care overall is moving toward greater transparency and patient recordings are going to become more common," Elwyn said.
"That means there would be tremendous benefit to patient advocacy groups, health care organizations, providers and policymakers working together to develop clear guidelines and policies around the responsible, positive use of open recordings," he added.
While some doctors and hospitals worry that taped appointments and procedures will be used against them, others take a more positive view. The Barrow Neurological Institute in Phoenix, for example, encourages patient-doctor recordings and rewards doctors who comply, the researchers said.
The report was published July 10 in the Journal of the American Medical Association .
More from CBS News

Doctors take on dental duties to reach low-income and uninsured patients

Arizona Supreme Court's abortion ruling sparks fear, uncertainty

Arizona's abortion ban likely to cause people to travel to states it's still legal

Musician Marcus King's new album focuses on his mental health journey
Situation in Haiti April 5, 2024
U.s. citizens in haiti, update january 10, 2024, information for u.s. citizens in the middle east.
- Travel Advisories |
- Contact Us |
- MyTravelGov |
Find U.S. Embassies & Consulates
Travel.state.gov, congressional liaison, special issuance agency, u.s. passports, international travel, intercountry adoption, international parental child abduction, records and authentications, popular links, travel advisories, mytravelgov, stay connected, legal resources, legal information, info for u.s. law enforcement, replace or certify documents.
Country Information
Share this page:
Prevention Tips
How the U.S. State Department Can Help if Your Child is Abducted Overseas
Children's Passport Issuance Alert Program
Child Abduction Frequently Asked Questions
Find Resources in Your State
American Samoa
Connecticut
District of Columbia
Massachusetts
Mississippi
New Hampshire
North Carolina
North Dakota
Northern Marianas Islands
Pennsylvania
Puerto Rico
Rhode Island
South Carolina
Virgin-Islands
West Virginia
South Dakota
Contacting Law Enforcement
Steps to Stopping an Abduction in Progress
Resources for Parents
Information about the Sean and David Goldman International Child Abduction Prevention and Return Act
Preventing a Possible Abduction
For frequently asked questions on how to prevent a possible abduction, please see the information below., what can i do if i think that my child’s other parent or relatives may take my child outside the united states.
Consider how you can take action and review our Prevention Tips .
We strongly encourage parents to consult with an attorney regarding what actions are appropriate for their particular circumstances, which may include, among other things, obtaining a court order that prohibits a child from traveling outside of the United States.
How effective are abduction prevention measures?
Prevention measures can be very effective if appropriate steps are taken in a timely manner. These steps include engaging law enforcement and legal representation to advocate on your behalf and securing court documents that protect you and your child. The Children's Passport Issuance Alert Program (CPIAP) can also help to prevent a possible abduction by alerting a parent to a U.S. passport application for their child.
A clear court order may be the most important preventative measure. Court orders may include provisions such as:
- prohibiting international travel of the child,
- specifying the beginning and end dates of visits,
- requiring supervised visitation,
- requiring the court’s approval to take the child out of the state or country, and/or,
- requiring a court or a neutral third party to hold a child’s U.S. and/or foreign passport(s).
Without a specifically worded order with travel restrictions for your child, law enforcement and airline personnel may not be able to prevent your child from leaving the United States.
Where can I go for legal advice?
Although we cannot recommend an attorney to you, an attorney in the United States may help you navigate the legal system. We strongly encourage parents to consult with an attorney regarding their particular circumstances.
What can law enforcement do if my child has been or may have been taken outside the United States?
Local law enforcement can work with you to have your child’s name entered into the National Crime Information Center (NCIC) database, to assist in searching for your child. If you believe your child has already been taken out of state, you can also notify the nearest FBI field office, located by state . Some law enforcement agencies may be less responsive if there is no court order for your child. If you have difficulty getting local law enforcement to focus on the search for your child, contact the National Center for Missing and Exploited Children’s (NCMEC) 24-hour hotline at 800-843-5678. NCMEC is a non-profit organization that provides support to parents whose children are missing, including domestic and international family abductions
What information should I provide to law enforcement?
Gathering pertinent information regarding your child and the person you think has taken the child may help officials involved in the search, such as:
- Photographs of the child and biographic information,
- Details about the person you think has taken the child and associates,
- Court orders regarding your child,
- Circumstances about when you last saw the child,
- Where you think they may travel,
- Travel itineraries, departure routes, or airlines/border crossings
Some law enforcement agencies may be less responsive if there is no court order for your child. Your attorney may also be able to assist in working with local law enforcement or the courts. If you have a court order that prohibits removing the child from the U.S. and a law enforcement contact, call 888-407-4747, or email [email protected] .
What is required for my child to travel outside of the United States?
The United States does not have exit controls or require two-parent consent for a minor to leave the country. If traveling from the United States to Canada, Mexico or the Caribbean, travelers are also subject to the Western Hemisphere Travel Initiative (WHTI). Under WHTI, countries have different entry and exit requirements for travelers and in some cases minors may exit the U.S. without a passport. To learn more about these requirements, including land and sea entry and exit laws for all travelers, review Customs and Border Protection’s information about WHTI.
What laws exist to help prevent child abduction?
International parental child abduction is a crime in every state and the District of Columbia under specified circumstances, and is also a federal crime under the International Parental Kidnapping Crime Act. Read more about laws and regulations .
My spouse is in the military, and I don’t want my child go overseas. Can you help?
We strongly encourage parents to consult with an attorney regarding their particular circumstances, and you can contact the Department of Defense.
What can I do if my child has been or may have been taken outside the United States?
Contact the Department of State’s Office of Children’s Issues at 888-407-4747 or [email protected] .
Start working with law enforcement as soon as possible. Keep a written record of the people and agencies you have contacted, as well as their telephone numbers and relevant contact information.
My child has been abducted, but is not going internationally. What can I do?
You can call the police. If you think your child has already been taken out of state, you can notify the nearest FBI field office, located by state . Some law enforcement agencies may be less responsive if there is no court order for your child. If you have difficulty getting local law enforcement to focus on the search for your child, contact the National Center for Missing and Exploited Children’s (NCMEC) 24-hour hotline at 800-843-5678. NCMEC is a non-profit organization that provides support to parents whose children are missing, including domestic and international family abductions.
Children's Passport Information
For frequently asked questions on children's passport information, please see the information below., who needs to sign for my child’s passport.
Generally, both parents or legal guardians are required to sign a passport application for a minor child under age 16. Please refer to our Passports for Minors Under Age 16 page for further information.
What Information about Your Child’s Passport is Available to You?
Passport information is protected by the Privacy Act of 1974. However, information regarding the application for and issuance of a passport to a minor is generally available to either parent, regardless of custody rights, as long as the requesting parent’s rights have not been terminated. Regarding the issuance or denial of United States passports to minors involved in custody disputes, please contact Passport Services.
What is required to apply for a passport for a minor under age 16?
All U.S. Passport applications for minor children under age 16 require that both parents/legal guardians consent or documentation showing that the other parent’s consent is not required (22 U.S.C. 213n and 22 C.F.R. 51.28). Passport applications for children under age 16 must be submitted in person at a passport agency or authorized passport application acceptance facility. For more information, review passport requirements for minors under age 16.

