November 17, 2020

The human skull can be grossly divided into a movable and an immovable part. The movable part is formed by the lower jaw called the mandible. The rest of the skull forms the immovable portion. These two parts of the skull are connected by a joint near the ear. This joint is the temporomandibular joint (TMJ).
The TMJ has three main parts. A temporal part, that is the part of the immovable portion of the skull. The temporal bone is a depression that receives the condyle. The condyle is a part of the mandible that makes the primary movements of the lower jaw. A disc located between the temporal bone and the condyle helps in the range of movements. The smooth movements of the articular disk are possible because of a fluid called the synovial fluid. This fluid acts as a lubricant, as a result of which our lower jaw can move freely during speech, chewing, etc.
The movements produced by the TMJ are protrusion (moving the lower jaw forward), retrusion (moving the lower jaw backward), elevation (mouth closure), depression (mouth opening), lateral excursion (side to side). In this article, we would be focusing on lateral excursion.
Simply put, lateral excursion is when the mandible moves to one side. But the mechanism behind this is not as simple as it sounds. The mandible is capable of two movements if we take the condyle as the hinge: rotation and translation. Imagine a vertical and horizontal axis passing through the condyles. The movement of the mandible with respect to the vertical axis is called rotation and with respect to the horizontal axis it is translation.
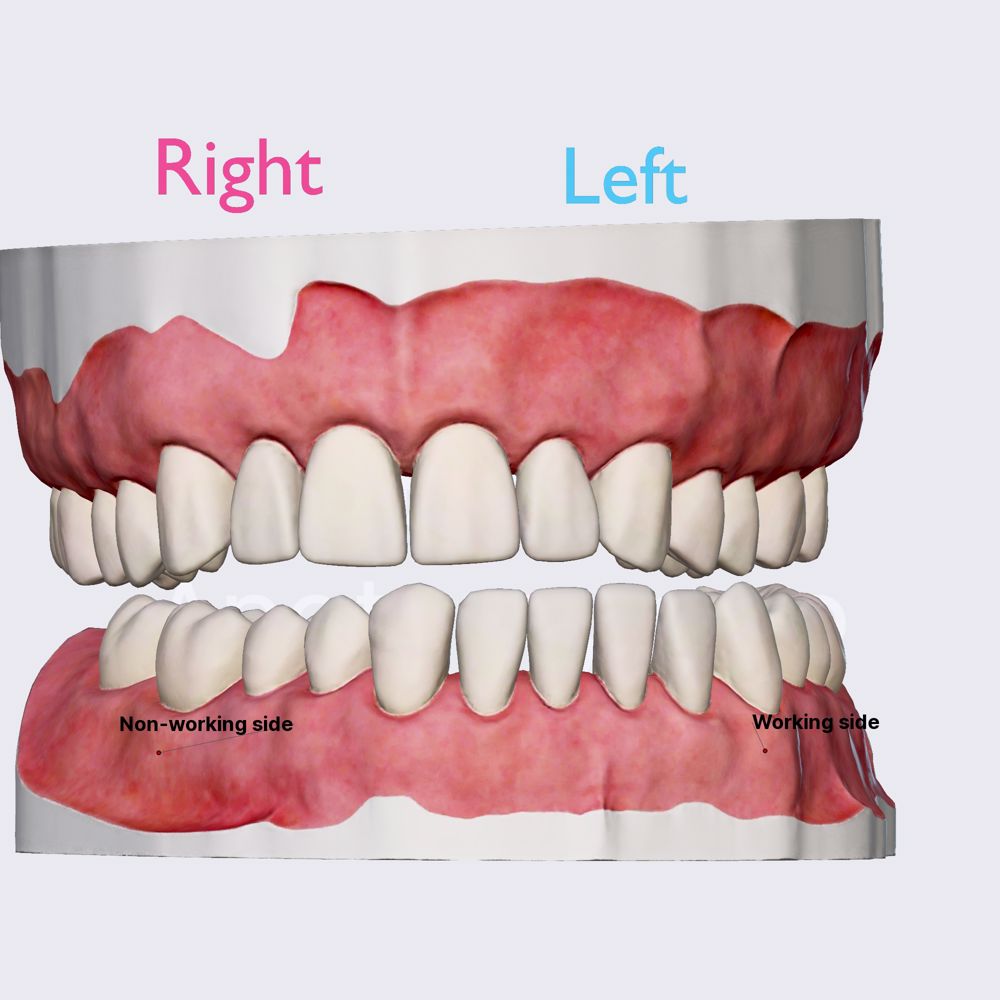
The forward movement of the mandible is a translatory motion. The sideways movement is a rotational motion. In lateral excursion, both these motions take place simultaneously. Let us understand this movement with an example. Imagine you want to move your lower jaw to the left side. This means that both the condyles would have to move towards the left. Since the jaw has to be moved to the left, the left condyle will rotate in the desired direction. In our case, the left side is the working side. The mandible is a single bone, if the left condyle moves, the right condyle will be also stretched towards the left. However, since there are many structures that limit this movement of the right condyle, it will simply move forward in translation. Hence, the right side in our example would be the non-working side.
The working and the non-working side function in conjunction to produce the desired movement. However, lateral excursion is not simply a movement attributed to the condyles. A key role is played by the muscles that are attached to the mandible. These are the muscles that find their origin in the immovable part of the skull are terminate their fibres in the moving mandible. The four muscles are lateral pterygoid, medial pterygoid, temporalis and masseter. Each of these muscles help the mandible to glide forwards, downwards and sideways to make the lateral excursion.
Lateral excursion is one of the key functional movements that helps in chewing. It ensures that we humans do not simply chop down the food by simply opening and closing the mouth but also grind it to make a proper bolus for effective digestion. Lateral excursion is the second key step when we chew our food. Once the mouth opens and the food enters the oral cavity, the jaw moves sideways and grinds the food, closes gradually and finally the teeth meet each other before the mouth comes back in a state of rest.
Lateral excursion might be hampered due to problems in the gnathic system. A locked jaw, tumour, traumatic injury, muscle pain, disk injuries, congenital disorders may contribute to improper or no lateral excursion movement. While some of these disturbances need surgical intervention or pharmacological cover, minor disturbances can be corrected with home techniques focusing on physiotherapy.
Prosthetic treatments that involve fabrication of complete dentures give notable emphasis on lateral excursion. During the fabrication of dentures, the upper and lower canines are made to touch each other as the sideway movement occurs. When they glide over each other, the back teeth are no longer in contact which ensures proper lateral excursion. This is also called canine guidance .
Thus, lateral excursion is one of the vital movements that the mandible can perform considering how the entire surrounding musculature comes into picture for normal functioning.

Partners and Sponsors

- Advertising with DentaGama
- Terms and Conditions
- Privacy Policy
- Cookies Policy
- Reviews Policy
© 2023 DentaGama All rights reserved
- Media Library
- Encyclopedia
- Universities
Unlock with Premium
- Dynamic occlusion: lateral excursion
The dynamic occlusion is the contact that teeth make during movements of the mandible - when the jaw moves side to side, forward, backward or at an angle. In dynamic occlusion, the contacts of the teeth are not points as in static occlusion, but they are described with lines.
- Dental occlusion
- Occlusal relationship
- Temporomandibular joint (TMJ)
- Joint capsule and ligaments of TMJ
- Movements of TMJ
- Static occlusion: centric occlusion
- Occlusion concepts: centric relation
- Angle's classification
- Angle's classification: Class I
- Angle’s classification: Class II, Division 1
- Angle's classification: Class II, Division 2
- Angle's classification: Class III
- Dynamic occlusion: canine guidance
- Dynamic occlussion: protrusion
- Curve of Spee
- Curve of Wilson
- Sphere of Monson
What Is Occlusion?
- First Online: 04 June 2022
Cite this chapter

- Stephen Davies 2
Part of the book series: BDJ Clinician’s Guides ((BDJCG))
1303 Accesses
The aim of this book is to explore the role of Occlusion in Dental Practice.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Smith BGN. Occlusion: 1. General considerations. Dent Update. 1991;18:141–5.
Google Scholar
O’Carroll EO, Leung A, Fine PD, Boniface D, Louca C. The teaching of occlusion in undergraduate dental schools in the UK and Ireland. Brit Dent J. 2019;227:512–7.
Article Google Scholar
Oxford University Press. Shorter Oxford English dictionary. Oxford: Oxford University Press; 1973.
Greenfield S, editor. The private life of the brain: emotions, consciousness, and the secret of self. London: Penguin Books. ISBN-13 978-0-141-00720-5.
Ash MM, Ramfjord SP. Occlusion. 4th ed. Philadelphia: Saunders; 1995. p. 76.
Horner GQ. The effects of positioning variations in transcranial radiographs of the temporomandibular joint: a laboratory study. Br J Oralmaxillofac Surg. 1991;29:241–2.
Posselt UOA. Studies in the mobility of the human mandible. Acta Odontol Scand. 1952;10:19.
Ramfjord SP, Ash MM. Occlusion. 2nd ed. Philadelphia: Saunders; 1971. p. 178.
Ash MM, Ramfjord SP. Occlusion. 4th ed. Philadelphia: Saunders; 1995. p. 84–5.
Davies SJ. Malocclusion—a term in need of dropping or redefinition? Br Dent J. 2007;202:12.
Gremillion HA. Relationship between TMD and occlusion. J Evid Base Dent Pract. 2006;6:43–7.
Moufti MA, Lilico JT, Wassell R. How to make a well-fitting stabilization splint. Dent Update. 2007;34:398–408.
Wise M. Occlusion and restorative dentistry for the general dental practitioner. Br Dent J. 1982;152:319–20.
Davies SJ. Occlusion in restorative dentistry: conformative, re-organised or unorganised. Dent Update. 2004;31:334.
Davies SJ, et al. Occlusion: is there a third way? A discussion paper. Br Dent J. 2021;321:160–2.
Download references
Author information
Authors and affiliations.
Specialist in Restorative Dentistry, Lecturer in Occlusal and Temporomandibular Studies, Division of Dentistry, Faculty of Biology, Medicine and Health, University of Manchester, A Lead Clinician, Temporomandibular Disorder Clinic, University Dental Hospital of Manchester, Manchester, UK
Stephen Davies
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Stephen Davies .
Rights and permissions
Reprints and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Davies, S. (2022). What Is Occlusion?. In: A Guide to Good Occlusal Practice. BDJ Clinician’s Guides. Springer, Cham. https://doi.org/10.1007/978-3-030-79225-1_1
Download citation
DOI : https://doi.org/10.1007/978-3-030-79225-1_1
Published : 04 June 2022
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-79224-4
Online ISBN : 978-3-030-79225-1
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Registered Nurse RN
Registered Nurse, Free Care Plans, Free NCLEX Review, Nurse Salary, and much more. Join the nursing revolution.
Protrusion, Retrusion, and Excursion Anatomy
In this anatomy lesson, I’m going to demonstrate protrusion, retrusion, and excursion , which are special body movement terms in anatomy that refer to forward (anterior), backward (posterior), or side to side movements.
Protrusion in Anatomy
Protrusion refers to the movement of a structure in an anterior (forward) direction. In fact, the word protrude means “projecting something forward.”
I call protrusion the kissing movement because it occurs when you pucker your lips like you’re going to give someone a kiss or stick out your tongue. Moving the mandible (lower jaw) forward is also an example of protrusion.

Retrusion in Anatomy
Retrusion is the opposite of protrusion. It refers to the movement of a structure in a posterior, or backward, direction. Putting your tongue back in your mouth, moving the lips back, or moving the mandible back are all examples of retrusion in anatomy.

Excursion in Anatomy
Finally, we have excursion , which refers to the side-to-side movement of the lower jaw (mandible). If you’ve ever heard of a character named Ernest P. Worrell, then you’ve definitely seen the excursion movement. He’s the character in those movies such as Ernest Goes to Camp, Ernest Goes to Jail, etc. When Ernest saw something nasty, he’d move his jaw back and forth and say, “Ewwww.”

Excursion can occur in either direction, and anatomists use directional terms to specify the type of excursion. When the mandible moves to either the left or right, it’s moving away from the body’s midline, so it’s called lateral excursion . When the mandible moves closer to the midline of the body, it’s called medial excursion .