What is required to apply for a passport for children who are 16 or 17 years old?
Although the two-parent consent requirement does not apply to children who are 16 or 17 years old, according to Department regulations , a passport may not be issued to a child if a parent or legal guardian who has custodial rights over a child has notified the Department in writing that he or she objects to issuance of the passport. For more information, review passport requirements for minors age 16 and 17.
How can I order copies of my child’s passport record?
Please follow the instructions listed on the Department’s website to order copies of a passport record .
Children’s Passport Issuance Alert Program
For frequently asked quesitons on the children's passport issuance alert program (cpiap), please see information below., what is the children’s passport issuance alert program.
The Children’s Passport Issuance Alert Program (CPIAP) allows the Department of State’s Office of Children’s Issues to contact the enrolling parent(s) or legal guardian(s) to verify whether the parental consent requirement for minor passport issuance has been met when a passport application has been submitted for an enrolled child. In addition, upon a child’s enrollment in the CPIAP, we may alert the enrolling parent(s) or legal guardian(s) of a pending passport application and past passport issuances for the child.
Who can be enrolled in CPIAP?
Only U.S. citizens or children who qualify for U.S. citizenship under the age of 18 can be enrolled in the CPIAP.
Who can request that a child be enrolled in the CPIAP?
- A parent or legal guardian,
- Law enforcement,
- Child Protective Services, or
- Someone acting legally on behalf of a parent, such as an attorney or family member
Please note that privacy laws and regulations may limit who we can notify if we receive a child’s passport application.
How do I enroll my child in the Children’s Passport Alert Program (CPIAP)?
To enroll a child in the CPIAP, please follow the CPIAP instructions.
How can I update my contact information?
To update us with your most recent contact information, email us at [email protected] , or call 888-407-4747.
Please immediately inform the Office of Children’s Issues of any changes to your contact information and submit any additional documents relevant to the application or issuance of a passport to your child. Additional documents may include, but are not limited to, divorce decrees, custody orders, protective orders, warrants, and police reports. Failure to do so may result in your child being issued a U.S. passport without notice to you and/or without your consent. It is your responsibility to immediately provide our office with all relevant and up-to-date information.
Does entering a child's name into CPIAP always prevent a passport from being issued?
No. Enrolling a child in the CPIAP does not guarantee that child will not be issued a passport. The parent or legal guardian who requests entry of his/her child into the program may consent to issuance of the passport for a passport to be issued in accordance with established parental consent procedures.
Also, a passport may be issued without consent of both parents or legal guardians if the applicant for the passport can establish that consent of both parents is not required under federal law (22 U.S.C. 213n and 22 C.F.R. 51.28). For example, a court order providing the applying parent or guardian with sole legal custody of the child or a court order specifically authorizing the child to travel internationally with the applying parent or guardian may permit issuance of a passport without the consent of the other parent or guardian. This is true even if the child has been enrolled into the CPIAP.
How do I Remove a Child from the CPIAP?
A child is automatically removed from the CPIAP when he/she reaches the age of 18.
If you enrolled your child in the CPIAP, your child is under 18, and you no longer wish to be notified of passport applications for your child, submit a copy of your photo ID and a notarized written statement (including the child’s name and date of birth) requesting the child’s removal from the program to [email protected] .
What if my child already has a U.S. passport?
You may enroll your child into the CPIAP even if he/she already has a passport. Enrolling your child will allow us to attempt to notify you if an application for renewal of the passport is received.
Can an issued U.S. passport be tracked or flagged?
There are no mechanisms in place to track the use of a U.S. passport. The CPIAP is not a method for tracking the use of a U.S. passport. See Prevention’s Take Action page if you have concerns about your child traveling outside of the United States.
Does the CPIAP apply to passports of another country?
This program does not apply to foreign passports. The CPIAP does not prevent a dual national from obtaining and traveling on a foreign passport.
Foreign countries have their own regulations regarding issuance and denial of their passports to U.S. citizen minors who have dual nationality. If there is a possibility that the child has another nationality, you may contact the country’s embassy or consulate directly to inquire about parental consent requirements for passports. See Prevention’s Take Action page if you have concerns about your child traveling outside of the United States.
Dual Nationality: Learn more about the impact of dual nationality
For frequently asked questions on the impact of dual nationality, please see information below., what is the impact that dual nationality may have on my child’s travel outside of the u.s..
Be aware that your child may acquire the citizenship or nationality of another country pursuant to that country’s laws, which may include acquisition through:
- Birth outside of the U.S.,
- Mother’s citizenship,
- Father’s citizenship, or
- Naturalization
It’s important to know if your child has acquired or may acquire the citizenship of another country because it could enable your child to
- Obtain a foreign passport,
- Travel on a foreign passport, and/or,
- Travel on a parent’s foreign passport
Some countries require children to travel on a parent’s passport and do not issue passports to children.
What steps can I take to prevent my child from being issued a passport from another country?
- Consider contacting the foreign embassy or consulate to confirm if your child may be documented as a citizen of that country . A child may acquire citizenship documentation of some foreign countries without consent of both parents. You should confirm the foreign country’s requirements with the foreign embassy or consulate directly.
- Please note that not all countries have two-parent consent requirements for passport issuance. Consider contacting the foreign embassy or consulate to obtain information on that country’s rules on passport issuance for minors and to learn if they have a passport notification program.
- Be aware that foreign governments may not recognize U.S. court orders. Foreign embassies and consulates in the U.S. may issue passports to children who are their nationals regardless of a U.S. court order.
What if my child has a passport of another country?
U.S. citizen children at risk for or involved in international abductions may have more than one nationality. The Department of State cannot prevent another country from issuing passports to children who are also nationals of that country. However, it may be helpful to ask a foreign embassy or consulate in the United States either to not issue a passport to your child, or to notify you of a passport application.
See Prevention’s Take Action page if you have concerns about your child traveling outside of the United States.
The information in this flyer is provided for general information only, is not intended to be legal advice, and may change without notice. Questions involving interpretation of law should be addressed to an attorney licensed in the relevant jurisdiction.
Learn about a country
External link.
You are about to leave travel.state.gov for an external website that is not maintained by the U.S. Department of State.
Links to external websites are provided as a convenience and should not be construed as an endorsement by the U.S. Department of State of the views or products contained therein. If you wish to remain on travel.state.gov, click the "cancel" message.
You are about to visit:
Free Minor Travel Consent Form

A minor travel consent form is a legal document, signed by a child's parents and/or legal guardians, giving permission for the child to travel with another adult. Any time a child travels abroad without both parents and/or legal guardians, U.S. Customs and Border Protection requires the child to have this written permission.
This document is particularly important in international travel situations. It can be used to establish guardianship whether the child is traveling abroad with only one parent or with another trusted adult, such as a family member, friend, or educator.
In today's world, where concerns about child safety are paramount-especially when it comes to child abduction, custody disputes, and human trafficking-a minor travel consent form serves as a protective measure. It provides clear, legally binding, written permission that can be verified by immigration officials, airline staff, or travel companies, to make sure that the child's travel is both safe and authorized.
Without this form, travel may be delayed or denied. Domestic and international authorities need to be able confirm the child's guardianship and obtain the necessary permissions before allowing the child to travel onward.
How to Use the Minor Travel Consent Form
The form available below is a comprehensive template, designed to be easily copy/pasted and adapted in a word processor like Microsoft Word or Google Docs.
Given the critical nature of this document, we also provide a downloadable minor travel consent form in PDF format for your convenience.
It's important to note that while this sample form is a valuable starting point, it should be tailored to fit the specific details and circumstances of your child's travel.
Also be advised that this form does not replace a legal power of attorney document that could be used to make critical medical care decisions on behalf of a child.
This form is regularly reviewed and updated to ensure that this form remains current with travel and child safety best practices, reflecting our commitment to providing reliable and authoritative travel resources.
Minor Travel Consent Form
To Whom It May Concern:
I/We, (Full Name(s) of Custodial and/or Non-Custodial Parent(s)/Legal Guardian(s))
am/are the lawful custodial parent(s) and/or non-custodial parent(s) or legal guardian(s) of:
(Full Name of Accompanying Person)
(U.S. or Foreign Passport Number)
Date and Place of Issuance of This Passport)
((Name of Foreign Country)
during the period of
((Dates of Travel: Departure and Return)
During that period,
((Childs Name)
will be residing with
((Name of Person with Whom the Child will be Residing in Foreign Country)
at the following address:
((Number/street address and apartment number)
((City, State/Province, Country)
((Telephone and fax numbers)
Signature: Date: (Custodial Parent, and/or Non-Custodial Parent or Legal Guardian)
Full Name:
Signed before me,
, (Full Name of Witness)
this at . ((Date) and (Location))
Signature of Witness:
Download: Minor Travel Consent Form
The Legal Implications of Traveling Without a Minor Consent Form
While the minor travel consent form is not a universally required legal document, a child traveling without one can lead to serious complications in many countries. Different nations have their own regulations regarding child travel. Being uninformed or unprepared can quickly lead to distressing situations for both you and your child.
1. International Legal Considerations:
- Country-Specific Requirements Vary: Each country has its own set of rules regarding minors traveling without their parents. For instance, some countries in Europe may require additional documentation, such as a birth certificate or a parental authorization letter, in addition to the travel consent form. You need to be sure your child and their traveling companion(s) comply with all of the requirements for each country they plan to travel to and through.
- Risk of Travel Disruption: Without a consent form, minors traveling abroad may face delays or even denied entry at border control checkpoints. This can lead to missed transportation departures and costly changes to your travel itinerary.
- Embassy and Consulate Involvement: In cases where a minor is detained due to lack of proper documentation, the local embassy or consulate of the child's home country may need to be involved. This can lead to complex legal situations that take significant amounts of tame and/or money to solve.
2. Domestic Legal Implications:
- Airline and Transportation Policies: Within the United States, airlines and other transportation services have specific policies regarding unaccompanied minors (more on this later). Lack of a consent form, even for domestic travel, can result in the child being denied boarding.
- Legal Custody Disputes: In cases of separated or divorced parents, traveling without a consent form can raise legal issues related to custody agreements. It's crucial to understand and adhere to the legal requirements stipulated in custody arrangements to avoid legal repercussions.
A minor travel consent form can help you avoid many of these situations. Before traveling, be sure to research the specific travel requirements of the destination country regarding minor travel. In addition to the resources provided on this site, this can also be done through a country's embassy website or by consulting with travel experts like registered passport expediting services .
In complex situations, such as shared custody or special travel circumstances, consulting with a legal expert can provide clarity and ensure compliance with both domestic and international laws.
Minor Travel Consent Form Notary Requirements
We strongly recommend that you have any child travel consent form notarized. This can prevent issues establishing the authority and credibility of your documentation.
It can be challenging to find and secure the services of a notary in person. Thankfully, it is possible to use an online notary service to notarize your minor travel consent form. This can save you serious time and stress.
We recommend using NotaryLive , a fully-secure, online notirization platform with an "Excellent" rating from TrustPilot . NotaryLive is fast, affordable, and fully compliant with state law, so you can be sure your notarized minor travel consent form is both legal and valid.
Unaccompanied Minors
Airlines have general rules about the ages and circumstances where children can fly alone, too. There are also usually additional fees that come with buying a ticket for a minor that will be traveling without an adult. As part of that extra cost, many airlines offer some additional supervisory and support services to be sure the traveling child is safe and comfortable while traveling on their own.
For more, check out our guide to unaccompanied minors traveling internationally . There, you will find details about the considerations, accommodations, and policies that apply to kids traveling internationally without an adult parent or guardian.
More Tips for Parents of Minors Traveling Abroad
Besides proper documentation, there are other ways to help a child have a safe international trip. Any time your child is traveling without you, give yourself peace of mind by taking these proactive steps.
Be Proactive In Shared Custody Situations
Parents who share custody of their children should each carry copies of the legal custody documents. You can also contact the embassy of the country or countries the minor child will be visiting to confirm travel entry requirements. This proactive step can help avoid issues at border crossings and during the child's stay abroad.
A simple notarized statement, such as the one below, should suffince in most cases.
"I, [PARENT NAME] acknowledge that [SPOUSE NAME] is traveling out of the country with my [SON/DAUGHTER] whom we share custody of. This authorization gives [SPOUSE NAME] my full permission to do so.
Use a GPS Tracker to Keep Track of Your Child While Abroad
GPS technology makes it possible to pinpoint a person's exact location, anywhere in the world. If your child is traveling without you, it makes sense to keep a GPS tracker on their person so that you know where they are. You can also use additional trackers to help keep tabs on your child's luggage or other valuables.
- Apple AirTags are small, inexpensive GPS tags that can be purchased individually or in packs of 4 . They use bluetooth connectivity and the vast number of Apple users across the globe to create a reliable GPS tracking network. Using your iPhone or Apple device, you can ping any AirTag that is linked to your AppleID and locate it quickly. Thanks to its small size, an AirTag can easily be tucked into luggage, sewn into a child's clothing, or stashed in a travel wallet.
- JioBit is an all-in-one GPS tracking system specifically designed for tracking your child. While it is more expensive than Apple AirTags, JioBit is a durable and secure alternative-particularly useful for those who don't already have an Apple device.
Use a Parent-Controlled Debit Card
Traveling costs add up. Everything from food, transportation, lodging, and fun comes with a price. If your child is traveling without you, you want to be sure they have the money they need, but also that it is being protected.
There are a number of debit cards that allow parents to keep an eye on their child's spending as well as their remaining balance. Should your child and their card become separated, you have the ability to prevent unauthorized purchases and possibly even get a replacement sent to wherever your child is staying.
Traveling with minors requires careful planning and a strict adherence to both American and international laws. This guide and the minor travel consent form we have shared are designed to provide you with the necessary information and tools to ensure a smooth and stress-free journey for your child. Whether your child is traveling with a guardian, as part of a group, or alone, the right preparation can make all the difference.
Remember, the safety and well-being of your child are paramount. By staying informed about the latest travel regulations and using our resources, you can confidently prepare for your child's next trip. If you have any further questions or need personalized advice, our team of travel experts is always here to assist you. Safe travels!
Related Articles and FAQs: International Travel with Minors
How to get a passport for a minor
Form DS-3053: Consent to Issue Passport to Minor
Where to apply for a minor's passport
Minor Passport FAQ
Expedite a child's passport in 24-48 hours
Can one parent apply for minor child's passport?
Is a minor consent form necessary?
What do grandparents need to travel with a grandchild?
Does father need consent to travel alone with minor child?
Does minor need passport to enter Canada?
Top 5 Questions About Expedited Passport Couriers
1. How can you get a passport when you're in a hurry? 2. What exactly does a passport expediter do? 3. Are passport expediting services legitimate? 4. How can I identify a reliable passport expeditor? 5. Is expedited passport service worth it?
U.S. Passport Service Guide - Who we are
For over 20 years, U.S. Passport Service Guide has helped American citizens understand and navigate the passport application process. We use our expertise and experience to help travelers get United States passports quickly and efficiently.
Our website currently receives over half a million visitors a month. We are committed to going the "extra mile" for all of our readers. Both passport officials and website visitors frequently write to express gratitude for the assistance we provide.
Please contact us if you have any travel related questions - especially ones about passports and visa expediting. We usually respond to e-mails within 24 hours, oftentimes the same day. We are committed to working with you until you get the answer you need.
International Travel
- Entry Requirements
- International Airfare
- International Cruises
- Travel Documents
- Travel Insurance
- Travel Tips
- Travel Warnings
Travel Resources
- Bestselling Luggage
- Top Destinations
- Travel Accessories
- Travel Articles
- Travel Business
- Travel Deals
- Travel Gifts
- Travel Links
- Travel Magazines
- Travel Tools
- Where to Stay
- Passport Information
- Expedited Passports
- Registered Couriers
- 24 Hour Passports
Travel Visas
- Visa Services