Protrusion and Retrusion vs Protraction and Retraction
What about protraction and retraction ? Some anatomy textbooks will refer to the forward movement of the mandible, lips, or tongue as protraction (instead of protrusion), and the backward (posterior) movement will be called retraction (instead of retrusion). The terms are sometimes used interchangeably, so use whatever method your anatomy professor suggests (they give you the grade, not me!).
However, some anatomists today use protraction and retraction to refer almost exclusively to the scapulae, as it is a combined movement (protraction is anterolateral, and retraction is posteromedial). In contrast, protrusion and retrusion are more of an anterior/posterior movement. Then again, some anatomists prefer not to use protraction and retraction at all, even when describing shoulder blade movement.
Protrusion, Retrusion, and Excursion in Healthcare
Healthcare professionals use protrusion, retrusion, and excursion when documenting, performing assessments on patients, or treating disorders. For example, in her head-to-toe assessment , Nurse Sarah asked me to stick out my tongue (an example of protrusion), to assess cranial nerve twelve .
In addition, something called a mandibular protrusion test (MPT) is sometimes used by anesthesiologists to predict difficult airways in patients.
Free Quiz and More Anatomy Videos
Take a free protrusion vs retrusion quiz to test your knowledge, or review our protrusion vs retrusion video . In addition, you might want to watch our anatomy and physiology lectures on YouTube, or check our anatomy and physiology notes .
Please Share:
- Click to print (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to share on Pocket (Opens in new window)
- Click to share on Telegram (Opens in new window)
Disclosure and Privacy Policy
Important links, follow us on social media.
- Facebook Nursing
- Instagram Nursing
- TikTok Nurse
- Twitter Nursing
- YouTube Nursing
Copyright Notice
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 08 September 2001
What is occlusion?
- S Davies 1 , 2 &
- R M J Gray 3
British Dental Journal volume 191 , pages 235–245 ( 2001 ) Cite this article
23k Accesses
39 Citations
5 Altmetric
Metrics details
In this part, we will discuss:
What 'occlusion' is
Why occlusion is important
The significance of 'ideal occlusion'
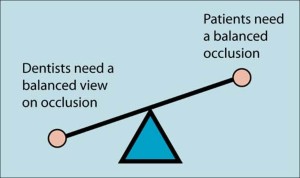
The aim of this series of papers is to explore the role of occlusion in dental practice. The range of opinion in the dental profession as to the importance of occlusion is enormous. 1 It is very important that the profession in general and practising dentists in particular have a balanced view of occlusion. This is more important than every patient having a balanced occlusion. The fact that the study of occlusion is characterised by extremes makes it confusing and possibly difficult for individual dentists to find a philosophy which is in line with contemporary good practice supported by evidence from practice-based research.
You have full access to this article via your institution.
Similar content being viewed by others
What is occlusion? Part 1

What is occlusion? Part 2

Occlusion: is there a third way? A discussion paper
'Occlusion' There is no escape Dentists cannot:
without being involved in occlusion
At one end of the spectrum are dentists who believe that they can go through their working lives with scant regard for their patients' occlusion. They seem to believe that essentially they can conduct their practice ignoring the occlusal consequences of the treatments that they perform daily. Whereas all dentists know of the importance of the good marginal adaptation of their restoration to the health of the adjoining dental and periodontal tissues, some dentists do not appreciate the potential consequences of poor occlusal contact to the opposing teeth and their supporting structures. This is bizarre given the fact that very few dental treatments do not involve the occlusal surfaces of teeth.
Conversely there is a body of opinion that considers occlusion to be such a central pillar in our working lives, and to be of such systemic import to the well being of our patients, that 'occlusion' takes on an almost mystic importance and attracts a cult like devotion ( Fig. 1 ). This can lead some dentists to advocate occlusion as being the key to resolving or preventing a range of disorders far removed from the masticatory system, for example prolapsed lumbar discs. Often such enthusiastic fervour is associated with a didactic prescription of 'occlusal rules' which must be adhered to in the treatment of every patient.
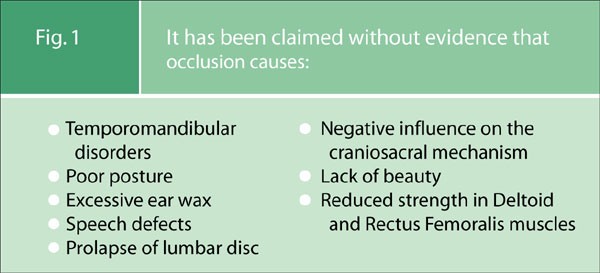
It has been claimed without evidence that occlusion causes:
The danger is that both of these approaches leads to inappropriate levels of patient care; patients suffer through either over or under treatment.
It is not surprising that these two extreme views co-exist so easily within a thinking profession because the one appears to provide the justification for the other. The 'occlusion doesn't matter' group probably justify their reluctance to become 'involved in occlusion' on the grounds of what they perceive to be the exaggerated and unsubstantiated claims of the group who believe occlusion to be the central pillar of holistic care. This congregation of opinion in turn may be so frustrated by the apparent disregard of the study of occlusion that they are led to 'gild the lily' by overstating the importance of occlusion and then in the absence of what they perceive to be an inability 'to see the obvious' they go on to lay down rules.
It is the objective of this series of papers to explore the role of occlusion in dental practice in a manner based on reason. There is good and bad practice in occlusion as in other aspects of clinical dentistry: we wish, therefore, to establish the concept of Good Occlusal Practice, which is applicable to all disciplines in dentistry.
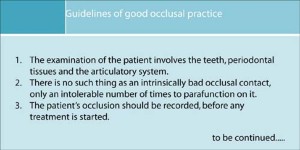
Guidelines of good occlusal practice
These should be guidelines not rules.
All patients are different, reacting to similar stimuli in different ways. So the detail of a patient's individual needs can and should be left to the individual clinician. These Guidelines of Good Occlusal Practice should appear to be common sense and, upon reflextion, we hope that the reader will agree that they are obvious. We argue that any fog that has descended over this subject must be cleared, because no practising dentist can care well for their patients without having regard for good occlusal practice.
The importance of occlusion in dental practice
'Occlusion' = Contacts between teeth
Occlusion can be defined very simply: it means the contacts between teeth.
Before describing the significance of the different ways in which occlusal contacts are made occlusion needs to be put into context.
The masticatory (or stomatognathic) system ( Fig. 2 ) is generally considered to be made up of three parts: the Teeth, the Periodontal Tissues, and the Articulatory System.
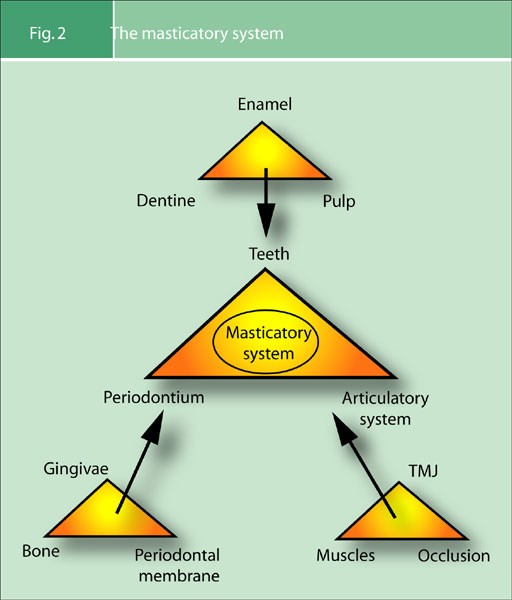
The masticatory system
It is a common criticism of dentists that our dental schools ignore the third part of the masticatory system, the articulatory system, in their teaching. It appears that dentists feel that their time at university did not prepare them adequately in this area; and this view seems to be the case worldwide. The undergraduate dental education must, however, by necessity concentrate initially on the first two parts of this triumvirate, because the dental schools must produce newly qualified dentists who are able to treat patients. Only once the dental undergraduate has an understanding of the diseases that affect the dental and periodontal tissues (parts 1 and 2 of the masticatory system) can the schools start to allow the student to treat patients. So there is justification for the study of the articulatory system being considered to be the third area of study from a chronological point of view. But because of the inescapable fact that almost all dental treatment has an occlusal consequence, it is wrong to consider the study of the articulatory system to be less important than the first two parts of the masticatory system. Given the increasing quantity of knowledge to be amassed in the modern undergraduate course, it may be that those responsible for setting the dental undergraduate curriculum will not be able to cover the articulatory system as they would wish. Now that there is a universal acceptance of the need for continuing education, it may be more realistic to consider a comprehensive study of the articulatory system as the first mandatory element of a post graduate dental education. But the articulatory system is the biomechanical environment in which dentists provide treatment. Although it maybe, by necessity, the last to be learnt it is not less important than the other parts of the masticatory system.
Is the articulatory system a true system?
( Fig. 3a , b )
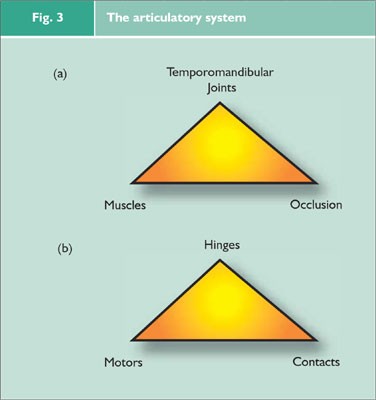
The articulatory system
A system is defined as: 'An assemblage that is connected or interdependent, so as to form a complex unity.'[OED] The articulatory system meets these criteria, so the answer to this question is: Yes.
In this system one can imagine the temporomandibular joints as the hinges, the masticatory muscles as the motors and the dental occlusion as the contacts ( Fig. 3b ).
When viewed in mechanical terms ( Fig. 3b ) it is clear that the elements of the articulatory system are inescapably connected. Furthermore, it can be argued that they are obviously interdependent because a change in any part will clearly affect the other two parts ( Fig. 4a ), but this effect will not necessarily be adverse.
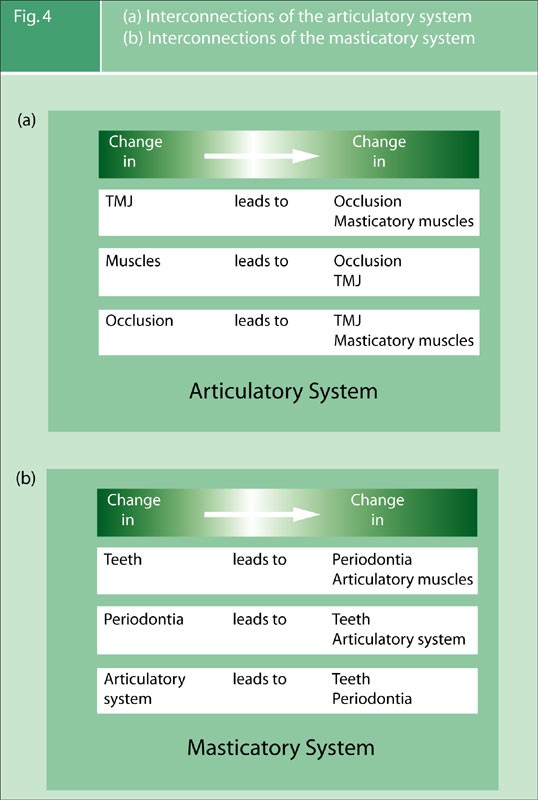
(a) Interconnections of the articulatory system (b) Interconnections of the masticatory system
The same sort of analysis of the interconnection within the masticatory system can be made ( Fig. 4 b ).
The importance of 'occlusion' in dental practice is based primarily upon the relationships that it has within these interconnected biomechanical systems. When one considers how almost all forms of dental treatment have a potential for causing occlusal change, the need to establish what constitutes good occlusal practice is overwhelming and obvious.
Analysis of occlusion
Having stated that occlusion simply means the contact between teeth, the concept can be further refined by defining those contacts between the teeth when the mandible is closed and stationary as the static occlusion, and those contacts between teeth when the mandible is moving relative to the maxilla as the dynamic occlusion.
Static occlusion
The first essential question when considering a patient's static occlusion is: 'Does centric occlusion occur in centric relation?'
This question will be clarified after defining terminology, which has been a 'red herring' and has been the cause of enormous and sometimes acrimonious debate. We, also, have preferred terms, but do not feel that they are important.
Centric Occlusion (CO) can be described as the occlusion the patient makes when they fit their teeth together in maximum intercuspation. Common synonyms for this are Intercuspation Position (ICP), Bite of Convenience or Habitual Bite. It is the occlusion that the patient nearly always makes when asked to close their teeth together, it is the 'bite' that is most easily recorded. It is how unarticulated models fit together. Finally, it should be remembered that it is the occlusion to which the patient is accustomed ie the habitual bite.
The word 'Centric' is an adjective. It should only be used to qualify a noun. Centric what?
Centric Relation (CR) is not an occlusion at all. CR has nothing to do with teeth because it is the only 'centric' that is reproducible with or without teeth present. Centric Relation is a jaw relationship: it describes a conceptual relationship between the maxilla and mandible. All attempts to lay down rigid definitions of centric relation are plagued by the fundamental difficulty that there is no sure or easy way of proving that the locating criteria have been achieved.
Centric Relation has been described in three different ways: anatomically, conceptionally, 2 and geometrically.
Centric Relation can be described as the position of the mandible to the maxilla, with the intra-articular disc in place, when the head of the condyle is against the most superior part of the distal facing incline of the glenoid fossa. This can be paraphrased as uppermost and foremost ( Fig. 5 ).