About Contact News Privacy Policy Cookie Policy Terms of Use Sitemap ©2024 U.S. Passport Service Guide, All Rights Reserved
- General Nursing
- Nursing Specialties
- Nursing Students
- United States Nursing
- World Nursing
- Boards of Nursing
- Breakroom / Clubs
- Nurse Q&A
- Student Q&A
- Fastest BSN
- Most Affordable BSN
- Fastest MSN
- Most Affordable MSN
- Best RN to BSN
- Fastest RN to BSN
- Most Affordable RN to BSN
- Best LPN/LVN
- Fastest LPN/LVN
- Most Affordable LPN/LVN
- Fastest DNP
- Most Affordable DNP
- Medical Assistant
- Best Online Medical Assistant
- Best Accelerated Medical Assistant
- Most Affordable Medical Assistant
- Nurse Practitioner
- Pediatric NP
- Neonatal NP
- Oncology NP
- Acute Care NP
- Aesthetic NP
- Women's Health NP
- Adult-Gerontology NP
- Emergency NP
- Best RN to NP
- Psychiatric-Mental Health NP
- RN Specialties
- Best RN Jobs and Salaries
- Aesthetic Nurse
- Nursing Informatics
- Nurse Case Manager
- Forensic Nurse
- Labor and Delivery Nurse
- Psychiatric Nurse
- Pediatric Nurse
- Travel Nurse
- Telemetry Nurse
- Dermatology Nurse
- Best NP Jobs and Salaries
- Family NP (FNP)
- Orthopedic NP
- Psychiatric-Mental Health NP (PMHNP)
- Nurse Educator
- Nurse Administrator
- Certified Nurse Midwife (CNM)
- Clinical Nurse Specialist (CNS)
- Certified Registered Nurse Anesthetist (CRNA)
- Best Free Online NCLEX-RN Study Guide
- The Nursing Process
- Question Leveling
- NCLEX-RN Question Identification
- Expert NCLEX-RN Test-Taking Strategies
- Best Scrubs for Nurses
- Best Shoes for Nurses
- Best Stethoscopes for Nurses
- Best Gifts for Nurses
- Undergraduate
- How to Become an LPN/LVN
- How to Earn an ADN
- Differences Between ADN, ASN, AAS
- How to Earn a BSN
- Best MSN Concentrations
- Is an MSN Worth It?
- How to Earn a DNP
- MSN vs. DNP
Going to Patient's home without patient consent
Nurses HIPAA
Published Apr 19, 2018

I work in home care. Normally a physician will send our company a referral for home care. We contact the patient, ask to go to their home for the initial Start-of-Care visit, then start services at that agreed upon visit. Recently our intake team said we are now required to drive out to a patient's home if they don't answer our phone calls/ return our phone calls. Their thought is "we need to do a well check on them". My thought is "they are not our patient's yet a well-check should be completed by the police".
Is this violating HIPAA by having us go to a patient's home without their consent?
Sometimes these patient's aren't aware the original referral even happened, so us going out to see them could be a surprise. What's the difference between me and a door to door salesman at that point.
One of our intake nurses says this violates HIPAA. I don't know if it does but don't want to violate HIPAA rules.

More Like This

- + Add a Comment
38,333 Posts
As far as I'm concerned, it violates HIPAA and asking to get some dire consequences. If they are that hard up for business, they should light a fire under their marketers.
Here.I.Stand, BSN, RN
5,047 Posts
There is no way ever, EVER, I would go to a pt's house without permission. If pt that were me, I would be livid. If I agree to home nursing, I am very capable of contacting the agency... and knowing that a professional used my medical record to track me down, would feel very violating.
Another thought: say you showed up to offer the nurse visits. Would the client necessarily feel free to decline? Is the agency satisfied with a "no," or do they expect you to probe and "educate?" The lack of a call-back is an easy, confrontation-free method of opting out. Then have to face the nurse unannounced? In their own home??
inthecosmos, BSN, MSN, RN, APRN
Wow, no. Absolutely not. HIPPA violation as the patient didn't consent. Therefore, you're using their PHI without permission.
NurseCard, ADN
2,847 Posts
I'm not understanding the HIPAA violation part.
Usually the patient, while in the hospital, agrees to use a certain
home health agency. THEN at that point, the patient's information
is sent to that home health agency, along with the patient's date
that they will be discharged home.
Nurse that will be doing the Start Of Care visit receives the
patient's information, again because the patient consented to
using that particular home health agency. I believe also, the
patient signs something before leaving the hospital, agreeing
that they will receive post acute care from that particular
Nurse contacts the patient to set up the start of care visit.
Nurse is unable to contact the patient, or any next of kin.
At THAT point, yes an agency may ask that nurse to just go
ahead and go to the house. For varying reasons, the patient
may not be able to be contacted. Phone may not be working.
Patinet may not be able to hear phone.
Some nurses are okay doing this, some are not. And some
agencies have a policy that the nurse does not go to the
house without having reached the patient first.
Again, though, where is the HIPAA violation? The patient
should have consented to that HH agency already before
a referral ever arrives.
Now, I HAVE been in just a couple of situations in which,
for reason unknown to me.. more than one HH agency
received a referral to see a patient. A couple of times.
Sometimes these patient's aren't aware the original referral even happened, so us going out to see them could be a surprise. What's the difference between me and a door to door salesman at that point. One of our intake nurses says this violates HIPAA. I don't know if it does but don't want to violate HIPAA rules.
Again... merely going to the house doesn't violate HIPAA. If a doctor or anyone
else just arbitrarily sends a patient's information to the HH agency without
permission, then yes that would be the HIPAA violation.
It is my genuine belief that this DOESN'T exactly happen like that.
SOMEONE gives the doctor permission to refer the patient to HH. It may
be the patient's POA. It may even be the patient, but then the
patient forgets that the doctor mentioned HH, and that the
patient okayed it. I mean, I've called patients on the phone
to set up the initial visit... and had the patient say something like
"Oh, Dr Jones set up home health for me? Wow... okay. Well,
come on out at 1pm, I'll be here".
I'll admit, I worked for a home health agency that used questionable practices.
However, even they understood that "no means no".
Again though, HH agencies don't just receive the patient's info without
the patient's consent. The patient or the POA *HAVE* agreed to home
There are PLENTY of nurses that will not go to the patient's house if
unable to reach the patient by phone, and that is perfectly fine as
far as I'm concerned. However, again, the mere act of going to the
house is not a HIPAA violation.

2,121 Posts
Even if the patient had consented to home health care when they were in the hospital and had forgotten they had done this, their records will show if they have said they would like to be contacted by phone and whether it is acceptable to leave a phone message. I agree with above posters that the agency nurse showing up at the patient's door when the patient has not already agreed to this nor confirmed their agreement for home health visits over the phone with the agency, is very inappropriate, and violates the patient's rights to their privacy and autonomy. The patient didn't give consent for their PHI to be used in this way. I too would be furious if this happened to me or my family member.
NRSKarenRN, BSN, RN
10 Articles; 18,314 Posts
I work in home care. Normally a physician will send our company a referral for home care. We contact the patient, ask to go to their home for the initial Start-of-Care visit, then start services at that agreed upon visit. Recently our intake team said we are now required to drive out to a patient's home if they don't answer our phone calls/ return our phone calls. Their thought is "we need to do a well check on them". My thought is "they are not our patient's yet a well-check should be completed by the police". Is this violating HIPAA by having us go to a patient's home without their consent?
I'm disagreeing with majority of above advice based on 30yrs in homecare and 10+yrs as Central Intake Mgr: There is no HIPAA violation as written/verbal order obtained from physician/hospital/SNF/insurance company for home care service eval.
Home Health agency is obligated to provide evaluation visit once homecare referral is accepted. For Medicare certified agencies, Medicare requires initial homecare eval within 48hrs of ordered start of care date to determine if patient meets homecare criteria especially homebound status and admission to homecare. Well check IS required with outcome documented along with notifying referral source inablity to reach patient.
Registered Nurse is admitting service when multi-disciplines requested. PT/ST may admit only when they are the primary service being requested. In our Philadelphia urban/suburban area, about 1/4 of our referrals have incorrect phone numbers/ phone service disconnected despite our community/hospital liaisons meeting patients prior to discharge due to forgetfullness, lengthy inpatient stay so bill not paid, financial issues, old age, fear of admitting home issues, cell phone voice mail full/out of minutes,etc.
Difficulty contacting patients has escalated over the past 5 years in my area.
Recommended strategies to decrease patient not found/wellness checks:
1. Referral source needs to provide patient and emergency contact info, so 2 sources to call.
2. Inner city hospitals with highly transient + homeless population: liaisons call phone numbers provided to see if working prior to sending referral to agency, immediately followup with patient to get alternate emergency contact # then possible.
Frail elderly often taken to different home upon children arriving to bring parent home from facility when they see condition of parent so liaisons try to get next of kin #.
3. When prior agency patient. Intake staff compare address+ phone numbers to prior address/phone to see if misplaced digits.
4. Physician referrals: When multiple calls left over 2 days, we contact the physician to request office staff contact patient that homecare being requested: patients often will recognize doctors office # / voice mail left then call agency to arrange eval visit.
6. Liaisons contacted in 24hrs when unable to reach patient: they will make double check phone #, attempt to locate another contact # in chart and male outreach call too reminding patient of request/consent to homecare visit.
5.. When patient unable to be contacted, wellness visit e.g drive-by is done AND we leave printed door knob card which is often successful in getting patient to contact agency:
ABC agency visited your home ______ (date) at request of __________ (insert physician name/hospital) to start home care service for Nursing / Physicial Therapy/ Speech Therapy (circle discipline).
Please call our toll free number: 888-888-8888, a nurse is on call 24hrs a day.
_______________________ (Professional prints name).
Hope this helps other homecare staff.