Functional anatomy of the temporomandibular joint
This is subject to debate. Some clinicians prefer the idea that centric relation occurs in an 'uppermost and midmost' position within the glenoid fossa; whereas very few people now support the idea that it is in an 'uppermost and rearmost' position. There is support for the uppermost and foremost hypothesis from a study of anatomy: the bone and fibrous articulatory surfaces are thickest in the anterior aspect of the head of the condyle and the most superior aspect of the articular eminence of the glenoid fossa. This is, however, of only academic interest and not of clinical significance as there is no reliable simple means of determining the exact position of the head of the condyle within the glenoid fossa.
Centric relation can be described as that position of the mandible relative to the maxilla, with the articular disc in place, when the muscles that support the mandible are at their most relaxed and least strained position. This description is pertinent to an understanding of 'ideal occlusion'. This definition supports the concept of a 'qualitative' relationship between a jaw position and another element of the articulatory system.
Geometrical
Centric Relation can be described 'as the position of the mandible relative to the maxilla, with the intra-articular disc in place, when the head of the condyle is in terminal hinge axis'.
In order to understand what this frequently used definition means it is easier, initially, to think about one side of the mandible only. The mandible opens by firstly a rotation of the condyle and then a translation which is downwards and forwards. Therefore, when the mandible closes the the terminal closure is purely rotational. At this phase of closure the mandible is describing a simple arc, because the centre of its rotation is stationary. This provides the 'terminal hinge point' (of rotation) of one side of the mandible; but because the mandible is one bone with two connected sides these two terminal hinge points are connected by an imaginary line: the terminal hinge axis. This axis is, therefore, envisaged by imagining the stationary, centres of rotation of each condyle whilst the mandible is moving only in the rotational phase of movement. It is the fact that the mandible is describing this simple arc, when the heads of condyle are in the terminal hinge axis which is of the most clinical significance. This will be discussed later, when the techniques for finding centric relation are presented.
Significance of Centric Relation
There may be arguments about the exact position of centric relation and on how that position is clinically best found. There is, however, a broad agreement between dentists who have studied this subject that there exists a reproducible position of the mandible relative to the maxilla, and that this position is reproducible irrespective of the guidance that the occlusal surfaces of the teeth may provide. Patients with no teeth still have a centric relation. Furthermore there is inter- and intra-operator reliability in finding it.
'Freedom in centric'
'Does Centric Occlusion Occur in Centric Relation?' This is an essential question.
Another aspect of the static occlusion is the presence or absence of 'freedom in centric', this is also known as 'long centric'.
As previously stated the word centric is an adjective and so strictly it should never be used without a defining noun. So this long established term would better read: Freedom in centric occlusion or long centric occlusion. Freedom in centric occlusion occurs when the mandible is able to move anteriorly for a short distance in the same horizontal and sagittal plane while maintaining tooth contact ( Fig. 6b ). Alternatively there will be no freedom in centric occlusion if either the front teeth or the posterior occlusion do not allow this horizontal movement ( Fig. 6a ).
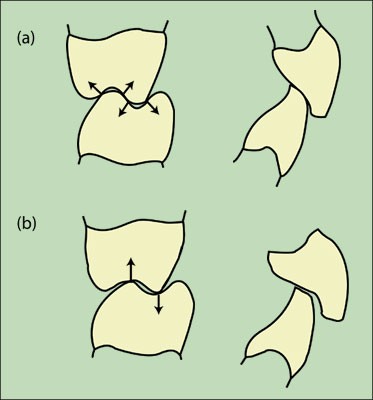
(a) No freedom in centric occlusion (b) Freedom in centric occlusion
An easier way of imagining Freedom in Centric Occlusion is to state that if the front teeth hit together as hard or harder than the back teeth, then there is no freedom in that centric occlusion. Two common examples of occlusions that may not have this freedom are firstly those which have an Angles Cl II div (ii) incisor relationship and secondly when anterior crowns have been provided with palatal surfaces which are too thick.
In Figure 6a , there is no freedom in centric occlusion as the occlusal contacts 'lock in' the mandible to the maxilla. Whereas in Figure 6b the mandbible can move anteriorly, for a short distance, in the same sagital and horizontal plane.
Other aspects of the static occlusion that can be described are the extent of the posterior support, the Angle's classification of the incisor relationship together with measurement of the overbite and overjet, and the existence of any cross bites.
The answer to the question: 'Does Centric Occlusion occur in Centric Relation?' is therefore essential, because it describes the relationship of the mandible to the maxilla when the teeth fit together.
Dynamic occlusion
Ideal Occlusion Q. Who or what is it ideal for? Posterior Interference Q. Who or what is it interfering with?
The dynamic occlusion refers to the occlusal contacts that are made whilst the mandible is moving relative to the maxilla. The mandible is moved by the muscles of mastication and the pathways along which it moves are determined not only by these muscles but also by two guidance systems.
The posterior guidance system of the mandible is provided by the temporomandibular joints. As the head of the condyle moves downwards and forwards the mandible is moving along a guidance pathway which is determined by the intra-articular disc and the articulatory surfaces of the glenoid fossa, all of which is enclosed in the joint capsule.
If teeth are touching during a protrusive or lateral movement of the mandible then those (touching) teeth are also providing guidance to mandibular movement. This is the anterior guidance and this is provided by whichever teeth touch during excentric movements of the mandible.
No matter how far back these teeth are they are anterior to the temporomandibular joints and so a patient with a severe anterior open bite would still always have anterior guidance of their mandible, it could, for instance be on the second molars. Therefore, despite the ambiguity of the word 'anterior' in the term anterior guidance, it does not mean that the anterior guidance of the mandible is always on the front teeth. This definition differs from that given in some restorative textbooks, when the term anterior guidance is used to describe only those anterior guidances which involve front teeth.
Anterior guidance may be further classified. 'Canine guidance' refers to a dynamic occlusion that occurs on the canines during a lateral excursion of the mandible. A canine protected occlusion refers to the fact that the canine guidance is the only dynamic occlusal contact during this excursive movement.
Group function. In this type of anterior guidance the contacts are shared between several teeth on the working side during a lateral excursion. To qualify for the term 'group function', the contacts would be towards the front of the mouth and the most anterior of the group would be the earliest and hardest contacts. This would contrast with a 'working side interference', which infers a heavy or early occlusal contact towards the back of the mouth during an excursive movement. A 'non working side interference' is an anterior guidance on the back teeth on the non working side during lateral excursion. The working side is the side of the mandible towards which the mandible is moving during a lateral excursion. The non working side is the side of the mandible away from which the mandible is moving. These terms can be confusing when considering the temporomandibular joints, because it is the TMJ on the non working side which is moving the most.
One reason why restorative textbooks define anterior guidance as being solely the dynamic occlusal contacts between the front teeth is that it is generally considered to be more ideal if the anterior guidance is on those front teeth. Furthermore, the fact that the word 'interference' is used to describe an occlusal contact between back teeth infers that this anterior guidance is less ideal than others. This introduces the concept of 'ideal occlusion' and this raises two important considerations:
If some occlusions are ideal, for what or for whom are they ideal?
If occlusal contact between back teeth is deemed a posterior interference with what is it interfering?
Ideal occlusion
Let us examine this concept and question whether it has any useful function in routine clinical dentistry.
If two molars on the side from which the mandible is moving during an excursive movement can be deemed to provide a non working side interference, then what are they interfering with?
The posterior guidance of the mandible is provided by the temporomandibular joints. As the head of the condyle translates down the articular eminence of the joint on the non working side (which, paradoxically is the side that is moving the furthest) the mandible is being guided by this joint. If, as this is happening, a posterior maxillary and mandibular tooth hit against each other and because these two posterior teeth are close to the joint, then there is potential for the contact between these two teeth to influence or 'interfere' with the movement of the condyle within that joint. Contrast this with the situation, where the anterior guidance is provided not by posterior teeth which are close to the joint, but by front teeth which are further away; then the likelihood of 'interference' of condylar movement within the non-working side temporomandibular joint is less.
Anterior guidance, therefore, on back teeth, whilst still providing anterior guidance to the mandible, is described as a posterior interference because it may interfere with the posterior guidance system of the mandible, namely the temporomandibular joints. Posterior interferences are, therefore, considered to be a less ideal type of dynamic occlusion; and the term ideal relates to whether or not it is ideal for another part of the articulatory system: the temporomandibular joints ( Fig. 7a ). The anterior guidance provided by front teeth is potentially more ideal for the temporomandibular joints for the simple reason that it is further away from the temporomandibular joints. Consequently it can be argued that one aspect of the occlusion (anterior guidance) may or may not be ideal for another part of the articulatory system.
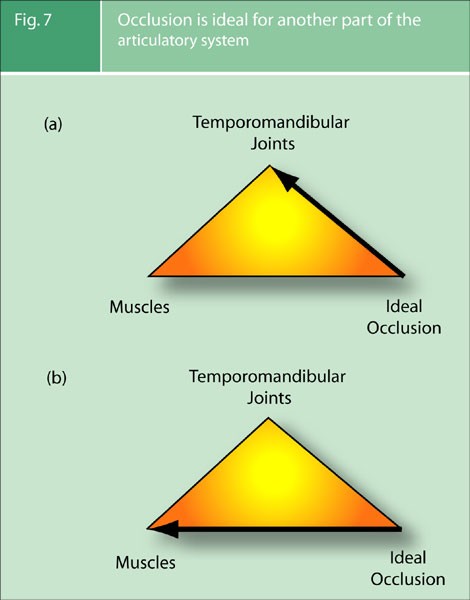
Occlusion is ideal for another part of the articulatory system
It is, also, potentially more ideal if the teeth fit together (centric occlusion), in a position of the mandible relative to the maxilla, with the disc in place, where the muscles supporting the mandible are at their most relaxed and least strained (conceptual description of centric relation). This establishes another criterion of the occlusion that can be considered ideal or not ideal for the other part of the articulatory system, namely the muscles of mastication ( Fig. 7b ).
Definition of ideal occlusion
There is no such thing as an intrinsically bad occlusal contact, only an intolerable number of times for that patient at that time in their life to function or parafunction on it
This is given in established texts as: 3
The coincidence of Centric Occlusion in Centric Relation (CO = CR), when there is freedom for the mandible to move slightly forwards from that occlusion in the same sagittal and horizontal plane (Freedom in Centric Occlusion).
When the mandible moves there is immediate and lasting posterior disclusion (anterior guidance on front teeth)
It is presented in this section only after having considered for what or whom this type of occlusion is ideal, and the justification of why a particular type of occlusion could be considered as being potentially ideal for other parts of the articulatory system.
It is of paramount importance to appreciate that the term 'ideal occlusion' means something quite different from the term 'correct occlusion'. To state that an occlusion is correct or wrong betrays a mechanistic approach to the subject. Patients are not machines and an occlusion can only be judged on the reaction that it produces in the tissues of the system in which it inter-reacts. That reaction will be infinitely variable between individuals and will in some contexts (ie TMD pain) vary within an individual with time.
Guidelines of Good Occlusal Practice should be established because they offer the most prudent way in which to provide dental treatment to one part of the system whilst avoiding a potentially adverse reaction in another.
The importance of ideal occlusion as a concept
1. pretreatment examination and records.
The first and most important reason for defining ideal occlusion is that it gives a benchmark against which patients' occlusion can be measured. This needs to be done before, during and after dental treatment; especially in this increasingly litigious environment.
It is of paramount importance that dentists examine and record the pre-existing occlusion before providing treatment which involves changes to that occlusion. Study models would be a good way of doing this as long as they are mounted on an articulator in centric relation. At least the condylar guidance angles would also need to be correctly set so that the dynamic occlusion was recorded. This is not practicable for the vast majority of dentists. Alternatively and infinitely more easily notes can be made, which describe the patient's occlusion. These notes use criteria of ideal occlusion as a benchmark. To record an occlusion using only the criteria of Angle's classification is of very limited value, whereas to use the benchmark of ideal occlusion is considerable more informative (see Fig. 8 ).
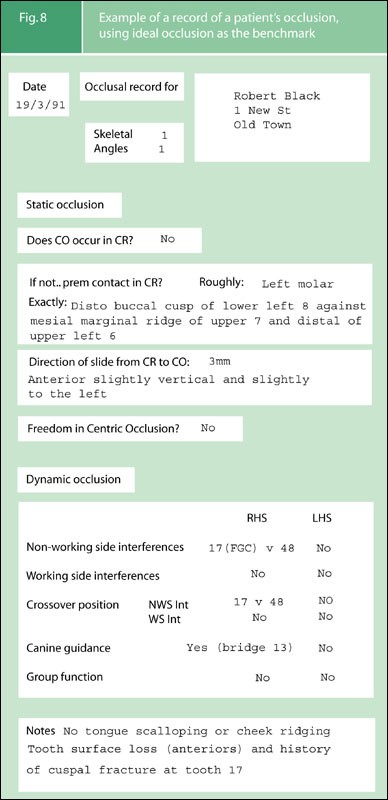
Example of a record of a patient's occlusion, using ideal occlusion as the benchmark
2. Treatment of Pain Dysfunction Syndrome (PDS)
Force > Resistance
Reduces tissue resistance
Causes failure
Promotes pain/dysfunction
The second reason why ideal occlusion is an important concept is found in the long held view that the most important factor in the development of Pain Dysfunction Syndrome (PDS) is 'the individual patient's lack of adaptation to a less than ideal occlusion'. 4 This is not describing a causal relationship between a less than ideal occlusion and PDS, as different patients will have different thresholds of tolerances to occlusion, in fact the same patients have a different tolerance to their occlusions at different times. It is, however, the case that some patients, at some times, do react adversely to their less than ideal occlusions; and this can lead to pain and dysfunction.
For these patients the provision of an ideal occlusion is, therefore, one but by no means the only way of treating the condition. When an ideal occlusion is provided this should always be initially in a temporary and reversible way: that is a stabilisation splint. The indications for the provision of an ideal occlusion in the patient's natural dentition, for the treatment of PDS are very rare.
3. Conformative versus reorganised approach
In providing treatment with an occlusal element, one of the first questions to be decided in the treatment planning stage is whether the aim is to maintain the same occlusion during treatment. If the pretreatment occlusion is to be preserved, then the is described as 'conformative approach'. 5
Some dental treatment, such as most major restorative and all orthodontic treatment, will however, inevitably change the patient's occlusion: this is known as the 'reorganised approach'. It is, therefore, prudent to design an occlusion that is more ideal and so potentially better tolerated by the patient's articulatory system.
Factors determining a patient's reaction to an occlusion
As stated an occlusion can only be judged as being good or bad in relation to the reaction it produces in the patient's tissues. In the same way that the danger of a substance can only be judged in relation to the concentration in which it occurs, a particular occlusal contact should be assessed in relation to the frequency at which it is made.
This is why bruxism is an important consideration in dentistry.
The 'occlusion' means the contacts between the teeth. The application of force from the muscles, through those occlusal contacts, results in load. Whether that load produces damage to tissues will depend on several factors:
The resistance of the tissues and/or restoration.
The magnitude of the force being applied.
The frequency of the force being applied.
The direction of the force being applied.
The number of contacts transmitting that force.
Risk management
The purpose of guidelines of good occlusal practice is to reduce the risk of damage occurring to the interrelated tissues of the masticatory system, and so increase the chances of a healthy function. This will reduce the chances of disease, mechanical failure and dysfunction or pain. Dentists can positively influence these factors as part of their care.
The next section of this work will present the criteria for, and the technique of, a quick and simple occlusal examination. Thereafter, in subsequent sections, we will present the concepts of good occlusal practice in different disciplines of clinical practice. At the conclusion of each section further points will be added to create the cumulative Guidelines of Good Occlusal Practice.
Smith B G N . Occlusion: 1. General Considerations. Dent Update 1991; 18 : 141–145.
Google Scholar
Gray R M J, Davies S J, Quayle A A . Temporomandibular disorders: a clinical approach . pp20 BDJ publications, 1995, 1997.
Ash M M, Ramfjord S P . Occlusion 4th ed.: pp84–85. Philadelphia: Saunders, 1995.
Ramfjord S P, Ash M M . Occlusion 2nd ed.: p178. Philadelphia: Saunders, 1971.
Wise M . Occlusion and restorative dentistry for the general dental practitioner. Br Dent J 1982; 152 : 319–320.
Article Google Scholar
Download references
Author information
Authors and affiliations.
GDP, 73 Buxton Rd, High Lane, Stockport, SK6 8DR
P/T Lecturer in Dental Practice, University Dental Hospital of Manchester, Higher Cambridge St., Manchester, M15 6FH
Honorary Fellow, University Dental Hospital of Manchester, Higher Cambridge St., Manchester, M15 6FH
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to S Davies .
Additional information
Refereed paper
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Davies, S., Gray, R. What is occlusion?. Br Dent J 191 , 235–245 (2001). https://doi.org/10.1038/sj.bdj.4801151
Download citation
Published : 08 September 2001
Issue Date : 08 September 2001
DOI : https://doi.org/10.1038/sj.bdj.4801151
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Comparison of occlusal digital analysis using t-scan in orthognathic surgery with only conventional orthodontic patients.
- R. Manikandhan
- S. Manikandan
- Sathya Shankar
Journal of Maxillofacial and Oral Surgery (2023)