Penelope_Pitstop, BSN, RN
2,365 Posts
HIPAA allows the passage of PHI from one protected entity to another for the purpose of treatment (which involves care coordination/case management) as long as it is given in a secure manner. As long as the physician, hospital, rehab unit, etc., has ensured secure delivery of PHI to the HHC agency, there is no violation. The SOC RN is using that information provided for the purpose of treatment as ordered by a provider who has an informed consent on file signed by the patient or designated party for the express purpose of disclosing said information appropriately.

trytounderstand
For the elderly or someone who is recovering and had had a recent stay in a hospital where they may have been treated and learned that "no" does not always mean "no". Because I have seen patients "educated" until they have accepted treatment they did not want or in same cases did not really need just because they were hounded or told they were being noncompliant and it was going in their record.
Showing up unannounced at a new client's home just because they have not answered the phone is wrong. If HH is that concerned that something is amiss and the possible client need helps should HH not contact their primary care provider or hospital/referrer and let this provider contact whoever they have listed as next of kin or emergency contact? On second thought, if they have actually been referred to HH this information should have been provided to them as well.
Then if all else fails have authorities with you to make sure there is nothing amiss at the patient's home and to have proof that the patient is willing for the nurse to enter their home since initial contact with the patient has not been made first. Just showing up could be construed as harassment or violation of patient's privacy. I would think they are not your patient/client until they have accepted your phone call and agreed to a visit before hand.
- Make My Plan
Can a Parent Take a Child Out of State Without Consent?
Determining whether you need consent to take your child out of state can be tricky.
Many states have laws regarding out-of-state travel to prevent parental kidnapping . How these rules apply to you depends on:
- Your type of custody
- Whether you are the custodial or noncustodial parent
- Your marital status
Alternatively, the court or parents can specify in a parenting plan whether parents need permission to take the child out of state.
There could be serious consequences for taking your child across state lines without consent. To avoid upsetting the other parent or getting in trouble with the law, know what's required of you before you decide to take a vacation or move states .
Visualize your schedule. Get a written parenting plan. Calculate your parenting time.
Make My Agreement Now
Who needs consent to take the child out of state?
The following people need consent to take their child out of state:
- Noncustodial parents
- Fathers whose paternity the government hasn't recognized
- Parents in active custody cases
- Parents with a court order requiring them to do so
Can a parent take a child out of state with joint custody?
Parents with joint custody can take the child out of state without consent so long as their custody order doesn't forbid it. But they must not get in the way of one another's relationship with the child. For example, if they take the child on a trip, they must be back in time for the other parent's visitation.
Married parents have joint custody of their children. A husband or wife can take the child out of state without permission.
Can a custodial parent take the child out of state without consent?
If you have sole custody , you can take the child out of state without consent, unless your custody order prohibits this. Your trip cannot interfere with the noncustodial parent's time with the child.
Mothers who aren't married when they give birth automatically have sole custody, so they can take the child out of state without the father's permission. This could change once the father establishes paternity and gets a custody order.
A custodial parent who wants to relocate to a different state must give the noncustodial parent written notice of the move and propose a parenting plan. Then the court decides whether to allow the move, or parents can settle the issue through an alternative dispute resolution method .
Getting permission to take your child out of state
Try to get the other parent's written consent before taking the child out of state even if you're not required to. Otherwise, they might use long or frequent trips as a reason to ask the court to change your custody order.
You could create a permission form for parents to fill out before leaving the state with the child. Consider hiring an attorney to draft this. It should cover:
- The travel itinerary
- Who's traveling with the child
- Contact info for the parent and child while they're away
In your parenting plan, you can require both parents to sign the form (possibly in front of a notary) before either one removes the child from the state.
If you think the other parent plans to keep the child from you, you can ask the court for an emergency order . Among other things, it could give the court power to confiscate the child's or parent's passport if that parent tries to take the child out of the country.
Punishments for taking the child without permission
If you defy your court order by taking the child somewhere without permission, you could be held in contempt of court , have to pay fines, lose your parental rights or face jail time.
Parental kidnapping laws are different in each state. Typically a parent must have an active custody order or case to be charged with parental kidnapping, unless they intentionally hide the child from the other parent.
Some countries have laws that require parents arriving at their border with a child to have written permission from the other parent.
Planning ahead
To prevent a return to court, state in your parenting plan whether parents need consent to take the child out of state.
The Custody X Change parenting plan template has you covered with provisions for out-of-area travel and moving. You can specify where parents may take the child and how much notice they must give. Plus, you can create custom provisions.
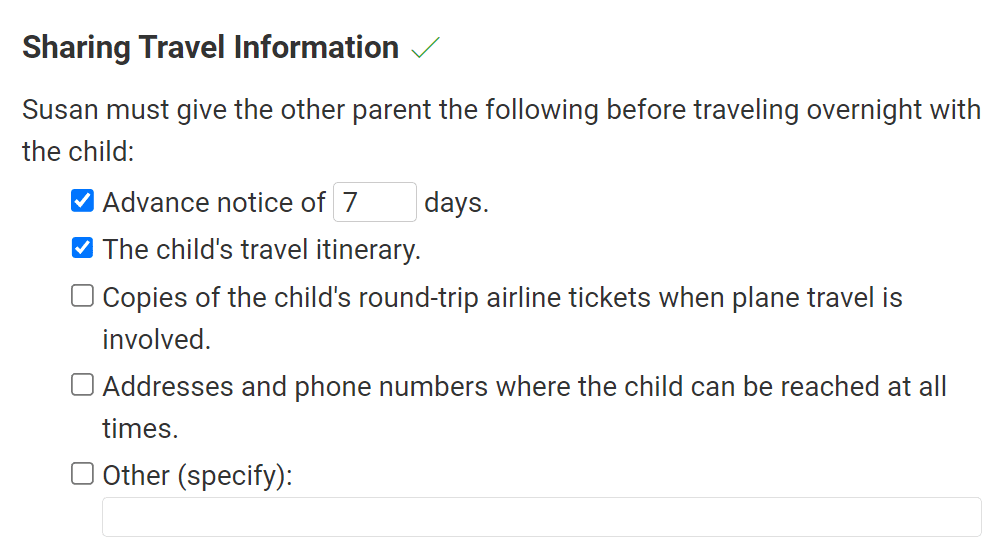
Your provisions and parenting schedules will be organized into a court-ready parenting plan.
It's just one of the ways Custody X Change helps you protect your child and your custodial rights.
Explore examples of common schedules
Explore common schedules, join the 60,000+ other parents who have used our co-parenting tools, organize your evidence.
Track your expenses, journal what happens, and record actual time. Print organized, professional documents.
Co-parent civilly
Our parent-to-parent messaging system, which detects hostile language, lets you collaborate without the drama.
Get an accurate child support order