Comparison of two different digital occlusal analysis methods
- Sibel Ezgi Bostancıoğlu
- Abdullah Toğay
- Evşen Tamam
Clinical Oral Investigations (2022)
OCLU-NET for occlusal classification of 3D dental models
- Mamta Juneja
- Ridhima Singla
- Prashant Jindal
Machine Vision and Applications (2020)
Computer simulations of food oral processing to engineer teeth cleaning
- C. G. Skamniotis
- M. N. Charalambides
Nature Communications (2019)
The restorative management of tooth wear involving the aesthetic zone
- S. B. Mehta
British Dental Journal (2018)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

- No menu assigned!
Complete Dentures Occlusal Schemes - Anatomic and Semi-Anatomic Occlusion
Complete Dentures»
Complete Dentures – Occlusal Schemes – Anatomic and Semiamatomic Occlusion — Course Transcript
- 1. 17. Occlusal Schemes – Anatomic and Semi-anatomic John Beumer III, DDS, MS and Michael Hamada DDS Division of Advanced Prosthodontics, Biomaterials and Hospital Dentistry UCLA School of Dentistry This program of instruction is protected by copyright ©. No portion of this program of instruction may be reproduced, recorded or transferred by any means electronic, digital, photographic, mechanical etc., or by any information storage or retrieval system, without prior permission.
- 2. Semi-anatomic Denture Teeth Begin by positioning the appropriate protrusive insert, and check to ensure that the incisal guide pin is set at zero and in contact with the incisal guide table. Protrusive insert Protrusive Inserts Zero setting
- 3. Background – Balanced occlusion Our objective in setting anatomic or semi-anatomic posterior teeth is to create a balanced occlusion. We wish to insure that all the posterior teeth as well as the anterior teeth maintain contact in lateral excursions. To ensure bilateral balance we place an anterior-posterior curve in the arch, called a compensating curve, which is analogous to the curve of Spee in natural dentition. In addition , we place a curve from side to side, the so called curve of Wilson. Semi-anatomic Denture Teeth
- 4. Mark the casts indicating midline, crest of the ridge, and the retromolar pad . These landmarks will be used to check your denture setup. Maxilla Midline Anterior land Mandible Ridge Retromolar pad Cast Landmarks
- 5. Anterior land Cast Landmarks – Maxilla Midline Incisive papilla
- 6. Lines indicating the crest of the ridge Cast Landmarks -Mandible Midpoint of retromolar pad Land Mark on land indicating the midpoint of the retromolar pad
- 7. As previously mentioned (13c, 1a), the wax rim is ideally contoured on the patient and used to mount the upper cast with a facebow transfer record. When the lower cast is mounted on the articulator with a centric relation record the plane of occlusion is readily seen. The three landmarks used to identify the plane of occlusion are: The midpoint of the retromolar pads bilaterally as previously marked on the mandibular cast. The incisal edge of the maxillary central incisors Setting the Maxillary Anterior Teeth
- 8. To set the remaining maxillary anterior teeth a clear glass or plastic slab is positioned on the mandibular record base to represent the plane of occlusion. When setting anatomic posterior teeth we recommend setting the maxillary posterior teeth before the mandibular posterior teeth. To aid in positioning the maxillary teeth, a line is inscribed on the slab indicating the crest of the mandibular ridge. Setting the Maxillary Anterior Teeth Mark indicating midpoint of the retromolar pad
- 9. Setting the Maxillary Anterior Teeth These two lines, inscribed on the plastic plane, indicate the crest of the alveolar ridge. These lines will be used to position the maxillary posterior denture teeth to insure that the mandibular posterior teeth are centered over the ridge. The lingual cusp tips of the posterior maxillary teeth should contact these lines. Lines indicating the crest of the ridge
- 10. Setting the Maxillary Anterior Teeth Soften some baseplate wax and attach some to the ridge lap portion of the other maxillary central incisor and attach it to the record base as shown. Set the lateral incisors and cuspids as shown previously (Section 13c, 1a Lingualized occlusion).
- 11. Setting the Maxillary Anterior Teeth Note the angulations of the anterior teeth in relation to the occlusal plane when viewed in profile. Occlusal plane
- 12. Setting the Maxillary Anterior Teeth “ Toed-in” Position Note how the cervical and incisal edges of the cuspid are aligned vertically (yellow line). The facial surface of the cuspid however, is canted inward and appears “toed in” (red line) due to the prominence of the cervical area of the tooth (yellow arrow). The centrals and laterals are inclined slightly towards the distal.
- 13. The long axis of the premolars should be perpendicular to the occlusal plane and the buccal and lingual cusp tips should touch the occlusal plane. Arranging the premolars in this way insures that the adjacent marginal ridges will be on the same level. This is an important factor when setting the opposing premolars. Setting the Maxillary Posterior Teeth Occlusal plane
- 14. The Maxillary Premolars Setting the Maxillary Posterior Teeth Both the buccal and lingual cusp tips of the maxillary premolars should contact the plane of occlusion. The lingual cusp tips should also contact the line inscribed on the plastic plane indicating the crest of the mandibular ridge. This will ensure that when the opposing mandibular denture teeth are properly positioned and in occlusion, their central fossae will be centered over the mandibular ridge.
- 15. Setting the Maxillary Posterior Teeth The curve of Wilson and the curve of Spee begin in the molar region. The mesial lingual cusp tip of the 1 st molar contacts the occlusal plane but the buccal cusp tips and the distal lingual cusp are elevated about .5mm off the occlusal plane (yellow line) . The Maxillary 1 st Molar
- 16. The Maxillary 2 nd Molar Setting the Maxillary Posterior Teeth The set up viewed in profile. Note that the mesial lingual cusp tip touches the plane of occlusion along with the buccal and lingual cusps of the premolars. The curve of Spee begins at the 1 st molar.
- 17. The Maxillary 2 nd Molar Setting the Maxillary Posterior Teeth The curve of Spee is continued by elevating the 2 nd molar off the plane of occlusion as shown. The 2 nd molar is elevated to an even greater degree than the 1 st molar, about 15 degrees in the average patient. When viewed from the distal it is set, like the 1 st molar, with a slight curve of Wilson. Occlusal plane
- 18. Setting the Mandibular Posterior Teeth Note that with this particular posterior tooth form, the mandibular cusps tips are designed to engage the embrasures of the opposing maxillary teeth. This true of almost all anatomic tooth forms designed for bilateral balance except the Ivoclar Ortholingual. Completed set up Centric
- 19. The Mandibular 1st Molar Setting the Mandibular Posterior Teeth Begin by positioning the mandibular 1 st molar. The mesial buccal cusp tip should engage the embrasure between the 1 st molar and 2 nd premolar. Therefore adjacent marginal ridges of the maxillary premolar and molar must be at the same level for the lower molar to properly engage them.
- 20. The Mandibular 1st Molar Setting the Mandibular Posterior Teeth Check the relationship from the lingual side. Make sure that the maxillary lingual cusp tips engage the the central fossa of the mandibular molar.
- 21. The Mandibular 1st Molar Setting the Mandibular Posterior Teeth Using a clear plastic ruler and the marks made on the cast check to insure that the 1 st molar is perfectly centered over the ridge. Make sure the central fossa of the molar is properly aligned over the ridge. If the central fossa is either buccal or lingual to the ridge make the appropriate adjustments. It is apparent that the molar is positioned too far to the buccal.
- 22. The Mandibular 1st Molar Setting the Mandibular Posterior Teeth Note the alignment of the central fossa.The molar is positioned too far to the buccal and should be moved towards to the lingual . If the remaining mandibular posterior teeth are arranged on this line the denture will be prone to tipping and its stability will be impaired. Line indicating the crest of the ridge After repositioning this tooth focus your attention on the maxillary posterior teeth and reposition them lingually so that the maxillary 1 st molar and 2 nd premolar properly occlude with the mandibular 1 st molar. Do not forget to move the 1 st premolar as well.
- 23. The Mandibular 1st Molar Setting the Mandibular Posterior Teeth The molar is twisted and positioned too far to the lingual. If the remaining posterior mandibular teeth are arranged along this line the space for the tongue will likely be insufficient. The molar must be moved slightly to the buccal and twisted clockwise so that the central fossa is parallel to the ridge line. Line indicating the crest of the ridge After repositioning this tooth the posterior maxillary teeth should be moved to the buccal so that they properly occlude with the mandibular molar and permit positioning the remaining mandibular posterior teeth over the ridge.
- 24. The Mandibular Premolars – Centric Setting the Mandibular Posterior Teeth Position the mandibular premolars. The buccal cusp of the 2 nd premolar should occlude with the the adjacent marginal ridges of the maxillary 1 st and 2 nd premolars.
- 25. The Mandibular Premolars – Centric Setting the Mandibular Posterior Teeth The buccal cusp of the mandibular 1 st premolar should engage the mesial marginal ridge of the opposing 1 st premolar. There should be a space between the 1 st premolar and the cuspid.
- 26. The Mandibular Premolars – Centric Setting the Mandibular Posterior Teeth Verify that the premolars are in solid centric occlusion. If lingual centric contacts are lacking, contacts in balancing position will be lacking.
- 27. The Mandibular Premolars – Working Setting the Mandibular Posterior Teeth When there is a lack of working side contacts at this stage of the setup check for the following discrepancies in the following order: Verify buccal centric Check for balancing interferences on the opposite side Slightly increase the curve of Wilson without compromising lingual centric
- 28. The Mandibular Premolars – Working Complete Denture Occlusion During the lateral excursion into working, with this cusp form, when the teeth are properly arranged, there should be no lingual cusp contacts between the maxillary and mandibular teeth.
- 29. The Mandibular Molars – Balancing Setting the Mandibular Posterior Teeth When you lack balancing side contacts at this stage of the setup, check for the following discrepancies in the following order. Verify lingual centric Check for working interferences on the opposite side
- 30. The Mandibular 2 nd Molar – Centric Setting the Posterior Mandibular Teeth Position the 2 nd molars in centric. Inappropriate positioning and angulation of the 2 nd molars can cause significant discrepancies in working, balancing and protrusive, and so you again must check the excursions carefully.
- 31. The Mandibular 2 nd Molar – Centric Setting the Mandibular Posterior Teeth Check lingual centric. Make sure that the lingual cusps of the maxillary 2 nd molar properly occludes with the central fossa of the mandibular 2 nd molar as shown.
- 32. Verify contacts in working excursions Setting the Mandibular Posterior Teeth Lack of working side contacts may be the result of: Poor buccal centric Insufficient curve of Wilson Working interferences in the 2 nd molar region Balancing interferences on the opposite side * Check these in the order cited .
- 33. Verify contacts in during balancing excursion Setting the Mandibular Posterior Teeth Lack of balancing side contacts may be the result of: Poor lingual centric Working interferences on the opposite side, particularly in the 2 nd molar region
- 34. The Central Incisors Setting the Mandibular Anterior Teeth Begin by setting the central incisors. The mesial surfaces should be on the midline.
- 35. Setting the Mandibular Central Incisors In most patients the labial surface of the mandibular incisors should be roughly perpendicular to the occlusal plane. Occlusal plane The Central Incisors
- 36. Determining the Amount of Vertical and Horizontal Overlap Setting the Mandibular Anterior Teeth The articulator is placed in the working and protrusive position, and the position of the central incisors adjusted to permit passive contact during lateral excursions. Working Protrusive
- 37. Setting the Mandibular Anterior Teeth Horizontal overlap This practice will idealize the amount of horizontal and vertical overlap and ensure that anterior guidance is not introduced into the setup. Horizontal overlap Vertical overlap
- 38. The Lateral Incisors and the Cuspids Setting the Mandibular Anterior Teeth Position the lateral incisors and cuspids in the same fashion as the central incisors. Take care not to introduce anterior guidance into the set up. The anterior teeth should be in only passive contact during lateral excursions. Working Protrusive
- 39. The Lateral Incisors and the Cuspids Setting the Mandibular Anterior Teeth Upon completion, the amount of vertical and horizontal overlap will be idealized and anterior guidance has not been introduced into the setup. Bilateral balance has been maintained.
- 40. Semi-anatomic Denture Teeth Check to ensure you have retained appropriate contacts in working, balancing and protrusive. Balancing Working Protrusive Completed set up Centric
- 41. Anatomic Denture Teeth (30 degree)
- 42. Anatomic Denture Teeth (30 degree) These teeth are arranged in the same fashion as the semi-anatomic teeth shown previously. Use the same sequence of steps as we have just shown.
- 43. Anatomic Denture Teeth (30 degree) Begin by positioning the appropriate protrusive insert, and check to ensure that the incisal guide pin is set at zero and in contact with the incisal guide table. Protrusive insert Protrusive Inserts Zero setting
- 44. Setting Anatomic Teeth (30 degree) When you are finished check to see that the posterior teeth are on plane and the posterior teeth centered over the mandibular ridge. Make corrections as necessary.
- 45. Setting Anatomic Teeth (30 degree) Check buccal and lingual centric.
- 46. Setting Anatomic Teeth (30 degree) Check to ensure you have retained appropriate contacts in working, balancing and protrusive. Balancing Protrusive Working
- 47. Trouble shooting Anatomic and Semi-anatomic Denture Teeth Lack of working side contacts Verify buccal centric. Restore centric contacts as necessary. Increase the curve of Wilson Eliminate any anterior guidance present on the working side. Check for balancing interferences on the opposite side and make adjustments as necessary.
- 48. Trouble shooting Anatomic and Semi-anatomic Denture Teeth Lack of balancing side contacts Verify lingual centric. Restore missing contacts as necessary. Eliminate any anterior guidance present on the opposite or working side. Check for working interferences on the opposite side particularly in the 2 nd molar region.
Most Viewed this Month
Sorry. No data so far.
New Lectures
Internal Links
- Maxillofacial Rehabilitation
- Oral Cancer Foundation
- Quintessence Publishing
- The Weintraub Center
Lecture Topics
- COMPLETE DENTURES
- FIXED PROSTHODONTICS
- IMPLANT DENTISTRY
- MAXILLOFACIAL PROSTHETICS
- REMOVABLE PARTIAL DENTURES
© 2024 Foundation for Oral-facial Rehabilitation. FFOFR is a tax-exempt public charity under 501 (3)(c)
- 汉语 – Lectures in Chinese
- Lectures in Spanish
- Sao Paulo, Brazil 2019
- Sponsorship

- Previous Article
- Next Article
Clinical Relevance
Introduction, methods and materials, conclusions, acknowledgments, effect of lateral excursive movements on the progression of abfraction lesions.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Guest Access
- Get Permissions
- Cite Icon Cite
- Search Site
I. D. Wood , A. S. A. Kassir , P. A. Brunton; Effect of Lateral Excursive Movements on the Progression of Abfraction Lesions. Oper Dent 1 May 2009; 34 (3): 273–279. doi: https://doi.org/10.2341/08-100
Download citation file:
- Ris (Zotero)
- Reference Manager
The results of this randomized controlled trial have direct relevance to clinical practice and provide some evidence that occlusal adjustment to prevent further progression of abfraction lesions cannot be supported currently.
The theory of abfraction suggests that tooth flexure arising from occlusal loads causes the formation and progression of abfraction lesions. The current study investigated whether reducing occlusal loading by adjusting the occlusion on a tooth during lateral excursive movements had any effect on the rate of progression of existing abfraction lesions. Recruited were 39 subjects who had two non-carious cervical lesions in the maxillary arch that did not need restoration and were in group function during lateral excursive movements of the mandible. One of the teeth was randomly selected to have the excursive occlusal contacts reduced by using a fine grain diamond bur. Centric occlusal contacts were not reduced. Impressions of the lesion were taken over a 30-month period to enable monitoring of the wear rate, and duplicate dies were poured into epoxy resin to allow for sectioning. The size of the lesions was measured using stereomicroscopic analysis of the sectioned epoxy resin dies, and the results were analyzed using an Independent t -test. No statistically significant difference in wear rates between the adjusted and non-adjusted teeth was found ( p >0.05).
Within the limitations of the current study, it was concluded that occlusal adjustment does not appear to halt the progression of non-carious cervical lesions; consequently, this procedure cannot be recommended.
As an aging population retains its teeth longer, the issue of tooth wear or non-carious tooth tissue loss is becoming increasingly important to the dental profession. The phrase “non-carious cervical tooth surface loss” has arisen in an attempt to embrace these kinds of lesions, which occur at the neck of the tooth. Unfortunately, far more confusion arises from the use of other terminologies, such as erosions and abrasions, which have been used at different times and in different locations to describe similar lesions.
In 1908, Black, in his seminal work on Operative Dentistry, discussed the problematic etiology of what he termed “erosions” and stated that, “Our information regarding erosion is far from complete and much time may elapse before its investigation will give satisfactory results.” 1 Black identified eight possible causes:
Faults in the formation of teeth
Friction from an abrasive toothpowder
Action of an unknown acid
Secretion of a diseased salivary gland
Physiological resorption, as with deciduous teeth
Acid associated with gouty diarethis
Action of alkaline fluids on calcium salts
Action of enzymes released by micro-organisms
After going through each hypothesis, in turn, finding fault with all, he concluded that he had no theory of his own to offer that did not have features that rendered it impossible.
Other researchers in the early part of the 20 th century also considered these lesions. Miller, in 1907, looked at “wastings” and concluded that brushing with coarse toothpowder was the likely cause. 2 In 1931, Ferrier was unable to find a reasonable explanation and, in 1932, Kornfeld made the observation that, in all cases of cervical erosion, he noticed heavy wear facets on the articulating surfaces of the teeth involved and that the erosion tended to be at the opposite side of the tooth to the wear facet. 3–4
The confusing use of the term erosion to describe a lesion that may actually be caused by mechanical abrasion is further compounded by the fact that, to a chemical engineer, the process described by dentists as erosion is known as corrosion. 5 Use of such imprecise terminology has contributed to both the difficulty of carrying out good quality research and making accurate diagnoses that enable appropriate treatments to be both recommended and provided.
Many practitioners have felt that over enthusiastic toothbrushing and the use of abrasive toothpastes were the primary causes of these lesions, but Lee and Eakle, in 1984, put forward the hypothesis that tensile stresses created in the tooth during occlusal loading may have a role in the etiology of cervical erosive lesions. 6 They described three types of stress placed on teeth during mastication and parafunction:
Compressive—the resistance to compression
Tensile—the resistance to stretching
Shearing—the resistance to twisting or sliding
The authors were of the opinion that, in a “non-ideal” occlusion, large lateral forces could be created that would result in compressive stresses on the side being loaded and tensile stresses on the opposite side. As enamel is strong in compression but weak in tension, it was suggested that those areas in tension were prone to failure. The region of greatest stress is found at the fulcrum of the tooth. The characteristic lesion described was wedge-shaped, with sharp line angles and was situated at or near the fulcrum of the tooth. It was suggested that the direction of the lateral force governed the position of the lesion, while its size was related to the amount of force and its duration.
Grippo put forward a new classification of hard tissue lesions of teeth. 7 He defined four categories of tooth wear as follows:
Attrition—the wearing away of tooth substance as a result of tooth-to-tooth contact during normal or parafunctional masticatory activity.
Abrasion—the pathological wear of tooth substance through biomechanical frictional processes, such as toothbrushing.
Erosion—the loss of tooth substance by acid dissolution of either an intrinsic or extrinsic origin; for example, gastric acid or dietary acids.
Abfraction—the pathologic loss of tooth substance caused by biomechanical loading forces. It was postulated that these lesions were caused by flexure of the tooth during loading, leading to fatigue of the enamel and dentin at a location away from the point of loading. The word “abfraction” was derived from the Latin “to break away.”
Grippo then further described five categories of abfraction:
Hairline cracks
Striations—horizontal bands of enamel breakdown
Saucer shaped—a lesion entirely within enamel
Semi-lunar shaped—a crescent shaped lesion entirely within enamel
Cusp tip invagination—a depression on the cusp tip seen in molars and premolars
By 1994, Lambert and Lindenmuth considered that the profession should now consider occlusal stress as a primary factor in the creation and progression of cervical notch lesions and a considerable body of theoretical work had accumulated to support this hypothesis. 8 A comprehensive review of abfraction lesions has recently been published, which concluded that the etiology of these lesions is multifactorial but that occlusal factors are a primary etiological factor. 9
This study investigated whether or not reducing excursive occlusal loading had any impact on the rate of progression of abfraction lesions in vivo . The test hypothesis (H t ) was that a reduction in lateral excursive loads would result in a reduction in the rate of abfraction lesion development. The null hypothesis (H o ) for this study was that there was no difference in the rate of abfraction lesion progression when excursive occlusal loads were reduced.
Subject Selection
Following ethical approval obtained from the local research ethics committee (Leeds East REC, Leeds, UK), 39 patients were recruited into the current study. They ranged in age from 18 through 75 years and had two abfraction lesions that did not require operative intervention. In addition, the test teeth had to be in group function during lateral excursive movements, with no mobility of the test or antagonist teeth being detectable clinically. In contrast, subjects were excluded from the study if:
The abfraction lesions were in teeth that had no antagonist
There was canine guidance in lateral excursion
There was more than 3 mm of pocketing
The teeth were mobile
There was poor oral hygiene
Other restorative treatment was required of the teeth included in the current study
The subject had poor general health
This study was designed as a randomized controlled trial, with each patient acting as his/her own control. In order to minimize operator bias, the tooth to be adjusted was allocated at random. This was achieved by recording each tooth according to FDI notation. For example, an upper right second premolar was recorded as 15 and an upper left first premolar as 24. Equal numbers of opaque envelopes were prepared with either the word “High” or “Low” in them. No identifying marks were present externally. The patient chose an envelope at random from within a box and opened it. If it contained the word “High,” then the tooth with the higher notation, for example, 24, as in the example above, was adjusted. Conversely, if the envelope contained the word “Low,” the tooth with the lower notation, that is, 15, was adjusted.
Operative Procedures
All subjects recently had full mouth examinations, including clinically appropriate radiographs and a periodontal screening, to check for attachment loss, gingival bleeding and mobility of the relevant teeth. The dynamic and static occlusal contacts of the test teeth were marked using red and blue Bausch 40 micron articulating paper (Dr Jean Bausch KG, Seefeld, Germany) respectively, after having dried the occlusal surfaces of the teeth with tissue held in Miller's forceps (Unodent, Witham, UK). The areas marked red were reduced using Hi-Di fine grain diamond finishing burs (Hi Di Burs, Dentsply, Weybridge, UK) in a water-cooled air turbine. Care was taken to leave the blue centric stops and the red point of maximum excursive contact intact to ensure occlusal stability. The adjusted area was lightly polished with Shofu abrasive cones (Shofu Dental GmbH, Ratingen, Germany) to reduce any surface roughness, and the occlusion was rechecked with articulating paper. Further adjustment, if required, was carried out as described above.
Full-arch impressions were taken using a polyether impression material (Impregum, 3M ESPE, Seefeld, Germany) in polycarboxylate disposable trays (Polytrays, Dentsply). The impressions were rinsed, disinfected and cast up immediately in blue die stone (Skillstone, Whip Mix Corporation, Louisville, KY, USA). The investigative procedures are summarized in Figure 1 .
Flow chart summarizing investigative procedures.
The subjects were followed-up at six, 18 and 30 months after baseline. At the follow-up appointments, routine full mouth examinations were carried out, along with appropriate radiographs and periodontal screening. The occlusion of the test teeth was marked again with red and blue articulating paper to check whether there had been any change. If the dynamic markings were heavy or if new dynamic markings were identified, these were adjusted as before and repolished. At each visit, impressions were also taken as described previously.
Model Analysis
To minimize operator error in the processing and measuring of the models, all the models were measured at the same time. In order to keep the original models intact, the test teeth were duplicated using a polyvinylsiloxane putty and wash (Provil Novo, Heraeus Kulzer GmbH, Hanau, Germany) and replica dies were cast in epoxy resin (Exacto-Form Model Resin, Bredent, Senden, Germany). Three points were marked on each model ( Figure 2 ) as follows:
Tip of the cusp
Midpoint of the lesion in the long axis of the tooth
Soft tissues along the same axis
A scalpel blade was used to make the marks, as it is thinner than a pencil.
The models were then sectioned using a low-speed sectioning machine (Model 650, South Bay Technology Inc, San Clemente, CA, USA) with a water-cooled diamond wheel saw (76.2 x 0.4 mm, Saint Gobian Abrasive, Gloucester, UK) according to the sectioning plan. The two sides were labeled A and B. This enabled both sides of the slice to be measured in order to provide an average value for the size of the lesion. The sections were then ready to be measured ( Figure 3 ).
Abfraction Area Measurement
The sections were washed under running water to remove any debris from the sectioning process. They were then examined by light-reflecting microscopy using a stereomicroscope (Type S Wild M3Z, Wild Heerburgg, Heerburgg, Switzerland) at 10× magnification. Each section was fixed to a glass slide and positioned under the microscope in such a way that the entire cross section of the abfraction area could be viewed and examined at right angles to the microscope lens. Live images from the microscope were transferred to a computer (Dell Latitude D510, Dell, Inc, Round Rock, TX, USA) by a built-in digital video camera (PEC 3010, Pulmix, Basingstoke, England). A digital micrograph was obtained from each section. The abfraction area measurement was carried out using image analysis with SigmaScan Software (SigmaScan Pro 5.0.0, Aspire Software International, Leesburg, VA, USA). The software counts the number of pixels enclosed within a defined boundary. In order to do this, the operator must define those boundaries around the lesion using a mouse and pointer on the computer screen. To minimize potential error, sequential lesions were measured at the same time, and two readings were taken from each side of the sample in an effort to get consistent values. The mean of the two measurements of abfraction area from each section was calculated. The mean of the two measurements from side A and side B was then worked out and recorded. In order to blind the operator, no means of identifying which tooth had been adjusted was made available at the time of analysis.
Data Analysis
Data was input into SPSS and the results were analyzed with a paired-samples t -test with the level of significance set at 0.05.
In total, 39 subjects were recruited into the study. They ranged in age from 35 years to 70 years, with a mean of 51 years and 3 months, sd ± 9.1 years. Two subjects failed to return and one patient was eliminated from the study because one of the test teeth sustained a cusp fracture and had to be restored. The distribution of the lesions is summarized in Table 1 . The abfraction area from models for five patients could not be measured for several reasons; therefore, data were obtained from a total number of 31 patients.
Distribution of Lesions
Statistical analysis revealed that there was no statistically significant difference between the rate of lesion progression for teeth that had been adjusted and those that had not at the six-, 18- and 30-month reviews ( p =0.510, p =0.682 and p =0.669, respectively). The results of the current study are summarized in Tables 2 and 3 . The test hypothesis that, reducing the occlusal load in lateral excursion would reduce the rate of progression of abfraction lesions, was therefore rejected.
Change in Mean Values of Area of Abfraction Lesions From Baseline
Change in Area of Abfraction Lesions in Square Millimeters From Baseline: Distribution of Lesions
The current study primarily investigated the hypothesis that reducing excursive occlusal loads on a tooth in lateral excursion would lead to a reduction in the rate of progression of abfraction lesions. The study was carried out in a primary care setting, in this case, a predominantly private general dental practice, with most of the subjects regularly attending the practice. It is often stated that, “real world research will lead to real world findings.” It was envisioned that, carrying out research in practice would make it easier to follow patients over a longer period of time than it is in a hospital setting, let alone test the feasibility of using this intervention in primary dental care to produce findings of clinical application in everyday practice. The relatively low dropout rate in this study is generally supportive of this principal.
The age range of the patients recruited, 31 to 70, with an average age of 51, tends to support the findings of Levitch and others, namely, that the prevalence of abfraction lesions increases with age. 10 In contrast to the findings of Pegoraro, no paired lesions were identified in patients under the age of 30. 11 That is not to say that lesions were not present in small numbers, but, if they were, they may not have been in group function in lateral excursion, which would have excluded them from the study. 11
The data in Table 1 is not, of course, strictly an accurate indicator of lesion distribution, as the mouths of the subjects were examined from the right side first, when initially screened, and, if lesions were identified in that quadrant, the left side was not included in the study. The data does, however, give some indication of the spread between premolar and molar lesions, which is slightly at variance with reports by Pegoraro and others and Radentz and others, which found maxillary molars to be the most frequently affected teeth. 11–12 It is, of course, possible that this slightly different distribution, when compared with the published literature, has arisen, because only teeth that were in group function during lateral excursion were eligible for inclusion in the current study.
During the recruitment period, it was interesting to note how many lesions were seen that were ineligible for inclusion, because they were either not in group function in lateral excursion or not at all in occlusion. Several patients had classic wedge-shaped lesions on teeth that had never been in occlusion, for example, anterior open bites caused by skeletal discrepancies, which would indicate that occlusal forces could have played no part in their etiology. This calls into question Kornfeld's observation that all teeth with cervical erosions had heavy occlusal wear facets and similarly throws into doubt Lee and Eakle's theory about the possible role of tensile stress in the etiology of NCCL. 4 , 6 It does, however, tend to support the theory that, not only abfraction lesions are multifactorial in etiology, but that clinically identical lesions may have different etiologies. Much like Black, the authors of the current study still do not have an explanation that satisfactorily explains the etiology of all these lesions without having some feature that renders it impossible. 1
Within the design of the current study, the centric occlusal stop and the stop in the position of maximum excursion were both maintained to prevent occlusal instability. These markings were checked at each review appointment and adjusted, if necessary.
It was noted that some patients had re-established full sliding contacts by the review visit, requiring further occlusal adjustment. This would have had the effect of reintroducing occlusal stresses into their lateral excursive movements and lessening the effect of adjustments done in the current study. This might explain the results obtained from the current study. As the centric stop was maintained in all cases of distortion under vertical loading, for example, barreling effects, as described by Goel and others, would still be active, so that the influence of occlusal forces cannot be ruled out completely. 13 It is possible that reducing the occlusal loads in lateral excursion by re-establishing canine guidance as suggested by Murray and others would be a more effective intervention. 14
A further factor not taken into account by the current study was the restorative condition of the teeth being monitored. It has been established by Rees that the presence of occlusal restorations in lower pre-molars significantly increases the cervical area stresses that occur during excursive loading, and it is not unreasonable to assume that the same effect would be found in maxillary teeth and could have had an influence on wear rates. 15
It was interesting to note that both sets of lesions continued to increase in size. This indicates that the measuring technique was subtle and effective enough to detect small changes and illustrates the progressive nature of the lesions being measured. As adjusting the excursive occlusal load did not affect the rate of progression, other factors, such as toothbrush abrasion and or acid erosion, may be contributing to this wear. Further research is still needed to improve diagnosis and allow for differentiation between the different etiologies, which may result in the formation clinically of very similar lesions, let alone allow for the investigation of interventions designed to stop the formation and progression of abfraction lesions.
Within the limitations of the current study, the results do not support removal of lateral excursive contacts by occlusal adjustment to reduce the rate of progression of abfraction lesions in maxillary teeth.
This study was sponsored by the Department of Health, Manchester, UK and was presented at the 35 th Annual Meeting and Exhibition of the AADR, the 30 th Annual Meeting of the CADR and the 83 rd Annual Meeting and Exhibition of ADEA, Orlando, Florida, March 8–11, 2006.
Author notes
Ian David Wood, general dental practitioner, Sale, Cheshire, UK
Ali Sabet Abbas Kassir, research fellow, Department of Fixed and Removable Prosthodontics, Leeds Dental Institute, Leeds, UK
Paul Anthony Brunton, professor and head of department, Department of Fixed and Removable Prosthodontics, Leeds Dental Institute, Leeds, UK
Recipient(s) will receive an email with a link to 'Effect of Lateral Excursive Movements on the Progression of Abfraction Lesions' and will not need an account to access the content.
Subject: Effect of Lateral Excursive Movements on the Progression of Abfraction Lesions
(Optional message may have a maximum of 1000 characters.)
Citing articles via
Get email alerts.