Child support is based on parenting time or overnights in most jurisdictions. Calculate time instead of estimating.
Succeed by negotiating
Explore options together with visual calendars and detailed parenting plans. Present alternatives and reach agreement.
Never forget an exchange or activity
Get push notifications and email reminders, sync with other calendar apps and share with the other parent.
Save up to $50,000 by avoiding court
Write your parenting agreement without lawyers. Our templates walk you through each step.
Long distance schedules
Third party schedules
Summer break
Parenting provisions
Scheduling:
How to make a schedule
Factors to consider
Parenting plans:
Making a parenting plan
Changing your plan
Interstate , long distance
Temporary plans
Guides by location:
Parenting plans
Scheduling guidelines
Child support calculators
Age guidelines:
Birth to 18 months
18 months to 3 years
3 to 5 years
5 to 13 years
13 to 18 years
Terminology:
Joint physical custody
Sole physical custody
Joint legal custody
Sole legal custody
Product features:
Software overview
Printable calendars
Parenting plan templates
Journal what happens
Expense sharing
Parenting time tracking
Calculate time & overnights
Ways to use:
Prepare for mediation
Get ready for court
Bring calm to co‑parenting. Agree on a schedule and plan. Be prepared with everything documented.
- 1. Visualize your schedule
- 2. Get a written parenting plan
- 3. Calculate your parenting time
No thanks, I don't need a parenting plan
- Skip to main content
- Skip to site information
Language selection
Help us to improve our website. Take our survey !
Consent letter for children travelling outside Canada
A consent letter demonstrates that a child has permission to travel outside Canada from every parent or guardian who is not accompanying them on the trip.
On this page
When to use a consent letter, how to write a consent letter.
A consent letter should be used for all cross-border travel when a child is travelling:
- with only 1 parent or guardian
- in the care of friends or relatives
- with a group, such as a sports, school, musical or religious group
This includes day trips and travel where a child will be with only 1 parent for part of a trip. For example, a child will leave Canada with both parents but will return with only 1 parent.
A consent letter is not a legal requirement in Canada, but it can simplify travel for Canadian children as it may be requested by immigration authorities when entering or leaving a foreign country or by Canadian officials or airline agents when re-entering Canada.
The person who is accompanying the child should bring the original signed letter rather than a copy. Officials may be less likely to question the authenticity of an original document.
If you are travelling with a child for whom you have always been the sole parent or guardian, you can bring a document that shows you are the child’s only parent or guardian, such as a copy of a long form birth certificate that identifies you as the only parent.
If the other parent is deceased and you have full custody of your child, you should bring a copy of the death certificate of the deceased parent when accompanying the child on a trip.
The definition of a child varies from country to country, so any child under 19 years old should carry a consent letter.
Using a letter of consent outside Canada
Countries have their own entry and exit requirements for children. The consent letter may not be considered sufficient by a country’s immigration authorities and there is no guarantee that they will recognize it. In some countries, your child may be deemed to be one of its citizens if you or the other parent is a citizen of that country. As a “deemed citizen,” your child may be subject to the same entry and exit requirements as other citizens of that country.
For more information, check the entry and exit requirements in the Travel Advice and Advisories for your destination country or contact the nearest embassy or consulate of the destination country before travelling.
Travel Advice and Advisories
Foreign representatives in Canada
Risk of abduction
If there is a risk that the accompanying parent will not bring your child back to Canada, consult a lawyer and proceed with caution before signing a consent letter.
International child abduction
There are no official guidelines for the content and format of a consent letter, but they usually include:
- the name of the child
- the names and contact information of parents or guardians
- the name and relationship of the person who is accompanying the child
- information on where the child is travelling and the duration of the trip
You may use 1 letter or multiple letters depending on the situation:
- If neither parent is accompanying the child, they can both sign 1 letter or they can each sign a separate letter
- Children from the same family who are travelling together may be listed on 1 letter
- Separate letters are recommended for children who will be travelling separately for part of the trip
- Consult a lawyer when writing a letter without specific dates or for frequent cross-border trips
A sample letter and interactive form are available to guide you in writing a consent letter:
- Sample consent letter
- Interactive form for writing a consent letter
You can change the letter to fit your specific situation, but you should try to include as much detail as possible.
The consent letter should be signed by:
- Parents who are married or in a common law relationship who are not accompanying the child travelling outside Canada
- custody of the child
- decision-making responsibility for the child
- guardianship of the child (in Alberta and British Columbia)
A court order or agreement may also specify who does or does not need to sign a consent letter for a child travelling abroad.
If the child is in temporary care: The consent letter should be signed by the appropriate child welfare agency representative granting consent for the child to travel with the accompanying person. If in doubt about who should sign the letter, consult a lawyer.
If one of the parents is deceased: If the child is travelling alone or without the surviving parent, the child should carry a consent letter signed by the surviving parent and a copy of the death certificate of the deceased parent.
Signature of a witness
Any adult may witness the signing of a consent letter. It is strongly recommended that a notary public witness and sign the letter as border officials may be less likely to question its authenticity.
If you are outside of Canada, a consular officer at a Canadian government office may witness the signing of a consent letter ( fees apply ).
- Children and travel
- Travelling with Children brochure
- International Child Abductions: A guide for affected parents
- Travelling as a dual citizen
- Children travelling to Canada (Immigration, Refugees and Citizenship Canada)
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