- About This Journal
- Permissions
- eISSN 1559-2863
- ISSN 0361-7734
- Privacy Policy
- Get Adobe Acrobat Reader
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Pocket Dentistry
Fastest clinical dentistry insight engine.
- Dental Hygiene
- Dental Materials
- Dental Nursing and Assisting
- Dental Technology
- Endodontics
- Esthetic Dentristry
- General Dentistry
- Implantology
- Operative Dentistry
- Oral and Maxillofacial Pathology
- Oral and Maxillofacial Radiology
- Oral and Maxillofacial Surgery
- Orthodontics
- Pedodontics
- Periodontics
- Prosthodontics
- Gold Member
- Terms and Condition
Occlusion, the Periodontium and Soft Tissues
The term “fremitus” describes tooth mobility when occlusal contacts are performed. It may either be observed visually or felt through the examiner’s fingertips, or both. It may occur when the patient closes into the intercuspal or retruded positions, or during excursions of the mandible.
Occlusal factors may be important in the aetiology of increased mobility, but there are often other reasons. These are considered in the following section. Where the occlusion interacts with these factors, it may worsen or prevent resolution of the mobility. An increased mobility associated primarily to occlusal overload is relatively uncommon, but it can mystify the unwary dentist, particularly when it affects multiple teeth.
Non-occlusally Related Causes for Tooth Hypermobility
The commonest cause of increased tooth mobility is inflammatory periodontal disease. All clinicians are aware that teeth tighten after successful periodontal treatment, but increased mobility can persist after the inflammation has been eliminated. Characteristically, radiographs of affected teeth show reduced alveolar support, but a normal periodontal ligament space. This is simply an amplification of physiological mobility (Fig 5-1) because of long clinical crown height and short attachment. Despite the apparent increased mobility, such teeth do not require occlusal treatment if not subject to occlusal interference.
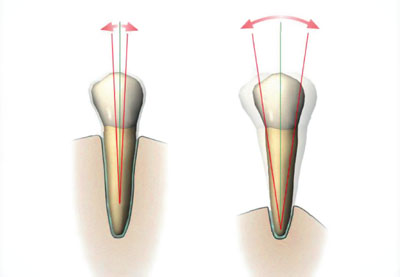
Fig 5-1 Although the tooth on the right is more mobile than the tooth on the left, the periodontal ligament is healthy and not widened. The increased mobility at the level of the occlusal plane is simply related to the longer clinical crown.
Only if the patient has discomfort from excessively hypermobile teeth during function, or if the mobility is increasing, might splinting be beneficial.
Other non-occlusal causes of increased mobility include:
root resorption
loss of periradicular bone support, for example due to periradicular inflammation or after apical surgery
recent trauma causing subluxation
fractured root
hormonal, occurring occasionally during pregnancy.
Occlusally Related Causes for Tooth Hypermobility
Habits such as bruxism can subject the teeth to loads which are higher and longer lasting than during normal function. This may, for poorly understood reasons, result in the periodontium adapting to the increased loads, rather than the neuromuscular system limiting load generation, as might be expected. Teeth with normal bone levels and normal attachment can still become hypermobile under such circumstances, with the response regarded as a physiological reaction to the mechanical insult. This is sometimes called “primary occlusal trauma”. Characteristically, the periodontal ligament becomes widened (Figs 5-2 and 5-3).
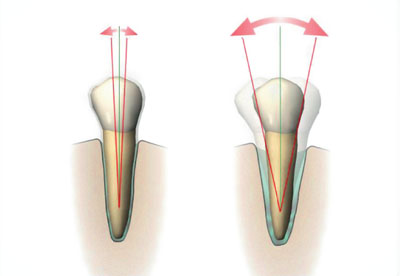
Fig 5-2 The tooth on the right shows the physiological response to a higher than normal occlusal force; its periodontal ligament has become widened (primary occlusal trauma).

Fig 5-3 A premolar with a widened periodontal ligament space. This is periodontal ligament widening, caused in this case by abnormal loading from a denture clasp.

Of course, teeth with a reduced but healthy periodontal support may undergo an increase in existing hypermobility if subjected to direct or indirect occlusal trauma. This is sometimes called “secondary occlusal trauma”. This terminology is not useful because the response to both primary and secondary occlusal trauma simply represents a normal physiological adaptation of the periodontium to increased occlusal loading.
A thorough clinical and radiographic examination will enable the cause of hypermobility to be identified. Increasing mobility is an important clinical symptom and sign to look out for. It can indicate an occlusal discrepancy which will benefit from correction.
In addition to conventional periodontal therapy, management of hypermobility caused by occlusal factors should be directed at:
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:
- Occlusion and Fixed Osseointegrated Implant Restorations
- The Intercuspal Position and Dentistry
- Normal Function and Avoiding Damage to Restored Teeth
- Deflective Contacts, Interferences and Parafunction
- Occlusion and Temporomandibular Disorders
- Occlusal Techniques
Stay updated, free dental videos. Join our Telegram channel
Comments are closed for this page.

VIDEdental - Online dental courses

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Dent Res Dent Clin Dent Prospects
- v.2(3); Summer 2008
Pattern of Occlusal Contacts in Eccentric Mandibular Positions in Dental Students
Fereidoun parnia.
1 Assistant Professor, Department of Prosthodontics, Faculty of Dentistry, Tabriz University of Medical Sciences, Tabriz, Iran
Elnaz Moslehi Fard
Katayoun sadr, negar motiagheny.
2 Post-graduate student, Department of Anesthesiology, Faculty of Medicine, Tabriz University of Medical Science, Tabriz, Iran
Background and aims
This study observed occlusal contacts and their area on the teeth during lateral mandibular movements. The percentage of each occlusal pattern was determined.
Materials and methods
Fifty subjects (male: 27, female: 23), aged 20-29 years, were included in the study. The criteria for selection were as follow: all subjects (i) were in their twenties; (ii) had normal occlusal alignment, no temporomandibular signs and symptoms with Angle’s Class I relationship; (iii) had full dentition except for third molars; (iv) had no history of orthodontic therapy; and (v) had no restorations involving a cusp. The occlusal contacts were recorded with occlusion foil in three lateral excursions: 1, 2 and 3 mm from the maximum intercuspation. Data were analyzed with chi-square test.
Most of working-side contact patterns were classified as group function (60%). Canine protection was rare (17%). Contact patterns other than canine protection and group function were found in 23% of the contact patterns on the right side. On the left side, group function was seen in 51%, canine protection in 21% and others patterns in 28% of the studied subjects.
On laterotrusion, most subjects had group function on the working side but canine protection was rare.
Introduction
The collective arrangement of the teeth in function is quite important and has been subjected to a great deal of analysis and discussion over the years. As the mandible moves laterally, the lower posterior teeth leave their centric contact with the upper teeth and travel sideways down a path dictated by the condyles in the back and by the lateral anterior guidance in the front. In the diversified literature on occlusion and its role for functional patterns of the masticatory system, 1 two concepts stand out: (1) Canine protection as described by D’Amico 2 is said to favor a vertical chewing pattern and to prevent wear of teeth, as in lateral occlusion where the canine guides the mandibular movement directly through contact or indirectly through periodontal receptors. (2) Group function as described by Beyron 3 following his observations on Australian Aborigines implies contact and stress on several teeth in lateral occlusion and indicates abrasion as a positive and inevitable adjustment.
The reason for bringing any teeth into lateral function is to distribute stress and wear over more teeth. Group function occlusion, which is also commonly known as unilateral balanced occlusion, is a widely accepted and used method of tooth arrangement in restorative dental procedures today. The group function of the teeth on the working side distributes the occlusal load. The obvious advantage is the maintenance of the occlusion. In group function occlusion, the contacting inclines must be perfectly harmonized to border movements of the condyles and the anterior guidance. Kleinberg 4 has pointed out the importance of the feedback mechanism between mechanoreceptors in the temporomandibular joint and the functional mandibular movement pattern.
In addition, a probable change in the input signals from the periodontal receptors after occlusal adjustment seems to affect the functional movement of the mandible. 4 Ingervall 5 recorded tooth contact patterns in laterotrusion, protrusion of the mandible, and in the retruded position in young men with varying types of occlusion. On protrusion, most subjects had contacts only on anterior teeth. Protrusive contacts were rare only on posterior teeth. On laterotrusion, most subjects had group function on the functional side. Contact on the nonfunctional side was found in half of the subjects in a 1.5-mm laterotrusive position and in one third of them in a 3-mm laterotrusive position. No correlation between the types of tooth contacts and mandibular dysfunction was found. 5 Yaffe & Ehrlich 6 recorded the dynamic contact pattern of teeth in lateral glide movement in 72 individuals, 19 to 35 years of age, with normal tooth alignment and Angle’s Class I molar and canine relationship. The lateral glide movement was divided into three stages to simulate the total range of events in lateral glide movement naturally demonstrated by the patient. This study has shown that lateral glide movement is a complex movement in which the nature of tooth contact is altering in location, direction, and number of teeth participating. Consequently the restoration of an occlusion in accordance with a given concept does not always apply to all patients. 6 The present study was designed to evaluate the incidence of occlusal patterns in a group of dental students.
Materials and Methods
Fifty subjects (male: 27, female: 23) aged 20–29 years (mean, 24.1 years) were included in the study. They were selected from a group of 225 undergraduate students of the Faculty of Dentistry, Tabriz University of Medical Sciences. The Research and Ethics Committee approved the study protocol and informed consent was obtained from the subjects after they were provided an explanation of the general nature of the study. The criteria for selection were as follow: all subjects (i) were in their twenties; (ii) had normal occlusal alignment, no temporomandibluar signs and symptoms with Angle’s Class I relationship; (iii) had full dentition except for third molars; (iv) had no history of orthodontic therapy; and (v) had no restorations involving a cusp.
The occlusal contacts were recorded with occlusion foil (8 μm thick, Occlusions Pruf-Folie, GHM, Germany) in three lateral excursions, after laterally sliding the mandibular incisal point on both sides, 1, 2 and 3 mm from the maximum intercuspation (MI). When recording the occlusal contacts, each patient was instructed to close in the intercuspal position and to slide the mandible laterally to the right and left side performing the three lateral excursive movements designed as lateral 1 (1 mm from MI), lateral 2 (2 mm from MI), and lateral 3 (3 mm from MI) on each side. Each subject was required to sit upright in a dental chair with the Frankfort plane almost horizontal. The subject’s head was not fixed. To control lateral position, marks were made on the upper central incisors with a sharp black water-resistant pencil from the mandibular midline. Three lines were marked on the maxillary incisor. In case of deviation of mandibular midline, a reference line was traced at the labial surface of the mandibular incisor in the intercuspal position to serve as a guide for the measurement. The blue occlusion foil was placed on the occlusal surface of the left-side most posterior mandibular molar, and the subject was requested to close his/her mandible to the MI. While a constant pulling force was maintained on the occlusion foil, red occlusion foil was put and the subject was requested to perform gliding movement to the right with the teeth in light contact. When the subject’s mandible moved 1 mm right from the intercuspal position, the presence or absence of an occlusal contact was examined. Only the red marks on teeth were considered to indicate occlusal contact. To prevent movement with mandibular opening or movement without occlusal contact and lateral-protrusive excursion, the movement was observed closely, and occasionally the subject was instructed to correct the movement. The movement was performed by the subject without any help from the examiner. When the subject could not perform the movement voluntarily, he or she was asked to practice with the use of a hand mirror. The examination was continued from the left-side most posterior molar to the left-side central incisor sequentially. For examination of the molars, the occlusion foil was placed on both the mesial and distal sides of the occlusal surface. The same procedure was performed for the 1, 2 and 3 mm right positions and also for the 1, 2 and 3 mm left positions. In addition, the working-side occlusal contacts were recorded in the same manner. All recordings were performed by the same examiner and were repeated. In the case of differing results, the existence of occlusal contact was re-examined and verified. All recordings were made between 10 o’clock in the morning and 4 o’clock in the afternoon to avoid possible diurnal variations. 7
Working-side occlusal contact patterns were determined for the total range of lateral positions and classified into three groups: canine protection, group function or others (occlusal patterns other than those described). Canine protection was defined as the contact of only working-side maxillary and mandibular canines in the total range of lateral positions from 1 to 3 mm. Group function was defined as the contacts of two or more working-side teeth in at least one lateral position, and/or as single tooth contacts on the working-side in different lateral positions, e.g. the contact of only first molars in the 1 mm position followed by the contact of only canines in the 2 and 3 mm positions. The others type was identified when a contact pattern other than those described above was observed, e.g. contact of only first premolars throughout the lateral positions or contact patterns with no working-side contacts. Data were analyzed with SPSS 15 statistical software. The differences between patterns were evaluated using chi-square test.
Figure 1 shows the number of working occlusal contacts recorded for each dental unit on right and left sides. The contact frequencies varied with the lateral position and with the tooth type. The working-side occlusal contacts were mostly on the first premolar in R1 (right 1 mm) followed by canine; but in L1 (left 1 mm), the percentage of contacts on canine and first premolar were the same. The frequency of contact on premolars decreased gradually from the 1 to 3 on both sides. In all lateral positions, the frequency of contact decreased from the canine to the first molar as the tooth type became located posteriorly. However, the contact on the first molar almost was as prevalent as that on the second premolar. The frequency of the working-side canine contact increased from the 1 to the 3 mm position.