International travel documents for children
See what documents a child needs to travel to or from the U.S. alone or with a parent or relative.
Children traveling to the U.S.
All children, including infants, must have their own travel documents such as a passport or document from a Trusted Traveler Program to enter the U.S. If you travel or are going to travel with a child, consider taking the following documents:
- If the child is traveling with only one of their custodial parents, they must have a letter of consent, preferably in English and notarized, from the other parent or signed by both parents. The letter should say "I acknowledge that my son/daughter is traveling outside the country with [the name of the adult] with my permission."
- If one parent has sole custody of the child, a copy of the custody document can take the place of the other parent's letter.
- Parents who frequently cross the border by land with a minor must always carry a letter of permission from the other parent.
U.S. citizen children traveling abroad
Ports of entry in many countries have security measures to prevent international child abduction . If you are traveling alone with your child, you may be required to present documentation proving you are the parent or legal guardian. You may also need a letter of permission from the other parent for your child to travel.
If your child travels alone, depending on the country, they may be required to present a notarized letter from both parents or their legal guardian. If a minor is traveling abroad and is not accompanied by both parents or a legal guardian, contact the embassy or consulate of the country you will be visiting and ask about entry and exit requirements for that country.
LAST UPDATED: December 6, 2023
Have a question?
Ask a real person any government-related question for free. They will get you the answer or let you know where to find it.
Landlord’s Right To Access Property in UK 2022: Can Landlords Visit Without Tenant Permission?
A landlord’s right to access property is a contentious topic. It’s not unusual to hear about landlords being accused of trespassing or sued for unlawful entry by a disgruntled tenant.
Although a property is owned by the landlord, this does not grant unlimited right of access without some form of agreement with the tenant. In most circumstances, landlords are required to give reasonable notice before any property visits, although there are some exceptions.
- What are the rules regarding a landlord’s right to access?
- Do landlords have the right to access for repairs?
- Why do landlords need right to access property?
- What are the right to access rules for property viewings?
- How much notice must a landlord give before visiting?
- Can a landlord enter a property without permission?
- What if the tenancy agreement says a landlord has the right to enter?
- Are there any exceptions to 24 hours’ notice?
- What if a tenant refuses access to the property?
- What action can landlords take to gain access to their property?
- What if a landlord enters the property without notice or consent?
Landlord access rights and quiet enjoyment
All tenants have the right to quiet enjoyment. This means they have the right to live in their rental property without interference from the landlord, letting agent, or anybody else.
Quiet enjoyment is an implied term, meaning that it does not need to be stated explicitly in a tenancy agreement to be enforced. The other primary implied term that landlords must follow is to keep the property in good repair and fit for human habitation.
Tenants must also follow implied terms. These are to pay rent and to treat the property in a tenant-like manner.
Although the landlord owns the property, they must get the tenant’s consent before visiting. If the landlord or anyone acting on the landlord’s behalf does enter the property without consent, they will be trespassing and will be in breach of the tenancy.
Up next: Tenant Rights When Renting Property In 2021
Landlord’s right to access and repair obligations
Section 11 of the Landlord and Tenant Act 1985 states that a landlord has an obligation to maintain and repair:
- The structure and exterior of the property (including drains, gutters and external pipes ),
- The installations in the property for the supply of water, gas and electricity and for sanitation, and
- The installations in the property for space heating and heating water .
The landlord, or someone instructed by the landlord, like a plumber or gas engineer , will need access to the property to carry out these repairs .
In addition to access for repairs, the landlord also has a right to view the condition of a property. The landlord, or someone acting as their agent, can gain access to the property at a “reasonable time of the day” but only after giving the tenant a minimum of 24 hours’ notice in writing and receiving the tenant’s consent.
Why do landlords need the right to access their property?
The main reason landlords or letting agents request the right to access a rental property is to carry out repairs, maintenance and property inspections. There are several safety inspections that all rental properties in the UK must have:
- Gas Safety inspection (every 12 months)
- Electrical inspection (every five years)
- Energy performance assessment (every ten years)
Landlords or letting agents may also want to carry out a mid-term inspection . This involves visiting the property midway through the tenancy to ensure everything is in good condition and to address any issues.
If the tenancy is ending, landlords or agents may want to carry out viewings whilst the tenant is still living in the property. If the tenant has given notice to leave the property, they’ll likely be happy to accommodate property viewings. However, if the tenant is content in the property but has been given notice by the landlord, the landlord should be sensitive to the situation.
Landlord’s right to enter: 24 hours’ notice before visiting a property
Once a tenant has moved in, landlords must give at least 24 hours’ written notice and get the tenant’s consent before visiting their rental property. A message or email is perfectly sufficient. The notice should include the time and date of the visit and who will be visiting the property, and why and the tenant must give their consent for the visit to go ahead.
Some landlords and tenants will be happy to arrange visits without formal written notice, such as a quick phone call. This is perfectly fine, but it’s important to note that a tenant is legally entitled to refuse entry if you do not give written notice.
Can landlords enter a property without the tenant’s permission?
Under The Housing Act 1988 , landlords must give at least 24 hours’ notice before visiting, and the tenant must give permission.
As the tenant is entitled to quiet enjoyment of their home, they can refuse access to the property if necessary. The main reason a landlord will be visiting the property is to carry out repairs or safety inspections , so most tenants will happily oblige.
Some tenants may prefer to be present for any property visits and may request a change of time or so that they can be there. Other tenants may be happy for the landlord to access the property whilst they are out, but it’s up to landlords (or their letting agents) and tenants to make arrangements that suit everyone involved.
Landlord’s right to request access for property viewings
Landlords can request access to show prospective tenants around the property, but landlords should be aware of the disruption involved – especially if the tenant has been served notice to vacate.
Keeping the house tidy and open to strangers seven days a week can be stressful for the tenant. If possible, the landlord and tenant should agree on a few days a week when the tenant will be happy to accept viewings.
As mentioned, landlords must give at least 24 hours’ written notice before visiting the property and have the tenant’s permission before visiting. The tenant is not obligated to accept the landlord’s request.
Landlord access rights and tenancy agreements
A tenant’s right to quiet enjoyment is an implied term, meaning any clause in a tenancy agreement that goes against it will be unenforceable.
Any clause in a tenancy agreement that ‘permits’ the landlord to visit the property whenever they like, without notice or permission, is an unfair term and considered void.
Landlord’s right to enter in emergencies
The only time a landlord has the right to access their rental property without permission is in an emergency. This is when there is a threat to the structure of the property or to life, such as:
- A fire in the property
- Structural damage that requires urgent attention
- Water flowing from the building
- A strong smell of gas
- Suspicion of a violent or criminal incident
- A serious concern for welfare
In these circumstances, an agent or landlord must be behaving ‘reasonably’ if they enter a property. They must be mindful of how they can justify their access should it be challenged later by the tenant.
As always, it is wise to obtain photographic evidence of any issue, make clear notes, log any police incident number, and get signed statements from any contractor present.
Unless it is an emergency, landlords or letting agents should always contact the tenant and give at least 24 hours’ written notice before any property visits.
What if my tenant refuses access to the property?
Sometimes a tenant may refuse access to the property. If it’s because the time or date doesn’t work well for them, you can rearrange it for a suitable time.
If a tenant doesn’t respond to your written notice, try contacting them again through a different method, e.g. calling them.
If a tenant has outright refused access or is still ignoring your attempts to get in touch, the best thing to do is to provide further information on the reason for visiting. For example, if it’s a gas safety check, you should inform the tenant in writing that:
- The gas check or repair work is for their own safety and possibly the safety of others
- They can be liable for the cost of any cancelled appointments
- They will be liable if they suffer injury or damage because of a fault in the property that the landlord was not able to fix
- They will also be liable if the property deteriorates because the landlord was not able to repair a fault
- They are risking their tenancy
Formal action for a landlord to gain property access
When every other avenue has been exhausted, and tenants are unreasonably refusing entry, the next step is to write a letter informing the tenant that you will begin a more formal route to gain access.
It’s unlikely that the situation will escalate to this level, but if it does, you should start by contacting your local environmental health department or the Health and Safety Executive . Explain the issue and ask them to contact the tenant to reiterate the importance of allowing access. In most cases, the tenant will allow access when the local council gets involved.
The least preferred strategy is to take legal action using the following three options:
- Apply for an injunction to allow access. This is quick but involves paying a court fee. Judges are usually sympathetic to landlord requests so long as they can prove they have taken all reasonable steps to resolve the matter out of court.
- Serve Section 21 notice seeking possession.
- If the tenancy is still within the fixed term, then it may be necessary to go for a court hearing under Section 8, citing Ground 12: any obligation of the tenancy has been broken. Although a discretionary ground, a judge is likely to be sympathetic if they are convinced the motivation is genuine.
What if a landlord enters the property without notice or permission?
In England and Wales, it is illegal for a landlord to enter their rental property without at least 24 hours’ notice to the tenant unless it is an emergency.
If a landlord does enter the property without notice and permission, this is a violation of the tenant’s right to quiet enjoyment and The Housing Act 1988 . In this circumstance, landlords could be prosecuted for harassment.
The Protection from Eviction Act 1977 states that a landlord will be “guilty of an offence” if their actions are “likely to interfere with the peace and comfort of the residential occupier or members of their household”.
Entering the property without permission, or trying to organise an excessive amount of visits, such as unnecessary monthly inspections, can be considered harassment.
Have you had issues with property access?
Fundamentally, a tenant has the right to exclude others from the property, including the landlord. Besides an emergency, any access to the property will need to be with the tenant’s consent. This is easily achieved if the tenant and landlord (or acting agent) have a clear line of communication and the suggested times are reasonable.
Have you had any issues regarding a landlord’s right to access and tenant consent before? Let us know in the comments.
Subscribe to our newsletter
The latest industry updates by email including legislation and tax advice to help you manage your rental property.
How much rent could I earn from my property?
Click to get a free rental valuation and call to discuss the next steps to letting out your property.
- How to Rent Guide
- Gas Safety Check Regulations
- Deposit Protection Schemes
- Landlord Inventories
- Electrical Safety Inspections (EICRs)
- Landlord Legionella Risk Assessments
- Property Photography Guide
- Frequently Asked Questions When Renting
- Company News
- Landlord Advice
- Property Finance
- Property Law
- Property News
- Rental Process
- Tenant Advice
- Uncategorised
Airbnb vs renting: which is more profitable for landlords and property investors.
Reading Time: 6 minutes When you’re investing in property, you want to spend your money wisely and get a worthwhile return. The property market is not for the faint-hearted, especially when it comes to […]
Lucy Cromwell
Landlord electrical safety – when did you last check your wires.
Reading Time: 6 minutes According to Electrical Safety First, a UK based charity, electricity is the cause of more than 20,000 fires a year – almost half of all accidental UK house fires. With […]