Figure 2 presents the number of non-working occlusal contacts recorded for each dental unit on right and left sides. The non-working-side contacts primarily involved the first and second molars, most frequently the second molar. The prevalence of non-working-side contacts decreased as the mandible moved from the 1 to 3 mm position on the premolars and molars.

Table 1 shows the percentage of occlusal patterns in mandibular lateral movement on the right and left sides. Most of working-side contact patterns were classified as group function (60%); canine protection was rare (17.3%), and contact patterns other than canine protection and group function were found in 23.7% of the contact patterns on the right side. On the left side, group function was found in 51.3%, canine protection in 20.7% and others in 28% of the contact patterns. Most of the subjects (66%) had the same pattern on both sides: 42% group function, 8% canine protection, and 16% others.
This study demonstrated that the occlusal contact pattern during lateral movement differs between 1 mm, 2 mm and 3 mm. In the position close to the maximum intercuspation, canine protection was seen to be the lowest.
The occlusal contact pattern varying with lateral positions should be a critical factor on diagnosis and treatment of occlusal disharmonies. The marked difference in the pattern of occlusal contacts between the 1, 2 and 3 mm positions, suggests that the contact pattern in the 1 mm position reflects a pattern of occlusal contact distinct from that commonly observed during lateral excursion.
In a study analyzing two working-side inter-occlusal contacts, a large number of subjects presented unclassified patterns of articulations. 8 More individuals had canine guidance on the left side, whereas the most frequent pattern on the right side was group function. 8 Another study on occlusal contact areas using a 3-D digitization measurement system found that, at intercuspal position, estimated occlusal contact areas were 12.6 mm 2 . 9 However, after 3.0 mm of lateral excursion, their areas were sharply reduced to 2.2 mm 2 .
Ogawa et al 10 - 12 found most contact patterns belonged to group function and a few to canine protection. They also found the presence of occlusal contacts in different lateral positions may have different effects on biomechanics of the related teeth. For instance, the force on individual teeth may be more traumatic in the more lateral positions because of the increased vector of the force. Occlusal force is transmitted to the teeth during four functional and parafunctional stages: mastication, swallowing, clenching and grinding. The occlusal contact during mastication and swallowing is suggested to occur mainly in lateral positions close to the MI, i.e. within 1 mm of the MI. 10 - 1 In addition, forces during these two functional movements are relatively low and their durations are short. Taking into consideration these various factors, the biomechanical significance of non-working-side occlusal contact may increase over the non-functional range of lateral movement corresponding to the 3 mm position. In the present study, incidence of non-working-side occlusal contact decreased from 1 to 3 mm; so it does not seem appropriate to deduce that contact in this position produces harmful force to the teeth or periodontal structures. However, this does not exclude the possibility that the non-working-side contacts in the position close to the MI may be important in masticatory function. 13
Most of working-side contact patterns were classified as group function. Canine protection was rare. Contact patterns other than canine protection and group function were found in 23% of the contact patterns on the right side. On the left side, group function was seen in 51%, canine protection in 21% and others patterns in 28% of the studied subjects. On laterotrusion, most subjects had group function on the working side but canine protection was rare.
- TheFreeDictionary
- Word / Article
- Starts with
- Free toolbar & extensions
- Word of the Day
- Free content
ex·cur·sion
- active assistive range of motion
- Acute Alcohol Intoxication
- aortocoronary bypass
- balancing side condyle
- Bennett movement
- Bilirubin and Bilirubin Fractions
- brain wave cycle
- breathing pattern, ineffective
- breathing-related sleep disorder
- clasp-knife rigidity
- clasp-knife spasticity
- Coagulation Factors
- concomitance
- coronary artery bypass
- exclusive provider organization
- exclusivity
- exclusivity period
- exconjugant
- excoriation
- excrementitious
- excrescence
- excrescency
- excretion urography
- excretory duct
- excretory duct of seminal gland
- excretory ducts of lacrimal gland
- excretory ductule of lacrimal gland
- excretory gland
- excretory organ
- excretory urography
- exculpatory
- excurvation
- excuse of infancy
- excycloduction
- excyclophoria
- excyclotropia
- excyclovergence
- excystation
- execution wound
- executive committee
- executive function
- executive information system
- executive letter
- Executive Monkey
- executive profile
- exemplar site
- exempt research
- exenatide acetate
- exencephalia
- exencephalic
- exculpating
- exculpation
- exculpations
- exculpatorily
- exculpatory clause
- Exculpatory evidence
- Excuria Recovery Services, LLC
- Excursion Inlet Seaplane Base
- Excursion Limit
- Excursion liner
- Excursion Maximum
- Excursion of Suspension
- excursion rate
- excursion steamer
- excursion ticket
- Excursion train
- Excursion trains
- excursionise
- excursionism
- excursionist
- excursionists
- excursionize
- Excursions Maritimes Tropéziennes
- excursively
- excursiveness
- Facebook Share
- More from M-W
- To save this word, you'll need to log in. Log In
Definition of excursion
Did you know.
In Latin, the prefix ex- means "out of" and the verb currere means "to run." When the two are put together, they form the verb excurrere , literally "to run out" or "to extend." Excurrere gave rise not only to excursion but also to excurrent (an adjective for things having channels or currents that run outward) and excursus (meaning "an appendix or digression that contains further exposition of some point or topic"). Other words deriving from currere include corridor , curriculum , and among newer words, parkour .
Examples of excursion in a Sentence
These examples are programmatically compiled from various online sources to illustrate current usage of the word 'excursion.' Any opinions expressed in the examples do not represent those of Merriam-Webster or its editors. Send us feedback about these examples.
Word History
Latin excursion-, excursio , from excurrere
circa 1587, in the meaning defined at sense 1a
Theme music by Joshua Stamper ©2006 New Jerusalem Music/ASCAP
Get Word of the Day delivered to your inbox!
Dictionary Entries Near excursion
excursional
Cite this Entry
“Excursion.” Merriam-Webster.com Dictionary , Merriam-Webster, https://www.merriam-webster.com/dictionary/excursion. Accessed 29 Apr. 2024.
Kids Definition
Kids definition of excursion.
from Latin excursio, excursion- "a going out," from excurrere "to run out, make an excursion, extend," from ex- "out, forth" and currere "to run" — related to current
Medical Definition
Medical definition of excursion, more from merriam-webster on excursion.
Nglish: Translation of excursion for Spanish Speakers
Britannica English: Translation of excursion for Arabic Speakers
Subscribe to America's largest dictionary and get thousands more definitions and advanced search—ad free!

Can you solve 4 words at once?
Word of the day.
See Definitions and Examples »
Get Word of the Day daily email!
Popular in Grammar & Usage
More commonly misspelled words, commonly misspelled words, how to use em dashes (—), en dashes (–) , and hyphens (-), absent letters that are heard anyway, how to use accents and diacritical marks, popular in wordplay, the words of the week - apr. 26, 9 superb owl words, 'gaslighting,' 'woke,' 'democracy,' and other top lookups, fan favorites: your most liked words of the day 2023, 10 words for lesser-known games and sports, games & quizzes.

English focus texts
- Phantom heads (Dental manikins)
- Bewegungsablauf
- Exkursionsbewegung
Want to give it a try ...
... or need professional advice? Get in touch with us or click Contact .
Word of the day
Focus text of the month.
- Folge uns auf
- google plus

IMAGES
VIDEO
COMMENTS
Lateral excursion is the second key step when we chew our food. Once the mouth opens and the food enters the oral cavity, the jaw moves sideways and grinds the food, closes gradually and finally the teeth meet each other before the mouth comes back in a state of rest. Lateral excursion might be hampered due to problems in the gnathic system.
Occlusion is an integral part of dental treatment as dentists cannot repair, move or remove teeth without affecting occlusion. 1. The masticatory system comprises the teeth, the periodontal tissues and the articulatory system. The articulatory system is in itself a triumvirate comprising the temporomandibular joint (TMJ), muscles of mastication ...
Dynamic occlusion: lateral excursion The dynamic occlusion is the contact that teeth make during movements of the mandible - when the jaw moves side to side, forward, backward or at an angle. In dynamic occlusion, the contacts of the teeth are not points as in static occlusion, but they are described with lines. ...
A demonstration of the lateral excursion and an explanation of when and why lateral excursion adjustment is necessary. Orig. air date: AUG 14 74This is part...
Occlusion (dentistry) Occlusion, in a dental context, means simply the contact between teeth. More technically, it is the relationship between the maxillary (upper) and mandibular (lower) teeth when they approach each other, as occurs during chewing or at rest. Static occlusion refers to contact between teeth when the jaw is closed and ...
Canine guidance - this means during lateral excursion of the mandible the canines are the teeth which guide the mandibles movement and the last to disclude ; Group function - this means during lateral excursion of the mandible, the tooth contact which guides the movement is shared between multiple teeth on the working side.
Occlusion is determined by a patient's articulatory system. Like traditional systems, it relies on motors, hinges and contacts - or muscles, the TMJ and tooth-to-tooth contact. 2. 1. Tooth ...
Occlusion is the static relationship between the incising or masticating surfaces. of the maxillary or mandibular teeth or tooth. 5 It is a static position, as the. mandible is not moving. On the ...
Occlusal Adjustment and Occlusal Equilibration. Occlusal adjustment is the alteration of the occlusal surfaces of teeth by the dentist to change the relationship of occlusal contacts. Although often used synonymously, it should be differentiated from occlusal equilibration, which is the planned alteration of occlusal surfaces to provide stable ...
excursions (WS) ¾ Non-working Side - side of the mandible that moves towards the midline during lateral excursion (NWS) ¾ Interferences - tooth contact that hinders ...
Occlusion can be very simply defined: it means the contacts between teeth. Before describing the significance of the different ways in which occlusal contacts are made Occlusion needs to be put into context. The Masticatory (or stomatognathic) System (Fig. 1.1) is generally considered to be made up of three parts:
Excursion can occur in either direction, and anatomists use directional terms to specify the type of excursion. When the mandible moves to either the left or right, it's moving away from the body's midline, so it's called lateral excursion. When the mandible moves closer to the midline of the body, it's called medial excursion.
There are three main concepts regarding tooth contact during the lateral excursion of mandibular movement: (1) balanced occlusion, which was developed from the work of Bonwill, 3 (2) canine guidance, described by D'Amico, 4 and (3) group function, as discussed by Beyron. 5. The relationship between static and dynamic occlusion is one of the ...
Similarly, if the overbite is incomplete, there may be a considerable delay during excursions before the anterior teeth come into contact. Rather more difficult to comprehend is the effect of the occlusal plane. On the one hand, a flat occlusal plane with a shallow angle to the horizontal plane - the patient's Frankfort plane - will ...
A 'non working side interference' is an anterior guidance on the back teeth on the non working side during lateral excursion. The working side is the side of the mandible towards which the ...
We wish to insure that all the posterior teeth as well as the anterior teeth maintain contact in lateral excursions. To ensure bilateral balance we place an anterior-posterior curve in the arch, called a compensating curve, which is analogous to the curve of Spee in natural dentition. In addition , we place a curve from side to side, the so ...
The current study primarily investigated the hypothesis that reducing excursive occlusal loads on a tooth in lateral excursion would lead to a reduction in the rate of progression of abfraction lesions. The study was carried out in a primary care setting, in this case, a predominantly private general dental practice, with most of the subjects ...
Occlusion, the Periodontium and Soft Tissues. The term "fremitus" describes tooth mobility when occlusal contacts are performed. It may either be observed visually or felt through the examiner's fingertips, or both. It may occur when the patient closes into the intercuspal or retruded positions, or during excursions of the mandible.
Group function is a contact pattern on two or more working side teeth throughout lateral excursion. The only problem with these definitions is the absence of a description for the position of mandible. ... In light of the given definition, canine guided and group function appears to imply an ideal therapeutic occlusion and is not a usable ...
Only the red marks on teeth were considered to indicate occlusal contact. To prevent movement with mandibular opening or movement without occlusal contact and lateral-protrusive excursion, the movement was observed closely, and occasionally the subject was instructed to correct the movement.
excursion. [ ek-skur´zhun] a range of movement regularly repeated in performance of a function, e.g., excursion of the jaws in mastication. adj., adj excur´sive. lateral excursion sideward movement of the mandible between the position of closure and the position in which cusps of opposing teeth are in vertical proximity.
excursion: [noun] a going out or forth : expedition. a usually brief pleasure trip. a trip at special reduced rates.
Definition from Glossary 1: a movement outward and back or from a mean position or axis; also, the distance traversed 2: in dentistry, the movement occurring when the mandible moves away from maximum intercuspation