Matthew Daines
Getting started as a landlord.
Reading Time: 3 minutes The UK’s property rental sector has seen phenomenal growth since the year 2000, and there are now around 5.4mn privately rented properties and households. This sector growth has doubled during […]
Shannon Hall
What should you do if an eclipse viewer ends up on your property without permission?

The impact the upcoming solar eclipse could have on northern Vermont is hard to imagine, with astronomical aficionados expected to swarm the state looking for the best spot to watch the moon black out the sun on April 8.
Northern Vermont will be in the path of totality − a narrow slice of geography with an optimal view of the moon perfectly in line with the sun. Some projections say the Green Mountain State could swell by 250,000 people over the span of about four days, increasing the population by 40%.
With a quarter-million people wandering around, it's not unreasonable to think a few of them could wind up uninvited on private property in search of eclipse-viewing nirvana − maybe your private property. What should you do?
Put out no trespassing signs. If that doesn't work ask them to leave.
Burlington Police Deputy Chief Wade Labrecque encourages residents to put out "no trespassing" signs ahead of the event that are signed and dated by the owner, according to Sarah Hernandez Timm, BPD's public information and community engagement officer.
"And if someone is breaking into a resident’s house, residents should call the police," Timm added in an email.
How about if someone isn't breaking into your house, but is ignoring your no trespassing signs and is on your property? What should you do then?
Dispatcher Savannah Robson of the Burlington Police Department said you should first politely ask the person or persons to leave. If that doesn't work, you can tell the person they're trespassing, and believe it or not, ask them to sign a Notice of Trespass .
Now, it's not hard to imagine a circumstance where the person trespassing is not amendable to signing a form acknowledging they're trespassing. In that case, Robson said, you don't need that signature before you call the police, as long as you tell the person they're trespassing.
"If they still refuse (to leave) we'll send an officer, if we have one," she said.
Note that the Burlington Police Department is short on officers
With her caveat, "if we have one," Robson is acknowledging that as of the end of 2023, the Burlington Police Department had 58 active duty officers , just over half of its historic average pre-2020, when the Burlington City Council voted to reduce funding and cut the number of officers in response to the death of George Floyd, a black man who was murdered by a white police officer in Minnesota.
More: What to know about the 2024 solar eclipse in VT: It's expected to bring 250,000 tourists
"Unfortunately that's the case, we are not up to full staffing," Robson said.
It's important to remember too that you have to be on your property when you call police about a trespasser, according to Robson. In the case of an apartment building, the manager, or someone the manager has designated, needs to be there.
If you're in immediate danger, you can call 911, but if the trespasser is just being annoying, Robson said to call dispatch at 802-658-2700, ext. 9.
Contact Dan D’Ambrosio at 660-1841 or [email protected]. Follow him on X @DanDambrosioVT.

IMAGES
VIDEO
COMMENTS
In these states, recording an encounter with a physician would not be allowed without the physician's consent (Elwyn G, et al. JAMA. 2017;318:513-514). Even if only one party's consent is needed to record a conversation under state law, other policies and protections may limit recording of physician visits.
They can take photos, shoot video, play music, and access the Internet. They can also be used to record healthcare provider appointments without the knowledge of the practitioner. Secretly recording clinical encounters may sound sneaky, but in 39 of 50 states, it's legal. Furthermore, research shows that recorded clinical encounters can be ...
In addition, recording the visit may inhibit the flow of information between the clinician and patient. Patients may be less likely to discuss sensitive health issues for fear an outside party might hear the recording. A patient recording a visit without the clinician's permission can result in a loss of trust, which is the basis of a strong ...
If you are doctor, there is a good chance that at least one of your last 10 patients recorded their visit—either with or without permission. This "new reality" has some doctors and health care ...
In summary, although doctors may have legal permission to record conversations without patient consent in certain states, they must exercise extra caution in adhering to ethical guidelines and federal laws like HIPAA. These guidelines and laws prioritize protecting patient privacy and confidentiality. It is always recommended for healthcare ...
But recording without permission might be illegal depending on where you live, ... The digital doctor's visit: Enormous potential benefits with equally big risk. May 14, 2018.
If a patient records a visit without the doctor's permission, that can result in a loss of trust, which is the basis of a strong physician-patient relationship. Only about a dozen states nationwide prohibit electronic recordings done without the explicit consent of all participants in the encounter. It is important to know the specific laws ...
For many clinicians, it is possible that some of their patients are recording their office visit, with or without permission. In a cross-sectional survey administered to the general public in the United Kingdom, 19 of 128 respondents (15%) indicated that they had secretly recorded a clinic visit, and 14 of 128 respondents (11%) were aware of someone covertly recording a clinic visit. 1 Because ...
Is it OK to record your doctor visit without permission? Posted at 10:56 PM, Aug 11, 2017 . and last updated 2017-08-14 10:53:57-04. Christine Martinello is no stranger to the doctor's office.
Covered entities typically need consent under HIPAA's privacy rule to disclose medical records. They cannot share medical information without permission. HIPAA defines covered entities. They include insurance companies, pharmacies, and health care professionals. Covered entities also include HMOs and government health plans, such as Medicaid.
For physicians, there's a good chance at least one of your last 10 patients recorded their visit, with or without permission, according to research from the Dartmouth Institute for Health Policy ...
Only in these states can patients legally record an office visit without their doctor's consent and vice versa. The authors said 39 states and Washington, D.C., follow the one-party consent rule ...
prohibiting international travel of the child, specifying the beginning and end dates of visits, ... Also, a passport may be issued without consent of both parents or legal guardians if the applicant for the passport can establish that consent of both parents is not required under federal law (22 U.S.C. 213n and 22 C.F.R. 51.28). ...
That doesn't work for us. We will let you know when we will allow visitors and it will not be until at least 2/4 weeks after birth. Stop making arrangements to visit without asking us - the answer is still no. ILs can rent the house across the street for a month if they wish - you cannot stop them.
Free Minor Travel Consent Form. A minor travel consent form is a legal document, signed by a child's parents and/or legal guardians, giving permission for the child to travel with another adult. Any time a child travels abroad without both parents and/or legal guardians, U.S. Customs and Border Protection requires the child to have this written ...
The patient or the POA *HAVE* agreed to home. health. There are PLENTY of nurses that will not go to the patient's house if. unable to reach the patient by phone, and that is perfectly fine as. far as I'm concerned. However, again, the mere act of going to the. house is not a HIPAA violation. Susie2310.
Many states have laws regarding out-of-state travel to prevent parental kidnapping. How these rules apply to you depends on: Your type of custody; Whether you are the custodial or noncustodial parent; Your marital status; Alternatively, the court or parents can specify in a parenting plan whether parents need permission to take the child out of ...
A consent letter should be used for all cross-border travel when a child is travelling: alone. with only 1 parent or guardian. in the care of friends or relatives. with a group, such as a sports, school, musical or religious group. This includes day trips and travel where a child will be with only 1 parent for part of a trip.
Children traveling to the U.S. All children, including infants, must have their own travel documents such as a passport or document from a Trusted Traveler Program to enter the U.S. If you travel or are going to travel with a child, consider taking the following documents: If the child is traveling with only one of their custodial parents, they ...
Antarctica is not off limits or guarded, as military activity is prohibited under the Antarctic Treaty. However, you still need permission to visit Antarctica from your own country or the country you will pass through ( tour operators usually handle this on your behalf). Without permission, it's unlikely that you'll be allowed to board ...
In England and Wales, it is illegal for a landlord to enter their rental property without at least 24 hours' notice to the tenant unless it is an emergency. If a landlord does enter the property without notice and permission, this is a violation of the tenant's right to quiet enjoyment and The Housing Act 1988.
Assessors need the permission of a homeowner to actually enter the property. This permission can be express or implied. For example, Wisconsin is considering a law to allow assessors the right to be free from trespassing charges as long as they act reasonably. Assessors should not stay longer than it takes to do their job, and they should work ...
Period of travel Name of foreign countries visited Purpose PROFORMA FOR TAKING PRIOR PERMISSION BY GOVERNMENT SERVANTS FOR PRIVATE VISITS ABROAD Part A — To be filled by the Government servant applying for visit abroad I. Name and Designation 2. Pay 3. Ministry/ Department 4. Passport No. 5. Details of private foreign travels to be undertaken:
Contact Dan D'Ambrosio at 660-1841 or [email protected]. Follow him on X @DanDambrosioVT. Up to 250,000 people are expected to travel to northern Vermont for the eclipse. Property owners may ...
Visit. Save. From . instagram.com ... 2023 Please do not recreate without permission ☺️ #macrame #macrameart #macramelight #macramelamp #macramelove #macramependantlight #macramependantlamp #macrameflower #functionalmacrame #macramedesign" ... Macrame Plant Hanger Without Tassel\ Ceiling Plant Hanger\ Macrame Plant Holder\ Boho Plant Hanger ...